Does diagnosis matter? Evaluating impact of pediatric chronic pain diagnosis on pain and function
Abstract
PURPOSE:
This study aimed to A) evaluate changes in pain and function following an outpatient interdisciplinary pain management program (IPMP) for children with different chronic pain conditions and B) explore differences in pain and function at baseline and discharge for different diagnoses.
METHODS:
A retrospective chart review was performed for 488 children who participated in an outpatient IPMP. Children’s pain and physical, social, and emotional functioning were assessed at initial evaluation, discharge, and one-to-two-month follow-up. Patients were stratified by diagnosis (complex regional pain syndrome [CRPS], headache, musculoskeletal pain, visceral pain, and widespread pain) to evaluate differences in pain and functioning at baseline and discharge.
RESULTS:
Children’s pain and function improved from initial evaluation to discharge. Those with headache and musculoskeletal pain exhibited better baseline physical and emotional functioning than other diagnostic groups (p = 0.03; p = 0.005; p = 0.002; p = 0.04). Children with CRPS displayed the worst baseline physical functioning (p = 0.003). Those with widespread pain exhibited the worst baseline emotional functioning at both initial evaluation and discharge (p = 0.009; p = 0.007).
CONCLUSION:
Children with CRPS, visceral pain, and widespread pain undergoing treatment in an IPMP exhibited the most impaired baseline functioning, while those with musculoskeletal pain and headache were least impaired. All exhibited improvements in pain and function following the IPMP.
1Introduction
Chronic pain, defined as pain lasting more than three months, is a serious issue within the pediatric population and affects 4–88% of children [1]. Those conditions can lead to impaired health-related quality of life [2], including increased school absences, diminished social interactions with peers, and decreased academic performance [3–6]. Additionally, having chronic pain as a child may predispose the child to pain in adulthood [7].
Due to the multifactorial nature of chronic pain in children, the most effective treatment approaches address the physical, psychological, environmental, and social factors that are inherent in chronic pain. Multiple studies and systematic reviews have highlighted the positive impact that interdisciplinary pain management programs (IPMPs) have on the functioning of children with pain [8–12]. These programs have become the gold standard for chronic pain management by aiming to reduce fear of pain, teach pain coping techniques, and improve physical functioning, while addressing the emotional needs of both patients and parents [8].
While multiple studies have found the effectiveness of IPMPs, a world-wide call has been issued to continue to examine the impact of IPMPs on various patient populations [13]. As Drotar described, there is a need for additional studies to replicate findings and thus improve their generalizability to other populations of children with chronic pain [14]. Furthermore, few studies to date have examined if certain pediatric chronic pain diagnoses respond differently to IPMPs. Current literature suggests that children with abdominal pain may experience less robust improvements following an IPMP [8]. Additionally, children with complex regional pain syndrome (CRPS) have been found to be more physically impaired than children with other chronic pain diagnoses [15]. It is also known that patients with centralized pain conditions, in which the central nervous system becomes sensitized to the pain experience, thus leading to a lower pain threshold, tend to be more psychologically distressed [16]. However, the interplay between pain type and response to an outpatient IPMP has not been explored.
The purpose of this study was to a) enhance the current literature by showing the efficacy of an outpatient IPMP for children with a variety of different chronic pain conditions, utilizing International Association for the Study of Pain (IASP) diagnoses, including widespread pain (WP), headache (HA), visceral pain (VP), CRPS, and musculoskeletal pain (MSK); b) explore baseline similarities and differences in pain and function of children with different chronic pain diagnoses; and c) evaluate the treatment responses for different chronic pain types. Based on studies to date and clinical experience, it was hypothesized that there would be baseline functional differences between diagnostic groups, with children who had centralized pain conditions (VP, CRPS, and WP) exhibiting the lowest levels of functioning and highest levels of pain at baseline. It was also hypothesized that all children would improve following the IPMP, regardless of pain diagnosis, but those with centralized pain conditions would demonstrate less improvement than others.
2Methods
2.1Design and participants
This retrospective cohort study was conducted at an urban, academic outpatient pain management clinic, following approval from the local institutional review board (STUX00216547). Children (ages 8–18) who received treatment in the outpatient pediatric IPMP between January 2009 and March 2020 were included in the study. Based upon their presentation, patients were placed into one of five diagnostic chronic pain categories outlined by IASP [17]: WP, HA, VP, CRPS, and MSK. If a patient had multiple pain diagnoses, they were placed in the group consistent with their primary, worst complaint. Patients were excluded from the study if they were diagnosed with functional neurological symptom disorder, since the Bath Adolescent Pain Questionnaire (BAPQ) has not been validated for use in this patient population. Those with fibromyalgia were placed in the WP group, and those with amplified musculoskeletal pain syndrome were placed in the MSK group. This study was not preregistered, and there were no manipulations.
2.2Treatment protocol
The IPMP involved the following domains: physical therapy, occupational therapy, psychological counseling, relaxation training, group therapy, and medication management by a pediatric rehabilitation specialist. The program consisted of one or two half-day sessions (approximately three to four hours) per week for four to eight weeks. Physical therapy emphasized improvement of joint stability, proprioception, muscle strength, and overall cardiovascular fitness. Occupational therapy focused on postural biomechanics, the safe completion of functional daily tasks, pacing, and development of a daily schedule. Psychological interventions included cognitive behavioral strategies to self-manage pain and stress, including relaxation techniques and the use of coping self-statements to help in times of distress. Medication management was seldom used but often focused on correcting poor sleep latency and providing relief as needed for breakthrough pain that did not respond to the above non-pharmacologic interventions. Parents were asked to attend the initial session, during which the treatment team reviewed the concept of self-perpetuating cycles of pain and urged parents to avoid asking their child about pain and instead focus on function. Also, parents were asked to attend the discharge session and encouraged to attend as many sessions in between as able.
2.3Outcome measures
Patients were evaluated at three time points: 1) initial evaluation, 2) discharge from the IPMP, and 3) at one-to-two-month follow-up. At each time point, patients were evaluated by the Numeric Rating Scale (NRS) and the BAPQ.
The NRS is a validated and reliable measure of pain in the pediatric population [18]. Children were asked to rate their average pain using an 11-point NRS ranging from zero (no pain) to 10 (worst pain imaginable).
The BAPQ is a comprehensive, 61-item instrument that consists of four subscales designed to assess the impact of chronic pain in adolescents [19]. The subscales measure daily functioning (social and physical), emotional functioning (depression, general anxiety, and pain-related anxiety), family functioning, and developmental functioning. Items are answered using a five-point frequency scale (0 = Never to 4 = Always) for all subscales, with the exception of developmental functioning, which uses a five-point scale ranging from zero (Very Behind) to four (Very Ahead) in response to various developmental tasks. Higher scores represent more impaired functioning for all subscales. The BAPQ is a valid and reliable measure of the impact of chronic pain on adolescents [19, 20]. Prior research validates the use of the BAPQ in a United States-based population and supports its use as an effective measure of change in an interdisciplinary treatment program [21].
2.4Statistical analysis
The continuous variables were reported using mean and standard deviation, while categorical variables were reported using the count and percentage. The significance of any differences in the mean age between diagnostic groups was analyzed using one-way analysis of variance, and for gender, chi-square analysis was used. For the dependent variables, BAPQ was tested for normality assumptions. The Kolmogorov-Smirnov test for normality suggested that BAPQ subscale variables were not normally distributed. Thus, dependent variables were analyzed using non-parametric tests (Wilcoxon sign test and Kruskal-Wallis test). The correlation between the variables was tested using Spearman correlation test. The difference in pain intensity and BAPQ for different evaluation timepoints was performed using least square means estimates by general linear models. Subgroup testing for individual diagnostic groups for BAPQ was performed using general linear models. For this portion of the analysis, all patients were grouped together into an “overall” group. All the analyses were done at significance level of 0.05. Analyses were performed using SAS 9.4.
3Results
A total of 488 patients were included in this study (Table 1). There was data for 488 at evaluation, 479 at discharge, and 245 at follow-up. Pain diagnoses included CRPS (n = 49, 10.0%), HA (n = 86, 17.6%), MSK (n = 117, 24.0%), VP (n = 49, 10.0%), and WP (n = 164, 33.6%). Twenty-three (4.7%) were missing a diagnosis. The mean age across groups was 14.3±2.4 years with a range of eight to 18 years. There was a significant difference in age across diagnostic groups (p = 0.0047). The patient population had 364 females (74.6%) and 124 males (25.4%). No difference in sex distribution was found between groups (p = 0.06).
Table 1
Demographic information of study participants
| Demographic information | N (%) |
| Patient Sex | |
| Female | 364 (74.6%) |
| Male | 124 (25.4%) |
| Number of Children | |
| Initial | 488 |
| Discharge | 479 |
| Follow-up | 245 |
| Diagnosis | |
| CRPS | 49 (10.0%) |
| HA | 86 (17.6%) |
| MSK | 117 (24.0%) |
| VP | 49 (10.0%) |
| WP | 164 (33.6%) |
| No diagnosis identified | 23 (4.7%) |
| Child’s Age Mean | 14.3±2.4 years |
| Child’s Age Range | 8–18 years |
| Child’s Age by Diagnosis | |
| CRPS | 13.7±3.1 years |
| HA | 14.8±2.2 years |
| MSK | 14.3±2.5 years |
| VP | 14.0±2.4 years |
| WP | 14.3±2.4 years |
CRPS = complex regional pain syndrome; HA = headache; MSK = musculoskeletal pain; VP = visceral pain; WP = widespread pain.
3.1Response to IPMP: Trending pain and BAPQ scores over time
Table 2 displays the mean initial, discharge, and follow-up scores for pain and each domain of the BAPQ. There was a statistically significant decrease in pain from initial to discharge and from initial to follow-up, with p-values displayed in Table 2. Similarly, there was also a significant decrease in each domain of the BAPQ from initial to discharge and from initial to follow-up (p-values displayed in Table 2).
Table 2
Pain and BAPQ scores for children at initial, discharge, and follow-up
| Initial | Discharge | Follow-up | P-value for Δ | P-value for Δ | |
| n = 488 | n = 479 | n = 245 | from Initial to Discharge | from Initial to Follow-up | |
| Pain Score | 6.1±1.8 | 4.3±2.5 | 3.5±2.7 | <0.001 * | <0.001 * |
| BAPQ Daily | 27.9±11.6 | 19.0±8.9 | 17.1±8.6 | <0.001 * | <0.001 * |
| BAPQ Emotional | 37.2±14.5 | 26.8±12.5 | 24.17±12.1 | <0.001 * | <0.001 * |
| BAPQ Family | 17.3±7.6 | 14.9±7.9 | 14.0±7.8 | <0.001 * | <0.001 * |
| BAPQ Development | 20.3±7.2 | 17.1±7.1 | 16.4±7.4 | <0.001 * | <0.001 * |
Higher pain scores indicate worse pain. Higher BAPQ scores indicate worse functioning. There were statistically significant improvements in scores across all domains of the BAPQ. Asterisks indicate statistical significance. BAPQ = Bath Adolescent Pain Questionnaire.
3.2Analysis of pain and BAPQ scores by chronic pain diagnosis
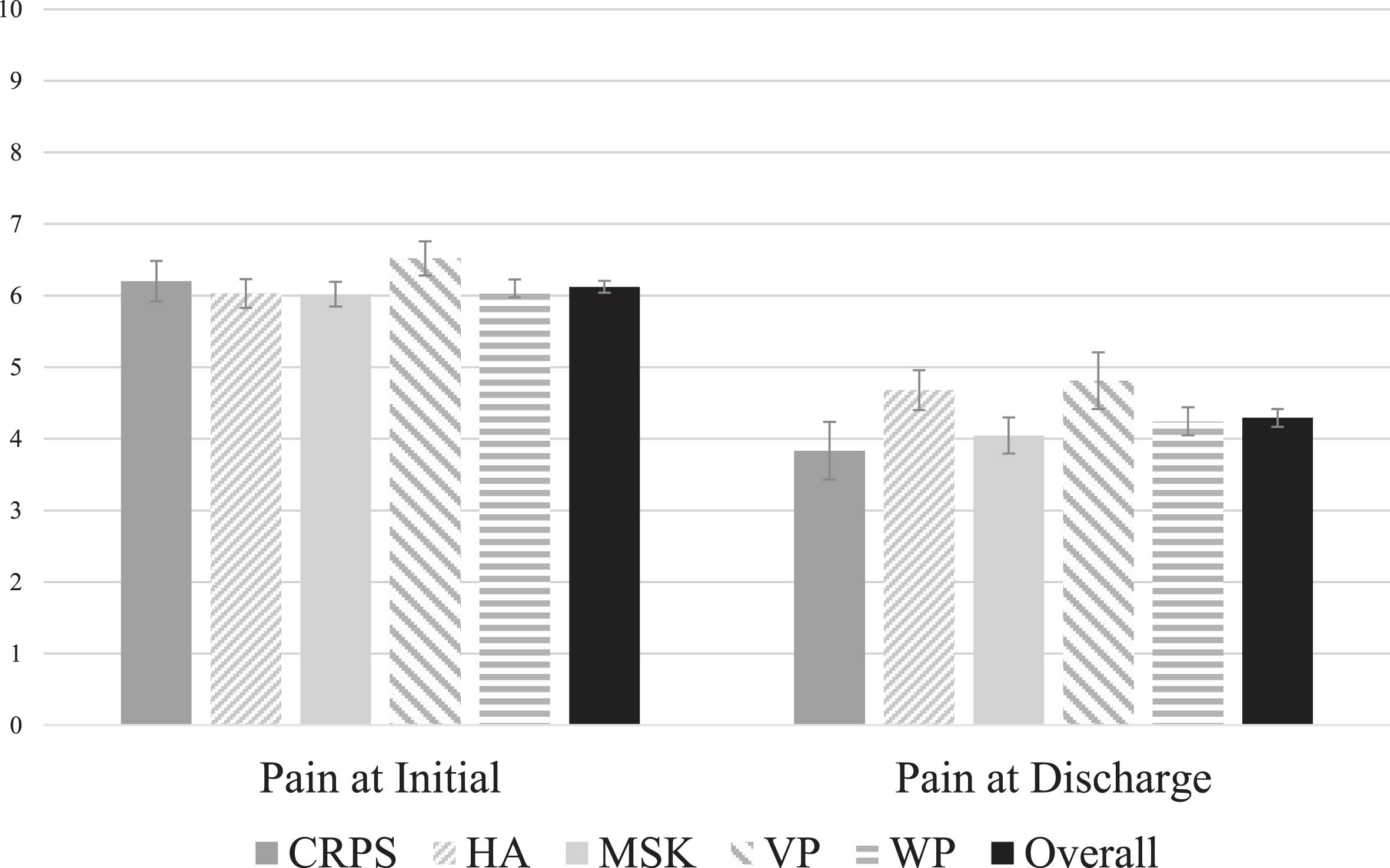
The average pain scores for each diagnosis at initial evaluation and discharge are displayed in Fig. 1. The average of the overall study population is graphed as a comparison. There were no differences detected when each diagnostic group was compared to the overall cohort, at both initial and discharge.
Fig. 1
Pain scores across chronic pain diagnoses, displayed at initial and discharge. There was a statistically significant decrease in pain scores for each group from initial to discharge. At both initial and discharge, there were no statistically significant differences when comparing each chronic pain diagnosis to the overall cohort. CRPS = complex regional pain syndrome; HA = headache; MSK = musculoskeletal pain; VP = visceral pain; WP = widespread pain.
Average BAPQ scores for each diagnostic group are displayed in Fig. 2. The average of the overall study population is graphed as a comparison. At the initial evaluation (Fig. 2a), patients with CRPS exhibited higher daily dysfunction scores, compared to overall (p = 0.003). Patients with HA showed lower daily and emotional dysfunction scores (p = 0.03; p = 0.005). Patients with MSK showed lower daily and emotional dysfunction scores (p = 0.02, p = 0.04). Patients with VP showed higher developmental dysfunction scores (p < 0.001). Those with WP showed higher emotional dysfunction scores (p = 0.009). For the remainder of the diagnoses and BAPQ subscales, there was no functional difference between the chronic pain diagnosis and the overall study population.
Fig. 2
A) Average baseline BAPQ scores for each diagnosis as compared to the overall average of all patients. B) Average discharge BAPQ scores for each diagnosis as compared to the overall average of all patients. Higher scores indicate worse functioning. Error bars represent standard error of the mean. Asterisks indicate the average for that group is statistically significantly different from the overall average. Overall indicates all patients grouped together. CRPS = complex regional pain syndrome; HA = headache; MSK = musculoskeletal pain; VP = visceral pain; WP = widespread pain; BAPQ = Bath Adolescent Pain Questionnaire.
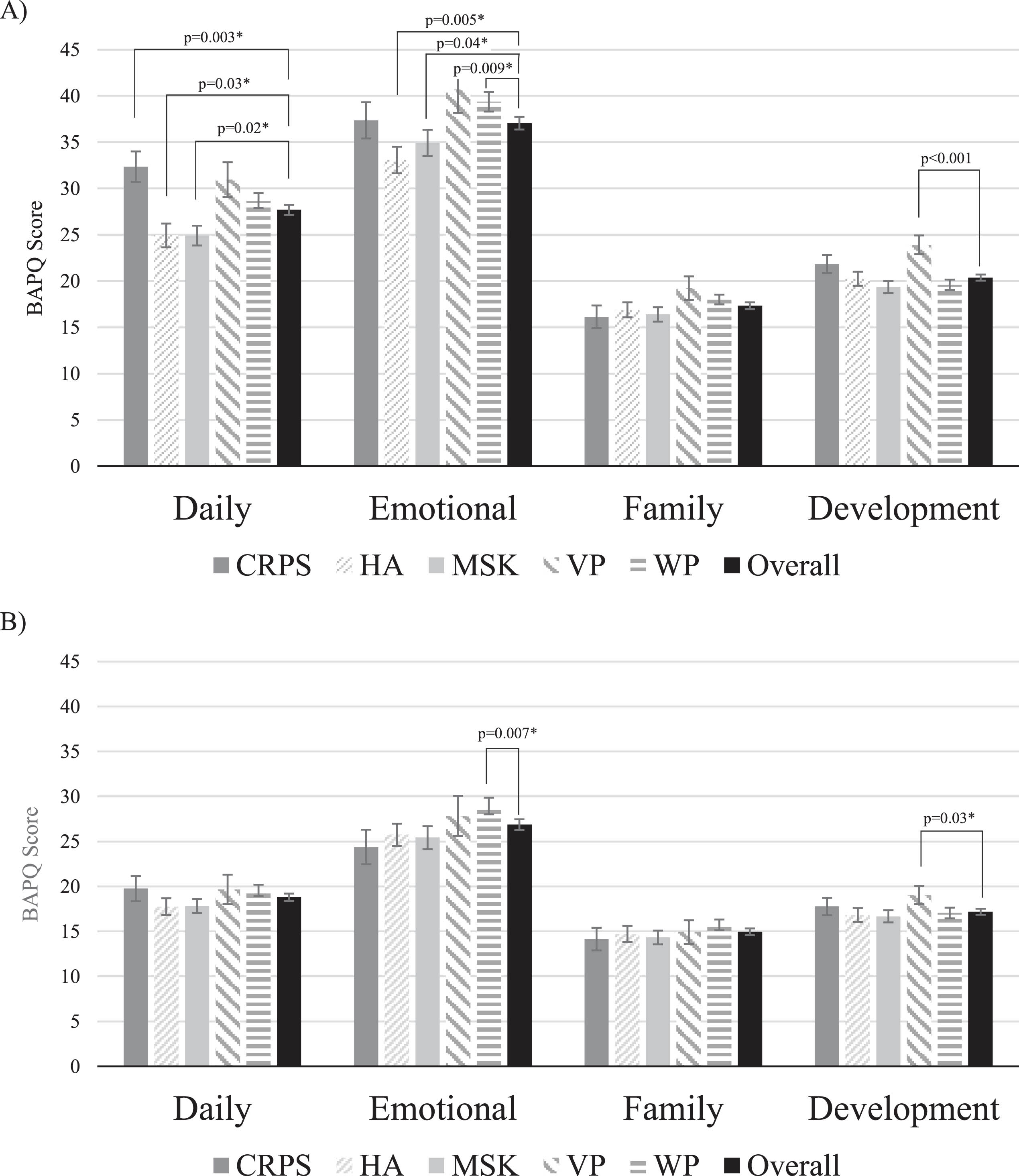
At discharge (Fig. 2b), patients with WP scored higher for the emotional dysfunction domain (p = 0.07). Patients with VP scored higher for development dysfunction (p = 0.004). For the remainder of the diagnoses and BAPQ subscales, there was no functional difference between the chronic pain diagnosis and the overall study population.
4Discussion
The current study provides an additional perspective on the interdisciplinary treatment of childhood chronic pain across multiple diagnoses in an outpatient setting. This is the only study to date that has examined children using the IASP chronic pain diagnoses to evaluate pain and function and did so using a large sample size. As hypothesized, groups of children with a variety of chronic pain disorders showed improvements in pain and functioning following an outpatient IPMP. Results of the present study agree with prior research that has demonstrated improvements in children following IPMPs [22–26]. The current study enhances prior research due to its large sample size in an urban, academic center.
The present study investigated if diagnosis affects baseline or discharge functioning for children during an IPMP. Notable differences were detected in baseline functioning. Although there was no one diagnosis in the present study that was clearly more or less impaired than the overall cohort for all domains of the BAPQ, certain themes can be drawn from the data. Children with HA and MSK were less physically and emotionally impaired at baseline. Those with CRPS were more physically impaired, which is in line with Logan et al., who found that those with CRPS are more physically impaired than children with other chronic pain diagnoses but have similar psychological functioning [15]. In the present study, patients with WP were more emotionally impaired. Findings from studies on fibromyalgia have cited the significant psychological distress associated with the condition [27]. Lastly, patients with VP exhibited lower levels of developmental functioning. It is possible that children with VP display additional symptoms beyond pain (constipation, diarrhea, bloating, menstrual irregularities, urinary disturbances) that limit them from developing normally alongside their peers. Taken together, the above findings support the hypothesis that patients with centralized pain conditions exhibit more psychological distress. This notion has been cited in the adult literature, with patients having chronic WP more than twice as likely to have depression symptoms than adults with chronic low back pain [16].
Bruce et al. also examined different chronic pain groups (abdominal pain, MSK, and HA) during an outpatient IPMP. In their cohort of children, they found that those with abdominal pain did not exhibit improvements in pain during the program, whereas those with MSK and HA did. Interestingly, children with HA and MSK showed continued improvements between discharge and three-month follow-up, whereas those with abdominal pain did not. Although it is difficult to compare the study by Bruce et al. with the present study due to different sample sizes, follow-up periods, and pain program specifics, it is notable that their study also highlighted similar themes for diagnostic groups. Many with VP suffer from functional abdominal pain, which has no clear organic cause. Additionally, it is also possible that due to differences in the nociceptive signaling and interpretation of somatic pain (comprising MSK and HA) and VP, their pain may also be experienced differently. Regardless, the findings from the present study highlight that children with VP or WP may require more targeted psychological and behavioral interventions than children with other chronic pain diagnoses that typically display less centralization, such as HA or MSK. The results of the present data can help guide practitioners who may practice in areas where psychological resources are scarce. When access to psychological resources or the ability to perform a psychological assessment is limited, the findings of this study provide crucial insight into the allocation of resources, which should include funneling these resources towards those with centralized pain conditions.
Interestingly many of the differences detected between diagnoses at baseline were no longer evident by discharge. This finding proves that the present outpatient IPMP can be effective for children with a wide variety of chronic pain diagnoses. Notably, however, children with WP continued to exhibit more impaired emotional functioning than their other chronic pain peers. Overall, there were improvements in all groups from start to finish of the program. Since there were fewer differences between groups at discharge compared to baseline, it can be inferred that the groups who were more impaired at baseline displayed a larger improvement over the course of the program. For example, groups of patients with CRPS started more impaired and displayed a larger improvement in physical functioning than those with HA and MSK, resulting in all three of those groups having similar physical functioning at completion of the program. Similarly, those with HA and MSK started less impaired emotionally compared to the other groups and therefore displayed less of an improvement over the course of the program. In knowing which groups make more progress over the course of an IPMP, these findings can again help guide practitioners in rural areas where IPMPs are not available. Providers can therefore have educated discussions with patients and families about the type of improvement that is typically seen for different chronic pain types during an IPMP. When taking into consideration the extensive travel, time, and energy that may be required to attend an IPMP, families will value knowing the type of improvement that is seen emotionally and physically for each chronic pain type.
The results of this study will provide crucial insight for pediatric chronic pain providers. Knowing that certain pain diagnoses may be more impaired at baseline can guide practitioners and aid with setting expectations for families regarding duration of treatment program or the amount of psychological intervention that may be necessary to optimize improvements. Future studies with longer term outcomes would be beneficial to determine if improvements for all diagnoses are sustained years after completion of the program. Additionally, future research should examine the role of parents and how interactions with their children may affect those with certain diagnoses. Lastly, because the BAPQ does not divide the emotional functioning domain into the different aspects of emotion, future research should examine if there are certain aspects of emotional functioning that are more impaired in certain groups of children.
5Limitations
This study had a few notable limitations. Retrospective chart reviews are inherently limited due to incomplete or limited documentation because the patient charts were not originally designed to collect data for research. Additionally, information regarding social determinants of health was not collected, including socioeconomic status, race, or ethnicity, nor was there an examination of adverse childhood events. Also, the involvement of parents, which may impact a child’s pain experience and recovery, or the length or frequency of treatment time in correlation to outcomes was not quantified. Understanding the impact of this variable could increase treatment efficiency. Furthermore, whether duration of pain at baseline impacts changes in function was not evaluated. Duration of pain has been shown to be associated with more severe disability in adults with chronic pain [28]. Although the majority of the patients had experienced pain for years prior to starting the IPMP, there is always a chance the improvement is solely due to the passage of time (i.e., regression to the mean). Additionally, the statistical analysis grouped patients together by diagnosis but did not examine the individual changes each patient experienced. There is definitely a role for future research that more closely examines each individual improvement. Lastly, the follow-up for this study was one to two months following completion of the IPMP, and many patients did not return for the one-to-two-month follow-up appointment. It is unknown if the children who exhibited more robust improvements did not return for follow-up, or if children who did not experience as many improvements were lost to follow-up. Longer term and more complete follow-up for patients could elucidate if certain diagnoses are more likely to exhibit sustained improvements. Additionally, many patients were lost to follow-up at the one-to-two-month follow-up appointment, which may have affected results.
6Conclusions
Overall, the functioning of children with many different chronic pain diagnoses improved over the course of an outpatient IPMP. Children with HA and MSK were less physically and emotionally impaired at baseline and those with CRPS, VP, and WP exhibited the most impaired baseline functioning. At discharge, children with WP continued to exhibit more impaired emotional functioning, but the majority of the remaining differences were not detectable by discharge between pain groups. Knowing baseline differences and improvements for different chronic pain types during an IPMP, these findings can help guide providers in resource-limited areas with management approach.
Acknowledgments
None.
Conflicts of interest
The authors have no financial interests to disclose.
References
[1] | King S , Chambers CT , Huguet A , et al. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain. (2011) ;152: (12):2729–38. doi: 10.1016/j.pain.2011.07.016 |
[2] | Petersen S , Hagglof BL , Bergstrom EI . Impaired health-related quality of life in children with recurrent pain. Pediatrics. (2009) ;124: (4):e759–67. doi: 10.1542/peds.2008-1546 |
[3] | Agoston AM , Gray LS , Logan DE . Pain in school: Patterns of pain-related school impairment among adolescents with primary pain conditions, juvenile idiopathic arthritis pain, and pain-free peers. Children (Basel). (2016) ;3: (4):39. doi: 10.3390/children3040039. |
[4] | Caes L , Fisher E , Clinch J , Tobias JH , Eccleston C . The role of pain-related anxiety in adolescents’ disability and social impairment: ALSPAC data. Eur J Pain. (2015) ;19: (6):842–51. doi: 10.1002/ej611 |
[5] | Logan DE , Simons LE , Stein MJ , Chastain L . School impairment in adolescents with chronic pain. J Pain. (2008) ;9: (5):407–16. doi: 10.1016/j.jpain.2007.12.003 |
[6] | Eccleston C , Wastell S , Crombez G , Jordan A . Adolescent social development and chronic pain. Eur J Pain. (2008) ;12: (6):765–74. doi: 10.1016/j.ejpain.2007.11.002 |
[7] | Walker LS , Dengler-Crish CM , Rippel S , Bruehl S . Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain. (2010) ;150: (3):568–72. doi: 10.1016/j.pain.2010.06.018 |
[8] | Bruce BK , Ale CM , Harrison TE , et al. Getting back to living: Further evidence for the efficacy of an interdisciplinary pediatric pain treatment program. Clin J Pain. (2017) ;33: (6):535–42. doi: 10.1097/AJP.0000000000000433 |
[9] | Hechler T , Kanstrup M , Holley AL , et al. Systematic review on intensive interdisciplinary pain treatment of children with chronic pain. Pediatrics. (2015) ;136: (1):115–27. doi: 10.1542/peds.2014-3319 |
[10] | Simons LE , Sieberg CB , Conroy C , et al. Children with chronic pain: Response trajectories after intensive pain rehabilitation treatment. J Pain. (2018) ;19: (2):207–18. doi: 10.1016/j.jpain.2017.10.005 |
[11] | Stahlschmidt L , Zernikow B , Wager J . Specialized rehabilitation programs for children and adolescents with severe disabling chronic pain: Indications, treatment and outcomes. Children (Basel). (2016) ;3: (4):33. doi: 10.3390/children3040033 |
[12] | Benore E , Webster EE , Wang L , Banez G . Longitudinal analysis of patient-reported outcomes from an interdisciplinary pediatric pain rehabilitation program for children with chronic migraine and headache. Headache. (2018) ;58: (10):1556–67. doi: 10.1111/head.13389 |
[13] | Hechler T , Ruhe AK , Schmidt P , et al. Inpatient-based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: Randomized controlled trial of efficacy and economic effects. Pain. (2014) ;155: (1):118–28. doi: 10.1016/j.pain.2013.09.015 |
[14] | Drotar D . Editorial: A call for replications of research in pediatric psychology and guidance for authors. J Pediatr Psychol. (2010) ;35: (8):801–5. doi: 10.1093/jpepsy/jsq049 |
[15] | Logan DE , Williams SE , Carullo VP , Claar RL , Bruehl S , Berde CB . Children and adolescents with complex regional pain syndrome: More psychologically distressed than other children in pain?. Pain Res Manag. (2013) ;18: (2):87–93. doi: 10.1155/2013/964352 |
[16] | Dickson C , Zhou A , MacIntyre E , Hypponen E . Do chronic low back pain and chronic widespread pain differ in their association with depression symptoms in the 1958 British Cohort?. Pain Med. (2023) ;24: (6):644–51. doi: 10.1093/pm/pnac170 |
[17] | Treede RD , Rief W , Barke A , et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. (2019) ;160: (1):19–27. doi: 10.1097/j.pain.0000000000001384. |
[18] | Banez GA , Frazier TW , Wojtowicz AA , Buchannan K , Henry DE , Benore E . Chronic pain in children and adolescents: 24-42 month outcomes of an inpatient/day hospital interdisciplinary pain rehabilitation program. J Pediatr Rehabil Med. (2014) ;7: (3):197–206. doi: 10.3233/PRM-140289 |
[19] | Eccleston C , Jordan A , McCracken LM , Sleed M , Connell H , Clinch J . The Bath Adolescent Pain Questionnaire (BAPQ): Development and preliminary psychometric evaluation of an instrument to assess the impact of chronic pain on adolescents. Pain. (2005) ;118: (1-2):263–70. doi: 10.1016/j.pain.2005.08.025 |
[20] | Eccleston C , McCracken LM , Jordan A , Sleed M . Development and preliminary psychometric evaluation of the parent report version of the Bath Adolescent Pain Questionnaire (BAPQ-P): A multidimensional parent report instrument to assess the impact of chronic pain on adolescents. Pain. (2007) ;131: (1-2):48–56. doi: 10.1016/j.pain.2006.12.010 |
[21] | Revivo G , Amstutz DK , Gagnon CM , McCormick ZL . Interdisciplinary pain management improves pain and function in pediatric patients with chronic pain associated with joint hypermobility syndrome. PM R. (2019) ;11: (2):150–7. doi: 10.1016/j.pmrj.2018.06.018 |
[22] | Eccleston C , Malleson PN , Clinch J , Connell H , Sourbut C . Chronic pain in adolescents: Evaluation of a programme of interdisciplinary cognitive behaviour therapy. Arch Dis Child. (2003) ;88: (10):881–5. doi: 10.1136/adc.88.10.881 |
[23] | Lynch-Jordan AM , Sil S , Peugh J , Cunningham N , Kashikar-Zuck S , Goldschneider KR . Differential changes in functional disability and pain intensity over the course of psychological treatment for children with chronic pain. Pain. (2014) ;155: (10):1955–61. doi: 10.1016/j.pain.2014.06.008 |
[24] | Harbeck-Weber C , Sim L , Morrow AS , Murad MH . What about parents? A systematic review of paediatric intensive interdisciplinary pain treatment on parent outcomes. Eur J Pain. (2022) ;26: (7):1424–36. doi: 10.1002/ej1986 |
[25] | Palermo TM , Law EF , Bromberg M , Fales J , Eccleston C , Wilson AC . Problem-solving skills training for parents of children with chronic pain: A pilot randomized controlled trial. Pain. (2016) ;157: (6):1213–23. doi: 10.1097/j.pain.0000000000000508 |
[26] | Wiertz C , Goossens M , Spek EM , Verbunt JA . A cognitive-behavioral program for parents of children with chronic musculoskeletal pain; A feasibility study. Eur J Pain. (2017) ;21: (9):1571–81. doi: 10.1002/ej1058 |
[27] | Ghiggia A , Bottiroli S , Lingiardi V , Tassorelli C , Galli F , Castelli L . Alexithymia and psychological distress in fibromyalgia and chronic migraine: A cross-sectional study. J Psychosom Res. (2022) ;163: :111048. doi: 10.1016/j.jpsychores.2022.111048 |
[28] | Peters ML , Sorbi MJ , Kruise DA , Kerssens JJ , Verhaak PF , Bensing JM . Electronic diary assessment of pain, disability and psychological adaptation in patients differing in duration of pain. Pain. (2000) ;84: (2-3):181–92. doi: 10.1016/s0304-3959(99)00206-7 |




