Treatment of oromandibular dystonia with botulinum toxin A improves apnea in a teenager with quadriplegic cerebral palsy: A case report
Abstract
This report describes a 15-year-old female with known spastic and dystonic quadriplegic cerebral palsy (CP), Gross Motor Function Classification System IV, and obstructive sleep apnea (OSA). She experienced decreased apneic episodes after receiving onabotulinumtoxin A (BoNT-A) injections for the treatment of oromandibular dystonia (OMD). After her OSA diagnosis, she initially received injections to the bilateral masseter and temporalis muscles with no effect on the frequency of nightly apneic episodes. Subsequently, the bilateral lateral pterygoid muscles were added and she was later noted to have fewer apneic episodes overnight. This case report describes the use of BoNT-A in the muscles of mastication for management of OMD and the ensuing improvement in OSA in a teenager with CP.
1Abbreviations
OnabotulinumtoxinA (BoNT-A), Cerebral Palsy (CP), Obstructive Sleep Apnea (OSA), Lateral Pterygoids (LPts), Gross Motor Function Classification (GMFCS), Single Event Multi-Level Chemoneurolysis (SEMLC), Continuous Positive Airway Pressure (CPAP)
1Case Report
This report describes a 15-year-old female with mixed tone quadriplegic cerebral palsy (CP), Gross Motor Function Classification System (GMFCS) IV [1], in the setting of hypoxic ischemic brain injury due to respiratory failure at birth (with brain MRI findings of ischemic injury of the thalami, cerebral white matter, parts of the cerebral cortex, and cerebellar white matter). She had oromandibular dystonia (OMD), and obstructive sleep apnea (OSA) and presented with decreased apneic episodes after receiving onabotulinumtoxinA (BoNT-A) injections to the muscles of mastication. She experienced OMD and had difficulty with both mouth opening and closing. She also had dystonia affecting her trunk and arms, and both dystonia and spasticity in her legs. Oral baclofen had been trialed, but had the side effect of sedation and was discontinued. No other enteral medications were trialed due to concerns about side effects of medications. As noted in Fig. 1 and Table 1, she began receiving single event multi-level chemoneurolysis (SEMLC) with BoNT-A and phenol to all four limbs for tone management at age eight. To address difficulty with mouth closing, the bilateral lateral pterygoid muscles (LPts) were added to the second round of SEMLC. She received ten sets of injections to the LPts over 3.5 years, with improvement in mouth closing ability leading to more effective communication and ease with eating. She then developed more difficulty with mouth opening and BoNT-A was applied to the bilateral masseter and temporalis muscles, not including the LPts.
Fig. 1
Timeline of chemodenervation. SEMLC: Single Event Multi-Level Chemoneurolysis; LPts: Lateral Pterygoids; BoNT-A: OnabotulinumtoxinA; OSA: Obstructive Sleep Apnea; CPAP: Continuous Positive Airway Pressure.
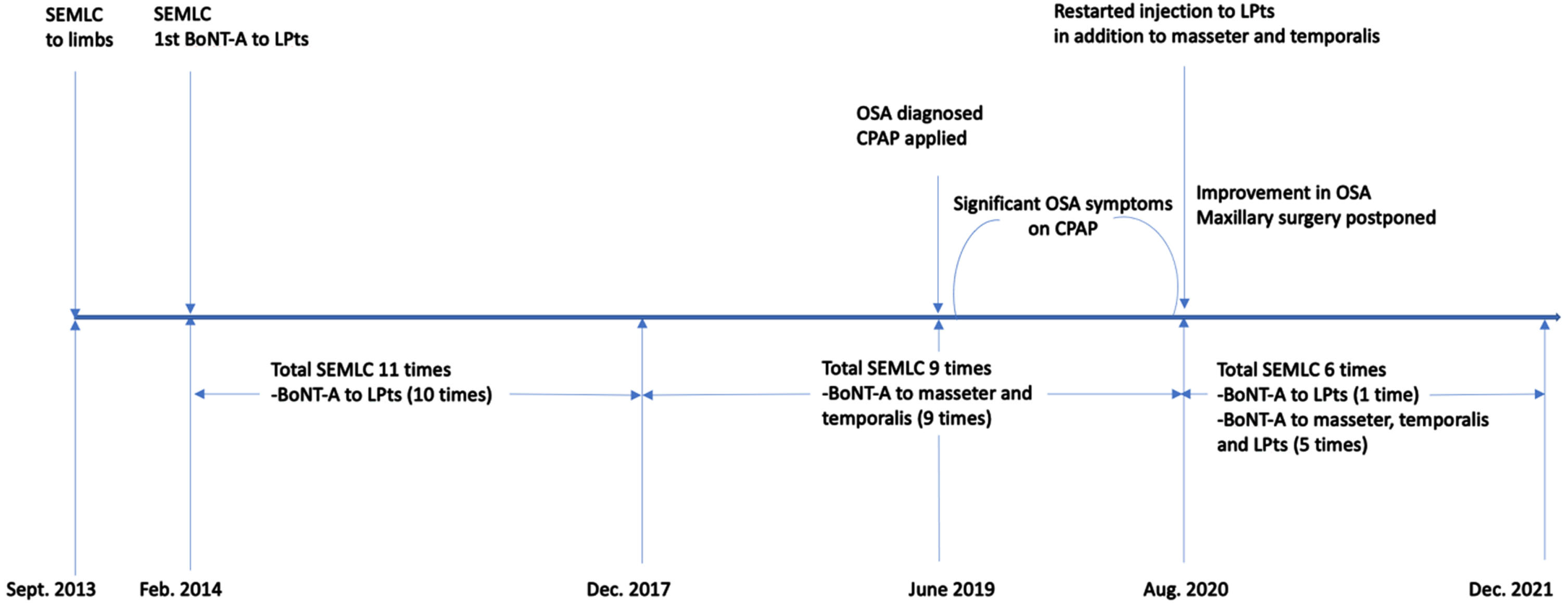
Table 1
Description and Procedure Details. OnabotulinumtoxinA (BoNT-A) injections were done under ultrasound and nerve stimulator guidance to increase accuracy and safety. Each injection for chewing muscles was done as part of single event multi-level chemoneurolysis including other limbs and/or trunk. In terms of dosing for chewing muscles, 10–20 units (U) were used per each lateral pterygoid (LPt), 10–25 U were used per each masseter and 10–30 U were used per each temporalis. Her weight range over eight years was 16.1–27.7 kg with a gradual increase
| Procedure Dates | BoNT-A units to LPts (R/L) | BoNT-A units to Masseter (R/L) | BoNT-A units to Temporalis (R/L) | Weight (kg) | Dose/ Weight/ LPts (Units) | Dose/ Weight/ Masseter (Units) | Dose/ Weight/ Temporalis (Units) |
| 09.17.2013 | X | X | X | 15.9 | X | X | X |
| 02.25.2014 | 10/10 | X | X | 16.1 | 0.62 U/kg | X | X |
| 06.11.2014 | 10/10 | X | X | 15.9 | 0.63U/kg | X | X |
| 10.08.2014 | 15/15 | X | X | 16.5 | 0.91U/kg | X | X |
| 03.03.2015 | 15/15 | X | X | 16.3 | 0.92U/kg | X | X |
| 08.11.2015 | X | X | X | 18.2 | X | X | X |
| 11.24.2015 | 15/15 | X | X | 19.5 | 0.77U/kg | X | X |
| 04.19.2016 | 15/15 | X | X | 20.0 | 0.75 U/kg | X | X |
| 08.16.2016 | 20/20 | X | X | 19.5 | 1.03U/kg | X | X |
| 12.20.2016 | 20/20 | X | X | 20.8 | 0.96U/kg | X | X |
| 05.09.2017 | 20/20 | X | X | 20.4 | 0.98U/kg | X | X |
| 08.22.2017 | 20/20 | X | X | 21.4 | 0.93U/kg | X | X |
| 12.12.2017 | X | 20/20 | 30/30 | 19.9 | X | 1.01U/kg | 1.51U/kg |
| 04.28.2018 | X | 20/20 | 30/30 | 21.4 | X | 0.93U/kg | 1.40U/kg |
| 07.31.2018 | X | 20/20 | 30/30 | 21.3 | X | 0.94U/kg | 1.41U/kg |
| 11.13.2018 | X | 20/20 | 30/30 | 21.1 | X | 0.95U/kg | 1.42U/kg |
| 03.26.2019 | X | 20/20 | 30/30 | 21.8 | X | 0.92U/kg | 1.38U/kg |
| 07.02.2019* | X | 20/20 | 20/20 | 21.8 | X | 0.92U/kg | 0.92U/kg |
| 10.29.2019♣ | X | 20/20 | 20/20 | 20.8 | X | 0.96U/kg | 0.96U/kg |
| 02.11.2020 | X | 25/25 | 20/20 | 23.6 | X | 1.06U/kg | 0.85U/kg |
| 05.26.2020 | X | 20/20 | 20/20 | 26.5 | X | 0.75U/kg | 0.75U/kg |
| 08.25.2020♦ | 20/20 | X | X | 27.7 | 0.72U/kg | X | X |
| 12.01.2020 | 20/20 | 10/10 | 10/10 | 27.0 | 0.74U/kg | 0.37U/kg | 0.37U/kg |
| 03.16.2021 | 20/20 | 10/10 | 10/10 | 27.6 | 0.72U/kg | 0.36U/kg | 0.36U/kg |
| 06.22.2021 | 10/10 | 20/20 | 30/30 | 26.4 | 0.38U/kg | 0.76U/kg | 1.14U/kg |
| 09.28.2021 | 15/15 | 20/20 | 25/25 | 27.2 | 0.55U/kg | 0.74U/kg | 0.92U/kg |
| 12.21.2021 | 15/15 | 25/25 | 20/20 | 0.55U/kg | 0.91U/kg | 0.73U/kg |
*Obstructive sleep apnea diagnosis was done; ♣Continuous positive airway pressure was applied; ♦BoNT-A injections to bilateral LPts were added. R = right; L = left.
At age 14 she was diagnosed with OSA and started on continuous positive airway pressure (CPAP) after her 7th BoNT-A injections to the masseter and temporalis muscles (Fig. 1). She had 3–7 episodes of apnea nightly, lasting 20 seconds as per her CPAP machine recorded logs. She was also noted to have micrognathia and retrognathia. While undergoing consultation for surgical management of OSA in the setting of her jaw abnormalities, she had two rounds of BoNT-A injections to the bilateral masseter and temporalis muscles without improvement in apneic episodes. After discussion with her surgeon, BoNT-A injections were suggested for both antagonist and agonist muscles of her jaw to manage dystonia and potentially OSA. However, her mother felt that the BoNT-A effect on dystonia of the masseter and temporalis was still present. Thus, she had injections to the LPts alone with a significant decrease in apneic events (Fig. 1, Table 1, Table 2). Her caregiver reported zero apneic episodes over three weeks and 1-2 episodes per night thereafter. Three months post-injections, when BoNT-A began to wear off, her apneic events increased to about three per night.
Table 2
Description of Oromandibular Injections After Diagnosis of Apnea. OnabotulinumtoxinA (BoNT-A) injections to the chewing muscles specifically are described after diagnosis of apnea. Their association with the reduction in number of apneic episodes is noted as well
| Procedure Dates | BoNT-A units to LPts (R/L) | BoNT-A units to Masseter (R/L) | BoNT-A units to Temporalis (R/L) | Number of Apneic Episodes per night | CPAP setting |
| 10.29.2019♣ | X | 20/20 | 20/20 | 3–7 | 20 cmH2O |
| 02.11.2020 | X | 25/25 | 20/20 | 3–7 | |
| 05.26.2020 | X | 20/20 | 20/20 | 3–7 | |
| 08.25.2020♦ | 20/20 | X | X | 0 for 3 weeks, then 1–2 thereafter | |
| 12.01.2020 | 20/20 | 10/10 | 10/10 | 1 for 2 months | |
| 03.16.2021 | 20/20 | 10/10 | 10/10 | <3 | |
| 06.22.2021 | 10/10 | 20/20 | 30/30 | <3 | |
| 09.28.2021 | 15/15 | 20/20 | 25/25 | <3 | |
| 12.21.2021 | 15/15 | 25/25 | 20/20 | <3 | 5 cmH2O |
♣CPAP was applied; ♦BoNT-A injections to bilateral lateral pterygoids (LPts) were added. R = right; L = left. CPAP = continuous positive airway pressure.
For her next treatment, she received BoNT-A injections to all three muscles of mastication including the bilateral LPts, temporalis, and masseter muscles. She again had fewer apneic episodes, averaging once nightly for two months. Thus, after her initial injections to the LPts, she received a total of five rounds of BoNT-A injections to these three muscles. (See Fig. 1, Table 1, and Table 2 for a timeline and procedural details.) Over this time period, she was able to decrease her CPAP setting from 30 cmH2O to 5 cmH2O. Her surgical intervention to improve jaw structure for OSA was postponed, and her apneic events decreased to fewer than three per night. There were no noted adverse events from her BoNT-A injections.
2Discussion
OMD is a significant concern in children with dystonic and/or spastic CP as it can impair eating, speaking, and/or breathing [2]. Additionally, there is a higher prevalence of OSA in children with CP due to adeno-tonsillar hypertrophy, micrognathia, and/or abnormal neuromuscular control [3, 4]. Though botulinum toxin has a well-known use for treatment of OMD [5, 6], and there is a case report of use of BoNT-A in a 51-year-old with OMD resulting in improvement of his OSA and symptoms [7], the efficacy of BoNT-A in treatment OMD in children with CP and its effect on OSA is not well studied.
The muscles of mastication addressed include the masseter, medial and lateral pterygoids, and the temporalis. The masseter and medial pterygoid muscles elevate and protrude the mandible, and the temporalis elevates and retracts the mandible. The LPts assist with mandibular depression and protrusion. If these muscles are dystonic, the dystonia can contribute to structural and functional problems of the mouth such as micrognathia, retrognathia, OSA, and/or eating and speaking difficulties – all of which this patient experienced. After BoNT-A injections to the chewing muscles there was improvement in many of these problems, most notably the decrease in her CPAP setting and frequency of apneic episodes. It is important to note she had the greatest improvement in her OSA after she received BoNT-A injections to both her mouth opening and closing muscles. The authors believe this is why the initial addition of injections to the LPts, while there was still a presumed effect on the masseters and temporalis, may have assisted with improvement in OSA, ultimately leading to the decision to treat all three muscles.
Treating both agonist and antagonist muscles when managing OMD is important since muscle co-contraction is a frequent problem in dystonic CP that can also affect concurrent OSA. Although CPAP and oral appliances are the usual treatment options for OSA, surgical interventions are often necessary, and may even be used initially in those with structural jaw problems, like this patient. Therefore, in patients with CP, the use of BoNT-A to treat OMD may, in turn, improve OSA, and subsequently decrease the need for surgery, by improving the coordination of agonist and antagonist muscles of mastication.
2.1Limitations
Because the improvement in OSA was not an expected effect, the authors do not have more specific data, such as sleep study information before and after injections. A previous case report by Hsu et al. describes the use of video polysomnography to assess the impact of jaw posturing on obstructive respiratory events, which may be applicable to patients with dystonia. Drug-induced sleep endoscopy can also be used to assess airway patency [7].
Acknowledgments
The authors have no acknowledgments. Prior poster presentation: American Academy of Cerebral Palsy and Developmental Medicine 75th Annual Meeting; 2021 Oct 6-9; Montreal, Quebec/Virtual.
Author contributions
All four authors contributed substantially to the writing of the manuscript and treatment of the patient.
Conflict of interest
No conflicts exist for authors. No funding was provided from any source and there were no financial benefits to the authors. Each author was involved with the contribution to patient care, procedures involved, and creation of this manuscript.
Ethical considerations
IRB exemption for case report per Columbia University Institutional Review Board/Privacy Board Policy.
References
[1] | Gross Motor Function Classification System (GMFCS). Allambie Heights, New South Wales, Australia: Cerebral Palsy Alliance [updated 2018; cited 2022 Feb 17], Available from: https://cerebralpalsy.org.au/our-research/about-cerebral-palsy/what-is-cerebral-palsy/severity-of-cerebral-palsy/gross-motor-function-classification-system/ |
[2] | Dystonia in Cerebral Palsy. Milwaukee: American Academy for Cerebral Palsy and Developmental Medicine; (2016) [cited 2022 Feb 17], Available from: https://www.aacpdm.org/publications/care-pathways/dystonia-in-cerebral-palsy |
[3] | Seddon PC , Khan Y . Respiratory problems in children with neurological impairment, Arch Dis Child. (2003) :88: (1):75–8. doi: 10.1136/adc.88.1.75 |
[4] | Kotagal S , Gibbons VP , Stith JA . Sleep abnormalities in patients with severe cerebral palsy, Dev Med Child Neurol. (1994) ;36: (4):304–11. doi: 10.1111/j.1469-8749.1994.tb11850.x |
[5] | Persaud R , Garas G , Silva S , Stamatoglou C , Chatrath P , Patel K . An evidence-based review of botulinum toxin (Botox) applications in non-cosmetic head and neck conditions, JRSM Short Rep. (2013) ;4: (2):10. doi: 10.1177/2042533312472115 |
[6] | Dadgardoust PD , Rosales RL , Asuncion RM , Dressler D . Botulinum neurotoxin a therapy efficacy and safety for oromandibular dystonia: a meta-analysis, J Neural Transm (Vienna). (2019) ;126: (2):141–8. doi: 10.1007/s00702-018-1960-7 |
[7] | Hsu N , Hsieh C , Thomas A , Chang M . Obstructive sleep apneadue to oromandibular dystonia and treated withbotulinum toxin, J Clin Sleep Med. (2020) ;16: (7):1209–12. doi: 10.5664/jcsm.8454 |




