Clinical assessment, treatment, and referral trends for adolescent runners seeking care at an injured runners’ clinic
Abstract
PURPOSE:
Over a 10-year time frame, this study aimed to evaluate diagnosis, treatment, and referral trends for adolescent runners seeking care for running-related injuries (RRIs) at a clinic that specializes in running medicine.
METHODS:
This study was a retrospective chart review of 392 adolescent runners (2,326 encounters) who sought care for RRIs between the years 2011 and 2021. Descriptive statistics were used to summarize clinical assessments, referrals, assistive devices, and medications prescribed or administered overall and by injury type. Chi-square analyses were used to compare proportions of services rendered across the 10-year time frame.
RESULTS:
Patients most frequently received manual evaluations or special tests during clinic visits. Most visits resulted in at least one referral (91%), primarily for physical therapy or gait-training. Assistive devices and medications/supplements were offered at only 18% of patient visits. The majority of assessments (X2 = 69.7, p = 0.002), treatments (X2: 23.6–43.8, p: < 0.001–0.003), and referrals (X2 = 132, p < 0.001) were for shin injuries. Larger proportions of nutrition assessments (X2 = 40.7, p < 0.001), interventions (X2 = 26.8, p = 0.003), and referrals (X2 = 27.5, p = 0.002) were performed in or after the year 2015.
CONCLUSION:
Clinic visits for shin injuries required the most clinical resources per episode of care. There were observed shifts in clinical assessment and treatment approaches to include more expanded nutritional and physiologic considerations.
1Introduction
Although running offers multiple health benefits to young athletes [1, 2], running-related injuries (RRIs) present substantial barriers to lifetime running participation [3–5]. Runners with lower extremity repetitive stress injuries frequently seek care from health care professionals to alleviate pain and disability [6]. There is substantial research exploring factors contributing to the development and exacerbation of RRIs, particularly for bone stress injuries and chronic musculoskeletal pathologies. Chronic RRIs constitute the largest injury burden in the broader running population [4, 7, 8]. Young runners are more susceptible to RRIs if they have inadequate nutrition and fueling [7–9], poor functional movement patterns [7, 10, 11], strength deficits, and altered lower extremity alignment [10, 12–14]. As such, the authors of the most recent consensus statement on minimizing the risk of RRIs among adolescent athletes recommended measuring and addressing these key factors in clinical practice through clinical assessments and therapeutic intervention [7, 15]. Additionally, there have been several consensus statements from the International Olympic Committee published in 2014 and 2018 illuminating Relative Energy Deficiency in Sport (RED-S; multi-system physiological dysfunction due to an imbalance between energy expenditure and dietary energy intake) and the need to include early recognition and treatment of physiological disruptions in relationship to overuse injuries in clinical practice [16, 17].
Despite the available evidence and current recommendations, there is comparatively little research exploring components of care for adolescents with RRIs presenting to outpatient clinical settings. A prior study that assessed treatment trends for high school cross-country runners determined that patients with RRIs primarily receive therapeutic interventions aimed at reducing pain and alleviating symptoms [6]. However, beyond pain relief, little is known about clinical approaches to care when it comes to addressing the multifactorial nature of RRIs, including but not limited to metabolic, nutritional, psychosocial, and physiological factors. There has been a breadth of emerging evidence on key factors influencing adolescent RRIs over the recent years and expert recommendations on injury management in this population [11, 15, 16]. As such, it is necessary to assess RRI treatment trends in clinical settings that specialize in the care for injured runners to determine how elements of clinical practice have evolved to align with current evidence-based recommendations. Additionally, assessing clinical diagnosis, treatment, and referral trends for adolescent RRIs would help determine how clinical resources are often allocated by injury types and body regions for this patient population.
The purpose of this study was to evaluate clinical assessment, treatment, and referral trends among adolescent runners seeking care at a hospital-affiliated Injured Runners Clinic (IRC) over a 10-year period (2011–2021). Specifically, the number and types of clinical assessments, assistive devices provided or prescribed, medications and supplements administered or prescribed, and patient referrals by injury characteristics and sex were assessed across the 10-year time frame.
2Materials and methods
2.1Patients
This study was a retrospective chart review of electronic patient records from a tertiary-care Children’s Hospital Sports Medicine Division IRC, where participating fellowship-trained sports medicine physicians treated adolescent patients with RRIs between 2011 and 2021. The IRC is a multidisciplinary clinic consisting of sports medicine physicians, athletic trainers, strength and conditioning specialists, physical therapists, sports nutrition specialists, and mental health professionals. The IRC is designed to provide special care for injured runners through diagnosis and/or injury recovery and return to running. The clinic is held twice weekly, and typically patients are runners referred from primary care physicians, general orthopedics/sports medicine physicians and surgeons, and/or adolescent medicine specialists. This specialty clinic operates within the hospital’s sports medicine and orthopedics departments and an affiliated sports injury prevention and rehabilitation center. The attending sports medicine physicians in the IRC had specialized training in running gait biomechanics through fellowship training. These physicians completed all physical assessments and diagnoses for any active running-related injuries using standard clinical assessment and care. They performed real-time running gait biomechanics assessments for patients to help guide return to running and running-related re-injury prevention when appropriate.
For the purpose of this study, patients between the ages 10 and 17 years who were diagnosed with a current RRI were included. The lower age limit reflected the youngest age of a patient seeking care in the clinic, and the upper limit was chosen to focus on only adolescent patients. Patients who had a previous surgery for their injury were excluded as this would affect patients’ course of care. Additionally, those whose mechanism of injury was not running-related were excluded from this analysis to ensure that true RRIs were assessed. The study was approved by the hospital’s Institutional Review Board. Participant assent and parental consent were exempt due to the retrospective design.
2.2Data collection
Treating physicians used a web-based secure electronic medical record system (PowerChart®, Cerner Corporation, North Kansas City, MO, USA) to record the date of visit, chief complaint, history of present injury, review of systems, physical examination, imaging, and the assessment/plan of action for all patient encounters.
2.3Data extraction
Patient health care records were identified within the hospital database using a formal search by department and encounter type (e.g., orthopedics, sports medicine, IRC), and filtered by year (2011–2021) to identify pertinent patient medical record numbers. Two members of the research team (AFDL, SBW) screened patient records to ensure patients fit the inclusion criteria for this study. One researcher (AFDL) extracted data for the qualifying patients to ensure data integrity. All patient encounters were extracted for each injury for which they presented to the IRC. Extracted data included injury details (injured body region, injury type [bone vs. soft tissue]) using ICD-9/10 codes. Data were also extracted pertaining to the number and type of clinical assessments, imaging, assistive devices provided or prescribed (e.g., crutches, walking boots, orthoses), medications administered or prescribed, and patient referrals for therapeutic interventions or consultations across all patient visits using Current Procedural Terminology (CPT) codes. Clinical assessments were categorized as physical examinations used to rule in or rule out injuries, including manual tests, such as palpation of injured body regions, and special tests using specific hands-on assessments, such as a Thompson test for Achilles tendon injury. All data were entered in a secure online platform (REDCap, Vanderbilt University, Nashville, TN, USA).
2.4Statistical analyses
Descriptive statistics were used to summarize the number and type of clinical assessments, assistive devices, medications/supplements prescribed or administered overall, and referrals by injured body region and by injury type. Chi-square analyses were used to compare proportions of services rendered by injury details (injured body region, injury type), and to assess the change in services rendered over the 10-year time frame. Apparent differences across injuries or demographics were further compared using post-hoc pairwise proportion comparisons. Alpha was set a priori to 0.05 for all analyses. All analyses were conducted in Jamovi (Version 2.3.21.0).
3Results
There were 392 patient records that met inclusion criteria for this study (277 females [F], 115 males [M]; age: 16.1±1.3; race: 70% White), with 2,326 total patient encounters (5±4 encounters per patient injury case) during the 10-year time frame. The majority of injuries were localized to the shins and were categorized as bone stress injuries. Patients underwent a mean of 1.70 clinical assessment tests per visit (Table 1). The majority (91%) of visits resulted in at least one referral (Tables 1 and 2). Assistive devices and medications were offered or prescribed at approximately 18% of patient visits (Tables 3 and 4).
Table 1
Clinical assessments across patient visits overall, by type of tests, and by injury
| Category | Visits with | Total | Clinical | Imaging assessments | Running assessments | Physical assessments | ||||||||
| Clinical assessments | Clinical assessments | Assessments per visit | MRI | X-Ray | DEXA | US | CT | Gait analysis | ICP test | Blood/urine tests | Manual/special tests | Tele-health | ||
| All Injuries | 2,326 N(%) | 3,961 N(%) | 1.70±0.75 (Mean±SD) | 450 N(%) | 456 N(%) | 131 N(%) | 91 N(%) | 8 N(%) | 394 N(%) | 14 N(%) | 150 N(%) | 2199 N(%) | 68 N(%) | |
| Body Region | Toes/Feet | 290 (12%) | 507 (13%) | 1.75±0.76 | 54 (12%) | 78 (17%) | 24 (18%) | 3 (3%) | 3 (38%) | 38 (10%) | 0 (0%) | 27 (18%) | 273 (12%) | 7 (10%) |
| Ankles | 194 (8%) | 316 (8%) | 1.63±0.70 | 36 (8%) | 45 (10%) | 3 (2%) | 8 (9%) | 0 (0%) | 35 (9%) | 0 (0%) | 3 (2%) | 185 (8%) | 1 (1%) | |
| Shins | 897 (39%) | 1569 (40%) | 1.75±0.78 | 198 (44%) | 158 (35%) | 74 (56%) | 11 (12%) | 0 (0%) | 163 (41%) | 8 (57%) | 88 (59%) | 821 (37%) | 48 (71%) | |
| Calves | 59 (3%) | 103 (1%) | 1.75±0.76 | 9 (2%) | 6 (1%) | 2 (2%) | 9 (10%) | 0 (0%) | 15 (4%) | 4 (29%) | 2 (1%) | 59 (3%) | 3 (4%) | |
| Knees | 304 (13%) | 484 (12%) | 1.59±0.63 | 35 (8%) | 67 (15%) | 2 (2%) | 13 (14%) | 0 (0%) | 59 (15%) | 0 (0%) | 5 (3%) | 302 (14%) | 1 (1%) | |
| Thighs/ | 75 (3%) | 127 (3%) | 1.69±0.88 | 18 (4%) | 11 (2%) | 5 (4%) | 4 (4%) | 1 (13%) | 9 (2%) | 2 (14%) | 5 (3%) | 72 (3%) | 0 (0%) | |
| Hamstrings | ||||||||||||||
| Hips | 366 (16%) | 640 (16%) | 1.75±0.73 | 74 (16%) | 80 (18%) | 16 (12%) | 37 (41%) | 2 (25%) | 56 (14%) | 0 (0%) | 18 (12%) | 351 (16%) | 6 (9%) | |
| Low Back | 121 (5%) | 180 (5%) | 1.49±0.69 | 25 (6%) | 9 (2%) | 5 (4%) | 4 (4%) | 2 (25%) | 16 (4%) | 0 (0%) | 1 (1%) | 116 (5%) | 2 (3%) | |
| Abdomen/Upper | 20 (1%) | 29 (<1%) | 1.45±0.76 | 1 (<1%) | 2 (<1%) | 0 (0%) | 2 (2%) | 0 (0%) | 3 (1%) | 0 (0%) | 1 (1%) | 20 (1%) | 0 (0%) | |
| Extremity | ||||||||||||||
| Injury Type | Bony | 1,326 (57%) | 2,261 (57%) | 1.71±0.74 | 273 (61%) | 254 (56%) | 113 (86%) | 61 (67%) | 5 (63%) | 219 (56%) | 7 (50%) | 80 (54%) | 1,251 (57%) | 41 (60%) |
| Soft Tissue | 1,000 (43%) | 1,700 (43%) | 1.70±0.75 | 177 (39%) | 202 (44%) | 18 (14%) | 30 (33%) | 3 (37%) | 175 (44%) | 7 (50%) | 70 (46%) | 948 (43%) | 27 (40%) | |
Abbreviations: MRI, magnetic resonance imaging; DEXA, dual-energy x-ray absorptiometry; US, ultrasound; CT, computed tomography; ICP Test, intracompartmental pressure testing.
Table 2
Devices across patient visits overall, by type of devices, and by injury details
| Category | Visits with device administration | Total | Devices | Off-loading devices | Supportive devices | Additional devices | ||||
| Devices | Per visit | Crutches | Boots | Orthoses | Braces/compression sleeves | Bone stimulator | Other | |||
| All injuries | 427 N(%) | 461 N(%) | 1.08±0.28 (Mean±SD) | 47 N(%) | 120 N(%) | 191 N(%) | 70 N(%) | 27 N(%) | 6 N(%) | |
| Body Region | Toes/Feet | 94 (22%) | 107 (23%) | 1.14±0.40 | 7 (15%) | 39 (33%) | 48 (25%) | 1 (1%) | 9 (33%) | 3 (50%) |
| Ankles | 54 (13%) | 56 (12%) | 1.04±0.19 | 3 (6%) | 17 (14%) | 22 (12%) | 13 (19%) | 1 (4%) | 0 (0%) | |
| Shins | 150 (35%) | 160 (35%) | 1.07±0.25 | 17 (36%) | 64 (53%) | 56 (29%) | 9 (13%) | 13 (48%) | 1 (17%) | |
| Calves | 12 (3%) | 12 (3%) | 1±0 | 0 (0%) | 0 (0%) | 10 (5%) | 2 (3%) | 0 (0%) | 0 (0%) | |
| Knees | 63 (15%) | 71 (15%) | 1.13±0.34 | 2 (4%) | 0 (0%) | 41 (21%) | 27 (39%) | 0 (0%) | 1 (17%) | |
| Thighs/ Hamstrings | 8 (2%) | 8 (2%) | 1±0 | 4 (9%) | 0 (0%) | 1 (1%) | 2 (3%) | 1 (4%) | 0 (0%) | |
| Hips | 30 (7%) | 30 (7%) | 1±0 | 12 (26%) | 0 (0%) | 10 (5%) | 5 (7%) | 3 (11%) | 0 (0%) | |
| Low Back | 16 (4%) | 17 (4%) | 1.06±0.25 | 2 (4%) | 0 (0%) | 3 (2%) | 11 (16%) | 0 (0%) | 1 (17%) | |
| Abdomen/ Upper Extremity | 0 (0%) | 0 (0%) | 0±0 | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Injury Type | Bony | 261 (61%) | 261 (57%) | 1±0 | 31 (66%) | 66 (55%) | 107 (56%) | 36 (51%) | 17 (63%) | 4 (67%) |
| Soft Tissue | 166 (39%) | 200 (43%) | 1.20±0.44 | 16 (34%) | 54 (45%) | 84 (44%) | 34 (49%) | 10 (37%) | 2 (33%) | |
Table 3
Medications/supplements across patient visits overall, by type of medication/supplement, and by injury details
| Category | Visits with Medication/Supplement Administration or Prescription | Total Medications/Supplements | Medications/Supplements Per Visit | Medications | Supplements | ||||||
| US-Guided Injection | Topical Analgesic | NSAIDs | Other | Vitamin D | Calcium | Iron | |||||
| All injuries | 397 N(%) | 519 N(%) | 1.31±0.47 (Mean±SD) | 76 N(%) | 62 N(%) | 112 N(%) | 13 N(%) | 137 N(%) | 95 N(%) | 24 N(%) | |
| Body Region | Toes/Feet | 40 (10%) | 62 (12%) | 1.45±0.55 | 5 (7%) | 4 (6%) | 1 (1%) | 2 (15%) | 29 (21%) | 17 (18%) | 4 (17%) |
| Ankles | 34 (9%) | 48 (9%) | 1.35±0.54 | 3 (4%) | 18 (29%) | 11 (10%) | 4 (31%) | 6 (4%) | 4 (4%) | 2 (8%) | |
| Shins | 129 (32%) | 179 (34%) | 1.43±0.50 | 5 (7%) | 11 (18%) | 21 (19%) | 1 (8%) | 76 (55%) | 53 (56%) | 12 (50%) | |
| Calves | 7 (2%) | 7 (1%) | 1±0 | 3 (4%) | 1 (2%) | 3 (3%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Knees | 44 (11%) | 52 (10%) | 1.14±0.35 | 10 (13%) | 10 (16%) | 21 (19%) | 0 (0%) | 5 (4%) | 4 (4%) | 2 (8%) | |
| Thighs/ Hamstrings | 11 (3%) | 15 (3%) | 1.36±0.50 | 3 (4%) | 0 (0%) | 1 (1%) | 0 (0%) | 5 (4%) | 6 (6%) | 0 (0%) | |
| Hips | 97 (24%) | 117 (23%) | 1.18±0.41 | 40 (53%) | 8 (13%) | 41 (37%) | 2 (15%) | 13 (9%) | 10 (11%) | 3 (13%) | |
| Low Back | 27 (7%) | 30 (6%) | 1.11±0.32 | 7 (9%) | 6 (10%) | 10 (9%) | 3 (23%) | 3 (2%) | 1 (1%) | 0 (0%) | |
| Abdomen/ Upper Extremity | 8 (2%) | 9 (2%) | 1.13±0.83 | 0 (0%) | 4 (6%) | 3 (3%) | 1 (8%) | 0 (0%) | 0 (0%) | 1 (4%) | |
| Injury Type | Bony | 191 (48%) | 293 (56%) | 1.53±0.51 | 53 (70%) | 33 (53%) | 65 (58%) | 11 (85%) | 68 (50%) | 47 (50%) | 16 (67%) |
| Soft Tissue | 206 (52%) | 226 (44%) | 1.10±0.54 | 23 (30%) | 29 (47%) | 47 (42%) | 2 (15%) | 69 (50%) | 48 (50%) | 8 (33%) | |
Abbreviations: US, ultrasound; NSAIDs, non-steroidal anti-inflammatory drugs.
Table 4
Referrals across patient visits overall, by type of referrals, and by injury details
| Category | Visits | Total | Referrals | Therapeutic/Training | Specialists | ||||
| with Referrals | Referrals | Per Visit | Physical Therapy | Gait-Training | Other | Nutrition | Psychiatry | ||
| All Injuries | 2,116 N(%) | 3,524 N(%) | 1.68±0.72 (Mean±SD) | 1,811 N(%) | 499 N(%) | 82 N(%) | 286 N(%) | 38 N(%) | |
| Body Region | Toes/Feet | 250 (12%) | 383 (11%) | 1.55±0.72 | 202 (11%) | 38 (8%) | 6 (7%) | 45 (16%) | 1 (3%) |
| Ankles | 180 (9%) | 277 (8%) | 1.56±0.66 | 164 (9%) | 37 (7%) | 6 (7%) | 14 (5%) | 2 (5%) | |
| Shins | 801 (38%) | 1465 (42%) | 1.85±0.78 | 652 (36%) | 212 (42%) | 39 (48%) | 164 (57%) | 21 (55%) | |
| Calves | 60 (3%) | 90 (3%) | 1.63±0.61 | 49 (3%) | 18 (4%) | 5 (6%) | 3 (1%) | 0 (0%) | |
| Knees | 291 (14%) | 467 (13%) | 1.58±0.60 | 273 (15%) | 81 (16%) | 5 (6%) | 13 (5%) | 1 (3%) | |
| Thighs/ Hamstrings | 71 (3%) | 115 (3%) | 1.68±0.72 | 60 (3%) | 16 (3%) | 3 (4%) | 7 (2%) | 0 (0%) | |
| Hips | 334 (16%) | 543 (15%) | 1.63±0.66 | 295 (16%) | 74 (15%) | 7 (9%) | 33 (12%) | 8 (21%) | |
| Low Back | 113 (5%) | 162 (5%) | 1.45±0.58 | 103 (6%) | 20 (4%) | 8 (10%) | 7 (2%) | 5 (13%) | |
| Abdomen/ Upper Extremity | 16 (1%) | 22 (1%) | 1.5±0.63 | 13 (1%) | 3 (1%) | 3 (4%) | 0 (0%) | 0 (0%) | |
| Injury Type | Bony | 1,164 (55%) | 1,990 (56%) | 1.23±0.83 | 1,014 (56%) | 293 (59%) | 41 (50%) | 157 (55%) | 26 (68%) |
| Soft Tissue | 952 (45%) | 1,534 (44%) | 1.61±0.85 | 797 (44%) | 206 (41%) | 41 (50%) | 129 (45%) | 12 (32%) | |
3.1Clinical assessments
Foot, calf, shin, and hip injuries all received an average of 1.75 clinical assessment tests per clinic visit (Table 1). Manual and/or special tests comprised the majority of clinical assessments (56%), followed by x-rays (12%), MRIs (11%), and running gait assessments (10% ; Table 1). There were significant differences in the proportion of clinical assessments by injured body region (X2(N = 2,326, df = 4) = 69.7, p = 0.002). Shin injuries accounted for the largest proportion of clinical assessments (40% of all clinical assessments), followed by hip injuries (16% of all clinical assessments). Shin injuries had the largest proportion of all imaging services ordered (39%), with MRI being the most frequently used imaging service (45% of imaging for shin injuries; Table 1). Running gait analyses (42%) and blood panels/urinalyses (59%) were primarily performed for patients with shin injuries (Table 1).
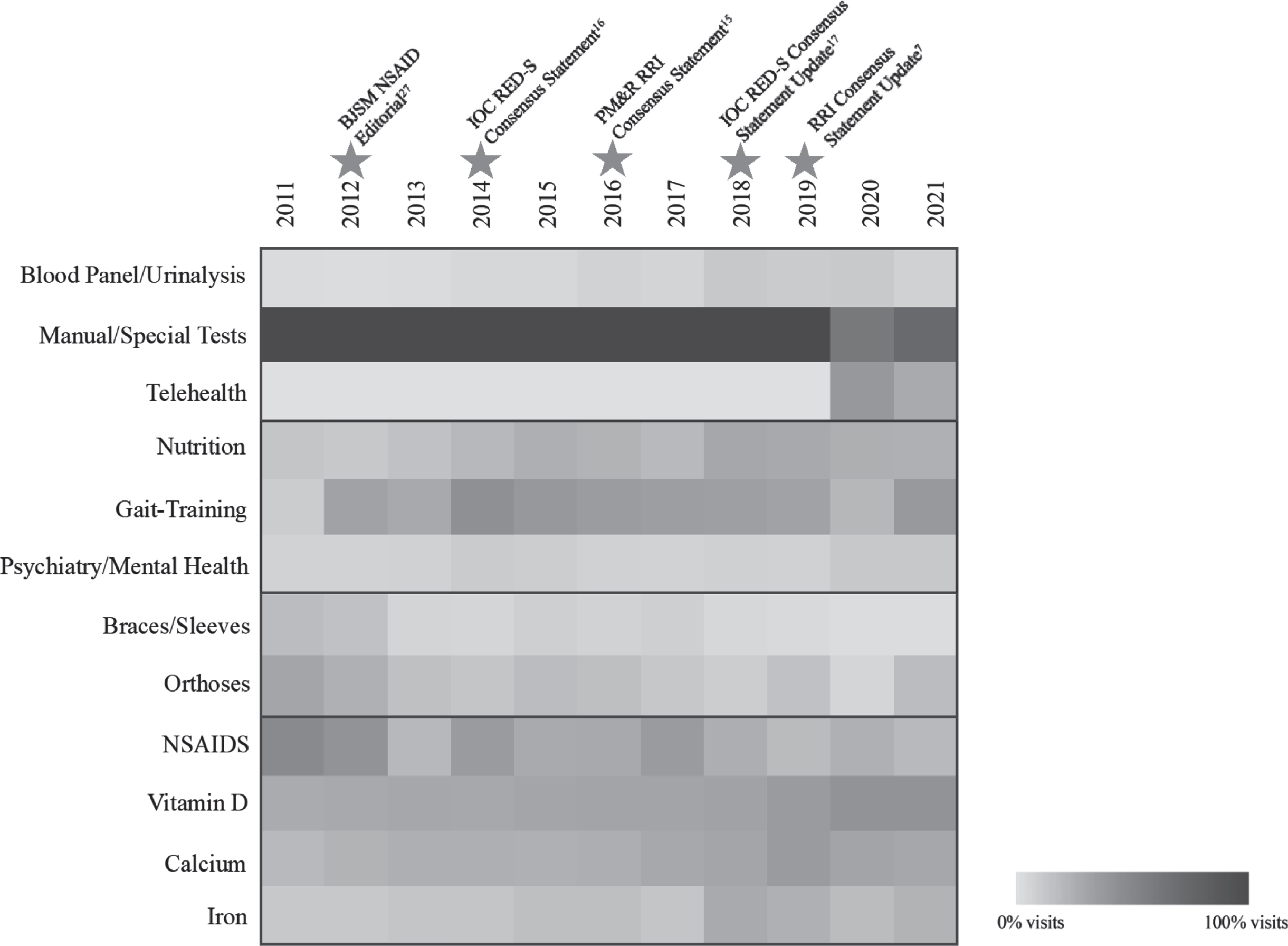
There were no significant differences in number of clinical assessments performed across injury types (X2(N = 2,326, df = 2) = 2.9, p = 0.71), sex (X2(N = 2,326, df = 2) = 0.1, p = 0.81), nor year of visit (X2(N = 2,326, df = 10) = 59.7, p = 0.16). There were significant differences in assessment types by injury types; a larger proportion of patients with bone stress injuries received blood panels/urinalyses (X2(N = 150, df = 2) = 7.0, p = 0.01) and dual-energy x-ray absorptiometry (DEXA) scans (X2(N = 131, df = 2) = 48.5, p < 0.001) compared to patients with soft tissue injuries (Table 1). There were also significant differences in assessment types by year (X2 range: 40.7–749.0, p < 0.001). A larger proportion of blood panels/urinalyses were performed in or after the year 2018 (average of 11% of visits) compared to 2011–2017 (average of 5% of visits; Fig. 1). Manual and/or special tests were more infrequently performed during the years 2020–2021 during the COVID-19 pandemic (average of 66% of visits in 2020–2021 vs. 100% previous years), as clinic visits shifted to telemedicine assessments (average of 33% of visits in 2020–2021 vs. 0% previous years; Fig. 1).
Fig. 1
Significant changes in clinical assessment, referral, device, and medication type trends over time. Caption: Pictogram depicting the percentage of visits including the respective diagnostic, referral, device, and medication/supplementation administration clinic trends from 2011-2021 (x-axis). Stars along the x-axis indicate the emergence of specific consensus statements regarding the management and care of injuries and adolescent runners.7,15,16,17,27 Darker hues represent more visits including the services. Only specific types of outcomes that were statistically significantly different over time are presented. Abbreviations: BJSM, British Journal of Sports Medicine; NSAIDs, non-steroidal anti-inflammatory drugs; IOC, International Olympic Committee; PM&R, Physical Medicine & Rehabilitation; RRI, running-related injuries; Meds, Medications; Supplem., Supplements..
3.2Assistive devices
Orthoses (41% of all devices) and walking boots (26%) were the most frequently provided devices for adolescent patients with RRIs (Table 2). There were significant differences in the proportion of assistive devices provided by injury types (X2 range: 76.9–106.0, p < 0.001). Those with toe/feet and knee injuries received the highest number of assistive devices per visit (Table 2). Braces and/or compression sleeves were most frequently provided to patients with knee injuries (39%), followed by ankle injuries (19%) and lower back injuries (16% ; Table 2). Walking boots and orthoses were most frequently provided to those with shin (boots: 53% ; orthoses: 29%) and toe/foot injuries (boots: 33% ; orthoses: 25%) compared to other injured body regions (Table 2).
There was not a significant difference in the number of assistive devices provided or prescribed by injury type (X2(N = 427, df = 4) = 1.2, p = 0.76), sex (X2(N = 427, df = 2) = 0.04, p = 0.84), nor year (X2(N = 427, df = 10) = 11.3, p = 0.336). There was a significant difference in the proportion of devices provided by year (X2(N = 427, df = 6) = 28.1, p = 0.002). A larger proportion of braces and/or compression sleeves were provided between 2011–2012 compared to later years (average 9% vs. 3%), and the same trend was noted for orthoses (average of 16% visits vs. 9% ; Fig. 1). There were no significant differences in specific devices by injury types or sex.
3.3Medications and supplements
The majority of medications and supplements administered or prescribed were vitamin D (26%), followed by non-steroidal anti-inflammatories (NSAIDs; 22%), calcium (18%), and ultrasound-guided corticosteroid injections (9% ; Table 3). Foot injuries received the highest number of medications or supplements per visit with administration or prescription (1.45±0.55), followed by injuries to the shins (1.43±0.50) and injuries to the thighs (1.36±0.50; Table 3). There was a significant difference in the types of medications and supplements by injury types (X2 range: 23.6–71.4; p-range: < 0.001–0.003); vitamin D, calcium, and iron supplements were most frequently administered or prescribed for patients with shin injuries (vitamin D: 56% ; calcium: 56% ; iron: 50%) compared to other injured body regions. NSAIDs were primarily provided for patients with shin injuries, while corticosteroid injections were primarily performed for those with hip injuries (Table 3).
A larger proportion of medications and supplements were prescribed or administered for patients with bone stress injuries compared to soft tissue injuries (X2(N = 397, df = 2) = 15.4, p < 0.001; Table 3). However, when assessing specific medication and supplement subtypes, there were comparable proportions of administrations or prescriptions across injury types. Although the proportion of medications and supplements prescribed or administered was similar across the observed years, there were significant differences in the types of medications and supplements by year (X2 range: 19.6–26.8; p-range: 0.003–0.03). NSAIDs were more frequently administered during the years 2011–2012 compared to later years (average of 9% of visits vs. 5% ; Fig. 1). Iron supplements were more frequently administered from 2018–2021 compared to previous years (average of 3% of visits vs. 1% ; Fig. 1). There were no significant differences in number or type medications by sex (X2(N = 397, df = 2) = 2.4, p = 0.12).
3.4Referrals
The majority of referrals across all injuries were for physical rehabilitation (52% of all referrals), followed by gait-training (14%) and nutrition consultations (8%). Patients with shin (43% gait-training referrals), knee (16%), and hip injuries (15%) were most frequently referred for gait-training compared to other injured body regions (X2(N = 2,116, df = 4) = 24.6, p = 0.002; Table 4). Patients with shin injuries had the highest number of total referrals (N = 1,465, 42% of all referrals) and referrals per visit (X2(N = 2,116, df = 4) = 132.0, p < 0.001; Table 4). Approximately half of all referrals for nutrition were for patients with shin injuries (X2(N = 286, df = 4) = 70.6, p < 0.001; Table 4).
There were significant differences in the proportion of nutrition types by year (X2 range: 23.8–31.0; p-range: < 0.001–0.01). There were higher proportions of nutrition referrals between the years 2015–2021 compared to 2011–2014 (average of 14% of visits vs. 7% ; Fig. 1). A similar trend was observed for increased gait-training referrals between 2014–2021 compared to 2011–2013 (22% of visits vs. 13% ; Fig. 1). There were significantly higher proportions of referrals for psychiatric consultation during the 2020–2021 years of the pandemic compared to previous years (4% of visits vs. 1% ; Fig. 1). There was not, however, a significant difference in the number of patient referrals by injury type (X2(N = 2,116, df = 4) = 3.6, p = 0.61), sex (X2(N = 2,116, df = 2) = 0.01, p = 0.94), nor year (X2(N = 2,116, df = 10) = 6.4, p = 0.78). Additionally, there were no significant differences in the specific types of referrals by injury type or sex.
4Discussion
Clinical assessments and treatment efforts were found to be most commonly dedicated to adolescent patients with running-related shin injuries seeking care at a specialized IRC. Most conditions were classified using patient history and physical examinations. Referrals primarily focused on physical rehabilitation and movement analyses. Most devices were offered for off-loading or stability, and supplements or NSAIDs were most frequently administered to RRI patients. There were key changes in treatment and referral patterns around the year 2015 and onward, coinciding with emerging evidence in sports medicine literature that influenced clinical care of adolescents with RRIs [7, 15].
Stress fractures to the shin and medial tibial stress syndrome (or “shin splints”) are major concerns for young runners [8, 18–21]. The current study suggests that shin injuries require the majority of clinical resources, highlighting the difficulty in diagnosing and managing injuries in this anatomical region given the high number of imaging and referrals, respectively [22, 23]. Shin injuries were diagnosed using the largest proportion of imaging services to differentiate subtle differences between medial tibial stress syndrome and bone stress injuries, allowing providers to discern the appropriate management path based on injury. Patients with repetitive stress injuries at the shin also have high likelihood of re-injury [24]. As such, it is unsurprising that RRIs involving the shin were treated with the largest proportion of offloading devices provided or prescribed to promote rest and re-imaging to clinically gauge healing.
Both bone stress injuries and shin injuries had the highest proportion of blood panels/urinalyses, nutrition referral patterns, and micronutrient supplements, with the largest upticks of these analyses and treatments occurring around the year 2015. These shifts in clinical management coincided with the emergence of the 2014 International Olympic Committee’s consensus statement on RED-S that emphasized the need for early recognition of metabolic disruption and nutritional education in the evaluation and management of overuse injuries [16]. Given that poor bone health is one prong of the female athlete triad and has been substantially associated with RED-S for males and females alike [16], it is unsurprising that bone stress injuries received the majority of these assessment, referral, and treatment resources [9, 25]. Furthermore, there were increased iron supplements prescribed from 2018 onward, which aligns with the consensus update recognizing hematologic abnormalities as key parts of the constellation of health-related problems linked to RED-S [17]. It was unexpected to find no significant difference in iron supplements between male and female patients; this may be attributed to equivocal numbers of blood samples taken across patients that led to identified iron deficiencies and subsequent supplements. While it is likely that other factors influenced treatment trends noted in this assessment, the publication of these consensus statements may partially explain the trends observed in the clinic. The IRC frequently engages in running-related research and conducts educational meetings quarterly, which supports the integration of evidence-based medicine into practice. This model may be considered as a framework for additional clinics across the country to improve long-term outcomes for runners; however, future prospective research is necessary to substantiate this notion. While biomarkers related to soft-tissue injury and recovery are rising in popularity [26], these areas of research are still developing [7, 25].
There was a downward trend in NSAID prescriptions for RRIs in this adolescent patient population following 2012. This coincided with the emergence of several research studies and journal editorials evaluating NSAID medications’ mechanism of action, efficacy, and potential risks and benefits, ultimately recommending that clinicians minimize the use of anti-inflammatory medications in the treatment of certain musculoskeletal injuries [27, 28]. The inflammatory process is designed to promote blood flow to injury sites to aid in tissue healing, and some studies have suggested that NSAIDs may suppress these effects and potentially lengthen the recovery process [29, 30]. These findings show that there have been key shifts in treatment trends with NSAID use based on expert recommendations. It appears that the focus of clinical management shifted towards interventions to address underlying factors, support bone health, and reduce biomechanical strain with reduced prescription of NSAIDs [6].
In juxtaposition to the adult running medicine literature, there is limited evidence assessing biomechanical contributors to the development of adolescent RRIs [7, 11]. One study identified slower cadence for young athletes with overuse shin and knee injuries, suggesting this gait parameter may be a target for intervention [31]. These findings suggest that gait-training referrals are frequently given to patients with shin injuries, which aligns with this available evidence. However, patients with additional RRIs were still referred for gait analysis and intervention, suggesting that clinicians may rely on data from adult runners to guide intervention. Continued explorations into biomechanical factors pertaining to a wider range of adolescent RRIs are warranted to facilitate effective diagnosis-specific gait-training interventions when indicated [7, 11]. Furthermore, evidence regarding associations between training volume and injury development among adolescents is needed to better facilitate recommendations for youth runners [32].
The COVID-19 pandemic distinctly influenced clinical treatment, as the format of visits had to transition to telehealth platforms during strict social isolation mandates. Telehealth visits were not a part of routine practice prior to the year 2020; however, this assessment approach may be advantageous in future practice to not only mitigate risk for infectious exposures, but also to reduce the barrier to seeking care for adolescent athletes [33]. Additionally, there were more psychiatric/mental health referrals for adolescent RRI patients between 2020 and 2021 compared to years prior. Previous research during early stages of the pandemic identified that runners who had to change their running behaviors, whether due to injury or other factors, had a higher propensity to report loneliness and negative affect on mental health questionnaires [34]. As such, mental health concerns were likely to become more prevalent and identified among adolescent runners with RRIs seeking clinical care. These changes highlight the importance of continued assessment of mental wellbeing to address psychosocial contributors to adolescent RRI and recovery [35].
4.1Future directions
With the continued development of novel treatment parameters (e.g., platelet-rich plasma injections) [36, 37] and continued research on micro- and macro-level contributors to injury [11], it will be important to continue to assess therapeutic interventions and successes for adolescent athletes seeking care. There is also a need to bolster the evidence regarding age-specific approaches to care for adolescent runners, given that metabolic assessments have been primarily conducted among adults [16, 17]. The continued impact on advancements in sports medicine will be essential to determine changes in assessment and treatment components of clinic visits as well as long-term outcomes following clinical intervention.
4.2Limitations
This study focused on clinic visit trends from a single location. The majority of the patients in the dataset were White females. Given this limitation, the findings may not reflect nationwide trends in more diverse populations. The study team did not have access to information regarding training volume and intensity, nor additional injury characteristics (e.g., time loss vs. non-time loss). However, these factors may have influenced patient care. The hospital-affiliated clinic had access to specialists for referrals to complement treatments, such as gait analysis and gait-training, which may not be possible across all clinical sites. As the hospital system was affiliated with a university, education regarding athlete health and best practices may have been more prevalent compared to other clinical settings. There were no data available to determine treatment success; however, future research should collect and measure patient-reported outcomes and other clinical markers to address this gap in the literature. All RRIs in this study were non-surgical and did not reflect treatment and referral patterns for more severe RRI cases.
5Conclusion/summary
Adolescent patients with running-related shin injuries received the most clinical assessments and treatment resources, as well as number of referrals during episodes of clinical care, suggesting that these injuries require considerably more clinical resources than other injuries. Across all injuries, the most common assessment, referral, and treatment approaches were manual/special tests, physical therapy, orthoses, and micronutrient supplements. There were shifts in clinical assessments and treatment approaches that suggest evolving, evidence-based shifts in clinical practice. Continued research on youth running will be essential for advancing clinical practice.
Acknowledgments
None.
Conflict of interest
Dr. Meehan receives royalties from 1) ABC-Clio publishing for the sale of his books, Kids, Sports, and Concussion: A guide for coaches and parents, and Concussions; 2) Springer International for the book Head and Neck Injuries in Young Athlete and 3) Wolters Kluwer for working as an author for UpToDate. His research is funded, in part, by philanthropic support from the National Hockey League Alumni Association through the Corey C. Griffin Pro-Am Tournament and a grant from the National Football League. There are no additional conflicts of interest to disclose.
Funding
None.
References
[1] | Hills AP , Dengel DR , Lubans DR . Supporting public health priorities: recommendations for physical education and physical activity promotion in schools, Prog Cardiovasc Dis.. (2015) ;57: (4):368–74. doi: 10.1016/j.pcad.2014.09.010. |
[2] | Lavie CJ , Lee D-C , Sui X , et al. Effects of Running on Chronic Diseases and Cardiovascular and All-Cause Mortality, Mayo Clin Proc. (2015) ;90: (11):1541–52. doi: 10.1016/j.mayoc2015.08.001. |
[3] | The National Federation of State High School Associations. 2018-2019 High School Athletics Participation Survey. [accessed 31 August 2018]. Available from: https://www.nfhs.org/media/1020412/2018-19 participation survey.pdf |
[4] | Tenforde AS , Sayres LC , McCurdy ML , Collado H , Sainani KL , Fredericson M . Overuse injuries in high school runners: lifetime prevalence and prevention strategies. PMR. (2011) ;3: (2):125–31; quiz 131. doi: 10.1016/j.pmrj.2010.09.009. |
[5] | Goldman JT , Miller E , Runestad S , Serpa R , Beck J . Should Adolescents Run Marathons?: Youth Marathon Training Injury Epidemiology and Risk Factors, Clin J Sport Med. (2022) ;32: (3):e293–e299. doi: 10.1097/JSM.0000000000000870. |
[6] | Marshall AN , McLeod TCV , Lam KC . Characteristics of Injuries Occurring During Cross- Country: A Report from the Athletic Training Practice- Based Research Network, J Athl Train. (2020) ;55: (12):1230–1238. doi: 10.4085/1062-6050-541-19. |
[7] | Krabak BJ , Roberts WO , Tenforde AS , et al. Youth running consensus statement: minimising risk of injury and illness in youth runners, Br J Sports Med. (2021) ;55: (6):305–318. doi: 10.1136/bjsports-2020-102518. |
[8] | Tenforde AS , DeLuca S , Wu AC , et al. Prevalence and Factors Associated with Bone Stress Injury in Middle School Runners, PM R. (2022) ;14: (9):1056–1067. doi: 10.1002/pmrj.12673. |
[9] | Ackerman KE , Holtzman B , Cooper KM , et al. Low energy availability surrogates correlate with health and performance consequences of Relative Energy Deficiency in Sport, Br J Sports Med. (2019) ;53: (10):628–633. doi: 10.1136/bjsports-2017-098958. |
[10] | DeJong Lempke AF , Whitney KE , Collins SE , dHemecourt PA , Meehan WP . Intrinsic and Extrinsic Factors Contributing to Running-Related Lower Limb Injuries Among Adolescent Runners, J Sports Sci. (2022) ;40: (22):2468–2474. doi: 10.1080/02640414.2022.2163353. |
[11] | McSweeney SC , Grävare Silbernagel K , Gruber AH , et al. Adolescent Running Biomechanics - Implications for Injury Prevention and Rehabilitation, Front Sports Act Living.46. (2021) ;3: :689846. doi: 10.3389/fspor.2021.689846. |
[12] | Rauh MJ . LEG-LENGTH INEQUALITY AND RUNNING-RELATED INJURY AMONG HIGH SCHOOL RUNNERS, Int J Sports Phys Ther. (2018) ;13: (4):643–651. |
[13] | Rauh MJ , Koepsell TD , Rivara FP , Rice SG , Margherita AJ . Quadriceps angle and risk of injury among high school cross-country runners, J Orthop Sports Phys Ther. (2007) ;37: (12):725–33. doi: 10.2519/jospt.2007.2453. |
[14] | Luedke LE , Heiderscheit BC , Williams DSB , Rauh MJ . Association of Isometric Strength of Hip and Knee Muscles with Injury Risk in High School Cross Country Runners, Int J Sports Phys Ther. (2015) ;10: (6):868–76. |
[15] | Krabak BJ , Snitily B , Milani CJE . Running Injuries During Adolescence and Childhood, Phys Med Rehab Clin N Am. (2016) ;27: (1):179–202. doi: 10.1016/j.pmr.2015.08.010. |
[16] | Mountjoy M , Sundgot-Borgen J , Burke L , et al. The IOC consensus statement: beyond the Female Athlete Triad–Relative Energy Deficiency in Sport (RED-S), Br J Sports Med. (2014) ;48: (7):491–7. doi: 10.1136/bjsports-2014-093502. |
[17] | Mountjoy M , Sundgot-Borgen JK , Burke LM , et al. IOC consensus statement on relative energy deficiency in sport (RED-S): update, Br J Sports Med. (2018) ;52: (11):687–697. doi: 10.1136/bjsports-2018-099193. |
[18] | Changstrom BG , Brou L , Khodaee M , Braund C , Comstock RD . Epidemiology of stress fracture injuries among US high school athletes, 2005-2006 through 2012-2013, AmJ Sports Med. (2015) ;43: (1):26–33. doi: 10.1177/0363546514562739. |
[19] | Rauh MJ , Macera CA , Ji M , Wiksten DL . Subsequent injury patterns in girls’ high school sports, J Athl Train. (2007) ;42: (4):486–94. |
[20] | Rauh MJ , Margherita AJ , Rice SG , Koepsell TD , Rivara FP . High School Cross Country Running Injuries: A Longitudinal Study, Clin J Sport Med. (2000) ;10: (2):110–6. doi: 10.1097/00042752-200004000-00005. |
[21] | Rauh MJ , Koepsell TD , Rivara FP , Margherita AJ , Rice SG . Epidemiology of Musculoskeletal Injuries among High School Cross-Country Runners, Am J Epidemiol. (2006) ;163: (2):151–9. doi: 10.1093/aje/kwj022. |
[22] | Winters M . The diagnosis and management of medial tibial stress syndrome: An evidence update, Unfallchirurg.. (2020) ;123: (Suppl 1):15–19. doi: 10.1007/s00113-019-0667-z. |
[23] | Galbraith RM , Lavallee ME . Medial tibial stress syndrome: conservative treatment options, Curr Rev Musculoskelet Med. (2009) ;2: (3):127–33. doi: 10.1007/s12178-009-9055-6. |
[24] | Winters M , Bakker EWP , Moen MH , Barten CC , Teeuwen R , Weir A . Medial tibial stress syndrome can be diagnosed reliably using history and physical examination, Br J Sports Med. (1272) ;52: (19):1267–1272. doi: 10.1136/bjsports-2016-097037. |
[25] | Heikura IA , Uusitalo ALT , Stellingwerff T , Bergland D , Mero AA , Burke LM . Low Energy Availability Is Difficult to Assess but Outcomes Have Large Impact on Bone Injury Rates in Elite Distance Athletes, Int J Sport Nutr Exerc Metab. (2018) ;28: (4):403–411. doi: 10.1123/ijsnem.2017-0313. |
[26] | Lee EC , Fragala MS , Kavouras SA , Queen RM , Pryor JL , Casa DJ Biomarkers in Sports and Exercise: Tracking Health, Performance, and Recovery in Athletes, J Strength Cond Res. (2017) ;31: (10):2920–2937. doi: 10.1519/JSC.0000000000002122. |
[27] | Bleakley CM , Glasgow P , MacAuley DC . PRICE needs updating, should we call the POLICE? Br J Sports Med. (2012) ;46: (4):220–1. doi: 10.1136/bjsports-2011-090297. |
[28] | Paoloni JA , Milne C , Orchard J , Hamilton B . Non-steroidal anti-inflammatory drugs in sports medicine: guidelines for practical but sensible use, Br J Sports Med. (2009) ;43: (11):863–5. doi: 10.1136/bjsm.2009.059980. |
[29] | Dubois B , Esculier J-F . Soft-tissue injuries simply need PEACE and LOVE, Br J Sports Med. (2020) ;54: (2):72–73. doi: 10.1136/bjsports-2019-101253. |
[30] | Vuurberg G , Hoorntje A , Wink LM , et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline, Br J Sports Med. (2018) ;52: (15):956. doi: 10.1136/bjsports-2017-098106. |
[31] | Luedke LE , Heiderscheit BC , Williams DSB , Rauh MJ . Influence of Step Rate on Shin Injury and Anterior Knee Pain in High School Runners, Med Sci Sports Exerc. (2016) ;48: (7):1244–50. doi: 10.1249/MSS.0000000000000890. |
[32] | Rauh MJ . Summer Training Factors and Risk of Musculoskeletal Injury Among High School Cross-country Runners, J Orthop Sports Phys Ther. (2014) ;44: (10):793–804. doi: 10.2519/jospt.2014.5378. |
[33] | Bate NJ , Xu SC , Pacilli M , Roberts LJ , Kimber C , Nataraja RM . Effect of the COVID-19 induced phase of massive telehealth uptake on end-user satisfaction, Intern Med J. (2021) ;51: (2):206–214. doi: 10.1111/imj.15222. |
[34] | Holmes HH , Monaghan PG , Strunk KK , Paquette MR , Roper JA . Changes in Training, Lifestyle, Psychological and Demographic Factors, and Associations With Running-Related Injuries During COVID-19, Front Sports Act Living. (2021) ;3: :637516. doi: 10.3389/fspor.2021.637516. |
[35] | Covassin T , Beidler E , Ostrowski J , Wallace J . Psychosocial Aspects of Rehabilitation in Sports, Clin Sports Med. (2015) ;34: (2):199–212. doi: 10.1016/j.csm.2014.12.004. |
[36] | Mitchkash M , Robinson D , Tenforde AS . Efficacy of Extracorporeal Pulse-Activated Therapy in the Management of Lower-Extremity Running-Related Injuries: Findings From a Large Case Cohort, J Foot Ankle Surg.. (2020) ;59: (4):795–800. doi: 10.1053/j.jfas.2020.02.008. |
[37] | de Vos RJ , Weir A , van Schie HTM , et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial, JAMA. (2010) ;303: (2):144–9. doi: 10.1001/jama.2009.1986. |




