Individuals and Families Affected by RYR1-Related Diseases: The Patient/Caregiver Perspective
Abstract
Background and objective:
Pathogenic variants of RYR1, the gene encoding the principal sarcoplasmic reticulum calcium release channel (RyR1) with a crucial role in excitation-contraction coupling, are among the most common genetic causes of non-dystrophic neuromuscular disorders. We recently conducted a questionnaire study focusing on functional impairments, fatigue, and quality of life (QoL) in patients with RYR1-related diseases (RYR1-RD) throughout the recognized disease spectrum. In this previous questionnaire study the medical perspective was taken, reflective of a study protocol designed by neurologists and psychologists. With this present study we wanted to specifically address the patient perspective.
Methods:
Together with affected individuals, family members, and advocates concerned with RYR1-RD, we developed an online patient survey that was completed by 227 patients or their parents/other caretakers (143 females and 84 males, 0–85 years). We invited 12 individuals, representing most of the patient group based on age, sex, race, and type and severity of diagnosis, to share their personal experiences on living with a RYR1-RD during an international workshop in July 2022. Data were analyzed through a mixed-methods approach, employing both a quantitative analysis of the survey results and a qualitative analysis of the testimonials.
Results:
Data obtained from the combined quantitative and qualitative analyses provide important insights on six topics: 1) Diagnosis; 2) Symptoms and impact of the condition; 3) Physical activity; 4) Treatment; 5) Clinical research and studies; and 6) Expectations.
Conclusions:
Together, this study provides a unique patient perspective on the RYR1-RD spectrum, associated disease impact, suitable physical activities and expectations of future treatments and trials, and thus, offers an essential contribution to future research.
INTRODUCTION
Pathogenic variants of RYR1, the gene encoding the principal sarcoplasmic reticulum (SR) calcium release channel (RyR1) with a crucial role in excitation-contraction coupling (ECC), are one of the most common genetic causes of non-dystrophic neuromuscular disorders. RYR1 pathogenic variants give rise to a wide variety of RYR1-related diseases (RYR1-RD) presenting throughout life, ranging from early-onset congenital myopathies to episodic manifestations in adulthood including malignant hyperthermia during anesthesia and exertional rhabdomyolysis on otherwise largely healthy individuals [1, 2]. This wide RYR1-associated clinical spectrum is due to the highly variable functional impact of different RYR1 pathogenic variants, mode of inheritance, as well as type and location of specific mutations.
We recently conducted a questionnaire study focusing on functional impairments, fatigue and quality of life (QoL) in Dutch patients exhibiting the entire clinical spectrum of RYR1-RD [3]. We could demonstrate that both permanent and episodic RYR1-RD are associated with a substantial disease impact, characterized by functional limitations and severe fatigue, resulting in significant loss of QoL. The results of this study raised awareness and recognition of typical symptoms in individuals affected by RYR1-RD. In addition, the study also improved patient management and defined specific areas in need of further research, particularly concerning the disease impact associated with these common neuromuscular disorders.
The perspective taken in the previous questionnaire study was the distinct medical perspective, reflective of a study protocol designed by neurologists and psychologists. Many clinicians, however, remain largely unaware of the impact of RYR1-RD on the daily life of their patients, and of their expectations towards future treatments. These aspects are gradually becoming a topic of research in other neuromuscular diseases [4, 5], but have not yet been covered in RYR1-RD. To address these issues, members of the RYR-1 Foundation, the international patient association dedicated to RYR1-RD, initiated an online survey in advance of an international scientific and patient workshop dedicated to these conditions. The results of this survey demonstrate the strong patient need to share their firsthand perspectives with the leading international RYR1 experts.
The “RYR-1-Related Diseases International Research Workshop: From Mechanisms to Treatments,” held on July 21 – July 22, 2022 in Pittsburg (PA, USA), was the first-ever patient-led international research workshop devoted exclusively to RYR1-RD [6]. The scientific goal of the workshop was to provide a forum that connects leading international RYR1 disease experts (researchers, clinicians, and geneticists) with affected individuals, family members, and patient advocates to share knowledge, exchange ideas, form collaborations, and develop new strategies for finding effective therapies. Additional objectives were to develop consensus recommendations for clinical/research priorities, to identify actionable items needed to move the field forward, and to provide a platform for trainees to engage with RYR1 patients/family members and established leaders in the field. During this workshop, the study team presented the results of the online survey and invited twelve patients to present their testimonial of living with RYR1. This manuscript describes the results of both the patient survey and the individual testimonials, using a mixed-methods approach; employing a quantitative analysis of the survey, and a qualitative analysis of the testimonials.
METHODS
Study team
The study team that designed and executed the survey consisted of 14 individuals, including affected individuals, family members, and advocates concerned with RYR1-RD. Three of these individuals (DH, BS, JR) participated in virtual meetings of the scientific and medical experts (AS, RD, NV) involved in planning and organizing the international workshop (from November 2021 through June 2022).
Design of online survey
The study team discussed a series of topics, based on what they had heard from different patients in internal discussions within the RYR-1 Foundation, to generate the first set of questions to evaluate and understand the daily challenges faced by individuals living with RYR1-RD. The resulting set of questions was subsequently discussed with the scientific and medical experts to evaluate the most relevant questions and to reach a consensus about the final questions based on clinical importance and relevance. This resulted in an survey of 21 questions covering five different themes: Demographics (1–3); Diagnosis (4–9); Symptoms and impact of the condition (10–12); Physical activity (13–16); and Clinical research and studies (17–21). The complete survey is included as Supplemental data A: Online survey.
This survey used a descriptive cross-sectional design and was available to all individuals with RYR1-RD that met the inclusion criteria through the online survey platform ‘Survey Monkey’. The survey was active from May 9th-June 25th, 2022. The inclusion criteria included: 1) Having received a medical diagnosis of a RYR1-RD; and 2) Being able to understand and write English language. For individuals <5 years old, parents or legal guardians were invited to complete the survey. Individuals between 5–17 years old were invited to involve their parents or legal guardians in answering the questions.
A purposive sampling approach was used, and the sampling frames included: “The RYR-1 Foundation” Facebook (FB), Twitter, and Instagram pages, “ryr1.org”; “RYR-1 Families” FB group; “Living with RYR-1 - Support Group” FB page; “Central Core Disease & Minicore: a place for support, learning & friends” FB page, and The RYR-1 Foundation’s email list. Specific instructions given were: ‘Provide the best guess if you are not completely sure’; and ‘Skip any question you do not want to answer’. Participants were informed that the goal of the survey was to help researchers and experts to further learn about and better understand the impact of living with a RYR1-RD, and to help researchers develop new strategies to identify and assess suitable therapies.
Invitation and instruction for testimonials
Firstly, patients who are member of the RYR-1 Foundation were invited via email. From those who reported being interested and the study team, participants were selected based on age, sex, race, and type and severity of diagnosis to represent a broad range of individuals affected by RYR1-RD. This selection was made by the patients who participated in the study group. A group of 12 individuals who were either directly or indirectly affected by an RYR1-RD were invited to provide brief testimonials (around 7 minutes) during the international workshop that summarize their perspective on what it is like to live with or care for someone with a RYR1-RD. These individuals were instructed to talk about the process of being diagnosed, symptoms and impact of RYR1-RD on their daily life, physical and mental well-being, their past and current treatments and expectations of future research. The participants were encouraged to include specific experiences, concerns, and ideas for researchers and medical experts. The written instruction for the testimonials is added as Supplemental data B: Instruction for testimonials.
Ethical considerations
Information was collected without asking survey respondents to disclose their identity. Consequently, information submitted was not considered protected health information. Hence, the Health Insurance Portability and Accountability Act (WMO) did not need to control the use of this information. Notwithstanding this, the RYR-1 Foundation has maintained strict safeguards to protect patient information from use or disclosure that is not consistent with its goals. Furthermore, the authors performed data acquisition, analysis, interpretation, and publication in line with the good clinical practice guidelines of Radboud university medical center. Finally, the Radboud Research Ethics Committee deemed this research not subject to the WMO (2024-17388).
Data storage and analysis
Quantitative data. Data from the survey were stored anonymously in an Excel file, and subsequently transferred to SPSS. Descriptive statistics were predominantly used to characterize the data (SPSS version 27, IBM, Armonk, New York). Graphs were prepared in Graphpad Prism software version 9.5.0 (Graphpad Software, San Diego, CA, USA). Spearman’s rho tests were used to assess the relation between symptoms, between ambulation status and symptoms, age of diagnosis and symptoms, and ambulation status and exercise frequency. The participants were also divided into two age groups to compare children to adults (age up to 17 and ≥18 years old). A Bonferroni correction was applied to counteract multiple comparisons between the different groups of RYR1-RD diseases. One-way ANOVA’s were used to compare the different RYR1-RD with regards to the number and type of physical and psychological symptoms.
Qualitative data. Patients presenting their testimonials were pseudo-anonymized: in the transcripts and analysis, only participant numbers were used. We collected demographic data of participants including age, sex, diagnosis, and role in patient community (patient/parent/another caregiver). All testimonials were audio-recorded. Testimonials that were only verbally presented (n = 9/12) were fully transcribed. All written testimonials were supplemented with additional information from the recordings. Both the written and fully transcribed testimonials were uploaded to Atlas-ti version 8.1 software and analyzed using a thematic analysis [7, 8]. Thematic analysis is a method for identifying, analyzing and reporting themes within the data [9]. Two researchers (LS and NV) independently analyzed the data through a process of inductive comparison and reasoning, starting from the data and the aim and not of preexisting theories. This aim was to get a better understanding of the life of a patient affected with a RYR1-RD, and expectations and wishes towards the future. The two researchers independently searched for the basic units of meaning by segmenting the data and giving these segments conceptual labels which were closely related to the participants’ words (open coding). Both authors compared and discussed these codes until they reached consensus. Next, they identified relations between the open codes and grouped those codes referring to the same phenomenon into categories (axial coding).
The categories were partly overlapping with the themes from survey: Diagnosis; Symptoms and impact of the condition; Treatment, and Expectations. For the main themes, subthemes were created (life before diagnosis, diagnosis, symptoms, effect on physical functioning, effect on daily life, effect on mental health, treatment, expectations, and gaining knowledge) and with three researchers (LS, SC, NV) the most meaningful quotes were selected per subtheme that best represented the themes.
RESULTS
A concise summary of the survey results and the testimonials were included in the workshop report [6]. We here present the full dataset, starting with the quantitative data followed by qualitative data on the following themes: 1) Diagnosis; 2) Symptoms and impact of the condition; 3) Physical activity; 4) Treatment; 5) Clinical research and studies, and 6) Expectations. Themes 1 and 2 were discussed in both the survey and testimonial. Theme 3 and 5 were only discussed in the survey and theme 4 and 6 only in the testimonials. In the testimonials, all themes were divided into different key aspects.
Responses
Survey The survey was completed by 227 patients, parents or other caretakers (143 females and 84 males). For the questions that were not completed by all the participants, it is indicated how many patients completed the questions. Participant ages ranged from 1 to 85 years with a mean age of 37±21 years old.
Testimonials 12 testimonials were presented during the workshop. Nine of these were provided as written text and complemented with the audio recording, and the other three were only available as audio recording and fully transcribed. The demographics of the participants providing the testimonials are presented in Table 1. The qualitative analysis resulted in the selection of 215 quotes, reflecting the four main themes (Table 2).
Table 1
Demographics of the participants that presented their testimonial at the RYR-1-Related Diseases International Research Workshop: From Mechanisms to Treatments (Pittsburgh, USA, July 2022)
| Participant/ | Current age | Age at | Age at | Sex | Race | Geographic | Diagnosis |
| testimonial | (yrs old) | onset | diagnosis | location | |||
| number** | (yrs old) | ||||||
| 1 | 65 | 57 | 61 | M | White | USA | MHS |
| 2 | 67 | Birth | 25 | F | White | USA | CCD |
| 3 | 41 | Birth | 33 | M | White | USA | CNM |
| 4 | 12* | Birth | 8 months | M | White | USA | Recessive RYR1-RD |
| 5 | 45 | Birth | 17 | F | White | Canada | CCD, MHS |
| 6 | 28 | Birth | 22 | F | Black | USA | CCD, MmD |
| 7 | 80 | Birth | 27 | F | White | USA | CCD |
| 8 | 59 | Birth | 44 | M | White | Brazil | CNM |
| 9 | 18 | Birth | 4 | F | White | USA | RYR1-RD (de novo) |
| 10 | 35 | Birth | <1 | M | White | USA | CCD |
| 11 | 40 | Childhood | 37 | M | White | USA | RYR1-RD |
| 12 | 11* | Birth | 5 | M | White | USA | RYR1-RD (de novo) |
*Testimonial was provided by the mother of the patient. **These numbers correspond to the patient numbers in the tables with quotes from the testimonials.
Table 2
Number of quotes in the different themes
| Theme | Number of quotes | |
| Diagnosis | 50 | |
| Life before the diagnosis | 14 | |
| Diagnosis | 36 | |
| Symptoms and impact of the condition | 108 | |
| Symptoms | 23 | |
| Effect on physical functioning | 28 | |
| Effect on daily life | 38 | |
| Effect on mental health | 19 | |
| Treatment | 19 | |
| Treatment | 19 | |
| Expectations | 38 | |
| Expectations | 22 | |
| Gaining knowledge | 16 | |
| Total | 215 | |
Below we describe the survey results followed by the results from the testimonials according to the main themes of each data collection tool as explained in the methods section. Numbers of patients and percentages are reported from the survey. Cases where not all participants responded to a specific question are explicitly indicated.
Diagnosis
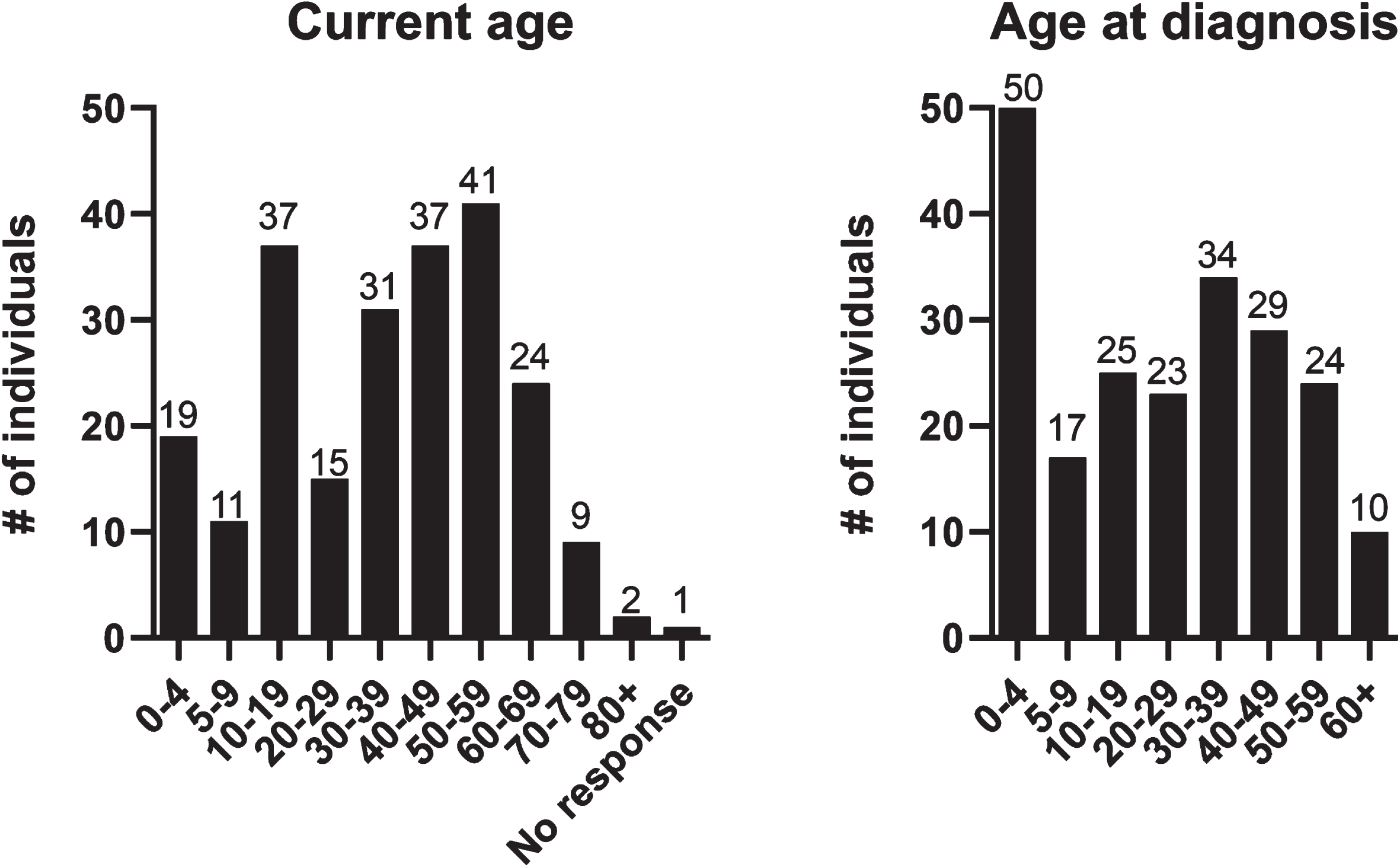
Survey results The diagnosis section of the survey consisted of six questions. Age of the respondents at diagnosis was variable, ranging from 1 to >60 years. 22% of the participants stated that they were diagnosed with RYR1-RD before 5 years of age (Fig. 1). Patients were diagnosed either by genetic testing only (n = 99/227, 44%), by both muscle biopsy and genetic testing (n = 85/227, 37%), or by muscle biopsy only (n = 28/227, 12%). In a small subset of cases, the diagnosis was presumed based on the phenotype and the presence of an affected first degree relative with a confirmed diagnosis of a RYR1-RD (n = 6/227, 3%). Eight patients (4%) indicated other combinations of the above-mentioned modes of diagnosis and one patient did not indicate the mode of diagnosis.
Fig. 1
The current age and the age at diagnosis. The y-axis depicts the number of patients for each age group. These histograms show the wide range of the current age of participants and the age at diagnosis.
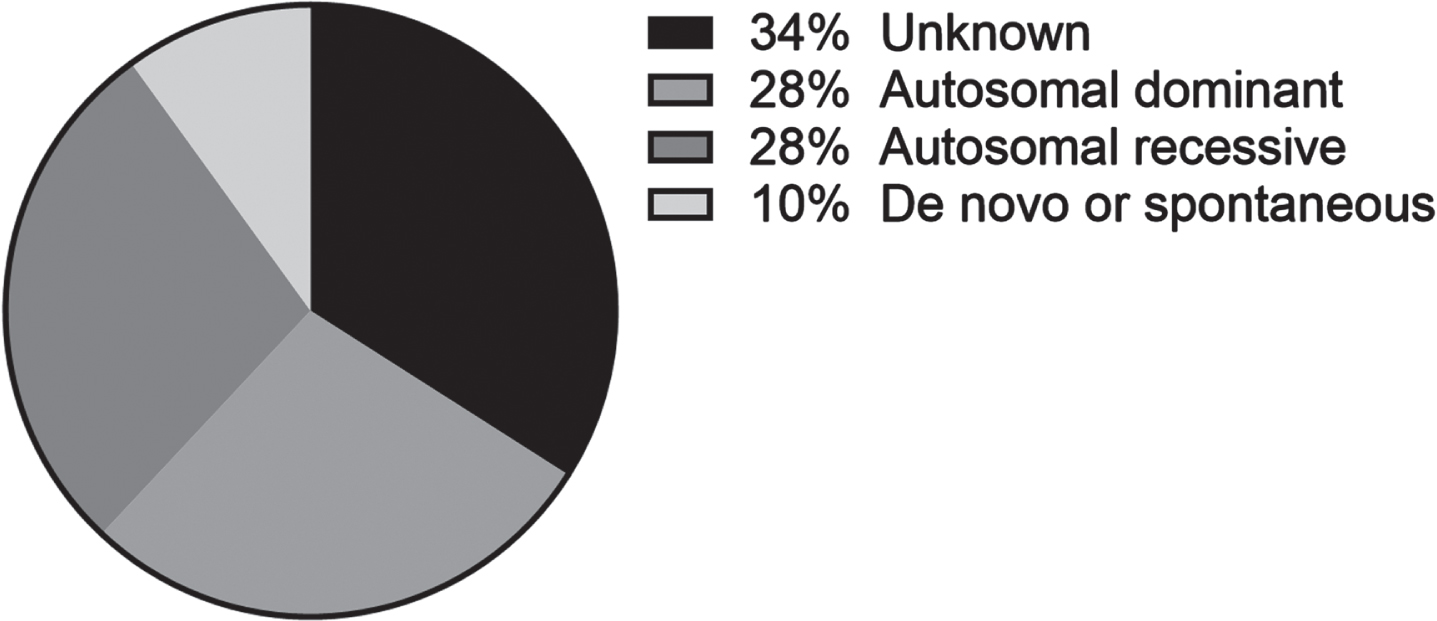
There was a wide range of RYR1-RD, with Central Core Disease (CCD) being most common (n = 92/173, 53%). Malignant Hyperthermia Susceptibility (MHS) (n = 29/173, 17%), Centronuclear Myopathy (CNM) (n = 10/173, 6%), Congenital Fiber Type Disproportion (CFTD) (n = 9/173, 5%), and Multi-minicore Disease (MmD) (n = 6/173, 3%) were other, but less frequent, diagnoses. 18 participants indicated ‘other’ for this question, with explanations of ‘unsure’, ‘unspecified’, or ‘new variant’ (Fig. 2A). Nine patients had a diagnosis of both MHS and a myopathy. Inheritance was autosomal dominant (AD) (n = 61/215, 28%), autosomal recessive (AR) (n = 59/215, 27%), or de novo or spontaneous (n = 21/215, 10%). Many of the participants reported not knowing the mode of inheritance (n = 74/215; 34%) (Fig. 2B).
Participants reported their current physical ability as able to walk unassisted (n = 145/223, 65%), able to walk with assistance (n = 27/223, 12%), require wheelchair assistance (n = 13/223, 6%), and require full-time use of a wheelchair (n = 38/223, 17%). Patients with an AR or de novo mutation more often required full-time wheelchair use (30.5% and 38% respectively, vs 5%, p < 0.001). Almost half of the participants considered their symptoms as progressive (n = 107/223, 47%), and one third reported those as stable (n = 77/223, 34%). Others were not able to rate their progression because of comorbidities or variable symptoms.
Fig. 2A
The genotypes of the included patients (N = 173). CCD: central core disease; MHS: malignant hyperthermia susceptibility; Other: unsure, unspecified or new variant; CNM: centronuclear myopathy; CFTD: congenital fibre type disproportion myopathy; MmD: multi-mini core disease. N = 173.
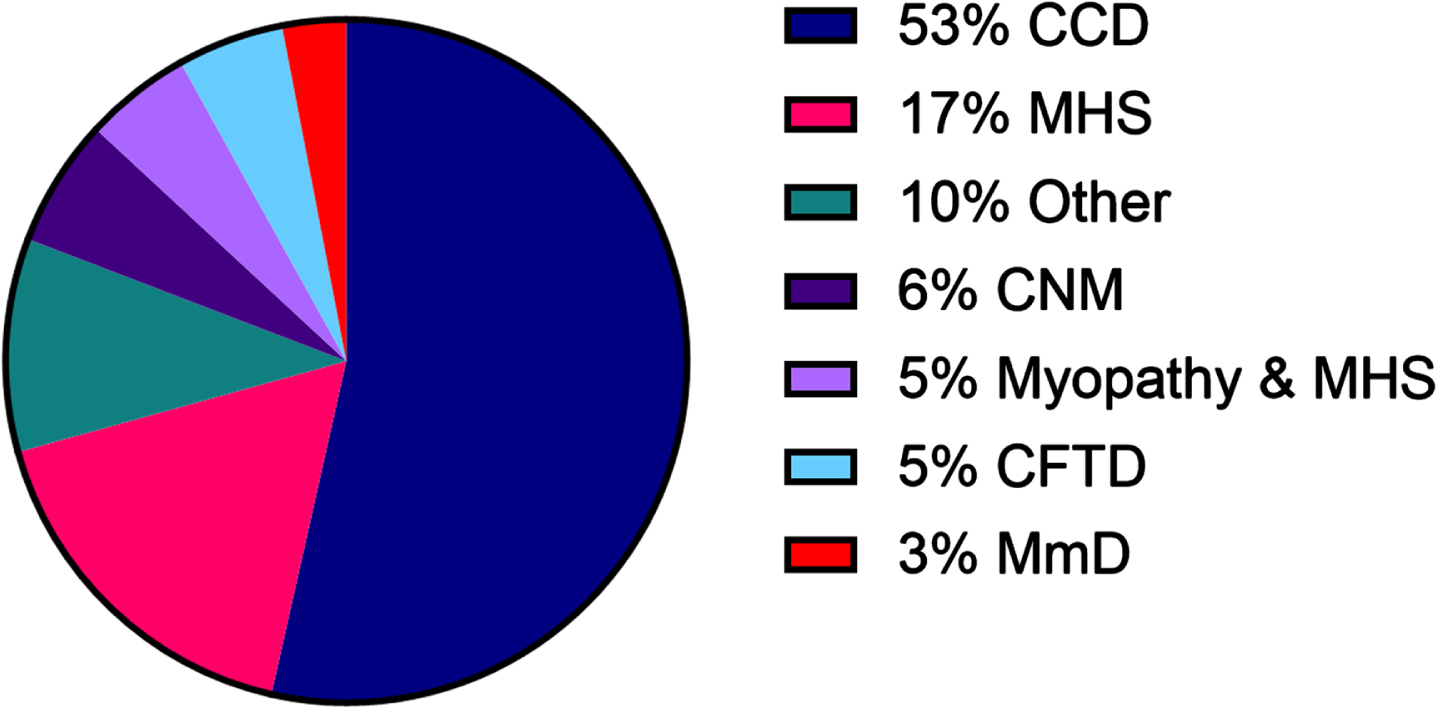
Fig. 2B
The different modes of inheritance of RYR1-RD (N = 215).
Results from the testimonials A total of 50 quotes illustrated the diagnostic process (Table 3). Several individuals mentioned a long diagnostic journey of months to several years, reaching (early) adult life when they were diagnosed, even though the onset of the disease was at birth. Some of these patients received an initial incorrect diagnosis, including mitochondrial disease or Cerebral Palsy, before the correct diagnosis of a RYR1-RD was finally established.
Table 3
Illustrative quotes on diagnosis (from testimonials)
| Key aspect | Quotes |
| Life before diagnosis | ‘To everyone’s surprise, including the doctor, I was born an unresponsive, very “floppy” and very lethargic. I was immediately sent to ICU and the doctors scrambled to figure out what was wrong with me. After 36 hours of no improvement, I was transferred to a specialized neonatal ICU. Failure to thrive, jaundice and breathing problems were all they could diagnose that first week. My mother was told I most likely had Cerebral Palsy. Once proven false, other possible diagnoses included Zellweger Syndrome and Adrenoleukodystrophy.’ – P6 |
| ‘When “C” was born after a normal pregnancy we had no indications that anything was different about him. However, in retrospect there were some early signs that were easy to dismiss initially but made sense later.’ – P12 | |
| ‘Being with him all day I realized that he was not running, jumping, navigating stairs, etc. like his older sister had at that age. While these things were noted during pediatrician visits, it was chalked up to him just being a “late bloomer”; he was almost three by the time I had to push his doctor harder to figure out what might be going on.’ – P12 | |
| Diagnosis | ‘We got her diagnosis when she was eight months old and I think those results took a couple of months to even come back’. – P4 |
| ‘RYR1 goes back at least eight generations in my family. For some of those generations in my family no one had met another affected individual or had a chance to interact the room for scientists and doctors that might just be the ones to find a treatment or cure.’ – P10 | |
| ‘While his myopathy has not been identified as a more specific type such as Central Core Disease, etc. it was a relief to have an answer, even if it is not something that any parent ever wants to hear.’ – P12 | |
| ‘The time we spent figuring out “C’s” diagnosis was difficult and lonely as parents; we didn’t know anyone else in the position that we were of trying to solve this mystery. But now we are part of this community and consider ourselves lucky to have the Foundation and all of you working hard to help us.’ – P12 |
Life before diagnosis. In the 1980 s and 1990 s, little information was known about RYR1-RDs. The pattern of weakness, age of onset, specific symptoms and the severity of symptoms often resulted in a wide differential diagnosis, and muscle biopsies were often required to confirm the diagnosis. In general, patients commented on the difficulty of being diagnosed with a rare disease. Patients underscored the early onset of symptoms including developmental delay, but also how these early signs were often missed or only acknowledged after several years.
Diagnosis. In general, patients mentioned their family history of RYR1-RDs through their parents, siblings, or other family members, going back for generations. They reported an intrafamilial variability of disease severity and the way they experienced their own diagnosis or the diagnosis of their child. One patient mentioned that they had to wait for months to see a neuromuscular specialist and for some patients it took years to be diagnosed. This caused a lot of stress for the patient and their family, mainly because of the associated uncertainty. Parents without a medical education background faced significant challenges in finding the right diagnostic path. Other parents mentioned that they felt lonely since they did not know anyone else with a similar experience. Additionally, these parents expressed how the RYR-1 Foundation and the patient community has helped them. Overall, patients described their diagnostic process as a long journey with many hospital visits, additional testing, and many unanswered questions. One parent mentioned the relief they felt when they finally had an answer to their child’s diagnosis, even though it was not the diagnosis they were hoping to hear. Most of the parents expressed their worries and stress about life going forward after diagnosis as well.
Symptoms and impact of the condition
Survey results This part of the survey consisted of three questions. The first question concerning general symptoms proposed several response options, including among others general muscle weakness, fatigue, and breathing difficulties, with an open option to list other symptoms. Patients were invited to report all symptoms that applied to them. General muscle weakness was most frequently reported (n = 190/227, 84%), followed by leg weakness (n = 185/227, 82%), difficulty running (n = 183/227, 81%), difficulty with stairs and getting up (n = 177/227, 78%), and fatigue (n = 168/227, 74%) (Fig. 3A & B). For the abovementioned symptoms, the MHS group had a significantly lower frequency, except for fatigue, compared to the myopathy group. No differences for these symptoms were found between different age groups (data not shown). There was also no correlation between age of diagnosis and number of symptoms (r(210) = –0.79, p = 0.253).
Fig. 3
Reported symptoms. The percentage of patients per group RYR1-RD divided into A) Muscle weakness and limitations in daily life, B) Various symptoms and C) Non-clinical challenges.
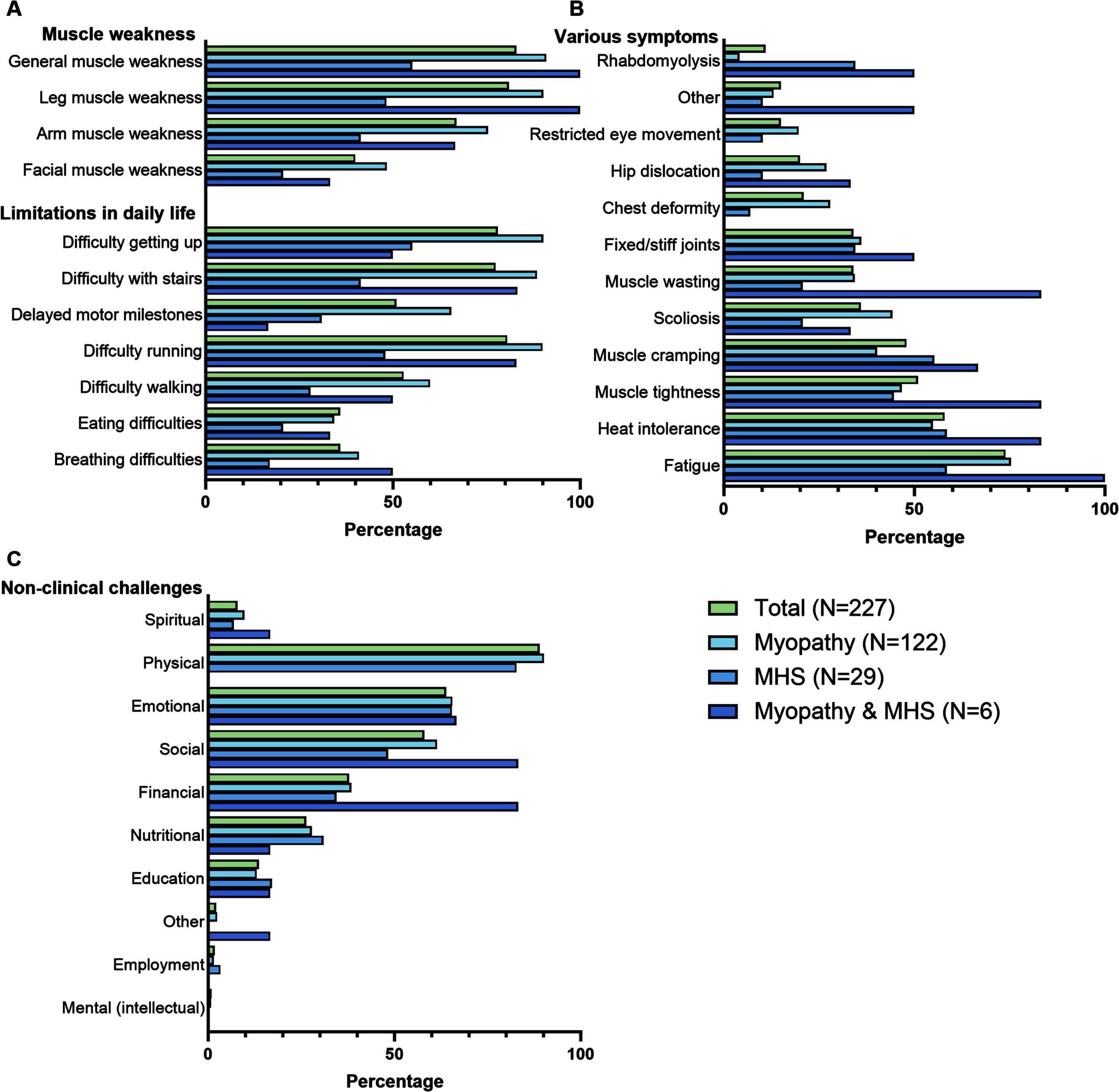
The patients that required full-time use of a wheelchair (n = 38) or walked with assistance (n = 13) had significantly more symptoms than those able to walk unassisted (n = 145) (mean number of symptoms 13.5±3.3 and 11.6±3.8 vs. 9.12±4.2 respectively; p < 0.001). Those who required full-time use of a wheelchair also reported significantly more frequent breathing difficulties than all other mobility groups (0.76±0.43 vs. 0.26±0.44, 0.37±0.49, and 0.31±0.48; p < 0.001). Breathing difficulties did not differ between different RYR1-RD types. Analyzing the difference between males and females resulted in significantly more total number of symptoms for females (10.8±4.1 vs 9.2±4.3; p = 0.004); in particular, females reported generalized muscle weakness more frequently (0.89±0.32 vs 0.75±0.44, p = 0.006). The mode of inheritance did not have an influence on the amount of symptoms. When correlating fatigue with limitations in daily life and muscle weakness, significant associations were found for all those symptoms, except for breathing difficulties and delayed motor milestones, with difficulties running and getting up having the largest correlation with fatigue. However, these associations were poor to fair [10] (Table 4).
Table 4
Correlation between fatigue and physical and non-clinical challenges
| Fatigue (N = 227) | p-value | ||
| Limitations in daily life | Eating difficulties | 0.216* | 0.001 |
| and muscle weakness | Breathing difficulties | 0.174 | 0.009 |
| General muscle weakness | 0.282* | <0.001 | |
| Facial muscle weakness | 0.244* | <0.001 | |
| Muscle weakness in the arms | 0.224* | <0.001 | |
| Muscle weakness in the legs | 0.235* | <0.001 | |
| Delayed motor milestones | 0.149 | 0.025 | |
| Difficulties getting up | 0.315* | <0.001 | |
| Difficulties walking | 0.265* | <0.001 | |
| Difficulties running | 0.319* | <0.001 | |
| Difficulties with stairs | 0.259* | <0.001 | |
| Non-clinical challenges | Social | 0.210* | 0.001 |
| Physical | 0.305* | <0.001 | |
| Education | 0.089 | 0.179 | |
| Mental (intellectual) | 0.056 | 0.402 | |
| Emotional | 0.119 | 0.074 | |
| Total well-being symptoms | 0.287* | <0.001 |
*p < 0.05/17 = 0.003.
The second question of this part of the survey was related to the impact of RYR1-RD on general well-being. The question ‘Does RYR-1 impact your well-being in any of the following areas’ prompted the following responses: ‘physically’ (n = 202/227, 89%), ‘emotionally’ (n = 145/227, 64%), ‘socially’ (n = 132/227, 58%), financially (n = 86/227, 38%), nutritionally (n = 60/227, 26%), educationally (31/227, 12%), and spiritually (n = 18/227, 7%) (Fig. 3C). In addition, respondents were asked to elaborate to this question with open comments (n = 168/227); examples of each category of these is presented in Table 5.
Table 5
Answers from survey participants on the open question on impact of RYR1-RD on various aspects of daily life (from survey)
| Physical | “Heat intolerance causes rapid overheating in warm environments such as small meeting rooms. Minor stress can also cause temperature spikes, excess sweating, and light-headedness” |
| Emotional | “Growing up I never knew why I had muscle weakness, but I always knew I wouldn’t let it define me. I played sports, I exercised, and I always tried to keep my spirits up. Some kids would laugh at me, but it taught me to be a better person, a kinder person. I never let it stop me from becoming a registered nurse and I’m thankful every day for my struggles because I’m better for them. Not every day is this easy to say, but I’m proud of myself.” |
| All | “This question is hard to answer in a “straight to the point” manner. Almost every aspect of my daily life revolves around my disability. Physically it is obvious with the symptoms involved, but what also must be considered with that is exercise, which is extremely limited, and how that affects my health. That plays into nutrition and what I eat, and being at a healthy weight, which can now have a negative impact on body image and emotional wellbeing. My emotional wellbeing and body image is also directly impacted with scoliosis, myotonia, &muscle tightness. I have physical and emotional pain, and grievance over the things I long to do but never can. My social life is dependent on what energy, if any, I must give that day. Financial wellbeing is directly correlated to energy as well. How much do I have to give? Do I put myself in a deficit? Have you ever heard of the Spoon Theory? If not, I’d suggest looking it up. It explains well what I mean.” |
| Physical and emotional | “Being always considered the different one is not easy, even simply going on vacation becomes a business as you must organize yourself to walk a little and avoid the stairs. The biggest difficulty was finding a life partner who accepts my physical condition and my limitations and discomforts.” |
| Financial | “I am denied insurance coverage of many treatments and equipment due to the lack of the insurance’s recognition of RYR-1 RD.” |
No differences were found between the different types of RYR1-RD (myopathy, MHS or both) for the most frequently mentioned non-clinical challenges (physical, emotional, and social) or the total number of non-clinical challenges. When differentiating between the different ambulation statuses, participants who require full-time wheelchair use reported more frequently social manifestations and a greater total number of other non-clinical challenges compared to those able to walk unassisted (0.76±0.43 vs 0.5±0.50; p = 0.017, and 3.9±1.7 vs 2.7±1.6; p < 0.001, respectively). Females more often reported their social well-being as adversely affected compared to male patients (0.64±0.48 vs 0.48±0.50; p = 0.018). Adults more often indicated their emotional well-being to be adversely affected compared to children (0.71±0.46 vs 0.48±0.50; p = 0.001). When assessing the correlation between these symptoms and fatigue, a few significant associations were found (Table 4) with only poor to fair correlations.
Results from the testimonials In total, 108 quotes were identified within this theme, with a selection of quotes presented in Table 6. The most common symptoms that emerged from the patient testimonials were both physical (in particular pain and fatigue) and social/emotional, noting both the physical and mental barriers that RYR1-RD introduced in their life. Many individuals indicated a beneficial effect of regular activity and exercise on their symptoms, while also expressing concerns and uncertainty regarding which types and frequency of activities may be most beneficial, while simultaneously trying to avoid excessive pain and muscle damage. Several individuals inquired about nutritional approaches that might promote muscle health. Others shared approaches that they experienced as beneficial, including supplementation with creatine and magnesium.
Table 6
Illustrative quotes on symptoms and impact of the condition (from testimonials)
| Key aspect | Quotes |
| Symptoms | ‘My therapists noticed the curvature in my spine early on. From the ages of 18 months to 12 years, I’ve been through a series of back braces and casts to treat my scoliosis before my severe S curve forced my spinal fusion in 2005. I’ve had over 14 operations.’ – P6 |
| ‘My symptoms continued to worsen, and my chronic fatigue became overwhelming. I’ve always been hypercapnic, but my CO2 levels became so severe that every morning I’d wake up with the effects of a hangover. Slurred speech, dizziness, and headaches plagued me every morning.’ – P6 | |
| ‘And I mention that I had struggles throughout my life, experienced a lot of leg cramps throughout my early childhood, would wake up to screaming and crying through the middle of the night and you know my mom knew that she had the same problem when she was a child, and we tried to seek numerous doctors to help out with that.’ – P11 | |
| Effect on physical functioning | ‘As a young boy, we realized that ‘T’ could ride his tricycle quite well so we decided to have a custom made tricycle for him as his core source of mobility.’ – P2 |
| ‘I was 3.5 before I was able to walk and when I did walk it was with pronounced limp. I couldn’t run very fast or far. Stairs without a rail were challenging.’ – P5 | |
| ‘I don’t stand up straight or walk without aid. I was unable to pick up my great granddaughter when she was 3 months old. Getting up from a fall would be impossible’ – P7 | |
| ‘During my childhood, even considering my difficulties comparing to other children I was very active, and according to my physical possibilities, I swam, I rode a bike, in short, I played a lot. But over the years I experienced a pattern of slow and steady physical deterioration, such as difficulty in climbing steps, getting up from a chair, maintaining balance, and an increased falling down risk.’ – P8 | |
| ‘When I was younger this meant that I couldn’t play sports with the kids during recess. As a dad sometimes it means I can’t keep up with my kids. Or throw our daughter in the air while playing in the pool. What I would give to be able to do this just once.’ – P10 | |
| Effect on daily life | ‘When I found that I began to avoid doing things or going places because of fatigue or fear of falling, I became open to the idea of using power mobility. I work in a large hospital and wouldn’t be able to continue working without power mobility.’ – P5 |
| ‘My friends assisted me when necessary, but never made me feel inferior to them and I love them for that. I was raised to be as independent as I could and was encouraged to participate in activities with other children even if I needed modifications. My family made sure that I had everything that I needed.’ – P6 | |
| ‘Who I am, who I’ve befriended, who I’ve loved, where I’ve lived, career I’ve chosen, how my children will see me are all intertwined with a little mutation somewhere in my DNA. RYR1 has made me who I am and that’s not necessarily a bad thing.’ – P10 | |
| Effect on mental health | ‘It was not until my mid-twenties that I was ready and mature enough to fully come to terms with this condition. It was then that I began to realize and comprehend it’s a part of who I am but is not how I am defined.’ – P3 |
| ‘While the road has never been easy, I have been very grateful for the many people I have met. I have two amazing parents and some fantastic friends. I have met some tremendous healthcare providers along the way. I must say there is no better feeling that having a healthcare provider as your ally. Someone in your corner, who understands your struggle and is willing to do what they can to assist you. It doesn’t always mean that it is going to work. But believe me that it has made a difference that they are willing to try.’ – P5 | |
| ‘I’ve always felt unstoppable but for the first time I felt somewhat defeated. My mind and my body were battling each other. A part of me wanted to keep going and enjoy life as I knew it, and another part of me kept telling me that it was impossible.’ – P6 | |
| ‘In elementary school I was separated from my peers and I had trouble making friends’ – P9 |
Symptoms. Symptoms of RYR1-RD presented in some patients at birth and developed later in life in others. Congenital symptoms included dislocated hips, fractured legs, and physical difficulties. Additionally, some patients had severe dental malocclusion, requiring jaw surgery. Other patients went through a series of back braces and operations to treat scoliosis. In addition to the physical limitations, non-neuromuscular symptoms like respiratory weakness and chronic fatigue were reported as well. Chewing and/or swallowing difficulties contributed to difficulty in maintaining weight. Being unable to regulate body temperature, suffering from leg cramps, or feeling numb in the legs were additional symptoms mentioned. In some patients, these symptoms continued to worsen over time.
Effect on physical functioning. Overall, patients experienced significant physical difficulties. This was mainly expressed through delayed attainment of motor milestones and muscle weakness. For example, being able to walk independently was a challenge. As patients became older, challenges remained for other physical activities like climbing stairs and/or running. Other difficulties that were mentioned included sitting down, getting up, bending over, tying shoelaces, standing up for a couple of minutes and maintaining balance. The severity in physical functioning varied amongst participants. Many patients reported not having been able to keep up with their peers in childhood or adulthood. Some (grand)parents expressed how they would like to keep up with their (grand)children. Most participants used various tools to cope with their physical struggles. One parent had made a custom tricycle for their child. Additionally, patients used forearm crutches, canes, wheelchairs and chair lifts. While the vast majority of participants shared their experiences with physical inabilities, a few participants mentioned that they had achieved most motor milestones and were still able to live a life without difficulty or much adaption.
Effect on daily life. Participants emphasized the effect of the condition on their daily life and how various symptoms affected their QoL. For example, some participants expressed how fatigue and fear of falling impacted their daily life. While some participants had just enough energy for work, other participants had to retire early due to their condition. The fatigue and pain were also reported as barriers to social participation, being a reason for some participants to avoid going out. One patient explained how there were small things that they were not able to do that would probably be taken for granted by healthy persons/other individuals. For example, being able to walk certain distances, climb a step or flight of stairs and lift heavier objects. Despite their limitations, patients wanted to be independent, and children wanted to keep up with their peers. Most patients mentioned how they can still function independently despite their disease, especially with some modifications, for example by using a (powered) wheelchair. Simultaneously, they also expressed how they required assistance with care and support by others. Patients explained how they were able to go to college, graduate, have a social life, take care of themselves, and feel accomplished and proud. However, patients also recognized how their condition, at least, partly defined them, impacting choices and how they felt they were seen by others. With age, these challenges became more frequent and impactful. For patients, an effective treatment would allow an improvement in daily life and becoming/remaining independent.
Effect on mental health. RYR1-RD impacted both patients and family members, experiencing a long process of accepting the condition. Parents felt lonely and isolated at times, not knowing anyone in a similar position. Some patients talked about the difficulties they faced during their childhood. Patients felt embarrassed, for example, about their scars, and one individual mentioned being bullied because of a back brace. In general, they found it difficult making friends. Family members felt episodes of guilt and had difficulties processing the condition as well. Overall, patients experienced feelings of disappointment, being defeated, and grief. The sense of being different caused feelings of loneliness. Additionally, it was also mentioned how patients felt very grateful for the support they received from family, friends, and healthcare providers. The willingness of healthcare providers to try to understand and assist patients was appreciated. Some patients mentioned how their religion, and the support of family and friends had strengthened them. While one participant explained the difficulty of asking for help, another participant mentioned how friends and family were an encouragement to participate in activities and become independent. Despite the difficulties and impossibilities patients experienced, it was also mentioned how some individuals tried to focus on all the possibilities they have. However, there was a need for professional support for mental health expressed for patients and family members.
Physical activity
Survey results This part consisted of four questions regarding the number and type of physical activity and the experienced strength preservation or improvement. Participants reported the frequency of physical activity as 1-2 times per week (n = 66, 29%), 3-4 times a week (n = 64, 28%), 5-6 times a week (n = 38, 17%), and at least daily (n = 23, 10%). Only 32 patients (14%) did not participate in physical activity or exercise at all. The frequency of physical activity did not differ between the different types of RYR1-RD. For the participants needing wheelchair assistance, a moderately negative correlation was found between amount of exercise and fatigue (r(12) = –0.622, p = 0.023).
A wide range of specific physical activities was reported by 193 patients, including walking (n = 130/193, 67%), physical therapy (n = 63/193, 33%), swimming (n = 53/193, 27%), weight and resistance training (n = 39/193, 20%), and cycling (n = 33/193, 17%). Most patients reported to be able to maintain or improve their strength and/or endurance (n = 94/197, 48%), while 52 patients (26%) experienced no improvement. The other participants (n = 51/197, 26%) indicated they were unsure. Reasons for not participating in sports were ‘I cannot design an exercise routine that works for me’ (23/40, 58%); ’I am concerned for my safety’ (n = 10/40, 25%); ‘I do not believe exercise will maintain or improve my condition’ (n = 9/40, 23%); and ‘I do not have time’ (n = 3/40, 8%).
Table 7
Illustrative quotes on treatment (from testimonials)
| Key aspect | Quotes |
| Treatment | ‘Though I still deal daily with fatigue and struggle with rigorous physical therapy, low dose dantrolene has given me an acceptable quality of life for retirement.’ – P1 |
| ‘I have the opportunity to participate in the NIH Clinical trial of the Rycal drug and I responded really well to it and I didn’t go into that study for myself. I went into it for my son and other people.’ – P11 | |
| ‘You know I’m constantly trying sports nutrition, supplementation as long as I can confirm that it’s a safe supplement try it for myself in hopes that if there’s not a drug out there like right now in the future that by the time my son gets a little bit older, I can help him say he might try this for your muscle cramps. You might try this for your fatigue.’ – P11 |
Treatment
Results from the testimonials In total, 20 quotes on previous and ongoing treatments were identified. A selection of quotes is presented in Table 7.
Currently there is no definitive treatment available for RYR1-RD. However, various therapies were being used to help relieve symptoms. Furthermore, a quarter of the patients reported how they optimized their nutrition and supplementation, for example, by taking creatine powder to promote muscle mass, as well as various vitamins. One MHS patient explained how they used low dose dantrolene and how this had led to an acceptable QoL. Another patient used non-invasive ventilation, allowing for a gain in energy and an overall better mood. Most patients had started some kind of physical therapy. In some cases, this was combined with occupational therapy and speech therapy. One patient mentioned the use of different types of treatment like heat therapy, massage, cupping, but also pain medications to reduce muscle pain and back spasms. Several patients had the opportunity to participate in a clinical drug trial, with an overall positive experience. In general, participants described that while the study drug was not expected to cure the disease, it had been the only option so far to potentially improve their QoL. Additionally, another motivator for participating in a clinical trial or trying various types of supplements was to find an effective treatment for others, especially for parents and their own children.
Clinical research and studies
Survey results The final part of the survey (five questions) covered whether participants would take part in clinical trials and what they thought researchers needed to know about living with a RYR1-RD. The question whether participants would be willing to take part in a clinical trial was largely answered positively (‘definitely participate’ (n = 90/226, 40%), ‘likely to participate’ (n = 102/226, 45%), ‘unlikely to participate’ (n = 22/226, 10%) ‘not participate’ (n = 10/226, 4%). The participants who answered negatively did so mainly out of concerns for impact on daily routine (n = 19/32, 59%), concerns for their safety (n = 16/32, 50%), and lack of belief in a treatment or a cure (n = 2/32, 6%).
With 154 patients responding to ‘what researchers need to know or understand better about living with RYR-1?’ the majority stated many issues other than strictly medical concerns (including pain) patients frequently face in their daily life. Also, participants indicated certain nutritional modifications and medications they thought might help with their symptoms. A selection of the responses to this open question are presented in Table 8. Finally, participant questions for the medical community primarily focused on improvement of physical and emotional well-being (n = 167/210, 80%), relieving everyday symptoms (n = 107/210, 51%), and the impact of environmental factors (n = 129/210, 61%).
Answers on the open question on what researchers need to know or better understand about living with RYR-1 RM (from survey)
| Question | Theme | Quotes |
| What researchers need to know about living with RYR-1 | Optimizing muscle | “Will overusing muscles lead to a long-term breakdown in muscle or just take longer to recover?” |
| “Would be wonderful to know anything that would promote muscle growth.” | ||
| “The profound fatigue and muscle cramps that can manifest at any time; chronic pain is a huge problem.” | ||
| Acute or progressive changes | “What triggers symptoms and how to guard against acute episodes.” | |
| “Progression of the disease, nutrition, medication that might help symptoms.” | ||
| Not just medical symptoms | “That many of the barriers we face are societal, structural, and attitudinal, not just medical.” | |
| Large variation | “The large variation in abilities and symptoms for each person. Each therapy and medical plan needs to be individualized and no patient should be compared to another.” | |
| A lot is still unknown (patients and physicians) | “That RYR1 gene mutation is basically unknown to the medical community and you feel like you’ on an island by yourself. Due to this, you can find yourself doubting that what you have is even real.” | |
| What is the #1 goal of treatment | Diet and exercise | “Programs/exercise plans to help maintain/build muscle for those that can. The usual workout routines I search for online are for more “able-bodied” people. Some people say that you shouldn’t exercise at all. And some people say you should. What is too much and what is not enough. Diet- when overweight what is the safest way to try and lose weight without losing muscle.” |
| Standards of care | “Education for health providers esp. with muscle sensitivity, heat intolerance/use of Dantrolene, surgical management.” | |
| Fatigue and pain | “Any treatments that can help with fatigue and pain. Alternative treatments, supplements or following a certain kind of diet that may be helpful.” | |
| Access to information and support | “Access to the correct equipment and access to information and support.” | |
| Questions for the medical community | Medical experts | “How do I find medical doctors that take this seriously.” |
| “How can I get my medical providers to understand my disorder and life challenges to receive better treatment and get them to document my health issues so that I can get the services, support, and care that I need.” | ||
| Successful strategies | “How could you help my daughter to continue the expensive therapies” | |
| “When physical exercise can trigger an episode how is someone with this condition best able to maintain a minimum level of fitness?” | ||
| “Best ways to maintain range of motion.” | ||
| “How can I let people know, without it being for pity, that this is a real thing that severely limits my life and daily activities? Invisibility is difficult: I don’t look like I have an issue.” | ||
| Aging/progression | “What can I do to improve my overall muscle tone as I age?” | |
| “How has RyR1 myopathies impacted other medical conditions and treatments” | ||
| RYR1 impact | “How do prescriptions (such as a statin) affect my body.” | |
| “Am I at risk for other future conditions as I age.” |
Table 9
Illustrative quotes on expectations (from testimonials)
| Key aspect | Quotes |
| Expectations | ‘That reinforced what I had just learned in NIH, that, Centronuclear Congenital Myopathy was not an unknown field, and made me believe in something I had never thought of before, which is the close existence of a drug to treat or alleviate the effects of the RYR1 related diseases.’ – P8 |
| ‘But as I’ve aged and watched my mom age, I’ve seen the more terrifying side of RYR1. Growing up we were told by our physician that the condition is not progressive or perhaps may progress very slowly. My experience has been different and there are many days that I look feel and function like a man twice my age.’ – P10 | |
| ‘There are moments I dream of what it would be like if a cure were discovered in my lifetime. It’s like those dreams you have been thinking about what you would do if you won the lottery what would it be like to be able to run? What would it be like to be able to join my wife a concert or a party without the fear of being knocked over? What would it be like to be able to chase after our daughter and keep up with her daughter in a park.’ – P10 | |
| Gaining knowledge | ‘Feeling dismissed by the system, I became the proverbial ‘physician heal thyself’. I poured over ryr1 literature for adult presentations, diagnostic options and established experts.’ – P1 |
| ‘Another great thing that happen was being presented to the RYR-1 Foundation, as being an organization with the purpose to bringing together people affected by RYR1 related diseases, promoting exchange of experiences between participants, in addition to supporting scientists working on the development of drugs and treatment.’ – P8 | |
| ‘And I want you to know that there’s a lot of valuable research that’s being done out there. The problem is it’s not getting connected to the patients, there’s not enough being done to get this into practice there’s lots useful things out there.’ – P11 |
Expectations
Results from the testimonials We identified 38 quotes on expectations of natural disease course and developments in research. A selection of quotes is presented in Table 9.
Expectations. Participants shared their thoughts and expectations regarding future treatments. In general, participants hope for an effective treatment, at least slowing down the progression of their disease. Some participants expressed the wish to regain strength, endurance, and the possibility of being able to perform activities like running, climbing stairs, or lifting objects. Other participants emphasized the motivation of helping other patients and families, for example, through participation in clinical trials to further advance the knowledge of the disease while also giving something back to the scientific community. One participant mentioned the wish to advocate for others and being able to get in contact with these patients. Several participants expressed the need for a cure for themselves and future patients to treat symptoms like muscle cramps, fatigue, and ophthalmoparesis. The expectation of decline in function over time was perceived as worrisome. While one participant elaborated on their experienced disease progression, another participant mentioned the fear as a parent with an affected child and the possible challenges for the future.
Gaining knowledge. Participants emphasized the importance of gaining knowledge about the condition and possible treatments. Most participants conducted their own search for information, mainly out of curiosity, but also due to a lack of sufficient information provided by their healthcare providers. Additionally, one participant mentioned the importance of comprehensive information, especially for people with a non-scientific background and due to the large amount of available information. Most participants expressed how much the diagnosis has meant for them, even with the absence of a cure. Simultaneously, participants also elaborated on the access to support. An understanding of the disease and knowing that research is being conducted was deemed impactful. Being able to meet people with a similar diagnosis and similar challenges was helpful as well. Participants had contact with others through social media, e-mail, and video calls. It was important for patients and family members to meet their peers and to be able to relate to other people. The crucial role of the patient organization was mentioned here as well, mainly by providing access to information, addressing the challenges, and connecting people. Finally, many individuals expressed their sincere gratitude for the work of the clinicians and researchers in the field, while also encouraging them to continue to make progress in therapy development.
DISCUSSION
Through the survey conducted in this study, we collected views of patients with a wide range of RYR1-RD (n = 227). The results show that individuals of all ages are affected by RYR1-RD, and that the age at diagnosis varies widely. Patients with a myopathy were diagnosed earlier than those with MHS (median of 18.5 and 29.0, respectively). Most patients, both with a myopathy and MHS, were ambulant, and approximately half of the participants considered their disease progressive. Based on the survey results and 12 testimonials, patients reported a large impact of RYR1-RD on their lives. Most survey respondents reported being engaged in regular physical activity or exercise, half of whom had experienced improvement of strength and/or endurance. Finally, most patients were willing to consider participation in future clinical trials.
When reflecting on these findings, we note that the reported types of RYR1-RD are similar to those reported in previous publications in the field, with CCD and MHS being the most prevalent [1, 2]. However, this study provides the most comprehensive patient perspective to date on the wide impact of RYR1-RD on daily life, providing unique and important insights for future consideration. Participants reported multiple domains of daily life influenced by their disease: physical, social, emotional, and less frequently, financial, nutritional, and spiritual. Only 8% of participants reported that the RYR1-RD did not impact their overall well-being. These findings are in line with a recent study on the health-related QoL in individuals affected with RYR1-RD [11]. The most valuable domains revealed by the qualitative analyses of this study were the importance of social impacts, the development of coping strategies, both physical and psychological, and the identification of fatigue and weakness as key symptoms.
The findings support previous observations from a questionnaire study in Dutch patients with RYR1-RD, demonstrating substantial functional impairments and chronic fatigue compared to healthy controls [3]. As expected, we found that, fatigue, pain, and associated physical and social difficulties were more pronounced in individuals with RYR1-related congenital myopathies compared to individuals with MHS. Emotional well-being was more impacted in adults than in children. Children were generally diagnosed at an earlier age, most likely owing to recent increased scientific and medical knowledge on RYR1-RD. Most adults remember only knowing something was wrong when they were young, but not what it was and how to deal with it. For most adult patients, their diagnosis was a long tortuous journey that took many years that also significantly impacted other family members.
Furthermore, our results showed a low correlation between fatigue and several other symptoms such as muscle weakness. However, fatigue resulted in a significant burden on their daily lives. Fatigue is influenced by several factors, directly or indirectly [12]. Therefore, the separate correlations can be low but the impact on fatigue high. We concluded that relatively mild cases of the RYR1-RD clinical spectrum are nevertheless associated with severe fatigue and functional limitations, resulting in substantial loss of QoL [3]. For example, the daily burden experienced by individuals with MHS was confirmed in our recent cross-sectional study showing a high prevalence of neuromuscular symptoms such as myalgia, muscle cramps and fatigue, resulting in frequent medical consultations to identify the cause of these symptoms [13]. Consistent with this, the combination of neuromuscular and non-neuromuscular symptoms occasionally worsening over time was described in the testimonials by some patients.
Patients with RYR1-RD reported to be physically active, frequently engaging in walking, cycling, physical therapy, and swimming or water aerobics, with no difference in frequency in training between individuals with different types of RYR1-RD. Remarkably, weight or resistance training was also reported by 17% of all patients, activities not usually recommended for individuals with myopathies [14–16]. A wide range of other physical activities and sports were reported, including horseback riding, yoga and Pilates. Difficulties finding a suitable form of exercise or concerns for safety were reported as specific barriers to participation in physical activities. Thus, guidance regarding recommended forms of exercise, physical therapy and training could be added to the recently developed clinical care guidelines developed by the RYR-1 Foundation [17]. Patients were found to make use of various tools to cope with their physical struggles. Physical function differed amongst the patients, and some expressed how they felt like they could still live a life without difficulty or much adaptation. However, the loss of strength and endurance over time can be a significant barrier to several types of activities. Patients were aware of the emotional impact of their disease, and thus, need resources to help them cope with these feelings, something especially experienced by parents. A similar mix of emotional responses was also reported in the testimonials. Although some patients mentioned challenging emotional aspects associated with living with a RYR1-RD, the support from family, friends and healthcare providers has helped them to cope with these feelings.
Finally, this study also offered a very helpful and unique patient perspective on future clinical trials. Most participants indicated that they were (likely) willing to participate, with the main barriers to participation being the anticipated impact on daily life activities and safety concerns. This information is important as the patient perspective and consideration of potential barriers for participation is highly relevant for clinical trial design and increasingly being considered. While perspectives have already been provided by patient advocacy groups for spinal muscular atrophy [5, 18], this valuable input is still lacking for many other neuromuscular conditions. Some participants also reported on their experiences related to ongoing or completed clinical trials. Future research should focus on the patient perspective towards therapeutic expectations and clinical trial design, which could significantly improve recruitment, retention, and study outcomes [5].
This study has several limitations. First, as participation in the survey was anonymous, diagnosis was reported by patients and could not be independently verified by the clinicians who had diagnosed them. This was a deliberate choice of the patients who initiated this survey to reduce ascertainment bias by not limiting participation to individuals with recent contact with medical care professionals. Second, the study design includes an ascertainment bias to individuals with access to internet and who were informed about the RYR-1 Foundation and its activities. Third, the survey consisted of customized questions only. The researchers had considered adding validated questionnaires on functional abilities or fatigue, but deliberately chose not to do so and to focus on the questions raised by the patient community. Being a non-validated questionnaire, the formulations of certain questions might have led to different interpretations, possibly impacting the results. For example, it was expected that breathing difficulties were more frequent for patients with a congenital myopathy compared to MHS. However, this was not found in the survey results, which could reflect different interpretations by participants of what constitutes breathing difficulties. If a question about the participants’ well-being does not reveal a particular problem, it does not necessarily mean that the specific well-being aspect is not different compared to individuals without an underlying myopathy or RYR1-RD. For example, if participants made alterations to their school program, their educational well-being might be like that of individuals without an underlying myopathy or RYR1-RD because they can go to school as they see fit. However, the questions used in this survey provide a general idea of how participants are impacted by their disease. Finally, the survey was only available in English, which may have resulted in a study population that is not globally representative.
An important strength of this study is that the survey was performed as a collaborative effort between the patient community, a patient advocate organization (RYR-1 Foundation), and clinician-researchers. The questions covered are topics that are important for the patient community. The design and execution of the survey, as well as presentation of the survey results and patients’ testimonials during the workshop, were supported and facilitated by the RYR-1 Foundation and results quantitatively and qualitatively evaluated in consultation with academic researchers. Nevertheless, this study was primarily driven by RYR1-RD patients and families, which resulted in robust participation, an aspect whose importance is increasingly recognized by both regulatory and reimbursement authorities.
In conclusion, this study provides a unique patient perspective on the diagnostic journey, disease impact, psychosocial challenges, physical activities, as well as patient expectations for future treatments and clinical trials of individuals with RYR1-RD.
ACKNOWLEDGMENTS
The authors would like to thank the RYR-1 Foundation Study team that designed and executed the study and all participants of this study for their time to complete the survey and for sharing their testimonials. Several authors of this publication are members of the Netherlands Neuromuscular Center (NL-NMD) and the European Reference Network for rare neuromuscular diseases (EURO-NMD).
FUNDING
This work was financially supported by the Princes Beatrix Fund (Grant number W.OR22-10) and the National Institutes of Health (Grant number AR078000).
CONFLICT OF INTEREST
Heinz Jungbluth is an Editorial Board member of this journal, but was not involved in the peer-review process nor had access to any information regarding its peer review.
The other authors report no further conflicts of interest.
DATA AVAILABILITY
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
SUPPLEMENTARY MATERIALS
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JND-240029.
REFERENCES
[1] | Snoeck M , van Engelen BG , Küsters B , Lammens M , Meijer R , Molenaar JP , et al. RYR1-related myopathies: A wide spectrum of phenotypes throughout life. Eur J Neurol. (2015) ;22: (7):1094–112. |
[2] | Lawal TA , Todd JJ , Meilleur KG . Ryanodine receptor 1-related myopathies: Diagnostic and therapeutic approaches. Neurotherapeutics. (2018) ;15: (4):885–99. |
[3] | van Ruitenbeek E , Custers JAE , Verhaak C , Snoeck M , Erasmus CE , Kamsteeg EJ , et al. Functional impairments,fatigue and quality of life in RYR1-related myopathies: A questionnaire study. Neuromuscul Disord. (2019) ;29: (1):30–8. |
[4] | Ramos-Platt L , Elman L , Shieh PB . Experience and perspectives in the US on the evolving treatment landscape inspinal muscular atrophy. Int J Gen Med. (2022) ;15: , 7341–53. |
[5] | Gusset N , Stalens C , Stumpe E , Klouvi L , Mejat A , Ouillade MC , de Lemus M . Understanding European patient expectations towards current therapeutic development in spinal muscular atrophy. Neuromuscul Disord. (2021) ;31: (5):419–30. |
[6] | O’Connor TN , van den Bersselaar LR , Chen YS , Nicolau S , Simon B , Huseth A , et al. RYR-1-related diseases international research workshop: From mechanisms to treatments pittsburgh, PA, U.S.A., 21-22 July 2022. J Neuromuscul Dis. (2023) ;10: (1):135–54. |
[7] | Priest H , Roberts P , Woods L . An overview of three different approaches to the interpretation of qualitativedata. Part 1: Theoretical issues. Nurse Res. (2002) ;10: (1):30–42. |
[8] | Vaismoradi M , Turunen H , Bondas T . Content analysis and thematic analysis: Implications for conducting aqualitative descriptive study. Nurs Health Sci. (2013) ;15: (3):398–405. |
[9] | Braun V , Clarke V . Using thematic analysis in psychology. Qualitative Research in Psychology. (2006) ;3: (2):77–101. |
[10] | Akoglu H . User’s guide to correlation coefficients. Turk J Emerg Med. (2018) ;18: (3):91–3. |
[11] | Capella-Peris C , Cosgrove MM , Chrismer IC , Emile-Backer M , Razaqyar MS , Elliott JS , et al. Mixed methods analysis of Health-Related Quality of Life in ambulant individuals affected with RYR1-related myopathies pre-post-N-acetylcysteine therapy. Qual Life Res. (2020) ;29: (6):1641–53. |
[12] | Kalkman JS , Schillings ML , Zwarts MJ , van Engelen BG , Bleijenberg G . The development of a model of fatigue in neuromuscular disorders: A longitudinal study. J Psychosom Res. (2007) ;62: (5):571–9. |
[13] | van den Bersselaar LR , Jungbluth H , Kruijt N , Kamsteeg E-J , Fernandez-Garcia MA , Treves S , et al. Neuromuscular symptoms in patients with RYR1-related malignant hyperthermia and rhabdomyolysis. Brain Communications. (2022) ;4: (6). |
[14] | Voet NBM . Exercise in neuromuscular disorders: A promising intervention. Acta Myol. (2019) ;38: (4):207–14. |
[15] | Voet NB , van der Kooi EL , van Engelen BG , Geurts AC . Strength training and aerobic exercise training for muscle disease. Cochrane Database Syst Rev. (2019) ;12: (12):Cd003907.. |
[16] | Afridi A , Rathore FA . What are the effects of strength training and aerobic exercise training for muscle disease? - A Cochrane Review summary with commentary. J Rehabil Med. (2021) ;53: (9):jrm00231. |
[17] | RYR1 Foundation. Chapter 9: Physical Activity and Physical Therapy (PT); 2022 [cited 2022 Nov]. Available from: https://ryr1.org/online-resources-category/physical-activity-physical-therapy |
[18] | McGraw S , Qian Y , Henne J , Jarecki J , Hobby K , Yeh WS . A qualitative study of perceptions of meaningful change in spinal muscular atrophy. BMC Neurol. (2017) ;17: (1):68. |




