Proceedings of the 15th International Newborn Brain Conference: Neuroprotection strategies in the neonate
Endogenous haptoglobin and hemoglobin levels in preterm infants and preterm rabbit pups with intraventricular hemorrhage
Amanda Kristiansson1,2, Katarzyna Wiatrowska2, Helena Karlsson1,2, Suvi Vallius1, Niklas Ortenlöf1, Claes Ekström1,2, Valérie Verdon3,4, Sandra Mena Perez3,4, Kirsten Guse3,4, Thomas Gentinetta3,4, Markus Brechmann5, David Ley1,2, Magnus Gram1,2
1Pediatrics, Department of Clinical Sciences Lund, 2Department of Neonatology, Skåne University Hospital, 3CSL Behring, CSL Biologics Research Center, 4Swiss Institute for Translational and Entrepreneurial Medicine, sitem-insel, 5CSL Behring Innovation GmbH
BACKGROUND: Cerebral intraventricular hemorrhage (IVH) is a major cause of neurodevelopmental impairment in preterm infants. IVH is characterized by vessel rupture and a rapid accumulation of blood within the ventricles. Subsequent hemolysis leads to the release of extracellular hemoglobin (Hb) into the cerebrospinal fluid (CSF). Hb and its metabolites initiate cytotoxic, oxidative, pro-inflammatory, and apoptotic pathways resulting in tissue damage. Scavenging of Hb, using haptoglobin (Hp), may therefore constitute a potential treatment in IVH. The aim of this study was to investigate i.) the scavenging capacity in the CSF of infants with IVH, and ii.) the clinical translatability of the preterm rabbit pup model of IVH.
METHODS: Prospective observational study at a level III NICU, Skåne University Hospital, Lund, Sweden. 16 extremely preterm infants with a mean (SD) gestational age at birth of 27.2 (2.7) weeks and birthweight 1042 (369) g. All infants developed either IVH grade III (N=11) or periventricular hemorrhagic infarction (N=5). All infants received a neurosurgically inserted intraventricular reservoir enabling longitudinal CSF withdrawal.
Rabbit pups were delivered prematurely by cesarean section at embryonal day 29 (Term = 31–32 days of gestation). IVH was induced by intraperitoneal injection of glycerol and confirmed by high-frequency ultrasound at 24 hours of age. Plasma and CSF were collected at sacrifice from pups (24–96 hours). Concentrations of cell-free Hb/total heme and Hp were determined in CSF (human and rabbit) and plasma (rabbit) samples.
RESULTS: Intraventricular CSF concentration of cell-free Hb (human) decreased during a 3-week period from a median (range) of 461 (1.5–511.3) μmol/L at time-point of insertion of reservoir to 0.4 (0.1–12.0) μmol/L (Figure 1). Concentrations of CSF Hp (human) were extremely low and did not vary over time. Comparing Hp (rabbit) levels between IVH and non-IVH, pups with IVH displayed significantly higher Hp levels in plasma, but lower in CSF (Figure 2). The total heme (rabbit) levels, assumed to correspond predominantly to Hb, in plasma (37.50 vs 20.77 μmol/L, p=0.006) and CSF were increased in pups with IVH, although not significantly in the CSF (40.75 vs 7.32 μmol/L, p=0.057) (Figure 3).
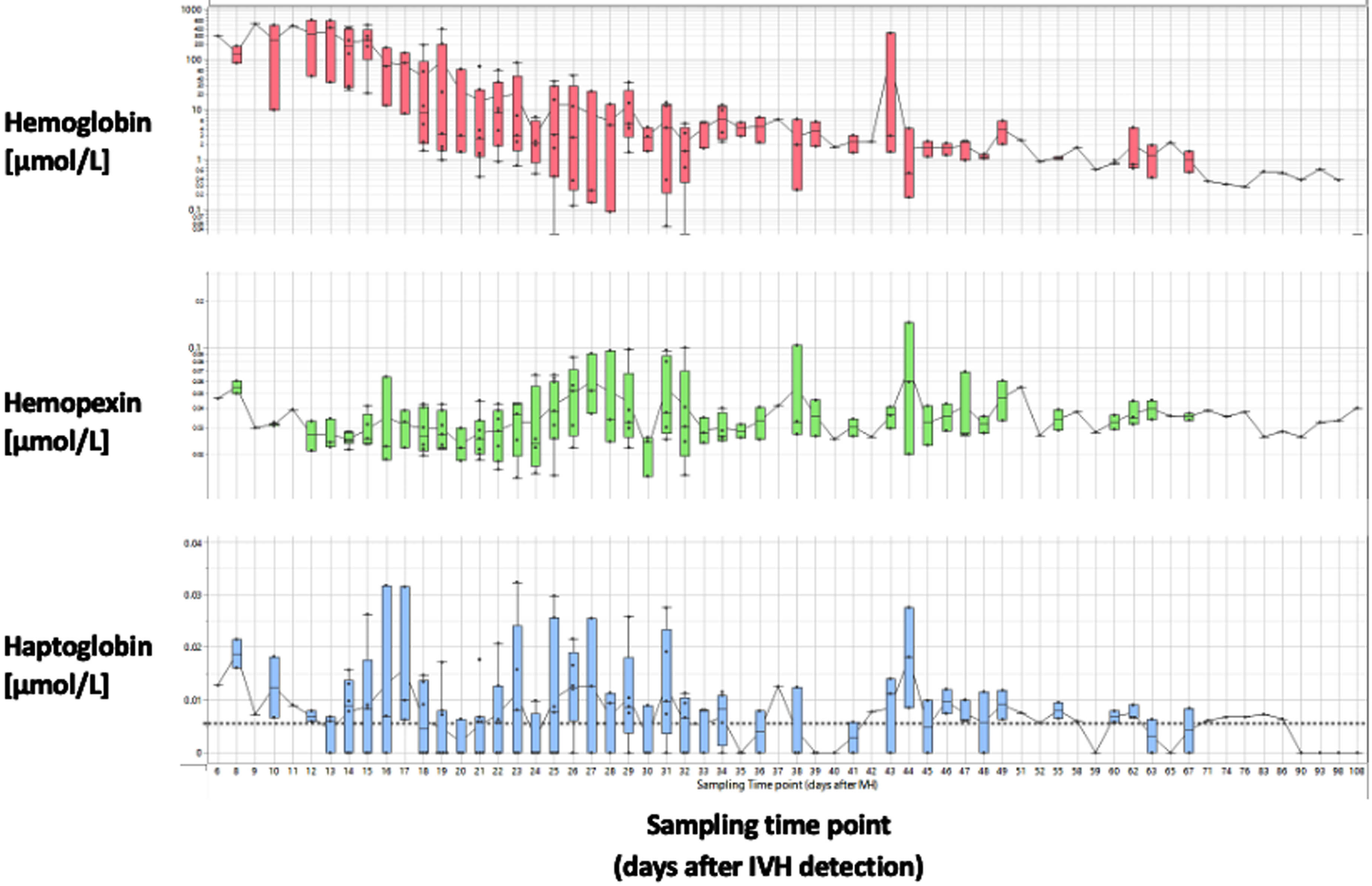
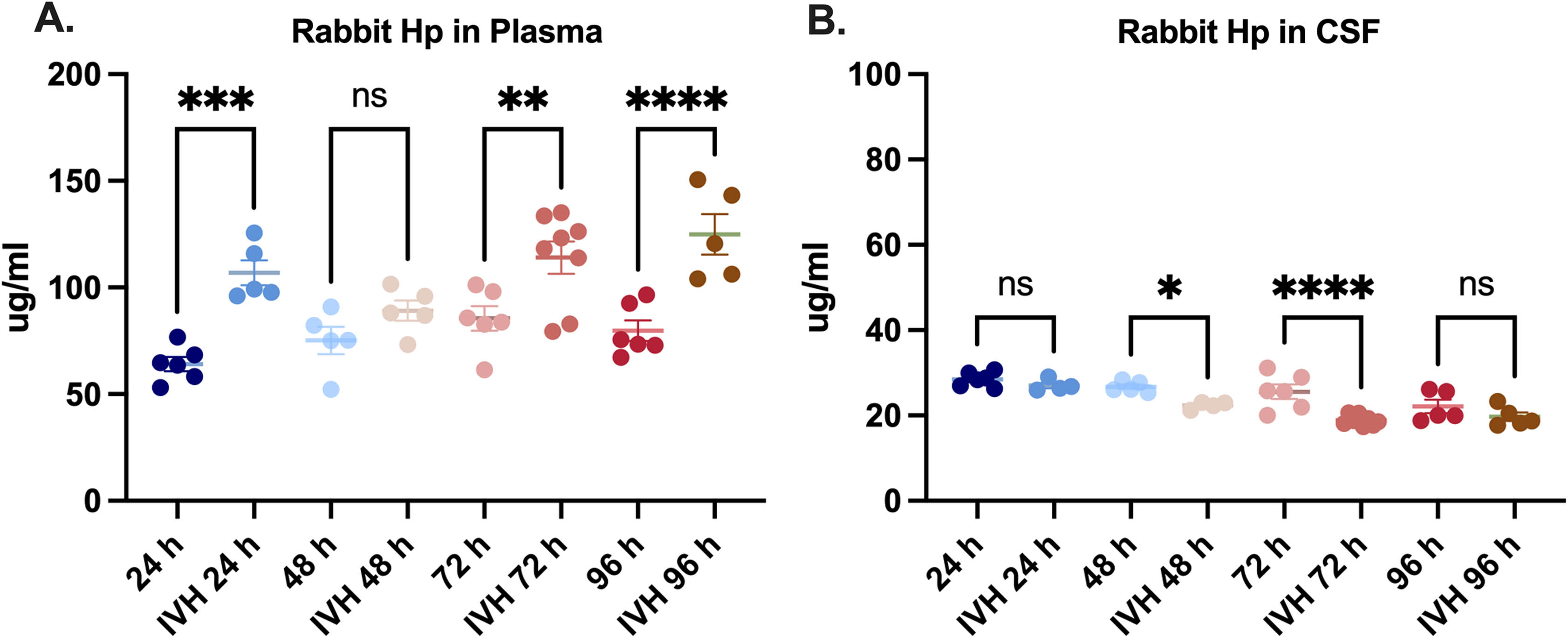
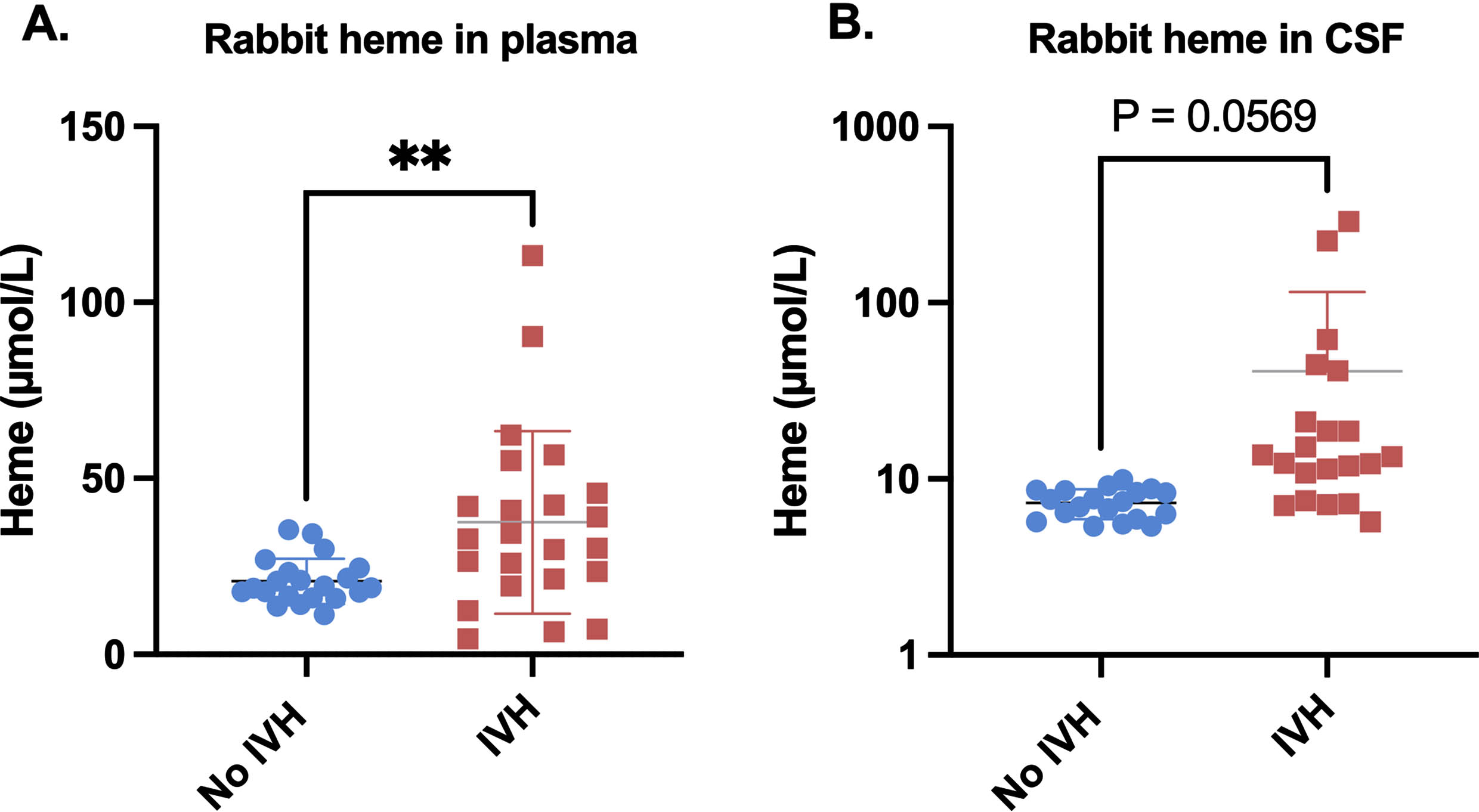
CONCLUSION: Intraventricular levels of cell-free Hb decreased rapidly during the first three weeks following cerebral IVH in preterm infants. Levels of Hp in CSF were extremely low throughout the study period indicating a severe deficit in endogenous cell-free Hb protection resources. Furthermore, results show that the rabbit pup model of IVH mimics aspects of IVH in preterm human infants, i.e., low Hp and high levels of Hb in the CSF. In conclusion, our data propose a role for hemoglobin scavengers as a treatment of IVH, and that the preterm rabbit pup model of IVH can be used to evaluate the therapeutic effect.
The effect of anakinra (il1 receptor antagonist) on immune dysfunction in infants with neonatal encephalopathy
Aoife Branagan1,2,3, Claudia Stanciu4, Johana Isaza-Correa1,2, Lynne Kelly1,2, Martin White1, Jan Miletin1, Claudine Vavasseur5, Eleanor J Molloy1,2,3,6
1Discipline of Paediatrics, Trinity College, The University of Dublin, 2Trinity Translational Medicine Institute & Trinity Research in Childhood Centre (TRiCC), Trinity College Dublin, 3Paediatrics, The Coombe Hospital, 4Paediatrics, Rotunda Hospital, 5Paediatrics, National Maternity Hospital, Holles Street, 6Neonatology and Paediatrics, Childrens Health Ireland
BACKGROUND: Neonatal encephalopathy (NE) is a clinical condition describing abnormal neonatal neurological function and incorporating multiple diverse aetiologies. Despite routine use of therapeutic hypothermia (TH), there is a significant burden of mortality and morbidity especially low- and middle-income countries. Therefore, there is an urgent need for the development of both stand-alone therapies and adjunctive treatments to TH. The pathophysiology of NE is based on immune dysregulation and inflammasome and interleukin 1 activation have been implicated. Anakinra (interleukin-1 receptor antagonist) is a short acing recombinant interleukin receptor antagonist, blocking both IL-1α and IL-1β activity and has been safely used in neonates. Our aim was to assess the impact of anakinra (IL1RA) on ex-vivo immune function of infants with NE as a potential therapeutic agent.
METHODOLOGY: We performed a prospective multicentre cohort study. Term infants with a diagnosis of NE undergoing TH were recruited. Blood samples were taken on days 1, 3 and 7 of life and compared with healthy neonatal controls. Innate immune function was analysed by flow cytometry for CD11b (cell activation, migration) and Toll-like receptor (TLR)-4 (recognition of lipopolysaccharide, LPS) in neutrophils (CD66b+) and subpopulations of monocytes (CD14/CD16) stimulated with and without LPS, treated with and without ILRA. Samples were assessed by reverse transcription–polymerase chain reaction for markers of inflammasome activation (NLRP3), downstream signalling of TLR4 (MyD88) and proinflammatory cytokines (IL1β).
RESULTS: Thirty-eight infants were recruited (NE =28; controls =10; total samples =60). In the NE group, 82% were Sarnat grade 2 encephalopathy and 36% had an abnormal MRI. There were no differences in innate immune function when assessed by CD11b or TLR4 after treatment with anakinra. Neutrophil CD11b, although initially suppressed, increased to baseline by day 7, indicating dysregulated immune responses. Neutrophil TLR4 was increased at all timepoints in infants with NE compared to control. PCR analysis showed significant increase in IL1β in infants with NE, both at baseline and after stimulation, which was not decreased by ILRA.
CONCLUSION: Ex-vivo treatment with anakinra does not alter immune function in infants with neonatal encephalopathy, and may not be a useful adjunctive therapy to TH.
The therapeutic potential of human MSCs in a double-hit model of encephalopathy of prematurity
Meray Serdar1, Markus Gallert1, Karina Kempe1, Kay-Anja Walther1, Mandana Rizazad1, Josephine Herz1, Ursula Felderhoff-Müser1, Ivo Bendix1
1Department of Pediatrics I/Neonatology & Experimental perinatal Neurosciences, Centre for Translational and Behavioral Sciences (C-TNBS), University Hospital Essen, University Duisburg-Essen
BACKGROUND: Premature born infants represent the largest patient cohort in pediatrics. Inflammation is one of the main risk factors for preterm birth and premature born infants are highly susceptible to different noxious stimuli like high oxygen concentrations (hyperoxia). As demonstrated previously, hyperoxia as well as inflammation induce perinatal brain injury affecting white and gray matter structures differently. Up to now, effective therapies are missing. Mesenchymal stem cells (MSCs) appear a promising therapeutic option because of their neuro-regenerative and immunomodulatory potential.
METHODOLOGY: At embryonic-day-20 pregnant dams received either a single intraperitoneal injection of 100 μg/kg lipopolysaccharide or sodium chloride. Pups of both sexes were exposed to hyperoxia (80% O) or room air at postnatal day 3 for 48 h. Human umbilical cord MSCs (50x10/kg bodyweight) or sodium chloride were administered intranasally immediately after hyperoxia. At postnatal day 11 white and gray matter injury, vascularisation, as well as neuroinflammatory responses are analyzed via immunhistochemistry and western blotting. Group comparisons (n=10-12) were either performed by ANOVA or Kruskal-Wallis and were corrected for multiple comparisons by Bonferroni or Dunn as appropriate.
RESULTS: The combination of maternal inflammation and postnatal hyperoxia induced a significant reduction of myelin basic protein expression, accompanied by a decreased fiber length and reduced numbers of intersections. These pronounced myelination deficits were significantly improved by MSC treatment. Furthermore, reduced brain volume in the double-hit condition was associated with a reduced expression of the layer 6 cortical neuronal marker T-box, brain, 1 (TBR1). The combination of maternal inflammation and postnatal hyperoxia induced a robust decrease in vessel density and an activation of microglia assessed by van-Willebrand staining and Iba1/CD68 co-staining, respectively. Importantly, therapeutic MSC-application improved these decisive outcome measures.
CONCLUSION: Within this newly established double-hit model of encephalopathy of prematurity, we detect promising therapeutic effects of a single intranasal MSC-application (at P5) at term-equivalent age (P11). If these effects translate into long-term functional and structural improvements will be assessed in future experiments.
Early arachidonic and docosahexaenoic supplementation in very premature infants and neurodevelopment at 2 years
Gunnthorunn Gunnarsdottir1, Helle C. Pfeiffer1, Tone Nordvik1, Kristina Wendel1, Marlen Fossan Aas1, Tom Stiris1, Anette Ramm-Pettersen1, Sissel J. Moltu1
1Oslo University Hospital
BACKGROUND AND OBJECTIVE: Neurodevelopmental sequelae of premature birth is a major medical challenge, and prevention is most wanted. The long-chain polyunsaturated fatty acids (LCPUFAs) Arachidonic acid (ARA) and Docosahexaenoic acid (DHA) are important for synaptogenesis, membrane function and myelination (1). They accumulate in neural tissue, most rapidly between the last trimester through to two years of age. Preterm infants have lower levels of DHA and ARA in neural tissue compared to term born infants (2). The purpose of this study was to evaluate the impact of essential fatty acid supplementation in very preterm infants on their neurodevelopmental outcome at the age of two.
METHODOLOGY: This is a follow-up study of a double blind, randomized controlled trial (RCT), in which infants born before 29 weeks gestational age (GA) were randomized to receive an enteral supplement of either 0.4ml/kg MCT-oil (medium chain triglycerides) or 0.4 ml/kg Formulaid (100mg/kg of ARA and 50mg/kg of DHA). The infants received supplementation from the 2nd day of life until 36 postmenstrual age (PMA). At 2 years of age, the children underwent assessment of cognitive function, language and motor skills, performed by a trained pediatrician, neuropsychologist and physiotherapist, all blinded to group allocation. The standardized tests used were Bayley Scales of Infant and Toddler Development, third edition (BSID-III) and Peabody Developmental Motor Scales second edition (PDMS-2).
RESULTS: In total, 120 infants were included in the original trial; mean GA at birth (range) was 26 weeks and 3 days (22 weeks and 6 days – 28 weeks and 3 days). Out of the 110 children who survived, 97 were assessed at the 2-year follow up and 93 had one or more neurodevelopmental scores available. The mean (range) corrected age when tested was 24 months+7 days (23 months - 26 months and 10 days). A two-sample t-test was performed to investigate the difference between the groups and the estimated effect size was calculated (STATA version 17, Stata Corp LP, College Station, TX) (Table 1).
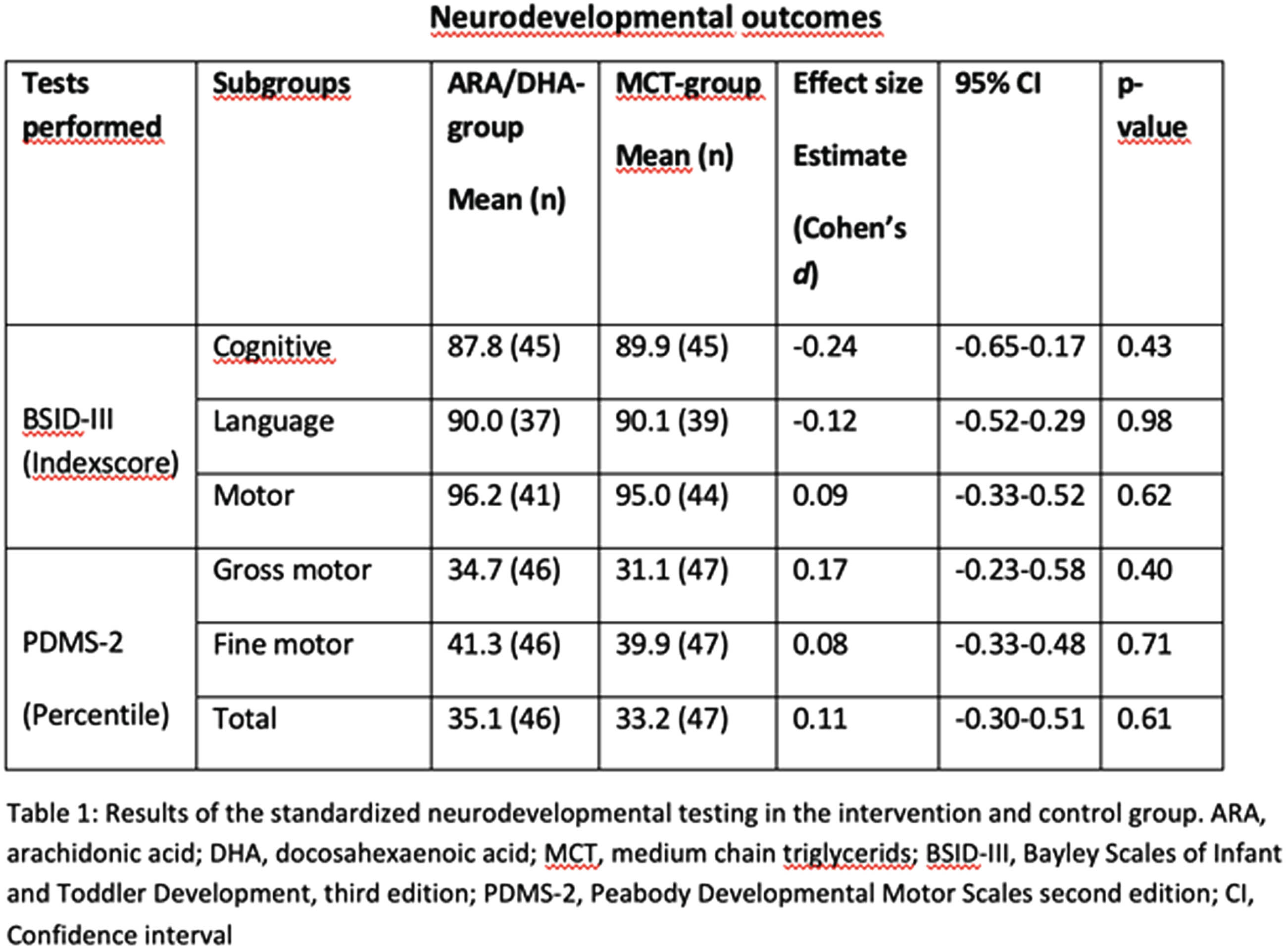
CONCLUSION: In-hospital supplementation with ARA and DHA in doses similar to estimated fetal accretion rates compared to standard treatment, did not result in significant differences in neurodevelopmental outcome, assessed with BSID-III and PDMS-2 scores at 2 years corrected age.
BIBLIOGRAPHY:
1. Embleton ND, Moltu SJ, Lapillonne A, van den Akker CHP, Carnielli V, Fusch C, et al. Enteral Nutrition in Preterm Infants (2022): A Position Paper From the ESPGHAN Committee on Nutrition and Invited Experts. J Pediatr Gastroenterol Nutr. 2023;76(2):248-68.
2. Gould JF, Roberts RM, Makrides M. The Influence of Omega-3 Long-Chain Polyunsaturated Fatty Acid, Docosahexaenoic Acid, on Child Behavioral Functioning: A Review of Randomized Controlled Trials of DHA Supplementation in Pregnancy, the Neonatal Period and Infancy. Nutrients. 2021;13(2):415.
Remote ischemic conditioning for neonates with hypoxic-ischemic encephalopathy: A phase I safety and feasibility trial
Emily Lo1, Brian Kalish2
1Division of Neonatology, Department of Paediatrics, The Hospital for Sick Children, University of Toronto, 2Division of Neonatology, Department of Paediatrics, The Hospital for Sick Children, Department of Molecular Genetics, University of Toronto
BACKGROUND: Hypoxic ischemic encephalopathy (HIE) is a devastating neurological injury that affects the neonate. Despite the standard of treatment of therapeutic hypothermia (TH), neonates with HIE experience significant mortality and morbidity (Azzopardi et al., 2009; Jacobs et al., 2013). Therefore, there continues to be a need for novel adjunctive therapies for HIE. Remote ischemic conditioning (RIC) is a novel therapeutic maneuver that creates cycles of ischemia-reperfusion to a remote site in the body, with the goal is to protect the organ exposed to greater ischemia from further injury. RIC has been shown to improve outcomes in animal studies of myocardial infarction and in adult stroke (Murry et al., 1986; Zhao et al., 2018). However, the effect of RIC on neonates with HIE has not been previously explored.
MATERIALS: A phase I safety and feasibility trial was conducted in a NICU with a sample size of 32 patients (16 control/16 intervention). The eligibility criteria included patients who were ≥35 weeks’ gestational age (GA) undergoing TH. The exclusion criteria included patients who were <35 weeks’ GA, who had known central nervous system malformations, known chromosomal or genetic anomalies, confirmed or suspected inborn error of metabolism, who required significant hemodynamic support, inhaled nitric oxide or fraction of inspired oxygen >50% for the four-hour period prior to RIC, or whose parents decided for withdrawal of life-sustaining treatment. RIC was administered with a blood pressure cuff applied to a limb and inflated and deflated to create ischemia-reperfusion cycles. Cohorts of four consecutive patients received escalating therapy of RIC. Clinical assessments of pain and components of vascular, cutaneous, muscular and neural complications were collected during RIC and compared between groups.
RESULTS: In this interim analysis, 30 of 32 patient were enrolled. The baseline characteristics of these patients are shown in Table 1 and the safety monitoring characteristics are shown in Table 2. The pain scores were not significantly different between the control and RIC group after the maneuver (PIPP 2.07 versus 3.07, p=0.24). Similarly, there was no statistical significant in the saturations between the groups (98.5% versus 98.1%, p=0.53). There was a statistical difference in the capillary refill time between the groups (2.4 versus 2.9 seconds, p=0.03), with the RIC group having a longer capillary refill time. There was no incidence of skin breakdown or bruising in either groups. There was a greater incidence of subcutaneous fat necrosis and acute kidney injury in the control group, but not statistically significant between groups. RIC was feasible in all enrolled patients randomized to the RIC group.
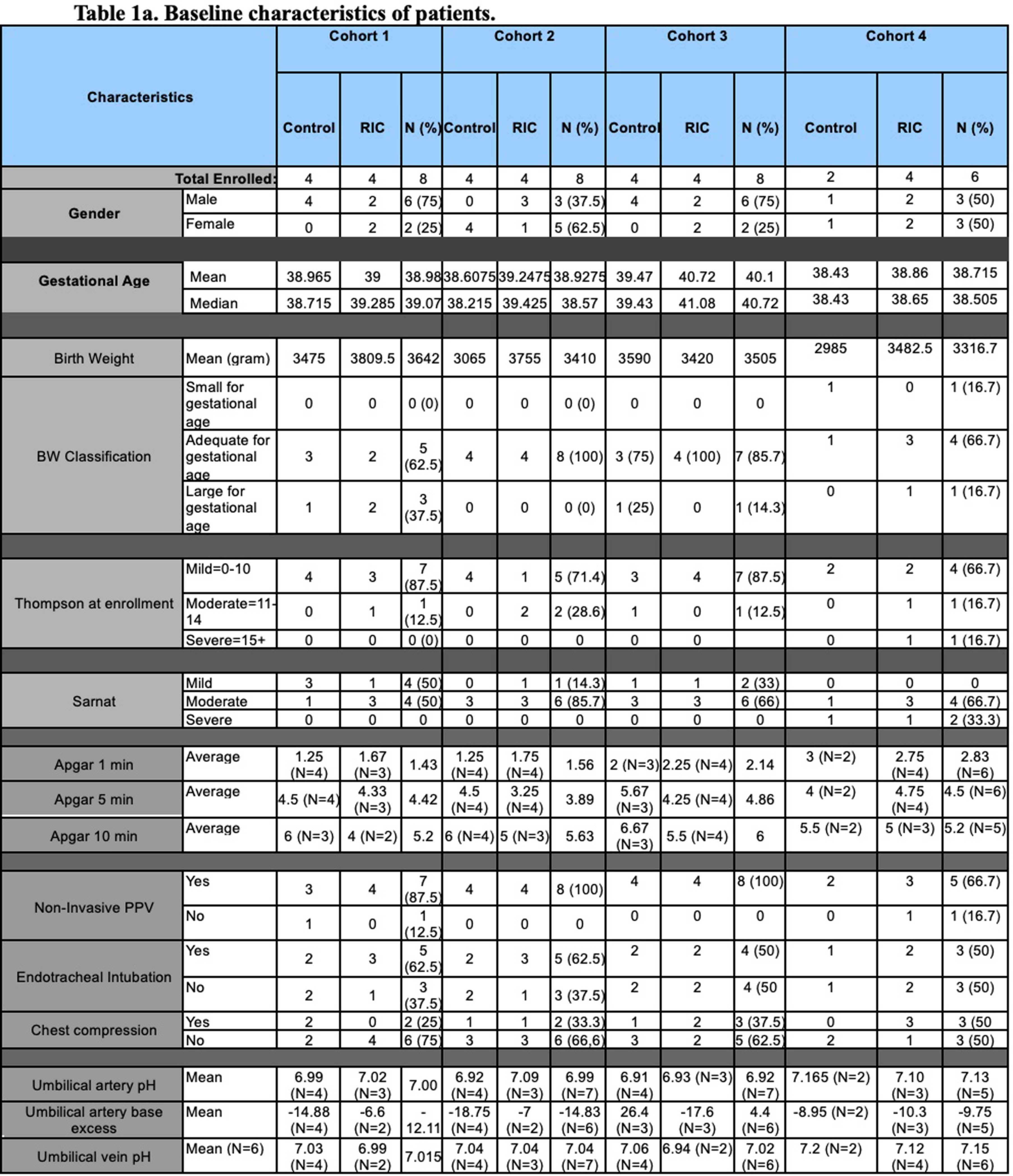
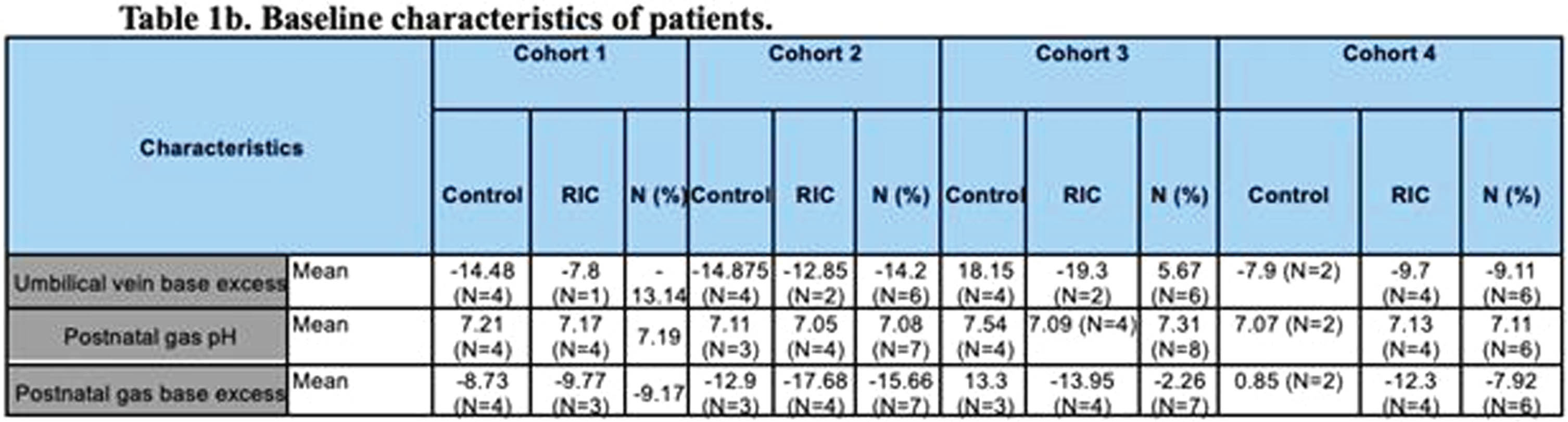
CONCLUSION: RIC in neonates with HIE undergoing TH is safe and feasible. A phase II trial is planned to determine the efficacy of RIC in HIE neonates as a novel, adjunctive therapy.
Sex differences in hippocampal testosterone content following neonatal hypoxia-ischemia
Ms Irem Isik1,2, Feyza Cetin2,3, Burak Ozaydin4, Nur Sena Cagatay2,3, Sefer Yapici2,3, Luc Collo5, Robin W. Goy5, Amita Kapoor5, Peter Ferrazzano2,3, Jon E. Levine5,6, Pelin Cengiz2,3
1University of Dublin, 2Waisman Center, University of Wisconsin-Madison, 3Department of Pediatrics, University of Wisconsin-Madison, 4Department of Neurological Surgery, University of Wisconsin-Madison, 5Wisconsin National Primate Research Center, University of Wisconsin-Madison, 6Department of Neuroscience, University of Wisconsin-Madison
BACKGROUND: Neonatal hypoxia-ischemia (HI) related encephalopathy is one of the major causes of learning and memory deficits in children. Clinical and experimental studies have shown that male newborns are two times more susceptible to the effects of HI, a phenomenon that is poorly understood. Our recent studies show that there is a sex difference in expression of the estrogen receptor alpha (ERa) which is upregulated in the female hippocampus following HI and confers sex-specific female-biased neuroprotection via neurotrophin receptor, tyrosine kinase B (1). The objective of this study is to determine sex hormone contents of the hippocampi following HI to investigate the availability of estradiol (E2) as a ligand to ERa produced by local aromatization of testosterone (T).
METHODOLOGY: Sham and HI surgeries were performed in postnatal day 9 C57BL/6J male and female mice using Vannucci’s HI model. Hippocampi were dissected, weighted and frozen immediately 3 days post-HI. For E2 and T content measurements, two hippocampi were pooled as n=1 and homogenized. Hormones were extracted and analyzed using LC-MS/MS (2). ANOVA was used for statistical analysis.
RESULTS: Hippocampal E2 (ng/g) contents were not significantly different between the experimental groups. Hippocampal T (ng/g) content was significantly higher in HI male IL (2.455±0.5984 pg/g, n:8) compared to HI female IL (0.8848±0.7454 pg/g, n:8) (p=0.0377). Male hippocampal E2 (ng/g) contents positively correlated with T contents (R2=0.5174, p=0.0017).
CONCLUSION: T content increases in male IL hippocampi and decreases in female IL hippocampi following HI. There is a sex difference in T levels in IL hippocampi following HI. The implications of the sex differences in the hippocampal sex steroid hormone contents maybe playing a role in long-term neurological outcomes following neonatal HI. Other hormone content measurements are being analyzed in a comprehensive manner and will help us identify targets to help improve neurological outcomes in a sex specific manner.
BIBLIOGRAPHY:
1. Cikla U, Chanana V, Kintner DB, Udho E, Eickhoff J, Sun W, et al. ERalpha Signaling Is Required for TrkB-Mediated Hippocampal Neuroprotection in Female Neonatal Mice after Hypoxic Ischemic Encephalopathy. eNeuro. 2016.
2. Kenealy BP, Kapoor A, Guerriero KA, Keen KL, Garcia JP, Kurian JR, et al. Neuroestradiol in the hypothalamus contributes to the regulation of gonadotropin releasing hormone release. J Neurosci. 2013.
Clinician stakeholder experience of Maine NET: a neonatal teleconsultation program to assess neonatal encephalopathy
Leah Marie Seften, Doctor Elizabeth Scharnetzki, Clairette Kirezi, Alexa Craig1
1Mainehealth, 2Tufts University School of Medicine
BACKGROUND: Serial neonatal encephalopathy (NE) exams are difficult to perform in rural community birth hospitals as most specialists are located hours away in the tertiary care center. In 2018, we developed and implemented a synchronous, acute care model of teleconsultation – the Maine Neonatal Encephalopathy Teleconsultation program (Maine NET). Maine NET provides remote, joint assessment for NE by neonatal neurology and neonatology at nine community hospitals.
OBJECTIVE: This study aimed to qualitatively assess clinicians’ experience using Maine NET. Our objective was to understand clinicians’ perceptions of Maine NET’s effectiveness and impact, as well as to identify limitations and opportunities for improvement.
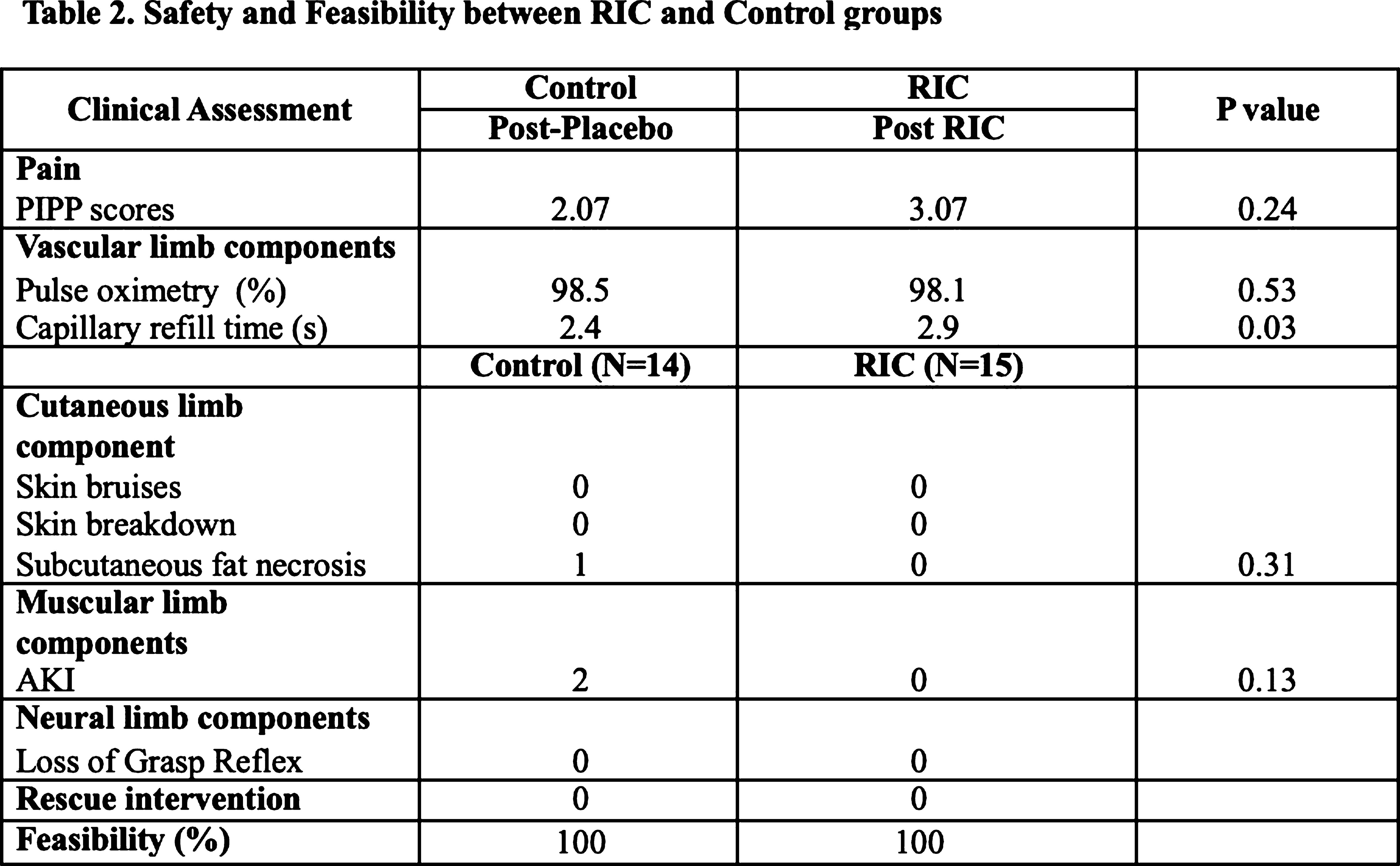
METHODOLOGY: We conducted virtual semi-structured interviews with clinicians from eight community hospitals and one neonatal intensive care unit who had participated in a MaineNET teleconsult from April 2018-October 2022. Interviews were transcribed and analyzed using inductive/deductive hybrid thematic analysis. Two researchers (LMS and ES) independently coded transcripts and met to discuss and reach consensus on themes.
RESULTS: Our sample had representation from each Maine NET hospital and consisted of 16 clinicians with interprofessional roles (3 neonatologists, 11 community physicians, 1 nurse, and 1 neonatal nurse practitioner). Clinicians overwhelmingly supported the program: “This program has truly saved babies’ lives and future function. I have not met any parents through this journey, who aren’t incredibly grateful for the care that is provided” and emphasized the benefit of collaboration between all care team members. Thematic analysis supported the hypothesized benefits of Maine NET, demonstrating that clinicians felt resource utilization, collaborative decision making, communication and continuity of care were improved (Table 1). Clinicians’ cited several additional benefits of Maine NET that were not originally hypothesized; these themes included reduced feelings of isolation, time pressure, and trauma (Table 1). Importantly, clinicians felt Maine NET also provided rural areas with more equitable access to neonatal specialists and educational opportunities specifically related to performing the NE exam and communicating with families about NE (Table 1). Telemedicine as a means for assessment for NE was felt to be “more than adequate to [assess] with the assistance of the pediatrician at the bedside.” Connectivity issues were repeatedly cited as a limitation in which clinicians noted utilizing to their own personal devices as an alternative to the program equipment: “We couldn’t get our computer to work because of a firewall issue and upgrade in the system, so we just used my phone”.
CONCLUSION: Maine NET was well-supported and was felt to positively impact delivery of care for newborns with concern for NE. Additionally, the program has improved resource allocation, collaboration decision making, communication and equity of care. Addressing technological challenges will be vital to the success and sustainability of the planned Maine NET expansion.
Mortality and complications in the management of hypoxic-ischemic encephalopathy with hypothermia in epic/latino neonatal network
Angela Hoyos2, Marco Belzu3, Manuel Benitez4, Ruben Hernandez4, Carlos Fajardo1, Luis Monterrosa5, Carolina Villegas6
1University Of Calgary, 2University El Bosque, 3Clínica Las Américas, 4Centenario Hospital de Especialidades Miguel Hidalgo, 5Saint John Regional Hospital, 6UASL. Hospital Central
BACKGROUND: A recent study reported that therapeutic hypothermia (TH) showed it doesn’t reduce the combined prognosis of mortality and disability at 18 months, in low- and middle-income countries for patients with hypoxic ischemic encephalopathy (HIE) who went into TH, suggesting that this therapeutic strategy should not be offered in such countries.
OBJECTIVE: To determine mortality and neurological response (in relation to Sarnat stages and death) before and after TH use in newborns with HIE in the EpicLatino network.
METHODOLOGY: The EpicLatino network collects data from neonatal units in Latin America, which are all located in low- and middle-income countries. Patient data was collected from 2015 to 2022 from units that admitted patients to therapeutic hypothermia. Mortality and Sarnat score were compared before and after TH. Wilcoxon Signed Rank Test was used for comparison between before and after TH.
RESULTS: This is a observational and retrospective study. A total of 437 neonates less than 3 days old at admission (Table 1) were found and 149 underwent therapeutic hypothermia. (Table 2) The Wilcoxon Signed Rank Test of 138 cases with all the information showed a significant difference (see Figure 1).
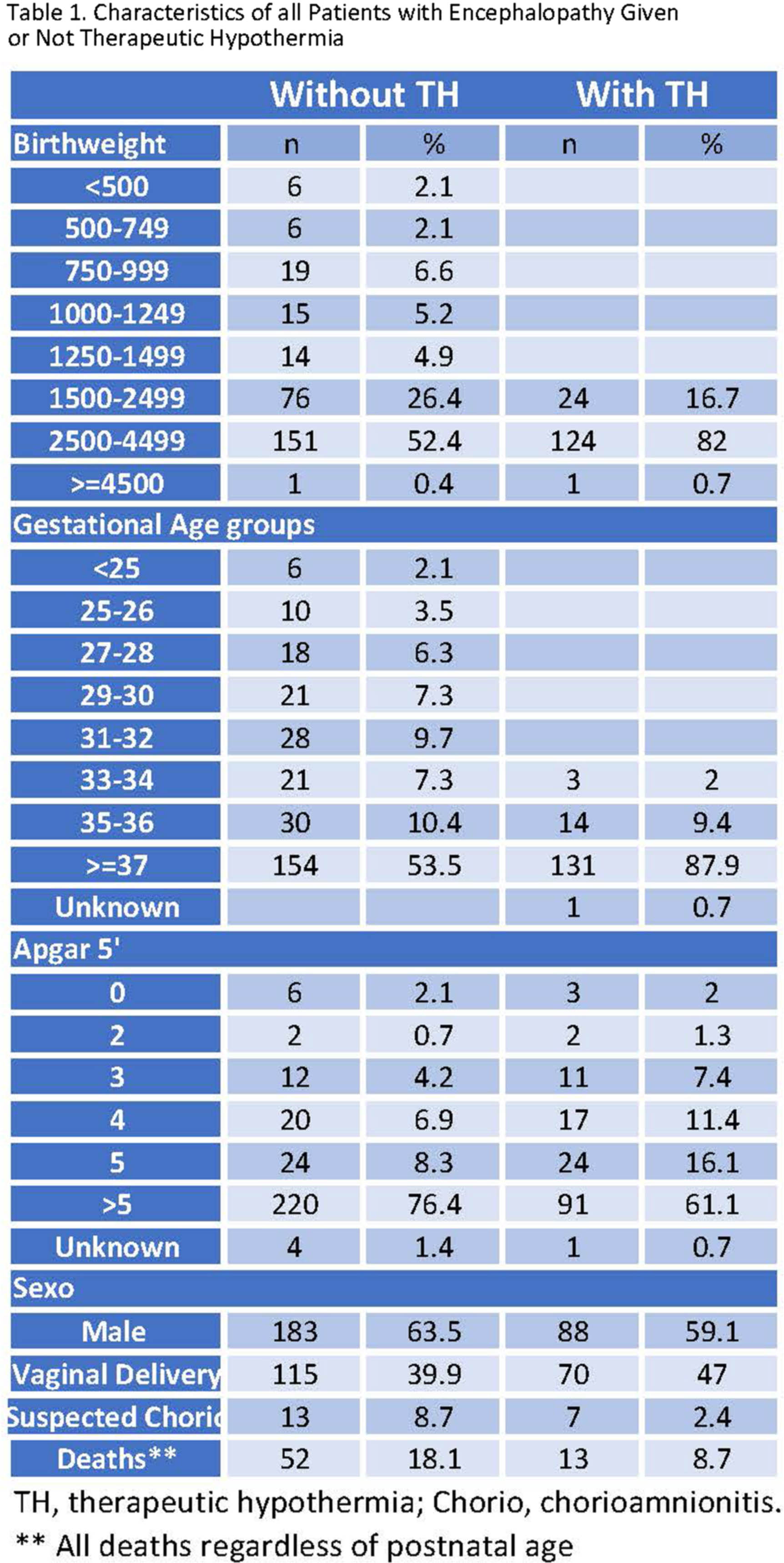
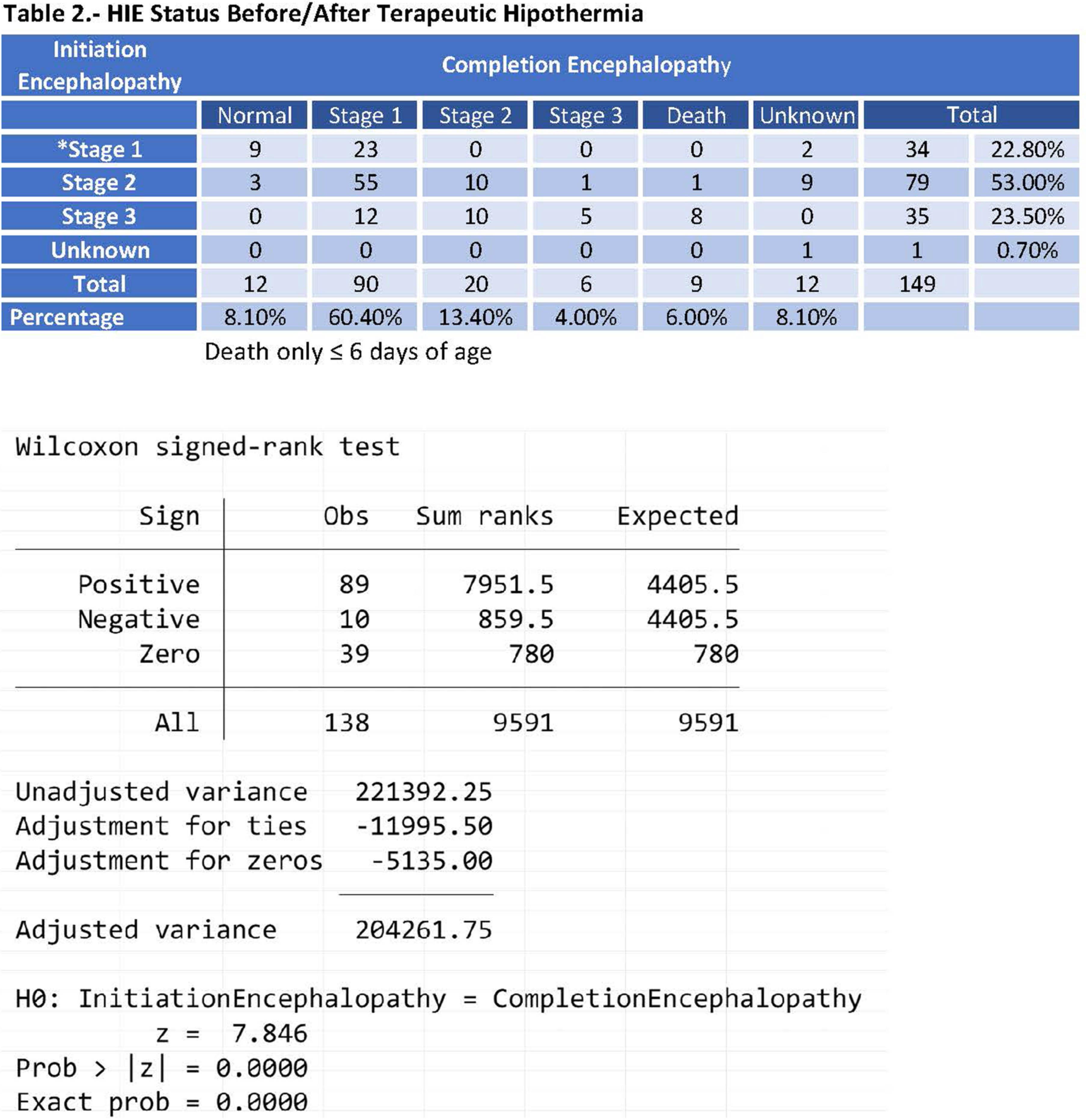
The total number of deaths was 13 patients, 9 of them died in the first 6 days of life and we assigned those deaths to TH. The rest of patients died on days 11, 14, 17 and 70 of life.
CONCLUSION: It could be concluded that in this group of patients, 64.5% they had better neurological results post therapeutic hypothermia with statistical significance as shown in Table 2 and Figure 1. The results obtained in this study, support the benefit of the use of TH in moderate to severe hypoxic ischemic encephalopathy in this group. We think that we could not randomize patients to TH and placebo and deprive some of them of this therapy. And we think that TH should not be withheld just for being in a low- or middle-income country. A very careful selection and strict protocol could be the answer.
Effect of telemedicine consults on time to assess neonatal encephalopathy in a rural state
Alexa Craig1, Leah Marie Seften, Anya Cutler
1Mainehealth, 2Tufts University School of Medicine
BACKGROUND: In Maine, the most rural state in the country, timely assessment of neonatal encephalopathy (NE) to determine eligibility for therapeutic hypothermia (TH) can be challenging due to large geographical distances between the tertiary care center and rural community hospitals. In order to improve our ability to assess NE, we developed a synchronous, acute care model of neonatal teleconsultation connecting nine community hospitals virtually with a neonatal neurologist and a neonatologist from the tertiary care center.
OBJECTIVE: We aimed to determine if the implementation of telemedicine consults in the community hospital would decrease the time to initiation of TH.
METHODOLOGY: We compared neonates treated with TH prior to implementation of the telemedicine consult program (pre-tele) to those treated after implementation (post-tele) for the primary outcome of time to initiation of TH. We also assessed short-term outcomes including seizures, and the combined outcome of severe injury on brain MRI as determined by the Weeke scoring system (gray matter subscore >9.5) or death. Group differences were assessed by Wilcoxon Rank Sum, Fisher’s Exact, and Chi-squared tests as appropriate.
RESULTS: There were 84 neonates in the pre-tele group and 62 in the post-tele group, all born in community hospitals and treated with TH. Mothers in the post-tele group were older and had higher rates of pregnancy complications such as gestational diabetes and preeclampsia/eclampsia (Table 1). The median Apgar scores and mean arterial cord gases and median NE scores did not differ between groups. The time to TH initiation was 4.0 hours (IQR 3, 5) for the pre-tele group and 4.5 hours (IQR 3, 5.5) for the post-tele group. There were no significant differences in the rates of seizure or severe brain injury on MRI/death based on group. Fewer neonates with mild NE were treated with TH in the post-tele timeframe (Figure 1).
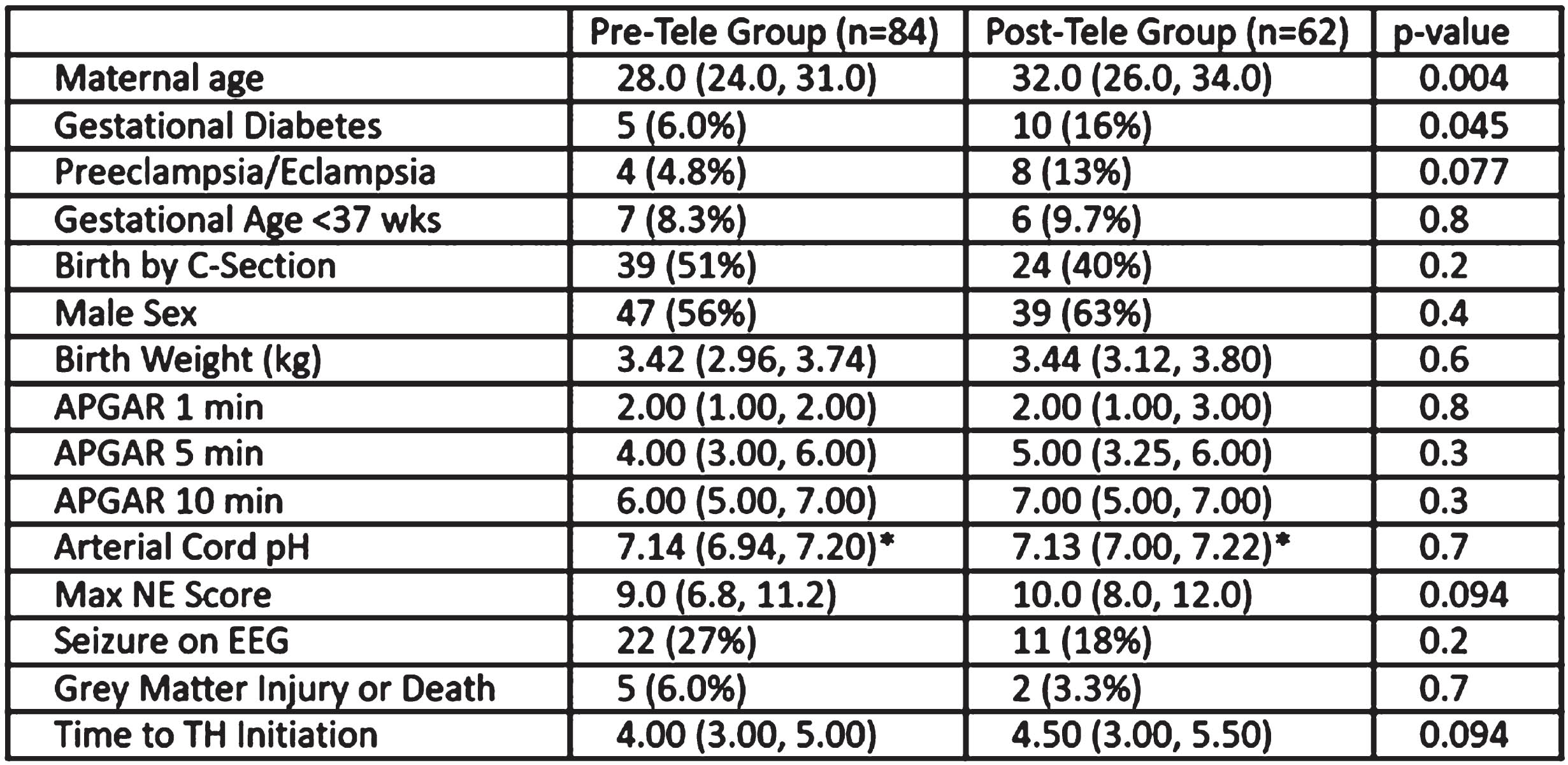
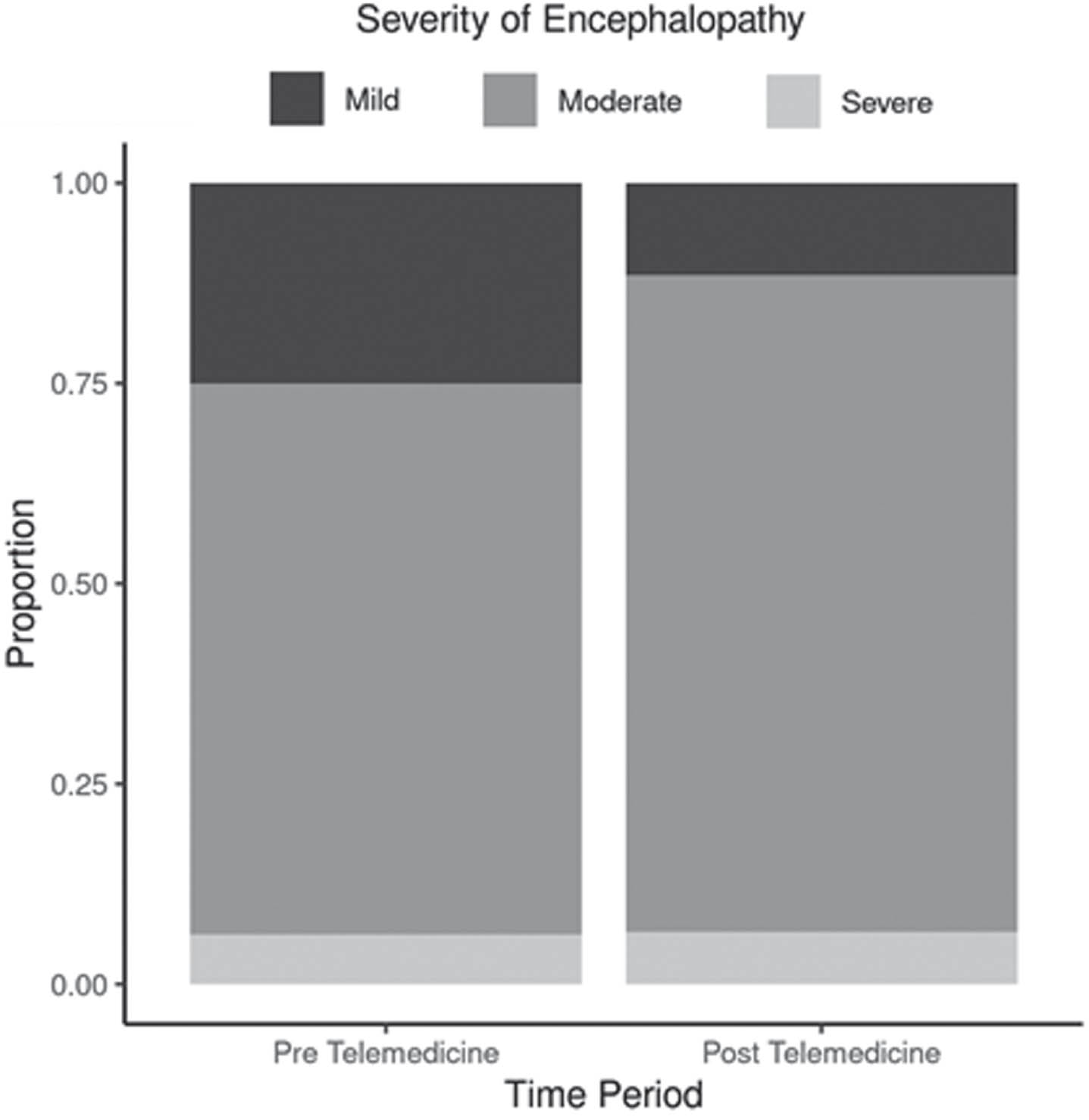
CONCLUSION: Telemedicine consults in the community hospital were associated with a 30-minute delay in initiation of TH, rather than a decrease in the time to initiate. There were however no differences in the short-term outcomes of seizures, or severe gray matter injury on MRI/death. Reassuringly, in the post-tele implementation period, fewer neonates with mild encephalopathy were treated with TH suggesting a potential unanticipated benefit in terms of improved patient selection.
Effects of caffeine on infants with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia
Rakesh Lavu1, Nicholas Nicoletti1, Sarah Worley1, Doctor Sreenivas Karnati1, Hany Aly1, Ceyada Acun1
1Cleveland Clinic Childrens Hospital
BACKGROUND: Therapeutic hypothermia is currently the standard of care for infants with moderate to severe Hypoxic Ischemic Encephalopathy (HIE). Several adjuvant therapies have been used to improve the neurodevelopmental outcomes in these infants. Caffeine, in addition to its diuretic effect on the kidney, has shown potential neuroprotective benefit in animal studies. The effects of caffeine on infants with HIE undergoing therapeutic hypothermia are still unknown.
OBJECTIVE: 1.To compare the changes in urine output and renal function in infants who did and did not receive caffeine while undergoing therapeutic hypothermia for moderate to severe HIE. 2. To compare the short-term outcomes such as seizures, MRI findings, EEG changes, length of stay and mortality during NICU stay in both groups.
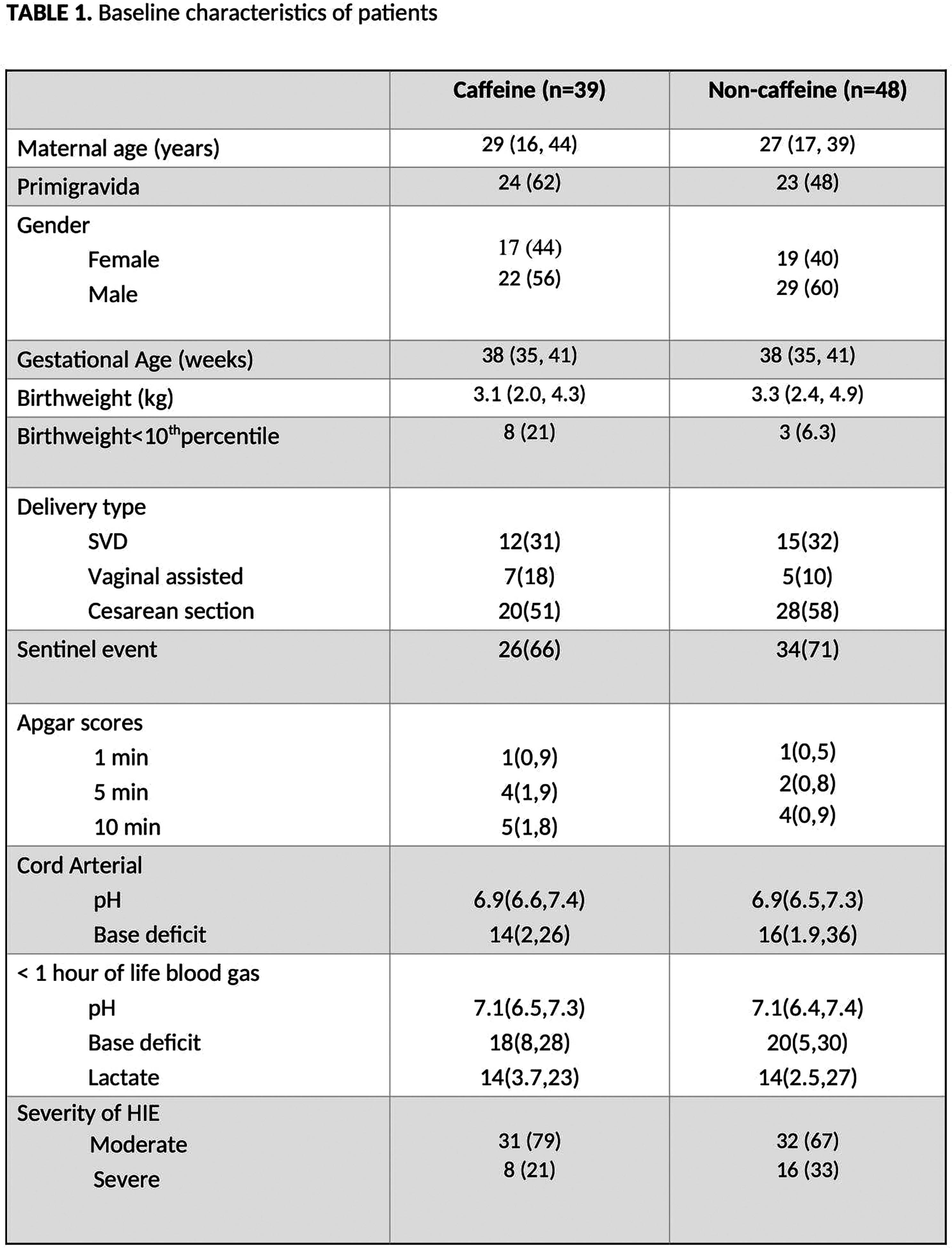
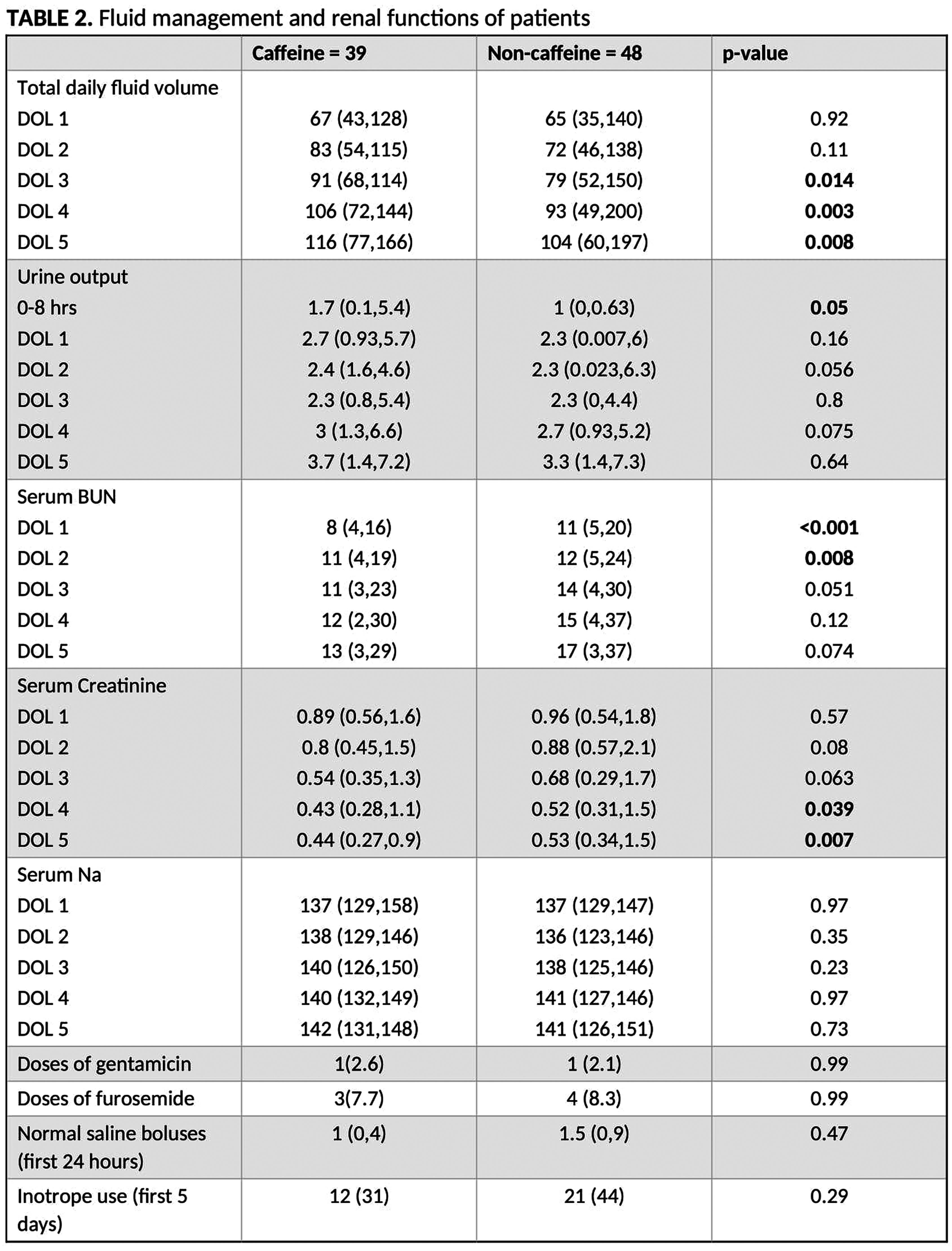
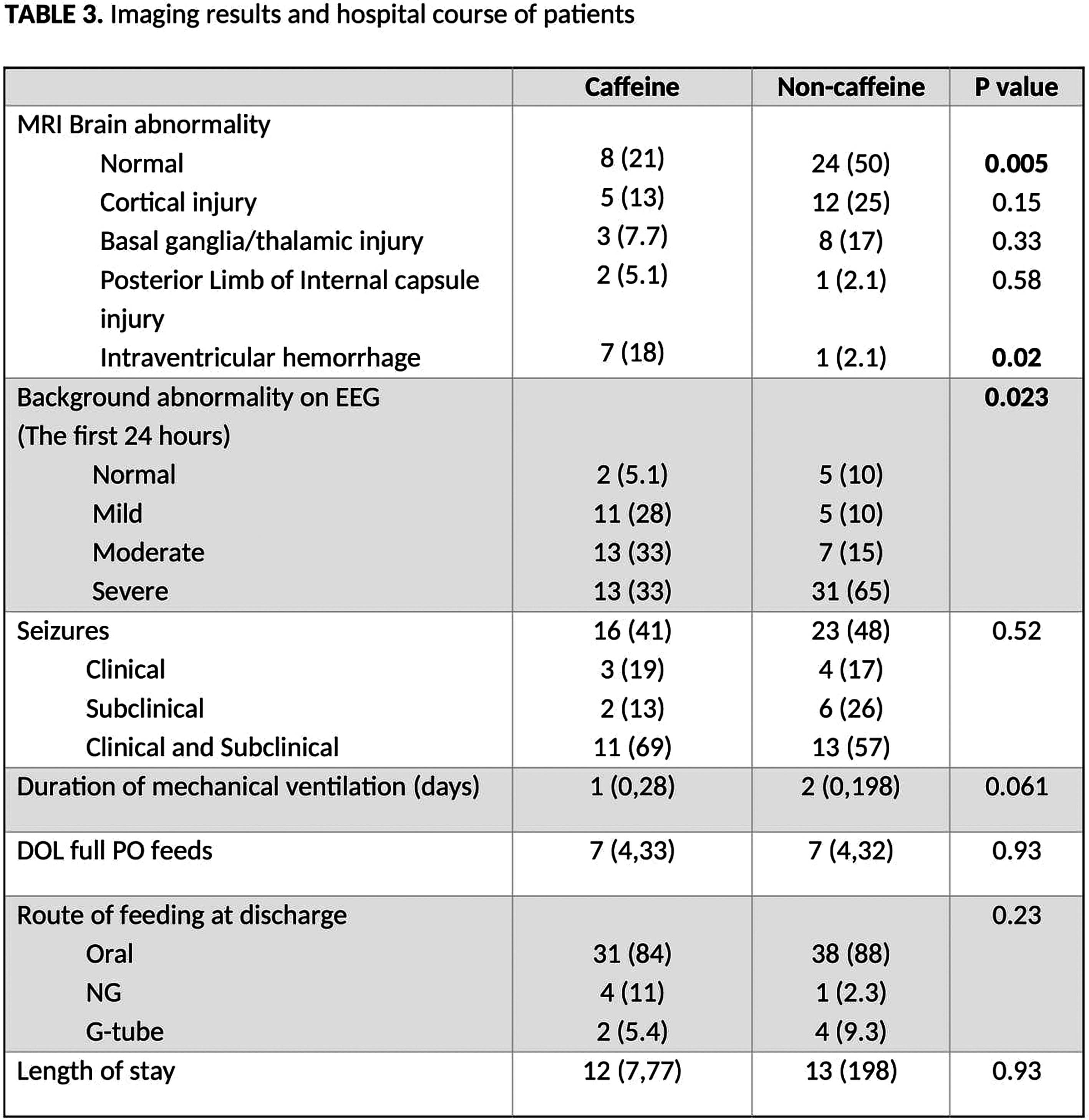
METHODOLOGY: This is a retrospective cohort study from January 2013 – December 2022. We reviewed charts of neonates born ≥36 weeks of GA, who were admitted with a diagnosis of moderate to severe HIE and treated with therapeutic hypothermia. Infants with severe congenital malformations or chromosomal anomalies were excluded from the study. The caffeine group received a onetime 20 mg/kg dose of caffeine.
RESULTS: A total of 87 infants underwent therapeutic hypothermia for moderate to severe HIE, of which 39 infants (45%) received caffeine with median time of administration being at 6 hours of life. Both the groups had similar baseline characteristics. There was overall improvement in the urine output in infants who received caffeine, particularly in the first 8 hours of life with median urine output of 1.7 vs 1 cc/kg/hr. Caffeine receiving neonates had better renal function with significantly lower BUN levels in first two days of life (8,11 vs 11,12) and lower serum creatine levels on DOL 4 (0.43 vs 0.52) and DOL 5 (0.44 vs 0.53). Infants who received caffeine had a significantly smaller proportion with normal MRI findings (21% vs 50%, p= 0.005) and had an increased incidence of IVH (18% vs 2.1%, p=0.02) when compared to non-caffeine group. Non-caffeine group had higher level of background EEG abnormality in the first 24 hours of life compared to caffeine group (p=0.023), however there was no difference in seizure frequency, length of stay or mortality between the groups.
CONCLUSION: The use of caffeine in neonates with HIE undergoing hypothermia was associated with an improvement in UOP and renal function. However, it was associated with a higher proportion of infants with abnormal MRI findings. A randomized trial will be needed to establish the efficacy and safety of caffeine in infants with HIE.
Using wharton’s jelly umbilical cord extracellular vesicles containing mature micrornas to treat premature brain injuries
Vera Tscherrig1,2, Valérie Haesler1, Marel Steinfort1,2, Amanda Brosius-Lutz1, Daniel Surbek1, Andreina Schoeberlein1, Marianne Joerger-Messerli1
1Department of Obstetrics and Feto-maternal Medicine, University Women’s Hospital, Inselspital, Bern University Hospital, Bern, Switzerland and Department for BioMedical Research (DBMR), University of Bern, Switzerland, 2Graduate School for Cellular and Biomedical Sciences (GCB), University of Bern, Bern, Switzerland
BACKGROUND: Premature birth is the primary cause of childhood morbidity and mortality. Premature birth often results in neurological injuries, such as premature white matter injury (WMI), leading to long term neurological impairments with global health and economic burdens. A promising therapeutic agent for WMI are mesenchymal stromal cell-derived small extracellular vesicles (MSC-sEV). They carry microRNAs (miRNAs), predicted to target mRNAs encoding for proteins involved in premature WMI. We hypothesize that miRNAs have a crucial function in the observed beneficial effects of MSC-sEV.
METHODOLOGY: Mesenchymal stromal cells were cultivated from the connective tissue of the human umbilical cord, the so-called Wharton’s jelly (WJ-MSC). Small EVs were isolated from the WJ-MSC’s supernatant by ultracentrifugation followed by size exclusion chromatography. The sEV were characterised using proteomics, western blot, ImageStream, and ZetaView analyses. The miRNA content of the sEV was measured with quantitative PCR. A luciferase assay was established to validate the miRNA-mediated repression of target genes, and a knock-down (kd) of DROSHA, a gene encoding an enzyme involved in miRNA maturation, in WJ-MSC was performed to evaluate the functionality of the sEV-miRNAs. In vitro assays were performed to analyse the regulatory potential of sEV on oligodendrocyte lineage differentiation and neuronal apoptosis. A previously established in vivo model of premature WMI was used to analyse the therapeutic effect of sEV-miRNAs. Near-infrared DiR-labelled sEV were used to validate the biodistribution of intranasally applied sEV.
RESULTS: The WJ-MSC-sEV comprised known sEV-criteria. They contained miRNAs predicted to be involved in WMI-related processes. The luciferase signal in the reporter cell line HEK293T, transfected with vectors containing the miRNA binding sites of TP53 or TAOK1, genes involved in WMI, was significantly reduced when sEV were added. This reduction indicates an inhibitory effect of sEV-miRNAs. Maturation of the oligodendrocyte lineage was enhanced after the addition of naïve sEV to the human oligodendrocytes (MO3.13). After oxygen-glucose deprivation, naïve sEV reduced apoptotic markers in neuroblastoma cells (N2a). In vivo, naïve sEV decreased microglia activation measured by Iba1 and CD68 expression and improved oligodendrocyte maturation reflected by the expression of myelin basic protein (Mbp). DROSHA kd in WJ-MSC led to the production of sEV with less miRNA cargo. These DROSHA kd sEV had a lower effect on the in vitro and in vivo assays than naïve sEV. In addition, intranasally applied sEV reach the brain and remain there for at least 24 hours.
CONCLUSION: Our results strongly indicate the critical relevance of the miRNA cargo in the therapeutic effect of MSC-sEV in premature WMI. Intranasal administration is a minimally invasive method to deliver MSC-sEV to the brain.
What happens to infants with perinatal-acidemia at birth that do not meet criteria for therapeutic-hypothermia?
Ana Alvarez Pagan1, Juhi Motiani, Catherine Hahn, Tara Lozy, Ariel Sherbany, Rakesh Chhabra, Marwa Khalil
1Hackensack University Medical Center
BACKGROUND: It is known that neonatal neurological status can evolve rapidly and progress from no or mild encephalopathy to more severe manifestations in the first hours to days after birth. Recent data in untreated infants with “mild” HIE show a higher range of abnormal neurologic outcomes through school age.
OBJECTIVE: Investigate the outcome among newborns with gestational age > 35 weeks born over 10 years with significant metabolic acidosis who did not meet therapeutic hypothermia (TH) criteria.
METHODOLOGY: Single-center retrospective chart review of newborns from Jan. 2013 to June 2022 with cord gas pH <7.0 and/or base excess ≥ 12 mmol/L born at a tertiary center. We excluded babies with birth anomalies, birth weight < 1800g, if they met TH criteria or required transfer or expired. Summary statistics were used to describe outcomes.
RESULTS: In this 10-year cohort, n=484 from 61,932 live births were identified with perinatal acidemia. 54 were excluded. 430 infants met our inclusion criteria. The mean pH was 7.06 (SD - 0.11) and the median for BD was -14.1 (IQR-15.3 to -12.3). Of these 248 (57.7%) were admitted to the NICU and 182 (42.3%) were admitted to the well-baby nursery (WBN). 78% (194/248) of admissions to the NICU were due to respiratory distress. Of those admitted initially to the WBN, 14.3% (26/182) required transfer to the NICU. 7/26 (27%) had hypoglycemia,6/26 (23%) had respiratory distress, 1/26 developed seizures. 9 patients had failed hearing tests at discharge. Access to long term outcomes was limited in our cohort; they included speech delay in 4, attention deficit hyperactivity disorder(ADHD) in 2, and autism spectrum disorder (ASD) in 2.
CONCLUSION: Infants who experience perinatal acidosis at birth but do not meet the criteria for therapeutic hypothermia are at an increased risk of being admitted to the NICU. These infants may experience short-term outcomes such as hypoglycemia, respiratory distress, and seizures, which may be signs of perinatal hypoxia-ischemia. It is worth noting that this cohort had adverse long-term neurodevelopmental outcomes. Therefore, it would be beneficial to monitor this population closely for signs of mild encephalopathy in an intensive care setting. Additionally, long-term follow-up could prove to be useful for patients, including neurodevelopmental assessments and services such as early intervention programs (EIP) if required. Further studies are necessary to address these findings.
BIBLIOGRAPHY:
1. Chalak, L. F. (2018). Best practice guidelines on management of mild neonatal encephalopathy: Is it really mild? Early Human Development, 120, 74.
2. Chalak, L. (2022). New Horizons in Mild Hypoxic-ischemic Encephalopathy: A Standardized Algorithm to Move past Conundrum of Care. Clinics in Perinatology, 49(1), 279–294.
Changes in circulating immune regulatory cells in infants with hypoxic ischemic encephalopathy under therapeutic hypothermia
Taylor Harris1, Aashish Gupta1, Madison Denney1, Chant Katrjian1, Karin Hermans1, Diane Wilson1, Vann Chau1, Donna Wall1, Amr El Shahed1
1The Hospital for Sick Children
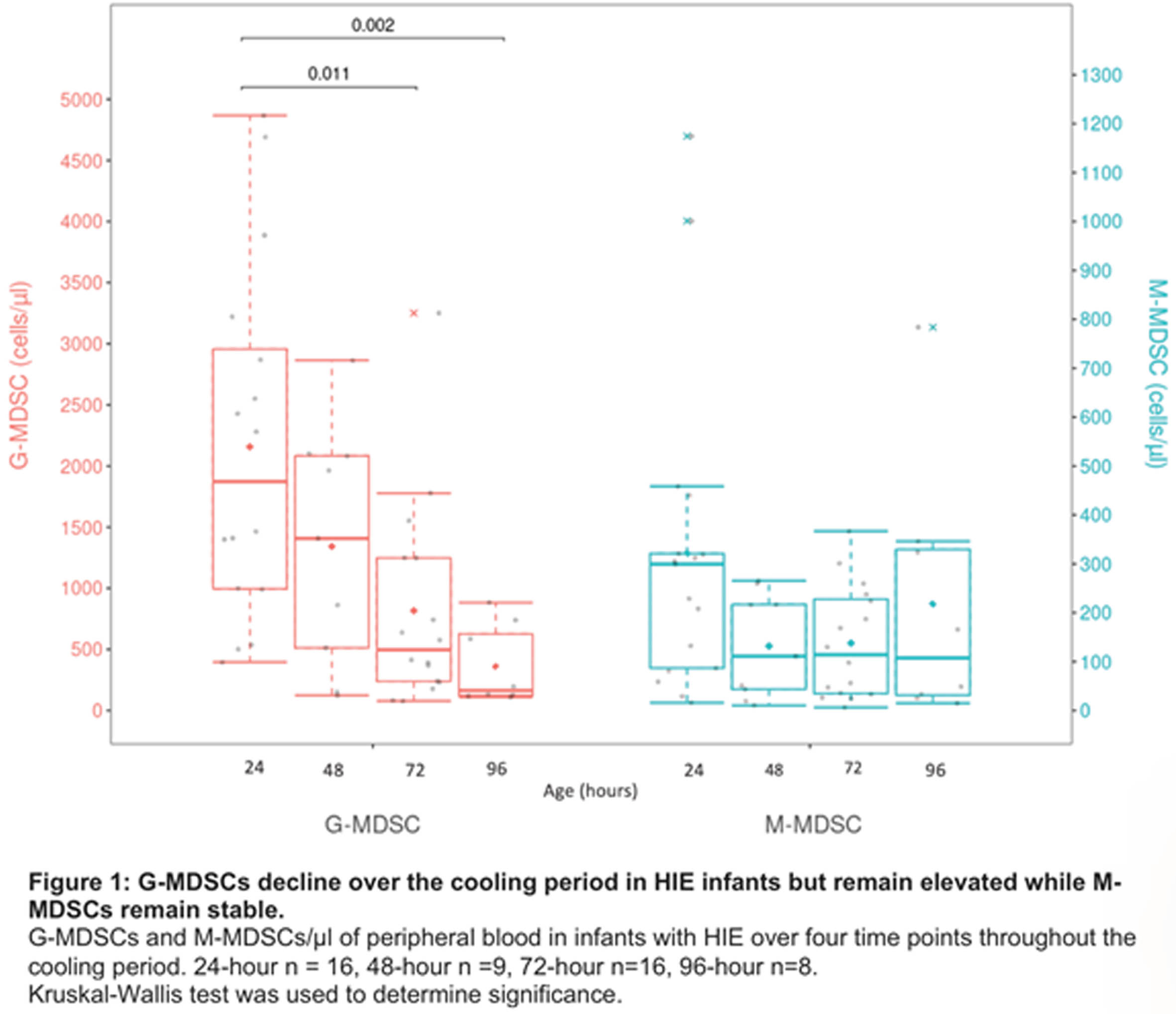
BACKGROUND: In hypoxic-ischemic encephalopathy (HIE), perinatal disruption of oxygenation to the brain triggers a potent secondary inflammatory cascade, causing neuronal cell death. Immature myeloid cells which expand under inflammatory conditions, exert profound anti-inflammatory responses, and may dampen this secondary neuronal cell death. Healthy newborns have high levels of CD34+ hematopoietic stem/progenitor and immune regulatory cells which soon diminish after birth. We postulate that these cells can be utilized to reduce the inflammatory cascade in HIE as an adjuvant strategy to therapeutic hypothermia (TH). The main purpose of our study is to establish baseline levels of circulating CD34+ and immune regulatory cells in HIE infants. It will serve as a foundation for future intervention trial focused on expanding autologous regulatory myeloid cells using G-CSF.
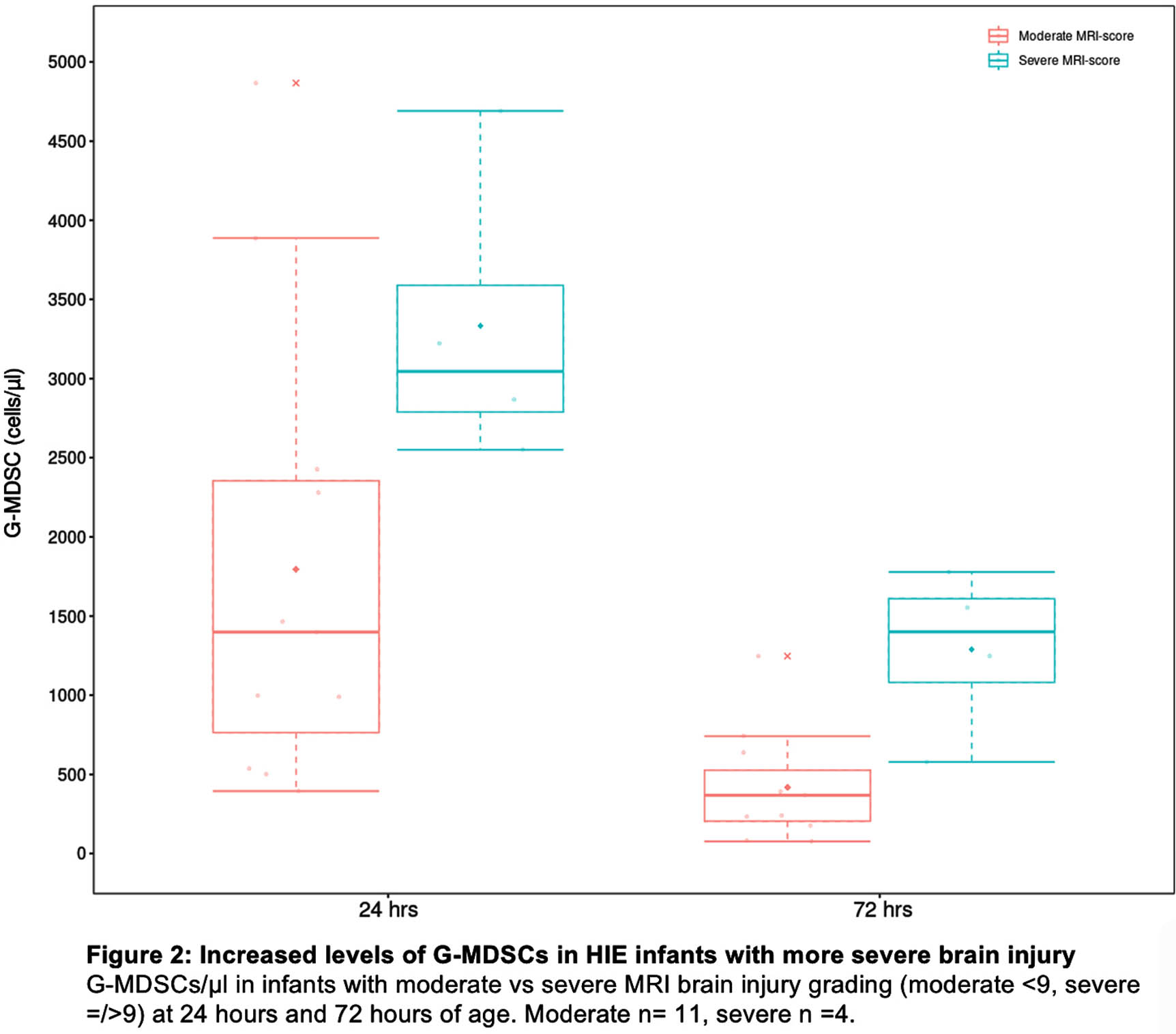
METHODOLOGY: Nineteen infants with HIE who underwent TH were enrolled in this prospective study. Circulating CD34+ and immune regulatory cells such as Granulocytic myeloid derived suppressor cells (G-MDSCs) and Monocytic myeloid derived suppressor cells (M-MDSCs) were measured daily over four time points during cooling and after rewarming by flow cytometry. Kruskal-Wallis test was used to determine statistical significance. Further, the degree of brain injury was scored by standard Magnetic Resonance Imaging (MRI) scoring published by Weeke et al. and Granulocytic-MDSCs levels were correlated with MRI scoring.
RESULTS: Of the 19 infants, 3 (16%), 14 (74%), and 2 (10%) infants presented with mild, moderate, and severe encephalopathy respectively. G-MDSCs (CD15/HLA-DR-/LOX-1+), normally not present in circulation, were present at birth (average = 1689, range = 394-3887 cells/μl) and decline (average = 371, range = 112-727 cells/μl; p<.05) by 96 hours. This suppressive population seems to be elevated in HIE infants with severe brain injury compared to those with less injury. M-MDSCs (CD33+, CD14+, HLA-DR-) were also elevated compared to healthy individuals and remained stable over the cooling period (average= 212 cells/μl, range = 6-1175 cells/μl).
CONCLUSION: Our findings affirm the link between immune regulatory cell levels and the severity of brain injury in infants with HIE. Our future research will explore the potential of G-CSF administration to augment these cells in order to mitigate second-phase inflammatory toxicity in this population.
BIBLIOGRAPHY:
1. He YM, Li X, Perego M, et al. Transitory presence of myeloid-derived suppressor cells in neonates is critical for control of inflammation. Nat Med. 2018;24(2):224-231.
2. Kim JP, Lee YH, Lee YA, Kim YD. A comparison of the kinetics of nucleated cells and CD34+ cells in neonatal peripheral blood and cord blood. Biol Blood Marrow Transplant. 2007;13(4):478-485.
3. Weeke LC, Groenendaal F, Mudigonda K, et al. A Novel Magnetic Resonance Imaging Score Predicts Neurodevelopmental Outcome After Perinatal Asphyxia and Therapeutic Hypothermia. J Pediatr. 2018;192:33-40.e2.
Omegaven is not cytoprotective after inflammation-amplified hypoxia-ischemia in a newborn piglet model
Christopher Meehan1, Raymand Pang1, George Maple1, Ellie Campbell1, Ilenia D’Angelo1, Yujin Kim1, Katie Tucker1, Fransisco Torrealdea1, Alan Bainbridge1, Nicola Robertson1,2
1University College London, 2University of Edinburgh
BACKGROUND: Therapies for neonatal encephalopathy (NE) are urgently needed in Low- and Middle-Income Countries where the burden of cases is high and therapeutic hypothermia (HT) may not be safe and effective (Thayyil, 2021). In Sub-Saharan Africa infection/inflammation increases the risk of NE (Tann, 2019). Omegaven is a fish oil lipid emulsion, containing Docosahexaenoic Acid and Eicosapentaenoic Acid, which are Omega-3 fatty acids, (n-3-FA) essential for neuronal membrane function and precursors for lipid mediators that regulate the inflammatory response (Dyall, 2015). Preclinical studies have shown varying neuroprotective efficacy using n-3-FA but without consensus on dosing (Williams, 2013; Hunn, 2018). Clinically, the safety of Omegaven at 1g/kg/d has been established (Gura, 2007).
OBJECTIVE: To assess the cytoprotective efficacy of Omegaven in an established newborn piglet model of inflammation amplified hypoxia ischaemia (IA-HI) in which HT is not beneficial.
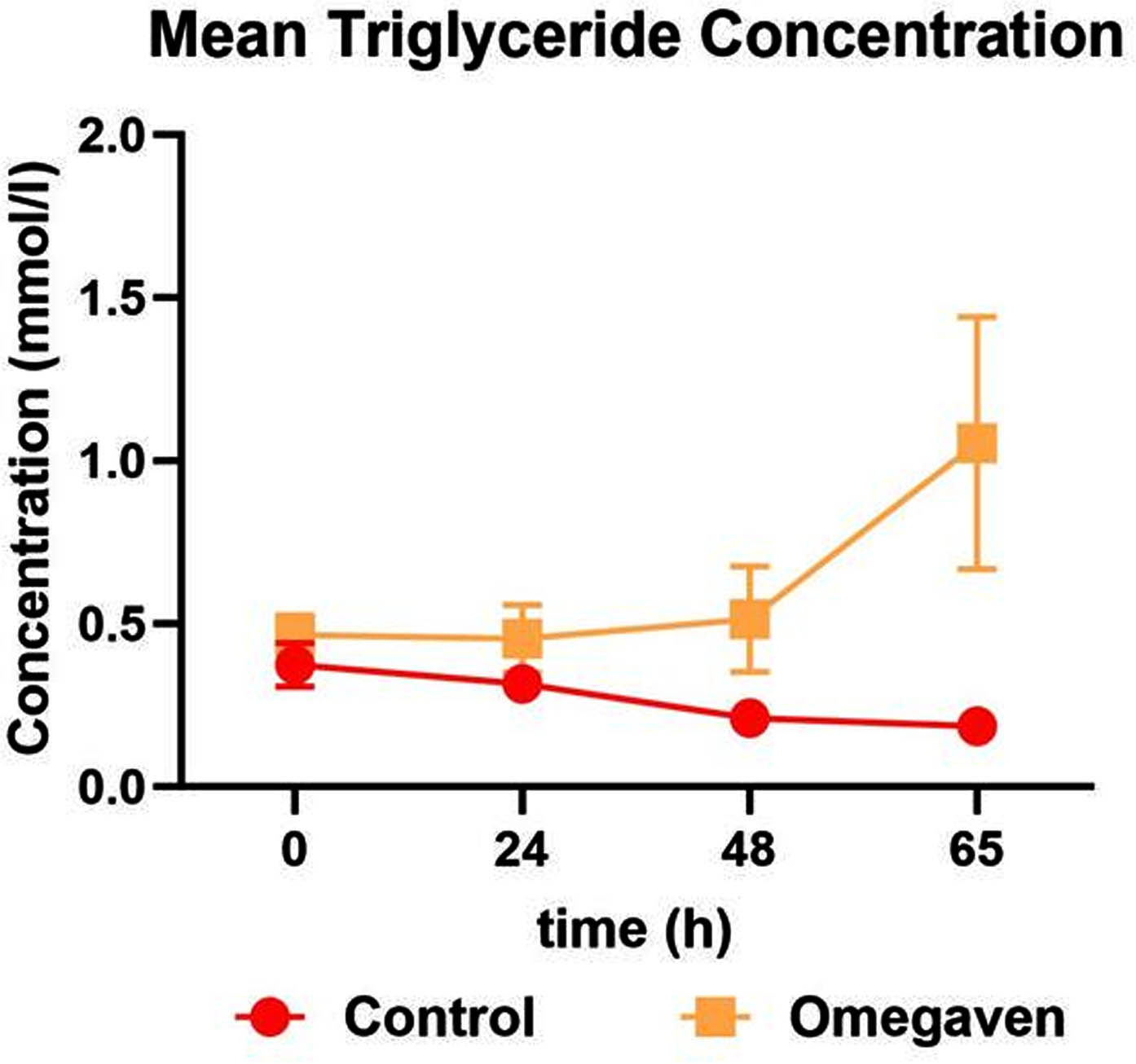
METHODOLOGY: Eleven newborn Large White Piglets (Male & Female) underwent inflammation-sensitisation with E.coli Lipopolysaccharide (2μg/kg bolus followed by 12h 1μg/kg/h infusion) and at 4h into infusion hypoxia-ischaemia (HI) by carotid artery occlusion and reduction of FiO2 to 6%. At 1h after HI, piglets were randomised to:
i. 0.9% Saline Control (n=6): 2h infusion of 8ml/kg at 1h & 4ml/kg at 24h & 48h.
ii. Omegaven (n=5): 12h infusion of 1g/kg at 1h, 24h & 48h.
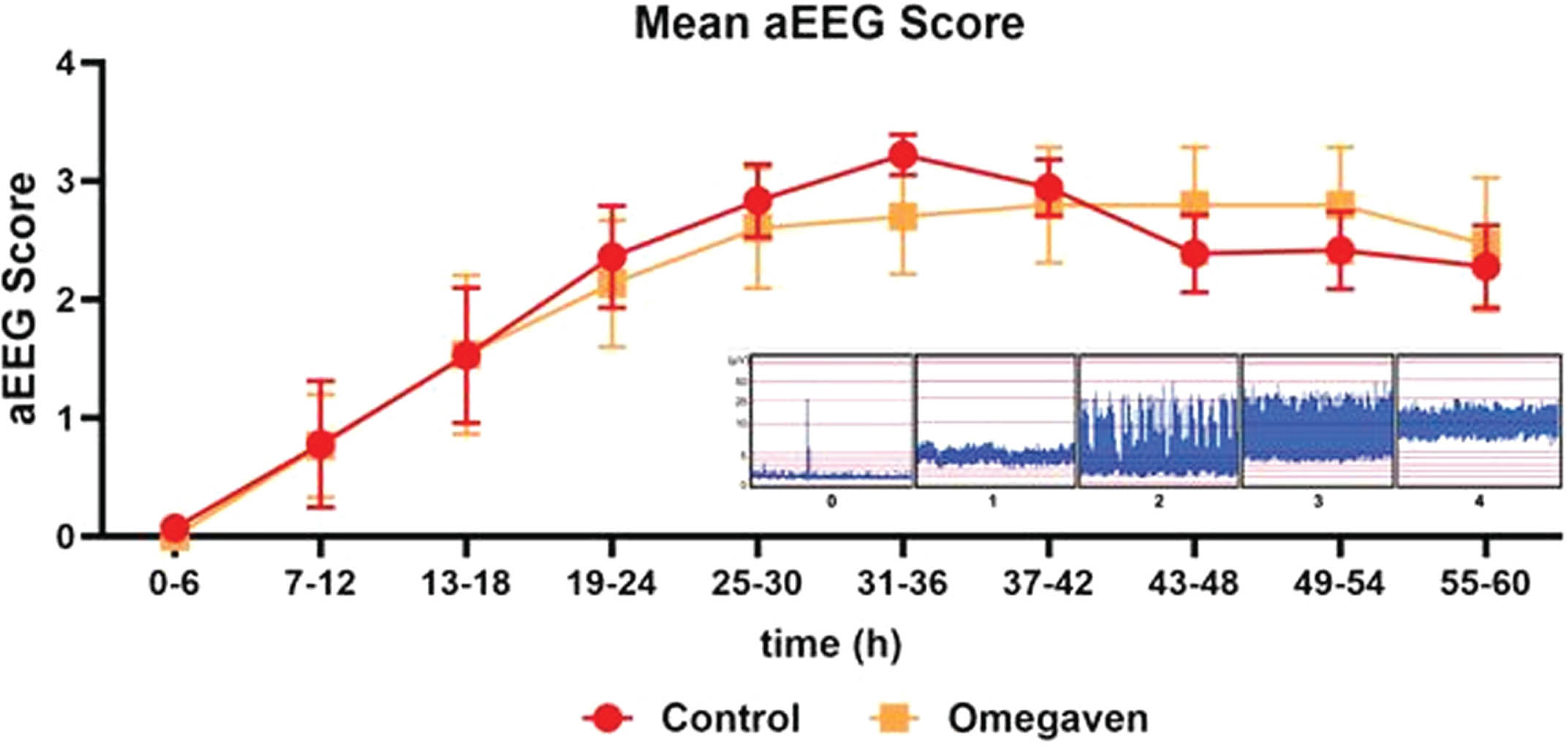
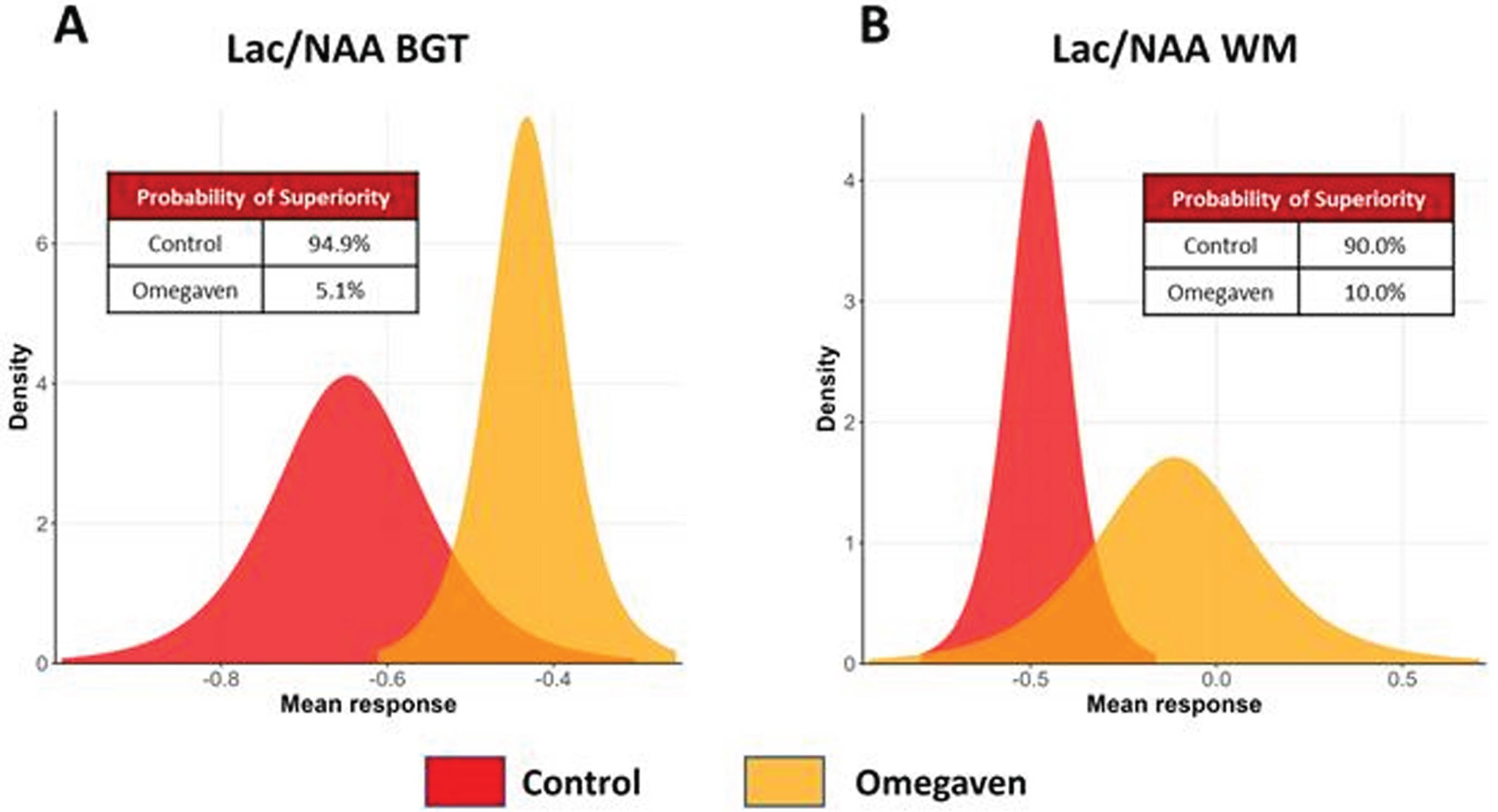
For all animals, physiological parameters and electroencephalogram (aEEG/EEG) were recorded continuously. 1H magnetic resonance spectroscopy (MRS) was acquired at 60h. Serum samples were collected serially for Liver Function Test (Royal Veterinary College Diagnostic Laboratory, UK). Piglets were euthanised at 65h and the brain dissected for immunohistochemistry. We used a Bayesian approach, with a non-informative prior. Data are presented as probability of treatment superiority (Prsup) for aEEG/EEG recovery and MRS Lactate/N-Acetylaspartate (Lac/NAA) in the basal ganglia & thalamus (BGT) and white matter (WM).
RESULTS: Insult severity was no different between groups. Significantly higher Triglyceride levels were observed in the Omegaven group at 65h (p=0.002). No significant group differences in other markers of liver function or physiological parameters were observed. There was no improvement in aEEG/EEG activity in the Omegaven group (PrSup = 63.9%). There was treatment inferiority in the Omegavan group on MRS, with increased Lac/NAA peak area ratio in both the Basal Ganglia/Thalamus (BGT) and White Matter (WM) voxels. The PrSup of Omegavan were 5.2% & 10% respectively.
CONCLUSION: Omegaven did not demonstrate protection in this model of IA-HI; The probability of treatment superiority reached the futility threshold for Lac/NAA at interim analysis. Alternative therapies are needed to improve NE outcomes.
Associations between clinical risk factors, placental pathology and MRI injury patterns in the HEAL trial
Jessica Wisnowski1, Sarah Monsell2, Claire Baldauf1, Tai-Wei Wu1, Lina Chalak3, Fernando Gonzalez4, Yi Li4, Robert McKinstry5, Yvonne Wu4, Sandra Juul2, Amit Mathur6
1Children’s Hospital Los Angeles, 2University of Washington, 3University of Texas Southwestern, 4University of California, San Francisco, 5Washington University , 6St. Louis University
BACKGROUND: Hypoxic ischemic encephalopathy (HIE) is a heterogenous disorder. The distribution of brain injury identified by MRI varies with the underlying cause and timing of the insult. Although clinical risk factors and placental pathology may offer insights into the timing or mechanism of injury, it remains to be determined whether these are associated with the pattern or acuity of brain injury observed on MRI.
METHODOLOGY: This is a posthoc analysis of data from the HEAL trial. Clinical risk factors were collected at the time of initial hospitalization. Placental pathology reports generated as part of clinical care were centrally reviewed by a placental pathologist. Placental abnormalities were characterized as acute only, chronic only, both acute and chronic, or none. MRI scans were collected prospectively using a harmonized protocol and scored centrally. Pattern of injury was characterized as central (involving basal ganglia or thalamus +/- perirolandic cortex), peripheral (bilateral watershed white matter +/- cortex), global (near total involvement of cerebrum), punctate white matter lesions (focal injury to periventricular white matter) or atypical (other). Acuity of injury was restricted to the infants who underwent MRI <=7 days, with acute brain injury defined by the presence of reduced diffusivity; subacute by MRI signal abnormalities without diffusion restriction; chronic by volume loss. We used Fisher’s exact test (categorical data), ANOVA (continuous), or a t-test (injury pattern) to determine whether there was an association between the clinical factors or placental abnormalities and MRI injury pattern or acuity and adjusted for multiple comparisons using the Bonferroni method.
RESULTS: MRI data were obtained from 473 of 500 (95%) infants enrolled in HEAL, with 414 (88%) acquired at <=7 days. 304 also had placental pathology. Among the clinical factors, 10-min APGAR <5, lower pH, higher base deficit and severe HIE were all associated with increased likelihood of the central pattern of brain injury (Table 1). Likewise, 10-min APGAR <5 and delivery room intubation were associated with higher rates of acute brain injury, while pH and base deficit showed linear relations, with the lowest pH (and largest base deficit) observed in infants with acute or acute + subacute brain injury followed by subacute (only) and then no brain injury (Table 2). Last, among placental factors, after corrections for multiple comparisons, there were no significant associations between placenta abnormalities and MRI injury pattern or acuity (Table 3).
CONCLUSION: Clinical factors reflecting metabolic and respiratory compensation were significantly associated with the central pattern and acute injury on MRI. While these factors may provide insight posthoc into the timing of injury, they are unlikely to be sufficiently discriminatory for guiding clinical management.
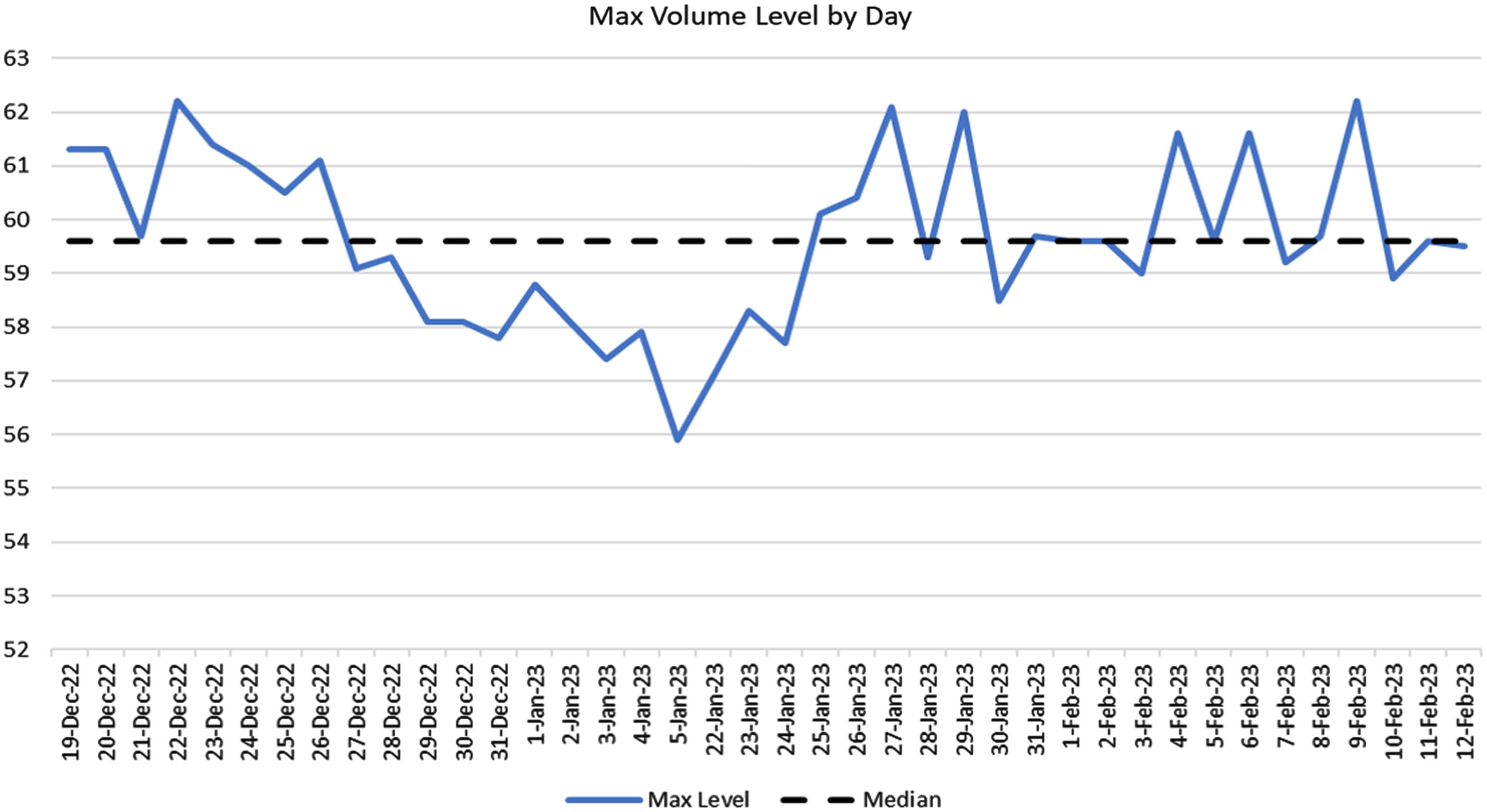
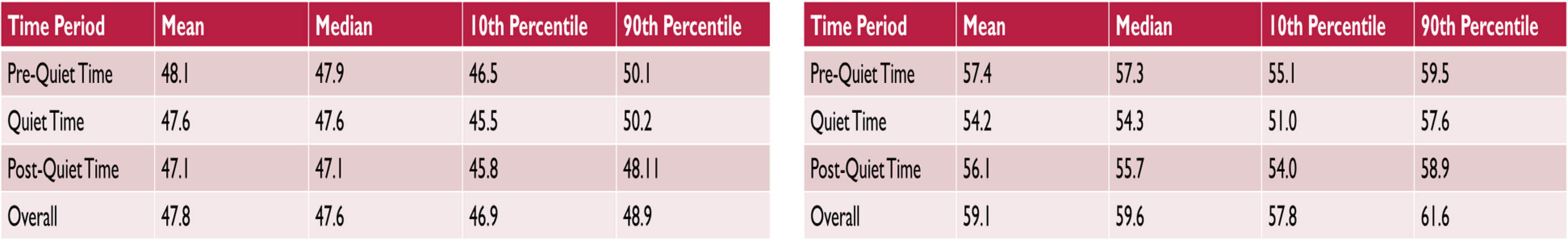
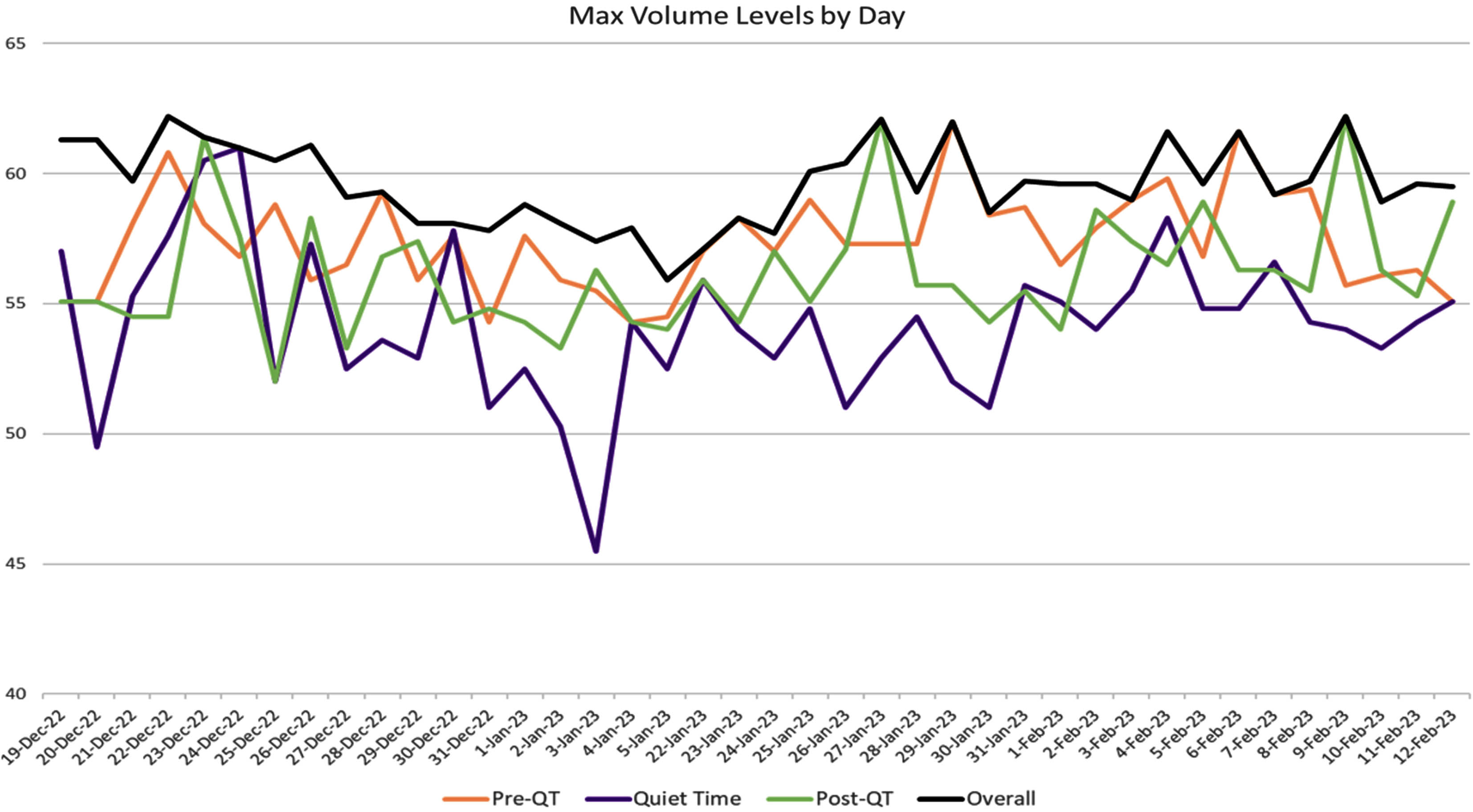
Quality improvement to trim environmental noise in neonatal intensive care unit – QUIETEN the NICU
Abhijeet Singla1
1University of Alberta, 2The Ottawa Hospital (TOH), 3The Ottawa Hospital (TOH), 4The Ottawa Hospital (TOH), 5The Ottawa Hospital (TOH), 6The Ottawa Hospital (TOH), 7The Ottawa Hospital (TOH)
BACKGROUND: Low sound levels are important for the normal neurological development of preterm infants. In addition to causing immediate physiological effects on babies’ heart rate, BP and respiratory rates, high levels of noise are known to elevate the stress levels of NICU staff and families. A previous observational study in our NICU showed mean noise levels between 61 dB to 65 dB, 90% of the time, significantly exceeding the AAP, CPS and WHO recommended sound levels of 45 dB.
OBJECTIVE: We conducted a QI project in our NICU aiming to reduce the mean ambient noise levels (LAeq avg) by 10% of the baseline over a period of 6 months.
METHODOLOGY: Baseline sound levels were collected using the SoundEar II noise meter. Root Cause analysis was conducted and multiple PDSA cycles were performed, culminating in the institution of several interventions (lowered monitor and ventilator alarm volumes, relocation of certain equipments) and the introduction of a new “Quiet Time (QT)” to the NICU. Pre-intervention surveys were distributed to healthcare workers and families. Sound levels were collected and analyzed after each PDSA.
RESULTS: Prior to the implementation, baseline LAeq avg in the NICU was 55.4 dB. With implementation of interventions in successive PDSA cycles, LAeq avg over 24 hour period decreased to 47.8 dB, while LAeq max were reduced to 59.1 dB from 82.4 dB. The most significant drop in peak levels was noted at the end of the first PDSA cycle after which the levels were stabilized. Effective interventions included the implementation of a scheduled “QT” period each day, dropping alarm volumes followed by extension of QT.
CONCLUSION: Our QI initiative successfully dropped the LAeq avg by approximately 14% of the baseline. Additional research is needed to determine effective and low-cost intervention strategies to further reduce noise in the NICU. NICU design modifications including single patient rooms, use of sound absorbing materials can significantly reduce noise. Consideration should also be given to automated remote sound level monitoring using digital and wireless sensors.
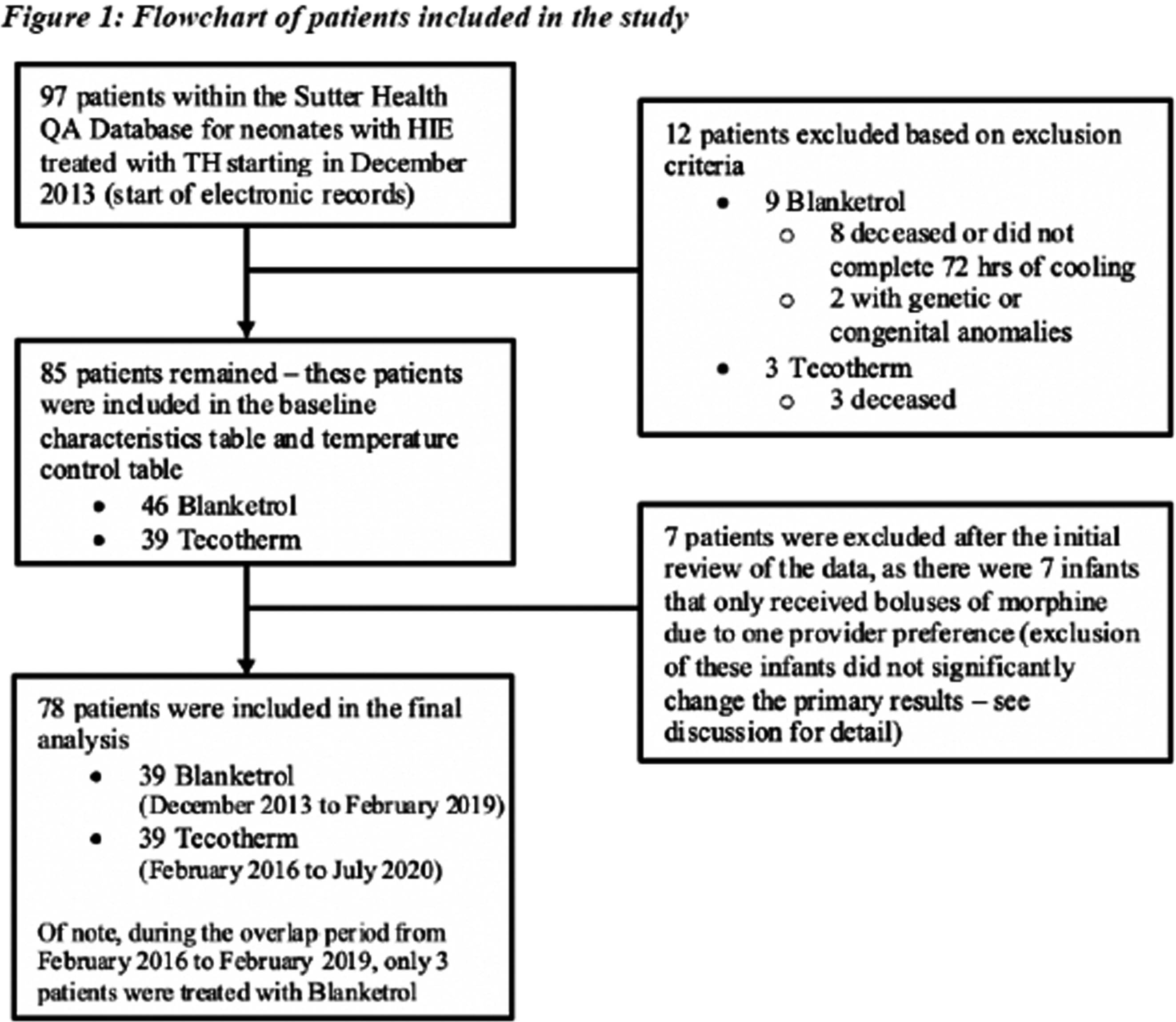
Morphine use in HIE neonates treated with therapeutic hypothermia: A comparison between blanketrol versus tecotherm
Camille Bloom1, Maggie Kucera, Nancy Chorne, Courtney Wusthoff, Katherine Mackenzie, Jennifer O’Malley
1Stanford University
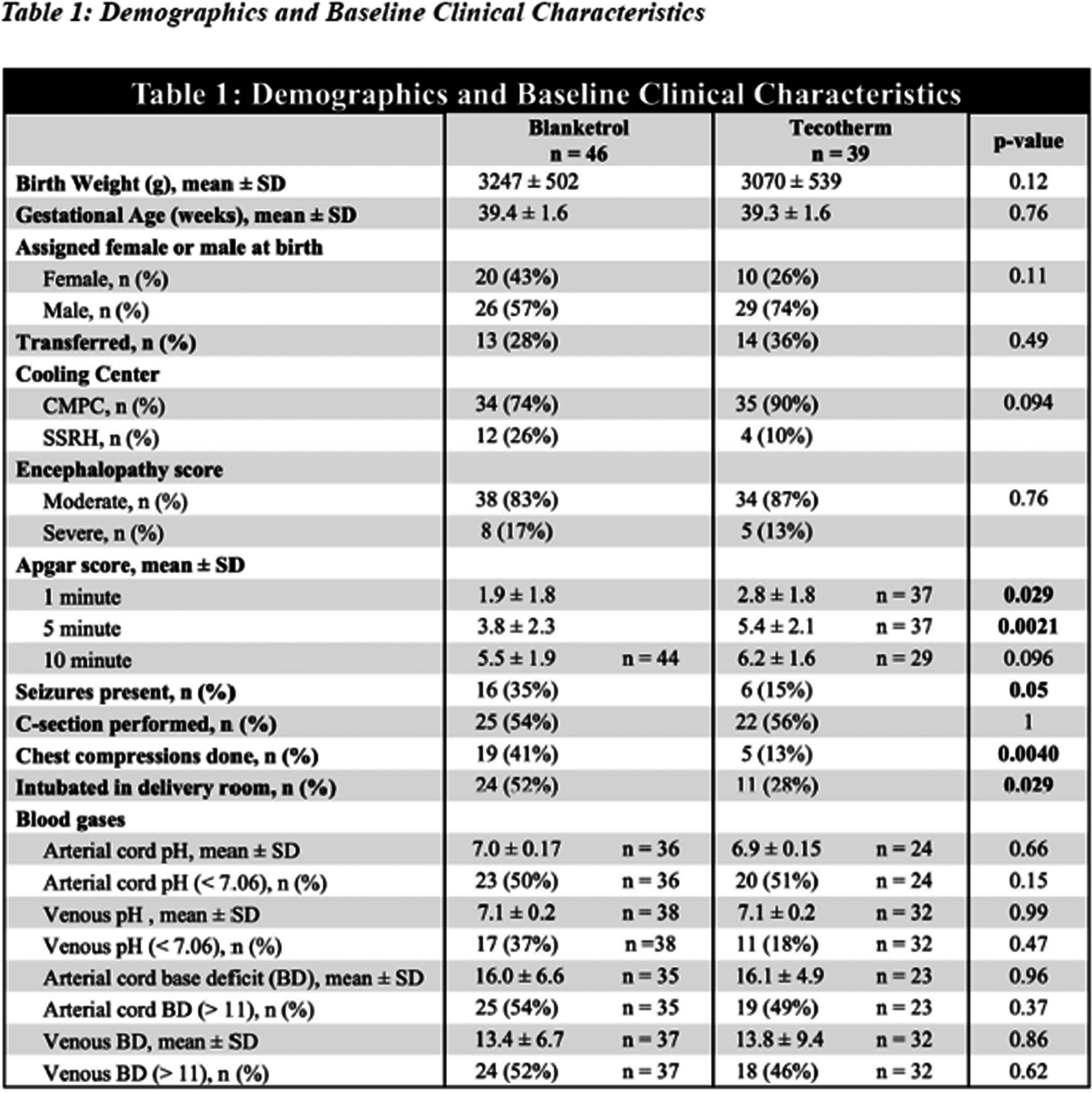
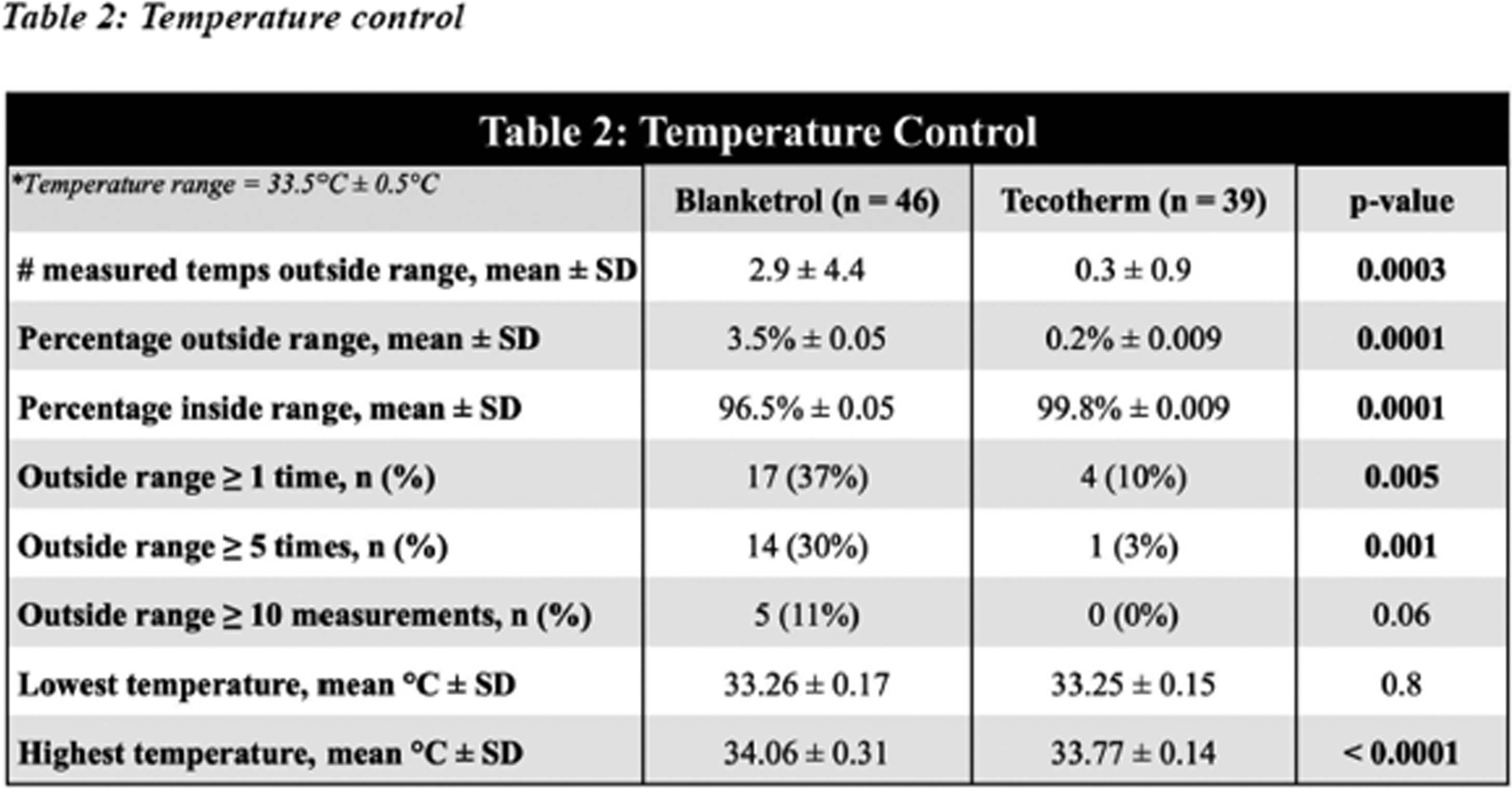
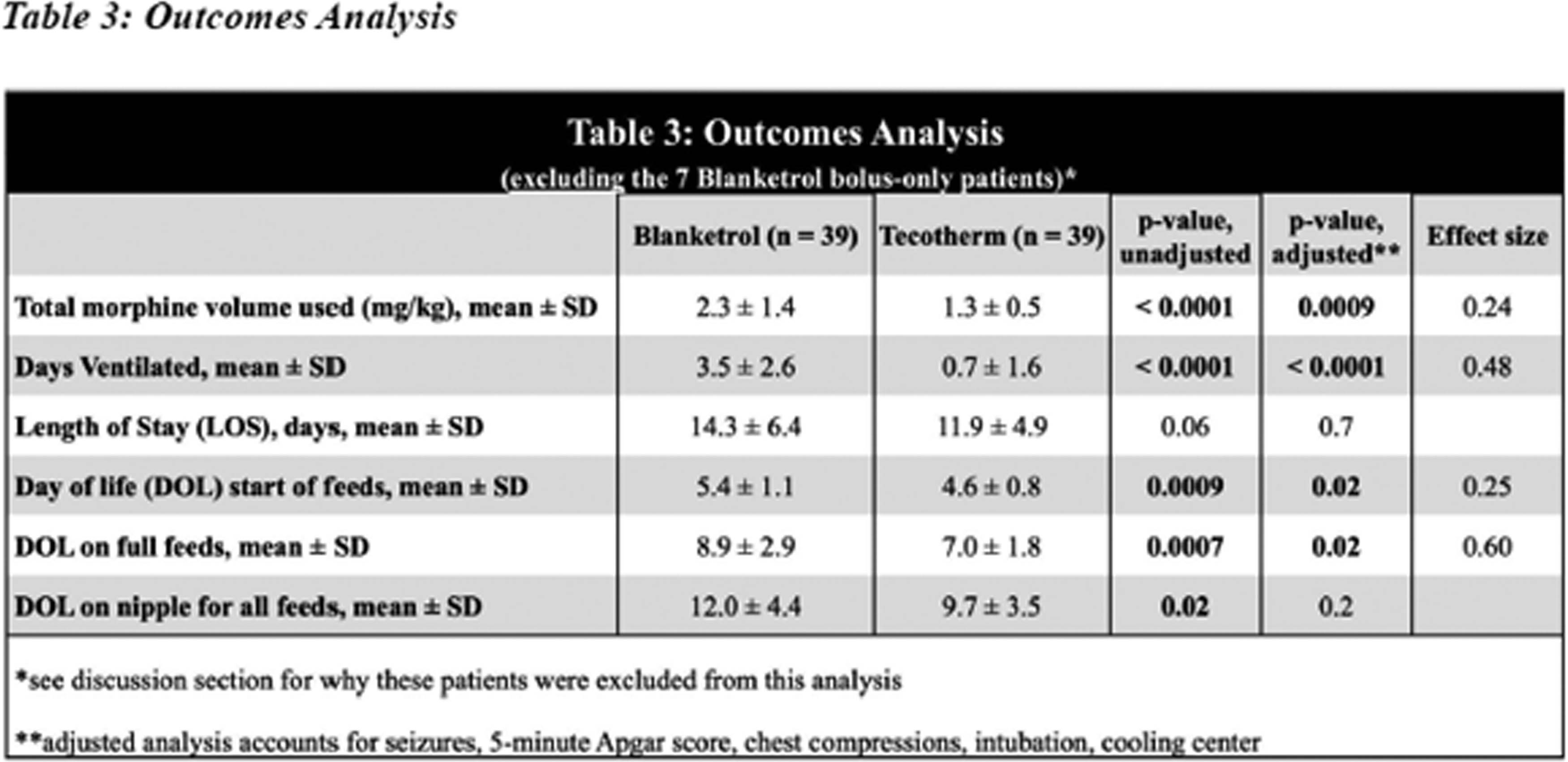
OBJECTIVE: This study compares total morphine use associated with two comparable cooling blanket devices for neonates undergoing therapeutic hypothermia (TH) for hypoxic-ischemic encephalopathy (HIE). Several Bay Area Sutter Health NICUs transitioned from use of Blanketrol to Tecotherm devices. The study compares the total volume of morphine use and temperature control in neonates who were cooled with either device.
METHODOLOGY: De-identified data was utilized from Sutter Health neonatal therapeutic hypothermia Qualitative Analysis (QA) database extracted via retrospective chart review of all neonates undergoing therapeutic hypothermia between 12/2013- 07/2020 in three Sutter Health Bay Area hospitals. Initially, 97 patients met inclusion criteria (neonatal encephalopathy and initiation of cooling therapy before 6 hours of life). After applying exclusion criteria (deceased, not completing 72 hours of cooling, genetic or congenital anomaly), 8 babies from the Blanketrol group were excluded for not completing 72 hours of cooling or deceased, and 2 for genetic anomalies, 3 babies from the Tecotherm group were excluded due to early demise. 85 infants remained in the study: Blanketrol (n = 46, 12/ 2013 to 2/ 2019) and Tecotherm (n = 39, 2/ 2016 to 7/ 2020). Demographic information did not differ between groups. Significant markers of illness severity were adjusted for in outcome analysis and included Sarnat score, seizures, c-section delivery, Apgar scores, chest compressions, intubation in delivery room, and cord blood gases. The primary outcome measure was the total morphine use (mg/kg). Secondary outcomes include length of stay, days on mechanical ventilation, highest serum creatine, feeding outcomes, and temperature accuracy. Statistical analysis was performed using R Studio. ANOVA to test the mean difference between the cohorts, Fishers’ exact test to compare the difference between cohorts. Multiple linear regression for potential confounding effects.
RESULTS: When compared to the Blanketrol cohort (n=46), the Tecotherm cohort (n=39) had more tightly regulated temperature control (p < 0.0001), and lower total volume of morphine used (Tecotherm 1.3 ± 0.5 mg/kg vs Blanketrol: 2.3 ± 1.4 mg/kg; p = 0.0009). The tecotherm cohort also outperformed Blanketrol in secondary outcomes including lower number of days ventilated (0.7 ± 1.6 (Tecotherm) vs. 3.5 ± 2.6 (Blanketrol); p <0.0001), faster initiation of feeding (T vs B; p = 0.02), and faster time to full feeds (T vs B; p = 0.02). There was no apparent statistically significant impact of device use on length of stay.
CONCLUSION: This study demonstrates significant differences in total morphine use and temperature regulation associated with two different cooling devices. While long-term outcomes are outside the scope of his study; the association of lower opiate exposure with tighter temperature control are clinically significant to short-term measures including decreased time on mechanical ventilation, earlier initiation of feeding, and faster time to full feeds.
Factors influencing feeding outcomes following neonatal hypoxic ischaemic encephalopathy: A mixed methods systematic review
Sarah Edney1, Anna Basu1, Anne Breaks2, Nadia Leake1, Judith Rankin1, Farag Shuweihdi3, Mari Viviers4, Kirstin Webster5, Lindsay Pennington1
1Newcastle University, 2Guy’s and St Thomas’ NHS Foundation Trust, 3University of Leeds, 4Imperial College Healthcare NHS Trust, 5University of Leicester
BACKGROUND AND OBJECTIVE: Hypoxic ischaemic encephalopathy (HIE) is a brain injury resulting from insufficient oxygenation during the perinatal period and is the most common form of brain injury in term-born neonates. Although there is a known association between HIE and feeding and swallowing disorders, at present most neonatal feeding interventions target healthy preterm infants and there are no interventions designed specifically for HIE. To better understand HIE-related feeding disorders and inform intervention development for this population, our systematic review aims to answer the question: ‘what factors influence feeding outcomes in infants and young children following neonatal HIE?’.
METHODS: JBI methods were used for this mixed methods systematic review[1, 2]. Eleven databases were searched first in November 2022 and again in July 2023. Pre-specified inclusion and exclusion criteria were used during screening (e.g. not born before 34 weeks gestational age). After de-duplication, 2779 titles and abstracts and 422 full texts were screened. All titles/abstracts were double-screened and 20% of full texts were double-screened. 138 relevant review papers were also searched, and the reference lists and subsequent citations for all included papers were screened for additional papers. Authors were contacted for clarification of details where necessary. Full methods for this systematic review are registered on PROSPERO (CRD42023375506).
RESULTS: 81 papers met the inclusion criteria. 44 papers included factors influencing enteral feeding progression and gastrointestinal complications, 62 included factors influencing oral feeding, and 10 included factors influencing breastfeeding and lactation. This presentation will describe identified factors influencing feeding outcomes, with a focus on those involving actions by staff and caregivers that are amenable to change (e.g. enteral feeding during therapeutic hypothermia, opioid exposure, neuroprotective drugs and therapies), thereby informing intervention delivery and development. No interventions targeting feeding/swallowing function or breastfeeding/lactation were identified in this review. Only one study used a standardised feeding assessment. No qualitative or mixed methods studies were found and no studies explored outcomes from the perspective of the child or family. Meta-analysis is planned for suitable outcomes e.g. the effect of therapeutic hypothermia on tube feed requirements at discharge.
CONCLUSION: High quality studies are urgently needed to improve our understanding of the factors influencing HIE-related feeding outcomes and inform the development of HIE-specific feeding interventions. Findings from this systematic review will shape a mixed methods doctoral project that seeks to generate additional knowledge for HIE-specific feeding intervention development.
BIBLIOGRAPHY:
1. Lizarondo, L., et al., Chapter 8: Mixed methods systematic reviews, in JBI Manual for Evidence Synthesis., E. Aromataris and Z. Munn, Editors. 2020, JBI.
2. JBI. 2023; Available from: https://jbi.global/.
Neonatal encephalopathy examination and interrater agreement among healthcare practitioners
Katie Hannon1, Sriya Roychaudhuri2, Aisling Garvey3,4, Brian H. Walsh3,4, Sara Cherkerzian1,5, Terrie Inder1,5,6, Mohamed El-Dib1,5
1Brigham And Women’s Hospital, 2University of British Columbia Faculty of Medicine, 3INFANT Centre, University College Cork, 4Cork University Maternity Hospital, 5Harvard Medical School, 6Children’s Hospital of Orange County
BACKGROUND: Therapeutic hypothermia (TH) is the standard of care for hypoxic-ischemic encephalopathy(1). Its implementation relies on clinically assessing the degree of neonatal encephalopathy (NE) in infants with relevant perinatal risk factors. While several variations of the assessment initially reported by Sarnat and Sarnat(2) are in practice, their interrater agreement has not been assessed.
OBJECTIVE: To assess the coherence of the NE assessment by healthcare practitioners with varying levels of experience.
METHODOLOGY: Infants born >34 weeks gestational age and assessed by a trained physician for NE in a single level three NICU, were video recorded ensuring confidentiality. The total score was calculated as the sum of ordinal scores (3 levels) across 8 subscales. Reference scores were determined by the consensus opinion of the research team. Thereafter, two de-identified videos, one of mild and another of moderate NE, were circulated via virtual platforms along with a short clinical vignette and a scoring survey over multiple centers in America and Ireland. The participants could opt to watch a 25-minute teaching video (by ME,TI) and score again. The degree of consistency was analyzed by comparing the difference between the measured total score and the reference, by NE status (mild v moderate) using independent-sample Mann-Whitney U test, and by experience, using Independent-Samples Kruskal-Wallis Test.
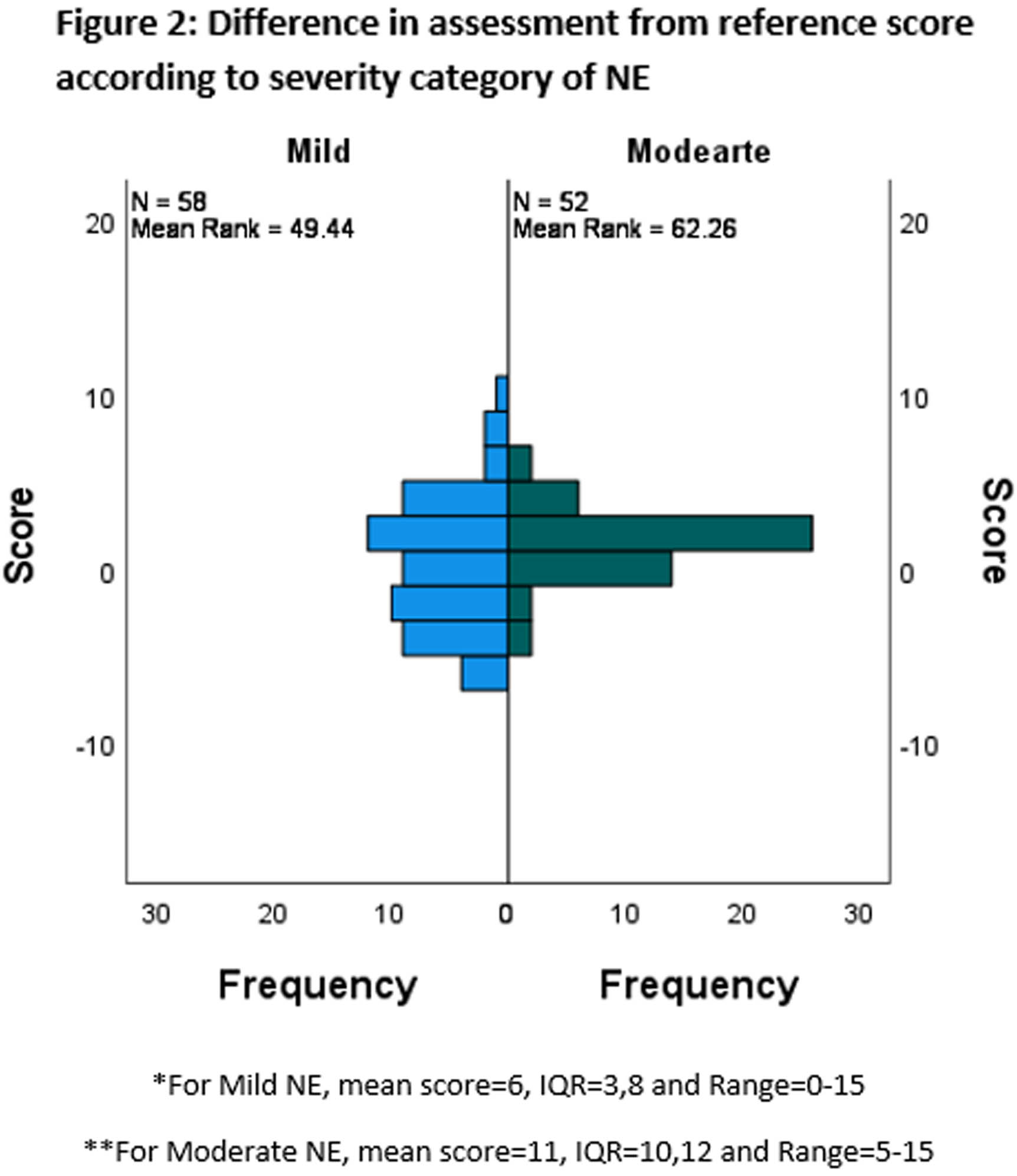
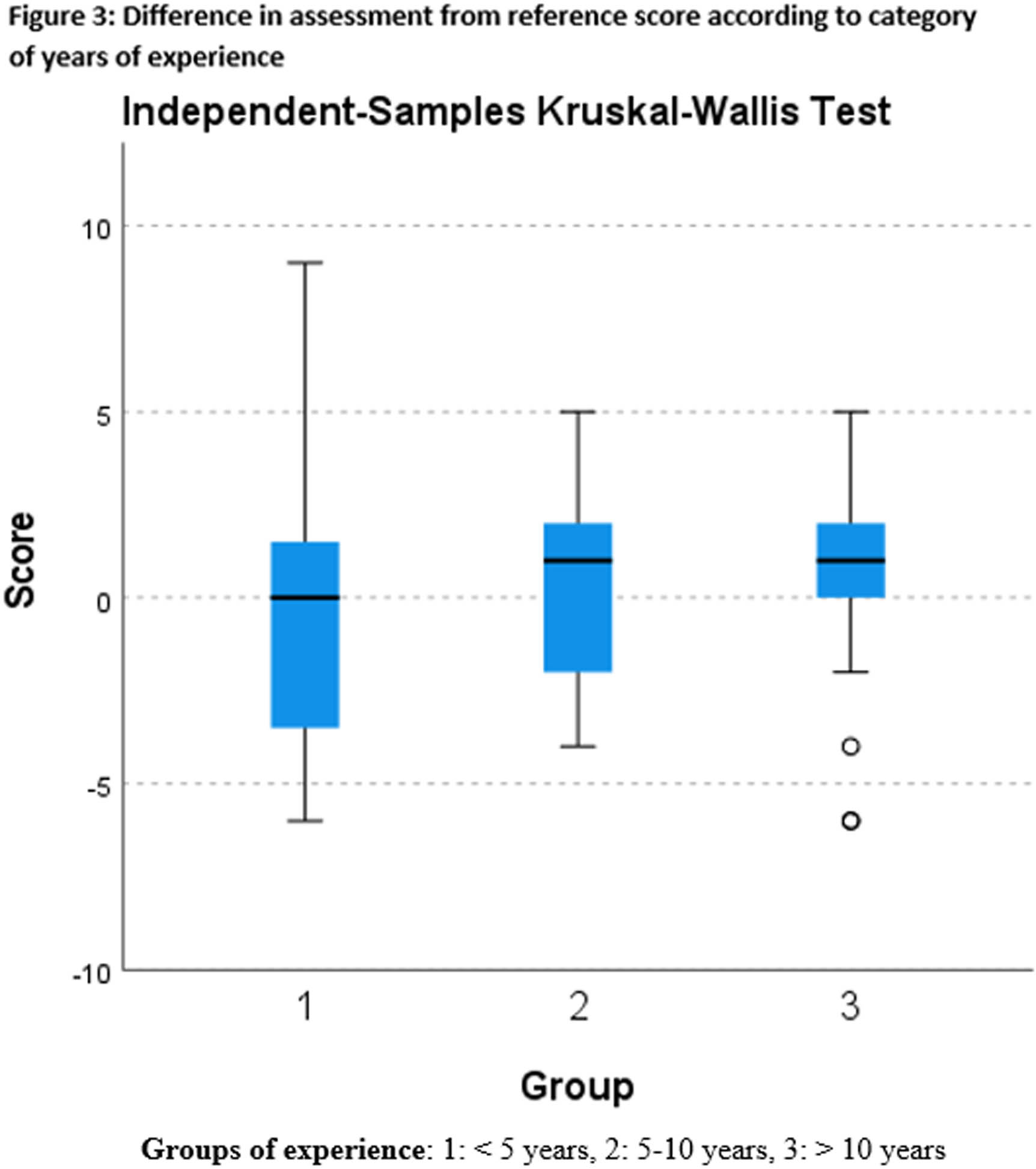
RESULTS: Of the 110 survey responses received, 101 (91.8%) were physicians and 93 (84.5%) were from level 3 or 4 units. 37 (33.6%) had >10 years of experience in their current role. There was wide variation in scores and tendency to overscore (Figure 1). Level of consciousness, spontaneous activity and neonatal reflexes had less agreement as opposed to tone and autonomic functions. The divergence from the reference score was significantly greater for mild compared with moderate NE (p=0.034)(Figure 2). While the difference did not significantly change by experience category (p = NS), the variability of the scores decreased with greater experience (Figure 3). 73 watched the teaching and scored again. Assessment of NE post-teaching showed similar results with no significant improvement in interrater agreement.
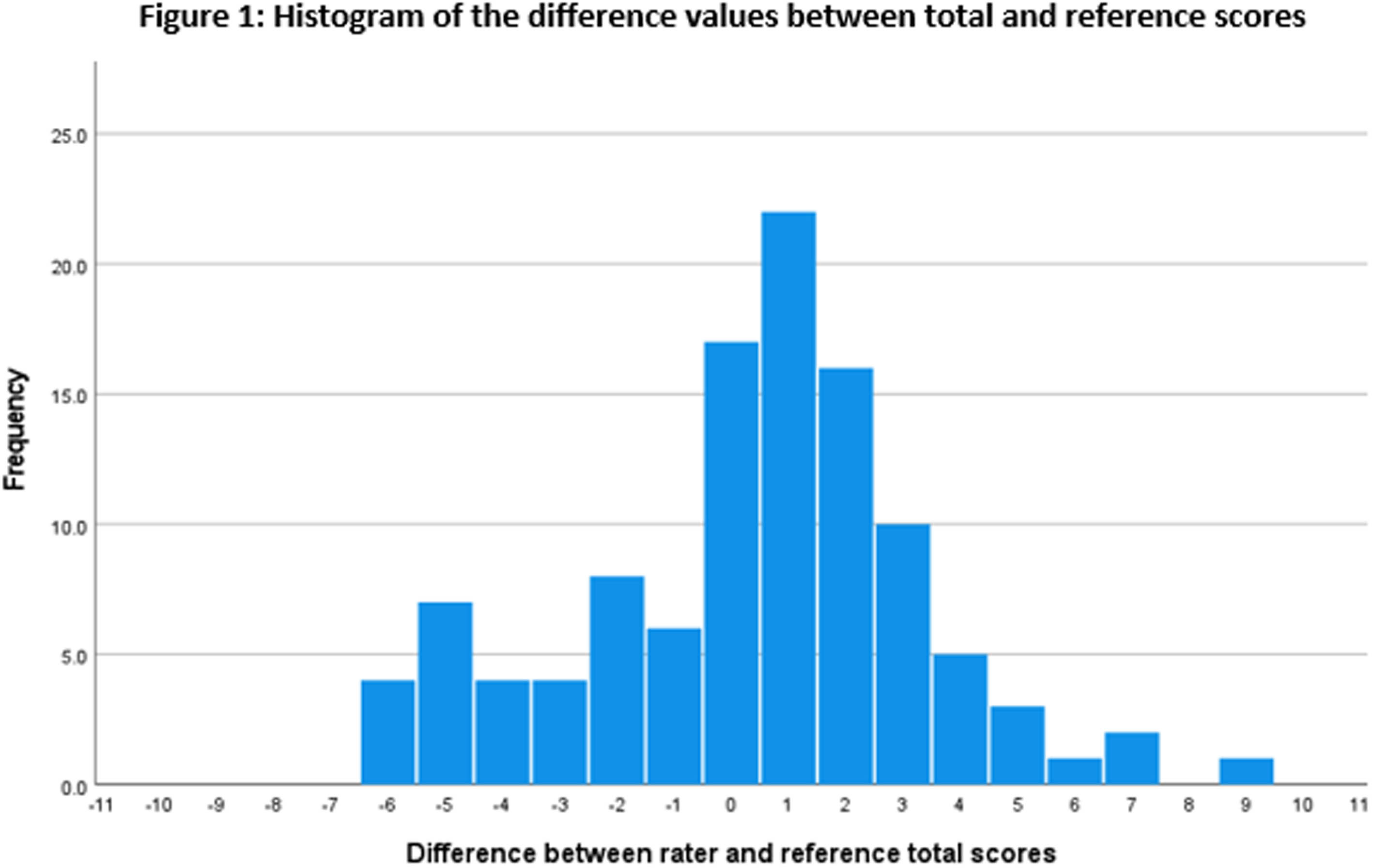
CONCLUSION: Assessment of NE varies among practitioners, especially in milder cases. A single teaching session may not suffice in increasing the skills and continuing education with active feedback and case-based teaching should be considered. Concomitant observation by multiple health professionals with expertise may be useful in confounding cases and deciding management in infants with NE.
BIBLIOGRAPHY:
1. COMMITTEE ON FETUS AND NEWBORN. Hypothermia and Neonatal Encephalopathy. Pediatrics. 2014 Jun 1;133(6):1146–50.
2. Sarnat HB, Sarnat MS. Neonatal encephalopathy following fetal distress: a clinical and electroencephalographic study. Arch Neurol [Internet]. 1976;33. Available from: https://doi.org/10.1001/archneur.1976.00500100030012




