HAP-PEE: A Danish National Study of Challenges Related to Urinating When Away from Home in Women with Neuromuscular Diseases, Impact on Activity and Participation and Prevalence of Lower Urinary Tract Symptoms
Abstract
Background:
Little is known about the challenges faced by women with a neuromuscular disease (NMD) when having to go to the toilet in other places than home; a topic that is highly important for participation and bladder health.
Objective:
The aim was to investigate whether women with NMD have problems in going to the toilet when not at home, the problems’ impact on their social activities, education, and working life, which strategies they use to manage the problems, and the prevalence of lower urinary tract symptoms (LUTS).
Methods:
A national survey containing questions on type of NMD, mobility, impacts on social activities, education, working life, and bladder health was developed by women with NMD and researchers. LUTS were assessed by the International Consultation on Incontinence Questionnaire Female Lower Urinary Tract Symptoms Modules (ICIQ-FLUTS). Female patients≥12 years (n = 1617) registered at the Danish National Rehabilitation Centre for Neuromuscular Diseases were invited.
Results:
692 women (43%) accepted the invitation; 21% were non-ambulant. 25% of respondents avoided going to the toilet when not at home. One third of respondents experienced that problems in going to the toilet impacted their social life. 43% of respondents refrained from drinking to avoid voiding when not at home, 61% had a low frequency of urinating, 17% had experienced urinary tract infections, and 35% had experienced urine incontinence. Problems were seldom discussed with professionals, only 5% of participants had been referred to neuro-urological evaluation.
Conclusion:
The results highlight the difficulties in urinating faced by women with NMD when not at home and how these difficulties impact functioning, participation, and bladder health. The study illustrates a lack of awareness of the problems in the neuro-urological clinic. It is necessary to address this in clinical practice to provide supportive treatment and solutions that will enable participation for women with NMD.
INTRODUCTION
Neuromuscular diseases (NMD) are a group of hereditary and acquired disorders that affect muscle strength and function. They are caused by dysfunction of the motor unit, involving the motor neurons in the spinal cord, the peripheral nerves, the neuromuscular junction or the muscle [1]. Each neuromuscular disease is rare with a prevalence of 1–10 : 100.000, but when grouped, the prevalence becomes more common with 100–300 : 100.000 [2]. Most NMDs progress throughout life, but the degree of physical impairment depends on the specific type of disorder; some patients never achieve ambulation, some patients loose ambulation, while others are ambulant throughout their lives. A neuromuscular disease affects not only physical but also daily functioning due to impairment caused by the disease and due to factors such as lack of accessibility, assistive devices, and/or assistance. Going to the toilet can be bothersome and limiting for people with impaired muscle strength when they are away from home. People who cannot transfer to and from a standard toilet have adapted toilet facilities in their homes and/or a practical assistant to provide supportive care in toilet situations. Leaving home can be problematic due to lack of accessible toilets; a reality that particularly applies to women as non-ambulant men do not have to transfer from their wheelchair to a toilet because they can use a portable urinal. Consequently, there is an increased risk that women with problems accessing a toilet will either prefer to stay at home or avoid emptying their bladder sufficiently throughout the day. This may lead to complications such as incontinence due to overflow from an over-distended bladder, repeated urinary tract infections, or sensory affection because of reduced or no intake of fluids during the day [3–5]. In addition to these profound health risks, women with NMD are at risk of social impairment, isolation, and reduced quality of life (QoL) due to inadequate access to toilet facilities. They may opt out of social activities and/or find it difficult to attend to their studies or jobs [6]. The inadequate access to toilet facilities severely impacts women with NMDs’ possibilities for participation as defined in the international classification of functioning (ICF) [7], and conflicts with the United Nations Sustainable Development Goal no. 6.2 which, among other things, aims to “achieve access to adequate and equitable sanitation and hygiene for all and end open defecation, paying special attention to the needs of women and girls and those in vulnerable situations”[8]. Only few studies have examined problems related to urologic sequalae in people with NMD and mainly in men. A study on 56 men with Becker muscular dystrophy (BMD) and Duchenne muscular dystrophy (DMD) found that LUTS are common and recommend that this should be addressed to improve QoL [9]. A review of 25 patients (8 women) with muscular dystrophy and spinal muscular atrophy found that urological complaints were typically related to functional incontinence among patients with NMD, whereas nephrolithiasis and urinary retention were more common in the spinal muscular atrophy group [10], and an evaluation of LUTS in people with CMT found that urinary symptoms were higher than controls [11]. Few studies have examined the impact on quality of life or participation [12]. NMD is not addressed in the EAU guidelines on neuro-urology which emphasizes the lack of knowledge on the subject [13]. There is a dearth of literature regarding the prevalence of neuro-urological problems in women with NMD, evidence-based care, biosocial factors, and health related consequences related to this area. A network for women with NMD under the Danish Muscular Dystrophy Organization called for more research on the subject. They had experienced that problems with not being able to urinate when they had to were persisting and not sufficiently addressed by the community and the health system. Thus, we found there was an emerging need to increase awareness and identify unmet needs in women with NMD.
AIM
The overall aim of this study was to investigate whether women with NMD have problems in going to the toilet when not at home, the problems’ impact on social activities, education, and work life, and the kind of strategies used to manage the problems. Secondary aims were to assess to which extent women with NMD experience bladder health problems, such as cystitis and lower urinary tract symptoms (LUTS) and the problems’ perceived impact on QoL.
MATERIAL AND METHODS
Study design
A national online questionnaire survey.
Setting
The National Danish Rehabilitation Centre for Neuromuscular Diseases (RCFM) [14] is recognized by the Danish Ministry of Health as a highly specialized hospital for neuromuscular rehabilitation. More than 3500 people with NMD are registered with the Centre which is most of the patients with NMD in Denmark. The study group is a collaboration between researchers at RCFM, the Department of Urology at Aarhus University Hospital, and three women with NMD from the Danish Muscular Dystrophy organization.
The study was approved by the local ethics committee (1-10-72-1-20).
Participants
Participants were recruited from RCFM’s patient database. At the end of October 2021, an invitation to participate in the study was sent to all female patients≥12 years of age registered with RCFM (n = 1617). The invitation was sent by means of a secure digital mailbox (“e-Boks”) used by nearly 90% of the Danish population aged 15 and above. Patients aged 12–14 were invited through their parents’ e-Boks; parents of patients aged 15–17 received a copy of their child’s invitation in their e-Boks’. Patients without an e-Boks were invited by email (n = 33). The invitation letter contained information about the study and a link to the survey. Patients were informed that their responses were anonymous and non-traceable and that they accepted participation by activating the link to the survey. Information about the study was also posted on the websites and social media of RCFM’s and the Danish Muscular Dystrophy Organization. After one month, patients received a reminder in their “e-Boks”, and information on the study was once again posted on websites and social media. The International Classification of Functioning, Disability and Health (ICF) was used as a framework for the study, as we wanted to illuminate influence on all areas of functioning (body, activities, and participation) [15].
Questionnaire
The questionnaire was set up in SurveyXact®, an online secure survey platform (Ramboll Denmark), and developed by the study group based on the results from three semi-structured focus group-interviews (in review elsewhere) [16] with ambulant and non-ambulant women with NMD. The aim of the focus-group-interviews were to identify problem areas in relation to urinating when not at home and to target questions for the questionnaire.
The questionnaire included questions on
• demographics (age, education, work), type of neuromuscular diagnosis (option to tick one of 26 pre-defined diagnoses, or to specify “other diagnosis”).
• level of mobility (climbs stairs, walks independently, walks with assistance, non-ambulant)
• upper limb function, scored by Brooke upper limb scale [17] an ordinal scale in six levels to classify arm function; highest level of function = 1, lowest level = 6
• transfer (with or without assistive devices and assistance)
• in-/dependency when going to the toilet (at home/not at home), time consumption and type of assistance if needed (assistive devices, friend, family, assistant)
• impacts on social activities, education and working life
• strategies to deal with the consequences
• advice from and contact to professionals related to the problem.
The extent of the perceived problem related to the question was rated on a numeric rating scale (NRS) [18] from which the respondent had to choose the number from 0–10 that best reflected the degree of the problem. Several of the questions allowed for elaborating on answers or adding information in an open comment field.
ICIQ-FLUTS questionnaire
The International Consultation on Incontinence Questionnaire – Female Lower Urinary Tract Symptoms (ICIQ-FLUTS) evaluates the presence or absence of LUTS and impact on QoL and is derived from the fully validated Bristol Female Lower Urinary Tract Symptoms questionnaire [19]. The questionnaire has 12 items in three subscales: filling symptoms (n = 4), voiding symptoms (n = 3), and incontinence symptoms (n = 5). Frequency of symptoms is scored from 0 (never) to 4 (all the time) with a supplementary NRS from 0–10 to assess bother (0 = not at all to 10 = a great deal). Bother scores indicate impact of symptoms for the individual patient, and thus the perceived impact on QoL, and are reported as 0≤2 = mild bother; 3≤6 = moderate bother and≥7–10 = severe bother.
STATISTICS
Statistical analyses were conducted using SPSS (IBM SPSS statistics version 26). Descriptive statistics were used to illustrate patient characteristics; mean and range were used for normally distributed variables, median and ranges for not normally distributed variables. Scores on NRS were considered ordinal scores and reported as median and range. Differences between groups (age, ambulation, diagnosis) were calculated by Kruskal-Wallis test. For influence of age, data was divided into three age groups (12–30 y, 31–50 y, and 51 + y), for influence of diagnosis, only diagnoses with > 15 respondents were included. Post hoc tests were used to investigate differences between groups; correlations were calculated by Spearman’s rho. Level of significance was set at p≤0.05.
RESULTS
The questionnaire was sent to 1617 women≥12 years; 751 accepted the invitation and activated the questionnaire; 59 respondents left the questionnaire without answering any of the questions or only the initial questions on age and diagnosis and were excluded due to missing data. Thus, the survey derived from 692 respondents corresponding to a response rate of 43%. The 26 pre-defined neuromuscular diagnoses in the survey met the diagnosis of 91% of the respondents; 8% did not find their diagnosis or did not know the type of their NMD. Mean age was 52.2 years (range 12–89 years); 12% were 12–30 years; 30% were 31–50 years and 58% were≥51 years. The oldest participants were found in the diagnosis groups inclusion-body myocitis (IBM) and amyotrophic lateral sclerosis/primary lateral sclerosis (ALS/PLS), and the youngest participants were found in the diagnosis groups Pompes/McArdles and congenital myopathy. 79% of respondents were ambulant, 21% were non-ambulant. There was no correlation between age-group and level of mobility (p = 0.343). The number of non-ambulant respondents were highest among participants with spinal muscular atrophy (66%), dystrophies (36%) and ALS/PLS (34%). Diagnosis, age, and mobility level are illustrated in Table 1.
Table 1
Diagnosis, age, and mobility level
| Diagnosis | Number | Mean age (range) | Mobility level (n) 1/2/3/4 |
| Muscular Dystrophy | *159 | 50.4 (15–89) | 50/22/31/56 |
| Charcot Marie Tooth | 132 | 55.3 (16–85) | 72/20/30/10 |
| Myastenia gravis | 80 | 54.0 (12–82) | 55/19/3/1 |
| Myotonic dystrophy type 1 | 79 | 47.4 (18–72) | 47/11/17/4 |
| Amyotrophic lateral sclerosis/ primary lateral sclerosis | 64 | 67.4 (50–82) | 14/5/24/21 |
| Spinal muscular atrophy type 2 and 3 | 44 | 44.6 (19–74) | 10/2/3/29 |
| Congenital myopathy | 27 | 41.4 (16–73) | 12/7/4/4 |
| Inclusion body myositis | 15 | 70.1 (55–79) | 5/0/7/3 |
| Mitochondrial myopathy | 12 | 46.4 (14–74) | 4/3/4/1 |
| Myotonia congenita | 7 | 44.7 (26–67) | 6/1/0/0 |
| Periodic paralysis | 6 | 51.8 (17–75) | 3/1/2/0 |
| Pompes/McArdle** | 3/3 | **30.2 (24–37) | 2/2/2/0 |
| Friedrich ataxia | 5 | 41.6 (21–67) | 0/0/1/4 |
| Other*** | 56 | 49.9 (16–79) | 27/14/6/8 |
| Total | 692 | 52.2 (12–89) | 307/107/134/141 |
*Muscular Dystrophy = facio-scapulo-humeral dystrophy, limb girdle dystrophies, dystrophinopaties, congenital dystrophy. **scores for Pompe/McArdle were calculated as one group. ***other represents 27 patients who could not find their diagnosis in the list of preprinted diagnoses and 29 patients who did not know their diagnosis. Mobility level represents 1 = climbs stairs, 2 = walks independently, 3 = walks with support, 4 = non-ambulant as highest level of function. Note that three persons did not report level of mobility.
Work and education
6% of the respondents were students; 11% had a full-time job; 26% worked part time or on special terms; 52% were pensioners/early pensioners; this was most evident in respondents > 50 years of age of whom 73% were pensioners.
Transferring
Questions on transferring were answered by 687 respondents; it was possible to tick more than one category. A total of 76% could get up from a chair independently, however, 50% needed support from armrests or a fixed piece of furniture during transfers, and 23% needed support from another person during transfers. 12% needed a hoist to transfer, 20% needed assistance to open a door; this included respondents that could climb stairs but had very weak hands.
Arm function
Questions on arm function (Brooke score) were answered by 677 respondents; 74% could lift their arms above the head (Brooke 1 and 2), 13% could lift a cup to the mouth (Brooke 3), 5% could lift their hands to the mouth (Brooke 4), another 5% could not lift their hands but use their fingers (Brooke 5), and three persons had no useful function of their hands (Brooke 6). Brooke scores were significantly associated with mobility (p = 0.029) but not with age (p = 0.204).
Going to the toilet
Questions were answered by 672 respondents; 39% considered going to the toilet when not at home a problem and 35% spent a lot of time and energy planning for toilet visits before going out. NRS scores from participants showed that the perception of the problem was significantly higher in non-ambulant respondents (p = 0.00), but the problem was present across all levels of mobility. 38% reported a need for adaptations in their bathrooms such as handles, armrests, special toilet seat, elevated toilet, and smart toilet. Adaptations were mainly mentioned by non-ambulant respondents and respondents who needed assistance for walking.
When at home, 84% of respondents could use their toilet independently; 16% (mainly non-ambulant) needed assistance; When not at home, the number of respondents that needed assistance for toilet visits increased to 27%. One fifth of them were students or in employment. Of this group, 25% experienced occasional urine incontinence, however, only 7% said that going to the toilet when not at home had consequences for their studies and working life. There could be a need for assistance to transfer to/from the toilet, to lock the door, to dry oneself, to (un)dress and/or to wash hands. In general, the respondents needed more time for toilet visits when away from home. When assistance was needed, it was provided by employed assistants (67%), home care (9%), spouses or family (17%), or friends and others (7%). Many respondents found it difficult to ask for help for toilet visits; this was especially pronounced when assistance was provided by family members or friends, but also respondents using employed assistance/care sometimes found it difficult to ask for help.
Limitations in activities and participation
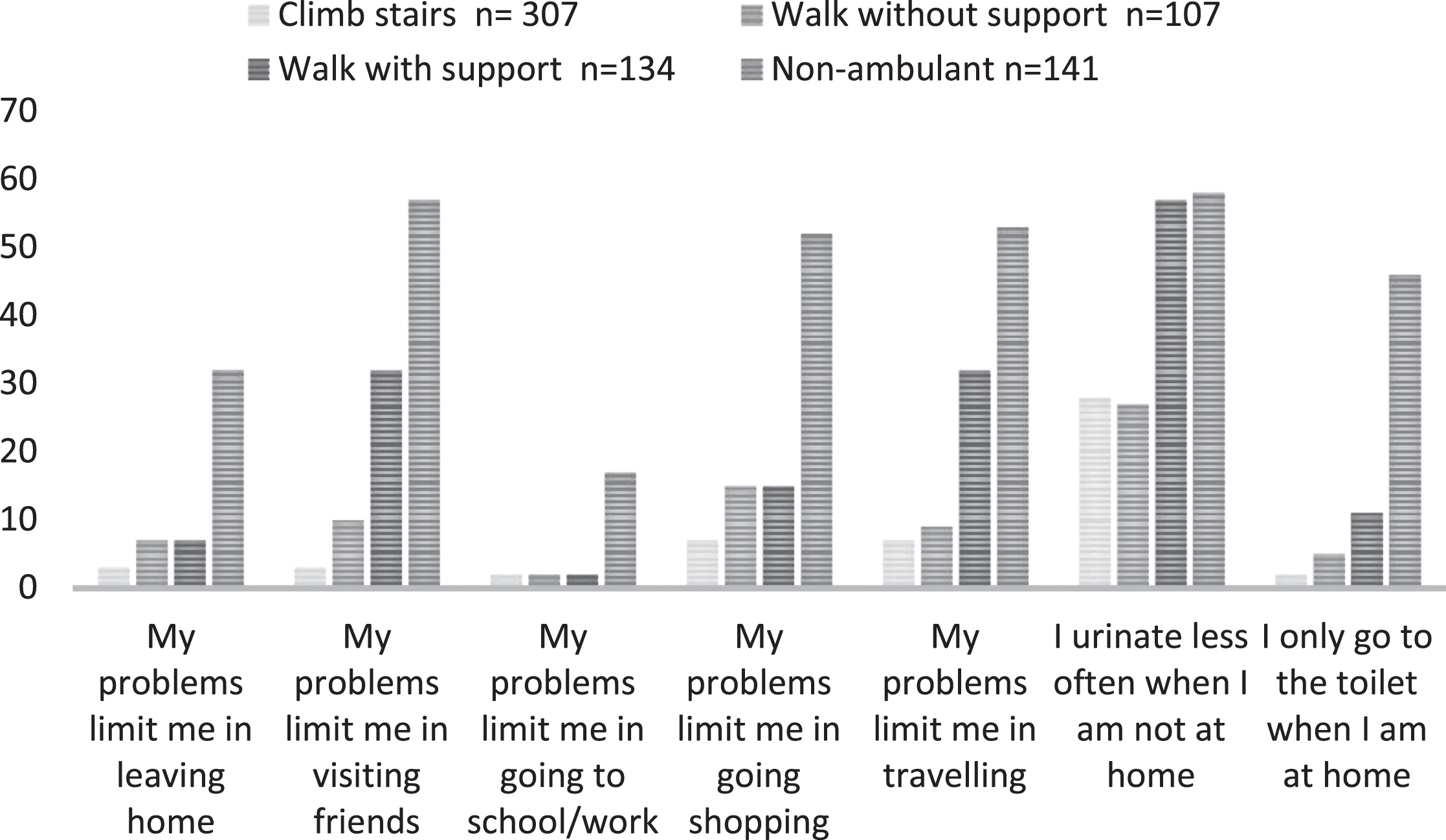
Questions on the perception of being limited in activities and participation were answered by 689 respondents. Overall, limitations were most pronounced in relation to visiting friends, going shopping and/or traveling, activities in which 21–24% of all respondents felt restricted. Being limited was associated with level of mobility (p = 0.000) but not with age (p = 0.280); although limitations in activities were experienced in all mobility groups, this was mostly related to respondents with impaired gait and/or to non-ambulatory respondents (Fig. 1).
Fig. 1
Impact on social activity and participation according to level of mobility. Bars illustrate the percentage of persons who experienced the problem in each of the four levels of mobility.
Biopsychosocial consequences and strategies
Questions on consequences and strategies were answered by 664 respondents. Limitation in fluid intake before going out was a strategy for 43%; holding urine when not at home was a strategy for 39%. Median time for holding one’s urine was four hours (0–22). Although not going to the toilet was related to level of mobility (p = 0.00), more than 25% of respondents who walked independently and climbed stairs also avoided going to the toilet when not at home. One third of the respondents commented on the consequences and strategies caused by problems in going to the toilet; examples are categorized according to ICF and displayed in Table 2.
Table 2
Biopsychosocial consequences due to difficulties in going to the toilet when not at home
| Body | Activities | Participation | Personal reaction |
| – Cystitis. | – Sparse fluid intake. | – Socially handicapped. | – Restricted and sad. |
| – Nervous bladder. | – Travel time must be limited. | – Isolation. | – Stress. |
| – Headache. | – Do not drink/party. | – Going home early. | – Embarrassed. |
| – Fatigue. | – Transfer to the toilet is unsafe/risk of falls. | – Cannot go shopping with my friends. | – Fear of leakage. |
| – Soreness in the skin due to a wet diaper. | – Toilet visits are time- consuming. | – Poor access to toilets. | – Speculations. |
| – Incontinence. | – Must always bring spouse for assistance. | – Cannot attend lectures and concerts. | – I feel left out of the community. |
| – Pain in bladder. | – Have stopped traveling. | – I feel I smell of urine. | |
| – Pain in kidney. | – Spend a lot of time planning toilet visit. | ||
| – Dehydration. |
Impacts are categorized according to the International Classification of Functioning, Disability and Health (ICF).
Lower Urinary tract infections (UTI) and lower urinary tract symptoms (LUTS)
The ICIQ-FLUTS questionnaire was answered by 590 women (85%). 17% of the respondents (n = 101) experienced recurrent urinary tract infections (rUTI) 13% of whom (n = 13) indicated monthly UTIs, and 82% indicated episodes with UTI every three to six months. The frequency of UTIs were associated with level of mobility with significantly more incidents of UTIs among women with lower mobility (p < 0.005). The frequency was not related to age.
Nocturia, defined as≥2 urinary episodes per night [20], was reported by 25% of the respondents. Bladder pain was associated with age (0.008) and mainly allocated to the group of older women. A low frequency of urinating (≤6 times a day) was reported by 61% of the respondents, whereas a high frequency (>8 times per day) was reported by 12%. Frequency was associated with age (p = 0.009), mobility level (p = 0.001), and NMD subtype (p = 0.003). Post-hoc analyses indicated that a higher frequency was related to the group of older respondents, and a lower frequency to non-ambulant respondents; and respondents with spinal muscular atrophy (SMA) or muscular dystrophy.
The experience of hesitancy and straining was the same across all groups, whereas experience of intermittency was associated with increasing age (p = 0.002). More than 50% of the respondents experienced urine leakage 22% of whom experienced leaking from time to time, 21% at least twice a week, 22% daily and 8% several times per day. Urine leak was associated with increasing age (p = 0.000). Urge and stress incontinence was associated with increasing age (p = 0.002) and mobility level (p = 0.001) but not with NMD subtype. Unexplained leakage of urine was associated with increasing age (p = 0.02); enuresis episodes were related to mobility level (p = 0.002) but not to age or subtype. Responses on LUTS are presented in Table 3.
Table 3
Lower urinary tract symptoms measured by ICIQ-FLUTS in 590 respondents
| Filling Symptoms (n/%) | Voiding Symptoms (n/%) | Urinary Incontinence (n/%) | ||||||||||
| Score | Nocturia | Urgency | Bladder | Frequency | Hesitancy | Straining | Intermittency | Urgency | Frequency | Stress | Unexplained | Nocturnal |
| pain | enuresis | |||||||||||
| 0/Never | 218 (36.9) | 91 (15.4) | 411 (69.4) | 360 (61.0) | 365 (61.7) | 406 (68.6) | 369 (62.3) | 234 (39.7) | 235 (39.8) | 258 (43.6) | 445 (75.2) | 502 (84.8) |
| 1 = Occasionally | 224 (38.0) | 325 (54.9) | 149 (25.1) | 146 (24.7) | 173 (12.3) | 147 (24.8) | 172 (29.1) | 262 (44.2) | 176 (29.8) | 242 (40.9) | 110 (18.6) | 61 (10.3) |
| 2 = Sometimes | 95 (16.1) | 76 (12.8) | 22 (3.7) | 55 (9.3) | 29 (31.5) | 19 (1.5) | 29 (4.9) | 58 (9.9) | 73 (12.4) | 37 (6.3) | 17 (2.9) | 14 (2.4) |
| 3 = Most of the time | 38 (6.4) | 34 (5.7) | 6 (1.0) | 16 (2.7) | 16 (2.7) | 12 (2.0) | 14 (2.4) | 26 (4.4) | 76 (12.9) | 33 (5.6) | 7 (1.2) | 4 (0.6) |
| 4 = All of the time | 15 (2.5) | 64 (10.8) | 1 (0.0) | 12 (2.0) | 5 (0.8) | 4 (0.6) | 4 (0.6) | 7 (1.2) | 27 (4.6) | 17 (2.9) | 8 (1.3) | 6 (1.0) |
| Median | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 |
| Range | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) | (0–4) |
Results of bother scores showed that problems with urine leakage during the day, urgency, and bladder pain had the greatest impact on QoL. 33% of the respondents reported a bother score≥3 corresponding to moderate to severe impact on QoL. Bother scores for the twelve FLUTS items are illustrated in Table 4.
Table 4
Lower urinary tract symptoms (LUTS) Impact on QoL
| N (%) | N (%) | N (%) | |
| Mild symptoms (0≤2) | Moderate symptoms (3≤6) | Severe symptoms (≥7–10) | |
| Nocturia | 399 (68) | 130 (22) | 61 (10) |
| Urgency (Hurry) | 324(55) | 118 (20) | 75 (13) |
| Bladder pain | 399 (67) | 97 (16) | 109 (18) |
| Frequency | 426 (72) | 121 (21) | 52 (9) |
| Hesitancy | 501 (85) | 69 (12) | 18 (3) |
| Straining | 514 (87) | 52 (9) | 22 (4) |
| Intermittency | 526 (89) | 47 (8) | 15 (3) |
| Urge urinary incontinence | 387 (66) | 131 (22) | 69 (12) |
| Frequency of urinary incontinence | 397 (68) | 117 (20) | 73 (12) |
| Stress urinary incontinence | 431 ((74) | 94 (16) | 62 (11) |
| Unexplained urinary incontinence | 499 (85) | 49 (8) | 39 (6) |
| Nocturnal enuresis | 539 (91) | 25 (4) | 23 (4) |
ICIQ-FLUTS bother scores for the twelve FLUTS items. Degree of bother is scored from 0 = not at all to 10 = a great deal.
The visibility of the problem among professionals and measures to remedy the problem
Questions about awareness of and approach to the problem among professionals were answered by 649 respondents;15% had discussed their voiding problems with their physician, whereas 48% had not. Only 5% of the respondents (n = 32) had been in contact with a urologist. Of those, 10 respondents were seen in an outpatient clinic every six month, 11 were seen once a year, and 13 every two years.
43% of the respondents had heard of assistive devices or remedies such as catheters (15%), female urine flasks (15%), adapted clothes/pants (16%), and incontinence pads (31%). Information about possible solutions were mainly obtained through the internet, social media, and physical networks. Information about the problem from professionals was sparse; 6% of the participants had heard of the problem and possible solutions from a physician and 10% from another professional.
DISCUSSION
In this study, we illustrate a range of problems women with NMD may experience in going to the toilet when not at home; problems that are burdensome for the individual woman and may have biopsychosocial consequences and impacts on all levels of functioning. Our results indicate that this is an underexposed problem in the clinic.
Our findings demonstrate the many challenges women with NMD face in going to the toilet, which is much more than accessibility, but involves being able to open the toilet door, transferring to and from the toilet, undress/dress, wash hands, etc. While level of mobility is as a predictive factor, our findings demonstrate that problems and consequences are present at all ages and levels of mobility. This is also illustrated by the increase in women who need assistance with toilet visits when they are away from home compared to being at home where necessary adaptations have been made. The fact that 39% of our respondents found it problematic to go to the toilet when not at home is worrying. It is a rather high percentage which illustrates the problem’s negative impact on women with disabilities who, therefore, are unable to participate in society on equal terms.
In all groups, the problems gave rise to dilemmas such as whether or not to go out or whether or not to drink to avoid toilet visits. The finding that 43% of respondents limited their fluid intake to avoid and postpone visits to the toilet when not at home was surprising and worrying as was the finding that holding urine for up to 22 hours was a strategy for 39% of the respondents. In this light, it is worrying that so few women were referred to urological clinics or in contact with professionals who can give advice on how to remedy the problems. This may suggest that urological and continence issues are sensitive and surrounded by taboo and that they are difficult to discuss even with healthcare professionals. At the same time, it also suggests that neurologist and other professionals are either not aware of the potential problem or forget to ask the patient.
Refraining from going to the toilet can cause problems such as recurrent urinary tract infections (UTI) [21]. This was demonstrated in a study by Jagtap et al [4] who not only found that holding urine for a long time was a risk factor for UTI but also that poor access to toilets was a common reason for holding urine. In our study, 17% of the women had problems with UTI with significantly more incidents of UTI among women with lower mobility. According to the European Association of Urology (EAU), the presence of recurring urinary tract infections (rUTI) should lead to comprehensive urological evaluation and treatment, however, in our study only 5% of the women had been in contact with a urology clinic. Our results demonstrate that holding urine was a strategy for many of the respondents: 61% of the women reported a low frequency of urinating≤6 times a day. A low frequency was found in all groups but was associated with respondents with lower mobility – in our study mainly allocated to the SMA and dystrophy group. This match the findings from Roth and all [10] who reviewed medical records from NMD patients referred to a urology clinic with LUTS and found that most of the patients were diagnosed with SMA and dystrophy.
Our study illustrates the prevalence of LUTS in a Danish population of women≥12 years of age with NMD where especially urgency and incontinence symptoms are frequent. The prevalence of LUTS in women with NMD is unknown, but in a study of patients with CMT, Khrut et all [11] showed that LUTS were significantly higher in women with CMT compared to age-matched controls. Our study was explorative without any controls, but the findings of a higher incidence of urgency and urinary incontinence was the same. Contrary to Khrut et al, we found a low urinary frequency among our respondents; a reason for this could be a wider range of mobility level in our study population than in the one represented in the study from Khrut et al.
In our study, LUTS was related to age as seen in other studies. In a study of 4000 women, Møller et al found [22] that age was positively associated with most LUTS, that stress incontinence increased from the age of 40, and that urgency and urge incontinence escalated with the increase in age. They also concluded that LUTS is present when a woman has symptoms once a week or more; in our study this was the case for 33%. Although age is associated with LUTS, it is not related to bother [22]; in our study 33% of respondents reported a bother score≥3corresponding to moderate to severe impact on QoL. Nocturia, urgency, frequency and incontinence were the most bothersome symptoms. This corresponds to the findings from Argwal et al [23] who, in a population-based cross-sectional study with 3727 individuals (53.7% female), found that the burden from incontinence symptoms were higher for women than men.
The fact, that our research was nationwide and based on a unique national register of women with NMD in Denmark is a strength as is the response rate of 43% that represents a high number of female patients with NMD. The fact that respondents represent more than 25 NMD subtypes can be considered a strength but also a limitation because we could not demonstrate specific problems for individual diagnoses or conversely that some types of NMD were represented by too few participants to be conclusive on the presence and degree of the problem. Our choice of inviting women with a wide range of NMD diagnoses, physical functioning, and ages to our study was based on the very sparse literature on the subject and our aim to assess the subject in the context of ICF [7] where all levels of functioning are considered. The length of the survey could be the reason why 59 individuals (8%) left the questionnaire after the initial questions and were excluded from the analyses: The response rate of the ICIQ-FLUTS questionnaire in the last part of the survey was lower than for the previous questions; the reason could be that it was placed at the end of the long questionnaire, or that it was omitted by women who did not find the questions on LUTS relevant; in this case there is a risk of type 1 errors in our analysis. However, we believe that the LUTS response rate (85% of total responders) is reasonable. This is the first nationwide population-based study to address psycho-social aspects and neuro-urological health problems in relation to functional level and challenges in going to the toilet in women with NMD; our results add to the limited evidence base and will hopefully inspire to future studies at a more specific level.
Our results add to the growing focus on the necessity of accessible toilets in the public [24, 25]. Furthermore, the results show that there is an urgent need to inform engage and exchange information on bladder health with the NMD community. One way to achieve the United Nations Sustainable Development Goal no. 6.2 to “achieve access to adequate and equitable sanitation and hygiene for all ... ” is to increase awareness and cooperation between all actors in the rehabilitation process to ensure regular multi-professional evaluation, fulfill unmet needs, discuss relevant assistive devices, prevent recurrent UTI, preserve bladder /continence function, and improve QoL.
CONCLUSION
Our study demonstrates that problems in going to the toilet and lower urinary tract problems is an under-examined topic in women with NMD. It is necessary to establish an evidence platform to address urological symptoms in clinical practice, and to provide supportive treatment and solutions that enable participation for women with NMD.
ACKNOWLEDGMENTS
We thank the many women who responded to our invitation to participate in the study and share their experiences. A special thanks to the group of women with NMD from the Danish muscular dystrophy organization who took the initiative to the study, among them the co-authors of the study SG, JNS, and AVP.
FUNDING
The study is partly financed by a project grant in nursing research from the Novo Nordisk Foundation.
CONFLICTS OF INTEREST
The authors have no conflict of interest to report.
DATA AVAILABILITY STATEMENT
The data supporting the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
[1] | Aeh E . Neuromuscular disorders: Clinical and Molecular Genetics: Wiley; (1998) . |
[2] | Deenen JC , Horlings CG , Verschuuren JJ , Verbeek AL , van Engelen BG . The Epidemiology of Neuromuscular Disorders: A Comprehensive Overview of the Literature. J Neuromuscul Dis. (2015) ;2: (1):73–85. |
[3] | Wyndaele JJ , Kovindha A , Madersbacher H , Radziszewski P , Ruffion A , Schurch B , et al. Neurologic urinary incontinence. Neurourol Urodyn. (2010) ;29: (1):159–64. 10.1002/nau.20852. |
[4] | Jagtap S , Harikumar S , Vinayagamoorthy V , Mukhopadhyay S , Dongre A . Comprehensive assessment of holding urine as a behavioral risk factor for UTI in women and reasons for delayed voiding. BMC Infect Dis. (2022) ;22: (1)521. 10.1186/s12879-022-07501-4. |
[5] | Nishi SK , Babio N , Paz-Graniel I , Serra-Majem L , Vioque J , Fitó M , et al. Water intake, hydration status and 2-year changes in cognitive performance: A prospective cohort study. BMC Med. (2023) ;21: (1)82. 10.1186/s12916-023-02771-4. |
[6] | Handberg C, Kristensen B, Jensen BT , Glerup S , Pharao AV , Strøm J , Werlauff U . Challenges in urinating when away from home experienced by women with neuromuscular diseases - Project HAP-PEE part 1. Neuromuscular Disorders. 33: :S173. |
[7] | World Health Organization. International classification of functioning, disability and health: ICF. Geneva: World Health Organization;.(2001) . doi: |
[8] | Organization WH. SDG Target 6.2/Sanitation and hygiene [Available from: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-6.2-sanitation-and-hygiene. |
[9] | LA B . Prevalence and bother of patient-reported lower urinary tract symptoms in the muscular dystrophies. J Pediatr Urol. (2016) ;12: (6), 398. |
[10] | Roth JD , Pariser JJ , Stout TE , Misseri R , Elliott SP . Presentation and Management Patterns of Lower Urinary Tract Symptoms in Adults Due to Rare Inherited Neuromuscular Diseases. Urology. (2020) ;135: 165–70. 10.1016/j.urology.2019.09.039. |
[11] | Krhut J , Mazanec R , Seeman P , Mann-Gow T , Zvara P . Lower urinary tract functions in a series of Charcot-Marie-Tooth neuropathy patients. Acta Neurol Scand. (2014) ;129: (5):319–24. 10.1111/ane.12176. |
[12] | Fisette-Paulhus I , Gagnon C , Girard-Côté L , Morin M . Genitourinary and lower gastrointestinal conditions in patients with myotonic dystrophy type 1: A systematic review of evidence and implications for clinical practice. Neuromuscul Disord. (2022) ;32: (5):361–76. 10.1016/j.nmd.2022.01.008. |
[13] | EAU Guidelines. EAU Guidelines Office, Arnhem, the Netherlands.; (2023) . doi: |
[14] | The Danish rehabilitation Centre for Neuromuscular Diseases (RCFM) [cited 2023. Available from: https://rcfm.dk/en/. |
[15] | United Nations General Assembly, Standard rules on the equalization of opportunities for persons with disabilities: resolution / adopted by the General Assembly, A/RES/48/96, (20 December 1993). |
[16] | Handberg CKB , Jensen BT , Glerup S , Pharao AV , Strøm J , Werlauff U . HAP-PEE - Challenges faced by women with neuromuscular diseases when having to urinate away from home. Nursing Open, ID: NOP-2023-Aug-1561. 2023. doi:. |
[17] | Brooke MH , Griggs RC , Mendell JR , Fenichel GM , Shumate JB , Pellegrino RJ . Clinical trial in Duchenne dystrophy. I. The design of the protocol. Muscle Nerve. (1981) ;4: (3)186–97. 10.1002/mus.880040304. |
[18] | Aitken RC . Measurement of feelings using visual analogue scales. Proc R Soc Med. (1969) ;62: (10):989–93. doi: |
[19] | Brookes ST , Donovan JL , Wright M , Jackson S , Abrams P . A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. Am J Obstet Gynecol. (2004) ;191: (1):73–82. 10.1016/j.ajog.2003.12.027. |
[20] | Brunner A , Riss P . Nocturia in women. Maturitas. (2011) ;70: (1):16–21. 10.1016/j.maturitas.2011.06.004. |
[21] | Carlson KV , Rome S , Nitti VW . Dysfunctional voiding in women. J Urol. (2001) ;165: (1):143–7; discussion 7-8. 10.1097/00005392-200101000-00035. |
[22] | Møller LA , Lose G , Jørgensen T . The prevalence and bothersomeness of lower urinary tract symptoms in women 40–60 years of age. Acta Obstet Gynecol Scand. (2000) ;79: (4):298–305. 10.1080/j.1600-0412.2000.079004298.x. |
[23] | Agarwal A , Eryuzlu LN , Cartwright R , Thorlund K , Tammela TL , Guyatt GH , et al. What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women. Eur Urol. (2014) ;65: (6):1211–7. 10.1016/j.eururo.2014.01.019. |
[24] | Smoyer AB , Pittman A , Borzillo P . Humans peeing: Justice-involved women’s access to toilets in public spaces. PLoS One. (2023) ;18: (3)e0282917. 10.1371/journal.pone.0282917. |
[25] | Erekson EA , Ciarleglio MM , Hanissian PD , Strohbehn K , Bynum JP , Fried TR . Functional disability and compromised mobility among older women with urinary incontinence. Female Pelvic Med Reconstr Surg. (2015) ;21: (3):170–5. 10.1097/spv.0000000000000136. |




