Qualitative feedback from caregivers in a multidisciplinary pediatric neuromuscular clinic
Abstract
OBJECTIVE:
This study explored family satisfaction and perceived quality of care in a pediatric neuromuscular care clinic to assess the value of the multidisciplinary clinic (MDC) model in delivering coordinated care to children with neuromuscular disorders, such as cerebral palsy.
METHODS:
Caregivers of 22 patients were administered a qualitative survey assessing their perceptions of clinic efficiency, care coordination, and communication. Surveys were audio-recorded and transcribed. Thematic analysis was completed using both deductive and inductive methods.
RESULTS:
All caregivers reported that providers adequately communicated next steps in the patient’s care, and most reported high confidence in caring for the patient as a result of the clinic. Four major themes were identified from thematic analysis: Care Delivery, Communication, Care Quality, and Family-Centeredness. Caregivers emphasized that the MDC model promoted access to care, enhanced efficiency, promoted provider teamwork, and encouraged shared care planning. Caregivers also valued a physical environment that was suitable for patients with complex needs.
CONCLUSION:
This study demonstrated that caregivers believed the MDC model was both efficient and convenient for pediatric patients with neuromuscular disorders. This model has the potential to streamline medical care and can be applied more broadly to improve care coordination for children with medical complexity.
1Introduction
Children with medical complexity (CMC) have significant chronic medical conditions, complex healthcare needs, substantial functional limitations, and high utilization of health services [1–3]. Caregivers and families of CMC face numerous barriers and increased caregiver burden when navigating the health care system [2–5]. Previous work by Kuo et al. demonstrated that caregivers of CMC spent an average of two hours per week on care coordination and reported between 11–15 physician visits over a one-year period. They went on to show that nearly 50% of caregivers felt that their child had at least one unmet medical service need such as preventative, dental, or specialty care [6, 7]. Caring for these complex patients requires diligent care coordination and communication between providers and patients. However, traditional models of care are often ineffective and can result in poorly managed care due to fragmented interactions and communication [4].
Multidisciplinary clinic (MDC) models, in which patients see multiple specialists in an integrated manner during a single visit, are an increasingly common approach to optimizing care coordination for CMC. For example, implementation of MDCs for children with craniofacial abnormalities increased efficiency of care, decreased delays in care, improved patient outcomes, and increased patient satisfaction [8, 9]. MDCs facilitate improved communication among different specialties, leading to a more collaborative approach to patient care and coordinated treatment plans [10]. Research increasingly supports the benefits of MDCs for sub-populations of CMC, such as patients with swallowing disorders [10], aerodigestive disorders [11, 12], hemophilia [13], diabetes [14], and cardiovascular disorders [15]. However, there is limited literature assessing the impact of the MDC model for children with neuromuscular disorders.
Few published studies focus on caregivers’ and families’ experiences and perceived quality of care in MDCs, yet their voices are essential in understanding what constitutes the ideal level of care [16]. Families have expressed that their unique expertise and experiences are essential in cultivating and implementing the long-evolving concept of family-centered care [17, 18]. This study aimed to understand drivers of family satisfaction and communication in a comprehensive multidisciplinary neuromuscular clinic.
2Methods
2.1Setting
The Comprehensive Neuromuscular Care Clinic (NMCC) consists of providers from 13 specialties who deliver coordinated care in a single visit to patients with a variety of neuromuscular disorders, such as cerebral palsy and muscular dystrophy. As part of an urban tertiary academic hospital, the NMCC primarily serves patients who are enrolled in this institution’s pediatric complex care program. To qualify for this program, children must have two or more chronic conditions (excluding asthma, obesity, or psychiatric conditions) and one major medical problem involving multiple organ systems, an immediate palliative care need, or technology dependence (wheelchair, feeding tube, tracheostomy, etc.). The NMCC serves around 75 patients per year, from a larger pool of 200–250 complex care program patients. Those attending the NMCC must have a specific neuromuscular disorder, such as cerebral palsy or spina bifida.
These complex care patients and their families typically face numerous barriers accessing coordinated care, as they frequently visit various specialists in multiple locations [1]. To address this specific barrier, patients in the NMCC attend a single clinic session where they are seen by multiple providers. Each provider visit is scheduled for 30 minutes, with patients remaining in a single room while providers rotate through patient rooms. At each visit, patients are seen by their complex care provider who is a general pediatrician in the complex care program. The NMCC convenes one to two times per month, with a session size of approximately 6–8 patients. This comprehensive clinic brings together a spectrum of specialists including those from complex care, child life, dentistry, pulmonology, neurology, neurosurgery, nutrition, occupational therapy, physical medicine and rehabilitation, orthopedic surgery, social work, and urology. Within this diverse team, there are physicians, physician assistants, nurse practitioners, therapists, social workers, and care coordinators.
2.2Participants
This study was approved by the Institutional Review Board. Informed consent was obtained for all participants in their preferred language. English- and Spanish-speaking caregivers of those enrolled in the NMCC were eligible to participate, due to availability of translation resources. The primary language of approximately 15% of families who attended the clinic was not English or Spanish. All eligible caregivers who had decision-making capacity for the patient were approached and consented for interviews between January 2021–May 2022. All caregivers provided written consent in English or Spanish prior to the interview. Those who had available time at the end of their visit were interviewed.
Demographic information about patients and their caregivers was elicited from interviews with direct questions about age, sex, race, ethnicity, and preferred language. Additional information about the patient’s insurance was gathered from electronic health record data. Additionally, demographic information from the overall clinic population was gathered via electronic health records to compare pertinent information.
2.3Data collection
In-depth individual interviews were conducted with caregivers using a structured interview guide to explore aspects of family satisfaction and perceived experiences in the clinic. One interview was completed per patient. Interviews were either in English or in Spanish with a professional virtual translator service, and the caregiver interview guide was translated into Spanish. Interviews were administered by three medical student research assistants, who were trained to conduct the interviews and were not providing direct care to the patients. Interviews were completed at the end of the clinic sessions, and caregivers were directly informed that their responses would have no impact on their care. All interviews were private, audio-recorded, and transcribed. Transcripts were verified and de-identified before coding.
2.4Data analysis
Thematic analysis of transcript data was completed. Using inductive line-by-line coding, two team members independently reviewed transcripts to generate initial codes, a preliminary codebook, and final coding scheme. Each transcript was double-coded, and coders met to reconcile discrepancies. During this process, overarching themes from the interviews were identified, defined, and iteratively reviewed as new themes emerged. Interviews were concluded when thematic saturation was reached [19].
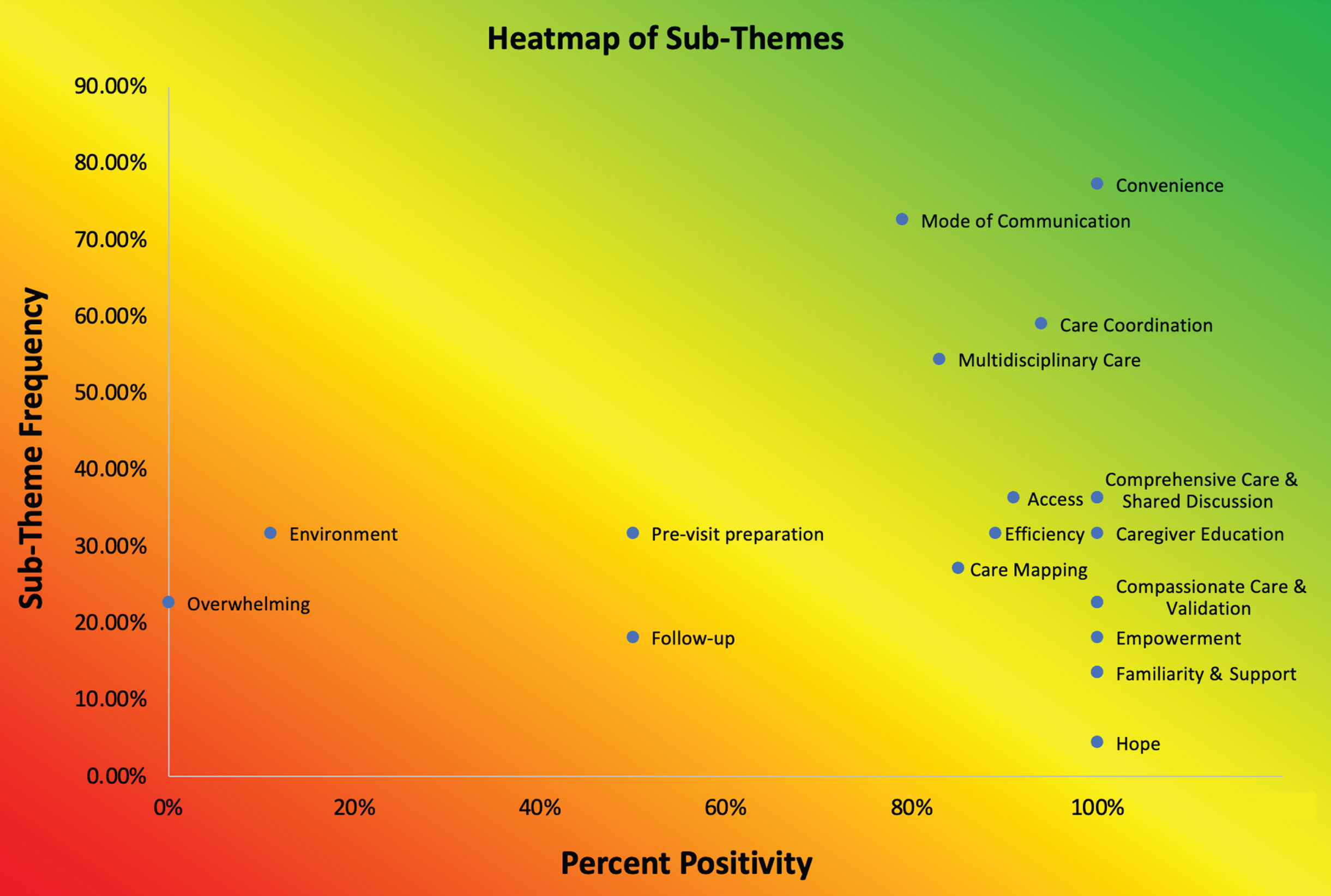
Four general themes were apparent in interviews. These were categorized into sub-themes, based on the individual codes in the transcripts and caregiver sentiments. For example, the broader theme of Care Delivery was divided into the following sub-themes in order of frequency: Convenience, Care Coordination, Access, Efficiency, Environment, Familiarity, and Overwhelming. Individual sub-themes were totaled and calculated to determine the percentage of caregivers interviewed who mentioned each sub-theme. Every code corresponding to a sub-theme was scored as positive, negative, or neutral, based on the specific question asked and research team consensus. These scores were plotted against the percentage of caregivers who mentioned each of them in order to create a heatmap.
3Results
A total of 22 caregivers, representing 22 unique patients, gave consent and completed the survey between January 2021 and May 2022. Caregivers of children in this study were predominantly biological parents (100%) and female (77.3%), and most reported English as their preferred family language (86.4%). Patients in this study ranged in age from four months to 16 years, with the majority between 0–4 years of age (68.2%). Additionally, most were covered primarily by public insurance (68.2%); 50% of children were identified as Hispanic, and 50% as male. Demographic findings were similar to the overall complex care program composition (55% male, 47% Hispanic). Regarding the medical complexity of patients in this study, approximately 55% had a diagnosis of spastic cerebral palsy, most with quadriplegia. The remaining 45% had a variety of other conditions, such as spina bifida, spinocerebellar ataxia, and X-linked myotubular myopathy. Additionally, every patient in the study utilized an assistive technology, with 82% dependent on more than one technology. Specifically, 77.3% utilized feeding tubes, and 68.2% utilized a wheelchair or adaptive stroller. Additional participant characteristics are presented in Table 1.
Table 1
Patient and caregiver demographics
| Demographics | Number (%) |
| Child age at enrollment | |
| Mean (SD) | 5.3 (5.3) |
| Median (Q1, Q3) | 3 (2,6.5) |
| 0–4 years | 15 (68.2%) |
| 5–12 years | 2 (9.1%) |
| 13–18 years | 5 (22.7%) |
| Child sex | |
| Male | 11 (50.0%) |
| Female | 11 (50.0%) |
| Relationship to child | |
| Biological parent | 22 (100%) |
| Caregiver gender | |
| Female | 17 (77.3%) |
| Male | 5 (22.7%) |
| Patient race | |
| Black or African American | 5 (22.7%) |
| White | 4 (18.2%) |
| Asian | 3 (13.6%) |
| More than 1 race | 1 (4.5%) |
| Other | 9 (40.9%) |
| Patient ethnicity | |
| Hispanic/Latino | 11 (50.0%) |
| Not Hispanic/Latino | 11 (50.0%) |
| Preferred language | |
| English | 19 (86.4%) |
| Spanish | 3 (13.6%) |
| Child primary insurance | |
| Public | 15 (68.2%) |
| Commercial | 7 (31.8%) |
| Neuromuscular diagnosis | |
| Spastic quadriplegic cerebral palsy | 10 (45.45%) |
| Spastic diplegic cerebral palsy | 2 (9.1%) |
| Other (e.g. spina bifida, myotubular myopathy) | 10 (45.45%) |
| Technology use | |
| Feeding tube | 17 (77.3%) |
| Wheelchair/adaptive stroller | 15 (68.2%) |
| Respiratory support (e.g. tracheostomy, ventilator) | 9 (40.9%) |
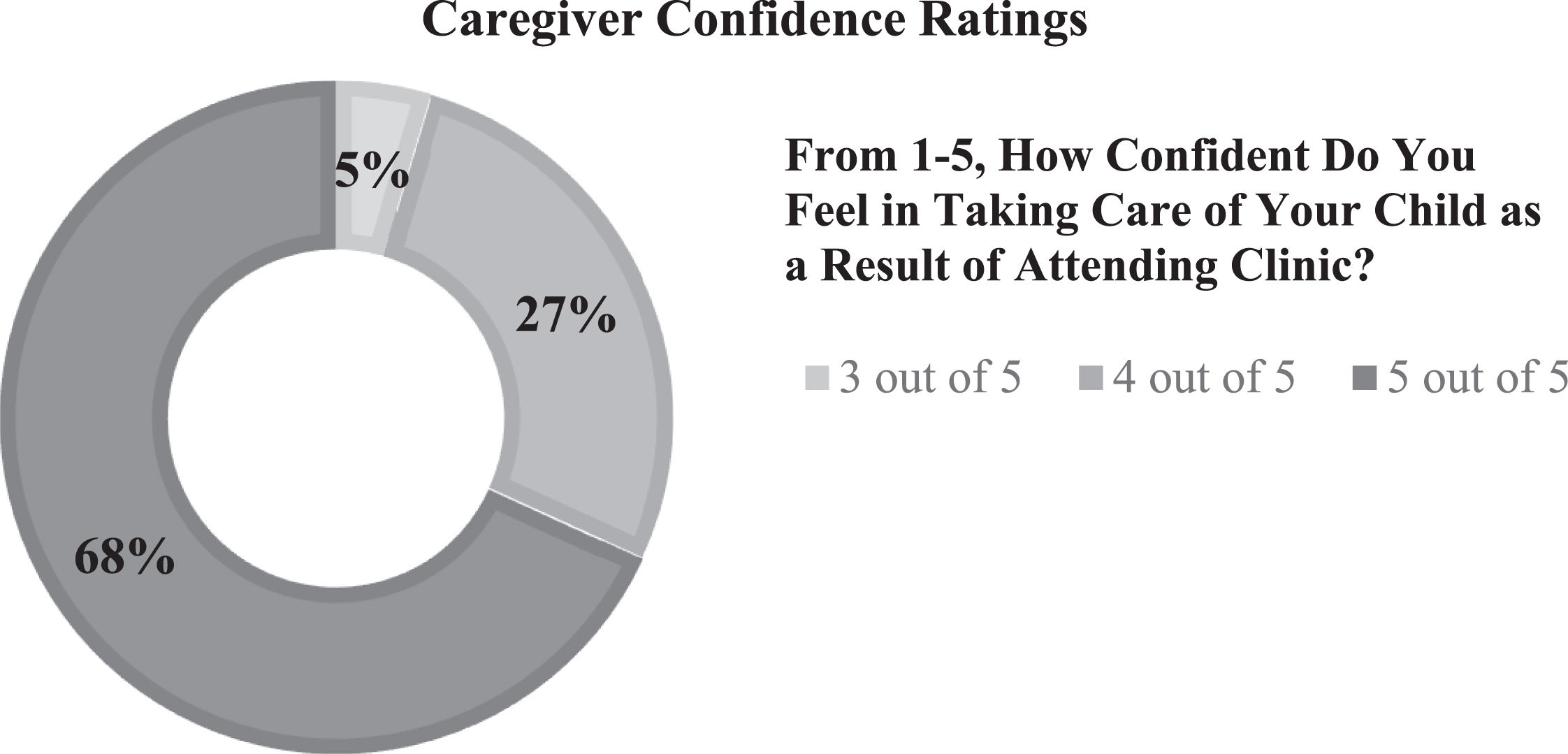
Patients saw an average of six specialists in a single MDC visit, with orthopedic surgery as the most commonly seen sub-specialty aside from the child’s primary complex care physician. All 22 participants provided a confidence rating on a Likert scale from 1–5 (1 = least confident, 5= most confident) when asked how confident they felt in taking care of the patient as a result of attending the clinic. Fifteen participants (68.2%) rated 5 out of 5 confidence, six participants (27.3%) rated 4 out of 5 confidence, and one participant (4.5%) rated 3 out of 5 confidence (Fig. 1). There were no responses below 3 out of 5. Additionally, all 22 caregivers (100%) reported that every provider communicated the next steps in the patient’s care.
Fig. 1
Caregiver Confidence Ratings. During interviews, caregivers were asked, “From 1–5, how confident do you feel in taking care of your child as a result of attending clinic?” In this Likert-type scale, 1 represented not at all confident and 5 represented the most. Responses ranged from 3 to 5, with a majority of caregivers noting their confidence was a 5.
Four overall themes emerged from the interviews with caregivers: 1) Care Delivery, 2) Communication, 3) Care Quality, and 4) Family-Centeredness. Care delivery (42%) and Communication (32%) were the most frequently discussed themes by caregivers, followed by Care Quality (16%) and Family-Centeredness (10%). For each theme, caregivers emphasized specific aspects of the clinic that impacted their personal experience, which were categorized into sub-themes. The four overarching themes and corresponding sub-themes are displayed in Fig. 2. Direct quotes from caregivers are included in Table 2.
Fig. 2
Themes & Notable Sub-Themes. Each theme was divided into sub-themes to further characterize caregiver sentiments. For example, the theme of Care Delivery was divided into the following sub-themes in order of frequency: Convenience, Care Coordination, Access, Efficiency, Environment, Familiarity, and Overwhelming.
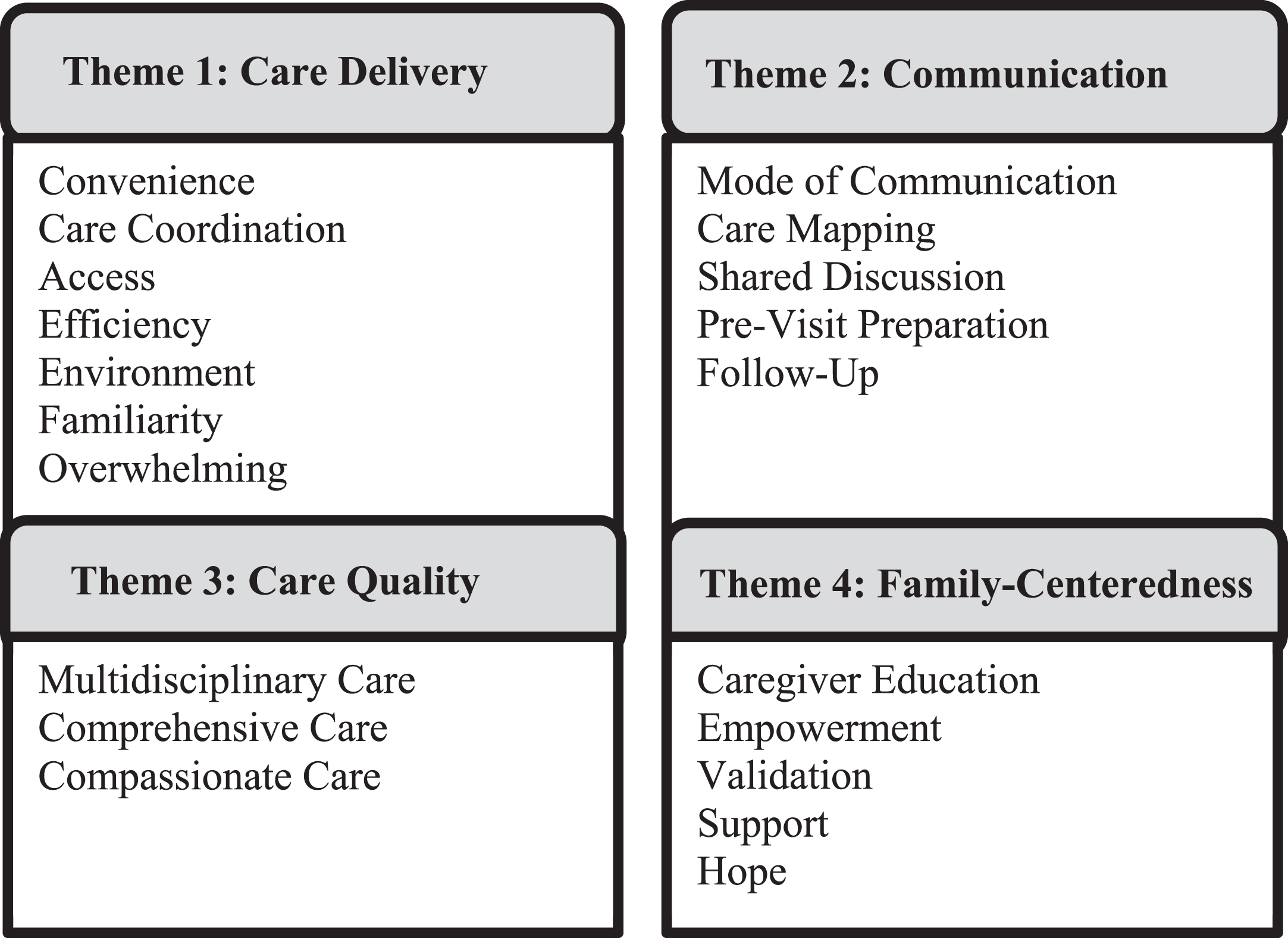
Table 2
Notable Caregiver Quotes
| Theme | Quote |
| Care Delivery | |
| Convenience | “Because of the many medical complications that my daughter has, being able to have those clinic moments where we can see multiple doctors at the same time is easier for us.” |
| Care Coordination | “The doctors can be here together, working with each other, and discussing her situation, and can come up with better ideas to how to treat her and make her life easier.” |
| Overwhelming | “I’m going to be honest, it’s stressful. There’s a lot going on back to back. He doesn’t like lying on the table or seeing the doctors.” |
| Environment | “A lot of these kids may, like my son, have a G-tube. We need something to hang it on the wall, like a pole or something here so we are able to accommodate his needs here. Still being able to feed him, keep him comfortable here as well.” |
| Communication | |
| Care Mapping | “I just took in a lot of great information about his present and what might be coming up in his future, which feels like a helpful map.” |
| Shared Discussion | “It’s been super helpful to have just the organization of the doctors and staff to help with appointments and communicate with each other and make the next steps super clear for me. What I need to do at home and what next appointments I have coming up.” |
| Care Quality | |
| Comprehensive Care | “Just meeting all of these disciplines today. The dental, we talked about dental hygiene. The orthopedic surgeon gave us exercises to help him increase his ability to stand. The dietician, was on the money, she got him to agree to eating a new food.” |
| Compassionate Care | “The doctors spend time with him, they were really gentle with him. They noticed that he might have been a bit nervous.” |
| Family-Centeredness | |
| Caregiver Education | “Even if we don’t need a doctor, they send them in and educate me on things that I didn’t realize could be a potential problem. The neurologist today educated me about seizures, which it’s kind of good to hear that stuff reinforced.” |
| Empowerment | “You guys have given me the tools and I’m making sure I’m using them!” |
| Hope | “Being able to have this clinic is also a way for us to have hope.” |
3.1Care delivery
The theme of Care Delivery encompassed various caregiver sentiments around the convenience, care coordination, access, efficiency, environment, and familiarity of the clinic compared to traditional models (Fig. 2). Caregivers (77%) noted that the convenience of seeing their providers in one setting, instead of through multiple appointments, was the most helpful aspect of the clinic. Importantly, according to 59% of caregivers, this MDC allowed for strong care coordination and teamwork among providers. One caregiver noted that the clinic ”keeps everyone on the same page and moving together as a team.” The workflow of the clinic was noted to be efficient, especially given that, on average, each patient saw six providers per visit. As one caregiver described, ”Everything went smoothly. I don’t know who facilitates the doctors coming in, but it always seems to work seamlessly.” Caregivers also described finding comfort in the familiarity of the clinic. They expressed that through continuous positive experiences, their children ”learn that it is not scary,” which is especially important for children who will see a considerable number of providers in their lifetime.
While caregiver comments about care delivery were largely positive, caregivers also addressed the potentially overwhelming clinic environment. They (23%) noted that coming to the clinic can be overwhelming with ”a lot going on back-to-back.” Likewise, 32% of caregivers commented on the physical environment of the clinic, with only 11% of those comments being positive. Specifically, caregivers emphasized the importance of both patient and caregiver comfort, especially when in the clinic for multiple hours. Many caregivers noted that the experience ”would be less overwhelming if they had breakfast or lunch.” The importance of having the physical environment, including patient rooms and waiting rooms, tailored to the specific needs of this population was strongly emphasized by caregivers.
3.2Communication
Communication emerged as a unanimously important theme with caregivers emphasizing the importance of communication before, during, and after appointments. The specific sub-themes of Communication included mode, care mapping, shared discussion, pre-visit preparation, and follow-up. Caregivers pointed out that preparation and advanced planning helped them stay organized. During visits, caregivers appreciated time to map out their child’s care and discuss concrete action plans. Also, they emphasized the importance of participation in decision-making about all aspects of their child’s care. Regarding the specific mode of communication, 55% of caregivers noted that written summaries were helpful tools, while 32% endorsed MyChart (an online portal) as their preferred communication system. Lastly, confidence in provider follow-up was an important aspect of caregivers’ sentiments towards communication.
3.3Care quality
Care Quality encompassed caregiver emphasis on comprehensive, multidisciplinary, and compassionate care. One caregiver said that the clinic ”helps with school, medication, making sure he sees all of his doctors and specialists, making sure he has everything he needs.” In addition, caregivers confirmed that the MDC model lent itself to comprehensive care across multiple disciplines. Many caregivers described that a highlight of the clinic was addressing all aspects of their child’s care with multiple specialists to paint a complete picture of their child’s health and health needs. Multiple caregivers specifically noted that the ability to see dental providers, nutritionists, and feeding specialists was a unique and integral part of their clinic experience. Lastly, caregivers acknowledged the importance of providing compassionate care to children who may not always experience it in the health care system.
3.4Family-centeredness
Family-Centeredness referred to an emphasis on caregiver education, empowerment, affirmation, and reinforcement. Caregivers expressed appreciation for education about current and future health care concerns, as well as learning more about resources. One caregiver conveyed, ”They educate me on things, such as seizures, that I didn’t realize could be a potential problem,” while another caregiver affirmed, ”I have learned a lot here!” In addition to education, caregivers expressed that with the help of the clinic, they felt empowered to care for and make decisions about their child. Caregivers also welcomed opportunities for both reinforcement and affirmation that ”we have been doing some of the right things.” Overall, they greatly emphasized the respect given to them as caregivers, as well as the family-centered nature of the clinic.
3.5Distribution of themes
A heatmap (Fig. 3) compared the frequency of caregivers who mentioned each sub-theme with how positive or negative those comments were, based on research team consensus. For example, the theme of Convenience was mentioned by 80% of caregivers, and 100% of these caregiver comments were positive. Themes such as Comprehensive Care and Shared Discussion also had 100% positivity but were mentioned by fewer caregivers (36%). More neutral comments included those about follow-up and pre-visit preparation, which had 50% positivity and were mentioned by 32% and 18% of caregivers, respectively. Conversely, more negative comments were focused on the potentially overwhelming clinic environment. While only 25–35% of caregivers mentioned the environment or overwhelming feelings, most comments were not positive.
Fig. 3
Heatmap of Sub-Themes. Percent positivity (x-axis) denotes the percent of comments about each sub-theme that were positive. Frequency of mention (y-axis) indicates the frequency of caregivers who mentioned each sub-theme.
4Discussion
This is the first study to qualitatively examine perspectives of caregivers for children in a multidisciplinary neuromuscular care clinic. Four main themes emerged from these interviews: Care Delivery, Communication, Care Quality, and Family-Centeredness. Caregivers emphasized that the unique format of the clinic promoted access to care, shared care planning, and caregiver empowerment. This study demonstrated that caregivers believed the MDC model was both efficient and convenient for caregivers and patients with neuromuscular disorders. Ultimately, this study suggested that multidisciplinary team models have great potential to streamline medical care, ease caregiver burden, and promote teamwork among providers who care for children with complex medical needs.
Previous MDCs have focused on care coordination; however, their target populations, locations, and structures varied substantially [12–14, 20–22]. Moreover, few studies have utilized caregiver and patient satisfaction as an outcome. In this study, themes Care Delivery and Care Quality clearly identified the need for convenient multidisciplinary care. Many caregivers specifically mentioned the availability of a wide variety of specialists, including those not seen at typical pediatrics clinics such as dentistry and nutrition. Not only did this allow for convenience in one visit, but caregivers expressed that this provided a comprehensive, whole-person approach to their child’s care. In a previous study by Chang et al., dissatisfaction was expressed due to perceived poor care coordination and lack of integrated care across teams of providers [23]. These points highlight why multidisciplinary care is especially important for CMC, as the focus on specific conditions can lead to neglect of the patient as a whole.
Further, convenience is largely associated with satisfaction. Previous literature has shown that both convenience and office environmental factors influence patient and caregiver perspectives when they critique healthcare settings [24–26]. In a similar manner, Allshouse et al. articulated that many primary care settings are unable to meet the clinical needs of CMC alone [16]. In this study, convenience was clearly a highly desirable trait and ultimately associated with patient and family satisfaction. By establishing access to multiple disciplines in one location, some of the burden can be taken away from caregivers when transporting patients and scheduling appointments for CMC. For example, transportation of CMC can be especially challenging in this setting due to significant functional limitations and high costs of specialized transportation in a large metropolitan area. Given that there are prior associations between low socioeconomic status and increased risk of various neuromuscular disorders, such as cerebral palsy, the financial burden of transportation on these caregivers becomes even more significant [7, 27–29]. Importantly, caregivers felt that the clinic format enhanced care coordination and teamwork among providers, allowing for more concise and efficient visits.
Communication also emerged as a frequently mentioned theme among caregivers. They described the inclusion of online communication and post-visit summaries as effective forms of information transmission. Similar concepts have been noted in previous reports in which patients have rated physicians higher online if they perceived them to have good communication skills [30]. For example, Butler et al. showed that pediatric surgeons who communicated effectively were more likely to receive higher online ratings and more positive comments [24]. All caregivers in this study felt that providers communicated the next steps in their child’s care, which ultimately makes caregivers more comfortable with their children’s providers.
The cumulative themes discussed by caregivers were largely positive in this study. The themes mentioned most frequently were convenience, mode of communication, care coordination, and multidisciplinary care (Fig. 3). Conversely, the environment of the clinic and its potential to be overwhelming fell towards the negative side. This is consistent with the current literature, which emphasizes that health care visits can be stressful and overwhelming for both CMC and their caregivers [16, 23, 31, 32]. While only 25–35% of caregivers in this study mentioned the environment or overwhelming feelings, the majority of these comments were negative. This can inform program leadership on pertinent areas that can improve the MDC experience. For example, providing basic refreshments, such as water and snacks, during these long visits would help families feel more comfortable. Pre-visit preparation and schedules given to caregivers can also help to alleviate some of the overwhelming feelings that they experience in the clinic when seeing multiple providers. Ultimately, increased communication between visits can also help prevent stressful experiences in the clinic.
5Limitations
Of note, the population in this study was limited to patients in an urban tertiary academic center, and this model may not be applicable to other contexts. While this study focused on the nuances of children with neuromuscular disorders, these issues overlap with many faced by CMC and their families. Lastly, as this study included only English- and Spanish-speaking patients, future studies can be expanded to include other languages.
In the future, this model has the potential to be standardized and more widely applied to children with various chronic medical conditions. This study suggests that families perceive MDCs to be effective at improving outpatient care coordination and communication for children with neuromuscular disorders as they consolidate appointments and providers into a single clinic day. There is also potential for future studies to assess clinical outcomes of patients enrolled in the NMCC, such as rates of hospitalization, length of hospital stays, and emergency department use. Cost analysis and financial outcomes can be utilized in the future to evaluate how this novel model impacts hospital systems.
Acknowledgments
The authors have no acknowledgments.
Conflict of interest
The authors have no conflicts of interest to report.
Ethical considerations
Institutional Review Board approval was received from the Icahn School of Medicine at Mount Sinai, and informed consent was obtained from all participants.
Funding
The authors have no funding sources to report.
References
[1] | Lin E , Scharbach K , Liu B , et al. A Multidisciplinary Home Visiting Program for Children With Medical Complexity. Hosp Pediatr. (2020) ;10: (11):925–31. doi: 10.1542/hpeds.2020-0093. |
[2] | Cohen E , Berry JG , Sanders L , Schor EL , Wise PH . Status Complexicus? The Emergence of Pediatric Complex Care. Pediatrics. (2018) ;141: (Suppl 3):S202–11. doi: 10.1542/peds.2017-1284E. |
[3] | Yu JA , Cook S , Imming C , et al. A Qualitative Study of Family Caregiver Perceptions of High-Quality Care at a Pediatric Complex Care Center. Acad Pediatr. (2022) ;22: (1):107–15. doi: 10.1016/j.aca2021.05.012. |
[4] | Chen AY , Schrager SM , Mangione-Smith R . Quality measures for primary care of complex pediatric patients. Pediatrics. (2012) ;129: (3):433–45. doi: 10.1542/peds.2011-0026. |
[5] | Van Orne J . Care coordination for children with medical complexity and caregiver empowerment in the process: A literature review. J Spec Pediatr Nurs. (2022) ;27: (3):e12387. doi: 10.1111/jspn.12387. |
[6] | Kuo DZ , Cohen E , Agrawal R , Berry JG , Casey PH . A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. (2011) ;165: (11):1020–6. doi: 10.1001/archpediatrics.2011.172. |
[7] | Kuo DZ , Goudie A , Cohen E , et al. Inequities in health care needs for children with medical complexity. Health Aff (Millwood). (2014) ;33: (12):2190–8. doi: 10.1377/hlthaff.2014.0273. |
[8] | Hoffman C , Yuan M , Boyke A , et al. Impact of a Multidisciplinary Craniofacial Clinic for Patients With Craniofacial Syndromes on Patient Satisfaction and Outcome. Cleft Palate Craniofac J. (2020) ;57: (12):1357–61. doi: 10.1177/1055665620948767. |
[9] | Laub DR , Ajar AH . A survey of multidisciplinary cleft palate and craniofacial team examination formats. J Craniofac Surg. (2012) ;23: (4):1002–4. doi: 10.1097/SCS.0b013e31824e67c2. |
[10] | Starmer HM , Dewan K , Kamal A , Khan A , Maclean J , Randall DR . Building an integrated multidisciplinary swallowing disorder clinic: Considerations, challenges, and opportunities. Ann N Y Acad Sci. (2020) ;1481: (1):11–9. doi: 10.1111/nyas.14435. |
[11] | Boesch RP , Balakrishnan K , Grothe RM , et al. Interdisciplinary aerodigestive care model improves risk, cost, and efficiency. Int J Pediatr Otorhinolaryngol. (2018) ;113: :119-23. doi: 10.1016/j.ijporl.2018.07.038. |
[12] | Ali SO , Yeung T , McKeon M , et al. Patient and caregiver experiences at a Multidisciplinary Tracheostomy Clinic. Int J Pediatr Otorhinolaryngol. (2020) ;137: :110250. doi: 10.1016/j.ijporl.2020.110250. |
[13] | Drayton Jackson M , Bartman T , McGinniss J , Widener P , Dunn AL . Optimizing patient flow in a multidisciplinary haemophilia clinic using quality improvement methodology. Haemophilia. (2019) ;25: (4):626–32. doi: 10.1111/hae.13768. |
[14] | Kaufman FR , Halvorson M , Carpenter S . Association between diabetes control and visits to a multidisciplinary pediatric diabetes clinic. Pediatrics. (1999) ;103: (5 Pt 1):948–51. doi: 10.1542/peds.103.5.948. |
[15] | Wolfe KR , Kelly SL , Liptzin DR , et al. Patient and Family Experience in a Multidisciplinary Clinic for Children With Single-Ventricle Heart Disease. J Patient Ex. (2020) ;7: (6):1384–90. doi: 10.1177/2374373520904214. |
[16] | Allshouse C , Comeau M , Rodgers R , Wells N . Families of Children With Medical Complexity: A View From the Front Lines. Pediatrics. (2018) ;141: (Supplement_3):S195–201. doi: 10.1542/peds.2017-1284D. |
[17] | Allshouse C . The importance of the family voice in quality measure development for children’s health care. Acad Pediatr. (2014) ;14: (5 Suppl):S8–9. doi: 10.1016/j.aca2014.02.006. |
[18] | Wells N , Partridge L . Families are key in improving quality. Acad Pediatr.S85-6. (2011) ;11: (3 Suppl). doi: 10.1016/j.aca2011.01.005. |
[19] | Fereday J , Muir-Cochrane E . Demonstrating Rigor Using Thematic Analysis: A Hybrid Approach of Inductive and Deductive Coding and Theme Development. International Journal of Qualitative Methods.. (2006) ;5: (1), 80–92. |
[20] | DeVries JK , Nation JJ , Nardone ZB , et al. Multidisciplinary clinic for care of children with complex obstructive sleep apnea. Int J Pediatr Otorhinolaryngol. (2020) ;138: :110384. doi: 10.1016/j.ijporl.2020.110384. |
[21] | Horvath LE , Yordan E , Malhotra D , et al. Multidisciplinary care in the oncology setting: Historical perspective and data from lung and gynecology multidisciplinary clinics. J Oncol Pract. (2010) ;6: (6):e21–6. doi: 10.1200/JOP.2010.000073. |
[22] | Robin NH , Baty H , Franklin J , et al. The multidisciplinary evaluation and management of cleft lip and palate. South Med J. (2006) ;99: (10):1111–20. doi: 10.1097/01.smj.0000209093.78617.3a. |
[23] | Chang L , Wanner KJ , Kovalsky D , Smith KL , Rhodes KV . “It’s Really Overwhelming”: Patient Perspectives on Care Coordination. J Am Board Fam Med. (2018) ;31: (5):682–90. doi: 10.3122/jabfm.2018.05.180034. |
[24] | Butler LR , Tang JE , Hess SM , et al. Building better pediatric surgeons: A sentiment analysis of online physician review websites. J Child Ortho. (2022) ;16: (6):498–504. doi: 10.1177/18632521221133812. |
[25] | Bakhsh W , Mesfin A . Online ratings of orthopedic surgeons: Analysis of reviews. Am J Orthop (Belle Mead NJ). (2014) ;43: (8), 359–63. |
[26] | Donnally CJ , Roth ES , Li DJ , et al. Analysis of Internet Review Site Comments for Spine Surgeons: How Office Staff, Physician Likeability, and Patient Outcome Are Associated With Online Evaluations. Spine (Phila Pa 1976). (2018) ;43: (24):1725–30. doi: 10.1097/BRS.0000000000002740. |
[27] | Solaski M , Majnemer A , Oskoui M . Contribution of socio-economic status on the prevalence of cerebral palsy: A systematic search and review. Dev Med Child Neurol. (2014) ;56: (11):1043–51. doi: 10.1111/dmcn.12456. |
[28] | Sundrum R , Logan S , Wallace A , Spencer N . Cerebral palsy and socioeconomic status: A retrospective cohort study. Arch Dis Child. (2005) ;90: (1):15–8. doi: 10.1136/adc.2002.018937. |
[29] | Carrilero N , Dalmau-Bueno A , García-Altés A . Comorbidity patterns and socioeconomic inequalities in children under 15 with medical complexity: A population-based study. BMC Pediatr. (2020) ;20: (1):358. doi: 10.1186/s12887-020-02253-z. |
[30] | Trehan SK , DeFrancesco CJ , Nguyen JT , Charalel RA , Daluiski A . Online Patient Ratings of Hand Surgeons. J Hand Surg Am. (2016) ;41: (1):98–103. doi: 10.1016/j.jhsa.2015.10.006. |
[31] | Spencer KA , Ramji J , Unadkat P , et al. Caregiver distress: A mixed methods evaluation of the mental health burden of caring for children with bladder exstrophy. Front Pediatr. (2022) ;10: :948490. doi: 10.3389/fped.2022.948490. |
[32] | Salley CG , Axelrad M , Fischer E , Steuer KB . But parents need help! Pathways to caregiver mental health care in pediatric hospital settings. Palliat Support Care. (2023) ;21: (2):347–53. doi: 10.1017/S1478951522001353. |




