How much do celiac patients know about gluten free diet?
Abstract
BACKGROUND:
Adherence to gluten free diet (GFD) has been the object of many studies but few have investigated its essential requisite: a thorough knowledge of gluten sources.
OBJECTIVE:
Our aim was to measure celiac patients’ knowledge of GFD and assess its determinants.
METHODS:
A 20-item questionnaire was submitted to our celiac outpatients who were asked to indicate which foods or situations might be at risk of gluten intake. A 20-point rating scale was built giving one point for each correct answer.
RESULTS:
154 patients were enrolled. The mean score of the knowledge test was 14.3±2.9. Focusing on the incorrect responses, only 20.8% of them would have placed patients at risk of consuming gluten while the other 79.2% concerned foods or situations that were unnecessarily avoided by the patients. A statistically significant lower score was obtained by patients aged over 60 years (p = 0.0002), without a degree or diploma (p = 0.0016), non-members of the Italian Celiac Association (p = 0.043), who never visited the Association website (p = 0.0002) and never ate outside (p = 0.0009).
CONCLUSIONS:
We identified some categories of celiac patients at risk of less knowledge of GFD who deserve special training and attention.
1Background
Coeliac disease (CD) is a chronic small intestinal immune-mediated enteropathy precipitated by exposure to dietary gluten in genetically predisposed people. Ingestion of gluten in CD patients causes villous atrophy in the small bowel and results in symptoms such as cramping, diarrhoea, iron deficiency anaemia, fatigue, weight loss, vitamin and mineral deficiencies. CD affects approximately 1% of the population, although it is estimated that a large number of people remain undiagnosed [1].
The only treatment for CD at present is a strict lifelong gluten-free diet (GFD), as even trace amounts of gluten are sufficient to trigger an immune response and impair histological healing [2]. There is sufficient evidence to suggest that compliance with a strict GFD decreases disease-related mortality and has a role in preventing some of the long-term complications, including osteoporosis and celiac-related malignancies [3].
Despite its obvious benefits, following a strict lifelong GFD remains one of the most challenging and intriguing issues. Strict adherence to the GFD has been estimated at between 40–90% depending on the method of evaluation and definition [4]. Due to the importance of strict adherence in CD, numerous researchers have investigated the factors related to GFD non-compliance in order to identify potential intervention targets. Despite a systematic review of adherence studies found that the most commonly reported correlates of GFD adherence fell into the broad categories of cognitive influences [4], limited information exists regarding patients’ awareness of GFD.
The aim of the current study was to evaluate how much celiac patients know about GFD and to assess significant predictive factors of less knowledge.
2Methods
Between March and December 2014 a questionnaire was submitted to the celiac outpatients followed at our Gastroenterology Unit. All patients were >18 years and on GFD for at least one year. An informed consent was signed before entering the study. The study was approved by the institutional review board of our hospital in accordance with the Helsinki Declaration of 2008.
The questionnaire was anonymous, submitted always by the same interviewer to avoid methodological bias and composed of two sections. The first part explored demographic features, how the patient was informed about GFD at the time of diagnosis, his/her celiac society membership, modalities of update on GFD and frequency of dining out.
In the second section GFD knowledge was assessed using a list of 20 foods/situations adapted from educational material provided by the Italian Celiac Association (AIC, Associazione Italiana Celiachia) (Table 1). Patients had to state whether each product could contain hidden gluten or not. Half of the questions involved foods/situations that really expose patients at risk of consuming gluten (a wrong answer to one of these questions was considered a major fault) while the other half concerned products that are gluten-free and therefore completely safe (minor fault in case of wrong answer). All questions were answered in a yes/no/do not know manner. One point was given for each correct answer and zero points for a wrong or do-not-know answer. A 20-point scale was used to define the level of knowledge. All data were recorded on an Excel ® spreadsheet.
2.1Statistics
Continuous variables were expressed as mean±standard deviation. The chi-square, or Fisher’s exact test when appropriate, was applied for categorical variables. The Student’s t test or ANOVA test were applied for continuous variables. A p value of less than 0.05 was considered significant. A statistical software program (SPSS version 11.0, SPSS Inc., Chicago, IL) was employed.
3Results
3.1Section #1
One hundred and fifty-four celiac patients were enrolled. Their demographic characteristics are displayed in Table 2.
Information about GFD had been provided to 83% of patients at the time of diagnosis, usually by gastroenterologists (92.2% ), while the remaining 17% was mostly trained by the AIC.
The 74.7% of patients (115/154) was member of the AIC. Among them 41 (35.6% ) always read the newsletter updates of the AIC, while patients that often, rarely or never read the updates were respectively 37 (32.2% ), 28 (24.3% ) and 9 (7.8% ).
Forty-eight patients (31.2% ) never logged into the AIC website in the last year whereas 38 (24.7% ) logged-in at least three times, 27 (17.5% ) logged-in from 4 to 6 times, 23 (14.9% ) from 7 to 12 times and 18 (11.7% ) visited the AIC websites more than 12 times.
The mean number of meals consumed outside was 5.9 per month (range 0–40); the restaurants adhering to the AIC network were chosen by the majority of patients (56.7% vs 28.2% of non-AIC restaurants and 15.1% of friends’ house).
3.2Section #2
The mean score of the knowledge test was 14.3±2.9 on a 20-point scale. Considering all the 3080 submitted questions, 71.7% of these had a correct answer while the wrong ones were 16.9% and the “do not know” 11.4% . The answers given by the patients to each question are shown in Fig. 1. The most wrong answers were about bloomy rind cheeses (correct answer in 24% ), whisky (29% ), mixed seed oil (39% ), gorgonzola cheese (49% ) and cosmetics (52% ).
Focusing on the incorrect responses, only 20.8% of them would have placed patients at risk of consuming gluten (major faults) while the other 79.2% (minor faults) concerned foods or situations that were unnecessarily avoided by the patients.
3.3Predictors of knowledge about GFD
Table 3 summarize factors potentially affecting knowledge about GFD.
It emerges that patients aged over 60 years (p = 0.0002), without a degree or diploma (p = 0.0016), non-members of the AIC (p = 0.043), who never visited the AIC website (p = 0.0002) and never ate outside (p = 0.0009) showed a significant lower level of knowledge about GFD.
Conversely no significant correlation was observed between gender, information on GFD received at the time of diagnosis, disease duration and reading of the AIC paper updates.
4Discussion
Knowledge about GFD is closely related to adherence, representing a pivotal requirement for a successful therapy. However limited data are present in literature regarding patient’s knowledge of GFD because several studies have only focused on the determinants of adherence.
Our paper revealed that patients aged over 60 years, without a high-school degree or diploma, non- members of AIC, who never visited the AIC website and never ate outside showed a significant worse knowledge about GFD. In literature only the study by Tomlin et al. was found to analyze factors associated with a better parental knowledge about GFD. The authors reported that knowing someone with CD, particularly in the same family, and researching about the disease were predictive of better parental knowledge while the level of parental education was not [5].
Possible explanations of our results can be speculated. A lack of familiarity with new technologies (website login, download of smartphone applications etc) of the elderly patients with a consequent reduced ability to be constantly updated can justify their worse knowledge about GFD. The same reasons could explain the relationship between the number of the AIC website login per year and the level of knowledge. A lack of motivation and update are likely the causes of poor knowledge in the patients non-members of AIC. The length of time elapsed from diagnosis did not influence a worse knowledge showing that to become familiar with GFD a long training is not necessary. Similarly no significant correlation was observed between patients who did not receive information on GFD at the time of diagnosis and knowledge. These result reflects the possibility for not trained patients to easily obtain recommendation about GFD otherwise (i.e. AIC website, other specialists). Finally in subjects who never ate outside was reported a significant lower level of knowledge probably because these patients have a less varied diet and therefore less interest in learning which products are gluten-free. Therefore training on GFD and consolidation of recommendation should be focused and stressed on these categories of patients.
Overall 83% of patients received information on GFD at the diagnosis, usually by gastroenterologists, while the remaining 17% did not and was trained by the AIC or other specialist. Comparing these data with a German study where only 9.4% of patients were trained by a doctor and 35.9% by the German Celiac Society, we might be satisfied [6].
Patients showed a good level of knowledge about GFD with a high percentage (71.7% ) of correct answers. Limited data are available in literature to compare these results. Tomlin et al. observed that only 33.3% of parents of celiac pediatric patients correctly identified gluten containing foods [5]. Conversely Charalampopoulos et al. described that 67.7% of parents of celiac pediatric patients correctly chose all gluten-free products from a list of 12 products [7]. In the paper of Sainsbury et al. the mean correct percent on the knowledge test, assessed using a 14-ingredient list, was 80.5% [8], whereas Silvester et al. found a percentage of correct answers ranging from 7 to 82% in a 10-item questionnaire [9].
An important result highlighted in our paper is that the majority of incorrect answers refer to products that patients wrongly believed containing gluten (minor fault). This data reveals how the improvement of knowledge and the continuous updating on GFD would allow a greater choice of products and would avoid unnecessary limitation in GFD. In fact in the last years the GFD has become easier to follow, with fewer restrictions as many products, once considered forbidden, have proven to be gluten-free.
We are aware of the limitation of this study: there is no agreed gold standard for defining and measuring knowledge about GFD. Therefore the questionnaire performed was not validated and the majority of questions submitted refer to foods typical of the Italian diet.
On the other hand we think this study is important in several regards. Firstly it is focused on the knowledge of GFD and not on the adherence and therefore it analyzes the pivotal element determining a correct therapy in celiac patients. Secondly we described predictors of less knowledge, rarely reported before in literature, and so we identified categories of patients needing more training and closer follow-up about GFD. Finally this paper emphasizes the need for larger and methodologically robust studies about GFD knowledge, focusing on definition and measurement of knowledge and on the use of validated survey instruments.
References
1 | Green P , Cellier C Celiac disease. N Engl J Med. (2007) ;357: :1731–43. |
2 | Rubio-Tapia A , Murray J Celiac disease. Curr Opin Gastroenterol. (2010) ;26: :116–22. |
3 | Green P , Jabri B Coeliac disease. Lancet. (2000) ;362: :383–91. |
4 | Hall N , Rubin G , Charnock A Systematic review. Adherence to a gluten-free diet in adult patients with coeliac disease. Aliment Pharmacol Ther. (2009) ;30: :315–30. |
5 | Tomlin J , Slater H , Muganthan T , Beattie RM , Afzal NA Parental knowledge of coeliac disease. Inform Health Soc Care. (2015) ;40: (3), 240–53. |
6 | Meyer KG , Fasshauer M , Nebel IT , Paschke R Comparative analysis of conventional training and a computer-based interactive training program for celiac disease patients. Patient Educ Couns. (2004) ;54: (3):353–60. |
7 | Charalampopoulos D , Panayiotou J , Chouliaras G , Zellos A , Kyritsi E , Roma E Determinants of adherence to gluten-free diet in Greek children with coeliac disease: A cross-sectional study. Eur J Clin Nutr. (2013) ;67: (6):615–19. |
8 | Sainsbury K , Mullan B Measuring beliefs about gluten free diet adherence in adult coeliac disease using the theory of planned behavior. Appetite. (2011) ;56: :476–83. |
9 | Silvester JA , Weiten D , Graff LA , Walker JR , Duerksen DR Living gluten-free: Adherence, knowledge, lifestyle adaptations and feelings towards a gluten-free diet. J Hum Nutr Diet. (2015) ; [Epub ahead of print], doi: 10.1111/jhn.12316. |
Figures and Tables
Fig.1
Answers given by the patients to each question of the questionnaire Section #2.
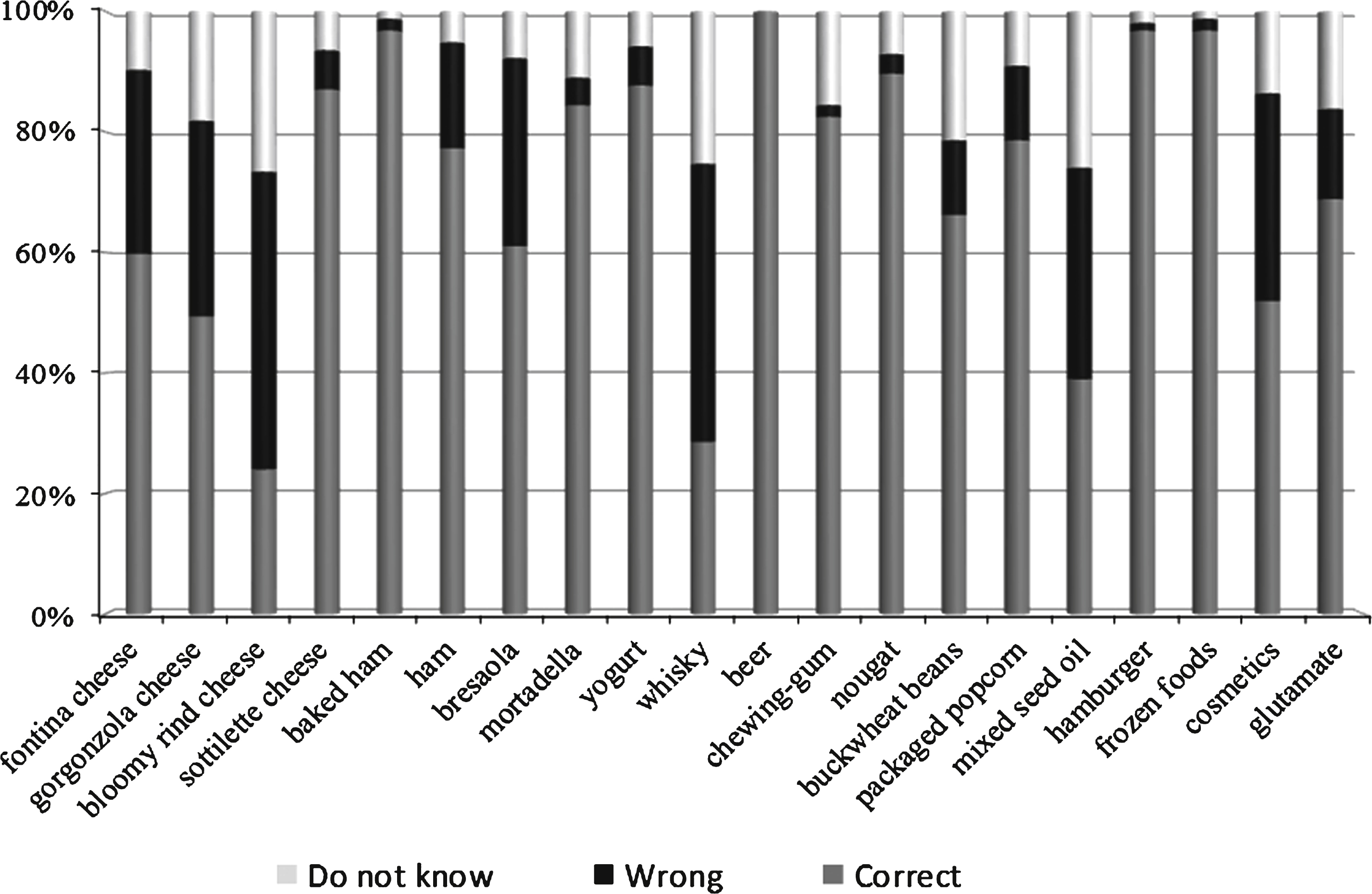
Table 1
Section 2 of the questionnaire. Celiac patients were asked to indicate foods/situations that really expose at risk of consuming gluten. The correct answers are provided
| Yes | No | I don’t know | |
| Fontina cheese | x | ||
| Gorgonzola cheese | x | ||
| Bloomy rind cheese | x | ||
| Sottiletta cheese | x | ||
| Baked ham | x | ||
| Ham | x | ||
| Bresaola | x | ||
| Mortadella | x | ||
| Yogurt | x | ||
| Whisky | x | ||
| Beer | x | ||
| Chewing-gum | x | ||
| Nougat | x | ||
| Buckwheat beans | x | ||
| Packaged popcorn | x | ||
| Mixed seed oil | x | ||
| Hamburger | x | ||
| All frozen foods are forbidden to celiac patients | x | ||
| Celiac patients must verify that cosmetics do not contain gluten | x | ||
| Foods containing glutamate as a preservative are forbidden for celiac patients | x |
Table 2
Demographic and clinical characteristics of patients enrolled in the study
| Number of patients enrolled (n) | 154 |
| Mean age (years±SD) | 39.8 ± 14.7 |
| Male [n (%)] | 44 (28.6) |
| Education [n (%)] | |
| Compulsory school | 40 (26) |
| High school | 68 (44.2) |
| Graduation | 46 (29.8) |
| Age at diagnosis (years ± SD) | 30.9 ± 16.0 |
| Length of time after diagnosis ( ± SD) | 8.7 ± 8.0 |
SD: standard deviation.
Table 3
Factors potentially affecting knowledge about GFD are listed
| Variables | Correct answer (mean ± SD) | p | |||
| Sex | Male | 13.7 ± 7.0 | 0.08 | ||
| Female | 14.6 ± 8.8 | ||||
| Age (years) | 16–20 | 14.6 ± 3.6 | 0.0002 *1 | ||
| 21–30 | 14.2 ± 6.0 | ||||
| 31–40 | 15.3 ± 7.0 | ||||
| 41–50 | 14.6 ± 9.6 | ||||
| 51–60 | 14.5 ± 7.1 | ||||
| > 60 | 11.1 ± 7.6 | ||||
| Education | Compulsory school | 13.1 ± 7.9 | 0.0016 *2 | ||
| High school | 14.3 ± 7.7 | ||||
| Graduation | 15.3 ± 7.9 | ||||
| Years after diagnosis | 1-2 | 14.9 ± 6.6 | 0.21 | ||
| 3–10 | 14.4 ± 8.8 | ||||
| > 10 | 13.8 ± 8.7 | ||||
| Information on GFD at diagnosis | Received | 14.6 ± 2.9 | 0.088 | ||
| Not received | 13.4 ± 2.8 | ||||
| ICA membership | Yes | 14.6 ± 2.8 | 0.043 | ||
| No | 13.5 ± 3.0 | ||||
| Reading of paper updates by ICA about GFD | Yes | 14.6 ± 2.9 | 0.95 | ||
| No | 14.6 ± 2.5 | ||||
| Login ICA website/year | None | 13.0 ± 6.1 | 0.0002 *3 | ||
| 1–6 | 14.5 ± 9.5 | ||||
| 7–12 | 15.5 ± 3.8 | ||||
| < 12 | 15.7 ± 9.2 | ||||
| Meals outside/month | None | 12.2 ± 9.0 | 0.0009 *4 | ||
| 1–5 | 14.6 ± 7.7 | ||||
| 6–10 | 15.2 ± 8.4 | ||||
| > 10 | 14.3 ± 5.4 | ||||
*1: overall p value. Pairwise comparisons were statistically significant for >60 vs 16–20 (p = 0.0022), >60 vs 21–30 (p = 0.0001), >60 vs 31–40 (p < 0.0001), >60 vs 41–50 (p = 0.0001) and >60 vs 51–60 (p = 0.0009). *2:overall p value. Pairwise comparisons were statistically significant for compulsory school vs high school (p = 0.0314), and compulsory school vs graduation (p = 0.0004). *3: overall p value. Pairwise comparisons were statistically significant for none vs 1–6 (p = 0.0094), none vs 7–12 (p < 0.0001) and none vs >12 (p = 0.0003). *4: overall p value. Pairwise comparisons were statistically significant for none vs 1–5 (p = 0.0003), none vs 6-10 (p = 0.0011) and none vs >10 (p = 0.016).




