The mediterranean diet: Healthy and sustainable dietary pattern in the time of Sars-Cov-2
Abstract
COVID-19, first reported in Wuhan, China in December 2019 quickly spread worldwide leading to serious health, social and economic consequences. A crucial role in the pathogenesis of severe disease has been attributed to the inflammatory status, that in more severe cases may evolve in an overproduction of pro-inflammatory cytokines (“cytokine storm)” and fatal outcome. Non-communicable diseases, nutritional disorders and advanced age, conditions associated with a low-grade systemic inflammation and immune function alterations, have been identified as major risks for severe COVID-19. General recommendations for fighting COVID-19 highlighted the paramount importance of adopting a healthy plant-based dietary pattern and healthy lifestyle.
The Mediterranean dietary pattern is considered as one of the healthiest dietary patterns, and its benefits are supported by a large body of evidence. Furthermore, it is considered as a sustainable lifestyle model. The aim of this research was to update the multiple benefits of the Mediterranean dietary pattern on physical and mental health, focusing on the effects that it may have in combating COVID-19. The potential effects and mechanisms of action of the main bioactive components of Mediterranean diet were also analyzed. Considering its effects in modulating inflammation and oxidative stress and supporting the immune system, the Mediterranean dietary pattern may be considered the most promising dietary approach to combat COVID-19.
1Introduction
Coronaviruses are a large group of single-stranded RNA viruses that are common among mammals and birds. Coronaviruses cause respiratory and, less frequently, gastrointestinal diseases [1]. In December 2019, a new type of coronavirus causing pneumonia and death was identified in Wuhan, China. This new coronavirus is called SARS-CoV-2 because it is genetically similar to SARS-CoV which caused the 2002 outbreak of severe acute respiratory distress syndrome. SARS-CoV-2 is the seventh known human coronavirus. The illness associated with infection by SARS-CoV-2 is named Coronavirus Disease discovered in 2019 or COVID-19. The disease has spread worldwide and has been declared by the World Health Organization as a global pandemic on March 12, 2020 [2]. Like other respiratory coronaviruses, SARS-CoV-2 is transmitted primarily via respiratory droplets, with a possible, but unproven, faecal–oral transmission route. The average incubation period is approximately 4–5 days before symptom onset, with 97.5%of symptomatic patients developing symptoms within 11.5 days. COVID-19 can manifest as an asymptomatic infection, or patients can present with a mild upper respiratory tract illness that may include cough, chills, fever, fatigue as well as shortness of breath [3]. In more severe cases, complications include acute respiratory distress syndrome, acute cardiac complications, multiple organ dysfunction syndrome, septic shock, and death [4].
Since the new coronavirus pandemic outburst, a plethora of studies have been conducted and published in an impressively short period of time, emphasizing potential risk and prognostic factors for the development and progression of COVID-19.
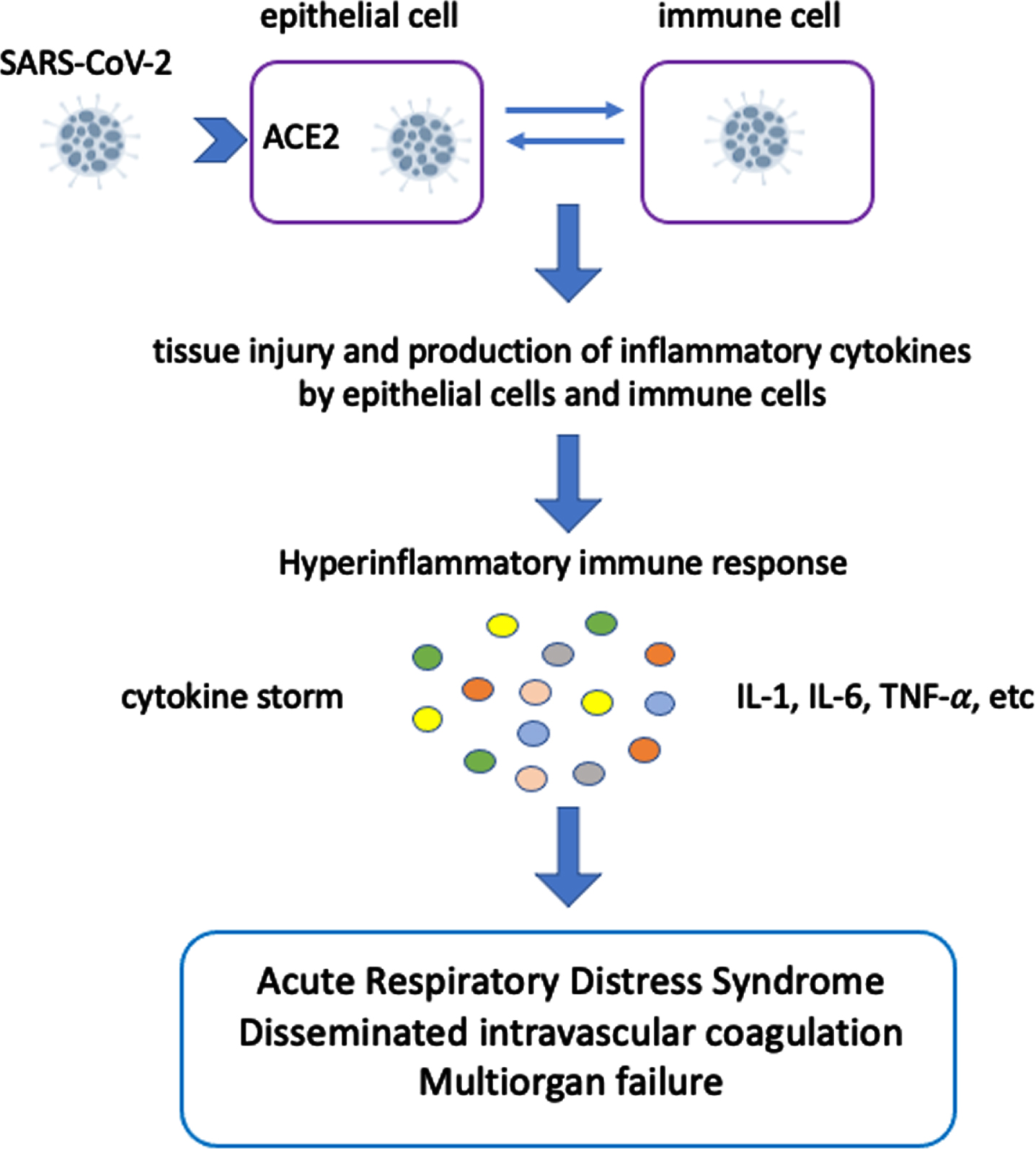
The severity of COVID-19 is mainly due to the host response to viral infection. A healthy immune response can eliminate the infected cells before the virus spreads, while a defective immune response of the host may result in an overproduction of pro-inflammatory cytokines (“cytokine storm”) [5]. The cytokine storm is an activation cascade of auto-amplifying cytokine production due to a defective host immune response to different triggers such as infections, malignancy, rheumatic disorders, etc. The current evidence suggests that SARS-CoV-2 infection unleashes a powerful, and apparently uncontrolled inflammatory response that most likely adds to the tissue damage already caused by the viral infection [6]. Excessive inflammation is associated with oxidative stress and increased coagulopathy (arterial and venous thromboembolisms). The high concentration of pro-inflammatory mediators damages cardiac, hepatic and renal systems leading to tumor necrosis factor-mediated acute respiratory distress syndrome, disseminated intravacular coagulation, multi-organ failure and death (Fig. 1) [7].
Fig. 1
Cytokine storm and its consequences in COVID-19.
2Risk factors of severe Covid-19
Many risk factors, including advanced age, male sex, non-communicable diseases and nutritional disorders, have been associated with COVID-19 severity and mortality (Table 1).
Table 1
Risk factors for COVID-19 adverse outcome
| Advanced age |
| Male sex |
| Non communicable diseases (such as obesity, diabetes, some types of cancer, chronic kidney disease, respiratory disease) |
| Malnutrition |
2.1Advanced age
The increased severity and mortality of COVID-19 observed in older individuals has been related to the phenomenon known as “inflammaging” characterized by an age-related increase in the levels of pro-inflammatory markers in blood and tissues, associated with an acquired immune system impairment (immune senescence), which can trigger a hyperinflammation syndrome and predispose to severe complications of COVID-19 and death [8]. In addition, older age is often associated with comorbid conditions, impaired nutritional status and sarcopenia, regardless of body mass index [9], that may further aggravate outcome. The situation is different in centenarians, in whom pro-longevity traits and anti-inflammatory markers seem to protect them against the adverse outcomes of inflammation [10]. A lower rate of COVID-19 deaths in the elderly aged over 90 years has also been reported in Italy confirming the resilience of this population in fighting against Covid-19 disease. A North to South decreasing gradient in the percentage of > 90 being infected has been also reported (6-8%in northern regions, and 1–4%in southern regions) [11]. Genetic and epigenetic factors, a long-life adherence to Mediterranean diet as well as living in less polluted areas have been implicated to explain these observations.
2.2Male-female differences in mortality rate
The reason why mortality rate is higher in males than in females is not clear. As ACE2 (angiotensin converting enzyme-2), the host cellular receptor used by SARS-Cov-12 as a gate for entering the cells, is located on the X chromosome, females may have alleles that make it resistant to COVID-19, thereby explaining the lower mortality rate. Another hypothesis is related to hormones. Oestrogen and testosterone have different immunoregulatory functions which could influence immune protection or disease severity in a different way [7].
A higher rate of inflammaging in men compared to females could also contribute to worsen COVID-19. In the elderly, especially men, IL-6 is chronically upregulated, and its elevation has been found a predictor of SARS-CoV-2 mortality [10]. As above mentioned, the situation is different in men aged > 90.
2.3Non-communicable diseases
The most common non-communicable diseases, including obesity, diabetes, cardiovascular disease, some types of cancer, respiratory disease, and chronic kidney disease, are characterized by a low-grade chronic systemic inflammation. On March 2020, the World Health Organization underlined that people with non-communicable diseases seem to be more vulnerable to severe complications of COVID-19 [12,13]. The link between viral infection severity and non-communicable diseases has been previously observed in other viral infections, such as influenza [14].
2.4Nutritional disorders
Both malnutrition and over nutrition have been reported as significant factors in the outcome of a variety of different infectious diseases.
A poor nutritional status is often associated with inflammation and oxidative stress, which in turn has a negative impact on the immune system [15]. The interaction between malnutrition and infectious disease has long been recognized [16]. Malnutrition is the primary cause of immunodeficiency worldwide, increasing the risk of infections and mortality. In a vicious circle, infections contribute to aggravate malnutrition. A retrospective observational study conducted in critically ill patients with COVID-19 in Wuhan reported that patients with higher scores of malnutrition had significantly higher mortality [17]. It is plausible to assume that malnutrition, due to its negative impact on immune function, may contribute to a worse outcome and/or a longer and more difficult recovery in critically ill patients with COVID-19. Lymphopenia, a marker of malnutrition, has been found to be a negative prognostic factor in patients with COVID-19 [4]. A recent study showed that low prealbumin levels predict the progression to acute respiratory distress syndrome thereby confirming the role of poor nutritional status and in particular the protein-calorie malnutrition in the evolution of Covid-19 outcome [18].
Overweight and obesity are among the most common comorbidity conditions in hospitalized COVID-19 patients and have been associated with higher risks of adverse outcomes [18, 19]. The strong correlation between obesity and complications of viral infections has been reported for influenza virus and previous coronaviruses causing widespread infections (SARS and MERS). In a review released by the World Obesity Federation on March 2021 which focused on the relationship between obesity and COVID-19, higher body mass index was found to be associated with increased risk of hospitalization, admission to intensive care and need for mechanically assisted ventilation. Higher BMI has also been found as one of the death factors of COVID-19. These increased risks have also emerged after adjusting data to age, ethnicity, income as well as to other demographic and socio-economic factors [20]. People with obesity who were affected by COVID-19 have also been reported to require longer hospitalization, longer oxygen treatment and longer SARS-CoV-2 shedding [21, 23]. In addition, it has been hypothesized that a large prevalence in the population of subjects with obesity, who have longer virus shedding, may increase the chance to spread the virus to others. Moreover, the reduced and delayed production of interferon in obese individuals could facilitate the appearance of more virulent strains, eventually increasing the overall mortality rate of an influenza pandemic [24]. Many factors may account for the high risk of severe COVID-19 in people with obesity. A central role has been attributed to chronic systemic inflammation as SARS-CoV-2 infection and obesity share some common metabolic and inflammatory reaction pathways [25]. Adipocytes of patients with visceral obesity and metabolic disorders are stimulated to release tumor necrosis factor-α, interleukin 6 and other pro-inflammatory mediators, while the production of the anti-inflammatory adiponectin is reduced, predisposing to inflammation and oxidative stress, that in turn negatively affect the immune function [26]. The word “metaflammation” was coined to design the status of metabolic inflammation in obesity [27]. Besides inflammation and impairment of immune system, reduced physical activity, the increased ACE2 expression in adipose tissue and lung, and microbioma dysbiosis have been included as additional factors to explain the high risk of severe COVID-19 outcomes in subjects with obesity [24]. The frequent association with comorbidities, such as diabetes, cardiac or pulmonary complications related to obesity, may further contribute to worsen COVID-19 outcome.
3Healthy eating habits, nutrition and physical activity to combat COVID-19
3.1Healthy eating habits
Optimal nutrition and healthy eating habits can help prevent or control many diseases, including infections. Increasing evidence demonstrates that dietary modifications and nutritional factors have a strong impact on immune function, chronic systemic inflammation and oxidative stress.
A healthy and balanced diet is of crucial importance for supporting immune system and reducing the risk of infections. Adequate intake of energy, proteins, minerals, vitamins (A, B6, B12, C, D, E, folate) and trace elements (zinc, iron, selenium, magnesium, and copper) plays an important role in supporting both the innate and adaptive immune system. Other nutrients such as omega-3 fatty acids also support the immune system by contributing to resolve the inflammatory response. Conversely, nutritional deficits impair the immune responses, increase the susceptibility to viral, bacterial, and fungal infections, and reduces the responses to vaccination.
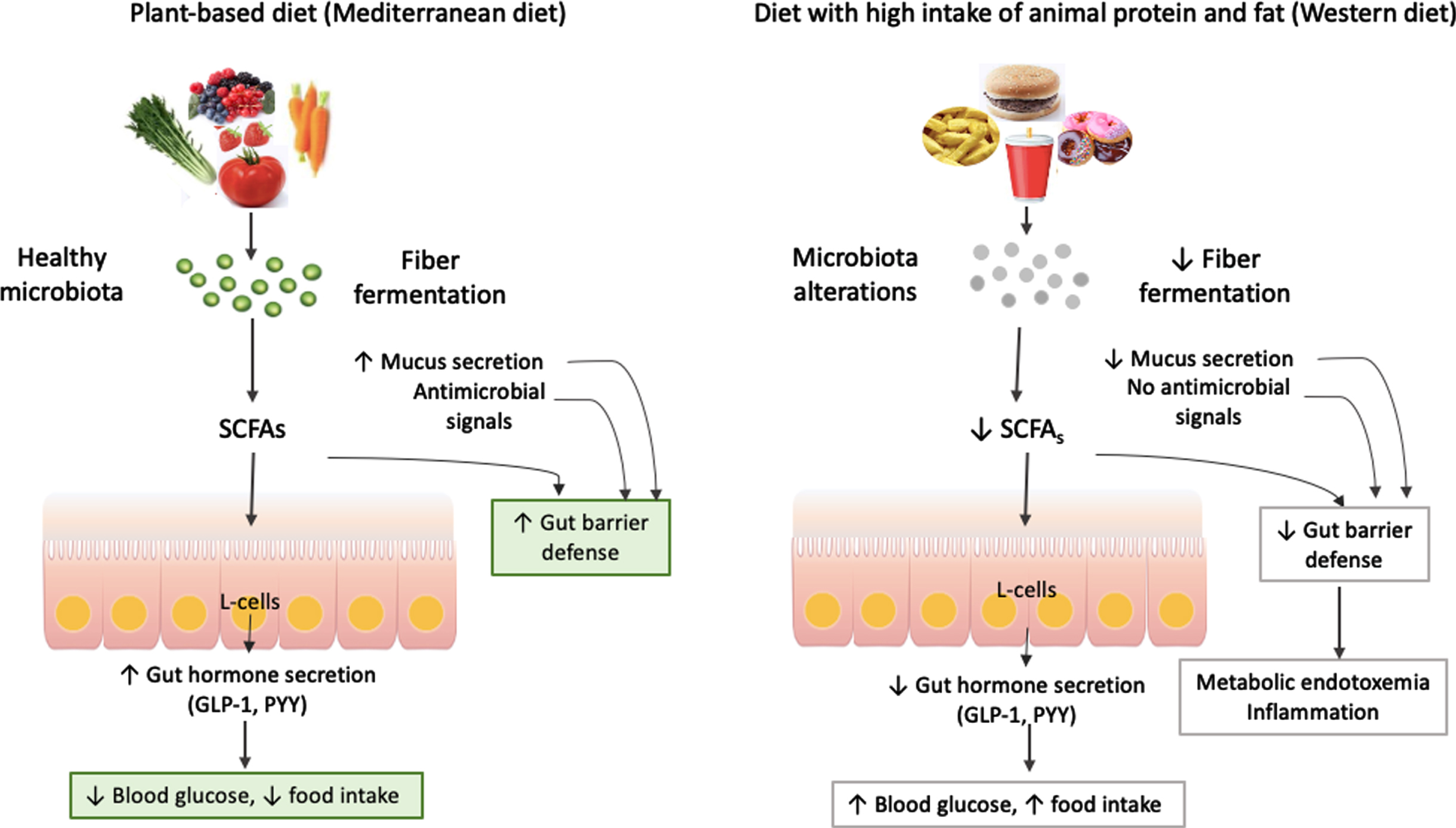
The microbiota plays an important role in modulating the immune system, and gut dysbiosis (i.e. alterations in the composition and function of microbiota) has been associated with various infectious diseases [15, 28]. In perfect symbiosis with the host, gut microbiota influences many areas of human health. On the other hand, gut dysbiosis has been implicated in the development of many diseases, including metabolic diseases such a diabetes and obesity, non-alcoholic fatty liver disease, cardiovascular, gastrointestinal, respiratory, immunological, neurodegenerative diseases, and cancer [29]. The balance between health and disease is mainly influenced by diet, genes and drugs. Mechanisms of the crosstalk between microbiota and host are extremely complex and have not yet been completely elucidated. An example of how gut microbiota may influence human metabolism in physiological conditions and in diseases is given in Fig. 2. Diet composition is the main determinant of gut microbiota composition and function. A plant-based diet, such as Mediterranean diet, with high consumption of fiber and low consumption of animal fat and animal protein has been linked to a metabolically healthy microbiota. Dietary fiber is metabolized and fermented by gut microbiota in the colon producing many compounds including short fatty acids (SCFAs) (propionate, butirrate and acetate). A healthy microbiota has been associated with a high mucus layer thickness and production of antimicrobial signals that increase gut barrier defenses. Propionate and butirrate bind to G protein-coupled receptors 41–43 expressed on the intestinal L-cells promoting the secretion of gut peptides, such as glucagon-like peptide-1 (GLP-1) involved in the regulation of glucose metabolism and peptide YY (PYY) involved in the regulation of food intake. Butirrate also activates PPAR-y promoting beta-oxidation and oxygen consumption, favouring anaerobic conditions in the intestinal lumen. Moreover, propionate can bind to G protein-coupled receptor 43 expressed on lymphocytes enhancing immune defenses. On the other side, metabolic diseases or a diet with high intake of animal fat and protein and low intake of fiber, such as Western diet, induce alterations of gut microbiota composition associated with reduced production of SCFAs and antibacterial signals, lower mucus layer, reduced secretion of intestinal peptides, impaired immune defense and proliferation of aerobic bacteria. These alterations cause a leakage of pathogen-associated molecular patterns including lipopolysaccharide (LPS) that increase in the blood and trigger a systemic low-grade inflammation and insulin resistance, common features of various non communicable metabolic diseases [30, 31].
Fig. 2
The relationships between diet, gut microbiota and metabolism.
Healthy dietary patterns also impact inflammation and oxidative stress. The Mediterranean dietary pattern has been shown to reduce inflammatory markers and oxidative stress, lowering the risk of infectious diseases and chronic illnesses [32], while Western dietary pattern favours inflammation and oxidative stress. Adopting healthy eating habits with plenty of fruits and vegetable is considered an important strategy during the Covid-19 outbreak, as outlined in the “Nutrition advice for adults during the COVID-19 outbreak” published by the World Health Organization [33]. Recommendations for a healthy and balanced diet during Covid-19 were also issued by other Health Organizations such as Food and Agriculture Organization of the United Nations [34], Center for Disease Control and Prevention [35], from national Governments and Nutrition Societies. Most of these documents encourage the consumption of fruits, vegetable and whole grain foods. The importance of vitamins and minerals was also highlighted to maintain a healthy immune function.
3.2Nutrition therapy
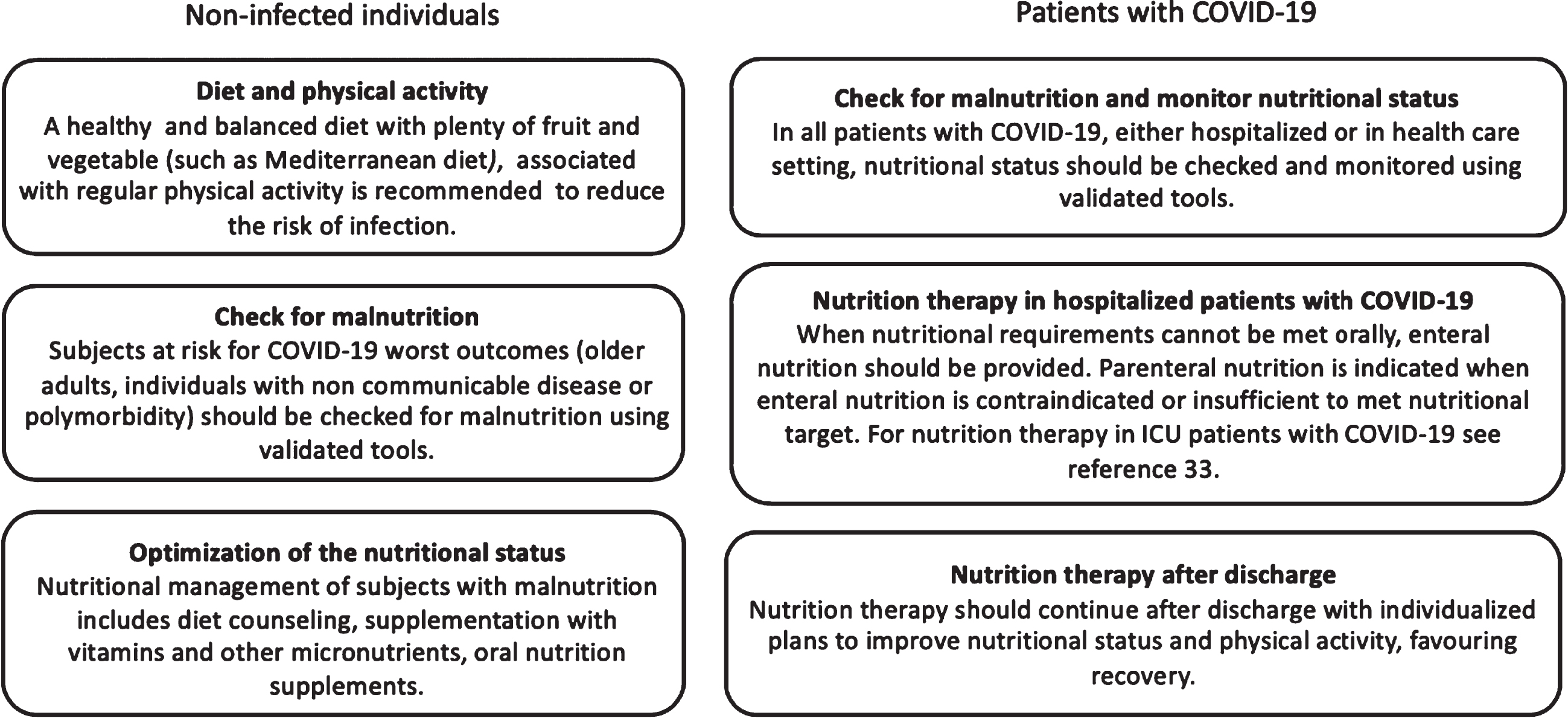
A practical guidance for nutritional management of COVID-19 patients has been released by the European Society for Clinical Nutrition and Metabolism (ESPEN) [36]. Nutrition therapy is recommended as an integral part of treatment to reduce morbidity, mortality and disability in general healthcare, as well as in hospital.
In non-infected individuals a healthy and balanced diet with plenty of food and vegetable, associated with regular physical activity, is recommended to increase immune defenses and reduce the infection risk. Non-infected individuals at risk for worst COVID-19 outcomes, namely older adults, individuals with non communicable diseases or polymorbidity, should be checked for malnutrition through validated screening tools. In subjects identified “at risk” by screening, the assessment for diagnosis and grading of the severity of malnutrition is needed. Since the definition of malnutrition includes the inability to preserve healthy body composition and skeletal muscle mass, persons with obesity should be also screened and investigated according to the same criteria. Sarcopenia and micronutrient deficiencies are often associated with obesity. Preserving nutritional status and preventing or treating malnutrition may mitigate complications and improve outcomes in subjects who might incur in COVID-19 in the future. COVID-19 symptoms such nausea, vomiting and diarrea reduce food intake and absorption, leading to malnutrition. Therefore, a good nutritional status is an advantage for people at risk for severe COVID-19. Nutritional mannagement of individuals with malnutrition includes counseling, supplementation with vitamins and other micronutrients, eventually associated with oral nutritional supplements (ONS) to cover nutrition deficits. ONS are commonly used as a supplement to diet but in some conditions they can be used as the sole source of nutrition since they have a balanced nutritional composition of macro-and micronutrients that reflect dietary recommendations for healthy people. Provision of daily allowances for vitamins and trace elements should be ensured to malnourished patients at risk for or with COVID-19 to maximize the anti-infective defenses.
In patients with COVID-19, whether hospitalized or in general healthcare, nutritional status should be checked and regularly monitored. When energy requirement cannot be met orally with diet counseling, supplements and ONS, enteral nutrition should be administered. Parenteral nutrition is indicated when enteral nutrition is contraindicated or insufficient to met nutritional targets. Patients with COVID-19 in intensive care unit (ICU), particularly older individuals and those with non communicable diseases or comorbidity, are at high risk of malnutrition and worse outcomes. The dramatic loss of skeletal muscle mass and function, due to catabolism, reduced mobility, reduced food intake and inflammation, is the major nutritional problem in ICU patients and in ICU survivors, favouring disability, poor quality of life and additional morbidity. Appropriate nutritional interventions may mitigate catabolism and improve outcome in these patients. The management of nutritional support in ICU-ventilated and non-ventilated COVID-19 patients is extensively reported in the above-mentioned ESPEN guideline [36].
Nutritional treatment should continue after discharge with individualized treatment plans. Nutritional management after discharge represents an opportunity to improve physical activity and dietary habits, favouring recovery and mitigating post-COVID health problems at the same time (Fig. 3).
Fig. 3
Nutritional management of COVID-19.
3.3Physical activity
Benefits of physical activity on physical and mental health are well known. There is evidence of the effectiveness of regular physical activity in the primary and secondary prevention of cardiovascular and other chronic noncommunicable diseases [37]. Furthermore, benefits on mental health, mood disorders (depression and anxiety), self-esteem, and well-being have been reported. Moreover, physical exercise leads to the reduction of inflammatory markers and oxidative stress [38], together with an improvement of the immune function. Thanks to its benefits on mental health, physical activity may alleviate psychological disturbances related to pandemia, quarantine and social isolation. The benefits of physical activity on psychological well-being during the COVID-19 lockdown have been recently reported [39]. Therefore, whenever possible and provided that local and national COVID-19 restrictions are respected, people without any symptoms or diseases should be encouraged to exercise, preferably outdoors (walking, jogging, cycling, gardening). Home-based exercise (staircase, walking, walking in place or around the apartment, stand-to-sit and sit-to stand as well as jumping) may also be done using online videos and educational programs. The intensity and duration of exercise need to be gradually increased. Personalized training according to age, clinical conditions and level of fitness is of paramount importance.
4Mediterranean dietary pattern
Plant-based diets have been associated to well-being and prevention of many chronic diseases. Benefits are mainly ascribed to the high contents of a variety of bioactive compounds in fruits and vegetables.
Among various healthy dietary patterns, the Mediterranean Dietary Pattern (MDP) is considered one of the healthiest worldwide. The benefits of adopting a MDP were reported more than 50 years ago, when a reduction in the risk of cardiovascular disease was observed among populations whose nutritional habits were consistent with those of the people from the Mediterranean basin, mostly Greece and Southern Italy. Although this dietary pattern varies between coastal and inland areas and depends on cultural differences, traditions, geographic location and food availability, the fundamental aspect of the traditional Mediterranean diet is the high content of plant-based foods with abundance of vegetables, legumes, whole grain bread and other cereals, nuts and seeds, fresh fruits, extra virgin olive oil as the principal source of fat, a low to moderate consumption of dairy products, fish, poultry, and eggs, a low consumption of red meat, and a moderate consumption of wine, especially red wine, preferably with meals [40, 41]. The MDP is poor in saturated fatty acids, and it is rich in monounsaturated fatty acids and long chain polyunsatured fatty acids, mainly from fish, particularly in certain Mediterranean areas, with a balanced ratio of n-6/n-3 essential fatty acids [42]. The MDP provides a high amount of fiber and antioxidants, phytochemicals, phenolic compounds, vitamins (A, C, D, E) and minerals (zinc, copper, selenium). It should be emphasized that the MDP is not only a set of foods but also a cultural model which involves the way foods are selected, produced, processed and distributed [43].
4.1Health benefits of MDP
The Mediterranean diet has long been reported to be protective against cardiovascular diseases, diabetes, neurodegenerative diseases [44–46], and various types of cancer (upper-digestive tract, stomach, colorectal, liver, pancreas and endometrial) [47]. Adherence to MDP pattern has been associated with a healthier body weight, lower waist circumference, and lower incidence of metabolic syndrome. Positive effects on age-related cognitive decline [48], depression [49], emotional disorders [50], well-being and quality of life [51] have been reported. The nutritional quality of Mediterranean diet has been also proved. People adhering to MDP fulfil their micronutrients intake, except for Vitamin D, better than persons on a Western diet [52].
The health benefits of MDP are related to the abundance of fruits and vegetables with high content of anti-inflammatory and antioxidant components (polyphenols, polyunsatured fat, fiber, vitamins, minerals) combined with a relatively low intake of pro-inflammatory nutrients characteristic of the Western dietary pattern (refined sugars, starches, trans-fatty acids, high-density foods). The Mediterranean diet has been found to significantly reduce inflammatory markers (IL-1, CRP) in subjects with obesity or diabetes [53]. The reduction of inflammation was higher than that obtained with other healthy diets, such as low-fat diet [54].
4.2The role of foods and of their bioactive compounds
Many studies highlighted the role of foods characteristic of the Mediterranean diet and of their bioactive components in the prevention of different types of cancer and cardiovascular diseases.
A potential role of Mediterranean diet and its components in combating SARS-CoV-2 has been also suggested.
The role of olive oil, berries and honey and of their bioactive compunds in the prevention and progression of different types of cancer and cardiovascular diseases has been extensively updated and discussed in a recent review [55].
Honey is a food newly introduced in the Mediterranean diet for its antioxidant capacity and richness in polyphenols. An interesting research published in 2020 showed that honey polyphenols are potential inhibitors of colon cancer stem cells, a subpopulation of high tumorigenic cells with an important role on relapses and metastases of colon cancer. These cells are characterized by the ability of self-renewal, resistance to chemotherapy and high capacity to survive eluding apoptosis and autophagy [56]. Other bioactive compounds from Mediterranean diet may have direct or indirect preventive, therapeutic or chemosensitizing effects on cancer stem cells deriving from different types of tumors, as suggest by several in vitro and in vivo studies [57]. A recent elegant study performed in Sprague Dawley rats demonstrated that the administration of Solanum trilobatum extract prior to a single oral dose of carbon tetrachloride (CCL4) inhibit the hepatotoxicity induced by CCL4 and enhance the antioxidant enzyme levels. The administration of Solanum trilobactum extract significantly reversed the histopathological changes induced by CCL4, further confirming the hepatoprotective and antioxidant properties of this extract [58]. The protective effects of berry in cancer and cardiovascular disease are supported by a large body of evidence [55]. A recent research showed that andean berry extract, rich in polyphenols with antioxidant activity, induces apoptosis in human colon cancer cells without mitochondrial damage [59]. Other studies focused on the antibacterial properties of natural berry juices on common oral pathogenic bacteria. Fruit and leaf extracts of Malacomeles denticulata significantly reduced some oral cariogenic and periodontal biofilm species, suggesting a potential role of these natural extracts in the prevention of dental caries and parodontopathy [60].
As reported in the above-mentioned studies, the health benefits of foods characteristic of Mediterranean diet are mainly attributed to their bioactive components. Among these, polyphenols are the largest and most studied group. Polyphenols are found not only in fruits and vegetables, but also in cereals, legumes, chocolate and beverages, such as tea and coffee. The large group of polyphenols is classified in two major classes: flavonoids and non-flavonoids, each class including various sub-classes. Polyphenols have limited bioavailability, as a substantial proportion is lost during the digestive process and only a small fraction is absorbed in the small intestine. The bulk of polyphenols reaches the colon where they interact with the gut microbiota and regulate microbial growth, thus exerting prebiotic-like effects. Microorganisms are crucial for polyphenol metabolism to produce bioactive compounds, and many health effects of polyphenols are mediated by gut microbiota.
Antioxidative, anti-inflammatory, anticarcinogenic, antimicrobial and immunomodulatory properties of polyphenols have been reported. Molecular mechanisms are complex and include their antioxidant properties, modulation of genes involved in antioxidant defenses, inflammation, metabolism regulation, proliferation and survival. The capacity of polyphenols to regulate epigenome has been proved, and recent studies highlighted the potential of flavonoids as a preventive and therapeutic tool for cancer, thanks to their ability for epigenetic regulation of cancer pathogenesis. In preclinical studies many bioactive compounds belonging to various flavonoid sub-classes (quercetin, kaempferol, myricetin, luteolin, apigenin, fisetin, EGCG, genistein, daidzein, silibinin, hesperetin, naringenin, cyanidin, delphinidin, malvidin, and pelargonidin) showed a strong potential for epigenetic regulation of cancer pathogenesis and progression [61]. Other studies highlighted the potential role of polyphenols as candidates for epigenetic targets in diabetes and related complications thanks to their ability to modulate metabolic and signaling pathways at various levels, from gene expression to epigenetic regulation, protein expression and enzyme activity. Preclinical epigenetic studies with various polyphenolic compounds support this hypothesis. Targeting epigenetic pathways to improve glucose homeostasis should represent a future ideal approach in the management of diabetes and related complications [62]. Engineering the flavonoid pathways has been proved to be an effective strategy to increase phenolic content and nutritional value of fruits with potential positive effects on health. For example, transgenic strawberry extracts obtained by genetic modification using a construct that overexpressed anthocyanidin synthase, a gene involved in anthocyanin metabolism, showed enhanced antioxidant and cytotoxic effects on human hepatic cancer cells [63].
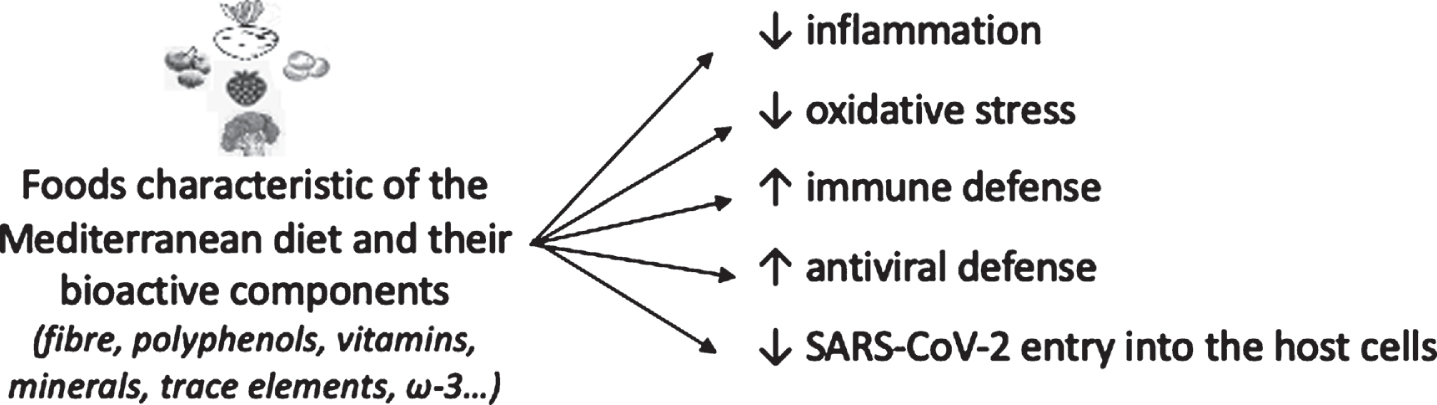
Foods characteristic of Mediterranean diet and their bioactive components have been suggested to play a role also in combating SARS-CoV-2. The efficacy of polyphenols against various pathogens and viruses (Epstein-Barr virus, enterovirus, herpes simplex virus, influenza virus and other virus causing respiratory tract-related infections) has been demonstrated [64]. The potential role of different nutrients and bioactive components from food sources in combating COVID-19 has been extensively reported in a recent paper [65].
The anti-inflammatory, antioxidant and immunomodulating properties of polyphenols, together with their positive effects on gut dysbiosis could contribute to control the inflammatory status triggered by SARS-Cov2. In addition, studies performed in the context of the 2003 SARS-CoV epidemic suggested direct inhibitory effects of polyphenols on virus entry into the host cells. Polyphenols (i.e. luteolin) could bind with high affinity to the surface spike glycoprotein of the virus, restricting its entry into the cells [66]. Molecular docking and dynamic simulation studies also showed that polyphenols could increase ACE2 receptor expression. The ACE2 downregulation triggered by SARS-Cov-2 facilitates the infection and has been implicated in the progression of the disease while ACE2 up-regulation may have protective effects on Covid-19 severity. Resveratrol, belonging to polyphenols’ stilbenoids group, is present in more than 70 plant species, especially in grapes’ skin, seeds, red wine and other foods. Several studies showed the capacity of resveratrol to interact with ACE2. A study in rats fed with 50 mg kg–1 day of resveratrol showed increased ACE2 protein level [67]. In another study, mice fed a high-fat diet supplemented with resveratrol reported a significant increase in ACE2 gene expression compared to mice fed a high fat diet, suggesting that resveratrol may mitigate the negative effects of high-fat diets on ACE2 gene expression [68]. In addition, an in vitro study performed in smooth muscle cells from human aorta showed that a 24-hour incubation with resveratrol significantly increased ACE2 gene expression and protein [69]. Taking into account the key role of ACE2 in SARS-CoV-2 disease, and the results of the above-mentioned preclinical studies, a potential role of resveratrol on SARS-CoV-2 infection and/or progression has been proposed [65,70]. Although numerous in vitro and in vivo studies suggest potential protective effects of polyphenols against SARS-CoV-2, clinical studies are needed for confirmation.
Besides polyphenols, other bioactive compounds and nutrients with anti-inflammatory, antioxidant and immunomodulatory properties may contribute to produce the health benefits of the MDP. These compounds include vitamins (particularly C, D, E, B), trace elements (zinc, copper, selenium, iron), healthy fats (alpha-linoleic acid, eicosapentaenoic acid and docosahexaenoic acid), and fiber. The potential role of these components in mitigating COVID-19 and other infections have been reviewed in recent papers [28, 65, 71, 72].
4.3The role of gut microbiota and gut-lung axis
Gut microbiota regulates immune function, inflammation and metabolism, and is considered a key player in the relationships between nutrients and infections. The pleiotropic effects of gut microbiota spread even at sites distant from intestine through short-chain fatty acids (SCFAs) and other microbiota metabolites that reach various organs via the bloodstream.
Patients with COVID-19 showed a dysbiosis, characterized by reduced bacterial diversity, a significantly higher relative abundance of opportunistic pathogens as well as a lower relative abundance of beneficial symbionts. Of further interest is the observation that certain baseline gut microbiota profiles (members of the bacterial phylum Firmicutes specifically, the genus Coprobacillus, and the two species Clostridium ramnosum and Clostridium hathewayi) were associated with increased clinical severity of COVID-19 disease [73]. In addition, a recent study showed that several gut commensals with known immunomodulatory potential such as Faecalibacterium prausnitzii, Eubacterium rectale and bifidobacterial were underrepresented in hospitalized patients with COVID-19 and remained low in samples collected up to 30 days after disease resolution demonstrating that dysbiosis may persist after clearance of the virus. Moreover, alterations of microbiota composition were found associated with inflammatory markers and dysfunctional immune responses in COVID-19 patients, suggesting that gut microbiota is likely involved in the modulation of host inflammatory responses [74]. Several mechanisms have been hypothesized. Individuals with severe COVID-19 disease present a dramatic decrease in the number of CD4+ and CD8+ T cells, more pronounced in patients in Intensive Care Unit [75]. SCFAs, metabolites of gut microbiota, may directly modulate gene expression of CD8+ cytotoxic T lymphocytes. In addition, the microbiota through its interaction with Toll-like receptor-mediated immune responses could be a player in the cytokine storm [76]. Finally, a potential effect of gut microbiota in modulating colonic ACE2 expression has been suggested. ACE2 is highly expressed in small intestinal enterocytes [77] and the expression in the colon is about 4 times higher than that in the lung. The interaction between gut microbiota and ACE2 receptors has been reported in other diseases such as cardiovascular diseases, intestinal inflammation, malnutrition, immunological and metabolic disorders [78].
Recently, a bidirectional cross-talk between gut microbiota and lung microbiota, named “gut-lung axis”, has emerged. Intact bacteria, their fragments or metabolites (SCFAs) may translocate across the intestinal barrier, reach the systemic circulation, and modulate the lung immune response, playing a central role in antiviral responses [79]. Previous studies demonstrated that respiratory infections are associated with modifications of gut microbiota composition. Moreover, an increased prevalence of pulmonary diseases has been reported in patients suffering from inflammatory bowel diseases such as Crohn disease and ulcerative colitis. Besides confirming the interaction between gut microbiota and lung, recent studies and meta-analyses demonstrated the efficacy of probiotics in reducing the incidence and improving outcomes of respiratory infections in humans [80, 81]. The hypothesis that gut microbiota manipulation with probiotics might have a role in the treatment of COVID-19 lung disease is suggestive, but clinical studies are necessary to confirm the efficacy and safety of this approach.
4.4Adherence to the MDP and Covid-19
Considering the anti-inflammatory properties and multiple health benefits of the MDP, a lower COVID-19 mortality rate would be expected in populations adhering to this pattern. However, epidemiological data do not always confirm this hypothesis. Several Mediterranean countries, such as Italy and Spain, had a high burden of the disease despite being the cradle of the Mediterranean diet. The decreased adherence to MDP, particularly in younger people, could at least in part account for this observation [82, 83]. On the other hand, a better adherence to Mediterranean diet in South Italy has been hypothesized to contribute to the lower mortality rate in South Italy compared to North Italy. However, caution should always be used comparing death rates by country and even between regions within a country because of many confounding factors, including the characteristics of the health care system, heterogeneity in accounting cases and deaths, urban or rural area, air pollution, differences in population age (older/younger), health-status composition of the population infected by SARS-CoV-2, and epigenetic/genetic factors. Pollution and higher population density may be also implicated. For example, population density is higher in North Italy compared to Central and South Italy. North Italy is recognized as one of the most polluted geographical areas in Europe. Air pollution, mainly due to particulate matter (PM), ozone, and other pollutants, is emerging as an important factor in COVID-19 transmission and mortality. PM could act directly as a carrier and indirectly as an amplifier of the effects on the lung [84]. Interestingly, the lowest mortality rates in Southern Italian regions were reported in Molise (0.007%) and Basilicata (0.005%) where the forest per capita ratio is higher, thereby suggesting that evergreen Mediterranean forests and shrubland plants might protect the population with the emission of immunomodulating bioactive organic compounds as well as supplying dietary sources of bioactive compounds [85].
The relationship between adherence to Mediterranean Diet and COVID-19 mortality has been assessed in a recent ecological study performed in 17 autonomous regions in Spain and in other 23 countries using the OECD (Well-Being Database for Mediterranean Adequacy Index score). A negative association between adherence to the Mediterranean Diet and COVID-19 cases and related deaths was found in this study, suggesting a role of Mediterranen diet in reducing COVID-19 infection rate and fatality [86]. A longitudinal epidemiological study conducted in Spain confirmed an inverse association between adherence to Mediterranean diet and risk of SARS-CoV-2 infection. In this study, the adherence to Mediterranean diet was assessed using the Mediterranean Diet Score (MDS) proposed by Trichopoulou. Better adherence to the Mediterranean diet was associated with lower risk of infection. The reduction was more than 60%in the group with higher adherence to the Mediterranean diet (MDS score > 6) [87]. Though these results suggest a role of Mediterranean diet in prevention and progression of COVID-19, the observational design of these two studies does not allow to prove a causal relationhip, and clinical trials are are needed for confirmation.
The impact of lockdown and quarantine on eating habits and physical activity deserves a comment. A large survey on Italian population, including 3533 Italians aged 12–86 years, showed that during COVID-19 lockdown a large proportion of responders (35.8%) consumed less healthy foods and 48.6%reported weight gain. Nevertheless, a higher adherence to the MDP, assessed using the MEDAS (a validated 14-items Mediterranean diet adherence screener), was found in the population group aged 18–30 years when compared to the younger and elderly population. A significantly greater adherence to the Mediterranean diet was observed in North and South Italy and in the Islands when compared to Central Italy. As expected, people with normal weight had a significant greater level of adherence to Mediterranean diet in comparison to people who were overweight or obese. A slight increase in physical activity has been also reported, especially for body-weight training, in 38.3%of respondents [88]. This study confirms the negative effects of lockdown on eating habits and physical activity. Neverthless, it also demonstrates that lockdown may be an opportunity to maintain or improve adherence to Mediterannean diet and increase physical activity. Similar data have been reported in another recent Italian survey [89]. Adherence to the MDP during COVID-19 should be particularly recommended for individuals at risk, such as those with obesity, diabetes and other non communicable diseases.
COVID-19 pandemic is lasting more than expected. The world has been experiencing the pandemia for a year and a half, and future scenarios are uncertain and difficult to predict [90]. In this context, adopting healthy eating habits and an active lifestyle becomes of paramount importance to combat COVID-19. Furthermore, the long-term maintenance of the lifestyle changes adopted during lockdown could be an opportunity for reducing the risks of future lifestyle-related diseases.
4.5MDP and Sustainability
Over the past decades the Mediterranean diet progressively evolved from a healthy dietary pattern to a model of sustainable diet. Considering current lifestyle changes, the Mediterranean diet pyramid was updated in 2010 and new elements were added such as: portion sizes based on frugality, local habits, biodiversity, seasonality, culinary activities, traditional, local and eco-friendly food products, conviviality, adequate rest and regular physical activity. Later, taking into account the increasing concern on environmental sustainability, four sustainable benefits that characterize the Mediterranean diet were incorporated into one single comprehensive “Med Diet 4.0 framework” [91]. The four sustainable benefits include: 1) major health and nutrition benefits; 2) low environmental impacts and richness in biodiversity; 3) high socio-cultural food values; 4) positive local economic returns. A sustainable diet is characterized by food safety and accessibility, healthy food, environment-friendliness and biodiversity, fair trade, locality/seasonality and protection of culture, heritage, and skills. Many studies have shown that plant-based diets such as Mediterranean diet have a lower environmental impact than other dietary patterns. The sociocultural historical heritage of MDP was highlighted in 2010 by UNESCO which recognized the Mediterranean Diet as “intangible heritage of humanity”.
5Conclusions
A healthy and balanced diet with adequate intake of energy and nutrients has been recommended by many Health Care Institutions to combat COVID-19.
Among different healthy dietary patterns, the MDP is the most widely studied and its health benefits are supported by a large body of evidence. The nutritional quality and sustainability of the MDP have been also proved.
Adherence to the MDP can help reduce the risk of Sars-CoV-2 infection, improve outcome and mitigate consequences of the disease by supporting immune system, reducing inflammation and oxidative stress (Fig. 4). The association with regular physical activity provides adjunctive benefits. Both the Mediterranean diet and physical activity improve well-being and may help cope with psychological distress related to pandemia and social isolation.
Fig. 4
Potential role of foods and their bioactive components from Mediterranean diet, in combating COVID-19.
In conclusion, taking into account the numerous benefits of the MPD on health, the MDP may be considered as the best dietary pattern to prevent COVID-19 in non-infected individuals, and it may be used as an adjunctive therapy to improve outcome and favour recovery in COVID-19 patients.
Acknowledgments including sources of support
The authors have no acknowledgments.
Funding
The authors report no funding.
Conflict of interest
The authors have no conflict of interest to report.
References
[1] | Weiss SR , Leibowitz JL . Coronavirus pathogenesis. Adv Virus Res. (2011) ;8: :85–164. DOI: 10.1016/B978-0-12-385885-6.00009-2 |
[2] | Rothan HA , Byrareddy SN . The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. (1024) ;109: :33. DOI: 10.1016/j.jaut.2020.102433 |
[3] | Xu Z , Shi L , Wang Y , Zhang J , Huang L , Zhang C , et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. (2020) ;8: :420–422. DOI: 10.1016/S2213-2600(20)30076-X |
[4] | Zhou F , Yu T , Du R , Fan G , Liu Y , Liu Z , et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. (2020) ;395: :1054–62. DOI: 10.1016/S0140-6736(20)30566-3 |
[5] | Mehta P , McAuley DF , Brown M , Sanchez E , Tattersall RS , Manson JJ . COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. (2020) ;395: :1033–34. 10.1016/S0140-6736(20)30628-0 |
[6] | Del Valle DM , Kim-Schulze S , Huang HH , Beckmann ND , Nirenberg S , Wang B , et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat Med. (2020) ;26: :1636–1643. DOI: 10.1038/s41591-020-1051-9 |
[7] | Tay MZ , Poh CM , Renia L , MacAry PA , Ng LFP . The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. (2020) ;20: (6):363–74. DOI: 10.1038/s41577-020-0311-8 |
[8] | Mueller AL , McNamara MS , Sinclair DA . Why does COVID-19 disproportionately affect older people? Aging. (2020) ;12: (10):9959–998. DOI: 10.18632/aging.103344 |
[9] | Graf CE , Pichard C , Herrmann FR , Sieber CC , Zekry D , Genton L . Prevalence of low muscle mass according to body mass index in older adults. Nutrition (2017) ;34: :124–9. DOI: 10.1016/j.nut.2016.10.002 |
[10] | Bonafè M , Pratichizzo F , Giuliani A , Storci G , Sabbatinelli J , Olivieri F . Inflamm-aging: why older men are the most susceptible to SARS-CoV-2 complicated outcomes. Cytokine Growth Factor Rev (2020) ;53: :33–37. DOI: 10.1016/j.cytogfr.2020.04.005 |
[11] | Angelini S , Pinto A , Hrelia P , Malagutti M , Buccolini F , Donini ML et al . The “Elderly” Lesson in a “Stressful” Life: Italian Holistic Approach to Increase COVID-19 Prevention and Awareness. Front Endocrinol (Lausanne). (2020) ;30;11: :579401. DOI: 10.3389/fendo.2020.579401 |
[12] | World Health Organization. Information note on COVID-19 and NCDs. Available online: https://www.who.int/internal-publications-detail/covid-19-and-ncds. Accessed March 23, 2020. |
[13] | Yang J , Zheng Y , Gou Xi , Pu K , Chen Z , Guo Q , et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: A systematic review and meta-analysis. Int. J. Infect. Dis. (2020) ;94: :91–95. DOI: 10.1016/j.ijid.2020.03.017 |
[14] | Van Kerkhove MD , Vandemaele KA , Shinde V , Jaramillo-Gutierrez G , Koukounari A , Donnelly CA , et al. Risk factors for severe outcomes following 2009 influenza a (H1N1) infection: A global pooled analysis. PLoS Med. (2011) Jul; 8: (7). DOI: 10.1371/journal.pmed.1001053 |
[15] | Calder PC . Nutrition, immunity and COVID-19. BMJ Nutrition, Prevention & health 2020. http://dx.doi.org/10.1136/bmjnph-2020-000085 |
[16] | Calder PC , Carr AC , Gombart AF , Eggersdorfer M . Optimal nutritional status for a well-functioning immune system is an Important factor to protect against viral infections. Nutrients. (2020) ;12: (4):1181. DOI: 10.3390/nu12041181 |
[17] | Zhao X , Li Y , Ge Y , Shi Y , Lv P , Zhang J , et al. Evaluation of nutrition risk and its association with mortality risk in severely and critically Ill COVID-19 patients. JPEN J Parenter Enteral Nutr. (2021) ;45: (1):32–42. DOI: 10.1002/jpen.1953 |
[18] | Wu C , Chen X , Cai Y , Xia J , Zhou X , Xu S , et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus Disease pneumonia in Wuhan, China. JAMA Intern Med (2020) ;180: (7):934–943. DOI: 10.1001/jamainternmed.2020.0994 |
[19] | Tamara A , Tahapary DL . Obesity as a predictor for a poor prognosis of COVID a systematic review. Diabetes Metab Syndr Clin Res Rev. (2020) ;14: (4):655–659. DOI: 10.1016/j.dsx.2020.05.020 |
[20] | World Obesity. Covid-19 and Obesity: The 2021 Atlas, March 2021. (http://www.worldobesity.org) |
[21] | Simonnet A , Chetboun M , Poissy J , Raverdy V , Noulette J , Duhamel A , et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. (2020) ;28: (7):1195–1199. DOI: 10.1002/oby.22831 |
[22] | Moriconi D , Masi S , Rebelos E , Virdis A , Manca ML , De Marco S et al. Obesity prolongs the hospital stay in patients affected by COVID-19 and may impact on SARS-COV-2 shedding. Obes. Res. Clin. Pract. (2020) ;14: :205–209. DOI: 10.1016/j.orcp.2020.05.009 |
[23] | Yang J , Hu J , Zhu C . Obesity aggravates COVID-19: a systematic review and meta-analysis. J Med Virol (2021) ;93: (1):257–261. doi: 10.1002/jmv.26237. DOI: 10.1002/jmv.26237 |
[24] | Luzi L , Radaelli MG . Influenza and obesity: Its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol. (2020) ;57: :759–764. DOI: 10.1007/s00592-020-01522-8 |
[25] | Michalakis K , Ilias I . SARS-CoV-2 infection and obesity: Common inflammatory and metabolic aspects. Diabetes Metab. Syndr. (2020) ;14: :469–471. DOI: 10.1016/j.dsx.2020.04.033 |
[26] | Ellulu MS , Patimah I , Khaza’ai H , Rahmat A , Abed Y . Obesity and inflammation: The linking mechanism and the complications. Arch. Med Sci. (2017) ;13: :851–863. DOI: 10.5114/aoms.2016.58928 |
[27] | Hotamisligil GS . Inflammation, metaflammation and immunometabolicdisorders. Nature (2017) ;542: :177–185. DOI: 10.1038/nature21363 |
[28] | Iddir M , Brito A , Dingeo G , Sosa Fernandez Del Campo S , Samouda H , La Frano MR et al Strengthening the Immune system and reducing inflammation and oxidative stress through diet and nutrition: considerations during the COVID-19 crisis. Nutrients. (2020) ;12: (6):1562. DOI: 10.3390/nu12061562 |
[29] | Chen Y , Zhou J , Wang L . Gut microbiota in human metabolic health and disease. Front Cell Infect Microbiol. (2021) ;17: :625913. doi: 10.3389/fcimb.2021625913 |
[30] | Cani PD . Human gut microbiome: hopes, threats and promises. Gut. (2018) ;67: :1716–1725. Doi: 10.1136/gutjnl-2018-316723 |
[31] | Fan Y , Pedersen O . Gut microbiota in human metabolic health and disease. Nat Rev Microbiol (2021) ;19: ;January 20. https://doi.org/10.1038/s41579-020-0433-9 |
[32] | Tsigalou C , Konstantinidis T , Parashaki A , Stavropoilou E , Voidarou C , Bezirtzoglou E . Mediterranean diet as a tool to combat inflammation and chronic diseases. An overview. (2020) ;8: (7):201. DOI: 10.3390/biomedicines8070201 |
[33] | World Health Organization. Nutrition advice for adults during the COVID-19 outbreak (19/06/2020). Available from http://www.emro.who.int. |
[34] | FAO 2020. Maintaining a healthy diet during the COVID-19 pandemic (available from: ww.fao.org.). |
[35] | CDC Center for Disease Control and Prevention. 2020. Food and Coronavirus Disease 2019 (COVID-19) (http://www.cdc.gov). |
[36] | Barazzoni R , Bischoff SC , Breda J , Wickramasinghe K , Krznaric Z , Nitzan D , et al. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-Cov-2 infection. Clin Nutr. (2020) ;39: :1631–1638. DOI: 10.1016/j.clnu.2020.03.022 |
[37] | Warburton DER , Bredin SSD . Health benefits of physical activity: A systematic review of current systematic reviews. Curr Opin Cardiol. (2017) ;32: :541–556. DOI: 10.1097/HCO.0000000000000437 |
[38] | Chen X , Sun X , Wang C , He H . Effects of exercise on inflammatory cytokines in patients with type 2 diabetes. Oxid Med Cell Longev. (2020) ;2020: :6660557. doi:10.1155/2020/6660557 |
[39] | Jenkins M , Houge-Mackenzie S , Hodge K , Hargreaves KE , Calverley JR , Lee C . Physical activity and psychological well-being during the COVID-19 lockdown: relationships with motivational quality and nature contexts. Front Sports Act Living. (2021) ;3: :637576. DOI: 10.3389/fspor.2021.637576 |
[40] | Bach-Faig A , Berry EM , Lairon D , Reguant J , Trichopoulou A , Dernini S , et al. Mediterranean Diet Foundation Expert GrouMediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. (2011) ;14: :2274–2284. DOI: 10.1017/S1368980011002515 |
[41] | Willett WC , Sacks F , Trichopoulou A , Drescher G , Ferro-Luzzi A , Helsing E , et al. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. (1995) ;61: :1402S–1406S. DOI: 10.1093/ajcn/61.6.1402S |
[42] | Marventano S , Kolacz P , Castellano S , Galvano F , Buscemi S , Mistretta A , et al. A review of recent evidence in human studies of n-3 and n-6 PUFA intake on cardiovascular diseases, cancer, and depressive disorders: Does the ratio really matter? Int. J. Food Sci. Nutr. 2015. DOI: 10.3109/09637486.2015.1077790 |
[43] | Trichopoulou A , Lagiou P . Healthy Traditional Mediterranean Diet: an expression of culture, history, and lifestyle. Nutr Rev (1997) ;55: :383–389. DOI: 10.1111/j.1753-4887.1997.tb01578.x |
[44] | Sofi F , Abbate R , Gensini GF , Casini A . Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. Am J Clin Nutr. (2010) ;92: :1189–1196. DOI: 10.3945/ajcn.2010.29673 |
[45] | Estruch R , Ros E , Salas-Salvado J , Covas MI , Corella D , Arós F , et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. (2018) Jun 21;378: (25):e34. DOI: 10.1056/NEJMoa1800389 |
[46] | Panagiotakos DB , Georgousopoulou EN , Pitsavos C , Chrysohoou C , Skoumas I , Pitaraki E , et al. Exploring the path of Mediterranean diet on10-year incidence of cardiovascular disease: TheATTICAstudy (2002–2012). Nutr Metab Cardiovasc Dis. (2015) ;25: (3):327–35. DOI: 10.1016/j.numecd.2014.09.006 |
[47] | Schwingshackl L , Schwedhelm C , Galbete C , Hoffmann G . Adherence to Mediterranean Diet and risk of cancer: an updated systematic review and meta-analysis. Nutrients. (2017) ;26;9: (10):1063. DOI: 10.3390/nu9101063 |
[48] | Valls-Pedret C , Sala-Vila A , Serra-Mir M , Corella D , de la Torre R , Martinez-Gonzalez MA , et al. Mediterranean diet and age-related cognitive decline: a randomized clinical trial. JAMA Intern Med. (2015) ;175: :1094–1103. DOI: 10.1001/jamainternmed.2015.1668 |
[49] | Psaltopoulou T , Sergentanis TN , Panagiotakos DB , Sergentanis IN , Kosti R , Scarmeas N . Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol (2013) ;74: :580–91. DOI: 10.1002/ana.23944 |
[50] | Holt ME , Lee JW , Morton KR , Tonstad S . Mediterranean diet and emotion regulation. Med J Nutr Metab. (2014) ;7: :163–172. DOI: 10.3233/MNM-140016 |
[51] | Galilea-Zabalza I , Buil-Cosiales P , Salas-Salvadò J , Toledo E , Ortega-Arzorìn C , Dìez-Espino J et al. Mediterranean diet and quality of life: Baseline cross-sectional analysis of the PREDIMED-PLUS trial. PLoS One. (2018) ;13: (6):e0198974. DOI: 10.1371/journal.pone.0198974 |
[52] | Castro-Quezada I , Román-Viñas , Serra-Majem L . The Mediterranean diet and nutritional adequacy: a review. Nutrients. (2014) ;6: :231–48. DOI: 10.3390/nu6010231 |
[53] | Schwingshackl L , Hffmann G . Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutr Metab Cardiovasc Dis (2014) ;24: :929–39. DOI: 10.1016/j.numecd.2014.03.003 |
[54] | Maiorino MI , Battistella G , Petrizzo M , Scappaticcio L , Giugliano G , Esposito K . Mediterranean diet cools down the inflammatory milieu in type 2 diabetes: the MEDITA randomized controlled study. Endocrine. (2016) Dec;54: (3):634–641. DOI: 10.1007/s12020-016-0881-1 |
[55] | Battino M , Forbes-Hernández TY , Gasparrini M , Afrin S , Cianciosi D , Zhang J , Manna PP et al. Relevance of functional foods in the Mediterranean diet: the role of olive oil, berries and honey in the prevention of cancer and cardiovascular diseases. Crit Rev Food Sci Nutr. (2019) ;59: (6):893–920. DOI: 10.1080/10408398.2018.1526165 |
[56] | Cianciosi D , Forbes-Hernández TY , Ansary J , Gil E , Amici A , Bompadre S , et al. Phenolic compounds from Mediterranean foods as nutraceutical tools for the prevention of cancer: The effect of honey polyphenols on colorectal cancer stem-like cells from spheroids. Food Chem. (2020) ;325: :126881. DOI: 10.1016/j.foodchem.2020.126881 |
[57] | Cianciosi D , Varela-Lopez A , Forbes-Hernandez TY , Gasparrini M , Afrin S , Reboredo-Rodriguez P , et al. Targeting molecular pathways in cancer stem cells by natural bioactive compounds. Pharmacol Res. (2018) ;135: :150–165. https://doi.org/10.1016/j.phrs.2018.08.006 |
[58] | Sini H , Devi KS , Anusha CS , Nevin KG . Edible Solanum trilobatum chloroform extract modulates CCL4 induced toxic changes in rat liver by enhancing the antioxidant activity. Med J Nutr Metab (2021) ;14: :115–126. DOI: 10.3233/MNM-200446 |
[59] | Arango-Varela S , Torres-Camargo D , Reyes-Dieck C , Zapata-Landono MB , Maldonado-Celis ME . Aqueous extract of andean berry induces apoptosis in human colon cancer cells without mitochondrial damage. J Berry Res. 2021: :1–16. DOI:10.3233/JBR-200684 |
[60] | Salinas-Peña E , Mendoza-Rodríguez M , Velázquez-González C , Medina-Solis CE , Pontigo-Loyola AP , Márquez-Corona M , et al. Antibacterial properties in-vitro of Mexican serviceberry extracts against dental biofilm species. J Berry Res (2021) ;11: :431–446. DOI: 10.3233/JBR-210718 |
[61] | Khan H , Belwal T , Efferth T , Farooqui AA , Sanchez-Silva A , Vacca RA et al. Targeting epigenetics in cancer: therapeutic potential of flavonoids. Crit Rev Food Sci Nutr. (2021) ;61: (10):1616–1639. doi: 10.1080/10408398.2020.1763910 |
[62] | Ullah H , De Filippis A , Santarcangeo C , Daglia M . Epigenetic regulation by polyphenols in diabetes and related complications. Med J Nutr Metab (2020) ;13: (4):289–310. DOI: 10.3233/MNM-200489 |
[63] | Giampieri F , Gasbarrini M , Forbes-Henandez YT , Mazzoni L , Capocasa F , Sabbadini S et al. Overexpression of the Anthocyanidin Synthase Gene in Strawberry Enhances Antioxidant Capacity and Cytotoxic Effects on Human Hepatic Cancer Cells. J Agric Food Chem. (2018) ;66: :581–592. DOI: 10.1021/acs.jafc.7b04177 |
[64] | Levy E , Delvin E , Marcil V , Spahis S . Can phytotherapy with polyphenols serve as a powerful approach for the prevention and therapy tool of novel coronavirus disease 2019 (COVID-19)? Am J Physiol Endocrinol Metab (2020) ;319: (4):E689–E708. DOI: 10.1152/ajpendo.00298.2020 |
[65] | Quiles JL , Rivas-García L , Varela-López A , Llopis A , Battino M , Sánchez-González C . Do nutrients and other bioactive molecules from foods have anything to say in the treatment against COVID-19? Environ Res. (2020) ;191: :110093. DOI: 10.1016/j.envres.2020.110053 |
[66] | Yi L , Li Z , Yuan K , Qu X , Chen J , Wang G , et al. Small molecules blocking the entry of severe acute respiratory syndrome coronavirus into host cells. J Virol (2004) ;78: (20):11334–9. DOI: 10.1128/JVI.78.20.11334-11339.2004 |
[67] | Tiao M-M , Lin Y-J , Yu H-R , Sheen J-M , Lin I-C , Lai Y-J , et al. Resveratrol ameliorates maternal and post-weaning high-fat diet-induced nonalcoholic fatty liver disease via renin-angiotensin system. Lipids Health Dis. (2018) ;17: :178. https://doi.org/10.1186/s12944-018-0824-3 |
[68] | Oliveira Andrade JM , Paraíso AF , Garcia ZM , Ferreira AVM , Sinisterra RDM , Sousa FB et al. Cross talk between angiotensin-(1-7)/Mas axis and sirtuins in adipose tissue and metabolism of high-fat feed mice. Peptides (2014) ;55: :158–165. https://doi.org/10.1016/j.peptides.2014.03.006 |
[69] | Moran CS , Biros E , Krishna SM , Wang Y , Tikellis C , Morton SK et al. Resveratrol inhibits growth of experimental abdominal aortic aneurysm associated with upregulation of angiotensin-converting enzyme 2. Arterioscler Thromb Vasc. Biol. (2017) ;37: :2195–2203. https://doi.org/10.1161/ATVBAHA.117.310129 |
[70] | Horne JR , Vohl MC . Biological plausibility between dietary fat, resveratrol, ACE2, and SARS-CoV illness severity. Am J Physiol Endocrinol Metab. (2020) ;318: (5):E830–833. DOI: 10.1152/ajpendo.00150.2020 |
[71] | Zabetakis I , Lordan R , Norton C , Tsoupras A . COVID-19: The Inflammation Link and the Role of Nutrition in Potential Mitigation. Nutrients. (2020) ;12: (5):1466. DOI: 10.3390/nu12051466 |
[72] | Daoust L , Pilon G , Marette A . Perspective: nutritional strategies targeting the gut microbiome to mitigate COVID-19 outcomes. Adv Nutr. 2021 Mar 30; nmab031. DOI: 10.1093/advances/nmab031 |
[73] | Zuo T , Zhang F , Lui GCY , Yeoh YK , Li AYL , Zhan H et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology. (2020) ;159: (3):944–55. DOI: 10.1053/j.gastro.2020.05.048 |
[74] | Yeoh YK , Zuo T , Lui GC , Zhang F , Liu Q , Li AY , et al. Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with Covid-19. Gut. (2021) ;70: (4):698–706. DOI: 10.1136/gutjnl-2020-323020 |
[75] | Diao B , Wang C , Tan Y , Chen X , Liu Y , Ning L , et al. Reduction and Functional Exhaustion of T Cells in Patients with Coronavirus Disease 2019 (COVID-19). Front Immunol. (2020) ;11: :827. DOI: 10.3389/fimmu.2020.00827 |
[76] | Weaver LK , Minichino D , Biswas C , Chu N , Lee JJ , Bittinger K , et al. Microbiota-dependent signals are required to sustain TLR-mediated immune responses. JCI Insight. Jan 10e70. (2019) Jan 10;4: (1):e124370. DOI: 10.1172/jci.insight.124370 |
[77] | Li M-Y , Li L , Zhang Y , Wang X-S . Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. (2020) Apr 28;9: (1):45. DOI: 10.1186/s40249-020-00662-x |
[78] | Wang J , Zhao S , Liu M , Zhao Z , Xu Y , Wang P , et al. ACE2 expression by colonic epithelial cells is associated with viral infection, immunity and energy metabolism. medRxiv 2020.02.05.20020545. DOI:10.1101/2020.02.05.20020545 |
[79] | De Oliveira GLV , Oliveira CNS , Pinzan CF , de Salis LVV , Cardoso CRB . Microbiota modulation of gut-lung axis. Front Immunol. (2021) ;12: :635471. DOI: 10.3389/fimmu.2021.635471 |
[80] | Hao Q , Dong BR , Wu T . Probiotics for preventing acute upper respiratory tract infections. Cochrane Database Syst Rev. (2015) ;2: :CD006895. DOI: 10.1002/14651858.CD006895.pub3 |
[81] | Su M , Jia Y , Li Y , Zhou D , Jia J . Probiotics for the Prevention of Ventilator- Associated Pneumonia: A Meta-Analysis of Randomized Controlled Trials. Respir Care. (2020) ;65: (5):673–685. DOI: 10.4187/respcare.07097 |
[82] | Veronese N , Notarnicola M , Cisternino AM , Inguaggiato R , Guerra V , Reddavide R , et al; MICOL study group.. Trends in adherence to the Mediterranean diet in South Italy: a cross sectional study. Nutr Metab Cardiovasc Dis. (2020) ;30: (3):410–17. DOI: 10.1016/j.numecd.2019.11.003 |
[83] | Moreno-Altamirano L , Hernandez-Montoya D , Soto-Estrada G , Garcia-Garcia JJ , Silberman M , Capraro S , et al. Changes in Mediterranean dietary patterns in Italy from 1961 to 2011. Med J Nutr Metab (2016) ;9: :171–181. DOI: 10.3233/MNM-16111 |
[84] | Conticini E , Frediani B , Caro D . Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut. (2020) ;261: :114465. DOI: 10.1016/j.envpol.2020.114465 |
[85] | Roviello V , Roviello GN . Lower Covid-19 mortality in Italian forested areas suggest immunoprotection by Mediterranean plants. Environ Chem Lett (2020) ;14: :1–12. DOI: 10.1007/s10311-020-01063-0 |
[86] | Greene MW , Roberts AP , Frugé AD . Negative Association Between Mediterranean Diet Adherence and COVID-19 Cases and Related Deaths in Spain and 23 OECD Countries: An Ecological Study Front Nutr. (2021) ;8: :591964. DOI: 10.3389/fnut.2021.591964 |
[87] | Perez-Araluce R , Martinez-Gonzales MA , Fernandez-Lazaro CI , Bes-Rastrollo M , Gea A , Carlos S . Mediterranean diet and the risk of COVID-19 in the ‘Seguimiento Universidad de Navarra’ cohort. Clin Nutr 2021 (article in press) |
[88] | Di Renzo L , Gualtieri P , Pivari F , Soldati L , Attinà A , Cinelli G , et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J Transl Med. (2020) ;18: (1):229. DOI: 10.1186/s12967-020-02399-5 |
[89] | Izzo L , Santonastaso A , Cotticelli G , Federico L , Pacifico S , Castaldo L et al. An Italian survey on dietary habits and changes during the COVID-19 lockdown. Nutrients. (2021) ;13: (4):1197. DOI: 10.3390/nu13041197 |
[90] | Scudellari M . How the pandemic might play out in and beyond. Nature. (2020) ;584: :22–25. DOI: 10.1038/d41586-020-02278-5 |
[91] | Dernini S , Berry EM , Serra-Majem L , La Vecchia C , Capone R , Medina FX , et al. Med Diet 4.0: the Mediterranean diet with four sustainable benefits. Public Health Nutr. (2017) ;20: (7):1322–1330.. DOI: 10.1017/S1368980016003177 |




