Prevalence and goal attainment with spinal orthoses for children with cerebral palsy
Abstract
PURPOSE:
Analyze the goals for treatment and attained goals for spinal orthoses in children with cerebral palsy (CP), and describe the use of spinal orthoses in relation to age, sex, gross motor function, and scoliosis.
METHODS:
Cross-sectional data for all children born between 2000 and 2014 and registered in the Swedish CP registry were analyzed in relation to age, sex, Gross Motor Function Classification System (GMFCS), and scoliosis. Treatment goals were to 1) prevent deformity; 2) improve stability/positioning; 3) improve head control; and 4) improve arm/hand function.
RESULTS:
Overall, 251 of the 2800 children (9%) used spinal orthoses, and the frequency increased significantly with age and GMFCS level; 147 of the 251 children had scoliosis. Several treatment goals were reported for most children. The most common goal was improved stability/positioning (96%), followed by head control (51%) and arm/hand function (38%). Only one third of the children used spinal orthoses to prevent deformities. The rate of goal attainment was 78–87% for the functional outcomes and 57% for the prevention of deformities.
CONCLUSION:
Although the goal of using spinal orthosis to prevent curvature progression remains important, we found that its functional benefits (stability, head control, arm/hand function) were of greater importance.
1.Introduction
1.1Cerebral palsy
Movement and posture are key problems for children with cerebral palsy (CP) [1]. These may present as difficulties with the adaptation and fine tuning of postural muscles, which possibly cause impaired stability [2]. A lack of stability can affect both head and hand control [3]. Without adequate support, there is an increased risk that children will develop functional quadriplegia and require higher levels of care and nursing [4], thereby reducing the individual’s independence. The severity of motor impairment can be classified according to the Gross Motor Function Classification System (GMFCS) [5]. Inability to deal with the effects of gravity, combined with immobility, spasticity, and muscle weakness, lead to an increased risk of developing muscle contractures, skeletal deformities, hip dislocation, and scoliosis from early childhood [6].
1.2Spinal orthoses
Lack of stability is often the main indication for supports such as spinal orthoses [7, 8]. Previous studies have reported that spinal orthoses can provide functional benefits such as stability [9], head control [7, 10], and hand control [7, 8], all of which preserve and improve functional abilities that are vital to the quality of life for children with CP. Spinal orthoses appear to be effective for the treatment of adolescent idiopathic scoliosis [11]; however, the results for neuromuscular scoliosis are more ambiguous [8, 9, 12]. The main indication for spinal orthoses in these patients is often to stabilize and delay the progression of the spinal curvature [8, 12]. Nevertheless, there remains a lack of knowledge regarding the treatment goals and the level of goal attainment for the use of spinal orthoses in children with CP [6].
1.3Scoliosis
Posture and stability can also be affected by scoliosis [7, 13, 14]. Scoliosis develops in approximately 25% of children with CP, and can be a significant problem depending on the child’s age, neurological subtype, and GMFCS level [14]. Scoliosis may progress into adulthood with a higher risk for individuals at GMFCS levels IV and V [15]. Pronounced scoliosis not only affects the spine but also has a great impact on quality of life and factors such as sitting ability, transfers, pain, and care needs [16]. Scoliosis that is left untreated can cause respiratory and cardiac complications and premature death [4]. Other available approaches that aim to improve stability include adaptive seating, orthotics, and postural management [13, 17], while surgery may be the definitive treatment option for scoliosis [9, 13, 17].
1.4Aim
Currently, there is a lack of knowledge regarding how spinal orthoses are used in the population of children with CP. The aim of the present study was to analyze the treatment goals for, and goal attainment levels with, spinal orthoses in a population of children with CP and to describe the use of spinal orthoses in relation to age, sex, gross motor function, and scoliosis.
2.Material and methods
2.1Ethical approval and consent
The study was approved by the Medical Research Ethics Committee at Lund University, and permission was obtained to extract data from the Swedish National Cerebral Palsy Surveillance Program and Registry (CPUP). All participants consented to contribute to research based on reported data.
2.2Data collection and participants
This cross-sectional study included all children with CP in Sweden born between 2000 and 2014 who were reported to and included in CPUP. Data were extracted from the most recent physiotherapy assessment for each child between 1 January 2013 and 31 December 2014. CPUP was initiated in the south of Sweden in 1994 to prevent hip dislocations, contractures, and deformities in children with CP [18, 19]. This combined surveillance program and registry represents all children with CP in Sweden with a coverage rate of over 95% [20]. The cohort includes children aged younger than 4 years with suspected but not yet confirmed CP. Usually, the child’s diagnosis is verified by a neuropediatrician at the age of 4 years, and children who do not fulfil the criteria are excluded. Exclusion and inclusion criteria are in accordance with those of the Surveillance of Cerebral Palsy network in Europe, including a brain injury occurring before the age of 2 years [21].
2.3Classifications and measurements
The children were examined twice a year by their local physiotherapist according to a standardized protocol until the age of 6 years and once a year thereafter [22]. The measurements were reported on a web-based survey form and are stored in the CPUP database.
Table 1
Details of the 2800 participants aged 0–14 years
| Age | Number of | Sex | GMFCS | |||||
|---|---|---|---|---|---|---|---|---|
| children | Boys | Girls | I | II | III | IV | V | |
| 6 | 3 | 3 | 0 | 3 | 0 | 0 | 3 | |
| 1 | 91 | 55 | 36 | 29 | 21 | 9 | 17 | 15 |
| 2 | 170 | 95 | 75 | 74 | 22 | 22 | 26 | 26 |
| 3 | 202 | 111 | 91 | 88 | 30 | 25 | 27 | 32 |
| 4 | 215 | 121 | 94 | 99 | 34 | 19 | 36 | 27 |
| 5 | 295 | 178 | 117 | 144 | 37 | 28 | 48 | 38 |
| 6 | 246 | 142 | 104 | 118 | 35 | 26 | 28 | 39 |
| 7 | 233 | 138 | 95 | 100 | 48 | 19 | 24 | 42 |
| 8 | 237 | 146 | 91 | 97 | 42 | 23 | 44 | 31 |
| 9 | 194 | 101 | 93 | 80 | 31 | 16 | 34 | 33 |
| 10 | 233 | 148 | 85 | 121 | 36 | 13 | 31 | 32 |
| 11 | 206 | 115 | 91 | 76 | 38 | 15 | 32 | 45 |
| 12 | 217 | 119 | 98 | 91 | 40 | 19 | 33 | 34 |
| 13 | 168 | 87 | 81 | 57 | 40 | 11 | 31 | 29 |
| 14 | 87 | 55 | 32 | 36 | 13 | 9 | 12 | 17 |
| Total | 2800 | 1614 | 1186 | 1210 | 470 | 254 | 423 | 443 |
2.3.1Gross Motor Function Classification System
Each child’s gross motor skills were classified according to the expanded and revised version of the GMFCS with the additional age band for 12 to 18 years, where level I describes the highest and level V describes the lowest functional level [5].
2.3.2Clinical examination of the spine
A clinical examination of the spine was performed by the physiotherapist with the child in a sitting position on a plinth, both in a forward bend and upright. This spinal examination has been evaluated for psychometric properties and shows a high concurrent validity compared with the radiographic Cobb angle, having a sensitivity of 75% (95% confidence interval [CI]; 19.4–99.4), specificity of 95.8% (95% CI; 78.9–99.9), and excellent interrater reliability (kappa
• No Scoliosis.
• Mild: A discreet curvature visible only on a thorough examination during forward bending.
• Moderate: An obvious curvature visible during both upright and forward bending positions.
• Severe: A pronounced curvature preventing the child from attaining an upright position without external support.
2.4Spinal orthoses – treatment goals and goal attainment
The use of a spinal orthosis was reported as “yes” or “no” for each child. All prefabricated or individually molded spinal orthoses were included. Treatment goals were set for each child by collaboration between the family and therapist based on four possible options available in the database: 1) prevent deformity, 2) improve stability/positioning, 3) improve arm/hand function, and 4) improve head control. Note that several goals could be reported for each child, depending on the child’s individual needs. In this study, we considered goal 1 to focus mainly on body structure, and the prevention of deformity was defined as prevention, reduction, or stabilization of scoliosis. Goals 2, 3, and 4 focus more on activities and body function, and are hereafter referred to as functional goals. Attainment for each goal chosen was noted as “yes” or “no”, that is, whether or not the child attained the intended goal using the spinal orthosis. All responses were reported by the physiotherapists in cooperation with the children and their families.
2.5Statistical analyses
For descriptive statistics, categorical data were reported as frequencies and percentages,
Table 2
The use of spinal orthoses in numbers and percentages of children with cerebral palsy, the structural and functional treatment goals and the rate of goal attainment relative to their age, sex, GMFCS level and degree of scoliosis
| Total number | Spinal orthosis | Prevent deformity | Improve stability/positioning | Improve arm/hand function | Improve head control | ||||||||||
| Age | N | N (%) | G | GA (%) | G | GA (%) | G | GA (%) | G | GA (%) | |||||
| | 6 | 0 | (0.0) | 0 | 0 | (0.0) | 0 | 0 | (0.0) | 0 | 0 | (0.0) | 0 | 0 | (0.0) |
| 1 | 91 | 1 | (1.1) | 1 | 0 | (0.0) | 1 | 0 | (0.0) | 0 | 0 | (0.0) | 0 | 0 | (0.0) |
| 2 | 170 | 6 | (3.5) | 1 | 0 | (0.0) | 5 | 5 | (100) | 3 | 2 | (67) | 5 | 4 | (80) |
| 3 | 202 | 14 | (6.9) | 2 | 1 | (50) | 14 | 12 | (86) | 5 | 4 | (80) | 7 | 6 | (86) |
| 4 | 215 | 14 | (6.5) | 4 | 2 | (50) | 13 | 11 | (85) | 8 | 6 | (75) | 10 | 6 | (60) |
| 5 | 295 | 27 | (9.2) | 5 | 4 | (80) | 25 | 24 | (96) | 12 | 11 | (92) | 15 | 12 | (80) |
| 6 | 246 | 19 | (7.7) | 10 | 7 | (70) | 19 | 16 | (84) | 8 | 7 | (88) | 12 | 10 | (83) |
| 7 | 233 | 2 | (10) | 8 | 6 | (75) | 23 | 20 | (87) | 9 | 7 | (78) | 12 | 7 | (58) |
| 8 | 237 | 25 | (10) | 7 | 4 | (57) | 24 | 21 | (88) | 11 | 8 | (73) | 13 | 11 | (85) |
| 9 | 194 | 26 | (13) | 7 | 5 | (71) | 26 | 22 | (85) | 8 | 7 | (88) | 10 | 9 | (90) |
| 10 | 233 | 19 | (8.2) | 8 | 7 | (88) | 18 | 17 | (94) | 5 | 5 | (100) | 10 | 8 | (80) |
| 11 | 206 | 25 | (12) | 9 | 4 | (44) | 24 | 19 | (79) | 5 | 4 | (80) | 10 | 8 | (80) |
| 12 | 217 | 24 | (11) | 11 | 4 | (36) | 24 | 21 | (88) | 12 | 9 | (75) | 12 | 11 | (92) |
| 13 | 168 | 19 | (11) | 5 | 2 | (40) | 18 | 16 | (89) | 6 | 5 | (83) | 7 | 4 | (57) |
| 14 | 87 | 8 | (9.2) | 5 | 1 | (20) | 7 | 5 | (71) | 4 | 2 | (50) | 4 | 3 | (75) |
| Sex | |||||||||||||||
| Boys | 1614 | 135 | (8.4) | 44 | 22 | (50) | 132 | 115 | (87) | 50 | 40 | (80) | 72 | 57 | (72) |
| Girls | 1186 | 116 | (9.8) | 39 | 25 | (64) | 109 | 94 | (86) | 46 | 37 | (80) | 55 | 42 | (76) |
| GMFCS | |||||||||||||||
| III | 254 | 4 | (1.6) | 1 | 0 | (0.0) | 3 | 2 | (67) | 1 | 1 | (100) | 0 | 0 | (0.0) |
| IV | 423 | 77 | (18) | 23 | 14 | (61) | 76 | 68 | (89) | 51 | 40 | (78) | 38 | 31 | (82) |
| V | 443 | 170 | (38) | 59 | 33 | (56) | 162 | 139 | (80) | 44 | 36 | (81) | 89 | 68 | (76) |
| Scoliosis | |||||||||||||||
| No | 2312 | 113 | (4.8) | 26 | 18 | (69) | 110 | 97 | (88) | 54 | 44 | (81) | 68 | 54 | (79) |
| Mild | 333 | 56 | (17) | 14 | 10 | (71) | 55 | 44 | (80) | 24 | 20 | (83) | 25 | 18 | (72) |
| Moderate | 71 | 39 | (55) | 16 | 9 | (56) | 36 | 34 | (94) | 5 | 4 | (80) | 14 | 10 | (71) |
| Severe | 64 | 43 | (67) | 27 | 10 | (37) | 40 | 34 | (85) | 13 | 9 | (69) | 20 | 17 | (85) |
| Total | 2800 | 251 | 83 | 47 | (57) | 241 | 209 | (87) | 96 | 77 | (80) | 127 | 99 | (78) | |
GMFCS
3.Results
3.1Demographics
In total, results from 2800 children (58% boys, 42% girls) with a median age of 7 years (range 0–14 years) were reported to the CPUP registry. The children were classified at GMFCS levels I (43%), II (17%), III (9.1%), IV (15%), and V (16%). The distributions of age, sex, and GMFCS levels are presented in Table 1.
3.2Spinal orthoses
Overall, 251 (9%) of the 2800 children, 135 (54%) boys and 116 (46%) girls, used spinal orthoses. Their median age was 8.0 years (range 1–14 years). The proportion of children using spinal orthoses increased with age (
Figure 1.
Number of children with each goal and the rate of goal attainment.
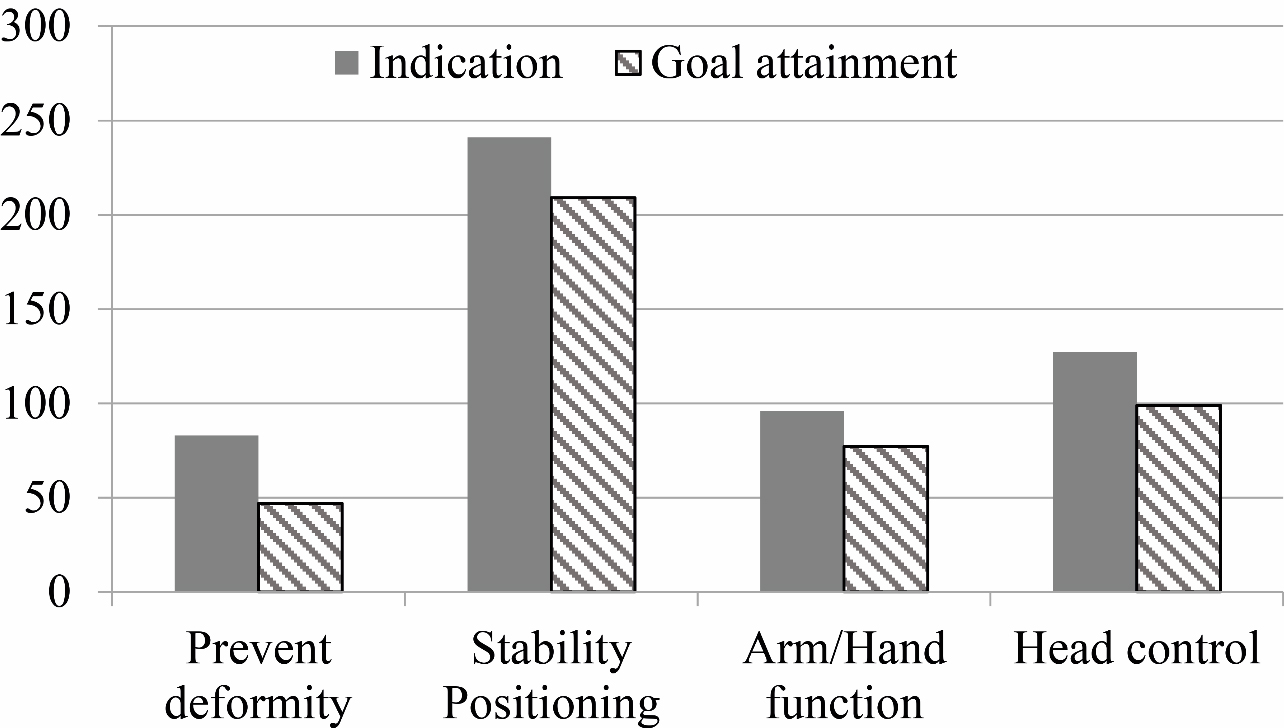
3.2.1Goals to improve function and goal attainments
Almost all children at GMFCS levels III to V used spinal orthoses to improve function with one or more of the following goals: improve stability/positioning; improve arm/hand function; or improve head control (Fig. 1). There were no significant differences in either goals or goal attainment levels in relation to age or sex (Table 2). Several goals were reported for most children. Improved stability and positioning were the most common treatment goals reported for 241 (96%) of the 251 children, of whom 209 (87%) attained the goal. These children ranged in age from 2 to 14 years. A higher proportion of children classified at GMFCS levels IV (99%) and V (95%) used spinal orthoses for stability/positioning (
3.2.2Goal to prevent deformity and goal attainment
Only one third of the children (83 of 251) used spinal orthoses to prevent deformity. Of these 83 children, 47 (57%) attained the goal, meaning their spine was either stabilized with no progression of spinal deformity or had improved over the previous year. These children ranged in age from 3 to 14 years. There were no significant differences in the goal to prevent deformity or goal attainment in relation to age or sex (Table 2). A higher proportion of children with moderate (41%) and severe scoliosis (63%) used spinal orthoses to prevent deformity compared with children with no (23%) or mild (25%) scoliosis only visible during forward bending. Goal attainment to prevent deformity was proportional to the severity of the scoliosis, ranging from 71% reported success in children with mild scoliosis to 37% in children with severe scoliosis. A higher proportion of children at GMFCS level V (59 of 170) than at GMFCS level IV (23 of 77) used a spinal orthosis to prevent deformity. Furthermore, goal attainment was slightly higher for children classified at GMFCS level IV (61%) than for those at GMFCS level V (56%) (Table 2).
3.3Scoliosis
The majority of children with scoliosis (339, 70%) were not treated with spinal orthoses. Scoliosis occurred as frequently in boys (17%) as in girls (17%). Nevertheless, a higher proportion of girls (75, 6.4%) than boys (60, 3.7%) had moderate or severe scoliosis (
4.Discussion
To our knowledge, this is the first study describing the use of spinal orthoses in a total population of children with CP. Slightly fewer than one in 10 children with CP used spinal orthoses. They were equally common in boys and girls, and usage increased with age and GMFCS level. Spinal orthoses were mostly used to improve functional outcomes, and the overall rate of goal attainment was high.
A stable posture and head control are important for optimizing function, although this can be challenging for children with severe postural deficits. For the vast majority (96%), the primary goal for the orthosis was improvement in stability/positioning. Almost nine of 10 attained this goal, consistent with the 90% success rate reported by Letts et al. [10]. Improved sitting ability has previously been reported for individuals at GMFCS levels III–V who used soft, rigid, or dynamic spinal orthoses [24, 25]. Not surprisingly, this treatment goal was reported more frequently for children at GMFCS levels IV and V than for children at level III, who usually require less trunk support. Improved head control was the second most common goal, and this was achieved in eight of 10 children, similar to the 85% success reported by Letts et al. [10]. Head control is also improved through better trunk stability [7, 8]. Use of a spinal orthosis to improve head control was slightly more frequent in children with severe scoliosis than in other groups. Other abilities, such as communication and eating, are closely connected to head control [2]. Lack of stability seriously affects arm/hand function and leads to reduced wheelchair mobility [3], whereas improved arm/hand function can enhance play and independence in activities of daily living [7, 8]. Twice as many children classified at GMFCS level IV than at levels III and V used a spinal orthosis to improve arm/hand function, highlighting the relationship between stability and arm/hand function for this group of children.
Only one in three of the children used a spinal orthosis to prevent or correct spinal deformity, making it the least common treatment goal. Goal attainment was reported by slightly fewer than three in five. These numbers are consistent with the results of a study by Olafsson et al. [12]. Seven in 10 children with mild scoliosis, but fewer than four in 10 with severe scoliosis, attained the goal of preventing spinal deformity, which indicated that the rate of goal attainment was proportional to the severity of the curvature. This may be explained by the better outcomes reported for spinal orthoses when used for smaller curvatures with radiographic Cobb angles
There are several limitations to this study. The goals for treatment and goal attainment levels were based on the performance in everyday life and not in a clinical setting, reported by the child’s physiotherapist, the child, and the caregivers. This means that there was a subjective component to the assessment; however, this demonstrated how goal attainment was perceived by the families in various settings and conditions. The number of children wearing spinal orthoses differed between GMFCS levels, with only a small number at GMFCS level III wearing spinal orthoses. The study also lacked detailed information regarding the type of spinal orthoses, including their materials and whether they were prefabricated or individually molded. In Sweden, the public health care system generally functions well, with free health care, orthotics, and assistive devices available for children with disabilities. There is no international consensus on the use of spinal orthoses; therefore, their use is likely to vary between countries. This was a cross-sectional study, where the design was used to document the status of a group at a particular point in time. It does not reflect changes over time. Nevertheless, a strength of this study was that all data had been systematically reported for the total population of children with CP in Sweden at all GMFCS levels, CP subtypes, and in both rural and urban settings.
5.Conclusions
Most children who use a spinal orthosis do so to improve function rather than prevent deformity. Goal attainment levels were high for stability, head control, and arm/hand function, indicating functional benefits for children in their daily lives. There appear to be higher goal attainment levels for prevention of deformity when spinal orthoses are used for mild scoliosis, and lower goal attainment levels when they are used for moderate or severe scoliosis. Because the ultimate treatment goal is to improve activity, participation, and quality of life, children with postural deficits should be given the opportunity to explore the functional benefits of a spinal orthosis.
Acknowledgments
We would like to thank the Norrbacka-Eugenia Foundation for grants and Stiftelsen för bistånd åt rörelsehindrade i Skåne for financial support.
Conflict of interest
The authors have no conflict of interest to report.
References
[1] | Rodby-Bousquet E, Czuba T, Hägglund G, Westbom L. Postural asymmetries in young adults with cerebral palsy. Dev Med Child Neurol. (2013) ; 55: : 1009-1015. doi: 10.1111/dmcn.12199. |
[2] | Carlberg EB, Hadders-Algra M. Postural dysfunction in children with cerebral palsy: Some implications for therapeutic guidance. Neural Plast. (2005) ; 12: : 221-228; discussion 263-272. doi: 10.1155/NP.2005.221. |
[3] | Lacoste M, Therrien M, Prince F. Stability of children with cerebral palsy in their wheelchair seating: Perceptions of parents and therapists. Disabil Rehabil Assist Technol. (2009) ; 4: : 143-150. doi: S10.1080/17483100802362036. |
[4] | Saito N, Ebara S, Ohotsuka K, Kumeta H, Takaoka K. Natural history of scoliosis in spastic cerebral palsy. Lancet. (1998) ; 351: : 1687-1692. doi: 10.1016/S0140-6736(98)01302-6. |
[5] | Palisano RJ, Rosenbaum P, Bartlett D, Livingston MH. Content validity of the expanded and revised gross motor function classification system. Dev Med Child Neurol. (2008) ; 50: : 744-750. doi: 10.1111/j.1469-8749.2008.03089.x. |
[6] | Morrell DS, Pearson JM, Sauser DD. Progressive bone and joint abnormalities of the spine and lower extremities in cerebral palsy. Radiographics. (2002) ; 22: : 257-268. doi: 10.1148/radiographics.22.2.g02mr19257. |
[7] | Rutz E, Brunner R. Management of spinal deformity in cerebral palsy: Conservative treatment. J Child Orthop. (2013) ; 7: : 415-418. doi: 10.1007/s11832-013-0516-5. |
[8] | Terjesen T, Lange JE, Steen H. Treatment of scoliosis with spinal bracing in quadriplegic cerebral palsy. Dev Med Child Neurol. (2000) ; 42: : 448-454. |
[9] | Miller A, Temple T, Miller F. Impact of orthoses on the rate of scoliosis progression in children with cerebral palsy. J Pediatr Orthop. (1996) ; 16: : 332-335. doi: 10.1097/01241398-199605000-00007. |
[10] | Letts M, Rathbone D, Yamashita T, Nichol B, Keeler A. Soft Boston orthosis in management of neuromuscular scoliosis: A preliminary report. J Pediatr Orthop. (1992) ; 12: : 470-474. |
[11] | Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the brace study of the scoliosis research society. J Bone Joint Surg Am. (1995) ; 77: : 815-822. |
[12] | Olafsson Y, Saraste H, Al-Dabbagh Z. Brace treatment in neuromuscular spine deformity. J Pediatr Orthop. (1999) ; 19: : 376-379. |
[13] | Imrie MN, Yaszay B. Management of spinal deformity in cerebral palsy. Orthop Clin North Am. (2010) ; 41: : 531-547. doi: 10.1016/j.ocl.2010.06.008. |
[14] | Koop SE. Scoliosis in cerebral palsy. Dev Med Child Neurol. (2009) ; 51: : 92-98. doi: 10.1111/j.1469-8749.2009.03461.x. |
[15] | Hägglund G, Pettersson K, Czuba T, Persson-Bunke M, Rodby-Bousquet E. Incidence of scoliosis in cerebral palsy. Acta Orthop. (2018) ; 1-5. doi: 10.1080/17453674.2018.1450091. |
[16] | Kotwicki T, Jozwiak M. Conservative management of neuromuscular scoliosis: Personal experience and review of literature. Disabil Rehabil. (2008) ; 30: : 792-798. doi: 10.1080/09638280801889584. |
[17] | Tsirikos AI, Spielmann P. Spinal deformity in paediatric patients with cerebral palsy. Current Orthopaedics. (2007) ; 21: : 122-134. doi: 10.1016/j.cuor.2007.01.001. |
[18] | Hägglund G, Alriksson-Schmidt A, Lauge-Pedersen H, Rodby-Bousquet E, Wagner P, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J. (2014) ; 96-B: 1546-1552. doi: 10.1302/0301-620X.96B11.34385. |
[19] | Hägglund G, Andersson S, Duppe H, Lauge-Pedersen H, Nordmark E, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy. The First Ten Years of a Population-based Prevention Programme. J Bone Joint Surg Br. (2005) ; 87: : 95-101. |
[20] | Westbom L, Hagglund G, Nordmark E. Cerebral palsy in a total population of 4-11 year olds in southern sweden. Prevalence and Distribution According to Different CP Classification Systems. BMC Pediatr. (2007) ; 7: : 41. doi: 10.1186/1471-2431-7-41. |
[21] | S.o.C.P.i.E. (SCPE), Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol. (2000) ; 42: : 816-824. |
[22] | Alriksson-Schmidt AI, Arner M, Westbom L, Krumlinde-Sundholm L, Nordmark E, Rodby-Bousquet E, et al. A combined surveillance program and quality register improves management of childhood disability. Disabil Rehabil. (2017) ; 39: : 830-836. doi: 10.3109/09638288.2016.1161843. |
[23] | Persson-Bunke M, Czuba T, Hägglund G, Rodby-Bousquet E. Psychometric evaluation of spinal assessment methods to screen for scoliosis in children and adolescents with cerebral palsy. BMC Musculoskelet Disord. (2015) ; 16: : 351. doi: 10.1186/s12891-015-0801-1. |
[24] | Nakamura N, Uesugi M, Inaba Y, Machida J, Okuzumi S, Saito T. Use of dynamic spinal brace in the management of neuromuscular scoliosis: A preliminary report. J Pediatr Orthop B. (2014) ; 23: : 291-298. doi: 10.1097/bpb.0000000000000034. |
[25] | Leopando MT, Moussavi Z, Holbrow J, Chernick V, Pasterkamp H, Rempel G. Effect of a soft boston orthosis on pulmonary mechanics in severe cerebral palsy. Pediatr Pulmonol. (1999) ; 28: : 53-58. |
[26] | Bertoncelli CM, Solla F, Loughenbury PR, Tsirikos AI, Bertoncelli D, Rampal V. Risk factors for developing scoliosis in cerebral palsy: A cross-sectional descriptive study. J Child Neurol. (2017) ; 32: : 657-662. doi: 10.1177/0883073817701047. |




