Analysis of a model for pediatric physical therapy and clinical education via telehealth
Abstract
A novel entry-level collaborative clinical learning experience (CLE) in pediatric physical therapy (PT) delivered via telehealth was implemented involving 12 families, 54 DPT students, and 12 clinical instructors (CIs). Children of various ages, a wide range of home environments, and diagnoses received individualized PT via telehealth during a four-week CLE. Retrospective quantitative and qualitative analyses of student documentation, video recordings of sessions, and CI, student, and caregiver survey responses were performed. All children demonstrated qualitative improvements and 73% demonstrated quantitative improvements. CIs, students, and caregivers believed the children benefited from the experience and 98% believed the children were able to work toward their goals. Most students (95%) and CIs (100%) felt that it was a valuable and effective learning experience. Most (>71%) CIs and students believed students were able to learn in all relevant domains of the clinical performance instrument. This model provides a unique CLE for students in both pediatric PT and telehealth.
1Introduction
The utilization of the telehealth delivery of services to children has increased exponentially in recent years due to the COVID-19 pandemic [1]. Telehealth allows for increased access to care for those who were previously unable to receive services due to geographic location, transportation issues, financial burdens, mobility concerns, or environmental and physical barriers [2–4]. In the context of the pediatric population specifically, the flexibility of telehealth decreases the family burden by decreasing the time taken off work, school absences, transportation of medical equipment to appointments, and the need to find care for other children in the home [5–9]. The efficacy of the telehealth delivery of physical therapy (PT) is generally supported in the literature across adult populations [10–16] but the literature on the telehealth delivery of PT in pediatrics is extremely limited [17–20]. Camden et al. [20] examined the effectiveness of telerehabilitation in children in a systematic review of 23 studies and reported that while the majority of the evidence focused on behavioral outcomes, the limited evidence that examined functional and motor outcomes suggests that telerehabilitation is effective.
Although evidence is lacking for the telehealth delivery of PT in pediatrics, the telehealth delivery of services promotes the cornerstone practices of pediatric PT including treating children in the natural environment (home) and utilizing a family-centered approach that fosters caregiver engagement. Preliminary evidence suggests that long-term cognitive development, motor development, and school performance are improved with treatment within the home [21–24]. Additionally, families report increased competence in caring for their children when services are provided in the home [25]. Furthermore, a meta-analysis of the evidence examining pediatric rehabilitation suggested that, when interventions are more family-centered in their orientation, the outcomes are more positive for the parent, family, and child [26]. Since the therapist performing telerehabilitation is requisitely hands-off, the nature of telehealth requires a more family-centered approach with a focus on caregiver-implemented interventions. That said, because telehealth requires complete engagement of the family, it may not be appropriate for some families who may be limited by intellectual capacity, digital or health literacy, or communication abilities.
The necessary involvement of the family in telerehabilitation should positively impact outcomes logically. This theory is supported by a recent qualitative analysis of a pediatric telehealth rehabilitation experience [18]. While studies provide preliminary evidence to support the efficacy of caregiver-implemented interventions on improving fine motor and gross motor skills in children [22, 27], research on the benefits of parental engagement in PT is limited and inconclusive [28]. Parental engagement is consistent with the coaching and hands-off role of the therapist in the “COPing with and CAring for infants with special needs” (COPCA) approach that targets active participation of the caregivers in early intervention and has shown great promise in the literature [29, 30]. The coaching approach is associated with improved motor development in children, improved caregiver confidence and engagement, family empowerment, and improved quality of life for both the caregivers and family as a whole [24, 25, 29, 31–36].
The landscape of healthcare has changed as telehealth has taken hold and, with this change, the education of future clinicians in telehealth service delivery must be considered. During the COVID-19 pandemic, more than 35% of pediatric therapists reported that over 75% of their caseload transitioned to telehealth and 76.1% of these therapists reported that they would consider providing telerehabilitation in the future [17]. However, only 14.6% had formal training in telerehabilitation [17]. The Federation of State Boards of PT has released recommendations for physical therapist practice through telehealth. Also, the American Physical Therapy Association (APTA) House of Delegates has endorsed telehealth as a delivery model [37–39]. The APTA has also developed a certificate series for the telehealth delivery of PT speaking to the need for education in this area [40]. Entry-level programs must therefore consider this shift towards increased telerehabilitation exposure when designing curricula to prepare future clinicians. Clinical educators across multiple disciplines believe that services delivered via student-led telehealth can meet the client’s needs and also achieve student learning outcomes [41]. Interestingly, a concern of clinical education via telehealth was a perceived decrease in efficiency when telehealth sessions were led by individual students. Specifically, educators felt that more time was needed to supervise students [41]. However, the clinicians believed that student preparation for telehealth prior to clinical placements was critical [41]. A recent qualitative case analysis of a collaborative pediatric PT clinical learning experience (CLE) integrated into the didactic curriculum with peer-to-peer learning provided a potential model for the integration of telehealth clinical education into entry-level PT curriculum [18]. The purposes of the present study were therefore to (1) describe a CLE in pediatric telerehabilitation for entry-level students across a variety of pediatric diagnoses and demographics, (2) to describe the interventions and outcomes associated with the telerehabilitation provided in this CLE, and (3) to examine the feasibility and acceptability of this model of pediatric PT delivery and clinical education.
2Methods
2.1Model description
As part of an entry-level pediatric PT course, groups of three to four students conducted an in-person examination of a child with their family under the supervision of a licensed physical therapist (called a clinical instruction [CI]). This in-person learning experience was intended to continue with intervention on a weekly basis but was discontinued after the examination due to the COVID–19 pandemic. In response, the learning experience transitioned to telehealth. The CIs, students and the legal guardians of the children provided written informed consent for participation in the sessions, video recording of all sessions (in person and via Zoom), and dissemination of findings.
Over a period of four weeks, these groups of three to four students completed four to five 60-minute telehealth pediatric PT sessions. The telehealth sessions with the children were provided in their homes with caregivers and siblings present (as this occurred during the COVID-19 pandemic). All sessions were carried out and recorded using password-protected Zoom video conferencing (Zoom Video Communications, San Jose, CA). All Zoom video recordings were stored in password-protected folders on the researchers’ computers and adherence to the HIPAA compliance checklist for videoconferencing was ensured [42]. In addition, all sessions were supervised by a CI who was a licensed physical therapist with prior experience treating pediatric populations. Students submitted documentation which included the history and examination, PT goals, and progress notes as a part of the CLE.
2.2Participants: Students, CIs, and families
Twelve CIs, including four DPT faculty members, and 54 second-year entry-level DPT students participated in the experience. Twelve children with disabilities and their families were recruited from local pediatric physical therapists to participate. There were nine boys and three girls ranging in age from 22 months to 19 years with a variety of diagnoses and functional levels. The data from one child/family could not be analyzed because the video recordings were not saved and therefore not available to the researchers resulting in data analysis of 11 children (eight boys and three girls). The caregivers who participated in the sessions, the level of sibling involvement, and the learning opportunities can be seen in Table 1. Learning opportunities were defined as the resources available for motor learning and development. Literature supports the importance of learning opportunities in childhood development using resources including space, equipment and toys, caregiver/family availability and time [43].
Table 1
Physical therapy participant characteristics
| Child | Gender | Age | Diagnosis | Caregivers involveda | Siblings involved | Sessions (days)b | Learning opportunities |
| L1 | Female | 4 years | CMV | Grandmother | One older | 5 (23) | Adequate |
| 2 | Male | 19 years | CP: spastic diplegia & ASD | Mother | None | 5 (9) | Adequate |
| 3 | Male | 22 months | CP: spastic hemiplegia | Mother and father | None | 4 (22) | Extensive |
| 4 | Female | 8 years | CP: spastic diplegia | Grandmother | None | 5 (24) | Limited |
| 5 | Male | 9 years | ASD | Grandmother | None | 5 (14) | Limited |
| 6 | Female | 15 years | CP: spastic hemiplegia | Mother | Multiple | 5 (13) | Extensive |
| 7 | Male | 9 years | CP: spastic hemiplegia | Mother and father | None | 4 (24) | Extensive |
| 8 | Male | 9 years | Nuclear factor 1 X deficiency | Mother | One older | 5 (14) | Adequate |
| 9 | Male | 8 years | Angelman syndrome | Mother and father | One older | 5 (17) | Adequate |
| 10 | Male | 8 years | Rett syndrome & ASD | 2 contracted caregivers | None | 5 (20) | Limited |
| 11 | Male | 10 years | CP: spastic quadriplegia | Mother | Multiple | 5 (18) | Extensive |
aCaregivers who participated in telehealth PT sessions. bTotal number of PT sessions the child participated in and the number of days between the first and last session. CP: cerebral palsy; CMV: cytomegalovirus; ASD: autism spectrum disorder.
2.3Collaborative telehealth learning experience procedure
Prior to the telehealth experience, the students and CIs reviewed and discussed guidelines for telehealth practice and key principles for the delivery of PT through telehealth [42, 44, 45]. This preparation included viewing recorded telehealth sessions followed by discussion and role playing. The discussions and role playing were focused on preparation for the visit, management of technology and maintaining a video presence, interpersonal skills including verbal communication, and client privacy and safety. Expected challenges and strategies to overcome these challenges were also discussed prior to the experience. The procedure for the learning experience was modeled after the one previously described [18].
The students conducted a telehealth preparation visit via Zoom with each family to gather additional history and subjective information from the caregivers. Also, they evaluated the home environment and available learning opportunities for each child under the supervision of a CI. After this initial telehealth visit, each student developed a long-term goal for the child based on the in-person examination data, the goals of the child and family, and the child’s home environment. All goals were discussed with the licensed pediatric PT faculty and families, and revised as appropriate. Students also developed and documented a plan of care to address their goal under similar faculty direction and family consultation during the remaining three to four PT sessions. The students met as a group to discuss and plan prior to each session, then emailed the caregivers the overall plan for the visit with a list of activities and materials they might use. This plan included any preparation needed before the visit (e.g., placing a constraint on the child’s left hand 10 minutes before the session to prepare for constraint induced movement therapy during the session) [46]. Each student was responsible for directing a portion of the session while the other students actively observed. During each session, the Zoom chat feature was used by the CIs to direct students on how to enhance, modify, or proceed with the interventions, as well as provide direct feedback on the students’ performance, critical analysis, and active observations. Students used the chat to provide feedback to peers to enhance the intervention, or the flow of the session, and to share their observations with the group. The chat was visible to all participants, including the caregivers, which allowed them to appreciate the feedback and direction the students were receiving from their peers and CI (as they would during an in-person experience). At the outset of the experience, the purpose of the chat was explained to the caregivers who were directed to limit their attention to or close the chat at their discretion to minimize interference to both the family/child and the student/family interaction. Upon completion of each session, the family left the Zoom video conference, and the students and supervising CI remained on the Zoom call to discuss their reflections from the session. Students documented a progress note for each session. The learning experience did not include a discharge assessment as the focus of the experience was on the provision of therapeutic interventions. In addition, while recommendations have been published on performing assessments via telehealth in the pediatric population since the time of the CLE [7, 47], there is very limited evidence about the use of motor assessments via telehealth in adults with neurologic conditions [48, 49] and only one study was identified specifically in the pediatric population [50].
2.4Provision of PT services
Three to four PT goals were set for each child leading to therapeutic focuses (Table 2). Goals focused on dynamic and static balance in various positions or activities, quantitative (e.g., percentage of reaches with the more involved extremity) and qualitative (e.g., use of a more precise vs. crude grasp) use of the upper extremity, gait quality, coordination, achievement and maintenance of various developmental positions, and aerobic fitness.
Table 2
Therapeutic sessions and outcomes
| Low Functional Levela | ||||
| Child | Exemplar Therapeutic Focus | Target Behaviors | Pre/Postb | Observations |
| Illustrative Intervention(s) | Operational Definition | |||
| 1 | Facilitation of developmental positionsProne prop with cushions to support upper trunk; Tall kneeling with chair support | Prone Prop StabilityTime(s) in prone prop (upper trunk off the floor, elbows anterior to shoulders) | 19.62/34.04 | Progressed ability to maintain stability from non-compliant to compliant surface |
| Stable Tailor SitTime(s) in upright tailor sit with head and trunk within 10 degrees of midline with external support provided no higher than pelvis | 4.56/35.69 | Caregiver improved ability to stabilize the child at an appropriate level | ||
| Stability in Extended Arm ProneSuccessful attempts (%) with bilateral UE extended in prone | 0/0 | |||
| 9 | Balance TrainingObstacle course for gait, balance and facilitation of transitional positions using toys of various heights; “Flamingo pose”: Single limb stance with caregiver providing UE support and cueing | Dynamic Balance During GaitPercentage of attempts a 4-inch obstacle was cleared when walking independently | 0/0 | Caregivers initiated interventions outside of scheduled therapy sessions |
| Static Standing BalanceMean number of seconds in static stance without UE support or stepping strategies | 0/2.56 | Caregivers improved cueing and level of assistance needed to perform interventions | ||
| Strengthening of bilateral LEsDynamic squatting with peanut ball between LEs; Standing hip flexor strengthening in single limb stance with bilateral UE support | Child increased the number of stairs he was able to ascend and descendChild was able to initiate stair climbing with less cueing | |||
| 11 | Facilitation of weight bearing and co-contraction of hip and shoulder girdleQuadruped positioning; Transitioning from quadruped to tall kneeling while rubbing shaving cream on vertical surface; Wheelbarrow walks with weight bearing through shoulder girdle | Static BalancePercentage of successful attempts child reached across midline while maintaining balance in sitting without upper or lower extremity support | 64.62/100 | Caregivers involved siblings in the therapy sessionsCaregiver confidence improved with instructing and directing therapeutic interventionsStudent communication to caregivers improved |
| Facilitation of weight shifting in stanceCruising around table to retrieve and open DVD case to find a cartoon character toy | Gait QualityMean number of steps the child took independently while cruising around family table | 2.13/1 | ||
| Facilitation of UE grasp in sitting and standing Music utilized to initiate UE reaching; Child motivated to reach for candy | Precision of GraspPercentage of successful attempts child held a spoon with a palmar supinate grasp during feeding compared to use of other grasp types | 0/40 | ||
| Middle Functional Levela | ||||
| 2 | Facilitation of transitional positionsMusical chairs to perform sit to stand transfers | Trunk Stability in Standing:Successful attempts (%) during reaching task in unsupported standing in which there was minimal postural sway and no stepping strategy | 18.5/10 | Caregiver improved level of preparation for therapy sessions |
| Balance Training/LE strengtheningSingle limb stance kicking a soccer ball | Single Limb StancePercentage of time in single limb stance with single UE support with minimal pelvic movement or trunk sway | 0/12.83 | Students improved rapport and communication with caregiver and child in the context of language barrier | |
| Stair Training Facilitation of appropriate sequencing on stairs | Reciprocal Stair ClimbingPercentage of steps foot cleared 7-inch step using unilateral UE support | 0/25 | Child improved initiation of a reciprocal pattern during stair climbing | |
| 4 | Core strengthening/Postural ControlSitting on large therapy ball while performing BUE activity; Tall kneeling on a couch cushion with ball toss | Postural Control: Single Limb StanceMean number of seconds in unsupported SLS without stepping strategy | 0/0 | Caregiver improved ability to instruct and encourage the child during therapy sessions |
| Stability in Tall kneelingPercentage of reaches in tall kneeling without loss of balance or protective response | 28.5/36.67 | |||
| Facilitation of fine motor skillsChalk drawing on deck with cues for dynamic tripod grasp; Placing beads on a string | Precision of Writing Grasp Percentage of initial grasps in writing tasks that utilized static/ dynamic tripod grasp | 75/58.33 | ||
| 6 | Balance TrainingStepping over tissue boxes, Tupperware and other household obstacles; Ambulation on grass including kicking and picking up rainbow playground ballAmbulation on couch cushions | Dynamic Balance in StandingPercentage of attempts a 6-inch or greater obstacle was cleared without loss of balance or stepping strategy | 56.75/75 | Caregivers improved level of preparation for the therapy sessionsSiblings helped with interventions and holding the camera |
| Strengthening of bilateral hip extensionSquat training; Step stance at the counter focused on hip extension | Gait QualityPercentage of steps taken with hip extended beyond neutral during stance phase | 14.40/8.93 | Student confidence improved and rapport was established with caregivers and patient | |
| Facilitation of UE use during ambulationCompletion of obstacle course while carrying household objects on a lunch tray | Dual Task PerformanceMean amount of time a lunch tray of items was carried while ambulating prior to loss of balance or dropped objects | 8.925/9.80 | ||
| 7 | Gait TrainingStepping over a stack of books to initiate foot clearance | Gait Quality: Foot clearancePercentage of steps taken on R in which there was no contact with floor during swing phase | 46/63.5 | Caregiver confidence and ability to provide the appropriate amount of positive feedback improved |
| Dynamic Balance Training Obstacle course incorporating stepping on sensory discs and couch cushions | Dynamic Balance During GaitPercentage of steps without use of UE support or stepping strategy to maintain balance | 50/88 | Students improved communicating feedback with caregivers | |
| Facilitation of grasp and releaseTurning pages of book for functional pincer grasp; Facilitation of reaching with R UE; Reaching for favorite toy to push buttons | Precision of GraspPercentage of grasps with R in which a pincer grasp was utilized (vs crude grasp) without verbal cues | 9/60.6 | ||
| 10 | Stair trainingAscending/descending stairs in home with use of handrails with focus on alternating steps | Stair ClimbingMean number of seconds to ascend and descend the full flight of steps in home | 40.84/110.1 | Although time to complete stairs increased, the child increased the number of alternating steps taken in a row with fewer verbal cues from caregivers |
| Facilitation of postural reactions and bilateral UE reachingReaching for food in supported standing at counter; Reaching for beads placed on the floor | Successful Reaching in stance Percentage of successful attempts to grasp a small object placed outside of base of support with either UE | 0/51.48 | Caregivers improved ability to incorporate appropriate incentives throughout the therapy sessions | |
| Dynamic Balance trainingSide stepping between chair and table | Dynamic Balance in stancePercentage of successful attempts child squatted to pick up an object and returned to stand without support | 55.19/50 | Caregivers improved verbal and tactile cues and feedback | |
| High Functional Levela | ||||
| Child | Exemplar Therapeutic Focus(s) Illustrative Intervention(s) | Target Behaviors Operational Definition | Pre/Postb | Observations |
| 3 | CIMT Placing toy cars in paper towel tube taped vertically to wall with constraint on | Right-Hand UsagePercentage of times child purposefully grasped and released an object with his R hand without verbal cues | 40.75/76.8 | Caregiver initiated therapeutic interventions outside of scheduled therapy sessions |
| Stair training Ascending and descending stairs and playset ladder to increase strength and facilitate reciprocal gait pattern | Stair ClimbingPercentage of steps negotiated with an alternating pattern | 14.08/0 | Noted improved quality of trunk movement during stair climbing | |
| Balance training Jumping on outdoor trampoline with decreasing levels of external support | BalancePercentage of attempted ball catches in standing without the use of a stepping strategy | 17.3/0 | Caregiver expressions of stress and anxiety during sessions decreased over time | |
| Dynamic BalancePercentage of steps taken on a compliant surface in which the child maintained an upright standing position | 40.9/42 | Child required less external support during activities | ||
| 5 | Facilitation of bilateral coordinationBasketball throwing and bouncing with BUE; Jumping jacks | Coordination/Bilateral IntegrationPercentage of jumping jacks performed with simultaneous and coordinated UE and LE movement | 29.07/29 | Caregiver confidence improved with instructing and directing therapeutic interventions |
| Dynamic Balance trainingKicking soccer ball; Playing basketball | Dynamic Standing Balance and CoordinationPercentage of attempts ball was successfully kicked the first time without stepping strategy | 0/0 | Students’ confidence and level of organization for the therapy sessions improved | |
| Single Limb StanceMean number of seconds in unsupported SLS without stepping strategy | 2.92/3.22 | Students improved in the use of demonstration of skills | ||
| 8 | Facilitation of transitional positions Duck Duck Goose game to initiate sit to stand from the floor | Floor transferPercentage of successful floor to stand transfers completed within 15 seconds | 40/85.95 | Caregiver improved ability to involve siblings in treatment sessions effectively |
| Balance TrainingObstacle course was navigated for gait, balance, and facilitation of transitional positions using everyday household items including kitchen table and chairs | Dynamic Standing Balance Percentage of obstacles on floor successfully navigated while ambulating without use of UE support or stepping strategies | 33.52/64.3 | Siblings helped initiate the interventions and improved level of assistance without interfering with therapy session | |
| Facilitation of grasp and releasePlacing marble in track that was vertically attached to refrigerator | Fine Motor PrecisionPercentage of successful attempts where marble was placed in track at eye level or higher | 58.35/0 | Progressed to using more challenging equipment during balance training | |
aThe children were categorized into three groups based on ability level: low, middle and high functioning. The low functioning group was defined as being unable to stand without external support, the middle functioning group as being able to stand and walk without upper extremity support, and the high functioning group as being able to run and jump. bBold indicates an improvement between pre and post treatment (unit of measurement either percentage or mean based on operational definition). BUE: bilateral upper extremities; CIMT: contraint induced movement therapy; LE: lower extremity; R: right; SLS: single leg stance; UE: upper extremity.
A variety of interventions were performed to target the goals designated for each child based on their functional level (Table 2). The low-functioning group was defined as being unable to stand without external support, the middle-functioning group as being able to stand and walk without upper extremity support, and the high-functioning group as being able to run and jump. For example, with goals related to balance training, children who were lower functioning performed interventions such as stepping over obstacles, standing still without upper extremity support, and reaching outside their base of support. Those categorized as middle functioning performed interventions such as clearing higher obstacles, maintaining balance in a single limb stance position, and ambulating without losing balance while holding an item with their upper extremities. Children categorized as higher functioning completed balance interventions such as ambulating over compliant surfaces, navigating obstacles of varying heights, maintaining single limb stance, and catching a ball without losing balance.
Each of the 11 children had different learning opportunities. Some had limited learning opportunities including one who lived in a group home, while others had extensive ones available to them. For those who had more resources available, there was a greater opportunity for incorporation of those resources into the treatment plan with the use of a variety of toys and other items. For example, one child had a trampoline which was used in treatment. Those with limited resources required greater creativity from the students and families for intervention implementation. In every case, various items were used in place of traditional PT clinical tools such as using couch cushions as a compliant surface or a tissue box as an obstacle to step over. The children’s siblings assisted in therapy in several ways including holding the camera, helping to stabilize the child being treated, helping to pass an item back and forth, retrieving items needed for the session, and demonstrating the activity to the child (e.g., follow the leader). In one case, an older adult sibling, with help from additional siblings, directed the session when their mother was not available for that session.
2.5Analysis of pediatric PT and CLE outcomes
All researchers performed an initial review of the videotaped recordings and the student documentation. Given the challenges with measurement via telehealth [18, 51] and that the researchers were reviewing videotaped recordings and the student progress notes, the researchers were unable to perform direct objective outcome measures to evaluate the child’s progress and therefore established target behaviors. After the initial review of documentation and video recordings, the researchers held several consensus meetings to establish the target behaviors and their operational definitions based on the goals set for each child and the observed focuses of the therapy (Table 2). Target behaviors were developed to assess quantitative outcomes based on the therapeutic focuses for each child. Each recorded session was then analyzed independently by two researchers (CM, MT, CD, or AH) to assess the target behaviors as well as subjective and qualitative outcomes. These researchers did not participate in the CLE. Consensus meetings were held to resolve any discrepancies between reviewers.
Upon completion of the retrospective analyses of the video recordings and documentation of the experience, the researchers sought to examine the participants’ perspectives on the feasibility and acceptability of both the PT and CLE. To do this, questionnaires were developed and distributed to the caregivers, CIs, and students who participated in the experience. The questionnaires were adapted from published ones examining the feasibility and acceptability of similar models [52, 53]. Additionally, to assess the perspectives regarding the CLE, questions were developed regarding how the experience addressed relevant items evaluated on the Clinical Performance Instrument (CPI), which is a validated measure utilized to evaluate PT student performance in their full-time CLEs [54]. The questionnaires were piloted to two experts in survey development and their feedback was incorporated prior to distribution. The questionnaires were distributed electronically 18 months after the experience and data were analyzed using Qualtrics Software (Qualtrics XM, Provo, UT).
3Results
3.1Outcomes: General observations
Over time, several observations were made in relation to the pediatric PT telehealth experience. At the beginning of the sessions, caregivers seemed nervous and provided limited assistance outside of what was asked by the students. As the sessions continued, some caregivers reported they had initiated novel activities outside of the scheduled telehealth sessions related to the therapeutic focuses they were working on within the sessions. An example included a caregiver continuing the fine motor activity throughout the week using small crackers and a small container during snack time to encourage carryover and progression of the activity. It was also noted that caregivers asked more questions and provided more input on new therapeutic ideas in order to better assist their child during the therapy sessions in the home as the sessions progressed. Inclusion of siblings in sessions also increased over time. This appeared to increase the engagement of the child in the session and decrease caregiver stress associated with caring for multiple children while participating in the therapy session. Over time, siblings assumed different roles within therapy sessions including performing the interventions, encouraging their sibling to actively participate in therapy, motivating their sibling, and helping the caregiver manage the computer or other device used for video communication. This allowed the caregiver to increase focus on the intervention, therapist instruction, and feedback.
Some technological issues were encountered during the sessions which limited carrying out interventions and assessment of results. These issues were experienced with six of the 11 children. The primary issue was a weak or disrupted internet connection, which often occurred when there was a change of location of treatment within the home, moving room to room, or when the session was relocated outside. The most common issues included a freezing or delayed screen, poor quality audio, or a decrease in the video quality. When these issues occurred, observations became obscured and it was difficult to visualize what was occurring at that point in the session for the students and CIs carrying out the interventions, as well as for the researchers’ video analyses. Of the six children with technological issues, one child had issues during every session while the others had issues occur in approximately 50% of the sessions. Poor internet connectivity occurred primarily with those families using phones rather than computers and those in more remote areas with limited broadband service availability. It also occurred frequently with those who changed location during the sessions for interventions that required a different room or being outside the home. Additionally, in some cases, the camera angle was not optimal for viewing certain tasks. This occurred with approximately 25% of the tasks analyzed. This was more likely to occur when there was only one parent or caregiver present, due to the difficulty of adjusting the camera angle while implementing the treatment and maintaining the safety of the child. These suboptimal camera angles also occurred more frequently in the higher-functioning children because the camera had to be moved throughout the sessions since the child was more mobile.
3.2Outcomes: Response to PT
Based on video analyses, all 11 children made qualitative and quantitative improvements in at least one target behavior (Table 2). Quantitative improvements were noted in 62.5% of the target behaviors of the children in the low-functioning group and in 64.3% and 50% of the children in the middle- and high-functioning groups, respectively. Children who made progress in more target behaviors were more likely to have more family members present during the sessions while those who made less improvement were more likely to have only one caregiver participating, substantial distractions within the environment, limited time between sessions, and limited access to resources. For example, the four children who had only one person present during the sessions made progress in five of the 12 (41.7%) target behaviors while the seven children with more than one person present (including siblings) made progress in 14 of the 21 target behaviors (66.7%).
Categorically, improvements were noted most in target behaviors related to static balance, dynamic balance, and stair navigation. All of the children with static balance as a target behavior showed improvement in this area, while 57% of the children with dynamic balance as a target behavior improved. While only 33% of children improved quantitatively in stair navigation, all of the children demonstrated qualitative improvements in stair climbing. Qualitative observations for improved stair navigation included decreased verbal cues needed, increased initiation of a reciprocal pattern, and an increase in the quality of trunk movement. Sixty-seven percent of the target behaviors related to grasp and upper extremity use and 71% of the target behaviors involving developmental and transitional positions showed improvements. Qualitative improvements were seen in transitional positions as noted through observations of progression to compliant surfaces, decreased level of support required, and use of more challenging equipment to complete tasks.
3.3Outcomes: Perspectives of experience
Ten of the 12 (83%) CIs, seven of the 12 (58%) caregivers, and 21 of the 54 (38%) students responded to the survey. Seventy-six percent of student respondents were female and the mean (standard deviation [SD]) age was 26.3 (1.4) years. The amount of prior experience with children (in any capacity) in student respondents varied from no experience (5%) to more than five years (29%). CI respondent demographics are presented in Table 3. Seventy percent of CI respondents and 90.5% of student respondents had little to no experience with telehealth prior to this experience. Following this experience, the average level of student interest based on a 100-point scale, ranging from no interest to complete interest, increased in both pediatrics (45.2 to 52.9) and telehealth (40.3 to 64.1).
Table 3
Clinical instructor demographics
| Age (mean (SD)) | 44.78 (9.92) |
| Gender (N (%)) | |
| Female | 10 (100%) |
| Male | 0 (0%) |
| Highest academic degree earned (N (%)) | |
| Bachelor’s degree | 2 (20%) |
| Master’s degree | 2 (20%) |
| Doctorate degree (DPT, tDPT, PhD) | 6 (60%) |
| Highest level physical therapy degree earned (N (%)) | |
| Bachelor’s degree | 2 (20%) |
| Master’s degree | 2 (20%) |
| Doctorate degree | 6 (60%) |
| ABPTS board certified clinical specialist (N (%)) | |
| Yes | 4 (40%) |
| No | 6 (60%) |
| Years practicing as a physical therapist (mean (SD)) | 18.8 (10.43) |
| Years of pediatric clinical experience (mean (SD)) | 15.8 (9.30) |
| Pediatric physical therapy practice settings (N (%)) | |
| Outpatient | 8 (28%) |
| Inpatient | 3 (10%) |
| Early intervention | 5 (17%) |
| Home care | 1 (3%) |
| School setting | 2 (7%) |
| Other (aquatics, orthotics casting, telehealth, NICU) | 2 (7%) |
| Academic | 8 (28%) |
| Years of experience as a clinical instructor (mean (SD)) | 16.1 (9.52) |
| Prior knowledge and experience with telehealth (N (%)) | |
| No knowledge or experience | 2 (20%) |
| Familiar but little knowledge and no experience | 5 (50%) |
| Extensive knowledge but no actual experience | 0 (0%) |
| Some knowledge and experience | 2 (20%) |
| Extensive knowledge and experience | 1 (10%) |
SD: standard deviation.
3.4Perspectives on the provision of PT
All CIs, students, and caregivers believed that the children and caregivers were able to work towards their PT goals during the experience. All Cis and caregivers, as well as 95% of students, believed the children benefited from the experience. In addition, all CIs believed that the students were able to build a connection with the caregivers, and 95% of students said the same. Seventy-one percent of caregivers believed they were able to build a connection with the students but only 54% of the caregivers believed the students were able to build a connection to the child. Eighty-six percent of caregivers believed they were able to effectively implement the interventions as instructed via telehealth and the remaining 14% were neutral on their ability. Ninety percent of the CIs and 86% of caregivers believed they could understand the clinical reasoning behind the PT interventions delivered via telehealth while the remaining respondents were neutral on their ability to understand the reasoning. All of the caregivers reported that they continued to implement some (80%) or all (20%) of the recommendations provided during the experience with most caregivers reporting that the reason for stopping implementation was shifting of goals and child progress (Fig. 1).
Fig. 1
Perspectives of the students (A), CIs (B), and caregivers (C) on the telehealth PT and learning experience from questionnaires. The percentage of students (A), CIs (B), and caregivers (C) who agreed/ disagreed with statements regarding the ability to benefit from the experience in regards to physical therapy intervention and student learning.
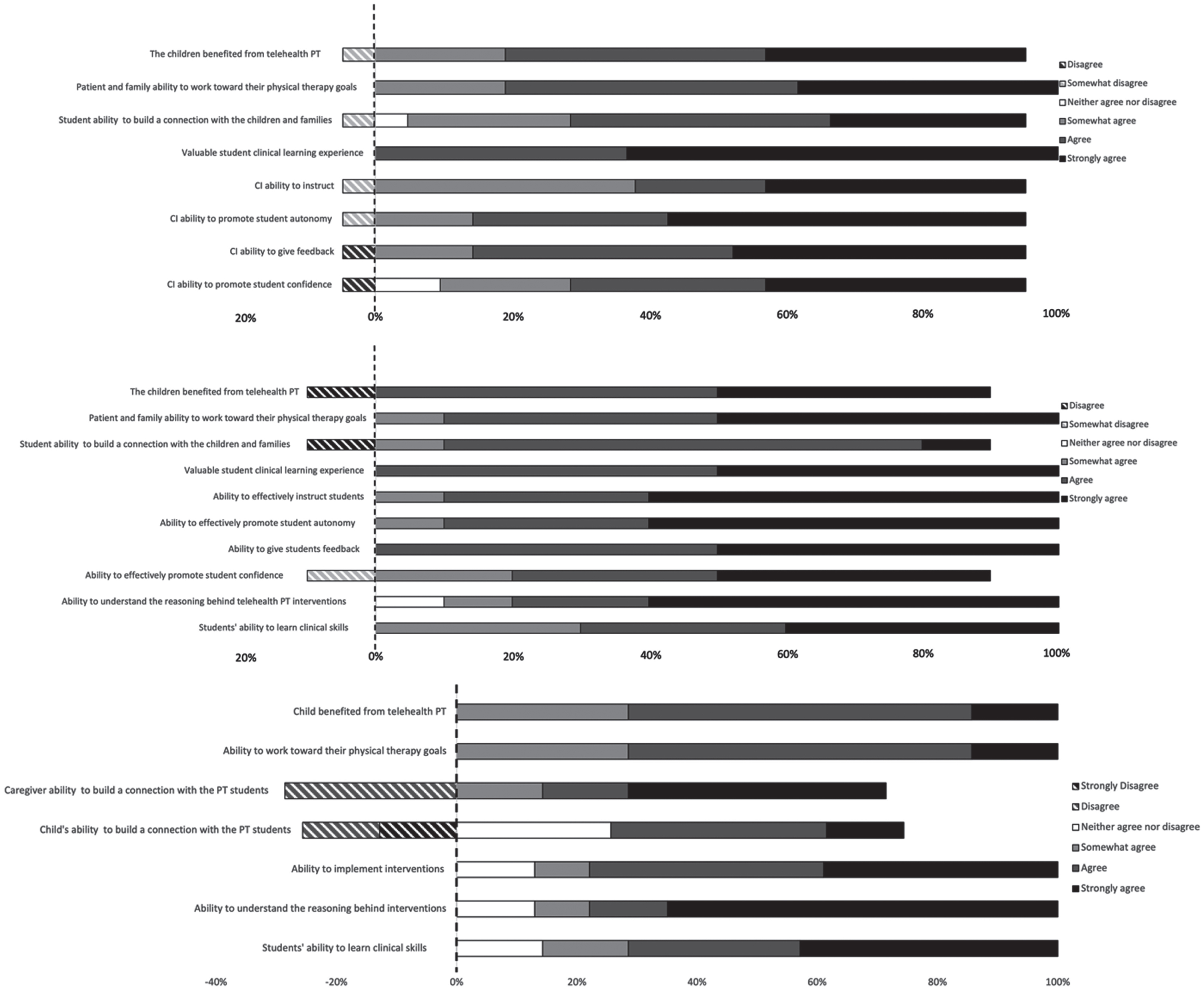
3.5Perspectives on the CLE
All CIs and all students believed that it was a valuable student CLE. All CIs and 95% of students believed the CIs were able to effectively instruct, provide feedback, and promote student autonomy via telehealth. Ninety percent of CIs and 86% of students also believed that CIs were able to promote student confidence through the learning experience. All CIs and 86% of families felt that the students were able to learn clinical skills through the experience while the remaining 14% of families were neutral (Fig. 1A–C).
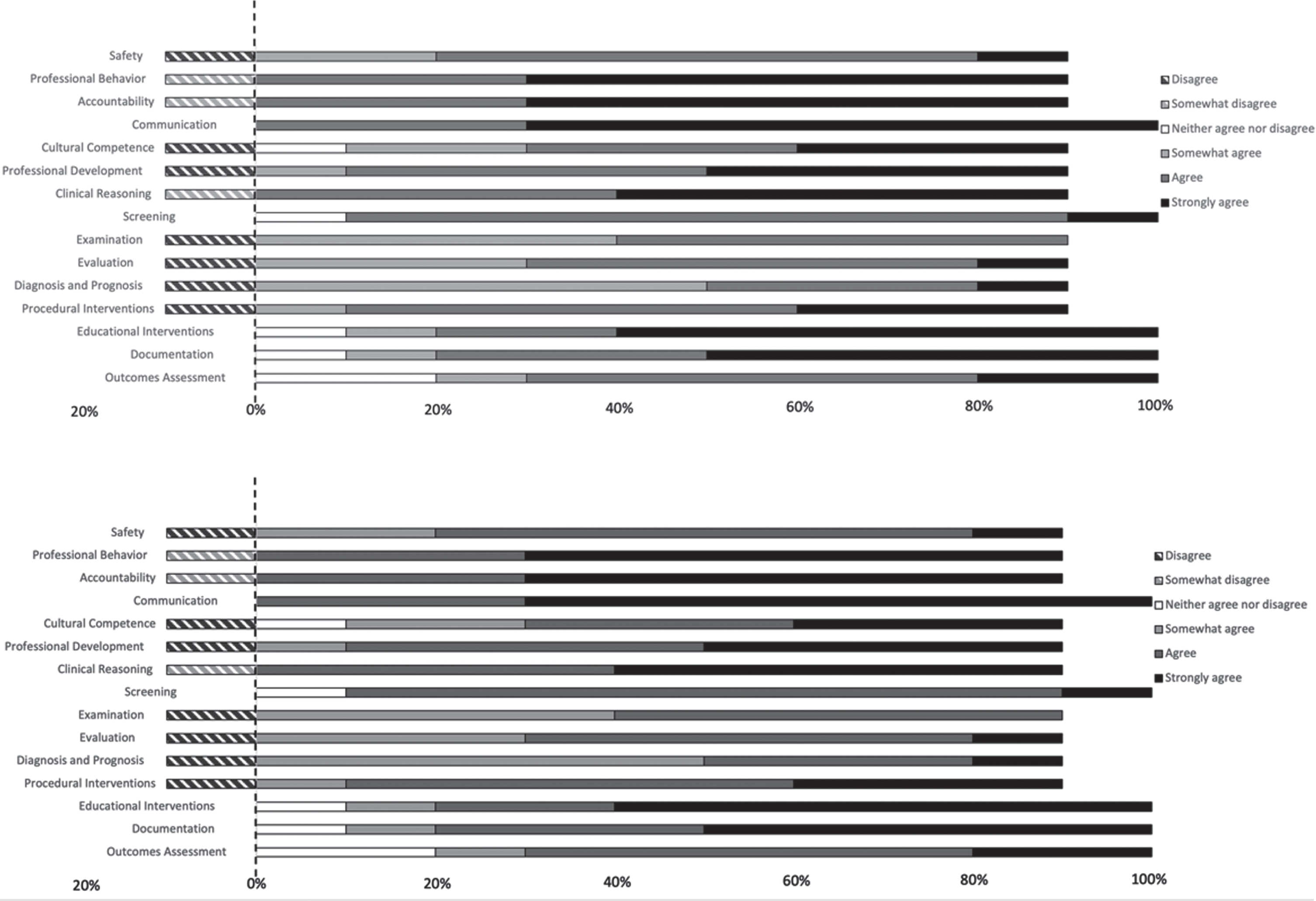
For 13 of the 15 relevant CPI domains, 90% or more of CIs believed the students were able to effectively learn. Eighty percent of CIs believed the students were able to effectively learn in the remaining domains (cultural competence and outcomes assessment). For 10 of the 15 relevant CPI domains, 90% or more of the students believed they were able to effectively learn. For the remaining domains, 86% believed they effectively learned in screening, 81% in examination, evaluation, and outcomes assessment while 71% believed they effectively learned in diagnosis and prognosis (Fig. 2).
Fig. 2
Perspectives of the students (A) and CIs (B) on the student ability to learn clinical skills in the 15 relevant CPI domains. The percentage of students (A) or CIs (E) who agreed/ disagreed with the statement “I feel that I was able to effectively learn clinical skills in the area of () through telehealth” is depicted. CPI: Clinical Performance Instrument.
3.6Qualitative perspectives
Students, CIs, and caregivers provided qualitative perspectives comparing the in-person delivery of PT and education to the delivery via telehealth (Appendix). The most commonly reported benefit of telehealth delivery by students and CIs was an increase in family engagement in therapy because of the “forced” nature of family involvement inherent to telehealth.
Students, CIs, and caregivers commented on the improved access to services with the telehealth delivery for both medically complex patients and patients whose access is limited by distance. The telehealth delivery was believed to be more convenient. One caregiver commented that it was less distracting and overwhelming to the child, particularly with multiple students present. The benefits of treating in the child’s natural environment was noted several times by both CIs and students, including the more meaningful nature of treating in the child’s home with the child’s family and toys.
In the area of student learning, several benefits of telehealth were noted including increased autonomy, learning of communication skills, patient/caregiver education skills, developing creativity, and ability to learn from peers. CIs also noted the benefit of increased discussion with the group for reflection without the family present (i.e., before and after the family joined the session). Finally, it was noted that having experience with telehealth is an important skill for the future.
CIs, students, and caregivers expressed the benefits of in-person therapy over telehealth. Manual contact and assessment were the most common limitations reported for telehealth. The lack of manual contact was thought to limit demonstration, ability to assess accurately, and provision of appropriate sensory cues. Interestingly, one CI noted that the lack of hands-on education might actually improve student skill development in that it forced students to verbalize the knowledge behind the skill. Challenges including visualization, technology, and safety were also noted with telehealth. Inability to visualize appeared to limit the assessment of performance most. Interpersonal connections and the ability to “play” were considered better in-person. This viewpoint was more strongly communicated by caregivers than it was by CIs or students. One perspective that emerged from the caregivers was the benefit of a hybrid model in which the caregiver could learn in person and practice at home with guidance via telehealth. Caregiver comments suggest that familiarity with PT improves the telehealth experience.
4Discussion
A retrospective evaluation was conducted of a novel pediatric telehealth collaborative CLE in which children with various levels of support and resources and of various ages and diagnoses participated. Based on empirical and subjective evidence, this model of delivery for pediatric PT appeared to benefit the children and their families. This report describes a model for a clinical experiential learning experience for PT students in both telehealth and pediatric settings that was feasible, easily implemented, and had perceived efficacy and benefits.
The current model illustrated the breadth and depth of pediatric PT that is possible through telehealth. The interventions implemented via telehealth ranged from developmental positioning and facilitation of fine motor skills, to higher level gait and balance training. Prior studies examining the telehealth delivery of health care services in pediatrics have primarily focused on therapies such as Applied Behavior Analysis (ABA) to target children on the autism spectrum [55, 56]. The limited literature examining the telehealth delivery of pediatric PT has focused predominantly on therapist perspectives of telehealth service delivery [1, 17]. Outside of the single case analysis from which the current report was based [18], the present evaluation is the first report to describe the nature of the interventions performed and the target behaviors of pediatric PT via telehealth. The interventions delivered via telehealth were able to capitalize on the learning opportunities within the children’s natural environment, such as with toy cars, paper towel holders, couch cushions, chalk, playground sets, trampolines, and play sets. While the lack of typical therapeutic equipment was considered a challenge in this telehealth model by both therapists and students, this forced the students to be more creative with their interventions which is a critical aspect of pediatric PT. Furthermore, this lack of equipment is a challenge faced by families trying to implement PT interventions in the home. Because caregivers in the present model reported using, adapting, and progressing these learning opportunities in between sessions, it is hypothesized that the utilization of resources already in the children’s environments enhanced the carryover. Because the treatment occurred in the child’s natural environment in which they interact in each day, the therapy itself was more meaningful [23, 47].
While students and instructors perceived examination and assessment as more challenging in this telehealth model, empirical analyses of target behaviors suggested that the children progressed even though the intensity and duration of the experience were limited. Specifically, all of the children progressed in at least one target behavior and progress was noted in a wide variety of target behaviors across all of the children. The biggest challenges reported in the present model related to lack of hands-on assessment and difficulty observing the children due to suboptimal camera angles or poor internet connectivity. This has been widely reported in the telehealth literature [5, 25, 56]. While recommendations have been published on performing assessments via telehealth in the pediatric population [7], there is very limited evidence on the use of motor assessments via telehealth in adults with neurologic conditions [48, 49]. Only one study was identified specifically in the pediatric population [50]. This is clearly an area in need of further investigation.
The present study documented several important observations over time in addition to changes in target behaviors. Across the cases, caregivers reported feelings of stress and anxiety in performing the interventions due to the lack of manual assistance from the therapists. The caregivers’ responsibility to maintain camera angles while simultaneously monitoring the child’s behavior and attention and performing the interventions appeared to instill a level of stress and anxiety in the caregivers. However, the reports and observations of caregiver anxiety decreased in most of these cases as the sessions progressed and the caregivers’ confidence appeared to increase. Therefore, a hybrid model of service delivery in which in-person sessions precede telehealth sessions might help to mitigate the stress associated with implementation. This hybrid model might also serve to enhance the building of interpersonal connections that were perceived to be more difficult with telehealth.
Sibling involvement in the sessions also increased over time in the present study. For some, the presence of siblings during therapy was initially distracting and stressful for the caregivers but this decreased over time as the siblings became more involved in the therapeutic sessions. The siblings assisted the caregivers with the intervention itself, motivated the child to participate, and even assisted the parent with technological support. Consistent with the literature [57], siblings positively influenced the learning opportunities and rehabilitation of children with disabilities. While the caregivers demonstrated and reported anxiety with the telehealth experience due to the responsibilities inherent in this mode of delivery, the active engagement of the caregivers appeared to increase caregiver involvement in between sessions. Such active engagement has been associated with empowerment and confidence [17, 18] and is consistent with findings reported with the utilization of the coaching method [31, 32]. Enhanced caregiver involvement has been associated with improved motor development in the child and quality of life for both the child and the family [30, 31, 34–36]. Therefore, utilization of the model described in the current study may not only increase the access of PT to families in remote areas, with transportation issues, or medically fragile children, but it may also serve to enhance outcomes associated with PT for children and their families.
The novel collaborative learning experience described in this report provided a model that can be used to address the documented need for the integration of experiential learning into the didactic portion of the curriculum in two critical areas: pediatrics and telehealth [58, 59]. The experiential CLE described appeared to be both feasible and effective based on data triangulated from videotape analyses as well as the perspectives of CIs, students, and caregivers. The majority of CIs, students, and caregivers believed this was an effective CLE. This experience was also believed to promote the confidence and autonomy of students, which was consistent with the qualitative case analysis of this model from which the present study was based [18]. While the CPI was not utilized in the model described, as this model is not considered a clinical education experience, both students and CIs believed that the CLE promoted the development of most of the domains targeted on the CPI, suggesting that this learning model would effectively develop clinical skills. Given the challenges reported with examination and assessment, it is not surprising that the domains associated with these skills were considered to be least effectively learned through telehealth.
There are several aspects of the current model that may have contributed to the perceived student learning. First, the literature suggests that experiential learning improves the understanding and application of course material including professional skills, interpersonal skills, and clinical skills [60–67]. Second, the collaborative nature of this model, including active observation, peer feedback (via the chat feature), treatment planning, and reflection (via planning meetings and assignments) were consistent with the enhanced learning reported in in-person collaborative experiences [68–70]. In addition to the perception of learning that occurred through this model, student interest in both pediatrics and telehealth increased, suggesting that the experience influenced not only cognitive but also affective domains. Students and CIs had minimal to no experience with telehealth prior to the experience, but after the experience most felt that telehealth should be continued as a venue for service delivery. This speaks to the perceived value of telehealth in clinical practice. Given that touch and personal connection (two areas perceived as limitations in the present model) are foundational aspects of the delivery of PT, it will never be replaced by telehealth. However, the widespread adoption of telehealth due to the COVID-19 pandemic has illuminated the many benefits of this model in the years to come. The perspectives reported in the present evaluation along with those in the literature strongly suggest that clinicians will continue to utilize telehealth as a mode of service delivery, highlighting the importance of developing effective learning experiences in telehealth for future clinicians.
Limitations of the present study must be considered. First, all analyses were completed retrospectively after the model was completed. The questionnaires were not distributed until 18 months after the experience and therefore recall bias must be considered. Second, established objective measures of the outcomes associated were not completed. The literature supports the challenge of assessment via telehealth [18, 51]. While recommendations have been published on performing assessments via telehealth in the pediatric population [7, 47], there is very limited evidence about the use of motor assessments via telehealth in adults with neurologic conditions [48, 49]. Only one study was identified specifically in the pediatric population [50]. Future studies are needed to examine measurement and assessment through telehealth. Furthermore, the empirical analyses in the present study were conducted on recordings of sessions that were not intended to be systematically analyzed. Inconsistent connectivity and suboptimal camera angles limited the systematic analyses. Because the purpose of developing the model was to provide an experiential learning experience in pediatric PT during the pandemic, objective and validated assessments of both the efficacy of the PT performed and the student learning were not completed. In addition, the model involved only four to five sessions for each child, and therefore, limited progress could be expected. Additionally, while 12 children and their families participated in the model, the videotaped sessions could only be retrieved for 11 of the children. Nevertheless, the wide range of child/family characteristics, the progress that was observed, and the positive perspectives of CIs, students, and caregivers strongly support the continued implementation of this model for both the delivery of service and clinical education. Systematic analyses of child/family and student outcomes associated with this model are warranted. While acceptable response rates for research have certainly been declining [71], the response rate for the student questionnaire (38%) must be considered a limitation. The higher response rates from caregivers and CIs and the consistency of their perspectives with those found for students does, however, support the trustworthiness of the student data and the overall findings.
5Conclusions
The delivery of pediatric PT via telehealth is feasible and has perceived benefits and efficacy for a wide range of children. This model provides a means of increasing access to pediatric PT that utilizes the natural environment and promotes family engagement. Additionally, this model provides a unique collaborative CLE for students in both pediatric PT and telehealth that appears to be effective across all domains based on the perceptions of CIs, students, and families.
Acknowledgments
The authors have no acknowledgements or funding to report.
Conflict of interest
There were no conflicts of interests.
Ethical considerations
The study was approved by the Shenandoah University Institutional Review Board (#983).
References
[1] | Hall JB , Woods ML , Luechtefeld JT . Pediatric physical therapy telehealth and COVID-19: Factors, facilitators, and barriers influencing effectiveness—a survey study. Pediatr Phys Ther. (2021) ;33: (3):112–8. doi: 10.1097/PEP.0000000000000800. |
[2] | Dietzen A , Ide W , Pavone L . Telehealth in pediatric rehabilitation medicine: A survey of clinician reported utilization and experience. J Pediatr Rehabil Med. (2020) ;13: (3):281–8. doi: 10.3233/PRM-200762. |
[3] | Marcin JP , Shaikh U , Steinhorn RH . Addressing health disparities in rural communities using telehealth. Pediatr Res. (2016) ;79: (1):169–76. doi: 10.1038/pr.2015.192. |
[4] | Bland KA , Bigaran A , Campbell KL , Trevaskis M , Zopf EM . Exercising in isolation? The role of telehealth in exercise oncology during the COVID-19 pandemic and beyond. Phys Ther. (2020) ;100: (10):1713–6. doi: 10.1093/ptj/pzaa141. |
[5] | Burke BL , Hall RW , Dehnel PJ , et al. Telemedicine: Pediatric applications. Pediatrics. (2015) ;136: (1):e293–308. doi: 10.1542/peds.2015-1517. |
[6] | Tenforde AS , Borgstrom H , Polich G , et al. Outpatient physical, occupational, and speech therapy synchronous telemedicine: A survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. Am J Phys Med Rehabil. (2020) ;99: (11):977–81. doi: 10.1097/PHM.0000000000001571. |
[7] | Rabatin AE , Lynch ME , Severson MC , Brandenburg JE , Driscoll SW . Pediatric telerehabilitation medicine: Making your virtual visits efficient, effective and fun. J Pediatr Rehabil Med. (2020) ;13: (3):355–70. doi: 10.3233/PRM-200748. |
[8] | Leonardsen ACL , Hardeland C , Helgesen AK , Grøndahl VA . Patient experiences with technology enabled care across healthcare settings- a systematic review. BMC Health Serv Res. (2020) ;20: (1):779. doi: 10.1186/s12913-020-05633-4. |
[9] | McConnochie KM , Wood NE , Herendeen NE , ten Hoopen CB , Roghmann KJ . Telemedicine in urban and suburban childcare and elementary schools lightens family burdens. Telemed J E Health. (2010) ;16: (5):533–42. doi: 10.1089/tmj.2009.0138. |
[10] | Kennedy CA , Warmington K , Flewelling C , et al. A prospective comparison of telemedicine versus in-person delivery of an interprofessional education program for adults with inflammatory arthritis. J Telemed Telecare. (2017) ;23: (2):197–206. doi: 10.1177/1357633X16635342. |
[11] | Paul L , Coulter EH , Miller L , McFadyen A , Dorfman J , Mattison PGG . Web-based physiotherapy for people moderately affected with multiple sclerosis; quantitative and qualitative data from a randomized, controlled pilot study. Clin Rehabil. (2014) ;28: (9):924–35. doi: 10.1177/0269215514527995. |
[12] | Tousignant M , Boissy P , Corriveau H , Moffet H , Cabana F . In-home telerehabilitation for post-knee arthroplasty: A pilot study. Int J Telerehab. (2009) ;1: (1):9–16. doi: 10.5195/ijt.2009.5997. |
[13] | Chatto CA , York PT , Slade CP , Hasson SM . Use of a telehealth system to enhance a home exercise program for a person with Parkinson Disease: A case report. J Neurol Phys Ther. (2018) ;42: (1):22–9. doi: 10.1097/NPT.0000000000000209. |
[14] | Lee AC , Davenport TE , Randall K . Telehealth physical therapy in musculoskeletal practice. J Orthop Sports Phys Ther. (2018) ;48: (10):736–9. doi: 10.2519/jospt.2018.0613. |
[15] | Lee ACW , Billings M . Telehealth implementation in a skilled nursing facility: Case report for physical therapist practice in Washington. Phys Ther. (2016) ;96: (2):252–9. doi: 10.2522/ptj.20150079. |
[16] | Seron P , Oliveros MJ , Gutierrez-Arias R , et al. Effectiveness of telerehabilitation in physical therapy: A rapid overview. Phys Ther. (2021) ;101: (6):pzab053. doi: 10.1093/ptj/pzab053. |
[17] | Hall JB , Luechtefeld JT , Woods ML . Adoption of telehealth by pediatric physical therapists during COVID-19: A survey study. Pediatr Phys Ther. (2021) ;33: (4):237–44. doi: 10.1097/PEP.0000000000000817. |
[18] | Fergus A , Hartsook K , Smith J , Hale M , Kellar D . A novel physical therapy learning experience in pediatrics via telehealth: A qualitative case analysis. JOPTE. (2021) ;35: (2):159–67. doi: 10.1097/JTE.0000000000000184. |
[19] | Gefen N , Steinhart S , Beeri M , Weiss PL . Lessons learned during a naturalistic study of online treatment for pediatric rehabilitation. IJERPH. (2021) ;18: (12):6659. doi: 10.3390/ijerph18126659. |
[20] | Camden C , Pratte G , Fallon F , Couture M , Berbari J , Tousignant M . Diversity of practices in telerehabilitation for children with disabilities and effective intervention characteristics: results from a systematic review. Disabil Rehabil. (2020) ;42: (24):3424–36. doi: 10.1080/09638288.2019.1595750. |
[21] | McManus BM , Carle AC , Poehlmann J . Effectiveness of Part C early intervention physical, occupational, and speech therapy services for preterm or low birth weight infants in Wisconsin, United States. Acad Pediatr. (2012) ;12: (2):96–103. doi: 10.1016/j.aca2011.11.004. |
[22] | Blauw-Hospers CH , Hadders-Algra M . A systematic review of the effects of early intervention on motor development. Dev Med Child Neurol. (2005) ;47: (6):421–32. doi: 10.1111/j.1469-8749.2005.tb01165.x. |
[23] | Dunst CJ , Bruder MB , Espe-Sherwindt M . Family capacity-building in early childhood intervention: Do context and setting matter? Sch Commun J ((2014) ;24: (1), 37–48. |
[24] | Bailey DB , Hebbeler K , Spiker D , Scarborough A , Mallik S , Nelson L . Thirty-six-month outcomes for families of children who have disabilities and participated in early intervention. Pediatrics. (2005) ;116: (6):1346–52. doi: 10.1542/peds.2004-1239. |
[25] | Iacono T , Dissanayake C , Trembath D , Hudry K , Erickson S , Spong J Family and practitioner perspectives on telehealth for services to young children with autism. In: Maeder AJ, Ho K, Marcelo A,Warren J, editors. Studies in Health Technology and Informatics. 231st volume. Amsterdam: IOS Press; 2016. pp. 63-73. |
[26] | Dunst CJ , Trivette CM , Hamby DW . Meta-analysis of family-centered help giving practices research. Ment Retard Dev Disabil Res Rev. (2007) ;13: (4):370–8. doi: 10.1002/mrdd.20176. |
[27] | Fergus A . A novel mobility device to improve walking for a child with cerebral palsy. Pediatr Phys Ther. (2017) ;29: (4):E1–7. doi: 10.1097/PEP.0000000000000451. |
[28] | Harniess PA , Gibbs D , Bezemer J , Purna Basu A . Parental engagement in early intervention for infants with cerebral palsy—A realist synthesis. Child. (2022) ;48: (3):359–77. doi: 10.1111/cch.12916. |
[29] | Akhbari Ziegler S , Hadders-Algra M . Coaching approaches in early intervention and paediatric rehabilitation. Dev Med Child Neurol. (2020) ;62: (5):569–74. doi: 10.1111/dmcn.14493. |
[30] | Dirks T , Hadders-Algra M . The role of the family in intervention of infants at high risk of cerebral palsy: a systematic analysis: Review. Dev Med Child Neurol. (2011) ;53: (Suppl 4):62–7. doi: 10.1111/j.1469-8749.2011.04067.x. |
[31] | Dirks T , Hielkema T , Hamer EG , Reinders-Messelink HA , Hadders-Algra M . Infant positioning in daily life may mediate associations between physiotherapy and child development—video-analysis of an early intervention RCT. Res Dev Disabil. (2016) ;53-54: :147–57. doi: 10.1016/j.ridd.2016.02.006. |
[32] | Akhbari Ziegler S , Mitteregger E , Hadders-Algra M . Caregivers’ experiences with the new family-centred paediatric physiotherapy programme COPCA: A qualitative study. Child Care Health Dev. (2020) ;46: (1):28–36. doi: 10.1111/cch.12722. |
[33] | Van Balen LC , Dijkstra LJ , Dirks T , Bos AF , Hadders-Algra M . Early intervention and postural adjustments during reaching in infants at risk of cerebral palsy. Pediatr Phys Ther. (2019) ;31: (2):175–83. doi: 10.1097/PEP.0000000000000585. |
[34] | Hielkema T , Hamer EG , Boxum AG , et al. LEARN 2 MOVE 0 to 2 years: developmental outcome of an early intervention randomized controlled trial in infants at very high risk for cerebral palsy. Dev Med Child Neurol. (2016) ;58: (S6):56. doi: 10.1111/dmcn.13322. |
[35] | McCarthy M , Leigh G , Arthur-Kelly M . Telepractice delivery of family-centred early intervention for children who are deaf or hard of hearing: A scoping review. J Telemed Telecare. (2019) ;25: (4):249–60. doi: 10.1177/1357633X18755883. |
[36] | Blauw-Hospers CH , Dirks T , Hulshof LJ , Bos AF , Hadders-Algra M . Pediatric physical therapy in infancy: from nightmare to dream? A two-arm randomized trial. Phys Ther. (2011) ;91: (9):1323–38. doi: 10.2522/ptj.20100205. |
[37] | Simkins J Innovations in Telehealth. Alexandria, VA: APTA; 2017 [cited 10 October 2022]. Available from: https://www.apta.org/aptamagazine/2017/04/01/innovations-in-telehealth |
[38] | Brennan D , Tindall L , Theodoros D , et al. A Blueprint for Telerehabilitation Guidelines. Int J Telerehab. (2010) ;2: (2):31–4. doi: 10.5195/ijt.2010.6063. |
[39] | Telehealth in Physical Therapy Alexandria, VA: The Federation of State Boards of Physical Therapy [cited 10 October 2022]. Available from: https://www.fsbpt.org/FreeResources/RegulatoryResources/TelehealthinPhysicalTherapy.aspx |
[40] | APTA Learning Center Alexandria, VA: APTA [cited 10 October 2022]. Available from: https://learningcenter.apta.org/ |
[41] | Ross MH , Whitehead A , Jeffery L , Hartley N , Russell T . Supervising students during a global pandemic: Clinical educators’ perceptions of a student-led telerehabilitation service during COVID-19. Int J Telerehab. (2022) ;14: (1):e6464. doi: 10.5195/ijt.2022.6464. |
[42] | Watzlaf VJM , Moeini S , Firouzan P . VOIP for telerehabilitation: A risk analysis for privacy, security, and HIPAA compliance. Int J Telerehab. (2010) ;2: (2):3–14. doi: 10.5195/ijt.2010.6056. |
[43] | Ramey CT , Ramey SL . Early learning and school readiness: Can early intervention make a difference? Merrill-Palmer Q. (2004) ;50: (4), 471–91. |
[44] | Workgroup on Principles and Practices in Natural Environments Seven Key Principles: Looks Like/Doesn’t Look Like. OSEP TA Community of Practice: Part C Settings; 2008 [cited 11 October 2008]. Available from: https://ectacenter.org/ pdfs/topics/families/Principles_LooksLike DoesntLookLike3_11_08.pdf |
[45] | McLean ME , Snyder P , Smith BJ , Sandall SR . The DEC recommended practices in early intervention/early childhood special education: Social validation. J Early Interv. (2002) ;25: (2):120–8. doi: 10.1177/105381510202500. |
[46] | Taub E , Ramey SL , DeLuca S , Echols K . Efficacy of constraint-induced movement therapy for children with cerebral palsy with asymmetric motor impairment. Pediatrics. (2004) ;113: (2):305–12. doi: 10.1542/peds.113.2.305. |
[47] | Camden C , Silva M . Pediatric telehealth: Opportunities created by the COVID-19 and suggestions to sustain its use to support families of children with disabilities. Phys Occup Ther Pediatr. (2021) ;41: (1):1–17. doi: 10.1080/01942638.2020.1825032. |
[48] | Venkataraman K , Amis K , Landerman LR , Caves K , Koh GC , Hoenig H . Teleassessment of gait and gait aids: Validity and interrater reliability. Phys Ther. (2020) ;100: (4):708–17. doi: 10.1093/ptj/pzaa005. |
[49] | Veras M , Kairy D , Rogante M , Giacomozzi C , Saraiva S . Scoping review of outcome measures used in telerehabilitation and virtual reality for post-stroke rehabilitation. J Telemed Telecare. (2017) ;23: (6):567–87. doi: 10.1177/1357633X16656235. |
[50] | Gavazzi F , Adang L , Waldman A , et al. Reliability of the telemedicine application of the gross motor function measure-88 in patients with Leukodystrophy. Pediatr Neurol. (2021) ;125: :34–9. doi: 10.1016/j.pediatrneurol.2021.09.012. |
[51] | Barton C , Caneiro J , Haines T , Malliaras P , Merolli M , Williams C . ‘It’s not hands-on therapy, so it’s very limited’: Telehealth use and views among allied health clinicians during the coronavirus pandemic. JSAMS. (2021) ;24: (S1):S43. doi: 10.1016/j.jsams.2021.09.111. |
[52] | Sicotte C , Lehoux P , Fortier-Blanc J , Leblanc Y . Feasibility and outcome evaluation of a telemedicine application in speech-language pathology. J Telemed Telecare. (2003) ;9: (5):253–8. doi: 10.1258/135763303769211256. |
[53] | Oprandi MC , Bardoni A , Corno L , et al. Feasibility and acceptability of a real-time telerehabilitation intervention for children and young adults with acquired brain injury during the COVID-19 pandemic: An experience report. Int J Telerehab. (2021) ;13: (2):e6423. doi: 10.5195/ijt.2021.6423. |
[54] | Cannon-Bowers JA , Tannenbaum SI , Salas E , Converse SA . Toward an integration of training theory and technique. Hum Factors. (1991) ;33: (3):281–92. doi: 10.1177/001872089103300. |
[55] | Vismara LA , McCormick C , Young GS , Nadhan A , Monlux K . Preliminary findings of a telehealth approach to parent training in autism. J Autism Dev Disord. (2013) ;43: (12):2953–69. doi: 10.1007/s10803-013-1841-8. |
[56] | Boisvert M , Lang R , Andrianopoulos M , Boscardin ML . Telepractice in the assessment and treatment of individuals with autism spectrum disorders: A systematic review. Dev Neurorehabil. (2010) ;13: (6):423–32. doi: 10.3109/17518423.2010.499889. |
[57] | Kresak K , Gallagher P , Rhodes C . Siblings of infants and toddlers with disabilities in early intervention. TECSE. (2009) ;29: (3):143–54. doi: 10.1177/0271121409337949. |
[58] | Smith SN , Crocker AF . Experiential learning in physical therapy education. Adv Med Educ Pract. (2017) ;8: :427–33. doi: 10.2147/AMEP.S140373. |
[59] | Schreiber J , Moerchen VA , Rapport MJ , et al. Experiential learning with children: An essential component of professional physical therapy education. Pediatr Phys Ther. (2015) ;27: (4):356–67. doi: 10.1097/PEP.0000000000000195. |
[60] | Kruger JS , Kruger DJ , Suzuki R . Assessing the effectiveness of experiential learning in a student-run free clinic. Pedagogy in Health Promotion. (2015) ;1: (2):91–4. doi: 10.1177/2373379915575530. |
[61] | Mori B , Carnahan H , Herold J . Use of simulation learning experiences in physical therapy entry-to-practice Curricula: A systematic review. Physiother Can. (2015) ;67: (2):194–202. doi: 10.3138/ptc.2014-40E. |
[62] | Benson JD , Provident I , Szucs KA . An experiential learning lab embedded in a didactic course: Outcomes from a pediatric intervention course. Occup Ther Health Care. (2013) ;27: (1):46–57. doi: 10.3109/07380577.2012.756599. |
[63] | Watson K , Wright A , Morris N , McMeeken J , Rivett D , Blackstock F , et al. Can simulation replace part of clinical time? Two parallel randomised controlled trials. Med Educ. (2012) ;46: (7):657–67. doi: 10.1111/j.1365-2923.2012.04295.x. |
[64] | Coker P . Effects of an experiential learning program on the clinical reasoning and critical thinking skills of occupational therapy students. J Allied Health. (2010) ;39: (4), 280–6. |
[65] | Falk-Kessler J , Benson JD , Witchger Hansen AM . Moving the classroom to the clinic: The experiences of occupational therapy students during a “Living Lab. ” Occup Ther Health Care. (2007) ;21: (3):79–91. doi: 10.1300/J003v21n03_05. |
[66] | Ohtake PJ , Lazarus M , Schillo R , Rosen M . Simulation experience enhances physical therapist student confidence in managing a patient in the critical care environment. Phys Ther. (2013) ;93: (2):216–28. doi: 10.2522/ptj.20110463. |
[67] | Silberman N , Litwin B , Fernandez-Fernandez A , Panzarella K . High fidelity human simulation improves physical therapist student self-efficacy for acute care clinical practice. J Phys Ther Educ 30: (1):14–24. doi: 10.1097/00001416-201630010-00003. |
[68] | DeClute J , Ladyshewsky R . Enhancing clinical competence using a collaborative clinical education model. Phys Ther. (1993) ;73: (10):683–9discussion 689-697. doi: 10.1093/ptj/73.10.683. |
[69] | Ladyshewsky RK , Barrie SC , Drake VM . A comparison of productivity and learning outcome in individual and cooperative physical therapy clinical education models. Phys Ther. (1301) ;78: (12):1288–98discussion 1299-1301. doi: 10.1093/ptj/78.12.1288. |
[70] | Wolff-Burke M , Fergus A , Ferrone D , Moulder A , Thompson K , Whitley JI . The collaborative clinical learning experience in physical therapy: student and instructor perspectives. Journal Phys Ther Educ. (2022) ;36: (2):146–53. doi: 10.1097/JTE.0000000000000235. |
[71] | Weston D . Public health and climate change. Aust N Z J Public Health. (2012) ;36: (2):104–6. doi: 10.1111/j.1753-6405.2011.00818.x. |




