The functional secondary effect after an integrated rehabilitative intervention to learn reading and writing in a girl with Rubinstein-Taybi syndrome
Abstract
PURPOSE:
A case report of a six-year and five-month-old female admitted with typical symptoms of Rubinstein-Taybi syndrome is presented. Clinical and rehabilitation settings where she acquired her reading, writing, and communication skills are described.
METHODS:
Because of her cognitive disabilities, a multidisciplinary and long-term intervention (2014–2020) was necessary. Treatment included orthoptic, psychomotor, logopedic, occupational, and neuropsychological care. Her family and school were involved.
RESULTS:
Increased attention led to decreased dysfunctional behaviors. Test results are still below average, but there has been significant improvement. Better communication skills resulted from increased phonetic range, improved articulation, lexical-semantic structure, comprehension, and production of sentences. Digital technologies played a significant role in enhancing her communication skills, not just in social interactions but also in school activities. The patient is oriented in time and space with the help of agendas and calendars. She can express her needs and compose concise narratives. As a result of acquiring functional skills, she is better equipped to handle real-life situations, which has led to increased social and family activities.
CONCLUSION:
This case report highlights the importance of personalized rehabilitation programs. Obtaining an early genetic diagnosis is crucial for timely tailored rehabilitation, and any delays in this process can hinder progress.
1Introduction
Rubinstein-Taybi syndrome (RTS) is a rare genetic disease [1] This syndrome usually occurs sporadically. Most cases are attributable to de novo mutations [2–4]. However, it can also be inherited as an autosomal dominant disorder [5].
Physical features include microcephaly, characteristic facial appearance, broad thumbs/halluces, and post-natal growth retardation. Behavioral and cognitive characteristics associated with RTS include impulsivity, repetitive behaviors, moderate to severe intellectual disability, and delayed speech [6]. The estimated prevalence at birth is about one in 100,000–125,000 live births [5, 7]. During infancy, individuals with RTS can establish good social relationships; in adulthood, sudden mood changes and obsessive-compulsive behavior can occur.
In 50–60% of cases, the syndrome is linked to mutations in cyclic-AMP-response element binding protein (CREB)-binding protein gene (CREBBP) localized at 16p13.3 [2–4, 8–10]. In 8–10% of cases, RTS is caused by a mutation of chromosome 22q13 encoding for E1-A associated protein p300 [4, 9–11]. CREBBP (RST1) and EP300 (RST2) genes express homologous proteins belonging to the KAT3 family of lysine acetyltransferases and play different roles in motor skill learning as transcriptional coactivators. The spectrum of CREBBP mutations includes point mutations (30–50% ) [2, 3, 8, 9] and deletions (10% ). In EP300, the genetic defects include 21-point mutations and five deletions [9, 11]. Finally, 30% of cases are caused by unknown genetic variations [12].
This case describes a female with RTS who underwent a multidisciplinary intervention to take care of her disabilities globally and promote her autonomy, functioning, and social integration in daily life. The study was conducted according to the World Medical Association Declaration of Helsinki. The Institutional Review Board of KOS-CARE approved the study, with approval number N.03, February 10, 2022. Written informed consent for publication was obtained from the family.
2Case report
The child is the second of three children, none of whom had phenotypic similarities with the patient. She was born at term (41st week) by partus caesareus after a normal pregnancy, weighing 3 kg 575 g. At age three, she underwent a right lachrymal duct stenosis correction [13, 14]. She had a history of recurrent respiratory infections, an episode of pyelonephritis, growth delay, coloboma on the optic nerve of the right eye [15], and patent ductus arteriosus with a slight-moderate left-right shunt [16], which was closed at the age of six; no major cardiopathy was reported.
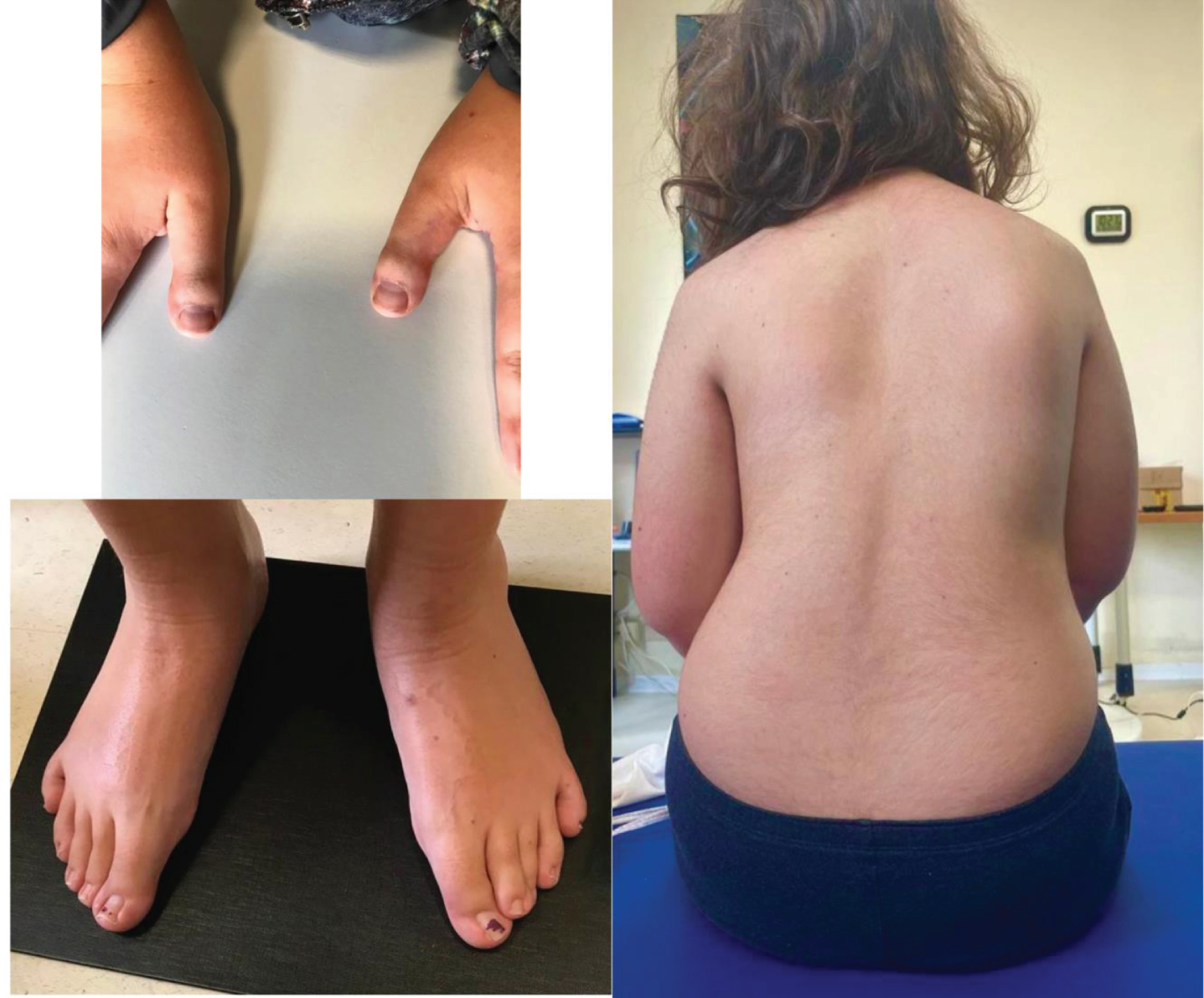
At six years and five months, she was admitted after undergoing rehabilitation, mainly language-focused, at another hospital. Clinical assessment revealed the smile characteristic of RTS, with a partial closure of the eyes, ogival palate [17], short fingers, broad thumbs, bilateral flat feet with overlapping of the second toe of the left foot, bilateral deviation of the fifth toe, initial structural scoliosis (Fig. 1), reduced eye-hand coordination, and autonomous pathway. No history of epileptic seizures nor pharmacological therapy was reported.
Fig. 1
Clinical findings of the patient. In the figure are represented the pictures of distinctive physical features, namely angled and broad thumbs (left, right), bilateral flat feet with overlapping of the second toe of the left foot and bilateral deviation of the fifth toe (left, bottom), and initial structural scoliosis (right). Permission was obtained from the parents for the use of the photographs.
Beyond delayed cognitive development, the child exhibited a language disorder characterized by reduced comprehension and simplified speech. She also had orofacial praxic difficulties and accentuated attention and memory fluctuations. Although social, she faced communication difficulties, necessitating an additional year of kindergarten to address her cognitive and linguistic delays. The child displayed poor coordination, struggling with object manipulation and daily activities when performed without adult assistance.
RTS was first suspected on clinical grounds at age three. Genetic testing for deletions in the region of the CREBBP gene [18] by fluorescence in situ hybridization in metaphase chromosomes from lymphocytes did not show deletions in either chromosome 16. The same technique extended to the region containing the EP300 gene did not show deletions in either chromosome 22. At age four years and three months, the diagnosis of RTS was confirmed by the multiplex ligation-dependent probe amplification technique (MRC Holland kit, Amsterdam, Netherlands), more sensitive than the standard method (denaturing high-performance liquid chromatography and direct sequencing) for detecting exonic deletions/duplications in CREBBP in genomic DNA extracted from peripheral blood. A variation was found in exon one of CREBBP. This variation is not reported in the literature or the Leiden Open Variation Database. The deletion was confirmed by independent analysis using the comparative genomic hybridization technique.
2.1Assessment
Gross motor development was evaluated using the Gross Motor Function Classification System [19]. Functional sitting was measured by the Level of Sitting Scale [20]. Finally, walking was assessed using the Six-Minute Walk Test [21].
An ophthalmologic exam was performed to measure visual acuity and oculomotor function.
Language was assessed using standardized tests, selected based on the patient’s developmental level. Test di Valutazione del Linguaggioa (TVL) [22] was used to measure denomination, word/sentence comprehension, and sentence repetition (metaphonological skills - Valutazione delle Competenze Metafonologiche) test [23]. Since her age exceeded the normative data of TVL (six years), the raw score was converted into the “age test” score for scoring purposes. Naming, lexical, and grammatical comprehension, as well as word/non-word and sentence repetition were evaluated using the Batteria per la Valutazione del Linguaggiob (4–12) [24]. Reading ability and comprehension were assessed with Prove di Lettura MT2 and MT3 tests [25, 26]. Writing ability was measured with the Batteria per la Valutazione della Dislessia e della Disortografia Evolutiva-2c, [27], while dictation was measured with the Batteria per la Valutazione della Scrittura e delle Competenze Ortografiched [28].
A neuropsychological assessment was conducted using age-standardized tests and semi-structured observations. Cognitive development was assessed with the Wechsler Preschool and Primary Scale of Intelligence-III [29] and Wechsler Intelligence Scale for Children-IV (WISC-IV) scales [30]; cognitive domains were evaluated with Batteria di Valutazione Neuropsicologicae (BVN 5-11) [31] and the Batteria di Valutazione Neuropsicologica per l’adolescenzaf (BVN 12–18) [32]. Short-term and visual-spatial memories, verbal recall, and phonemic and category fluency were evaluated. The Developmental Test of Visual-Motor Integration (VMI) [33] was used to study visual-motor integration capacity.
The Canadian Occupational Performance Measure (COPM) [34] was administered at age 13 to explore the impact of technologies on the patient’s self-perception of performance and satisfaction with daily living activities.
2.2Goals and intervention
A multidisciplinary intervention was performed, aligning therapeutic goals with the family to improve visuomotor coordination, attention, communication, language, and executive functions. Additional aims included promoting school inclusion and providing family training. Parent sessions focused on emotional support, communication improvement, and stress reduction [35, 36], with guidance on managing dysfunctional behaviors (impulsiveness, distractibility, repeatability). Regarding motor functions, all administered scales showed a ceiling effect, indicating no deficits. As a result, no additional actions were taken.
Due to visual difficulties, the child received immediate optical correction and orthoptic treatment. Ophthalmologic examination revealed low vision in both eyes (corrected visual, 6/10), ptosis in the right upper eyelid, an oculomotor disorder characterized by intermittent exotropia, bilateral deficits in elevation and depression, hyperfunction of small oblique muscles, abduction deficit of the right eye, and an anomalous hyperextended head position. An accommodation target was utilized to address these issues, along with presenting objects systematically to stimulate pursuit and saccadic eye movements, improving attention and location scanning accuracy [37]. Surgery in September 2015 partially corrected the strabismus.
Eye-hand coordination exercises involving horizontal and vertical lines were recommended to practice right-left laterality movements and wrist flexion/extension.
Speech therapy aimed to enhance communication, focusing on lexical-semantic structure, comprehension, morphosyntactic production, and overall communicative effectiveness. Stereognosis with physical shapes (Fig. 2) was used to promote learning alphabet letters.
Fig. 2
Facilitation for learning to write the letter “A”. The child was asked to follow a sinusoidal track, staying within the path (black lines) without touching the two edges (left). Since she had difficulty recognizing and learning abstract shapes (letters or geometric figures), stereognosis recognition of shapes was employed, using tangible forms, such as the tree crown (middle) or the roof of a house (right).
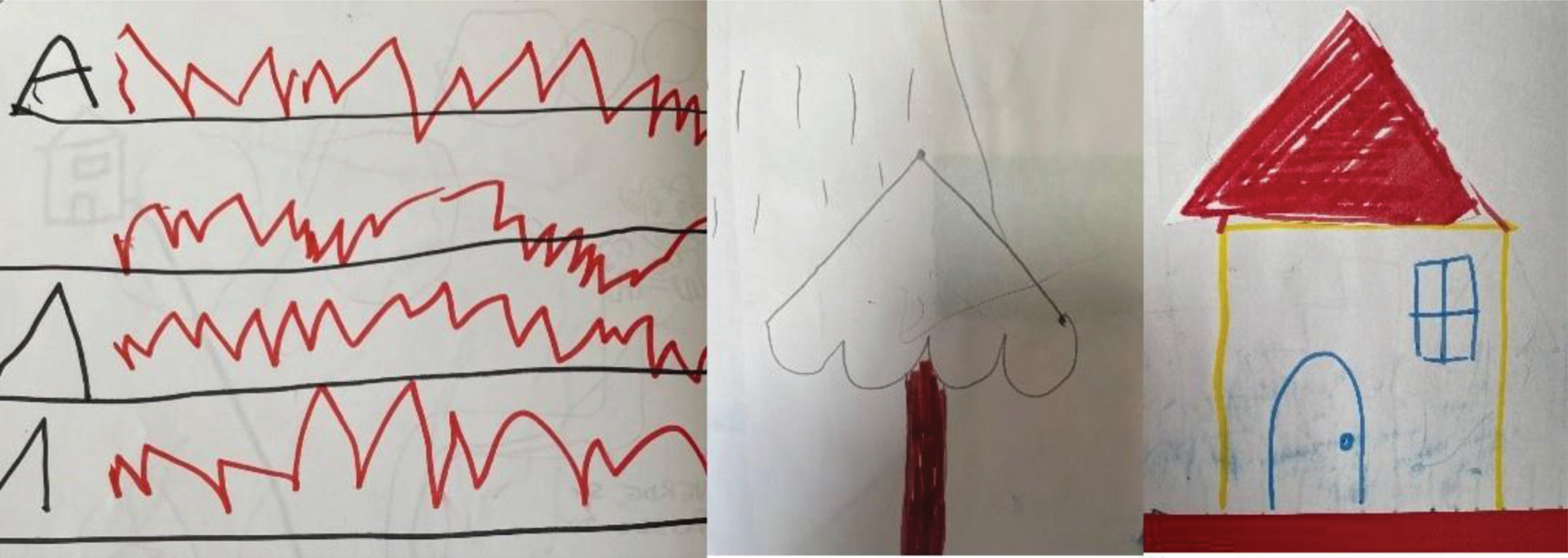
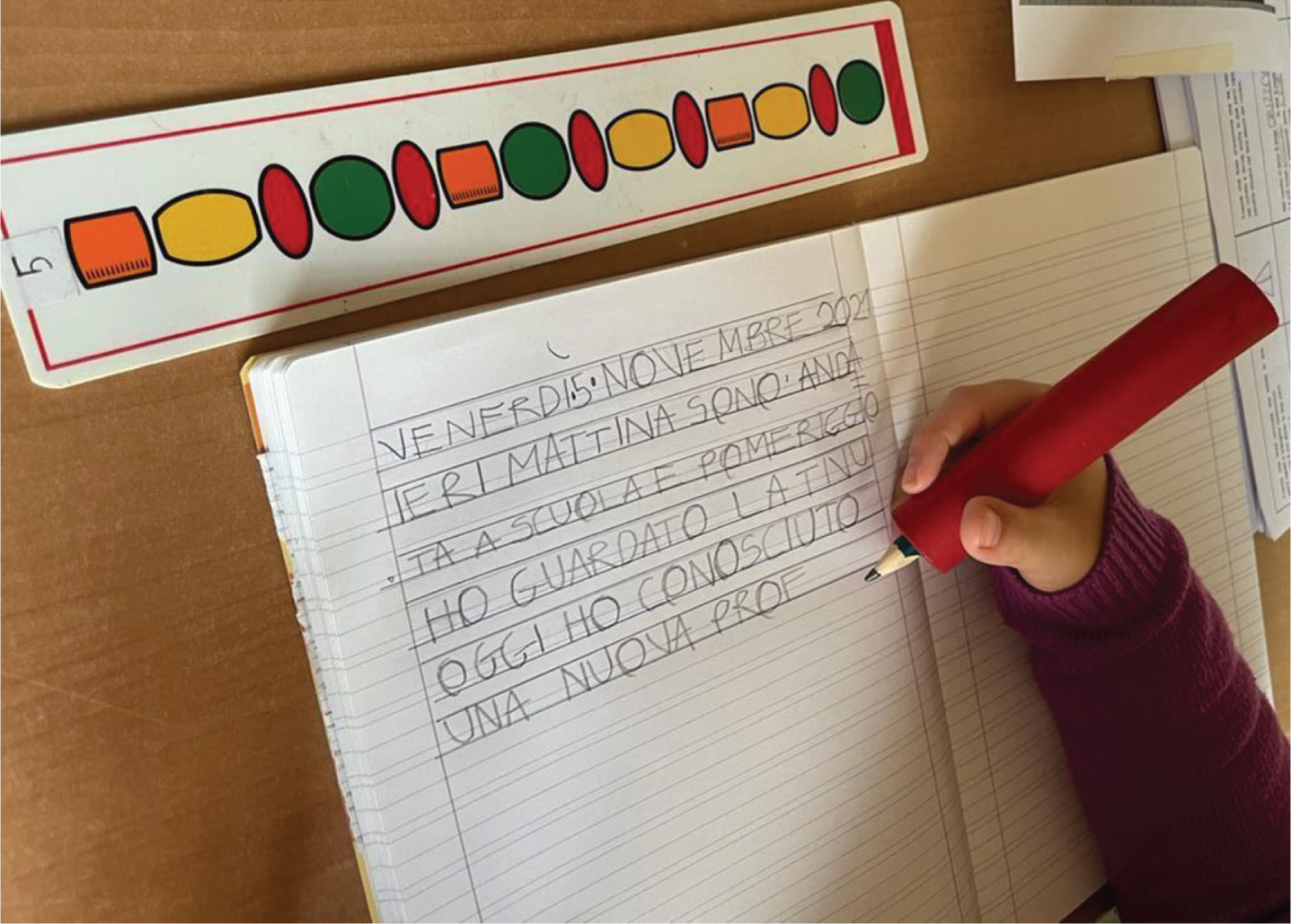
Capital letters on double-lined paper were used as well (Fig. 3).
Fig. 3
Correct holding of pencil and facilitation for writing letters on lined paper. An adaptive device facilitated a proper grip of the writing instrument, resulting in legible writing. Following a prolonged period of gradual learning, she has demonstrated the capability of producing uppercase block letters on a spacious, lined paper featuring double-line spacing.
The syllabic method was applied for reading and writing [38].
Cognitive abilities were developed using the Feuerstein method of Instrumental Enrichment (IE), initially basic [39], then the standard IE [40].
Psychomotor treatment aimed to enhance motor skills and spatial awareness through exercises targeting personal, peripersonal, and extrapersonal space. Fine and praxic movements were practiced with selective reinforcement for the right hand.
Activities included time-space orientation tasks like writing the date and sequencing daily activities.
Occupational therapy incorporated digital technologies, like smartphones and computers, to teach her internet browsing (Google Chrome; YouTube), the use of word-processing software (OOo4Kids, version 1.3; Microsoft Office Suite), and text messaging.
3Results
The patient’s language skills were monitored longitudinally, revealing consistent improvement despite scores on each test remaining below normative data. Notably, improvements were observed in orofacial apraxia [41], reading, word/sentence comprehension, and naming [42], as detailed in Tables 1 and 2.
Table 1
Evaluation of language and learning (age 6.8–8.8 years)
| Speech tests | 2014 (6.8 years) | 2015 (7.8 years) | 2016 (8.8 years) | ||||
| TVL (Cianchetti 1997) | Range | RS | AGEequiv | RS | AGEequiv | ||
| Word comprehension | 0–80 | 59 | 42–47 months | 65 | 48–53 months | ||
| Phrase comprehension | 0–36 | 19 | 30–35 months | 27 | 48–53 months | ||
| Phrase repetition | 0–15 | 4 | 30–35 months | 5 | 45 months | ||
| Naming | 0–40 | 15 | 30–35 months | 30.5 | 59 months | ||
| “Denominazione di figure” a | RANGE | RS | SD | RS | SD | ||
| (Brizzolara, 1989) | |||||||
| High frequency | 0–50 | 18 | –5.6 | 42 | –0.4 | ||
| Low frequency | 0–50 | 7 | –2.6 | 18 | –2.3 | ||
| “Test delle prassie oro-facciali” b | RANGE | RS | SD | RS | SD | RS | SD |
| (Bearzotti, 2003) | |||||||
| Orofacial praxis (imitation) | 0–12 | 7 | –7.8 | 12 | + 0.5 | 12 | + 0.5 |
| Oroverbal praxis (imitation) | 0–12 | 10 | –1.3 | 12 | + 0.5 | 12 | + 0.5 |
| Sequences (imitation) | 0–6 | 3 | –4.9 | 4 | –3 | 4 | –3 |
| Parallel movements (imitation) | 0–6 | 3 | –6 | 5 | –5 | 5 | –5 |
| CMF infant school | RANGE | RS | % il | ||||
| (Marotta Vicari, 2008) | |||||||
| Syllabic synthesis | 0–15 | 13 | 10th | ||||
| Minimal word pairs | 0–15 | 12 | 10th–25th | ||||
Legend: TVL: “Test di Valutazione del Linguaggio” [Language Assessment Test]; CMF: “Competenze metafonologiche” [Phonological skills]; RS: raw score; AGE equiv: equivalent age; SD: standard deviation away from the mean for age; % il: percentile; ≤-2SD: poor performance; between -2SD and -1SD: at risk; between -1SD and 0SD: normal performance; ≤5th: poor performance; 5th-10th: at risk; >10th: normal. aNaming pictures. bOrofacial praxis test.
Table 2
Evaluation of language and learning (age 10.2–13.2 years)
| SPEECH TESTING | 2017 (10.2 years) | 2018 (11.2 years) | 2019 (12.2 years) | 2020 (13.2 years) | |
| BVL 4–12 (Marini et al. 2015) | RANGE | RS SD | RS SD | RS SD | RS SD |
| Naming | 0–67 | 50 < 2SD at 11.6–11.11 y. | 56 < 2SD at 11.6–11.11 y. | ||
| Reading comprehension School age | 0–42 | 19 < 2SD at 10.0–10.5 y. | 21 < 2SD at 11.0–11.5 y. | 27 < 2SD at 11.6–11.11 y. | 24 < 2SD at 11.6–11.11 y. |
| Grammatical comprehension | 0–40 | 17 < 2SD at 10.0–10.5 y. | 27 –2SD at 11.0–11.5 y. | 30 –2 SD at 11.6–11.11 y. | 31 –2 SD at 11.6–11.11 y. |
| Word repetition | 0–15 | 14 < 2SD at 10.0–10.5 y. | 14 < 2SD at 11.0–11.5 y. | 14 < 2SD at 11.6–11.11 y. | |
| Non–word repetition | 0–15 | 8 < 2SD at 10.0–10.5 y. | 8 < 2SD at 11.0–11.5 y. | 13 < 2SD at 11.6–11.11 y. | |
| Phrase repetition Preschool age | 0–20 | 8 < 2SD at 5.6–5.11 y. | 10 < 2SD at 5.6–5.11 y. | ||
| Phrase repetition School age | 0–20 | 7 < 2SD at 11.6–11.11 y. | |||
| Reading and writing tests | RANGE | RS SD | |||
| (Martini 1995) | |||||
| Reading plain disyllabic words (paroxytone) | 0–10 | 8 E –8SD, T–2.1SD | |||
| Reading trisyllabic words | 0–10 | 9 E–1SD, T –1SD | |||
| Reading disyllabic groups | 0–10 | 4 E–8SD, T–0.3SD | |||
| Writing plain disyllabic words | 0–10 | 9 E–2.6SD | |||
| Writing trisyllabic words | 0–10 | E–4.7SD | |||
| Writing disyllabic groups | 0–10 | 7 E–1.6SD | |||
| MT 2 (Cornoldi et al. 1998) | |||||
| Reading comprehension | T: 0.93 syll/sec E 8 | ||||
| MT 3 (Cornoldi et al. 2016) | T: 0.81 syll/sec 30th–40th, | ||||
| Reading comprehension | |||||
| MT2 (Cornoldi et al. 1998) | RANGE | RS | RS | ||
| Written comprehension | 0–15 | 10 | 9 | RS | |
| MT3 (Cornoldi et al. 2016) | |||||
| Written comprehension | 0–12 | 2 < 5th | |||
| DDE–2 (Sartori et al. 2007) | T: –2.4SD 36: –4SD | T: –6SD E 44: –14SD | |||
| Reading words | E 12 –11 S DE 11 | E 6 –5SD | |||
| Writing words | |||||
| Writing non–words | 4SD | E 7 –2.5SD | |||
| BVSCO–2 (Tressoldi et al. 2019) | E 16 < 5th | ||||
| Dictation |
Legend: BVL: Batteria per la valutazione del Linguaggio [Language Assessment Battery]; MT: Valutazione delle Competenze Metafonologiche; DDE: Batteria per la valutazione della dislessia e della disortografia evolutiva [Battery for evaluation of dyslexia and developmental dysorthography]; BVSCO: Batteria per la Valutazione della Scrittura e della Competenza Ortografica [Writing and Spelling Competence Evaluation Battery]; RS: raw score; SD standard deviation away from the mean for age; E: errors; y: years; T: time; Syll/sec: syllables per second.
Currently, she can compose simple essays through self-dictation and write individual words in printed capitals, albeit with minor orthographic errors resembling those of native Italian speakers with aphasia [43]. She makes errors when reading short, simple, and printed texts in capitals. Rereading with a ruler reduces the risk of missing a line and improves decoding accuracy.
Regarding cognitive assessment (Table 3), processing speed subtests of the WISC-IV [30] scale were not administered because of her hand-eye coordination difficulties. The General Ability Index (GAI) was calculated, and her score was below average, falling in the range of moderate intellectual disability according to the Diagnostic and Statistical Manual of Mental Disorders criteria [44, 45].
Table 3
Cognitive assessment
| 2014 | 2016 | 2017 | 2018 | 2019 | 2020 | ||||||||
| NEUROPSYCHOLOGICAL TESTS | RANGE | RS | WS/SS | RS | WS/SS | RS | WS/SS | RS | SS | RS | WS/SS | RS | SS |
| WPPSI–III (Wechsler, 2008) | |||||||||||||
| Block design | 0–40 | 12 | WS 1 | ||||||||||
| Information | 0–34 | 24 | WS 5 | ||||||||||
| Matrix reasoning | 0–29 | 11 | WS 5 | ||||||||||
| Vocabulary | 0–43 | 21 | WS 6 | ||||||||||
| Picture concept | 0–28 | 13 | WS 6 | ||||||||||
| Word reasoning | 0–28 | 10 | WS 4 | ||||||||||
| Coding | 0–65 | 3 | WS 1 | ||||||||||
| Receptive vocabulary | 0–38 | 19 | WS 3 | ||||||||||
| Picture naming | 0–30 | 15 | WS 3 | ||||||||||
| VERBAL IQ | 50–151 | 86 | |||||||||||
| PERFORMANCE IQ | 42–158 | 74 | |||||||||||
| FULL SCALE IQ | 38–162 | 79 | |||||||||||
| GENERAL LANGUAGE COMPOSITE | 48–152 | 58 | |||||||||||
| WISC–IV (Orsini, 2012) | |||||||||||||
| Block design | 0–50 | 0 | WS 1 | 1 | WS 1 | 1 | WS 1 | 5 | WS 1 | 8 | WS 2 | ||
| Similarities | 0–44 | 7 | WS 5 | 9 | WS 5 | 10 | WS 5 | 12 | WS 5 | 13 | WS 5 | ||
| Picture concepts | 0–28 | 3 | WS 1 | 9 | WS 5 | 10 | WS 5 | 8 | WS 3 | 10 | WS 4 | ||
| Vocabulary | 0–68 | 17 | WS 5 | 13 | WS 2 | 18 | WS 3 | 16 | WS 2 | 22 | WS 3 | ||
| Matrix reasoning | 0–35 | 10 | WS 6 | 15 | WS 9 | 7 | WS 2 | 10 | WS 4 | 11 | WS 3 | ||
| Comprehension | 0–42 | 1 | WS 1 | 2 | WS 1 | 6 | WS 2 | 2 | WS 1 | 3 | WS 1 | ||
| VERBAL COMPREHENSION INDEX | 46–154 | 62 | 56 | 60 | 56 | 58 | |||||||
| VISUAL–PERCEPTUAL REASONING INDEX | 41–159 | 52 | not interpretable | 52 | 52 | 54 | |||||||
| IAG GENERAL ABILITY INDEX (GAI) | 42 | 50 | 48 | 51 | |||||||||
| BVN 5–11 (Bisiacchi, 2005) | |||||||||||||
| Visual naming | 0–20 | 9 | SS 63.8 | 10 | SS67.6 | ||||||||
| Syntactic comprehension | 0–18 | 9 | SS 35 | ||||||||||
| Word free recall | 0–16 | 3 | SS 61.6 | 5 | SS 72.7 | 5 | SS 73.3 | ||||||
| Visuospatial short–term memory | 0–7 | 0 | 2 | SS 49.5 | 2 | SS 50.1 | 2 | SS 39.8 | |||||
| Verbal selective reminding | |||||||||||||
| Recall | 0–64 | 21 | 40 | SS 70.8 | 38 | SS 30.1 | 43 | SS 18.3 | |||||
| Delayed Recall | 0–8 | 0 | 5 | SS 76.0 | 6 | SS 58.4 | 4 | SS 44.3 | |||||
| Category fluency | 0–inf | 14 | 17 | SS 54.6 | 14 | SS 46.9 | 15 | SS 54.9 | |||||
| Phonemic fluency | 0–inf | 12 | SS 71 | 9 | SS 67.3 | ||||||||
| BVN 12–18 (Gugliotta, 2009) | |||||||||||||
| Visuospatial short–term memory | 0–7 | 2 | SS 41.2 | 2 | SS 41 | ||||||||
| Verbal selective reminding | |||||||||||||
| Recall | 0–96 | 47 | SS 45.8 | 50 | SS 33 | ||||||||
| Delayed Recall | 0–12 | 1 | SS 12.3 | 0 | |||||||||
| Phonemic fluency | 0–inf. | 5 | SS 58.6 | 10 | SS 47.8 | ||||||||
| Category fluency | 0–inf. | 17 | SS 39.5 | 20 | SS 39.3 | ||||||||
| VMI (Preda, 2000) | 0–27 | 6 | SS 56 | 10 | SS 63 | 8 | SS 53 | 9 | SS 52 | 10 | SS 56 | 11 | SS 56 |
| Visual test | 0–27 | 6 | SS 52 | 8 | SS 45 | ||||||||
| Motor test | 0–27 | 6 | SS 46 | 10 | SS 52 | ||||||||
Legend: WPPSI: Wechsler Preschool and primary scale of intelligence; WISC: Wechsler Intelligence Scale for Children; BVN: Batteria di Valutazione Neuropsicologica [Neuropsychological Evaluation Battery]; VMI: Developmental Test of Visual-Motor Integration; RS: raw score; WS: weighted score; SS: standard score.
Scores on BVN 5-11 [31] and BVN 12–18 [32] showed that her visual-spatial memory span remained constant. The ability to learn unstructured verbal material and delayed recall of items remained poor. However, improvements were seen in internal lexical access. Visual-motor integration capabilities, as tested by VMI, remained reduced across all collections.
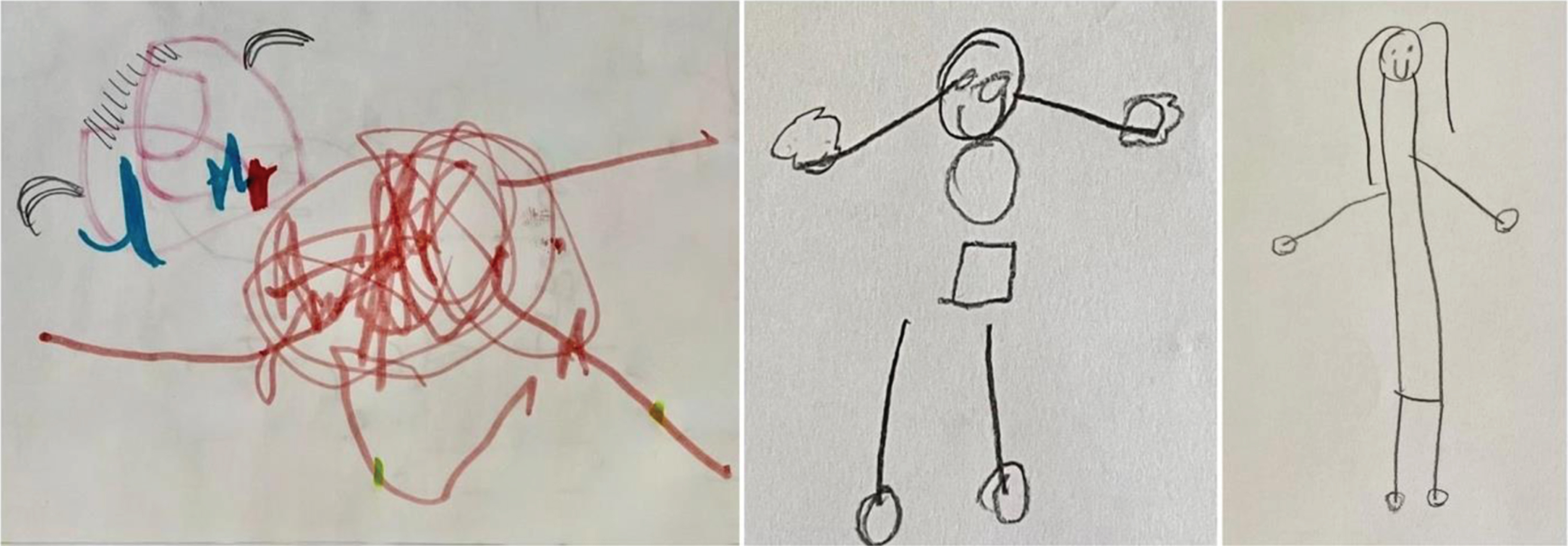
The Draw-a-Person test [46–48] showed progress. In the last administration, the child could draw a human figure with all the elements and details in the correct positions (Fig. 4).
Fig. 4
Progress in drawing the human figure. In the most recent version (age 13), some progress was noticed compared to the previous performance. Indeed, the human figure was recognized, the drawing was well-placed on the page, details such as the face with eyes, mouth, and hair were depicted, and the trunk was elongated with correctly placed legs and arms. The drawing matched a mental age of five years.
Although formal measures assessing inattention and/or impulsivity were not used in this study, clinical observations revealed improvements in focused and sustained attention, with a partial reduction of impulsive behaviors. Note that no medications were administered.
Finally, the scores on the COPM scale (Table 4) demonstrated a significant increase in both self-perception of her performance and degree of satisfaction, meaning that the treatment was effective.
Table 4
Scores on Canadian Occupational Performance Measure (COPM) (age 13)
| 2020 | 2020 | |||
| Occupational Performance | Performance T1 | Satisfaction T1 | Performance T2 | Satisfaction T2 |
| Problems | ||||
| Listening to music | 3 | 2 | 7 | 9 |
| Texting | 2 | 4 | 10 | 10 |
| Browsing on the internet | 1 | 2 | 9 | 8 |
| Composing narratives | 4 | 3 | 8 | 10 |
| Total score | 10 | 11 | 34 | 37 |
| Average score | 2.5 | 2.75 | 8.5 | 9.25 |
The child identified the most important problems and ranked them in order of importance: listening to music (importance rate, 9), texting (importance rate, 8), browsing the internet (importance rate, 8), and composing narratives (importance rate, 7). For each problem, she rated it based on performance and satisfaction. The average score was calculated by adding together the performance and satisfaction scores for all problems (total score) and dividing by the number of problems. The assessment (T1) and reassessment (T2) were performed at the beginning and end of treatment, respectively. The treatment is considered effective if the change in performance and/or satisfaction is greater than two (Performance Average Score T2 – Performance Average Score T1, Satisfaction Average Score T2 – Satisfaction Average Score T1).
4Discussion
The case describes a girl with RTS, which is known to cause behavioral and neuropsychiatric issues. However, there is a lack of data about its natural progression [49]. Age-related changes have been described in RTS with mood difficulties, and temper tantrums may increase with age [50]. The pathogenic variant can affect behavioral, cognitive, and emotional characteristics [51]. No RTS-specific interventions or treatments exist [49]; diagnostic criteria and care practices are heterogeneous worldwide [52]. However, international recommendations for clinical diagnostic criteria, molecular investigations, long-term management of physical and behavioral issues, and care planning for different types of RTS are now available [52]. To date, therapies directed toward speech, behavior, and daily living skills, like the one presented, have proven crucial [49]. It has been demonstrated that early speech and language therapy is beneficial in supporting the development of communication and subsequently reducing challenging behaviors, which leads to a better quality of life [50].
In this instance, due to her severe intellectual disability, a multidisciplinary approach was necessary to improve the patient’s reading, writing, and daily life skills.
Addressing the previously neglected visual difficulties was crucial in enabling the child to perform optimally and achieve the goals set by the speech and psychomotor therapists. Collaborating with a team of specialists across different settings improved her ability to stay engaged in the same task for longer periods of time. This resulted in a reduction of the most regressive and dysfunctional aspects of her behavior [53]. Family involvement from the early phases and a continuous dialogue with teachers were crucial too.
While test results did not demonstrate improvements, her social and conversational skills have progressed notably. She actively engages in conversations, poses questions, and articulates her interests and needs. She can independently express her requests and share personal accounts using reading and writing for orientation, enhancing her autonomy in familiar environments [54].
Furthermore, her communication abilities and social interactions have been enhanced through the utilization of computers and smartphones. These technologies have not only facilitated educational accessibility but also fostered increased engagement in school activities.
5Conclusions
A long-term multidisciplinary rehabilitation [55], like the one presented, increased her independence in daily life and enabled the application of acquired functional and communication skills, despite her intellectual disability which affected her test scores.
The cognitive delay associated with these disorders and the limits imposed by the syndrome result in low investment in rehabilitation programs [56]. This issue is further compounded by delays in genetic diagnosis and challenges in tailoring specific rehabilitation programs. However, personalized programs focusing on individual skills are crucial for enhancing autonomy and quality of life [47]. Continuous counseling and support from family, school, and social environments are essential for successful rehabilitation outcomes in patients with complex disabilities.
Acknowledgments
The authors have no acknowledgments.
Conflict interest
The authors have no conflict of interest to report.
Ethical considerations
The family gave written informed consent for the study.
References
[1] | Rubinstein JH , Taybi H . Broad thumbs and toes and facial abnormalities. A possible mental retardation syndrome. Am J Dis Child. (1963) ;105: (6):588–608. doi: 10.1001/archpedi.1963.02080040590010 |
[2] | Bartsch O , Schmidt S , Richter M , et al. DNA sequencing of CREBBP demonstrates mutations in 56% of patients with Rubinstein-Taybi syndrome (RSTS) and another patient with incomplete RSTS. Hum Genet. (2005) ;117: (5):485–93. doi: 10.1007/s00439-005-1331-y |
[3] | Bentivegna A , Milani D , Gervasini C , et al. Rubinstein-Taybi Syndrome: spectrum of CREBBP mutations in Italian patients. BMC Med Genet. (2006) ;7: :77. doi: 10.1186/1471-2350-7-77 |
[4] | Stevens CA . Rubinstein-Taybi Syndrome. In: Adam MP , Everman DB , Mirzaa GM . editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; (2002) . |
[5] | Hennekam RC . Rubinstein-Taybi syndrome. Eur J Hum Genet. (2006) ;14: (9):981–5. doi: 10.1038/sj.ejhg.5201594 |
[6] | Adrien JL , Taupiac E , Thiébaut E , et al. A comparative study of cognitive and socio-emotional development in children with Rubinstein-Taybi syndrome and children with Autism Spectrum Disorder associated with a severe intellectual disability, and in young typically developing children with matched developmental ages. Res Dev Disabil. (2021) ;116: :104029. doi: 10.1016/j.ridd.2021.104029 |
[7] | Milani D , Manzoni FM , Pezzani L , et al. Rubinstein-Taybi syndrome: clinical features, genetic basis, diagnosis, and management. Ital J Pediatr. (2015) ;41: :4. doi: 10.1186/s13052-015-0110-1 |
[8] | Petrij F , Giles RH , Dauwerse HG , et al. Rubinstein–Taybi syndrome caused by mutations in the transcriptional co-activator CBP. Nature. (1995) ;376: (6538):348–351. doi: 10.1038/376348a0 |
[9] | Roelfsema JH , Peters DJ . Rubinstein–Taybi syndrome: clinical and molecular overview. Expert Rev Mol Med. (2007) ;9: (23):1–16. doi: 10.1017/S1462399407000415 |
[10] | Fergelot P , Van Belzen M , Van Gils J , et al. Phenotype and genotype in 52 patients with Rubinstein–Taybi syndrome caused by EP300 mutations. Am J Med Genet A. (2016) ;170: (12):3069–82. doi: 10.1002/ajmg.a.37940 |
[11] | Negri G , Milani D , Colapietro P , et al. Clinical and molecular characterization of Rubinstein-Taybi syndrome patients carrying distinct novel mutations of the EP300 gene. Clin Genet. (2015) ;87: (2):148–54. doi: 10.1111/cge.12348 |
[12] | Fadly MdA , Ismail A , Keong TM , Yusoff NM , Zakaria Z . Chromosomal 16p microdeletion in Rubinstein–Taybi syndrome detected by oligonucleotide-based array comparative genomic hybridization: a case report. J Med Case Rep. (2012) ;6: :30. doi: 10.1186/1752-1947-6-30 |
[13] | Naik JM , Naik MN , Ali MJ . Lacrimal drainage anomalies in Rubinstein-Taybi syndrome: case report and review of literature. Orbit. (2019) ;38: (4):335–337. doi: 10.1080/01676830.2018.1515961 |
[14] | Marabotti A , Giannecchini G , Cariello A , et al. A. Stenosis of the lachrymal system in Rubinstein-Taybi syndrome. Ophthalmologica. (2002) ;216: (4):272–6. doi: 10.1159/000063837 |
[15] | van Genderen MM , Kinds GF , Riemslag FC , Hennekam RC . Ocular features in Rubinstein-Taybi syndrome: investigation of 24 patients and review of the literature. Br J Ophthalmol. (2008) ;84: (10):1177–84. doi: 10.1136/bjo.84.10.1177 |
[16] | Stevens CA , Bhakta MG . Cardiac abnormalities in the Rubinstein-Taybi syndrome. Am J Med Genet. (1995) ;59: (3):346–8. doi: 10.1002/ajmg.1320590313 |
[17] | Bloch-Zupan A , Stachtou J , Emmanouil D , et al. Oro-dental features as useful diagnostic tool in Rubinstein-Taybi syndrome. Am J Med Genet A. (2007) ;143A: (6):570–3. doi: 10.1002/ajmg.a.31622 |
[18] | Van Gils J , Magdinier F , Fergelot P , Lacombe D . Rubinstein-Taybi Syndrome: A Model of Epigenetic Disorder. Genes (Basel). (2021) ;12: (7):968. doi: 10.3390/genes12070968 |
[19] | Palisano RJ , Rosenbaum P , Bartlett D , Livingston MH . Content validity of the expanded and revised Gross Motor Function Classification System. Dev Med Child Neurol. (2008) ;50: (10):744–50. doi: 10.1111/j.1469-8749.2008.03089.x |
[20] | Field DA , Roxborough LA . Validation of the relation between the type and amount of seating support provided and Level of Sitting Scale (LSS) scores for children with neuromotor disorders. Dev Neurorehabil. (2012) ;15: (3):202–8. doi: 10.3109/17518423.2012.673177 |
[21] | ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. (2002) ;166: (1):111–7. doi: 10.1164/ajrccm.166.1.at1102 |
[22] | Cianchetti C , Fancello GS . Test TVL. Test di valutazione del linguaggio. Livello prescolare. Trento: Edizioni Erickson; (1997) . |
[23] | Marotta L , Trasciani M , Vicari S . Prova CMF. Valutazione delle competenze metafonologiche. Con CD-ROM. Trento: Erickson; (2008) . |
[24] | Marini A , Marotta L , Bulgheroni S , Fabbro F . Batteria per la valutazione del linguaggio in bambini dai 4 ai 12 anni (BVL 4-12). Firenze: Giunti OS; (2015) . |
[25] | Cornoldi C , Colpo G . Prove Di Lettura MT per La Scuola Elementare-2 Seconda Elementare. Firenze: Giunti, OS; (1998) . |
[26] | Cornoldi C , Carretti B . Dimostra MT-3 clinica: la valutazione delle abilità di lettura e comprensione per la scuola primaria e secondaria di I grado. Firenze: Giunti Edu; (2016) . |
[27] | Sartori G , Job R . DDE-2 Batteria per la valutazione della dislessia e della disortografia evolutiva-2: protocollo di registrazione. Firenze: Giunti OS; (2007) . |
[28] | Tressoldi PE , Cornoldi C , Re AM . BVSCO-2: Batteria per la Valutazione della Scrittura e della Competenza Ortografica-2: manuale e materiali per le prove. Firenze: Giunti; (2019) . |
[29] | Wechsler D , Fancello GS , Cianchetti C . WPPSI-III: Wechsler preschool and primary scale of intelligence: manuale di somministrazione e scoring. Firenze: Giunti OS; (2008) . |
[30] | Orsini A , Pezzuti L , Picone L . WISC-IV: Contributo alla taratura italiana. Firenze: Giunti OS; (2012) . |
[31] | Bisiacchi PS , Cendron M , Gugliotta M , et al. BVN 5-11: batteria di valutazione neuropsicologica per l’età evolutiva. Trento: Erickson; (2005) . |
[32] | Gugliotta M . BVN 12-18: batteria di valutazione neuropsicologia per l’adolescenza. Trento: Edizioni Erickson; (2009) . |
[33] | Preda C . VMI developmental test of visual motor integration. Italian version. Firenze: OS; (2000) . |
[34] | Carswell A , McColl MA , Baptiste S , Law M , Polatajko H , Pollock N . The Canadian Occupational Performance Measure: a research and clinical literature review. Can J Occup Ther. (2004) ;71: (4):210–22. doi: 10.1177/000841740407100406 |
[35] | Bidzan M , Koszewska A , Bieleninik Ł . The quality of life of the parents of a child with Rubinstein-Taybi syndrome. Acta Neuropsychol. (2021) ;11: (1):53–76. |
[36] | De Gaetano K , Saviola D , Brunetti D , De Tanti A . The importance of assessing parent stress in families with children with severe neuromotor and intellectual disability - a pilot study. Appl Neuropsychol Child. (2022) ;11: (4):804–810. doi: 10.1080/21622965.2021.1971525 |
[37] | Saviola D , Chiari M , Battagliola E , et al. Diagnostic work-up and rehabilitation of cerebral visual impairment in infancy: A case of epileptic perinatal encephalopathy due to KCNQ2-related channelopathy. J Pediatr Rehabil Med. (2018) ;11: (2):133–137. doi: 10.3233/PRM-170440-2 |
[38] | Bertelli B , Cremonesi P , Castagna MG , Belli PR . Imparare a leggere e scrivere con il metodo sillabico-Vol. 2: Attività di consolidamento delle sillabe CV (Vol. 2). Trento: Erickson; (2013) . |
[39] | Kozulin A , Lebeer J , Madella-Noja A , et al. Cognitive modifiability of children with developmental disabilities: a multicentre study using Feuerstein’s Instrumental Enrichment–Basic program. Res Dev Disabil. (2010) ;31: (2):551–9. doi: 10.1016/j.ridd.2009.12.001 |
[40] | Feuerstein R , Rand Y , Hoffman M , et al. Cognitive modifiability in retarded adolescents: effects of Instrumental Enrichment. Pediatr Rehabil. (2004) ;7: (1):20–9. doi: 10.1080/13638490310001655140-1 |
[41] | Bearzotti F , Tavano A , Fabbro F . Development of orofacial praxis of children from 4 to 8 years of age. Percept Mot Skills. (2007) ;104: (3 Pt 2):1355–66. doi: 10.2466/pms.104.4.1355-1366 |
[42] | Brizzolara D , Cipriani P , Chilosi AM , De Pasquale L . L’apprendimento del linguaggio scritto nei bambini con difficoltà di acquisizione del linguaggio orale: Continuità o discontinuità. Apprendimento e Patologia Neuropsichica nei primi anni di scuola. Modelli interpretativi della clinica. (1994) :124–35. |
[43] | Luzzatti C , Laiacona M , Allamano N , et al. Writing disorders in Italian aphasic patients. A multiple single-case study of dysgraphia in a language with shallow orthography. Brain. (1998) ;121: (Pt 9):1721–34. doi: 10.1093/brain/121.9.1721 |
[44] | Roehr B . American Psychiatric Association explains DSM-5. BMJ. (2013) ;346: :f3591. doi: 10.1136/bmj.f3591 |
[45] | American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-5), tr. it. Milano: Raffaello Cortina; (2014) . |
[46] | Yule W , Lockyer L , Noone A . The reliability and validity of the Goodenough-Harris drawing test. Br J Educ Psychol. (1967) ;37: (1):110–1. doi: 10.1111/j.2044-8279.1967.tb01906.x |
[47] | Oakland T , Dowling L . The Draw-a-Person Test: Validity Properties for Nonbiased Assessment. Learning Disabil Quart. (1983) ;6: (4):526–534. doi: 10.2307/1510541 |
[48] | Imuta K , Scarf D , Pharo H , Hayne H . Drawing a close to the use of human figure drawings as a projective measure of intelligence. PLoS One. (2013) ;8: (3):e58991. doi: 10.1371/journal.pone.0058991 |
[49] | Qu’d D , Schmitt LM , Leston A , et al. Behavioral and neuropsychiatric challenges across the lifespan in individuals with Rubinstein-Taybi syndrome. Front Genet. (2023) ;14: :1116–919. doi: 10.3389/fgene.2023.1116919 |
[50] | Awan N , Pearson E , Shelley L , Greenhill C , Tarver J , Waite J . The behavioral phenotype of Rubinstein-Taybi syndrome: A scoping review of the literature. Am J Med Genet A. (2022) ;188: (9):2536–2554. doi: 10.1002/ajmg.a.62867 |
[51] | Hennekam RC , Baselier AC , Beyaert E , et al. Psychological and speech studies in Rubinstein-Taybi syndrome. Am J Ment Retard. (1992) ;96: (6), 645–60. |
[52] | Lacombe D , Bloch-Zupan A , Bredrup C , et al. Diagnosis and management in Rubinstein-Taybi syndrome: first international consensus statement. J Med Genet. (2024) :jmg2023–109438. doi: . 10.1136/jmg-2023-109438 |
[53] | Taupiac E , Lacombe D , Thiébaut E , et al. Psychomotor, cognitive, and socio-emotional developmental profiles of children with Rubinstein-Taybi Syndrome and a severe intellectual disability. Journal of Intellectual & Developmental Disability. (2021) ;46: (1):80–89. doi: 10.3109/13668250.2020.1776455 |
[54] | Stella G , Biancardi A . Le difficoltà di lettura e scrittura: strategie per il recupero nel 1° ciclo della scuola elementare. Omega; (1994) . |
[55] | Trabacca A , Russo L . Children’s rare disease rehabilitation: from multidisciplinarity to the transdisciplinarity approach. Eur J Phys Rehabil Med. (2019) ;55: (1):136–137. doi: 10.23736/S1973-9087.17.04900-0 |
[56] | Saviola D , De Gaetano K , Galvani R , et al. Rehabilitation in a rare case of coffin-siris syndrome with major cognitive and behavioural disorders. J Pediatr Rehabil Med. (2021) ;14: (3):525–532. doi: 10.3233/PRM-200785 |
Notes
a In English, Language Assessment Test.
b Language Assessment Battery.
c Battery for the Evaluation of Dyslexia and Developmental Dysorthography-2.
d Battery for the Evaluation of Writing and Spelling Skills.
e Neuropsychological Evaluation Battery.
f Neuropsychological Evaluation Battery for Adolescence.




