Life Experiences in Neuromuscular Tracheotomized Patients in Times of Covid-19
Abstract
Background:
The management of tracheotomy at home can be very complex, affecting the patient’s quality of life.
Objectives:
This case series study aimed to explore the experiences of patients affected by neuromuscular diseases (NMD) concerning tracheostomy and Invasive Mechanical Ventilation (IMV) management at home during the COVID-19 health emergency in Italy.
Methods:
Semi-structured interviews and the following instruments were used: Connor and Davidson Resilience Scale (CD-RISC-25); Acceptance and Action Questionnaire-II (AAQ-II); State-Trait Anxiety Inventory (STAI); Langer Mindfulness Scale (LMS). Descriptive analyses, correlations, and qualitative analyses were carried out.
Results:
22 patients [50% female, mean age = 50.2 (SD = 21.2)] participated in the study. Participants who showed high levels of dispositional mindfulness in terms of novelty-seeking (r = 0.736, p = 0.013) and novelty production (r = 0.644, p = 0.033) were those with higher resilience. The main emotion that emerged was the fear of contagion (19 patients, 86.36%), due to the previous fragile condition, leading to a significant sense of abandonment. The tracheostomy’s perception is seen in extremes as a lifesaver or a condemnation. The relationship with the health professionals moves from satisfaction to a feeling of abandonment with a lack of preparation.
Conclusions:
The relationship between resilience, flexibility, state anxiety and dispositional mindfulness offers ways to reinforce tracheostomy management at home, even in critical periods when going to the hospital may be difficult.
ABBREVIATIONS
HIMV | Home Invasive Mechanical Ventilation |
NVS | Non-Invasive Ventilation Support |
ICUs | Intensive Care Units |
QoL | Quality of Life |
HRQoL | Health-Related Quality of Life |
ALS | Amyotrophic Lateral Sclerosis |
SMA | Spinal Muscular Atrophy |
DMD | Duchenne Muscular Dystrophy |
COPD | Chronic Obstructive Pulmonary Disease |
IPA | Interpretative Phenomenological Analysis |
ECAS | Edinburgh Cognitive and Behavioural ALS Screen |
MOCA | The Montreal Cognitive Assessment |
CD-RISC-25 | Connor and Davidson’s Resilience Scale |
AAQ-II | Acceptance and Action Questionnaire-II |
STAI | State-Trait Anxiety Inventory |
LMS | Langer Mindfulness Scale |
INTRODUCTION
Patients affected by Neuromuscular Disease (NMD) and other chronic respiratory conditions may develop chronic respiratory failure (CRF) and mechanical ventilation dependency [1, 2]. At that point, the options available become either continuous Non-invasive Ventilation Support (NVS) via a nasal/oronasal/mouthpiece/abdominal band interface, or sometimes in combination, either invasive mechanical ventilation (IMV) via a tracheostomy and a tracheal tube. Both these forms of ventilation allow patients to continue to live at home with different impacts on Quality of Life (QoL) [3–6]. The improvements in the intensive care setting with the lower complications of peri-tracheotomy procedures and the advances in the ventilators available have allowed Home Invasive Mechanical Ventilation (HIMV) to become increasingly available for patients surviving life-threatening illnesses. This picture allows treating patients outside the Intensive Care Units (ICUs) [2] with different outcomes in terms of Health-Related Quality of Life (HRQoL) [7–9]. A recent review of the international literature on mechanically ventilated patients in invasive and non-invasive modes revealed the difficulties that patients associate with mechanical ventilation [10]. Specifically, it indicates that participants find it difficult to make an informed choice in favour of invasive HMV, willing to have more decision-making support [11–13]. Indeed, they need to receive comprehensive information on living with HMV, tailored to their needs [14–16], especially about adverse events [17].The initial lack of communication has been described as traumatic [18] often when there was a lack of support from qualified medical personnel approaching this delicate period [19]. The COVID-19 pandemic has created unprecedented challenges for clinical care and research in NMD and CRF in HIMV who often have been feeling abandoned [20, 21], an aspect also found in caregivers [22]. Multidisciplinary team care, nutrition, aids, home healthcare, and hospice have become more difficult to obtain and, in some places, unavailable. Therefore, opportunities were considered and offered to overcome some of these problems through telemedicine [23] and new measurements [24–29]. However, little data are available on the real patients’ perceptions, experiences, and management of HIMV during the health emergency and the lockdown period.
Study aims
The main aim was to increase understanding of the experiences of people with neuromuscular or chronic respiratory diseases concerning the management of tracheostomy during the COVID-19 health emergency in Italy.
Specific objectives were:
– To investigate the presence of a correlation between levels of resilience, flexibility, state anxiety, and dispositional mindfulness in patients coping with tracheostomy management at home, during the pandemic;
– To explore words and metaphors used to describe one’s management and emotional experience.
METHODS
Ethics
This study was conducted following the Declaration of Helsinki, approved and overseen by Comitato Etico della Sezione “IRCCS Fondazione Don Carlo Gnocchi” del Comitato Etico IRCCS Regione Lombardia. (Reference: 08_09/12/2021). Patients provided a consent form before any study activity, including the collection of any of their data.
Study design
This is a prospective multicentre quanti-qualitative case series study, based on Interpretative Phenomenological Analysis (IPA) [30], which prioritized participants’ lived experiences. It is reported according to the COREQ guidelines [31].
Recruitment, setting and participants
Participants were purposively recruited from 10th December 2021 to 30th April 2022 thanks to the consultation of the databases of the Cardio-Respiratory Rehabilitation Unit of the IRCCS Fondazione Don Carlo Gnocchi in Milan and the General Respiratory and Respiratory intensive care unit (RICU) of the Policlinico ‘Aldo Moro’ Hospital in Bari. Due to the pandemic and to overcome the difficult logistical travels of patients, already in highly complex care situations, they were contacted by phone and/or e-mail. The planned assessment and interviews were conducted similarly.
Inclusion and exclusion criteria
– Inclusion criteria: adults diagnosed with a neuromuscular disease (i.e., Amyotrophic Lateral Sclerosis or ALS, Spinal Muscular Atrophy or SMA, Duchenne Muscular Dystrophy or DMD) with a tracheostomy at the time of the COVID-19 pandemic.
– Exclusion criteria: the presence of cognitive impairments that significantly limited comprehension of the contents of the tests carried out and the interview, assessed using the Edinburgh Cognitive and Behavioural ALS Screen (ECAS) [32] in the case of patients with ALS or The Montreal Cognitive Assessment (MOCA) in case of the other diseases [33]. Patients who comply with the cut-off scores of these tests have a formal indication for a full neuropsychological assessment. Cognitive impairments, previously ascertained and reported in the Clinical File in the case of Duchenne Muscular Dystrophy and Spinal Muscular Atrophy, were also considered.
Materials and data collection
The completion of the entire assessment took approximately 30 minutes and was carried out with the support of a duly trained Psychologist.
Demographic and clinical data
Socio-demographic data were collected: age, gender, level of education, profession (current or previous), and marital status.
The following clinical-medical data were collected: whether it is H24 ventilation or partial ventilation and for how long; usage of open ventilation (yes/no); motivation for tracheostomy (elective or urgent); time of illness; diagnosis-tracheostomy time; type of onset (if ALS); drug therapy taken; Percutaneous Endoscopic Gastrostomy (PEG) (yes/no); phonatory valve during open ventilation (yes/no); last night-time polygraphy done in ventilation; usage of O2 or not (and if so, how much).
Psychological test
The following psychological tests were administered:
– Connor and Davidson’s Resilience Scale (CD-RISC-25) [34], consists of five factors: 1. personal competence and tenacity (8 items); 2. self-confidence and management of negative emotions (7 items); 3. positive acceptance of change and secure relationships (5 items); 4. control (3 items); 5. spiritual influences (2 items). It is based on a 5-point Likert scale, ranging from 1 “totally false” to 5 “totally true”.
– Acceptance and Action Questionnaire-II (AAQ-II) [35], is designed to detect flexibility, and an individual’s ability to cope with, accept, and adjust to difficult situations [36]. The AAQ-II was developed to establish an internally consistent measure of the mental health and behavioural effectiveness model of ACT. The AAQ-II began as a 10-item scale, but after the final psychometric analysis, it was reduced to a 7-item scale.
– State-Trait Anxiety Inventory (STAI) [37], designed to detect trait anxiety. The STAI is a psychological questionnaire based on a 4-point Likert scale and consists of 40 questions on a self-report basis. It measures state anxiety, or anxiety about an event, and trait anxiety, or level of anxiety as a personal characteristic. Higher scores are positively correlated with higher levels of anxiety.
– Langer Mindfulness Scale (LMS) [38], measures dispositional mindfulness, which is also known as trait mindfulness, and it is a type of awareness that involves paying attention to one’s thoughts and feelings in the present moment without judgment. In this study, it was specifically declined in people with neuromuscular disease who were facing tracheostomy management at home during the pandemic period. It is a questionnaire of 21 questions that assesses four domains associated with mindfulness thinking: novelty seeking, engagement, novelty production, and flexibility. An individual who seeks novelty perceives every situation as an opportunity to learn something new. An individual who scores high in engagement is likely to notice more details about his or her specific relationship with the environment. An individual who produces novelty generates new information to learn more about the situation current situation. Flexible people welcome a changing environment rather than resist it.
At the end of this phase, if available and in a position to do so, the participant was subjected to a semi-structured interview aimed at investigating how he/she managed the tracheotomy and his/her emotional experiences during the COVID-19 period (Table 1). Interview schedule probes were used to consider relevant issues within the aims of the research. This interview, with prior consent and if possible, was audio-recorded to ensure greater reliability of the data, and if the participant showed signs of fatigue, it was conducted at a second meeting. Its administration took no longer than 20 minutes.
Table 1
Interview schedule
| Semi-structured Interview Schedule |
| 1.What do you think has changed in the management of tracheotomy during COVID-19? |
| 2.How is the home care received during the period of the medical emergency? |
| 3.How do you feel/are you feeling about this management? |
| 4.What kind of changes have you noticed in your relationship with home healthcare professionals? |
| 5.What difficulties are you experiencing with the management of the tracheotomy during the health emergency? |
| Possible prompts: When?/How often?/Physical?/Emotional?/Practical? |
| 6.What difficulties are you experiencing with the management of the tracheotomy during the lockdown period? |
| Possible prompts: When?/How often?/Physical?/Emotional?/Practical? |
| 7.What emotions are you predominantly experiencing during the medical emergency period? |
| Possible prompts: Can you think of specific situations? |
| 8.What emotions are you predominantly experiencing during the lockdown period? |
| Possible prompts: Can you think of specific situations? |
| 9.Which metaphor would you used to describe tracheostomy? |
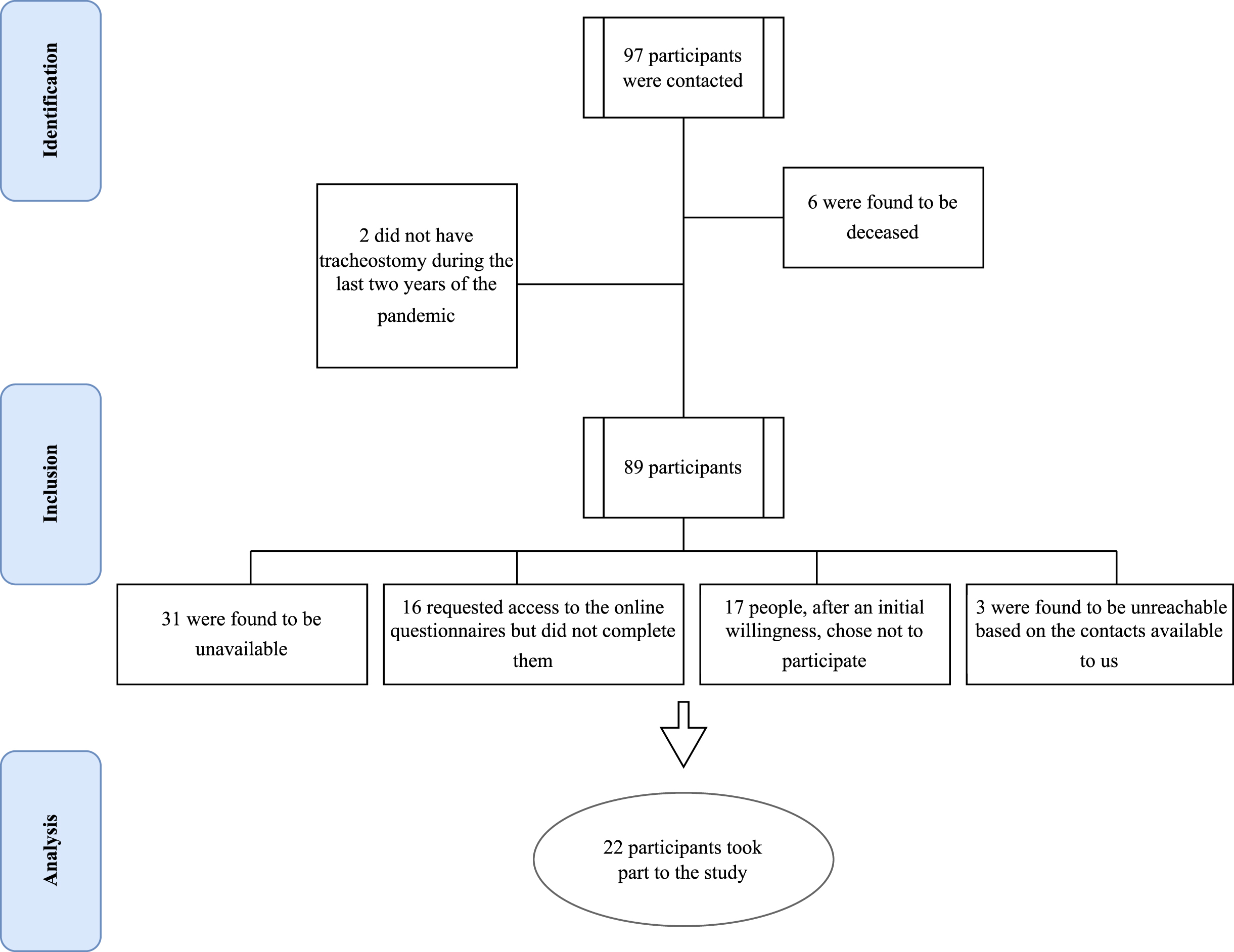
Fig. 1
Flow Chart of the study participants.
Data analysis
Quantitative analyses are statistical-descriptive, to describe the sample. Based on the distribution of the variables of interest, non-parametric rank correlations (Spearman rho correlation) were carried out to identify the relationships between the variable explored by the administration of the questionnaires as well as with the experiences expressed in the semi-structured interviews, the sample characteristics themselves and what emerged from the tests used. These analyses were conducted using the Jamovi software (version 2.2.2).
Qualitative analyses were conducted on the semi-structured interviews, audio-recorded (whenever possible), transcribed verbatim, and anonymized, based on IPA, to identify themes, sub-themes, frequency of words used, and metaphors. IPA assumes that the analyst is interested in learning something about the psychological world of the interviewee. This may be in the form of beliefs and constructs that are made manifest or suggested by the interviewee’s speech, or it may be that the analyst believes that the interviewee’s story can be said to represent a piece of the interviewee’s identity. In either case, meaning is central, and the aim is to try to understand the content and complexity of these meanings rather than to measure their frequency. During data analysis, which is flexible and dynamic, the focus is therefore on meanings during the analysis process. The main steps of analysis using IPA can be summarised as follows: -reading and re-reading the text in depth; -noting free associations and exploring the semantic content; -identifying themes and connections between them; -identifying recurring sub-themes and their connections; -noting the idiosyncratic aspects of the considered interviews; -observing metaphors and linguistic and temporal references [30]. These analyses were conducted using NVivo software (version 12, QSR international®).
Full triangulation of the identified themes was guaranteed by two authors in parallel [EV, PP], disagreements were discussed with a third author [PB] and a process of constant comparison between themes and transcripts.
RESULTS
Participants demographics
Figure 1 shows the flow diagram of the study participants’ recruitment. Table 2 shows the principal socio-demographic and clinical information of the 22 participants who took part in the study, who all underwent permanent tracheostomy surgery thus a life-long intervention. Only 5 (22.72%) of them accepted to release the interview.
Table 2
Socio-demographic and clinical information of the participants
| Variables | Levels | N (%) | M (SD) |
| Total (N) | 22 (100%) | ||
| Age (M, SD) | 50.2 (21.2) | ||
| Gender (n, %) | Men | 9 (40.9%) | |
| Women | 11 (50%) | ||
| Prefer not to say | 2 (9.1%) | ||
| Marital Status (n, %) | Married | 11 (50%) | |
| Divorced | 1 (4.5%) | ||
| Separated | 0 | ||
| Single | 8 (36.4%) | ||
| Widower | 0 | ||
| Other | 2 (9.1%) | ||
| Education (n, %) | Primary School | 0 | |
| Secondary School | 2 (9.1%) | ||
| High School | 9 (40.9%) | ||
| Bachelor’s degree | 1 (4.5%) | ||
| Master’s degree | 3 (13.6%) | ||
| Other Specialisations (e.g., PhD) | 2 (9.1%) | ||
| None | 5 (22.7%) | ||
| Disease | Amyotrophic Lateral Sclerosis (ALS) | 10 (45.4%) | |
| Spinal Muscular Atrophy (SMA) | 3 (13.63%) | ||
| Congenital Myopathies | 2 (9.09%) | ||
| Miasthenia Gravis | 1 (4.5%) | ||
| Muscular Distrophy | 2 (9.09%) | ||
| Other | 2 (9.09%) | ||
| Kind of onset (only in case of ALS) | Bulbar | 3 (30%) | |
| Spinal (lower limbs) | 5 (50%) | ||
| Respiratory | 2 (20%) | ||
| Non Invasive Ventilation (NIV) before tracheostomy | Yes | 5 (22.72%) | |
| No | 2 (9.09%) | ||
| I don’t know | 1 (4.54%) | ||
| No answer | 14 (63.63%) | ||
| Where did you try NIV for the first time? | At the hospital | 3 (13.63%) | |
| At home | 2 (9.09%) | ||
| No answer | 17 (77.27%) | ||
| Problems with NIV | Congiuntivitis, connective or corneal ulcers | 1 (4.54%) | |
| Skin abrations or ulcerations due to the mask | 2 (9.09%) | ||
| Dry nose and mouth | 2 (9.09%) | ||
| Use of cough machine | Yes | 2 (9.09%) | |
| No | 3 (13.63%) | ||
| Years of illness | 13.2 (19.7) | ||
| Years from diagnosis | 9.58 (11.5) | ||
| Diagnosis-tracheostomy time (Days) | 1560 (3217) | ||
| Ventilation | h24 | 8 (36.36%) | |
| Partial | 4 (18.18%) | ||
| No answer | 10 (45.45%) | ||
| If partial, how many hours? | 9.40 (10.2) | ||
| Use of open ventilation | Yes | 3 (13.63%) | |
| No | 9 (40.9%) | ||
| Percutaneous Endoscopic Gastrostomy (PEG) | Yes | 11 (50%) | |
| No | 2 (9.09%) | ||
| Phonatory valve during open ventilation | Yes | 3 (13.63%) | |
| No | 9 (40.9%) | ||
| I’ve tried it in the past, but I can’t use it | 1 (4.54%) | ||
| Use O2 or not | Yes | 7 (31.81%) | |
| No | 6 (27.27%) | ||
| No answer | 9 (40.9%) | ||
| How much? | 0.95 (0.96) |
Notes. M = Mean; SD = Standard Deviation; N = Number.
The relationships between resilience, flexibility, state anxiety and dispositional mindfulness
Participants who showed higher levels of dispositional mindfulness in terms of novelty seeking (r = 0.736, p = 0.013) and novelty production (r = 0.644, p = 0.033) were those who showed higher levels of resilience. Specifically, the subscale of personal competence and tenacity correlates positively with dispositional mindfulness in terms of novelty seeking (r = 0.745, p = 0.012). Similarly, novelty-seeking correlates positively with a high level of self-confidence and emotion management (r = 0.691, p = 0.023) as well as with positive acceptance of change and secure relationships (r = 0.829, p = 0.002).
Considering the subscale of novelty production inherent to the LMS, however, high levels are found where there are high scores in self-confidence and emotion management (r = 0.686, p = 0.020) and positive acceptance of change and secure relationships (r = 0.739, p = 0.009).
Moreover, where there are higher levels of engagement, anxiety is greater (r = 0.682, p = 0.021) but, at the same time, flexibility is also raised (r = 0.632, p = 0.037).
From Non-Invasive Ventilation Support (NVS) to tracheostomy: A journey through metaphors
For those who have experienced the use of Non-Invasive Ventilation Support (NVS) before being tracheostomised, NVS is described as “if you were in an oven”; “artificial respiration” or, in more positive terms, as “a doctor running to the rescue” or “a life preserver”. On the other hand, the tracheostomy is metaphorically and positively described as “a way out”, what “keeps me alive”, and “an angel who runs to save me”. Some see it as “the anteroom of death” or “like a robot”, while another participant has an ambivalent view of it, describing it as “a salvation, but at the same time an impediment”.
In a major part of the cases (5; 29.4%), participants underwent tracheostomy in an emergency, even though they knew it might have happened, and, for 4 participants (23.5%) this need was extensively verified and explored discussing it with the doctors. Three participants (17.6%) had the opportunity to discuss extensively with the doctors and a psychologist and 3 other participants referred that it was unexpected and practised in an emergency context (3; 17.6%). Finally, in one case (50%) the decision was made by the parents before the person was of age, and in another to avoid internal decubitus (1; 50%). In Table 4, some beliefs and information related to before and after a tracheotomy are illustrated.
Table 4
Beliefs and information related to before and after a tracheotomy
| About the tracheotomy, I was told. . . | N (%) |
| My quality of life would have improved | 3 (13.6%) |
| I would have been able to continue my activities of daily living (e.g. at home, with my loved ones, work…) | 0 |
| I would have had more years to live | 2 (9.09%) |
| I would no longer be able to communicate | 3 (13.6%) |
| I would no longer be able to eat | 3 (13.6%) |
| Other | 3 (13.6%) |
| No answer | 8 (36.3%) |
| Before receiving the tracheostomy, I thought that. . . | |
| My quality of life has improved | 5 (22.7%) |
| I was able to resume and/or continue my activities of daily living (e.g. at home, with my loved ones, work. . .) | 2 (9.09%) |
| I feel that I have many more years ahead of me | 2 (9.09%) |
| I can no longer communicate verbally | 3 (23.1%) |
| I can no longer eat | 4 (18.1%) |
| Other | 0 |
| No answer | 7 (31.8%) |
| After receiving the tracheostomy, it happened that. . . | |
| I died the day I made it | 1 (4.54%) |
| No answer | 21 (95.45%) |
Superordinate themes, themes, and subthemes
As mentioned above, only five participants (22.7%) accepted to take part in the semi-structured interviews, mainly because of communication issues and fatigue. The major topics were grouped into four superordinate themes, divided into themes and sub-themes, as depicted in Table 3.
Table 3
Organisation of superordinate themes, themes and subthemes emerging from the analyses, together with examples of quotations
| Superordinate Themes | Themes | Subthemes | Examples of citations |
| Emotions | Lockdown period | Reactive emotions | < <A little worried> > (Pt. 4) |
| Difficult emotions | < <That we are forgotten, that we are not respected> > (Pt. 3) | ||
| Overall emergency period | Reactive emotions | < <Serenity> > (Pt. 5) | |
| Difficult emotions | < <Completely abandoned> > (Pt. 1) | ||
| Challenges and difficulties | Protective behaviours | Passive adaptation | < <Thank God everything went well> > (Pt. 2) |
| Difficulties | < <...the only sadness was the loneliness that was felt in the long run. . .> > (Pt. 2) | ||
| Counterproductive Aspects | Passive adaptation | < <Occasional nursing care helped> > (Pt. 5) | |
| Difficulties | < <Total disarray. . .> > (Pt. 3) | ||
| Relationships | Family-related | Positive | N/A |
| Negative | < <...I am used to a life with friends, but that has always been the case, so the lockdown was all there. . .> > (Pt. 2) | ||
| Outside | Positive | < <We felt a bit isolated. Generally, more than discreet, so we realised it was for the long haul....> > (Pt. 5) | |
| Negative | < <And where are they?> > (Pt. 1) | ||
| Satisfaction | Coping alone | Continuity | < <Unfortunately, when events are so strong and you cannot change them, and when man cannot do anything to change certain things, you have to act intelligently and realise that that is the situation and you have to move on> > (Pt. 2) |
| Discontinuity | N/A | ||
| Coping with who? | Continuity | < <Sufficient> > (Pt. 4) | |
| Discontinuity | < <Non-existent assistance> > (Pt. 2) |
Emotions
Both the emotions experienced during the lockdown and the entire course of the medical emergency can be distinguished as either reactive emotions to the situation or difficulties. During the lockdown, 3 people (60% ; 3% coverage) perceived that they had been abandoned or forgotten, often including a sense of loss or worry (2 people; 40% ; 2% coverage). Isolation and abandonment, on the other hand, are the emotions mainly described by 4 of the participants (80% ; 6% coverage) concerning the entire period of the medical emergency.
Challenges and difficulties
Protective behaviour in the face of the challenges encountered raised as well as the main difficulties. Among the latter, note the perception of being alone, without help (1 participant; 20% ; 2% coverage), or in a confusing context (1 participant; 20% ; 2% coverage).
Relationships
In the superordinate theme of “relationships”, it is possible to distinguish relationships within the family unit from those with the outside world, often described in positive, supportive, or lacking terms. The most radical change was seen in the relationship with the outside world and with those health professionals who previously went to their homes. Indeed, participants complained about the absence or scarcity of contact, contributing to an increased sense of perceived isolation (3 participants; 60% ; 6% coverage). It should also be noted that no one refers to their caregiver or family unit as a reminder of the care, because they tend to take it for granted and continuous.
Satisfaction
“Satisfaction” was mainly focused on the one hand, on one’s abilities and those of the caregiver to cope with the management of the tracheostomy independently and, on the other hand, on the instructions previously received. Apart from one participant (20% ; 2 references; 4% coverage), who had continuity of care guaranteed during the entire course of the pandemic period at home, the other four people (80% ; 5 references; 10% coverage) report a total lack of satisfaction, precisely because of the lack of services meeting their needs and the lack of continuity of care.
DISCUSSION
This study for the first time in the literature explored the experiences of patients affected by NMD and CRF living with tracheotomies and HIMV during the COVID-19 pandemic period. Results raised the presence of patients with diverse backgrounds and marital and educational statuses and it is still unknown how these factors may help approach the stress pandemic related in different ways [29, 39]. The mean age of patients involved was 50±21 ranging between young adult and elderly stages of life with a long disease course behind a mean of 10 years from diagnosis. Interestingly, the predisposition to mindfulness and flexibility to novelty-seeking appears to be the winning strategy for higher resilience. Moreover, personal competence and tenacity statistically significantly correlate to a positive mindfulness predisposition. Thus, novelty-seeking positively also correlates with higher levels of self-confidence and emotion management with positive acceptance of change and secure relationships. In the late stages of ALS disease, the literature describes that patients undergoing long-term IMV may develop changes in personality causing a higher level of distress for their selves and their caregivers [40]. Moreover, the level of depression among patients affected by NMD diseases is higher compared to the general population [41]. Indeed, it has been found that the more negative the patients’ approach and behaviours to the illness and stressors, the higher the connected caregivers’ burden [42]. The positive and mindfulness approach to novelty seeking, therefore, may be of help in coping with the distress related to ALS and other chronic respiratory diseases even in periods of intense psychological distress such as the recent pandemic has been. Studies in the literature describe coping strategies of long terms patients and carers which can be of help in improving the QoL of both living with the distress of ALS disease [43]. Moreover, this mindfulness novelty-seeking coping strategy can also be implemented through group-based intervention which may help address the lack among patients and caregivers to improve the care burden, anxiety, and/or depression [44–46].
Another interesting point that was highlighted in the interviews is that even though the idea of tracheotomy was anticipated before the rescue event third of the participants received it in an emergency setting. As prior research studies showed, most patients undergo tracheotomy without any consent or proper long and exhaustive discussion with the caring physician because the procedure is performed during an emergency [47, 48]. Also, in our experience for some neuromuscular patients tracheotomy is performed in an acute setting telling them that it could be temporary and can be removed in a longer or shorter time.
All these stressful experiences sum up in patients’ and caregivers’ lives and resonate with their experiences during a period of more intense stress such as during the pandemic [49]. One of the major problem with the continuous use of the NIV is interface intolerance or lack of interface rotational strategy which may lead to emergency tracheotomy [50]. The tracheostomy is seen by patients in a way that often is contra posed. Indeed, if from one side HIMV is seen with a positive connotation as “a way out”, what “keeps me alive”, or even “an angel who runs to save me”; from the other side is seen as “the anteroom of death”, “like a robot”, or” salvation, but at the same time an impediment”. These feelings of fear and sadness tracheotomy related may be implemented by the small percentage of patients interviewed that use open ventilation [3 (13.63%)] or pronation valves [3 (13.63%)]. The first is a modality of ventilation and the second one is a one-side direction valve respectively which allows patients to speak again despite the presence of the tracheotomy and HIMV. The inability to speak again enhances the feeling of abandonment and separation.
Patients with tracheostomy and mechanical ventilation have an impaired cough mechanism. Coughing is an important defence mechanism to remove irritants, pollutants, bacteria, phlegm or any foreign objects (food, liquids, secretions) that have entered the airway, thus preventing aspiration pneumonia [51]. When the material enters below the vocal folds and into the airway, this is termed aspiration. As shown by Chatwin, normal trans tracheal suctioning with a catheter is not completely effective in more than 90% of cases and thus peripheral secretions are not removed [52]. Mechanical insufflation-exhalation (MI-E) applied to the tracheostomy cannula in patients with amyotrophic lateral sclerosis (ALS) undergoing invasive home mechanical ventilation is an effective procedure for managing bronchial secretions [53]. Interestingly, cough machines are still not used in most neuromuscular patients interviewed (60%). The reasons behind this were not explored and we do not know whether this is related to the fact that physicians who perform the emergency tracheotomy (ICU, ENT), Respiratory and Neurology physicians are still not aware of the importance of the bronchial clearance secretions during IMV, or to continuing to use it after the tracheotomy if before hands the patients were using it non-invasively [54]. Another possible explanation could be related to the delay in the delivery of the cough machine due to the pandemic and the manufacturing crisis around the world.
Unfortunately, only a small group of patients tracheotomized were able to complete the semi-structured interviews concerning feelings and how they adjusted to the tracheostomy management. This was mainly because of communication issues and fatigue expressed by the patients at the time of the call. However, from the very few interviews gathered, four themes were explored “emotions”, “challenges and difficulties”, “relationships”, and “satisfaction”. In the emotions, patients expressed an intense sense of abandonment and isolation. These feelings were further expressed in the second theme of “challenges and difficulties” as a sense of helplessness and confusion. The sense of abandonment is a common feeling experienced by individuals who are affected by chronic illnesses like neuromuscular diseases and use tracheostomy. The COVID-19 pandemic has added additional stress to these persons and may exacerbate feelings of abandonment. Reduced access to in-person support and healthcare services, as well as increased social isolation, may contribute to these feelings [22, 55]. It is important for individuals to seek out available resources, such as virtual support groups, telehealth services, and mental health services, to help cope with these feelings. Telehealth allows individuals with neuromuscular disease to receive mental health support from the comfort and safety of their own homes, which can be especially important for those who are immunocompromised. Additionally, telehealth services can help address barriers to care, such as transportation and mobility limitations, that may make in-person appointments challenging for individuals with neuromuscular disease. Overall, telehealth psychological support can help improve the mental and emotional well-being of individuals with the neuromuscular disease during the pandemic. In the “relationship” theme the absence of usual figures of health care providers who were used to visiting their homes contributed to the sense of isolation which is interconnected with the last theme of “satisfaction”. Indeed, the pandemic period created a sudden hiatus, a complete lack of services meeting their needs and a lack of continuity of care. This continued at least until the start of telemedicine which is not jet provided everywhere nor with continuity [29, 56].
Strengths, limitations, and future research
This study presents some limitations. Firstly, the study low sample size, which is, moreover, limited to the availability of two centres and the people who participated. In this regard, it is important to note that, in this study, patients with neuromuscular disease were considered in a specific condition such as home tracheostomy management in the pandemic period, thus a rarity within the rarity, which impacted the recruitment process. However, the survey response rate was 29.2%, which is in line with reported response rates of the internet or phone-based surveys [57]. Second, the QoL of these patients has not been evaluated during this study. The reason for this is the length of the usual QoL questionnaires and the relatively small time available for each interview given the weakness of the patients involved [58]. Third, the questions formulated leave space for many other items not explored. We acknowledge much missing info, and we hope to further expand in other studies. For instance, we know that none of the participants reported testing positive for COVID-19, but we have no news about their family members. In addition, the inability to meet all participants in person limited the opportunity to have available clinical data such as those about blood gas analysis, spirometry, and night-time polygraphy, which would have helped to better delineate the picture concerning residual functional and respiratory abilities. On the other hand, because they are people with a rare disease and in a peculiarly vulnerable condition during the pandemic period, priority was given to their clinical protection. The major strength of this study is that is the first of its kind to explore the experiences of patients dependent on HIMV during the period of the pandemic. Furthermore, the information gathered forced us to face how and what to implement among the supporting services either in person or via telemedicine that should be offered to these patients by the local hospitals and communities. Future studies should evaluate the QoL of patients on HIMV, and how and what has changed before and after the pandemic period. Furthermore, telemedicine support of care has had a positive impact on these fragile patients’ lives.
CONCLUSIONS
This is the first study that has explored the experiences of patients affected by NMD and CRF on HIMV during the pandemic pictures. It emerged a strong feeling of detachment and loneliness related to the lack of continuity in the service provided. However, the predisposition to mindfulness and flexibility to novelty-seeking appears to be the winning strategy for higher resilience. Moreover, personal competence and tenacity statistically significantly correlate to a positive mindfulness predisposition. Further studies will be warranted to fill the gap that this pandemic created with new resources to support from distance and to provide tools to raise the level of mindfulness, flexibility, and novelty-seeking among these patients.
CONFLICT OF INTEREST
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
AUTHOR CONTRIBUTIONS
EV, PB and PP contributed to the design and implementation of the research, the analysis of the results and the writing of the manuscript. EV, PP, DCM, CM, VV, FP, CGE and PB approved the final version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
FUNDING
No funding was provided for this study.
ACKNOWLEDGMENTS
We are very grateful to the patients who, although in complex personal and clinical situations, participated with interest in this study.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author, [EV], upon reasonable request.
REFERENCES
[1] | Banfi P , Pierucci P , Volpato E , Nicolini A , Lax A , Robert D , et al. Daytime noninvasive ventilatory support for patients with ventilatory pump failure: A narrative review. Multidiscip Respir Med. (2019) ;14: (1):38. |
[2] | Crimi C , Pierucci P , Carlucci A , Cortegiani A , Gregoretti C . Long-term ventilation in neuromuscular patients: Review of concerns, beliefs, and ethical dilemmas. Respiration. (2019) ;97: (3):185–96. |
[3] | Pierucci P , Crimi C , Carlucci A , Carpagnano GE , Janssens JP , Lujan M , et al. REINVENT: ERS International survey on REstrictive thoracic diseases IN long term home noninvasive VENTilation. ERJ Open Res. (2021) ;7: (2):00911–2020. |
[4] | Fiorentino G , Annunziata A , Coppola A , Marotta A , Simioli F , Imitazione P , et al. Intermittent abdominal pressure ventilation: An alternative for respiratory support. Melani A, editor. Can Respir J. (2021) ;2021: :1–5. |
[5] | Pierucci P , Di Lecce V , Carpagnano GE , Banfi P , Bach JR . The intermittent abdominal pressure ventilator as an alternative modality of noninvasive ventilatory support. Am J Phys Med Rehabil. (2022) Feb;101: (2):179–83. |
[6] | Bach JR . Amyotrophic lateral sclerosis. Chest. (2002) ;122: (1):92–8. |
[7] | Huttmann SE , Windisch W , Storre JH . Invasive home mechanical ventilation: Living conditions and health-related quality of life. Respiration. (2015) ;89: (4):312–21. |
[8] | Hannan LM , Sahi H , Road JD , McDonald CF , Berlowitz DJ , Howard ME . Care practices and health-related quality of life for individuals receiving assisted ventilation. A cross-national study. Ann Am Thorac Soc. (2016) ;13: (6):894–903. |
[9] | Schwarz SB , Mathes T , Majorski DS , Wollsching-Strobel M , Kroppen D , Magnet FS , et al. Living conditions and autonomy levels in COPD patients receiving non-invasive ventilation: Impact on health related quality of life. BMC Pulm Med. (2021) ;21: (1):255. |
[10] | Nelißen V , Metzing S , Schnepp W . Erfahrungen außerklinisch invasiv und nicht invasiv beatmeter Menschen –eine systematische Literaturrecherche qualitativer Forschungen. Pneumologie. (2018) ;72: (07):514–22. |
[11] | Dreyer PS , Steffensen BF , Pedersen BD . Life with home mechanical ventilation for young men with Duchenne muscular dystrophy. J Adv Nurs. (2010) ;66: (4):753–62. |
[12] | Lindahl B , Sandman PO , Rasmussen BH . Meanings of living at home on a ventilator. Nurs Inq. (2003) ;10: (1):19–27. |
[13] | Gale NK , Jawad M , Dave C , Turner AM . Adapting to domiciliary non-invasive ventilation in chronic obstructive pulmonary disease: A qualitative interview study. Palliat Med. (2015) ;29: (3):268–77. |
[14] | Dagrunn N Dyrstad MNSc, ICCN, PhD, Britt S Hansen ICCN, PhD, Evy M Gundersen ICCN Mns. Factors that influence user satisfaction: Tracheotomised home mechanical ventilation users’ experiences. J Clin Nurs 22: (3–4):331–8. |
[15] | Fahim A , Kastelik JA . Palliative care understanding and end-of-life decisions in chronic obstructive pulmonary disease. Clin Respir J. (2014) ;8: (3):312–20. |
[16] | Ceriana P , Surbone S , Segagni D , Schreiber A , Carlucci A . Decision-making for tracheostomy in amyotrophic lateral sclerosis (ALS): A retrospective study. Amyotroph Lateral Scler Front Degener. (2017) ;18: (7–8):492–7. |
[17] | Lipprandt M , Liedtke W , Langanke M , Klausen A , Baumgarten N , Röhrig R . Causes of adverse events in home mechanical ventilation: A nursing perspective. BMC Nurs. (2022) ;21: (1):264. |
[18] | Laakso K , Markström A , Idvall M , Havstam C , Hartelius L . Communication experience of individuals treated with home mechanical ventilation. Int J Lang Commun Disord. (2011) ;46: (6):686–99. |
[19] | Hirano YM , Yamazaki Y , Shimizu J , Togari T , Bryce TJ . Ventilator dependence and expressions of need: A study of patients with amyotrophic lateral sclerosis in Japan. Soc Sci Med. (2006) ;62: (6):1403–13. |
[20] | Cabona C , Ferraro PM , Meo G , Roccatagliata L , Schenone A , Inglese M , et al. Predictors of self-perceived health worsening over COVID-19 emergency in ALS. Neurol Sci. (2021) ;42: (4):1231–6. |
[21] | D’Alvano G , Buonanno D , Passaniti C , De Stefano M , Lavorgna L , Tedeschi G , et al. Support needs and interventions for family caregivers of patients with Amyotrophic Lateral Sclerosis (ALS): A narrative review with report of telemedicine experiences at the time of COVID-19 pandemic. Brain Sci. (2021) ;12: (1):49. |
[22] | Pierucci P , Volpato E , Grosso F , De Candia ML , Casparrini M , Compalati E , et al. Caregivers of neuromuscular patients living with tracheostomy during COVID-19 pandemic: Their experience. J Clin Med. (2023) ;12: (2):555. |
[23] | Pierucci P . Tele-consultation: A new promised land? Pulmonology. (2023) ;29: (1):2–3. |
[24] | Andrews JA , Berry JD , Baloh RH , Carberry N , Cudkowicz ME , Dedi B , et al. Amyotrophic lateral sclerosis care and research in the United States during the COVID-19 pandemic: Challenges and opportunities. Muscle Nerve. (2020) ;62: (2):182–6. |
[25] | Vasta R , Moglia C , D’Ovidio F , Di Pede F , De Mattei F , Cabras S , et al. Telemedicine for patients with amyotrophic lateral sclerosis during COVID-19 pandemic: An Italian ALS referral center experience. Amyotroph Lateral Scler Front Degener. (2021) ;22: (3–4):308–11. |
[26] | Bertran Recasens B , Rubio MA . Neuromuscular diseases care in the era of COVID-19. Front Neurol. (2020) ;11: :588929. |
[27] | Wu F , Burt J , Chowdhury T , Fitzpatrick R , Martin G , van der Scheer JW , et al. Specialty COPD care during COVID- Patient and clinician perspectives on remote delivery. BMJ Open Respir Res. (2021) ;8: (1):e000817. |
[28] | Tsutsui M , Gerayeli F , Sin DD . Pulmonary rehabilitation in a post-COVID-19 world: Telerehabilitation as a new standard in patients with COPD. Int J Chron Obstruct Pulmon Dis. (2021) ;16: :379–91. |
[29] | Ambrosino N , Pierucci P . Using telemedicine to monitor the patient with chronic respiratory failure. Life. (2021) ;11: (11):1113. |
[30] | Smith JA , Shinebourne P . Interpretative phenomenological analysis. American Psychological Association. 2012. |
[31] | Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) ;19: (6):349–57. |
[32] | Poletti B , Solca F , Carelli L , Madotto F , Lafronza A , Faini A , et al. The validation of the Italian Edinburgh Cognitive and Behavioural ALS Screen (ECAS). Amyotroph Lateral Scler Front Degener. (2016) ;17: (7–8):489–98. |
[33] | Nasreddine ZS , Phillips NA , Bédirian V , Charbonneau S , Whitehead V , Collin I , et al. The montreal cognitive assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) ;53: (4):695–9. |
[34] | Connor KM , Davidson JRT . Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. (2003) ;18: (2):76–82. |
[35] | Bond FW , Hayes SC , Baer RA , Carpenter KM , Guenole N , Orcutt HK , et al. Preliminary psychometric properties of the acceptance and action questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behav Ther. (2011) ;42: (4):676–88. |
[36] | Kashdan TB , Rottenberg J . Psychological flexibility as a fundamental aspect of health. Clin Psychol Rev. (2010) ;30: (7):865–78. |
[37] | Spielberger CD . State-Trait Anxiety Inventory for Adults (STAI-AD). 1983. |
[38] | Pirson MA , Langer E . Developing the langer mindfulness scale. Acad Manag Proc. (2015) ;(2015) (1):11308. |
[39] | Krishnamoorthy Y , Nagarajan R , Saya GK , Menon V . Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. (2020) ;293: :113382. |
[40] | Marconi A , Meloni G , Fossati F , Lunetta C , Bastianello S , Melazzini M , et al. Aggressiveness, sexuality, and obsessiveness in late stages of ALS patients and their effects on caregivers. Amyotroph Lateral Scler. (2012) ;13: (5):452–8. |
[41] | Rabkin JG , Goetz R , Factor-Litvak P , Hupf J , McElhiney M , Singleton J , et al. Depression and wish to die in a multicenter cohort of ALS patients. Amyotroph Lateral Scler Front Degener. (2015) ;16: (3–4):265–73. |
[42] | Lillo P , Mioshi E , Hodges JR . Caregiver burden in amyotrophic lateral sclerosis is more dependent on patients’ behavioral changes than physical disability: A comparative study. BMC Neurol. (2012) ;12: (1):156. |
[43] | Pagnini F , Phillips D , Langer E . A mindful approach with end-of-life thoughts. Front Psychol. (2014) ;5: . |
[44] | Burke T , Wilson O’Raghallaigh J , Maguire S , Galvin M , Heverin M , Hardiman O , et al. Group interventions for amyotrophic lateral sclerosis caregivers in Ireland: A randomised controlled trial protocol. BMJ Open. (2019) ;9: (9):e030684. |
[45] | Siciliano M , Santangelo G , Trojsi F , Di Somma C , Patrone M , Femiano C , et al. Coping strategies and psychological distress in caregivers of patients with Amyotrophic Lateral Sclerosis (ALS). Amyotroph Lateral Scler Front Degener. (2017) ;18: (5–6):367–77. |
[46] | van Groenestijn AC , Schröder CD , Visser-Meily JMA , Reenen ETKV , Veldink JH , van den Berg LH . Cognitive behavioural therapy and quality of life in psychologically distressed patients with amyotrophic lateral sclerosis and their caregivers: Results of a prematurely stopped randomized controlled trial. Amyotroph Lateral Scler Front Degener. (2015) ;16: (5–6):309–15. |
[47] | Hirano YM , Yamazaki Y , Shimizu J , Togari T , Bryce TJ . Ventilator dependence and expressions of need: A study of patients with amyotrophic lateral sclerosis in Japan. Soc Sci Med. (2006) ;62: (6):1403–13. |
[48] | Ceriana P , Surbone S , Segagni D , Schreiber A , Carlucci A . Decision-making for tracheostomy in amyotrophic lateral sclerosis (ALS): A retrospective study. Amyotroph Lateral Scler Front Degener. (2017) ;18: (7–8):492–7. |
[49] | Spurr L , Tan HL , Wakeman R , Chatwin M , Simonds A . P102 Psychosocial themes of the impact of the COVID-19 pandemic and shielding in adults and children with earlyonset neuromuscular disorders and their families. In: The wider impact of the pandemic. BMJ Publishing Group Ltd and British Thoracic Society; 2021, pp. A122-A122. |
[50] | Pierucci P , Portacci A , Carpagnano GE , Banfi P , Crimi C , Misseri G , et al. The right interface for the right patient in noninvasive ventilation: A systematic review. Expert Rev Respir Med. (2022) ;16: (8):931–44. |
[51] | Bach JR . Amyotrophic lateral sclerosis. Chest. (2002) ;122: (1):92–8. |
[52] | Chatwin M , Toussaint M , Gonçalves MR , Sheers N , Mellies U , Gonzales-Bermejo J , et al. Airway clearance techniques in neuromuscular disorders: A state of the art review. Respir Med. (2018) ;136: :98–110. |
[53] | Sancho J , Servera E , Vergara P , Marín J . Mechanical insufflation-exsufflation vs. tracheal suctioning via tracheostomy tubes for patients with amyotrophic lateral sclerosis: A pilot study. Am J Phys Med Rehabil. (2003) ;82: (10):750–3. |
[54] | Hanayama K , Ishikawa Y , Bach JR . AMYOTROPHIC LATERAL SCLEROSIS: Successful treatment of mucous plugging by mechanical insufflation-exsufflation1. Am J Phys Med Rehabil. (1997) ;76: (4):338. |
[55] | Magliano L , Citarelli G , Esposito MG , Torre V , Politano L . Impact of the COVID-19 pandemic on neuromuscular rehabilitation setting. Part Patients and families’ views on the received health care during the pandemic. Acta Myol Myopathies Cardiomyopathies Off J Mediterr Soc Myol. (2022) ;41: (2):89–94. |
[56] | Deml MJ , Minnema J , Dubois J , Senn O , Streit S , Rachamin Y , et al. The impact of the COVID-19 pandemic on the continuity of care for at-risk patients in Swiss primary care settings: A mixed-methods study. Soc Sci Med. (2022) ;298: :114858. |
[57] | Cook DA , Wittich CM , Daniels WL , West CP , Harris AM , Beebe TJ . Incentive and reminder strategies to improve response rate for internet-based physician surveys: A randomized experiment. J Med Internet Res. (2016) ;18: (9):e244. |
[58] | Rolstad S , Adler J , Rydén A . Response burden and questionnaire length: Is shorter better? A review and meta-analysis. Value Health. (2011) ;14: (8):1101–8. |




