Auricular bean embedding improves urination in epidural labor analgesia: A single center randomized controlled study
Abstract
BACKGROUND:
Acupoint buried beans on the auricle is a feasible method to prevent and treat postpartum urinary retention.
OBJECTIVE:
This study investigated the effect of auricular acupoint buried beans on postpartum urination and maternal and fetal outcomes following epidural analgesia for labor.
METHODS:
Two hundred forty primiparas underwent vaginal trial labor analgesia from May 2020 to January 2021 and were randomly placed into the intervention and control groups. Both groups received epidural labor analgesia. Maternal urination during labor, 2 h postpartum, and the time for first postpartum urination were recorded as primary outcomes, with maternal and infant outcomes documented as secondary results. Statistical analysis was performed using the independent sample
RESULTS:
Two hundred eight study participants were subsequently included in the results, i.e., 105 patients in the intervention group and 103 in the control group. The intervention group comprised a significantly lower number of patients with excessive residual urine volume at cervical dilatation of 5–6 cm (
CONCLUSION:
Auricular acupoint embedded beans can improve the urination status at cervical dilatation of 5–6 cm and 2 h postpartum, as well as significantly shorten the duration of labor.
1.Introduction
Epidural labor analgesia (ELA) is widely used. Although it can greatly reduce maternal labor pain, studies have found that ELA drugs affect the normal reflex arc of urination, weaken the contraction of abdominal muscles and the diaphragm, cause urination and bladder pain, as well as postpartum urinary retention [1, 2, 3, 4, 5]. Direct bladder catheterization is the solution to urinary retention during and after delivery.
Acupuncture is a component of traditional Chinese medicine (TCM) [6]. Acupoint paste [7] and ear acupoint buried beans [8-1] have been used as acupuncture treatment [11] for urinary retention. The long-term development of TCM supports its theoretical system and therapies with more advantages than Western medicine. Not only do TCM drugs have no toxic side effects, but their non-invasive treatment methods are also more humane. Ear acupoints are scattered on the auricle and correspond to different points in the viscera [12]. The stimulation of ear acupoints can, in turn, stimulate the corresponding viscera and regulate them. Pressing the specific ear point corresponding to urination can excite the brain’s paracentral lobule, which controls urination, enabling the peripheral nervous system to regulate kidney and bladder function for urination [13, 14]. As such, theoretically and practically, using acupoint buried beans on the auricle is a feasible method to prevent and treat postpartum urinary retention. The present study explores the effect of auricular buried beans on epidural delivery.
2.Materials and method
2.1Study participants
Two hundred forty full-term primigravida women, who met the inclusion criteria and were admitted in our hospital between May 2020 and January 2021, were selected as study participants. When participants had regular contractions lasting 20–25 s, spaced 5–6 min apart, and the uterine opening was 2–3 cm, vaginal trial labor was performed in the delivery room. Randomization and intervention were initiated after the administration of ELA.
The study’s inclusion criteria were: (1) Pregnant women aged 18–34 years, at term (37–41 weeks), and having a singleton pregnancy. (2) Pregnant women with a normal fetal heart monitoring score and cervical dilatation of 2–3 cm for ELA. (3) An estimated fetal size of 2500–4000 g, with normal orientation and fetal heart monitoring. (4) Pregnant women with no reproductive tract malformation and no comorbidities or previous history of severe pregnancy complications. (5) Pregnant women who volunteered to participate in the study.
The study’s exclusion criteria were: (1) Patients with bladder retention or continuous catheterization before ELA. (2) Patients with a communication disorder.
The following were excluded from the analysis: (1) All screened and eligible study participants who withdrew from the study for any reason. (2) Women with incomplete data. (3) Delivery using forceps or cesarean section.
2.2Intervention program
Both the control and intervention group participants received epidural anesthesia while in labor. Both groups were advised regarding diet, drinking water, avoiding staying in bed for a long time, and passing urine every 2 h. They were also instructed not to increase the epidural dose due to experiencing pain when the wound was being closed under local infiltration anesthesia or nerve block to avoid urinary retention caused by anesthetic overdose. The injection of epidural drugs was stopped after the first stage of labor, and both groups had their epidural catheters removed by the anesthesiologist before they left the delivery room. The women in both groups were advised to eat, drink warm water, and void within 6 h of delivery.
In the intervention group, acupuncture beans were placed on specific ear points in addition to epidural anesthesia and routine care. Sympathetic, renal, bladder, urethra, and Shenmu points were selected, as described by Wei [15]. The ear point was first pressed vertically with the index finger or thumb until there was swelling or the patient experienced numbness or pain. The pressure was maintained for 10 s and repeated two or three times at 30 min intervals up to 2 h postpartum while paying attention to how much the patient could tolerate.
2.3Evaluation indicators
2.3.1General situation questionnaire
The questionnaire that was used in this study included demographic data, i.e., age, gestational weeks, education level, marital status, occupation, family per capita monthly income, medical payment method, details of diet and fluids consumed, and the amount of infusion received.
2.3.2Primary outcome indicators
(1) The primary outcome of this study was whether the patient could pass urine independently or needed catheterization [16, 17]. Other signs were a palpable bladder above the pubic symphysis despite the urge to void and a residual urine volume of 100 ml on ultrasonography.
(2) The urination score table was used to record the degree of urinary retention. The method adopts the scoring table recommended by the Guidelines for Clinical Research of New Chinese Medicine Drugs [18]. A higher score indicated more serious urinary retention symptoms. The scale has internal consistency reliability of 0.90 and good validity (Table 1).
Table 1
Urination score table
| Symptoms and signs | 0 Points | 1 Points | Two points | Three points |
|---|---|---|---|---|
| Urinary condition | Normal | The urine is thin and linear | Urinary flow breaks into a line | Urine drip out |
| Wait time | t | 1 min | 3 min | t |
| Abdominal symptoms | Symptomless | The lower abdomen is full of boredom | Small abdominal distension, full | Small bloating, full, pain |
2.3.3Secondary outcome measures
The recorded secondary outcome measures were the times of the three stages of labor, the volume of postpartum bleeding, neonatal weight, neonatal Apgar score, and neonatal hospitalization. Postpartum blood loss [19] was measured by either weighing or using volume methods. Bleeding volume (ml)
2.4Data collection method
Questionnaire Star software was used to conduct the survey. The women in both groups completed the general data questionnaire when they enrolled for ELA. Two hours following delivery and before leaving the delivery room, the participants completed the details relating to their diet and whether they had passed urine.
A B-mode ultrasound (model UMT-150) was used to measure residual urine volume in the bladder when cervical dilatation was 5–6 cm and again at 2 h postpartum. The ultrasound examination was carried out at the patient’s bedside by doctors trained in its use. The procedure lasted 3–5 min.
The following information was collected from the case records: data related to delivery, epidural analgesia time, delivery time, labor duration, postpartum bleeding volume, neonatal Apgar score, and neonatal weight.
2.5Statistical methods
SPSS Statistics version 25.0 for Windows (IBM Corp., Armonk, NY, USA) was used for statistical analysis. Measurement data were described using mean and standard deviation. The independent sample
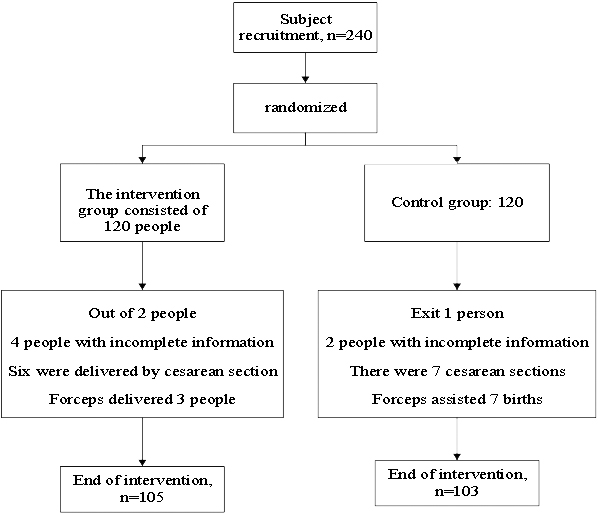
Figure 1.
Flowchart of the research object.
3.Results
Two hundred forty women were initially enrolled in the study. In the intervention group, the following participants were excluded from the study: two patients who were unwilling to cooperate, four patients with incomplete data, six patients who underwent a cesarean section, and three patients who required delivery using forceps. Subsequently, 105 patients were included in the intervention group. In the control group, the following participants were excluded: one patient unwilling to cooperate, two patients with incomplete data, seven patients who underwent a cesarean section, and seven patients who required delivery using forceps. Subsequently, the final control group included 103 eligible participants. Figure 1 shows a flow chart of the study participants.
3.1General comparison of the study participants
The baseline maternal data included age, weight, height, education, occupation, gestation, infusions received, diet, and water intake information. The two groups were comparable concerning these characteristics (
Table 2
Comparison of maternal demographic characteristics of the two groups (
| Project | Groups ( |
|
| ||
| Intervention group ( | Control group ( | ||||
| Age (year) | 28.72 | 28.27 | 1.020 | 0.310 | |
| Labor body weight (kg) | 65.21 | 64.96 | 0.270 | 0.790 | |
| Pregnancy week (day) | 280.51 | 276.89 | 2.751 | 0.282 | |
| Occupation | Staff | 71 (67.62) | 80 (77.67) | 0.990 | 0.983 |
| Liberal professions | 18 (17.14) | 8 (7.77) | |||
| Unemployed people | 16 (15.24) | 15 (14.56) | |||
| Per capita monthly income (yuan) | 98 (93.33) | 97 (94.17) | 0.801 | ||
| 1000 | 7 (6.67) | 6 (5.83) | |||
| Home residence | City | 69 (65.71) | 69 (66.99) | 0.850 | |
| Rural area | 36 (34.29) | 34 (33.01) | |||
| Medical payment method | Medical insurance | 91 (86.67) | 92 (89.32) | 0.541 | |
| At one’s own expense | 13 (12.38) | 11 (10.68) | |||
| At public expense | 1 (0.95) | 0 | |||
| Education level | Junior college Below | 6 (5.71) | 9 (8.73) | 0.903 | |
| Junior college | 50 (47.62) | 46 (43.81) | |||
| Undergraduate course | 24 (22.86) | 29 (28.16) | |||
| Master’s degree or above | 25 (23.81) | 19 (18.45) | |||
| Infusion volume during the labor process (ml) | 467.14 | 505.049 | 0.342 | ||
| Diet volume during labor (ml) | 426.71 | 418.50 | 0.953 | ||
| Drinking water volume during the production process (ml) | 708.48 | 597.96 | 0.914 | ||
| Newborn body weight (g) | 3179.62 | 3261.46 | 0.152 | ||
3.2Comparison of urination conditions among the study participants
This study analyzed the maternal residual urine volume at cervical dilatation of 5–6 cm and 2 h postpartum. The non-parametric rank-sum test showed that the number of patients requiring postpartum catheterization in the intervention group was significantly lower than in the control group (
Table 3
Comparison of maternal urination in the two groups (
| Project | Intervention group ( | Control group ( |
|
| |
|---|---|---|---|---|---|
| Residual urine volume of 5 to 6 c m in open uterine | 88.76 | 127.5 | 0.013 | ||
| mouth (ml) | |||||
| Total residual urine volume (ml) | 100.10 | 95.92 | 0.652 | ||
| Residual urine (ml) | 81.67 | 99.42 | 0.601 | ||
| Intrapartum catheterization number of | 0 times | 54 (51.43) | 31 (30.10) | 0.0003 | |
| times | One time | 35 (33.33) | 37 (35.92) | ||
| Two times | 12 (11.43) | 27 (26.21) | |||
| Three times | 4 (3.81) | 8 (7.77) | |||
| Does urinary retention occur at uterine | Yes | 73 (69.52) | 58 (56.31) | 4.629 | 0.031 |
| mouth opening from 5 to 6 cm | Deny | 32 (30.48) | 45 (43.69) | ||
| Urinary retention occurs during full | Yes | 74 (70.48) | 64 (62.14) | 0.381 | 0.538 |
| uterine mouth opening | Deny | 31 (29.52) | 39 (37.86) | ||
| Urinary retention occurs after childbirth | Yes | 95 (90.48) | 77 (74.76) | 3.968 | 0.546 |
| Deny | 10 (9.52) | 26 (25.24) | |||
| Dividing status integral | 0.50 | 1.13 | |||
| Abdominal symptom integral | 0.30 | 0.70 | |||
| Time integral for urination | 0.50 | 0.98 | |||
| Total points | 1.60 | 2.81 | |||
| Postpartum catheterization | 0 times | 95 (90.48) | 86 (83.50) | 0.141 | |
| One time | 10 (9.52) | 17 (16.50) | |||
3.3Comparison of maternal and infant outcomes among the study participants
3.3.1Comparison of the duration of each stage of labor between the two groups
In this study, the delivery time, the duration of the first, second, and third stages of labor, and the total labor duration of the two groups were compared. The results showed that the difference between the delivery time, first stage, and total labor duration between the two groups was statistically significant (
Table 4
Comparison of labor duration between two groups (
| Project | Intervention group ( | Control group ( |
|
|
|---|---|---|---|---|
| Labor analgesia distance from labor time (min) | 362.65 | 464.21 | 0.004 | |
| First labor time (min) | 561.76 | 741.46 | 0.003 | |
| Second labor time (min) | 40.57 | 56.11 | 0.005 | |
| Third labor time (min) | 7.08 | 5.13 | 0.090 | |
| Total labor time (min) | 609.41 | 802.69 | 0.004 |
3.3.2Comparison of maternal fever and neonatal conditions between the two groups
According to the analysis, there was no significant difference in the occurrence of maternal fever (
Table 5
Comparison of maternal and infant outcomes between the two maternal groups (
| Project | Divide into groups | Intervention group ( | Control group ( |
|
|
|---|---|---|---|---|---|
| Fever during the labor process | Yes | 10 (9.5) | 14 (13.6) | 0.841 | 0.360 |
| Deny | 95 (90.5) | 89 (86.4) | |||
| Postpartum 2 h (ml) | 196.57 | 207.62 | 0.120 | ||
| Whereabouts of the newborn | Direct rooming-in | 56 (53.33) | 53 (51.46) | 0.710 | |
| Observation ward for | 38 (36.19) | 37 (35.92) | |||
| high-risk children | |||||
| Neonatal department | 11 (10.48) | 13 (12.62) | |||
| Asphyxia neonatorum | Yes | 0 | 2 (1.94) | 2.831 | 0.091 |
| Deny | 105 (100) | 101 (98.06) | |||
4.Discussion
4.1The effect of ear acupoint buried beans on epidural delivery
In this study, ear-acupoint pressure was used in the intervention group. Applying the beans during ELA could promote urination at a cervical dilatation of 5–6 cm, reduce the postpartum catheterization rate, shorten the first postpartum urination time, and promote the first postpartum instance of urination. Suen et al. [20, 21, 22, 23] also showed that ear acupoint buried beans positively relieved maternal urinary retention. This may have been the result of the rich distribution of blood vessels in the auricle. The positioning of ear-point buried beans is based on the auricle ear points and the body’s meridians, which reflect specific internal organs. The stimulation of specific ear points can be effective in the treatment of a variety of diseases [24, 25, 26, 27]. In this study, the kidney, bladder, and urethra points were regularly stimulated to strengthen bladder contraction and effectively alleviate spasms and urethral edema, thereby promoting urination.
Ear-point buried beans can improve the time to early urination following the administration of ELA for women in labor, as well as postpartum, and reduce urinary retention and catheterization rates, thereby providing clinical benefits.
4.2The effect of ear acupoint buried beans on maternal and infant outcomes
Labor in primiparas can often last for an extended period, and the pain that is experienced during this time can often prompt the patient to request a cesarean section, thus increasing the rate at which this procedure is performed. Currently, an intraspinal block is a widely used analgesic method [27]. However, this approach has often led to reports of adverse reactions, such as a prolonged second stage of labor, an elevated cesarean section rate, hypotension, urinary retention, dizziness, and nausea [28, 29]. Furthermore, whether these analgesic drugs have long-term effects on newborns remains unclear. Therefore, it is of great significance that a safe analgesic method is established that does not affect the mother or the infant’s health and shortens the labor process, thus encouraging natural delivery. This study found that ear acupoint buried beans shortened the duration of maternal labor and did not cause any adverse outcomes for the mother or her infant. Taylor et al. [30, 31, 32, 33, 34] also reported that ear acupoint buried beans could relieve labor pain and shorten delivery time. This may be because the Shenmen point is the essential point of Shaoyin, which nourishes yin and lowers fire, relieves pain, and enriches and calms the mind. Sympathetic acupoints have a strong analgesic effect on viscera. Wang Weixing seed is used to press repeatedly at the Shenmen and sympathetic acupoints to regulate each nervous system of the human body, alleviate smooth muscle spasms, and effectively relieve the puerpera’s tension and pain, thereby indirectly shortening the labor process and being safe for mothers and newborns [33, 34, 35, 36, 37, 38, 39, 40].
4.3Study limitations
This study enrolled women aged 18–34 years who underwent single, full-term vaginal delivery. With the establishment of the three-child policy in China and the universality of epidural analgesia for delivery, research must be conducted that includes mothers of advanced age and multiparous pregnant women. This study only applied blinding to the data collectors; the research participants were not blinded, which may have introduced an element of bias.
5.Conclusion
Ear acupoint buried beans can improve early active urination following the administration of an epidural for labor, promote urination at cervical dilatation of 5–6 cm, reduce the postpartum catheterization rate, encourage first postpartum urination, and shorten the time to first postpartum urination. Therefore, ear acupoint buried beans can be applied to future clinical practice. Studies incorporating larger sample sizes should be conducted to ensure the rigor and reliability of this study’s conclusions and thoroughly explore the effect of ear acupoint buried beans on ELA.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of Fujian Maternity and Child Health Hospital, College of Clinical Medicine for Obstetrics, Gynecology and Pediatrics. Written informed consent was obtained from all participants.
Funding
The study was supported by a hospital fund from Fujian Maternity and Child Health Hospital (No. YCXMH20-04).
Conflict of interest
None to report.
References
[1] | Liu X, Zeng R, Chen Q, Ke D, Zhu Z. The effect of epidural analgesia on maternal-neonatal outcomes: a retrospective study. Ginekol Pol. (2021) . |
[2] | Kawasoe I, Kataoka Y. Prevalence and risk factors for postpartum urinary retention after vaginal delivery in Japan: A case-control study. Jpn J Nurs Sci. (2020) ; 17: (2): e12293. |
[3] | Mulder FE, Oude Rengerink K, van der Post JA, Hakvoort RA, Roovers JP. Delivery-related risk factors for covert postpartum urinary retention after vaginal delivery. Int Urogynecol J. (2016) ; 27: (1): 55-60. |
[4] | Shen X. Clinical study on the effect of epidural labor analgesia on maternal and infant perinatal outcomes. (05), (2018) . |
[5] | Li YY. Construction and application of a risk prediction model for urinary retention after vaginal delivery. Southern Medical University. (09), (2019) . |
[6] | Lauterbach R, Ferrer Sokolovski C, Rozenberg J, Weissman A. Acupuncture for the treatment of post-partum urinary retention. Eur J Obstet Gynecol Reprod Biol. (2018) ; 223: : 35-38. |
[7] | Zhu Y, Wang F, Zhou J, et al. Effect of acupoint hot compress on postpartum urinary retention after vaginal delivery: A randomized clinical trial. JAMA Netw Open. (2022) ; 5: (5): e2213261. |
[8] | Wu G. Clinical study on auricular acupoint pressing in the prevention of postpartum urinary retention in the third stage of labor. Guangzhou University of Traditional Chinese Medicine. (01), (2017) . |
[9] | Tang CH, Yan Q, Wei L, Li Y, Lu CJ. Clinical observation on treatment of urinary retention after stroke with moxibustion combined with auricular point embedding and nursing intervention. Clinical Research of Traditional Chinese Medicine. (2019) ; 11: (27): 32-34. |
[10] | Chen P, Jiang Y. Observation on the effect of auricular point embedding beans on urinary retention after combined spinal and epidural anesthesia. Electronic Journal of Practical Clinical Nursing. (2019) ; 4: (20): 23. |
[11] | Lu XY. Auricle formation and inversion of auricular acupoint distribution. Shanghai Journal of Acupuncture and Moxibustion. (2017) ; 36: (07): 866-869. |
[12] | Zhou JZ, Cheng HL, Chen H, et al. Based on autonomic nerves, this paper discusses the regulating effect of auricular acupoint therapy on gastrointestinal tract. Shanghai Journal of Acupuncture and Moxibustion. (2022) ; 41: (01): 107-110. |
[13] | Wirz-Ridolfi A. The history of ear acupuncture and ear cartography: Why precise mapping of auricular points is important. Med Acupunct. (2019) ; 31: (3): 145-156. |
[14] | Mercante B, Ginatempo F, Manca A, Melis F, Enrico P, Deriu F. Anatomo-physiologic basis for auricular stimulation. Med Acupunct. (2018) ; 30: (3): 141-150. |
[15] | Wei R. Study on the evolution of acupoints before Song Dynasty. Beijing University of Chinese Medicine. (08), (2021) . |
[16] | Sallami S, Ben Amara F, Slimeni O, Ben Rhouma S, Ben Rais N, Horchani A. Postpartum-urinary retention. Tunis Med. (2011) ; 89: (6): 576. |
[17] | Xu SH, Song Q, Wang J, Shang AJ. Advances in diagnosis and treatment of acute urinary retention. General Nursing. (2017) ; 15: (36): 4502-4505. |
[18] | Xu LF. Clinical effect of auricular acupoint pressure on preventing urinary retention after anorectal disease. (05), (2016) . |
[19] | Liu XH, He L. Prevention and management of postpartum hemorrhage. Chinese Journal of Practical Gynecology and Obstetrics. (2020) ; 36: (02): 123-126. |
[20] | Suen L, Yeh CH, Yeung S, Yeung J. Is the combined auriculotherapy approach superior to magneto-auriculotherapy alone in aging males with lower urinary tract symptoms? A randomized controlled trial. Aging Male. (2020) ; 23: (5): 544-555. |
[21] | Li X, Li ZM, Tan JY, et al. Moxibustion for post-stroke urinary incontinence in adults: A systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. (2021) ; 42: : 101294. |
[22] | Ren JJ, Tian HC, Wang YF, Li YT, Xu Q, Tian L. Effectiveness and safety of moxibustion for poststroke insomnia: A systematic review and meta-analysis. World J Tradit Chin Med. (2022) ; 8: : 199-209. |
[23] | Waldum ÅH, Staff AC, Lukasse M, Falk RS, Sørbye IK, Jacobsen AF. Intrapartum pudendal nerve block analgesia and risk of postpartum urinary retention: A cohort study. Int Urogynecol J. (2021) ; 32: (9): 2383-2391. |
[24] | Vakilian K, Ghaemmaghami M, Sheikhganbari N, Shabani F, Vahedi M. Reducing Labor Anxiety with Auriculotherapy: A Randomized Clinical Trial Study. Chin J Integr Med. (2021) . |
[25] | Mafetoni RR, Rodrigues MH, Jacob L, Shimo A. Effectiveness of auriculotherapy on anxiety during labor: A randomized clinical trial1. Rev Lat Am Enfermagem. (2018) ; 26: : e3030. |
[26] | Fróes N, Arrais F, Aquino PS, Maia JC, Balsells M. Effects of auriculotherapy in the treatment of nausea and vomiting: A systematic review. Rev Bras Enferm. (2021) ; 75: (1): e20201350. |
[27] | Cha HS, Park H. Effects of auricular acupressure on obesity in adolescents. Complement Ther Clin Pract. (2019) ; 35: : 316-322. |
[28] | Lu YY, Cai JJ, Jin SW, et al. Application of dural puncture epidural technique for labor analgesia. Zhonghua Yi Xue Za Zhi. (2020) ; 100: (5): 363-366. |
[29] | Song Y, Du W, Zhou S, et al. Effect of dural puncture epidural technique combined with programmed intermittent epidural bolus on labor analgesia onset and maintenance: A randomized controlled trial. Anesth Analg. (2021) ; 132: (4): 971-978. |
[30] | Taylor SL, Giannitrapani KF, Ackland PE, et al. The implementation and effectiveness of battlefield auricular acupuncture for pain. Pain Med. (2021) ; 22: (8): 1721-1726. |
[31] | Cheng SI, Norman RM, DeMeo D, et al. The feasibility of blinding intraoperative electro-auricular acupuncture under neuraxial anesthesia. Med Acupunct. (2021) ; 33: (4): 286-294. |
[32] | Oviedo JD, Marquez E, Gold MA, Westhoff CL. Auricular acupressure and auricular acupuncture as an adjunct for pain management during first trimester aspiration abortion: A randomized, double-blinded, three-arm trial. Contraception. (2021) ; 103: (5): 342-347. |
[33] | Yang J, Ganesh R, Wu Q, et al. Battlefield acupuncture for adult pain: A systematic review and meta-analysis of randomized controlled trials. Am J Chin Med. (2021) ; 49: (1): 25-40. |
[34] | Zhang XW, Gu YJ, Wu HG, Li KS, Zhong R, Qi Q, et al. Systematic review and meta-analysis of acupuncture for pain caused by liver cancer. World J Tradit Chin Med. (2022) ; 8: : 402-12. |
[35] | Hendawy HA, Abuelnaga ME. Postoperative analgesic efficacy of ear acupuncture in patients undergoing abdominal hysterectomy: A randomized controlled trial. BMC Anesthesiol. (2020) ; 20: (1): 279. |
[36] | Giannitrapani KF, Ackland PE, Holliday J, et al. Provider perspectives of battlefield acupuncture: Advantages, disadvantages and its potential role in reducing opioid use for pain. Med Care. (2020) ; 58 Suppl 2 9S(2 9 Suppl): S88-S93. |
[37] | Alimoradi Z, Kazemi F, Gorji M, Valiani M. Effects of ear and body acupressure on labor pain and duration of labor active phase: A randomized controlled trial. Complement Ther Med. (2020) ; 51: : 102413. |
[38] | Vas J, Cintado MC, Aranda-Regules JM, Aguilar I, Rivas Ruiz F. Effect of ear acupuncture on pregnancy-related pain in the lower back and posterior pelvic girdle: A multicenter randomized clinical trial. Acta Obstet Gynecol Scand. (2019) ; 98: (10): 1307-1317. |
[39] | Ndubisi C, Danvers A, Gold MA, Morrow L, Westhoff CL. Auricular acupuncture as an adjunct for pain management during first trimester abortion: A randomized, double-blinded, three arm trial. Contraception. (2019) ; 99: (3): 143-147. |
[40] | Liu M, Tong Y, Chai L, et al. Effects of auricular point acupressure on pain relief: A systematic review. Pain Manag Nurs. (2021) ; 22: (3): 268-280. |




