“Virtual reality fixed me”: A case report of the use of virtual reality during intensive interdisciplinary pain treatment
Abstract
Virtual reality (VR) is an innovative technology with the potential to enhance treatment for children with chronic pain and functional symptoms. Currently, little is known about patients’ experiences of VR in the setting of intensive interdisciplinary pain treatment (IIPT). This study aimed to better understand how patients engage with and benefit from VR. This case report focuses on a 12-year-old female with amplified musculoskeletal pain syndrome and comorbid functional neurological disorder receiving treatment in inpatient IIPT. VR was incorporated into physical/occupational and recreational therapy sessions. A semi-structured interview was completed one-month post-discharge. Qualitative analysis revealed three major themes: Process of Change (VR was unique/immersive, reduced pain focus, challenged skepticism, and changed pain perception), Efficacy (VR increased movement, supported transitioning from a wheelchair to walking independently, and increased confidence, excitement, and surprise), and Engagement (VR aided in acknowledging progress, increased camaraderie, was fun, and challenged patient to extend treatment goals made in VR to real life). Therapist observations of the benefits and barriers to using VR in treatment are described. Overall, this report indicates that VR may be a helpful tool to use with existing IIPT interventions to enhance patient engagement in treatment and improve functionaloutcomes.
1Introduction
Adequate management of pediatric pain remains highly challenging, poorly understood, and significantly undertreated [1]. Inadequate management of pain is associated with poor quality of life, economic burden, and a high risk of persistent pain and opioid misuse in adulthood [2–4]. Additionally, a growing number of pediatric patients with chronic pain have comorbid functional neurological disorder (FND)1, further complicating treatment and leading to poor outcomes [5].
The treatment of pediatric chronic pain has evolved significantly over the last 30 years, shifting from a focus on pharmacologic to non-pharmacologic and non-opioid therapy as first-line treatments [4, 6]. Similarly, the understanding of FND has shifted from being regarded as a diagnosis of exclusion without many treatment options to a diagnosis with positive symptoms and emerging behavioral treatments [7]. In particular, the last several years have seen an emergence in the use of non-pharmacologic digital health tools, particularly in managing chronic pain and functional symptoms [8, 9].
Virtual reality (VR) is one such technology that has the potential to enhance management of pediatric pain and functional symptoms [8–10]. VR provides an immersive, multisensory, three-dimensional environment that allows participants to have a modified experience of reality by creating a sense of “presence” in which the patient feels that they are physically in the virtual world [11]. Research has found VR modulates pain-signaling through distraction, helping patients to shift focus and build skills while enhancing their sense of control [12]. Mechanistically, VR is thought to compete with pain signaling pathways and aid in reorganizing neural networks, resulting in improved functioning [13, 14]. However, a full understanding of the mechanism for the efficacy of VR is not yet completely elucidated. Nevertheless, the use of VR in pediatric patients with chronic pain and functional symptoms may be particularly beneficial, as children and adolescents typically have experience using this technology and are open to participating in engaging and imaginative experiences [15].
While VR is an innovative technology with the potential to enhance treatment for pediatric patients with chronic pain and functional symptoms, little is known about patients’ actual experiences using VR in intensive interdisciplinary pain treatment (IIPT). These programs aim to normalize patients’ activity to premorbid levels of function while increasing self-management through coordinated and concurrent treatment from specialists in pain and rehabilitation medicine, behavioral psychology, and physical therapy (PT), recreational therapy (RT), and occupational therapy (OT). IIPT programs treat patients with the highest levels of pain and disability who have failed treatment at other levels of care (e.g., inpatient, outpatient); innovative and engaging treatment tools are especially needed to restore function for those with such severe impairment. The current study utilized qualitative analysis of a case report to identify themes related to the experience of using VR as a first step to better understand how pediatric patients can engage with and benefit from VR during IIPT.
2Methods
2.1Patient description
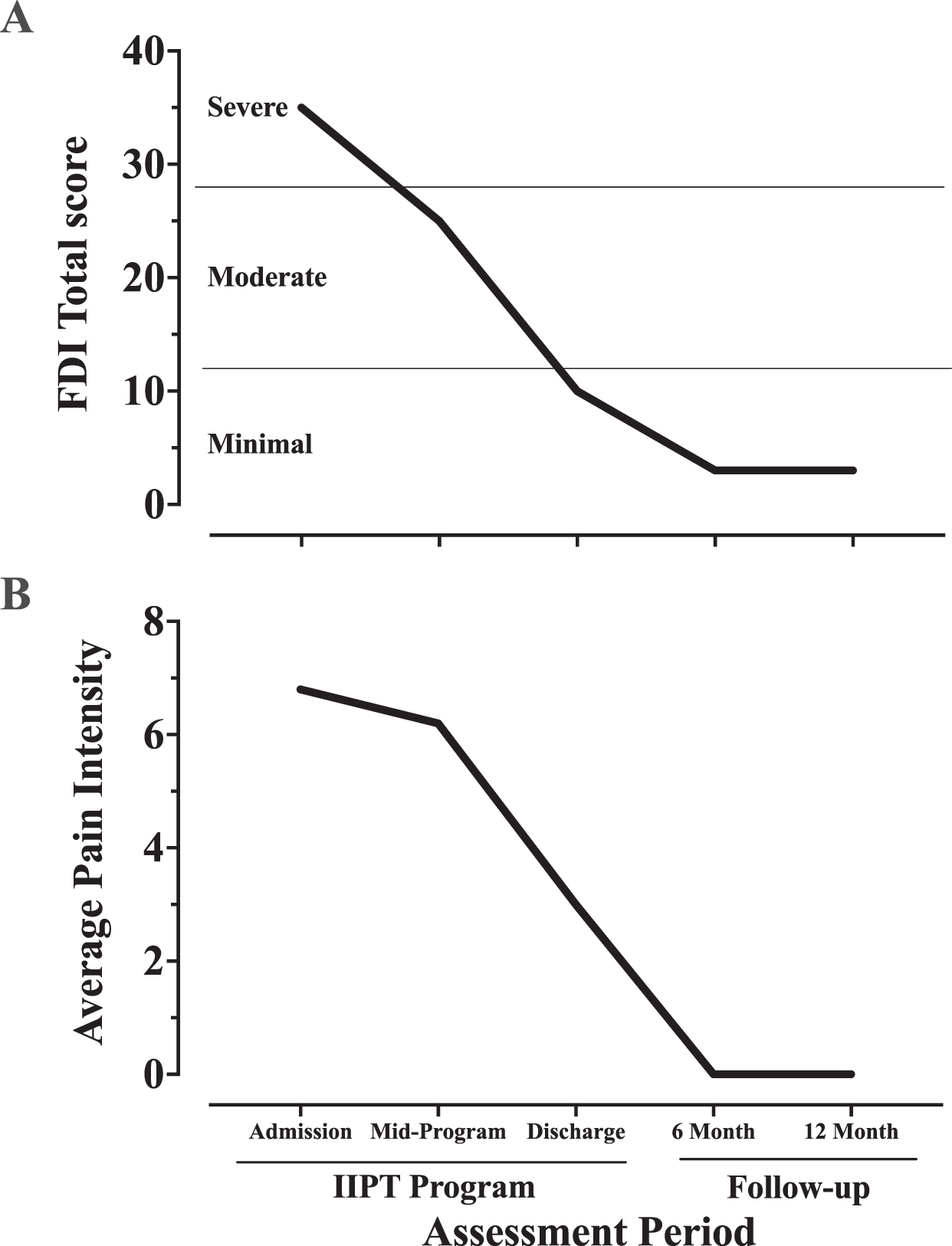
A 12-year-old female with a long history of amplified musculoskeletal pain syndrome and comorbid FND presented with pain in her left shoulder, elbow, wrist, and right knee. The pain began when she was five years old and was exacerbated by a shoulder and knee injury in the past year, resulting in increased pain as well as functional limb paralysis and weakness. As a result, she became functionally debilitated and required a wheelchair for mobility. She described her pain as constant and made worse by even the slightest movement of her extremities. Her pain and disability were in the severe range (e.g., ratings of average pain of 6.8 on a 0–10 visual analog scale; ratings of >30 on the Functional Disability Inventory [FDI] indicating severe disability; Fig. 1A and 1B), impacting functional ability, activities of daily living, school attendance, physical functioning, social interaction, and emotional adaptation. Physical and occupational therapists observed impairments in the following areas: mobility, strength, balance, range of motion, gross motor skills, fine motor coordination, activity demand tolerance, gait deviation, abnormal positioning, stair negotiation, and activity tolerance. Her pain (average intensity of 3 out of 10; Fig. 1A) and disability (FDI score of 10; Fig. 1B) demonstrated significant reductions at discharge and two follow-up periods (six and 12 months).
Fig. 1
Reporting of (A) disability on the Functional Disability Inventory (FDI) and (B) average pain intensity during and following inpatient intensive interdisciplinary pain treatment.
2.2Setting
The patient was admitted to an inpatient IIPT program for six weeks [16]. Briefly, she received three hours of individual OT and PT daily and two hours of group-based RT weekly among other program treatments (see Williams et al. [15] for a detailed program description and outcomes).
2.3Integration of VR into clinical care
VR was incorporated into OT/PT once a week during a 45-minunte individual session and once a week during a one-hour group session in RT, for a total of five PT/OT sessions and five RT sessions. Off-the-shelf games, including Tilt Brush (Google), Beat Saber (Beat Games), and Fruit Ninja (Halfbrick Studios), were delivered by an HTC Vive Pro HMD. The use of VR was tailored to the goals of the individual therapy sessions.
OT: VR was used to help the patient achieve OT-related goals, including activity tolerance/functional endurance, grip strengthening, active reaching and range of motion, dynamic balance, activity in stance, functional mobility, and desensitization. Specific games used to work toward those goals included Tilt Brush (reaching, grip, coping, changing positions), Beat Saber (coordination, mobility, balance, speed), and Fruit Ninja (standing, endurance, coordination).
PT: VR was used as an enhancement to traditional PT treatment options, both as an incentive and for skill building. Specifically, VR games provided a highly engaging distraction during bilateral lower extremity weight bearing in stance/sitting or range of motion activities. Functional positions and movements were practiced in the unique VR environments to improve acceptance of these in everyday life. The patient also enjoyed playing VR games as a reward after accomplishing specific goals as a fun/enjoyable treatment option.
RT: The patient used VR during a therapist-facilitated one-hour group session with one to two other IIPT program patients. While one patient used the VR headset, the others watched their performance on the screen. Patients either worked on a collaborative art project (Tilt Brush) that engaged them physically and creatively or competed against each other in games (Beat Saber, Fruit Ninja).
2.4Data collection and analysis
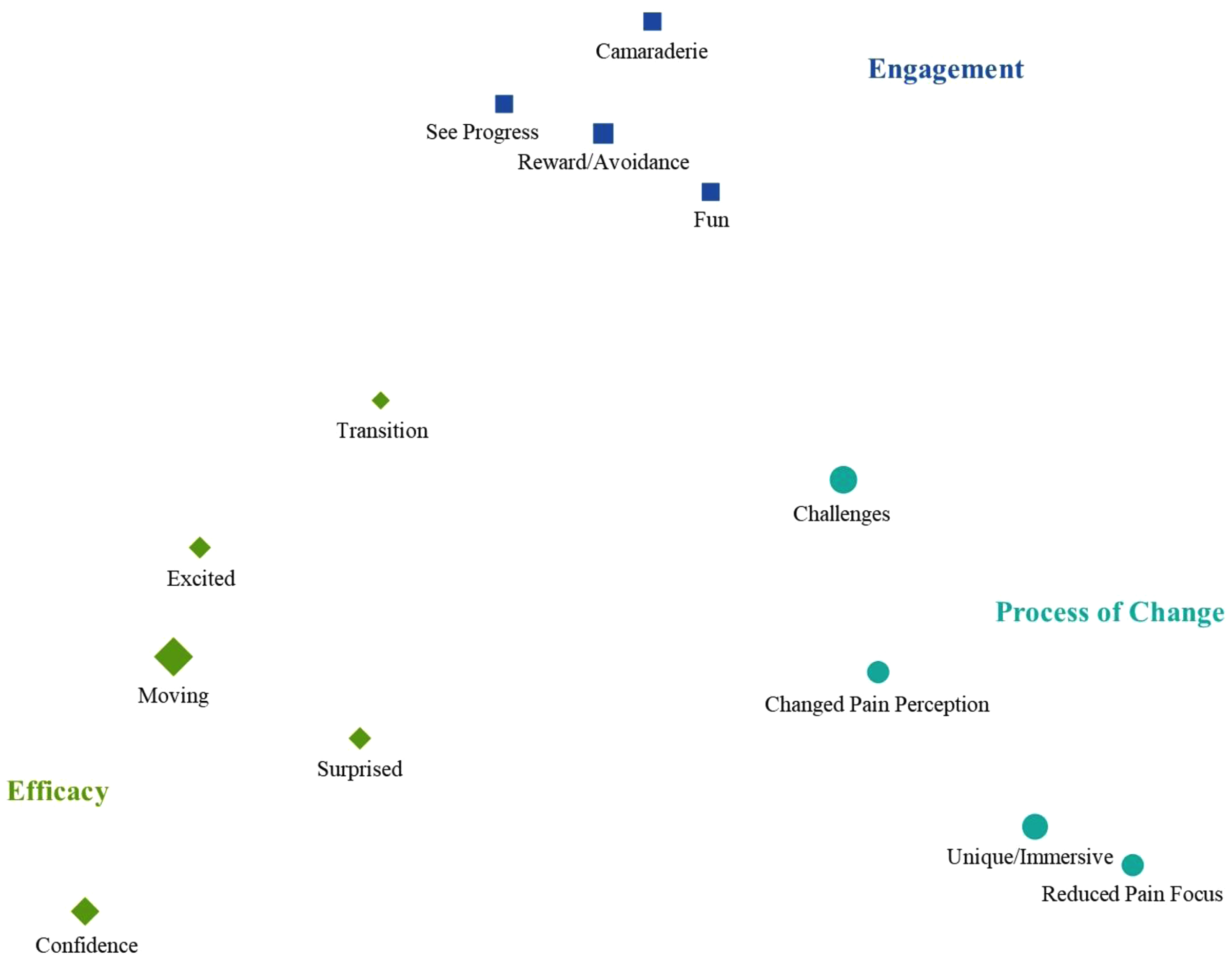
A doctoral-level psychologist (KLK), who was not involved in the patient’s care, completed a semi-structured interview around a series of prompts with the patient one month after discharge from the program; this was the only time point when she was interviewed about her VR experience (see Table 1). The interview was transcribed and checked against the audio recording for accuracy. The transcript of the interview was coded to identify themes related to the patient’s experience with VR. Two doctoral psychologists (SLC, KJH) separately coded the interview and then met to discuss discrepancies, identify code labels, and collapse codes as warranted. In total, 144 patient sentences/phrases were coded into 14 categories. Code mapping using multidimensional scaling was conducted with MAXQDA 2022 (VERBI Software, 2021) to identify overarching themes based on how the codes clustered (Fig. 2). Occupational, physical, and recreational therapists (NDS, ETD, KS) also provided their observations of the clinical benefits and potential barriers to using VR in their respective treatment. This study was approved by the Institutional Review Board; the patient provided verbal assent, and her parents provided written informed consent.
Table 1
Interview prompts for VR case study in IIPT
| Tell me a little bit about your experience with virtual reality (VR) when you were in the FIRST Program. What did you like or not like about it? |
| Is VR different or the same as other techniques you have used in therapies prior to coming to FIRST? If same/different, how so? |
| How was VR integrated into your therapy sessions? |
| Was VR used to help you achieve any goals you may have set in the FIRST Program? |
| Did you do your VR sessions individually or in a group setting? |
| What did you like about doing it individually versus with a group? What did you not like? What did you like about doing it in a group versus individually? What did you not like? |
| How was VR different than other things (treatments/activities) you did in OT/PT/Rec Therapy? |
| Did you prefer VR over other activities? Why or why not? |
| Did any of your therapists use VR as a motivator/reward? |
| How do you think your body responded to VR? What about your mind? Were you surprised about how your body/mind responded to VR? |
| Did VR help you do things physically that you were not able to do before coming to the FIRST Program? [If yes] What do you think was different about VR that made this change possible? |
| Did VR change the way you feel about yourself or your physical abilities? |
| Did VR help reduce any potential feelings of fear or anxiety associated with movement/pain? [If yes] How so? |
| Is there anything else you would like to share about your experience with VR that I didn’t ask about already? |
VR: virtual reality; IIPT: intensive interdisciplinary pain treatment; OT: occupational therapy; PT: physical therapy; Rec: recreational.
Fig. 2
Code mapping using multidimensional scaling was conducted with MAXQDA 2022 (VERBI Software, 2021) to identify overarching themes based on how the codes clustered.
3Results
3.1Patient’s experience
Three overarching themes were identified: Process of Change, Efficacy, and Engagement, along with the stand-alone code Safe.
Process of Change included four codes. Unique/Immersive captured the patient’s experience of engaging in VR. Reduced Pain Focus included descriptions of being distracted and highly engaged. Challenges captured the patient’s report of being skeptical of VR and feeling like the coping strategies she tried in the past “didn’t work” for her as well as VR worked during IIPT. Changed Pain Perception included statements about how thinking about pain changed during VR. Taken together, these codes capture the presumed mechanism of change for the patient –an immersive experience that helped to redirect attention away from pain and ultimately led to changed pain perception with an increase in functioning, including her unique challenges along the way.
Efficacy included five codes. Moving was the largest code category and focused on the patient’s report of beginning to move, increasing her movement, and meeting program and personal goals. The Transition code captured her progress in movement, increasingly requiring fewer supports and walking independently. The codes of Confidence, Surprised, and Excited, captured the patient’s experience of being surprised by the VR experience and that it “worked,” along with her increased feelings of confidence and success associated with thisexcitement.
Finally, Engagement included four codes: See Progress, Camaraderie, Fun, and Reward/Avoidance. The first three code titles are self-explanatory and included the patient’s ability to see progress throughout VR activities, social interaction with other patients, and enjoyment of VR, respectively. The Reward/Avoidance code captured the patient’s dilemma with the fact that, while VR helped her to walk for the first time in a year, it now meant that she would be expected to walk in settings outside of VR as well.
The code Safe did not share relationships with any other codes. It captured that the patient felt safe taking risks during VR sessions and was supported by the intervention team.
A summary of codes and themes with representative quotes is presented in Table 2. The visual spacing of the codes is presented in Fig. 2. Overall, the patient described the VR intervention as a very positive, helpful tool that facilitated her recovery from a high level of impairment to complete functional restoration over the course of her IIPT program. As she noted at the end of the interview: “If I do ever end up having to go back to the FIRST program, I’m gonna be like ‘VR right now’ it fixed me the last time…I feel like it’s a really good and valuable tool.”
Table 2
Themes, codes, and representative quotes from the qualitative analysis
| Theme | Code | Representative Quotes |
| Process of Change | Unique/immersive | “Definitely different in a good way, uh, because I’ve struggled with coping techniques a lot in the past, and feeling like they don’t work for me…but VR is kinda its…own section of coping techniques.” |
| “It’s not just distraction it’s like…your mind and body are fully immersed in this experience…it’s more of an experience that you’re a part of…you’re using your full body.” | ||
| “It’s a good way to get you to move without you realizing that you’re actually moving.” | ||
| “There’s just lots of different variables…and I’ve never really done anything like that before.” | ||
| Reduced pain focus | “It was something that I could do easily and not…focus on the pain as much.” | |
| “Once I started doing it you kinda just forget about everything that’s actually going on outside of the VR helmet.” | ||
| “Fully immersed in something…then you’re not even really thinking about [pain].” | ||
| Changed pain perception | “It was less painful…it’s a confusing statement that it’s less painful because it was still very painful, but it was way less than what it would be when I wasn’t doing it in VR.” | |
| “[Being] fully immersed in something because then you’re not even really thinking about pain.” | ||
| “I think I responded well to it…I wasn’t incredibly sore or super painful afterwards…outside of VR then normally I would be really sore and painful for a while afterwards.” | ||
| Challenges | “Just like in the beginning, it was hard to even think about why VR would be helpful.” | |
| “I thought ‘don’t tell me about my progress, cause if you tell me, I’m gonna become more hesitant to do anything.”’ | ||
| “I’m also stubborn so I was like ‘you can’t prove it unless you’re recording it.”’ | ||
| Efficacy | Moving/meeting goals | “The first time that I fully extended my left shoulder that I injured two years ago and haven’t moved…I did that in VR.” |
| “A lot of movement goals like cause I haven’t been moving. [I] haven’t been using my right knee very much at all or my left shoulder or left elbow or right hand…I moved pretty much all of those in like the second or third VR session.” | ||
| “I get in my own head a lot…I would get so caught up in thinking about [moving] that I wouldn’t actually do it. You’re not even thinking about [moving]. You’re just like ‘oh well…I’m not doing this. It’s the floaty person in VR who’s doing it.”’ | ||
| “I walked in VR in OT…it was like one of the first times I walked without holding on to anything.” | ||
| “I was like fangirling over everything that I did. I’m like ‘oh my gosh I did this for the first time in VR and now I can like do this again.”’ | ||
| “I moved my left shoulder all the way for the first time in VR and now I get…[to] reach the top shelf of the pantry without [having] someone help me.” | ||
| Surprised | “I would fight, especially my OT a lot, about it cause I’m like ‘I did not walk’ she’s like ‘you literally just did it yesterday in VR…I watched you do it yesterday. I’m going to record you next time’ and I’m like ‘do it’ so she did and I’m like ‘what? Wait, I actually did that?’ I did it in VR but my body also did it outside of VR.” | |
| “The first time that I [walked] without holding on to anyone or anything. I didn’t hold anyone’s hand. I didn’t hold on to a walker. I didn’t use anything and I was really happy about that and got excited and…after I took the VR headset off, I’m like ‘wow I actually just did that.”’ | ||
| Gain Confidence | “It was easier to learn confidence.” | |
| “[VR] helped me kinda gain confidence in walking.” | ||
| “I feel like that was a big turning point to realize that I can do the same stuff in VR that I can [do] outside of VR.” | ||
| Efficacy | Excited | “The first time that I walked back and forth between two mat tables without anything…I asked them to record me so I could send it to people, and I sent a huge group chat with all of my family...It was really exciting and my phone didn’t even chime twice cause everybody texted back in the same minute.” |
| “I mean it was just in general amazing.” | ||
| Transitioning | “[VR] gave you a base of moving, and then you work on the little things, like the other things outside of VR.” | |
| “Then once I got a general base back of walking, then I could work on not turning my ankles in or not turning them out too far outside of VR.” | ||
| Engagement | Fun | “That was fun and it was a fun way to [get] me to be active and move.” |
| “Would choose VR most of the time because I really like VR.” | ||
| Reward/Avoidance | “If [OT or PT] was pretty boring then a lot of the times I would just be like ‘okay, well, let me just get through this then I’ll just be able to do VR.”’ | |
| “Oh, I get to do VR. Well, okay, let’s not have to do therapy for like an hour. I’ll take it.” | ||
| Comradery | “We would do competitions in the [VR] games…it was also a great way to bring us, other FIRST patients, together…a good way to not be forced together.” | |
| See Progress | “I also like having other people [in VR].” | |
| “It made it easier for me to realize accomplishments.” | ||
| Safe | Safe | “Doing it individually especially for the first time, I think was a good thing. It’s like you don’t feel like anyone’s like judging you.” |
| “Helpful to have people there to hold you accountable and be able to encourage you. And help you up and help you be able to reach your goals and not be on your own.” | ||
| “I feel like… the [VR] group felt like very safe space.” |
Note. Some unneeded “like” and “um” utterances were removed from the text for increased readability. VR: virtual reality; OT: occupational therapy/therapist; PT: physical therapy.
3.2Therapists’ observations
The RT, OT, and PT therapists agreed that incorporating VR facilitated significant functional improvements for this patient (see Table 3). Specifically, therapists noted that she progressed in active range of motion in bilateral upper extremities, stood for longer periods, initiated steps without walker support, improved grasp, and exhibited decreased pain behaviors more successfully during activities in VR compared to non-VR sessions. Table 4 presents a summary of the clinical lessons (challenges and solutions) learned from the therapy team regarding incorporating VR into treatment for this individual patient.
Table 3
Clinical observations regarding use of VR in rehabilitation
| Therapy Type | Observations Before and During Sessions with VR |
| Occupational Therapy (OT) | This patient had many OT-related challenges at admission. She could not grasp with her right hand or reach above heart level with her arms. Her functional impairments limited her ability to complete daily activities (e.g., self-care tasks, chores, leisure activities). |
| Without VR, she was hesitant to reach with her upper extremities and had significant pain behaviors. | |
| With VR, she reached fully overhead with no pain behaviors. She improved her grasp to hold the VR remote for 45 minutes. She improved her ability to stand each session without breaks; without VR, she initially stood for five minutes, but with VR, she stood for 15 minutes. She took her first independent steps in VR and eventually stood and walked independently for an entire session. | |
| Physical Therapy (PT) | This patient presented to the IIPT admission with severe, longstanding (greater than one year) functional impairments; she could not stand and demonstrated a very limited active range of motion of bilateral lower extremities. |
| Communicating about her performance in VR across therapies helped promote the translation of movement in non-VR sessions, which resulted in consistency of functional performance in all settings. | |
| Towards the end of her stay, although she was medically cleared to perform tasks like running and jumping, the patient was very anxious to perform these tasks in PT. However, while utilizing VR with RT, she engaged in multiple high-level balance/jumping activities without issue, which she could then carry over to PT. This performance and communication allowed us to address this barrier before discharge. | |
| Recreational Therapy (RT) | This patient identified many barriers to leisure participation upon program admission, including physical and functional limitations, decreased social/peer interaction, and loss of control over choosing activities. |
| VR sessions in RT were conducted in a group format. After the first VR session, she expressed increased self-esteem and felt proud of herself. She also moved her right arm for the first time with no pain behaviors and repeated the movement outside the headset with encouragement from the therapist and peers. | |
| She advanced each week, leading up to performing her preferred sport (basketball) for the first time in VR. She recognized the positive use of VR to achieve physical and psychosocial goals and advocated using VR in other sessions to facilitate similar changes. |
VR: virtual reality; IIPT: intensive interdisciplinary pain treatment.
Table 4
Lessons learned about challenges and solutions to incorporating VR into a pain rehabilitation treatment
| Lessons | Challenges | Solutions |
| Timing | It is important to consider the proper timing of when to introduce the VR intervention in terms of a patient’s willingness and readiness to try a new tool and, practically, finding the right time when it is appropriate and feasible to complete. Some patients may need to build up to doing some basic tasks without hands-on assistance before starting VR; others may need VR to achieve those goals. | Set individual goals and timelines for the introduction of VR with patients. |
| Grading | Playing VR games can be exciting for kids, but many tend to stop/give up if they are not successful or it feels too challenging right away. | Start with simple games and encourage breaks; work up to more complex activities with increased physical cues. Find the “just right” challenge level to build confidence and motivate participation. |
| Equipment | Set-up takes time, and equipment can be temperamental (e.g., charging, updates), taking away from clinical intervention time. VR requires appropriate gym space availability. | Have a regular time and space to use VR and utilize support staff to help the clinical staff members with set up. |
| Masks | Wearing masks (e.g., during COVID-19 restrictions) can make headsets fog up more frequently. | Taping the mask over the nose bridge has been helpful. |
| Comorbid Symptoms | Sometimes patients have dizziness, nausea, fatigue, or other somatic symptoms that interfere with participation in VR due the nature of a very immersive visual experience. | Pace the time in VR as needed; start with a small amount of time and work up. |
| Provide psychoeducation regarding autonomic symptoms and how the patient can use coping skills to focus on function in VR as they do in other settings. | ||
| Carryover | Carrying over gains made in VR to functional activities outside of VR can be challenging for patients. It can be frustrating for patients and therapists to make significant gains during VR and not have the same performance outside of VR. | Taking videos and pictures of patients performing tasks in VR can be helpful. Show those and discuss the gains observed and expectations for carryover with patients after VR sessions. |
VR: virtual reality.
4Discussion
This qualitative analysis of a case report demonstrated the positive benefits of incorporating VR into the treatment of a pediatric patient with chronic pain and comorbid FND, complementing previous studies using VR in pediatric pain patients [9, 10]. Specifically, three major themes were identified, including the unique impact of VR on the process of change to decrease attention to pain and improve function, how VR helped the treatment itself be more effective, and the high degree of engagement she experienced using VR. Similar themes were observed by Griffin and colleagues [9], who reported positive experiences (e.g., enjoyment), distraction from pain, decreases in pain, and increased function with VR by patients. Furthermore, patients reported not initially enjoying or believing that VR would be helpful (similar to Challenges in the theme Process of Change), but they were willing to give VR a try. In addition, therapists agreed that including VR was a successful and fun way to enhance traditional therapies and facilitate significant physical and psychosocial improvement for this patient. These responses were comparable to clinician interviews by Griffin and colleagues [9], suggesting that VR helped patients achieve their rehabilitation goals, reduced pain, and increased function while overcoming psychological barriers to rehabilitation.
Although VR appeared to play a strong role in assisting with this patient’s functional recovery, it is important to appreciate other factors that may have influenced her improvement. It is possible that this patient’s positive experience was impacted by the treatment setting in which she received VR intervention. Two cornerstones of IIPT are the coordinated team approach and intensity of therapies, both of which likely contribute to the observed faster responses to IIPT vs. outpatient treatment among highly impaired patients with chronic pain [17]. In this case report, both the patient and therapists noted times when team communication and carryover to the next session was critical, particularly when a new movement first happened in VR. This team’s communication and interdisciplinary environment likely contributed to the rapid improvement observed for this patient. While it is likely that similar successful outcomes could be achieved by incorporating VR into pain treatment conducted in other settings (e.g., outpatient), it is possible that the number of sessions or timeline of recovery could similarly vary. Additionally, the lessons learned by the clinical staff (as mentioned in Table 4) may be used for consideration when working with other patients and may provide a launch point for future researchers, although they may not be applicable with every patient or in every situation. Finally, in terms of limitations with the current case study, no information (e.g., open-ended questions, immersiveness) was collected after each VR session that could have provided insight into the progression of these themes (e.g., themes may become more positive with more exposure) or factors contributing to the positive impact of VR (e.g., more positive with more immersiveness). Measurement of pain, immersiveness (e.g., Child Presence Questionnaire [18]), and post-VR session interviews of patients and providers should be considered.
In summary, this case report highlights the versatility of VR as a tool that providers from various disciplines can successfully incorporate into treatment. Notably, each discipline used the same tool differently to improve function and target different goals across individual and group sessions. Future studies incorporating VR into pain treatment would benefit from a greater focus on the clinical decision-making surrounding the choice of when to use VR, patient characteristics that impact outcomes, and utilization in other treatment settings. More rigorous trials are needed, especially trials integrating insights from both patients and clinicians during the design of VR-based interventions for pain rehabilitation. These trials will allow for the evaluation of the added value of VR in pain treatment while providing an understanding of the mechanisms underlying how VR effectively reduces pain and enhances function (see review by Logan and colleagues on VR-based school simulation [10]). For example, one potential trial would randomize patients to receive VR content in a graded, goal-based manner (e.g., starting with simple physical challenges in VR and gradually adjusting difficulty, as outlined in Table 3). Alternatively, patients might receive external feedback through three-dimensional movement capture during the VR session (e.g., see an avatar or representation of themselves moving in sync with their actual movements). To conclude, further investigation is warranted to determine the optimal approach for integrating these strategies into effective pain rehabilitation using virtual reality.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The FIRST program received funding from the Junior Co-operative Society of Cincinnati Children’s Hospital Medical Center for the purchase of the VR equipment.
Declaration of interest
Authors have no financial relationships relevant to this article to disclose and no potential conflicts of interest.
References
[1] | Eccleston C , Fisher E , Howard RF , et al. Delivering transformative action in paediatric pain: a Lancet Child & Adolescent Health Commission. Lancet Child Adolesc Health. (2021) ;5: (1):47–87. doi: 10.1016/S2352-4642(20)30277-7. |
[2] | King S , Chambers CT , Huguet A , et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. (2011) ;152: (12):2729–38. doi: 10.1016/j.pain.2011.07.016. |
[3] | Dahlhamer J , Lucas J , Zelaya C , et al. Prevalence of Chronic Pain and High-Impact Chronic Pain Among Adults – United States, 2016. MMWR Morb Mortal Wkly Rep. (2018) ;67: (36):1001–6. doi: 10.15585/mmwr.mm6736a2. |
[4] | Groenewald CB . Opioid-prescribing Patterns for Pediatric Patients in the United States. Clin J Pain. (2019) ;35: (6):515–20. doi: 10.1097/AJP.0000000000000707. |
[5] | Mason I , Renee J , Marples I , et al. Functional neurological disorder is common in patients attending chronic pain clinics. Eur J Neurol. (2023) ;30: (9):2669–74. doi: 10.1111/ene.15892. |
[6] | Dowell D , Haegerich TM , Chou R . CDC Guideline for Prescribing Opioids for Chronic Pain – United States, 2016. MMWR Recomm Rep. (2016) ;65: (1):1–49. doi: 10.15585/mmwr.rr6501e1. |
[7] | Aybek S , Perez DL . Diagnosis and management of functional neurological disorder. BMJ. (2022) ;376: :o64. doi: 10.1136/bmj.o64. |
[8] | Goudman L , Jansen J , Billot M , et al. Virtual Reality Applications in Chronic Pain Management: Systematic Review and Meta-analysis. JMIR Serious Games. (2022) ;10: (2):e23440. doi: 10.2196/34402. |
[9] | Griffin A , Wilson L , Feinstein AB , et al. Virtual Reality in Pain Rehabilitation for Youth With Chronic Pain: Pilot Feasibility Study JMIR Rehabil Assist Technol. (2020) ;7: (2):e02262. doi: 10.2196/22620. |
[10] | Logan DE , Khanna K , Randall E , O’Donnell S , Reks T , McLennan L . Centering Patient and Clinician Voices in Developing Tools to Address Pain Related School Impairment: A Phase I Study of a Virtual Reality School Simulation for Children and Adolescents with Chronic Pain. Children (Basel). (2023) ;10: (10):1644. doi: 10.3390/children10101644. |
[11] | Trost Z , France C , Anam M , Shum C . Virtual reality approaches to pain: toward a state of the science. Pain. (2021) ;162: (2):325–31. doi: 10.1097/j.pain.0000000000002060. |
[12] | Carrougher GJ , Hoffman HG , Nakamura D , et al. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. (2009) ;30: (5):785–91. doi: 10.1097/BCR.0b013e3181b485d3. |
[13] | Colloca L , Raghuraman N , Wang Y , et al. Virtual reality: physiological and behavioral mechanisms to increase individual pain tolerance limits. Pain. (2020) ;161: (9):2010–21. doi: 10.1097/j.pain.0000000000001900. |
[14] | Gatica-Rojas V , Mendez-Rebolledo G . Virtual reality interface devices in the reorganization of neural networks in the brain of patients with neurological diseases. Neural Regen Res. (2014) ;9: (8):888–96. doi: 10.4103/1673-5374.131612. |
[15] | Gold JI , Mahrer NE . Is Virtual Reality Ready for Prime Time in the Medical Space? A Randomized Control Trial of Pediatric Virtual Reality for Acute Procedural Pain Management. J Pediatr Psychol. (2018) ;43: (3):266–75. doi: 10.1093/jpepsy/jsx129. |
[16] | Williams SE , Homan KJ , Crowley SL , et al. The Impact of Spatial Distribution of Pain on Long-Term Trajectories for Chronic Pain Outcomes After Intensive Interdisciplinary Pain Treatment. Clin J Pain. (2020) ;36: (3):181–8. doi: 10.1097/AJP.0000000000000793. |
[17] | Simons LE , Sieberg CB , Pielech M , Conroy C , Logan DE . What does it take? Comparing intensive rehabilitation to outpatient treatment for children with significant pain-related disability. J Pediatr Psychol. (2013) ;38: (2):213–23. doi: 10.1093/jpepsy/jss109. |
[18] | Gold JI , Kim SH , Kant AJ , Joseph MH , Rizzo AS . Effectiveness of virtual reality for pediatric pain distraction during i. v. placement. Cyberpsychol Behav. (2006) ;9: (2):207–12. doi: 10.1089/cpb.2006.9.207. |
Notes
1 Functional neurological disorder is a condition in which a patient experiences at least one symptom of altered voluntary motor or sensory function that is incompatible with recognized neurological or medical conditions and results in significant functional impairment.




