Rehabilitation and functional outcomes for thoraco-omphalo-ischiopagus conjoined twins five years after separation: A case report
Abstract
Conjoined twins are identical twins joined in utero and are a rare phenomenon. This report discusses a case of female thoraco-omphalo-ischiopagus tripus conjoined twins. The twins were separated at age two, and once medically stable, spent one month in inpatient rehabilitation to improve their sitting balance and gross motor skills. This was followed by outpatient physical therapy. The twins initially had customized ZipZac seats, which they were able to wheel independently. After six months of therapy, the girls began walking with posterior walkers and prostheses. The hemipelvectomy prosthesis included a customized thoracolumbosacral orthosis component and was directly attached to a non-articulated pylon. A manual-locking hip joint was added to accommodate sitting. An articulated ankle-foot orthosis was used for the intact leg. Care of formerly conjoined twins requires comprehensive care from a multidisciplinary team involving, but not limited to, a physiatrist, orthopaedic surgeon, physical therapist, and orthotist/prosthetist. Complex congenital limb deficiencies are often a major undertaking for the rehabilitation team as continuous treatment and management are needed throughout the patient’s lifetime due to growth, development, and evolving physical demands. Anatomic variations must be examined on a case-by-case basis but often include limb deficiencies, orthopedic abnormalities, and organ comorbidities.
1Introduction
Conjoined twins are identical twins joined in utero and are a rare phenomenon, 1 in 50,000–100,000 births. 40–60% are stillborn, and 35% of live births die within 24 hours [1]. Females have a slightly higher predominance, 2 : 1 to 3 : 1 [2]. There are many types of conjoined twins, with the suffix “-pagus” meaning conjoined twins, and the nomenclature prefix describing the area of conjoining. For example, thoraco indicates the torso or chest, omphalo relating to the navel or umbilicus, and ischio indicating the hip. Thoracopagus twins, joined at the sternum and upper abdominal wall, and omphalopagus twins, who share an anterior abdominal wall, make up about 75% of cases [3]. Ischiopagus twins, who share a pelvis, intestinal tracts, and abnormal legs, represent <5% of cases [3]. Due to the significant variability with conjoined twins and their atypical anatomy, rehabilitation after separation is a case-by-case process and requires a skilled clinical assessment and team approach, including physicians, nurses, therapists, prosthetists, and orthotists. This report describes a case of female thoraco-omphalo-ischiopagus conjoined twins and their rehabilitation.
2Case report
Female thoraco-omphalo-ischiopagus tripus conjoined twins were born at 32 weeks and six days gestational age. They were conjoined facing and leaning away from each other (Figs. 1 and 2). They were joined from the lower chest down and had separate hearts, lungs, stomachs, and gallbladders but shared a single pericardial sac, diaphragm, liver, large intestine, bladder, cloacal opening, pelvis, and three legs.
Fig. 1
The thoraco-omphalo-ischiopagus tripus conjoined twins were conjoined facing and leaning away from each other. They were joined from the lower chest down. (Written photo consents obtained.)

Fig. 2
The conjoined twins shared a pelvis and had three legs (one of which was shared and not pictured). (Written photo consents obtained.)

Separation required extensive planning and thus was not completed until the twins were 28 months old. Just prior to surgery, they were able to sit unassisted for a brief period of time though, technically, only one would be sitting upright while the other would have to lean away and use their hands for support. The twins were able to crab crawl starting at 12 months, though Twin B had difficulty keeping her head up due to positioning. Each twin had proprietary control of one leg and shared a third leg that had two patellae and malformed feet. Twin A had primary motor control. The girls were attempting to pull to stand though this was limited. Both twins used their arms equally and could assist with dressing and removing socks. The twins were communicating verbally with roughly a 50-word vocabulary. They took nutrition and hydration through a nasogastric tube with minimal attempts by mouth with purees. The girls were able to vocalize and express the urge to void but had not yet been toilet trained.
Surgery required 17 hours and a team of 50 specialists at Lucile Packard Children’s Hospital Stanford. Upon separation, each twin had half a liver, half a gastrointestinal tract with an ileostomy or colostomy, a single kidney and ureter, a neobladder made from half of the shared bladder, a vesicostomy, and one intact hemipelvis connected to a lower extremity (Fig. 3). One twin also required a thoracoabdominal myocutaneous flap from the shared third leg, which was not functional and therefore not salvaged. After separation, the twins spent 13 weeks recovering, dealing with skin flaps, hypertension, renal failure, and follow up procedures before beginning inpatient rehabilitation.
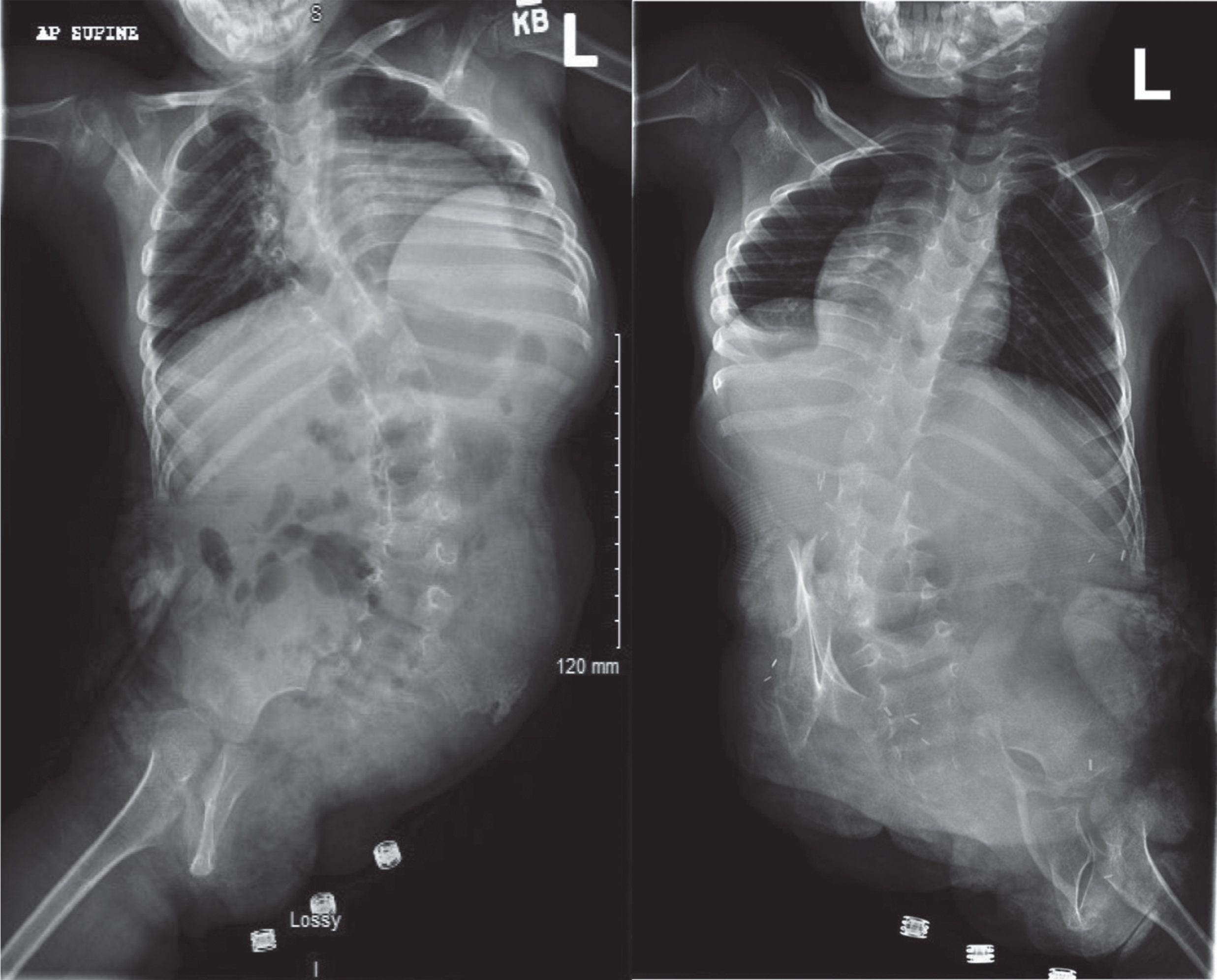
Fig. 3
Scoliosis radiographs of the twins post-separation reveal each twin had a hemipelvis.
Navigating mobility and maximizing independence for these twins required the use of a combination of resources, therapy venues, and clinicians. Rehabilitation often involves multiple stages and in the case of these conjoined twins, therapy was provided prior to separation surgery (prehabilitation), post-operatively in acute inpatient rehabilitation, and post hospital discharge in community-based outpatient therapy.
Prehabilitation therapy was facilitated through early intervention via in-home therapy services to aid the twins in progressing with developmental milestones. This included weekly physical, occupational, and speech therapy, with the goals of achieving independence with sitting, scooting, and self-feeding.
When they were medically stabilized post-surgery, the twins were transferred to University of California –Davis for inpatient rehabilitation. This consisted of three hours a day of therapy, including physical, occupational, and speech therapy. The overall objective of inpatient rehabilitation was for the twins to learn new motor patterns as well as postural and body mechanics for functional sitting, mobility, and feeding.
Upon admission to inpatient rehabilitation, the twins were similar in functional ability. In terms of gross motor ability, both girls had poor trunk control and were unable to sit independently or crawl due to their atypical anatomy and posture. Twin B was slightly more advanced with bed mobility, rolling at a supervision level. Otherwise, both twins required minimal assistance for bed mobility, total assist for transfers, total to minimal assist for sitting and standing, and total assist for locomotion. For personal care, both Twins A and B required total assistance for feeding, grooming, bathing, dressing, and toileting. Both were incontinent of bowel and bladder due to their vesicostomy and ileostomy or colostomy. They were both dependent for swallowing and required a nasogastric tube.
The twins spent a total of 20 days in inpatient rehabilitation. By the time of discharge, they had made significant motor gains and only required supervision for a modified crawl and wheelchair mobility. Each twin was able to scoot as well as bump up and down stairs in the sitting position. For balance, both were at a supervision level for sitting and moderate assist for standing. These Functional Independence Measure (FIM) scores are noted in Table 2. Minimal improvements were made with regard to continence, swallowing, and cognition. These scores are not included. The patients’ and guardians’ input were regularly assessed throughout the rehabilitation process and during weekly team meetings.
Table 1
Functional Independence Measures (FIMs) level classification
| No helper |
| 7 Complete independence (timely, safely) |
| 6 Modified independence (device –safety, extra time) |
| Helper –modified dependence |
| 5 Supervision or set up (patient = 100% effort) |
| 4 Minimal assist (patient = 75+% effort) |
| 3 Moderate assist (patient = 50+% effort) |
| Helper –complete dependence |
| 2 Maximal assist (patient = 25+% effort) |
| 1 Total assist (patient=<25% effort) |
| 0 Activity does not occur; use this only at admission |
Table 2
Functional Independence Measures (FIMs) at admission and discharge 20 days later from inpatient rehabilitation at age two
| Admission | Discharge |
| Twin A | |
| Total gross and fine motor FIM score at admission = 30 | Total gross and fine motor FIM score at discharge = 58 |
| Mobility FIM (bed mobility, rolling, assume sit, transfers) At admission = 13 | Mobility FIM (bed mobility, rolling, assume sit, transfers) At discharge = 18 |
| Balance (sitting, standing) At admission = 7 | Balance (sitting, standing) At discharge = 14 |
| Locomotion (crawling, gait, wheelchair, stairs) At admission = 4 | Locomotion (crawling, gait, wheelchair, stairs) At discharge = 10 |
| ADLs (feeding, grooming, bathing, toileting, dressing) At admission = 6 | ADLs (feeding, grooming, bathing, toileting, dressing) At discharge = 16 |
| Twin B | |
| Total gross and fine motor FIM score at admission = 31 | Total gross and fine motor FIM score at discharge = 59 |
| Mobility FIM (bed mobility, rolling, assume sit, transfers) At admission = 14 | Mobility FIM (bed mobility, rolling, assume sit, transfers) At discharge = 19 |
| Balance (sitting, standing) At admission = 7 | Balance (sitting, standing) At discharge = 14 |
| Locomotion (crawling, gait, wheelchair, stairs) At admission = 4 | Locomotion (crawling, gait, wheelchair, stairs) At discharge = 10 |
| ADLs (feeding, grooming, bathing, toileting, dressing) At admission = 6 | ADLs (feeding, grooming, bathing, toileting, dressing) At discharge = 16 |
ADLs: activities of daily living.
The twins were discharged to outpatient therapies, with medical follow up at Shriners Hospital for Children –Northern California. Additionally, they received their prostheses at Shriners Hospital and eventually received further therapy services there as well. Services in the community were provided at state-funded therapy centers that specialize in physical and occupational therapy for children with physical disabilities.
Once home, the twins required custom bracing and equipment to progress through multiple levels of mobility. They were fitted for custom manual wheelchairs and were also given ZipZac chairs (Fig. 4) that they could transfer in and out of and self-propel around home and school. The chairs were customized by Shriners with flexible, custom-formed foam to support each twin’s hemipelvis at midline as well as with parent push handles for use in the community.
Fig. 4
The twins received ZipZac chairs that were customized by Shriners with flexible, custom-formed foam to support each twin’s hemipelvis at midline as well as with parent push handles for use in the community. (Written photo consents obtained.).

Each twin was measured for a custom thoracolumbosacral orthosis (TLSO) (Fig. 5), which could serve multiple purposes, mainly to provide a base of support for sitting and to act as the socket for their eventual ambulation with a prosthesis. An additional medical goal of the TLSO was to stabilize each girls’ kyphosis and scoliosis, which were a consequence of their hemivertebrae and hemipelvis. Accommodation of their spinal deformities and medical complexities (i.e., ileostomy or colostomy, vesicostomy, skin flap) required unique, individualized prosthetic and orthotic design/planning. Marionette strings were added (Fig. 6) to the proximal end of the prosthesis for therapists to assist with balance and weight bearing. Of note, while the hemipelvectomy socket trim line can usually be lower profile, these needed to be higher for the twins to provide the needed spine support. This was somewhat complicated by the presence of their ileostomy/colostomy which limited the surface area available for applying corrective forces to the curve. Additionally, adequate suspension for a hemipelvectomy prosthesis often requires a shoulder strap, but this was not needed for these twins given they already had a TLSO component that would provide more surface area for suspension [4].
Fig. 5
The prosthetists made custom thoracolumbosacral orthoses for the twins. (Written photo consents obtained.).

Fig. 6
The custom thoracolumbosacral orthoses had attached marionette strings for aid with ambulation. (Written photo consents obtained.).

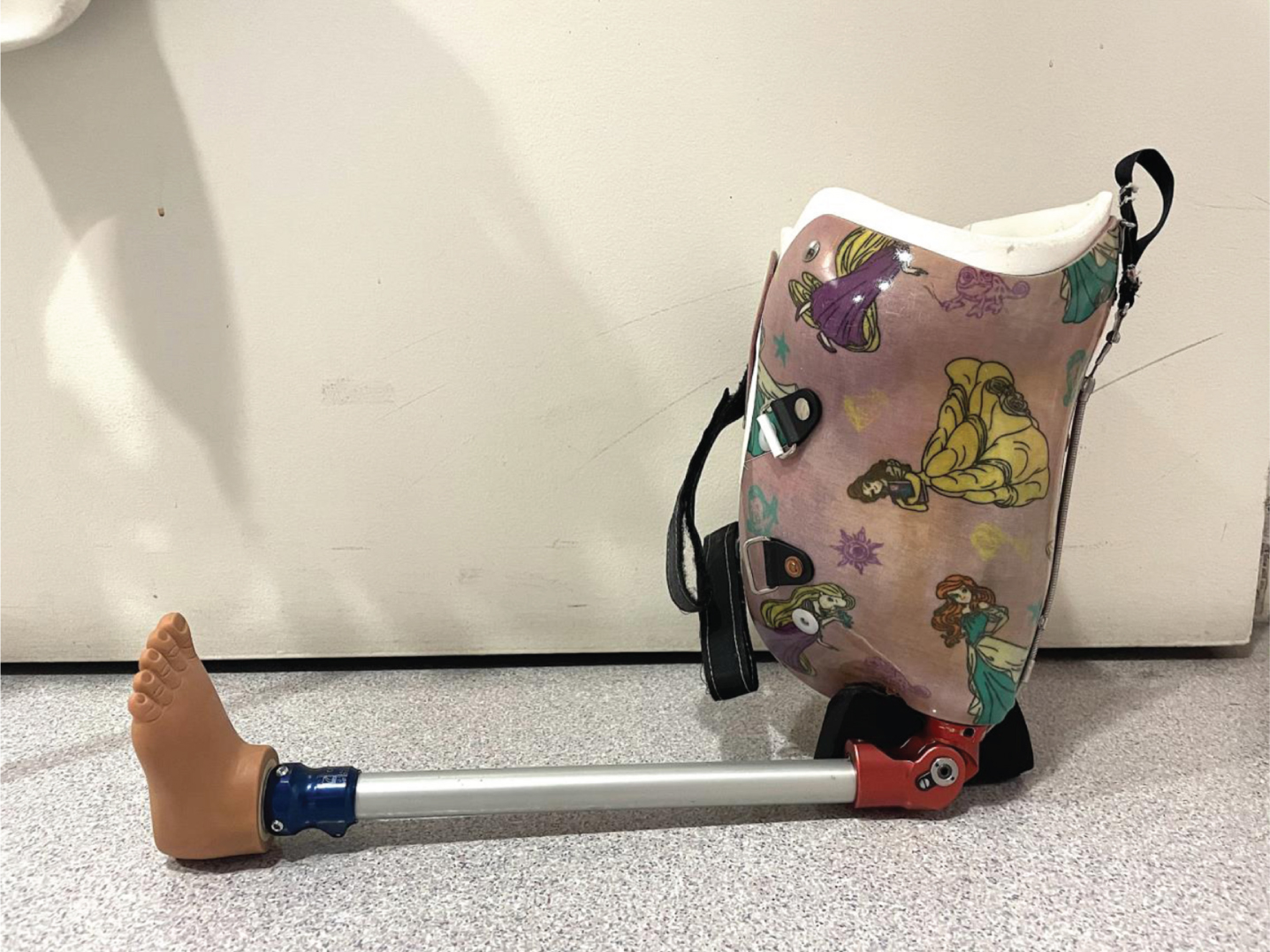
Within six months following inpatient rehabilitation, the twins progressed to pulling to stand and began cruising without a prosthesis in parallel bars. It was not until approximately a year and a half after separation (at age three years and 10 months) that they were walking with prostheses and posterior walkers. The hemipelvectomy prosthesis included a non-articulated pylon with a solid ankle cushion heel foot for a stable base of support. This was directly connected to the TLSO (Figs. 7, 8). A manual-locking hip joint was added to accommodate sitting. An articulated ankle-foot orthosis was used for the intact leg.
Fig. 7
The hemipelvectomy prosthesis included a non-articulated pylon with a solid ankle cushion heel foot for a stable base of support. This was directly connected to the thoracolumbosacral orthosis.

Fig. 8
The custom thoracolumbosacral orthosis served multiple purposes, one of which was to provide a base of support for sitting.
Both twins used a walker intermittently for years for longer distance mobility, when they were ill, or when they had a prosthesis needing repair. After several years with a walker, at about age five years and six months, the twins progressed to using Lofstrand crutches (Fig. 9) and multi-axial feet. Now, five years since separation, they are community ambulators, walking without the use of assistive devices (Fig. 10). Whereas they were previously using a manual locking knee joint as a hip joint due to their size, they now have a polycentric hip joint and will be provided a prosthetic knee. The plan is for a 4-bar polycentric knee with a single axis foot, with positioning of the center of gravity anterior to the knee for improved knee stabilization.
Fig. 9
After several years with a walker, the twins progressed to using Lofstrand crutches. (Written photo consents obtained.)

Fig. 10
The twins now ambulate without an assistive device. (Written photo consents obtained.)

One of the benefits of separation is that the twins have been able to develop their own dispositions and trajectories. For example, one twin was bolder than the other and was unafraid to fall, and therefore progressed to walking independently without assistive devices sooner than the other. Though the timeline is not precisely known because the twins’ progression was not always linear, it is known that the bolder twin progressed to independent ambulation about two months prior to the other. Discovering each twin’s personality is certainly rewarding during the care and rehabilitation of conjoined twins. Personality can also play a role in catering the therapy, equipment, and prosthesis for each child.
3Limitations
While compliance to outpatient therapy was not objectively assessed, the twins were typically seen weekly. Assessment of functional ability with validated outcome measures was not reported for the period of outpatient rehabilitation as they received therapy at multiple places that used different scoring methods (FISC [Functional Improvement Score], FIM). Additionally, given the limitations of the scales, the authors felt that descriptions of their mobility and prostheses would be more informative.
4Discussion
Outcomes for conjoined twins post-separation have historically been poor and the chance of survival was difficult to estimate given limited data, especially for those conjoined at multiple anatomic regions. In one review of eight separations in Memphis, Tennessee, from 1953 to 2016, all sets except for one experienced at least one fatality before, during, or as a result of separation [5]. In another study of 40 cases of conjoined twins, those that underwent separation had a 60% survival rate [6]. This overall post-separation survival rate is similar to other outcomes published, such as cases from 1964–2006 in the UK and in South Africa [7]. In that study, the total survival rate was 66%, but ranged from 0% for cephalopagus (twins conjoined dorsally at the head) to 100% for pygopagus (twins conjoined dorsally at the sacrum and at the perineum).
At this time, there are limited publications on mobility or functional outcomes in conjoined twins, either while conjoined or post-separation [8]. In this case, these twins, having one hemipelvis each, can essentially be considered as hemipelvectomy patients. A hemipelvectomy is a type of amputation in which half the pelvis and the entire associated leg are removed. Transpelvic and translumbar losses, as well as hip disarticulations, have been estimated to comprise fewer than 2% of all amputations in the United States [9].
Outcomes have been published regarding hemipelvectomy in adults. With respect to mobility, prior studies on adults found that only 4.4% of external hemipelvectomy patients were able to use a prosthesis without external support; 81% used crutches, with or without prosthesis; 9% remained wheelchair-dependent; and 6% were essentially bedridden [10, 11]. However, there are very few papers on pediatric external hemipelvectomy outcomes including ambulation. There is one case study by Haim et al. of a 16-month-old boy who suffered a traumatic hemipelvectomy [12]. After 5.5 months he was able to walk with his prosthesis and walker for short distances, and four years post injury was using his prosthesis and walking daily with bilateral forearm crutches.
Energy consumption is a major limitation to prosthetic use with more proximal amputations, and prosthetic fitting for an external hemipelvectomy is no exception. Hip disarticulations are similar in amputation level, and gait studies have shown that the use of those prostheses requires up to 125–200% more effort compared to the energy consumption of walking for a non-amputee [9, 13]. Walking speed with a hemipelvectomy prosthesis has been reported as 50% slower compared to controls. In the past, locked joints were used in these prostheses, but now, free moving joints at the hip, knee, and ankle levels have become more common. With newer componentry, walking speed is still decreased though somewhat improved at 40% slower than that of control [4, 10]. Increased efficiency in joints improves balance and decreases the need for assistive devices for ambulation [4].
Complex congenital limb deficiencies are often a major undertaking for the rehabilitation team as continuous treatment and management are needed throughout the patient’s lifetime due to growth, development, and evolving physical demands. Infants may be fitted with lower-limb prostheses as early as six months of age or when they attempt to accomplish a seated or an upright position [14]. The conjoining of twins certainly adds another layer of complexity and thus delay in prosthetic fitting. However, in general, prosthetic fitting should be as early as possible given the physical and psychological benefits of early fitting [9]. Prosthetic fitting in congenital limb deficiency also presents a challenge as pediatric prostheses are limited by size, availability, and the ability to accommodate growth. Additionally, the componentry has to be much smaller than for the adult prosthesis and must be durable enough to withstand the greater wear and tear of an active child [15].
5Conclusion
Thoraco-omphalo-ischiopagus conjoining of twins is a rare phenomenon and presents a unique challenge in rehabilitation and prosthesis/orthosis development. Anatomic variations must be examined on a case-by-case basis and often include limb deficiencies, orthopedic abnormalities, and organ comorbidities. Rehabilitation should be a team effort involving multiple disciplines including, but not limited to, a physiatrist, orthopedic surgeon, therapists, and orthotist/prosthetist. Due to multiple medical comorbidities associated with conjoining of twins, acute inpatient rehabilitation may be best at a multispecialty hospital for optimized availability of medical consultants and collaborative plan of care.
This case reports the successful rehabilitation of separated conjoined twins with hemipelvectomy who were able to achieve functional ambulation without an assistive device. It illustrates the various issues involved in their rehabilitation management, including some of the important considerations required with complex prosthetic planning.
Acknowledgments
With special thanks to our favorite twins and their amazing and supportive parents.
Conflict of interest
There are no known conflicts of interest associated with this publication, and there has been no significant financial support for this work that could have influenced its outcome.
Ethical considerations
Consent for manuscript writing, publication, and all figures including Figs. 1 and 2 was provided by the twins and their guardian for full use in manuscript publication without modification of the images required. IRB approval was not required for manuscript writing and publication. Figures 1 and 2 were not photos taken with the intent for inclusion in the manuscript but were the best available for demonstrating the unique appearance and level of conjoining.
References
[1] | Mathew RP , Francis S , Basti RS , et al. Conjoined twins – role of imaging and recent advances. J Ultrason. (2017) ;17: (71):259–66. doi:10.15557/JoU.2017.0038. |
[2] | Khan YA . Ischiopagus tripus conjoined twins. APSP J Case Re. (2011) ;2: (1), 5. |
[3] | Bianchi DW , Crombleholme TM , D’Alton ME , Malone FD Conjoined twins. In: Bianchi DW, Crombleholme TM, D’Alton ME, Malone FD, editors. Fetology: diagnosis and management of the fetal patient. New York: McGraw-Hill; 2000. p. 893-9. |
[4] | Houdek MT , Kralovec ME , Andrews KL . Hemipelvectomy high-level amputation surgery and prosthetic rehabilitation. Am J Phys Med Rehabil. (2014) ;3: (7):600–810.1097/phm.0000000000000068. |
[5] | Carlson TL , Daugherty R , Miller A , Gbulie UB , Wallace R . Successful separation of conjoined twins: the contemporary experience and historic review in Memphis. Ann Plast Surg. (2018) ;80: (6S Suppl 6):S333–9. doi:10.1097/SAP.0000000000001342. |
[6] | Brizot MdL , Liao AW , Lopes LM , et al. Conjoined twins: prenatal diagnosis, delivery and postnatal outcome. Rev Bras Ginecol Obstet. (2011) ;33: (5), 211–8. |
[7] | Frawley G . Conjoined twins in –state of the art and future directions. Curr Opin Anaesthesiol. (2020) ;33: (3):381–7. doi:10.1097/ACO.0000000000000864. |
[8] | Tozzi M , Zant RSV . Rehabilitation of conjoined twins pre- and postsurgical separation. Phys Occup Ther Pediatr. (2017) ;37: (2):139–54. doi:10.3109/01942638.2016.1150382. |
[9] | Michael JW , Jorge M Prosthetic options for persons with high-level and bilateral lower-limb amputation. In: Lusardi MM,Jorge Milagros, Nielsen C, editors. Orthotics and prosthetics in rehabilitation. Missouri: Elsevier Saunders; 2013. p. 685-96. |
[10] | Houdek MT , Andrews K , Kralovec M , et al. Functional outcome measures of patients following hemipelvectomy. Prosthet Orthot Int. (2016) ;40: (5):566–72. doi:10.1177/0309364615574164. |
[11] | Beck LA , Einertson MJ , Winemiller MH , DePompolo RW , Hoppe KM , Sim FF . Functional outcomes and quality of life after tumor-related hemipelvectomy. Phys Ther. (2008) ;88: (8):916–27. doi:10.2522/ptj.20070184. |
[12] | Haim S , Laufer Y , Leonid K , et al. Hemipelvectomy after severe pelvic injury in factor VII deficiency toddler. Injury. (2015) ;46: (6):1178–82. doi:10.1016/j.injury.2014.11.010. |
[13] | Nowroozi F , Salvanelli ML , Gerber LH . Energy expenditure in hip disarticulation and hemipelvectomy amputees. Arch Phys Med Rehabil. (1983) ;64: (7):300–3. |
[14] | Smith DG , Burgess EM , Zetti JH Special considerations: fitting and training the bilateral lower-limb amputee. In: Bowker HK, Michael JW, editors. Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles. Rosemont: American Academy of Orthopedic Surgeons; 1992. |
[15] | Is pediatric progress in O&P keeping pace with kids? Northglenn: The O&P Edge; 2006 [cited 20 May 2021]. Available from: https://www.oandp.com/articles/2016-04_02.asp. |




