New concept of orthosis treatment for knee osteoarthritis: Clinical and radiological outcomes
Abstract
BACKGROUND:
Given the increasing numbers of young patients with knee osteoarthritis there is a need for treatments that can postpone a joint prosthesis (total knee replacement).
OBJECTIVE:
As an alternative to the effective yet invasive knee joint distraction procedure, a knee orthosis was developed aiming to unload the affected knee and improving synovial fluid flow. The aim of this study was to examine the effectiveness of using a load-reducing orthosis for two months on functioning, pain, and disease progression (e.g. amount of damaged cartilage) in patients with symptomatic osteoarthritis of the knee for at least one year.
METHODS:
This is an interventional single-center pilot study. Ten patients with symptomatic osteoarthritis of one knee (5 males/5 females; median age 57; age range 42–59) used a custom-made orthosis for 60 days during daily life activities that involved knee loading (e.g. standing, walking, but not during stair climbing). Cycling was not allowed. Clinical outcomes were assessed up to 24 months after intervention at 6 timepoints using patient reported-outcome measures Western Ontario and McMaster Universities Osteoarthritis (WOMAC) range 0–100; Visual Analogue Scale (VAS), range 0–100 for pain. Minimum joint space width (mJSW) was assessed using knee images digital analysis (KIDA) and articular cartilage volume with magnetic resonance imaging (MRI) using custom software at baseline and at 12 and 24 months follow-up.
RESULTS:
Clinically beneficial effects were found for functioning (WOMAC improvement compared to baseline ranged between 18 points at 3 months follow-up and 31 points at 12 months follow-up, with only the 24-months follow-up (improvement of 27 points) not reaching statistical significance (
CONCLUSION:
This study demonstrates that use of a custom-made knee-unloading orthosis for 60 days can result in improved functional ability and decrease in pain in relatively young patients with knee osteoarthritis. No effect on disease progression could be evidenced.
1.Introduction
Knee osteoarthritis (OA) is the most common joint disorder [1]. The lifetime risk of developing symptomatic knee OA is estimated at around 45% [2, 3]. If conservative treatment fails, total knee replacement (TKR) is a highly effective procedure that provides reliable relief from pain and improved physical function with a high level of patient satisfaction [4, 5]. The number of knee replacement operations is increasing yearly. Over 40% of all knee replacements and up to 44% of all total knee revisions are performed in patients under 65 [6]. The known limited lifespan of TKR and the high-demand expectation of a prosthesis from relatively young patients with knee OA together with the increasing number of TKRs constitute costly healthcare [7, 8]. Hence development of alternative treatments for knee OA, specifically those that can postpone a prosthesis is needed. If the primary TKR of a patient can be postponed to a period of life that patients are less demanding, it might give more patient satisfaction after TKR and less revisions of TKR resulting in reducing healthcare costs [9].
Knee joint distraction (KJD) is a promising development that has emerged as a joint-preserving treatment for endstage osteoarthritis [10]. Recent studies suggest that KJD can reverse cartilage tissue structure damage in severe knee OA while yielding significant clinical improvement [11, 12]. This newly formed cartilage-like tissue is stable and mechanically effective to the extent that the joint space width (JSW) increases at radiographic examination [13, 14].
KJD is an invasive surgical intervention that involves placement of an external fixation frame over the patient’s knee for 6–8 weeks. Disadvantages besides two surgical procedures are pin-tract infections, short-term stiffness with muscle atrophy after the distraction period, and possible major psychological burden as it hinders patients during sleep and makes personal hygiene more difficult [15].
To avoid the drawbacks and aiming to keep the benefits of KJD, an orthosis was developed that maintains the conditions thought of as being favorable for cartilage repair: unloading the affected knee during loading activities and maintaining synovial fluid flow by leg flexion and extension, which gives good natural joint homeostasis and might release chondroprotective molecules/Mesenchymal stem cells [16].
The orthosis unloads the knee, although not 100%, since the passive muscle tone and knee capsule are still present and will keep loading the knee. The orthosis allows the knee to flex normally, hoping to give a natural synovial fluid flow. We hypothesize that this orthosis will also result in reduced symptoms and regeneration of cartilage in an osteoarthritic knee joint. Primary objective of this pilot study is to examine the effectiveness of using a load-reducing orthosis for two months on functioning in patients with knee OA. Secondary objective is to examine the effect of using a load-reducing orthosis for two months on pain and disease progression (e.g. amount of damaged cartilage).
2.Materials and methods
2.1Study design
This is an interventional pilot study conducted in a single center in the Netherlands. The study was approved by the regional medical ethics committee in Leeuwarden (in Dutch: Regionale Toetsingscommissie Patiëntgebonden Onderzoek, RTPO no. 982), and registered in the Dutch Trial registry (NTR 6556, registered 4 July 2017; https://onderzoekmetmensen.nl/en/trial/23870).
2.2Study participants
Eligible patients were recruited by two orthopedic surgeons. Inclusion criteria were ages 25–60, primary symptomatic unilateral OA in the tibiofemoral joint for at least one year, and OA severity moderate to severe (Kellgren and Lawrence 2 or higher) but below the level required for joint replacement or arthrodesis. Exclusion criteria were symptomatic OA in both knees, generalized OA (genetic), mechanical axis deviations
Table 1
Individual baseline characteristics of the ten participating patients
| No. | Gender (male/female) | Affected side (left/right) | Age (years) | BMI (kg/m2) | Most affected compartment (medial/lateral) | KL (1–4) |
|---|---|---|---|---|---|---|
| 1 | M | L | 59 | 26 | Lateral | 2 |
| 2 | F | R | 56 | 21 | Medial | 3 |
| 3 | F | L | 58 | 28 | Medial | 4 |
| 4 | M | L | 42 | 27 | Medial | 4 |
| 5 | M | R | 51 | 30 | Lateral | 3 |
| 6 | F | R | 55 | 30 | Medial | 4 |
| 7 | F | L | 58 | 24 | Medial | 3 |
| 8 | M | R | 53 | 23 | Medial | 3 |
| 9 | M | R | 59 | 26 | Medial | 4 |
| 10 | F | L | 59 | 24 | Medial | 3 |
| Ratio | 5/5 | 5/5 | ||||
| Median (IQR) | 57.0 (6.5) | 26.3 (5.0) |
KL, Kellgren Lawrence grade (1–4, higher score indicates more arthrosis).
Baseline characteristics of the ten participating patients are presented in Table 1. Patients (5 males; 5 females) ranged between ages 42 and 59, and 80% had medial compartment OA. Except for patient 1, all patients were classified with Kellgren and Lawrence grade 3 or 4.
2.3Intervention
Figure 1.
Example of the custom-made orthosis worn by a patient.

One orthosis was produced for each patient, the orthosis was modified to match the geometry of every participant. The orthosis design was inspired by upper-leg prosthetics and fixed to the body via an adapted upper-leg socket such as known from upper-leg prosthetics (Fig. 1). The bottom of the socket was removed to allow the upper leg to pass. The body weight is transferred to the orthosis via a combination of tuberosity support, friction to the skin and leg volume containment. In this way the weight is transferred directly to the floor by the orthosis, bypassing and unloading the knee and the ankle – so the patient stands on the orthosis, not on the foot. Another important feature of the orthosis is to preserve movement of the knee joint for maintaining synovial fluid flow and thus nutrition of the cartilage. The lower-leg part of the orthosis is therefore connected to the upper-leg part by two hinges (medial and lateral). The hinges are essentially aligned with the knee joint. The lower leg is not fixed directly to the lower-leg part of the orthosis, but to an extra set of bars that is fixed to the lower-leg part under an angle when the orthosis is in full extension. This prevents the lower leg to reach full extension and thus will avoid that the joint surfaces come into direct contact, which for a healthy knee is the mechanism to stabilise the joint during heel strike. To prevent pelvic tilt, the patient wears a sole that is fixed under the shoe of the other leg. The sole increases the height of the shoe and prevents any leg length discrepancy caused by using the orthosis.
Patients were given permission to take the orthosis at home and use it after a supervised training session, during the 60 days study period without further supervision. To ensure full unloading of the knee joint during the intervention period, patients used the orthosis every day for 60 days during all activities that comprised knee loading (e.g. standing, walking). Cycling could be complex with the orthosis, so it was not allowed. Also stair climbing could be complex, so it is done without orthosis and with crutches. At night in bed, or while sitting for a longer period where no loading of the knee was required, the orthosis could be removed. The orthosis was also removed when showering, with patients using an external support to remain stable and not load the knee. To compare the orthosis with Knee Joint Distraction (KJD) treatment, the same duration of 2 month (60 days) intervention was chosen [13]. After the intervention period patients were instructed to use physical therapy to retain muscle strength, stability, and mobility.
2.4Outcomes
2.4.1Patient-reported outcomes
The primary outcome to assess clinical improvement is the Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index. This patient-reported outcome measure is an osteoarthritis-specific questionnaire for pain, stiffness, and functioning with a score range for the total and subscales between 0 and 100, where a higher score indicates fewer symptoms [17]. A secondary clinical outcome measure is the Visual Analogue Scale (VAS) for pain [18, 19] (range 0–100, higher score indicating more pain). Last, a 4-point Likert scale was used as clinical outcome measure of patient satisfaction with the treatment results.
2.4.2Imaging
Magnetic resonance imaging (MRI) acquisition was performed with a 1.5 T Philips Achieva dStream, with a dStream Knee 16ch coil using a 3D spoiled gradient recalled (T1 FFE) sequence with fat suppression (repetition time 19 ms; echo time 9 ms; flip angle 15 degrees; slice thickness 1.5 mm; in-plane resolution 0.3125
2.4.3Experiences with the orthosis
Patients kept a daily log about their experiences during the intervention period. Skin-related problems due to use of the orthosis or other problems related to wearing the orthosis were registered.
2.4.4Adverse events
Participants’ charts were screened for complications during the 24-month study period.
2.5Follow-up
Both WOMAC and VAS were assessed at six timepoints: at baseline (pre-intervention), and at 3-, 6-, 12-, 18-, and 24-months follow-up. Patient satisfaction was obtained once, at final follow-up (24 months). MRI and standardized X-rays were performed at baseline and at 12- and 24-months follow-up.
2.6Data analysis
Descriptive statistics were used to present the data, considering the small sample size using medians and interquartile ranges (IQR), with minimum and maximal ranges. Frequencies and percentages were used to present categorical data. A Wilcoxon signed rank test was used to analyze differences between two timepoints. Data was analyzed using IBM SPSS (version 25.0), and a
3.Results
3.1Patient-reported outcomes
Figure 2 presents the clinical outcome scores. WOMAC total and WOMAC function scores after 3 months and at 6, 12, and 18 months are statistically significantly higher than baseline. For the subscales pain and stiffness, scores at 6, 12, and 18 months are significantly higher than baseline. VAS pain score decreased compared to baseline; at all timepoints the score was significantly lower than baseline. Compared to the median VAS pain score of 69 at baseline, a reduction in pain score between 41 and 56 points was found at the follow-up timepoints. For WOMAC total score absolute differences on the follow-up timepoints compared to baseline (median score 58) were 18, 27, 31, 26, and 27, respectively. At 24 months eight patients were satisfied/very satisfied with the result of the treatment. Two patients were unsatisfied/very unsatisfied.
3.2Imaging
Table 2
Results of the MRI analysis and KIDA X-ray of the MAC (most affected compartment)
| Baseline | 1-year follow-up | 2-year follow-up | ||||
|---|---|---|---|---|---|---|
| MRI ThCtAB (mm) | 1.2 (0.5), (0.7–2.3) | 1.1 (0.5), (0.6–2.3) | 1.0 (0.4), (0.6–2.2) | 0.007* | 0.005* | 0.047* |
| MRI dABp (%) | 20.3 (21.2), (0.7–64.0) | 23.2 (23.6), (0.9–65.8) | 25.1 (23.3), (1.0–64.4) | 0.005* | 0.005* | 0.169 |
| MRI ThCcAB (mm) | 1.5 (0.4), (1.4–2.3) | 1.4 (0.4), (1.2–2.3) | 1.4 (0.4), (1.2–2.2) | 0.009* | 0.005* | 0.028* |
| MRI VC (mm3) | 1418 (913), (856–2719) | 1287 (876), (695–2718) | 1220 (773), (765–2586) | 0.005* | 0.005* | 0.022* |
| KIDA mJSW (mm) | 0.0 (1.2), (0.0–4.3) | 0.1 (0.4), (0.0–4.7) | 0.0 (0.8), (0.0–4.7) | 0.574 | 0.441 | 0.256 |
Presented are: median (IQR), (min-max),
Figure 2.
Upper graph: median WOMAC score and VAS pain score in time for the 10 patients. Lower graph: median WOMAC scores per subscale in time for the 10 patients.
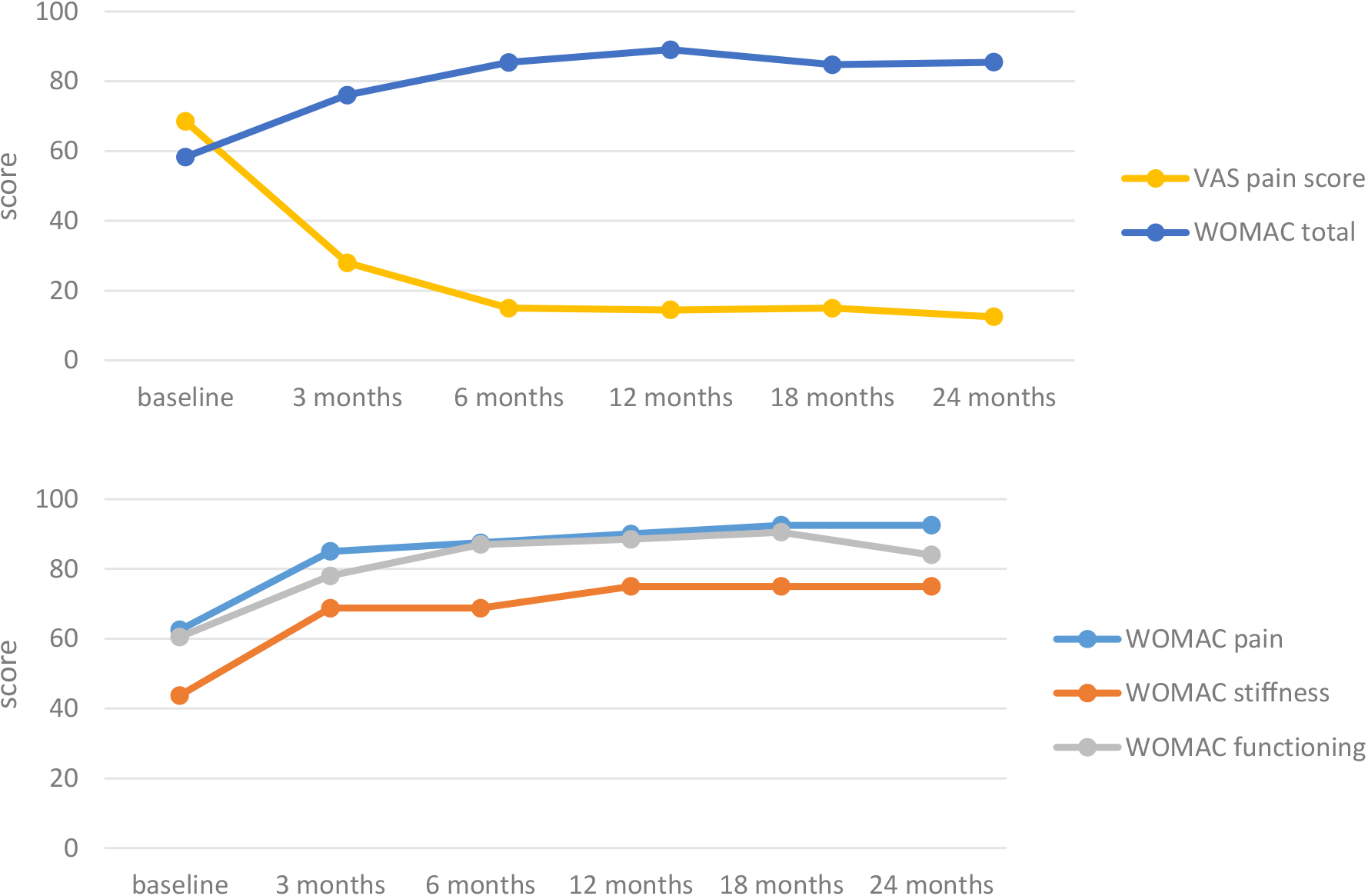
Table 2 presents the MRI and KIDA X-rays results. All MRI cartilage parameters show a significant worsening at 1- and 2-years follow-up compared to baseline. Between the 2-year and 1-year timepoints a significant worsening was found on all parameters, except for the percentage of subchondral bone area that was denuded. Median mJSW based on the KIDA X-rays was zero at each timepoints. No significant difference between timepoints was found on this outcome.
3.3Experiences with the orthosis
Patients registered during the intervention period had several problems and difficulties with the orthosis. Overall, the period was experienced as physically and mentally taxing. The main problem was friction of the orthosis, leading to irritated skin and superficial wounds. Patients indicated that after a few weeks the orthosis became too loose and had to be adjusted, because of the reduction in muscle tissue (atrophy). They documented several technical problems like stuck hinges, broken Velcro, and loosened screws. Patients also documented having back pain or a painful contralateral side because of the change in load and gait.
At the six-months follow-up timepoint 6 out of 10 patients indicated having some kind of physical therapy, at 12-months follow-up this was still the case in 4 patients.
3.4Adverse events
Regarding complications obtained from the charts, approximately one year after the intervention period one patient (patient 4) had a painful cyst in the affected knee that was surgically removed with no residual complaints. Two patients (9 and 10) – who both indicated being unsatisfied/very unsatisfied with the treatment result – were on the waiting list for a partial knee replacement because of persistent complaints at the time of the last study follow-up.
3.5Summary of results
This study aimed to investigate the effectiveness of using a custom-made orthosis in young patients (age
4.Discussion
The current study had a comparable design as that of Wiegant et al. [13], who investigated the effectiveness of knee joint distraction as a joint-preserving procedure in young patients with endstage knee OA. Theirs, as well as other knee-joint distraction studies [12], demonstrated clinical improvement as well as cartilage repair post-surgery lasting at least 2 years. In the current study using the same outcome measures – WOMAC and VAS pain – a similar pattern of a quick clinical improvement was observed already at 3 months, reaching a plateau at 6 months that was sustained until 18 months for the WOMAC score and 24 months for the VAS pain score. For both outcome measures the improvement found in scores exceeds the minimal clinically important differences and can therefore considered as clinically relevant [25, 26]. These findings are in agreement with and reflected by the self-perceived satisfaction scores obtained at 24-months follow-up, where 80% of patients indicated being satisfied/very satisfied with the treatment results. Despite these similar clinical findings, we found no improvements on cartilage parameters, probably as a result of the substantially different nature of the two interventions [27].
Literature on the effectiveness of knee-unloading braces suggests that the custom-made orthosis under investigation is more in line with these types of braces than with knee joint-distraction surgery. A review from 2016 concluded that even though use of an unloading brace results in both pain and functional improvement, similarly to the current findings, biomechanical evidence does not demonstrate a beneficial effect on disease progression [28]. Beck et al. [27] recently provided some new evidence by studying the effect of bracing on damaged cartilage using enhanced MRI (dGEMERIC) mapping, demonstrating not only a clinical effect (reduction in pain and functioning) but also some positive effects on biomechanical properties of the damaged cartilage in patients with unicompartmental knee OA and varus or valgus malalignment. At 3-months follow-up beneficial effects were found in amount of collagen, proteoglycan concentration, and cartilage edema. But in agreement with the current study no positive effects could be evidenced in T1-dGEMERIC and T2* relaxation times, thickness, or extent of damaged cartilage area [27]. Considering the working mechanisms of orthoses and braces, these similar findings are perhaps unsurprising. Where the orthosis in our study was largely designed to unload the entire knee joint, knee-unloading braces aim to minimize compressive forces on the affected knee joint compartment too, by applying an external force to the joint that distracts the stress from the affected compartment [28].
An explanation for the discrepancy between clinical and radiological outcomes in this study is that the clinical outcomes are all patient-reported and might therefore be subject to a placebo effect. Similarly to what was found in knee-unloading studies, where discomfort like skin irritation and poor brace fit is common [28], resulting in low compliance [29] and a low likelihood of continued use of the brace after 1–2 years (28% and 25% regular use) [30], the intervention was experienced as intensive, given the use of the custom-made orthosis for 60 days during all knee-loading activities. In the current trial patients only needed to wear the orthosis during one 60-day period, and all patients who agreed to participate sustained this period, even though it was experienced as hard and demanding, physically as well as mentally. This probably reflects patients’ belief in the potential of the treatment, giving credibility to the suggestion of the presence of a placebo effect. Another explanation for the improvement in symptoms, with the cartilage parameters showing the natural worsening course of the OA, is that after six months 60% of patients indicated having physical therapy (under the supervision of a physical therapist) after the intervention period. They all had muscle atrophy to a certain degree – the orthosis had to be adjusted at least once during the intervention period for becoming too wide – and needed to regain their strength, coordination, and gait. This rehabilitation period with physical therapy, which continued at least until the 12-month follow-up timepoint in 40% of patients, may have resulted in a reduction of symptoms, considering the high-quality evidence that pain and physical functioning in patients with knee OA can be improved by exercise and weight loss [31].
Even though this study has it strengths in that it aimed to investigate the effectiveness of a relatively non-invasive knee orthosis, with a design similar to a previous study [13] to make comparison possible, several limitations need to be discussed. First, the lack of a control group: without a control group there is no direct insight into the natural course of clinical and radiological outcomes of a similar patient group during the study period, or into the use of another treatment like physical therapy under therapist supervision as primary intervention. Another limitation is the relatively short follow-up period of 24 months. Even though this is comparable to other studies on knee joint distraction [32, 33], it would be interesting to investigate the effectiveness at longer follow-up. A third limitation is that it is unknown how much load on the knee remained when using the knee unloading orthosis, as a result of that in-vivo load measurements are not possible. Last, there is our small group of participating patients, with no a priori sample size calculation conducted beforehand, as it was a pilot study. The reduced number of patients has risks resulting in a low power, with a higher chance of a type-II error – which means the inability to demonstrate a significant effect, when there is in fact a difference in timepoints or between groups. This does not seem to be an issue in the current study, since several significant differences were found on clinical as well as MRI parameters.
5.Conclusions
This study demonstrates that using a custom-made knee-unloading orthosis for two months can lower pain and improve functional ability in relatively young patients (
Ethics statement
All methods were carried out in accordance with relevant guidelines and regulations. The RTPO medical ethics committee in Leeuwarden approved the study protocol (RTPO 982). All participants provided signed informed consent before participation.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
This work was supported by the Martini Research Fund, the D.H. Heijne foundation, and the Gratama foundation (grant number 2018/012). These funding sources had no involvement in the study design, data collection, analysis, data interpretation, or writing of the report, nor in the decision to submit the article for publication.
Author contributions
MRH performed patient inclusion and data interpretation, and drafted and submitted the manuscript. AJdV coordinated the study; conducted data collection, statistical analysis, and data interpretation; and reviewed the manuscript. GJV initiated the study, designed the orthosis under investigation, and reviewed the manuscript. RWB designed the study, performed patient inclusion, and reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgments
The authors thank M.J. de Ronde and J.M. Hut-de Jong for their help in the data collection for this clinical trial. They also wish to acknowledge the help of M. Klein with the appropriate MRI settings and for providing the required information on the data analysis of the MRI subsection. They likewise thank E.E.G Hekman for his contribution to the design of the orthosis.
Conflict of interest
GJV designed the orthosis under investigation. None of the other authors have any conflict of interest to report.
References
[1] | Felson DT. Epidemiology of hip and knee osteoarthritis. 1. Epidemiol Rev. (1988) ; 10: (1): 1-28. |
[2] | Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM, et al. Osteoarthritis: New insights. Part 1: The disease and its risk factors. Ann Intern Med. (2000) Oct 17; 133: (8): 635-646. |
[3] | Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum. (2008) Sep 15; 59: (9): 1207-1213. |
[4] | Lützner J, Kasten P, Günther K, Kirschner S. Surgical options for patients with osteoarthritis of the knee. Nat Rev Rheumatol. (2009) Jun; 5: (6): 309-316. |
[5] | Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, et al. Health-related quality of life after knee replacement. J Bone Joint Surg Am. (1998) Feb; 80: (2): 163-173. |
[6] | Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. (2009) Oct; 467: (10): 2606-2612. |
[7] | Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, et al. Cost-effectiveness of total knee arthroplasty in the United States: Patient risk and hospital volume. Arch Intern Med. (2009) Jun 22; 169: (12): 1113-2. |
[8] | Bitton R. The economic burden of osteoarthritis. Am J Manag Care. (2009) Sep; 15: (8 Suppl): 230. |
[9] | van der Woude, J A D, Nair SC, Custers RJH, van Laar JM, Kuchuck NO, Lafeber, F P J G, et al. Knee joint distraction compared to total knee arthroplasty for treatment of end stage osteoarthritis: Simulating long-term outcomes and cost-effectiveness. PLoS One. (2016) May 12; 11: (5): e0155524. |
[10] | Jansen MP, Mastbergen SC. Joint distraction for osteoarthritis: Clinical evidence and molecular mechanisms. Nat Rev Rheumatol. (2022) Jan; 18: (1): 35-46. |
[11] | Intema F, Thomas TP, Anderson DD, Elkins JM, Brown TD, Amendola A, et al. Subchondral bone remodeling is related to clinical improvement after joint distraction in the treatment of ankle osteoarthritis. Osteoarthritis Cartilage. (2011) Jun; 19: (6): 668-675. |
[12] | Jansen MP, Boymans, Tim AEJ, Custers RJH, Van Geenen, Rutger CI, Van Heerwaarden RJ, Huizinga MR, et al. Knee joint distraction as treatment for osteoarthritis results in clinical and structural benefit: A systematic review and meta-analysis of the limited number of studies and patients available. Cartilage. (2021) Dec; 13: (1_suppl): 1113S-1123S. |
[13] | Wiegant K, van Roermund PM, Intema F, Cotofana S, Eckstein F, Mastbergen SC, et al. Sustained clinical and structural benefit after joint distraction in the treatment of severe knee osteoarthritis. Osteoarthritis Cartilage. (2013) Nov; 21: (11): 1660-1667. |
[14] | Jansen MP, Mastbergen SC, MacKay JW, Turmezei TD, Lafeber F. Knee joint distraction results in MRI cartilage thickness increase up to 10 years after treatment. Rheumatology (Oxford). (2022) Mar 2; 61: (3): 974-982. |
[15] | Takahashi T, Baboolal TG, Lamb J, Hamilton TW, Pandit HG. Is Knee Joint Distraction a Viable Treatment Option for Knee OA?-A Literature Review and Meta-Analysis. J Knee Surg. (2019) Aug; 32: (8): 788-795. |
[16] | Itthipanichpong T, Farooqi A, Menta SV, Ranawat AS. Joint distraction for the treatment of knee osteoarthritis. Journal of Cartilage & Joint Preservation. (2023) ; 100107. |
[17] | Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. (1988) Dec; 15: (12): 1833-1840. |
[18] | Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med. (2001) Dec; 8: (12): 1153-1157. |
[19] | Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. (1978) Aug; 37: (4): 378-381. |
[20] | Eckstein F, Ateshian G, Burgkart R, Burstein D, Cicuttini F, Dardzinski B, et al. Proposal for a nomenclature for magnetic resonance imaging based measures of articular cartilage in osteoarthritis. Osteoarthritis Cartilage. (2006) Oct; 14: (10): 974-983. |
[21] | Burgkart R, Glaser C, Hyhlik-Dürr A, Englmeier KH, Reiser M, Eckstein F. Magnetic resonance imaging-based assessment of cartilage loss in severe osteoarthritis: Accuracy, precision, and diagnostic value. Arthritis Rheum. (2001) Sep; 44: (9): 2072-2077. |
[22] | Graichen H, von Eisenhart-Rothe R, Vogl T, Englmeier K, Eckstein F. Quantitative assessment of cartilage status in osteoarthritis by quantitative magnetic resonance imaging: Technical validation for use in analysis of cartilage volume and further morphologic parameters. Arthritis Rheum. (2004) Mar; 50: (3): 811-816. |
[23] | Eckstein F, Buck RJ, Burstein D, Charles HC, Crim J, Hudelmaier M, et al. Precision of 3.0 Tesla quantitative magnetic resonance imaging of cartilage morphology in a multicentre clinical trial. Ann Rheum Dis. (2008) Dec; 67: (12): 1683-1688. |
[24] | Marijnissen ACA, Vincken KL, Vos, P A J M, Saris DBF, Viergever MA, Bijlsma JWJ, et al. Knee Images Digital Analysis (KIDA): A novel method to quantify individual radiographic features of knee osteoarthritis in detail. Osteoarthritis Cartilage. (2008) Feb; 16: (2): 234-243. |
[25] | Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS. How much pain is significant? Defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty. J Arthroplasty. (2018) Jul; 33: (7S): S71-S75.e2. |
[26] | Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. What is the Minimum Clinically Important Difference for the WOMAC Index After TKA? Clin Orthop Relat Res. (2018) Oct; 476: (10): 2005-2014. |
[27] | Beck S, Dittrich F, Busch A, Jäger M, Theysohn JM, Lazik-Palm A, et al. Unloader bracing in osteoarthritis of the knee – Is there a direct effect on the damaged cartilage? Knee. (2023) Jan; 40: : 16-23. |
[28] | Steadman JR, Briggs KK, Pomeroy SM, Wijdicks CA. Current state of unloading braces for knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. (2016) Jan; 24: (1): 42-50. |
[29] | Brouwer RW, van Raaij TM, Verhaar JAN, Coene LNJEM, Bierma-Zeinstra SMA. Brace treatment for osteoarthritis of the knee: A prospective randomized multi-centre trial. Osteoarthritis and Cartilage. (2006) ; 14: (8): 777-783. |
[30] | Squyer E, Stamper DL, Hamilton DT, Sabin JA, Leopold SS. Unloader knee braces for osteoarthritis: Do patients actually wear them? Clin Orthop Relat Res. (2013) Jun; 471: (6): 1982-1991. |
[31] | Jamtvedt G, Dahm KT, Christie A, Moe RH, Haavardsholm E, Holm I, et al. Physical therapy interventions for patients with osteoarthritis of the knee: An overview of systematic reviews. Phys Ther. (2008) Jan; 88: (1): 123-136. |
[32] | Jansen MP, Besselink NJ, van Heerwaarden RJ, Custers RJH, Emans PJ, Spruijt S, et al. Knee joint distraction compared with high tibial osteotomy and total knee arthroplasty: Two-year clinical, radiographic, and biochemical marker outcomes of two randomized controlled trials. Cartilage. (2021) Apr; 12: (2): 181-191. |
[33] | van der Woude JAD, Wiegant K, van Heerwaarden RJ, Spruijt S, van Roermund PM, Custers RJH, et al. Knee joint distraction compared with high tibial osteotomy: A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. (2017) Mar; 25: (3): 876-886. |




