The utility of combined neuroendoscopic- and laparoscopic-assisted ventriculo- peritoneal shunt as a treatment for patients with communicating hydrocephalus
Abstract
BACKGROUND:
Ventriculo-peritoneal shunt (VPS) is one of the routine methods used to treat communicating hydrocephalus.
OBJECTIVE:
To sum up the clinical effectiveness of ventriculo-peritoneal shunt (VPS), assisted with neuroendoscopy and laparoscopy, for the treatment of patients with communicating hydrocephalus.
METHODS:
From January 2010 to 2014, we performed VPS surgery on 209 patients with communicating hydrocephalus, using neuroendoscopy and laparoscopy, which helped to implant the shunt catheter in a suitable position in the ventricles and abdominal cavity, respectively. The subsequent survival following the surgery was analyzed using Kaplan-Meier analysis.
RESULTS:
A total of 209 patients received 255 VPSs or revisions and all the operations were successfully completed. Open operation or oraniotomy was not needed for any technical complications, while 46 revisions were performed. After the operations, 203 patients with communicating hydrocephalus exhibited improvement of symptoms following surgery. The follow-up period ranged from one month to four years; the shunt surgery efficiencies were 91.0%, 86.7%, 83.9%, and 82.0% in the first, second, third, and fourth years, respectively.
CONCLUSION:
For ventriculo-peritoneal shunt, laparoscopy and neuroendoscopy can help to implant shunt catheter in a suitable position, in the ventricles or abdominal cavity, respectively. Hence, the combination of the two techniques can reduce the failure rate of VPS, and has an obvious impact on survival following the surgery.
1.Introduction
Ventriculo-peritoneal shunt (VPS) is one of the routine methods used to treat communicating hydrocephalus; however, this neurological surgery is also associated with the highest failure rate, of which shunt blockage is the major cause [1]. In the present study, we evaluated the feasibility and efficiency of using neuroendoscopic- and laparoscopic-assisted VPS placement as a treatment for patients with communicating hydrocephalus.
2.Materials and methods
2.1Patients
From January 2010 to January 2014, neuroendoscopic- and laparoscopic-assisted VPS surgery was performed on 209 patients with communicating hydrocephalus in the Department of Neurosurgery at PLA General Hospital in China. The 209 patients consisted of 93 men and 116 women. The age of patients ranged from 7 months to 79 years, with the average age being 38.1 years. The hydrocephalus occurred postoperatively in 71 patients with ruptured aneurysm, 28 patients with hypertensive cerebral haemorrhage, 7 patients with traumatic brain injury, and 85 patients with various brain tumours (e.g., acoustic neuroma, pineal tumours, and central neurocytoma). Other causes included normal pressure hydrocephalus (
2.1.1Symptoms and signs
The main clinical manifestations included 201 cases of headache and dizziness, 119 cases of nausea and vomiting, 80 cases of walking instability, 123 cases of memory impairment, 86 cases of blurred vision and papilloedema, 36 cases of somnolence, 6 cases of seizure, and 5 cases of urinary abnormalities or incontinence. The head circumference increased in 17 cases.
2.1.2Diagnostic examination
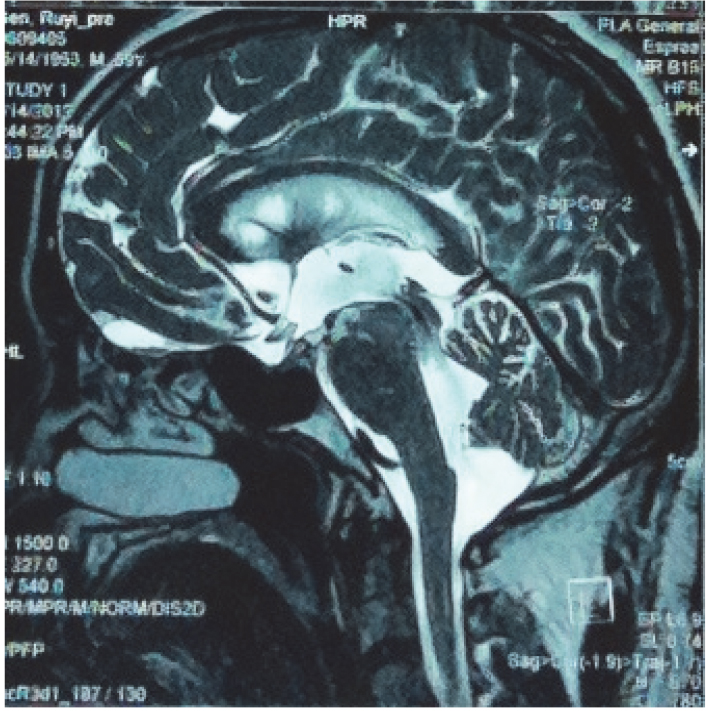
Preoperative magnetic resonance imaging (MRI) in the axial and sagittal planes was performed for all 209 patients (Figs 1 and 2) to confirm the diagnosis of communicating hydrocephalus. Lumbar puncture was performed in the two patients without obvious ventricle enlargement, based on their MRI images; together with the evaluations of their symptoms, the diagnosis of normal pressure hydrocephalus was confirmed in these two patients.
Figure 1.
A preoperative T2-weighted magnetic resonance image from a 59-year-old male patient who was admitted to our hospital owing to ‘headache for 1 year, and aggravated headache for 1 week’. The image shows ventricular enlargement and bilateral frontal horn oedema.
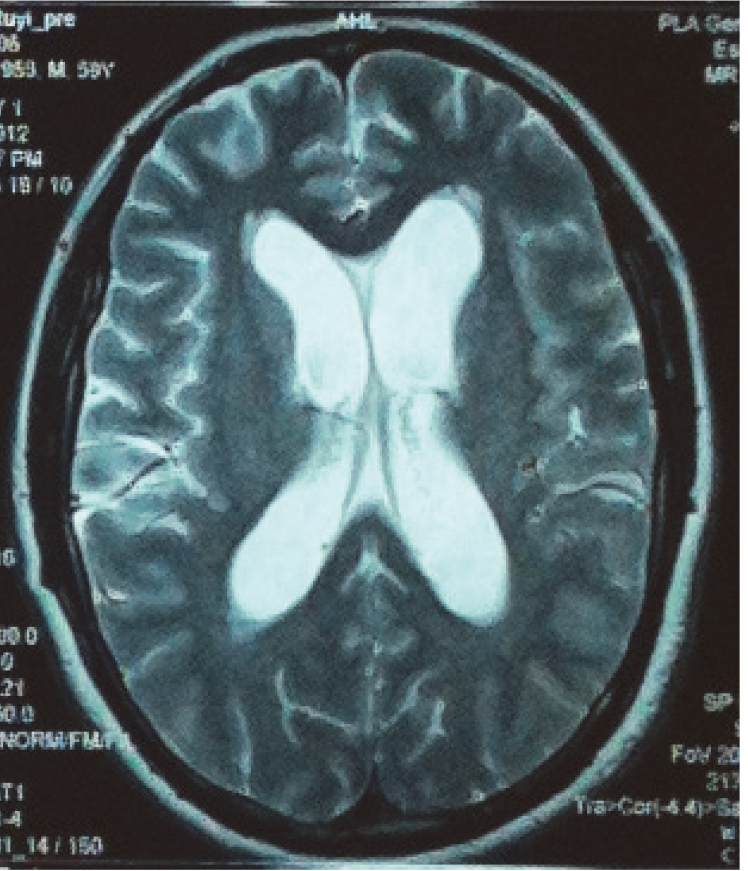
Figure 2.
A three-dimensional magnetic resonance image acquired using sampling perfection with application-optimized contrasts using different flip-angle evolution showing a clear flow void at the cerebral aqueduct, indicating communicating hydrocephalus.
2.2Surgical procedures for VPS placement
After inducing general anaesthesia using tracheal intubation, the patient was placed in a supine position without a head stabilisation device. The patient’s head was flexed and tilted about 60
2.3Follow-up evaluations
With the day after surgery being considered as day 1 of the follow-up period, the remaining follow-up evaluations were set at 1 month, 3 months, 6 months, and 1 year postoperatively. After the first year, evaluations were performed at 1-year intervals, unless the patient reported discomfort. For patients with shunt failure, the cut-off point was the date of failure. If no shunt failure occurred during the follow-up period, the last follow-up evaluation was treated as the cut-off point. The shunt surgery results were divided into two categories as follows: (1) shunt failure, which included any shunt-related complications that required surgical treatment; and (2) successful shunting, which included cases without shunt failure, according to the last imaging examination or phone interview. Cases with postoperative infection or hydrocephalus symptoms, or those diagnosed as hydrocephalus, using CT/MRI, that required surgical repair/adjustment or removal of the shunt, were categorised as shunt failure. However, cases in which conservative treatment was successful, and no operation was needed, were still categorised as successful shunting.
The causes of failure were categorised as: infection, proximal shunt obstruction, distal shunt failure, and shunt valve or connection malfunction. Infection was diagnosed based on positive bacterial cultures. Instances of shunt-valve and shunt-tubing exposure were also considered infection. Shunt blockages were assessed using a neuroendoscope or laparoscope during the operation. Only those patients in whom shunt failure was the direct cause of death were labelled as ‘deceased’, while all other cases were categorised as successful shunting, with the last follow-up evaluation treated as the cut-off point.
During surgery, cases of visceral injury, vascular injury, hernia, or resolving to open operation from laparoscopy were considered operative complications, and thus, were not categorised as shunt failures.
2.4Statistical analysis
Data were analysed using the SPSS 16.0 statistical analysis package (IBM, NY, USA). The effective survival following the VPS operations was analyzed using Kaplan-Meier plots.
3.Results
3.1Surgical results
We performed 255 VPS operations on 209 patients. All the operations were completed successfully. No craniotomies or open operations were needed for any technical complications.
3.2Clinical results
After surgery, the clinical symptoms of 203 of the patients with hydrocephalus were alleviated to varying degrees. There were 13 cases of low intracranial pressure, which improved after pressure adjustment. Brain CT of some patients, 1 week after the operation, did not show any discernible reductions in the size of the ventricular system, but the subarachnoid space was clearly visible on the brain surface. Follow-up brain CT images acquired from 189 patients, 1 month–4 years postoperatively, revealed that the size of the ventricular system was significantly lower than that before the surgery (Fig. 3), whereas the images acquired from 20 patients did not show any obvious changes. The cerebrospinal fluid pressure, as measured by lumbar puncture, 1 week postoperatively, was lower than the preoperative pressure.
3.3Follow-up results
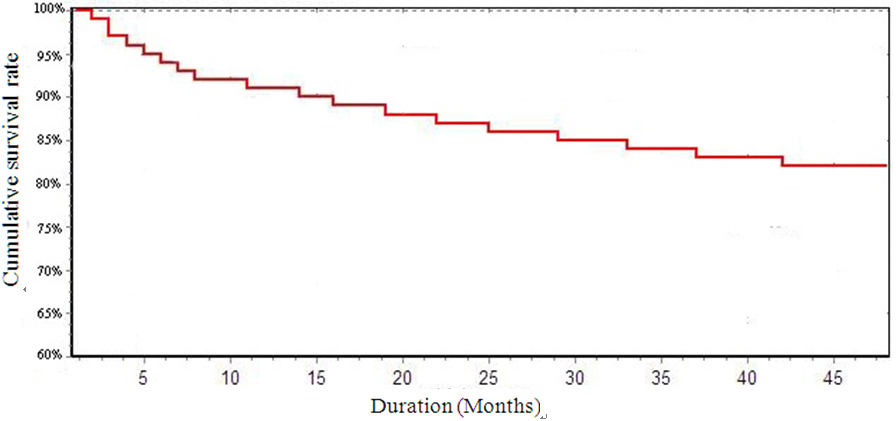
The follow-up period ranged from one month to four years, with a median of 2.1 years. No patients were lost during the follow-up period. Based on the follow-up data, the efficiency of the shunt system was 91%, 86.7%, 83.9%, and 82% at 1, 2, 3, and 4 years postoperatively, respectively. The efficiency of the shunt system across time is shown by the Kaplan-Meier plot in Fig. 4.
Figure 3.
In this follow-up computed tomogrpahy image acquired 1 month postoperatively, the shunt position at the ventricular end remained accurate. Ventricular enlargement was reduced. The frontal horn oedema was no longer visible, and the patient’s headaches were alleviated.
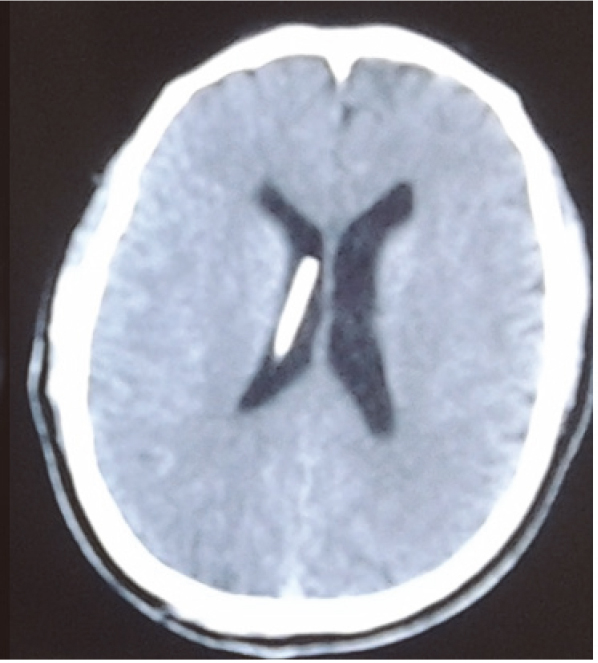
Figure 4.
The survival curve for the use of neuroendoscopic- and laparoscopic-assisted ventriculo-peritoneal shunt placement to treat communicating hydrocephalus
3.4Complications and shunt obstruction
In this study, 20 patients experienced shunt failure, requiring repair, of which 19 cases were related to catheter obstruction at the peritoneal end, while one case was related to shunt pump malfunction. No technical complications occurred at the ventricular end of the shunt. Shunt failure occurred 1–42 months after surgery. Of the 20 patients with shunt failure, 16 underwent two repair surgeries, three underwent three repair surgeries, and one underwent five repair surgeries, resulting in a total of 46 revisions. The reasons for the repairs were as follows: 7 patients had blockages at the peritoneal end, resulting from the aseptic wrapping of the omentum around the catheter opening, one patient had shunt valve malfunction, and 12 patients had infections (including one deceased patient). None of the patients experienced incisional hernia at the abdomen, intraoperative bleeding, shunt catheter exposure, or postoperative epilepsy. The patient who underwent five repair surgeries eventually died of severe infection, and the bacterial cultures were positive for Acinetobacter baumannii. Two other patients died from a primary disease that was unrelated to the hydrocephalus.
4.Discussion
4.1Neuroendoscopic-assisted VPS
Comprehensive data show that about half of the VPS obstructions are caused by ventricular terminal blockage, mainly due to wrapping of the catheter tip by the choroid plexus [2]. In this study, with the assistance of a neuroendoscope, the ventricular end of the catheter was placed at the frontal horn of the right ventricle, from Frazier’s point, via the occipital angle, which avoids choroid plexus wrapping. During the 4-year follow-up period, we did not observe blockages at the ventricular end of the catheter in any of the 209 patients in our study; thus, our ventricular obstruction rate was lower than that reported for conventional shunt insertion [3].
For patients with hydrocephalus with previous intracranial infections, more sediment debris is present in the ventricles owing to inflammatory reactions, which can cause shunt occlusion following VPS. During the neuroendoscopic-assisted VPS operation in this study, ample volume of Ringer’s lactate solution was applied, at 37
4.2Laparoscopic-assisted VPS
Compared to conventional VPS surgery, laparoscopic-assisted VPS is less invasive, and allows the surgeon to directly visualize the peritoneal shunt placement. In this study, the shunt catheter was placed accurately in the rectouterine pouch of the pelvic cavity in all 255 shunt surgeries, with the assistance of a laparoscope. Prior to completing the operation, adequate drainage was confirmed by direct visualization. At 4 years postoperatively, 82% of the shunts were still effective; this rate is higher than those reported for both traditional shunting and neuroendoscopic-assisted surgeries [4, 5]. In the present study, the incidence of infection was 5.7% (12/209), and all 12 cases of infection were due to peritoneal shunt blockage, possibly caused by peritoneal inflammation of bacteria-containing cerebrospinal fluid. The incidence of infection observed was similar to that reported by Naftel et al. in their study of 810 patients who underwent laparoscopy-assisted catheter placement, and that reported for traditional catheter insertion through open operation [6].
For laparoscopy-assisted shunt operations, the shunt tip is usually placed in the rectouterine pouch of the pelvic cavity or in the hepatodiaphragmatic space. In the latter case, in-situ fixation of the catheter is required, which is not optimal for younger patients who are still growing. In our study, all catheters were placed in the rectouterine pouch of the pelvic cavity. During the 4-year follow-up period, 7 of the 209 patients developed aseptic wrapping of the omentum around the catheter tip, which is lower than the ratio reported by Naftel et al. for a larger population [6]. We considered the cause of inclusion in these 7 cases to be aseptic inflammation of the abdominal cavity, stimulated by the high level of proteins in the cerebrospinal fluid, and pseudocysts caused by the accumulation of the cerebrospinal fluid.
Laparoscopic-assisted surgery has several disadvantages, including pneumoperitoneum-induced cardiovascular and respiratory abnormalities. Additionally, Argo et al. [7] reported one case in which a liver cyst was accidentally punctured during laparoscopic-assisted surgery. Similarly, Danan et al. reported a case of accidental piercing of the abdominal aorta, and subsequent haemorrhagic shock, in a patient whose spine projected forward, and in whom the abdominal aorta was pressing against the anterior abdominal wall [8]. The patient eventually died of complications related to multiple organ failure.
4.3Combined utility of neuroendoscopy and laparoscopy during VPS surgery
At present, an increasing number of VPS operations are performed with the assistance of either neuroendoscopy or laparoscopy; however, only a few studies have used both techniques to assist in VPS placement [9, 10]. In the present study, VPS placement was performed under the combined assistance of neuroendoscopy and laparoscopy, which permitted both the ventricular and peritoneal termini of the shunt to be placed at the optimal anatomical locations. The 4-year efficiency of shunts placed using this approach was 82%, which is higher than that of the shunts placed via conventional shunting operations and shunting operations assisted by neuroendoscopy or laparoscopy alone [4, 5]. These findings indicate that using both neuroendoscopy and laparoscopy during shunt placement is preferable to traditional methods.
According to Villavicencio et al, using neuroendoscopy to assist in shunting may reduce the occurrence of ventricular end obstruction, but increase the possibility of peritoneal end obstruction, thus, reducing the long-term efficiency of the shunt [5]. The authors reported that the increased likelihood of peritoneal end obstruction is due to the frequent inspection of the ventricles with the endoscope during neuroendoscopic-assisted surgery, which causes mechanical injury to the brain parenchyma, thereby producing more debris and increasing the amount of protein in the cerebrospinal fluid. Additionally, the opening of the peritoneal catheter is often slit-like, which produces brain-tissue debris and blood during neuroendoscopic-assisted surgery; this debris may then block the slit-like tip of the peritoneal catheter, resulting in a higher risk of peritoneal section obstruction.
Similar observations were made in this study, as most of the shunt failures were related to complications in the abdominal cavity, while none of the 209 patients developed ventricular end obstruction. However, the shunt efficiency in the present study was higher than that reported by Villavicencio et al. [5]. One potential explanation for the higher efficiency reported in the present study is that although laparoscopy-assisted intraperitoneal catheterization may produce blockages at the slit-like opening of the peritoneal catheter owing to ventricular debris and blood flowing along the catheter, the continuous flushing performed with Ringer’s lactate solution throughout the neuroendoscopic-assisted portion of the surgery may have removed much of the brain-tissue debris and blood. Despite its drawbacks, laparoscopic-assisted VPS surgery is beneficial because it permits exact catheter placement, and is minimally invasive.
Currently, the infection rate during shunting operations remains controversial. Several studies have reported reduced infection rates for laparoscopy-assisted shunting operations, and suggested that these reductions were related to the semi-closed state of the abdomen during laparoscopic surgery [11, 12]. In contrast, other studies have not reported any alterations in the infection rate, with the authors proposing an increased possibility of infection during neuroendoscopic- and laparoscopic-assisted surgery, since both general surgeons and neurosurgeons participate in the operation [6, 13]. In our study, only the first two surgeries were performed with the aid of general surgeons, with the remaining operations performed solely by neurosurgeons. However, even without both groups of doctors, our infection rate was close to that reported for the traditional operation. Therefore, we do not believe that laparoscopic-assisted VPS surgery reduces the incidence of infection.
5.Conclusion
In conclusion, our results suggest that using both neuroendoscopy and laparoscopy during VPS surgery for patients with hydrocephalus is feasible and beneficial. Specifically, neuroendoscopy helps to ensure that the catheter is accurately placed at the desired location at the ventricular end, while laparoscopy allows minimally invasive and accurate catheter insertion at the abdominal cavity. The joint application of both techniques improves the success rate of the surgery, reduces surgical trauma and complications, and is in line with the requirements of minimally invasive neurosurgery. With the development and popularization of endoscopic surgical techniques, VPS surgery assisted by neuroendoscopy and laparoscopy may be an optimal treatment strategy patient with communicating hydrocephalus.
Conflict of interest
None to report.
References
[1] | Drake JM, Kestle JR, Milner R, et al. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery, (1998) ; 43: (2): 294-303. |
[2] | Wang Z. Ventriculo-peritoneal shunt in the treatment of traumatic hydrocephalus in adults through the frontal approach. China Practical Medical, (2007) ; 2: (20): 63-64. |
[3] | Cao M, Yu R, Dong W. Analysis and treatment of common complications after ventriculo peritoneal shunt. Chinese Journal of Clinical Neurosurgery, (2011) ; 16: (10): 621-622. |
[4] | Chen X, Wu X, Qi T, et al. Survival analysis of ventriculoperitoneal shunts with or without endoscopic assistance. Chinese Journal of Neuromedicine, (2006) ; 5: (5): 506-509. |
[5] | Villavicencio AT, Leveque JC, McGirt MJ, et al. Comparison of revision rates following endoscopically versus nonendoscopically placed ventricular shunt catheters. Surgical Neurology, (2003) ; 59: (5): 375-379. |
[6] | Naftel RP, Argo JL, Shannon CN, et al. Laparoscopic versus open insertion of the peritoneal catheter in ventriculoperitoneal shunt placement: review of 810 consecutive cases. J Neurosurg, (2011) ; 115: (1): 151-158. |
[7] | Argo JL, Yellumahanthi DK, Ballem N, et al. Laparoscopic versus open approach for implantation of the peritoneal catheter during ventriculoperitoneal shunt placement. Surg Endosc, (2009) ; 23: (7): 1449-1455. |
[8] | Danan D, Winfree CJ, McKhann GM. Intra-abdominal vascular injury during trocar-assisted ventriculoperitoneal shunting: case report. Neurosurgery, (2008) ; 63: (3): E613. |
[9] | Feng B, Cai M, Sun Y, et al. Clinical analysis of ventriculo-peritoneal shunt assisted by neuroendoscope and laparoscope in the treatment of hydrocephalus. Chinese Journal of Practical Neruous Diseases, (2011) ; 14: (9): 80-82. |
[10] | Graff-Radford NR. Normal pressure hydrocephalus. Neurol Clin, (2007) ; 25: (3): 809-832. |
[11] | Yi F, Bai J, Ma J, et al. Clinical research of laparoscope-assisted ventriculoperitioneal shunt for treating hydrocephalus. Chongqing Medical Journal, (2012) ; (13): 1270-1271. |
[12] | Roth J, Sagie B, Szold A, et al. Laparoscopic versus non-laparoscopic-assisted ventriculoperitoneal shunt placement in adults. Surg Neurol, (2007) ; 68: (2): 177-184. |
[13] | Kast J, Duong D, Nowzari F, et al. Time-related patterns of ventricular shunt failure. Child’s Nervous System, (1994) ; 10: (8): 524-528. |




