Facilitators and Barriers to Wearing Hand Orthoses by Adults with Duchenne Muscular Dystrophy: A Mixed Methods Study Design
Abstract
Background:
To retard shortening of finger flexors in patients with Duchenne muscular dystrophy (DMD), hand orthoses are prescribed. However, many patients do not wear the orthoses regularly. To optimize orthotic interventions, we need insight into the factors influencing compliance.
Objective:
To evaluate the compliance regarding hand orthoses in an adult DMD population and to explore experiences and perceptions of DMD patients wearing orthoses, and of their caregivers.
Methods:
Mixed methods observational study, combining quantitative and qualitative data from medical charts combined with qualitative semi-structured interviews using a constant comparative method and a short validated questionnaire (D-QUEST).
Results:
65 medical charts were analyzed. 48 patients were assessed as needing hand orthoses, of whom 37.5 % were compliant. Qualitative data analyses revealed (1) motivation: preservation of hand function; (2) barriers: discomfort and impediments; (3) facilitators: good fit and personalized wearing schedule; (4) fitting process: satisfactory, but patients do not readily seek help when barriers appear.
Conclusions:
Patients are motivated to wear hand orthoses, but often discontinue use because of orthosis-and disease-specific barriers. The identification of these barriers leads to practical and feasible recommendations concerning the orthoses and the fitting process, such as less rigid material, preservation of some function while wearing the orthoses, and fixed evaluation points. The findings were confirmed by the D-QUEST.
INTRODUCTION
Duchenne muscular dystrophy (DMD) is a progressive X-linked neuromuscular disease that occurs in 1 in 5,000 live-born boys, resulting in muscular weakness, associated motor delays, loss of ambulation, respiratory impairment, and cardiomyopathy [1, 2]. Survival has improved in the past decades thanks to multidisciplinary care, a combination of non-invasive mechanical ventilation support, management of spinal deformity, prevention and management of cardiomyopathy-related heart failure and glucocorticoid treatment [3]. Although, the use of corticosteroids delays loss of ambulation, patients remain wheelchair-bound for the greater part of their lives, meaning they heavily depend on their arm function [4]. However, their arm function also weakens around the age of 13, and performance of activities with their hands becomes more and more difficult [5].
The involvement of the arms has a pattern of proximal to distal, meaning the hand function declines in later stages of the disease. In particular, the elbow, wrist and hand can develop contractures [6]. Stiffness seems to have a strong negative influence on arm function [6]. Shortening of the long finger flexors results in decreased mobility in wrist extension with the fingers extended, which is detrimental for maintenance of hand function in DMD patients [7]. Wrist and finger extension enables patients whose proximal muscles are already weakened to lift their hands and manipulate small objects such as joysticks and help them move their forearms around the tray of their wheelchair [7]. The loss of hand function further reduces quality of life and the ability to perform and participate in daily living activities [8].
The current available treatment for these impeding long finger flexor contractures are passive hand orthoses; however, compliance to wearing hand orthoses appears low. Hand orthoses aim at maintaining an active range of motion for the fingers and wrist, and at slowing the development of contractures [9]. The benefit of orthoses was studied in DMD patients with a wrist extension of less than 50 degrees by Weichbrodt et al. [7]. Their results indicated positive effects on joint mobility, grip strength and fine motor function. However, despite these favorable results, only three of the eight patients in that study continued to wear the orthoses in the follow-up phase, due to fitting problems or other reasons. This corresponds with our experiences from clinical practice, where we notice that many patients do not wear the hand orthoses regularly, for a variety of reasons. To successfully retard shortening of finger flexors with hand orthoses, we need to understand the factors that influence patients’ compliance.
The aims of this study were as follows:
– to evaluate compliance in wearing hand orthoses of adult DMD patients visiting the Neuromuscular Center of Nijmegen
– to explore experiences and perceptions of DMD patients who are advised to wear hand orthoses, as well as the experiences and perceptions of their primary caregivers.
METHODS
Design
This is a mixed methods observational study, combining quantitative and qualitative data from medical charts with semi-structured interviews using a constant comparative method [10] and a short validated questionnaire.
Participants
From the database, we included all patients aged 18 and older who had a clinical and/or DNA-established diagnosis of Duchenne muscular dystrophy, and had visited the Neuromuscular Center of Radboud University Medical Center in Nijmegen, the Netherlands.
From the group of patients who were advised to wear hand orthoses and who had received the orthoses at least six months previously, we selected patients and their primary caregivers to undergo interviews and complete a validated questionnaire (D-QUEST) about their satisfaction with the devices. The researchers used information from previous visits to purposively select patients with varying histories of compliance. The intention was to include the perspectives of very compliant patients, less compliant patients and patients who did not wear their orthoses at all. We aimed to include 6–10 patients and their caregivers, until saturation was reached. Patients and their primary caregivers needed to be able and willing to participate in the interview.
Procedures
Retrospective data
We gathered quantitative data about the recommendation for and compliance to hand orthoses and, if available, qualitative data on perceptions and experiences with hand orthoses from the medical charts. The need for hand orthoses was assessed by an experienced occupational therapist and was declared when the maximum wrist extension with extended fingers was less than 20 degrees. Another indication of the need for orthoses is the perceived stiffness of the long finger flexors and the progress of the shortening compared to previous visits (>10 degrees per year). When the hands were entirely dysfunctional because of severe deformity, orthoses were no longer indicated, except to prevent care problems. Information on compliance and qualitative data about perceptions and experiences were extracted from notes on orthosis wearing taken during the follow-up visits by the rehabilitation physician, occupational therapist, or other health-care professionals.
Semi-structured interviews
We asked patients and their primary caregivers about their perceptions of the use of orthoses, their experiences in wearing orthoses, the perceived information about hand orthoses, their experiences concerning the process of fitting, and the course of events after delivery. Besides, we asked about their activities and participation in daily life. Finally, we asked if they had recommendations for improving the orthoses, the process or the compliance. The interview guide was created and discussed by occupational therapists with research experience, a physiotherapist and rehabilitation physicians (interview guide available in the appendix). The researchers (SH, NB, MZ, LdW, FvW) were trained in the interview technique and supervised by an experienced qualitative researcher (EC), a rehabilitation physician and an occupational therapist with vast clinical experience.
To gain additional insight into the upper extremity function of the interviewed population, the Brooke scale [11, 12] was used. In the Brooke scale, the score range is from 1 to 6; 1 means that the patient can fully abduct the arms until they touch above the head, and 6 means that the patient cannot raise the hands to the mouth and has no useful function of the hands.
D-QUEST
D-QUEST stands for Dutch version of Quebec User Evaluation of Satisfaction with Assistive Technology. This is a validated questionnaire evaluating the satisfaction with a device and the fitting process, using a 5-point Likert scale. The higher the score, the more satisfied patients are with the orthoses. Question items on the device were size, weight, adjustability, safety, sustainability, ease of use, comfort, effectiveness. Question items on the process were delivery services, repairs and servicing, professional services, and follow-up services. Finally, patients were asked to select three aspects from the items on the D-QUEST that they found most important [13, 14].
Orthoses
The orthoses used in our clinical practice are custom-made, using thermoplastic material and soft straps. The shape of the splint depends on the degree of deformity of the hand and the stretch with which the patients are comfortable. Furthermore, it depends on the position in bed, the degree of transpiration and the need for adjustments, for example to handle an alarm. Two examples of orthoses used by the patients are seen in Figs. 1 and 2.
Fig. 1
Volar view of an orthosis with integrated alarm button.
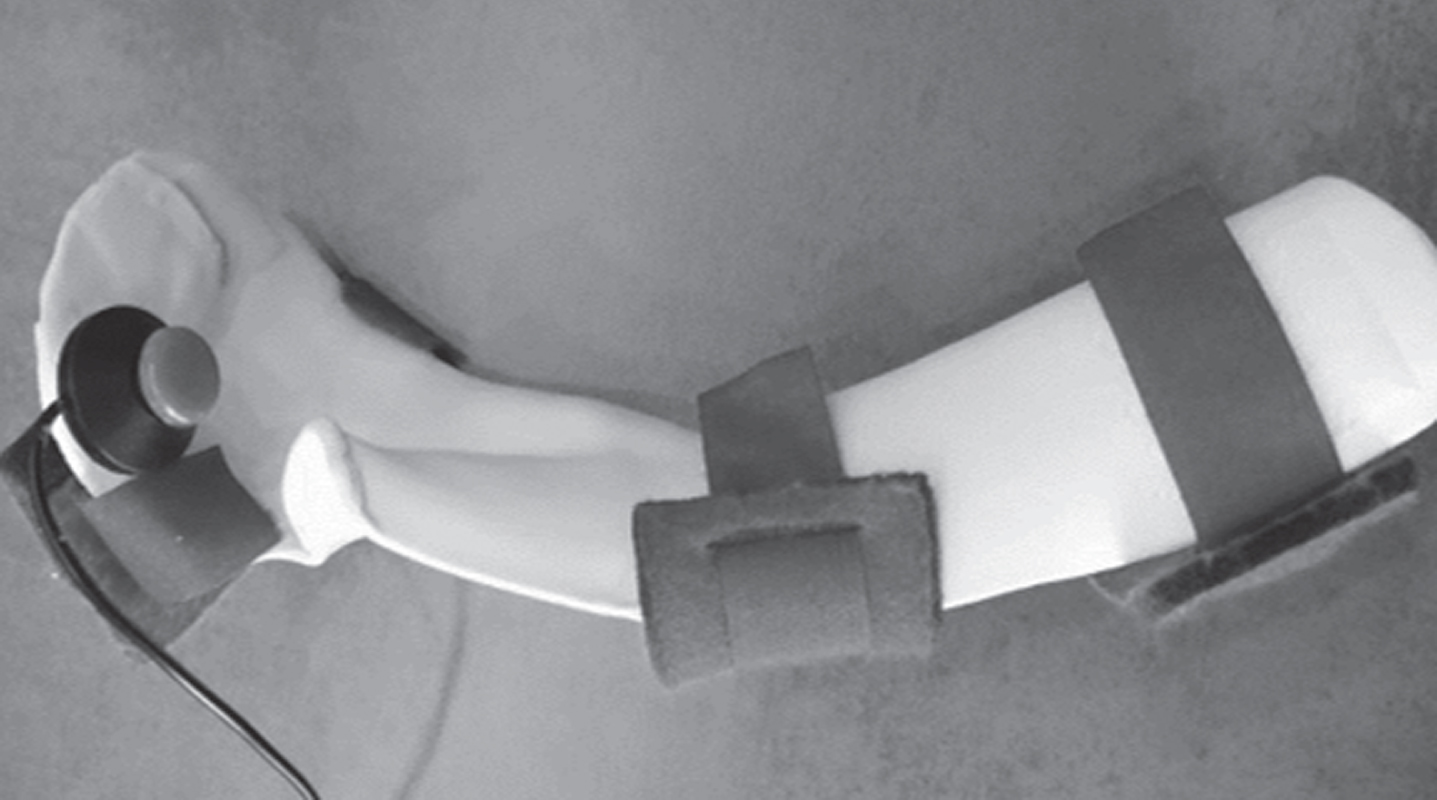
Fig. 2
Dorsal view of an orthosis with additional padding near the web space.

Data analysis
A descriptive analysis was performed on the quantitative data from the medical charts. Atlas-Ti 8.4.20 software was used to analyze the qualitative data gathered from the medical charts and the interview transcripts. Interview analysis involved three phases: (1) transcription of the interviews; (2) reading and coding of the interviews; and (3) discussing and interpreting the findings with the research group (SH, EC, YvdE, MJ, IdG, NB, MZ, LdW, FvW), using a constant comparative method to ensure the data were reviewed in depth. This process resulted in the formulation of categories and themes [10].
After training, four occupational therapy students (NB, MZ, LdW, FvW) performed interviews with two patients and their caregivers, followed by transcription and coding. The findings and the need to include additional interview topics were discussed with the experienced qualitative researcher (EC). Then, the students did another four interviews which were subsequently analyzed and discussed by the research group of experienced clinicians and researchers. Finally, one more interview was held by the main researcher (SH), who confirmed that saturation had been reached.
Next, results from the D-QUEST were analyzed. For all parts of the D-QUEST questionnaire, mean and median outcomes were calculated. Satisfaction with the orthoses and satisfaction with the services were discussed separately. Finally, we listed the five factors from the D-QUEST that patients considered most important.
Ethical approval
Written informed consent was requested from each participant and their primary caregiver separately. In addition, permission was requested to record the interviews and take pictures of the orthoses. Data were anonymized and handled according to guidelines for good clinical practice. Our study was approved by the local medical ethics committee (no. 2019-5718).
RESULTS
Findings from the medical charts
The medical charts of 65 patients (>18 years) were analyzed. Forty-eight patients (73.5%) had a wrist extension of less than 20 degrees with extended fingers and had been advised to wear hand orthoses by the occupational therapist. Of these patients, 18 (37.5%) used the orthoses regularly, meaning every night or every other night, at least four times a week. Additionally, qualitative data of 41 patients (63% of all medical charts) was available concerning perceptions and experiences in wearing orthoses. Common perceptions of patients were that orthoses were necessary (n = 8), but negative experiences in the past with leg or hand orthoses discouraged some patients from starting another course of orthosis use (n = 3). Common experiences with the current orthoses were discomfort and pain due to fitting problems (n = 11), or to stiff material on their trunk in supine positions (n = 4). Others included sleeping problems (n = 3); limitations of hand function while wearing the orthoses, such as not being able to operate an alarm (n = 7); and sweating (n = 2). Some patients were not motivated or forgot to wear the orthoses (n = 3). An important practical comment from one patient was that the orthoses were fitted in a seated position, while they were worn in asupine position, which caused fitting problems.
Findings from the interviews
The main characteristics of the patients participating in the interviews (n = 7) are summarized in Table 1. The patients’ age varied from 21 to 34. Six patients suffered from cardiomyopathy, five patients needed non-invasive ventilation and two were on steroids. Six patients lived with their parents and one lived in a care setting. One patient had a Brooke score of 4 (“can raise hands to the mouth, but cannot raise an 8-ounce glass of water to the mouth”), while all others scored 5 or higher on the Brooke scale (“cannot raise hands to the mouth, but can use hands to hold a pen or pick up pennies from the table”, to “no useful function of the hands”). Four of the patients had an occupation, for which the use of a computer was crucial. The main other daily activities were gaming, computer, cell phone use and wheelchair hockey.
Table 1
Patient characteristics
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | |
| Age | 22 | 26 | 30 | 26 | 26 | 34 | 21 |
| Cardiomyopathy (y/n) | n | y | y | y | y | y | y |
| Ventilated (y/n) | n | y, non- invasive | y, non-invasive | y, non-invasive | y, non-invasive | y, non-invasive | n |
| Steroid use (y/n/previous) | y | n | n | n | n | n | y |
| Living situation | With parents | With parents | With parents | In a care setting | With parents | With parents | With parents |
| Most frequent caregivers | Parents | Parents | Parents, homecare | Professional caregiver | Parents and care team | Parents | Parents |
| Brooke | 5 | 5/6 | 5/6 | 6 | 5/6 | 5/6 | 4 |
| Time orthoses advised | 3 years ago | 8 months ago | 3 years ago | 5 years ago | right: 6years ago, left: 2years ago | 6 months | 2 years ago |
| Wearing time | Stopped, previously: 4–5 hours per night | Stopped, previously: 3–4 nights a week, 4–5 hours | Every night, alternating, >8 hours | Wears mainly the left side >8 hours | 3–4 times/wk alternating, >8hours | During the day 30–90 minutes | 3–4 times/week alternating, >8hours |
| Occupation | Administrator | - | Chairman | Activity center: editing movies | Administrator | – | Seeking further education |
| Leisure activities | Gaming | Computer | Wheelchair hockey | Gaming | Gaming, going out | Computer, cell phone | Computer, wheel-chair hockey |
Four themes were identified which affected the use of hand orthoses: (1) motivation: preservation of hand function; (2) barriers: discomfort and impediments; (3) facilitators: a good fit, easy to put on and personalized wearing schedule; and (4) fitting process: fitting needs regular attention.
Motivation: Preservation of hand function
The main reason why patients (6 out of 7) used orthoses was their perception that their hand function would be preserved, and that participation in important activities would remain possible for a longer period. The most important activities for which patients used their hand function were working with the computer, using a cell phone, gaming and wheelchair sports. “In daily life I use the computer and cell phone a lot, it shouldn’t happen that you can’t use them anymore”[D3]. Four of the seven patients experienced preservation of function, and this gave them extra motivation to continue wearing the orthoses. One patient sensed more suppleness of the fingers after wearing the orthoses; however, another patient experienced some stiffness in the beginning after removing the orthoses. One of the caregivers mentioned that the previous experience with contractures in the legs were a good motivation to prevent contractures in the upper extremity as much as possible.
Barriers: Discomfort and impediments
We distinguished two different categories of difficulties in wearing the orthoses. The first category involved barriers with the orthoses themselves: five of the seven patients experienced fitting problems such as pressure spots on the knuckles or at the edges of the orthoses, pain due to too much stretch on the muscles while wearing the orthoses, or a numb feeling in the hand or fingers when wearing the orthoses for a longer period. “The orthoses pushed too hard; I couldn’t keep them on”[D1].These complaints were resolved for three patients during the follow-up visits, whereas they remained a barrier to wearing orthoses in the other cases. Additionally, two caregivers experienced abundant sweating of the patients when wearing hand orthoses, due to the limited permeability of the material, which increased discomfort and the risk of intertrigo. “In the morning, when we remove the orthoses, there is a trickle of water in them.”[caregiver, D4].
The second category involved disease-specific barriers. To start, three patients explained that the morning and evening care rituals are very time-consuming and putting on and taking off orthoses requires a great deal of effort. “At the moment, the bedtime ritual takes so much time, I would rather sleep than put on the orthoses” [D2]. Another common experience is that wearing orthoses causes additional limitations in moving the arms and hands. The weight of an orthosis further limits the ability to lift the forearm. “Normally he is using the fingers to ‘crawl’ to move his forearm. With orthoses, this way of moving the arm becomes impossible” [parent, D1]. The decreased mobility of the arms, in combination with the hardness of the material, has a negative influence on comfort when lying in bed, which is in many cases already decreased. This situation can subsequently lead to sleeping problems. “I often woke up because of the orthoses, this was not okay, because then my parents had to come downstairs to remove them and put my arm in the right position” [D1]. In addition, restriction of movement increased patients’ dependence, as they needed help to put on and remove the orthoses. Moreover, they were not able to operate their alarm at night. This was an important topic in four of the interviews, as it was frightening both for patients and their caregivers. “If something was wrong, or I needed to turn over at night, I couldn’t operate the alarm. In the end, this was why I stopped wearing the orthoses back then. Now that I have an orthosis that leaves my index finger free to move, I can use the alarm and I do wear the orthoses” [D3].
Two parents added that changes in the care regime were difficult for their son. Orthoses have to fit precisely because the wearer has high sensitivity and a limited ability to adjust the orthoses. “He cannot stand the orthoses, he feels every bump” [parent, D7]. One participant had a remark on the timing of the recommendation to wear the orthoses. This recommendation was issued when his hand function was still adequate; to him, this felt a bit strange.
Facilitators: A good fit, easy to put on and personalized wearing schedule
Factors that helped in wearing orthoses were in many cases the opposite of the reported barriers. When orthoses fit well, did not hurt and/or did not hamper sleeping, patients felt less resistance to wearing them. One patient preferred wearing the orthoses during the day while watching a movie, because of the distraction. He then was less aware of the orthoses. The wearing schedule was also important. The option of wearing the orthosis on alternate days improved adherence in three patients and the addition of a tubular bandage underneath the orthosis helped to relieve discomfort. The appearance of the orthoses did not matter for 5 of 7 patients “The appearance doesn’t matter to me, I wear the orthoses at night, I don’t have to show them to anyone”[D3]. Three patients became more accustomed to the orthoses after wearing them for a longer period. One participant suggested more fancy colors.
Six of the caregivers mentioned that putting on and taking off the orthoses was easy and quick; however, it would help if patients could put on andremove the orthoses themselves. Besides, two of them mentioned that experiences from peers (parents with a son with DMD) could help in the motivational proces: “I spoke to parents of one of his peers from his hockeyteam about the orthoses and discussed how they dealt with this” [parent, D7].
Fitting process: Fitting needs regular attention
Six of the seven patients were satisfied with the fitting process and the information received during this process. Nonetheless, some important remarks were made. First, even if the orthoses fit immediately during the visit to the hospital, this was not a guarantee of success when wearing them at home. Sometimes patients experienced discomfort after a few hours. One participant also found that, the fit deteriorated even after a longer period, probably due to progression of the hand deformity.
The second important finding was that a majority of the patients (4 out of 7) did not contact their (para) medical professionals in case of problems, so the discomfort or impeding factors were not reported, and thus not resolved. Instead of addressing the problems, patients discontinued wearing the orthoses. Two of them said that, looking back, they should have sought help sooner. “Now it’s going well. I should have called sooner, but at one point I thought the orthoses were a nuisance, so I didn’t wear them. But, actually, I had to report it” [D3]. One participant did address the discomfort, but received an unsatisfactory answer: “They said I should try it again and for a longer period; that was not what I was hoping for” [D6].
The most important reasons patients had for not calling were that it was too much effort, it was not worth taking the extra time, they forgot or had other priorities, or it was not a standard topic during annual visits to the hospital. “I think I didn’t report it, because I could handle the discomfort” [D5]. Some indicated that it would have helped if there was an extra evaluation opportunity a few weeks after the delivery, while two patients found it pleasant that they did not receive unnecessary appointments. They all felt it was possible to contact the occupational therapist when necessary.
If we asked about the role of the professionals in the decision to wear the orthoses, five patients stated that the occupational therapist and the rehabilitation physician had the greatest influence on the decision. Parents were supportive in remembering, but they left the decision to wear the orthoses to their adult son. “I keep encouraging him to wear the orthoses, keep them in sight. But that’s all I can do” [parent,D1]. Two caregivers mentioned that peers could at least influence their sons’ knowledge of orthoses, but this was neither addressed nor confirmed in the interviews with the patients.
D-QUEST
Five of the 7 patients completed the D-QUEST, while 2 of the patients did not want to fill out the questionnaire. The results of the D-QUEST are displayed in Table 2. First, the orthosis-specific section: the items ”safety” and “adjustability” were indicated as “not applicable” by 4 and 2 patients respectively. The lowest score was on the ease of use (median 4, range 2–5). Regarding the process, the patients were generally satisfied; all process items had a median score of 4, and a range from 4–5.
Table 2
Result of the D-QUEST
| N = 5 | Items D-QUEST | Valid | Not applicable | Median (range) |
| Orthosis-specific | Size | 5 | 0 | 4 (3–4) |
| Weight | 5 | 0 | 4 (4–5) | |
| Adjustability | 1 | 4 | 5 (5) | |
| Safety | 3 | 2 | 5 (4–5) | |
| Sustainability | 5 | 0 | 4 (3–4) | |
| Ease of Use | 5 | 0 | 4 (2–5) | |
| Comfort | 5 | 0 | 4 (4) | |
| Effectiveness | 4 | 1 | 4.5 (4–5) | |
| Orthoses in general | 5 | 0 | 4 (3–4) | |
| Process-specific | Delivery services | 5 | 0 | 4 (4–5) |
| Repairs and servicing | 3 | 2 | 4 (4–5) | |
| Professional services | 5 | 0 | 4 (4–5) | |
| Follow-up services | 5 | 0 | 4 (4–5) | |
| Process in general | 5 | 0 | 4 (4–5) |
The most important factors listed by the patients include “comfort” (4×); “ease of use”, “effectiveness” and “weight” (3×); “professional services” (1×).
DISCUSSION
This study has provided insight into the factors that influence compliance with hand orthosis wearing in DMD patients. In our population the compliance appeared low; only 18 of the 48 patients who were advised to wear hand orthoses actually wore them. We identified motivations, barriers and facilitators related to wearing hand orthoses in DMD patients which lead to practical recommendations.
The motivation of patients to wear the orthoses was driven by the idea and/or realization that they could maintain their hand function, activities and participation level. This is in line with previous literature showing strong relationships between muscle strength, ROM and distal motor function of the upper limbs, suggesting the importance of maintaining adequate levels of range of motion, with the long-term goal of preserving distal motor function of the upper limbs [9, 15]. Besides, the patients in our study mentioned that professionals had considerable influence on their motivation and compliance.
We found two categories of barriers: orthosis-specific barriers and DMD-specific barriers. The orthosis-specific barriers, including complaints about the material, permeability, fitting issues and pain due to too much stretch have not been previously described in the DMD population wearing hand orthoses. However, a study within the broader neuromuscular field reported that hand orthoses can interfere with activities, cause pain, disturb sleep and increase of the burden of care [16]. Moreover, Andringa et al. [17] described dynamic hand-wrist orthosis tolerance in daily use in chronic stroke patients. In this study, compliance was influenced by performing special activities such as going out, shopping, swimming, or cycling. This study also mentioned problems such as wearing clothes with sleeves too narrow to fit the orthosis, lack of help with putting on the orthosis, problems of tolerance, such aspain in the fingers or extensormuscles, or being tired of wearing the orthosis. Pressure ulcers were also reported. Although the target population differs, the orthosis-specific barriers are similar.
The DMD-specific factors, such as the great number of care interventions, further limiting of function and dependence on others, are impediments to compliance. This is also seen in other studies where aids are implemented to support DMD patients. For example, during a pilot study on supported standing, adherence was affected mostly by practical factors (device malfunction, long school days limiting time at home), but by motivational factors and physical factors as well [18].
Additionally, a web-based questionnaire showed that, despite the existence of upper extremity impairments, only 9% of the DMD patients used supportive aids [6]. Van der Heide et al. [19] studied the perceived benefits of dynamic arm supports and their relatively high levels of non-use. They found that availability and insufficient support for important movements were reasons for the non-use. Besides, caregivers are needed to put on and remove the arm support, while in some cases it is more convenient for patients and caregivers to support the activity itself instead of using the support. We confirm in our study that the disease-specific barriers do not always outweigh the benefits of aids.
The decision to prescribe hand orthoses, and its timing, are points of discussion. To our knowledge, there is no evidence-based guideline available. On the basis of clinical experience, Weichbrodt et al. [7] recommended orthoses when the passive wrist extension with extended fingers dropped to 50 degrees. In our clinical practice, we advise orthoses when wrist extension with extended fingers drops below 20 degrees. As we mentioned before, other factors such as the use of the hands, increased loss of mobility and stiffness of the joints influence the decision to recommend hand orthoses. We recommend further research to obtain better insight into the natural course of the shortening, which can aid the timing of the recommendation for hand orthoses.
A limitation of our study was that compliance was distracted from the medical charts, which can lead to an overestimation if patients tended to give socially desirable answers. To enhance and monitor compliance more precisely, it would be useful to involve occupational therapists from the community who can visit the patients or make use of diaries completed by patients or their caregivers.
Multiple strengths of this study can be identified as well. A major strength is that the interviews focused on participants’ perceptions and experiences, so patients had the opportunity to address all relevant aspects of the orthoses and the fitting process. Triangulation took place by asking both patients and their caregivers to give input. Barring a few small disagreements, no major differences were found in their experiences with hand orthoses. This is probably because the majority of the caregivers left the responsibility of wearing the orthoses to their sons. Another strength was the purposive selection, resulting in different views on compliance and strengthening the corresponding opinions. Moreover, triangulation was also created by comparison of the qualitative data from the medical charts with the data from the interviews [20], which gave comparable topics. Finally, to objectify our qualitative data, we deliberately administered the D-QUEST after completing the interviews. In this way, patients were not biased in mentioning themes which were important to them during the interviews. Nevertheless, the results from the D-QUEST confirmed the findings of the qualitative research. The topics selected by our patients, namely comfort, ease of use, effectiveness and weight, were also selected by patients in other studies using the D-QUEST [21]. This confirms our previous findings that many orthosis-specific barriers can be generalized to different populations.
After identifying motivations, barriers and facilitators, we can formulate practical and feasible recommendations to enhance compliance in wearing hand orthoses. First, we recommend using light and permeable material with a soft coating, and to provide stretch, but avoid too much stretch which causes pain. It is also important to fit the orthoses in the position they are eventually used (most of the time in a supine position), as this will increase the chance of a good fit. Putting on or removing the orthoses should be quick and easy. Additionally, we recommend looking for ways to help patients do this on their own. One patient challenged the professionals to incorporate stretching opportunities into their daily activities, such as modified controllers, as many patients play computer games for several hours a day. We support the idea of incorporating the use of a stretching orthosis into daily activities.
In addition, we recommend that professionals should identify incentives and barriers concerning the use of orthoses at the very beginning of the process, before manufacturing the orthoses. This includes items such as patients’ ability to operate the alarm or use a cell phone, evaluation of sleeping positions, and feasibility of the wearing schedule. This way, expectations can be managed and barriers can be overcome before the orthoses are actually used.
Finally, our results show that patients did not ask for help when barriers appeared. They discontinued wearing the orthoses, or gave in to the barriers without ringing the bell. Therefore, we recommend fixed evaluation points after delivery of the orthoses, to help patients to address problems and solve them whenever possible. Because problems can occur on both the short and long term, we advise that the occupational therapist from the neuromuscular team should perform an evaluation in the phase shortly after the delivery of the orthoses. In the chronic phase, the occupational therapist in the community can be instructed to plan home visits and evaluate the orthoses.
In conclusion, this study has revealed the most important motivations, barriers and facilitators involved in wearing hand orthoses by DMD patients, which has led to practical and feasible recommendations. This gives us the opportunity to improve care and compliance, and to prevent further shortening of the long finger flexors with the help of orthoses. Additional research on the recommendation to wear hand orthoses, including the timing of their implementation during the course of the disease, is warranted.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
ACKNOWLEDGMENTS
The authors sincerely thank the patients and their primary caregivers for their contribution to this study. We also thank Nick Benders, Laura de Weerd, Femke van Wezel and Marie Ziegler, occupational therapy students at the HAN University of Applied Sciences, Arnhem and Nijmegen, for conducting the interviews and transcripts and for their involvement in the interpretation process.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JND-200506.
REFERENCES
[1] | Birnkrant DJ , Bushby K , Bann CM , Apkon SD , Blackwell A , Brumbaugh D , et al. Diagnosis and management of Duchenne muscular dystrophy, part diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional management. The Lancet Neurol. (2018) ;17: (3):251–67. doi: 10.1016/s1474-4422(18)30024-3 |
[2] | Mendell JR , Lloyd-Puryear M . Report of MDA muscle disease symposium on newborn screening for Duchenne muscular dystrophy. Muscle Nerve. (2013) ;48: (1):21–6. doi: 10.1002/mus.23810 |
[3] | McDonald CM , Henricson EK , Abresch RT , Duong T , Joyce NC , Hu F , et al. Long-term effects of glucocorticoids on function, quality of life, and survival in patients with Duchenne muscular dystrophy: a prospective cohort study. Lancet. (2018) ;391: (10119):451–61. doi: 10.1016/s0140-6736(17)32160-8 |
[4] | Bello L , Gordish-Dressman H , Morgenroth LP , Henricson EK , Duong T , Hoffman EP , et al. Prednisone/prednisolone and deflazacort regimens in the CINRG Duchenne Natural History Study. Neurology. (2015) ;85: (12):1048–55. doi: 10.1212/wnl.0000000000001950 |
[5] | Janssen M , Harlaar J , Koopman B , de Groot IJM . Unraveling upper extremity performance in Duchenne muscular dystrophy: A biophysical model. Neuromuscul Disord. (2019) ;29: (5):368–75. doi: 10.1016/j.nmd.2019.03.006 |
[6] | Janssen MM , Bergsma A , Geurts AC , de Groot IJ . Patterns of decline in upper limb function of boys and men with DMD: an international survey. J Neurol. (2014) ;261: (7):1269–88. doi: 10.1007/s00415-014-7316-9 |
[7] | Weichbrodt J , Eriksson BM , Kroksmark AK . Evaluation of hand orthoses in Duchenne muscular dystrophy. Disabil Rehabil. (2018) ;40: (23):2824–32. doi: 10.1080/09638288.2017.1347721 |
[8] | Lue YJ , Chen SS , Lu YM . Quality of life of patients with Duchenne muscular dystrophy: from adolescence to young men. Disabil Rehabil. (2017) ;39: (14):1408–13. doi: 10.1080/09638288.2016.1196398 |
[9] | Bartels B , Pangalila RF , Bergen MP , Cobben NA , Stam HJ , Roebroeck ME . Upper limb function in adults with Duchenne muscular dystrophy. J Rehabil Med. (2011) ;43: (9):770–5. doi: 10.2340/16501977-0841 |
[10] | Corbin JS , A. Basics of qualitative research: Techniques and procedures for developing grounded theory. 4h ed. SAGE pub: 2015. |
[11] | Connolly AM , Malkus EC , Mendell JR , Flanigan KM , Miller JP , Schierbecker JR , et al. Outcome reliability in non-ambulatory boys/men with Duchenne muscular dystrophy. Muscle Nerve. (2015) ;51: (4):522–32. doi: 10.1002/mus.24346 |
[12] | Brooke MH , Griggs RC , Mendell JR , Fenichel GM , Shumate JB , Pellegrino RJ . Clinical trial in Duchenne dystrophy. I. The design of the protocol. Muscle Nerve. (1981) ;4: (3):186–97. doi: 10.1002/mus.880040304 |
[13] | Joseph M , Constant R , Rickloff M , Mezzio A , Valdes K . A survey of client experiences with orthotics using the QUEST 2.0. J Hand Ther. (2018) ;31: (4):538–43. doi: 10.1016/j.jht.2018.07.002 |
[14] | Wessels RD , De Witte LP . Reliability and validity of the Dutch version of QUEST 2.0 with users of various types of assistive devices. Disabil Rehabil. (2003) ;25: (6):267–72. doi: 10.1080/0963828021000031197 |
[15] | Wagner MB , Vignos PJ Jr , Carlozzi C . Duchenne muscular dystrophy: a study of wrist and hand function. Muscle Nerve. (1989) ;12: (3):236–44. doi: 10.1002/mus.880120313 |
[16] | Craig J , Hilderman C , Wilson G , Misovic R . Effectiveness of Stretch Interventions for Children With Neuromuscular Disabilities: Evidence-Based Recommendations. Pediatr Phys Ther. (2016) ;28: (3):262–75. doi: 10.1097/pep.0000000000000269 |
[17] | Andringa AS , Van de Port IG , Meijer JW . Tolerance and effectiveness of a new dynamic hand-wrist orthosis in chronic stroke patients. NeuroRehabil. (2013) ;33: (2):225–31. doi: 10.3233/nre-130949 |
[18] | Townsend EL , Bibeau C , Holmes TM . Supported Standing in Boys With Duchenne Muscular Dystrophy. Pediatr Phys Ther. (2016) ;28: (3):320–9. doi: 10.1097/pep.0000000000000251 |
[19] | van der Heide L , de Witte L . The perceived functional benefit of dynamic arm supports in daily life. J Rehabil Res Dev. (2016) ;53: (6):1139–50. doi: 10.1682/jrrd.2015.06.0099 |
[20] | Fusch PI & Ness LR . Are We There Yet? Data Saturation in Qualitative Research. The Qual Rep. (2015) ;20: (9):1408–1416. Available from https://nsuworks.nova.edu/tqr/vol20/iss9/3. |
[21] | Swinnen E , Lefeber N , Werbrouck A , Gesthuizen Y , Ceulemans L , Christiaens S , et al. Male and female opinions about orthotic devices of the lower limb: A multicentre, observational study in patients with central neurological movement disorders. NeuroRehabil. (2018) ;42: (1):121–30. doi: 10.3233/nre-172214 |




