Seeking a low value of HbA1c may be dangerous under recurrent episodes of hypoglycaemia: A short report
Abstract
During the last decades, HbA1c became a standard assay in the control of risks for diabetic complications. Epidemiological studies and clinical trials have explored and determined the relationship between HbA1c and mean blood glucose. However, for patients and health care providers, a clear understanding of this relationship is necessary for setting appropriate day-to-day blood glucose testing goals aiming to achieve specific HbA1c targets while avoiding hypoglycaemia.
1Background
The effect of intensive treatment of diabetes on the development and progression of long-term complications of type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) was considered by the Diabetes Control and Complications Trial Research Group (DCCT) [1] and the U.K. Prospective Diabetes Study Group (UKPDS) [2]. The two studies established the relationship between the glycated haemoglobin (HbA1c) levels and risks for diabetic complications in T1DM and T2DM.
Consequently, the HbA1c assay became widely accepted and used for assessing chronic glycaemia [3]. More precisely, different epidemiologic studies and clinical trials have explored the relationship between HbA1c and the mean blood glucose (MBG) [4, 5]. Using a linear regression on data of DCCT (n = 1439 patients), Rohlfing et al. found that HbA1c and mean plasma glucose (MPG) were correlated (r2 = 0.82) and hence determined the following relationship between HbA1c and MPG [4]:
Nonetheless, the values of measured and computed HbA1c may be in very good agreement while the daily blood glucose may show large variations with dangerous recurrent mild and severe episodes of hypoglycaemia. An illustration is provided by the following case.
2Case presentation
Although the guidelines given by diabetes associations worldwide, and the recommendations generally provided by doctors advise people with diabetes to avoid hyperglycaemia as well as hypoglycaemia, we think that the case presented here is interesting for the following reasons:
1. The 27 old patient (B.W) is a doctoral student living with T1DM since the age of one year,
2. B.W is a citizen of a low-medium income country where students have no medical insurance and cannot afford insulin pumps nor continuous self-monitoring systems,
3. She is convinced that avoiding high levels of blood glucose is the main rule to avoid complications of diabetes or at least to delay them as far as possible,
4. The link between daily high blood glucose and complications has constituted a psychological fear of hyperglycaemia and consequently pushed her to undergo recurrent episodes of hypoglycaemia,
5. With time, the patient has become unaware of hypoglycaemia and her family has noticed that a hypoglycaemia from which B.W used to recover after ten to fifteen minutes if a 15–20 g sugary drink was taken, is now needing one hour and a huge quantity of sugar. During the last three months, unawareness represented around 75% of all hypoglycaemia episodes (for capillary glucose <70 mg/dl).
3Data collection
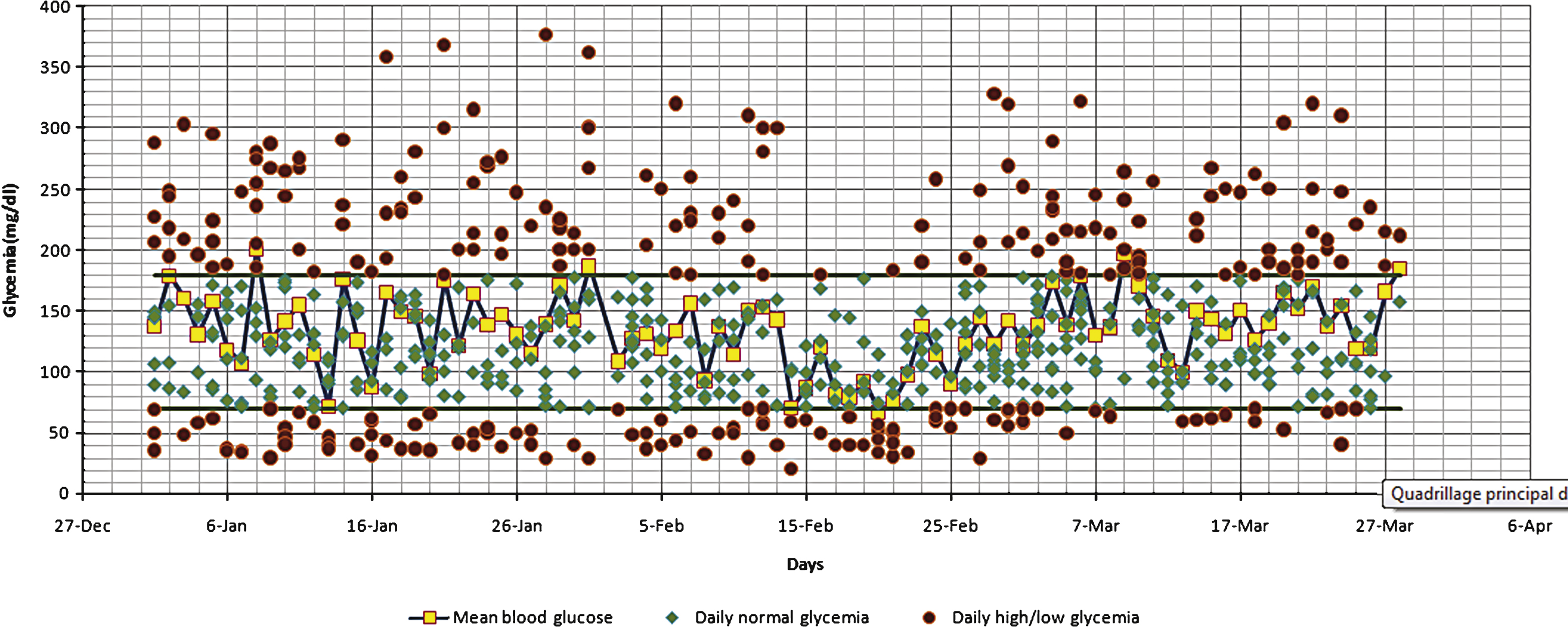
Using a self-monitoring glucometer, the patient performed nearly 700 finger stick capillary glucose tests over three months, representing an average of 7 to 8 measurements per day. Figure 1 below shows that during the three months period, the average blood glucose was ideally situated between 70 mg/dl and 180 mg/dl. On the other hand, the patient has excessively suffered from recurrent mild and severe hypoglycaemia (over the three months period, the number of hypoglycaemia episodes was 115 of which 15 (13% ) were severe episodes).
4Comparison of computed and measured HbA1c
The measured value of HbA1c was obtained through a Biological Laboratory using a HPLC, D-10 HbA1c Technics. At the end of the three months period, measured HbA1c was: 7.2% .
Using MPG = 1.1 MBG and the inverse of relations ( *) and ( **) to compute HbA1c as a function of MPG (HbA1c = 2.6 + 0.03 * MPG and HbA1c = 1.63 + 0.035 * MPG), provided the calculated HbA1c = 7.3% and HbA1c = 7.1% respectively. The measured and computed HbA1c appear in a good agreement.
5Discussion
Ogawa et al. showed that glycaemic standard deviation is not associated with A1c, but has a significant positive correlation with fasting plasma glucose, glycated albumin(GA) and GA/A1c ratio [6]. Kilpatrick et al. established that HbA1c, MBG and glucose variability measurements each have an independent role in determining an individual’s risk of hypoglycemia in type 1 diabetes [7]. Ceriello et al. reported that hyperglycaemia after recovery from hypoglycaemia worsens cardiovascular risks in healthy subjects and subjects with T1DM [8].
As stressed by diabetes associations worldwide, HbA1c is a “must” for diabetes control but its traps should be kept in mind. For instance, a patient may be falsely reassured by a low HbA1c obtained by alternating episodes of hypo-hyperglycaemia [9]. In this direction, the present case illustrates clearly the insufficiency of the measured value of HbA1c as a criterion of good glycaemic control because this value reflects only the average blood glucose and does not capture the glycaemic variations. In the case of a diabetic suffering from recurrent hypoglycaemia (as our case), there may be a compensating effect between lower and higher glycaemic values, leading to a MBG corresponding to an ideal HbA1c. In such a case, the patient may be very happy with his or her achievement when he or she must be very careful about the danger of repetitive episodes of low blood glucose. Indeed, many studies have shown that hypoglycaemia constitutes a high risk of morbidity and mortality [10–14]. McCoy et al. followed a cohort of 1,013 patients with T1DM and T2DM and found that after 5 years, patients who reported severe hypoglycaemia had 3.4-fold higher mortality compared with those who reported mild/no hypoglycaemia [10]. A similar rate of mortality (4% ) was reported by Patterson et al. in EURODIAB population-based cohorts of T1DM [11]. Higher rates (6% , 7% and 10% ) of deaths caused by hypoglycaemia among patients with T1DM were reported by Jacobson et al. [12], Feltbower et al. [13] and Skrivarhaug et al. [14].
6Conclusion
While recalling that HbA1c constitutes a standard assay in the control of risks for diabetic complications, it should also be stressed that HbA1c may be insufficient or even misleading in the case of patients suffering from hypoglycaemia. Moreover, treatment of hypoglycaemia is generally accompanied by high levels of blood glucose but the two adverse events are not seen in HbA1c. The 2015 ADA’s diabetes guidelines indicates that a less stringent target (HbA1c <8) should be sought in case of hypoglycaemia [4]. Interpreting HbA1c as a measure of MBG is meaningful only in the case of stable glycaemia, and a clear understanding of the relationship between MBG and HbA1c is necessary for achieving low HbA1c levels while avoiding hypoglycaemia. Finally there should be more sensitisation about the danger of hypoglycaemia for patients who seek a HbA1c <7, especially for people with T1DM living in developing countries where specialists of diabetes give more importance to the value of HbA1c since the majority of patients have few or no self monitoring data.
For patients and health care providers, a clear understanding of the relationship between MBG and HbA1c is necessary for setting appropriate day-to-day BG testing goals with the expectation of achieving specific HbA1c targets while avoiding hypoglycaemia [6].
Consent
The authors confirm that the patient has given her consent for the Case Report to be published.
Competing interests
The authors affirm that there is no competing interest.
References
1 | The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications of insulin-dependent diabetes mellitus. New England Journal of Medicine. (1993) ;329: :977–86. |
2 | UK Prospective Diabetes Study Group (UKPDS). Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. (1998) ;352: :837–53. |
3 | American Diabetes Association (ADA). Standards of medical care in diabetes. Diabetes Care. (2015) ;38: (Supp l):S1–S93. |
4 | Rohlfing CL , Wiedmeyer HM , Little RR , England JD , Tennili A , Goldestein DE . Defining the Relationship Between Plasma Glucose and HbA1c Analysis of glucose profiles and HbA1c in the Diabetes Control and Complications Trial. Diabetes Care. (2002) ;25: (2):275–8. |
5 | Nathan DM , Kuenen J , Borg R , Zheng H , Schoenfeld D , Heine RJ . Translating the A1C assay into estimated average glucose values. Diabetes Care. (2008) ;31: :1473–8. |
6 | Ogawa A , Hayashi A , Kishihara E , Yoshino S , Takeuchi A , Shichiri M . New Indices for Predicting Glycaemic Variability. PLoS ONE. (2012) ;7: (9):e46517. |
7 | Kilpatrick ES , Riqby AS , Goode K and Atkin SL . Relating mean blood glucose and glucose variability to the risk of multiple episodes of hypoglycaemia in type 1 diabetes. Diabetologia. (2007) ;50: (12):2553–61. |
8 | Ceriello A , Esposito K , Piconi L , Ihnat MA , Thorpe JE , Testa R , Boemi M , Giugliano D . Oscillating Glucose Is More Deleterious to Endothelial Function and Oxidative Stress Than Mean Glucose in Normal and Type 2 Diabetic Patients. Diabetes. (2008) ;57: :1349–54. |
9 | Ladyzynski P , Foltynski P , Bak MI , Sabalinska S , Krzymien J , Kawiak J . Validation of a hemoglobin A1c model in patients with type 1 and type 2 diabetes and its use to go beyond the averaged relationship of hemoglobin A1c and mean glucose level. Journal of Translational Medicine. (2014) ;12: :328–. |
10 | McCoy RG , Van Houten HK , Ziegenfuss JY , Shah ND , Wermers RA , Smith SA . Increased Mortality of Patients With Diabetes Reporting Severe Hypoglycemia. Diabetes Care. (2012) ;35: (9):1897–901. |
11 | Patterson CC , Dahlquist G , Harjutsalo V . Early mortality in EURODIAB population-based cohorts of type 1 diabetes diagnosed in childhood Diabetologia (2007) ;50: :2439–42. |
12 | Jacobson AM , Musen G , Ryan CM . Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research GrouLong-term effect of diabetes and its treatment on cognitive function. N Engl J Med. (2007) ;356: :1842–52. |
13 | Feltbower RG , Bodansky HJ , Patterson CC . Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes: Results from the Yorkshire Register of Diabetes in Children and Young Adults. Diabetes Care. (2008) ;31: :922–6. |
14 | Skrivarhaug T , Bangstad H-J , Stene LC , Sandvik L , Hanssen KF , Joner G . Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia. (2006) ;49: :298–305. |
Figures and Tables
Fig.1
Daily variation and mean of blood glucose during three months.