Factors influencing caregiver buy-in to early intervention physical therapy
Abstract
OBJECTIVE:
The family-centered care framework of Early Intervention (EI) has shifted the focus toward caregiver engagement, but the underlying processes that build this are unknown. The aims of this study were 1) to describe the process of caregiver engagement in therapy and (2) to identify factors perceived to influence caregiver buy-in, confidence, and engagement in EI.
METHODS:
This preliminary descriptive study utilized quantitative questionnaires and qualitative semi-structured interviews of EI participants (23 caregivers and four physical therapists). Interviews were transcribed and theme coded until saturation was achieved and a concept map was developed.
RESULTS:
All caregivers believed that their children benefited from EI, that they were empowered and confident in caring for their children, and their quality of life improved based on the quantitative data. The qualitative data revealed that building a rapport and therapeutic relationship is the foundation to developing buy-in. Reciprocal communication is critical to the relationship and the buy-in. Caregiver knowledge and awareness of progress foster caregiver buy-in and confidence once the relationship is established.
CONCLUSION:
Improved understanding of the factors influencing the development of buy-in will provide a framework for the clinician to enhance caregiver buy-in. Enhanced buy-in may promote parental engagement and improved outcomes for the child and family.
1Introduction
Early identification and intervention services for infants under the age of three with or at risk for developmental delay are provided under Part C of the Individual with Disabilities Education Act. Given the neural plasticity that underlies the processes in development, Early Intervention (EI), including physical therapy, is widely advocated for children with developmental disorders [1]. However, based on a thorough high level systematic review, the limited literature examining the efficacy of pediatric physical therapy on the motor and cognitive development of high-risk infants that is available varies greatly [2]. Another systematic review suggested that the large variety of approaches studied in the literature may account for some of this inconsistency [3]. Further systematic analyses of the evidence reported the interventions that most benefit preterm infants (mimicking the intrauterine environment) differ from those that appear to most benefit children after term age (developmental programs), which may explain some of the variability of approaches reported in the literature [4, 5]. A 2016 systematic review specifically examining children with cerebral palsy (CP), the most widely treated population in pediatric physical therapy, concluded that the evidence regarding the impact of EI on motor development, while promising, remains inconclusive [6]. Interventions reported in this systematic review varied greatly; however, Neurodevelopmental Treatment (NDT) was the most commonly studied, and most of the studies also included a parental education component [6]. Other systematic reviews examining a more heterogeneous population of children with or at high risk for developmental delay did not support a beneficial effect of traditional physical therapy approaches, including NDT and Vojta [3, 4] on motor development, but concluded the impact on cognitive development is more promising [3]. Interestingly, a large retrospective exploratory study reported the intensity of EI, regardless of the discipline or interventions performed, is associated with increases in functional outcomes [7], which suggests EI is indeed effective and service providers should consider maximizing the intensity of treatment. As family-centered practices are an integral part of EI [8], the incorporation of parents within and outside of the treatment time is a logical and feasible approach to increase therapy intensity [9]. Consistent with this approach, the outcomes of EI motor training and general developmental programs in which parents learn how to promote infant development have historically been identified as the most promising within the literature [3, 4].
The family-centered care framework of EI has shifted focus toward parental engagement in EI, but the outcomes of this shift are inconclusive in the research [10]. Nevertheless, the efficacy of approaches that included active participation of the caregiver in the provision of therapies at improving motor, social, and language skills has been reported. For example, one case report described a caregiver-implemented and clinician-monitored constraint-induced movement therapy program that was associated with both quantitative and qualitative improvements in upper extremity function in an 18-month-old child with hemiplegia [11]. Another case report described a caregiver-implemented, clinician-monitored gait program using the “Upsee” that was associated with quantitative and qualitative improvements in gait as well as clinically significant changes in the Gross Motor Function Measure (GMFM)-66 [12]. Similarly, a larger cross-site randomized controlled trial examining a 12-week caregiver-mediated Social ABC program for children with autism reported significant increases in functional communication skills such as responsiveness and social initiation, as well as increases in language skills [13].
Although coaching is well-accepted in EI, the term is poorly defined [14]. “COPing with and CAring for infants with special needs” (COPCA) is a specific coaching program that targets the active participation of the caregivers and shows great promise according to a recent systematic review [15]. Caregivers who participate in COPCA report higher levels of confidence and empowerment carrying out interventions in the home with their child when compared to caregivers who do not receive coaching [16]. Coached caregivers also challenge their children more outside of therapy, as evidenced by specifically placing their child in more challenging positions during daily activities, which was associated with higher levels of functional independence according to a randomized controlled trial comparing families who were coached and those who received traditional infant therapy [17]. Higher levels of confidence in caregivers were positively correlated with higher motor performance in children as measured by the GMFM according to a cross-sectional exploratory analysis of families with children with CP [18]. Direct evidence from two empirical controlled trials reported that coaching results in significant improvements with motor performance, and those improvements are greater than those seen in families provided with standard care [19, 20]. Taken together, these findings support the theory that coaching results in enhanced confidence and efficacy of the family and, in turn, enhanced motor development in the child.
While coaching can build caregiver confidence and change caregiver engagement in and outside of therapy, the underlying process that builds that confidence and engagement is unknown. Therapeutic alliance is a working relationship between the patient and therapist, which has been linked to engagement in stroke rehabilitation and treatment outcomes in cardiac and musculoskeletal populations [21–25]. Therapeutic alliance, however, has not been examined in EI. The aims of this study were 1) to describe the process of caregiver engagement in therapy and (2) to identify factors perceived to influence caregiver buy-in (therapeutic alliance), confidence, and engagement in EI.
2Methods
2.1Design
This preliminary descriptive study was approved by the Shenandoah University Institutional Review Board (IRB #945). There were no conflicts of interest. The quantitative portion of the study included a questionnaire that was created with Qualtrics software (Qualtrics XM, Provo, UT) and administered to participating caregivers. The qualitative portion utilized a grounded theory approach to explore the development of caregiver buy-in to EI physical therapy services. Therefore, a hypothesis was not initially determined in order to allow a theory to develop from the collected data from the participants. For the qualitative portion of the study, semi-structured interviews between researchers and caregivers or physical therapists (PTs) were conducted over Zoom conference calling (Zoom Video Communication, San Jose, CA).
2.2Participants
The researchers used a convenience sample of caregivers of children who received or were currently receiving EI physical therapy services in the region. The regional EI agency provides services to nearly 400 families who live across 1,125 square miles in five rural counties. Families from this database who received at least three months of EI physical therapy services within the past two years were recruited via email or mail, depending on their access to the internet. A total of 55 caregivers were invited to participate in the study. In order to protect the privacy of the families receiving EI, the questionnaires were sent directly from the EI agency. Thus, no personal identification information was provided to the researchers unless the families agreed to provide it for participation in an interview. A total of 27 caregivers completed the questionnaire, reflecting a 49.1% response rate. Caregivers were asked if they would be willing to participate in a follow-up interview with the researchers. Based on availability, the researchers were able to conduct interviews with four caregivers. Two additional caregivers who did not participate in the original survey agreed to participate in interviews. In order to triangulate the data, the researchers also collected data from PTs using a convenience sample. A questionnaire was sent to two PTs who provided EI physical therapy services to the children of all the caregivers who were recruited. In addition to these two therapists, two additional PTs practicing in EI in the region participated in semi-structured interviews.
2.3Procedures
2.3.1Questionnaire development and distribution
The caregiver questionnaire was developed by the researchers to collect information from caregivers regarding their demographics and experience with EI physical therapy services. The guiding questions for the questionnaire were 1) What are caregiver perceptions on the effectiveness of EI?; 2) What is the level of caregiver engagement in EI?; 3) What is the level of caregiver confidence and comfort with EI interventions?; and 4) What are the factors influencing engagement, confidence, and comfort with EI interventions? Likert items were intentionally worded positively in order to decrease threats to validity and reliability [26]. Also consistent with literature on questionnaire development, midpoints were not included in the Likert items as it was expected that the respondents would have an opinion of EI and to minimize inaccurate perceptions of neutral or use of this choice due to lack of familiarity [27]. Prior to distribution, the questionnaires were sent to two individuals with experience providing physical therapy through EI and two individuals with experience in questionnaire development and analysis. Items were revised based on their feedback. There were 45 items in the final questionnaire focused on the caregiver’s perceptions of their child’s EI physical therapy experience and their level of participation and buy-in with their child’s EI (Appendix A).
2.3.2Interview design and implementation
Semi-structured interviews were conducted between two researchers and one participant using password-protected Zoom conference calling (Zoom Video Communication, San Jose, CA) based on guiding questions (Appendix B), which were presented in an open-ended format. Interviewers used these questions to facilitate a discussion of the participant’s experiences with EI and perspectives on caregiver buy-in. Once each interview was complete and the participant had left the session, the two researchers participated in peer debriefing, including a discussion of the main ideas and insights from the interview. Immediate interpretations of the verbal and non-verbal observations (such as how important concepts were to participants) were discussed in this peer debriefing to enhance trustworthiness of the findings. All interviews were recorded then transcribed verbatim. The transcription document was then audited by two researchers who did not do the transcription to ensure accuracy and trustworthiness of the data. All interview transcripts were sent to participants for member checking to ensure accuracy of the data.
2.4Data analysis
Quantitative data from the questionnaires were analyzed using SPSS Statistics Software version 28 (IBM, Armonk, NY). Qualitative data were analyzed by two independent researchers to identify and organize themes using an inductive approach to thematic analysis [28, 29]. Specifically, after an initial review of the transcription, each researcher generated initial codes based on the participant’s quotes as well as the researcher’s interpretation. Each researcher was blinded to initial codes developed by the other researcher. To further minimize bias and enhance trustworthiness, this initial coding was performed by researchers who had no experience with school-based physical therapy or telehealth. The researchers then had a consensus meeting to determine the preliminary codes in the context of the literature and the guiding questions of the study. Consistent with the constructivist grounded theory approach, this iterative comparative analysis was utilized to enhance theoretical sensitivity [30, 31]. The analysis resolved coding discrepancies and identified quotes that did not fit into the current codes in order to identify new potential codes. Once coding was determined, all interview data were analyzed by the two independent investigators to develop themes from those codes as described by Charmaz [32] and others [33]. Themes were chosen based on the commonality of the responses as well. As themes emerged, response codes were reassigned into the theme that best represented the code. This process continued until saturation was reached and no new themes emerged, which occurred after three PT interviews and after five caregiver interviews [34]. Exemplar quotes were selected from transcripts to represent each individual code. A concept map was developed by all the investigators through several consensus meetings to discuss the emergent themes and their relationships.
3Results
3.1Quantitative findings from the questionnaires
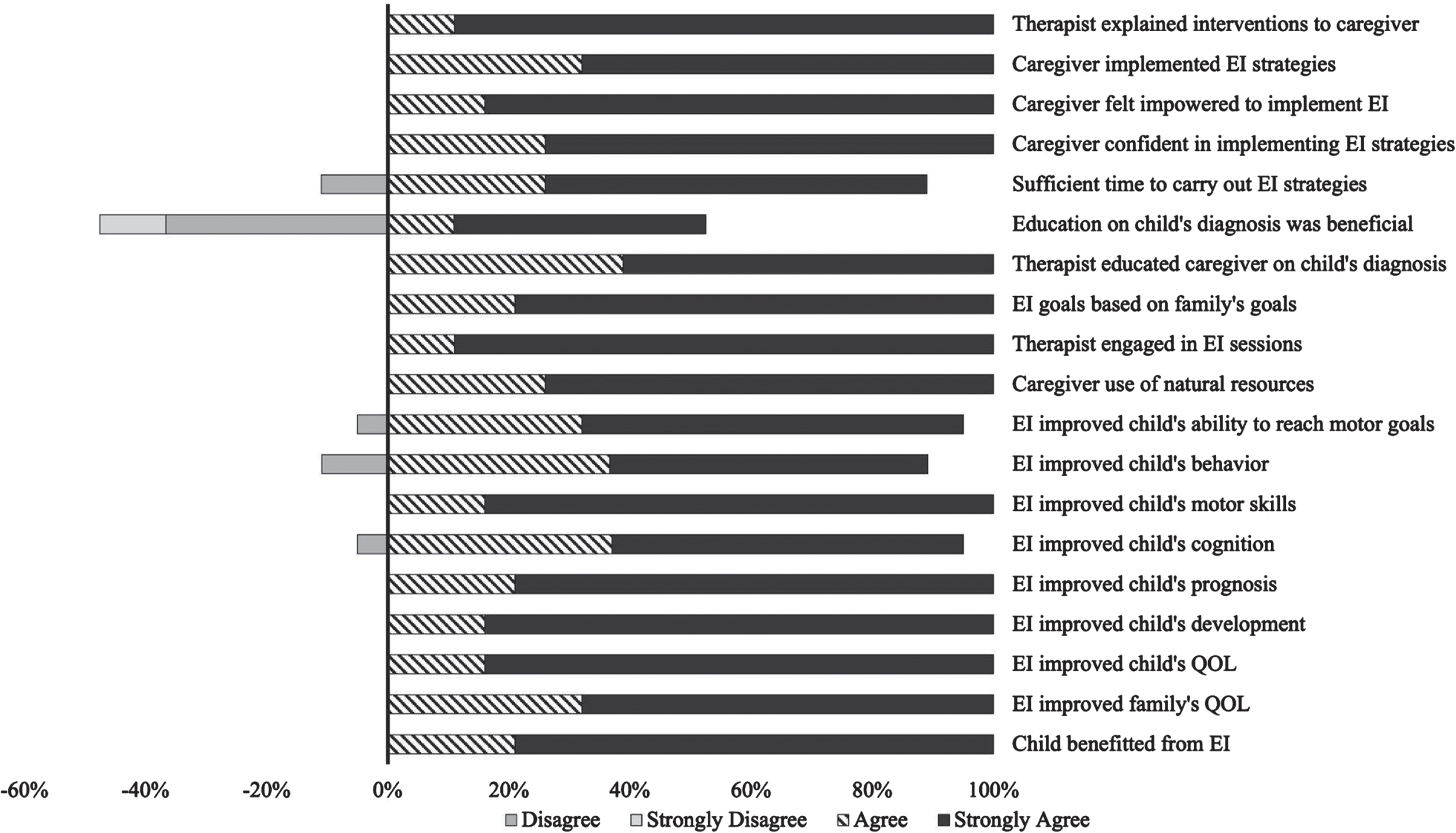
Descriptive statistics from the caregiver data collected through the questionnaires are presented in Table 1. The results from the caregiver questionnaires regarding their perception and experience with EI physical therapy are presented in Table 2 and Fig. 1. All of the caregivers said they felt comfortable incorporating strategies provided by the PT into their child’s routine either immediately (80%) or after a few sessions (20%). Regarding caregivers’ implementation of EI strategies, 42.1% incorporated them more than three times per week, 26.3% incorporated them 2–3 times per week, and 31.6% incorporated them less than or equal to once per week. While there is variability in these results, variability and custom treatment plans implemented by the clinicians were recognized. The two most common reasons for the caregivers continuing EI physical therapy activities outside of sessions was improvement noted with the child (25.8%) and the ability for them to incorporate them into their daily routine (25.8%). All of the caregivers felt that EI physical therapy services had benefited their child and improved quality of life. Likewise, all of the caregivers felt empowered in caring for their child from experiences with EI physical therapy services and that they had the appropriate resources to do so. All caregivers also felt that EI physical therapy services were based on their family’s goals and that their family’s quality of life was improved. When asked about the caregivers’ knowledge of their child’s diagnosis and its impact on their ability to continue physical therapy activities outside of sessions, 47% said it had no impact. All but one caregiver (95%) believed that their child had cognitively improved due to EI physical therapy services. Similarly, all but two caregivers felt that their child’s behavior had positively changed due to EI physical therapy services.
Table 1
Child and family information from quantitative data
| Caregiver age (mean (SD), years) | 32.3 (7.2) | Referral source for EI (n (%)) | |
| Pediatrician | 14 (51.8) | ||
| Self | 7 (25.9) | ||
| Service length (mean (SD), months) | 16.1 (9.9) | Other (Neurologist, NICU, FP, DSS) | 6 (22.2) |
| Services received within EI other than PT (n (%)) | |||
| Family composition (mean (SD)) | OT | 16 (59.2) | |
| #of caregivers | 2.0 (0.7) | SLP | 9 (33.3) |
| #of children | 2.0 (1.6) | Devel. spec. | 8 (29.0)) |
| Neurology | 10 (37.0) | ||
| Relationship to child (n (%)) | Cardiology | 5 (18.5) | |
| Parent | 18 (66.7) | Orthopedics | 7 (25.9) |
| Foster parent | 3 (11.0)) | Othera | 7 (25.9) |
| Grandparent | 3 (11.0) | ||
| Caregiver experience with services received for children outside of EI (n (%)) | |||
| Education (n (%)) | PT | 9 (33.3) | |
| Bachelor’s degree or above | 11 (40.7) | OT | 8 (29.6) |
| SLP | 6 (22.2) | ||
| Marital status (n (%)) | Otherb | 3 (11.1) | |
| Married | 19 (70.3) | No services | 8 (29.6) |
| Unmarried | 7 (25.9) | ||
| Other | 1 (3.7) | ||
| Caregiver experience with services for self (n (%)) | |||
| Household annual income (n (%)) | PT | 5 (18.5) | |
| Less than $24,999 | 7 (25.9) | OT | 3 (11.1) |
| $25,000–49,999 | 7 (25.9) | SLP | 2 (7.4) |
| $50,000 – 99,999 | 9 (33.3) | Other (nutrition) | 1 (4.8) |
| More than $100,000 | 4 (14.8) | No services | 14 (3.7) |
Devel. Spec.: developmental specialist, DSS: Department of Social Services, EI: early intervention, FP: Family practice, NICU: Neonatal Intensive Care Unit, PT: physical therapy, OT: occupational therapy, SD: standard deviation, SLP: speech language pathology. Other services received in EI included hearing, ophthalmology, gastrointestinal, applied behavioral analysis (ABA) therapy, allergist care, pulmonology, nutrition. b. Other services outside of EI: ABA, constraint-induced movement therapy.
Table 2
Quantitative findings from the caregiver questionnaires
| Caregiver responses | n (%) | Caregiver responses | n (%) |
| Immediacy of confidence in EI | Influential factors for EI discontinuation | ||
| Strategies | Child turned three years old | 5 (22.7) | |
| Immediately | 15 (80.0) | Child’s goals accomplished | 3 (13.6) |
| After a few sessions | 4 (20.0) | Child still receiving services | 10 (45.5) |
| Otherb | 3 (13.6) | ||
| Degree of confidence in EI strategies (0–10) | |||
| 10 | 10 (53.0) | Influential factors for EI continuation | |
| 9 | 3 (16.0) | Child improvement | 17 (25.8) |
| 8 | 4 (21.0) | Child enjoyed activities | 11 (16.7) |
| 7 | 1 (5.0) | Family enjoyed activities | 6 (9.0) |
| 6 | 1 (5.0) | Incorporation into daily activities | 17 (25.8) |
| Confident in performing activities | 15 (22.7) | ||
| PT strategies in EI | |||
| Stepping/crawling | 13 (68.4) | Recommendation for EI improvement | |
| Tummy time | 10 (52.6) | Increase hands on/in person | 7 (36.8) |
| Stretches | 6 (31.6) | Extend past three years of age | 2 (10.5) |
| Equipment use | 6 (31.6) | Otherc | 2 (10.5) |
| Sitting/sit to stands | 5 (26.3) | No changes | 7 (36.8) |
| Joint compressions | 5 (26.3) | ||
| Othera | 15 (78.9) | ||
| Caregiver implementation of EI | Influential factors to buy-in | ||
| Strategies | Child improvement | 15 (83.3) | |
| > 3x times per day | 8 (42.1) | Child reaching milestones | 4 (22.2) |
| 2–3 times per day | 5 (26.3) | Child achieving goals | 3 (16.7) |
| < 1 time per day | 6 (31.6) |
a. handling, encouraging arm use, balance activities, posture, orthotic use. b. too busy, lack of improvement. c. more time, more visits, shorter visits. EI: early intervention, PT: physical therapy.
Fig. 1
Caregiver Perspectives on Early Intervention (EI) from Questionnaire. The bars represent the percentage of caregivers who agreed or disagreed with the Likert statements. Bars to the left of 0% reflect disagreement and bars to right reflect agreement. QOL: quality of life.
3.2Qualitative findings from interviews
The demographics of the PT and caregiver interview participants are presented in Table 3. In the interviews, caregivers discussed their experiences with EI physical therapy services and its impact on their child. Clinicians reflected on their perceptions of caregiver buy-in and the factors influencing buy-in, including the strategies they used to foster it. The following themes emerged from the caregiver and clinician interviews: building rapport to create a relationship, approaches to promote buy-in, and gaining confidence. Exemplar quotes supporting the themes and codes that emerged are presented in Table 4.
Table 3
Caregiver and physical therapist interview participant characteristics
| Caregiver | Relationship to Child | Children in Home | Caregivers in Home | Child’s Diagnosis | Outside Employment | Confidencea | Benefits of EIb | Knowledge Engagementb | ||
| Caregiver 1 | Mother | 2 | 2 | Seizures, frontotemporal hemorrhage | Yes | 10 | 3.8 | 3.5 | ||
| Caregiver 2 | Foster Mother | 3 | 2 | Prematurity, substance exposure | Yes | 9 | 3.9 | 3.4 | ||
| Caregiver 3 | Mother | 6 | 2 | Prematurity | No | 10 | 3.8 | 3.7 | ||
| Caregiver 4 | Mother | 3 | 2 | Prematurity, torticollis | Yes | 10 | 3.9 | 3.7 | ||
| Caregiver 5 | Mother | 2 | 2 | Joubert sensorineural hearing loss | No | 8 | 3.8 | 3.5 | ||
| Caregiver 6 | Mother | 4 | 2 | Hypotonia | No | 9 | 3.9 | 3.7 | ||
| Therapist | Age | Gender | Marital Status | Household Income | Parent (#)c | Highest PT Degree | Highest Degree Earned | Years EI | Years PT | % Caregiver Buy-Ind |
| Therapist 1 | 33 | Female | Single | $50,000–90,000 | 3 | DPT | DPT | 9 | 9 | 55 |
| Therapist 2 | 30 | Female | Married | > $100,000 | 2 | DPT | DPT | 5 | 6 | 60 |
| Therapist 3 | No Answer | Female | Married | No Answer | 2 | Unknown | Unknown | 27 | 35 | 75 |
| Therapist 4 | 26 | Female | Single | $50,000–90,000 | 0 | DPT | DPT | < < 1 | 2 | 70 |
a. Confidence incorporating PT into daily routines (0–10: no confidence-extremely confident) from questionnaire, b. Mean caregiver perception (0–4: strongly disagree-strongly agree) on the benefits of EI and their knowledge and engagement, respectively, from questionnaire, c. Refers to the number of children the therapist had as a parent, d. Therapist perception of the percentage of families that buy-in to EI, EI: Early Intervention, DPT: Doctor of Physical Therapy, PT: physical therapy.
Table 4
Qualitative findings from caregiver questionnaire
| Theme: Building rapport to create a positive relationship | |
| Quote | Code |
| “[Being compassionate and understanding meant, more than anything because [The PT] being compassionate..helps me to understand a lot of stuff. [Our PT] always cared about what he felt and how he was.” - Caregiver 1 | Appreciation and understanding |
| “I had a child walk in [in] just his underwear and she’s like it’s fine I have kids like it happens all the time, like there was no judgment.”-Caregiver 2 | |
| “I wasn’t a mom but I had a lot of baby experience because I babysat all the time. I think my expectations were very high of the families and then, as I became a mother and had young children of my own I realized whoa, ‘I’m asking these families to do something that they probably just don’t have time in a day to do’. My expectations for what I expected of them change significantly over time and.” - Therapist 3 | |
| “[Our PT] made it simple enough for me to understand so I could continue when she left. [Others] would speak in Dr jargon what have you and I’m like ‘I don’t know what the heck you just said, you’re gonna have to dumb it down for me’. But with her, I never had to worry about that, because she was always telling me.. this is how we can do it from here, you guys can add other things to continue when I’m gone. So she made it simple enough for me to understand.” - Caregiver 1 | Communication |
| “I think that when you talk to them in layman’s term.. you talk to them..at their level then they don’t feel like you’re looking down on them and your are one on one and you’re. straight talking like ‘buddy you know we can just shoot the breeze”’ - Caregiver 3 | |
| “[The PT] came into our home and [Our PT] just dove right in. [The PT] took her shoes off and jumped down on the floor.” - Caregiver 4 | Comfort |
| “He would get so frustrated and [the PT] would get down on the floor with him and would be like ‘it is OK, we can try and try again until we get it right.’ And he would stop getting upset and he would be ready to do it again.” - Caregiver 1 | Patience |
| “[Our PT] was always open to answering any question. You know what the next steps are, what should we do in this situation, she was always very open and honest about all of them.” - Caregiver 5 | Approachability |
| “We talk about what the coaching model is and what it’s going to look like and what their responsibility is in that coaching style. [So when we’re there [only] once a week every other week once a month, whatever it might be. we’re not able to make progress on a day to day basis, unless [the family carries] it over and I think once you explain that to them.”- Therapist 3 | Shared responsibility |
| “So if I had a question, [the PT would answer and also show me] how to do it have him do it, and then show ways to either help hold.. and then ways to extend like ‘oh he’s getting good at this we can extend that by putting an obstacle in his path or by making the surface a little bit less steady”’ - Caregiver 6 | |
| Theme: Approaches that promote buy-in | |
| Quote | Code |
| “We go over.. what services and what types of things our program can provide and what the concerns of the parents are because ultimately that’s the biggest thing. Early intervention is addressing the concerns that the family has. [It] doesn’t always have to be the numbers or the things that are written down on the page” - Therapist 4 | Patient and family centere |
| “I wanted someone to be as focused on him and about him. If, you know, if this was going to be therapy for him, it needed to be all about him because she actually focused on him and talked to him. She would always ask what were some things that we thought or we felt that he needed to work on.” - Caregiver 1 | |
| “[the PT said] we’ll never push her and never make her do anything more than what her body was ready to do, and she just really made me feel comfortable that way.” -Caregiver 4 | Coaching |
| “When I first started, we weren’t really doing a coaching model, it was much more a medical model like we just did it all for them. And I do really believe in the coaching style and I actually do believe in families. Once they learn how to do it and they can have the same result that I have, it just empowers them and they feel so great that they can make a difference and they don’t have to just wait for somebody to do it for them.” -Caregiver 3 | Integration into daily routine |
| “Absolutely every time we have time on the ground we do things [with her to help her progress]. Every time that we’re in her high chair there are different variations that our PT.. gave us so it’s not always on the floor all the time.. When we’re giving her a bath or she’s in her high chair eating or she’s doing different things, [the PT gae us ways to] not make it so mundane.. You know, [if we are] always doing it and [doing it] throughout the day is what she is trying to push.”- Caregiver 5 | |
| “We really work on things that they normally do in their daily lives but [the families] don’t think about. [I show them]... ways they can tweak it a little bit to make it purposeful play.” -Therapist 4 | Demonstration and feedback |
| “When [the PT] was demonstrating she was fully hands on with the twins. And I would watch to see what she’s doing. And then she would have me make sure that I was doing it properly, and [the key was] hands on.” - Caregiver 3 | Relaying progress and observations |
| “So it needs to really be brought to the light by the therapist to say ‘look, last week he only did it three times and today you just did it seven’ for them to really, really bring it out and bring their attention to that too. [The PT] would definitely say ‘Oh, my goodness, you know he wasn’t able to do that for more than you know, three minutes and now look he’s doing this’... This was [so important] for me to see”- Caregiver 3 | |
| “Every time [the PT] comes in she [says things] like ‘I can’t believe that she’ll pass toys from one hand to another, with the new sounds that she’s making or..that she’s doing things that and two weeks ago with it too much you wanted to do.” - Caregiver 5 | Explanation |
| “[We use] the early learning profile,... [which] addresses all the families’ concerns. [The family gets] a big report [detailing] everything their child isn’t isn’t doing at their age level compared to peers of the same age so they know.. what’s going on with their child.. And then we have the IFSP meeting so all of that is..reiterated. [The families [get] the same speech over and over,.. so I don’t always have to go in and explain why [something is happening.” - Therapist 1 | Reinforcement |
| “With telehealth. I started [following] up after visits and sending them.. recaps, because [the families were likely] overwhelmed with what just happened over zoom and I couldn’t do hand over hand assistance [and] I felt like I had to compensate a little bit [but now] I’ve just stuck to doing that, even though we’re in person” - Therapist 2 | |
| “Our physical therapist that we worked with was absolutely wonderful and sending follow up afterwards and asking any questions, very encouraging and great at demonstrating things, but then also to see if there was anything that I had trouble with. “ - Caregiver 2 | |
| Theme: Gaining Confidence | |
| Quote | Code |
| “When I started seeing him do the things by himself without being prompted, without being asked, when he had more mobility, when he would start running and and I knew she was getting to him when he was doing the things without being asked, or he would bring me things [and say things like], ‘let’s throw the ball today mommy.’ “-Caregiver 1 | Importance of progress |
| “The day that I watched my daughter roll over for the first time. Oh, [that is when] I bought in. I tear up [as a] mother, now that was the day that I was like ‘this is really going to help her’. I never thought it was going to happen and when she finally did that I [saw it as] a sign that we need to keep going, because if she can do this, then she can do anything as long as we just continue on and just be open and just try our best.”- Caregiver 5 | |
| “When the families understand what we are doing and why we are doing it, things happen. When I hear families [say] ‘I came up with a new way to get him to pull up to stand’ or ‘look at the game we came up with to use his right hand’, I know I did it. The families will only follow through when they think it really matters and they do it [better] when they get the reasoning behind it” -Therapist 2 | Caregiver knowledge |
| “I feel like.. having somebody else out of the box brings in perspective and.. it works..I have seven children and a lot of them have gone through [EI} and I am such an advocate of it.” – Caregiver 3 | Validation |
Strategies including explanation, coaching, reinforcement, integration into daily routines, being family-centered, providing feedback, and relating progress were utilized by the therapists to develop rapport with the families. This involved open communication, idea sharing, shared responsibility, comfort, appreciation, patience and approachability, which helped build the relationship between the therapist and the family and was the foundation for developing caregiver buy-in. Once this foundational relationship was established, validation, gaining knowledge and seeing child progress enhanced the caregiver’s confidence, which promoted buy-in and continued confidence. With caregiver buy-in came further confidence leading to more buy-in and the continuation of this virtuous cycle. These relationships are depicted in the concept map (Fig. 2).
Fig. 2
The concept map depicting qualitative themes and their relationships. Several strategies were utilized by the therapists which developed rapport with the families. This rapport helped build the relationship between the therapist and the family, which was the foundation for developing caregiver buy-in. Once this foundational relationship was established, validation, gaining knowledge and seeing child progress enhanced the caregiver’s confidence which promoted buy-in and continued confidence.

3.2.1Theme: Building a rapport to create a relationship
Caregivers and clinicians expressed the importance of building a rapport to create a relationship between the clinician and the family which served as the foundation for developing buy-in. The quality of communication appeared to greatly impact the development of rapport. From the caregiver perspective, conveying information in a relatable manner helped them to better understand the reasoning and purpose of interventions and considerations. Furthermore, clinician understanding and appreciation of the family’s concerns and situation appeared to be essential to the building of rapport. This empathy ultimately enhanced the relationship between the clinician and the family.From the clinician perspective, experience as a parent appeared to help them set more realistic expectations of the families and build a better understanding of the family situation. Clinician experience as a parent also served to validate the clinician to the caregiver. The PT’s comfort level in the home as well as their patience seemed to bring more comfort to the family, build rapport and strengthen the relationship between the family and the therapist. The approachability of the therapist and willingness to answer questions and discuss concerns also emerged as a critical element in the development of rapport. In a similar light, the importance of idea sharing between the therapist and family fostered mutual respect which strengthened the relationship further. In addition to the sharing of ideas, the sharing of responsibility for the implementation of interventions, including carryover between sessions by the caregiver, served to enhance the development of the therapeutic relationship. The sharing of ideas and responsibility emerged through the clinician’s perspective as part of the coaching model and from the caregiver’s perspective as both a reflection of respect for the caregiver’s ideas as well as a source of empowerment for the caregiver.
3.2.2Theme: Approaches that promote buy-in
Both caregiver and clinician participants relayed several approaches that were utilized by the PTs in EI that promoted the development of caregiver buy-in. The patient-/family-centered approach in EI was widely perceived to have the most impact on the development of buy-in. From the clinician perspective, this was expressed through prioritizing the family concerns, while the caregivers relayed that the focus of the PT was on the child and not outside factors or logistical issues. When the PTs responded to and prioritized the family’s concerns and questions, the relationship was strengthened, trust grew, and buy-in resulted. Incorporating the coaching approach allowed the family/child to be even more centered in the process, resulting in empowerment of the family. This empowerment appeared to result in the family taking on more responsibility for care in between sessions. Consistent with the family-centered approach, integrating activities into the family’s daily routine emerged as a strategy that was perceived to enhance carryover and buy-in. Both caregivers and therapists relayed examples of integrating therapy into play and other daily routines as well as making feasible modifications to daily activities that would promote therapeutic goals. The participants also expressed that demonstration with feedback and explanation enhanced caregiver confidence and understanding of the therapeutic activities. Specifically, therapists relayed the importance of explaining the reasoning behind interventions and activities while caregivers reported they were better able to implement the recommendations when they understood the reasoning behind the activity or intervention. These strategies further supported the importance of communication in the development of buy-in. Clinician and caregiver participants also considered reminders and follow-ups as effective strategies used by clinicians to enhance caregiver buy-in. One of the benefits of the reminders and follow-ups was the provision of reinforcement of the family/child’s progress that caregivers reported helped to further build their confidence. Reinforcement of findings across disciplines and consistency of communications including review of the Individualized Family Service Plan were additional types of reinforcement considered as promoters of the development of buy-in. Clear communication of child progress and observations were noted as specific content that enhanced caregiver understanding. Therapists reported that they did this intentionally while caregivers reported that hearing the therapist’s observations, including those of the child’s progress, helped the caregiver to understand what the therapy was focusing on and that the therapy was actually effective. This enhanced understanding ultimately contributed to caregiver buy-in.
3.2.3Theme: Gaining confidence
Both clinician and caregiver confidence were deemed critical in the development of buy-in once the relationship was formed. Therapists expressed that they specifically implemented strategies to enhance caregiver confidence and family competence. The explicit communication of progress emerged as an effective strategy for developing buy-in. The progress itself helped to build the caregiver’s confidence in themselves and in the physical therapy. Caregivers reported that the observations of progress validated their ability and efficacy in following through with therapy. In addition, having knowledge of the processes involved in EI as well as the underlying reasoning for the therapeutic interventions contributed greatly to the caregiver’s confidence in themselves and in the efficacy of EI. Finally, the caregivers viewed having the outside perspective of the therapist as validation for the caregiver, which promoted their confidence further.
4Discussion
This study examined the development of caregiver buy-in to physical therapy in the EI setting. The quantitative portion of the study overwhelmingly supported the perception of EI efficacy for the child and family for this sample as well as the development of family empowerment, family engagement and buy-in through EI. The process and factors involved in the development of this strong buy-in emerged in the qualitative portion of the study. The development of a therapeutic relationship through the building of rapport between the caregiver and the therapist was considered foundational for the development of buy-in (Fig. 2). The quality, nature and amount of communication was deemed critical along with a family-centered approach with an appreciation of and integration of the family’s daily routine. Ultimately, the caregivers experienced an increase in confidence that fostered buy-in. A virtuous cycle of reinforcement then occurred between caregiver confidence and buy-in.
The therapeutic relationship described in the present study involved the development of a social connection through an appreciation of the family situation and a mutual comfort level between the clinician and the family. The relationship described in the present study is consistent with the therapeutic alliance described in the literature. Psychology literature describes this alliance as involving a working relationship and social connection [35]. A meta-analysis examining the therapeutic relationship in psychotherapy in 53 studies found that empathy and genuineness were moderately correlated with therapeutic alliance [36]. In the present study, empathy emerged as an understanding of the family’s situation including their challenges. The parental context including the busy family life and having multiple children has been proposed as a primary factor in low parental adherence in EI [37]. The results of the present study suggested that this contextual understanding of the family situation was enhanced by the therapist’s own experience as a parent, which served to further validate the therapist to the caregivers and build caregiver trust. Recent studies on the experiences of parents with high-risk children transitioning from the neonatal unit to EI services emphasize the importance of trust and authenticity throughout the continuum of care [37, 38]. Related to the appreciation of the family situation and contexts, utilizing a family-centered approach and integration therapy in the daily routine of the family enhanced the relationship and alliance. An improvement in family quality of life is associated with family empowerment, which may improve the parent-child interaction. In the long term, this will positively influence child development [16, 39, 40]. The incorporation of therapy into the daily routines of the family along with the clinician’s appreciation of the family situation reported in the present study reflected a family-centered approach. Participants believed this incorporation into daily routines promoted buy-in by highlighting the meaningfulness of the interventions, considering the busy schedules of the families and providing opportunities for families to note developmental changes in their everyday lives. Preliminary literature supports the efficacy of parental incorporation of treatment into their daily routines in the development of motor exploratory problem-solving skills in infants [41]. Given that the present study found that incorporating treatment into daily routines was perceived to promote buy-in, it can be hypothesized that caregiver buy-in contributes to the improved outcomes reported in the literature.
The present study identified communication and interpersonal skills as critical to the development of the therapeutic relationship. Interestingly, none of the participants expressed that the technical skills of the therapist impacted the relationship and ultimately buy-in. The literature has reported similar findings in an older pediatric population; specifically, the therapist’s trust and relational skills were considered more important than technical skills, speaking to the importance of therapeutic alliance in pediatric rehabilitation [42]. In the EI setting, the therapeutic relationship with the caregiver is even more critical. The participants in the present study emphasized the importance of communication in a relatable manner as critical to building rapport and caregiver understanding. The literature supports that communication at an appropriate level can improve parent receptiveness and learning [41, 43–45]. Given that gaining knowledge was seen as essential in the process of developing buy-in in the present study, the importance of communicating in an understandable manner is paramount for the family. In addition, the nature of the communication provided impacted the development of buy-in. Participants described demonstration and feedback as two critical types of communication. The feedback provided by the therapist served to encourage the caregivers and foster confidence in the caregivers. Without this feedback, caregivers were unsure of their ability to follow through with therapeutic recommendations and were therefore less likely to do so. Feedback not only supported the ability of the caregivers to follow through but also reinforced the caregiver’s observations. Supporting the parent’s sensitivity to infant behaviors and other observations has been shown to encourage the caregivers and further build the parental connection with the health care provider [37, 46].
Communication that is reciprocal in nature emerged as critical for the development of the therapeutic relationship and buy-in. The process of sharing ideas and responsibilities over time appeared to lead to feelings of respect and empowerment. Both therapists and caregivers expressed the importance of sharing therapeutic strategies and observations and receiving feedback on these ideas. Developing knowledge over time improved caregiver confidence in their abilities and observational skills leading to improved confidence and buy-in. However, knowledge alone did not appear to be sufficient in that both caregivers and therapists believed that the caregivers needed to have responsibilities to partake in the therapy to develop this confidence and buy-in. A similar perception has been reported in older pediatric populations in which both the parents and the children themselves have expressed the desire to contribute to the direction of therapy [40]. Other studies examining EI have emphasized the importance of collaboration, caregiver involvement and co-designing treatment [16, 37, 45, 47, 48]. However, the present study is the first one that has suggested that this sharing of responsibilities contributes to the therapeutic relationship and buy-in. Such collaboration between healthcare practitioners and their clients is also consistent with the coaching method described in the EI setting. A tenet of the coaching technique is caregiver engagement. Preliminary evidence suggests that such engagement can positively impact quality of life for the family and motor outcomes in the children [4, 17].
While the development of the therapeutic relationship between the therapist and caregiver sets the foundation, other factors were also considered essential to the ultimate development of caregiver confidence and buy-in. Building caregiver knowledge in the areas of development, resources and services instilled confidence in the caregivers in the present study, consistent with the parental responsiveness to education reported in the literature [6, 41, 44]. While many caregivers reported that their child’s progress enhanced the buy-in and promoted the caregiver engagement in therapy, the majority of participants also noted that therapist communication was needed to bring awareness of progress and to validate the progress observed. The therapists appeared to promote the caregiver’s ability to note small changes in the child’s abilities and motor function. The literature supports that celebrating goal achievement and observing positive change improves parental motivation and engagement, which will positively impact the child’s outcomes[37, 44, 47, 49]. Similarly, follow-up communication not only heightened caregiver awareness of the child’s progress and the expectations of the child and caregiver in between sessions, it also encouraged the caregivers by reinforcing their knowledge, abilities and impact on the child, further promoting caregiver confidence. This supports the importance of communication not only in the building of the therapeutic relationship but throughout the process of developing buy-in and caregiver confidence.
While the present study illuminated the importance of building a relationship, communication, knowledge and progress in the development of buy-in, the impact of this buy-in on child and family outcomes must be considered. A reciprocal connection between therapeutic relationship and functional outcomes has been reported across populations supporting the importance of the therapeutic relationship reported in the present study [21–25, 50].The present study found that the caregivers were able to implement the therapeutic strategies, suggesting parental engagement. However, parental engagement and efficacy were not directly measured. While it is hypothesized that there is a direct relationship between buy-in or therapeutic alliance, engagement and efficacy, the relationship should be investigated. The examination of therapeutic buy-in in EI on short and long term family and child outcomes is also warranted.
There are limitations to the present study that must be considered. Based on the quantitative findings, all caregivers reported strong buy-in and positive perceptions of the efficacy of EI. Therefore, a comparison of the EI process in those that did not develop buy-in was not possible. It may have been difficult to capture the caregivers who did not develop buy-in because they are theoretically more likely to discontinue services and less likely to respond to surveys. It also is possible that response bias resulted in the positive perception of EI. While there is evidence that presenting items in descending order as done in the present study could result in a primacy effect and therefore positive bias [51], there is also evidence that there is no difference in descending vs ascending ordered items [52]. Furthermore, because the questionnaires were sent directly from the EI agency, no personal identification information was given to the researchers unless the families agreed to provide it for participation in an interview. Therefore, the researchers had no information on those families who chose not to participate in the study. Nevertheless, the process involved in those that did develop buy-in emerged through the present study. While the sample size involved in the qualitative portion of the study was small, data saturation did occur, suggesting that the themes identified were comprehensive. It is conceivable that homogeneity of the sample contributed to the saturation in the small sample size. The present study also triangulated the data from caregivers and therapists, adding to the trustworthiness of this small sample.
5Conclusions
Based on the results of this preliminary investigation, the development of caregiver buy-in in EI appears to be a process that is built upon a strong therapeutic relationship between the therapist and caregiver. The nature and types of communication used by the therapist are thought to promote the rapport needed to build the relationship as well as the caregiver confidence associated with buy-in. The reciprocal nature of the communication and responsibilities of the therapist and caregiver seem to strengthen the relationship and result in increased caregiver confidence and buy-in. Explicit understanding of therapeutic goals and approaches along with awareness of progress appears to facilitate the development of buy-in and confidence once the therapeutic relationship has been built. Given that caregiver buy-in in EI can impact short and long term outcomes of the child and family, the implications of understanding the process involved in developing this buy-in can be far reaching.
Acknowledgments
We would like to recognize Corinne Wallis DPT for her assistance with data collection and analysis.
Conflict of interest
No funding was received from any organization for this work and there is no conflict of interest including financial, consultant, institutional, or relational.
Supplementary material
[1] The Appendix is available in the electronic version of this article: https://dx.doi.org/10.3233/PRM-230025.
References
[1] | Ulrich BD Opportunities for Early Intervention Based on Theory, Basic Neuroscience, and Clinical Science.. Phys Ther. (2010) ;90: (12):1868–80 doi: 10.2522/ptj.20100040 |
[2] | Spittle A , Orton J , Anderson PJ , Boyd R , Doyle LW Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev. (2015) ;2015: (11):CD005495. doi: 10.1002/14651858.cd005495.pub4 |
[3] | Blauw-Hospers C , Degraafpeters V , Dirks T , Bos A , Hadder-Algra M Does early intervention in infants at high risk for a developmental motor disorder improve motor and cognitive development? Neurosci Biobehav Rev. (2007) ;31: (8):1201–12 doi: 10.1016/j.neubiorev.2007.04.010 |
[4] | Blauw-Hospers CH , Hadders-Algra M A systematic review of the effects of early intervention on motor development. Dev Med Child Neurol. (2005) ;47: (6):421–32 doi: 10.1017/s0012162205000824 |
[5] | Hadders-Algra M Challenges and limitations in early intervention. Dev Med Child Neurol. (2011) ;53: (Suppl 4):52–5 doi: 10.1111/j.1469-8749.2011.04064.x |
[6] | Morgan C , Darrah J , Gordon AM , et al. Effectiveness of motor interventions in infants with cerebral palsy: a systematic review. Dev Med Child Neurol. (2016) ;58: (9):900–9 doi: 10.1111/dmcn.13105 |
[7] | McManus BM , Richardson Z , Schenkman M , Murphy N , Morrato EH Timing and Intensity of Early Intervention Service Use and Outcomes Among a Safety-Net Population of Children. JAMA Netw Open. (2019) ;2: (1):e187529. doi: 10.1001/jamanetworkopen.2018.7529 |
[8] | Dunst CJ , Espe-Sherwindt M Family Centered Practices in Early Childhood. In: Reichow B, Boyd BA, Barton EE, Odom SL, editors. Handbook of Early Childhood Special Education. Springer International Publishing Switzerland. 2016 doi: 10.1007/978-3-319-28492-7_3 |
[9] | Mahoney G , Perales F The role of parents in early motor intervention. Downs Syndr Res Pract.. (2006) ;10: (2):67–73. doi: 10.3104/reviews.307 |
[10] | Harniess PA , Gibbs D , Bezemer J , Purna Basu A Parental engagement in early intervention for infants with cerebral palsy—A realist synthesis. Child Care Health Dev. (2021) ;48: (3):359–77 10.1111/cch.12916 |
[11] | Fergus A , Buckler J , Farrell J , Isley M , McFarland M , Riley B Constraint-Induced Movement Therapy for a Child with Hemiparesis: A Case Report. Pediatr Phys Ther. (2008) ;20: (3):271–83. doi: 10.1097/pe0b013e318181e569 |
[12] | Fergus A A Novel Mobility Device to Improve Walking for a Child With Cerebral Palsy. Pediatr Phys Ther. (2017) ;29: (4):E1–E7 10.1097/pe0000000000000451 |
[13] | Brian JA , Smith IM , Zwaigenbaum L , Bryson SE Cross-site randomized control trial of the Social ABCs caregiver-mediated intervention for toddlers with autism spectrum disorder. Autism Res. (2017) ;10: (10):1700–11. doi: 10.1002/aur.1818 |
[14] | Ward R , Reynolds JE , Pieterse B , Elliott C , Boyd R , Miller L Utilisation of coaching practices in early intervention in children at risk of developmental disability/delay: a systematic review. Disabil Rehabil. (2019) ;42: (20):1–22. doi: 10.1080/09638288.2019.1581846 |
[15] | Dirks T , Hadders-Algra M The role of the family in intervention of infants at high risk of cerebral palsy: a systematic analysis. Dev Med Child Neurol. (2011) ;53: (Suppl 4):62–7. doi: 10.1111/j.1469-8749.2011.04067.x |
[16] | Hielkema T , Boxum AG , Hamer EG , et al. LEARN2MOVE 0–2 years, a randomized early intervention trial for infants at very high risk of cerebral palsy: family outcome and infant’s functional outcome. Disabil Rehabil. (2020) ;42: (26):3762–70. doi: 10.1080/09638288.2019.1610509 |
[17] | Dirks T , Hielkema T , Hamer EG , Reinders-Messelink HA , Hadders-Algra M Infant positioning in daily life may mediate associations between physiotherapy and child development—video-analysis of an early intervention RCT. Res Dev Disabil. (2016) ;53-54: 147–57. doi: 10.1016/j.ridd.2016.02.006 |
[18] | Pierce SR , Skorup J , Paremski AC , Prosser LA The Relationship between the Family Empowerment Scale and Gross Motor Function Measure-66 in Young Children with Cerebral Palsy. Child Care Health Dev. (2021) ;47: (1):.112–8. doi: 10.1111/cch.12807 |
[19] | Ziegler SA , von Rhein M , Meichtry A , Wirz M , Hielkema T , Hadders-Algra M The Coping with and Caring for Infants with Special Needs intervention was associated with improved motor development in preterm infants. Acta Paediatr. (2020) ;110: (4):1189–200. doi: 10.1111/apa.15619 |
[20] | Van Balen LC , Dijkstra LJ , Dirks T , Bos AF , Hadders-Algra M , Early Intervention and Postural Adjustments During Reaching in Infants at Risk of Cerebral Palsy. Pediatr Phys Ther. (2019) ;31: (2):175–83. doi: 10.1097/pe0000000000000585 |
[21] | Babatunde F , MacDermid J , MacIntyre N Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature. BMC Health Serv Res. (2017) ;17: (1):375. doi: 10.1186/s12913-017-2311-3 |
[22] | Lawton M , Haddock G , Conroy P , Sage K Therapeutic Alliances in Stroke Rehabilitation: A Meta-Ethnography. Arch Phys Med Rehabil. (2016) ;97: (11):1979–93. doi: 10.1016/j.apmr.2016.03.031 |
[23] | Burns JW , Evon D Common and specific process factors in cardiac rehabilitation: Independent and interactive effects of the working alliance and self-efficacy. Health Psychol. (2007) ;26: (6):684–92. doi: 10.1037/0278-6133.26.6.684 |
[24] | Ferreira PH , Ferreira ML , Maher CG , Refshauge KM , Latimer J , Adams RD The Therapeutic Alliance Between Clinicians and Patients Predicts Outcome in Chronic Low Back Pain. Phys Ther. (2012) ;93: (4):470–8. doi: 10.2522/ptj.20120137 |
[25] | Fuentes J , Armijo-Olivo S , Funabashi M , et al. Enhanced Therapeutic Alliance Modulates Pain Intensity and Muscle Pain Sensitivity in Patients With Chronic Low Back Pain An Experimental Controlled Study. Phys Ther. (2013) ;94: (4):477–89 doi: 10.2522/ptj.20130118 |
[26] | Chyung SY , Barkin JR , Shamsy JA Evidence-based survey design: The use of negatively worded items in surveys. Performance Improvement. (2018) ;57: (3):16–25. doi: 10.1002/pfi.21749 |
[27] | Chyung SY , Roberts K , Swanson I , Hankinson A Evidence-based survey design: The use of a midpoint on the Likert scale. Performance Improvement. (2017) ;56: (10):15–23. doi: 10.1002/pfi.21727 |
[28] | Braun V , Clarke V Using thematic analysis in psychology. Qualitative Research in Psychology. (2006) ;3: (2):77–101. doi: 10.1191/1478088706qp063oa |
[29] | Braun V , Clarke V Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf D, Sher KJ, editors. APA handbook of research methods in psychology, Vol. 2. Research designs: Quantitative, qualitative, neuropsychological, and biological (pp. 57–71). American Psychological Association; 2012. pp. 57-71. doi: 10.1037/13620-004 |
[30] | Birks M , Mills J Grounded Theory. 2nd ed. VitalSource;2015. |
[31] | Chun Tie Y , Birks M , Francis K Grounded Theory Research: A design framework for novice researchers.SAGE Open Med. (2019) ;7: :2050312118822927. doi: 10.1177/2050312118822927 |
[32] | Charmaz K Constructing Grounded Theory. 2nd ed. Sage Publications, Inc; 2019. |
[33] | Qureshi HA , Ünlü Z Beyond the paradigm conflicts: A four-step coding instrument for grounded theory. International Journal of Qualitative Methods. 2020:19. doi: 10.1177/1609406920928188 |
[34] | Guest G , MacQueen KM , Namey EE Applied Thematic Analysis. Los Angeles, CA: Sage; 2012. |
[35] | Joyce AS , Ogrodniczuk JS , Piper WE , McCallum M The alliance as mediator of expectancy effects in short-term individual therapy. J Consult Clin Psychol. (2003) ;71: (4):672–9. doi: 10.1037/0022-006x.71.4.672 |
[36] | Nienhuis JB , Owen J , Valentine JC , et al. Therapeutic alliance, empathy, and genuineness in individual adult psychotherapy: A meta-analytic review. Psychother Res. (2018) ;28: (4):593–605. doi: 10.1080/10503307.2016.1204023 |
[37] | Gibbs D , Harniess P , Crossley SL “The Constant by Our Side”—Mothers’ Experiences of Early Intervention Therapy Services for Infants With Emerging Signs of Complex Neurodevelopmental Difficulties. Infants & Young Children. (2019) ;32: (4):255–69. doi: 10.1097/iyc.0000000000000149 |
[38] | Ballantyne M , Bernardo S , Sozer A , et al. A whole new world: a qualitative investigation of parents’ experiences in transitioning their preterm child with cerebral palsy to developmental/rehabilitation services. Dev Neurorehabil. (2019) ;22: (2):87–97. doi: 10.1080/17518423.2018.1434698 |
[39] | Fergus A , Hartsook K , Smith J , Hale M , Kellar D A Novel Physical Therapy Learning Experience in Pediatrics Via Telehealth: A Qualitative Case Analysis. Journal of Physical Therapy Education. (2021) ;35: (2):159–67. doi: 10.1097/jte.0000000000000184 |
[40] | Guillamón N , Nieto R , Pousada M , et al. Quality of life and mental health among parents of children with cerebral palsy: the influence of self-efficacy and coping strategies. J Clin Nurs. (2013) ;22: (11-12):1579–90. doi: 10.1111/jocn.12124 |
[41] | Dusing SC , Tripathi T , Marcinowski EC , Thacker LR , Brown LF , Hendricks-Muñoz KD Supporting play exploration and early developmental intervention versus usual care to enhance development outcomes during the transition from the neonatal intensive care unit to home: a pilot randomized controlled trial. BMC Pediatr. (2018) ;18: (1):46. doi: 10.1186/s12887-018-1011-4 |
[42] | Crom A , Paap D , Wijma A , Dijkstra PU , Pool G Between the Lines: A Qualitative Phenomenological Analysis of the Therapeutic Alliance in Pediatric Physical Therapy. Phys Occup Ther Pediatr. (2020) ;40: (1):1–14. doi: 10.1080/01942638.2019.1610138 |
[43] | Basu AP , Pearse JE , Baggaley J , Watson RM , Rapley T Participatory design in the development of an early therapy intervention for perinatal stroke. BMC Pediatr. (2017) ;17: (1):33. doi: 10.1186/s12887-017-0797-9 |
[44] | Basu AP , Pearse J , Watson R , et al. Feasibility trial of an early therapy in perinatal stroke (eTIPS). BMC Neurol. (2018) ;18: (1):102. doi: 10.1186/s12883-018-1106-4 |
[45] | Morgan C , Novak I , Dale RC , Guzzetta A , Badawi N GAME (Goals - Activity - Motor Enrichment): protocol of a single blind randomised controlled trial of motor training, parent education and environmental enrichment for infants at high risk of cerebral palsy. BMC Neurol. (2014) ;14: 203. doi: 10.1186/s12883-014-0203-2 |
[46] | Holmström L , Eliasson AC , Almeida R , et al. Efficacy of the Small Step Program in a Randomized Controlled Trial for Infants under 12 Months Old at Risk of Cerebral Palsy (CP) and Other Neurological Disorders. J Clin Med. (2019) ;8: (7):1016. doi: 10.3390/jcm8071016 |
[47] | Eliasson AC , Holmström L , Aarne P , et al. Efficacy of the small step program in a randomised controlled trial for infants below age 12 months with clinical signs of CP; a study protocol. BMC Pediatr. (2016) ;16: (1):175. doi: 10.1186/s12887-016-0711-x |
[48] | Broggi MB , Sabatelli R Parental Perceptions of the Parent-Therapist Relationship: Effects on Outcomes of Early Intervention. Phys Occup Ther Pediatr. (2010) ;30: (3):234–47. doi: 10.3109/01942631003757602 |
[49] | Mattern-Baxter K , McNeil S , Mansoor JK Effects of Home-Based Locomotor Treadmill Training on Gross Motor Function in Young Children With Cerebral Palsy: A Quasi-Randomized Controlled Trial. Arch Phys Med Rehabil. (2013) ;94: (11):2061–7. doi: 10.1016/j.apmr.2013.05.012 |
[50] | Cole MB , McLean V Therapeutic Relationships Re-Defined. Occupational Therapy in Mental Health. (2003) ;19: (2):33–56. doi: 10.1300/j004v19n02_03 |
[51] | Weng LJ , Cheng CP Effects of response order on Likert-type scales. Educational and psychological measurement. (2000) ;60: (6):908–24. doi: 10.1177/00131640021970989 |
[52] | Hofmans J , Theuns P , Baekelandt S , Mairesse O , Schillewaert N , Cools W Bias and changes in perceived intensity of verbal qualifiers effected by scale orientation. Survey Research Methods. (2007) ;1: (2):97–108. doi: 10.18148/srm/2007.v1i2.79 |




