Driving and Parkinson’s Disease: A Survey of the Patient’s Perspective
Abstract
Background:
Parkinson’s disease (PD) is a multi-system disorder that can impact on driving ability. Little is known about how these changes in driving ability affect people with PD, making it difficult for clinicians and carers to offer appropriate support.
Objective:
To assess patient views concerning the effect of PD on their driving ability, the impact of these changes and how they manage them.
Method:
An online survey was created by a team of clinicians, people with PD, their carers, and representatives from Parkinson’s UK. People with PD throughout the United Kingdom were invited to participate through Parkinson’s UK’s website, newsletter and Parkinson’s Excellence Network email list.
Results:
805 people with PD took part in the survey. We found that the loss of a driving licence had an adverse impact on employment, socialisation, travel costs and spontaneous lifestyle choices. Multiple changes in driving ability related to PD were described, including that impulse control disorders can have an adverse impact on driving. Changes in driving ability caused people to change their driving practices including taking shorter journeys and being less likely to drive at night. Participants advised managing changes in driving ability through planning, vehicle adaptions, maintaining skills and self-assessment.
Conclusion:
This study demonstrates the impact that changes in driving ability can have on the lifestyle of people with PD and reveals the strategies that individuals adopt to manage these changes.
INTRODUCTION
Parkinson’s disease (PD) causes progressive decline in motor function resulting in bradykinesia, rigidity, tremor, and postural instability. It can also be associated with a decline in cognitive function [1], visuo-spatial deficits [2], sleepiness [3], variable effectiveness of medications [3], and changes in decision making [4]. This myriad of symptoms is likely to impact on the ability to perform a complex motor and visual-spatial task like driving. Indeed, on-road and driving simulator studies have shown that, compared to controls, people with PD make more errors during maneuvers and at traffic lights [5], have delayed decision making, use mirrors less effectively [6], have poorer reaction times and vehicle control [7, 8] and an overall deterioration of driving ability when presented with dual stimuli [9, 10]. As a result, people with PD may alter the way they drive. This includes reducing the distance and duration of journeys [3] and being less likely to drive at night or alone [5]. People with PD stop driving earlier compared to a control group adjusted for age, gender, education, and miles driven per week [11]. As a consequence, their fitness to drive needs to be regularly reviewed [12].
Physicians and people with PD have both been found to be poor at predicting driving ability [13–15]. Perhaps with this in mind, a considerable focus of research has been to identify the best methods for physicians and allied professionals to assess a person with PD’s fitness to drive [16–18]. No method of off-road testing has been found to be reliable in predicting driving ability in people with PD and the gold standard remains on-road assessment [16–18]. The majority of those with PD referred for driving assessment (perhaps, because of a concern regarding driving ability) have their license removed, with cognitive impairment being the best predictor of an adverse outcome [19].
The loss of the ability to drive or being prevented from driving by a licensing authority can lead to depression [20], decreased activity outside of the home [21], social isolation [22], and more reliance on care givers [23]. The overall impact of not being able to drive on quality of life is likely to be significant. Understanding this impact is vital for developing appropriate guidelines for clinicians and providing suitable support for people with PD, yet there is relatively little literature available regarding the perspective of people with PD. We looked to address this gap by asking people with PD about how their driving has changed since diagnosis and what impact this has had on their lives.
MATERIALS AND METHODS
We created a survey for people with PD hosted online at SurveyMonkey® [24]. Questions were written after consultation with clinicians involved in the care of people with PD, people with PD and their carers and a representative from Parkinson’s UK. The survey was piloted with the same group and changes made based on their suggestions. It was available for completion from 21 January 2017 until 18 June 2017. People with PD were invited to participate through Parkinson’s UK’s website, newsletter, and Parkinson’s Excellence Network email list. We estimate that 3000 people with Parkinson’s would have had the opportunity to complete the survey.
The first section of the survey outlined the purpose of the survey and that results may be published. Participants were then given the option of proactively opting in in order to participate.
The survey structure is shown in Supplementary Material 1, with the full list of survey questions shown in Supplementary Material 2. Respondents who had never held a driving license exited the survey after answering basic demographic questions only. Respondents who had not driven within the last three years only answered questions about the circumstances of losing their license and the impact it had. Access to several questions in the survey was dependent on the prior answers given by the participants.
Free text responses to the survey were reviewed by two researchers (LO, PB). Thematic analysis of the data was performed [25]. Firstly, the researchers worked independently, reviewing the responses and identifying themes emerging through an inductive, iterative process [25]. The two researchers then met to compare notes. Themes were discussed, challenged, and refined. Repeated reading and discussion of transcripts continued until consensus was reached. This triangulation between researchers enhanced the credibility of the conclusions drawn.
RESULTS
Demographics and effect of loss of driving license
Table 1 shows the demographics of the 805 people who completed the survey and their driving status. It also describes the impact on lifestyle that the loss of a driving license had on the survey respondents. We found that the loss of a driving license, be it voluntarily or following instruction from the UK licensing authority (DVLA) had an adverse impact on employment, socialization, travel costs and ability to make spontaneous lifestyle choices.
Table 1
Demographics and driving status of survey respondents and the impact of relinquishing driving license
| Mean age | 67 years (range 35–88) | |
| Gender | Males | 59%(n = 474) |
| Females | 41%(n = 331) | |
| Time since Parkinson’s diagnosed (n = 726, mean = 7 years, range 0–56 years) | 0–5 years | 48%(n = 349) |
| 6–10 years | 30%(n = 217) | |
| 11–15 years | 15%(n = 106) | |
| Greater than 15 years | 7%(n = 54) | |
| Driving license status (n = 747) | Current license holder | 84%(n = 629) |
| Former license holder | 14%(n = 105) | |
| Never had a license | 2%(n = 13) | |
| Additional vehicles to a car (n = 41) | Minibus | 7 |
| Lorry | 4 | |
| Van | 17 | |
| Moped (under 50 cc) | 3 | |
| Motorbike (over 50 cc) | 10 | |
| Driving essential for work (n = 675) | Yes | 12%(n = 82) |
| No | 25%(n = 172) | |
| Retired | 63%(n = 421) | |
| Home circumstances (n = 621) | Lives alone | 17%(n = 105) |
| Lives with someone who drives | 73%(n = 454) | |
| Lives with someone who does not drive | 10%(n = 62) | |
| Personal care (n = 528) | Independent | 88%(n = 465) |
| Requires help | 12%(n = 63) | |
| Home environment (n = 665) | Rural | 39%(n = 259) |
| Urban | 29%(n = 194) | |
| Suburbs | 32%(n = 212) | |
| Symptom profile (n = 630) | Significant memory problems | 10%(n = 59) |
| Episodes of confusion | 10%(n = 61) | |
| Difficulty in concentrating | 22%(n = 132) | |
| Excessive sleepiness | 22%(n = 137) | |
| Medication regime (respondents selected all that applied –n = 510) | Levodopa preparation | 85%(n = 431) |
| Dopamine agonist | 50%(n = 254) | |
| COMT inhibitor | 15%(n = 79) | |
| MOA-B inhibitor | 38%(n = 194) | |
| Anticholinergic | 2%(n = 10) | |
| Cholinesterase inhibitor | 1%(n = 7) | |
| Respondents who have relinquished license (n = 95) | Relinquished license voluntarily | 67%(n = 64) |
| License removed by driving authorities | 33%(n = 31) | |
| Disagreed with decision of driving authority | 61%(n = 19) | |
| Appealed decision of driving authority | 16%(n = 5) | |
| Since relinquishing license (n = 95) | Had to stop working | 7%(n = 7) |
| Less socially active | 84%(n = 80) | |
| Transportation costs increased | 39%(n = 37) | |
| Less spontaneous lifestyle choice | 82%(n = 78) |
Collisions while driving
15%(n = 104) of 672 survey respondents who had driven in the last 3 years stated they had been involved in a collision since being diagnosed with PD, of whom 15 respondents had two collisions and 2 respondents had 3 collisions.
Changes in driving function and style
Respondents indicated that they experienced changes in driving function and style since being diagnosed with PD. Table 2 details the changes they have had in their functions related to driving since their diagnosis of PD and adaptations they have made to their vehicles.
Table 2
Changes in driving style since diagnosis of Parkinson’s disease
| Respondents who answered ‘Yes’ | |
| Since being diagnosed with Parkinson’s disease have you . . . | |
| Had changes in vision? (n = 644) | 22%(n = 141) |
| Had changes in head and neck movement? (n = 648) | 33%(n = 214) |
| Had difficulty judging speed and distances? (n = 635) | 19%(n = 122) |
| Had difficulty with maneuvers? (n = 637) | 41%(n = 264) |
| Become lost more frequently? (n = 625) | 8%(n = 47) |
| Had changes in your ability to drive safely? (n = 636) | 17%(n = 130) |
| Changed or adapted your car? (n = 657) | 26%(n = 169) |
| Adaptations made to vehicles (respondents could select all that applied) | |
| Automatic transmission | 149 |
| Hand Controls | 2 |
| Reversed foot pedals | 5 |
| Higher/larger car purchased | 14 |
| Smaller car purchased | 4 |
| Keyless entry/ignition | 1 |
| Parking sensor/cameras | 4 |
| Blind spot eliminator | 1 |
| Steering wheel adaption | 2 |
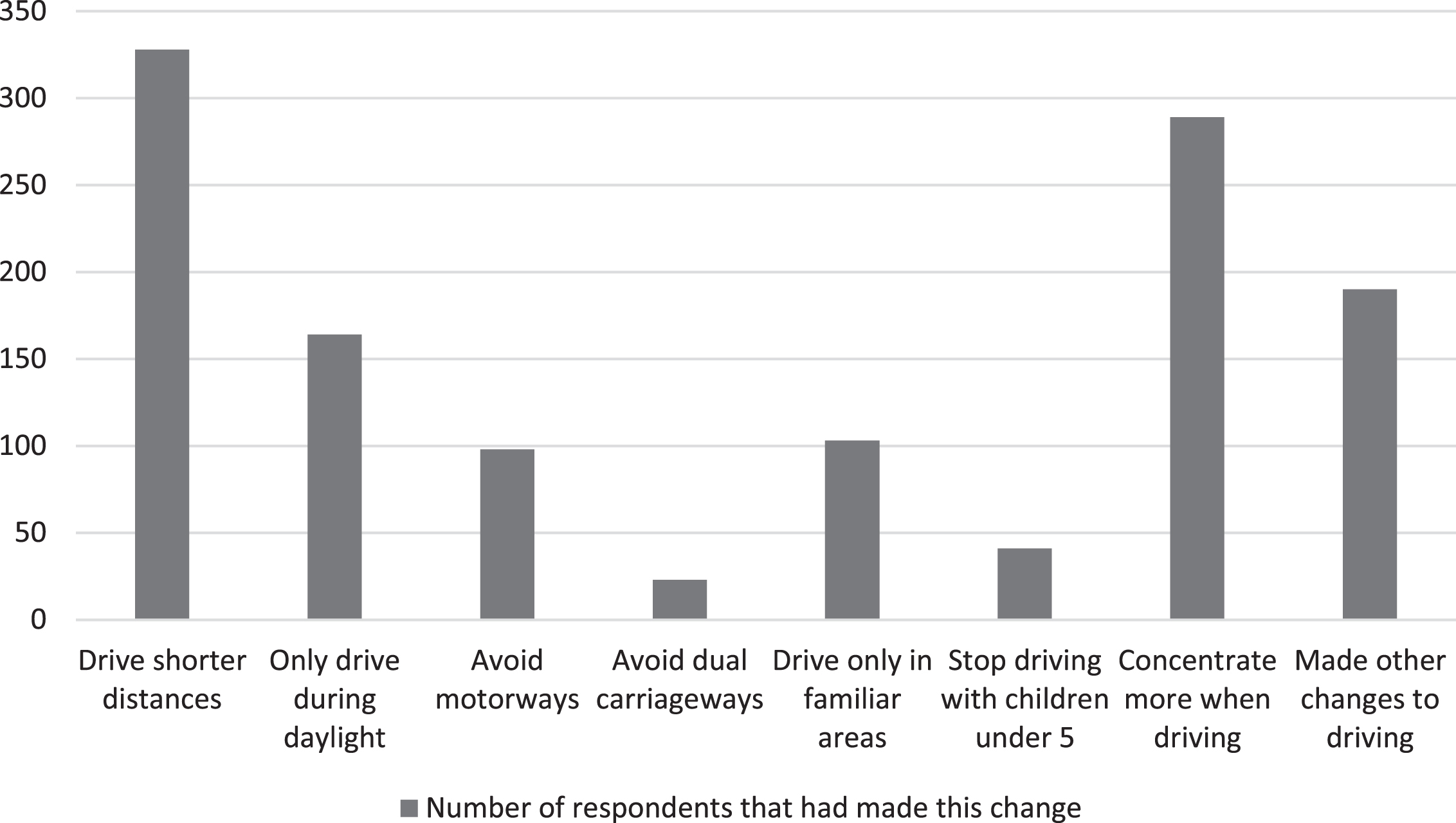
Respondents were also asked to select ways in which they have modified their driving style since being diagnosed with PD. They could select all the changes that they had made and the results are detailed in Fig. 1.
Fig. 1
Ways in which respondents have modified their driving style since diagnosis with Parkinson’s Disease.
Concerns related to driving
We asked if respondents had concerns about their own driving, 18%(n = 95/528) said they did. 12%(n = 65/542) of respondents had family or friends who had expressed concerns about their driving. In addition, 14%(n = 90/643) of respondents had felt sleepy while driving and 16%(n = 102/638) found spoken word programs distracting while driving.
Impulse control disorder and off time
Of the survey respondents 10%(n = 69/688) had been told they had impulse control disorder by a healthcare professional and 2%of survey respondents (n = 11/559) said that an impulse behavior had an adverse effect on their driving, including speeding, driving when sleepy, taking unsafe short cuts and road rage.
47%of survey respondents (n = 295/628) indicated that they suffered from wearing off of their medication. Of this group 41%(n = 125/305) said they needed to fit their driving around their ‘on’ time, with a small number of respondents (n = 8/277) saying that their ‘on’ time was not predictable enough to manage this safely.
Tips for driving from people with Parkinson’s disease
From analysis of the responses to a question asking respondents whether they had any tips for driving with PD four themes emerged.
1Planning
Respondents described the importance of planning journeys around the times of the day where traffic was minimal, avoiding night time journeys and ensuring the driver knows the route prior to setting off.
“Mentally rehearse the route that you are going to take beforehand....it saves any confusion as you are approaching a junction or roundabout about which direction to take” Respondent 588
They also stressed that journeys should be planned around when medications are providing benefit and that breaks in journeys should be made to avoid missing tablets.
“Work out your effective time to drive. Adjust the medication times to suit your lifestyle. If you get signs of wearing off stop in a convenient safe place, take your tablet and rest” Respondent 205
2Vehicle adaptations
Using automatic transmission, satellite navigation and higher cars for ease of access were all advised by our survey respondents.
“I would definitely encourage PD people to change to an automatic car. It is less tiring and so releases more energy to concentrate on other aspects of driving” Respondent 601
3Maintaining skills
Respondents gave advice to maintain driving skills by seeking driving tuition and assessment from Driving Mobility centres. They also advised maintaining physical and mental health, particularly by using puzzles or crosswords.
“Exercise helps to keep the neck mobile –essential for driving safely” Respondent 190
“Keep your brain active, maths, reading, crosswords, don’t watch TV.....study the route and if required plan it” Respondent 291
4Self-assessment
Respondents emphasized the need to assess your own ability to drive. This included prior to driving when making decisions about journey length and safety, but also while driving, noting when fatigue began and when medications were wearing off.
“Listen to your body! Don’t drive if you are tired. Take frequent breaks on a long trip” Respondent 336
DISCUSSION
Our survey captured the opinions of a large and varied sample of people with PD. One of the novel features of our study was asking people with PD about the impact of relinquishing their driving license.
Adverse effects on employment, socialization, transport costs and the ability to make spontaneous lifestyle choices were all identified. This is in keeping with the social isolation and decreased activity outside the home seen in people without Parkinson’s who lose their ability to drive [21, 22]. It is notable that these problems arise despite the high proportion of people living with someone who can drive and the spread of rural, urban, and suburban environments. Furthermore, these issues occur in a developed nation with access to subsidized public transport, social services, and charity support.
Our results show that people with PD make a variety of changes to their driving style in order to accommodate the changes in function caused by their condition. The frequency of people having to take shorter journeys and avoiding driving at night suggests this too could have an impact on socialization and lifestyle choices. To minimize these detrimental effects those involved in the care of people with PD need to optimize the ability of people with PD to drive safely and review whether their access to alternative forms of transport is sufficient.
The survey results highlight the impact of both motor and non-motor symptoms of PD on driving. In particular, it draws attention to the effect impulsivity can have on driving and suggests that people with PD should be counselled about this risk. Both the impact of wearing off and fatigue were emphasized by our survey respondents in their free text responses. Previous studies [3, 26–28] exploring sleep issues in people with PD also investigated respondent’s propensity to fall asleep whilst driving. These studies also employed survey methods with 2 studies recruiting participants via a single center [26, 27], 1 study via multiple sites [28] and 1 study via their national PD Association [3].
Fatigue leading to dozing while driving was found to occur in PD [26, 28] and increased daytime sleepiness is a risk factor for sudden onset sleepiness while driving [3, 27]. The insight provided by this survey into how these problems are managed by people with PD could be used as a basis for advice provided by healthcare professionals. In particular, we call attention to the four themes of planning, vehicle adaptations, maintaining skills and self-assessment as a basis for realistic and practical guidance that can be given to people with PD.
We acknowledge the limitations of collecting data through an online survey. This method was chosen in order to gather data from a large number of people with PD. Completing the survey required internet access and the cognitive capacity to complete the task which could have limited its accessibility. The demographics detailed in Table 1 suggest the sample is representative of the PD population in the United Kingdom who do not have cognitive impairment. We acknowledge that the low number of people on cholinesterase inhibitors, and that we did not collect diagnostic data regarding cognition, means that we cannot be confident our data is representative of people with cognitive impairment. Not all participants completed the survey in full, which is demonstrated in the variable total respondents to each question in our results. We have no mechanism for verifying the accuracy of the responses given. The survey questions had not been validated against the medical records or objective driving assessment of those people with PD involved in the survey development. Studies in small groups of people with PD have shown a poor correlation between their self-estimates of their driving behavior and their actual driving behavior [16]. Former drivers generally underestimate the costs of running a car and this needs to be considered in relation to their response about transport costs. Recruitment of a control group was not undertaken as the surveyed population was too large for a reliable control group to be recruited. We did not use a validated tool for assessment of PD severity through an online survey so we are unable to draw correlation between the severity of a respondents PD and their driving outcomes with the data gathered.
Future research should look to provide insight into the impact that driving authorities, clinicians and the voluntary sector have on how people with PD change their driving practices. In addition, the impact that changes in driving ability can have on carers for people with PD is worthy of further study. Greater knowledge of these areas would allow healthcare professionals and driving authorities to better tailor the advice they provide about driving to people with PD and their carers.
ACKNOWLEDGMENTS
A grant was received for this project from Parkinson’s UK. Parkinson’s UK had no role in the design of the research or preparation of this article. Parkinson’s UK did promote the survey used in this research via their website and email.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
ETHICAL APPROVAL AND CONSENT
Northumbria Healthcare NHS Foundation Trust Ethics Review Board advised that formal ethical approval was not required for this study.
Participants were consented to take part in the study through a written statement at the beginning of the survey which explained the purpose of the survey and how the results would be used. They were required to select that they consented to the description in the written statement in order to begin the survey.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD-212686.
REFERENCES
[1] | Dubois B , Pillon B ((1997) ) Cognitive deficits in Parkinson’s disease. J Neurol 244: , 2–8. |
[2] | Uc EY , Rizzo M , Anderson SW , Qian S , Rodnitzky RL , Dawson JD ((2005) ) Visual dysfunction in Parkinson disease without dementia. Neurology 65: , 1907–1913. |
[3] | Meindorfner C , Körner Y , Möller JC , Stiasny-Kolster K , Oertel WH , Krüger HP ((2005) ) Driving in Parkinson’s disease: Mobility, accidents, and sudden onset of sleep at the wheel. Mov Disord 20: , 832–842. |
[4] | Weintraub D , David AS , Evans AH , Grant JE , Stacy M ((2015) ) Clinical spectrum of impulse control disorders in Parkinson’s disease. Mov Disord 30: , 121–127. |
[5] | Wood JM , Worringham C , Kerr G , Mallon K , Silburn P ((2005) ) Quantitative assessment of driving performance in Parkinson’s disease. J Neurol Neurosurg Psychiatry 76: , 176–180. |
[6] | Cordell R , Lee HC , Granger A , Vieira B , Lee AH ((2008) ) Driving assessment in Parkinson’s disease–a novel predictor of performance? Mov Disord 23: , 1217–1222. |
[7] | Stolwyk RJ , Charlton JL , Triggs TJ , Iansek R , Bradshaw JL ((2006) ) Neuropsychological function and driving ability in people with Parkinson’s disease. J Clin Exp Neuropsychol 28: , 898–913. |
[8] | Thiri Kyaw W , Nishikawa N , Moritoyo T , Tsujii T , Iwaki H , Nomoto M ((2013) ) Evaluating the driving ability in patients with Parkinson’s disease using a driving simulator. Intern Med 52: , 871–876. |
[9] | Stolwyk RJ , Triggs TJ , Charlton JL , Iansek R , Bradshaw JL ((2005) ) Impact of internal versus external cueing on driving performance in people with Parkinson’s disease. Mov Disord 20: , 846–857. |
[10] | Stolwyk RJ , Triggs TJ , Charlton JL , Moss S , Iansek R , Bradshaw JL ((2006) ) Effect of a concurrent task on driving performance in people with Parkinson’s disease. Mov Disord 21: , 2096–2100. |
[11] | Uc EY , Rizzo M , Johnson AM , Emerson JL , Liu D , Mills ED , Anderson SW , Dawson JD ((2011) ) Real-life driving outcomes in Parkinson disease. Neurology 76: , 1894–1902. |
[12] | Uc EY , Rizzo M , O’Shea AMJ , Anderson SW , Dawson JD ((2017) ) Longitudinal decline of driving safety in Parkinson disease. Neurology 89: , 1951–1958. |
[13] | Heikkilä VM , Turkka J , Korpelainen J , Kallanranta T , Summala H ((1998) ) Decreased driving ability in people with Parkinson’s disease. J Neurol Neurosurg Psychiatry 64: , 325–330. |
[14] | King D , Benbow SJ , Barrett JA ((1992) ) The law and medical fitness to drive–a study of doctors’ knowledge. Postgrad Med J 68: , 624–628. |
[15] | Zesiewicz TA , Cimino CR , Malek AR , Gardner N , Leaverton PL , Dunne PB , Hauser RA ((2002) ) Driving safety in Parkinson’s disease. Neurology 59: , 1787–1788. |
[16] | Crizzle AM , Classen S , Uc EY ((2012) ) Parkinson disease and driving: An evidence-based review. Neurology 79: , 2067–2074. |
[17] | Jitkritsadakul O , Bhidayasiri R ((2016) ) Physicians’ role in the determination of fitness to drive in patients with Parkinson’s disease: Systematic review of the assessment tools and a call for national guidelines. J Clin Mov Disord 3: , 14. |
[18] | Klimkeit EI , Bradshaw JL , Charlton J , Stolwyk R , Georgiou-Karistianis N ((2009) ) Driving ability in Parkinson’s disease: Current status of research. Neurosci Biobehav Rev 33: , 223–231. |
[19] | Lloyd K , Gaunt D , Haunton V , Skelly R , Mann H , Ben-Shlomo Y , Henderson EJ ((2020) ) Driving in Parkinson’s disease: A retrospective study of driving and mobility assessments. Age Ageing 49: , 1097–1101. |
[20] | Fonda SJ , Wallace RB , Herzog AR ((2001) ) Changes in driving patterns and worsening depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci 56: , S343–351. |
[21] | Marottoli RA , de Leon CFM , Glass TA , Williams CS , Cooney LM Jr., Berkman LF ((2000) ) Consequences of driving cessation: Decreased out-of-home activity levels. J Gerontol B Psychol Sci Soc Sci 55: , S334–340. |
[22] | Mezuk B , Rebok GW ((2008) ) Social integration and social support among older adults following driving cessation. J Gerontol B Psychol Sci Soc Sci 63: , S298–303. |
[23] | Taylor BD , Tripodes S ((2001) ) The effects of driving cessation on the elderly with dementia and their caregivers. Accid Anal Prev 33: , 519–528. |
[24] | SurveyMonkey Inc., https://www.surveymonkey.com |
[25] | Braun V , Clarke V ((2013) ) Successful Qualitative Research: A Practical Guide for Beginners, Sage Publishing, London, UK. |
[26] | Ondo WG , Dat Vuong K , Khan H , Atassi F , Kwak C , Jankovic J ((2001) ) Daytime sleepiness and other sleep disorders in Parkinson’s disease. Neurology 57: , 1392–1396. |
[27] | Brodsky MA , Godbold J , Roth T , Olanow CW ((2003) ) Sleepiness in Parkinson’s disease: A controlled study. Mov Disord, 18: , 668–672. |
[28] | Ghorayeb I , Loundou A , Auquier P , Dauvilliers Y , Bioulac B , Tison F ((2007) ) A nationwide survey of excessive daytime sleepiness in Parkinson’s disease in France. Mov Disord 22: , 1567–1572. |




