Can tibia-first total knee arthroplasty using computer-assisted system improve anterior and posterior knee stability?
Abstract
BACKGROUND:
Total knee arthroplasty (TKA) is a widely performed procedure to alleviate pain and restore function of patients with end-stage knee osteoarthritis.
OBJECTIVE:
The study aim was to determine if tibia-first (TF) total knee arthroplasty (TKA) using a novel computer-assisted surgery (CAS) system can yield better anterior and posterior (AP) knee stability.
METHODS:
Patients with knee osteoarthritis with obvious varus knee who met the indication for and underwent TKA from May 2019 to November 2020 were included. Forty-one measured resection (MR)-TKAs and 32 TF-TKAs were compared. The varus-valgus ligament balance and joint tension at a joint center-gap setting equal to the tibial-baseplate thickness were measured, and appropriate polyethylene inserts with 0
RESULTS:
The horizontal gap balance was significantly closer in the TF-TKA group than the MR-TKA group for 0
CONCLUSION:
TF-TKA using a novel CAS system provided better AP knee stability with close to horizontal gap balances.
1.Introduction
Total knee arthroplasty (TKA) is a widely performed procedure to alleviate pain and restore function of patients with end-stage knee osteoarthritis (KOA). Prerequisites of successful TKA are restoring coronal mechanical alignment within 3
Computer-assisted surgery (CAS) for TKA has become widely used since the mid-2000s [2], and CAS-TKA has been reported to provide better sagittal and coronal component alignment [3]. On the other hand, however, better functional outcome or longer implant survivability after navigation-assisted TKA has not been demonstrated from past studies using registry data [4]. A plausible reason is that most CAS systems can provide only static information for 0
The “tibia-first” (TF) technique uses the tibial resection plane to guide femoral component rotation, which removes the need for identification of individual landmarks on the distal femur to identify a reference axis and may have the advantage of predicting the final soft-tissue balance before femoral osteotomies [8]. This technique might result in good ligamentous balance without excessive soft-tissue release and lead to accurate femoral resection.
Therefore, we hypothesized that better AP knee stability could be achieved by TF-TKA using a novel CAS system than by the conventional measured resection technique (MR)-TKA. The purpose of this study was to test this hypothesis.
2.Material and methods
2.1Patient enrollment
Institutional Bioethics Committee for Medical Research approved the study and waived the requirement for informed consent from individual participants (Approval ID: A20-067). Patients with KOA with varus knee who met the indication for and underwent TKA from May 2019 to November 2020 were included, and MR-TKA was performed from May 2019 until February 2020. TF-TKA was performed from March 2020 to November 2020. All surgeries were performed by one senior board-certified orthopedic surgeon.
The indication of TKA was diagnosed on the basis of clinical findings, such as a decreased ROM, decline in activities of daily living, and radiological findings according to the Kellgren-Lawrence classification. The exclusion criteria were history of previous TKA who planned to undergo revision surgery, patients after high-tibial osteotomy, or patients with previous collateral ligament injury because of the potential effects of these conditions on postoperative AP knee stability.
2.2Surgical procedure for the MR technique
MR-TKAs were performed by using a cruciate-retaining, cemented, fixed-bearing implant (Attune; DepuySynthes, Inc., Warsaw, IN, USA) using a mid-vastus approach. Pneumatic tourniquets were applied to all patients. The anterior cruciate ligament was dissected and the posterior cruciate ligament (PCL) was retained in all cases. Patella resurfacing was not performed. Infrapatellar fat pad excision was only performed when the surgical visual field was insufficient and was minimized to avoid anterior knee pain [9]. We performed a mechanically aligned TKA to achieve neutral coronal mechanical limb alignment by making the femoral and tibial bone cuts such that the rectangular flexion and extension gaps were perpendicular to the mechanical axes. The surgery was performed according to the manufacturer’s instructions. The distal femoral cut was made by using an intramedullary alignment system. The posterior femoral cuts were made with a referencing guide to make the bony resection line parallel to the surgical epicondylar line and perpendicular to Whiteside’s line. The proximal tibial cut was made by using an extramedullary alignment system. Significant posterior osteophytes were removed. Trial components were inserted, and the ROM of the knee and other intraoperative parameters were checked as described above. Release of the collateral and retinacular ligaments to balance the flexion and extension gaps was not performed. The definitive components were introduced with cement fixation, and a final evaluation of the ROM was made.
2.3Surgical procedure of the TF technique using a CAS
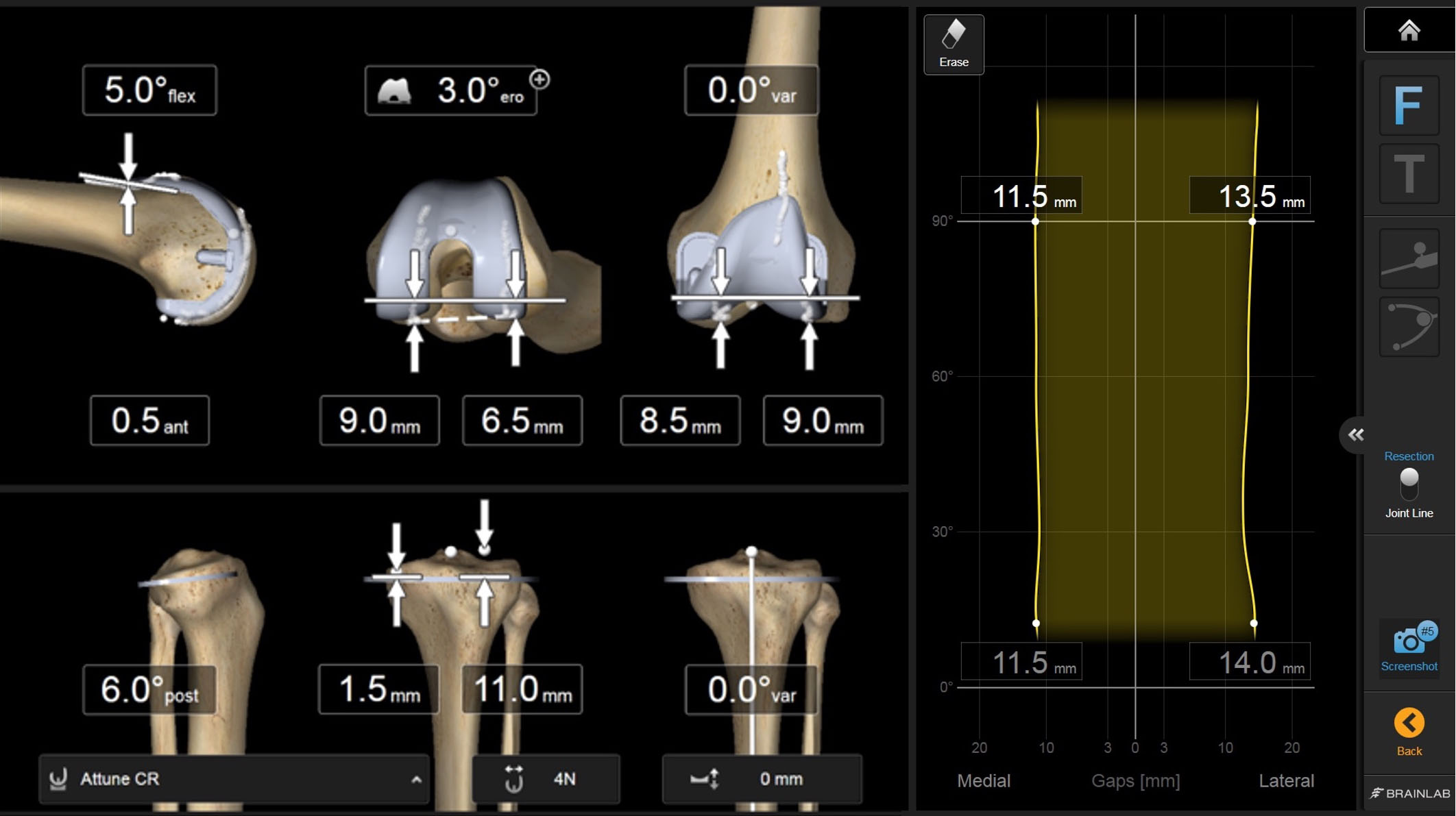
TF-TKAs were performed by using the same implant and approach as used for the MR technique. First, anatomical landmarks and the individual biomechanical knee data were obtained; the ROM, varus-valgus angles of the leg axis, and gap sizes throughout the entire ROM were obtained at the beginning of surgery for registration of the navigation system [5]. A tibial osteotomy was first performed to ensure that the tibial bony resection was perpendicular to the anatomical tibial axis. Insertion of the PCL was protected by creating a bony island if necessary. After tibial bony resection, the necessary osteophyte removal was performed but medial collateral ligament (MCL) release, if required, was not performed. Following the tibial bony resection, the gap sizes were measured dynamically by performing varus-valgus stress tests for the medial and lateral gaps to balance the extension gap by using a tibial trial component. Those stress tests were performed from extension to full flexion. The amount of distal femoral osteotomy was determined parallel to the tibia shown on the screen of the navigation system. Then, the amount of the posterior femoral osteotomy and varus-valgus balance were determined on the screen of the navigation system to create an adequate gap. Based on the gaps obtained, the femoral component position was planned to reach total balance, meaning identical medial and lateral gaps throughout the entire ROM (Fig. 1). The distal femoral cut was made first followed by the dorsal cut. The same dynamic varus-valgus stress tests after femoral resections with all trial components placed were performed. The definitive components were introduced with cement fixation, and a final evaluation of the ROM was made.
Figure 1.
The right screen shows a graph of gaps from full knee extension to full flexion. The lateral gap is shown on the right side, and the medial gap is shown on the right side. The left screen shows the component alignments and estimated widths of bony resection.
2.4Intraoperative joint-gap measurement using a tensor
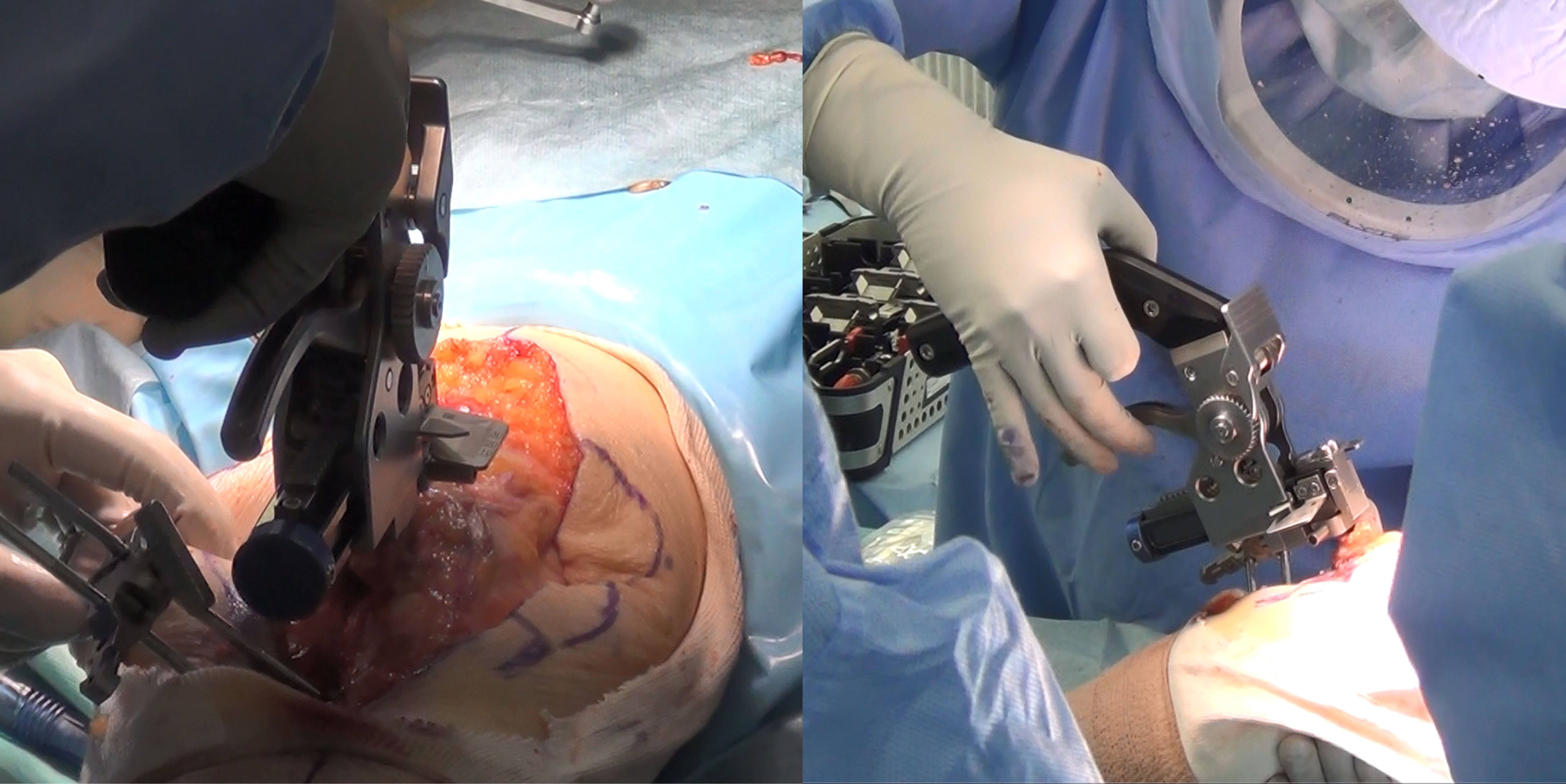
Following each bony resection, we fixed the tensor and femoral trial prostheses, and the patella was reduced. At this point, we measured the varus-valgus ligament balance and a joint tension at a joint center-gap setting equal to the tibial baseplate thickness, and appropriate polyethylene inserts of 0
Figure 2.
Measurements of the varus-valgus ligament balance and joint tension at a joint center-gap setting equal to the tibial baseplate and an appropriate polyethylene insert.
2.5Postoperative measurement of AP laxity by using a Kneelax 3 arthrometer
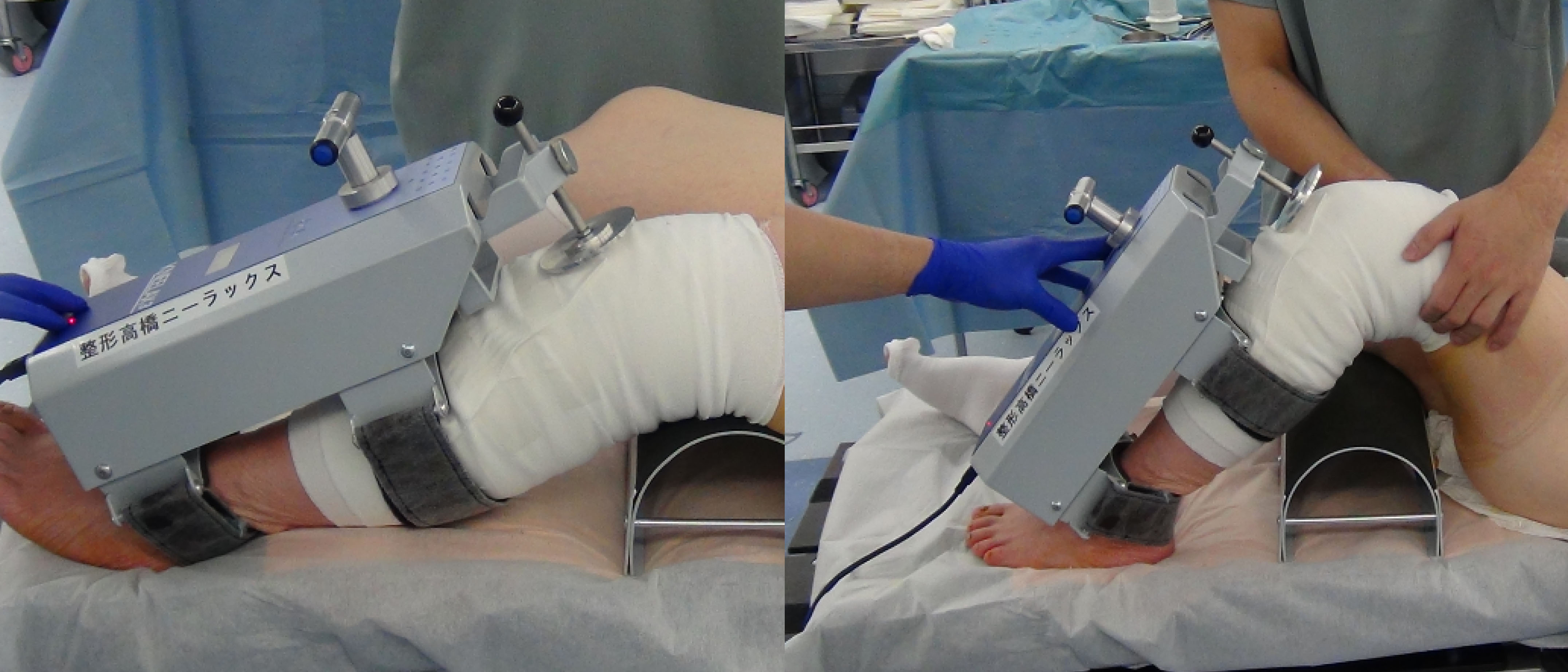
Immediately after surgery, anesthetized patients underwent knee AP laxity measurement by using a Kneelax 3 arthrometer with 30
Figure 3.
Postoperative knee AP laxity measurements made by using a Kneelax 3 arthrometer at 30
2.6Statistical analysis
Data are presented as the mean and standard deviation. A priori power analysis was performed by using G* Power 3.1 (Franz Paul, Kiel, Germany). A sample size of 19 patients in the TF-TKA group and 38 patients in the MR-TKA group was calculated to achieve 80.2% power with an effect size of 0.8 to test the null hypothesis. There were 32 patients in the TF-TKA group and 41 patients in the MR-TKA group, and post hoc analysis showed 91.7% power with an effect size of 0.8. Values of
3.Results
3.1Patient characteristics
A total of 73 patients, 32 in the TF-TKA group and 41 in the MR-TKA group, were included, with 26 males and 47 females and an average age of 72.5
Table 1
Patient demographics
| Parameter | |
|---|---|
| Sex | 26 males/47 females |
| Age (years) | 72.5 |
| HKA | 12.2 |
HKA denotes the hip-knee angle in degrees.
Table 2
Comparisons of preoperative backgrounds
| TF-TKA | MR-TKA | ||
|---|---|---|---|
| Male/female | 13/19 | 13/28 | 0.47 |
| Age (years) | 73.3 | 71.8 | 0.37 |
| Preoperative HKA ( | 13.4 | 10.6 | 0.063 |
HKA, MR, and TF denote; hip knee angle, measured resection, and tibia first, respectively.
3.2Comparisons of bony resection width
No significant differences in the width of bony resection in the distal femur and proximal tibia on the medial and lateral sides and in the dorsal femur on the lateral side between the TF-TKA and MR-TKA were observed. On the other hand, the width of bony resection in the dorsal femur on the medial side was significantly smaller in the TF-TKA group than in the MR-TKA group (9.0
Table 3
Comparisons of the width of bony resection measurements
| TF-TKA | MR-TKA | ||||
|---|---|---|---|---|---|
| Distal femur (mm) | |||||
| Medial | 7.6 | 7.0 | 0.066 | ||
| Lateral | 6.7 | 7.0 | 0.20 | ||
| Dorsal femur (mm) | |||||
| Medial | 9.0 | 9.8 | 0.039 | ||
| Lateral | 6.8 | 6.8 | 0.93 | ||
| Proximal tibia (mm) | |||||
| Medial | 4.4 | 3.5 | 0.098 | ||
| Lateral | 10.4 | 10.7 | 0.37 | ||
3.3Comparisons of intraoperative joint-gap measurements using a tensor
The horizontal gap balance was significantly closer in the TF-TKA group than in the MR-TKA group with 0
Table 4
Comparisons of gap-balance measurements
| Knee-flexion angle | TF-TKA ( | MR-TKA ( | |||
|---|---|---|---|---|---|
| 0 | 0.25 | 2.4 |
| 0.001 | |
| 30 | 0.094 | 1.6 | 0.0018 | ||
| 45 | 1.3 | 0.0046 | |||
| 60 | 1.1 | 0.022 | |||
| 90 | 0.13 | 0.95 | 0.19 | ||
| 120 | 0.94 | 1.5 | 0.37 | ||
Table 5
Comparisons of gap-tension measurements
| Knee-flexion angle | TF-TKA (lbf) | MR-TKA (lbf) | |
|---|---|---|---|
| 0 | 20.3 | 19.2 | 0.49 |
| 30 | 16.5 | 17.4 | 0.55 |
| 45 | 18.1 | 18.0 | 0.99 |
| 60 | 18.4 | 18.3 | 0.97 |
| 90 | 19.2 | 19.1 | 0.96 |
| 120 | 22.7 | 21.8 | 0.55 |
3.4Comparisons of intraoperative AP laxity measurements
Translation was significantly smaller in the TF-TKA group than in the MR-TKA group for AP laxity with 30
Table 6
Comparisons of postoperative anterior-posterior knee-laxity measurements
| TF-TKA | MR-TKA | ||
|---|---|---|---|
| AP translation of 30 | 8.8 | 10.7 | 0.0079 |
| AP translation of 90 | 7.2 | 7.2 | 0.91 |
AP, MR, and TF denote; anterior-posterior, measured resection, and tibia first, respectively.
4.Discussion
There were several main findings in this study. First, postoperative AP laxity after TKA was significantly smaller in the TF-TKA group than in the MR-TKA group for 30
We aim to achieve equal medial and lateral gaps when we perform TKA [11], and those gaps ideally should be equal throughout the entire ROM [12]. However, conventional static gap measurements were made only at extension and at 90
The surgical principle of TF-TKA is that it respects the integrity of soft tissues. It is a common observation that soft-tissue release is significantly reduced by using computer navigation [15]. Following proximal tibia resection, we used a navigation system to determine the extension and rotational alignments of the femoral component based on the gap sizes measured dynamically by performing varus-valgus stress tests for the medial and lateral gaps to balance the extension gap by using a tibia trial component. Subsequently, we performed distal and posterior femoral resections. A potential advantage of using the TF-TKA is that it can prevent mismatch before and after resection of the femoral posterior condyle and placement of the femoral component [8]. In addition, bony resection can be set with increments of 0.5 mm and angles with increments of 0.5
4.1Limitations
There were several limitations in this study. First, we did not assess the interobserver variation in instrumental measurements for the reason mentioned earlier. Second, all TKA surgeries were CR-TKAs performed by one consultant knee surgeon who used the mid-vastus approach. Therefore, these results cannot be generalized to TKAs using others approaches or to posterior-stabilized TKA. Third, a comparison between pre- and postoperative joint lines was not performed in this study but is a topic for future investigation. Fourth, it is uncertain if the lesser AP knee stability in both the mid- and deep-flexion angles and the closer to horizontal gap balances in extension-to-mid-flexion knee angles were related to the TF technique, use of the novel CAS system, or a combination of both. A future separate analysis would be required to answer this important clinical question.
Despite these limitations, this study is the first to show that TF-TKA using a novel CAS system achieved better AP knee stability in mid- and deep-flexion angles than those achieved by using the conventional MR-TKA, with closer to horizontal gap balances in extension-to-mid-flexion knee angles. Future comparative studies would be required to determine if these findings will result in better clinical outcomes and patient satisfaction.
5.Conclusions
This study showed that better AP knee stability in mid-flexion angles and closer to horizontal gap balances were achieved by TF-TKA using a novel CAS system than by MR-TKA.
Conflict of interest
None to report.
References
[1] | Figgie HE, 3rd, Goldberg VM, Figgie MP, Inglis AE, Kelly M, Sobel M. The effect of alignment of the implant on fractures of the patella after condylar total knee arthroplasty. J Bone Joint Surg Am. (1989) ; 71: (7): 1031-9. |
[2] | Lee CM, Dhillon MK, Sulaiman MA. A computer-assisted, tibia-first technique for improved femoral component rotation in total knee arthroplasty. Arthroplast Today. (2018) ; 4: (1): 78-84. |
[3] | Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplasty. (2012) ; 27: (6): 1177-82. |
[4] | Roberts TD, Clatworthy MG, Frampton CM, Young SW. Does computer assisted navigation improve functional outcomes and implant survivability after total knee arthroplasty? J Arthroplasty. (2015) ; 30: (9 Suppl): 59-63. |
[5] | Mehliss V, Strauch Leira M, Serrano Olaizola A, Scior W, Graichen H. Proven accuracy for a new dynamic gap measurement in navigated TKA. Knee Surg Sports Traumatol Arthrosc. (2019) ; 27: (4): 1189-95. |
[6] | Matsumoto T, Takayama K, Muratsu H, Ishida K, Hashimoto S, Hayashi S, et al. Relatively loose flexion gap improves patient-reported clinical scores in cruciate-retaining total knee arthroplasty. J Knee Surg. (2018) ; 31: (6): 573-9. |
[7] | Keggi JM, Wakelin EA, Koenig JA, Lawrence JM, Randall AL, Ponder CE, et al. Impact of intra-operative predictive ligament balance on post-operative balance and patient outcome in TKA: A prospective multicenter study. Arch Orthop Trauma Surg. (2021) ; 141: (12): 2165-74. |
[8] | Matsumoto T, Muratsu H, Kubo S, Matsushita T, Ishida K, Sasaki H, et al. Soft tissue balance using the tibia first gap technique with navigation system in cruciate-retaining total knee arthroplasty. Int Orthop. (2012) ; 36: (5): 975-80. |
[9] | Duan G, Liu C, Lin W, Shao J, Fu K, Niu Y, et al. Different factors conduct anterior knee pain following primary total knee arthroplasty: A systematic review and meta-analysis. J Arthroplasty. (2018) ; 33: (6): 1962-71 e3. |
[10] | Shi X, Shen B, Kang P, Yang J, Zhou Z, Pei F. The effect of posterior tibial slope on knee flexion in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2013) ; 21: (12): 2696-703. |
[11] | Whiteside LA, Kasselt MR, Haynes DW. Varus-valgus and rotational stability in rotationally unconstrained total knee arthroplasty. Clin Orthop Relat Res. 1987: (219): 147-57. |
[12] | Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA. Soft-tissue balancing during total knee arthroplasty in the varus knee. J Am Acad Orthop Surg. (2009) ; 17: (12): 766-74. |
[13] | Ramappa M. Midflexion instability in primary total knee replacement: A review. SICOT J. (2015) ; 1: : 24. |
[14] | Wilson CJ, Theodoulou A, Damarell RA, Krishnan J. Knee instability as the primary cause of failure following Total Knee Arthroplasty (TKA): A systematic review on the patient, surgical and implant characteristics of revised TKA patients. Knee. (2017) ; 24: (6): 1271-81. |
[15] | Lee DH, Park JH, Song DI, Padhy D, Jeong WK, Han SB. Accuracy of soft tissue balancing in TKA: Comparison between navigation-assisted gap balancing and conventional measured resection. Knee Surg Sports Traumatol Arthrosc. (2010) ; 18: (3): 381-7. |




