Self-Image in Women with Parkinson’s Disease
Abstract
There is a fundamental gap in knowledge in how Parkinson’s disease manifests and affects women throughout their hormonal life cycle, resulting in unmet needs and adversely impacting women’s quality of life. A set of questionnaires was developed and deployed through Fox Insight (open access) to address these issues by gathering data. This is the data from the first survey. The data from the questions regarding self-image were striking. 61% of women report that their Parkinson’s disease negatively impacts their self-image. Here we explore the negative impact of Parkinson’s disease on women to begin to fill the gaps in knowledge.
SELF-IMAGE IN WOMEN WITH PARKINSON’S DISEASE
Parkinson’s disease (PD) is quite unique in how it manifests in those affected—symptomatology, progression, response to treatment, and prognosis differ among individuals although diagnosed based on cardinal features. In order to achieve directed individualized patient-centric care, these variable factors in the context of age, cultural nuances, and gender-specific differences, must be considered. It is apparent that there is a significant deficit in the knowledge and research about how women manifest and cope with PD throughout different hormonal life stages with gaps in knowledge of sex-specific physical, emotional, mental, and psychosocial needs and how these change throughout a woman’s life [1].
Current literature is scarce and conflicting with how this disease affects women. There are currently no expert opinion guidelines on how to manage PD symptoms in this group. This need has led to the PD Avengers (The Global Alliance to End Parkinson’s) “Women and PD Working Group” to develop and deploy a cross-sectional questionnaire in Fox Insight, an online, longitudinal health study of people with and without PD [2]. A comprehensive set of questionnaires was developed and disseminated. The goal, to gather life experience from women with PD: diagnosis, symptoms, medication efficacy and management, home and lifestyle choices, hormone replacement, pregnancy, and birth history. It aims to broaden our knowledge of the lived experience of women with PD as it changes with hormonal status and life stages.
As the data is reviewed, an area of significant impact noted is self-image and how it correlates with quality of life for women with PD.
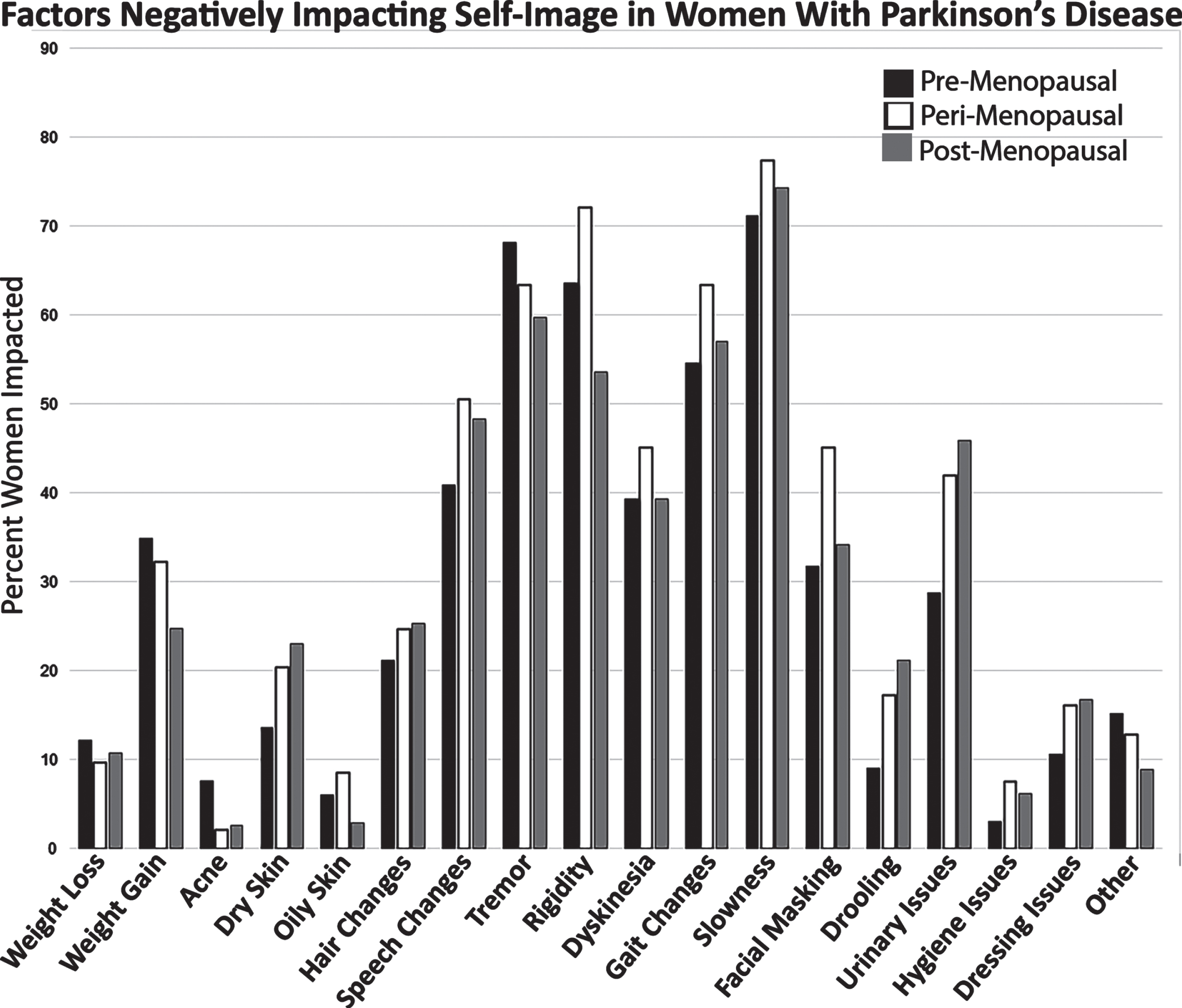
2,627 women participated in the Experience of Women with PD survey that was disseminated through Fox Insight. 13 women were excluded from further analysis as they were not diagnosed with PD for 2,614 participants. The data was further grouped into pre (4%), peri (6%), and post-menopausal (88%) cohorts. Women that selected “Not sure” or “Prefer not to answer” were not included in further analysis. It is worth noting that the sample size for pre-menopausal is small demonstrating that more needs to be done to engage and increase participation of this group as there are 2,849 women that are 45 and younger that have participated in past FI surveys (number with PD is unknown). The peri-menopausal group is also small, but much more representative due to the transient nature of this life stage. For the question, “Has your Parkinson’s disease diagnosis affected your self-image?”: 1,490 women responded yes, PD negatively impacted self-image (pre 63%, peri 61%, post 57%), 100 women responded yes, positively impacted self-image (pre 4%, peri 3%, post 0.5%), 702 responded that PD had no impact on self-image (pre 23%, peri 20%, post 27%), and 313 women responded as not sure if PD impacted their self-image (pre 1%, peri 1%, and post 1%). The “yes, negatively” group had the highest responses with motor symptoms showing they were most concerned about slowness and tremor (Fig. 1). After motor symptoms, women next report that speech changes and urinary issues negatively impact their self-image (Fig. 1). Furthermore, 2,611 women responded to, “Does Parkinson’s interfere with your social interactions?”: 242 women reported always and 1,485 reported sometimes (66%).
Fig. 1
Factors Negatively Impacting Self-Image in Women with PD. The data indicate that the slowness, rigidity, and tremor had the greatest impact on negative self-image. This is closely followed by urinary issues, speech changes, and dyskinesia.
Self-esteem may be defined as an overall sense of value or worth, a devalued concept of self-image resulting from the internalization of negative stereotypes. This construct is influenced by many factors including genetics, age, life experience, socioeconomic status, societal opinion, and health. In the case of PD, those traits that are externally visible, including tremor, excessive saliva and drooling, gait disturbances, dyskinesia, freezing, and facial masking, can be particularly impactful as their visibility may result in perceived or real external judgement. Our data confirm that these issues impact women.
Visible symptoms, like those highlighted above (Fig. 1), that are difficult to hide can result in feelings of embarrassment. Many people with PD conceal their diagnosis, trying to mask some of their clinical symptoms in public to avoid what may be thought of as scrutiny and judgement. Self-stigma is not only associated with exterior, noticeable symptoms, but also progressive loss of functionality, loss of self-efficacy and autonomy [3].
Our data support these findings from the few publications in this area. For example, in their publication Counselling in Disability and Illness, the authors write, “women who become disabled may feel unattractive or even repulsive. Limitation of movement or pain or deformity can all attack a woman’s self-image to a destructive degree.” [4].
Poor self-image or self-stigma is closely interconnected with depression and poor quality of life [5]. We know that women with PD suffer from depression at a rate of 1.3 times greater than men [6]. Low self-esteem, therefore, may have a larger impact on overall quality of life for women than for men.
In one small study [6], feelings of irritability, agitation, self-punishment, loss of pleasure, and self-dislike were mostly connected with women, reflecting predominant worthlessness and self-reproach. And women give significantly more negative assessment of their quality of life than men in “mobility", “emotional well-being", “social support", and “bodily discomfort” [7]. Self-perceived stigma was predicted by younger age and greater depression severity when quality of life was evaluated with the PDQ39 questionnaire (motor symptoms, functioning with regards to Activities of Daily Living and mood). As depression increases, the relation between PD and stigma strengthens [5]. As the survey data reveal the majority of women reported that PD negatively impacted their self-image. Stigma or poor self-image isolates and marginalizes people with PD leading to increased depression and other mental health issues, ultimately decreasing quality of life since depression is recognized as a prevalent, significant contributor to life experience. 66% of women reported that social interaction was impacted by their PD. Given that mood disorders are more prevalent in women, addressing this aspect of how a woman views herself, may be used to guide gender-specific management.
As PD is the fastest-growing and second-largest neurological condition worldwide, it warrants equality in research. High-quality, prospective, longitudinal studies analyzing gender differences may identify reliable sex-sensitive biomarkers and social markers that could translate into a more tailored clinical approach for the diagnosis and management of women, leading to improved quality of life for women with PD. Understanding differences will allow a more tailored approach to an optimization of the life experience for women with PD. These data, along with the full questionnaire, are available in Fox DEN. To access this data, researchers must complete a data use agreement at: https://foxden.michaeljfox.org. Further surveys around the impact of Parkinson’s for women pre, peri and post menopause are forthcoming.
ACKNOWLEDGMENTS
PD Avengers Women and PD Working Group: Richelle Flanaghan, Gaynor Edwards, Diane Bramble, Joy Milne, Shilpa Rao, Sabela Avion, Dr Perdita Barran, Dr Tash Fothergill-Misbah, Dr Annelien Oosterbaan, Dr Ignacio Mata, Dr Annette Hand
Leslie Kirsch ED, Joshua Gottesman, The Michael J Fox Foundation for Parkinson’s Research
Brittany Contreras, Monica Korell MPH, Caroline M Tanner MD PhD, Department of Neurology, Weill Institute for Neurosciences, University of California, San Francisco
The Fox Insight Study (FI) is funded by The Michael J. Fox Foundation for Parkinson’s Research. We would like to thank the Parkinson’s community for participating in this study to make this research possible.
Data used in the preparation of this manuscript were obtained from the Fox Insight database (https://foxinsight-info.michaeljfox.org/insight/explore/insight.jsp) on 21/12/22. For up-to-date information on the study, visit https://foxinsight-info.michaeljfox.org/insight/explore/insight.jsp.
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
REFERENCES
[1] | Subramanian I , Mathur S , Oosterbaan A , Flanagan R , Keener AM , Moro E ((2022) ) Unmet needs of women living with Parkinson’s disease: Gaps and controversies. Move Disord 37: , 444–455. |
[2] | Smolensky L , Amondikar N , Crawford K , Neu S , Kopil CM , Daeschler M , Riley L ; 23andMe Research Team; BrownE, Toga AW , Tanner C ((2020) ) Fox Insight collects online, longitudinal patient-reported outcomes and genetic data on Parkinson’s disease. Sci Data 7: , 67. |
[3] | Maffoni M , Giardini A , Pierobon A , Ferrazzoli D , Frazzitta G ((2017) ) Stigma experienced by Parkinson’s disease patients: A descriptive review of qualitative studies. Parkinsons Dis 2017: , 7203259. |
[4] | Fleming V , Tolson D , Schartau E ((2004) ) Changing perceptions of womanhood: Living with Parkinson’s disease. Int J Nurs Stud 41: , 515–524. |
[5] | Salazar RD , Weizenbaum E , Ellis TD , Earhart GM , Ford MP , Dibble LE , Cronin-Golomb A ((2019) ) Predictors of self-perceived stigma in Parkinson’s disease. Parkinsonism Relat Disord 60: , 76–80. |
[6] | Perrin AJ , Nosova E , Co K , Book A , Iu O , Silva V , Thompson C , McKeown MJ , Stoessl AJ , Farrer MJ , Appel-Cresswell S ((2017) ) Gender differences in Parkinson’s disease depression. Parkinsonism Relat Disord 36: , 93–97. |
[7] | Hristova DR , Hristov JI , Mateva NG , Papathanasiou JV ((2009) ) Quality of life in patients with Parkinson’s disease. Folia Med 51: , 58. |




