The relationship between forward head posture and neck pain disability in chronic whiplash-associated disorders
Abstract
PURPOSE:
To investigate the association between forward head posture (FHP) and neck pain disability in patients with chronic whiplash associated disorders (WAD).
METHODS:
This study was a secondary analysis based on data from a randomized controlled study. The study involved patients with chronic WAD reporting their disability using the Neck Disability Index (NDI). FHP was measured with a goniometer. Analyses of correlations and logistic regressions were performed controlling for age, gender, duration of symptoms, WAD-grade (the Quebec Task Force on Whiplash-Associated Disorders classification), bodily pain (the Short-Form 36 Health Survey (SF-36) and kinesiophobia, an irrational fear of physical movement and activity (the Tampa Scale of Kinesiophobia (TSK-SV).
RESULTS:
The inclusion criteria was fulfilled by 113 patients (81 women, 32 men). Mean age 48.1 years. Mean duration of symptoms 9.7 years. There was no significant correlation between FHP and neck pain disability (rs = 0.004, p = 0.968). A logistic regression analysis showed no significance for FHP neither with (p = 0.418) nor without (p = 0.991) control for age, gender, duration of symptoms, WAD-grade, kinesiophobia and bodily pain. In the multiple model kinesiophobia (p = 0.013) and bodily pain (p = < 0.001) were the only significant predictors. Kinesiophobia was also significantly correlated with both neck pain disability (rs = 0.467, p < 0.001) and FHP (rs = 0.202, p = 0.047), thus being a confounder to the possible correlation between these variables.
CONCLUSIONS:
There is no significant correlation between neck pain disability and FHP for patients with chronic WAD. Results suggest that physiotherapists should increase their focus on kinesiophobia, since it is associated with both FHP and neck pain disability.
1Introduction
A whiplash injury may occur when the head moves rapidly back and forth, as a result of the acceleration/deceleration forces that affect the neck [1]. These injuries are primarily caused by motor vehicle collisions, although they can also follow as a result of other accidents, and lead to clinical complaints that are referred to as “whiplash-associated disorders” (WAD) [1]. The most common complaint is neck pain but a number of other symptoms such as headache, dizziness, visual symptoms, auditory symptoms and paraesthesia can occur [1, 2]. It is likely that WAD results from cervical sprain or strain although the exact pathophysiology is not known [3]. WAD can be of short duration, up to one month, but can also persist up to 17 years or more [2, 4, 5].
“The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders” (BJD), have conducted a systematic review and a best evidence synthesis on neck pain and its associated disorders, including WAD [6]. According to BJD, globally 50% of the patients are still affected one year after their injury [7]. Approximately half of these patients experience persistent moderate/severe pain and disability, the other half having milder levels of pain and disability [8]. Different mechanisms seem to be involved in sustaining the pain complaints in WAD. While evidence suggests that hypersensitivity of the central nervous system plays a significant role, the underlying mechanisms of this central sensitization is still unclear [9]. Also psychological and sociodemographic factors may be potential contributors to the development of chronic pain and disability in patients with WAD, although the results are equivocal [10].
The incidence of reported WAD in Western countries has increased during the period 1970 to 2000 [3]. In North America and Western Europe the annual incidence is likely to be at least 300 per 100 000 inhabitants (0.3%) [3]. Although a more recent, but smaller, Swedish study conducted during the period 2000–2009 show a lower annual incidence (235 per 100 000 inhabitants) [11]. Even if females seem to be at slightly greater risk of developing WAD, the gender association is still unclear [3].
Severity of symptoms at the time of injury (WAD-grade according to the Quebec Task Force on Whiplash-Associated Disorders (QTF) classification [1]) is a risk factor for slower recovery in patients with WAD [7, 12]. WAD-grade is rated 0–4: Grade 0 equals no complaint about the neck and no physical sign(s). Grade 2 equals neck complaint and musculoskeletal sign(s). Grade 4 equals neck complaint and fracture or dislocation [1]. It is also suggested that WAD-grade is related to neck pain disability six months post injury [13].
Patients with chronic WAD have been shown to have significantly more forward head posture (FHP) than controls without neck problems [14]. FHP is defined as a posture were the head is anterior to the theoretical plumb line through the center of gravity of the body [15]. Among physiotherapists, there seems to be a lack of consensus on optimal posture [16].
FHP increases the activity in cervical extensor muscles in asymptomatic subjects [17, 18]. At FHP the moment arm and the load moment increases, which consequently increases the muscle activity in order to support the weight of the head/neck [17, 18]. It is possible that the higher levels of muscle activity, which could elevate the levels of muscle strain and loading of cervical spine structures, can contribute to the development of neck pain [17]. However, it is unclear if FHP predisposes for neck pain or if neck pain causes a more extensive FHP [19].
Both patients with WAD and patients with insidious onset neck pain are shown to have a dysfunction in the deep cervical flexor muscles [20, 21]. Specific deep cervical muscle exercises can improve both neck disability, pain intensity, forward head posture and neck-muscle strength in patients with chronic mechanical neck pain [22–24].
FHP is significantly correlated with both neck pain disability and pain severity in patients with chronic neck pain [15, 25], and neck pain of unclear duration [26], of non-traumatic origin. Though when age and gender is taken into account, the significance decreases or disappears [15, 26].
Studies have identified neck pain intensity and kinesiophobia as important contributors to neck pain disability in WAD [27, 28]. However, it remains unclear whether FHP impacts neck pain disability in WAD. Since WAD is the result of an injury that can occur at any age, it may be relevant to separate the effect of age from the effect of the duration of symptoms as factors affecting disability.
The objective of this study was to investigate the association between FHP and neck pain disability in patients with chronic WAD.
2Materials and methods
2.1Study design
This study was a secondary analysis based on data from a randomized controlled study published elsewhere [29]. The recruitment process and eligibility criteria for this study were the same as for the intervention study, as described below.
2.2Participants
All patients with a medical diagnosis of whiplash injury (assessed by their general practitioner) and/or the term whiplash mentioned anywhere in the electronic medical record were extracted. The search included the electronic medical records of all 30 primary health care centres in Southern Älvsborg County, Sweden [29]. Southern Älvsborg County is located in the southwest of Sweden with a mixture of urban, village and rural conditions, and a population of approximately 270 000 [29].
Based on sample size calculations of the intervention study and expected response rates, about half of these patients were randomly contacted via a mailed survey with the patient-reported outcomes and consent information [29]. To be eligible for inclusion patients were required to have had a whiplash injury with WAD-grade I, II or III according to the QTF classification [1], report that they currently had pain and to have visited any of the primary health centres in Southern Älvsborg County during 2001 to 2005 [29]. Patients were not eligible if they suffered from other comorbid conditions that would interfere with treatment and/or measurement of outcomes, for example contraindication to exercise or other painful conditions, and/or had poor comprehension of the Swedish language [29]. Eligible patients were invited for a visit to the research centre to conduct measurements.
The computerized search of the electronic medical journal identified 3 570 individual patients [29]. A random sample of 1 573 patients were selected for contact by a mailed survey, 996 responded. Of these patients, 372 were eligible for inclusion. The patients were invited for a visit to the research centre to conduct measurements. The study size was arrived at in the intervention study and was therefore fixed at 113 patients [29].
Ethical approval for the clinical trial, which the current study was based on, was obtained from the regional ethics review board in Gothenburg (DNR 500–06).
2.3Procedure
Data on neck pain disability, age, gender, duration of symptoms, kinesiophobia and bodily pain was obtained in the mailed survey. The outcome assessor (AS), a registered physiotherapist, conducted a clinical examination to establish the WAD-grade and measure FHP during the visit to the research centre [29]. The potential bias in manual assessment of head posture was reduced since it was conducted by only one assessor.
2.4Outcome measures
2.4.1Neck pain disability
The Neck Disability Index (NDI) was used assessing self-rated pain-related disability associated with activities of daily living [30]. It consists of ten items, each scored 0–5 points for a maximum score of 50 [30]. Higher scores represent greater disability [30]. The NDI has good validity (Cronbach’s alpha 0.74–93) and test-retest reliability (0.90 –0.93) [31–33].
2.4.2Measurement of FHP
FHP was measured with the goniometer procedure described by Nilsson et al and Engh et al. [14, 34], a method which is quick and easy to use. A universal goniometer (OB Rehab AB, Solna, Sweden) was used to measure FHP in degrees. When measured the participants stood barefoot and bare from the waist up (women wore a brassiere). Participants were instructed to “stand as usual, looking forward with your arms at your sides”. The centre of the goniometer’s protractor was placed at the level of the orifice of the external ear on the left side. The fixed arm was held vertically. A spirit level was attached to it, to confirm the vertical alignment. The moving arm rested on the patients left shoulder. Higher degrees were equivalent with increased FHP. For goniometer position, see Fig. 1. This method of measuring head posture has a high intra- and inter-rater reliability [14, 34].
Fig. 1
Goniometer position in measurement situation.

2.4.3Measurement of kinesiophobia
Kinesiophobia was measured with the Swedish version of the Tampa Scale of Kinesiophobia (TSK-SV) [35]. The TSK-SV consists of 17 statements addressing self-rated fear of (re)injury due to movement or activities [35]. Each item has a 4-point scale ranging from 1–4, the total sum score range from 17 to 68 [35]. Higher scores indicate higher levels of kinesiophobia [35]. The TSK-SV is reliable for patients with WAD [36]. It is considered to have acceptable face and content validity [35].
2.4.4Measurement of bodily pain
Bodily pain was measured with the pain subscale of the Short-Form 36 Health Survey, version 2 (SF-36) [37]. Scores ranging from 0–100 [38]. Higher scores indicate less pain [39]. The SF-36 is a responsive instrument for measuring pain in patients with chronic WAD [37, 39].
2.5Variable category and categorization
For some of the analyses, neck pain disability (NDI) was categorized in two groups with a total sum score below/above 20 (0–20 versus > 20) in order to use logistic regression. The reason for choosing this cut off value was that it is in the middle of the scoring interpretation for the NDI [30], and that an NDI score > 20 is significantly related to poor outcome 3 years after the injury [40]. Only one patient in the sample had WAD grade I. This patient was merged into WAD grade II to simplify the analyses.
2.6Data analysis
The outcome measures were neck pain disability, FHP, age, gender, duration of symptoms, WAD-grade, kinesiophobia and bodily pain. The association between neck pain disability and FHP, with and without confounder adjustments, was analysed. Data from all measurements (except FHP) were analysed in order to detect each variables potential to confound the possible correlation between neck pain disability and FHP.
No patients were completely excluded from the analyses. Due to partial missing data some of the correlations are based on fewer observations, see Table 2. Available background variables were controlled for in the correlation analyses.
Table 2
Spearman correlation matrix
| Neck disability index (total sum score)* | Forward head posture (degrees) | Age (years) | Gender† | Duration of symptoms (years) | Grade of whiplash- associated disorders‡ | Tampa scale of kinesiophobia (total sum score)§ | |
| Forward head posture (degrees) | 0.004 (p = 0.968) n = 99 | ||||||
| Age (years) | –0.062 (p = 0.525) n = 106 | 0.267** (p = 0.006) n = 106 | |||||
| Gender† | 0.183 (p = 0.061) n = 106 | –0.288** (p = 0.003) n = 106 | –0.102 (p = 0.280) n = 113 | ||||
| Duration of symptoms (years) | –0.128 (p = 0.199) n = 102 | 0.186 (p = 0.062) n = 102 | 0.197* (p = 0.040) n = 109 | –0.011 (p = 0.910) n = 109 | |||
| Grade of whiplash-associated disorders‡ | 0.354** (p < 0.001) n = 106 | 0.005 (p = 0.963) n = 106 | 0.057 (p = 0.550) n = 113 | 0.200* (p = 0.033) n = 113 | –0.069 (p = 0.475) n = 109 | ||
| Tampa scale of kinesiophobia (total sum score)§ | 0.467** (p < 0.001) n = 98 | 0.202* (p = 0.047) n = 98 | –0.205* (p = 0.036) n = 105 | –0.076 (p = 0.442) n = 105 | –0.185 (p = 0.061) n = 103 | 0.064 (p = 0.516) n = 105 | |
| Bodily pain, subscale of Short Form-36 (total sum score)‖ | –0.642** (p < 0.001) n = 106 | 0.036 (p = 0.717) n = 106 | 0.102 (p = 0.281) n = 113 | –0.059 (p = 0.533) n = 113 | 0.240* (p = 0.012) n = 109 | –0.186* (p = 0.049) n = 113 | –0.434** (p = < 0.001) N = 105 |
*Higher scores represent greater disability. †Categorized men/women. ‡Grade of whiplash-associated disorders according to the Quebec Task Force classification. The grades are dichotomized; grade I and II coded 0, grade III coded 1. §Tampa scale of kinesiophobia, Swedish version. Higher scores indicate higher levels of kinesiophobia. ‖Total sum score from the Short Form-36 scale addressing bodily pain. Higher scores indicate less pain.
In testing for normality of data we found that data were not normally distributed, according to Shapiro-Wilk test, therefor non-parametric tests were used in the correlation analyses.
Pairwise correlations of all variables in the study were investigated. Spearman’s rank correlation coefficient (rs) was used in all correlation analyses. The calculating of statistical power is based on Pearson’s correlation coefficient (r) [41], adjusted with the asymptotic relative efficiency (ARE) correction factor (3/π)2 = 0.912 to detect the power for rs [42]. The sample size was estimated based on power calculations in the original RCT study. A logistic regression analysis was used to study the association between neck pain disability and FHP. The analysis included one bivariate model with only FHP and one multiple model including the variables age, gender, and duration of symptoms, WAD-grade, kinesiophobia and bodily pain. The estimated precision for odds ratios (OR) was given with 95% confidence intervals (CI). The level of significance for all tests was set to p = 0.05.
“Statistical Package for the Social Sciences” (SPSS) software, version 21.0, (IBM Corp., Armonk, NY) was used for the statistical analyses. The Simple Interactive Statistical Analysis (SISA) calculator was used for the calculation of statistical power [41]. The statistical power to detect a hypothetical Spearman correlation of 0,3 between FHP and the NDI was 87% at a significance level of.05 with 113 patients [41].
3Results
The study included 113 patients (81 women and 32 men). Mean age 48.1 years. Mean duration of symptoms 9.7 years [29]. For details of patient recruitment and dropouts, see Fig. 2. For details of descriptive data, see Table 1.
Fig. 2
Details of patient recruitment and dropouts.
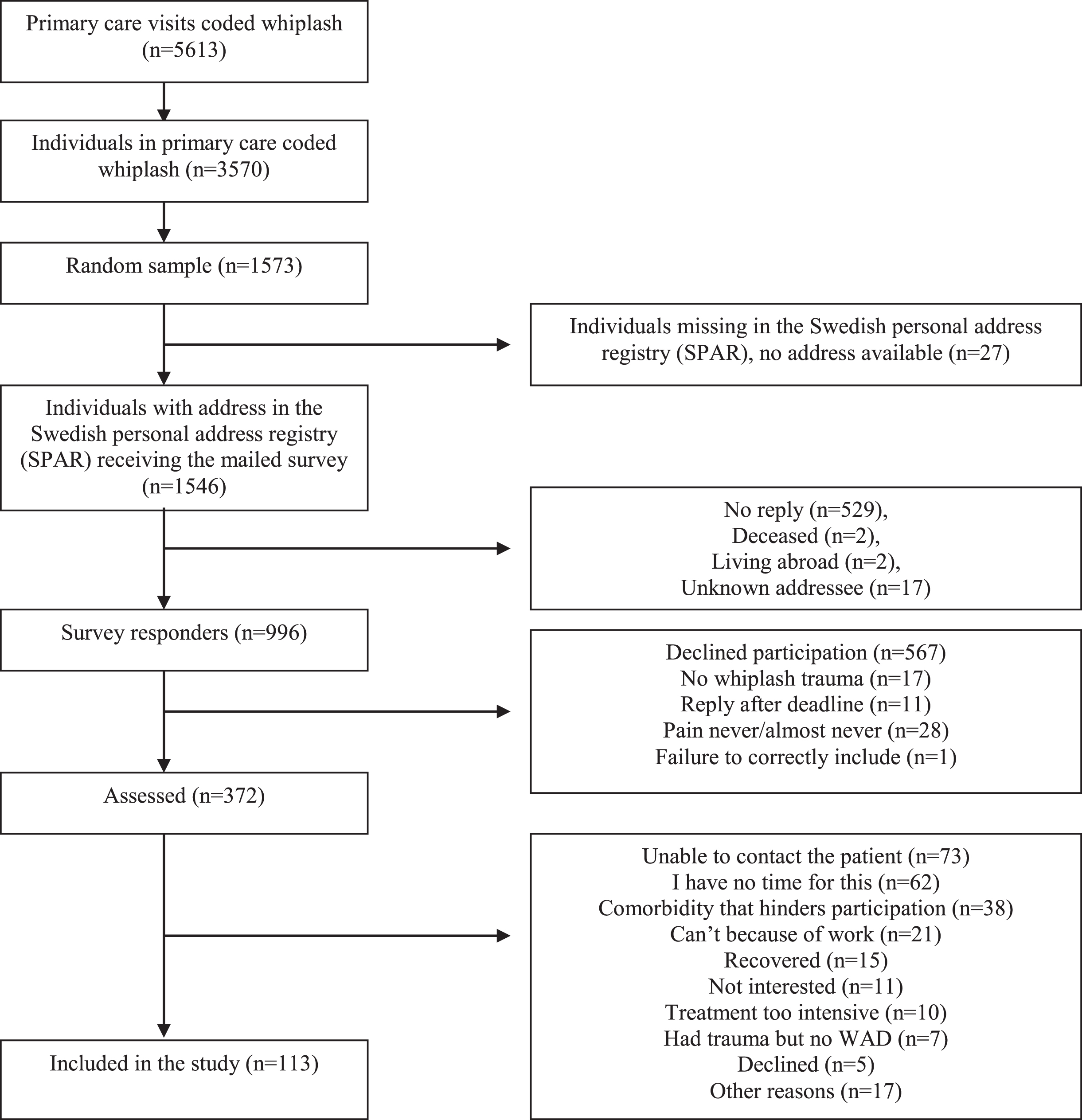
Table 1
Descriptive statistics
| Included patients | Missing patients | |||
| Number/Variable/Statistics | Men | Women | Total | Missing (n) |
| Number (n) | 32 (28.3%) | 81 (71.7%) | 113 | 0 |
| Age (years) | 0 | |||
| Mean | 50.7 | 47.0 | 48.1 | |
| Median | 49.0 | 47.0 | 48.0 | |
| Standard deviation | 14.0 | 11.5 | 12.3 | |
| Range (min-max) | 53 (26–79) | 49 (18–67) | 61 (18–79) | |
| Grade of whiplash-associated disorder (n)* | 0 | |||
| Grade I | 1 (3.1%) | 0 (0%) | 1 (0.9%) | |
| Grade II | 12 (37.5%) | 17 (21%) | 29 (25.7%) | |
| Grade III | 19 (59.4%) | 64 (79%) | 83 (73.5%) | |
| Duration of symptoms (years) | 4 | |||
| Mean | 11.0 | 9.2 | 9.7 | |
| Median | 7.0 | 7.5 | 7.0 | |
| Standard deviation | 11.7 | 7.2 | 8.6 | |
| Range (min-max) | 46 (2–48) | 43 (1–44) | 47 (1–48) | |
| Neck disability index (total sum score)† | 7 | |||
| Mean | 17.3 | 20.3 | 19.4 | |
| Median | 14.5 | 21.0 | 19.0 | |
| Standard deviation | 9.0 | 7.9 | 8.3 | |
| Interquartile range | 17 | 12 | 13 | |
| Range (min-max) | 30 (7–37) | 34 (2–36) | 35 (2–37) | |
| Forward head posture (degrees) | 7 | |||
| Mean | 43.0 | 38.6 | 39.9 | |
| Median | 43.0 | 38.0 | 39.0 | |
| Standard deviation | 6.9 | 4.6 | 5.7 | |
| Range (min-max) | 31 (31–62) | 24 (30–54) | 32 (30–62) | |
| Tampa scale of kinesiophobia (total sum score)† | 8 | |||
| Mean | 37.5 | 35.3 | 35.9 | |
| Median | 37.0 | 35.0 | 36.0 | |
| Standard deviation | 10.5 | 8.5 | 9.1 | |
| Interquartile range | 14 | 10 | 12 | |
| Range (min-max) | 47 (21–68) | 43 (18–61) | 50 (18–68) | |
| Bodily Pain, subscale of Short Form -36 (total sum score)† | 0 | |||
| Mean | 35.4 | 34.5 | 34.7 | |
| Median | 41.0 | 32.0 | 41.0 | |
| Standard deviation | 19.4 | 18.7 | 18.9 | |
| Interquartile range | 27 | 19 | 19 | |
| Range (min-max) | 72 (0–72) | 84 (0–84) | 84 (0–84) | |
*Grade of whiplash-associated disorders according to the Quebec task force classification. †The variable is regarded as ordinal scale data in the present study. To facilitate comparisons with other studies which have regarded this variable as ratio scale data, central tendency and dispersion are also given as mean and standard deviation.
3.1Correlations between all included variables
A correlation matrix is shown in Table 2. There was no significant correlation between FHP and neck pain disability. (rs = 0.004; p = 0.968). Neck pain disability was positively correlated with kinesiophobia (rs = 0.467; p = < 0.001) and WAD-grade (rs = 0.354; p = < 0.001) and negatively correlated with bodily pain (rs = –0.642; p = < 0.001). Median NDI for WAD grade II was 13 and for WAD grade III 22. FHP was positively correlated with kinesiophobia (rs = 0.202; p = 0.047) and age (rs = 0.267; p = 0.006) and negatively correlated with gender (rs = –0.288; p = 0.003). Median FHP for men was 43 and for women 38.
Kinesiophobia was significantly correlated with both neck pain disability and FHP and may therefore confound the possible correlation between these variables.
3.2Association between neck pain disability (NDI below/above 20) and FHP
A bivariate logistic regression analysis showed that FHP was not significantly associated (p = 0.991; 95% CI for OR, 0.931–1.075) with NDI, see Table 3. The dichotomisation of the NDI total sum score resulted in 49 patients below and 57 patients above the cut off value of 20.
Table 3
Logistic regression analysis of the association between neck pain disability (Neck Disability Index below/above 20) and forward head posture (FHP) with and without confounder adjustments
| Unadjusted estimates (n = 99) | ||||||
| Predictors | B* | SE | p-value | Odds Ratio | 95% CI for Odds Ratio | |
| Lower | Upper | |||||
| FHP (degrees) | 0.000 | 0.037 | 0.991 | 1.000 | 0.931 | 1.075 |
| Confounder-adjusted estimates (n = 89) | ||||||
| FHP (degrees) | 0.046 | 0.057 | 0.418 | 1.047 | 0.936 | 1.172 |
| Age (years) | 0.041 | 0.032 | 0.200 | 1.042 | 0.979 | 1.108 |
| Gender† | 1.675 | 0.918 | 0.068 | 5.339 | 0.883 | 32.272 |
| Duration‡ (years) | 0.014 | 0.046 | 0.763 | 1.014 | 0.927 | 1.110 |
| WAD-grade§ | 0.845 | 0.750 | 0.260 | 2.327 | 0.535 | 10.127 |
| TSK-SV‖ | 0.126 | 0.051 | 0.013 | 1.134 | 1.027 | 1.253 |
| Bodily pain¶ | –0.092 | 0.026 | 0.000 | 0.912 | 0.866 | 0.960 |
*The regression coefficient. †Categorized men/women. ‡Duration of symptoms. §Grade of whiplash-associated disorders according to the Quebec task force classification. The grades are dichotomized; grade I and II coded 0, grade III coded 1. ‖Tampa scale of kinesiophobia, Swedish version, total sum score. Higher scores indicate higher levels of kinesiophobia. ¶Total sum score from the Short form-36 subscale addressing bodily pain. Higher scores indicate less pain.
3.3Association between neck pain disability (NDI below/above 20) and FHP with confounder adjustments
A multiple logistic regression analysis showed no significant association between neck pain disability and FHP (p = 0.418; 95% CI for OR, 0.936–1.172), see Table 3. Two variables, kinesiophobia (p = 0.013; 95% CI for OR, 1.027–1.253) and bodily pain (p = < 0.001; 95% CI for OR, 0.866–0.960), were significantly associated with NDI. None of the other variables (age, gender, duration of symptoms and WAD-grade) showed any significance, the p-values varied from 0.068 to 0.763.
4Discussion
No significant correlation was found between neck pain disability and FHP for patients with chronic WAD. A multiple logistic regression including FHP, age and gender, duration of symptoms, WAD-grade, kinesiophobia and bodily pain was significant only for kinesiophobia and bodily pain. The results suggest that physiotherapists should have an increased focus on kinesiophobia, since it is associated with both FHP and neck pain disability.
To the authors’ knowledge, no other study has investigated the association between neck pain disability and FHP in patients with WAD. In chronic neck pain, studies present conflicting evidence of an association between FHP and pain [15, 25, 26]. According to “The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders” (BJD) [43], WAD and other neck pain do not differ once serious pathology has been excluded so it is unclear why the results in the present study differ from others. There is no reason to believe that the different instruments for measuring neck pain disability can explain the difference in result [33]. Nor is the difference in duration of symptoms a probable reason for the result disparity [15]. Similar to our findings a previous study on patients with cervical-craniofacial pain also found no significant correlation between FHP and neck pain disability [44].
The instruments for measuring FHP where different in the present and in all of the previous studies but, in contrast to the present study, the previous studies all measured the same angle [15, 25, 26]. Also the measuring position differed. In one of the previous studies the patients were sitting [26], in the other two they were standing [15, 25]. The measuring position may have an impact of the result as FHP increase in sitting posture compared to standing [45]. Nevertheless, the values of FHP obtained through different methods are comparable and all methods measure the same underlying variable.
In the present study gender appears to be a confounder because of its correlation with FHP, with male gender being associated with more FHP, and strong tendency towards correlation with NDI (p = 0.061). This interpretation is supported by the fact that in a previous study controlling for the effect of age and gender the association between FHP and neck pain disability disappeared when these adjustments were done [26]. This result indicate that gender may be a relevant variable in the interpretation of studies investigating the relationship between FHP and neck pain disability [15, 25].
Age in the present study (mean 48.1 years) was significantly correlated with FHP but not with neck pain disability (p = 0.525), therefore not a confounder. However, in one of the studies on patients with neck pain, age (mean 39.92 years) was a confounder but adjusting for age revealed that the correlation between FHP and neck pain disability remained significant [15]. The conflicting findings make hypotheses about age as a confounder uncertain at this point.
Our findings suggest that kinesiophobia is associated with both FHP and neck pain disability. Kinesiophobia is describing “an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or reinjury” [46, 47]. The theoretical framework is the cognitive-behavioural model describing the mechanism how fear of movement/(re)injury may contribute to the maintenance of chronic pain disability [46]. Results evaluating the ability of the fear-avoidance model to predict WAD symptoms and outcomes are not consistent [10]. A recent systematic review in patients with WAD show that it is unclear whether kinesiophobia is associated with disability, and that the association between pain catastrophizing, pain intensity and disability has not been clearly established [48]. Our results contribute to the current evidence by supporting a link between kinesiophobia and neck pain disability. Further studies on these associations are needed.
In the present study kinesiophobia was significantly correlated with both neck pain disability and FHP and may therefore act as a confounder. It may be that the correlations found between these variables in the studies of patients with neck pain are spurious and would have been affected by the presence of kinesiophobia in a regression analysis [15, 25]. This correlation between kinesiophobia and neck pain disability correspond to previous findings [49–51]. To the authors knowledge there are no other studies on the correlation between kinesiophobia and FHP. The hypothesis that a psychological variable such as kinesiophobia may be reflected in head posture warrants further investigation in future studies.
Kinesiophobia was also significantly negatively correlated with age and had a strong tendency to be negatively correlated with duration of symptoms, indicating that the older the patient, or the longer the duration, the less the kinesiophobia. However, previous works do not support these correlations on patients with chronic WAD and the hypothesis requires confirmation because the sample in the present study had significantly longer duration of symptoms [49, 50].
In the present study only two variables, kinesiophobia and bodily pain, were significantly associated with NDI above/below 20 in the regression analysis. The results suggest that it is unlikely that FHP can explain neck pain disability in patients with chronic WAD of long duration. Kinesiophobia and bodily pain seems to be more important factors explaining this disability. The present study found no support for the hypothesis that forward head posture affects neck pain disability in patients with chronic WAD of long duration.
4.1Study limitations
This study was a secondary analysis based on data from a randomized controlled study. Since the present study is observational it is not possible to draw final conclusions about causal associations. Patients with WAD-grade 0 and IV were excluded in the study. The results are mainly valid for patients with chronic WAD grade II and III. Only one patient in the sample had WAD grade I. This patient was merged into WAD grade II to simplify the analyses. This gives a small skewness of the sample towards WAD grade II and III. The recruitment of participants was carried out more than 10 years ago, which might affect the generalizability of the results. The cut off value of 20 on the NDI was chosen because it is in the middle of the scoring interpretation for the NDI and was significantly related to poor outcome 3 years after the injury [31, 40]. Several recovery cut offs of the NDI are reported [52, 53]. Due to lack of consensus about the most relevant cut off, our choice of cut off can be regarded a limitation. While the goniometer was chosen as a well-established, cost-effective and quick clinical tool, it involves a risk of measurement bias. As the goniometer assessment was conducted by only one assessor, the risk of bias was reduced. Technological alternatives such as video movement analysis or wearable sensors to evaluate head posture might have improved the measurement, which is suggested for future studies.
5Conclusions
There is no significant correlation between neck pain disability and FHP for patients with chronic WAD of long duration. A multiple logistic regression including FHP, age and gender, duration of symptoms, WAD-grade, kinesiophobia and bodily pain was significant only for kinesiophobia and bodily pain. The clinical implications for physiotherapists are that FHP has less importance for neck pain disability in this group of patients and that kinesiophobia should be attended to since it is associated with both FHP and neck pain disability.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to report.
References
[1] | Spitzer WO , Skovron ML , Salmi LR , Cassidy JD , Duranceau J , Suissa S , et al. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash” and its management. Spine. (1995) ;20: (8 Suppl 8):1–73. |
[2] | Jansen GB , Edlund C , Grane P , Hildingsson C , Karlberg M , Link H , et al. Whiplash injuries: diagnosis and early management. The Swedish Society of Medicine and the Whiplash Commission Medical Task Force. Eur Spine J. (2008) ;17: (Suppl 3):355–417. |
[3] | Holm LW , Carroll LJ , Cassidy JD , Hogg-Johnson S , Cote P , Guzman J , et al. The burden and determinants of neck pain in whiplash-associated disorders after traffic collisions: results of the Bone and Joint Decade -Task Force on Neck Pain and Its Associated Disorders. Spine. (2008) ;33: (4 Suppl 4):52–9. |
[4] | Suissa S , Harder S , Veilleux M . The relation between initial symptoms and signs and the prognosis of whiplash. Eur Spine J. (2001) ;10: (1):44–9. |
[5] | Bunketorp L , Nordholm L , Carlsson J . A descriptive analysis of disorders in patients 17 years following motor vehicle accidents. Eur Spine J. (2002) ;11: (3):227–34. |
[6] | Rydevik B . Editorial Preface: The Bone and Joint Decade –Task Force on Neck Pain and Its Associated Disorders. Spine. (2008) ;33: (4S):S3. |
[7] | Carroll LJ , Holm LW , Hogg-Johnson S , Cote P , Cassidy JD , Haldeman S , et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. (2008) ;33: (4 Suppl 4):83–92. |
[8] | Ritchie C , Hendrikz J , Kenardy J , Sterling M . Derivation of a clinical prediction rule to identify both chronic moderate/severe disability and full recovery following whiplash injury. Pain. (2013) ;154: (10):2198–206. |
[9] | Van Oosterwijck J , Nijs J , Meeus M , Paul L . Evidence for central sensitization in chronic whiplash: a systematic literature review. Eur J Pain. (2013) ;17: (3):299–312. |
[10] | Turk D , Robinson J , Duckworth M . The Impact of Psychosocial and Contextual Factors on Individuals Who Sustain Whiplash-Associated Disorders in Motor Vehicle Collisions. Psychol Inj Law. (2018) ;11: (3):218–32. |
[11] | Styrke J , Stalnacke BM , Bylund PO , Sojka P , Bjornstig U . A 10-year incidence of acute whiplash injuries after road traffic crashes in a defined population in northern Sweden. PM & R: the journal of injury, function, and rehabilitation. (2012) ;4: (10):739–47. |
[12] | Walton DM , Pretty J , MacDermid JC , Teasell RW . Risk factors for persistent problems following whiplash injury: results of a systematic review and meta-analysis. J Orthop Sports Phys Ther. (2009) ;39: (5):334–50. |
[13] | Sterling M . A proposed new classification system for whiplash associated disorders–implications for assessment and management. Man Ther. (2004) ;9: (2):60–70. |
[14] | Nilsson BM , Söderlund A . Head posture in patients with whiplash-associated disorders and the measurement method’s reliability - A comparison to healthy subjects. Adv Physiother. (2005) ;7: (1):13–9. |
[15] | Yip CH , Chiu TT , Poon AT . The relationship between head posture and severity and disability of patients with neck pain. Man Ther. (2008) ;13: (2):148–54. |
[16] | Korakakis V , O’Sullivan K , O’Sullivan PB , Evagelinou V , Sotiralis Y , Sideris A , et al. Physiotherapist perceptions of optimal sitting and standing posture. Musculoskeletal Science & Practice. (2019) ;39: :24–31. |
[17] | Edmondston SJ , Sharp M , Symes A , Alhabib N , Allison GT . Changes in mechanical load and extensor muscle activity in the cervico-thoracic spine induced by sitting posture modification. Ergonomics. (2011) ;54: (2):179–86. |
[18] | Caneiro JP , O’Sullivan P , Burnett A , Barach A , O’Neil D , Tveit O , et al. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther. (2010) ;15: (1):54–60. |
[19] | Silva AG , Punt TD , Sharples P , Vilas-Boas JP , Johnson MI . Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Arch Phys Med Rehabil. (2009) ;90: (4):669–74. |
[20] | Jull GA . Deep cervical flexor muscle dysfunction in whiplash. J Musculoskelet Pain. (2000) ;8: (1-2):143–54. |
[21] | Jull G , Kristjansson E , Dall’Alba P . Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther. (2004) ;9: (2):89–94. |
[22] | Suvarnnato T , Puntumetakul R , Uthaikhup S , Boucaut R . Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: a randomized controlled trial. J Pain Res. (2019) ;12: , 915–25. |
[23] | Park D-S , Lee G-C . PR_ The Effect of Strengthening Exercise of Deep Neck Flexors on Chronic Neck Pain. Arch Phys Med Rehabil. (2006) ;87: (11):e38. |
[24] | Tsiringakis G , Dimitriadis Z , Triantafylloy E , McLean S . Motor control training of deep neck flexors with pressure biofeedback improves pain and disability in patients with neck pain: A systematic review and meta-analysis. Musculoskeletal Science & Practice. 2020;50. |
[25] | Lau HM , Chiu TT , Lam TH . Measurement of craniovertebral angle with Electronic Head Posture Instrument: Criterion validity. J Rehabil Res Dev. (2010) ;47: (9):911–8. |
[26] | Lau KT , Cheung KY , Chan KB , Chan MH , Lo KY , Chiu TT . Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man Ther. (2010) ;15: (5):457–62. |
[27] | Kamper SJ , Maher CG , Menezes Costa Lda C , McAuley JH , Hush JM , Sterling M . Does fear of movement mediate the relationship between pain intensity and disability in patients following whiplash injury? A prospective longitudinal study. Pain. (2012) ;153: (1):113–9. |
[28] | Robinson JP , Theodore BR , Dansie EJ , Wilson HD , Turk DC . The role of fear of movement in subacute whiplash-associated disorders grades I and II. Pain. (2013) ;154: (3):393–401. |
[29] | Seferiadis A , Ohlin P , Billhult A , Gunnarsson R . Basic body awareness therapy or exercise therapy for the treatment of chronic whiplash associated disorders: a randomized comparative clinical trial. Disabil Rehabil. (2016) ;38: (5):442–51. |
[30] | Vernon H , Mior S . The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. (1991) ;14: (7):409–15. |
[31] | Vernon H . The Neck Disability Index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther. (2008) ;31: (7):491–502. |
[32] | Pietrobon R , Coeytaux RR , Carey TS , Richardson WJ , DeVellis RF . Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine. (2002) ;27: (5):515–22. |
[33] | Hoving JL , O’Leary EF , Niere KR , Green S , Buchbinder R . Validity of the neck disability index, Northwick Park neck pain questionnaire, and problem elicitation technique for measuring disability associated with whiplash-associated disorders. Pain. (2003) ;102: (3):273–81. |
[34] | Engh L , Fall M , Hennig M , Söderlund A . Intra- and inter-rater reliability of goniometric method of measuring head posture. Physiother Theory Pract. (2003) ;19: (3):175–82. |
[35] | Lundberg MKE , Styf J , Carlsson SG . A psychometric evaluation of the Tampa Scale for Kinesiophobia —from a physiotherapeutic perspective. Physiother Theory Pract. (2004) ;20: (2):121–33. |
[36] | Bunketorp L , Carlsson J , Kowalski J , Stener-Victorin E . Evaluating the reliability of multi-item scales: a non-parametric approach to the ordered categorical structure of data collected with the Swedish version of the Tampa Scale for Kinesiophobia and the Self-Efficacy Scale. J Rehabil Med. (2005) ;37: (5):330–4. |
[37] | Taft C , Karlsson J , Sullivan M . Performance of the Swedish SF-36 version 2.0. Qual Life Res. (2004) ;13: (1):251–6. |
[38] | Garratt AM , Ruta DA , Abdalla MI , Buckingham JK , Russell IT . The SF36 health survey questionnaire: an outcome measure suitable for routine use within the NHS? BMJ306. (1993) ;306: (6890):1440–4. |
[39] | Angst F , Verra ML , Lehmann S , Gysi F , Benz T , Aeschlimann A . Responsiveness of the cervical Northern American Spine Society questionnaire (NASS) and the Short Form 36 (SF-36) in chronic whiplash. Clin Rehabil.. (2012) ;26: (2):142–51. |
[40] | Miettinen T , Leino E , Airaksinen O , Lindgren KA . The possibility to use simple validated questionnaires to predict long-term health problems after whiplash injury. Spine. (2004) ;29: (3):E47–51. |
[41] | Uitenbroek DG . Simple Interactive Statistical Analysis. Quantitative skills Web site. Available from: http://www.quantitativeskills.com/sisa/statistics/correl.htm. Published 1997. |
[42] | Hollander M , Wolfe DA . Nonparametric statistical methods. Chichester; New York: Wiley; (1999) . |
[43] | Nordin M , Carragee EJ , Hogg-Johnson S , Weiner SS , Hurwitz EL , Peloso PM , et al. Assessment of neck pain and its associated disorders: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. (2008) ;33: (4 Suppl 4):101–22. |
[44] | López-De-Uralde-Villanueva I , Beltran-Alacreu H , Paris-Alemany A , Angulo-Díaz-Parreño S , La Touche R . Relationships between craniocervical posture and pain-related disability in patients with cervico-craniofacial pain. J Pain Res. (2015) ;8: :449–58. |
[45] | Shaghayegh Fard B , Ahmadi A , Maroufi N , Sarrafzadeh J . Evaluation of forward head posture in sitting and standing positions. Eur Spine J. (2016) ;25: :3577–3582. |
[46] | Vlaeyen JS , Kole-Snijders AJ , Rotteveel A , Ruesink R , Heuts PTG . The role of fear of movement/(re)injury in pain disability. Journal of Occupational Rehabilitation. (1995) ;5: (4):235–52. |
[47] | Kori SH , Miller RP , Todd DD . Kinisophobia: A new view of chronic pain behavior. Pain Management. (1990) ;3: (1):35–43. |
[48] | Luque-Suarez A , Falla D , Morales-Asencio JM , Martinez-Calderon J . Is kinesiophobia and pain catastrophising at baseline associated with chronic pain and disability in whiplash-associated disorders? A systematic review. Br J Sports Med. (2020) ;54: (15):892. |
[49] | Vernon H , Guerriero R , Soave D , Kavanaugh S , Puhl A , Reinhart C . The relationship between self-rated disability, fear-avoidance beliefs, and nonorganic signs in patients with chronic whiplash-associated disorder. J Manipulative Physiol Ther. (2011) ;34: (8):506–13. |
[50] | Vernon H , Guerriero R , Kavanaugh S , Soave D , Moreton J . Psychological factors in the use of the neck disability index in chronic whiplash patients. Spine. (2010) ;35: (1):E16–21. |
[51] | Vernon H , Guerriero R , Kavanaugh S , Soave D , Puhl A . Self-rated disability, fear-avoidance beliefs, nonorganic pain behaviors are important mediators of ranges of active motion in chronic whiplash patients. Disabil Rehabil. (2013) ;35: (23):1954–60. |
[52] | Pool JJ , Ostelo RW , Hoving JL , Bouter LM , de Vet HC . Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine. (2007) ;32: (26):3047–51. |
[53] | Kato S , Takeshita K , Matsudaira K , Tonosu J , Hara N , Chikuda H . Normative score and cut-off value of the Neck Disability Index. J Orthop Sci. (2012) ;17: (6):687–93. |




