Proceedings of the 15th International Newborn Brain Conference: Long-term outcome studies, developmental care, palliative care, ethical dilemmas, and challenging clinical scenarios in neonatal neurology
Systematic review of cerebral palsy in survivors of hypoxic-ischemic encephalopathy in low- and middle-income countries
Antti Kukka1,2, Sara Waheddoost3, Nick Brown1,2, Helena Litorp1,4, Ashish KC1,5
1Department of Women’s and Children’s Health Uppsala University, 2Department of Pediatrics, Gävle Regional Hospital, 3Department of Pediatrics, Karolinska University Hospital, 4Department of Global Public Health, Karolinska Institutet, 5School of Public Health and Community Medicine, University of Gothenburg
BACKGROUND: Cerebral palsy (CP) is the most common motor disorder in childhood. Hypoxic-ischemic encephalopathy (HIE) remains the leading cause of cerebral palsy in low- and middle-income countries (LMICs). We conducted a systematic review and meta-analysis on the prevalence of CP in survivors of HIE in LMICs.
METHODOLOGY: Peer-reviewed original articles were searched from November 2009 to November 2021 as previously published (1). The search was updated on 14/10/2023 with modified inclusion criteria:
-LMIC by World Bank classification
-Gestational age at birth ≥35 weeks
-Clinical diagnosis of CP ≥1 year of follow-up
-Clinical diagnosis of encephalopathy ≤24 hrs of birth
-Proof of asphyxia, any of:
oAbnormal umbilical cord or neonatal blood sample ≤1 hr of birth (pH ≤7.1 or base excess ≤-12 or lactate ≥6)
oApgar score ≤6 at 5 or 10 min
oResuscitation at 5 or 10 min
oNo cry by 5 or 10 min
oSentinel event
Two reviewers independently screened first all the titles and abstracts, and then full texts to determine inclusion. Risk of bias was assessed using modified Newcastle Ottawa Scale for cohort studies. Forest plots with 95% confidence intervals (CI) were created with Freeman Tukey double arcsine transformation and meta-analyses were conducted using inverse variance of heterogenicity model in MetaXL V.5.3.
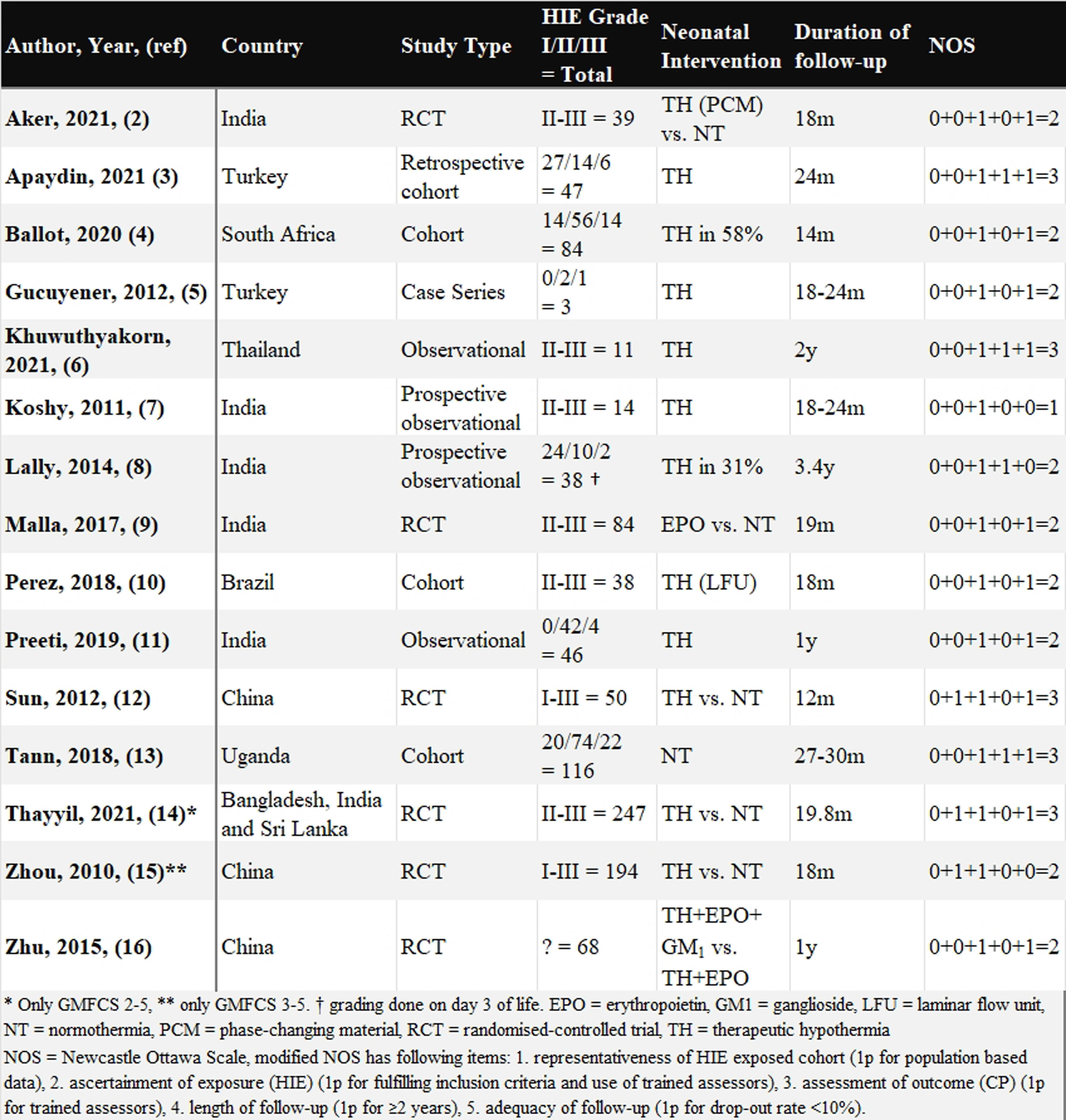
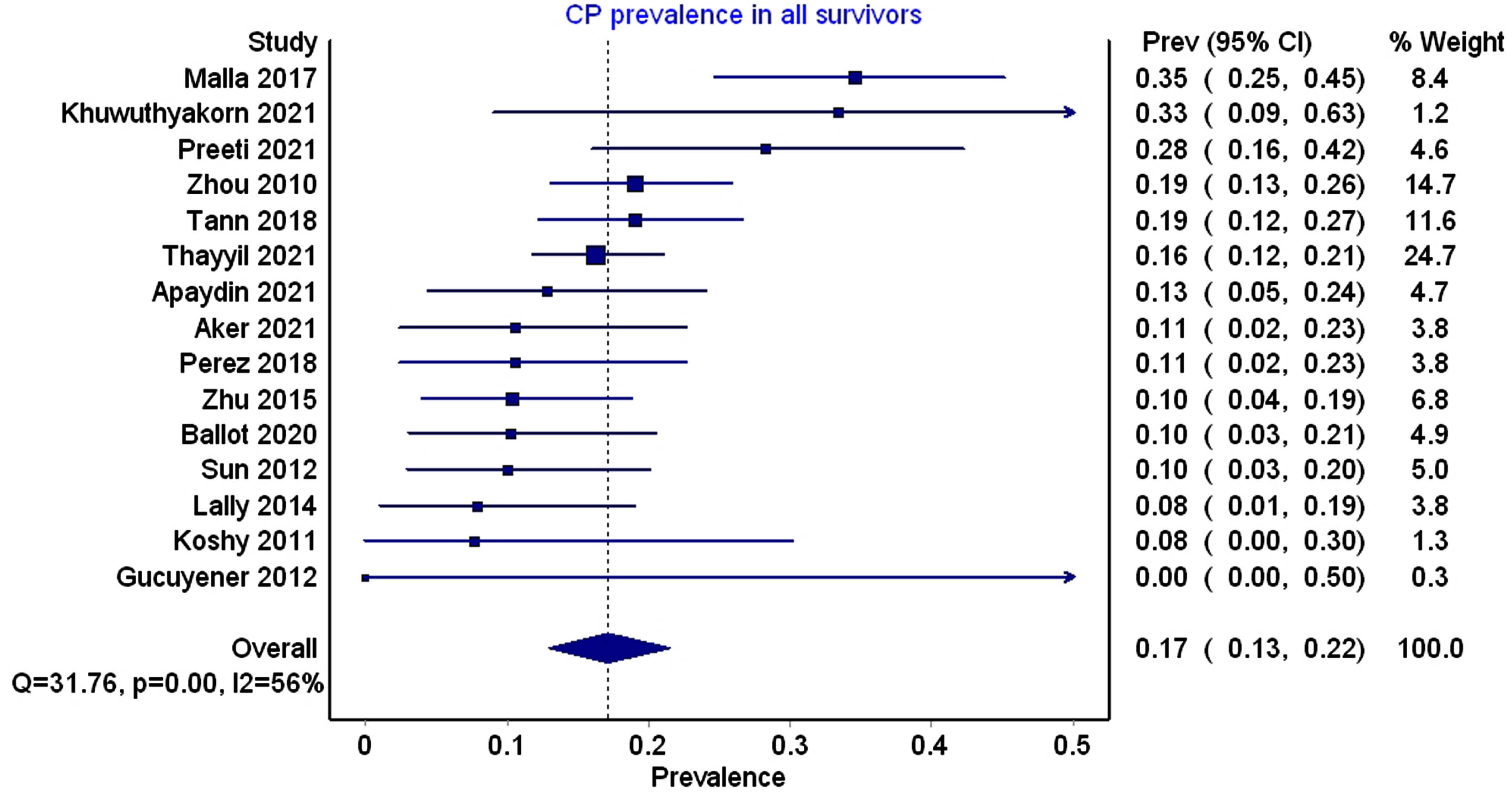
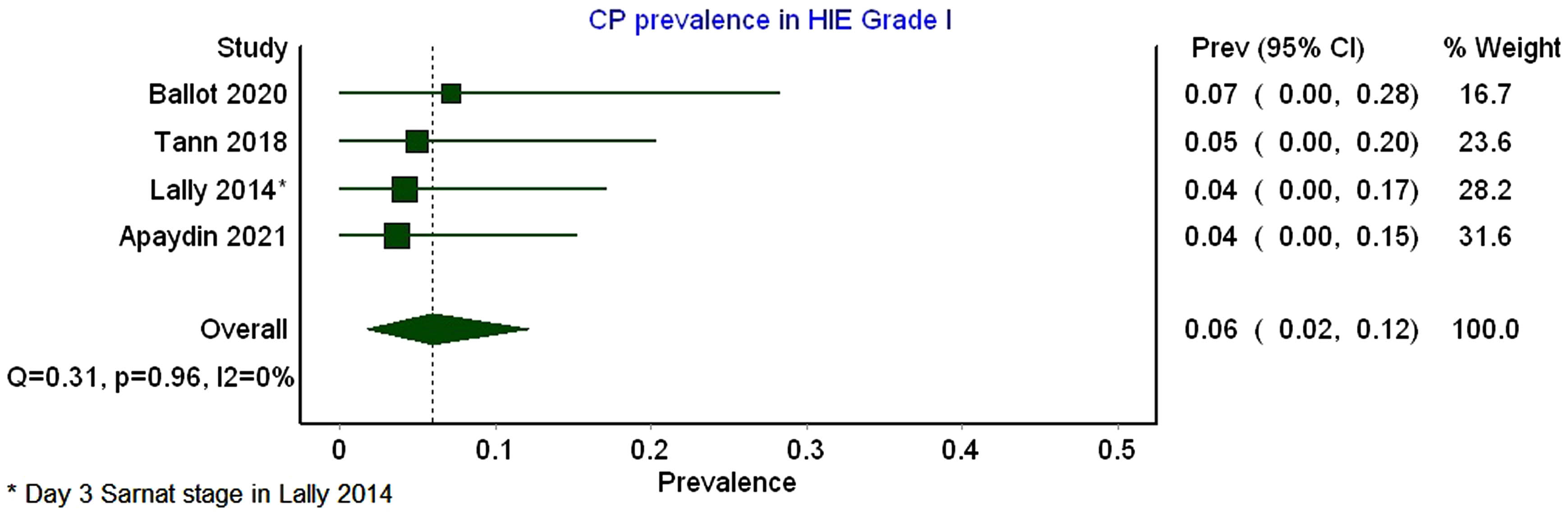
RESULTS: original search produced 1322 unique records and the update 199 new titles and abstracts that were screened. Full-text evaluation of 272 records resulted in 15 included papers (Table 1). High risk of bias was identified due to most studies being from tertiary hospitals. Altogether 995 infants who survived HIE were included out of whom 171 (17%, 95% CI 13-22%) developed CP (Figure 1). The estimate did not change by limiting results to those with follow-up of ≥2 years. Few studies reported outcomes disaggregated by severity of HIE, which showed clear association to risk of CP: mild 6% (95% CI 2-12%, 4 studies, Figure 2), moderate 18% (13-24%, 4 studies) and severe 42% (11-76%, 4 studies).
CONCLUSION: Approximately one fifth of HIE survivors develop cerebral palsy in LMICs. Even infants with mild HIE are at risk. Targeted neonatal follow-up programs are needed to provide early intervention for these children
BIBLIOGRAPHY:
1. Kukka et al. BMJ Glob. Health. 2022;7:e010294
2. Aker et al. Arch. Dis. Child. Fetal Neonatal Ed. 2022;107:32–8
3. Apaydin et al. Early Hum. Dev. 2021;163:105487
4. Ballot et al. SAMJ. 2020;110:308–312
5. Gucuyener et al. Brain Dev. 2012;34:280–286
6. Khuwuthyakorn et al. Arch. Dis. Child. 2021;106:516–517
7. Koshy et al. Indian Pediatr. 2011;48:982–3
8. Lally et al. PLOS ONE 2014;9:e87874
9. Malla et al. J Perinatol. 2017;37:596–601
10. Perez EC Paediatr. 2018;7:1073–1078
11. Preeti et al. J. Neonatal-Perinat. Med. 2019;12:127–134
12. Sun et al. Acta Paediatr. 2012;101:e316–e320
13. Tann et al. EClinicalMedicine 2018;6:26–35
14. Thayyil et al. Lancet Glob. Health 2021;9:e127385
15. Zhou et al. J. Pediatr. 2010;157:367–3
16. Zhu et al. Eur. Rev. Med. Pharmacol. Sci. 2015;19:3955–3960
Neurobehaviour of HIV-exposed infants - the need for monitoring and intervention in the newborn period
Gina Rencken1
1University of Kwazulu Natal
BACKGROUND: The newborn infant is a complexly organized, competent being, who plays an active role in shaping their environment through their increasing skills in autonomic regulation, motor control, regulation of state and social interaction. Infants born to HIV positive mothers, are exposed to HIV and antiretroviral therapy inutero, and may experience adverse effects from this.
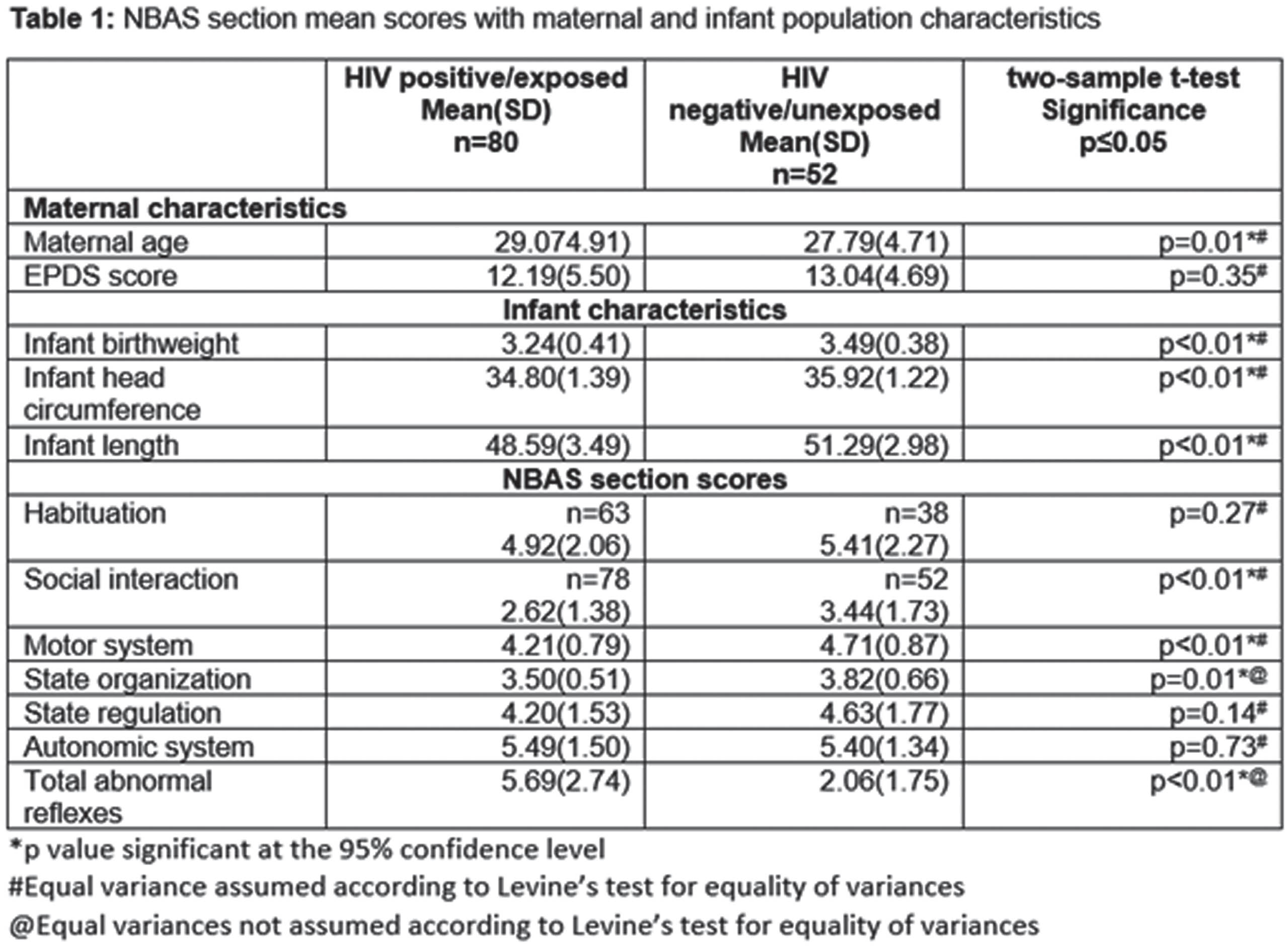
METHODS: A cross-sectional study of 132 mother-infant dyads from a large public health hospital in South Africa were assessed using the Neonatal Behavioural Assessment Scale and the Edinburugh Postnatal Depression Scale on day two of life. Medical and demographic data was collected, including maternal age, HIV status, length of time on antiretrovirals, relationship status, employment status, gravid status, mode of delivery, infant anthropometrics and infant gender. Data was input into IBM SPSS statistics 21, where frequencies and percentages for descriptive analysis, and Chi-square and student’s two sample t-tests were run to compare data from HIV infected-exposed and HIV uninfected-unexposed mothers and infants.
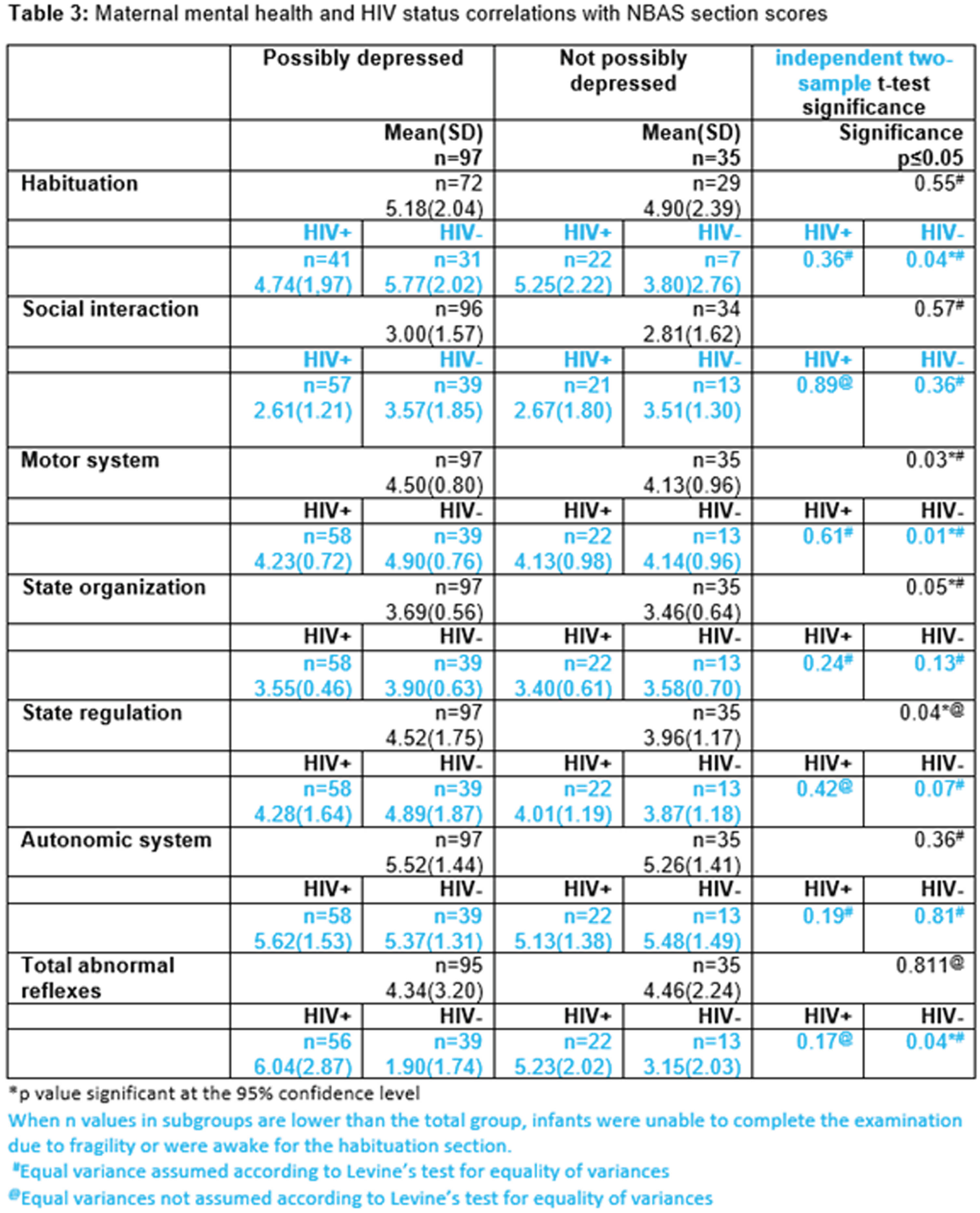
RESULTS: HIV exposed infants were smaller than HIV unexposed infants, even though low birth weight was an exclusion criteria. Statistically significant differences were found between HIV exposed and unexposed infants in neurobehavioiral items of social interaction (p = 0.00), motor system (p = 0.00) and state organization (p = 0.01), with HIV exposed infants performing less optimally in these domains. HIV exposed infants also presented with more abnormal reflexes. Infants born to depressed mothers showed superior motor skills, state organization and state regulation than infants born to mothers who did not score in the possibly depressed range.
CONCLUSION: HIV exposed infants have inferior neurobehavioural functioning, which may affect their quality of life and ability to develop a reciprocal relationship with a primary caregiver. This may have an effect on development, behaviour and mental health in later childhood. HIV exposed infants should be monitored closely and their functioning in autonomic stability, motor control, regulation of state and social interaction assessed regularly. Guidance for caregivers in incorporating strategies into the care of these infants is essential to buffer the possible long term negative effects on development.
BIBLIOGRAPHY:
1. Brazelton TB, Nugent KJ. The neonatal behavioural assessment scale, fourth edition. Clinics in Developmental Medicine No.190. Mac Keith Press; 2011.
2. Ibanez G, Charles M, Firhan A, et al. Depression and anxiety in women during pregnancy and neonatal outcome: Data from the EDEN mother–child cohort. Early Human Development. 2012;88980:643–9.
3. World Health Organization (WHO) (2013, 30 June) Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection’ ISBN 978 92 4 154968 4.
4. Delicio AM, Lajos G J, Amaral E, et al. Adverse effects of antiretroviral therapy in pregnant women infected with HIV in Brazil from 2000 to 2015: a cohort study. BMC Infectious Diseases. 2018;18(485).
Cord blood inter-alpha inhibitor levels: potential neonatal brain health biomarkers in hypoxic ischemic encephalopathy
Lynn Bitar1, S. Stonestreet2, Yow-Pin Lim2, Xiaodi F. Chen2, Yu-Lun Liu1, Lina Chalak1, Srinivas Kota
1Division of Neonatal-Perinatal Medicine, University of Texas Southwestern Medical Center, USA, 2The Warren Alpert Medical School of Brown University
BACKGROUND: Neonates are at risk for infection and inflammation because of their immature immune systems. Inter-alpha inhibitor proteins (IAIPs) are a family of endogenous proteoglycans with a wide range of immunomodulatory effects. Reductions in IAIPs levels have been reported in inflammatory conditions including sepsis and necrotizing enterocolitis. Animal studies have also shown low levels of IAIP in hypoxic ischemic encephalopathy (HIE). The focus of this study is to determine blood IAIP concentrations in neonates with HIE.
METHODS: This is a single-center prospective cohort study of newborns born at or after 36 weeks of gestation who were admitted to the intensive care unit of Parkland Health hospital over a one-year period. Blood samples from the umbilical artery (UmA) were collected from neonates before and after placental delivery to measure IAIP levels in three different groups of infants. Term pregnancies were divided into three groups: Group 1 “reference control” included uncomplicated term births delivered by repeat cesarean-section in the absence of labor, group 2 “triple threat” group consisted of women with clinical chorioamnionitis, non-reassuring fetal heart pattern or meconium-stained amniotic fluid with fetal acidosis, whereas group 3, consisted of newborns with moderate or severe hypoxic ischemic encephalopathy (HIE) who met criteria to receive therapeutic hypothermia. Blood levels of IAIPs were quantitatively measured by a competitive ELISA using monoclonal antibodies specifically against human IAIPs.
RESULTS: The study included a total of 57 newborns: control (Group 1, n=9), triple threat (Group 2, n=4) and moderate and severe HIE (Group 3, n=44) groups. Measurement of IAIP cord serum concentrations in each of the study groups revealed a significant decrease in IAIP concentrations (p=0.002) in the moderate to severe HIE group compared with each of the other study groups (Figure 1).
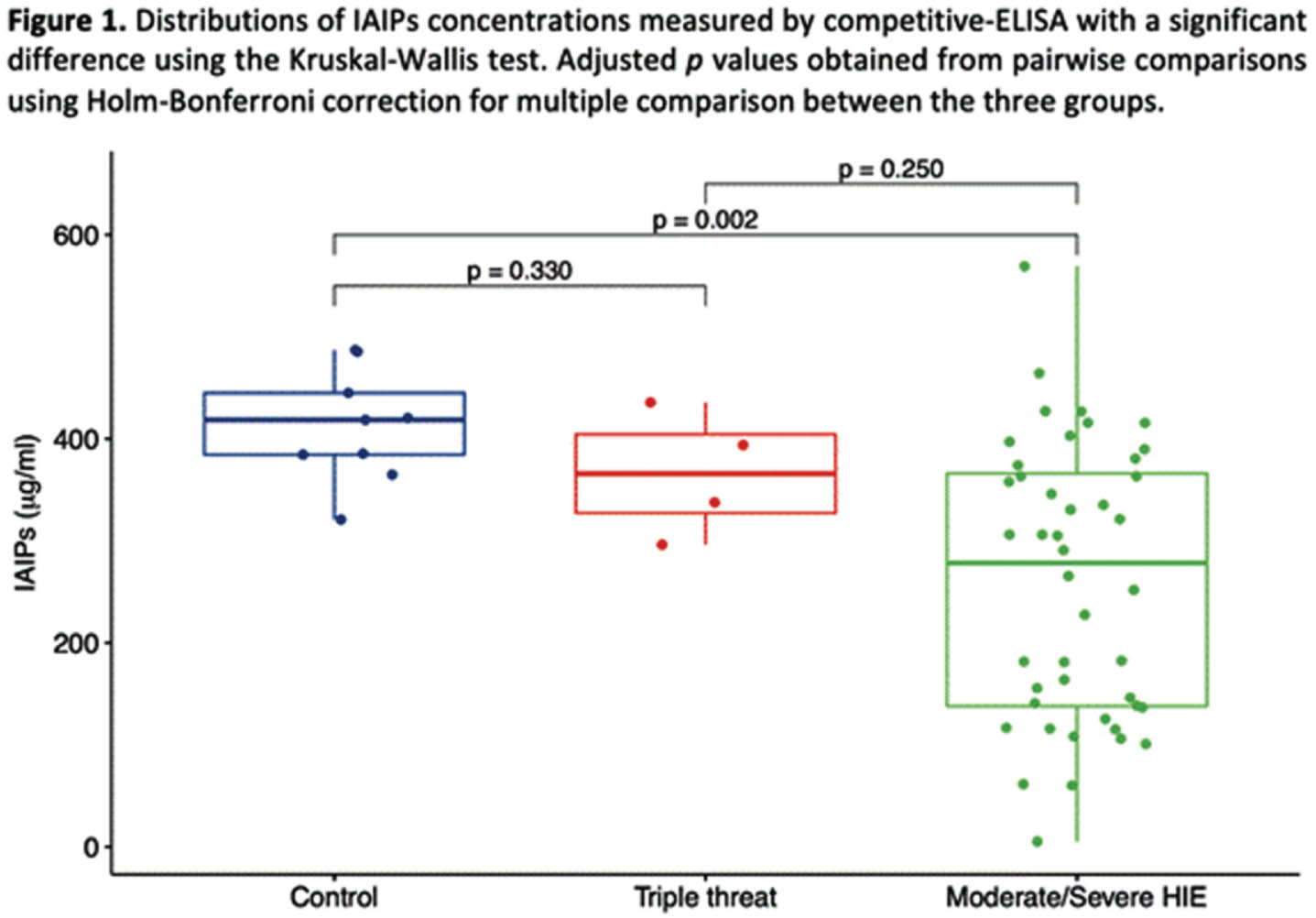
CONCLUSION: Infants exposed to moderate to severe HIE have lower concentrations of IAIPs in umbilical arterial cord blood than healthy full-term control infants and infants exposed to a “triple threat.” These findings suggest that there is a potential utility of IAIP concentrations in cord blood as biomarkers to determine infants potentially at risk for HIE in neonates. Furthermore, future work could examine the relationship between IAIP concentrations and the severity of HIE. IAIP levels could have diagnostic and therapeutic implications in the management of HIE.
Association between childcare arrangements and language development in preterm children: a cross-sectional study
Ludovic Legros1, Stéphanie De Leeuw1, Gilda Delens1
1Chr Sambre Et Meuse
BACKGROUND: Despite advances in perinatal care, prematurity remains a significant contributor to neurodevelopmental comorbidities, including language delay. In addition to perinatal risk factors associated with prematurity, language development is significantly impacted by the child’s environment. Notably, former preterm infants are often kept away from daycare settings during their early years due to their increased vulnerability to community-acquired infections. However, daycare settings create a favorable environment by providing rich language exposure, fostering social interactions with both peers and caregivers, and facilitating access to early childhood professionals. These factors may have the potential to influence the language development of former preterm infants. Yet, the potential impact of prolonged social exclusion on language development has not been extensively studied. This study aims to investigate the influence of daycare attendance on language development among preterm children at two years corrected age (CA).
METHODOLOGY: This retrospective cross-sectional study included 78 preterm infants, born between January 1, 2017, and December 31, 2019, with a gestational age <32 weeks and/or a birthweight <1500 g, who underwent neurodevelopmental assessment at two years CA. Language development was assessed using the Bayley Scales of Infant-Toddler Development, third edition (Bayley-III). Children attending daycare (n = 42; defined by attending daycare at least once a week) were compared to children exclusively cared for by their parents or close family members (n = 36) (Table 1). We conducted a relative risk (RR) analysis to explore the association between daycare attendance and the risk of language delay (Bayley-III language composite score < 85) (Figure 1).
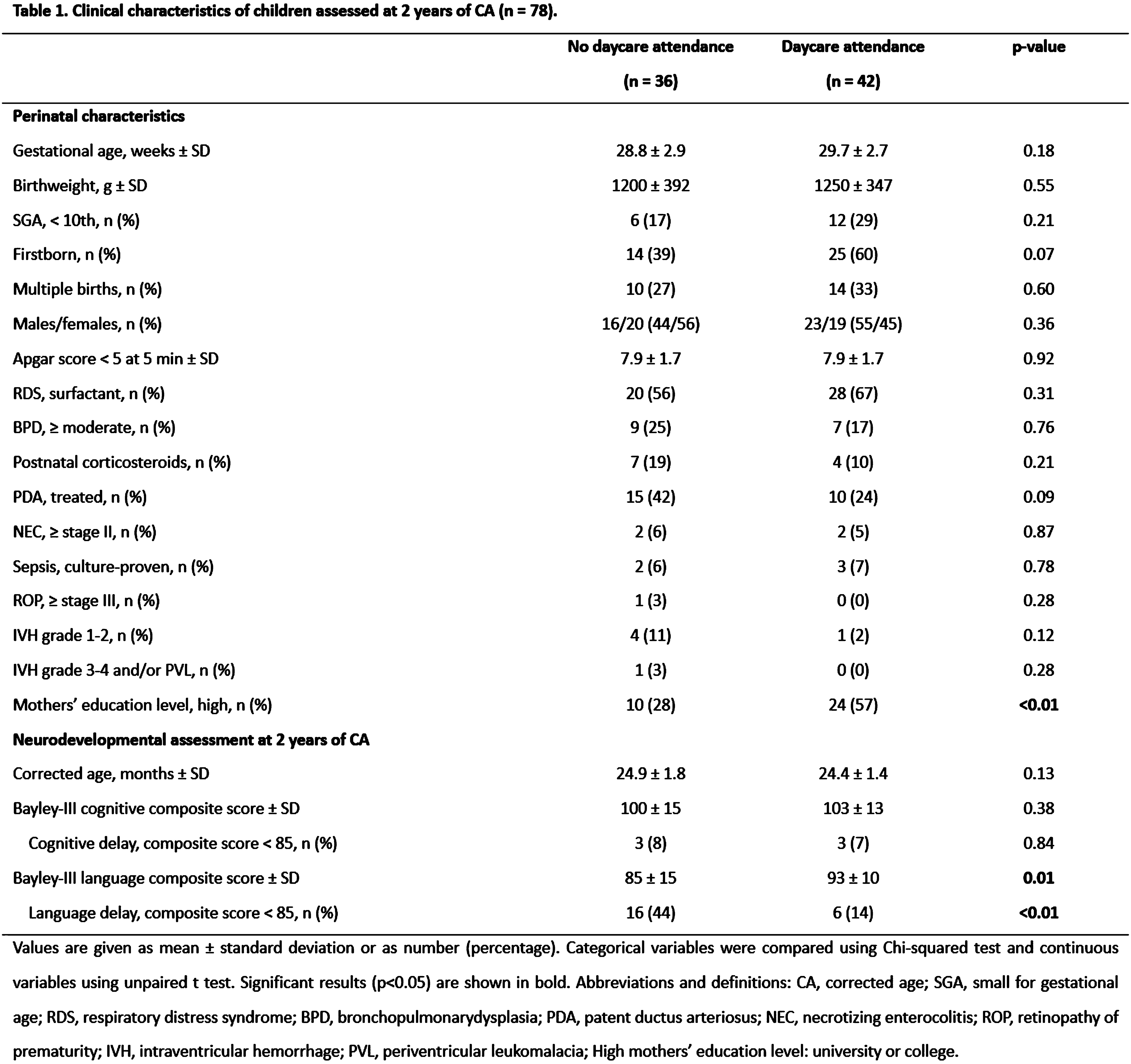
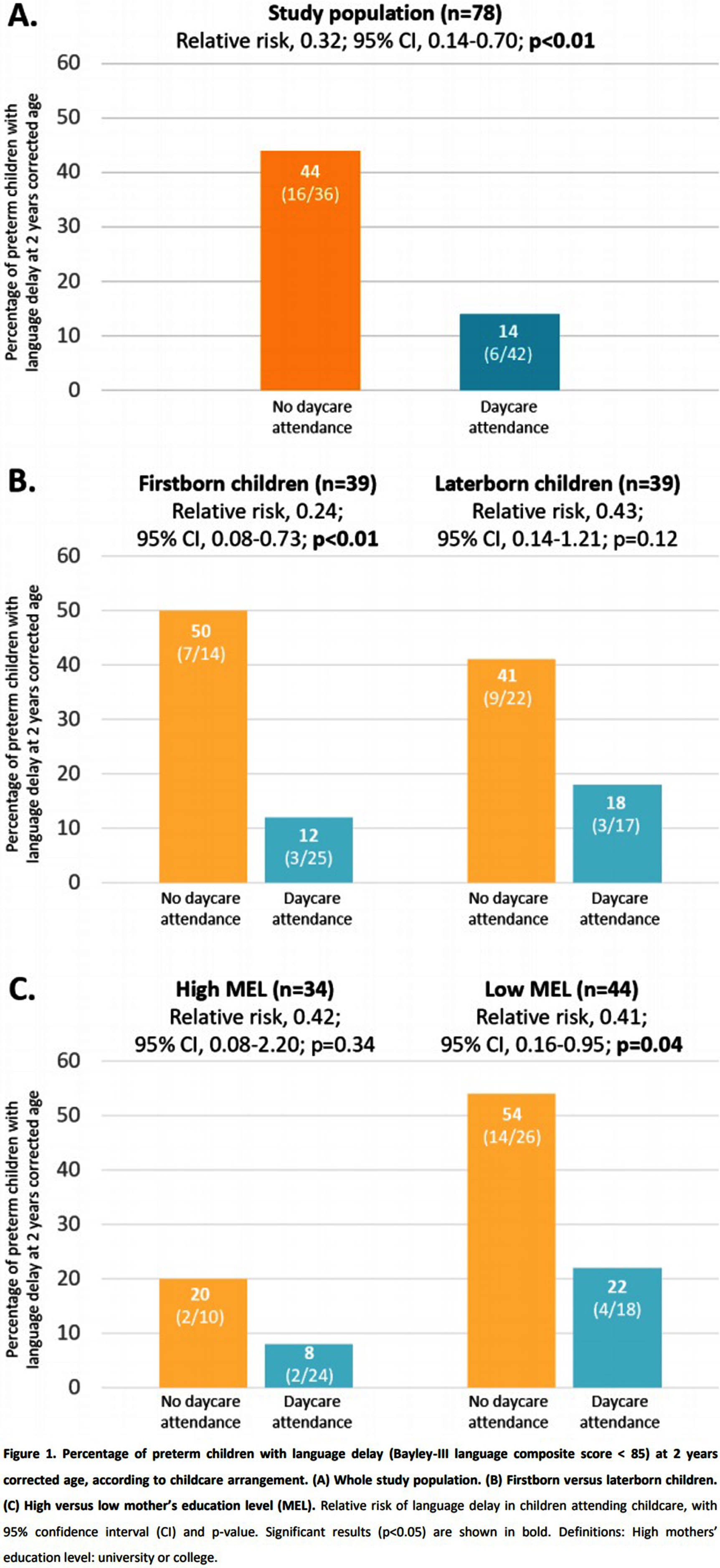
RESULTS: The prevalence of language delay was significantly lower in the daycare group (14% versus 44%, p<0.01) (Table 1). Relative risk analysis showed a protective and significant association between daycare attendance and language delay (RR 0.32, 95% confidence interval (CI) 0.14-0.70, p<0.01). Since the daycare group contained more laterborn and individuals with a high level of mother’s education (MEL), we conducted a subgroup analysis, which revealed a significant impact of daycare within the firstborn and low MEL group (respectively RR 0.24, 95% CI 0.08-0.73, p<0.01; and RR 0.41, 95% CI 0.16-0.95, p=0.04) (Figure 1). Moreover, in all the subgroups, the prevalence of language delay was lower among children attending daycare.
CONCLUSION: Daycare attendance appears to have a positive impact on language development at two years CA in preterm children, particularly among firstborn and children with low MEL. These findings underscore the importance of language stimulation and child’s environment in the language development of preterm children.
BIBLIOGRAPHY:
1. Flensborg-Madsen, T., Grønkjær, M., & Mortensen, E. L. (2019). Predictors of early life milestones: Results from the Copenhagen Perinatal Cohort. BMC pediatrics, 19(1), 420.
2. Vohr B. (2014). Speech and language outcomes of very preterm infants. Seminars in fetal & neonatal medicine, 19(2), 78–83.
Early shared reading influence on language skills at 2 years corrected age in preterm children
Ludovic Legros1, Gilda Delens1
1Chr Sambre Et Meuse
BACKGROUND: Preterm children are at risk for language development delays. Early shared reading has been demonstrated to enhance language development and functional brain connectivity in full-term children. Therefore, recent research examines the potential benefits of NICU reading programs for the language development of preterm children. Indeed, early reading to preterm newborns improves their direct exposure to parental voices and facilitates contingent communication. Children’s books provide parents with a more structured framework for interacting with their infants, offering enriched linguistic input characterized by richer language and grammar. It also enhances parental involvement and sense of control. Furthermore, NICU reading programs may have lasting effects by encouraging ongoing reading practices after discharge. Consequently, this study aims to evaluate the impact of reading habits during the first two years of life following NICU discharge (including a NICU reading program) on language development.
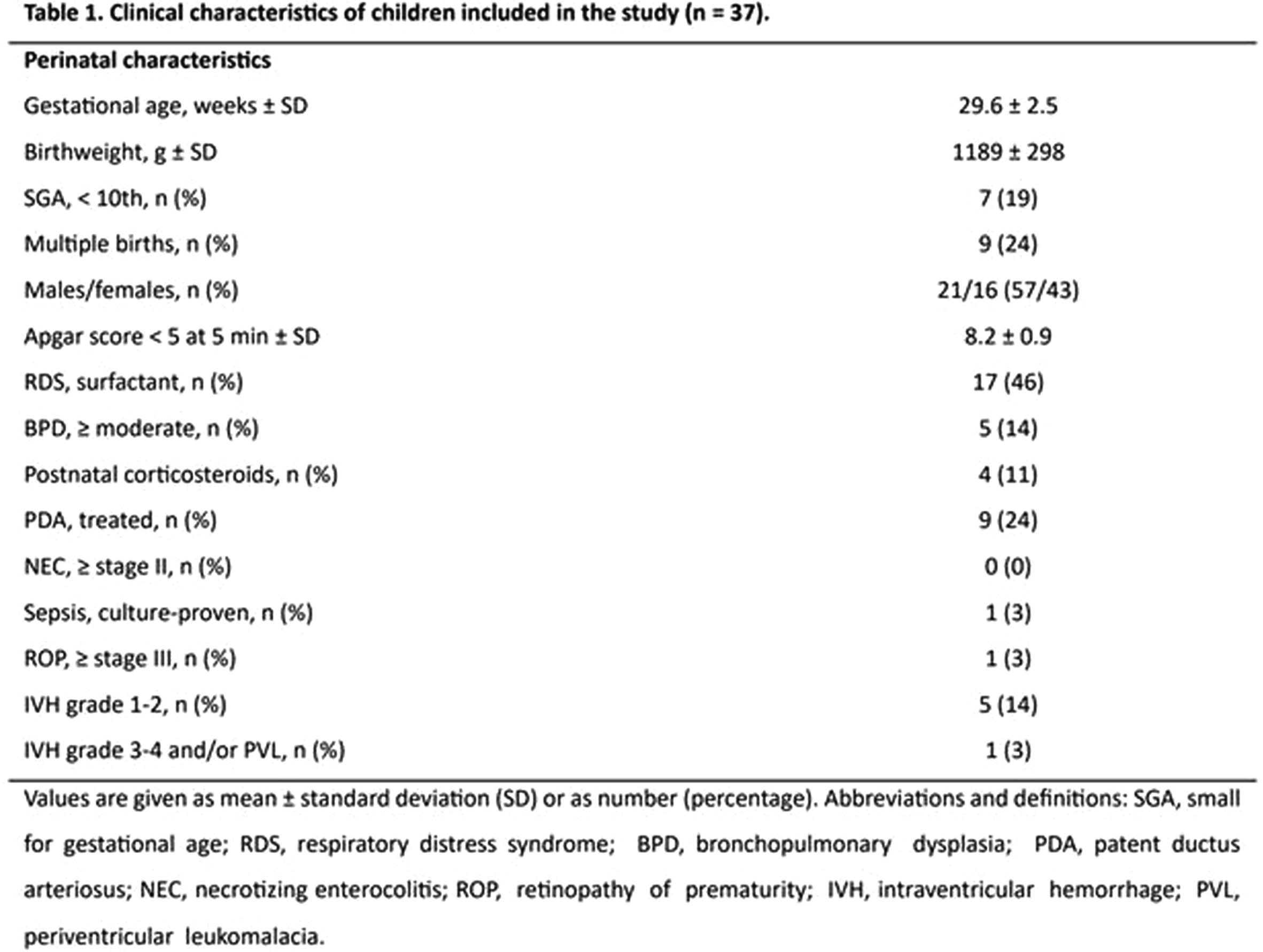
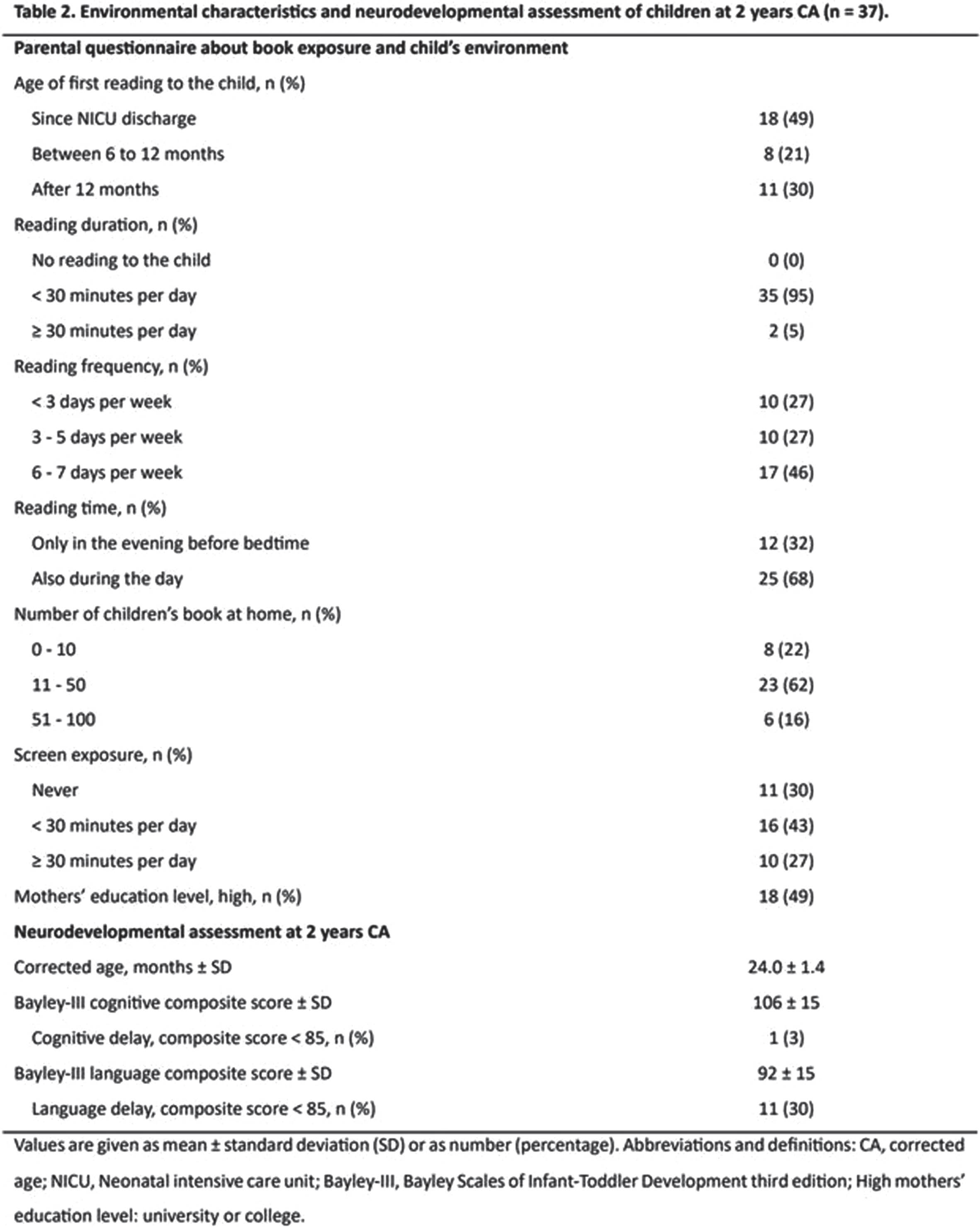
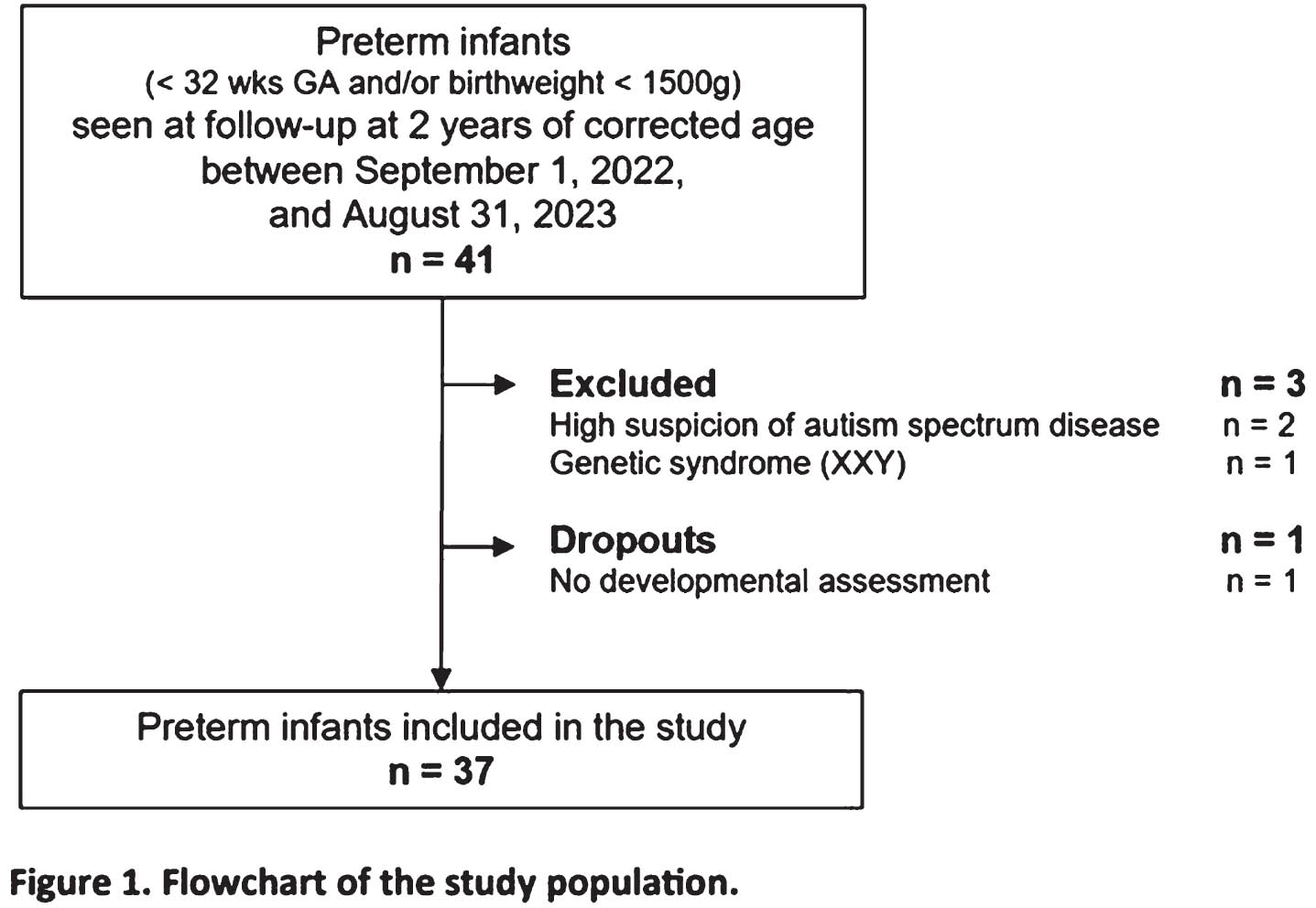
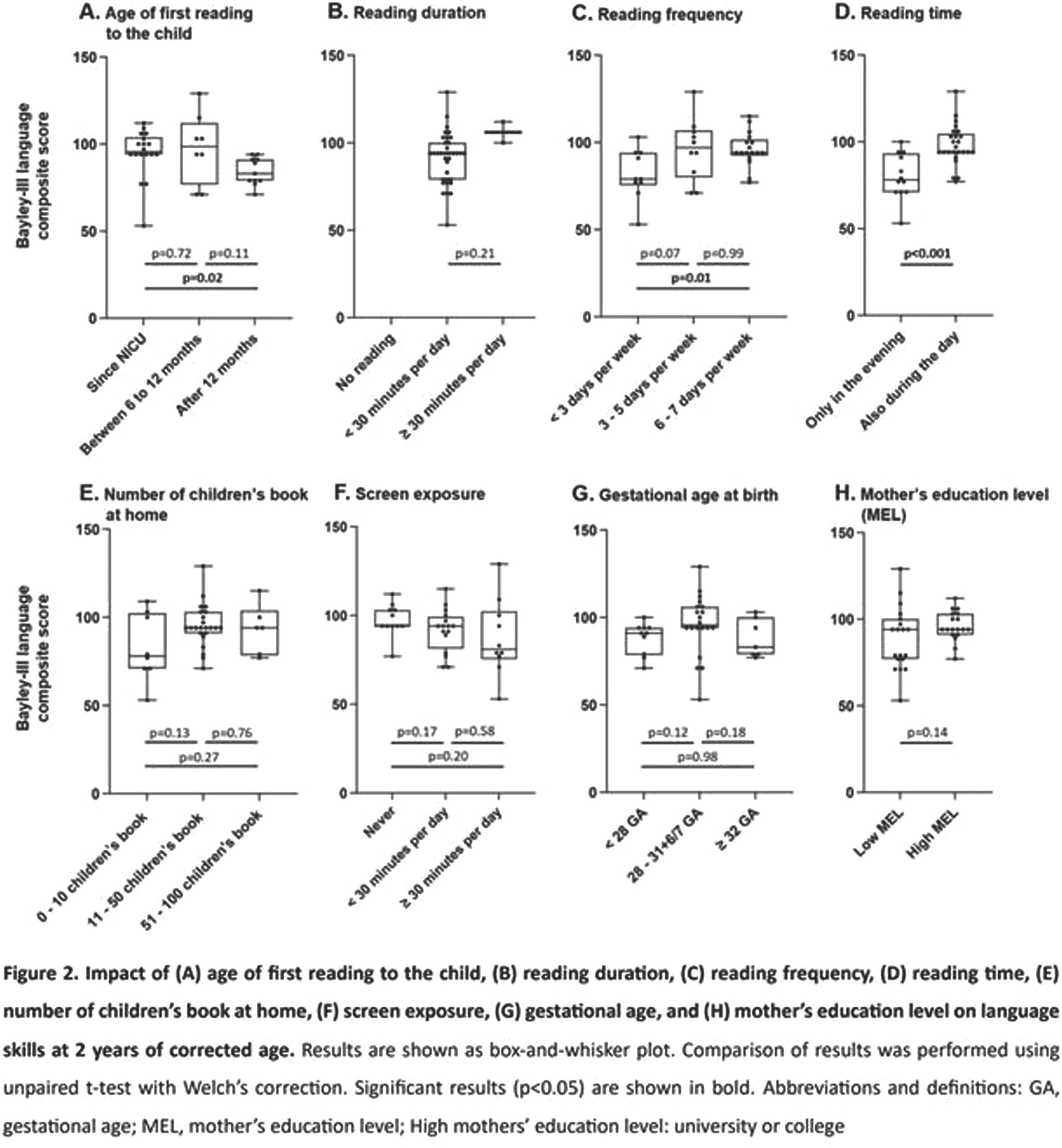
METHODOLOGY: This prospective cross-sectional study included 37 preterm infants born with a gestational age of <32 weeks and/or a birthweight of <1500 g. These infants underwent neurodevelopmental assessments at two years corrected age (CA), including a language assessment by the Bayley Scales of Infant-Toddler Development, third edition (Bayley-III). Simultaneously, parents completed a questionnaire regarding their reading habits during the first two years of life. An unpaired t-test with Welch’s correction was employed to compare the language scores (Bayley-III language composite scores) among groups with varying responses to reading exposure and to child’s environment. The results are visually represented in a box-and-whisker plot.
RESULTS: In our study, the mean Bayley-III language composite score at two years CA was 92 ± 15. Approximately half of the parents (49%) continued to engage in shared reading with their child immediately after NICU discharge, while the vast majority of parents (95%) read to their child for less than 30 minutes daily. Significantly, language scores showed associations with the age of first shared reading after discharge (p=0.02), the frequency of reading (p=0.01), and the timing of reading (evening-only vs. also during the day; p<0.001). Conversely, in our cohort, factors such as the number of children’s books at home, screen exposure, and mother’s education level did not have significant impacts on language scores.
CONCLUSION: The age of first shared reading and book exposure during the first years of life appear to have a positive impact on language development at two years CA in preterm children. Although our study is limited by its small sample size and the absence of a historical control group before NICU reading programs, our results remain robust and underscore the crucial role of early shared reading for preterm children.
BIBLIOGRAPHY:
Boissel L, Guilé JM, Viaux-Savelon S, et al. A narrative review of the effect of parent-child shared reading in preterm infants. Front Pediatr. 2022;10:860391
A QI initiative to optimize attendance rates at a NICU high risk follow-up program
Tatiana Nuzum, Robert Angert, Ashley Duhaime, Sadaf Kazmi
1Hassenfeld Children’s Hospital at NYU Langone, 2NYCH+H Bellevue Hospital Center
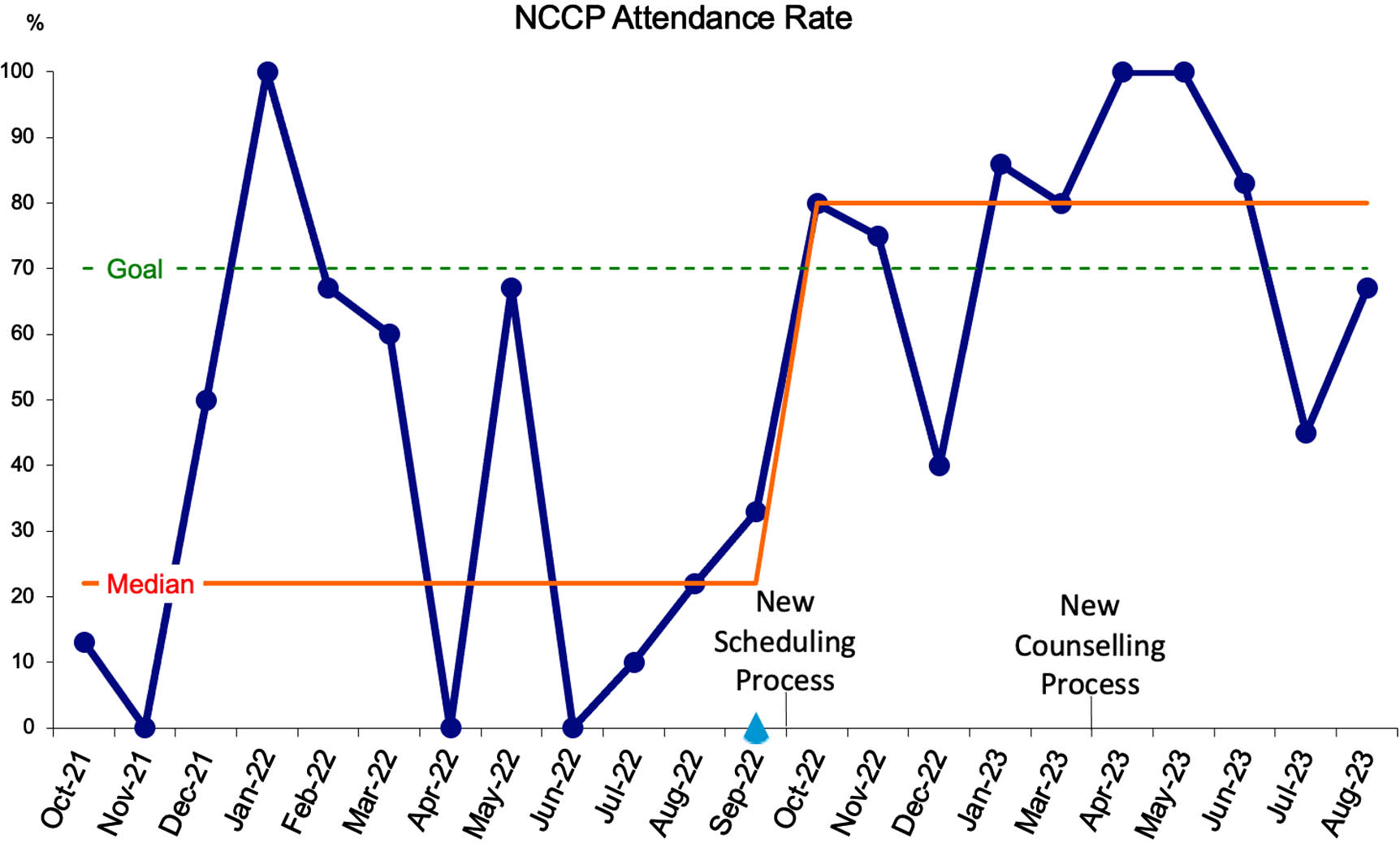
BACKGROUND: NICU graduates are at high-risk for neurodevelopmental impairment (NDI), especially those born premature or with neurologic injuries. Our Neonatal Comprehensive Care Program (NCCP) is a high-risk neurodevelopmental follow-up clinic that performs developmental assessments, to ensure that NDI is detected early. NCCP follows eligible graduates from two Level IV NICUs – NYU Langone and Bellevue Hospital Centers. Bellevue Hospital (BH) serves a more diverse, socioeconomically disadvantaged population. Over a 1-year period, we noted that NCCP 1st-visit attendance rates for NYU infants was 70% but only 30% for BH infants. We also saw that more than half of BH infants with neurologic injury were never scheduled for NCCP.
OBJECTIVE: To improve attendance rates of BH patients at 1st-visit appointments to 70% over one year from October 2022 to September 2023.
METHODS: Baseline attendance rates were collected from October 2021 to September 2022. A Key Driver Diagram (Figure 1) and Process Map were formulated to guide our approach, which included a new scheduling process (PDSA #1) and counselling process (PDSA #2).
Scheduling process (PDSA #1 Oct 2022): The scheduling process was adjusted so that all eligible infants were scheduled for an appointment prior to discharge and that information was included in the discharge summary. Online and EMR tracking systems were created to serve as reminders for when infants should be referred and scheduled. Accurate contact information and language of preference was obtained from caregivers prior to discharge, to allow for reminder calls one week prior to scheduled appointments.
Counseling process (PDSA #2 Apr 2023): The responsibility of counselling caregivers prior to discharge on the importance of NCCP was transferred to part of the medical team that was familiar with the clinic and had been provided education. A counselling script was created to ensure consistent, accurate information was provided. A clinic brochure, available in multiple languages, was also provided. We then followed attendance rates prospectively for 12 months to evaluate for change.
RESULTS: Median attendance rates improved from 22% to 80% following study interventions (Figure 2). Monthly attendance varied between 40-100%. Three to eleven infants were scheduled each month. No eligible infants were discharged home without being referred to NCCP.
CONCLUSION: A comprehensive scheduling and counselling process tailored to the needs of our population proved to be successful in improving NCCP attendance rates. Attendance rates exceeded the goal of the study team, which was set in an attempt to achieve equity between our clinic populations. Continuing to track attendance will determine long-term sustainability of these interventions.
Postoperative neuromonitoring is associated with neurodevelopmental outcome in infants with d-transposition of the great arteries
Anurudhya Karthikeyan1,2, Rashed Chowdhury1,2, Bohdana Marandyuk1, Joaquim Miro3, Nancy Poirier3, Anne-Monique Nuyt1,4, Anne Gallagher1,5, Marie-Josée Raboisson3, Mathieu Dehaes1,2,6
1Research Center, Sainte-Justine University Hospital Centre, 2Institute of Biomedical Engineering, University of Montreal, 3Department of Cardiology, Sainte-Justine University Hospital Centre, Université de Montréal, 4Department of Pediatrics, Sainte-Justine University Hospital Centre, Université de Montréal, 5Department of Psychology, Sainte-Justine University Hospital Centre, Université de Montréal, 6Department of Radiology, Radio-oncology and Nuclear Medicine, University of Montreal
BACKGROUND AND OBJECTIVE: D-transposition of the great arteries (dTGA) is the second most severe cyanotic congenital heart disease and requires reparative surgery early in life1. While reparative surgery has improved survival rates2, infants with dTGA are at risk of adverse neurodevelopmental outcomes3, 4. The identification of early biomarkers of brain health may help to improve risk stratification and neurodevelopmental outcome. Our objective was to examine the associations between early postoperative cerebral metabolic/hemodynamic parameters and 2-year neurodevelopmental outcome in infants with dTGA.
METHODOLOGY: In our single-center prospective observational study, 35 infants with dTGA were recruited between 2017 and 2021. Exclusion criteria included infants born prematurely, low birth weight, genetic syndrome, other cardiac defects, and previous cardiac surgeries. Non-invasive bedside optical neuromonitoring was used to measure cerebral hemoglobin oxygen saturation and an index of microvascular cerebral blood flow during the 72h following the end of aortic cross-clamping. Peripheral arterial oxygen saturation and blood hemoglobin concentration were retrieved from the medical charts during this period and used to estimate indices of cerebral oxygen metabolism and oxygen delivery. Timepoint measurements were averaged over the 72h period. Neurodevelopmental outcome was assessed at 2 years of age using the Bayley scales of infant and toddler development Ed. III and IV. Spearman’s rank correlation test was used to examine the associations between cerebral metabolic/hemodynamic parameters and neurodevelopmental scales. Benjamini-Hochberg method was used to correct for multiple comparisons.
RESULTS: Patient demographics and clinical variables are showed in Table 1. Postoperatively, indices of cerebral blood flow and oxygen delivery were positively associated with both language receptive communication (p=0.048; rho=0.46 and p<0.001; rho=0.70, respectively) and gross motor (p=0.048; rho=0.46 and p<0.01; rho=0.54, respectively) scores.
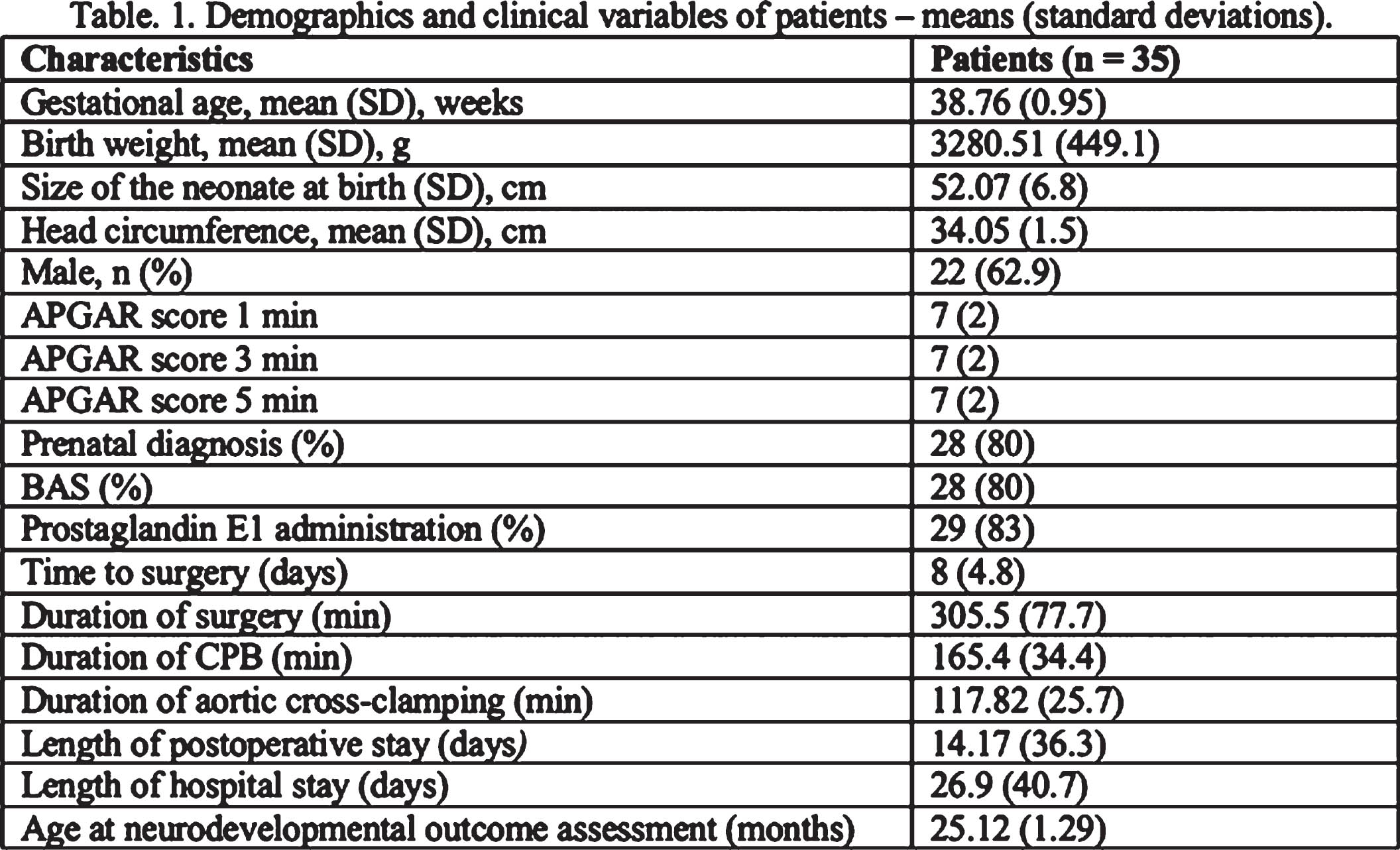
CONCLUSION: Higher cerebral blood flow and delivery indices measured in the early postoperative period may reflect a better hemodynamic transition to normal circulation and recovery in infants with dTGA5. Their associations with 2-years Bayley scales suggest their potential importance as biomarkers of brain health and neurodevelopment. These results suggest the inclusion of bedside optical neuromonitoring to evaluate early neurodevelopmental risk and as a potential screening tool to assess neuroprotective intervention strategies.
BIBLIOGRAPHY:
1. Castaneda, A., Thorac Cardiovasc Surg, 1991. 39 Suppl 2: p. 151-4.
2. Morfaw, F., et al., Syst Rev, 2020. 9(1): p. 231.
3. Rollins, C.K., Newburger, J. W., Circulation, 2014. 130(14): p. 124-126.
4. Marino, B.S., et al., Circulation, 2012. 126(9): p. 1143-72.
5. Villafane, J., et al., J Am Coll Cardiol, 2014. 64(5): p. 498-511.
Efficacy of the brief ADEC for autism spectrum disorder screening in NICU follow up
Darrah Haffner1, Ann Levine1, Lindsay Bartram2, Joseph Stanek1, Laurel Slaughter1, Nathalie Maitre3
1Nationwide Children’s Hospital/Ohio State University College of Medicine, 2Atrium Health/Wake Forest University School of Medicine, 3Children’s Healthcare of Atlanta/Emory University School of Medicine
BACKGROUND: The prevalence of autism spectrum disorder (ASD) is high amongst children who required the Neonatal Intensive Care Unit (NICU), including those with history of preterm birth(1). However, there are no recommendations for enhanced screening of ASD in this population. Observational screening tools may be most appropriate for this purpose due to co-occuring conditions(2). We aimed to assess the efficacy of the Brief Autism Detection in Early Childhood (BADEC) to identify children in a NICU Follow Up Program at high risk for ASD.
METHODS: The BADEC is a shortened version of the ADEC, a level 2 direct observational screening tool that has good validity in assessing ASD risk in NICU Follow Up. Two versions have been proposed, each containing five different overlapping items from the original ADEC (Table 1)(4,5). Items are administered in a standardized manner over 5 minutes. Best estimate clinical diagnoses (BEC) were based on DSM-5 criteria. Children considered at high risk were referred for clinical ASD evaluations. Sensitivity, specificity and area under the curve (AUC) were calculated. Spearman’s correlation coefficients were used to assess BADEC scores with Bayley-III scores.
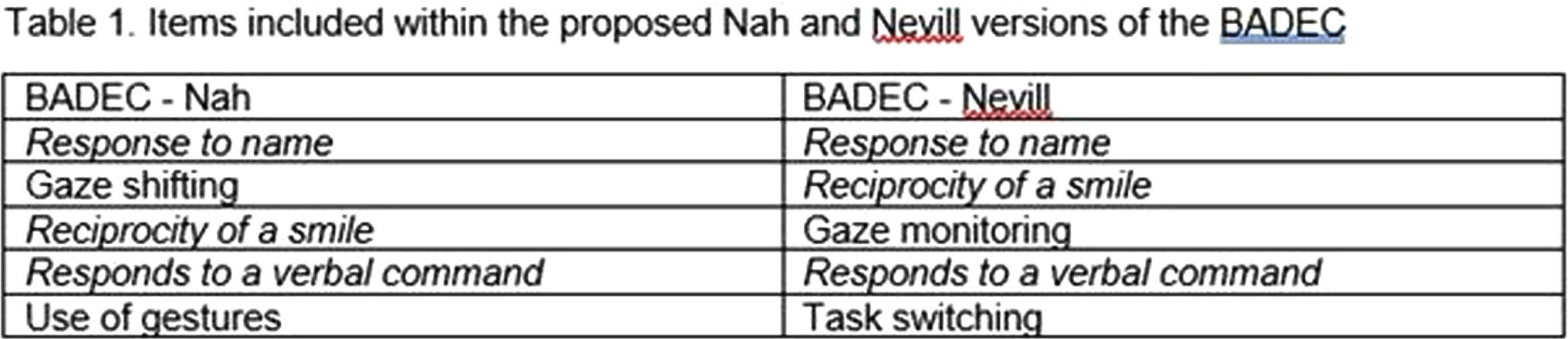
RESULTS: 69 children (mean gestational age 28 weeks) were included; 9 were ultimately diagnosed with ASD. Twelve (17%) children were identified as high risk for ASD on the BADEC. Twelve were identified as high risk using the Nah criteria, 9 of which were diagnosed with ASD. 8 children were identified using the Nevill criteria, all of which diagnosed with ASD. The BADEC scored with Nah criteria had 100% sensitivity and 95% specificity (Table 2). The BADEC scored with Nevill criteria had 89% sensitivity and 100% specificity. High risk for ASD designations had moderate negative correlations with cognitive (Nah rs=-0.46; Nevill rs=-0.45), expressive language (Nah rs=-0.52; Nevill rs=-0.47), and receptive language (Nah rs=-0.55; Nevill rs=-0.52) scores on the Bayley-III.
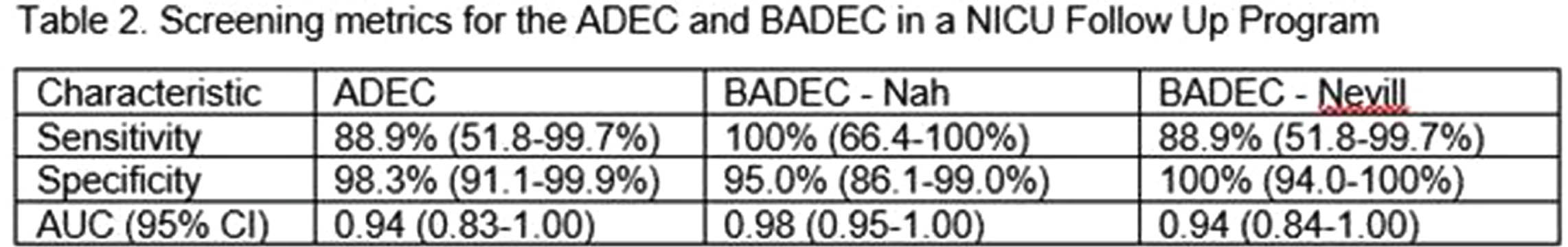
CONCLUSION: The BADEC is a fast and easy-to-use tool for ASD screening. In a NICU Follow Up Program, where screening and therefore sensitivity of evaluations are prioritized, the BADEC with Nah criteria yielded the best performance, accurately capturing all children later diagnosed with ASD.
BIBLIOGRAPHY:
1. Hirschberger RG, et al. Co-occurrence and Severity of Neurodevelopmental Burden at Age Ten Years in Children Born Extremely Preterm. PedNeur. 2018;79:45-52.
2. Kim SH, et al. Predictive Validity of the Modified Checklist for Autism in Toddlers Born Very Preterm. Jpeds. 2016;178:101-107.e102.
3. Haffner DN, et al. The Autism Detection in Early Childhood Tool: Level 2 autism spectrum disorder screening in a NICU Follow-up program. IBD. 2021;65:101650
4. Nah YH, et al. Development of a brief version of the Autism Detection in Early Childhood. Autism. 2019;23(2):494-502.
5. Nevill RE, et al Brief Report: Replication and Validation of the Brief Autism Detection in Early Childhood in a Clinical Sample. JADD. 2019;49(11):4674-4680.
Developmental coordination disorder in preterm Brazilian children and motor development
Carolina Panceri1,2, Nadia Cristina Valentini2, Renato Procianoy3,4, Rita C Silveira3,4
1Department of Physical Education, Physiotherapy and Dance, Universidade Federal do Rio Grande do Sul (UFRGS), 2Department of Physical Education and Occupational Therapy, Hospital de Clínicas de Porto Alegre, 3Department of Pediatrics and Neonatology, Universidade Federal do Rio Grande do Sul (UFRGS) , 4Neonatal Unit, Hospital de Clínicas de Porto Alegre
BACKGROUND AND OBJECTIVE: Preterm children are at higher risk for Development Coordination Disorder (DCD) than full-term children. DCD is characterized by poor motor coordination with significant interference in activities of daily living such as school tasks, play, self-care, and leisure. However, there is no evidence about this subject in children from low- and middle-income countries.
METHODOLOGY: to determine the prevalence of DCD in preterm Brazilian children across different gestational ages (extremely and very preterm) and investigated if motor development in the first year of life predicts DCD at preschool age we enrolled 63 preterm children in a follow-up clinic for high-risk infants. Bayley Scales of Infant and Toddler Development (BSITD-III) was used to assess motor development at 4, 8, and 12 months. The Movement Assessment Battery for Children (MABC-2) was used to assess motor coordination performance at pre-school age, neurological conditions were provided by neurologist in the follow-up clinic, and parents’ interviews were used to understand the children’s difficulties at home or schools; all these information was used as criteria to diagnose DCD according to the Diagnostic and Statistical Manual of Mental Disorders. Logistic regression and receiver-operating characteristics curves were used.
RESULTS: The prevalence of DCD was 52.38%, extremely preterm children had lower scores in MABC-2 than very preterm, and motor performance at 12 months was a significant predictor for DCD at preschool age. The chance of DCD at preschool age increases by 7.1% (95% CI: 1.8 - 13.9, p = .006) for each point that the motor composite score decreases. Further, analyses of the receiver-operating characteristics curve demonstrated that the area under the curve for motor assessments at 12 months was 0.68 (95% CI 0.54 – 0.83; p = .026), demonstrating the best cut-off point of the BSITD-III composite score is 98.5 with 52% sensibility and 78% specificity. At 4 and 8 months no significant associations were found.
CONCLUSION: Assessments before 12 months of age may not be appropriate to predict DCD, however at 12 months we found an incremented of risk for DCD of 7% for each point that the motor composite score decreases. This information is precious to LMIC since fewer resources are available for children with subtle impairments or with less known disorders, such as DCD; often, those children are underdiagnosed. Also, given the limited evidence in this field in low-middle-income countries, more research is needed to draw robust evidence regarding this issue.
BIBLIOGRAPHY:
Blank R et al. (2019). Dev Med Child Neurol, 61(3), 242-285;Bolk J et al (2018). JAMA Pediatr, 172(8), 765-774. Valentini NC et al (2021). Front. Psychol, 12, 753551.
The HNNE and KIDOKORO score as predictors of poor neurodevelopment outcome in extremely premature infants
Ilias Chatziioannidis1, Kostantia Tsoni1, Angelos Baltatzidis2, Eugenia Rouka1, Ioanna Giannopoulou1, Athanasia Anastasiou2, Kosmas Sarafidis1
11st Department of Neonatology and Neonatal Intensive Care, School of Medicine, Aristotle University of Thessaloniki, Ippokrateion General Hospital, 2Department of Radiology, Ippokrateion General Hospital
BACKGROUND: Premature infants are at increased risk of brain damage and poor neurodevelopment. Hence, early outcome prediction is crucial both for parental counselling and application of interventions.
AIM: To assess the role of the Hammersmith Neonatal Neurological Examination (HNNE) and KIDOKORO brain MRI score in predicting adverse neurodevelopmental outcome in infants born extremely premature.
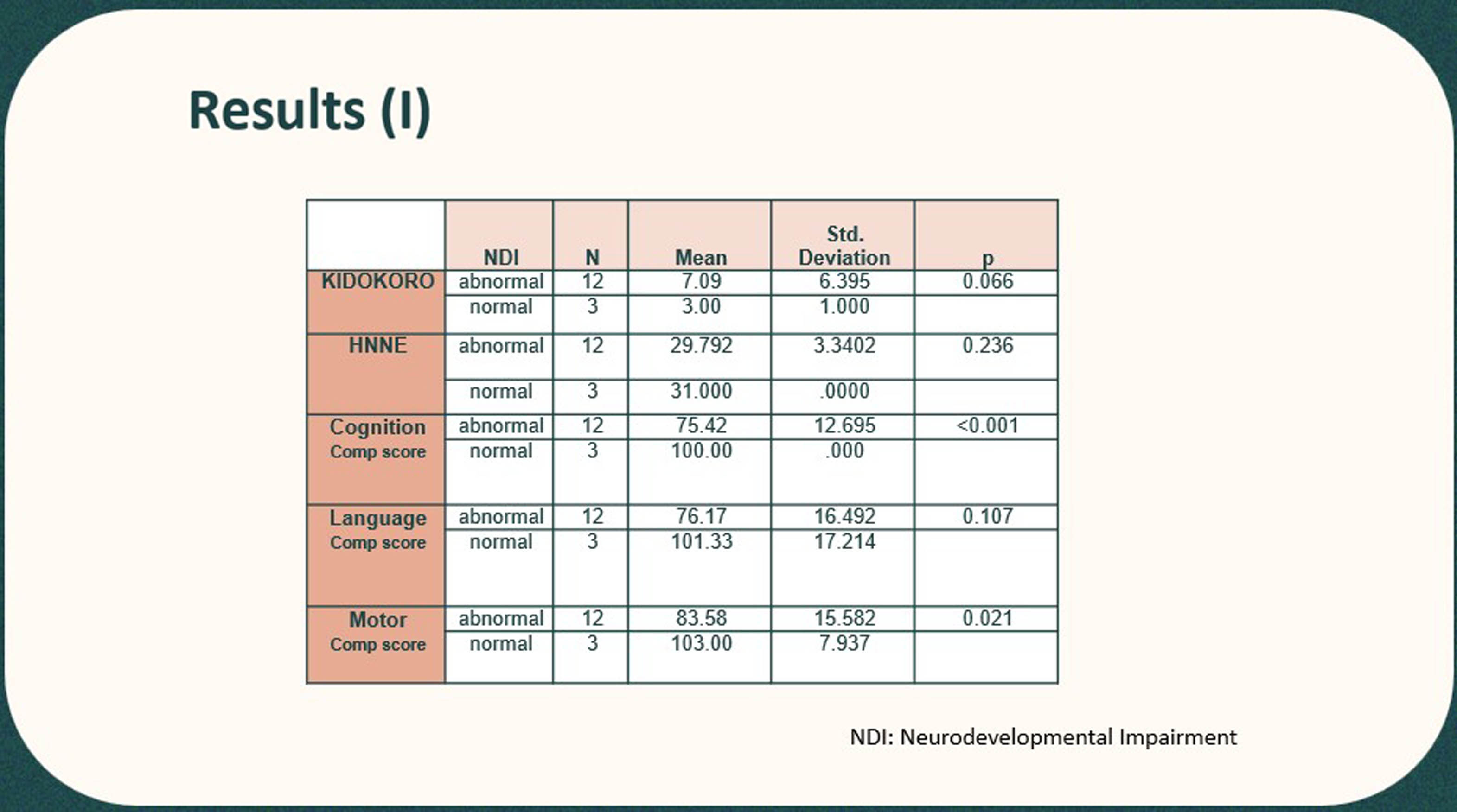
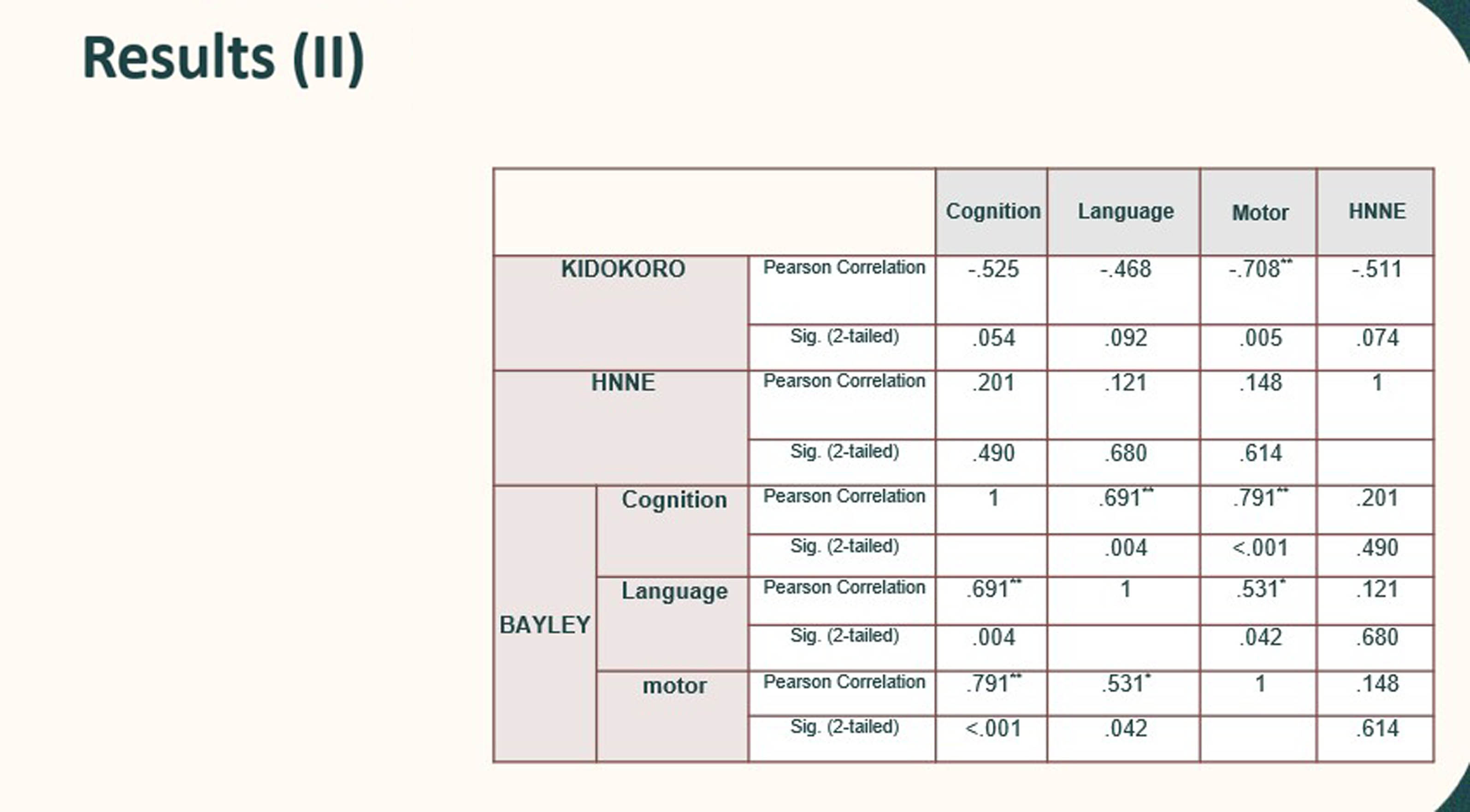
PATIENT-METHODS: Retrospective study involving extremely premature infants evaluated at full-term corrected age (HNNE and brain MRI) at the corrected age of 18-24 months (Bayley III test: cognitive, verbal and motor scale). Neonates with a Bayley III composite score of <85 and hearing/vision disorders were considered to have abnormal neurodevelopment.
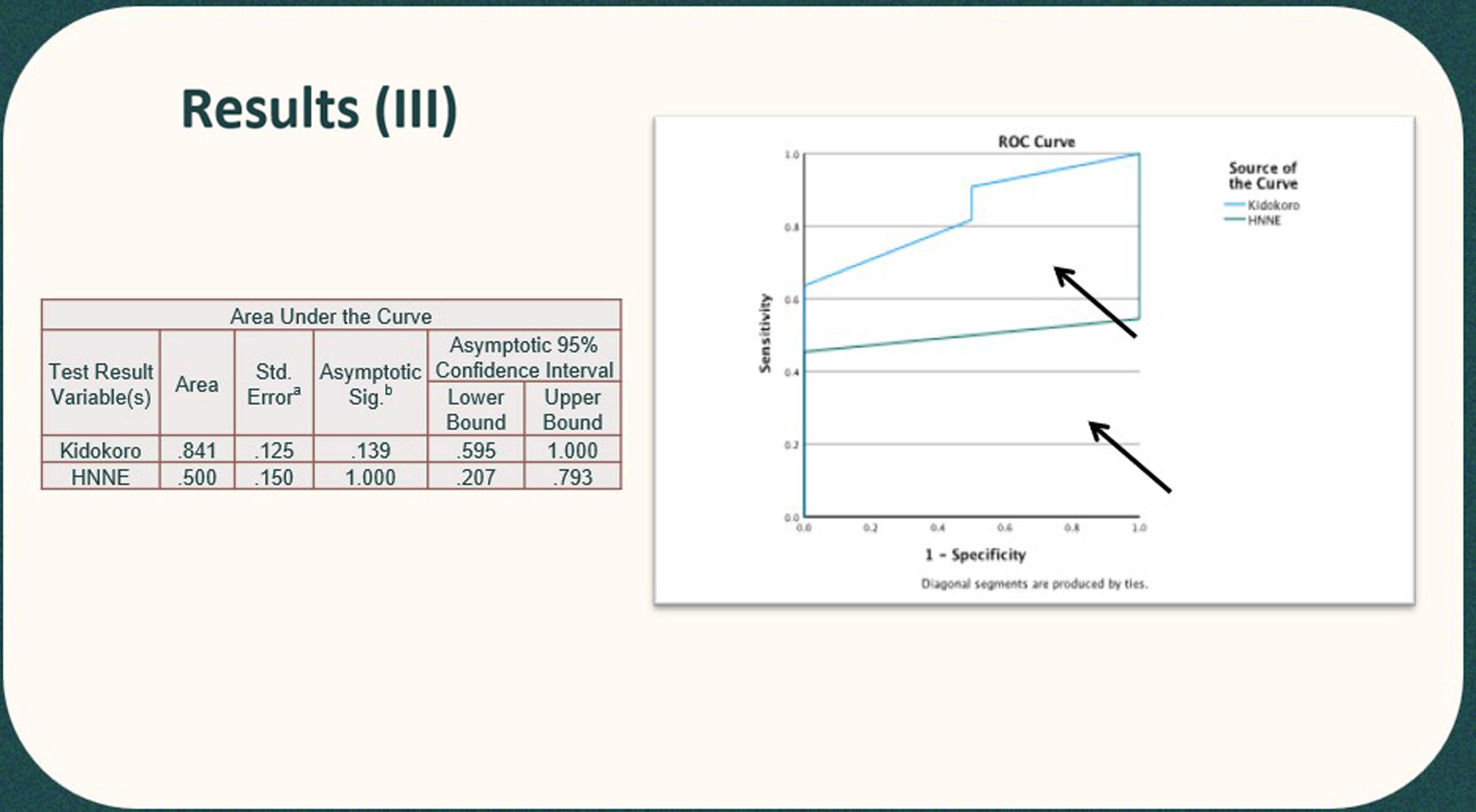
RESULTS: 15 infants with median gestational age of 26 (25-27) weeks were studied. At the corrected age of 19 (15-25) months, 80% of them had abnormal neurodevelopment outcome. Infants with abnormal neurodevelopment compared to those with normal outcome had higher KIDOKORO (7.09±6.39 vs. 3±1 respectively, p=0.27) and lower HNNE scores (29.79±3.34 vs. 31±0, respectively , p=0.06). Also, infants with adverse outcome had lower composite scores at all Bayley III scales. The AUC value for the KIDOKORO score and HNNE in predicting adverse outcome were 0.841 and 0.5, respectively.
CONCLUSION: Assessment of extremely premature infants at 40 weeks corrected age using the KIDOKORO score seems to be more accurate than HNNE for the prediction of poor neurodevelopmental outcome at the corrected age of 18-24 months.
REFERENCES:
1. Kidokoro H, Neil JJ, Inder TE. New MR Imaging Assessment Tool to Define Brain Abnormalities in Very Preterm Infants at Term, AJNR Am J Neuroradiol, 2013 34:2208-14.
2. X J.M. George, X S. Fiori, X J. Fripp, et al. Validation of an MRI Brain Injury and Growth Scoring System in Very Preterm Infants Scanned at 29- to 35-Week Postmenstrual Age, AJNR Am J Neuroradiol, 2017; 38:1435–42 .
3. Romeo DM, Ricci D, van Haastert IC et al. Neurologic Assessment Tool for Screening Preterm Infants at Term Age. J Pediatr 2012;161(6):1166-8.
Neurodevelopment at 12-18 months of children exposed to COVID-19 in utero
Keimarisse Colon1, Polaris Gonzalez1, Inés García-García1, Juanita Negrón-Pagán1, Leticia Gely-Rojas1, Lourdes García-Tormos1, Cynthia García-Coll1, Lourdes García-Fragoso1
1University Of Puerto Rico - School of Medicine
BACKGROUND: The potential for neurodevelopmental morbidity in offspring exposed prenatally to SARS-CoV-2 is a scientific concern (Shook, Sullivan, Lo, Perlis, and Edlow, 2022). The first year of life is characterized by a unique period of rapid neuronal growth and refinement, which ultimately establishes the foundation for lifelong brain architecture (Cusick and Georgieff, 2016; Meredith, 2015). Infants and neonates exposed to environmental stressors during this timeframe are vulnerable to neurodevelopmental impairments that can remain across their lifespan. The purpose of this study was to analyze the neurodevelopment of infants who were exposed to COVID-19 infection during pregnancy.
METHODOLOGY: Subjects studied were infants, whose mothers had COVID-19 infection during pregnancy, admitted to the UPR affiliated hospitals, or referred for follow-up at the High-Risk Clinics. Quarterly follow-up of infants with Ages and Stages questionnaire (ASQ-3) and Bayley-III test at 12-18 months of age. Medical record review of mothers and infants at birth. IRB approved.
RESULTS: The sample consisted of 138 infants who are now 12 months of corrected age or more (91 [66%] were exposed at delivery, 47 [34%] were exposed during pregnancy). The majority of infants were born full term (M=37 weeks) and 23 infants (17%) were born prematurely (26-36 weeks of gestation). ASQ-3 results showed that at 12 months follow-up (n=85) 15% showed a neurodevelopmental delay. Motor delays were more common during this period. At the 15-month follow-up (n=76), 21% showed delay. Delayed motor milestones were more common as well. At 18 months follow-up (n=54), 15% showed delay. Communication skills at 18 months showed a higher delay (11%) compared to other areas of development. Out of 138 infants, 40 were also assessed with the Bayley-III test. Bayley’s scores are evaluated in three domains (cognitive, motor, language). In general, 50% of the infants (n=40) showed mild delay (<85) and 23% (n=9) significant delay (<70) in at least one domain. In the Cognitive Composite Score, 7.5% (n=3) showed mild delay with 2.5% showing a significant delay. The Motor Composite Score showed a 17.5% (n=7) scoring <85 and 2.5% showing significant motor delay. The Language Composite Score was highly impacted in our subgroup with almost half of the group having a language delay (45%) <85, significant in 22.5%.
CONCLUSION: These results evidence neurodevelopmental delays (motor and language abilities) in a cohort of infants exposed in-utero to SARS-CoV-2. A significant delay in the development of language milestones was evident in the 18-month follow-up and within the subgroup of infants who had both assessment. Further statistical analysis is needed to test the association of these delays with/without in utero exposure to SARS-CoV-2 controlling for possible effects of sex and gestational age.
Impact of trajectory of post-hemorrhagic ventricular dilatation on neurodevelopmental outcomes in preterm infants
Grace Musiime1, Khorshid Mohammad1, Grace Kwong1, Sarfaraz Momin1, Leonora Hendson1, Jay Riva-Cambrin1, James Scott1, Hussein Zein1, Selphee Tang1, Amina Benlamri1, Lara Leijser1
1University of Calgary
BACKGROUND: Post-hemorrhagic ventricular dilatation (PHVD) in preterm infants can be progressive or resolve spontaneously over time. The developmental implications of natural trajectory and influence of neurosurgical intervention on neurodevelopmental impairment (NDI) are not well characterized.
OBJECTIVE: To assess in preterm infants the impact of PHVD trajectory on neurodevelopmental outcome at 21 months corrected age (CA), as indexed with lateral ventricular size measurements from cranial ultrasound (cUS), during a study period of a local historic late neurosurgical intervention approach.
METHODS: A retrospective cohort study of all preterm infants (<29 weeks’ gestation) born between 2010-2018 with any grade of intraventricular hemorrhage and ≥3 cUS during throughout the neonatal period. PHVD was defined as anterior horn width >6mm and/or ventricular index >97th percentile for postmenstrual age as measured from serial cUS. Infants were divided into three groups: no PHVD, PHVD without intervention and symptomatic PHVD requiring neurosurgical intervention. Group differences are being evaluated using Fisher’s exact or Pearson’s chi-squared test for categorical variables and analysis of variance for continuous variables where normality assumption was confirmed by Shapiro-Wilk’s test or Kruskal-Wallis test if normality assumption was not confirmed. A generalized linear model is being used to investigate neurodevelopmental outcomes at 21 months CA as assessed using the Bayley Scales of Infant Development 3rd Edition (BSID-III), the Gross Motor Functional Classification System (GMFCS) and validated hearing and vision tests, accounting for confounding variables for the three groups. Severe NDI is defined as ≥1 of BSID-III motor, cognitive or language composite score > 70, GMFCS 3 to 5, hearing aid or cochlear implant or bilateral visual impairment. Approval from the Conjoint Human Research Ethics Board at the University of Calgary was obtained (REB 20-1165); requirement for informed consent from participants for this study with anonymized data was waived. Data was extracted from clinical charts and neonatal-perinatal databases, and cUS reviewed on the electronic image reviewing system.
TIMELINE: Data collection is complete. Data analysis is ongoing, it is anticipated that this will be completed in November 2023.
IMPACT: The findings of this study will help inform clinical decision making regarding timing of intervention for PHVD and optimizing neurodevelopmental follow up of affected infants.
BIBLIOGRAPHY:
1. Lai GY, et al. Timing of Temporizing Neurosurgical Treatment in Relation to Shunting and Neurodevelopmental Outcomes in Posthemorrhagic Ventricular Dilatation of Prematurity: A Meta-analysis. J Pediatr. 2021 Jul;234:54-64.e20
2. Nieuwets A, et al. Post-hemorrhagic ventricular dilatation affects white matter maturation in extremely preterm infants. Pediatr Res. 2022 Jul;92(1):225-232.
3. Groulx-Boivin E, Paquette M, Khairy M, Beltempo M, Dudley R, Ferrand A, Guillot M, Bizgu V, Garfinkle J. Spontaneous resolution of post-hemorrhagic ventricular dilatation in preterm newborns and neurodevelopment. Pediatr Res. 2023 Oct;94(4):1428-1435.
GMA and HINE support early diagnosis of cerebral palsy in infants with neonatal encephalopathy
Sara Moss1, Jen Keene1, Lauren Ayala1, Mariana Baserga1, Sarah Winter1, Betsy Ostrander1
1Primary Children’s Hospital
BACKGROUND: Cerebral palsy (CP) is the most common motor sequela of neonatal encephalopathy (NE). Early diagnosis is imperative to allow for early intervention. The General Movements Assessment (GMA) and Hammersmith Infant Neurologic Exam (HINE) are validated tools for early CP detection and risk stratification in premature infants at risk for developmental delay[1]. Several groups have explored GMA and HINE in small cohorts of infants with NE but have conflicting results with some indication that the association between GMA and CP may be abolished by therapeutic hypothermia (TH)[2,3]. Therefore, there is no clear evidence that performing GMA and HINE on cooled infants provides diagnostic value.
OBJECTIVE: To examine the relationship between GMA, HINE, and risk of CP in a cohort of infants who have undergone TH and establish if HINE and GMA support the early diagnosis of CP.
METHODS: Retrospective cohort study from a large single center that included surviving infants with moderate or severe NE who underwent TH between 2018-2023. The center for neurodevelopmental follow up at University of Utah has participated in the CP Early Detection initiative since 2018[4], with both GMA and HINE initially administered to all infants who underwent TH for NE at 3 months of life by validated examiners. Patients were followed for at least 12 months.
RESULTS: Of 201 infants who underwent TH, 177 survived the initial hospitalization, and 72% (N = 130) were seen in follow-up. CP was diagnosed in 14 patients (11%). The absence of fidgety movements at the 3-month GMA was highly associated with CP (p-value = <0.0001, sensitivity 89%, specificity 91%) (Table 1). Similarly, all HINE assessments were associated with CP at 3 months (p-value <0.0001, sensitivity 80% specificity 95%), 6 months (p <0.0001, sensitivity 82%, specificity 100%), and 9 months (p <0.0001, sensitivity 89%, specificity 92%) with an area under the receiver operating curve ranging from 90% - 95% (Figure 1).
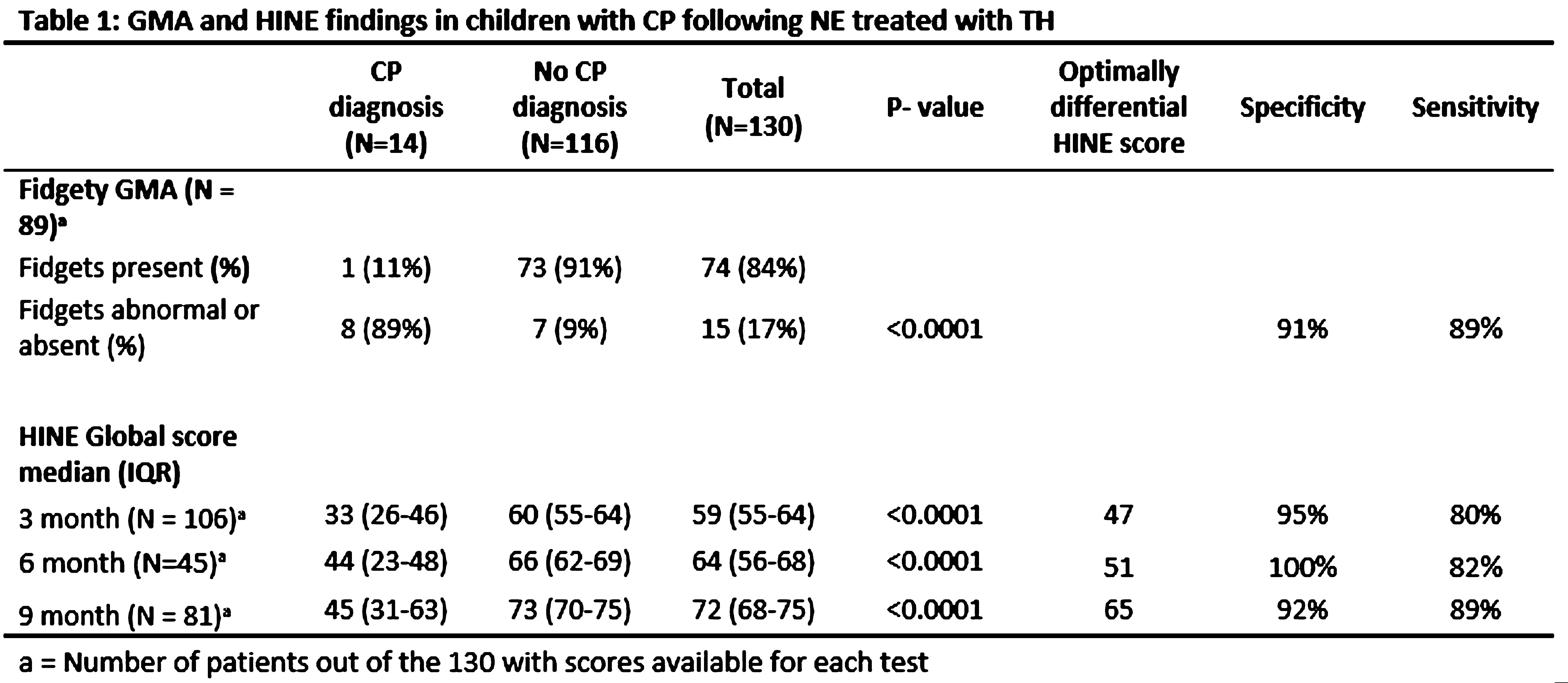
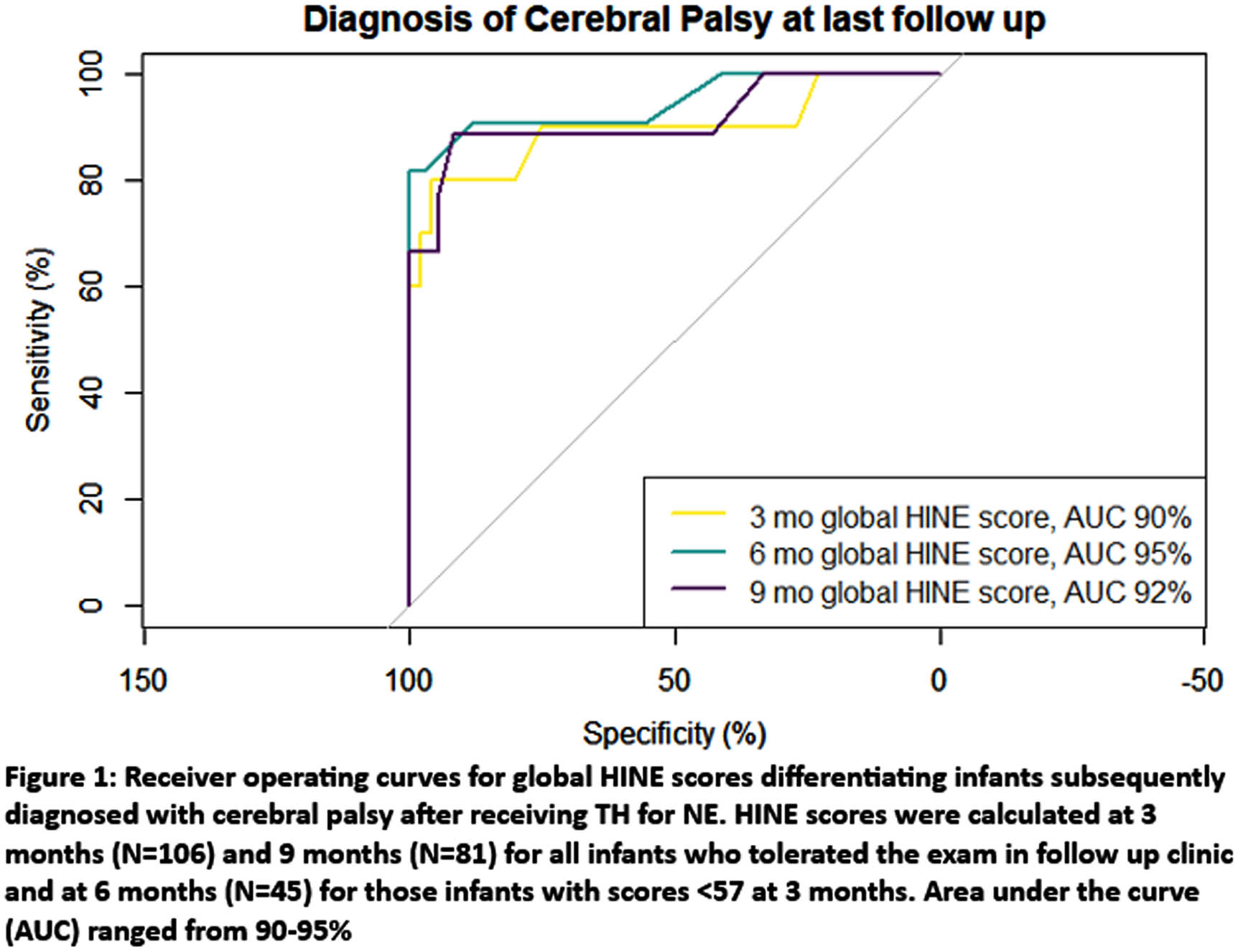
CONCLUSION: GMA and HINE were predictive of CP in term infants with NE who had undergone TH. The presence or absence of fidgets on GMA at 3 months and the HINE score at 3, 6 and 9 months were all highly associated with CP diagnosis with >80% sensitivity and > 90% specificity. The optimal HINE score for predicting CP may differ from premature infants and will benefit from further analysis. Ongoing analysis will also include trajectory data for repeated HINE and GMA scoring, and evaluation of HINE and GMA combined to predict CP.
BIBLIOGRAPHY:
[1] Novak I et al. JAMA Pediatrics 2017;171:897–907
[2] Glass HC et al. Pediatric Neurol 2021;118:20–5
[3] Ferrari F et al. European Journal of Paediatric Neurology 2023;42:53–9.
[4] Maitre NL et al. Pediatrics 2020;145
Intraventricular haemorrhage and special educational need at 8 years of age; retrospective cohort study
Miklós Szabó, Andrea Valek, József Halász, Hajnalka Barta
1Semmelweis University Division of Neonatology Department of Pediatrics, 2Heim Pál National Institute of Paediatrics, 3Pro Rekreatione Toparti Outpatient Clinic
BACKGROUND AND OBJECTIVE: Intraventricular haemorrhage (IVH) is a devastating complication of preterm birth, considerably worsening the basic burden of prematurity on neurodevelopmental outcome1. However, follow-up data of the different severity grades of IVH is highly scarce, especially as we proceed to later childhood and school-age. Linkage of patient and school registries could overcome this difficulty, and provide valuable outcome data on former preterm infants 2. The aim of our study was to investigate the relationship of IVH, prematurity and male sex and occurence of adverse school-age outcome defined by special educational need (SEN).
METHODOLOGY: This retrospective cohort study is part of a nationwide investigation, linking clinical data of 8,029 surviving infants, born ≤32 gw between 2005-2014 and treated at any NICU of Hungary, with the SEN at the age of 8 years data of the national school database. Occurrence of SEN was assessed in subgroups created based on IVH severity, gestational age and sex. Pearsons’s Chi-square and Fisher’s exact test were used to compare occurrence of SEN in subgroups, and logistic regression was performed to calculate odds ratios of grade of IVH, gestational age and sex for school-age SEN.
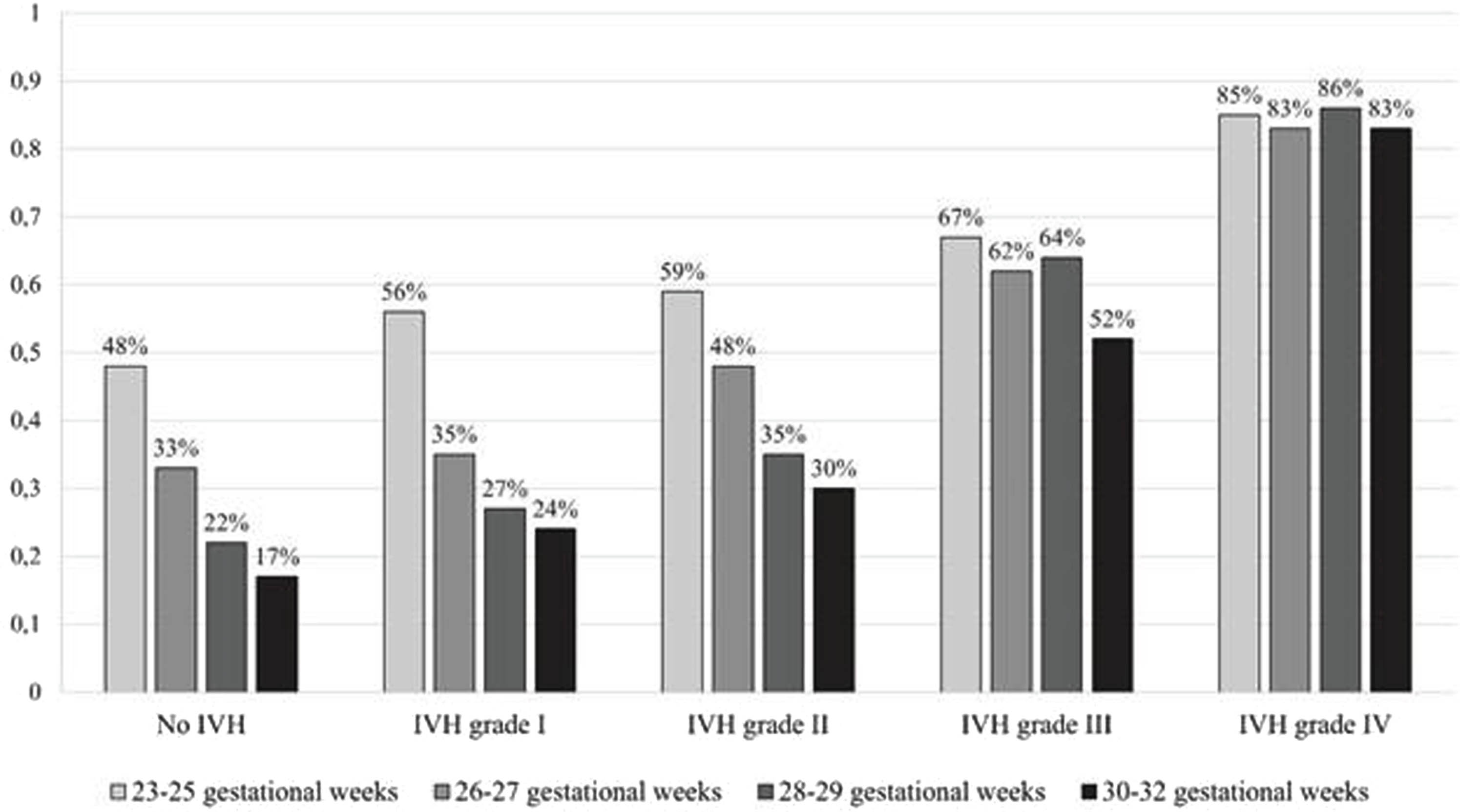
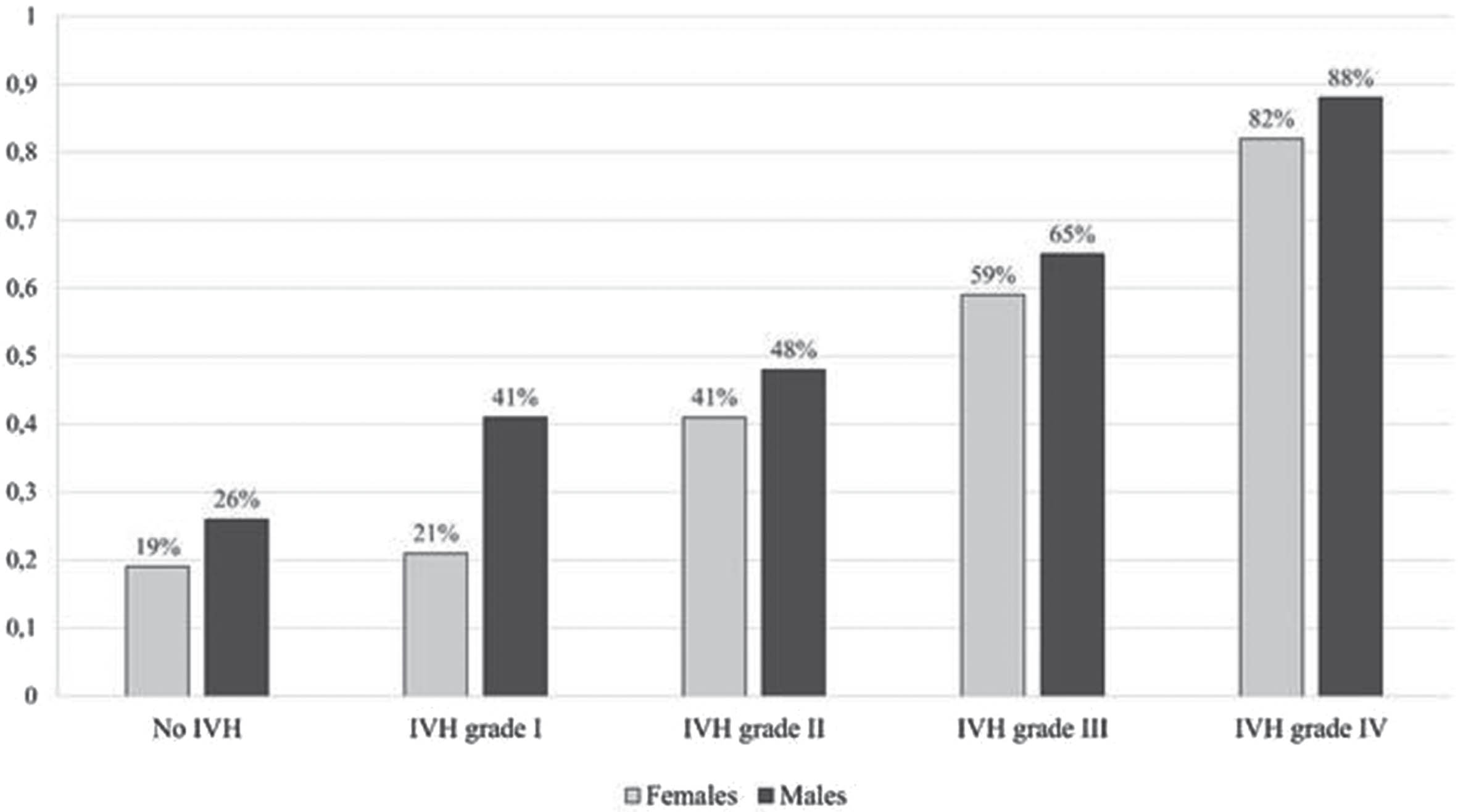
RESULTS: A total of 1,758 infants (17%) were diagnosed any grade IVH, in whom SEN occurrence was 48%. Occurrence rates of IVH grades and corresponding SEN were: grade I: 8% (SEN 31%), grade II: 7% (SEN 45%), grade III: 5% (SEN 63%) and grade IV: 2% (SEN 85%). Subgroup analysis by gestational age revealed that higher IVH severity (grade III and IV) resulted in similar SEN occurrence throughout the gestational age spectrum, whereas grade I-II IVH showed increasing SEN occurrence with decreasing gestational age (Figure 1, p<0.001). Subgroup analysis based on infant sex suggested that female sex has an apparent protective effect against both prematurity associated and IVH associated SEN, however this later diminished by advanced severity IVH (Figure 2, p<0.001). Regression model shows, that odds ratio for SEN 1.59 (95%CI 1.51-1.67) for IVH grade as a continuous variable, 0.65 (95%CI 0.62-0.69) for advanced gestational age in weeks and 1.56 (95%CI 1.40-1.74) for male sex.
CONCLUSION: Longterm developmental effects of IVH of preterm infants deeply affected by factors like severity of IVH, gestational age and sex. Further research is warranted to provide more personalized care to reduce the lifelong burden of neurological complications associated with preterm birth and IVH, even of low grades IVH.
BIBLIOGRAPHY:
1. Dorner RA, at al.. Preterm neuroimaging and neurodevelopmental outcome: a focus on intraventricular hemorrhage, post-hemorrhagic hydrocephalus, and associated brain injury. J Perinatol. 2018; 38(11):1431-1443.
2. Mackay D, at al. Obstetric factors and different causes of special educational need: retrospective cohort study of 407 503 school children. BJOG 2013;120:297–308.
The Bavarian longitudinal study: Altered cortical macro- und microstructure in very preterm born adults
Benita Schmitz-Koep1, Aurore Menegaux1, Dieter Wolke2, Peter Bartmann3, Christian Sorg1, Dennis Hedderich1
1Technical University of Munich, School of Medicine, Department of Diagnostic And Interventional Neuroradiology, 2University of Warwick, Department of Psychology, 3University Hospital Bonn, Department of Neonatology and Pediatric Intensive Care
BACKGROUND: Preterm birth has a high global prevalence of approximately 11%.1 It is associated with increased mortality and morbidity, particularly an elevated risk of cognitive impairments.2 Individuals born preterm show structural alterations in the central nervous system that remain detectable into adulthood. In this work, we combine insights from two studies to shed light on the long-term consequences of preterm birth on macro- and microstructural properties of the cortex.3,4
METHODOLOGY: A well-known measure of cortical macrostructure is cortical thickness (CTh; see Figure 1). In the first study, CTh was analyzed in a large, prospectively collected cohort of 101 very preterm-born adults (<32 weeks of gestation and/or birth weight <1,500 g) and 111 controls at 26 years of age using magnetic resonance imaging (MRI) and surface-based morphometry. Regarding cortical microstructure, the percent contrast of gray-to-white matter signal intensities (GWPC; see Figure 1) has been proposed as an in vivo MRI-based proxy measure.5 The second study examined GWPC at different percentile fractions across the cortex in 86 preterm-born adults and 103 controls of the same cohort, also at 26 years of age. Cognitive performance was assessed by full-scale intelligence quotient (IQ) using the Wechsler Adult Intelligence Scale in both studies.
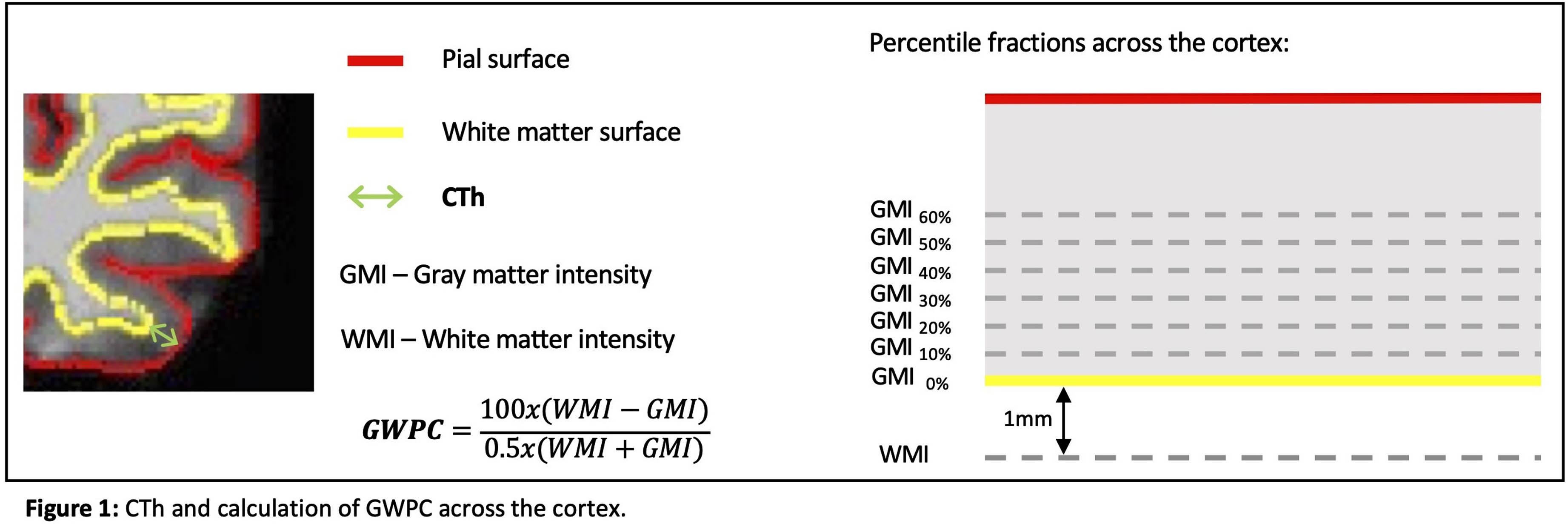
RESULTS: In the first study, CTh was lower in preterm-born adults compared to controls in frontal, parietal, and temporal associative cortices, predominantly in the left hemisphere (see Figure 2). Furthermore, CTh in the left hemisphere mediated the relationship between preterm birth and IQ. In the second study, GWPC was lower in frontal, parietal, and temporal associative cortices after preterm birth, predominantly in the right hemisphere. Differences were pronounced in middle cortical layers (20%-40%). On the other hand, GWPC was higher in right paracentral lobule (see Figure 2). Furthermore, right paracentral GWPC was negatively correlated with IQ (p<0.05).
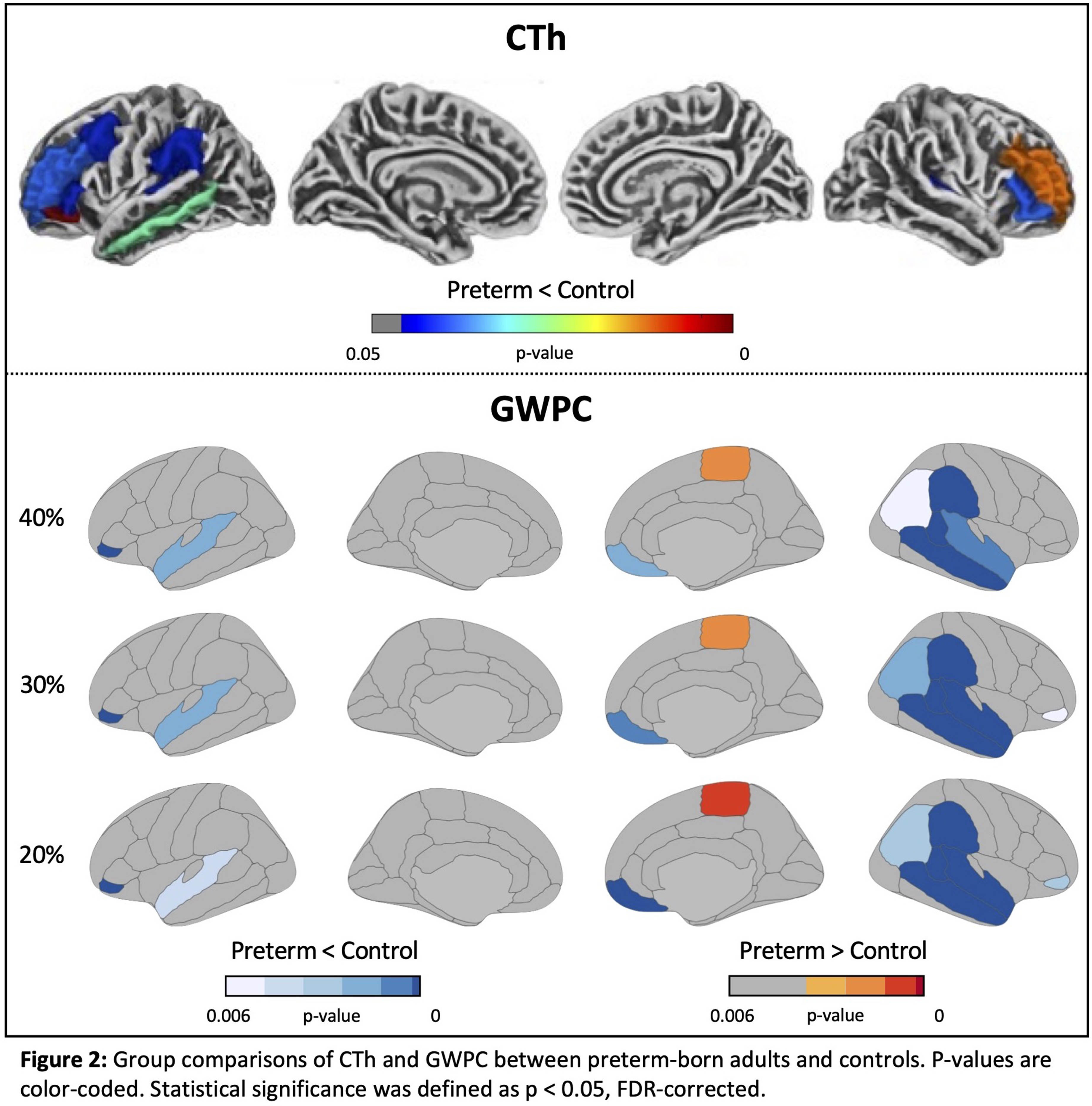
CONCLUSION: Combined, these studies suggest that preterm birth is associated with long-term alterations in cortical structure, affecting both macro- and microstructure. The results suggest differential effects of prematurity on associative and primary cortices. Furthermore, CTh in the left hemisphere and right paracentral GWPC were associated with IQ, and therefore potentially contribute to cognitive deficits that persist into adulthood following preterm birth.
BIBLIOGRAPHY:
1 Chawanpaiboon, S. et al. The Lancet Global Health, 7(1) (2019)
2 Wolke, D., Johnson, S., & Mendonça, M. Annual Review of Developmental Psychology, 1(1), 69–92 (2019)
3 Schmitz-Koep, B. et al. Human Brain Mapping, 41(17), 4952–4963 (2020)
4 Schmitz-Koep, B. et al. CNS Neuroscience & Therapeutics, 29(11), 3199–3211 (2023)
5 Andrews, D. S. et al. Cerebral Cortex, 27(2), 877–887 (2017)
Social factors and neurodevelopmental outcomes of infants born preterm during and before the COVID-19 pandemic
Gabriel Côté-Corriveau1,2, Sriya Roychaudhuri1, Danielle Sharon1, Hoda El-Shibiny1, Mohamed El-Dib1,3, Terrie Inder1,3,4, Carmina Erdei1,3
1Division of Newborn Medicine, Department of Pediatrics, Brigham and Women’s Hospital, 2Sainte-Justine University Hospital, 3Harvard Medical School, 4Division of Neonatology, Children’s Hospital of Orange County and University of California, Irvine
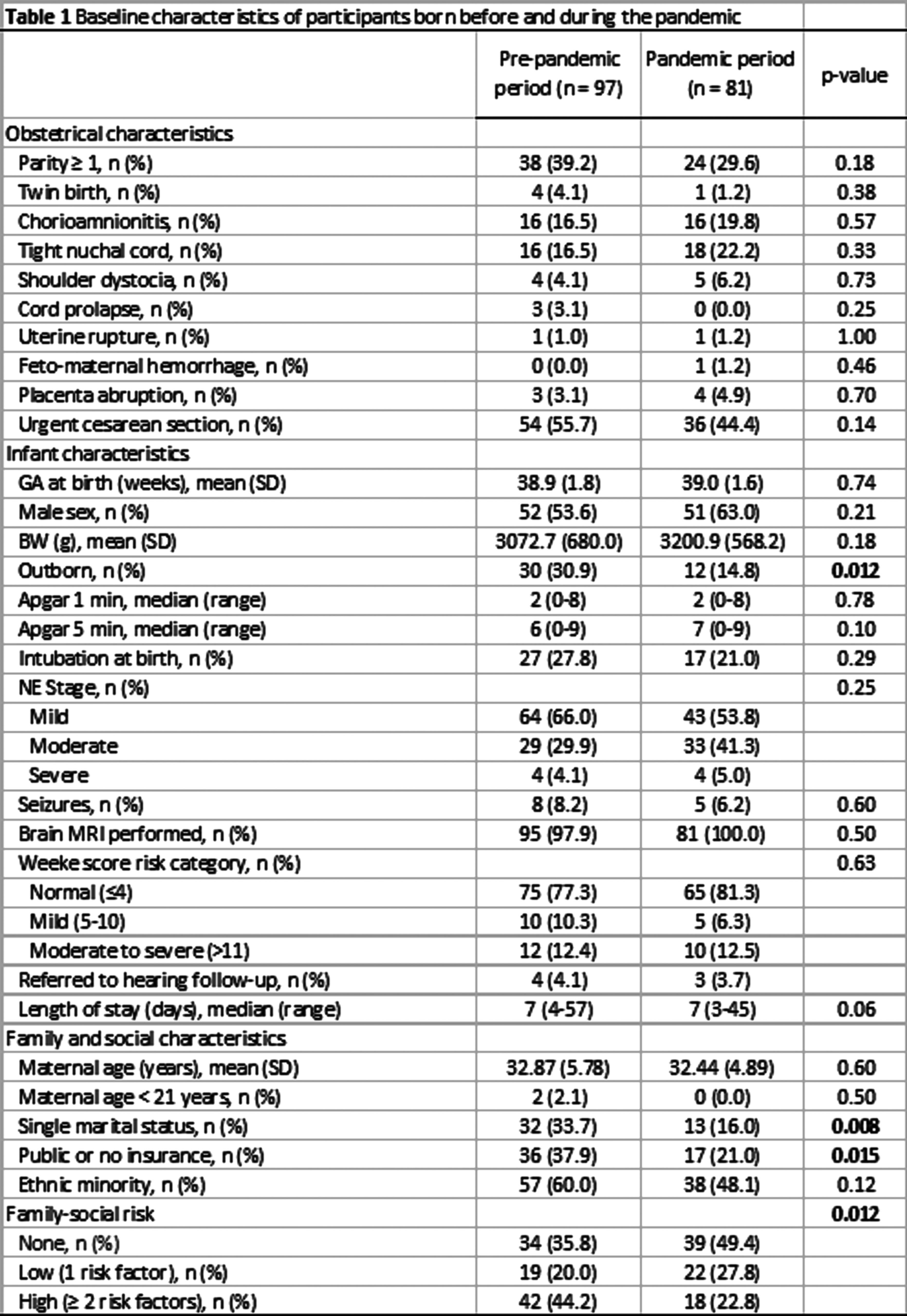
BACKGROUND: Infants born very preterm (VP) may have been especially vulnerable to the repercussions of the pandemic, as social factors can influence neurodevelopment.(1) Yet, the impact of the pandemic and social factors on developmental outcomes of VP infants remains insufficiently understood. We aimed to assess the neurodevelopmental outcomes of VP infants during vs before the COVID-19 pandemic, and examine the potential implications of family and community-level social factors.
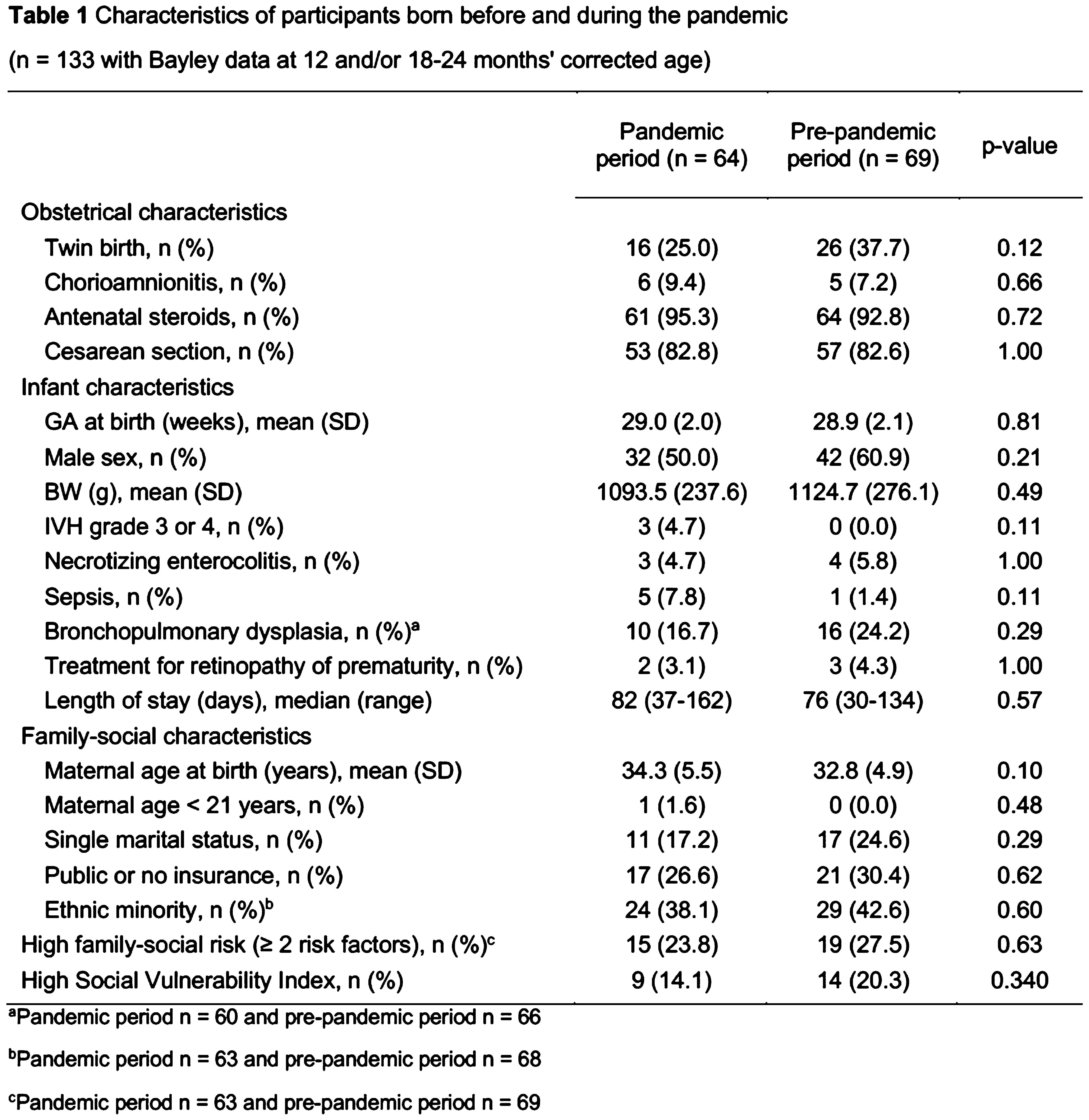
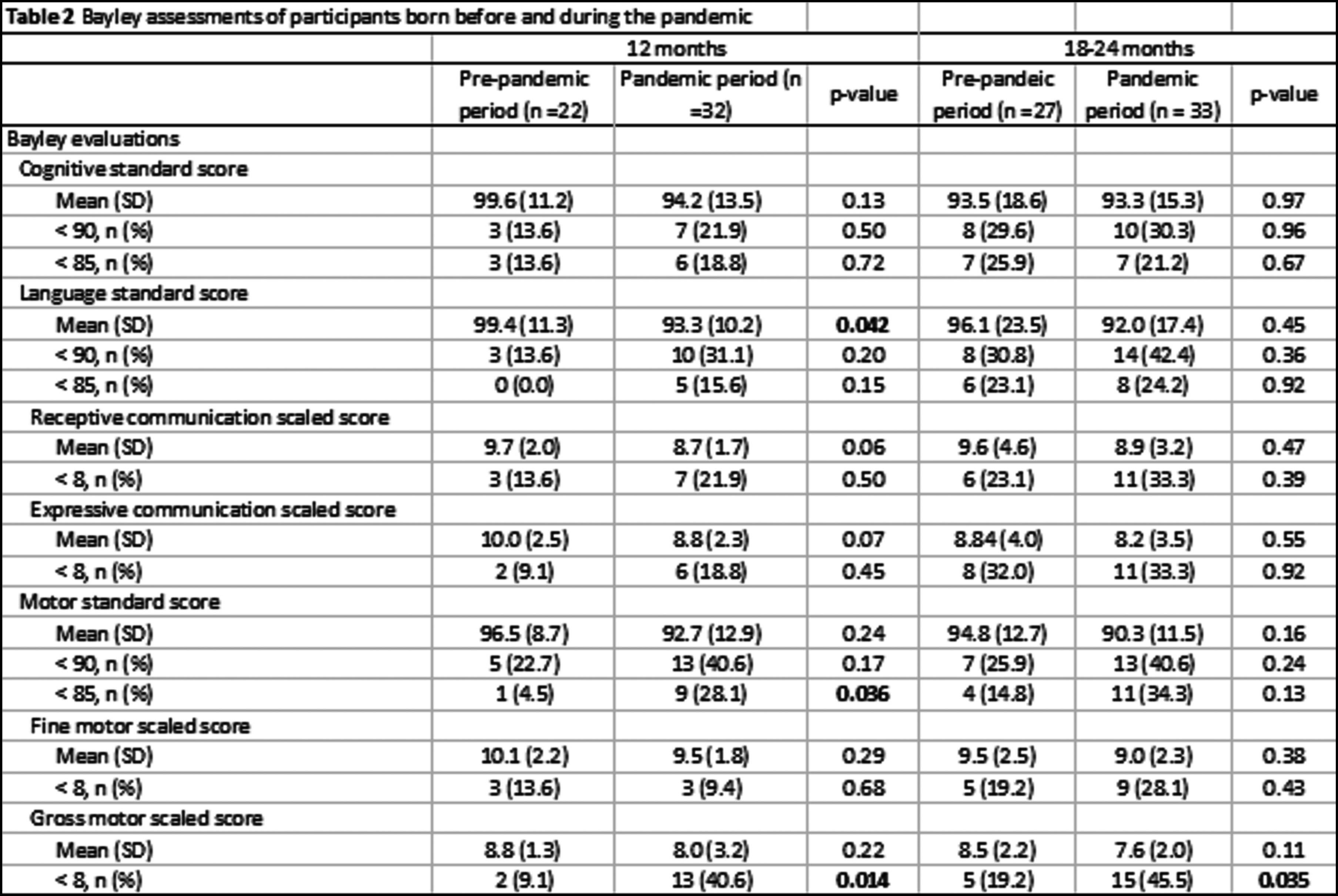
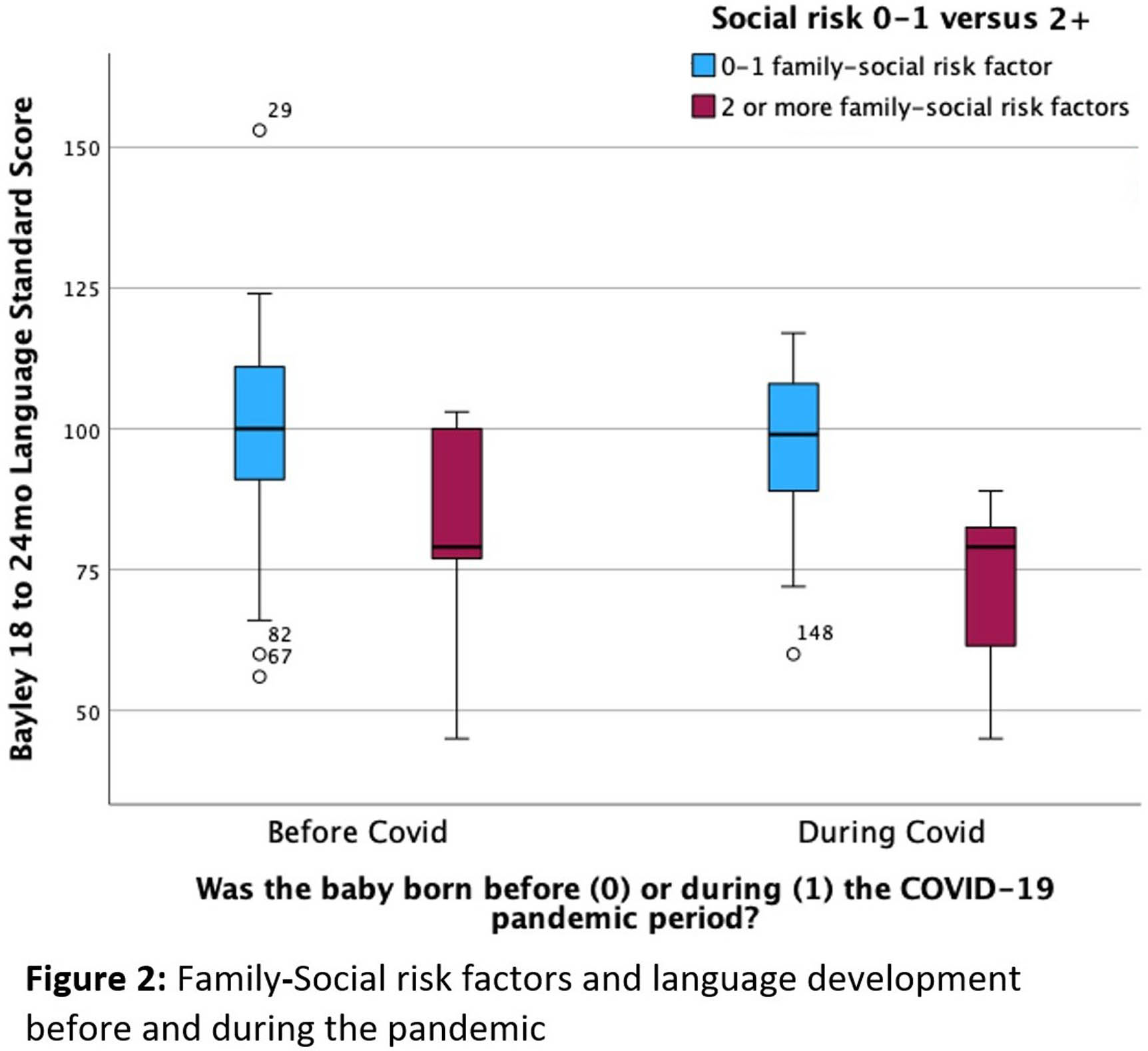
METHODOLOGY: We conducted a retrospective review of a cohort of VP infants born ≤ 32 weeks’ gestational age and ≤ 1500 grams in a level-III NICU. We examined VP infants born during (03/2020 - 09/2021) vs before (10/2017 - 12/2019) the COVID-19 pandemic. The outcome measures were neurodevelopmental scores on the Bayley Scales of Infant Development 4th edition at 12 months, and at 18-24 months’ corrected age. We identified infants with high family-social risk (≥ 2 risk factors including maternal age < 21 years, single marital status, public or no insurance, and ethnic minority). We documented the neighbour-level CDC Social Vulnerability Index (SVI). We examined associations of developmental outcomes with the pandemic period, family-social risk, and SVI using t-tests and chi-square tests.
RESULTS: Obstetrical, neonatal, and social characteristics were similar between infants born during (n =64) vs before (n = 69) the pandemic (Table 1). Compared with VP infants born before, infants born during the pandemic had lower language scores (88.8 vs 93.1; p = 0.054) and expressive communication scores (7.6 vs 8.8; p = 0.005) at 12 months, but differences faded by 18-24 months (Table 2). Regardless of the pandemic period, high family-social risk and SVI were associated with lower cognitive and language scores at 18-24 months. Associations were strongest for language scores, whether comparing the family-social risk (79.6 vs 95.9; p < 0.001) or SVI (79.0 vs 94.7; p < 0.001). The decrease in cognitive and language scores relative to family-social risk and SVI did not appear to differ during vs before the pandemic (Figure 1).
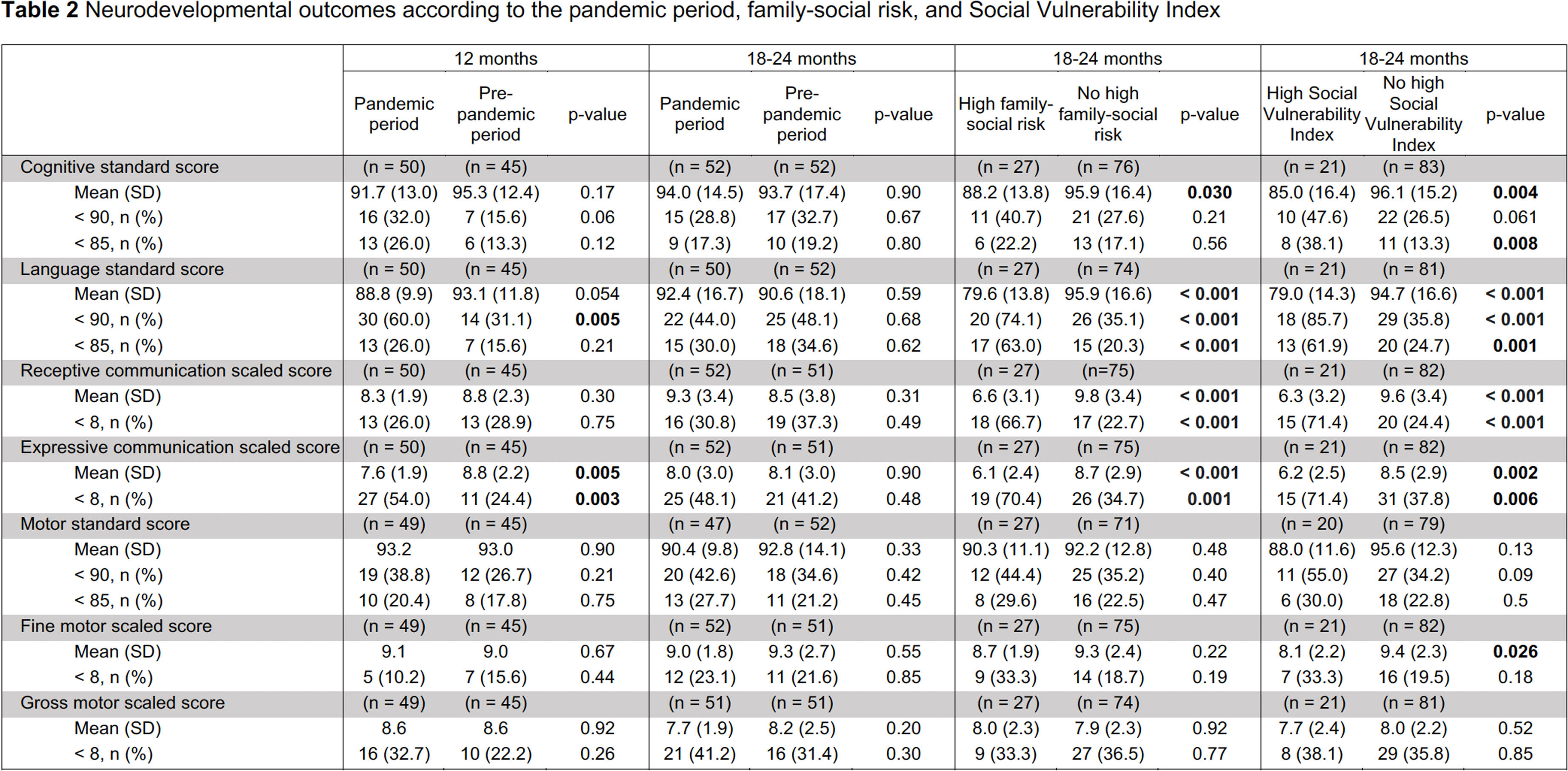
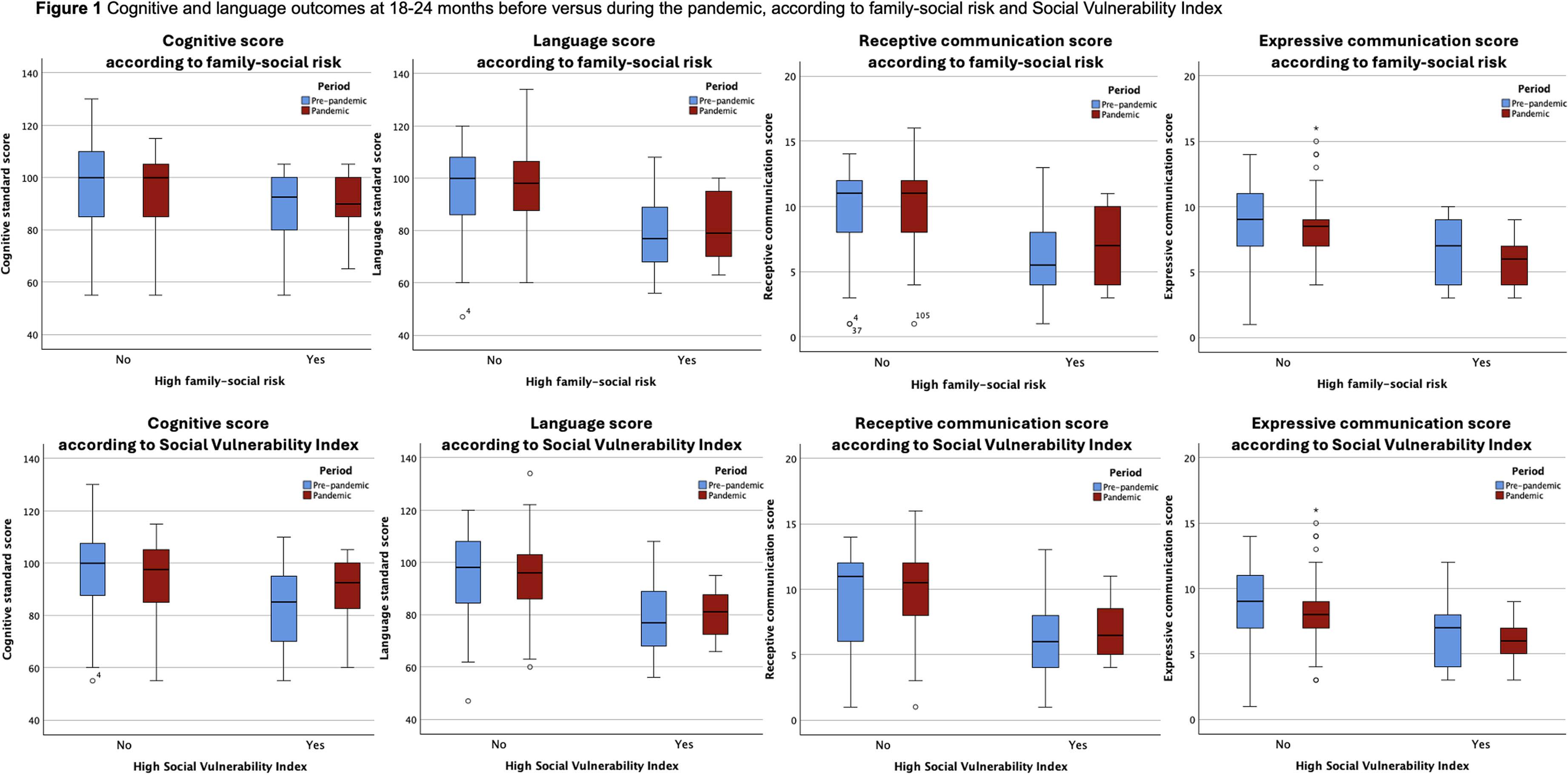
CONCLUSION: In this retrospective study, VP children born during the COVID-19 pandemic experience significantly lower expressive communication skills at 12 months; this effects attenuates by 18-24 months corrected age. High family and community-level social vulnerability correlates with lower cognitive and language scores. Further studies are needed to better understand the transient and/or persistent effects of the pandemic on developmental trajectories of VP infants.
BIBLIOGRAPHY:
1. Erdei C, Austin NC, Cherkerzian S, Morris AR, Woodward LJ. Predicting School-Aged Cognitive Impairment in Children Born Very Preterm. Pediatrics. 2020;145(4):e20191982. doi:10.1542/peds.2019-1982
Neurodevelopmental outcomes of infants evaluated for but not treated with therapeutic hypothermia
Danielle Sharon1, Elizabeth Singh1, Hoda El-Shibiny1, Aisling Garvey2, Brian Walsh2, Carmina Erdei1,3, Terrie Inder4, Mohamed El-Dib1,3
1Brigham And Women’s Hospital, 2University College Cork, 3Harvard Medical School, 4Childrens Hospital of Orange County
BACKGROUND: Therapeutic hypothermia (TH) is the standard of care for neonatal encephalopathy (NE). Although there is ongoing debate regarding the criteria for TH treatment, the criteria and protocol used in the Brigham and Women’s Hospital, which we have previously published, include infants with milder NE. Amplitude-integrated EEG (aEEG) is frequently incorporated into the evaluation. Whether these criteria, inclusive of mild encephalopathy, can screen out those with acute brain injury and adverse neurodevelopmental outcomes who might benefit from TH is unknown. Our primary aim was to evaluate outcomes in a set of infants who were evaluated for TH but did not receive TH with neonatal MRI and 2-year developmental outcomes.
METHODOLOGY: We enrolled infants who were screened for but not treated with TH between April 2019 and August 2021. All brain MRIs were obtained within the first week of life. Infants were followed up at two years of age to obtain a standard Bayley-4 assessment conducted by a clinical psychologist. Neurodevelopmental delay was defined as any BSID-4 standard score < 85 (1 SD below mean).
RESULTS: Thirty-nine infants were enrolled in the study with their detailed demographic and clinical characteristics reported in Table 1. Of the 39 infants, 34 (87.2%) had no evidence of acute perinatally acquired hypoxic-ischemic brain injury (Thiim et al,2023). Twenty-six infants, three of whom had acute brain injury, returned for a 2-year follow-up Bayley-4 assessment. 13 (50%) had neurodevelopmental delay in either cognitive, language, or motor areas. Only one of the three infants with acute neonatal brain injury had neurodevelopmental delay. When compared to these without delay, infants with neurodevelopmental delay had higher 1-hour base deficit and higher lactate levels. Additional results from the Bayley assessments are in Table 2.
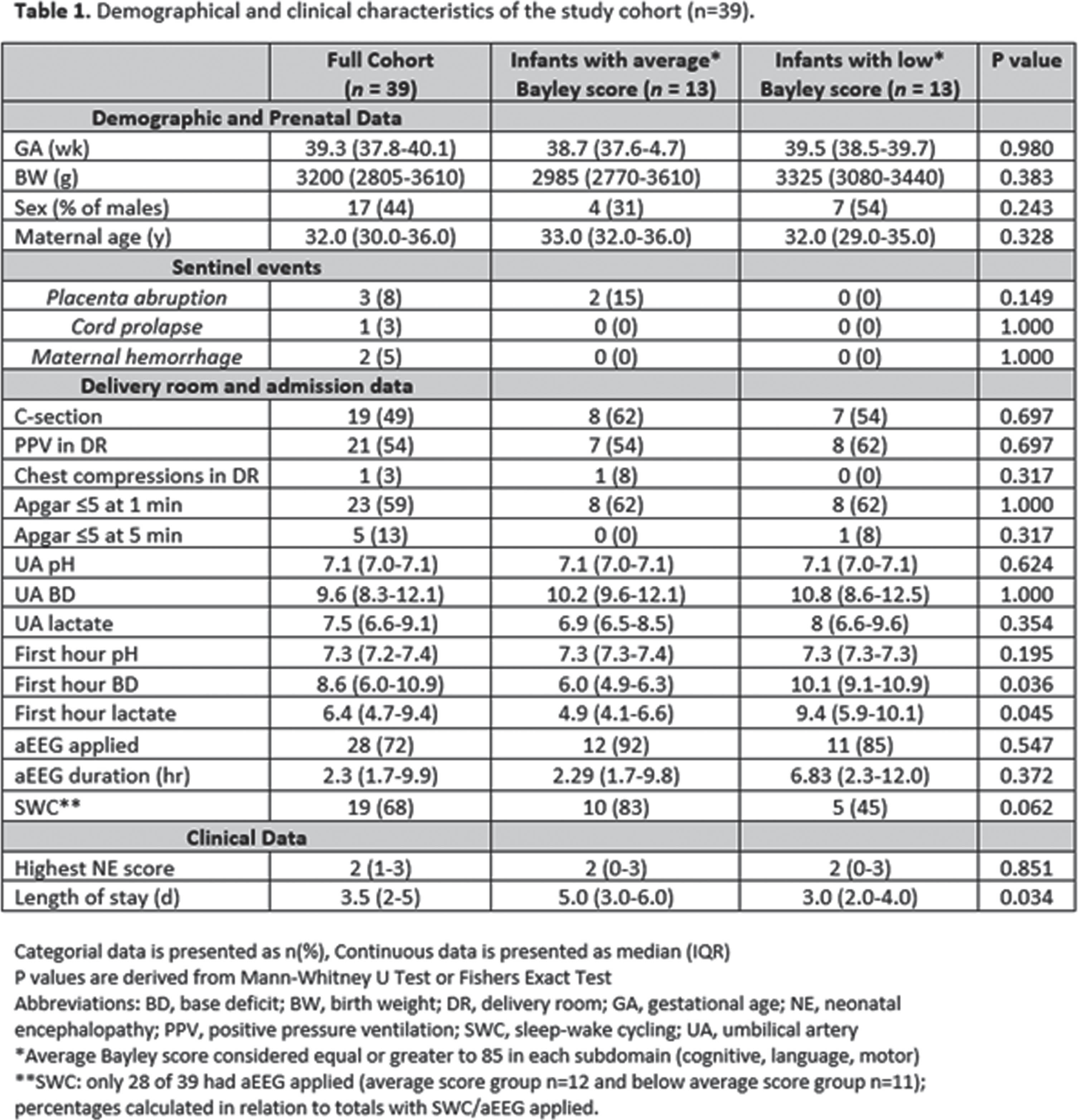
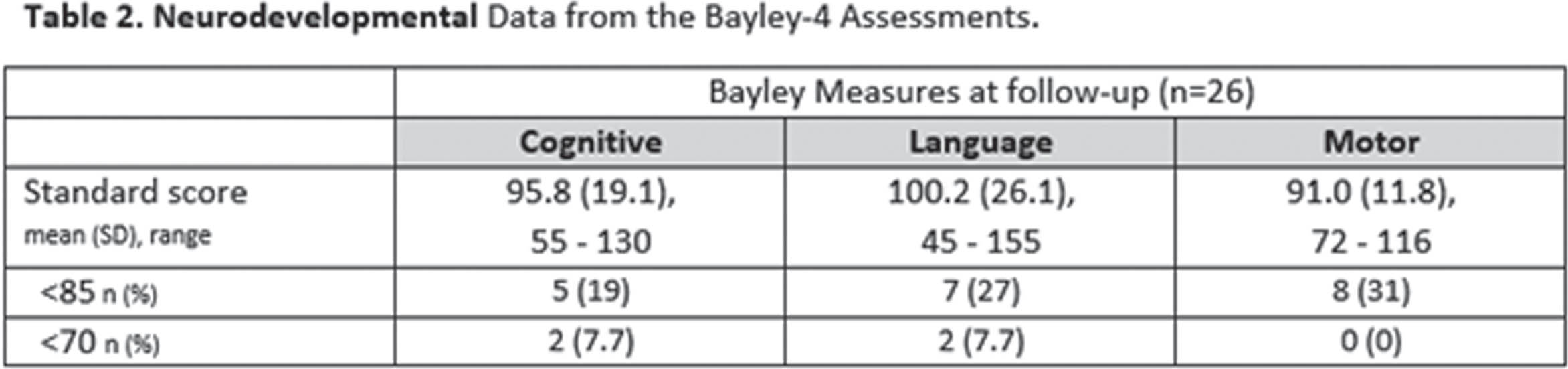
CONCLUSION: Results suggest that the current expanded TH criteria, inclusive of mild NE, is effective at detecting most infants with acute hypoxic-ischemic injuries. It is notable that a large percentage of these infants continue to be at risk for neurodevelopmental delay. Application of neuroimaging and neurodevelopmental follow-up in infants considered for hypothermia but not receiving treatment remains worthy of consideration. Whether recovery of blood gases can identify those with the highest risk needs further studying.
BIBLIOGRAPHY:
1. Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. The Cochrane database of systematic reviews. 2013;1:CD003311.
2. Brigham and Women’s Hospital TH Clinical Practice Guidelines. https://www.brighamandwomens.org/assets/BWH/pediatric-newborn-medicine/pdfs/th-cpg-amended.pdf
3. Bayley N, Aylward GP. Bayley Scales of Infant and Toddler Development-Fourth Edition Administration Manual. Bloomington, MN: NCS Pearson; 2019.
4. Thiim KR, Garvey AA, Singh E, Walsh B, Inder TE, El-Dib M. Brain Injury in Infants Evaluated for, But Not Treated with, Therapeutic Hypothermia. J Pediatr. 2023; 253:304-309.
Perceived impacts of the physical environment in a hybrid-design NICU according to interdisciplinary staff
Gabriel Côté-Corriveau1,2, Danielle Sharon1, Elizabeth Singh1, Yvonne Sheldon1, Tina Steele1, Terrie Inder1,3,4, Carmina Erdei1,3
1Division of Newborn Medicine, Department of Pediatrics, Brigham and Women’s Hospital, 2Department of Pediatrics, Sainte-Justine University Hospital, University of Montreal, 3Harvard Medical School, 4Division of Neonatology, Children’s Hospital of Orange County and University of California, Irvine
BACKGROUND: The neonatal intensive care unit (NICU) environment may play an important role in facilitating the sensory experiences of preterm and/or ill infants during a critical window for brain development.(1) Feedback from NICU staff about the perceived effects of NICU design on newborns, families, and themselves may help optimize the NICU environment. The objective of this study is to assess the perceptions of NICU staff working within a hybrid design unit about the environment surrounding newborns, and the impacts of NICU design on patient and staff experience.
METHODOLOGY: This is a survey study within a hybrid design level-III NICU, where high-risk infants initiate their stay in single-family rooms (SFR) and typically transition to semi-open bays (SOB) when medically stable. We surveyed the interdisciplinary NICU staff, including attending physicians, nurses, nurse practitioners, physician assistants, respiratory therapists, allied health professionals (developmental therapists, dietitians, pharmacists), clinical research members, and mental health providers (social workers).
RESULTS: The sample was composed of 127 interdisciplinary NICU staff members (Table 1). The majority believed that meaningful infant-directed language (87%) and music with human voice (69%) were the most beneficial auditory exposures for infants in the NICU. Electronic sounds and noise were the main auditory components reported by staff (48%) in SFR, while distant language was perceived as the most prevalent auditory exposure in SOB (44%). 31% of respondents preferred to work in SFR, while 29% preferred SOB, and the remainder (40%) reported no preference. The main perceived advantages of SFR were more privacy for families (97%), a quieter environment (70%), and improved facilitation of breastfeeding (59%) and skin-to-skin (58%) practices. For SOB, advantages were reported as creating a safer work environment (59%), more benefits of music therapy (48%) and adapted visual stimuli (41%), and easier interactions with colleagues (40%). SFR was perceived as best to favor parent-infant bonding (68%), while SOB appeared superior for social connections among families (77%).
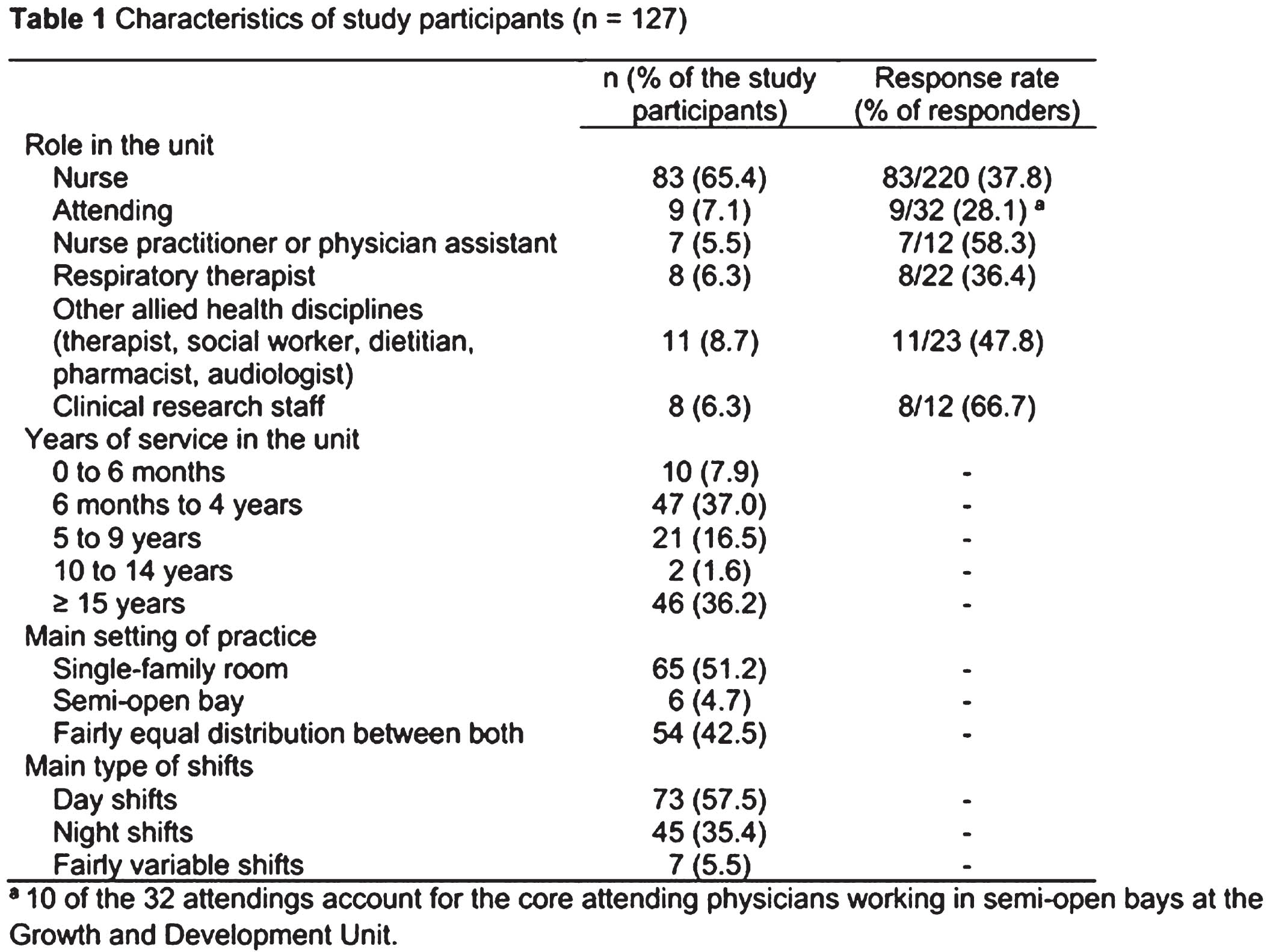
CONCLUSION: Interdisciplinary NICU staff reported varied perceptions on the optimal sensory environment for infants and families. The two NICU physical environments were perceived to have different advantages for patients, families, and the staff. The NICU design may be a modifiable factor which could be leveraged to best support the individual needs of each infant and family within family-centered developmental care framework.
BIBLIOGRAPHY:
1. Tierney AL, Nelson CA. Brain Development and the Role of Experience in the Early Years. Zero Three. 2009;30(2):9-13.
Predictors of neurodevelopmental impairment in preterm infants with unremarkable cranial ultrasound: A Canadian population-based cohort
Jehier Afifi1, Prakesh Shah2, Seungwoo Lee3, Karen Thomas4, Lindsay Richter5, Kamini Raghuram2, Anie Lapointe7, Amit Mukerji8, Jaideep Kanungo9, Alyssa Morin10, Walid El-Naggar11, On behalf of the Canadian Neonatal Follow Up Network
1Dalhousie University, 2University of Toronto, 3Lunenfeld-Tanenbaum Research Institute, Sinai Health, 4McMaster University, 5University of British Columbia, 7University of Montreal, 8McMaster University, 9University of British Columbia, 10University of Sherbrooke, 11Dalhousie University
BACKGROUND: Extreme preterm infants are at high-risk of brain injury and neurodevelopmental impairment (NDI). Previous studies reported significant NDI (sNDI) in preterm infants with no abnormalities on cranial ultrasound screening (CUS), traditionally perceived to have favorable outcomes (1,2). Recent data from population-based cohorts outlining clinical predictors of sNDI in those infants are lacking.
OBJECTIVES: (1) to describe the incidence, perinatal and neonatal characteristics of NDI and sNDI in extreme preterm infants with unremarkable CUS using the Canadian Neonatal Follow Up Network (CNFUN) database; (2) to develop a prediction model of sNDI (any of: CP = GMFCS stage 3, Bayley III <70 in any domain, deafness requiring aids, or bilateral blindness) in those infants.
METHODOLOGY: A retrospective review of a population-based cohort of infants born at 220/7 - 286/7 weeks’ gestation between April 2009 and December 2018. We included infants with unremarkable CUS (no hemorrhage, periventricular leukomalacia or ventricular dilatation) who had neurodevelopmental assessment at 18-24 month of corrected age at a CNFUN Center. We compared the baseline characteristics between infants with no NDI and those with any NDI and sNDI. The population sample was then randomly split into training and testing datasets in 70:30 ratio for model’s development and validation, respectively. Multivariate logistic regression with GEE accounting for clustering by multiples and within site was used. The model’s calibration, discrimination and diagnostic properties in the validation dataset were reported.
RESULTS: Out of 7463 eligible infants, 4327 (58%) were included. Of those, 2501 (59%) had no NDI and 1736 (41%) had NDI. sNDI accounted for 14% of the cohort and one third of those with NDI (Figure 1). Perinatal and neonatal characteristics of the three groups are shown in Table 1. On internal validation, maternal hypertension, maternal level of education, gestational age, male sex, ROP≥ stage 3 and systemic steroids were predictive of sNDI (Table 2). The prediction model had Sensitivity 0.91, NPV 0.90, AUC-ROC 0.69 (95% CI 0.64-0.73) and Precision Recall-AUC 0.37 (95% CI 0.30, 0.45)(Figure 2). The model calibration using Hosmer-Lemeshow test (p =0.98) indicated a good model fit.
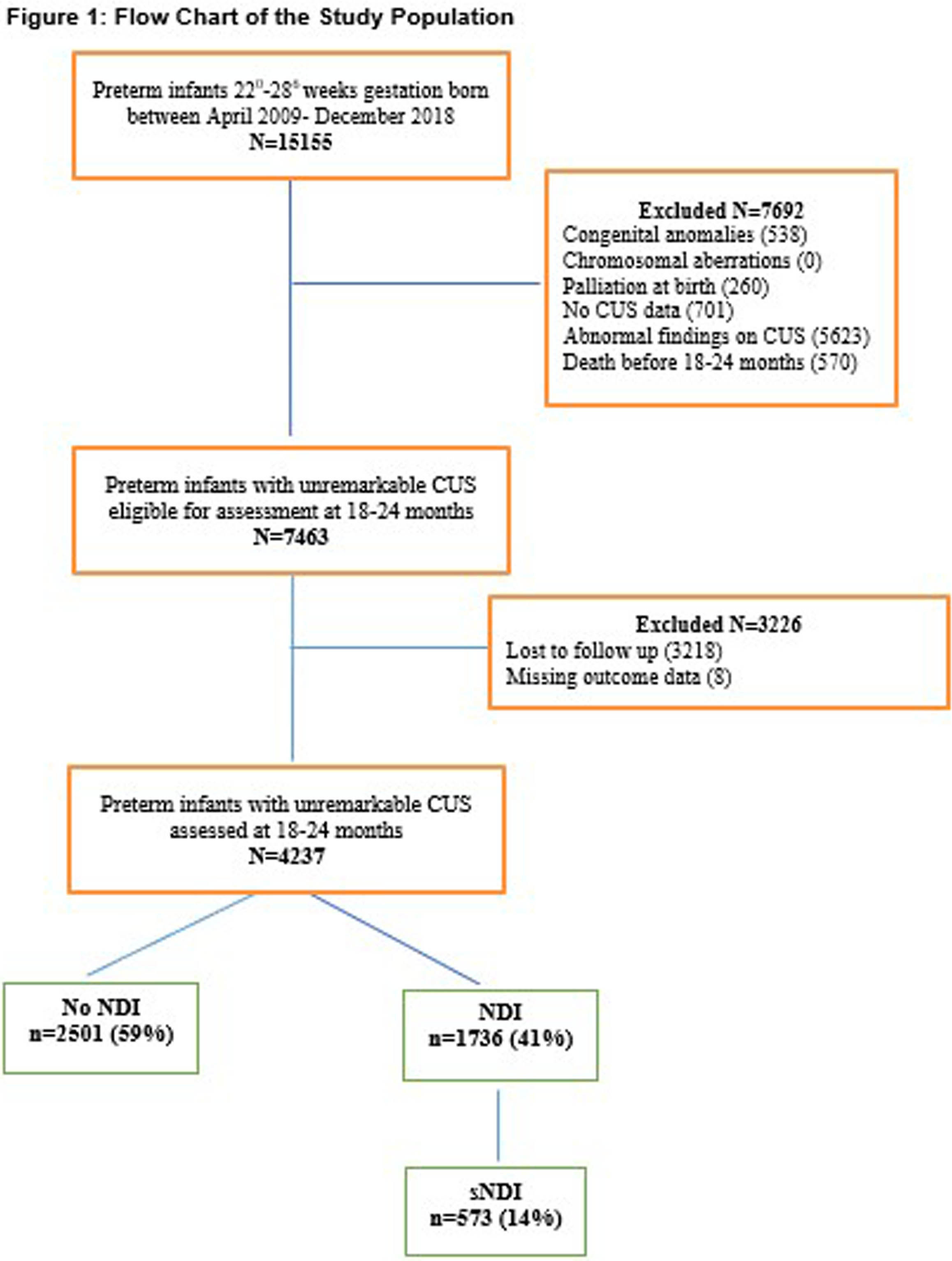
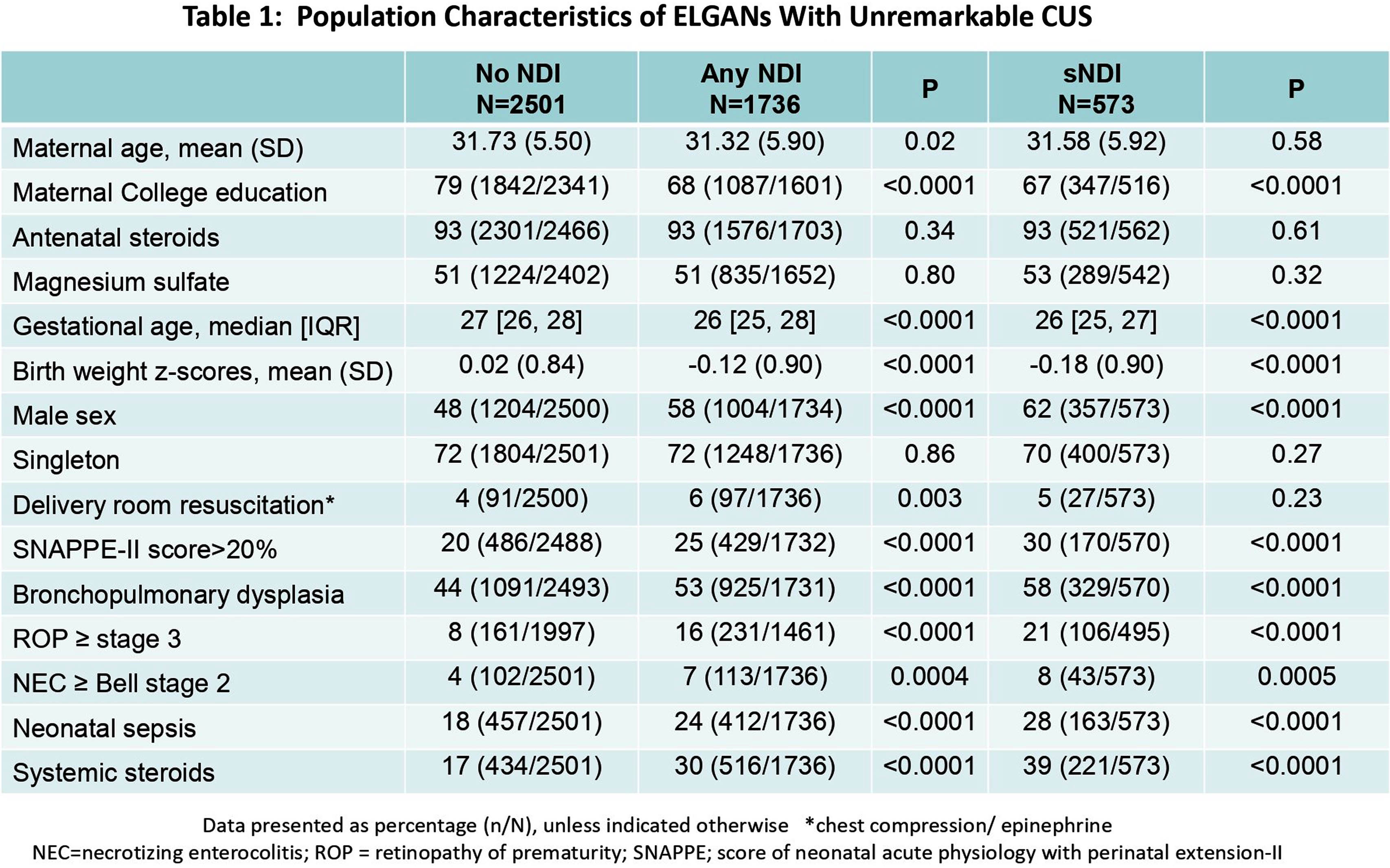
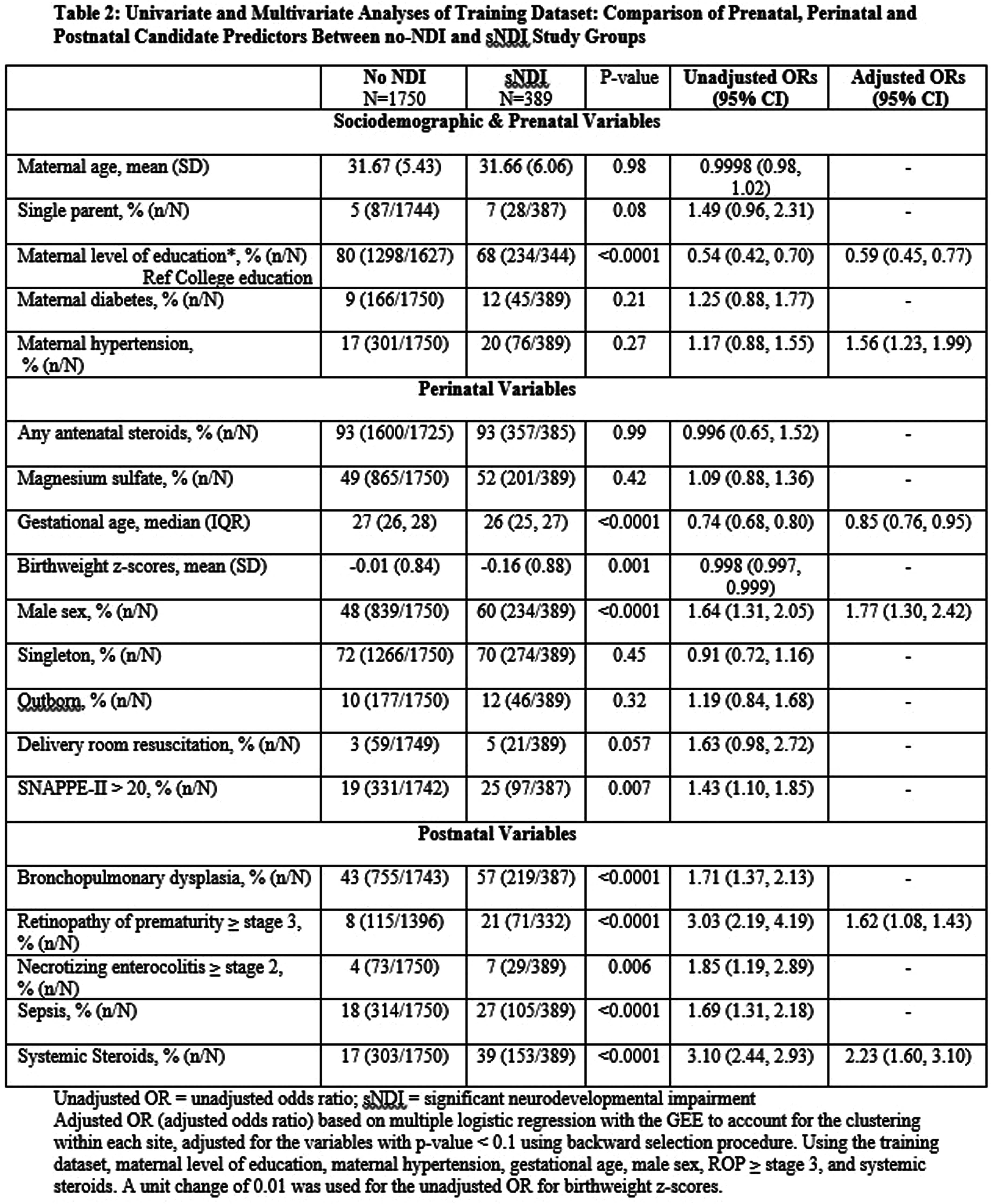
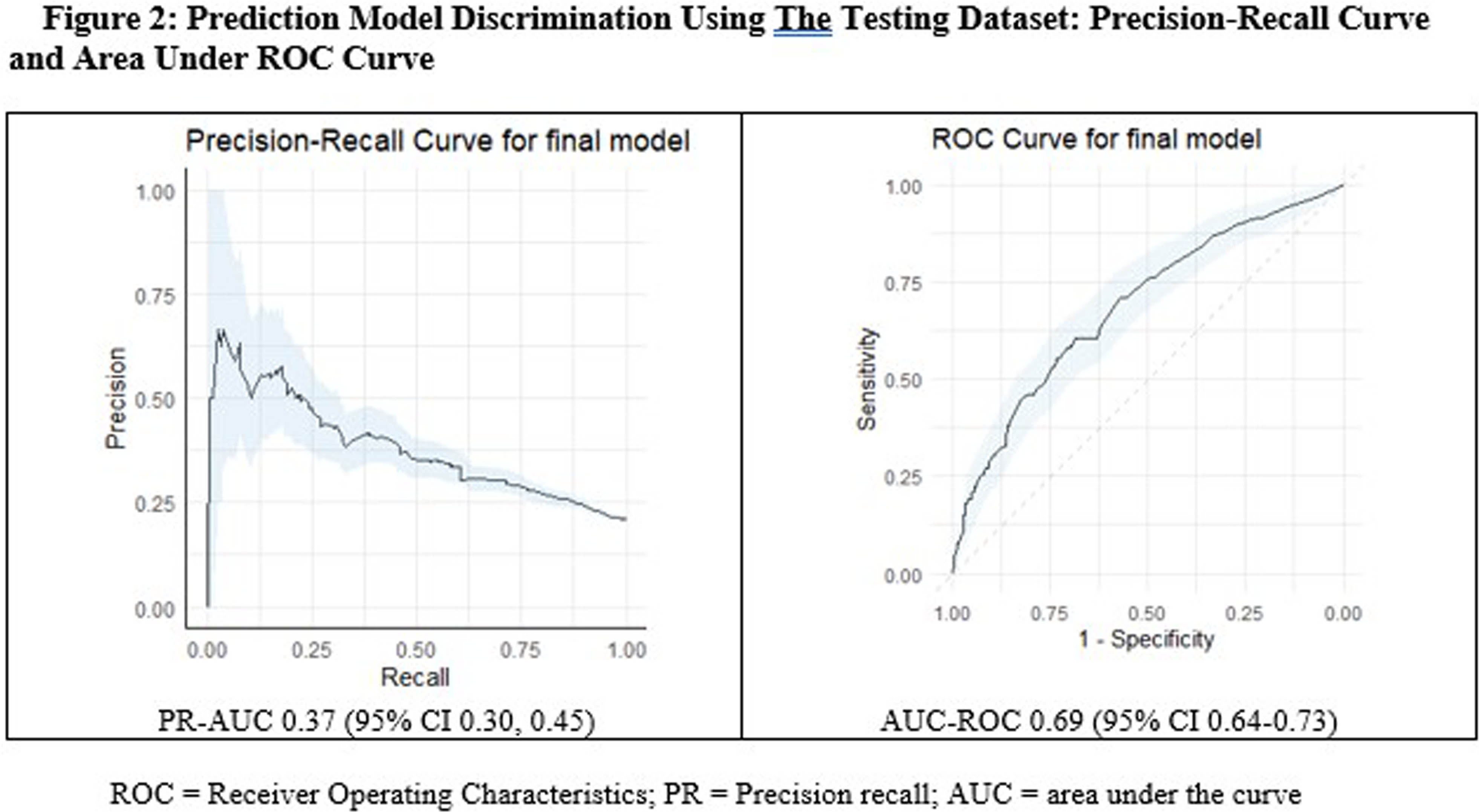
CONCLUSION: In this national cohort, 2 out of 5 extreme preterm infants with unremarkable CUS had NDI and 1 in 7 had sNDI. The prediction model had high sensitivity and NPV, but poor discrimination. This study can help clinicians to identify at-risk infants who may benefit from early targeted interventions.
BIBLIOGRAPHY:
1. Laptook AR, O’Shea TM, Shankaran S, Bhaskar B; NICHD Neonatal Network. Adverse neurodevelopmental outcomes among extremely low birth weight infants with a normal head ultrasound: prevalence and antecedents. Pediatrics. 2005 Mar;115(3):673-80.
2. Sampath V, Bowen J, Gibson F. Risk factors for adverse neurodevelopment in extremely low birth weight infants with normal neonatal cranial ultrasound. J Perinatol. 2005 Mar;25(3):210-5.
Examining the impact of maternal depressive symptoms on early neurodevelopment in infants born preterm
Gabriel Côté-Corriveau1,2, Ariane Léveillée3, Catherine Bernard1, Léanne Brabant1, Mélanie Gagnon1, Véronique Belval1, Mi-Suk Kang Dufour1, Anik Cloutier1, Mathieu Dehaes1,4,5, Marie-Noelle Simard1,6, Thuy Mai Luu1,2
1Research Center, Sainte-Justine University Hospital Center, 2Department of Pediatrics, Sainte-Justine University Hospital Center, 3Department of Obstetrics and Gynecology, Division of Neonatology, University of Montreal Hospital Center, 4Institute of Biomedical Engineering, University of Montreal, 5Department of Radiology, Radio-oncology and Nuclear Medicine, University of Montreal, 6School of rehabilitation, University of Montreal
INTRODUCTION: Maternal postpartum depression (PPD) may affect child development.(1) Giving birth prematurely also increases the risk for PPD.(2) Infants born between 29 and 36 weeks gestational age (GA) represent the majority of preterm births and display developmental vulnerabilities, yet they receive little attention in research and clinical follow-up. The impact of PPD for infants born preterm remains unclear. The aim of this study is to assess the association between maternal PPD risk and child developmental outcomes at two years corrected age (CA) in infants born at 29-36 weeks GA.
METHODOLOGY: We conducted a prospective cohort study of infants born at 29-36 weeks GA that were admitted in a neonatal intensive care unit for at least 48 hours (n = 192). Mothers completed the Edinburg Postnatal Depression Scale at term-equivalent age (TEA) and at 3.5 months CA. The exposure measure was high PPD risk (score > 10) at TEA, 3.5 months CA, and at both TEA and 3.5 months CA, relative to low PPD risk. We measured developmental outcomes at two years CA with the Bayley Scales of Infant and Toddler Development-IV (Bayley-IV), MacArthur Bates Communicative Development Inventories, and Child Behavioral Checklist (CBCL). We assessed the relationship between PPD risk and developmental outcomes using linear and Poisson regression models.
RESULTS: The study population was composed of 192 participants, with a mean GA of 33.2 (±2.0) weeks and mean birth weight of 1860 (±522) grams (Table 1). There were 23 women (12.0%) with high PPD at TEA, 10 (5.2%) at 3.5 months CA, and 13 (6.8%) at both timepoints. At two years CA, a high proportion of children displayed delays across the developmental areas (Table 2). Infants of mothers with high PPD risk at TEA were 2.6 (95% CI 1.2-5.6) times more likely to have cognitive delay compared with infants of low-risk mothers (Table 3). High PPD risk at both TEA and 3.5 months CA was associated with an increased risk of delays in language and socio-emotional areas. There was no association with motor skills.
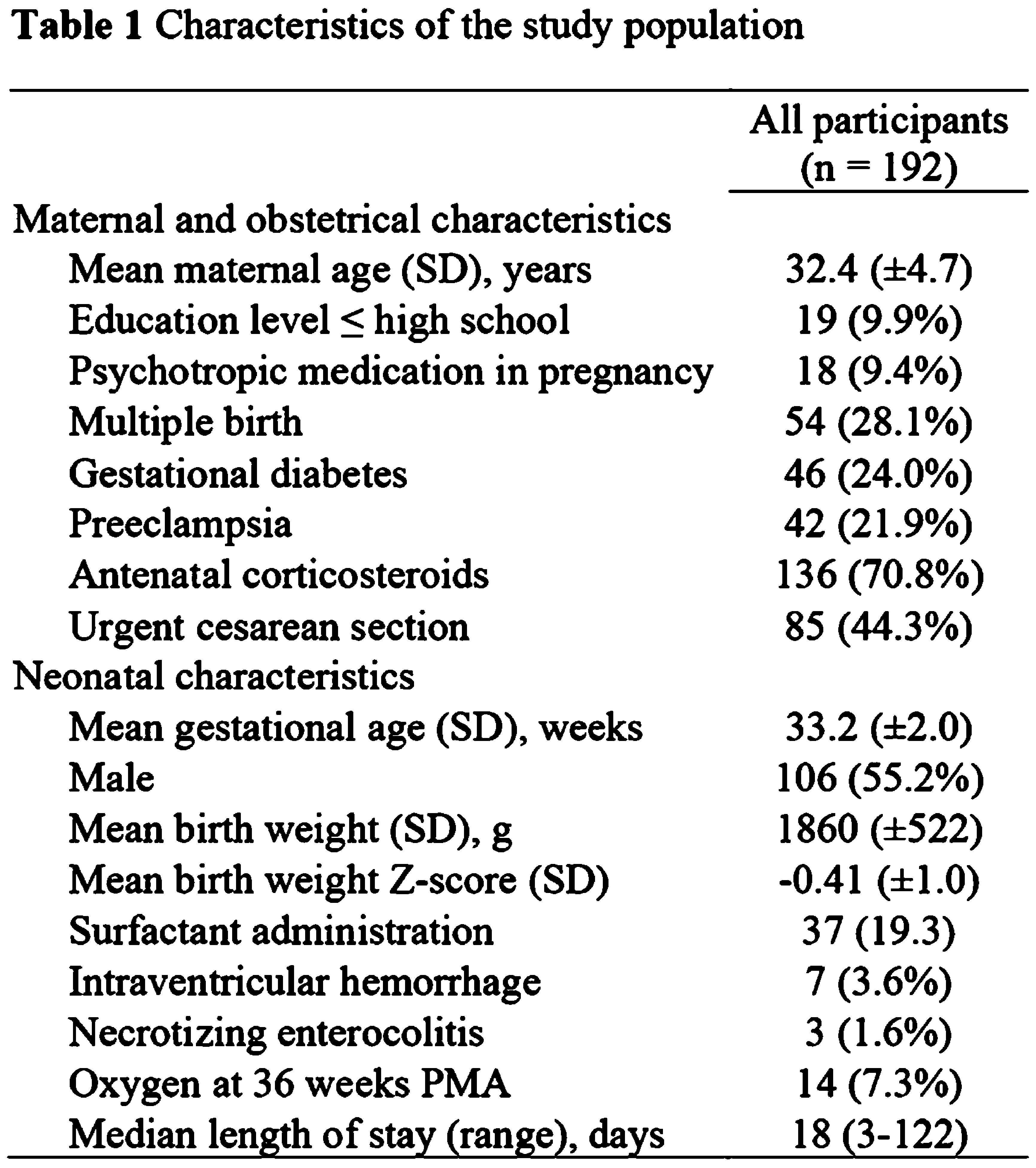
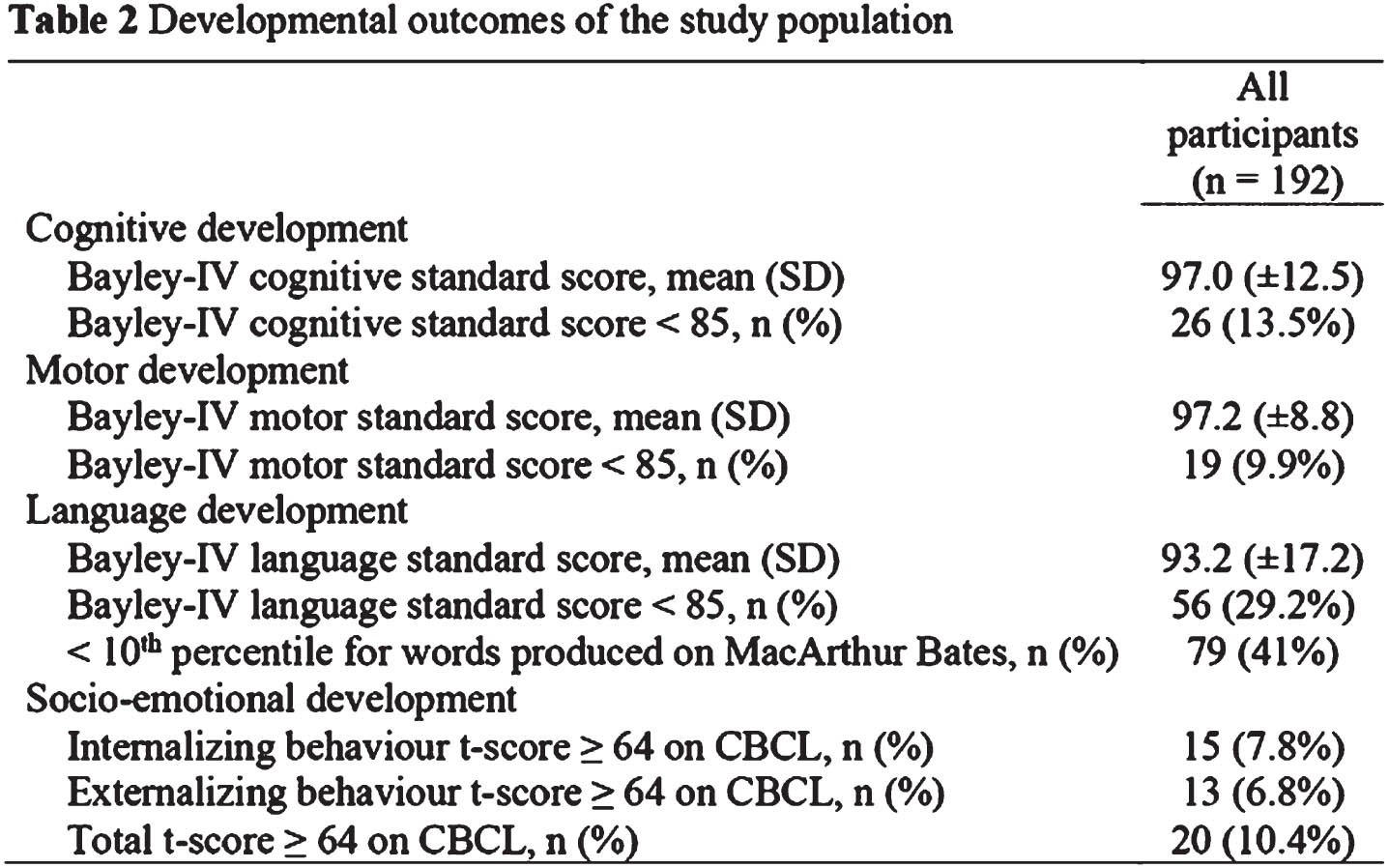
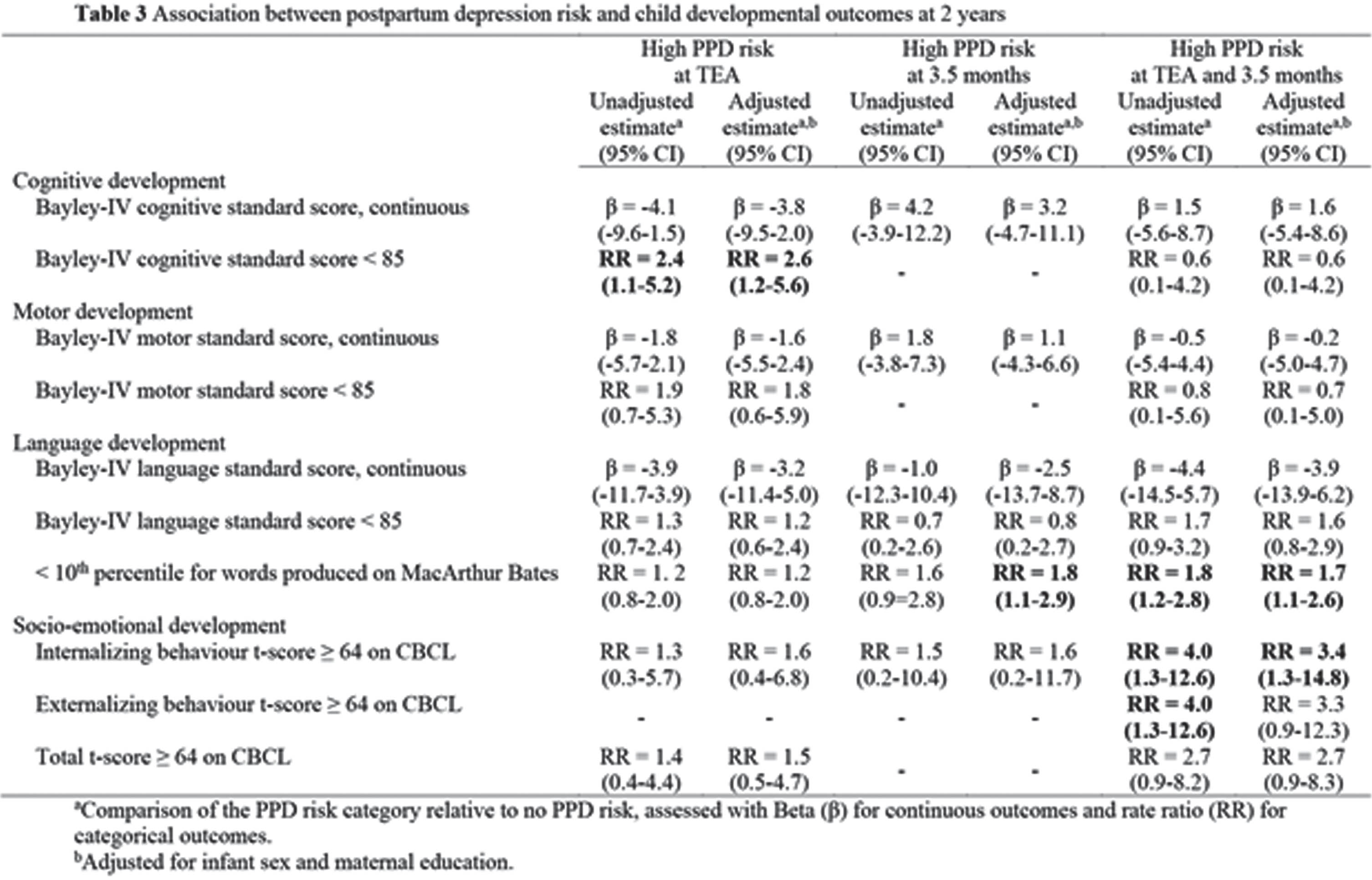
CONCLUSION: High levels of maternal PPD symptoms may increase the risk of cognitive, language, and socio-emotional delays in infants born at 29-36 weeks GA. The findings highlight the need to enhance PPD screening and care strategies for both preterm infants and their mothers.
BIBLIOGRAPHY:
1. Netsi E, Pearson RM, Murray L, Cooper P, Craske MG, Stein A. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry. 2018;75(3):247-253. doi:10.1001/jamapsychiatry.2017.4363
2. Côté-Corriveau G, Paradis G, Luu TM, Ayoub A, Bilodeau-Bertrand M, Auger N. Longitudinal risk of maternal hospitalization for mental illness following preterm birth. BMC Med. 2022;20(1):447. doi:10.1186/s12916-022-02659-9
Developmental outcomes in infants born during the Covid-19 pandemic and who underwent therapeutic hypothermia
Sriya Roychaudhuri1,2, Gabriel Cote-Corriveau1,3, Danielle Sharon1, Hoda El-Shibiny1, Terrie Inder1,4,5, Mohamed El-Dib1,4, Carmina Erdei1,4
1Division of Newborn Medicine, Department of Pediatrics, Brigham and Women’s Hospital, 2Division of Neonatal-Perinatal Medicine, Department of Pediatrics, Surrey Memorial Hospital, University of British Columbia, 3Department of Pediatrics, Sainte-Justine University Hospital, University of Montreal, 4Harvard Medical School, 5Division of Neonatology, Children’s Hospital of Orange County and University of California
BACKGROUND: The pandemic disrupted the social structure and medical services and compounded the stress in families of hospitalized infants.(1) Incidence and management of newborn encephalopathy (NE) benchmark healthcare practices. Infants with NE who undergo therapeutic hypothermia (TH) are vulnerable to brain injury (2), yet developmental outcomes in this population during the pandemic remain unknown.
OBJECTIVE: To assess the impact of Covid-19 pandemic and family-social risk on early neurodevelopment of infants with NE.
METHODOLOGY: We conducted a retrospective review of infants treated with TH for NE in a level 3 center. We compared outcomes of infants born during the pandemic, from 03/2020–09/2021, to infants born before, from 10/2017–12/2019 (Figure 1). Neurodevelopmental outcomes were assessed using the Bayley Scales of Infant Development 4th edition (BSID-4) at 12 months and at 18-24 months corrected age. Baseline demographic data were retrieved, and post-rewarming MRIs were scored for injury. We assessed associations of developmental outcomes relative to the pandemic period using t-tests and chi-square tests and examined the impact of high family-social risk (≥2 risk factors including maternal age <21 years, single marital status, public or no insurance, and ethnic minority) graphically.
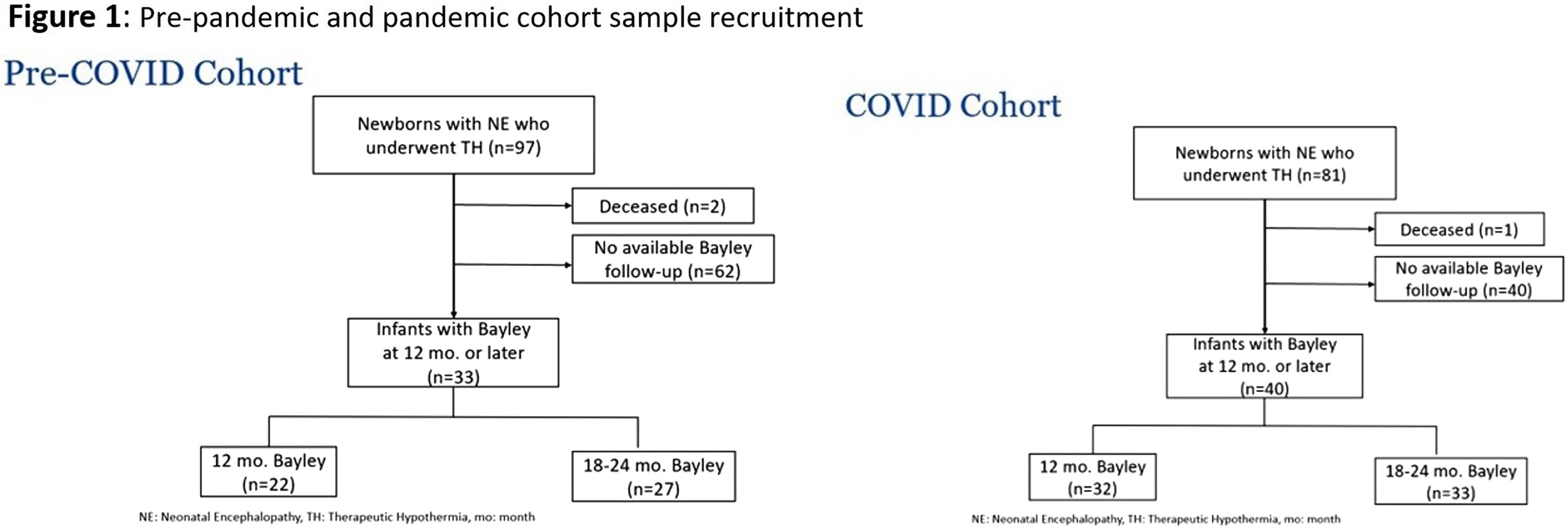
RESULTS: There was no significant difference between perinatal characteristics and baseline severity of injury due to NE in the two cohorts (Table 1). However, the pre-pandemic cohort appeared to experience increased family-social risk (p=0.012). Compared with the pre-pandemic period, infants treated with TH during the pandemic displayed lower language scores (93.3 vs 99.4; p=0.042) and more motor delays (28.1% vs 4.5%; p=0.036) at 12 months (Table 2). Gross motor impairments were more prevalent during the pandemic up to 24 months of age (45.5% vs 19.2%; p=0.035). ASQ and MCHAT scores were comparable. During the pandemic, the gap between language scores of infants from at-risk families compared to low-risk families appeared wider (Figure 2).
CONCLUSION: This study suggests that motor and language outcomes of infants treated with TH for NE may be impacted by the COVID-19 pandemic. The developmental differences despite similar healthcare delivery could possibly reflect limited access to care and post-discharge supportive services, increased family stress, and/or other social factors that may have been impacted by the pandemic. The findings highlight that infants from socially at-risk families may be especially vulnerable in periods such as the COVID-19 pandemic.
BIBLIOGRAPHY:
1. Hosseinzadeh P, Zareipour M, Baljani E, Moradali MR. Social Consequences of the COVID-19 Pandemic. A Systematic Review. Investig Educ En Enfermeria. 2022 Mar;40(1):e10.
2. Ouwehand S, Smidt LCA, Dudink J, Benders MJNL, de Vries LS, Groenendaal F, et al. Predictors of Outcomes in Hypoxic-Ischemic Encephalopathy following Hypothermia: A Meta-Analysis. Neonatology. 2020;117(4):411–27.
Neurodevelopmental outcome of infants born to SARS-CoV-2 positive versus negative mothers during the COVID-19 pandemic
Vanda Pal1,2, Borbala Lukacs1, Krisztina Vargane Tari3, Petra Sztahovits2, Agnes Kothencz2, Miklos Szabo1, Agnes Jermendy1, Csaba Nador2, Fanni Pekli-Toth2
1Department of Pediatrics, Semmelweis University, 2Department of Obstetrics and Gynecology, Ulloi St Division, Semmelweis University, 3Peto Andras Faculty, Semmelweis University
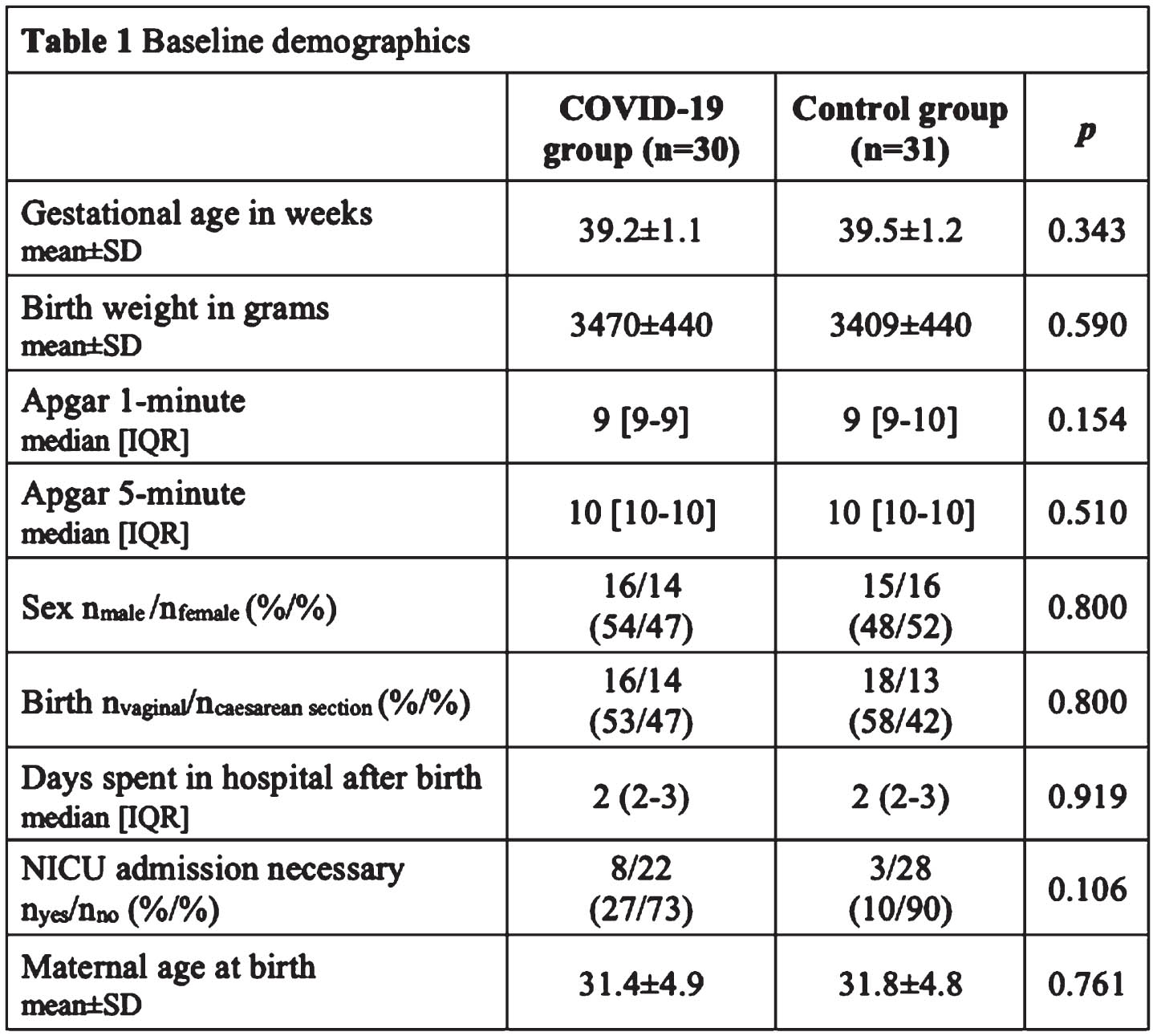
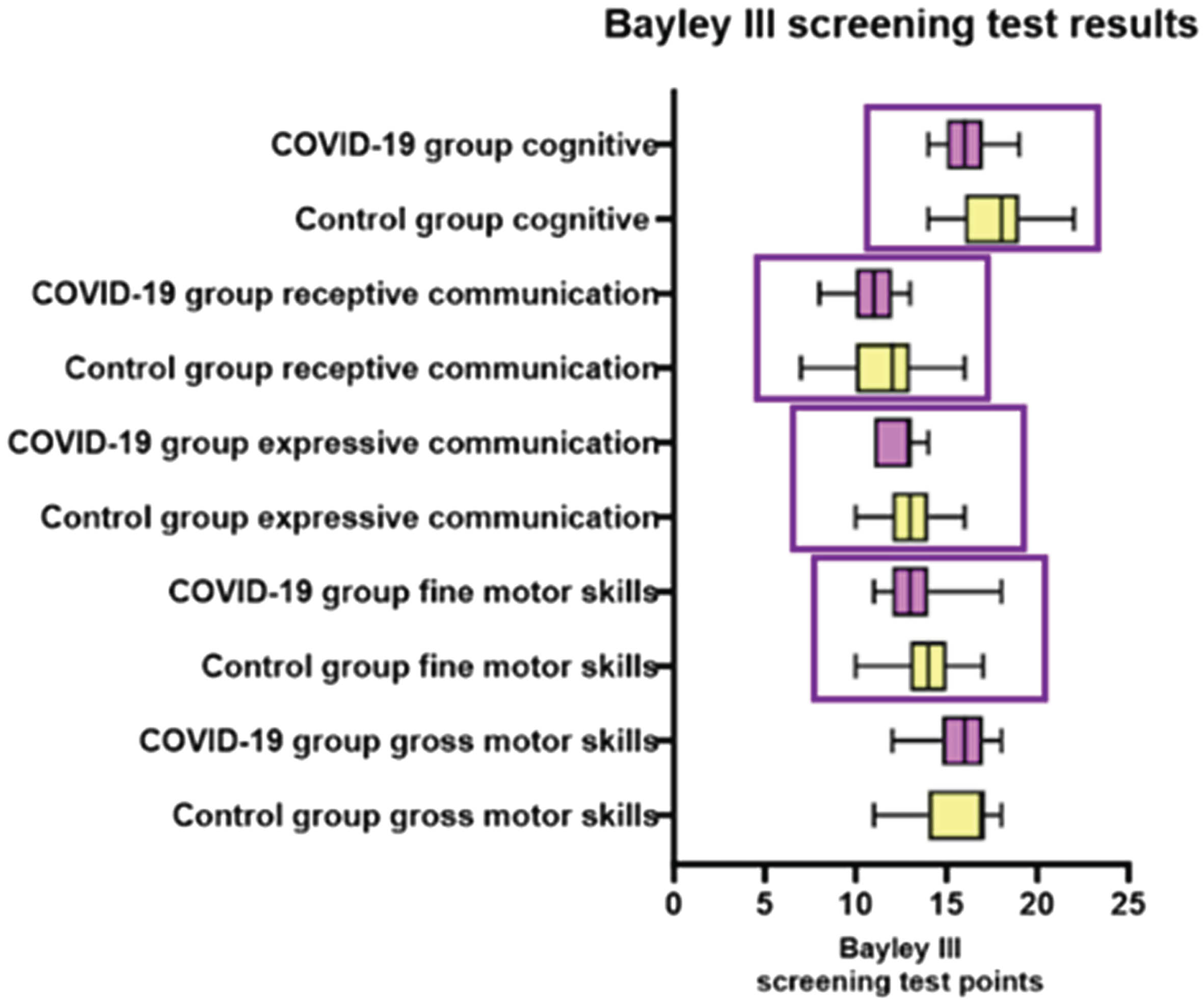
BACKGROUND: Perinatal morbidity and mortality are low among infants born to SARS-CoV-2 infected mothers, however little is known about their long-term neurodevelopmental outcomes. Maternal SARS-CoV-2 infection may have led to increased stress levels, anxiety and poor mental health in families, possibly carrying a risk for neurodevelopmental problems 1. Our aim was to assess the effect of maternal SARS-CoV-2 infection on the neurodevelopmental outcomes of the infants born during the COVID-19 pandemic.
METHODOLOGY: We conducted a case control study between January 2022 and May 2023 at the follow-up clinic of the NICU of the Department of Obstetrics and Gynecology, Ulloi St Division, Semmelweis University, Budapest, Hungary. Infants who were born to SARS-CoV-19 infected mothers (COVID-19 group, n=30) and uninfected mothers (control group, n=31) were examined at 1 year of age using the Bayley Scales of Infant and Toddler Development 3rd edition screening test tool. We also collected data on the duration of breastfeeding (≤6 months vs. >6 months) and maternal education level (no higher education vs. higher education). Preterm infants and patients with missing data in any of the 5 Bayley subtests were excluded. Our primary outcomes were the absolute Bayley III test scores. Data are shown as median [interquartile ranges].
RESULTS: Baseline demographics were similar in the two groups (Table 1). The Bayley III screening tests were completed at a mean age of 12±2 months. We have found that the COVID-19 group scored lower than the control group on the following subtests: cognitive (16 [15-17] vs. 18 [16-19] points, respectively; p=0.002), receptive communication (11 [10-12] vs. 12 [10-13] points; p=0.028), expressive communication (13 [11-13] vs. 13 [12-14] points; p=0.030) and fine motor skills (13 [12-14] vs. 14 [13-15] points; p=0.034). There was no difference in the gross motor skills scores (16 [14.75-17] vs. 17 [14-17], respectively; p=0.342). Duration of breastfeeding and maternal education level were similar in the COVID-19 and control groups.
CONCLUSION: We found significantly lower cognitive, communication and fine motor skill scores but not gross motor skill scores among infants born to SARS-CoV-2 positive mothers compared to controls. Early targeted interventions may ameliorate these impairments and pave the way for long-term follow-up of this vulnerable population.
BIBLIOGRAPHY:
1. Lavallée A, Dumitriu D. Low Risk of Neurodevelopmental Impairment in the COVID-19 Generation Should Not Make Researchers Complacent. JAMA Netw Open. 2022;5(10):e2238958. doi:10.1001/jamanetworkopen.2022.38958
The Bavarian Longitudinal Study (BLS) - Cortico-subcortical structural connectivity is altered in very preterm-born adults
Aurore Menegaux1, Jil Wendt1, Benita Schmitz-Koep1, Dennis Hedderich1, Claus Zimmer1, Dieter Wolke2, Peter Bartmann3, Christian Sorg1
1Klinikum Rechts der Isar, Technical University of Munich, 2University of Warwick, 3University Hospital Bonn
BACKGROUND: Preterm birth is associated with significant risks for long-term impairments in brain structure and cognitive functions (1). At the microscopic level, the transient inflammatory and hypoxic-ischemic events occurring during premature birth disrupt the development of subplate neurons and pre-oligodendrocytes, both of which play a crucial role in the establishment of thalamo-cortical connections and the maturation of the claustrum (2,3). Altered thalamo-cortical connectivity and claustrum microstructure have previously been reported in preterm-born infants (4,5). This study combines findings from two investigations aiming at exploring the long-term consequences of prematurity on these subplate and pre-oligodendrocyte-dependent systems (6).
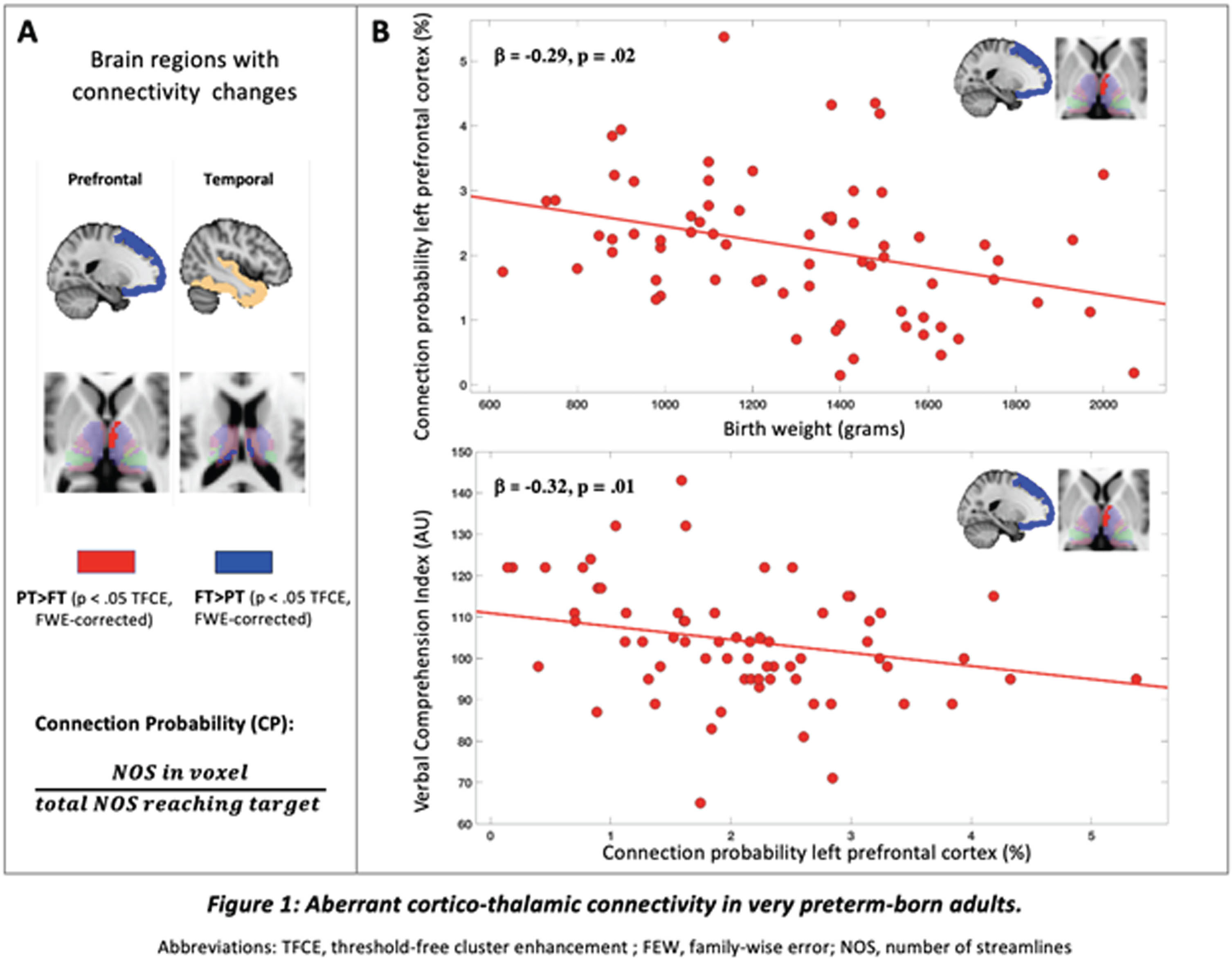
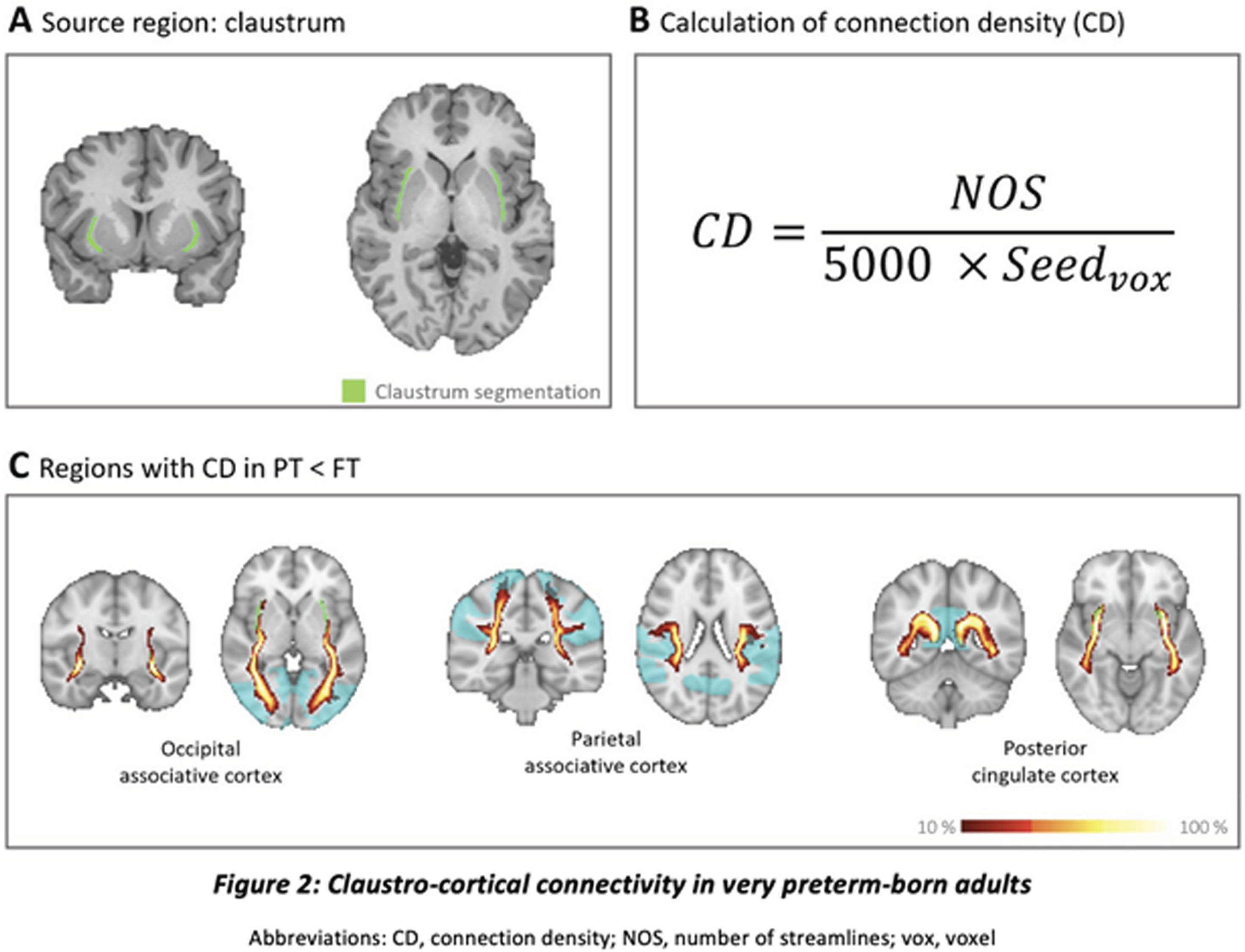
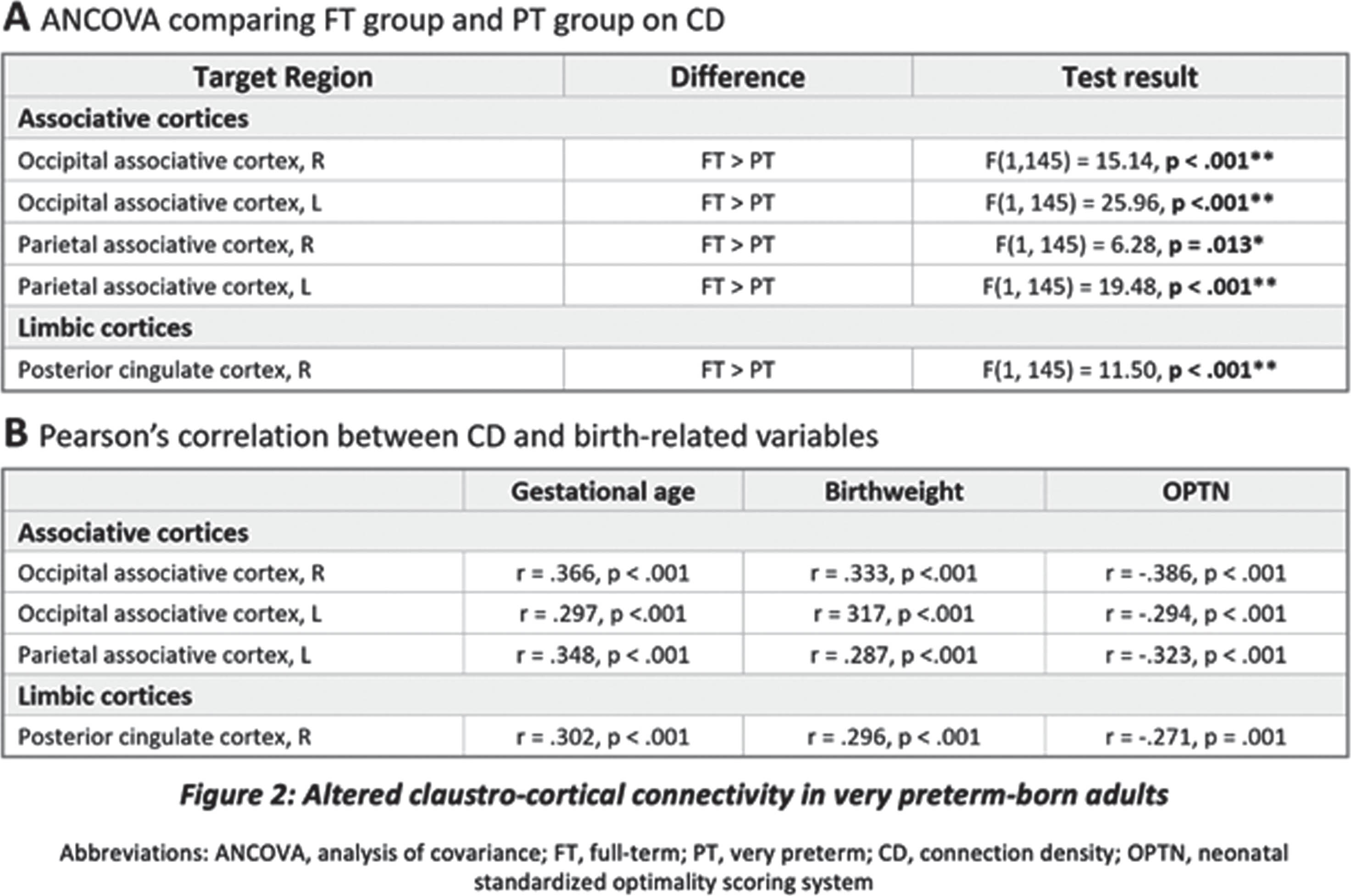
METHODOLOGY: Thalamo-cortical (TC) and claustro-cortical (CC) connections were reconstructed from diffusion-weighted imaging data using probabilistic tractography. Streamlines were generated between bilateral thalami or claustra and cortical regions of interest (see Figure 1A and 2A-C). Connection probability was chosen as metric of TC structural connectivity in a sample of 67 very preterm (PT) and 70 full-term (FT) born adults while CC connectivity was measured as connection density in 65 PT and 81 FT born adults of the BLS at 26 years. In both studies, cognitive performance was assessed by full-scale intelligence quotient (IQ) using the Wechsler Adult Intelligence Scale. Additionally, a verbal comprehension subtest score was computed in the first study. Neonatal medical complications were assessed using a standardized optimality scoring system (OPTI). Differences between groups and their associations with prematurity or cognitive variables were performed via ANCOVAs and linear regressions (study 1) or Pearson correlations (study 2) respectively.
RESULTS: Findings revealed increased connectivity between the left thalamus and left prefrontal cortex in very preterm-born adults, which was associated with both lower birth weight and a lower verbal comprehension score (Figure 1A-B). Furthermore, decreased connectivity between bilateral thalami and temporal cortices in PT born adults positively correlated with the duration of ventilation during the neonatal period (Figure 1A). Finally, lower connectivity between bilateral claustra and parieto-occipital cortices in PT born adults was associated with lower gestational age, birth weight and a higher degree of neonatal complications (Figure 3A-B). Lower left claustro-occipital connectivity was also associated with lower IQ.
CONCLUSION: Together, these findings suggest that prematurity has a lasting impact on cortico-subcortical white matter connectivity, particularly in subplate/pre-oligodendrocytes-derived systems. Furthermore, these alterations are linked to the degree of prematurity and have implications for the persistence of cognitive impairments into adulthood.
BIBLIOGRAPHY:
1. Wolke, D., Johnson, S., & Mendonça, M. Annual Review of Developmental Psychology, 1(1), 69–92 (2019)
2. Ghosh, A. et al. Nature, 347, 179–181 (1990)
3. Bruguier, H. et al. Journal of Comparative Neurology, 28, 2956–2977 (2020)
4. Ball et al. Cortey, 347, 49(6), 1711-1721 (2013)
5. Neubauer, et al., Neuroimage clinical, 37, 103286 (2023)
6. Menegaux, A. et al. Cortex 141, 347-362 (2021)
Sociodemographic characteristics and behavioral outcomes in infants with hypoxic-ischemic encephalopathy
Marie Cornet1, Emily Taketa1, Bryan Comstock2, Natalie Chan1, Hannah Glass1, Elizabeth Rogers1, Sandra Juul2, Patrick Heagerty2, Yvonne Wu1
1Ucsf Benioff Children’s Hospital, 2University of Washington
BACKGROUND: Despite therapeutic hypothermia, half the infants with hypoxic-ischemic encephalopathy (HIE) die or have neurodevelopmental impairment. The frequency, characteristics, and risk factors for behavioral challenges after HIE remain unclear.
OBJECTIVE: To characterize the behavioral outcomes of HIE survivors at 2 years of age, and to identify sociodemographic and clinical risk factors for atypical behavior.
METHODOLOGY: In this secondary analysis of the HEAL Trial (NCT# 02811263), infants with moderate or severe HIE whose caregivers completed the Child Behavior Checklist (CBCL) at two years (i.e., 22-36 months) of age were included. We defined the primary outcome “atypical behavior” as having > 1 behavior rated as clinically significant on the CBCL. We further describe the types and frequencies of all clinically atypical and borderline atypical behaviors. We analyzed the associations between sociodemographic, maternal, and infant clinical factors, and atypical behavior using Chi-squared, Fisher’s Exact test, and t-test as appropriate. Using logistic regression, we evaluated the associations between sociodemographic factors and atypical behavior, adjusting for potential confounders.
RESULTS: Among 435 HIE survivors, 408 (94%) had CBCL data available and comprised the study population. A total of 59 (14%) had at least one atypical behavior at age 2 years, and 33 (8%) had more than one. The most common atypical behaviors were autism spectrum problems (8%), withdrawn (6%), and attention problems (4%, Figure 1). A total of 95 (24%) infants had > 1 borderline atypical behavior. On univariate analysis, maternal factors associated with a higher risk of atypical behavior included younger age, lower education attainment, identifying as Black, and having a non-English language preference (Table 1). In multivariate analysis, lower maternal education was the only independent risk factor for atypical behavior; compared to infants whose mothers completed college, those whose mothers did not finish college (OR 5.4, 95% CI 1.6-18) or never attended college (OR 8.0, 95% CI 2.5-25.9) had a significantly higher risk of atypical behavior. Other sociodemographic and clinical factors were not significantly associated with atypical behavior (Table 2).
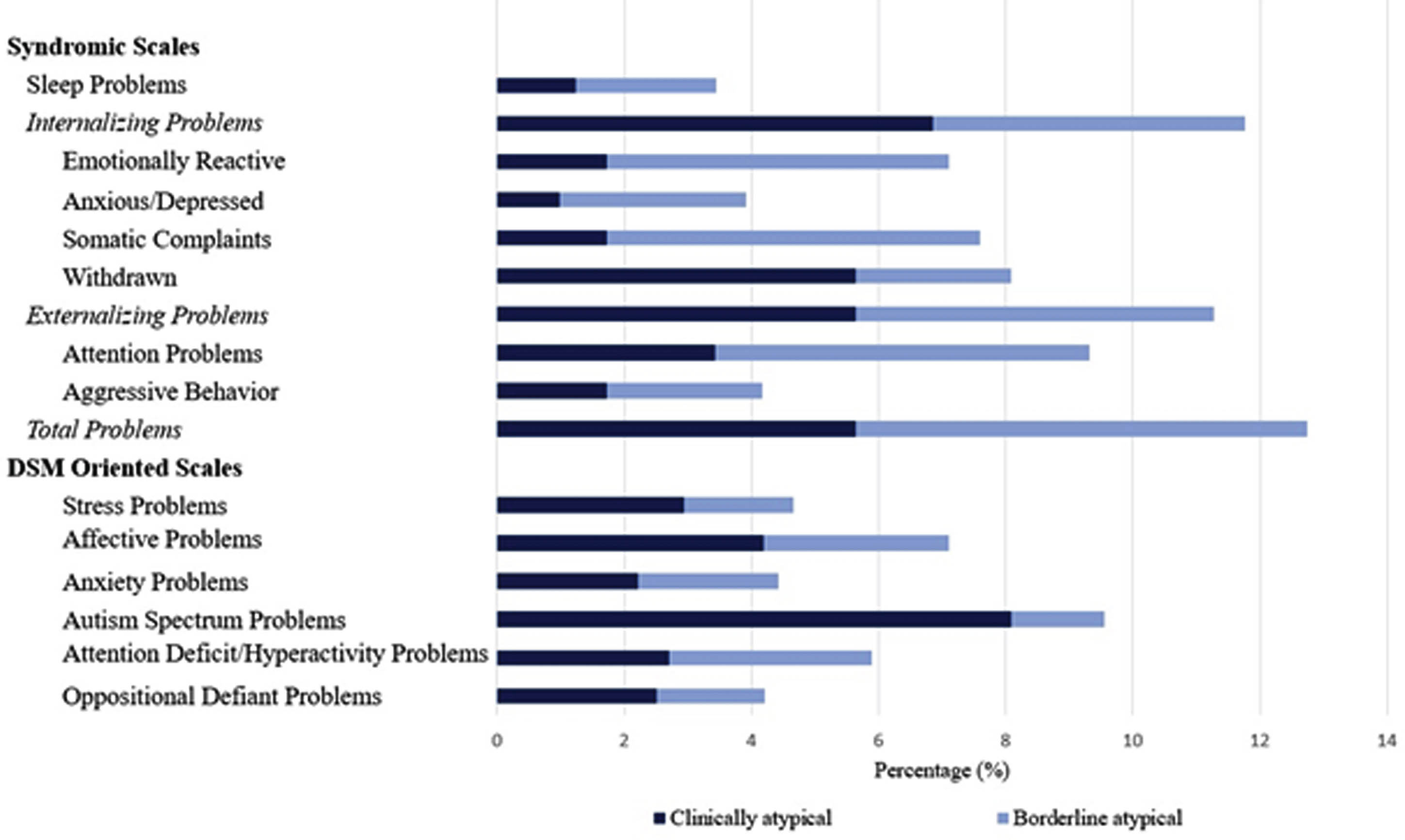
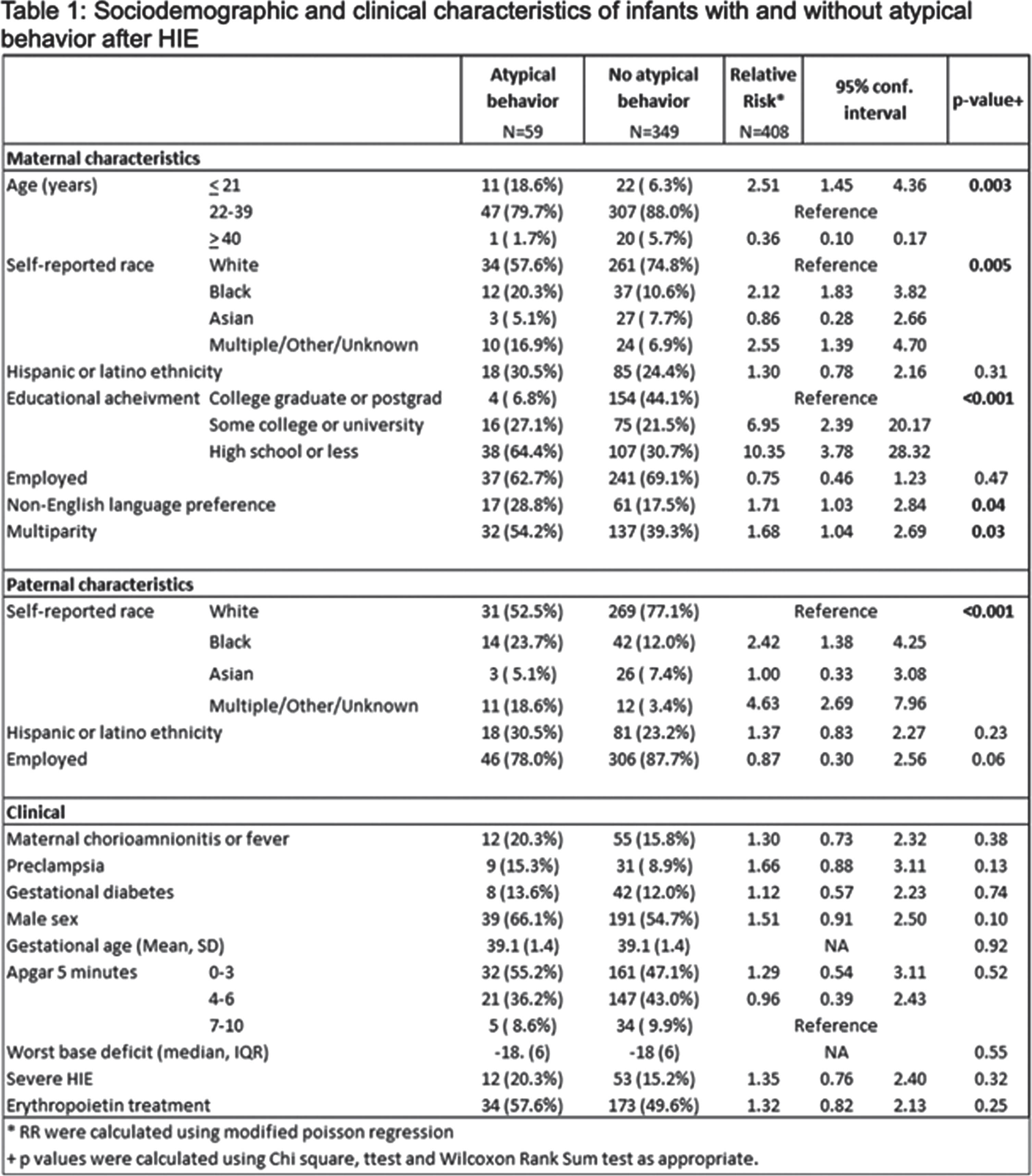
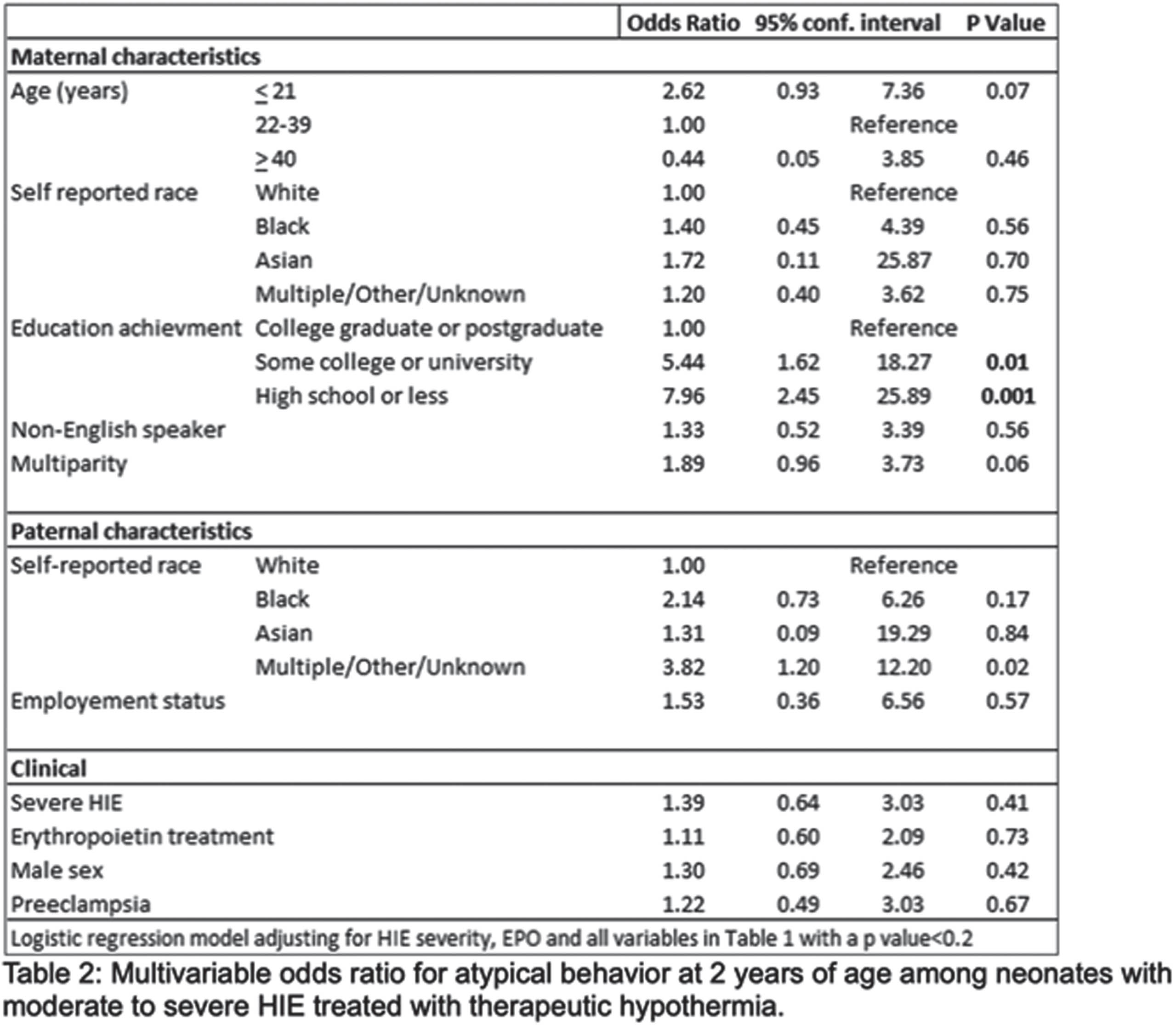
CONCLUSION: Among survivors of HIE, maternal educational attainment was independently associated with the risk of atypical behavior, whereas clinical severity of HIE was not. These findings highlight the importance of social drivers of health in recovery following HIE and identify potential opportunities to improve health equity.
Neurodevelopmental outcome and cerebral oxygenation in preterm infants with intraventricular hemorrhage
Julia Elis1, Mirjam Steiner1, Vito Giordano1, Monika Olischar1, Angelika Berger1, Katharina Goeral1
1Medical University of Vienna
BACKGROUND AND OBJECTIVE: Intraventricular hemorrhage (IVH) is one of the key factors leading to adverse neurodevelopmental outcomes in premature infants. This study investigates the relationship between neurodevelopmental outcomes of preterm neonates who experienced IVH and their cerebral oxygenation levels monitored by near-infrared spectroscopy (NIRS) during the first 20 weeks of life. By examining these connections, our objective is to gain deeper insights into the developmental trajectories of these infants.
METHODOLOGY: In this prospective study, preterm neonates with a gestational age <33 weeks born from 2013 to 2023 were investigated. Regional cerebral oxygen saturation (rScO2) was monitored repetitively from IVH diagnosis for nearly 20 weeks of life. Analysis involved assessing the duration of rScO2 values falling outside the established normal range (<55% or >85%) as well as the computation of fractional cerebral tissue oxygen extraction (cFTOE). Between 2 and 3 years corrected age, infants were tested using Bayley-III, and developmental delay was classified as mild (<85 points), moderate (<70 points), and severe (<55 points). Median NIRS values were analyzed according to those neurodevelopmental outcome categories.
RESULTS: This study included 116 preterm infants diagnosed with IVH, born with a median gestational age of 25.4 (24.3-27.6) weeks. Among them, 31.0% (n=36) did not survive, while 69.0% (n=80) were tested at a median corrected age of 2.02 (1.99-2.08) years. Our findings revealed significant disparities in cerebral oxygenation levels among outcome groups. Specifically, infants with severe cognitive impairment exhibited lower rScO2 values (61.1% vs. 55.9%, p=0.04), longer durations of rScO2 outside the established normal range (10.5% vs. 46.7%, p=0.05), and higher levels of cFTOE (0.35 vs. 0.40, p=0.04) compared to IVH infants showing normal development. Similar differences were observed for motor outcome (rScO2: 62.9% vs. 56.0%, p=0.04; cFTOE: 0.32 vs. 0.40, p=0.03). However, patients with mild or moderate cognitive and motor impairment did not show significant differences compared to IVH patients without developmental delay. Furthermore, no correlations were found between language scores and NIRS parameters.
CONCLUSION: This study emphasizes the profound cerebral effects and neurodevelopmental consequences in neonates affected by IVH. A correlation between measured cerebral oxygenation parameters during the first 20 weeks of life and adverse neurodevelopmental outcome was demonstrated, particularly in cases with severe cognitive and motor impairment.
Parent-child interaction and child development in the context of NE
Elizabeth Nixon1, Chelo Del Rosario1, Eleanor Molloy1, Jean Quigley1
1Trinity College Dublin
BACKGROUND: Research investigating the development of children born with NE has focused on clinical outcomes measured using standardised instruments. However, due to the heterogeneity of NE, the developmental profile of NE remains relatively undefined and the underlying processes that influence the development of children affected have yet to be investigated. The examination of parent-child interactions is a well-established approach widely used to examine developmental processes that influence child development but has yet to be applied in the context of those born with NE. In an attempt to provide further insight into the impact of NE on development this research examined the association between interactions between mothers and children born with NE and children’s language and cognitive developmental abilities.
RESULTS: Mother-child dyads where children were born with NE (n= 17, mean age 56.35 months) and dyads with children born without complications (n = 17, mean age 53.12 months) were compared. Naturalistic interactions of children and their mothers at play were recorded and an age-appropriate standardised assessment of development was administered to assess children’s developmental abilities. Overall, children born with NE were found to perform significantly worse on assessments of language abilities. However, no differences were observed in domains of cognition apart from lower speed of processing in the cohort of children aged 4 and older. Developmental risk factors associated with NE such as neonatal risk, autism traits, executive functioning and sleep problems and associations with developmental outcome scores were also examined. A sizeable proportion of the children born with NE exhibited a high number of autism traits and EF deficits. More than half of children who showed these developmental risk factors also received below average scores on assessments of language and motor abilities and the language and motor abilities in children born with NE were highly correlated. These findings suggest that children who exhibit autism traits and EF difficulties are more likely to experience delays in language and motor development and further that deficits in motor functioning caused by NE are linked to difficulties in other domains of development.
CONCLUSION: Analysis of the speech produced during interaction revealed that mothers of children born with NE used fewer words per turn compared to mothers of children born without complications, a pattern of speech that may assist in sustaining the child’s attention. Further, children born with NE used more nouns in their speech compared to children born without complications. This noun bias may indicate difficulties in acquiring and using more advanced language structures and word types. These novel findings provide a more detailed picture of the development of children born with NE and identify specific areas for NE specific interventions.
Early intervention guided by the general movements examination at term corrected age: Short term outcomes
Adrian Ioan Toma1,2, Alexandra Florinana Nemes1,2, Andree Necula1, Roxana Stoiciu1, Alina Fieraru1, Adelina Alexe3
1Life Memorial Hospital, 2University Titu Maiorescu. Faculty of Medicine, 3Independent Kinetotherapy Practice
BACKGROUND: The early identifications of the former premature neonates at risk for neurologic sequelae could lead to early intervention and a better prognosis. The more simple the identification means are, the more prone are to be applied in a larger population. The aim of our research was to identify if the general movements patterns noted at term equivalent age in the former premature infants could guide early intervention and lead to a better prognosis.
METHODOLOGY: Among a population of 44 premature neonates (mean gestational age 33.59 weeks (+2.43 weeks) examined at term equivalent age, there were identified 10 neonates with a cramped-synchronized general movements motor pattern. These neonates were included in an early intervention programme, consisting in physiotherapy executed both by the therapist and by the parents at home. They were again examined at the age of three months corrected age. There were noted the presence or absence of the fidgety movements and the MOS (motor optimality score). The examinations were performed by certified specialists.
RESULTS: 9 of the 10 former premature infants presented normal fidgety movements and a MOS of 20-24 ( mean 22 with normal foot to foot contact present in 7/10, normal hand to hand contact present in 5/10. The atypical patterns noted were side to side movements of the head 5/10, head centered 9/10, asymetrc tonic neck reflex 9/10 and jerky movements 10/10.
CONCLUSION: early intervention in our group of patients allowed the improvement of the infaust prognosis given by the presence of the cramped-synchronized movement pattern and this conduct should be part of all the follow up programs.
Understanding the development of higher order cognitive skills in infants born preterm: A pilot study
Srishti Jayakumar2, Jade Robinson3, Marilee Allen2, Vera Burton1, Gwendolyn Gerner1
1Kennedy Krieger Institute, 2Johns Hopkins University School of Medicine, 3Johns Hopkins University
BACKGROUND: The AB task, developed by Piaget1 requires the presence of object permanence and examines behavioral responses associated with development inhibitory control and working memory, which comprise early executive function (EF). Historically, it is well documented that healthy and typically developing infants demonstrate increasing success on this task from ages 7 ½ to 12 months. Development of early EF is less understood in children born preterm, despite evidence that by school-age, many have impairments regardless of structural brain injury.2 Thus, understanding the development of inhibitory control and working memory in this population is critical to promote early detection of EF impairments and inform targeted early interventions.
METHODOLOGY: A cross-sectional cohort of children born preterm were enrolled. Pertinent data were extracted from electronic medical records (i.e., clinical imaging results). The AB task, described by Diamond,³ was administered across four chronological age groups (i.e., 9-10, 11-12, 13-15, and 16-18 months). Measures of dispersion and center were calculated for the sample. Percentages of training and reversal trials success were calculated for each age group and compared across age groups.
RESULTS: Across the entire sample, mean gestational age was 28.5 weeks (SD=3.12). 34% had a history of structural brain injury on clinical imaging. Successful completion of 2-second delay training for ages 9-10 (30.8% success on training) and 11-12 months (54.5% success) was limited but improved with chronological age, increasing sharply between ages 13-15 months (73.3%) and continuing to improve by 16-18 months (85.7%). There was no success on reversal trials in the 2-second delay condition for ages 9-10 months, and 11-12. Success on reversal in ages 13-15 and 16-18 months increased but remained below 50%. There was limited progression to delay trials. Of those who progressed, success was <10%.
CONCLUSION: In Diamond’s³ cross sectional study of typically developing full-term infants, success on the AB task with 2-second delay was achieved by 12 months. In this cross-sectional pilot study of preterm infants, all aspects of performance were delayed and task success on the 2- second delay condition remained below 50% by ages 16-18 months. Although degree of prematurity and the presence of structural brain injury may contribute to these findings, these factors alone do not explain the observed findings. This study describes a low-cost method to detect subtle delays in development to facilitate timely intervention.
BIBLIOGRAPHY:
1. Piaget, J. The Construction of Reality in the Child. Basic Books. New York. 1954 [Original French edition, 1937]
2. Taylor, G. & Clark, A.C. Executive function in children born preterm: Risk factors and implications for outcome. Seminars in Perinatology. 2016; 40: 520-529.
3. Diamond, A. Development of the ability to use recall to guide action, as indicated by infants’ performance on AB. Child Development. 1985; 56: 868-883.
Neurological outcomes of a multidisciplinary premature follow-up model in Israel
Alla Kuzminsky1, Elena Segal, Noy Huta, Tal Wald, Alon Kalter, Tamar Steinberg
1Shnaider’s Children Medical Center of Israel
2Kupat Holim Clalit
BACKGROUND: An increase in preterm deliveries is noticed all over the world (1.3.4). In Israel, 10% of deliveries are born preterm yearly (2,8). Prematurity is an important risk factor for neurological complications (1.3.5.6.9), including cerebral palsy (CP), growth developmental delay (GDD), autism spectrum disorder (ASD), developmental language disorder (DLD) and learning disorders. The Israeli ministry of health recommends the initiation of developmental follow up as soon as possible after discharge, to prevent these complications and facilitate developmental catch up(8). Therefore, a multidisciplinary clinic that follows preterm babies was established both in Schneider’s Medical Center and Child Developmental Center, Clalit, in Natanya. These clinics accept babies born before 32+6 weeks of gestation or weights less than 1500 grams. This study aims to test if early follow up results in earlier diagnosis of common neurological complications, and if early intervention improves neurological outcomes.
METHODOLOGY: Follow up centers were established 5 years ago, and more than 400 children are being followed. This work presents data of 132 children who completed 2 years of follow up. For each child, developmental quotient (DQ) scores by Griffith Developmental Assessment III (19), were assessed at each visit. Every child underwent 3-4 developmental assessments from the age of 3-4 months to the age of 24 months. When complication was diagnosed, intervention (physiotherapy, occupational therapy and speech therapy) was promptly initiated.
RESULTS: Neurological complication rates were 16% for GDD (DQ<70), 6% for ASD and 10% for CP. 30% babies were diagnosis of CP as early as 6 month with mean diagnosis given at 13 month. As the babies grow up a decline of the DQ scores was found, while language component of the Griffith score was shown the most affected (Figure1).
Fig 1.
Developmental profile of the entire study, divided into 4 visits by age (1st visit at 3-6 months of chronological age, 2 visits at 6-9 months of , 3rd visit at 12-15 months and 4th visit at the age of 24-25 m), also divided into 4 developmental scales (cognitive, speech, fine motor and auditory motor).
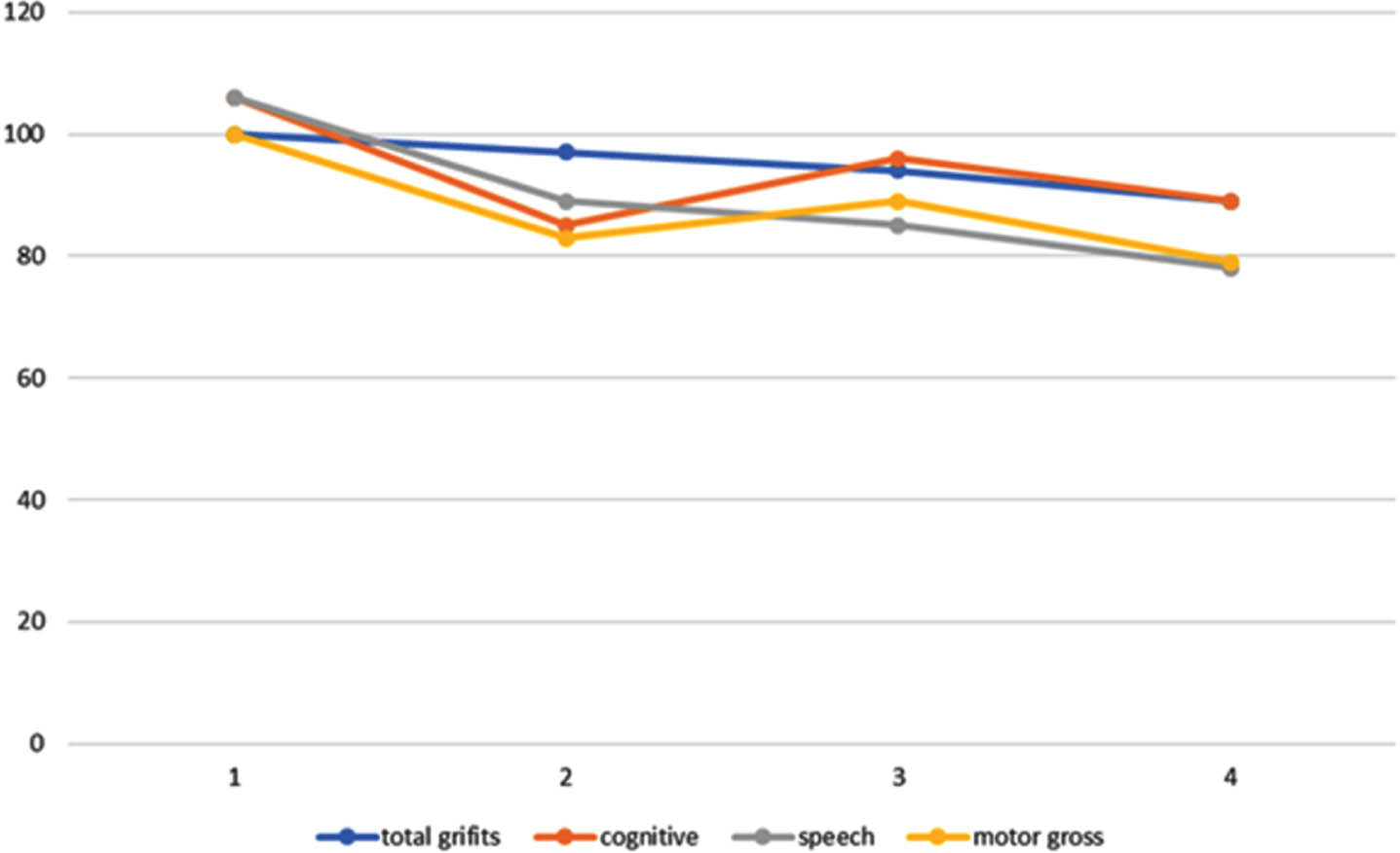
Fig 2.
DQ by 4 visits in the follow up preterm clinics.
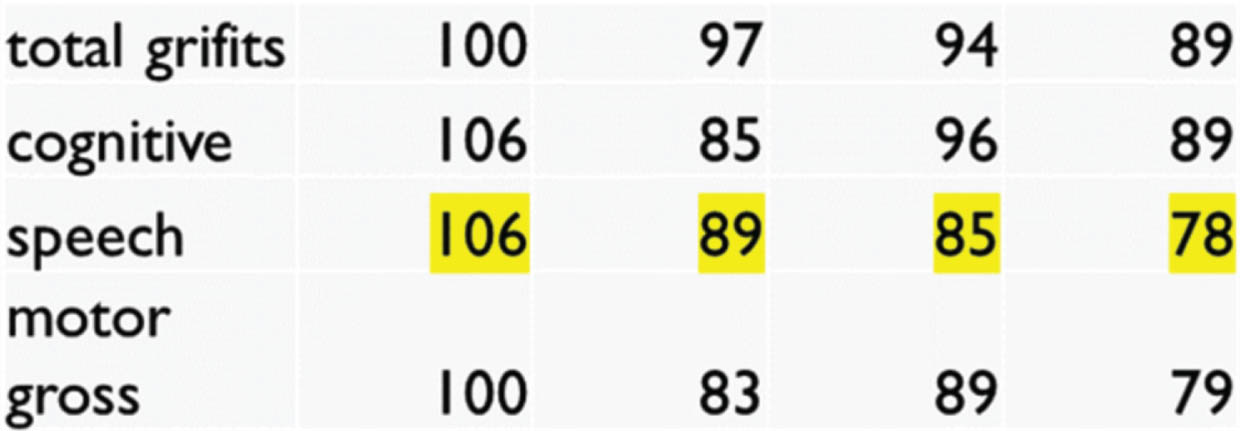
CONCLUSION: Early follow-up for preterm babies aims to identify primary signs of developmental delay and promotes early intervention. We found that crucial diagnosis, as CP, can be established as early as 6 month age. Prompt diagnosis made therapy possible.
During our follow up, a decline in DQ was demonstrated for all developmental fields, language abilities were profoundly affected, been an additional risk factor for future complications. Therefore, we believe preterm babies should be monitored well after 24 month age.
Evaluating 2-year outcomes using language-based and non-verbal, tablet-based developmental test in an ethnically diverse population
Colleen Haughey1, Muthanna Samara2, Neil Marlow3, Deirdre Murray1
1University College Cork, 2King’s College London, 3University College London
BACKGROUND: The Bayley Scales of Infant and Toddler Development are one of the most commonly used methods of standardised developmental assessment (1). The Bayley-III was standardised in English, relying on the child’s ability to understand verbal instruction. Although multiple translated versions exist, few countries have re-standardised the test using local languages. In contrast, Babyscreen—a non-verbal, tablet-based assessment—may provide comparable scores across different ethnic and language groups (2). Qatar comprises a highly diverse society, allowing us to examine the effect of ethnicity on developmental testing. Our aim was to assess the effect of ethnicity on scores from both Bayley-III and Babyscreen.
METHODOLOGY: A secondary data analysis of a prospective cohort study of preterm and term infants born in Qatar between September 2016 and September 2017 (Q-Prem). The gestational age (GA) of the Q-Prem cohort was purposefully skewed towards preterm birth. Outcome evaluation at 24 months, corrected gestational age (CGA), included Bayley-III composite scores for motor, cognitive, and language skills—in the child’s home language—and Babyscreen (1, 2). Data analysis was performed using R version 4.3.2.
RESULTS: Of the 710 infants entered into Q-Prem, 321 completed both Bayley-III and Babyscreen at 24mths and are analysed here. Median GA was 32.8 weeks (IQR 30.1-36.0), birthweight 1980g (1250-2520), and CGA 24.1m (24.0-24.3). Maternal ethnicity was categorised in 5 groups: 88 Arab Qatari, 149 Arab non-Qatari, 42 South Asian (Indian, Pakistani, Bangladeshi), 25 Filipino, 17 Other. Scores in all groups were lower than expected norms among both term and preterm infants: overall Bayley-III cognitive composite 95.5 (SD 13.9), motor 91.9 (SD 13.8), language 87.4 (SD 11.7). In contrast, Babyscreen scores were similar to published norms for term infants: mean 12.7 (SD 3.7) (2). Cognitive composite scores varied by GA: infants <32w (n=125): 92.7 (SD 13.7); 32-36 weeks (n=153): 97.2 (SD 13.9); infants >36 weeks (n=43) 97.4 (13.2). Cognitive composite scores correlated with GA (p=0.001), and CGA (p=0.001). Babyscreen scores correlated with birth weight z-score only (p=0.03). There was significant variation in outcome across ethnic groups for the Bayley-III cognitive and motor domains (p<0.001). Babyscreen scores were similar across ethnic groups (Figure 1).
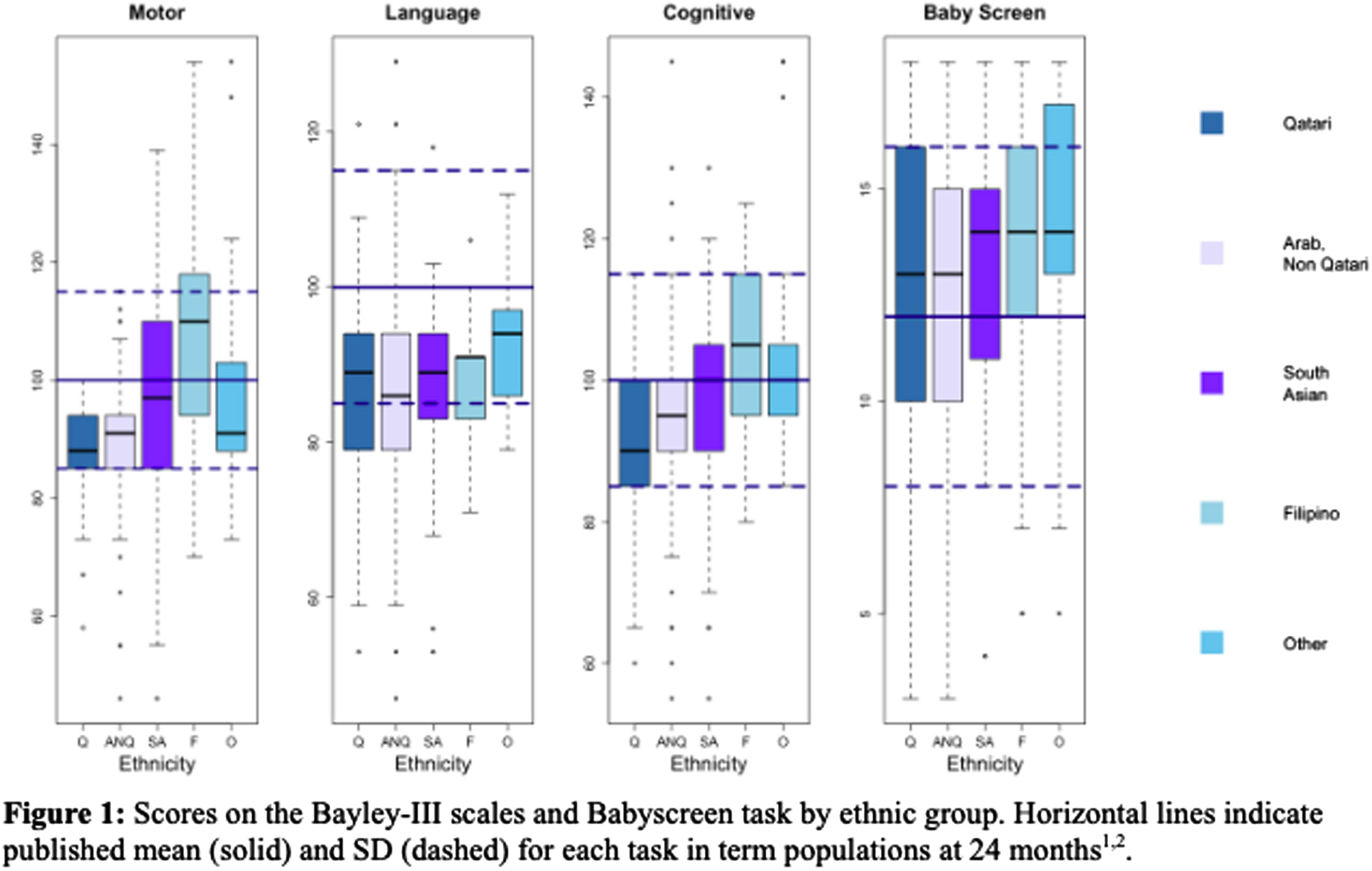
CONCLUSION: In this diverse group of high-risk infants at 24 months, Bayley-III cognitive, motor, and language scores varied by ethnic group despite administration in the child’s home language. In contrast, Babyscreen scores were similar across ethnicities and may provide comparable outcomes in different ethnic groups.
REFERENCES:
(1) Albers et al. Bayley Scales of Infant and Toddler Development– Third Edition. San Antonio, TX: Harcourt Assessment. Journal of Psychoeducational Assessment. 2007 Jun 1;25(2):180–90.
(2) Casey T et al. Validation of a touchscreen assessment tool to screen for cognitive delay at 24 months. Developmental Medicine & Child Neurology. 2023;00:1-9
Early detection of cerebral palsy in Ireland- network implementation
Pamela O’Connor1, Joanne Egan2, Brona Fagan3, Anna Hamill3, Breda Hayes3, Mairead Hughes2, John Kelleher4, Sara Kift4, Eithne Lennon2, Colette Lynch5, Margaret Moran3, Madeleine Murphy2, Deirdre Murray1, Kannan Natchimuthu5, Roisin Phipps4, Mary-Ann Ryan1, Deirdre Sweetman2, Susan Vaughan5, Rachel Byrne6, Nathalie Maitre7
1INFANT Research Centre, 2The National Maternity Hospital, 3The Rotunda Hospital, 4The Coombe Women and Infant’s Hospital, 5Cork University Maternity Hospital, 6The Cerebral Palsy Foundation, 7Emory University
BACKGROUND: Early diagnosis of cerebral palsy (CP) is critical to allow evidence-based interventions when plasticity is greatest. In 2017, international guidelines for early detection of CP were published.1 Implementation of these guidelines across a large US network was shown to reduce the age of CP diagnosis to <9.5 months of age. In Ireland the four Tertiary NICUs deliver >50% of all births, and care for the majority of high-risk infants (HRIF) nationally; >70% of Very Low Birth Weight Infants, and all Therapeutic Hypothermia cases. Our study aim is through consistent implementation of these international guidelines to reduce the age at CP diagnosis to <12 months of age across a network of tertiary NICU HRIF follow-up programs in Ireland.
METHODOLOGY: This is a three year implementation research project. The initial focus has been to establish a collaborative national network across all tertiary NICUs, and implement standardized assessments for HRIF follow-up based upon international guidelines across this network. The study is using plan-do-study-act and Lean methodologies to achieve this. Detection tools include the General Movements Assessment (GM), Hammersmith Infant Neurologic Examination (HINE), and a standardized assessment of motor function, performed at specific time points. For inclusion, HRIF is being defined as; preterm <32 weeks gestation or birth weight <1500 gm, neonatal encephalopathy or significant neurological risk factors (based on neuro-imaging findings or persistently abnormal neurological exam). The primary outcome is age at CP diagnosis. Data were acquired during the 9-month baseline period and is now being collected quarterly throughout the study. Balancing measures will be clinic no-show rates and parent perception of the diagnosis visit. Clinic teams conducted strengths, weaknesses, opportunities, and threats analyses, process flow evaluations, standardized assessments training, and parent questionnaires.
RESULTS: A collaborative network across the four Tertiary NICU HRIF follow-up programs in Ireland was established in 2022. Training in relevant assessments was provided (Number of staff trained: GMs n=19; HINE n=51) and a process for fidelity to procedures and scoring was established. At baseline, the mean age of CP diagnosis across the Network was >2 years of age. Initial enrollment in the standardized assessment pathways was staggered across centres, with the first going-live in May, and the last in September, 2023. Over the first quarter of enrollment across all sites, 134 HR infants have been included, with enrollment on-going.
CONCLUSION: Implementation of international guidelines for early detection of CP is feasible across a national collaborative network of tertiary NICU HRIF follow-up clinics in Ireland. The impact of implementing these guidelines on the age of CP diagnosis in Ireland, and pre-specified balancing measures, is awaited.
BIBLIOGRAPHY:
1. Novak I, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr.2017;171(9):897-907.
HINE trajectories in children with cerebral palsy identified in high-risk follow-up
Vera Joanna Burton1, Sujatha Kannan, Gwendolyn Gerner, Ruth Getachew, Gayane Yenokyan, Andrea Duncan
1Kennedy Kreiger Institute
BACKGROUND: Hammersmith Infant Neurologic Examination (HINE) is a standardized neurologic exam for infants between 2-24 months, made up 26 items with a total score up to 78 and an asymmetry score. Scores can be compared to optimality cutoffs to support early diagnosis. Some prognosis is also possible for infants diagnosed with cerebral palsy. We wanted to understand the longitudinal trajectories of HINE scores in infants diagnosed with cerebral palsy.
METHODOLOGY: Clinical records were reviewed for 62 children diagnosed with cerebral palsy in two high-risk infant follow-up clinics with HINE scores from at least 2 visits between 3 months and 2 years. Trajectories were calculated for premature infants, perinatal stroke (PAIS), congenital malformations and neonatal encephalopathy (NE).
RESULTS: Change in HINE score between clinic visits for 61 children (19 with NE, 6 with PAIS) were compared using linear mixed effect model, pulling the data across visits by diagnostic group and accounting for within-child correlation of scores over the follow-up time. The model estimated a 0.35-point change in the NE and Premature groups, that did not reach statistical significance (p = 0.85). The corresponding change in the perinatal stroke group was 14.7 (95% confidence interval 2.3 to 27.1, p = 0.020). Asymmetry scores remained consistent across visits, with >5 cut off distinguishing the PAIS group from the others as early as 3-4 months.
CONCLUSION: Children with PAIS with resultant hemiplegia continued to increase HINE scores throughout the first two years of life. In contrast, HINE scores remained stable for premature infants with brain injury and children with NE diagnosed with cerebral palsy. Understanding change or lack of change in individual trajectories will be useful in designing clinical trials that target neurologic injury. Trajectory information may also provide information to aid with prognosis or when serial HINE scores are used as part of diagnosis.
BIBLIOGRAPHY:
1. Hay, Krystal, et al. «Hammersmith infant neurological examination asymmetry score distinguishes hemiplegic cerebral palsy from typical development.» Pediatric neurology 87 (2018): 70-74.
2. Novak et al, 2017 Early Accurate Diagnosis and Early Intervention in Cerebral palsy: Advances in Diagnosis and Treatment. JAMA Pediatrics 171.9. (2017): 897-907.
3. Ricci, Daniela, et al. «Sequential neurological examinations in infants with neonatal encephalopathy and low apgar scores: relationship with brain MRI.» Neuropediatrics 37.03 (2006): 148-153.
4. Romeo, Domenico M, et al. «Neuromotor development in infants with cerebral palsy investigated by the Hammersmith Infant Neurological Examination during the first year of age.» European Journal of Paediatric Neurology 12.1 (2008): 24-31.
5. Romeo, Domenico M, et al. «Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: a critical review of the literature.» Developmental Medicine & Child Neurology 58.3 (2016): 240-245.
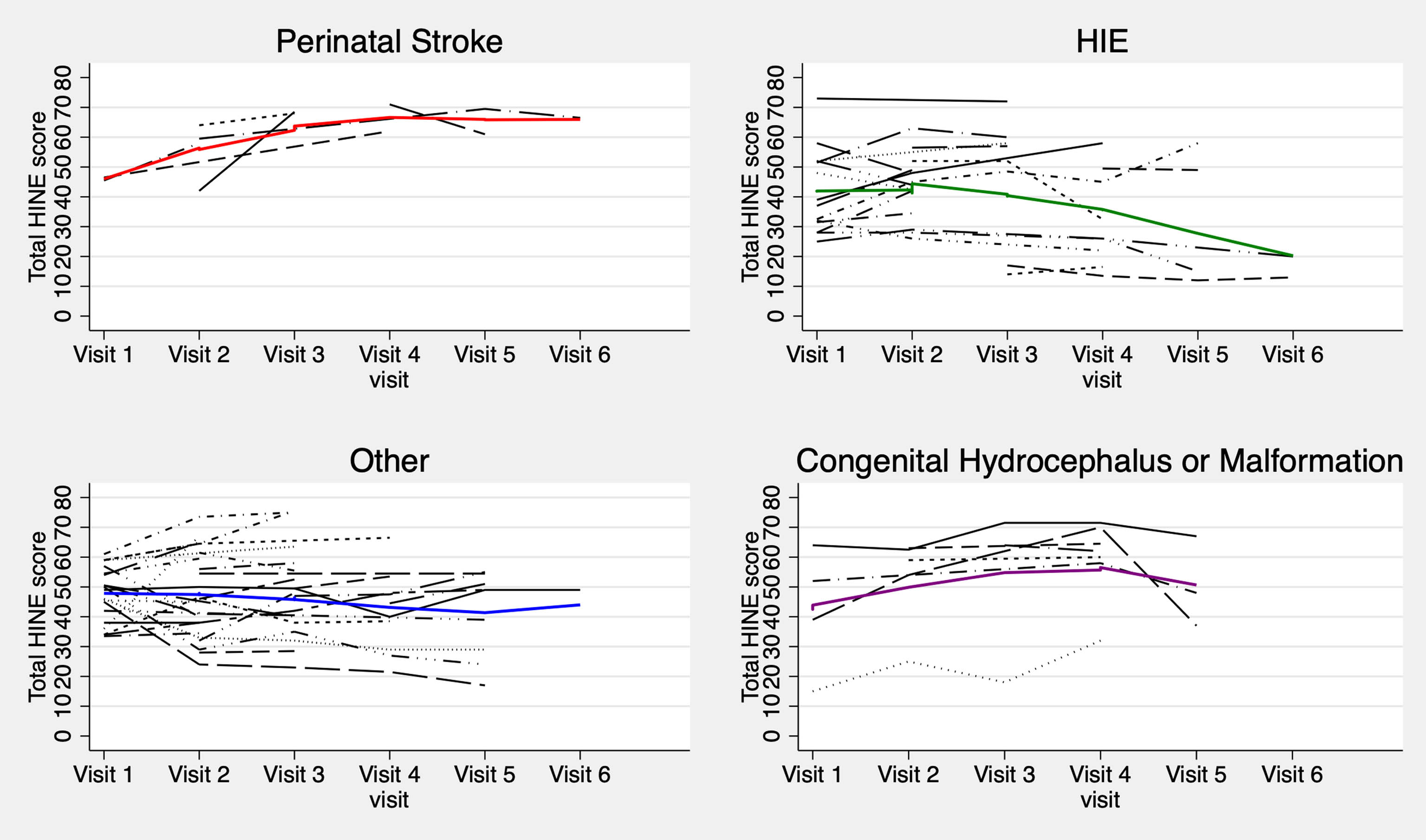
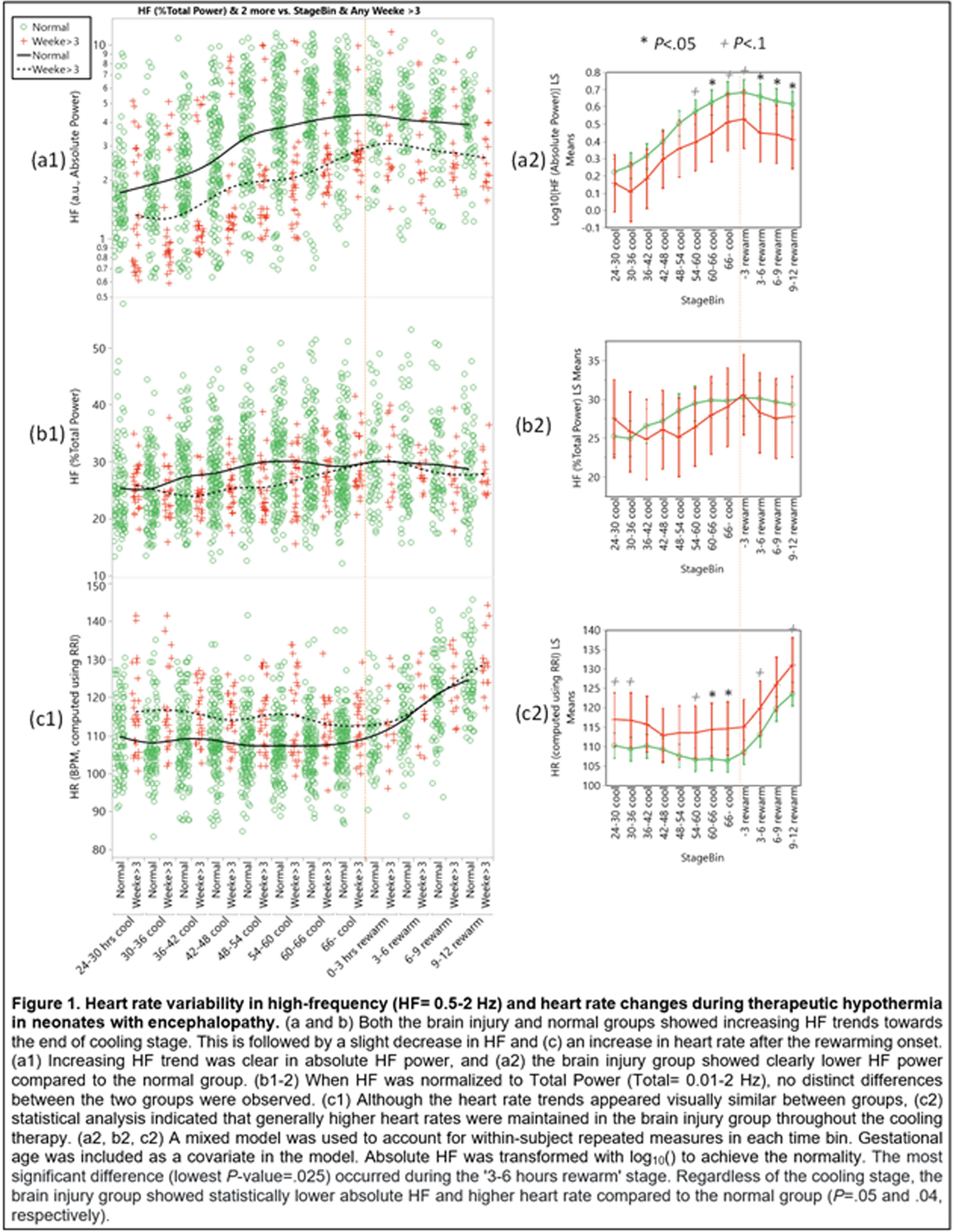
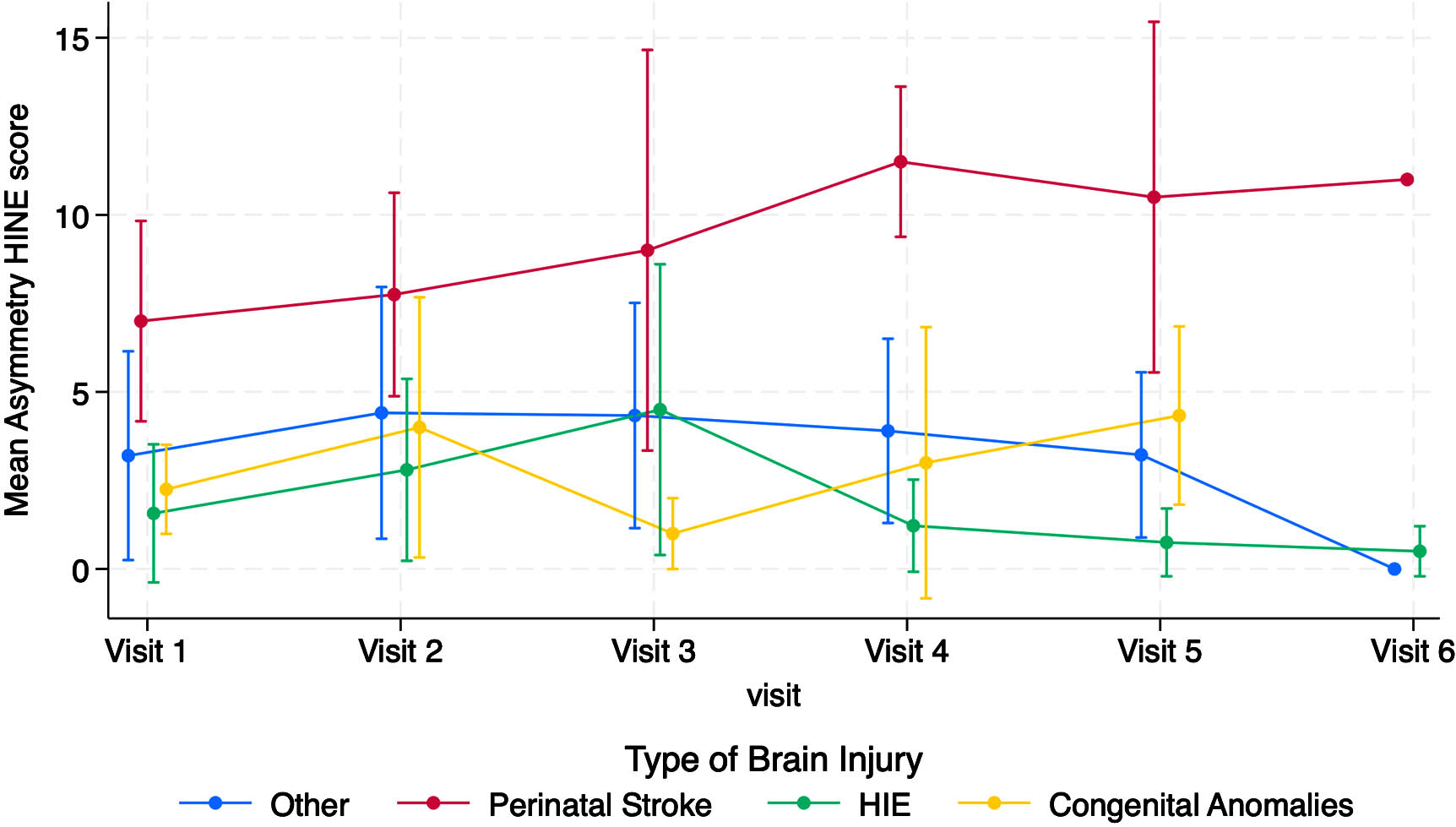
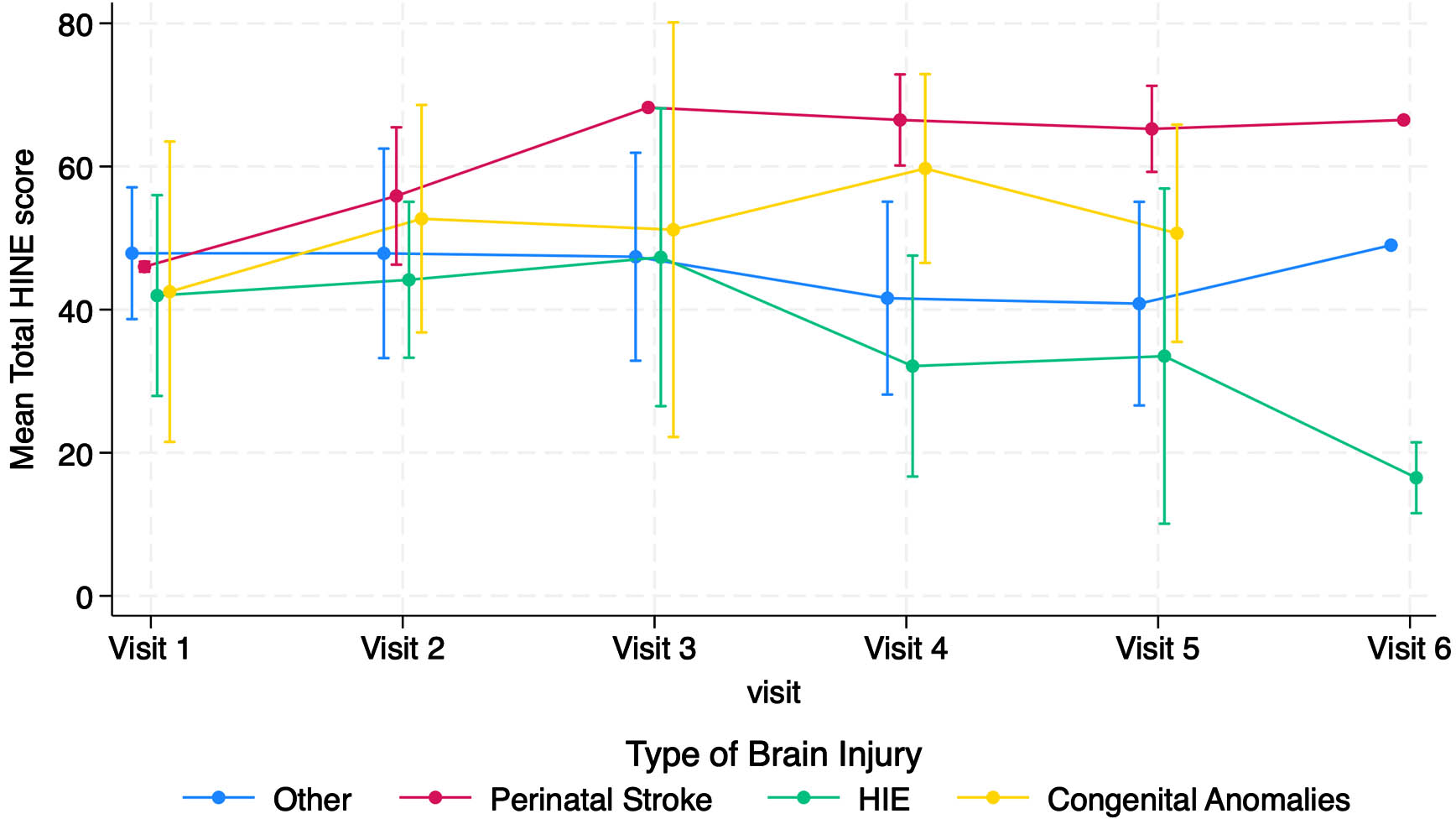
Neurodevelopmental outcomes of neonates with hypoxic-ischemic encephalopathy: The role of neighborhood disadvantage
Srishti Jayakumar1, Jordan Kuiper3, Amii Kress4, Raul Chavez-Valdez1, Kathryn Carson4, Amaris Keiser1, Frances Northington1, Gwendoyln Gerner5, Vera Joanna Burton5
1Division of Neonatal-Perinatal Medicine, Johns Hopkins University School Of Medicine, 2Neurosciences Intensive Care Nursery, 3George Washington University, 4Johns Hopkins Bloomberg School of Public Health, 5Kennedy Krieger Institute
BACKGROUND: Despite the improved neurodevelopmental outcomes in high-risk NICU graduates associated with receipt of services at high-risk infant clinics following NICU discharge, follow-up rates are low for several reasons. Individual and family-level factors have been shown to impact follow-up care of neonates surviving hypoxic-ischemic encephalopathy (HIE). However, there is a lack of literature examining how neighborhood characteristics affect neurodevelopmental outcomes of children with a history of neonatal HIE.
PURPOSE: Our aim was to elucidate the relationship between neighborhood disadvantage and neurodevelopmental outcomes of neonates who survived HIE.
METHODOLOGY: 57 infants with moderate to severe HIE who underwent therapeutic hypothermia (TH) were enrolled between 2010 and 2015. Using electronic medical records, we obtained clinical and sociodemographic characteristics including birth anthropometrics, gestational age, sex, cord pH, base deficit, Apgar scores at 1 and 5 minutes, brain MRI NICHD scores, peak creatinine and alanine transaminase levels. To quantify neighborhood disadvantage, we used the Area Deprivation Index (ADI), a well-validated metric including domains of income, education, employment and housing quality. We used Capute and Mullen scores, and Gross Motor Function Classification System to assess cognitive and motor outcomes respectively at 24 months. Logistic regressions were performed to assess differences in cognitive outcomes and overall neurodevelopment by ADI quartiles adjusted for MRI grade.
RESULTS: Among infants with HIE treated with TH, ADI scores were associated with cognitive outcomes at 24 months and ADI scores. Infants residing in areas with the highest ADI scores (reflecting the greatest neighborhood disadvantage) had significantly greater odds of moderate and severe cognitive disability compared to those with the lowest ADI scores (reflecting the least neighborhood disadvantage), when compared to national and state rankings (OR 29.43, p = 0.013 and OR 16.03, p = 0.043 respectively), after adjusting for MRI NICHD grade. There were significantly higher odds of combined cognitive and motor disability in infants living in areas with higher ADI scores, even after adjusting for severity of MRI grade.
CONCLUSION: For the first time, we show that neighborhood disadvantage has a detrimental impact on neurodevelopmental outcomes of infants surviving HIE. Further research elucidating the role of contributory factors will allow for identification of populations most at risk and aid the development of evidence-based, targeted interventions to improve long-term outcomes.
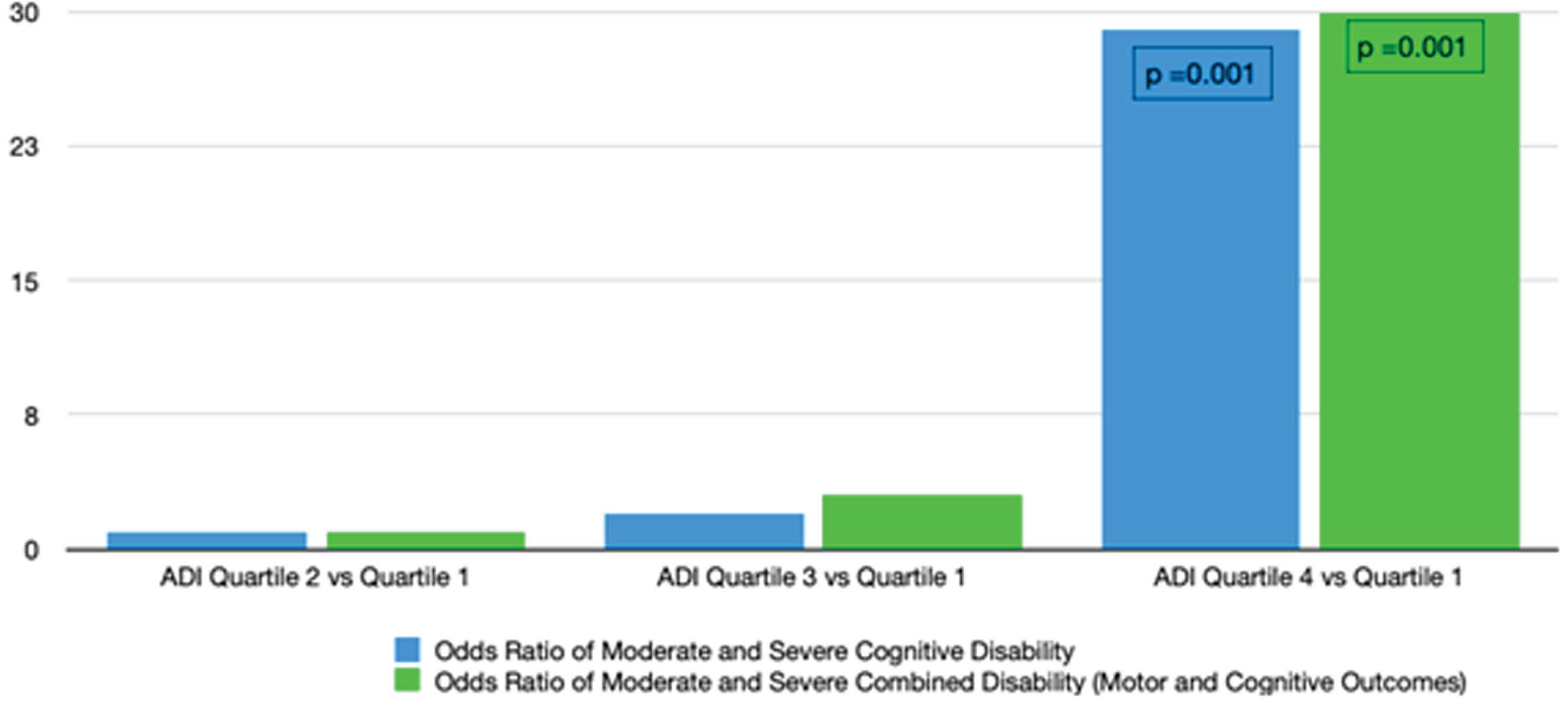
Cognitive outcomes of neonates with hypoxic-ischemic encephalopathy treated with hypothermia: The impact of socioeconomic vulnerability
Srishti Jayakumar1, Jordan Kuiper2, Amii Kress3, Raul Chavez-Valdez1,4, Corina Mills4, Kathyrn Carson3, Amaris Keiser1, Frances Northington1,4, Gwendolyn Gerner4,5, Vera Joanna Burton4,6
1Johns Hopkins School Of Medicine, 2George Washington University, 3Johns Hopkins Bloomberg School of Public Health, 4Neurosciences Intensive Care Nursery, 5Department of Neuropsychology, Kennedy Krieger Institute , 6Neurology and Neurodevelopmental Medicine, Kennedy Krieger Institute
BACKGROUND: The role of maternal and neonatal factors in neurodevelopmental outcomes of infants surviving hypoxic-ischemic encephalopathy (HIE) treated with therapeutic hypothermia (TH) is established. However, there is limited literature examining how sociodemographic factors affect neurodevelopmental outcomes in these neonates.
PURPOSE: Our aim was to elucidate the relationship between county-level socioeconomic vulnerability and cognitive outcomes of neonates surviving HIE.
METHODOLOGY: 43 infants with moderate to severe HIE who underwent TH were enrolled between 2010 and 2015. Using electronic medical records, we obtained clinical and sociodemographic characteristics including birth anthropometrics, gestational age, sex, cord pH, base deficit, Apgar scores at 1 and 5 minutes, brain MRI NICHD scores, peak creatinine and alanine transaminase levels in the first 24 hours. We used the CDC Social Vulnerability Index (SVI), a well-validated metric comprising four themes based on 16 US Census indicators to assess vulnerability for the infant’s county of residence. We used Mullen scores comprising four subscales to assess cognitive and motor outcomes at 24 months. Regression analyses were performed to assess differences in outcomes in Mullen subscales by SVI quartiles adjusted for MRI NICHD scores.
RESULTS: Among infants with HIE treated with TH, we observed significant MRI NICHD score-adjusted associations for county-level exposures including socioeconomic status (p = 0.04), household characteristics (p = 0.01), and housing type and transportation (p=0.01) with Mullen Visual Reception scores at 24 months (Figure 1). Similarly, we observed significant adjusted associations for socioeconomic status (p = 0.005), household characteristics (p = 0.007), and housing type and transportation (p=0.01) with Expressive Language scores at 24 months. While this association persisted between Fine Motor scores and each SVI theme, Receptive Language scores were preserved. Within each theme and across all components of the Mullen, infants from areas with higher SVI had significantly lower Mullen scores than infants from areas with less disadvantage.
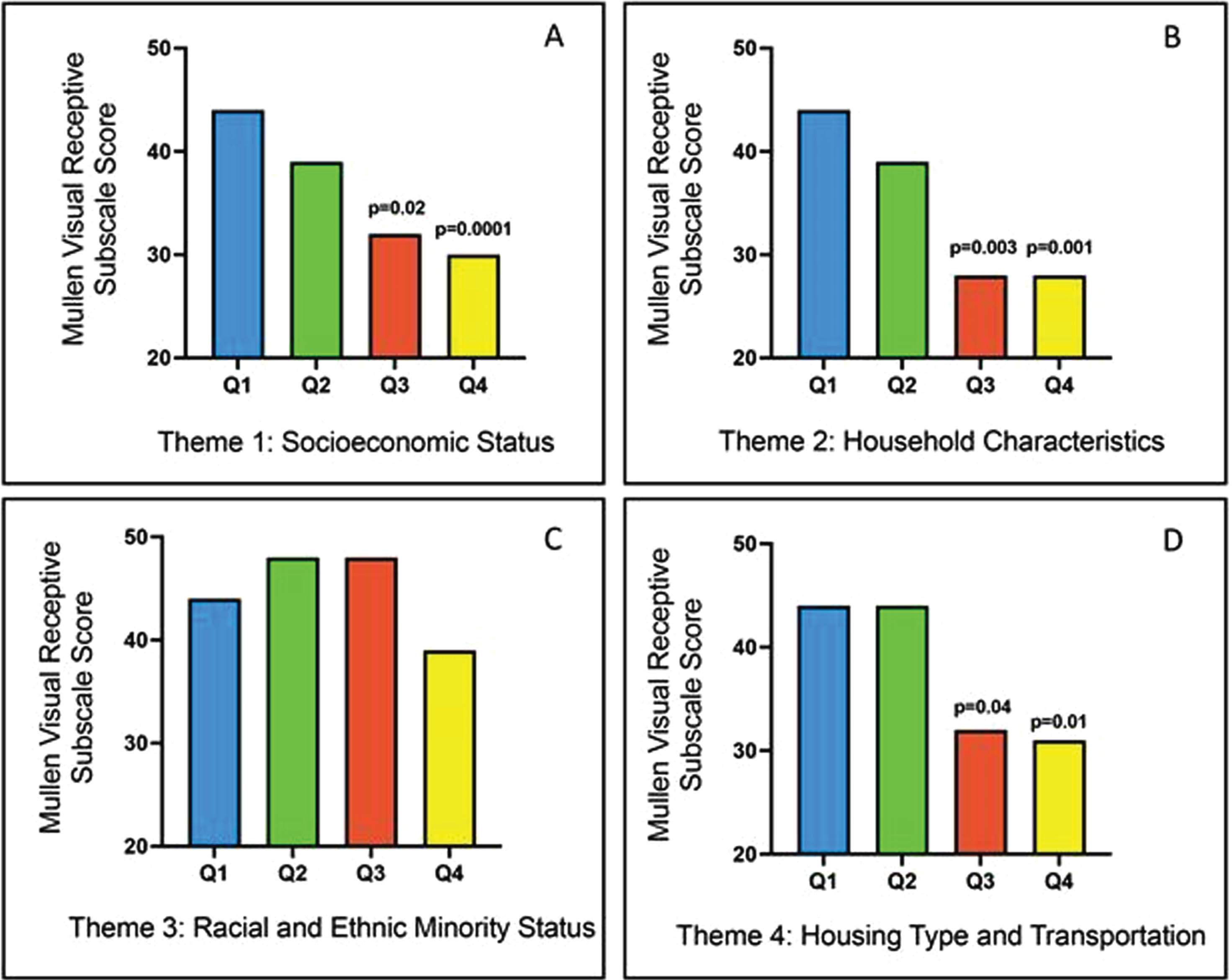
CONCLUSION: All themes of county-level social vulnerability have a detrimental impact on all components of neurodevelopmental outcomes of children with a history of neonatal HIE. Further research elucidating the specific contributions of these individual components will allow for identification of populations most at risk. This will aid the development of evidence-based, targeted interventions to improve outcomes and the realization of each child’s full potential.
Difficult conversations in fetal neonatal neurology: National survey of educational experiences of child neurology residents
Monica Lemmon, Doctor Ashley Bach1, Dawn Gano2, Charu Venkatesan3, Sonika Agarwal1
1Division of Neurology, Children’s Hospital of Philadelphia, 2Departments of Neurology and Pediatrics, University of California San Francisco, 3Division of Neurology, Cincinnati Children’s Hospital
BACKGROUND AND OBJECTIVE: Fetal and neonatal neurology (FNN) is a growing subspecialty within child neurology, to which residents have varying exposure. FNN often involves difficult conversations regarding uncertain or poor prognosis. Resident exposure to FNN and educational needs around these difficult conversations are not well characterized. We aimed to assess the exposure of child neurology residents to FNN and to characterize educational needs around communicating with families during difficult conversations.
METHODOLOGY: This is a descriptive, survey-based study of the educational experiences of child neurology residents in the neurology portion of their training. An anonymous RedCap survey was distributed by email to program directors of all child neurology programs in the United States, to be distributed to residents for optional, voluntary completion. All respondents completed the survey between March and August 2023.
RESULTS: Fifty child neurology residents in training programs from 12 states completed the survey. Half spent 1-4 weeks, and 42% spent >4 weeks, this academic year on an inpatient service that consulted on a range of NICU patients (1 to 21+) per week. Half had participated in one or more fetal neurology consultations in the preceding 6 months. Most residents were interested in increasing clinical exposure to neonatal neurology (78%) and fetal neurology (88%). Many residents had been part of a difficult conversation in the NICU or fetal neurology clinic (84%), with two-thirds having led at least one of these conversations in the preceding 6 months. Many reported a negative experience during the disclosure of serious news or discussion of prognosis with a family (60%), and greater comfort with delivering diagnoses and prognoses in neonatal neurology than in fetal neurology. Most residents had prior training in communication skills (94%), most commonly during medical school and pediatric residency. Fewer had communication training specific to FNN (30%), but nearly all were interested in improving their ability to conduct difficult conversations about goals of care and prognosis in FNN (94%).
CONCLUSION: Child neurology residents have variable exposure to FNN and are often an integral part of difficult conversations with families. A minority had communication training specific to FNN and nearly all were interested in increasing clinical exposure and improving their ability to conduct difficult conversations in FNN, highlighting an educational need in FNN curriculum development.
Improving seizure safety advice for families of infants with hypoxic-ischaemic encephalopathy: A quality improvement project
Danielle Clifford1, Anne O’Sullivan1, Orla Smyth1, Martin J. White1,2,3
1The Coombe Hospital, 2Children’s Health Ireland at Crumlin, 3Royal College of Surgeons Ireland
BACKGROUND AND PURPOSE: Hypoxic Ischaemic Encephalopathy affects 1-2 per 1,000 live full-term births in Ireland. Many of these infants are treated for seizures during their stay in the NICU (36% in 2020) and approximately 10-30% will go on to have seizures long-term (1). Despite this, there is currently no formalised seizure safety information given to parents prior to discharge from our unit.
METHODOLOGY: A chart review was performed of infants who were diagnosed with grade 2-3 encephalopathy over the past three years, to ascertain whether seizure safety advice was given prior to discharge. As a result of this review, formal seizure safety advice has been developed for parents of infants with HIE prior to discharge home.
RESULTS: Of the 32 infants identified as HIE since 2021, 14 charts were available for review and initial analysis. Of these, 13 were born in our centre and 1 baby was transferred to our unit for therapeutic hypothermia. All 14 infants had a modified Sarnat grade 2 and received therapeutic hypothermia. 9 had clinical seizures, 8 had electrographic seizures and 9 were treated with an anti-epileptic medication during their inpatient stay. While 5 were discussed with or referred to neurology, only 3 were discharged on anti-epileptic medications. Seizure safety advice was documented as discussed with 3 families and a further family who had concerns regarding abnormal movements at the 6-week follow-up also had a discussion regarding seizure safety at that point. One infant passed away during their inpatient stay. The majority of these infants, therefore, did not receive any advice regarding seizure safety prior to discharge home. Of those infants who did not have charts available for review, 16 discharge letters were reviewed. All received therapeutic hypothermia. 9 had clinical seizures, 6 had electrographic seizures. 7 were treated with an anti-epileptic drug during their inpatient stay and 2 were documented to have been discussed with or referred to neurology. None of these patients were documented as being discharged on anti-epileptic drugs, nor were any documented to have had seizure safety discussions. Analysis is ongoing and remaining charts will be reviewed.
CONCLUSION: As a result of this ongoing review, seizure safety advice for families is being formalised and will be integrated to the discharge first aid classes which are provided for families leaving the NICU. A copy of the information leaflet is attached, Figure 1.
BIBLIOGRAPHY:
1. San Lazaro Campillo I MJ, Corcoran P, Meaney S,, McKenna P FP, Greene RA, Murphy J on behalf of, Group. NTHS. Neonatal Therapeutic Hypothermia in Ireland, Annual Report 2016-2020.; 2020.
Sensory processing in infancy at population-level: who is most at-risk?
Emma Butler1, Linda O Keeffe2, Michelle Spirtos3, Mary Clarke1
1RCSI, 2UCC, 3TCD
BACKGROUND: Sensory Processing (SP) refers to how the nervous system receives, modulates, integrates and organises sensory stimuli including behavioural responses to sensory input (Miller & Lane, 2000) and is indispensable for a wide variety of activities that humans engage in, including regulation, perception, motor performance, learning and behaviour. (Yoshimura et al., 2017). There are known elevated rates of SP difficulties in neurodevelopmental disorders such as ADHD, ASD & DCD (Pfeiffer et al., 2015; Little et al., 2017; Mikami et al., 2021) but analysis of population samples show that children with typical development (Little et al., 2017) also display sensory difficulties. Very little research focuses on SP in infants despite it being a key factor in regulatory disorders. Additionally, there is a dearth of research investigating the antecedents to SP difficulties, possibly because most longitudinal population-based cohort studies do not include a standardised measure of SP and as a result it is an over-looked area of research in child development.
METHODOLOGY: This study used secondary analysis of 14,166 babies recruited at birth in the ELFE cohort who were followed prospectively and had sensory information available at 1-year. Public and patient involvement was used to agree 10 characteristics indicative of sensory difficulties. Latent Class Analysis was conducted to identify latent sensory classes. Multinomial logistic regression identified prognostic factors of these latent sensory classes.
RESULTS: 3 sensory classes, a ‘typical’ group, a ‘possible’ difficulty group (only different from ‘typical’ in relation to adaptability and sleep problems) and a ‘definite’ difficulty group characterised by more difficult to calm, disliking confined spaces, less adaptable, more anxious, unable to keep still, slight concerns around food and sleep problems were identified. Infants experiencing low, moderate and high social risk were RRR 1.5 (CI 1.3-1.9), 2.3 (CI 1.9 – 2.7) and 3.5 (CI 2.6-4.8) times more likely to be categorised as ‘definite’ sensory problems compared to infants with no social risk. No one perinatal factor increased the risk of being ‘definite’ compared to ‘typical’ but the total number of pregnancy exposures experienced were associated with increased relative risk of ‘definite’ compared to ‘typical’ in a dose-response fashion. (RRR 1.5 for 1 exposure (CI 1.2-1.9), 1.9 for 2 (CI 1.5-2.5), 2.1 for 3 (CI 1.6-2.9), 2.4 for 4 (CI 1.6-3.6) and 3.0 for 5+ (CI 1.7-5.3) pregnancy exposures).
CONCLUSION: 21.3% of infants displayed behaviours indicative of sensory difficulties. Whilst cumulative social risk differentiated between the typically developing group and atypical groups, cumulative pregnancy exposures differentiated between those with ‘definite’ sensory difficulties and ‘possible’ difficulties. Males and females equally experienced sensory problems in infancy. Given this prevalence rate, longitudinal cohort studies should strongly consider including standardised sensory measures to allow future research to examine antecedents and potential prognostic ability of sensory difficulties in infancy.
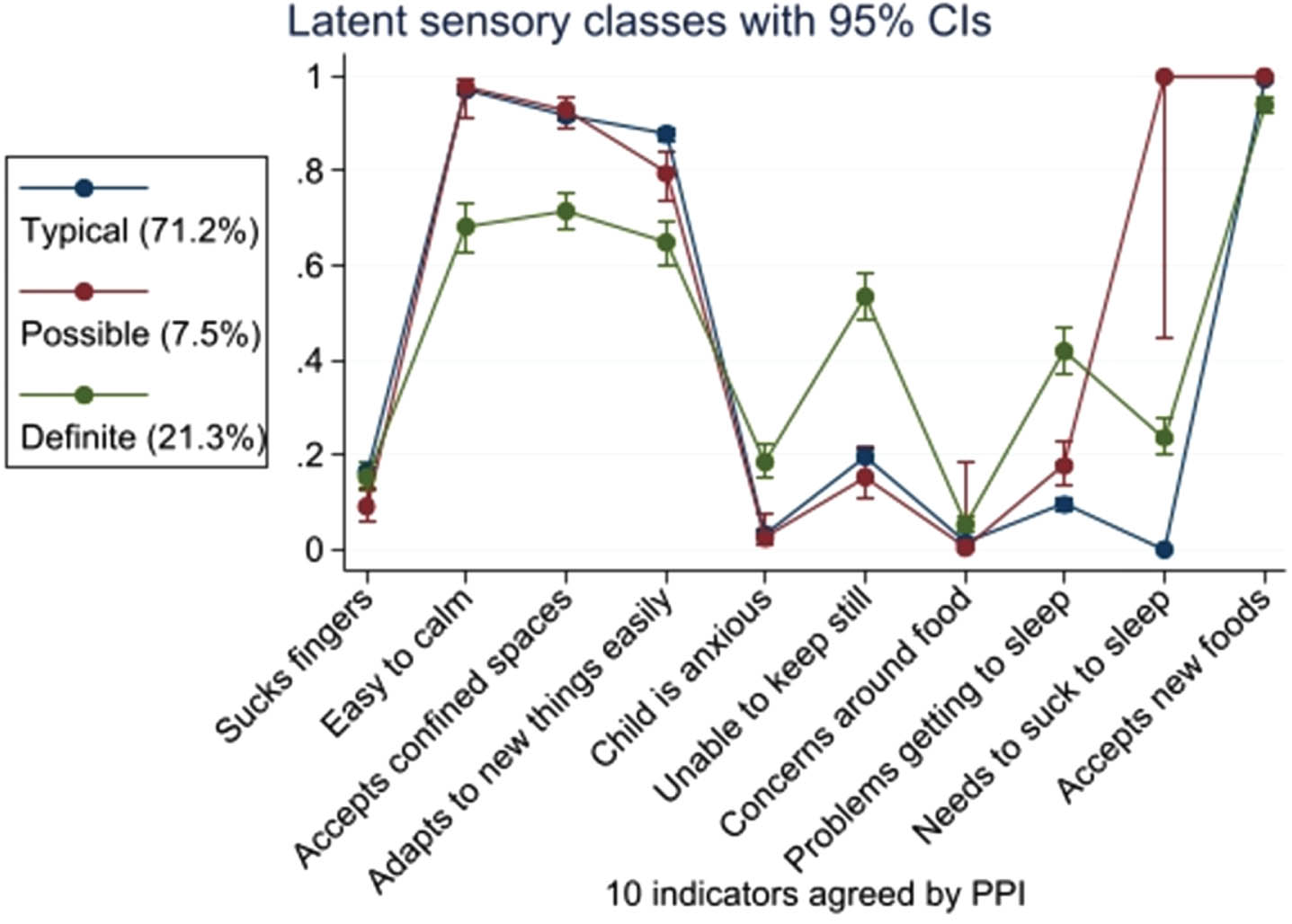
Auditory experiences of very preterm infants in relation to NICU room type and parental presence
Gabriel Côté-Corriveau1,2, Danielle Sharon1, Elizabeth Singh1, Yvonne Sheldon1, Deborah Cuddyer1, Terrie Inder1,3,4, Carmina Erdei1,3
1Division of Newborn Medicine, Department of Pediatrics, Brigham and Women’s Hospital, 2Sainte-Justine University Hospital, University of Montreal, 3Harvard Medical School, 4Division of Neonatology, Children’s Hospital of Orange County and University of California, Irvine
BACKGROUND: Infants born very preterm (VP) display rapid brain development including the auditory cortex before term equivalent age (TEA). This critical period occurs in the neonatal intensive care unit (NICU), where meaningful auditory experiences can enhance brain development, while prolonged adverse exposure to noises and/or excessive silence may be detrimental.(1) We examined the trajectories of auditory exposures of VP infants before TEA, and assessed implications of room type and parental presence.
METHODOLOGY: We conducted a prospective study of infants born < 33 weeks’ gestational age in a hybrid design level-III NICU, where VP infants typically transition from single-family room (SFR) to semi-open bay (SOB) when they achieve medical stability. We used the Language Environment Acquisition (LENA) device to collect weekly auditory recordings of 16 hours for of up to 6 consecutive weeks for each infant. Room type (SFR vs SOB) and parental presence (6 hours or more vs less than 6) were documented at each measurement. We assessed the evolution of auditory exposures with advancing postmenstrual age (PMA) using repeated measure correlations.
RESULTS: We obtained 128 recordings among 25 VP infants. 73 measurements (57%) were performed in a SFR and 44 (34%) while parents were present 6 hours or more. The NICU auditory environment was predominantly composed of silence (53.2±27.4%), electronic sounds (19.0±18.9%), and noise (15.6±19.4%), while distant language (6.4±7.4%) and meaningful language (4.3±3.5%) represented the minority exposure. With advancing PMA, there was an increase in meaningful language (r = 0.54, p = 0.001) and a decrease in noise (r = -0.59, p<0.001) exposures (Figure 1). These trajectories continued as infants transitioned from SFR to SOB (Figure 2). The degree of exposure to meaningful language and adult word count appeared greater with high parental presence, especially before 37 weeks’ PMA (Figure 3).
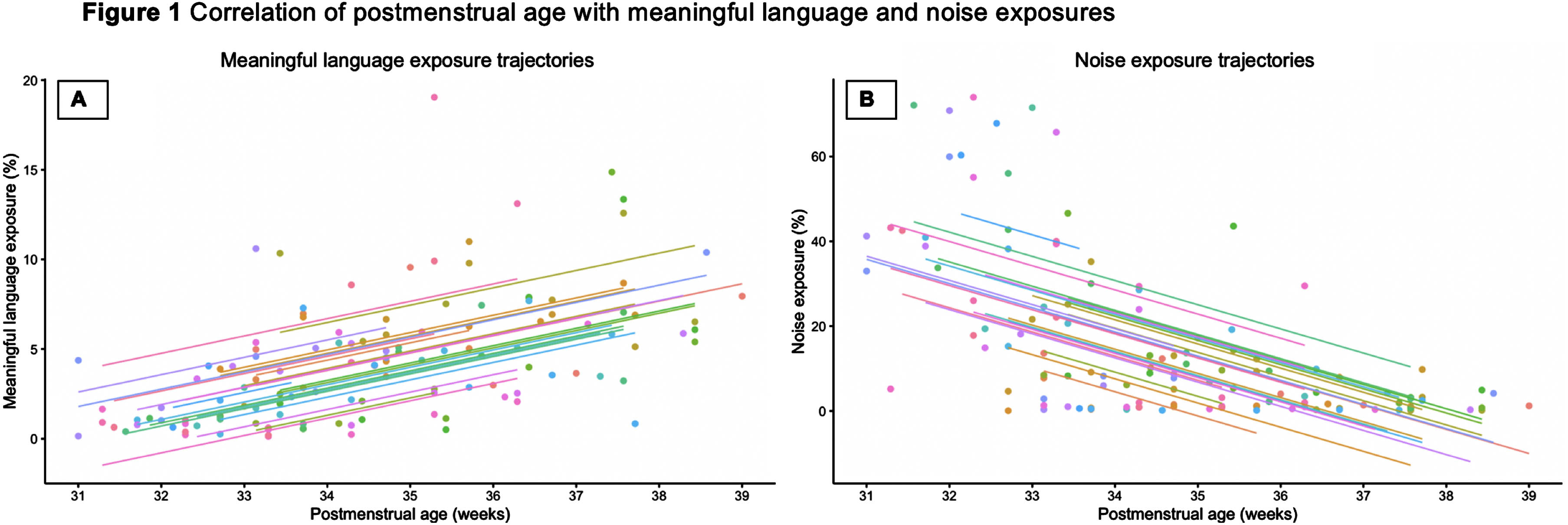
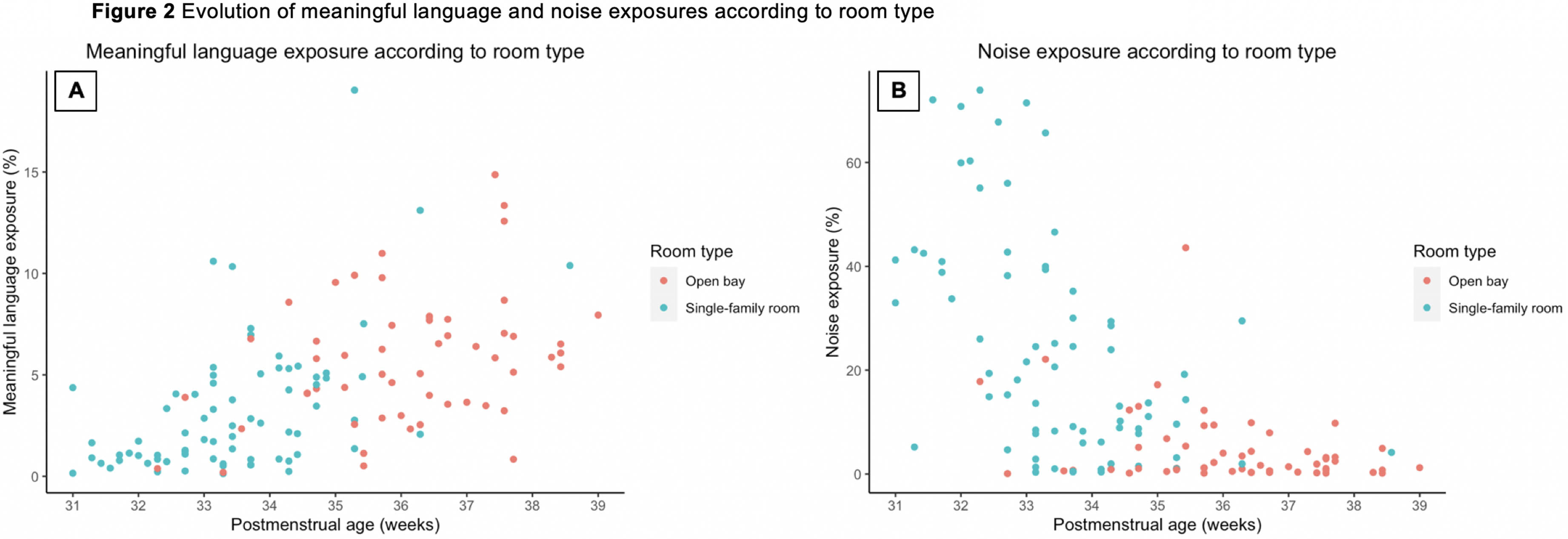
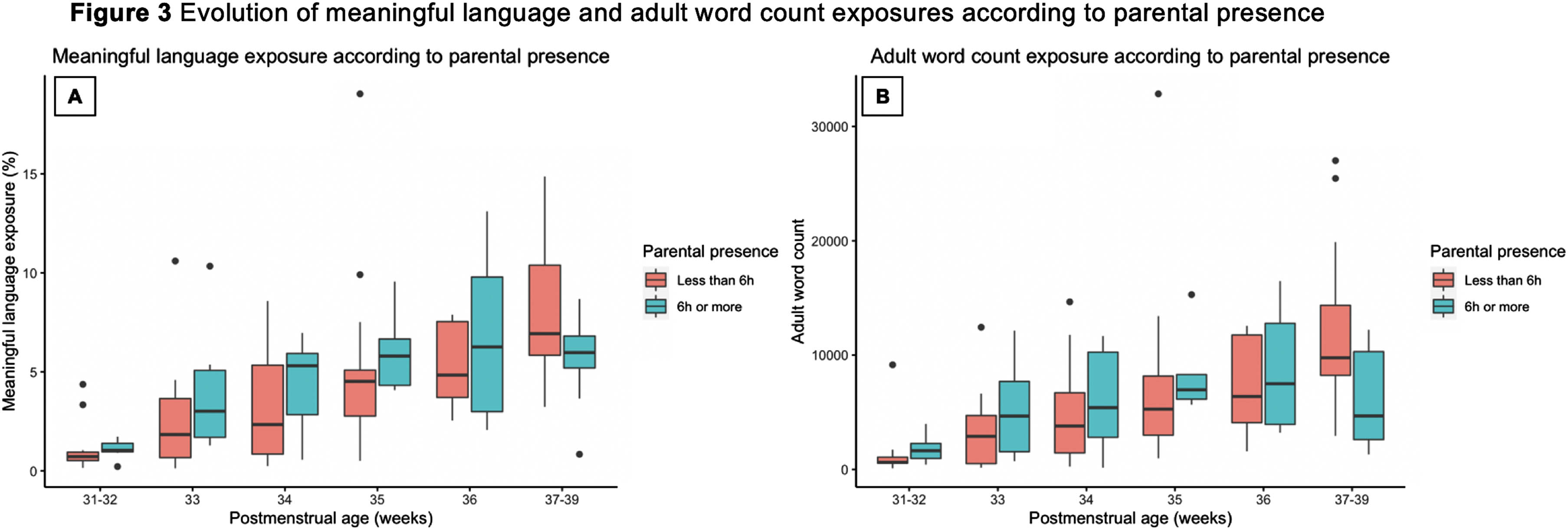
CONCLUSION: VP infants experienced primarily silence and undesirable exposures while in the NICU before TEA, with limited exposure to meaningful language. The increase in meaningful language and decrease in noise exposures with advancing PMA continued as infants transitioned to SOB. Higher parental presence appeared to coincide with more meaningful language and adult word count exposures in the earliest PMAs. Modifiable NICU environmental factors including architectural design and parental presence may play a role to optimize auditory experiences of VP infants before TEA.
BIBLIOGRAPHY:
1. Maitre NL, Key AP, Chorna OD, et al. The Dual Nature of Early-Life Experience on Somatosensory Processing in the Human Infant Brain. Curr Biol. 2017;27(7):1048-1054. doi:10.1016/j.cub.2017.02.036
Read in the NICU: a pilot study on the application of the new Italian guidelines
Lorenzo Riboldi1, Chiara Peila1, Patrizia Strola1, Doctor Francesco Raimondi1, Alessandra Coscia1
1Neonatal Unit, Department of Public Health and Pediatrics, University of Turin
BACKGROUND: Recent evidence demonstrates the benefit of parental reading as an Infant and Family-Centered Individualized Developmental Care (DC) practice in neuroprotection and development support of preterm infants admitted to Neonatal Intensive Care Units (NICUs). In 2021, the Italian multicentre project “La cura della lettura” elaborated the guidelines to promote this practice of DC among the parents of premature newborns hospitalized in NICUs through the involvement of the entire nursing staff. The objective of the pilot study is to qualitatively describe, according to the Brazelton neonatal behavioral assessment, the signs of stability and/or stress of the preterm infants before, during and after the intervention of the parents’ reading, according to the indications provided by guidelines. Furthermore, we want to investigate whether there are significant changes in the main neonatal physiological parameters before, during, and after the reading proposal. Finally, the study intends to evaluate the parental reception of this DC practice in nursing practice.
METHODOLOGY: A single-center, analytical-descriptive cohort study was conducted on 12 clinically stable LBW premature infants with a minimum of 1 week of life admitted to NICU. Both parents were asked to read daily during the hospital stay. During one of the shared reading sessions, a 45 ‘ behavioral observation was carried out (15’ before, 15 ‘during, 15’ after the intervention); for each 15’ interval the observed neonatal stability and/or stress signals were reported, according to the concepts of the Brazelton’s APIB and NIDCAP methods, and HR, RR, SpO2 were detected.
RESULTS: The proposal was positively received by the parents and there were no differences in neonatal behavioral signs between maternal/paternal readings. During and after the intervention, there were no significant episodes of destabilization. Compared to the 15’ pre-reading, the gradual reduction of movements and the transition, more or less rapid, towards a state of sleep was frequently observed. In some premature newborns, signs of visual and auditory orientation and attention towards the reader have been reported. During the reading, there was an increase in the signs of self-regulation of the motor system, and in particular in suckling attempts. A general reduction in stress signals when compared with the pre-reading observation was also reported. Regarding the values of physiological parameters, no significant differences were found (p < 0.05), although trends are observable, in particular in the SpO2 (whose average values are higher during reading).
CONCLUSION: The observations confirm that parental reading in NICU is a safe practice of DC, associated with sleep neuroprotection, greater autonomic stability, a reduction in signs of stress and an increase in behavioral signs of neonatal stability and self- regulation. Further studies with major cohorts and evaluating neurodevelopmental follow-up at 12-24-36 months are indicated.
Parent-important outcomes in the treatment of neonatal encephalopathy
Fiona Quirke1,2,3, Shabina Ariff4, Malcolm R Battin5, Caitlin Bernard6, Frank H. Bloomfield7, Mandy Daly8, Declan Devane1,2,9,10, David M. Haas6, Patricia Healy9, Tim Hurley1,11, Vincent Kibet12, Jamie J Kirkham13, Sarah Koskei14, Shireen Meher15, Eleanor J. Molloy1,11, Maira Niaz16, Elaine Ní Bhraonáin17, Christabell Okaronon12, Farhana Tabassum18, Karen Walker19,20,21,22, Linda Biesty23
1Health Research Board Neonatal Encephalopathy PhD Training Network (NEPTuNE), 2Health Research Board – Trials Methodology Research Network (HRB-TMRN), University of Galway, 3School of Medicine, University of Limerick, 4Department of Paediatrics & Child Health, Aga Khan University, 5Auckland District Health Board, 6Department of Obstetrics and Gynecology, Indiana University, 7Liggins Institute, University of Auckland, 8Advocacy and Policymaking, Irish Neonatal Health Alliance, 9Evidence Synthesis Ireland, University of Galway, 10Cochrane Ireland, University of Galway, 11Department of Paediatric and Child Health, Trinity College Dublin, 12AMPATH, 13Centre for Biostatistics, The University of Manchester, Manchester Academic Health Science Centre, 14Moi University, 15Institute of Life Course and Medical Sciences, University of Liverpool, 16Department of Paediatrics & Child Health, Aga Khan University, 17Family Support Liaison, Irish Neonatal Health Alliance, 18Aga Khan University, 19Department of Newborn Care, Royal Prince Alfred Hospital, 20Faculty of Medicine and Health, University of Sydney, 21The George Institute for Global Health, 22Council of International Neonatal Nurses, 23Qualitative Research in Trials Centre (QUESTS), University of Galway
BACKGROUND: Overall, the COHESION Study aimed to develop a Core Outcome Set (COS) for interventions for the treatment of neonatal encephalopathy. The first steps in this study were to identify important outcomes that had been reported in trials and that were considered important to parents and caregivers of infants diagnosed with neonatal encephalopathy, hypoxic ischemic encephalopathy, or birth asphyxia. This abstract highlights the findings from our qualitative interviews with parents and caregivers from high-income and low- to middle-income countries.
METHODOLOGY: We conducted interviews twenty-five interviews in both high-income (n=11) and low- to middle-income countries (n=16) with parents of infants diagnosed with neonatal encephalopathy, birth asphyxia, or hypoxic ischemic encephalopathy. Interviews were conducted via zoom in high-income countries and either face-to-face or by telephone in low- to middle-income countries. All interviews were transcribed and, using a thematic analysis approach, we identified discrete outcomes and outcome domains that were considered important to this group of parents.
RESULTS: Parents identified 54 outcomes overall, which mapped to 16 outcome domains. The domains identified were neurological outcomes, respiratory outcomes, gastrointestinal outcomes, cardiovascular outcomes, motor development, development (psychosocial), development (special senses), cognitive development, development (speech and social), other organ outcomes, survival/ living outcomes, long-term disability, hospitalisation, parent-reported outcomes and adverse events.
CONCLUSION: This study provides insight into the outcomes that parents of infants diagnosed with neonatal encephalopathy have identified as most important to be considered in the process of developing a COS for the treatment of neonatal encephalopathy. Although many of the outcomes identified were clinical outcomes, which crossed over with our findings from the literature, parents highlighted unique outcomes that would not have been included had the interviews not been conducted. Interviews conducted within the COS development, allow additional outcomes to be identified that are important to parents in the care of their infant.
BIBLIOGRAPHY:
Quirke F, Ariff S, Battin M, et alCore outcomes in neonatal encephalopathy: a qualitative study with parents. BMJ Paediatrics Open 2022;6:e001550. doi: 10.1136/bmjpo-2022-001550




