The Cause and Duration of Emergency Admissions to Hospital in People with Idiopathic Parkinson’s Disease, Under the Care of a UK Service, During the First Year of the COVID-19 Pandemic
Abstract
Background:
People with Parkinson’s disease (PD) have higher rates of hospitalisation and healthcare utilisation compared to the general population. The COVID-19 pandemic caused significant changes in admissions to hospital and access to healthcare. People with PD are some of the most vulnerable to such changes. There is no pre-existing data on the cause and duration of admission to hospital of people with PD during the COVID-19 pandemic.
Objective:
To determine the cause, duration, and outcome of hospital admissions to Northumbria Healthcare NHS Foundation Trust (NHCFT) for people with idiopathic Parkinson’s disease (IPD) in 2020.
Methods:
All people with IPD who had an emergency admission to NHCFT between 01/01/2020 and 31/12/2020 were identified. Demographic and disease characteristics, the number, duration, cause of admission and the location prior to admission were collected from an audit of medical notes.
Results:
271 people with IPD had one or more emergency admissions to NHCFT between 01/01/2020 and 31/12/2020. There was a total of 453 emergency admissions, with a median duration of 5 (IQR 2-13) days. The most common causes of admission to hospital were PD-related motor dysfunction (includes falls with no other underlying cause or associated injury) and injury (includes falls with fracture), at 78 (17.2%) and 70 (15.5%) respectively.
Conclusions:
People with IPD had a short duration but high number of emergency admissions to hospital. Our chronological data on number of admissions shows a peak in admissions during August 2020. As a result of these findings and emerging data we suggest that individuals with PD deconditioned during 2020.
INTRODUCTION
There are an estimated 145,519 individuals living with Parkinson’s disease (PD) in the United Kingdom (UK) [1]. People with PD have significantly higher rates of hospital admissions and healthcare utilisation compared to the general population [2–4]. It is established that the most common causes of admission in people with PD are infections (urinary tract infection and pneumonia), gastrointestinal disorders, falls and fractures, and PD-related motor and psychiatric conditions [5]. Understanding the cause of admissions in people with PD can aid healthcare services to identify those most at risk of admission and develop policies to aid in the prevention of admission.
On 11 March 2020, the World Health Organization (WHO) declared that the severe acute respiratory syndrome coronavirus two (SARS-CoV-2 or COVID-19) was a pandemic [6]. In response, the UK government enforced two national lockdowns, on 23 March 2020 and 5 November 2020, and encouraged only essential use of the National Health Service (NHS) [7–9]. Whilst national restrictions and guidance prevented the spread of COVID-19, they created barriers to individuals with pre-existing health conditions accessing healthcare and created fear that using healthcare facilities would result in COVID-19 infections [10–12].
A systematic review of the COVID-19 pandemic and impact of government restrictions found that hospital admissions reduced by 28% globally [10, 13]. In the UK admissions decreased by 25.5% from 2019-2020 to 2020-2021 [14]. Data from Germany shows that, during the peak of COVID-19, admissions for any cause decreased by 36.6%, but in people with PD admissions decreased by 66.6% [15]. However, there are no data looking at the cause and duration of admissions in people with PD during the COVID-19 pandemic.
It is important to determine the impact of the COVID-19 pandemic and government policies on the duration and causes of admission to hospital for people with PD. By understanding the changes in health utilisation, health services can prepare for future threats to people with PD accessing healthcare services and reduce the sequelae of such events.
MATERIALS AND METHODS
Ethics and consent
This study was registered with the audit department at Northumbria Healthcare NHS Foundation Trust (NHCFT) As an audit ethical approval was not required. Informed consent was not required for this study as it involved a review of existing clinical data.
Setting, participants, and inclusion/exclusion criteria
The NHCFT has a catchment of around 500,000 individuals. The NHCFT PD service covers two local government areas in the North East of England: North Tyneside and Northumberland. There is a mixed population demographic; urban areas have a higher index of multiple deprivation and the rural population have a lower index of multiple deprivation. All individuals are initially admitted to Northumbria Specialist Emergency Care Hospital (NSECH), which serves as the acute medical hospital for NHCFT.
The NHCFT PD service is run by geriatricians with an interest in PD in conjunction with PD nurse specialists and other multidisciplinary team members. Throughout 2020 the PD nurse specialists remained in their posts and provided their usual standard of care for individuals with PD, allowing for the circumstances, with more remote working taking place.
All patients with a diagnosis of idiopathic PD (IPD) (including PD dementia (PDD)), Lewy body dementia (LBD), vascular parkinsonism or atypical parkinsonian disorder, who had an emergency or elective admission to NHCFT, between 01/01/2020 and 31/12/2020 had their admissions retrospectively recorded. Outpatient attendances and accident and emergency attendances without admission were not included.
Only patients with a diagnosis of IPD (including PDD) were included in the final analyses. Individuals with atypical parkinsonian disorder, vascular parkinsonism, and LBD were excluded as their presentation, progression, symptomology, and resultant management differs from those with IPD. Atypical parkinsonian disorder conditions included cortico-basal degeneration, multiple systems atrophy, or progressive supranuclear palsy. In the final data analyses, only emergency admissions were included.
Data collection
Patients were identified from the PD service central database for NHCFT.
Medical notes were obtained for those identified with an admission. Data on diagnosis of PD, gender, age, and disease stage as Hoehn and Yahr score were recorded [16]. When the diagnosis was not immediately clear from the records, RW reviewed the diagnosis based on medical notes. Hoehn and Yahr scores were recorded directly from previous documentation in clinical records or were determined by PE on analysis of functional status in patient records.
Number of admissions and whether they were emergency or elective was recorded. Each emergency admission to hospital was reviewed and the duration, primary cause, outcome, and location before admission were recorded. Cause of admission was coded using identical methodology to a previous study conducted in the same setting. In order to record the severity of a fall; in those with motor dysfunction (fall) and an injury, “injury” was reported as the primary cause of admission, and in those with motor dysfunction (fall) and no injury, “PD-related motor” was reported as the primary cause of admission [17]. Individuals with a high clinical suspicion of COVID-19 (lymphopenia, new cough, shortness of breath, desaturation) but without a positive COVID-19 test were included as COVID-19 [18]. Primary cause of admission was recorded from the discharge summary. If the primary cause was not clear the admission document was reviewed. Cause of death was recorded from the death certificate summary. Location prior to admission was recorded from the admission document.
Data analysis and statistical methods
Standard descriptive statistics (e.g., median, mean, frequency, inter-quartile range (IQR)) were used to summarise the data.
Data from NHS digital, Hospital Admitted Patient Care Activity was used for the number of finished admission episodes (all cause) in England, in 2020 [14]. A finished admissions episode: each episode relates to a period of care for a patient under a single consultant at a single hospital. UK Government data was used for the number of positive COVID-19 cases (people who have had at least one positive COVID-19 test result), in the UK during 2020 [19].
RESULTS
Population characteristics
For 2020, 289 individuals with a diagnosis of IPD were admitted to NHCFT, of whom 271 had an emergency admission. 95 individuals had two or more admissions and 42 had three or more admissions. One individual had 10 admissions in 2020.
Demographic details and disease severity are displayed in Table 1. The individuals were predominantly male (65.7%), Hoehn and Yahr score III (40.2%) and had a median age of 80.
Table 1
Demographics and disease stage in those with IPD who had an emergency admission to NHCFT
| Demographic | 2020, n = 271 |
| Gender | |
| Male | 178 (65.7%) |
| Female | 93 (34.3%) |
| Median age, y (IQR) | 80.0 (74.5–84.0) |
| 41–50 | 1 (0.4%) |
| 51–60 | 7 (2.6%) |
| 61–70 | 27 (10.0%) |
| 71–80 | 111 (40.9%) |
| 81–90 | 110 (40.6%) |
| >90 | 15 (5.5%) |
| Dementia | |
| Diagnosis recorded | 47 (17.3%) |
| Diagnosis not recorded | 224 (82.7%) |
| Hoehn and Yahr Score | |
| I | 7 (2.6%) |
| II | 61 (22.5%) |
| III | 109 (40.2%) |
| IV | 44 (16.2%) |
| V | 50 (18.5%) |
IQR, interquartile range.
Location prior to admission
Nearly three quarters of admissions were from individuals own home, 322 (71.1%). Admissions from a care home were the second highest location, 94 (20.8%).
Length of stay
The median duration of admission to NHCFT was 5 days (IQR 2-13).
Cause of death
Thirty-three individuals died whilst admitted to NHCFT in 2020, of whom 13 (39.4%) died of pneumonia and 7 (21.2%) died of COVID-19 (Table 2).
Table 2
Underlying primary cause of emergency admission and death and location prior to admission in individuals with IPD
| Admissions in 2020 (n = 453) | |
| Median duration of admission, days (IQR) | 5 (2–13) |
| Primary cause of admission | |
| Pneumonia* | 57 (12.6%) |
| CAP | 43 |
| Aspiration pneumonia | 14 |
| COVID-19 | 19 (4.2%) |
| Injury | 70 (15.5%) |
| UTI | 37 (8.2%) |
| Other Infection | 14 (3.1%) |
| PD related motor | 78 (17.2%) |
| PD related psychiatric | 16 (3.5%) |
| PD drug compliance | 11 (2.4%) |
| Orthostatic hypotension | 10 (2.2%) |
| Other cardiac cause | 28 (6.2%) |
| Gastrointestinal | 47 (10.4%) |
| Stroke | 6 (1.3%) |
| Other | 60 (13.3%) |
| Location prior to admission | |
| Care home | 94 (20.8%) |
| Own Home | 322 (71.1%) |
| Respite care | 3 (0.7%) |
| Sheltered accommodation | 31 (6.8%) |
| Tertiary Hospital | 3 (0.7%) |
| Cause of death | n = 33 |
| Pneumonia* | 13 (39.4%) |
| COVID-19 | 7 (21.2%) |
| Parkinson’s disease | 3 (9.1%) |
| Sepsis | 2 (6.1%) |
| Other | 8 (24.2%) |
*Pneumonia includes community acquired pneumonia and aspiration pneumonia. CAP, community acquired pneumonia; IQR, interquartile range; PD, Parkinson’s disease. Injury includes fall with fracture. PD-related motor (includes falls with no other underlying cause or associated injury). PD-related psychiatric (includes hallucination and delirium with no other underlying cause). PD drug compliance (includes medication non-compliance and overdose).
Chronology of admissions
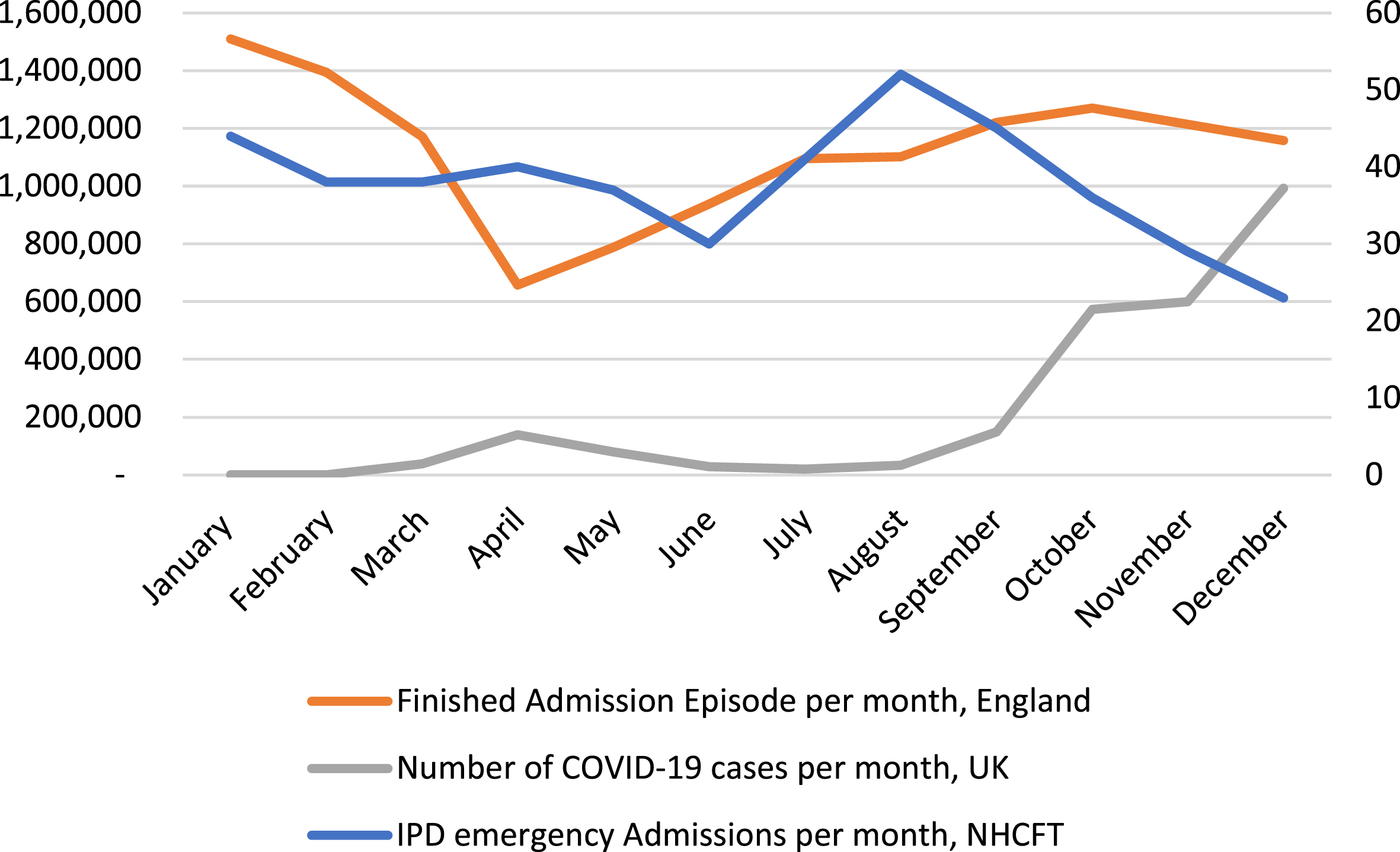
Figure 1 displays the number of emergency admissions in people with IPD to NHCFT compared to the number of COVID-19 cases in the UK and finished admission episodes in England during 2020. The number of emergency admissions in people with IPD to NHCFT decreased in the first six months of 2020. Between June and August 2020 there was a rapid increase in the number of emergency admissions. From August 2020 to 2021 emergency admissions decrease.
Fig. 1
The number of emergency admissions in people with IPD to NHCFT, compared to the number of COVID-19 cases (people who have had at least one positive COVID-19 test result), in the UK by specimen date and the number of finished admission episode (all cause) in England, in 2020.
Cause of admission
In 2020, A total of 453 emergency admissions occurred in those with IPD. The most common causes of admission to hospital were PD-related motor (includes falls with no other underlying cause or associated injury) and injury (includes falls with fracture), at 78 (17.2%) and 70 (15.5%) respectively. Table 2 displays the duration and cause of, and location prior to admission.
Nineteen (4.2%) individuals were admitted due to COVID-19 infection. Three of the 19 individuals were treated for a high clinical suspicion of COVID-19 infection despite a negative COVID PCR test result. An additional two patients had a diagnosis of COVID-19 infection recorded in their records, but this was not the primary cause of admission.
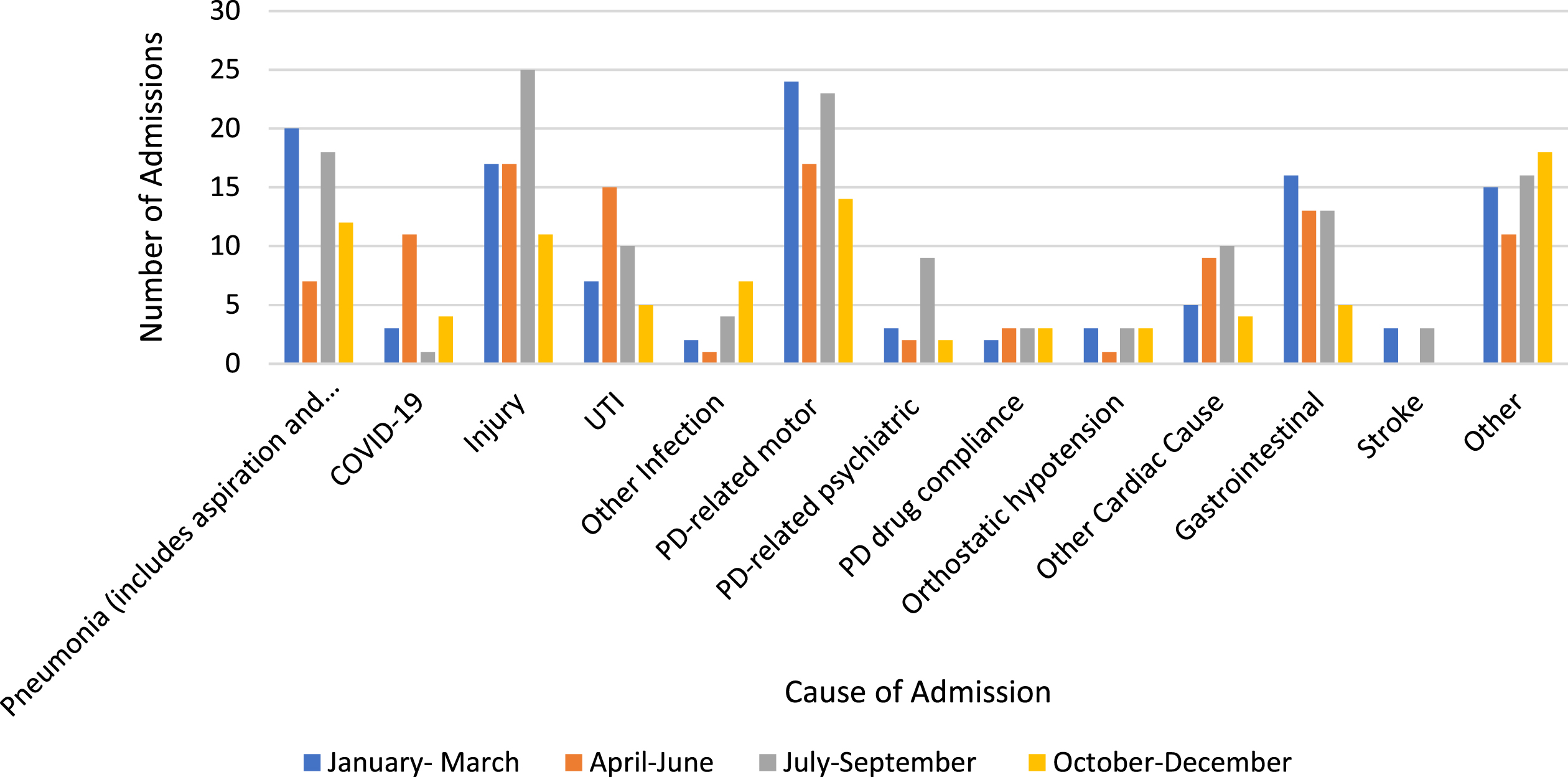
Figure 2 displays that cause of admissions per quarter, in 2020. There is a peak in admissions due to injury in the third quarter (July-September 2020).
Fig. 2
The number of emergency admissions in people with IPD to NHCFT by cause of admission, per quarter in 2020.
DISCUSSION
To our knowledge this is the first paper to show the number, duration, and cause of admissions as well as location prior to admission of individuals with IPD for the whole of 2020 and thereby covering the start of the COVID-19 pandemic. There were approximately 1,000 people with IPD under the NHCFT PD service at the start of 2020 of whom 271 had one or more admissions to hospital.
The median duration of admission to hospital (five days) was shorter than that of a study of 324,055 admissions for people with PD in England between 2009 and 2013, which found the mean length of stay to be 16 days [20]. Additionally, data from NHCFT in 2017 show that the median length of stay of individuals with IPD was 7 days (IQR 2-19). From the start of the pandemic until 15 April 2020 the UK government encouraged rapid discharge of people admitted from care homes back to care homes. Rapid discharges included individuals recovering from COVID-19 infection and did not require a confirmed negative COVID-19 test [21]. Further investigation is required to determine the rate of readmission and the interval of time between discharge and readmission during the COVID-19 pandemic. The encouragement of rapid discharges may have contributed to shortened admission duration and premature discharges, with a possible increase in readmissions. By understanding this, government policy can be adapted to protect those who are most vulnerable and optimise the use of health services.
Figure 1 compares COVID-19 infections in the UK with IPD emergency admissions to NHCFT during 2020. Emergency admissions for individuals with IPD are initially high, which is consistent with increased admissions during winter months. For the first six months of 2020, IPD emergency admissions decrease as COVID-19 cases increase within the UK. The first national lockdown was introduced on 23 March 2020 [9]. IPD emergency admissions peak in August 2020, which we hypothesise could be due to two factors; change in government policy and the deconditioning of individuals with IPD during lockdown. From 4 July 2020, the UK government encouraged the public to utilise essential and non-essential services which could have prompted individuals previously afraid of utilising health services to attend hospital [22]. Almost half of individuals with PD self-reported less physical activity during the COVID-19 pandemic, which correlated with worsening physical symptoms [23]. Further contributing factors to deconditioning of people with PD are the “hidden sorrow” of COVID-19; social isolation, and psychosocial stress which worsen symptoms [24–26]. As the second wave of COVID-19 increases into the autumn of 2020 and the second national lockdown was introduced IPD emergency admissions decrease [7]. Further research is required to confirm that there is a causative relationship between change in government policy and deconditioning of individuals during 2020.
The greatest primary causes of admission in our study were PD-related motor causes and injuries. This is similar to results from a systematic review and meta-analysis, which found that the main cause of admission for people with PD, prior to COVID-19, was infections (urinary tract infection and pneumonia) and worsening motor manifestations of PD, and falls or fractures [5]. However, compared to a previous publication of data from NHCFT that examined cause of admissions for individuals with IPD, who were Hoehn and Yahr III to V, we found a greater number of admissions due to injury (including falls with fractures) [17]. National admissions decreased by 25.5% during the COVID-19 pandemic, it may be that other causes of admission did not present to hospital and these results reflect the high proportion of admissions due to injury or PD-related motor [14]. However, Fig. 2 displays that cause of admissions in 2020, per quarter. There is a peak in admissions due to injury in the third quarter of 2020 (July –September) and a high number of admissions due to PD-related motor causes. These correlate to the easing of UK government easing of COVID-19 pandemic lockdowns. The high number of admissions due to injuries and the change in causes in admissions during 2020 supports the suggestion that individuals with IPD deconditioned during lockdown. It is important to understand if those with PD are more likely to have an injury after COVID-19 pandemic lockdowns as this can aid in the development of effective interventions to prevent the deterioration of those with PD in the community, to maintain motor function and to reduce emergency admissions to hospital. There is an association between frequent neurologist consultations, availability of open access clinics and medication compliance and a reduced number of emergency admissions [27]. The integration of these services as an online or community-based service may be effective in future pandemics or when there is limited access to health care services.
Admissions from own home made up 71.1%, and admissions from care homes 20.8% of admissions. Between 20 January 2020 and 28 June 2020 the rate of emergency admissions to hospital for residential and nursing home residents in England decreased by 36% and 38% respectively [28]. This has been attributed to government policy; primary care and community health services were asked to support care homes with the aim to reduce admissions to hospital [29]. It is known that individuals with IPD are more likely to be admitted to hospital [2–4]. To determine the impact of this government policy the location prior to admissions should be compared to previous data. Deaths for individuals with IPD in care homes should be compared for 2020 to previous data to see if there was an excess of deaths in care homes potentially due to reduced admissions to hospital.
Seven and a half percent all admissions resulted in death, which is similar to previous data, which reports the mortality rate for emergency inpatient admission for people with PD in the UK to be 7.0% in males and 5.8% in females [20]. Individuals with IPD, and in particular those with dementia, have a higher risk of mortality than the general population [30].
Limitations
The study has some limitations. Descriptive statistics were used to summarise the data. Data only included inpatient outcomes. Comparison of inpatient and community outcomes would enable further conclusions to be drawn from the data. There is no previous data set to compare to. Previous results from the same area would have enabled us to determine if there were significant changes to outcomes within the same population. Deaths were only recorded for inpatient admissions. Inpatient and outpatient deaths would have enabled us to determine the total mortality rate in 2020 within the PD NHCFT population. The data is UK specific and reflects changes because of UK government policy. However, the response and outcomes are applicable to any healthcare setting impacted by COVID-19.
Conclusion
We found that people with IPD had a shorter duration of admission to hospital and a higher number of admissions due to PD motor symptoms and injuries during 2020 than reported previously. Our chronological data on number of admissions shows a peak in admissions during August 2020. As a result of these findings and emerging data we suggest that individuals with PD deconditioned during 2020. Further research is required into deconditioning of patients, location prior to admission and deaths within the community. This will enable effective, community-based interventions and informed government policies to be developed which support those with PD in future pandemics and with reduced access to healthcare.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial or not-for profit sectors.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
[1] | Parkinson’s UK. The Incidence and Prevalence of Parkinson’s in the UK. London, UK. (2018) . |
[2] | Gandhi AB , Onukwugha E , Albarmawi H , Johnson A , Myers DE , Gray D , Alvir J , Hynicka L , Shulman LM ((2021) ) Healthcare resource utilization associated with Parkinson disease among Medicare beneficiaries. Neurology 97: , e597–e607. |
[3] | Hobson DE , Lix LM , Azimaee M , Leslie WD , Burchill C , Hobson S ((2012) ) Healthcare utilization in patients with Parkinson’s disease: A population-based analysis. Parkinsonism Relat Disord 18: , 930–935. |
[4] | Weir S , Samnaliev M , Kuo TC , Tierney TS , Walleser Autiero S , Taylor RS , Schrag A ((2018) ) Short-and long-term cost and utilization of health care resources in Parkinson’s disease in the UK. Mov Disord 33: , 974–981. |
[5] | Okunoye O , Kojima G , Marston L , Walters K , Schrag A ((2020) ) Factors associated with hospitalisation among people with Parkinson’s disease–A systematic review and meta-analysis. Parkinsonism Relat Disord 71: , 66–72. |
[6] | World Health Organisation.WHODirector-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. (2020) ; https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. Accessed 15/11/2021. |
[7] | UK Government. PM Commons statement on coronavirus: 2 November. In. Vol 2020. www.gov.uk (2021) . |
[8] | UK Government. Prime Minister’s statement on coronavirus (COVID-19): 16 March 2020. In. Vol 2020. www.gov.uk (2020) . |
[9] | UK Government. Prime Minister’s statement on coronavirus (COVID-19): 23 March 2020. In. Vol 2020. www.gov.uk (2020) . |
[10] | Roy CM , Bollman EB , Carson LM , Northrop AJ , Jackson EF , Moresky RT ((2021) ) Assessing the indirect effects of COVID-19 on healthcare delivery, utilization and health outcomes: A scoping review. Eur J Public Health 31: , 634–640. |
[11] | Hsiang S , Allen D , Annan-Phan S , Bell K , Bolliger I , Chong T , Druckenmiller H , Huang LY , Hultgren A , Krasovich E ((2020) ) The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 584: , 262–267. |
[12] | Flaxman S , Mishra S , Gandy A , Unwin HJT , Mellan TA , Coupland H , Whittaker C , Zhu H , Berah T , Eaton JW ((2020) ) Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 584: , 257–261. |
[13] | Moynihan R , Sanders S , Michaleff ZA , Scott AM , Clark J , To EJ , Jones M , Kitchener E , Fox M , Johansson M ((2021) ) Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 11: , e045343. |
[14] | NHS Digital. Hospital Admitted Patient Care Activity 2020-21. Hospital Admitted Patient Care Activity (2021) ; https://digital.nhs.uk/data-and-information/publications/statistical/hospital-admitted-patient-care-activity/2020-21. Accessed 15/11/2021. |
[15] | Scherbaum R , Kwon E-H , Richter D , Bartig D , Gold R , Krogias C , Tönges L ((2021) ) Hospital admissions for neurodegenerative diseases during the first wave of the COVID-19 pandemic: A nationwide cross-sectional study from Germany. Brain Sci 11: , 1219. |
[16] | Hoehn MM , Yahr MD ((1998) ) Parkinsonism: Onset, progression, and mortality. Neurology 50: , 318–318. |
[17] | Klaptocz J , Gray WK , Marwood S , Agarwal M , Ziegler J , Webb Z , Prabhakar M , Hand A , Oates L , McDonald C ((2019) ) The pattern of hospital admissions prior to care home placement in people with Parkinson’s disease: Evidence of a period of crisis for patients and carers. J Aging Health 31: , 1616–1630. |
[18] | Fu L , Wang B , Yuan T , Chen X , Ao Y , Fitzpatrick T , Li P , Zhou Y , Lin Y-f , Duan Q ((2020) ) Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J Infection 80: , 656–665. |
[19] | UK Government. Cases in England, People Tested Positive. Coronavirus (COVID-19) in the UK (2021) ; https://coronavirus.data.gov.uk/details/cases. Accessed 30/11/2021. |
[20] | Low V , Ben-Shlomo Y , Coward E , Fletcher S , Walker R , Clarke CE ((2015) ) Measuring the burden and mortality of hospitalisation in Parkinson’s disease: A cross-sectional analysis of the English Hospital Episodes Statistics database 2009–2013. Parkinsonism Relat Disord 21: , 449–454. |
[21] | Daly M ((2020) ) COVID-19 and care homes in England: What happened and why? Soc Policy Adm 54: , 985–998. |
[22] | UKGovernment. Prime Minister’s statement on coronavirus (COVID-19): 23 June (2020) . https://www.gov.uk. Accessed 16/11/2021. |
[23] | van der Heide A , Meinders MJ , Bloem BR , Helmich RC ((2020) ) The impact of the COVID-19 pandemic on psychological distress, physical activity, and symptom severity in Parkinson’s disease. J Parkinsons Dis 10: , 1355–1364. |
[24] | Helmich RC , Bloem BR ((2020) ) The impact of the COVID-19 pandemic on Parkinson’s disease: Hidden sorrows and emerging opportunities. J Parkinsons Dis 10: , 351. |
[25] | Sulzer D , Antonini A , Leta V , Nordvig A , Smeyne RJ , Goldman JE , Al-Dalahmah O , Zecca L , Sette A , Bubacco L ((2020) ) COVID-19 and possible links with Parkinson’s disease and parkinsonism: From bench to bedside. NPJ Parkinsons Dis 6: , 18. |
[26] | Hemmerle AM , Herman JP , Seroogy KB ((2012) ) Stress, depression and Parkinson’s disease. Exp Neurol 233: , 79–86. |
[27] | Muzerengi S , Herd C , Rick C , Clarke CE ((2016) ) A systematic review of interventions to reduce hospitalisation in Parkinson’s disease. Parkinsonism Relat Disord 24: , 3–7. |
[28] | Grimm F , Hodgson K , Brine R , Deeny SR ((2020) ) Hospital admissions from care homes in England during the COVID-19 pandemic: A retrospective, cross-sectional analysis using linked administrative data. Int J Popul Data Sci 5: , 1663. |
[29] | NHS Improvement and NHS England. COVID-19 response: Primary care and community health support care home residents. (2020) ; https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/COVID-19-response-primary-care-and-community-health-support-care-home-residents.pdf. Accessed 16/11/2021. |
[30] | Xu J , Gong D , Man C , Fan Y ((2014) ) Parkinson’s disease and risk of mortality: Meta-analysis and systematic review. Acta Neurol Scand 129: , 71–79. |




