Effects of body orientation and direction of movement on a knee joint angle reproduction test in healthy subjects: An experimental study
Abstract
BACKGROUND:
Joint position sense test assess patient mobility and proprioceptive ability. Yet, application used under different conditions may biases reproduction error resulting in different therapeutic consequences.
OBJECTIVE:
To investigate knee angle reproduction test under different test conditions.
METHODS:
25 healthy subjects (mean
RESULTS:
Absolute mean knee angle reproduction error showed significant difference for body position and vibration (Position: 95% CI 0.71 to 2.32;
CONCLUSION:
Body orientation and movement direction influence the resulting knee angle reproduction error in healthy subjects. Practitioners are advised to use standardised test procedures when comparing different within- and between-patient results.
Trial registration: DOI 10.17605/OSF.IO/AFWRP.
1.Introduction
The return to sports of an athlete after injury is a multifaceted and often challenging decision [1, 2, 3, 4], made daily by clinicians, physiotherapists, and coaches [5, 6]. One important criterion is the state of the proprioceptive feedback mechanisms, which are required to determine an adequate movement pattern [7, 8, 9, 10]. Accurate proprioception is a determinant of knee stability and plays a major role in daily activities, exercises, and sports [11]. Proprioception has been shown to be particularly reduced after anterior cruciate ligament (ACL) injuries [12, 7, 13]. The ACL is a key component of knee stability. Clinical evidence suggests that proprioceptive deficits exist in posture after anterior cruciate ligament reconstruction [14, 15, 16, 17, 18]. In their systematic review and meta-analysis, Flemming et al. indicated that proprioceptive feedback is still compromised 6–24 months following surgical treatment [19]. Thus, damage to the ACL may impair the ability to reproduce joint angles [20]. Reproducing knee angles as one parameter of correct knee functioning relies on a variety of different mechanoreceptors and muscle spindles as the main sources of information [7, 21, 22]. Ruffini end organ-like receptors and Golgi tendon receptors enable an adequate joint position sense, that is, the perception of relative muscle and joint position during movement [23]. Injury or surgery of the anterior cruciate ligament strongly affects mechanoreceptor function and negatively affects knee function, including lower extremity neuromuscular activation [18, 24, 25]. As adequate knee angle reproduction relies on continuous neuromuscular activation, deficient proprioceptive feedback with poor joint position sense can result in reduced knee angle reproduction [8]. Therefore, the sense of individual joint position seems to be a crucial parameter for a safe return to activity. However, the mechanism underlying joint position sense during adequate functional posture has not been completely elucidated [26, 7]. Moreover, it is associated with fatigue and can therefore be used to predict injury risk resulting from a delayed neuronal response [26]. Since joint position sense could provide key information to reduce the risk of injury and improve surgical outcomes [26, 27], the assessment of joint position sense in physiotherapeutic practice may lead to a safer return to activity after injury. Further, proprioceptive exercise can reduce pain and stiffness after ACL injury [28]. A major restriction in orthopaedic-physiotherapeutic practice is the current inconsistency in proprioception measurements in knee angle reproduction testing [23, 8]. As the mechanoreceptor activation pattern depends on body orientation and movement direction, we hypothesised that variations in test procedures can lead to different therapeutic consequences. Comparison of previous studies remains difficult due to heterogeneity in study protocols, equipment, and testing positions [29]. Therefore, the aim of the present study was to investigate the knee angle reproduction test as a measurement of joint position sense under varying test conditions, such as different body orientations and movement directions.
2.Methods
A clinical randomised trial with blinded outcome assessors was undertaken for two consecutive days. The study was done in accordance with the ethical standards of the Committee on Human Experimentation of the institution in which the experiments were done and in accordance with the Declaration of Helsinki of 1964 and its later amendments or comparable ethical standards. The study was approved by the Institutional Ethics Board of the Sports University Cologne (152/2019). The experimental design was preregistered on ‘Open Science Framework’ (DOI 10.17605/OSF.IO/AFWRP). Participants were recruited through voluntary participation. Consenting participants were allocated using a stratified random allocation sequence to three different test conditions (direction: ex
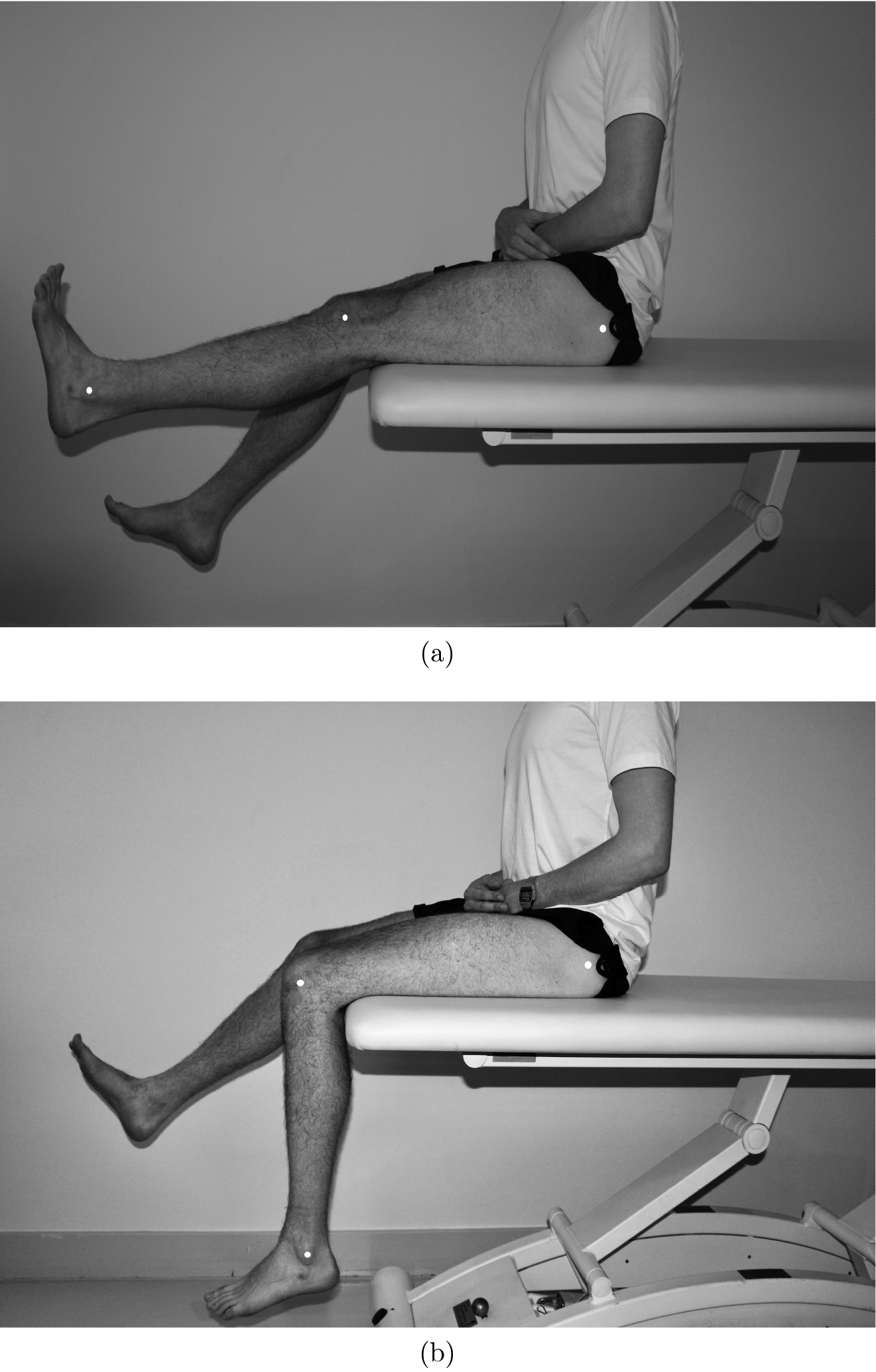
Figure 1.
Knee angle reproduction test: a sitting, starting from extension; b sitting, starting from flexion.
2.1Intervention
Prior to testing, participants were familiarised with the study protocol via standardised verbal instructions. To preclude general angle reproduction disabilities, reproduction errors were tested on an elbow angle reproduction test in advance. Participants were asked to reproduce 90
Figure 2.
Knee angle reproduction test: a prone position, starting from flexion, b prone position, starting from extension.
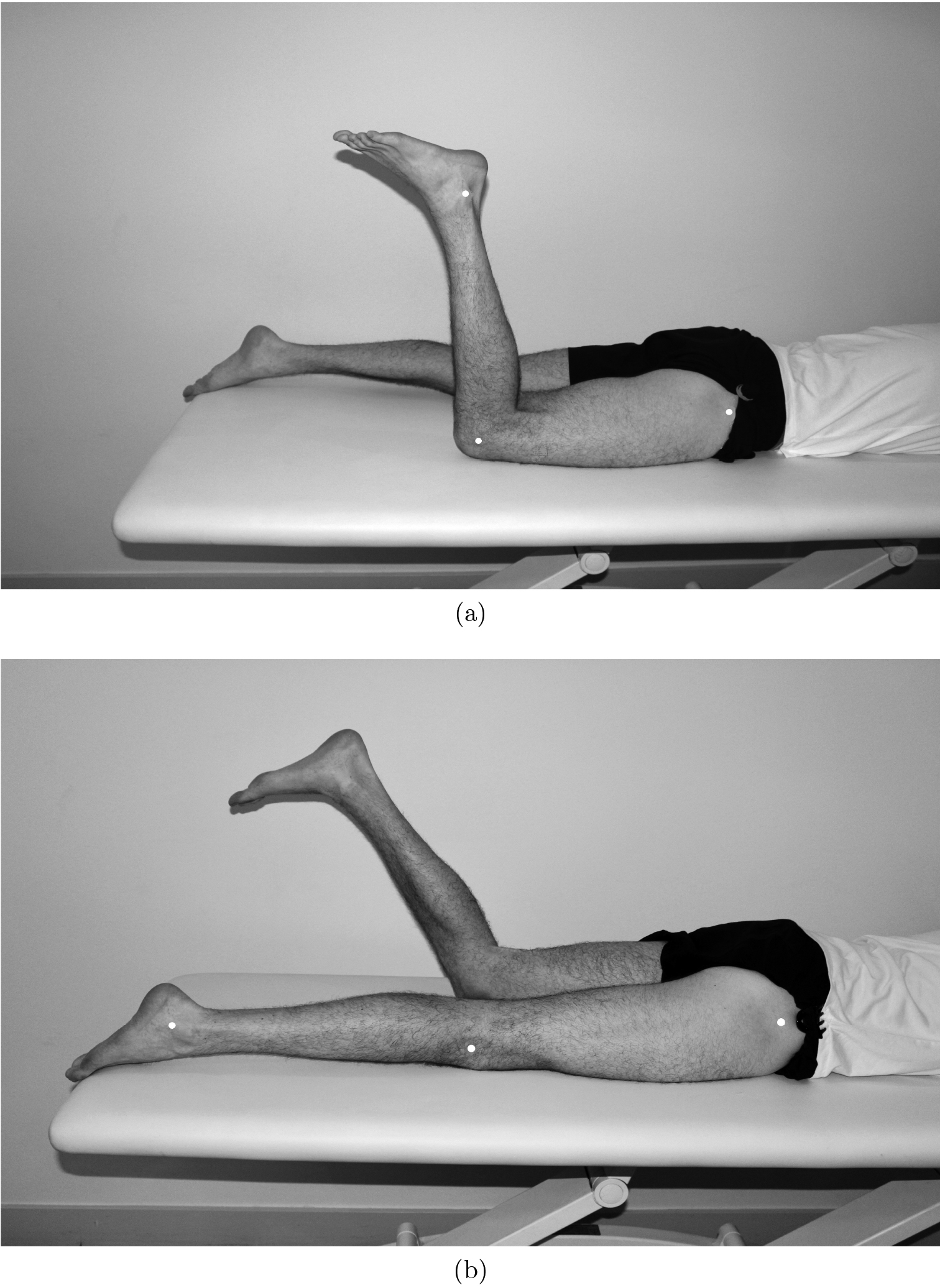
Additionally, the participants performed the same procedure during the manipulation of the semitendinosus tendon. A common method of anterior cruciate ligament reconstruction is semitendinosus tendon allografting [5, 34, 35, 36, 37, 38]. Therefore, vibration was applied to disturb the proprioceptive function of the semitendinosus tendon, mimicking post-surgical neuromechanical behaviour. Vibration was induced by a customised engine (‘Braun’ engine, 120 Hz) [39]. A frequency above 80 Hz was selected, as this was previously shown to activate and influence the majority of sensory fibres [17, 40, 41]. For the testing procedure, each participant lay down or sat on an adjustable physiotherapy bench. The participant’s left knee was set passively to a random angle chosen by the test operator. Previous studies have indicated no clinically important differences in proprioceptive performance between dominant and non-dominant limbs in trained participants [42, 43, 44, 45]. Next, the participants were instructed to actively reproduce the left knee angle with the right leg. For the subsequent knee angle determination, fixed anatomical landmarks were tagged: tuberculum majus humeri, epicondylus lateralis humeri, processus styloideus radii, trochanter major femoris, lateral knee joint cavity, and alleolus lateralis (shown in Figs 1 and 2). Each test included five trials. To minimise proprioceptive transfer to the next test, the participants walked around for about two minutes between tests. The participants were blindfolded for all conditions to prevent visual feedback.
2.2Outcome measures
The outcome measure was the knee angle reproduction error, measured as degree [
2.3Statistical analysis
Statistical analyses were performed using R (Version 3.3.3). Data were checked for missing values, distribution, and outliers and descriptively summarised as means
3.Results
Twenty-five healthy young students (age
3.1Pre-test
Comparison of the reproducibility of the elbow angle on the same side and on the contralateral side (mirroring) showed no statistically significant differences (mirroring: t (24)
Table 1
Descriptive values of self-chosen target knee angle and the resulting absolute reproduction error in the prone and sitting position with and without vibration induced on the semitendinosus tendon in a knee angle reproduction test (n
| Extension | Flexion | Vibration | Min | Max | Reproduction error mean | SE | 95% confidence interval | |
|---|---|---|---|---|---|---|---|---|
| Sitting position [ | ||||||||
|
| 98 | 170 | 7.03 | 0.65 | 5.70–8.37 | |||
|
| 122 | 183 | 5.81 | 0.54 | 4.69–6.93 | |||
|
|
| 46 | 174 | 5.38 | 0.34 | 4.67–6.08 | ||
|
|
| 123 | 196 | 5.28 | 0.50 | 4.25–6.31 | ||
| Prone position [ | ||||||||
|
| 51 | 157 | 6.37 | 0.63 | 5.04–7.66 | |||
|
| 65 | 166 | 5.26 | 0.45 | 4.34–6.19 | |||
|
|
| 52 | 162 | 6.80 | 0.75 | 5.26–8.34 | ||
|
|
| 110 | 169 | 8.70 | 0.84 | 6.98–10.4 |
Figure 3.
Boxplot of the difference in knee angle reproduction error including all repetitions: light grey
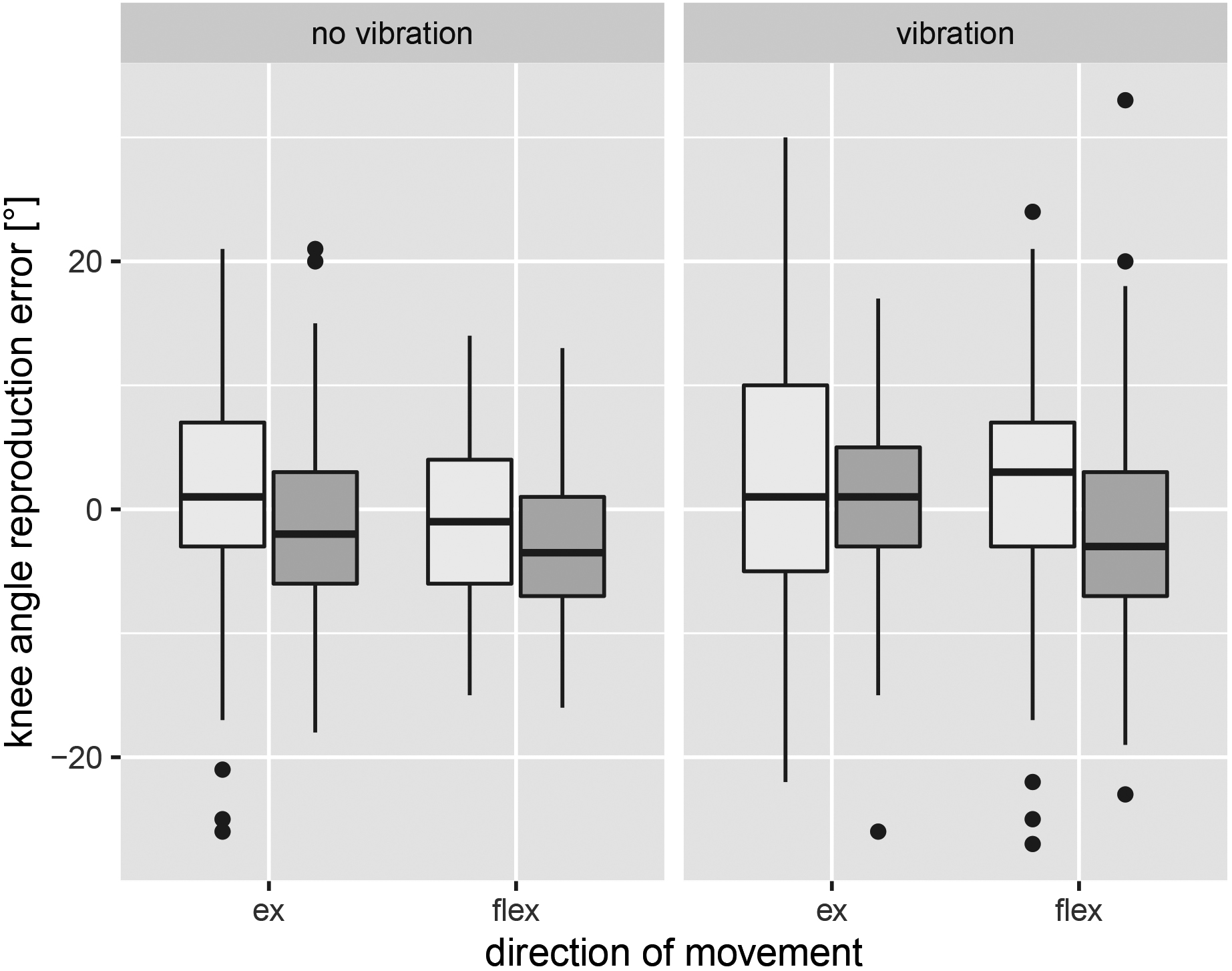
Figure 4.
Boxplot of the signed mean difference in knee angle reproduction error: light grey
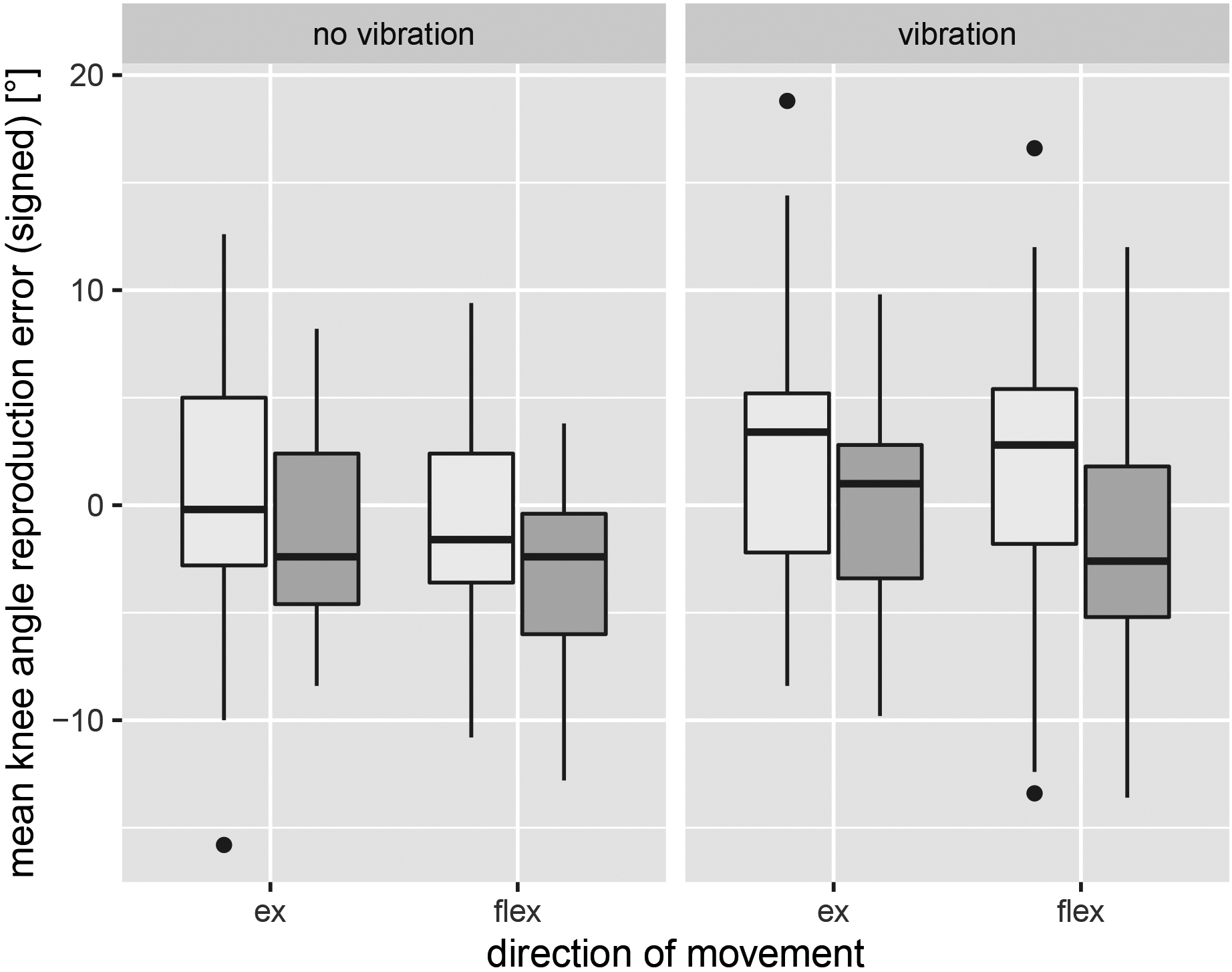
Figure 5.
Boxplot of the absolute mean difference in knee angle reproduction error: light grey
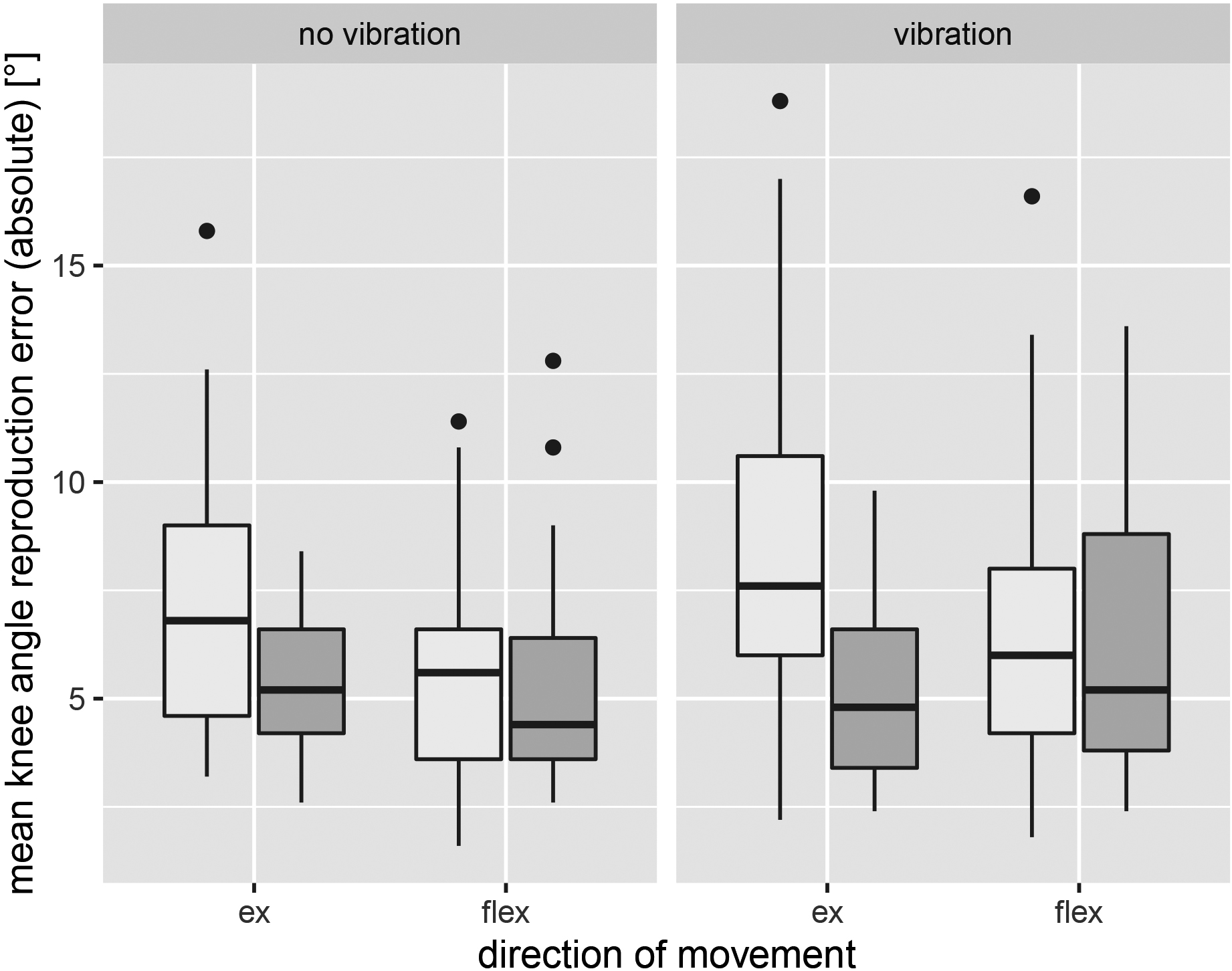
3.2Effect of the intervention
Inspection of the normal Q-Q plot indicated that the data were normally distributed for each group. Levene testing revealed no deviation from homoscedasticity for signed angle reproduction error (
4.Discussion
The aim of the present study was to evaluate joint position sense by investigating knee angle reproduction ability under different testing conditions. The results confirmed the hypothesis that the ability to reproduce knee angles differs between sitting and prone positions. The results further indicate that the initial starting position, either from knee flexion or extension, influences reproduction ability. These findings are of great practical importance, as currently the literature does not prescribe uniform standards regarding the starting position of the joint position sense test [7, 8, 46]. Based on our results, the general ability to reproduce knee joint angles is not interchangeable between different starting positions and body orientations. An adequate reproducibility of the knee joint angle from the prone position cannot be directly compared with the same results from the sitting position. A possible explanation for this could be the difference in body position in space and especially in the position of the head (upright versus horizontal) [47]. Different tactile feedback on the thigh could also have influenced the resulting position sense [9]. In a seated position, tactile feedback is primarily given on the back of the thigh, whereas in a prone position, tactile feedback is more likely to be found on the front. The somatosensory system is responsible for the perception of haptics, movement, position of body segments, temperature changes, and pain [48]. To perceive these diverse sensory impressions, the somatosensory system has a large number of mechanoreceptors at its disposal. Various body orientations might be relayed to different mechanoreceptors, thus making standardisation of test methods paramount. Further, primary cilia (PC) play a crucial role in the signalling between the intra- and extracellular space. Grevenstein et al. [49] detected a significantly lower rate of PC positive cells compared to other tissues and ligaments of other species, which might be a tissue-specific characteristic of the ACL [49]. Third, the elongation ability of the muscle-tendon unit of the ischiocrural musculature might be reduced while sitting with both legs extended. Furthermore, the predominant pre-tension of the m. quadriceps femoris, depending on the aforementioned stretching ability, may have caused better reproducibility [50, 51]. In addition to the elasticity of ligament and tendon structures, other factors can also play a role in carrying out a knee angle reproduction test [52], such as restrictions on movement in the elderly or those with orthopaedic injuries limiting the choice of starting position. To mimic the clinical setting, testing was performed in non-weight-bearing conditions, even though weight-bearing might be more functional [41]. Therefore, transferring the results to daily activities should be done with caution. Clinical studies have shown possible impairments of proprioception in the knee joint in patients with anterior cruciate ligament rupture and lower neuromuscular activity in anterior cruciate ligament reconstruction [7, 24, 14, 16, 17]. This can be attributed to disturbed neural feedback caused by the destruction of the mechanoreceptors in the anterior cruciate ligament or the muscle spindle, as well as by the removal of the neural feedback of the semitendinosus or patella tendon after surgery [7, 18, 53]. Following Bock et al. [39], the present study used vibration as an interference source to induce impairment of neuronal feedback and thus proprioception of the knee joint in healthy subjects. The aim was to simulate the neuronal injury mechanisms of semitendinosus plastic surgery in anterior cruciate ligament reconstruction and to examine the possible effects on proprioception. It was expected that manipulating the semitendinosus tendon by vibration would induce a significantly reduced ability to reproduce knee angles under all joint position sense test conditions. The results showed that vibration represents a recognisable influence and thus serves as a source of interference with proprioception. However, it is questionable whether the vibration causes a disturbance in the neuronal feedback of the semitendinosus tendon. There could be other possible factors, such as the attachment of the vibration device or a pure sensitivity disturbance of the skin surface due to vibration [54]. However, anterior cruciate ligament reconstruction by means of semitendinosus allograft surgery potentially has far more consequences than what induced vibration is capable of simulating [55]. One possible approach could be the use of artificial intelligence (AI) to might reduce the risk of neurological damage and improve clinical outcome prediction. Especially in the field of diagnostics and therapy AI has already shown considerable advantages [56, 57, 58, 59]. This could be beneficial for the patients’ rehabilitation process. This is the first study to investigate and confirm the impact of body orientation and direction of movement in an active knee angle reproduction test, considering possible interaction effects. A potential influence of body orientation and movement direction, even in healthy athletic persons, could be suspicious of an even greater discrepancy in orthopedically impaired patients. Further research in non-healthy subjects, such as anterior cruciate ligament patients, is recommended before drawing clinical conclusions. To date, the current literature remains difficult to compare with the present results, because different testing protocols, equipment, and no uniform concerning testing positions have been used. Further, no studies have considered possible interaction effects between body orientation and direction of movement of the knee [46, 52]. This is the first study to compare the results of different body orientations and directions of movement in an active knee angle reproduction test.
5.Conclusion
Due to the reproduction errors in knee angle reproduction tests determined by different test conditions, practitioners are advised to use standardised test procedures to progress their clinical value and implementation into daily practice. The results in different settings should be critically analysed – that is, a direct comparison between the prone and sitting positions in a practical approach might not be recommended. Furthermore, considering the economic health aspects, the choice of test conditions should be based on the participants’ resources to perform their best results. Practitioners should be aware that varying test conditions can lead to different therapeutic consequences. Future studies should focus on additional influencing factors on testing procedures, such as weight-bearing conditions. However, it would be of great interest to elucidate how the resulting reproduction error depends on the knee in setting the target angle.
5.1Clinical messages
• Body orientation has an influence on knee angle reproducing capabilities, whereas reproduction error is significantly higher in the prone position.
• Direction of movement (starting from knee extension or knee flexion) might have a practical influence on knee angle reproduction errors.
• There is evidence that disruption of senso-motoric feedback leads to a decline in reproductive capacity.
• Practitioners should be aware that varying test conditions can lead to different therapeutic consequences.
Authors contribution
Juliane Wieber: Conceptualisation, Methodology, Software, Formal analysis, Investigation, Data curation, Writing-Original Draft, Visualisation, Project administration.
Jasmin Brandt: Conceptualisation, Methodology, Investigation, Writing-Original Draft.
Eva Hirschhäuser: Conceptualisation, Methodology, Software, Investigation, Writing-Original Draft.
Maike Pieper: Conceptualisation, Methodology, Formal analysis, Investigation, Writing-Original Draft.
Robert Rein: Conceptualisation, Data curation, Software, Formal analysis, Supervision, Project administration.
Philip Catalá-Lehnen: Resources, Proof-Reading-Original Draft, Data interpretation.
Bjoern Braunstein: Conceptualisation, Software, Resources, Data curation, Supervision, Project administration.
Funding
This research did not receive any funding from public, non-profit and/or commercial organisations.
Acknowledgments
The authors would like to thank all the subjects who participated in the study.
Conflict of interest
The authors declare that there is no conflict of interest.
References
[1] | Webster KE, Hewett TE. What is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Medicine. (2019) ; 49: : 917-929. |
[2] | Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy: The Journal of Arthroscopic & Related Surgery. (2011) ; 27: (12): 1697-1705. |
[3] | Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. British Journal of Sports Medicine. (2016) ; 50: (13): 804-808. |
[4] | Lai CC, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: A systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. British Journal of Sports Medicine. (2018) ; 52: (2): 128-138. |
[5] | Ardern CL, Glasgow P, Schneiders A, Witvrouw E, Clarsen B, Cools A, Gojanovic B, Griffin S, Khan KM, Moksnes H, Mutch SA, Phillips N, Reurink G, Sadler R, Silbernagel KG, Thorborg K, Wangensteen A, Wilk KE, Bizzini M. 2016 Consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. British Journal of Sports Medicine. (2016) ; 50: (14): 853-864. |
[6] | Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. New England Journal of Medicine. (2010) ; 363: (4): 331-342. |
[7] | Han J, Waddington G, Adams R, Anson J, Liu Y. Assessing proprioception: A critical review of methods. Journal of Sport and Health Science. (2016) ; 5: (1): 80-90. |
[8] | Li L, Ji ZQ, Li YX, Liu WT. Correlation study of knee joint proprioception test results using common test methods. Journal of Physical Therapy Science. (2016) ; 28: (2): 478-482. |
[9] | Stone KD, Keizer A, Dijkerman HC. The influence of vision, touch, and proprioception on body representation of the lower limbs. Acta Psychologica. (2018) ; 185: : 22-32. |
[10] | Roberts D, Fridén T, Stomberg A, Lindstrand A, Moritz U. Bilateral proprioceptive defects in patients with a unilateral anterior cruciate ligament reconstruction: A comparison between patients and healthy individuals. Journal of Orthopaedic Research: Official Publication of the Orthopaedic Research Society. (2000) ; 18: (4): 565-571. |
[11] | Domeika A, Slapšinskaitė A, Razon S, Šiupšinskas L, Klizienė I, Dubosienė M. Effects of an 8-week basketball-specific proprioceptive training with a single-plane instability balance platform. Technology and Health Care. (2020) ; 28: (5): 561-571. |
[12] | Dhillon MS, Bali K, Prabhakar S. Proprioception in anterior cruciate ligament deficient knees and its relevance in anterior cruciate ligament reconstruction. Indian Journal of Orthopaedics. (2011) ; 45: (4): 294-300. |
[13] | Tayfur B, Charuphongsa C, Morrissey D, Miller SC. Neuromuscular Function of the Knee Joint Following Knee Injuries: Does It Ever Get Back to Normal? A Systematic Review with Meta-Analyses. Sports Medicine. (2020) ; 1-18. |
[14] | Hopper DM, Creagh MJ, Formby PA, Goh SC, Boyle JJ, Strauss GR. Functional measurement of knee joint position sense after anterior cruciate ligament reconstruction. Archives of Physical Medicine and Rehabilitation. (2003) ; 84: (6): 868-872. |
[15] | Jerosch J, Prymka M. Propriozeptive Fähigkeiten im Bereich des Kniegelenks bei Patienten nach vorderer Kreuzbandruptur. Der Unfallchirurg. (1996) ; 99: (11): 861-868. |
[16] | Kaur M, Ribeiro DC, Theis JC, Webster KE, Sole G. Movement patterns of the knee during gait following ACL reconstruction: A systematic review and meta-analysis. Sports Medicine (Auckland, NZ). (2016) ; 46: (12): 1869-1895. |
[17] | MacDonald PB, Hedden D, Pacin O, Sutherland K. Proprioception in anterior cruciate ligament-deficient and reconstructed knees. The American Journal of Sports Medicine. (1996) ; 24: (6): 774-778. |
[18] | Relph N, Herrington L, Tyson S. The effects of ACL injury on knee proprioception: A meta-analysis. Physiotherapy. (2014) ; 100: (3): 187-195. |
[19] | Fleming JD, Ritzmann R, Centner C. Effect of an anterior cruciate ligament rupture on knee proprioception within 2 Years after conservative and operative treatment: A systematic review with meta-analysis. Sports Medicine. (2022) ; 52: (5): 1091-1102. |
[20] | Suydam SM, Cortes DH, Axe MJ, Snyder-Mackler L, Buchanan TS. Semitendinosus tendon for ACL reconstruction: Regrowth and mechanical property recovery. Orthopaedic Journal of Sports Medicine. (2017) ; 5: (6). |
[21] | Proske U, Wise AK, Gregory JE. The role of muscle receptors in the detection of movements. Progress in Neurobiology. (2000) ; 60: (1): 85-96. |
[22] | Hanzlíková I, Richards J, Hébert-Losier K, Smékal D. The effect of proprioceptive knee bracing on knee stability after anterior cruciate ligament reconstruction. Gait Posture. (2019) ; 67: : 242-247. |
[23] | Grob KR, Kuster MS, Higgins SA, Lloyd DG, Yata H. Lack of correlation between different measurements of proprioception in the knee. The Journal of Bone and Joint Surgery British Volume. (2002) ; 84: (4): 614-618. |
[24] | Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. The American Journal of Sports Medicine. (2000) ; 28: (3): 336-344. |
[25] | Nagai T, Bates NA, Hewett TE, Schilaty ND. Effects of localized vibration on knee joint position sense in individuals with anterior cruciate ligament reconstruction. Clinical Biomechanics (Bristol, Avon). (2018) ; 55: : 40-44. |
[26] | Romero-Franco N, Montaño-Munuera JA, Jiménez-Reyes P. Validity and Reliability of a Digital Inclinometer to Assess Knee Joint-Position Sense in a Closed Kinetic Chain. Journal of Sport Rehabilitation. (2017) ; 26: (1). |
[27] | Barrett D. Proprioception and function after anterior cruciate reconstruction. The Journal of Bone and Joint Surgery British Volume. (1991) ; 73: (5): 833-837. |
[28] | Ojoawo AO, Olaogun MO, Hassan MA. Comparative effects of proprioceptive and isometric exercises on pain intensity and difficulty in patients with knee osteoarthritis: A randomised control study. Technology and Health Care. (2016) ; 24: (6): 853-863. |
[29] | Strong A, Arumugam A, Tengman E, Röijezon U, Häger CK. Properties of knee joint position sense tests for anterior cruciate ligament injury: A systematic review and meta-analysis. Orthopaedic Journal of Sports Medicine. (2021) ; 9: (8): 23259671211007878. |
[30] | Deshpande N, Connelly DM, Culham EG, Costigan PA. Reliability and validity of ankle proprioceptive measures. Archives of Physical Medicine and Rehabilitation. (2003) ; 84: (6): 883-889. |
[31] | Elangovan N, Herrmann A, Konczak J. Assessing proprioceptive function: Evaluating joint position matching methods against psychophysical thresholds. Physical Therapy. (2014) ; 94: (4): 553-561. |
[32] | Gonzales TI, Goble DJ. Short-term adaptation of joint position sense occurs during and after sustained vibration of antagonistic muscle pairs. Frontiers in Human Neuroscience. (2014) ; 8: : 896. |
[33] | Larsen R, Lund H, Christensen R, Røgind H, Danneskiold-Samsøe B, Bliddal H. Effect of static stretching of quadriceps and hamstring muscles on knee joint position sense. British Journal of Sports Medicinek. (2005) ; 39: (1): 43-46. |
[34] | Suydam SM, Cortes DH, Axe MJ, Snyder-Mackler L, Buchanan TS. Semitendinosus tendon for ACL reconstruction: Regrowth and mechanical property recovery. Orthopaedic Journal of Sports Medicine. (2017) ; 5: (6). |
[35] | Ardern CL, Webster KE. Knee flexor strength recovery following hamstring tendon harvest for anterior cruciate ligament reconstruction: A systematic review. Orthopedic Reviews. (2009) ; 1: (2). |
[36] | Barenius B, Webster WK, McClelland J, Feller J. Hamstring tendon anterior cruciate ligament reconstruction: Does gracilis tendon harvest matter? International Orthopaedics. (2013) ; 37: (2): 207-212. |
[37] | Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: Is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clinical Orthopaedics and Related Research. (2017) ; 475: (10): 2459-2468. |
[38] | Chen H, Liu H, Chen L. Patellar tendon versus 4-strand semitendinosus and gracilis autografts for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials with mid-to long-term follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery. (2020) ; 36: (8): 2279-2291. |
[39] | Bock O, Pipereit K, Mierau A. A method to reversibly degrade proprioceptive feedback in research on human motor control. Journal of Neuroscience Methods. (2007) ; 160: (2): 246-250. |
[40] | Bosco C, Cardinale M, Tsarpela O. Influence of vibration on mechanical power and electromyogram activity in human arm flexor muscles. European Journal of Applied Physiology and Occupational Physiology. (1999) ; 79: (4): 306-311. |
[41] | Layne CS, Chelette AM, Pourmoghaddam A. Impact of altered lower limb proprioception produced by tendon vibration on adaptation to split-belt treadmill walking. Somatosensory & Motor Research. (2015) ; 32: (1): 31-38. |
[42] | Ghai S, Driller MW, Masters RSW. The influence of below-knee compression garments on knee-joint proprioception. Gait & Posture. (2018) ; 60: : 258-261. |
[43] | Jerosch J, Prymka M. Knee joint proprioception in normal volunteers and patients with anterior cruciate ligament tears, taking special account of the effect of a knee bandage. Archives of Orthopaedic and Trauma Surgery. (1996) ; 115: (3-4): 162-166. |
[44] | Azevedo J, Rodrigues S, Seixas A. The influence of sports practice, dominance and gender on the knee joint position sense. The Knee. (2021) ; 28: : 117-123. |
[45] | Hancock GE, Hepworth T, Wembridge K. Accuracy and reliability of knee goniometry methods. Journal of Experimental Orthopaedics. (2018) ; 5: (1): 1-6. |
[46] | Baumeister J. Zentralnervöse und motorische Auswirkungen einer Verletzung und Rekonstruktion des vorderen Kreuzbandes bei sensomotorischen Aufgaben [Dissertation]. Universität Paderborn. Paderborn; (2007) . |
[47] | Liu JZ, Kubo M, Aoki H, Liu N, Kou PH, Suzuki T. A study on the difference of human sensation evaluation to whole-body vibration in sitting and lying postures. Applied Human Science: Journal of Physiological Anthropology. (1995) ; 14: (5): 219-226. |
[48] | Lephart SM, Pincivero DM, Rozzi SL. Proprioception of the ankle and knee. Sports Medicine. (1998) ; 25: (3): 149-155. |
[49] | Grevenstein D, Oppermann J, Winter L, Barsch F, Niedermair T, Mamilos A, et al. First detection of primary cilia in injured human anterior cruciate ligament: A pilot study with pathophysiological reflections. Pathology-Research and Practice. (2022) ; 237. |
[50] | Ribot-Ciscar E, Roll JP. Ago-antagonist muscle spindle inputs contribute together to joint movement coding in man. Brain Research. (1998) ; 791: (1-2): 167-176. |
[51] | Gisler T. Dehnung des M. quadriceps femoris aus anatomisch-physiologischer Sicht. Differenzierte Längendiagnostik und Dehninterventionen für den M. rectus femoris und die drei Mm. Vasti. Schweiz Z Med Traumatol. (2012) ; 13: (60): 116-124. |
[52] | Wilke C, Froböse I. Quantifizierung propriozeptiver Leistungen von Kniegelenken. Deutsche Zeitschrift für Sportmedizin. (2003) ; 54: (2): 49-54. |
[53] | Duchman KR, Lynch TS, Spindler KP. Graft selection in anterior cruciate ligament surgery: Who gets what and why? Clinics in Sports Medicine. (2017) ; 36: (1): 25-33. |
[54] | Sherrick CE. Variables affecting sensitivity of the human skin to mechanical vibration. Journal of Experimental Psychology. (1953) ; 45: (5): 273-282. |
[55] | D’Alessandro P, Wake G, Annear P. Hamstring pain and muscle strains following anterior cruciate ligament reconstruction: A prospective, randomized trial comparing hamstring graft harvest techniques. Journal of Knee Surgery. (2012) Sep; 26: (02): 139-144. |
[56] | Hafizović L, Čaušević A, Deumić A, Bećirović LS, Pokvić LG, Badnjević A. The Use of Artificial Intelligence in Diagnostic Medical Imaging: Systematic Literature Review. In: 2021 IEEE 21st International Conference on Bioinformatics and Bioengineering (BIBE). IEEE; (2021) . pp. 1-6. |
[57] | Kunze KN, Rossi DM, White GM, Karhade AV, Deng J, Williams BT, et al. Diagnostic performance of artificial intelligence for detection of anterior cruciate ligament and meniscus tears: A systematic review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. (2021) ; 37: (2): 771-781. |
[58] | Rovčanin A, Skopljak S, Suleiman S, Smajović A, Bečić E, Bečić F, Spahić Bećirović L, Gurbeta Pokvić L, Badnjević A. Application of artificial intelligence in diagnosis and therapy of prostate cancer. IFAC-PapersOnLine. (2022) ; 55: (4): 74-79. |
[59] | Šeho L, Šutković H, Tabak V, Tahirović S, Smajović A, Bečić E, Deumić A, Spahić Bećirović L, Gurbeta Pokvić L, Badnjević A. Using artificial intelligence in diagnostics of meningitis. IFAC-PapersOnLine. (2022) ; 55: (4): 56-61. |




