The Subjective Experience of Living with Parkinson’s Disease: A Meta-Ethnography of Qualitative Literature
Abstract
Background:
A better understanding of the subjective experience of living with Parkinson’s disease (PD) and the factors that influence this experience can be used to improve wellbeing of people with PD (PwP).
Objective:
To gain more insight in the subjective experience of PD from the PwP’s perspective, and the factors that contribute to this experience.
Methods:
In this qualitative review, we performed a systematic search of qualitative studies discussing the subjective experience of PD and extracted reported themes (first order themes). Using a meta-ethnographic approach, we categorized the first order themes into second order themes, and created a third order construct: a holistic model of the subjective experience of living with PD.
Results:
We included 20 studies with a total sample of 279 PwP. Data-extraction yielded 227 first order themes, which were categorized into the second order themes: 1) Awareness, 2) Disruption, 3) Adjustment, 4) The external environment, and 5) The changing self. With these themes, we developed the “model of dialectic change” which conceptualizes life with PD as a transformative journey, wherein PwP employ strategies to stabilize their changeable relationship with their external environment, while simultaneously redefining their self-concept.
Conclusion:
Our findings indicate that not only the symptoms of PD, but also the manner in which these cause disruptions in the PwP’s interaction with their personal environment and self-concept, determine the subjective experience of PD and
quality of life. Some PwP experience problems with adjusting, resulting in psychological distress. This calls for a holistic, multidisciplinary and participatory approach of PD.
INTRODUCTION
Parkinson’s disease (PD) is a neurodegenerative disorder that is accompanied by motor and non-motor symptoms, including cognitive decline, autonomic failure and neuropsychiatric disorders. Due to the progressive nature of PD, these symptoms can eve-ntually result in functional and psychosocial limitations, with a major impact on the social, professional and family life of people with PD (PwP) [1, 2]. While this can understandably have a negative impact on quality of life, other factors like social support, life engagement, self-acceptance and a person with PD’s (PwP’s) perceptions of their condition are important determinants of life satisfaction and wellbeing of PwP, as well [3, 4]. However, as clinicians’ approaches to PwP are rooted within the clinical paradigm, conversations between PwP and medical professionals are often limited to symptoms and treatment effects [5]. Important personal factors that influence the subjective experience of living with PD may therefore not be addressed during the clinical consultations.
Since the 1990s, there is an increasing interest in qualitative research focusing on the subjective experience of PwP, and the factors that influence this experience. This type of research can provide important insights to decrease distress in PwP and to improve communication and health-related quality of life. Soundy and colleagues (2014) performed a previous qualitative meta-ethnography on the subjective experience of PD [6]. However, the authors of this article focused specifically on generalized hope and wellbeing, while the subjective experience of PD also encompasses other aspects, e.g., negative experiences of living with PD. The aim of this study therefore is to review the qualitative literature on the subjective experience of PD, in order to establish a holistic model of the subjective experience of PD from the PwP’s perspective, and the factors that contribute to this experience.
METHODS
The protocol for this qualitative meta-analysis is registered online in PROSPERO (registration number CRD42019131506) [7].
Search strategy and study selection
In collaboration with a medical librarian (LS) we performed a comprehensive search of the bibliographic databases PubMed, Embase.com, PsycINFO (via Ebsco), Cinahl (via Ebsco) and Scopus, spanning all entries up until March 11, 2019. Search terms included both controlled terms and free text terms. The terms ‘Parkinson disease’ AND ‘experience’ (including synonyms and closely related words) were used as index terms or free-text words. For the complete search string, we refer to the Supplementary Material. The search was performed without language or date restrictions.
We included studies with a qualitative design, in-cluding interviews, focus groups and photovoice studies, describing the subjective experience of PD from a PwP’s perspective. Qualitative historical studies and case studies, as well as articles that focused on a particular aspect of PD, such as a single symptom, or experiences with interventions, were excluded. Our study sample consisted of people with self-reported or medically confirmed PD. Studies using mixed samples were only included if the results for PwP were reported separately.
Duplicates were removed from the search results. Titles and abstracts were first screened for eligibility by two authors independently (SR and ES), and full text articles of potentially eligible studies were read carefully. Disagreement over the eligibility of particular studies was resolved through discussion, including a third author (KR). SR and ES independently assessed the quality of included studies using the Consolidated Criteria for Reporting Qualitative Research (COREQ), which are used to evaluate three domains: 1) reporting on the research team and its reflexivity, 2) the rigor of the study design, and 3) the quality of the analytical process and resultant findings [8]. The quality of articles with a COREQ score lower than 13 out of 32 were discussed by SR, ES and KR, with a main focus on COREQ domain 2 and 3, and articles of insufficient quality were excluded.
Data collection and analysis
For this study, we used the meta-ethnographic approach, which was introduced by Noblit and Hare (1988) as a qualitative counterpart to the quantitative systematic review [9]. However, while quantitat-ive reviews deal with the evaluation or summarization of ‘objective knowledge’ (i.e., measurable facts), the meta-ethnographic approach is interested in ‘constructed knowledge’: concepts and perceptions, that are— according to the philosophical position of objective idealism— collectively shared. Rather than trying to ascertain the veracity of the results of the studies under review, the meta-ethnography aims to provide a synthesis that is mindful of both the commonalities of the constructed knowledge under review and the context in which this knowledge was generated.
The process of data-collection started with SR and ES independently reading the included articles, and collating the first order themes, i.e., the the-mes and subthemes reported by the authors of the article, in an Excel file (Microsoft Excel for Windows, 2016). The first order themes were compared by the two authors, and disagreements regarding interpretation of particular themes were resolved through discussion.
The analysis of the first order themes was performed by SR and KR, using the principles of the constant comparative method [10]. Through repeated comparison of the first order themes, similar concepts were rearranged into second order themes. Simultaneously, representational differences that are indicative of consequential contextual variation were identified.
As a final step in the meta-ethnography, SR and KR analyzed the relationship between the second order themes. Potential relationships between the second order themes were assessed in light of the thematic relations reported in the original studies (first order relations). Through this exercise, the researchers ar-rived at a third order construct, i.e., a model, of the subjective experience of living with PD and the factors that influence this experience, based on a synthesis of the reviewed literature. To decrease the influence of subjective bias, the second order themes and model were discussed by the two authors repeatedly, bearing the following criteria in mind:
1. The final model ought to accommodate the largest number of first order themes
2. In order to avoid disembedding the concepts from their context, the first order relationships reported in the original studies were included to the greatest extent possible
3. The meta-analysis ought to create novel insights.
As a final step, we performed a member check by presenting the results to two patient-researchers from the Dutch Parkinson’s disease Association (RH and KV).
RESULTS
Systematic search
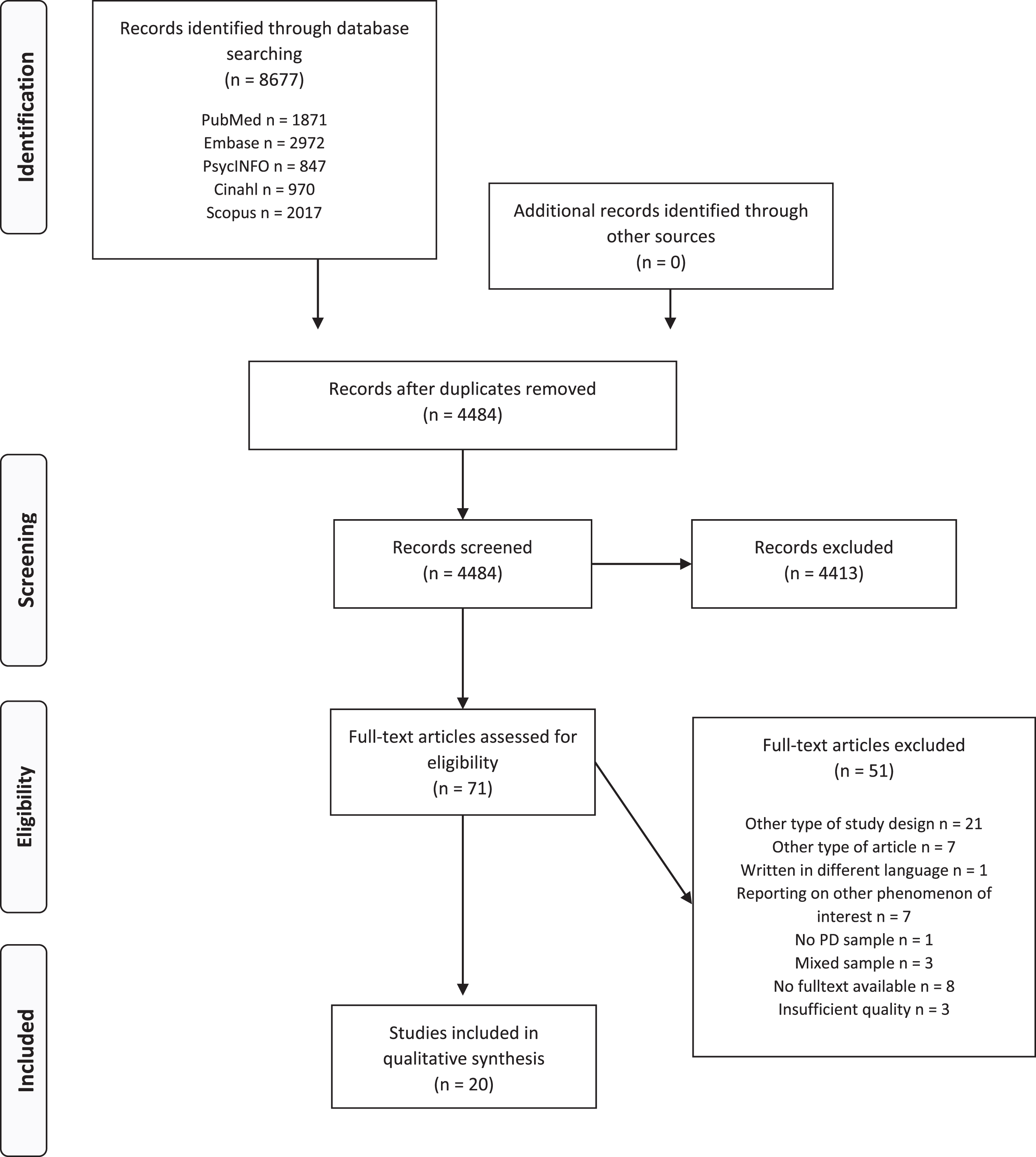
A total of 71 full-text articles were assessed for eligibility, of which 48 were excluded, resulting in a total of 23 included studies. Based on insufficient quality, we excluded three studies more studies, resulting in a final number of 20 articles in the meta-ethnography. The selection procedure is shown in the PRISMA flow diagram (Fig. 1).
Fig. 1
Flow chart.
Critical appraisal
The mean total COREQ score of included studies was 18/32, with a range between 13 and 22. Included studies scored lowest on COREQ domain 1 (mean score of 2/8, range 0 – 4), with most studies failing to report details about the researchers and their previous relationship with the study participants. While the study design was presented clearly in most studies, reasons for non-participation, the presence of non-participants during interviews and whether the researchers took field notes, were not reported in multiple studies, resulting in a mean score of 9/15 on COREQ domain 2 (range 7 – 12). Data-analysis and reporting of findings was rated overall as sufficient, with a mean score of 6/9 on COREQ domain 3 (range 2 – 8), although most studies failed to report details on the use of software, and whether they performed a member-check.
Details of the included studies are provided in Table 1. Across all studies, a total of 279 PwP were included. Of these PwP, 137 were female and 142 male. The mean age and age range was not disclosed in all studies, but reported ages of participants varied from 32 to 95 years.
Table 1
Study characteristics of the included studies
| Study | Aim and focus of study | Qualitative method and study setting | Method of sampling | Study population and number of participants | Gender and age of participants (mean and range) | Duration of illness (mean and range) | COREQ score |
| Caap-Ahlgen | To explore women’s | Interviews. | Purposive | PwP: n = 8 | Female: n = 8, male: n = 0. | Mean not reported, | 19 |
| et al. (2002) [23] | experiences of living | Participant’s home. | (age, disease | Mean age = 70 y, | range 5– 15 y. | ||
| with symptoms | duration, civil | range 68– 80 y. | |||||
| related to PD, | status) | ||||||
| and to analyze | |||||||
| how the symptoms | |||||||
| influence their | |||||||
| quality of life | |||||||
| Chiong-Rivero | To identify health- | Focus groups and | Purposive (gender, | Mixed. | Female: n = 26, male: n = 22. | Mean and range | 17 |
| (2011) [31] | related quality of | interviews. Study | age, ethnicity, age | PwP: n = 48; | Mean age = 63 y, | not reported. | |
| life domains or themes | setting not | of disease onset) | caregivers: | range not reported. | |||
| that reflect patients’ | specified. | n = 15 | |||||
| perceptions on living | |||||||
| with PD in a | |||||||
| comprehensive matter | |||||||
| Davis et al. | To determine the self- | Focus groups. | Convenience | PwP: n = 9 | Female: n = 3, male: n = 6. | Mean = 10 y, | 17 |
| (2003) [17] | perceived physical | Church. | Mean age = 71 y, | range 3– 20 y. | |||
| limitations and compensatory | range 51– 85 y. | ||||||
| strategies of individuals | |||||||
| living with Parkinson’s disease | |||||||
| Eccles et al. | To investigate how people | Interviews. | Purposive | PwP: n = 11 | Female: n = 4, male: n = 7. | Mean = ?, | 17 |
| (2011) [32] | with PD perceive | Participant’s home. | (selection criteria | Mean age = 72 y, | range 1.5 y– 16 y. | ||
| the cause and their | not reported) | range 59– 82 y. | |||||
| control of their disease | |||||||
| Haahr | To explore PwP’ lifeworld | Interviews. | Convenience | PwP: n = 11 | Female: n = 3, male: n = 8. | Mean = 15 y, | 13 |
| (2010) [24] | and way of managing life with | Participant’s home. | Mean age = 60 y, | range 7– 29 y. | |||
| advanced PD prior to | range 47– 67 y. | ||||||
| DBS and to illuminate | |||||||
| what they expect from | |||||||
| life following DBS | |||||||
| Hermanns et al. | To explore the illness | Photovoice. | Convenience | PwP: n = 9 | Female: n = 7, male: n = 2. | Mean = 5 y, | 22 |
| (2015) [20] | experience of people with PD | University. | Mean age = 63 y, | range not reported. | |||
| range 39– 76 y. | |||||||
| Kang et al. | To examine the level of | Interviews. | Convenience | PwP: n = 8 | Female: n = 5, male: n = 3. | Mean = 7 y, | 20 |
| (2015) [18] | success as defined by people with | Participant’s home. | Mean age = 66 y, | range 2– 16 y. | |||
| PD, and to find what | range 57– 78 y. | ||||||
| contributes to the | |||||||
| level of success | |||||||
| Liao et al. | To explore the illness | Interviews. | Purposive | PwP: n = 15 | Female: n = 6, male: n = 9. | Mean not reported, | 19 |
| (2013) [26] | experience of older Taiwanese | Medical center. | (selection criteria | Mean = 73 y, | range 4– 20 y. | ||
| individuals at different | not reported) | range 65– 80 y. | |||||
| stages of PD | |||||||
| Lutz et al. | To deepen the current | Photovoice. | Convenience | PwP: n = 6 | Female: n = 2, male: n = 4. | Mean and range | 19 |
| (2018) [14] | understanding of the experience | Clinic or | Mean age = 67 y, | not reported. | |||
| of living with PD and | participant’s home. | range 57– 73 y. | |||||
| its implications for occupation | |||||||
| Marr | To examine the experience | Interviews. | Not specified | PwP: n = 6 | Female: n = 3, male: n = 3. | Mean not reported, | 17 |
| (1991) [12] | of living with PD | Participant’s home. | Mean age is not reported, | range 2– 15 y. | |||
| range 53– 79 y. | |||||||
| Nazzal et al. | To describe the daily living | Interviews. | Convenience | PwP: n = 8 | Female: n = 4, male: n = 4. | Mean = 7 y, | 16 |
| (2017) [33] | experience and impact on lives | University. | Mean age = 57 y, | range 2– 14 y. | |||
| of Jordanian individuals | range 32– 76 y. | ||||||
| with PD | |||||||
| Olsson et al. | To describe the meaning of | Interviews. | Convenience | PwP: n = 9 | Female: n = 9, male: n = 0. | Mean not reported, | 17 |
| (2015) [21] | feeling well as experienced | Participant’s home. | Mean age is not reported, | range 3– 19 y. | |||
| by women with PD | range 46– 65 y. | ||||||
| Shaw et al. | To investigate the current | Interviews. | Convenience | PwP: n = 12 | Female: n = 5, male: n = 7. | Mean not reported, | 16 |
| (2017) [34] | ethical issues of recognizing | Study setting | Mean age is not reported, | range 11 mo– 24 y. | |||
| and managing PD from | not specified. | range 51– 86 y. | |||||
| a patients’ perspective | |||||||
| Sjödahl Hammerlund | To explore the overall | Interviews. | Purposive | PwP: n = 19 | Female: n = 11, male: n = 8. | Mean not reported, | 17 |
| (2018) [19] | impact of living with PD | Study setting | (gender, age, | Mean age is not reported, | range 3– 27 y. | ||
| not specified. | disease duration | range 55– 84 y. | |||||
| and severity) | |||||||
| Soleimani et al. | To explore the primary | Interviews. | Purposive | PwP: n = 17 | Female: n = 7, male: n = 10. | Mean = 6 y, | 20 |
| (2016) [15] | concerns and perceptions of | Participant’s home. | (gender, age, | Mean age = 72 y, | range 1– 16 y. | ||
| people living with PD | educational level, | range 60– 90 y. | |||||
| employment status, | |||||||
| disease duration | |||||||
| and severity) | |||||||
| Sperens et al. | To explore how people with | Interviews. | Convenience | PwP: n = 24 | Female: n = 10, male: n = 14. | Mean = 8 y, | 20 |
| (2018) [22] | PD manage the effect of the | Participant’s home | Mean age = 61 y, | range 1– 19 y. | |||
| disease on everyday life and | or telephone. | range 46– 80 y. | |||||
| to investigate gender similarities | |||||||
| and differences concerning this issue | |||||||
| Stanley– Hermanns | To understand how persons with PD | Interviews and | Purposive | PwP: n = 14 | Female: n = 7, male: n = 7. | Mean and range | 17 |
| et al. (2010) [16] | construct their illness experience and | field work. | (disease severity, | Mean age = 68 y, | not reported. | ||
| manage living with the | Study setting | ability to | range 38– 82 y. | ||||
| disease on a daily basis | not specified. | articulate | |||||
| subjective | |||||||
| experience) | |||||||
| Vann-Ward et al. | To identify, explore and theorize | Interviews, observation, | Purposive | PwP: n = 25 | Female: n = 10, male: n = 15. | Mean not reported, range | 15 |
| (2017) [13] | the social and psychological | videos and documents. | (selection criteria | Mean age is not reported, | 3 mths to 30 y. | ||
| processes used by people with PD | Participant’s home | not reported) | range 40– 95 y. | ||||
| and telephone. | |||||||
| Williams et al. | To examine the experiences of older | Interviews. | Convenience | Mixed. | Female: n = 3, male: n = 10. | Mean and range | 18 |
| (2008) [25] | people with late stage PD and to | Participant’s home. | PwP: n = 13; | Mean = 76 y, range 61– 89 y. | not reported. | ||
| understand the transitions experienced | caregivers: | ||||||
| by patients and their families | n = 13 | ||||||
| as they encounter greater disability | |||||||
| Wressle et al. | To study how PD affects daily living | Interviews. | Strategic | Mixed. | Female: n = 4, male: n = 3. | Mean not reported, | 18 |
| (2007) [35] | from the perspective of both patient | Participant’s home | PwP: n = 7; | Mean age is not reported, | range 2– 5 y. | ||
| and relative, and to identify factors | and medical unit. | family members | range 64– 77 y. | ||||
| that can facilitate their daily living | of PwP: n = 9 |
Data analysis and synthesis
The extraction of data resulted in a total of 227 first order themes. Nineteen first order themes could not be categorized because they did not describe specific content (e.g., “complexity”), or because they were not specific enough (e.g., the first order theme “challenging perspectives” referred to acceptance of the diagnosis, decreased physical activity, curtailment of social activities and emotional losses). These themes were excluded from the meta-analysis. Through comparison, the 208 included first order themes were all categorized into five second order themes: 1) Awareness (n = 17 first order themes), 2) Disruption (n = 35), 3) Adjustment (n = 77), 4) The external environment (n = 44), and 5) The changing self (n = 34). A full description of these themes and subthemes is provided in the codebook in Table 2.
Table 2
Codebook
| Second order themes (no. of first order themes per second order theme) | Definition | Second order subthemes (no. of first order themes per second order subtheme) | Definition | Examples of first order theme |
| Adjustments | Coping strategies used | General | General or non-specific | Coping with the disease |
| (n = 77) | to deal with the | (n = 10) | coping strategies | |
| disruptions caused | Medication | (Adjusting to) the use | Dealing with the unpredictable effects | |
| by Parkinson’s | (n = 9) | of antiparkinsonian agents | of medication; considering medicine | |
| disease | Physical exercise | Using physical exercise | Staying active; putting physical | |
| (n = 2) | as a means to cope with PD | exercise into practice | ||
| Planning for the future | Plans and hopes for | Treatment choices in the | ||
| (n = 4) | future treatment of PD | future; envisioning a future | ||
| Problems | Difficulties in coping with PD | Crumbling managing strategies | ||
| (n = 11) | and routines; coping fatigue | |||
| Psychological strategies | Attitudinal adjustments or rhetorical | Maintaining a positive outlook; | ||
| (n = 13) | strategies employed to cope with PD | using downward comparison | ||
| Routines | Behavioral patterns developed | Managing time and energy; | ||
| (n = 19) | to cope with PD | to be foreseeing and plan | ||
| Social strategies | Modifications in social interactions | Concealing oneself from | ||
| (n = 7) | employed to cope with PD | others; social disclosure | ||
| Spirituality | Religious or meta-physical cognitions | Surrendering to a higher | ||
| (n = 2) | meant to cope with PD | power to weather the storm | ||
| Awareness | The level of awareness | Emerging Symptoms | Awareness of the development of physical | Noticing something is different |
| (n = 17) | of symptoms and | (n = 2) | or cognitive symptoms consistent | |
| knowledge about PD | with the diagnosis of PD | |||
| Cognizance | Recognition of (the implications of) emerging | Interpreting the symptoms | ||
| (n = 12) | symptoms and/ or the attendant diagnosis of PD | |||
| Ignorance | Unawareness of (the implications of) emerging | Ignorance about the symptoms | ||
| (n = 3) | symptoms and/ or the attendant diagnosis of PD | |||
| Disruption | Disruptions due to | Mental symptoms | Cognitive deterioration or | Mental alterations |
| (n = 35) | symptoms, limitations | (n = 4) | psychological alterations | |
| or negative emotions | Negative affect and | Fears, anxieties, depressed mood or | Fears and uncertainty about the future | |
| or thoughts | cognitions | ruminations arising from PD | ||
| (n = 10) | ||||
| Physical incompetence | Loss of physical functioning | Being constrained in daily life | ||
| (n = 15) | ||||
| Physical symptoms | Physical motor and non-motor | Loss of control over limb movements | ||
| (n = 6) | symptoms of PD | |||
| External | The personal context | Health care support | Health care for PD | Accessibility to health care |
| environment | that impacts the | (n = 8) | ||
| (n = 44) | experience of | Professional changes | Changes or termination of | Early retirement or involuntary |
| living with PD, or is | (n = 4) | employment due to PD | loss of employment | |
| changed due to PD | Social changes | Changes in socialization patterns or | Compromised social participation | |
| (n = 13) | relationships due to PD | |||
| Social support | Benefits arising from social connections | Feelings of comfort with social contacts | ||
| (n = 9) | ||||
| Stigma &shame | Negative affect relating to PD that stymies | Stigma and other feelings about PD | ||
| (n = 10) | social or professional interaction | |||
| The changing | Changes of body-image, | Perceiving the body | Sensory experiences of the body | Controlled by or controlling the body |
| self | self-image and identity | (n = 8) | and attendant cognitions | |
| (n = 34) | due to (the | Reconstructing the self | Re-articulating one’s self-concept to accord | Forming new identities |
| consequences of) PD | (n = 11) | with the constraints of life with PD | ||
| Self-image and identity | Cognitions about (aspects of) the self | A sense of being deprived | ||
| (n = 5) | on one’s self-worth | |||
| The eroding self | Untenable beliefs about the self | Becoming dependent on others for care | ||
| (n = 8) | ||||
| The former self | Past events and beliefs about the self | Significant events | ||
| (n = 2) |
Following our comparative analysis, we identified two overarching thematic relationships. A first set of themes relates to disruptions (i.e., physical and mental symptoms, negative affect and cognitions caused by PD), the way in which these disruptions may be alleviated or exacerbated by the external (i.e., social, professional and medical) environment, as well as the adjustments (coping strategies) employed by PwP. A second cluster of themes stresses the evolving nature of life with PD and includes awareness of PD and changes in self-perception and identity (the changing self), as the disease progresses over time.
Our “model of dialectic change” (see Fig. 2) encompasses both relationships. Central to this model is the dialectic between stability and instability, as well as the ongoing negotiation between the external environment and the self. Inspired by Hegel’s dialectics (2010) [11], our model holds that this dialectic is comprised of three states: stability, instability, and unity. A sense of stability results from closely held beliefs about the self and the role of the self within the personal environment. Instability arises when the individual is presented with a contradictory truth that renders these prior beliefs untenable. The arrival at a new equilibrium requires a process of concurrent negation and preservation, whereby the original understanding about the self and the social roles is somehow unified with its contradiction.
Fig. 2
Model of dialectic change.
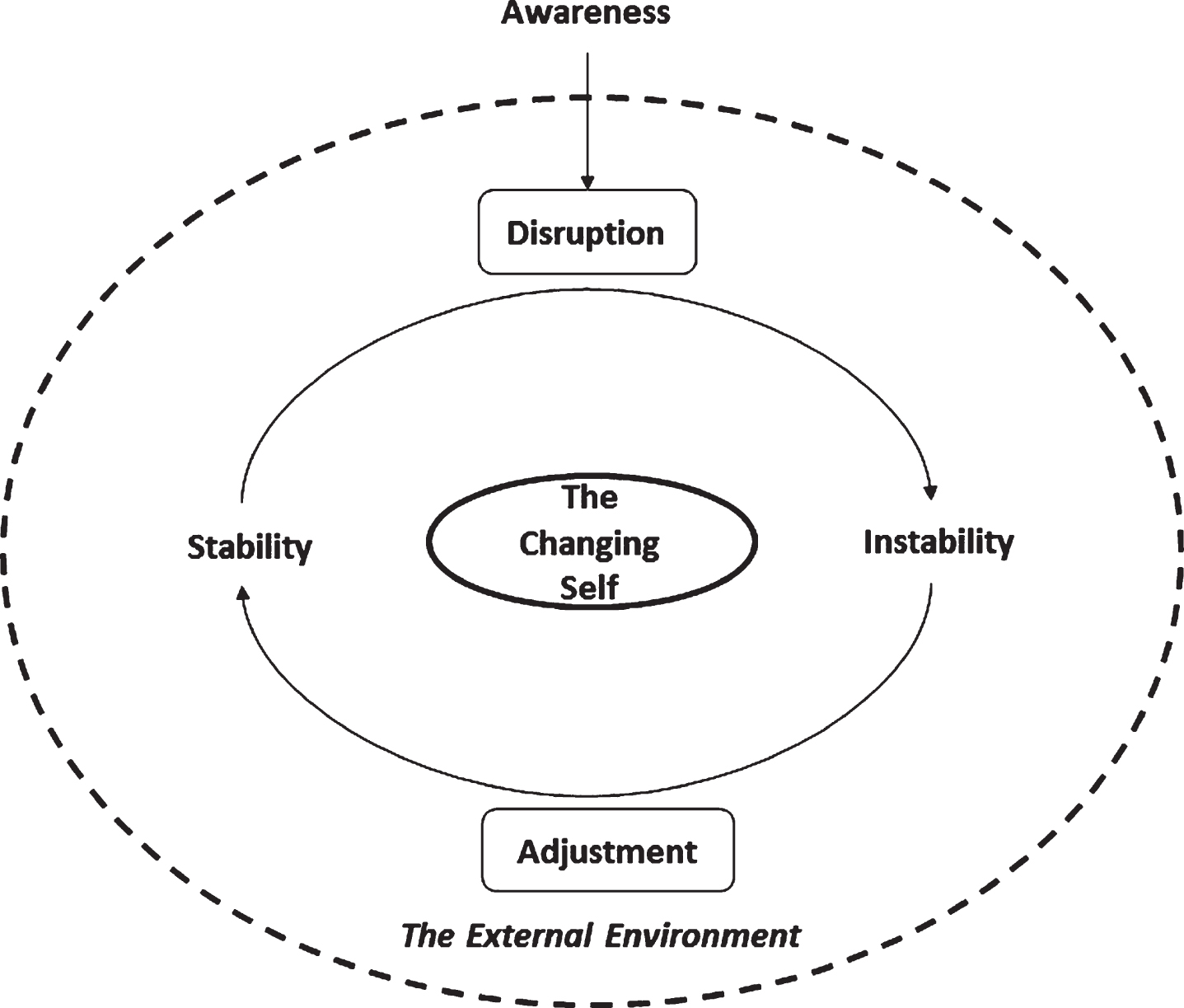
The start of this dialectic process is generally marked by the diagnosis, which necessitates that PwP in some way reconcile their diagnosis of PD with their prior concept of the (healthy) self [12, 13], and periodically resurfaces when symptoms exacerbate and/or interrupt the personal status quo. PwP frequently respond to the resulting instability through adjustments that are aimed at maintaining the extant self-concept [13– 16]. These adjustments can be psychological strategies, e.g., employing relativism or downward comparison [17– 19], but often address the external environment. For example, PwP may start a new form of treatment, implement new daily routines, or rely more on support from their family [9, 12, 13, 17– 22].
However, if external adjustments prove incapable of preventing changes in physical or cognitive functioning that preclude the performance of tasks or roles that the person with PD strongly identifies with, the self-concept rather becomes the focus of the dialectic process [16, 23], e.g., a person with PD who considered his independence as an important personal trait will need to redefine his self-concept when he becomes increasingly dependent on others due to physical limitations. This requires a ‘sifting and sorting’ of previously held beliefs about the self and identification of alternative or novel representative traits [13– 15, 19].
Notable is that our “model of dialectic change” suggests that it is not necessarily the prevalence or intensity of symptoms, but rather the degree of perceived stability that primarily determines a PwP’s quality of life. Stability in turn depends on the degree to which PwP are able to sustain roles, activities and closely held beliefs about the self [13– 15, 19]. The interaction between symptoms, physical and cognitive limitations, and individual notions of stability highlighted by our model suggests it does not necessarily follow that instability is more frequent or intense in the later stages of PD. However, during late stage PD, potentially successful coping strategies do become less numerous and/or effective [24], e.g., motor symptoms might no longer be sufficiently reduced by medications, and social interactions may be hampered by cognitive or speech problems. The-refore, episodes of instability may become more dominant in later disease stages [16, 25, 26].
In sum, our model conceptualizes life with PD as a transformative journey, wherein PwP employ strategies intended to stabilize their changeable relationship with their external environment, as well as actively engage in a continuous process of reconstituting the self.
Our member check with two patient-researchers of the Dutch Parkinson’s disease association (RH and KV) affirmed that the results of our meta-ethnography summarize their experience of living with PD. However, as they pointed out, the model is not specific to the experience of living with PD; it is also be app-licable to the process of adjustment after life-events during an average person’s life. However, both pat-ient-researchers emphasized this does not detract from its value, as people living with PD are people first and patients second.
DISCUSSION
In this study, we aggregated the qualitative literature on the subjective experience of PD by performing a meta-ethnography of 208 first order themes derived from 20 included studies, resulting in a “model of dia-lectic change”. Capturing the evolving nature of life with Parkinson’s, our model demonstrates how life with PD is accompanied by disruptions, that dem-and that PwP make repeated behavioral and psychological adjustments to maintain a stable relationship to both their external environment and their self-concept.
Our review highlights two main approaches to stabilization. The first aims at maintaining or restoring normal interaction with the external environment, e.g., medical treatment aims to provide relief from symptoms and physical disability, while care and social support aim at limiting the effect of disabilities on performance of PwP’s roles and tasks. The second approach focuses on resolving the dissonance that arises when physical or cognitive limitations render closely held beliefs about the self unattainable. This is achieved through a process of re-evaluation of the self, discarding old and discovering new activities and traits that are central to the self-concept. While this is a natural process for some PwP, others may experience problems adjusting, resulting in psychological distress [4].
The two approaches described above imply clear and complementary roles for the neurologist and other (para)medical health care professionals, like PD nurses, psychologists and psychiatrists, advocating a multidisciplinary approach to PD. While the neu-rologist is responsible for education of the PwP and his/her significant others, treatment of symptoms, and referral to other health care professionals, the PD nurse, psychologist and psychiatrist may provide support or treatment for PwP with difficulties adjusting to new symptoms or limitations, who experience psy-chological distress, and who are struggling with re-defining the self. An example of a treatment that addresses these issues is acceptance and commitment therapy (ACT); a psychotherapy that aims at helping a person to accept and endure unpleasant feelings, like symptoms of PD, and to clarify and take action on personal values, thereby increasing psychological flexibility and helping the PwP to live a valuable life in spite of these symptoms [27].
Our analysis also emphasizes the reciprocity between health care professional and PwP. The concepts of stability and instability are both encompassing of, and deeply embedded within the everyday lives of PwP. While PwP depend on medical professionals to augment their ability to maintain stability and address episodes of disruption, medical professionals, in turn, require participatory engagement of PwP to define the beliefs and activities that are central to the PwP’s notions of stability and concepts of self. Given the progressive and transformative nature of PD, the collective search for stability is a continuous process, rather than a one-time intervention.
Soundy and colleagues (2014) performed a previous qualitative meta-ethnography on the subjective experience of PD [6]. However, as their analysis focused on factors that influence generalized hope in PwP, only eight of their included studies overlap with ours, and their “model of hope enablement” cannot be directly compared to our model of dialectic change. However, there is some overlap between the models: the model of Soundy and colleagues also underscores the importance of social contacts and meaningful activities for the maintenance of self-concept and experienced quality of life [6]. As a general and intuitive theory of life with transformative events, our model covers a broader spectrum of relevant themes, while providing insights into the challenges of living with PD as well as the relevant measures and actions that healthcare practitioners and PwP can take to achieve stability. It may therefore be used in the education of PwP and their significant others, or in a participatory approach to consultation in order to assess the various stabilizing and destabilizing factors that are relevant to the person with PD.
A widely used theoretical framework for examining the perceptual, behavioral and cognitive pro-cesses involved in the management of health threats is the ‘Common Sense Model of Self-regulation’ (CSM) [28, 29]. The CSM describes the processes that generate an individual’s perception of a health threat, procedures for management, and a system for creating and implementing actions. The model has proven useful in PwP as well. For example, Hurt and colleagues (2006) used the CSM to study barriers for seeking treatment for non-motor symptoms in PwP, and found that uncertainty about the relationship of non-motor symptoms to PD and lack of clarity around treatments were common [30]. Our model of dialectic change shows some similarities with the CSM. For example, both models describe how a ‘disturbance’ or health threat can initiate different processes that result in ‘adjustments’ or actions, like lifestyle changes and seeking treatment. In both models, the influence of the personal environment (social contacts, physicians, etc.) in this process is acknowledged. However, where the CSM focusses more on perception of symptoms, illness and treatments, our model emphasizes the impact of the PD on the perception of the self. Moreover, the chronic model as described by Leventhal and colleagues (2016) in their historical narrative on the CSM, does not seem to encompass the progressive nature of disorders like PD. In this review, the aut-hors acknowledge that some chronic conditions, like asthma, are accompanied by acute episodes, just like PD. However, PD differs from the chronic health threats mentioned in this review (hypertension, as-thma and heart failure) in the sense that due to disease progression, at some point external adjustments may become insufficient in performing roles that PwP strongly identify with. This shifts the focus from perception of the illness, treatment and self-man-agement, to the self. We therefore feel that our model of dialectic change is a valuable contribution to the current literature on health psychology, especially for people with PD and other progressive neurological disorders.
A strength of this study was the broad literature search in five different databases, that resulted in 4484 articles (after removal of duplicates). As we excluded 4413 (98%) based on our in- and exclusion criteria, we think that it’s unlikely that we failed to retrieve some of the relevant articles that were published. However, a limitation of this study is the limited number and variable quality of qualitative studies on the subjective experience of PD from the PwP’s perspective. Moreover, although we excluded case reports, almost half of the studies included small samples, which increases the risk of overestimating themes, or not being able to capture all themes. However, the included studies reported on a total 279 PwP, with disease duration ranging between several months to 30 years, and a comparable number of males and females in the age range of 32 to 96 years old. We therefore feel that this meta-analysis covers a study sample with considerable relevant variation. Moreover, we extracted a total of 227 first order themes from the included articles, providing an expansive and varied representation of life with PD. Our member check confirmed that our model of dialectic change summarizes their experience of living with PD, which increased our confidence that the results of this meta-ethnography represent the subjective experience of living with PD from the perspective of the PwP. However, the limited number of two patient-researchers from the same national and cultural background can be viewed as a final limitation of this study.
In conclusion, our meta-ethnography demonstrated that the physical and cognitive deterioration accompanying PD presents challenges to the maintenance of PwP’s personal equilibrium and self-concept and requires considerable adaptability and mental fortitude. Adjustment problems and psychological distress are therefore not uncommon. Successful treatment therefore ought to define its approach and objectives not only based on symptoms, but also the manner in which these impinge on PwP’s developing self-concepts. Not only the neurologist, but also the PD nurse, psychologist, psychiatrist and, most importantly, PwP themselves as well as the people in their personal environment, can play an important role in this process. This meta-ethnography therefore advocates a multidisciplinary treatment approach of PD which is holistic, dynamic, and participatory.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
ACKNOWLEDGMENTS
This work was financially supported by the Dutch Parkinson’s disease association (Parkinson Vereniging) [grant number 2018-R05, 2018].
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD202299.
REFERENCES
[1] | Shulman L , Gruber-Baldini A , Anderson K , Vaughan C , Reich S , Fishman P , Weiner W ((2008) ) The evolution of disability in Parkinson disease. Mov Disord 23: , 790–796. |
[2] | Hartley S , McArthur M , Coenen M , Cabello M , Covelli V , Roszczynska-Michta J , Pitkänen T , Bickenbach J , Cieza A ((2014) ) Narratives reflecting the lived experiences of people with brain disorders: Common psychosocial difficulties and determinan. PLoS One 9: , e96890. |
[3] | Damiano A , Snyder C , Strausser B , Willian M ((1999) ) A review of health-related quality-of-life concepts and measures for Parkinson’s disease. Qual Life Res 8: , 235–243. |
[4] | Vescovelli F , Sarti D , Ruini C ((2019) ) Well-being and distress of patients with Parkinson’s disease: A comparative investigation. Int Psychogeriatr 31: , 21–30. |
[5] | Boersma I , Jones J , Carter J , Bekelman D , Miyasaki J , Kutner J , Kluger B ((2016) ) Parkinson disease patients’ perspectives on palliative care needs: What are they telling us?. Neurol Clin Pract 6: , 209–219. |
[6] | Soundy A , Stubbs B , Roskell C ((2014) ) The experience of Parkinson’s disease: A systematic review and meta-ethnography. ScientificWorldJournal 2014: , 613592. |
[7] | Rutten S , PROSPERO International prospective register of systematic reviews, https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=131506, |
[8] | Tong A , Sainsbury P , Craig J ((2007) ) Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: , 349–357. |
[9] | Noblit G , Hare R ((1988) ) Meta-ethnography: Synthesizing qualitative studies, Sage Publications, Beverly Hills and London. |
[10] | Corbin J , Strauss A ((1990) ) Grounded theory research: Procedures, canons, and evaluative criteria. Qual Sociol 13: , 3–21. |
[11] | Hegel GWF ((2010) ) Encyclopedia of the Philosophical Sciences in Basic Outline, The Cambridge Hegel Translations, Cambridge University Press, Cambridge |
[12] | Marr J ((1991) ) The experience of living with Parkinson’s disease. J Neurosci Nurs 23: , 325–329. |
[13] | Vann-Ward T , Morse JM , Charmaz K ((2017) ) Preserving self: Theorizing the social and psychological processes of living with Parkinson disease. Qual Health Res 27: , 964–982. |
[14] | Lutz S , Holmes J , Rudman D , Johnson A , LaDonna K , Jenkins M ((2018) ) Understanding Parkinson’s through visual narratives: “I’m not Mrs. Parkinson’s”. Br J Occup Ther 81: , 90–100. |
[15] | Soleimani MA , Bastani F , Negarandeh R , Greysen R ((2016) ) Perceptions of people living with Parkinson’s disease: A qualitative study in Iran. Br J Community Nurs 21: , 188–195. |
[16] | Stanley-Hermanns M , Engebretson J ((2010) ) Sailing the stormy seas: The illness experience of persons with parkinson’s disease. Qual Rep 15: , 340–369. |
[17] | Davis JT , Ehrhart A , Trzcinski BH , Kille S , Mount J ((2003) ) Variability of experiences for individuals living with Parkinson disease. Neurol Rep 27: , 38–45. |
[18] | Kang M-Y , Ellis-Hill C ((2015) ) How do people live life successfully with Parkinson’s disease?. J Clin Nurs 24: , 2314–2322. |
[19] | Sjödahl Hammarlund C , Westergren A , Åström I , Edberg A-K , Hagell P ((2018) ) The impact of living with Parkinson’s disease: Balancing within a web of needs and demands. Parkinsons Dis 2018: , 4598651. |
[20] | Hermanns M , Greer DB , Cooper C ((2015) ) Visions of living with Parkinson’s disease: A photovoice study. Qual Rep 20: , 336–355. |
[21] | Olsson M , Nilsson C ((2015) ) Meanings of feeling well among women with Parkinson’s disease. Int J Qual Stud Health Well-being 10: , 28730. |
[22] | Sperens M , Hamberg K , Hariz G-M ((2018) ) Challenges and strategies among women and men with Parkinson’s disease: Striving toward joie de vivre in daily life. Br J Occup Ther 81: , 700–708. |
[23] | Caap-Ahlgren M , Lannerheim L ((2002) ) Older Swedish women’s experiences of living with symptoms related to Parkinson’s disease. J Adv Nurs 39: , 87–95. |
[24] | Haahr A , Kirkevold M , Hall EO , Ostergaard K ((2010) ) Living with advanced Parkinson’s disease: A constant struggle with unpredictability. J Adv Nurs 67: , 408–417. |
[25] | Williams S , Keady J ((2008) ) ‘A stony road... a 19 year journey’: ‘Bridging’ through late-stage Parkinson’s disease. J Res Nurs 13: , 373–388. |
[26] | Liao YC , Wu YR , Tsao LI , Lin HR ((2013) ) The experiences of Taiwanese older individuals at different stages of Parkinson disease. J Neurosci Nurs 45: , 370–377. |
[27] | Graham C , Gouick J , Krahé C , Gillanders D ((2016) ) A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev 46: , 46–58. |
[28] | Leventhal H , Phillips L , Burns E ((2016) ) The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J Behav Med 39: , 935–946. |
[29] | LeventhalH, NerenzD, SteeleC ((1984) ) Illness representations and coping with health threats. In: A Handbook of Psychology and Health. Erlbaum, Hillsdale, NJ. |
[30] | Hurt C , Rixon L , Chaudhuri K , Moss-Morris R , Samuel M , Brown R ((2006) ) Identifying barriers to help-seeking for non-motor symptoms in people with Parkinson’s disease. J Health Psychol 24: , 561–571. |
[31] | Chiong-Rivero H , Ryan GW , Flippen C , Bordelon Y , Szumski NR , Zesiewicz TA , Vassar S , Weidmer B , Garcia RE , Bradley M , Vickrey BG ((2011) ) Patients’ and caregivers’ experiences of the impact of Parkinson’s disease on health status. Patient Relat Outcome Meas 2011: , 57–70. |
[32] | Eccles FJ , Murray C , Simpson J ((2011) ) Perceptions of cause and control in people with Parkinson’s disease. Disabil Rehabil 33: , 1409–1420. |
[33] | Nazzal MS , Khalil H ((2017) ) Living with Parkinson’s disease: A Jordanian perspective. Scand J Occup Ther 24: , 74–82. |
[34] | Shaw ST , Vivekananda-Schmidt P ((2017) ) Challenges to ethically managing Parkinson disease: An interview study of patient perspectives. J Patient Exp 4: , 191–196. |
[35] | Wressle E , Engstrand C , Granérus A-K ((2007) ) Living with Parkinson’s disease: Elderly patients’ and relatives’ perspective on daily living. Aust Occup Ther J 54: , 131–139. |




