Proceedings of the 14th International Newborn Brain Conference: Long-term outcome studies, developmental care, palliative care, ethical dilemmas, and challenging clinical scenarios in neonatal neurology
Primary care developmental screening of term and late preterm nicu graduates
Herrera S1, Herrera S, Cabacungan E, Cohen S
1Medical College Of Wisconsin, Milwaukee, United States
BACKGROUND: Infants ≥ 34 weeks gestation are at relatively low-risk for developmental delay and do not qualify for high-risk infant follow-up based on prematurity alone. However, with prolonged neonatal intensive care unit (NICU) hospitalization and life-sustaining interventions, there is an increased risk for neurodevelopmental impairment in this population. Currently, there is no standardized risk stratification to predict which infants ≥ 34 weeks gestation are at highest risk for delays. We aim to compare key clinical characteristics of infants with normal vs. abnormal developmental screening in the primary care setting. Our secondary aim is to identify which infants in this cohort would benefit most from early developmental intervention. We hypothesize that gestational age alone is not predictive of normal development.
METHODS: We performed a retrospective cohort study of infants born ≥ 34 weeks gestation between 1/2013-12/2015, admitted to the Children’s Wisconsin (CW) NICU, and followed by a Wisconsin-based primary care provider for routine developmental screening at 3-6 years of age. Developmental screening results reported either in the primary care visit note or any CW subspecialty clinic note were included for analysis. Screening was considered abnormal if developmental concerns in cognition, motor, language, and/or social domains were documented. In addition, neonatal diagnoses, procedures, and clinical characteristics were extracted. Mann Whitney, Chi-Square, and Fisher’s exact tests were used to compare patients with normal vs. abnormal preschool age development.
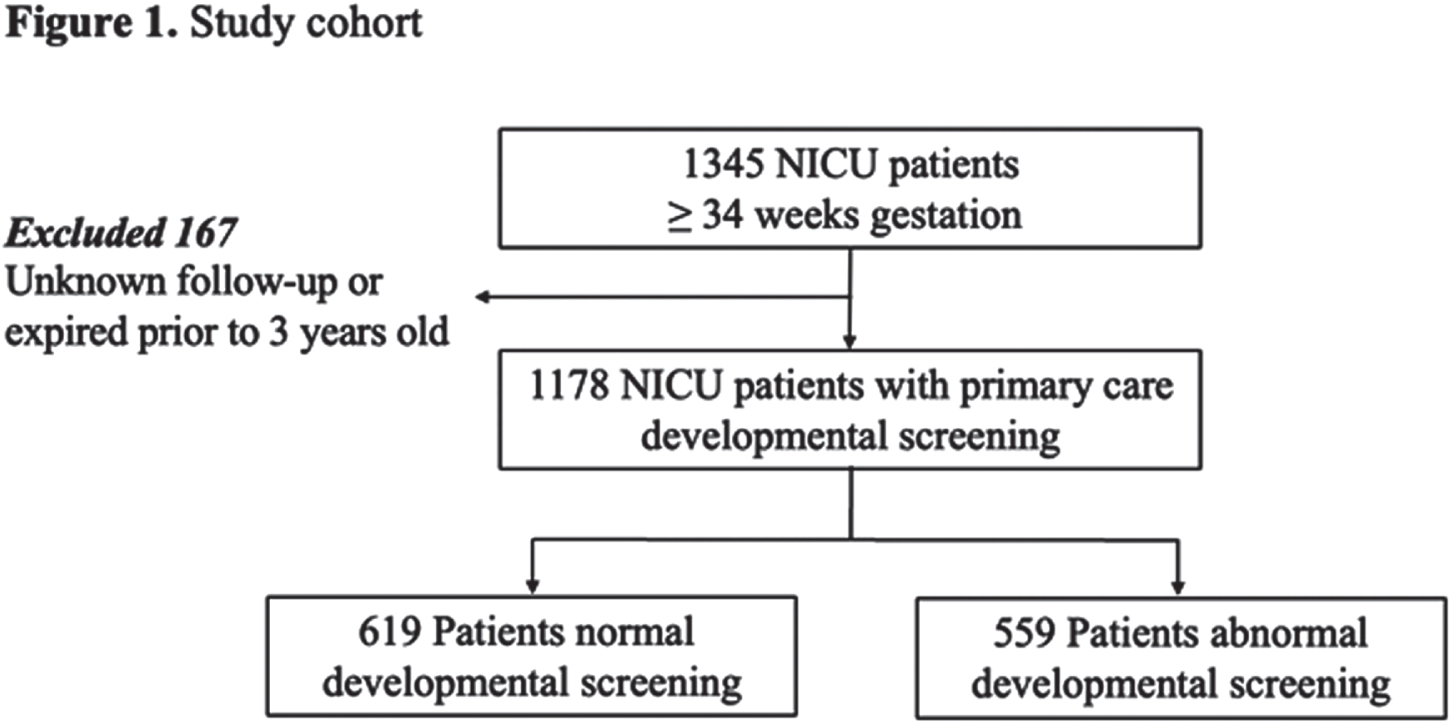
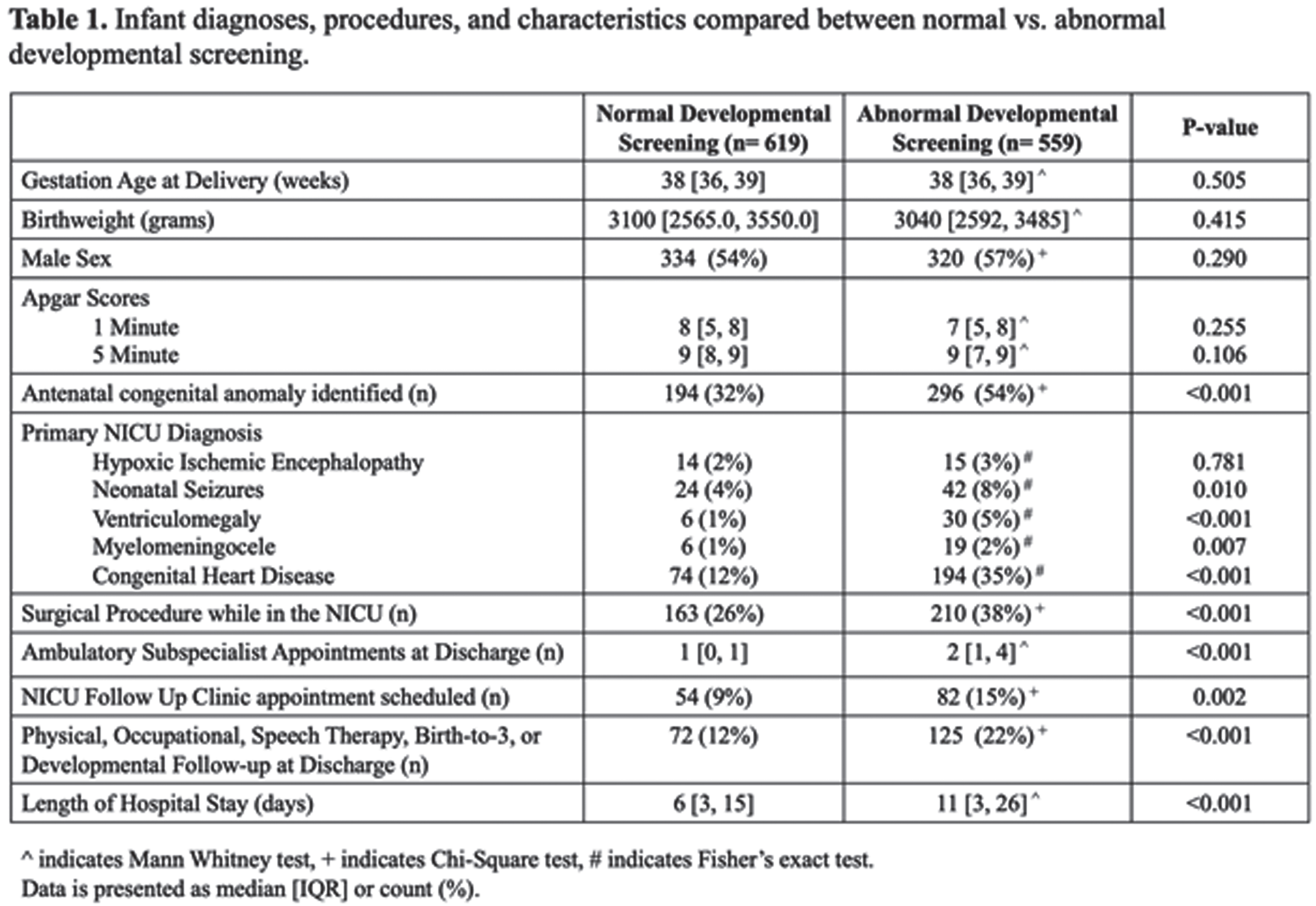
RESULTS: We screened 1345 NICU infant charts, and 88% received primary care developmental screening (Figure 1). We identified 559 (47%) infants with abnormal developmental screening results. Infants with abnormal developmental screens were more likely to have an antenatal congenital anomaly (32% vs. 54%, p<0.001), NICU surgical procedure (26% vs. 38%, p<0.001), prolonged length of NICU stay (6 days vs. 11 days, p<0.001), or more than one subspecialist appointment after discharge (1 vs. 2, p<0.001) (Table 1). The most common diagnoses in patients with abnormal development were congenital heart disease and ventriculomegaly. At discharge, only 15% of infants with abnormal developmental screens were referred to NICU follow-up clinic and only 22% were referred to physical, occupational, speech, or NICU follow-up services.
CONCLUSION: NICU characteristics negatively impact developmental screening in a presumed low-risk population. These results can be used to revise current NICU follow-up inclusion criteria and improve developmental outcomes through early intervention services.
Parental holding of infants with Hypoxic Ischemic Encephalopathy (HIE) during therapeutic hypothermia
Glennon C1
1LPCH At Stanford, Palo Alto, United States
BACKGROUND AND PURPOSE: Therapeutic hypothermia (TH) is the only treatment shown to reduce mortality and disability in affected infants and improves neurologic outcome for term and near-term infants with moderate to severe HIE. Historically, parents have not held their infants during TH for a variety of reasons including the potential to warm the infant, extra efforts required to securely transfer infant from the bed to the parent, and due to safety concerns related to possible equipment dislodgement. Simultaneously, parents may feel a loss of normalcy and have an impaired ability to bond with their infant. The purpose of this study was to determine the feasibility of parental holding during TH by monitoring vital sign stability and to assess parental attitudes around holding.
MATERIALS OR METHODOLOGIES: From 2018 until 2021 we used an algorithm to determine holding eligibility of infants. Written informed parental consent was obtained for all patients. Parents of enrolled subjects were encouraged to commit a minimum of 1 consecutive hour of holding. During the maintenance phase of TH heart rate, core temperature, oxygen saturations and regional saturations (cerebral) were recorded for one hour before holding, during the holding experience, and for one hour after holding. Synchronized data were collected from the Philips bedside monitor, INVOS NIRS monitor, and Blanketrol III using the Moberg Component Neuromonitoring System (CNS). Infants remained on the cooling blanket atop of a pillow in the parent’s lap during holding. After the holding event(s) a parent survey was administered, and responses were deidentified to encourage candid feedback.
RESULTS: We enrolled 24 infants in our study and recorded 40 holding events during the maintenance phase of TH. Eleven infants were held more than once. Five infants had seizures during TH but none while being held. There were no adverse events and no significant vital sign disturbances associated with holding during TH. While 11% of parents reported anxiety about potentially adversely affecting their infants during holding, 88% of respondents felt it was very important to hold their infant at least once per day/visit if deemed medically safe to do so. Furthermore, 86% reported holding their infant significantly improved their emotional and/or physical well-being. 100% of respondents indicated that the holding experience had a significant positive impact or some positive effect on their infant. 8% of mothers even reported an associated increase in milk production.
CONCLUSIONS/IMPACT: This study found holding infants during therapeutic hypothermia can be done safely for infants with HIE and can provide feelings of emotional well-being to NICU parents.
REFERENCES
[1] Craig, Alexa K. et al. Maternal Holding During Therapeutic Hypothermia for Infants with Neonatal Encephalopathy is Feasible. Acta Paediatrica. 2019; 108 (9):1597-1602.
Neonatal imitation of late preterm infants and its prognostic value
Simsir M1, Engur D2, Yilmaz C1, Zengi I3, Gencpinar P4, Soykan A5, Olgac Dündar N4
1Department of Pediatrics, University Of Health Sciences, Izmir, Izmir, Türkiye, 2Department of Neonatology, University Of Health Sciences, Izmir, Izmir, Türkiye, 3Department of Public Health, Izmir Katip Çelebi University, Izmir, Türkiye, 4Department of Pediatric Neurology, Izmir Katip Çelebi University, Izmir, Türkiye, 5Egem Rehabilitation Center, Izmir, Turkiye
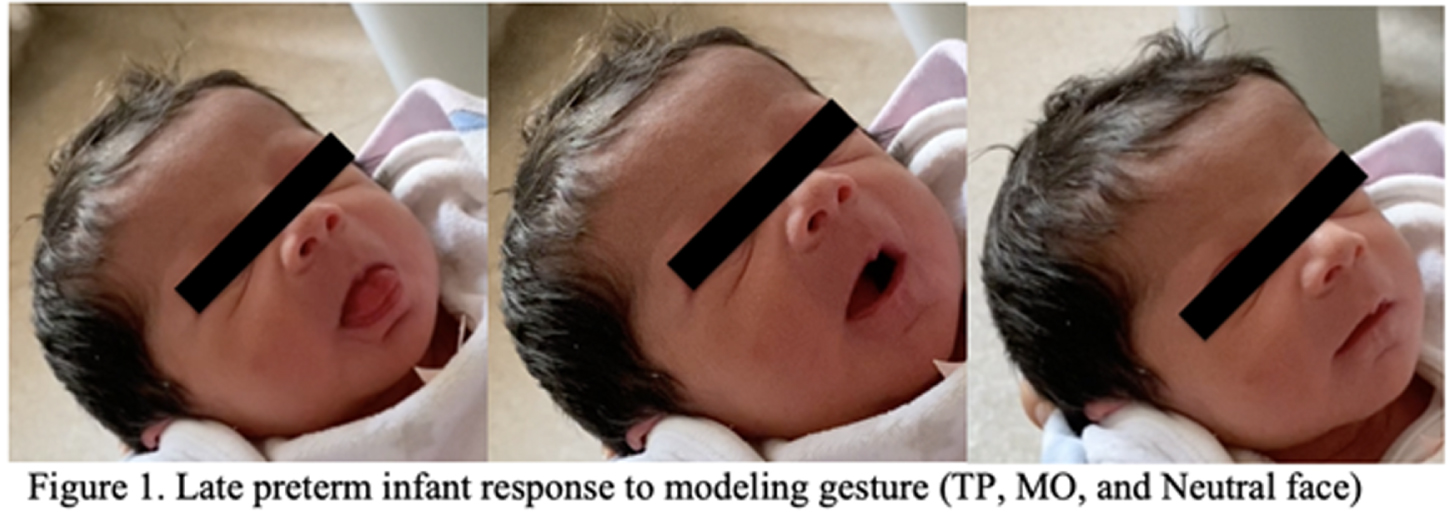
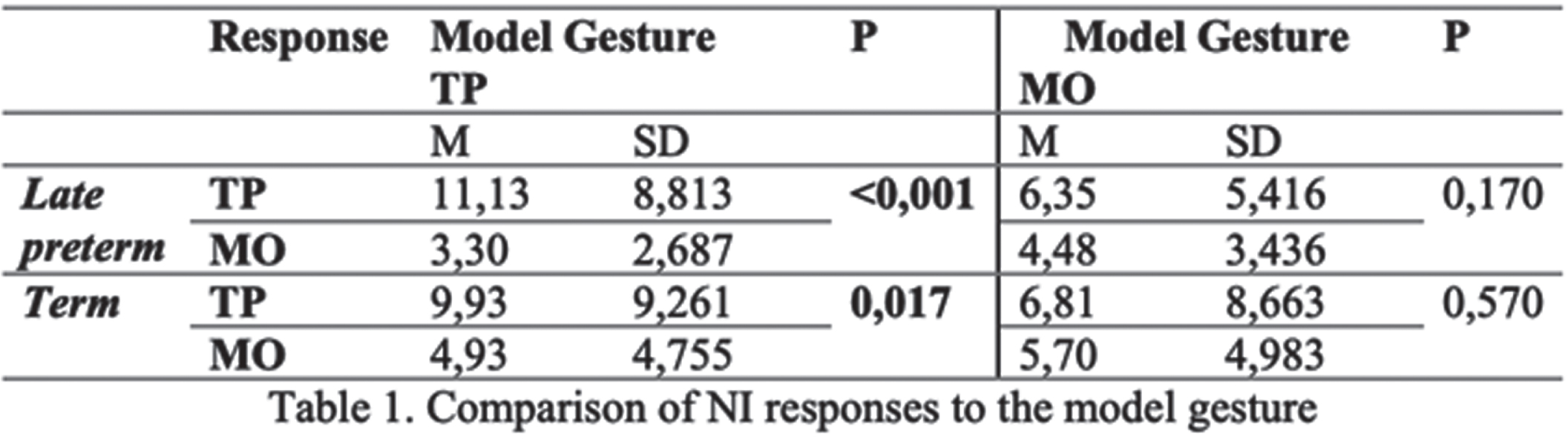
Newborn infants can imitate the modeled gesture even within the first hours of life following birth. This mimicry mechanism is called neonatal imitation (NI). Imitation of an action that was not learned indicates that newborns can see and demonstrate proprioception and perceptual-motor coordination and match it with the model. In this study, we investigated the presence of NI in healthy late-preterm newborns, compared their NI responses with healthy term infants, and explored its prognostic value with follow-up visits. 36 term and 36 late preterm infants were included. NI responses were tested within 12-72 hours after birth. Babies with congenital anomalies and infants hospitalized and lost interest during the study period were excluded from the study. The test was performed in a quiet, adequately lit environment when the infants were awake, fed, and calm. The model showed gestures to the infants for 20 seconds, then stood with a neutral face for 20 seconds. The test continued for 4 minutes for each gesture. A researcher scored the video recordings according to the criteria specified in the literature3. 23 late preterm and 27 term infants were tested for two facial gestures: Mouth opening (MO) and tongue protrusion (TP) (Figure 1). Infants were followed-up until postmenstrual 51 weeks and evaluated twice at postmenstrual 45th and 51st weeks for Prechtl’s General Movements Assessment. Both groups yielded a significantly higher number of TP responses following the TP gesture of the model (p<0.001, p=0.017). (Table 1). The TP responses of late preterm and term infants were 19(82%) and 20 (74%), respectively, whereas only 9 out of 23 (39%) preterm infants and 15 out of 27 (55%) term infants displayed NI responses for MO. In the follow-up, one of the preterm infants displayed poor repertoire movement, and one of the term infants had cramp synchronized pattern general movements; nevertheless, both had a positive response for TP in the neonatal period. In conclusion, late preterm displayed similar NI responses compared to term newborns. NI scores did not show a correlation with GM assessments in our study. The differences in NI and its prognostic significance can be better understood through longitudinal follow-up and further studies in larger patient groups.
REFERENCES
[1] Heimann M, Nelson Ke, Schaller J. Neonatal İmitation Of Tongue Protrusion And Mouth Opening: Methodological Aspects And Evidence Of Early İndividual Differences. Scand J Psychol. 1989;30(2):90-101. Doi:10.1111/J.1467-9450.1989.Tb01072.X
[2] Einspieler C, Prechtl Hfr. Prechtl’s Assessment Of General Movements: A Diagnostic Tool For The Functional Assessment Of The Young Nervous System. Ment Retard Dev Disabil Res Rev. 2005;11(1):61-67. Doi:10.1002/Mrdd.20051
[3] Meltzoff An, Moore Mk. Imitation İn Newborn Infants: Exploring The Range Of Gestures Imitated And The Underlying Mechanisms. Dev Psychol. 1989;25(6):954-962. Doi:10.1037/0012-1649.25.6.954
Challenges in recruitment for an acute neonatal seizure trial
Roth E1, Lowe C1, Alkhadem Z1, Li R2, Chang T1,3, Anwar T1, Tsuchida T1
1Department of Neurology, Children’s National Hospital, George Washington University School of Medicine & Health Sciences, 111 Michigan Ave , United States, 2Vanderbilt University School of Medicine, Nashville, United States, 3In Memory of the Late Dr. Taeun Chang (197-2022), we acknowledge her substantial contribution to the conception and design of this work
BACKGROUND: Newborns have one of highest rates of seizures across childhood, which can put them at risk for epilepsy and neurodevelopmental disabilities later in life.1 Despite this, neonatal seizure treatment trials are rarely conducted due to ethical considerations, difficulties in trial design, and limited hospital resources and personnel.2-4 We highlight a single center’s experience and the challenges encountered in screening, enrolling, and consenting for an acute neonatal seizure treatment trial.
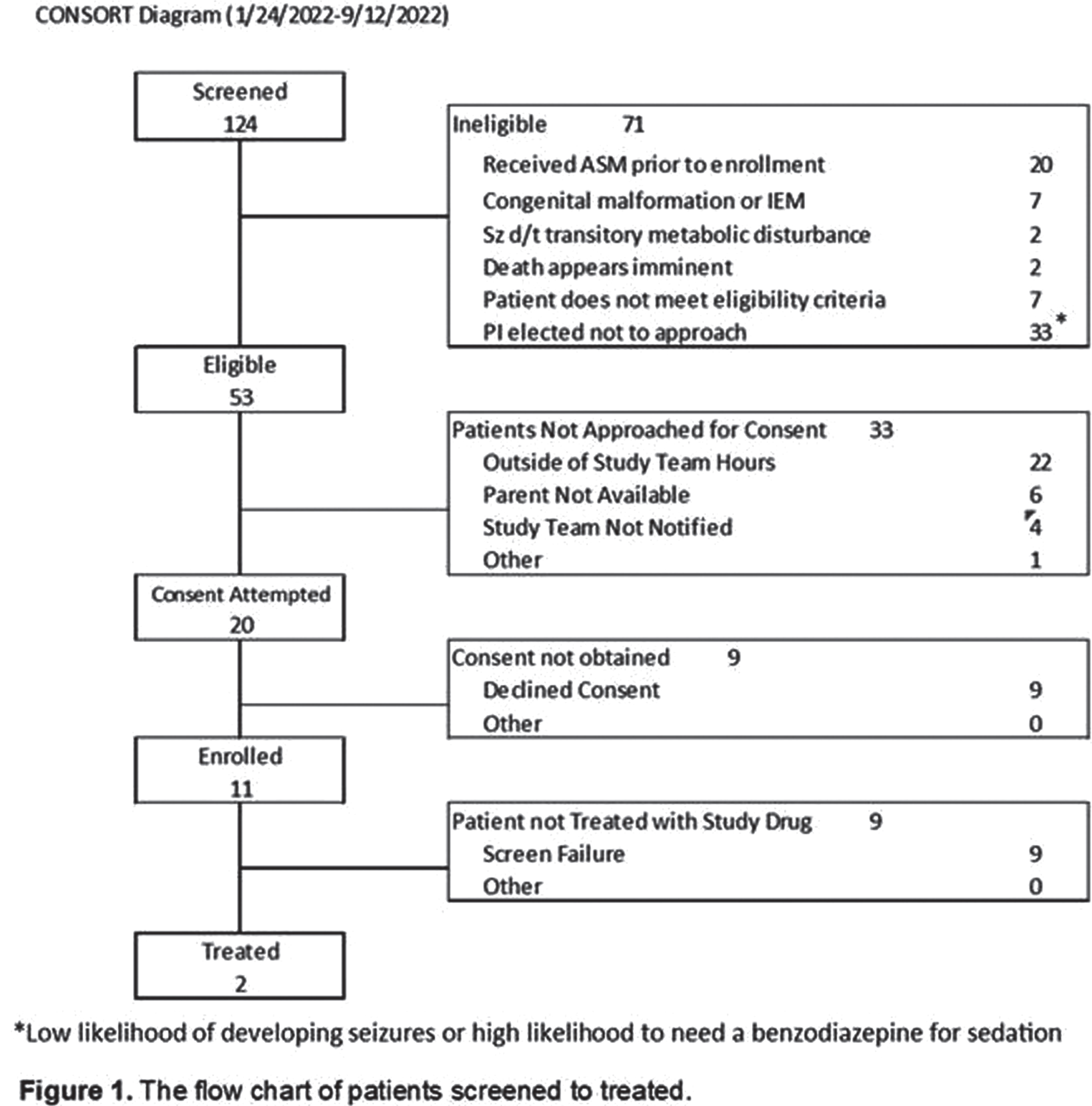
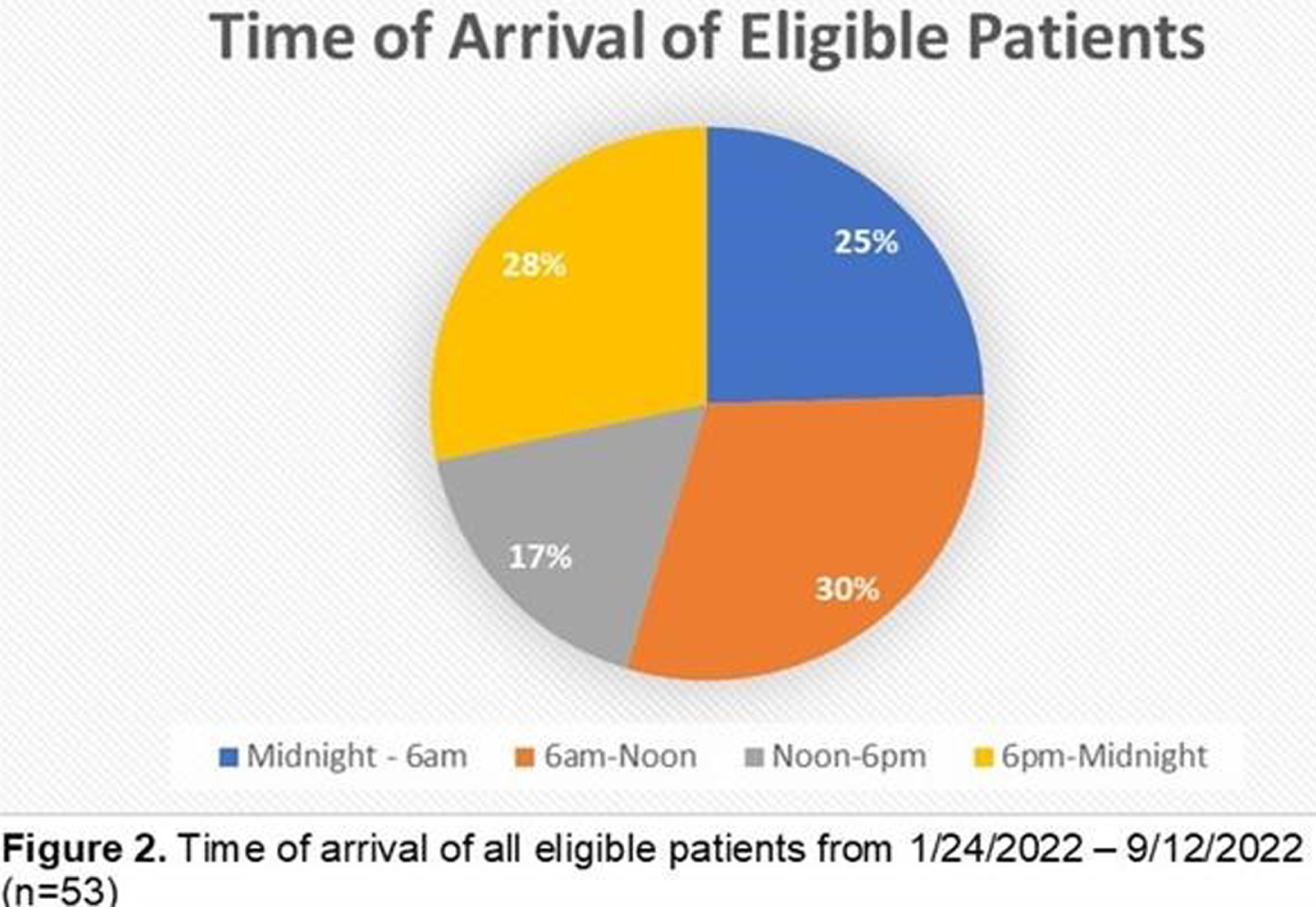
METHODS: Children’s National (CN) is the lead site of an acute symptomatic neonatal seizure trial for a new formulation of phenobarbital. Two physician investigators and two study coordinators at CN screened patients being transferred for continuous video electrographic encephalography (EEG) in the NICU between 1/24/2022 and 9/12/2022. Starting July 1st, the study team implemented updated consenting methods by presenting patients’ parents with condensed study information. The study team recorded each patient’s date and time of arrival, eligibility status, reason consent was declined, and reasons eligible patients were not approached (study team unavailable, parent or guardian not available, the study team not notified, or other). Study team screening hours were between 6:00 and 23:00 including weekends and holidays. Eligible patients were tracked for date and time of first EEG seizure.
RESULTS: Of the 124 patients screened, 53 were eligible for the study (Fig 1). 53% (28/53) arrived at CN NICU between 18:00 and 6:00 (Fig 2). Twenty of those eligible were approached for consent, 11 consented and 2 patients received study drug (Fig 1). The reasons eligible patients were not enrolled are as follows: patient arrived outside of study team hours (22/42=52%); parent declined consent (9/42=21%); unavailable parent (6/42=14%); lack of study team notification of patient (4/42=10%); and expiration of study drug (1/33=3%) (Fig 3). Some of these patients went on to have seizures within the time they would have been eligible to receive study drug (Fig 3). Study team availability was 76% on weekdays and 64% during off hours (weekends and holidays). 67% of the time the team was unavailable due to Investigational Drug Services restricting screening to business hours for the first 28 days of the study and unexpected death of one of the co-investigators pausing screening for 16 days. These 44 days account for 17 out of the 22 patients that arrived outside of study team hours. Condensing the consent script in July increased our study enrollment from 45% to 71%. There was no correlation in the consent rate between consent conducted in-person compared to consent conducted over the phone.

CONCLUSION: Limited availability of study staff after hours (18:00-6:00) is a major impediment to enrolling neonates in an acute seizure trial. A shorter, focused consent script increased study enrollment both in person and over the phone.
REFERENCES
[1] Uria-Avellanal C., Marlow N., Rennie J. M. Outcome following neonatal seizures. Semin. Fetal Neonatal Med. 2013; 18, 224–232.
[2] Laventhal N., Tarini B. A., Lantos J. Ethical issues in neonatal and pediatric clinical trials. Pediatr. Clin. North Am. 2012; 59, 1205–1220.
[3] Amin S. B., McDermott M. P., Shamoo A. E. Clinical trials of drugs used off label in neonates: ethical issues and alternative study designs. Account. Res. 2008; 15, 168–187.
[4] Soul JS, Pressler R, Allen M, Boylan G, Rabe H, Portman R, Hardy P, Zohar S, Romero K, Tseng B, Bhatt-Mehta V, Hahn C, Denne S, Auvin S, Vinks A, Lantos J, Marlow N, Davis JM; International Neonatal Consortium. Recommendations for the design of therapeutic trials for neonatal seizures. Pediatr Res. 2019; 85(7), 943-954.
Long term neurodevelopment and predictors of outcome in a single center cohort of infants with neonatal encephalopathy
Zahalka A1, Marks1, Abramsky1, Shelef I1, Michaelovsky A1, Farkash Novik E1, Goldshtein M1, Ozalvo D1, Shany E1
1Ben Gurion University of the Negev, Beer-sheva, Israel
BACKGROUND AND PURPOSE: Neonatal encephalopathy (NE) is a leading cause of mortality and morbidity worldwide. Throughout the years different bio and electrophysiological markers such as amplitude integrated EEG (aEEG), conventional EEG, evoked potentials, magnetic resonance imaging (MRI) and physical examination were found to have significant predictive ability for long term neurodevelopmental outcome. The purpose of this study was to assess the distinct and combined contribution of different markers for prediction of long-term outcome.
MATERIALS OR METHODOLOGY: Infants born after 35 weeks of gestation, between November 2014 and May 2019 in Soroka medical Center, Beer-Sheva, Israel, diagnosed with moderate to severe NE of presumed hypoxic ischemic origin, monitored with aEEG and with brain MRI before 10 days of age were included in the study. Infants with cerebral malformations/hemorrhage/infection/stroke, inborn error of metabolism or genetic disorder were excluded.
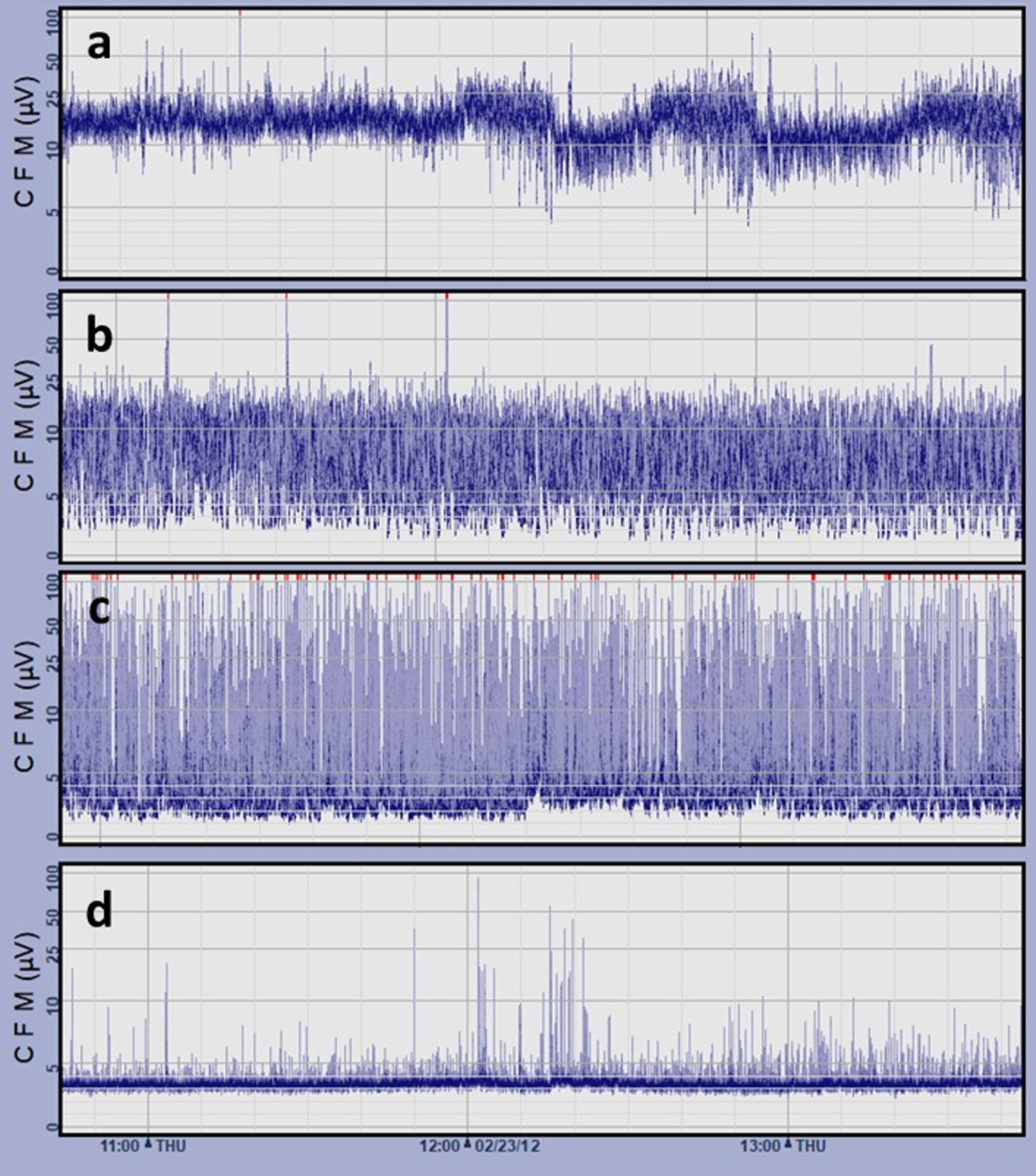
Early life demographic and clinical data were prospectively collected. Continuous neuromonitoring with aEEG (figure 1) during the first 4 days of life was assessed for seizures and daily background activity was dichotomized to:
1. Normal/near normal: Continuous or discontinuous background
2. Abnormal: Burst suppression, low voltage or isoelectric background Early life MRI (table 2) was scored according to a modified Rutherford et al. scoring that included diffusion sequences and dichotomized to:
3. Normal/mild abnormalities
4. Moderate to severe abnormalities

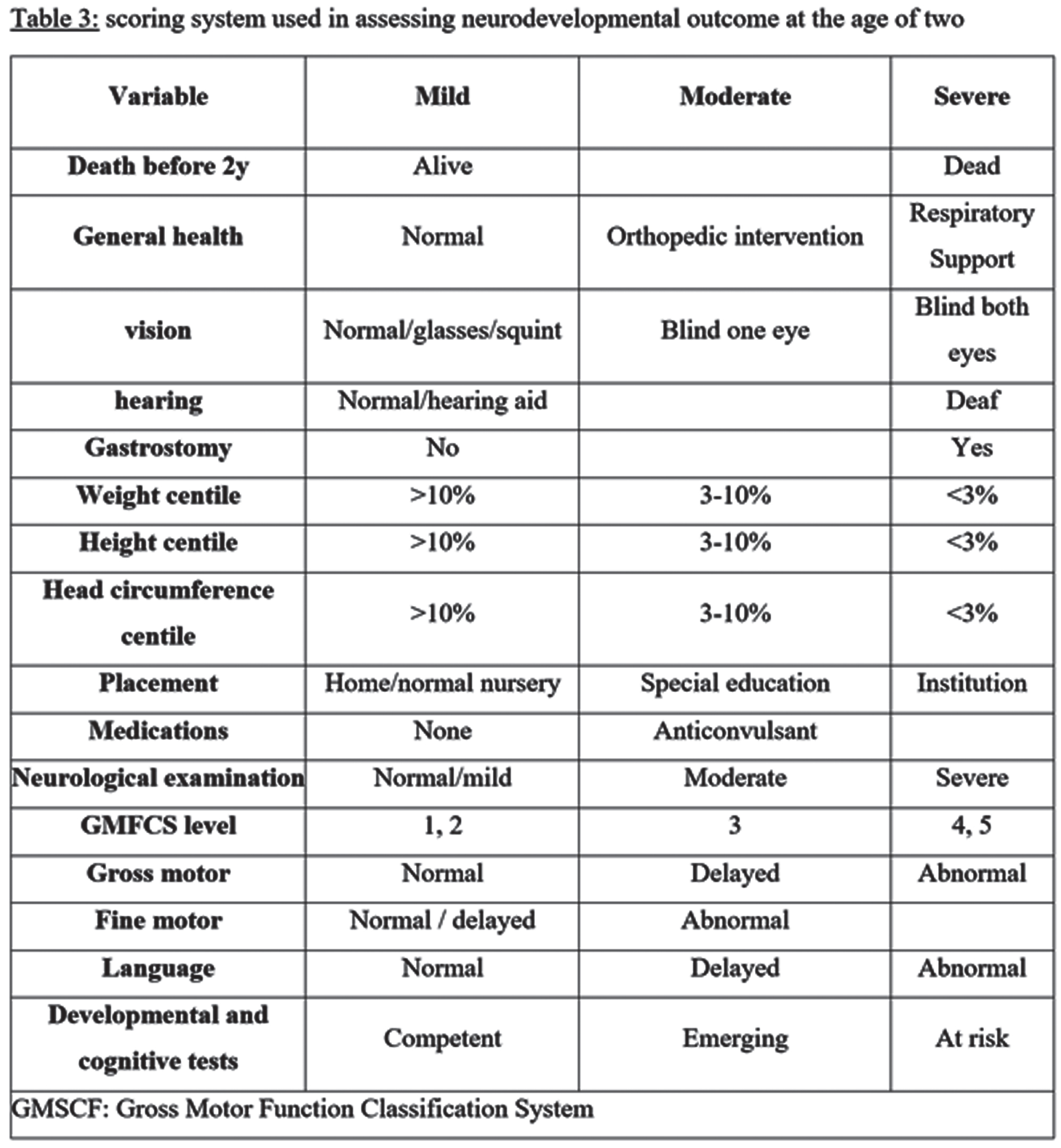
Outcome after 2 years of age was assessed using data collected from the child developmental center, medical records and personal communication with parents and dichotomized to: 1. Normal/mildly abnormal, 2. Moderately/severely abnormal. Clinical data as described in table 3 was used to categorize outcome. Multivariable binary logistic regression was performed on the basis of univariable analysis to develop the best predictive model for long term outcome.
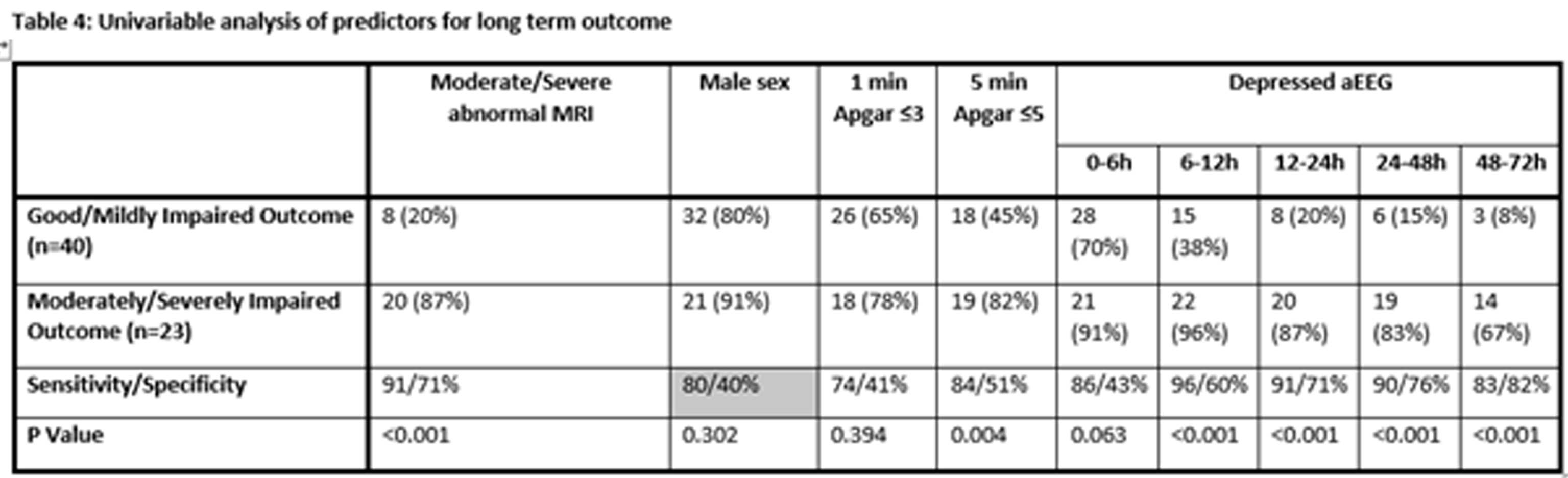
RESULTS: Sixty-three out of 76 infants were included in the study. Eleven (17.5%) and 29 (46%) had good or mildly impaired outcome respectively, 3 (4.8%) and 20 (31.7.7%) had moderate or severe outcome respectively (including 9 (24.3%) who died). Univariable model is presented in table 4. In multivariable models, best combined predictors of outcome were: 5 minutes Apgar score (p=0.004), aEEG at the second day of life (p<0.001) and MRI (p<0.001).
CONCLUSION AND IMPACT: Despite improvement in intensive care and the advent of hypothermia, early biomarkers are significantly associated with outcome. International and national registries of neonatal encephalopathy with long term outcome are important tools for monitoring trends, changes and new therapies.
REFERENCES
[1] Hamelin S et al. Neurophysiol Clin. 2011 Feb;41(1):19-27.
[2] Kontio T et al. Clin Neurophysiol. 2013 Jun;124(6):1089-94.
[3] Shankaran S et al. J Pediatr. 2015 Nov;167(5):987-93.
[4] Rutherford M et al. Lancet Neurol. 2010;9(1):39–45
[5] Okereafor A, et al. Pediatrics. 2008;121(5):906–14.
Functional brain networks after perinatal stroke: Results from a pilot study
Kavčič A1, Demšar J2, Soltirovska Šalamon A1
1Division of Pediatrics, Department of Neonatology, University Medical Centre Ljubljana, Ljubljana, Slovenia, 2Faculty of Computer and Information Science, University of Ljubljana, Ljubljana, Slovenia
BACKGROUND AND PURPOSE: An increasing number of studies facilitates functional brain networks to analyze cognitive function in diverse neurological conditions. Focal brain injury seems to impact functional brain networks on a local and a global scale. Long term changes of functional brain networks after perinatal stroke have not been studied extensively so far. Our aim was to explore functional brain networks after perinatal stroke with EEG-based functional connectivity. We were interested in whole brain and intra-hemispheric functional network characteristics.
METHODOLOGY: A test-control pilot study was conducted in a total number of 27 individuals. Inclusion criteria for the test group were: a history of perinatal stroke – either arterial ischemic or hemorrhagic stroke, term delivery, age at inclusion 5-18 years and absence of other neurological disabilities. Inclusion criteria for the control group were: healthy children and adolescents, with no history of brain injury or known neurologic conditions, term delivery and age at inclusion 5-18 years. We recorded a 64-channel resting-state EEG in 27 participants (13 from the test group and 14 from the control group). Individuals from the control group were matched to the test group by age and gender. We processed EEG data and calculated functional connectomes for each participant and analyzed differences in connectome graph metrics between the two groups. Several metrics reflecting network properties were investigated. We were interested in whole brain networks and intra-hemispheric networks (ipsilesional and contralesional). The strength of the inter-hemispheric connections was also studied. We used characteristic path as a metric reflecting the level of synchronization, clustering coefficient as a metric of network segregation, small-worldness and modularity as metrics of network organization and degree variance as an indirect metric of network topology.
RESULTS: Test group functional networks had indices of higher segregation with increased clustering coefficient and increased small-worldness on both whole brain and intra-hemispheric scale. A more regular topology with lower degree variance was present in functional brain networks of the test group compared to the control group. Ipsilesional hemisphere of the test group also had a more regular topology with lower degree variance compared to the contralesional hemisphere. A total number of inter-hemispheric links was higher in the test group.
CONCLUSION/IMPACT: Our study suggests that perinatal stroke impacts functional brain networks organization and topology in a long term. According to our results, indices of functional brain network disruption persist years after initial brain injury. Our pilot study shows that high-density EEG can be used for investigating functional networks after perinatal stroke. Future studies should focus on exploring the options of using this method for prognostication, especially with trying to find the correlation between functional brain networks characteristics and cognitive outcome in children and adolescents with perinatal stroke.
REFERENCES
[1] Aerts H, Fias W, Caeyenberghs K, Marinazzo D. Brain networks under attack: Robustness properties and the impact of lesions. Brain. 2016;139(12):3063-3083. doi:10.1093/brain/aww194
[2] Stam CJ. Modern network science of neurological disorders. Nat Rev Neurosci. 2014;15(10):683-695. doi:10.1038/nrn3801
[3] Alstott J, Breakspear M, Hagmann P, Cammoun L, Sporns O. Modeling the impact of lesions in the human brain. PLoS Comput Biol. 2009;5(6):e1000408.
[4] Ilves N, Ilves P, Laugesaar R, et al. Resting-State Functional Connectivity and Cognitive Impairment in Children with Perinatal Stroke. Neural Plast. 2016;2016. doi:10.1155/2016/2306406
[5] Saunders J, Carlson HL, Cortese F, Goodyear BG, Kirton A. Imaging functional motor connectivity in hemiparetic children with perinatal stroke. Hum Brain Mapp. 2019;40(5):1632-1642.
[6] van Diessen E, Numan T, van Dellen E, et al. Opportunities and methodological challenges in EEG and MEG resting state functional brain network research. Clin Neurophysiol. 2015;126(8):1468-1481. doi:10.1016/j.clinph.2014.11.018
[7] Haartsen R, van der Velde B, Jones EJH, Johnson MH, Kemner C. Using multiple short epochs optimises the stability of infant EEG connectivity parameters. Sci Rep. 2020;10(1):1-13. doi:10.1038/s41598-020-68981-5
[8] Carvalhaes C, De Barros JA. The surface Laplacian technique in EEG: Theory and methods. Int J Psychophysiol. 2015;97(3):174-188. doi:10.1016/j.ijpsycho.2015.04.023
[9] Vinck M, Oostenveld R, Van Wingerden M, Battaglia F, Pennartz CMA. An improved index of phase-synchronization for electrophysiological data in the presence of volume-conduction, noise and sample-size bias. Neuroimage. 2011;55(4):1548-1565. doi:10.1016/j.neuroimage.2011.01.055
[10] Sporns DO. Networks of the Brain.; 2015. doi:10.1017/CBO9781107415324.004
[11] Rubinov M, Sporns O. Complex network measures of brain connectivity: Uses and interpretations. Neuroimage. 2010;52(3):1059-1069. doi:10.1016/j.neuroimage.2009.10.003
[12] Bullmore E, Sporns O. Complex brain networks: Graph theoretical analysis of structural and functional systems. Nat Rev Neurosci. 2009;10(3):186. doi:10.1038/nrn2575
Cerebral Sinovenous thrombosis in the term neonates: Diagnostic and prognostic challenges
Toma A1,2, Cuzino I1, Gont B1, Petcariu B1, Iriciuc M3
1Life Memorial Hospital/Neonatology, Bucharest, Calea Grivitei 365, România, 2University Titu Maiorescu. Faculty of Medicine, Bucharest, Str Gh Petrascu 67, Romania, 3Life Memorial Hospital/Radiology, Bucharest, Calea Grivitei 365, Romania
BACKGROUND AND AIM: Our case series represent the experience of one maternity hospital and a referral neonatal neurology centre in the diagnosis and follow up of the cases of cerebral sinovenous thrombosis (CSVT) in term neonates.
MATERIAL AND METHODS: During a 4 years interval, there were diagnosed 4 cases of neonatal CSVT in patients born in the hospital and another 6 cases were referred to our follow up centre. All the cases were referred after extensive cerebral ultrasound training – doctors were trained to recognize the signs poiting to possible CSVT and to ask for second opinion and MRI in these cases. There are presented: the clinical sings and ultrasound and MRI findings in the neonatal period and follow-up, the results of the aEEG monitoring, the results of the coagulation and pro-thrombotic tests, the neurologic outcome of the cases.
RESULTS: 9 out of 10 cases were symptomatic at diagnosis: seizures in 5/10 cases, apnea in 4/10 cases, respiratory distress in 1/10 cases. One case was asymptomatic in the neonatal period- diagnosed at 3 days by ultrasound, the history noted a period of decreased fetal movements one week before delivery. In all the cases, the ultrasound examination suggested the diagnosis – one case bilateral lesions of different ages, one case intraparenchimal hyperechogenicity, periventricular hemorrhagic infarctions 5 cases ; 3 cases – thalamic haemorrhages, 2 cases peri/intraventricular hemorrhages (several cases had associations of lesions). In all the cases, the diagnosis was confirmed by MRI. Clinical seizures were present in 3/3 cases with thalamic lesions and in 4/7 case with parenchymal lesions. In 2/7 cases monitored with aEEG , electrical-only seizures were present. In 3 cases,a deficit of factor V Leyden was found both in the mother and the child. No thrombolytic therapy was used. 7 patients were discharged on anticonvulsant treatment the treatment was stopped between 3-12 months - the patients were seizure-free after stopping the medication. 8/10 cases presented with deficit of the head growth. All the patients presented with unilateral motor deficit – in two cases, the deficit was transitory. In all the other cases walking was possible, age for independent was delayed (mean - 15 months). Language deficit was present in 5/10 cases and cognitive deficit in 4/10 cases. The main determinants for unfavourable outcome were thalamic lesions or bilateral lesions.
CONCLUSIONS: Although a rare occurrence, CSVT could be diagnosed in the neonatal period. The cases are almost allways symptomatic. The diagnosis is suggested by the ultrasound and confirmed by MRI. The neurological sequelae are present in all the cases consisting in motor sings, seizures - transitory - and cognitive and language deficits. A better knowledge of this entity could increase the awareness and increase the frequency of diagnosis.
Early intervention in preterm infants: Effects on neurodevelopmental outcome at preschool age
Bonfanti C1, Fontana C1, Schiavolin P2, Gangi S1, Porro M1, Meloni S1, Pesenti N1,3, Mosca F1,2, Fumagalli M1,2
1Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, NICU, Milan, Italy, 2Department of Clinical Sciences and Community Health, University of Milan, Milan, Italy, 3University of Milano-Bicocca, Division of Biostatistics, Epidemiology and Public Health, Department of Statistics and Quantitative Methods, Milan, Italy
BACKGROUND: Prematurity is associated with an increased risk of acute and chronic postnatal morbidities and long-term neurodevelopmental disabilities, even in absence of major brain injury. Early intervention strategies in preterm infants, based on parental training and multisensory stimulations, have been shown to be effective in positively modulating brain maturation and short-term neurodevelopment [1, 2]. However, little is known about long-term effects on neurodevelopment, due to significant heterogeneity among intervention protocols and target population [3].
PURPOSE: to determine, in preterm-birth children, the effects of an early intervention program on neurodevelopment at preschool age (5-6 years) and to evaluate the neurodevelopmental profile through childhood.
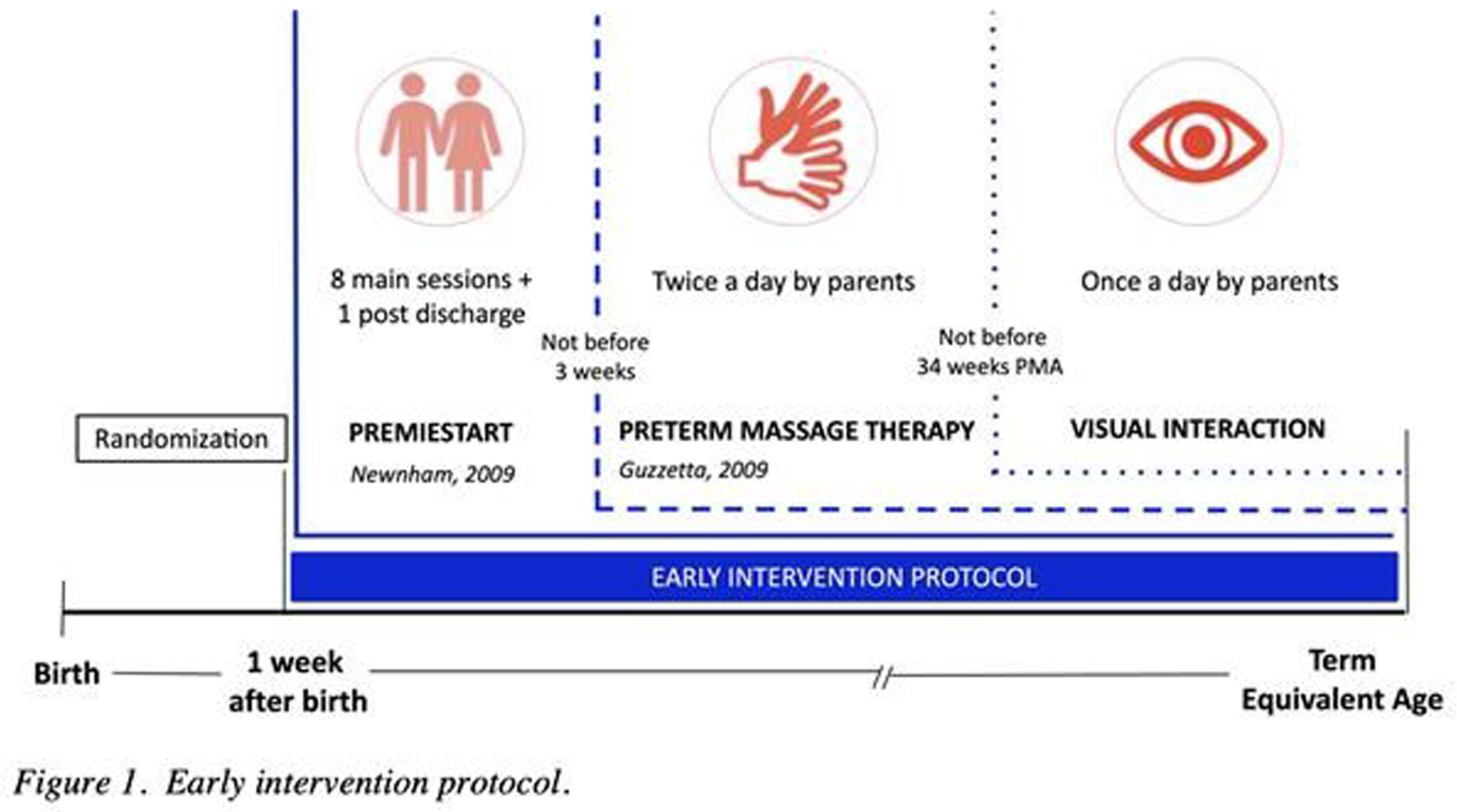
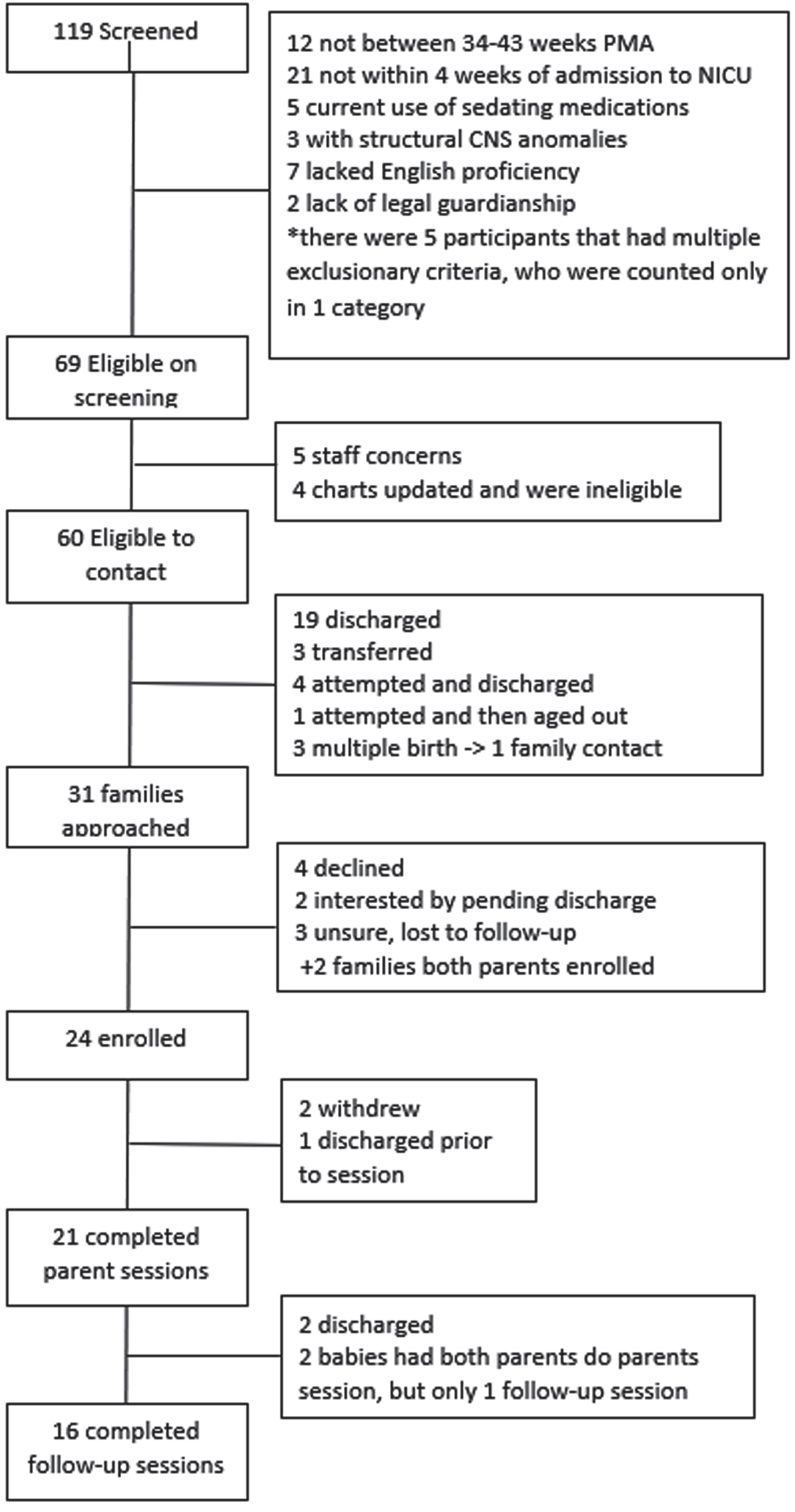
METHODS: this is an ancillary study, part of a larger RCT [4], that included preterm infants born between 25+0 and 29+6 weeks of gestational age (GA) without severe neonatal comorbidities. Infants were randomized to receive early intervention (EI) or standard care (SC). SC, according to NICU protocols, included Kangaroo Mother Care and minimal handling. EI included, in addition to routine care, parental training and multisensory experiences (infant massage and visual interaction) performed by parents (Figure 1) [5]. Neurodevelopment was assessed between 5 and 6 years chronological age with the Griffiths Scales, the Child Behavior Checklist (CBCL), and the Movement ABC-2.
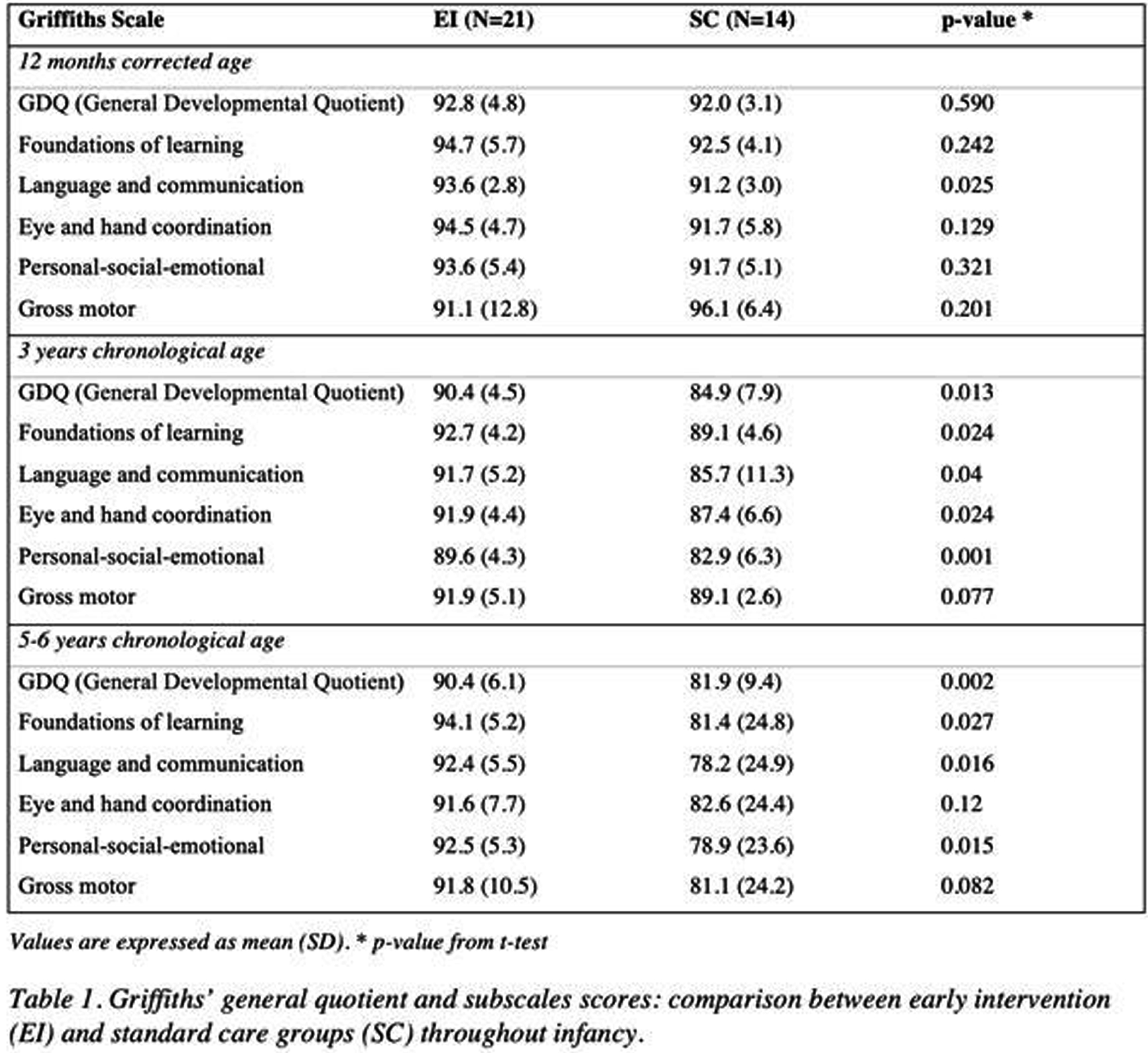
RESULTS: 70 preterm infants were enrolled in the RCT and 35 (EI n = 21, SC n = 14) completed the long-term follow-up, as reported in the flowchart (Figure 2). The EI group showed, at preschool age, a normal neurodevelopmental outcome with significantly higher mean General Developmental Quotient (GDQ = 90.4, p-value = 0.002), compared to SC group that exhibited a mean score below the normal range (GDQ = 81.9) (Table 1). Moreover, the mean difference in GDQ scores increased of 2.03 points for each additional year in favor of the EI group, becoming statistically significant from 3 years (p-value = 0.013) and being confirmed at 5-6 years (p-value = 0.002) (GDQ and subscale scores throughout infancy are reported in Table 1). No differences in the CBCL scores were observed between the two groups, with all the infants being within the normal range (< 60). At the Movement ABC-2 the EI group showed a higher, although not significant, total standard score compared to the SC group (mean = 8.44 versus 6.82, p-value 0.187) (Table 2), a difference that decreased when adjusting for GA and socio-economic status.
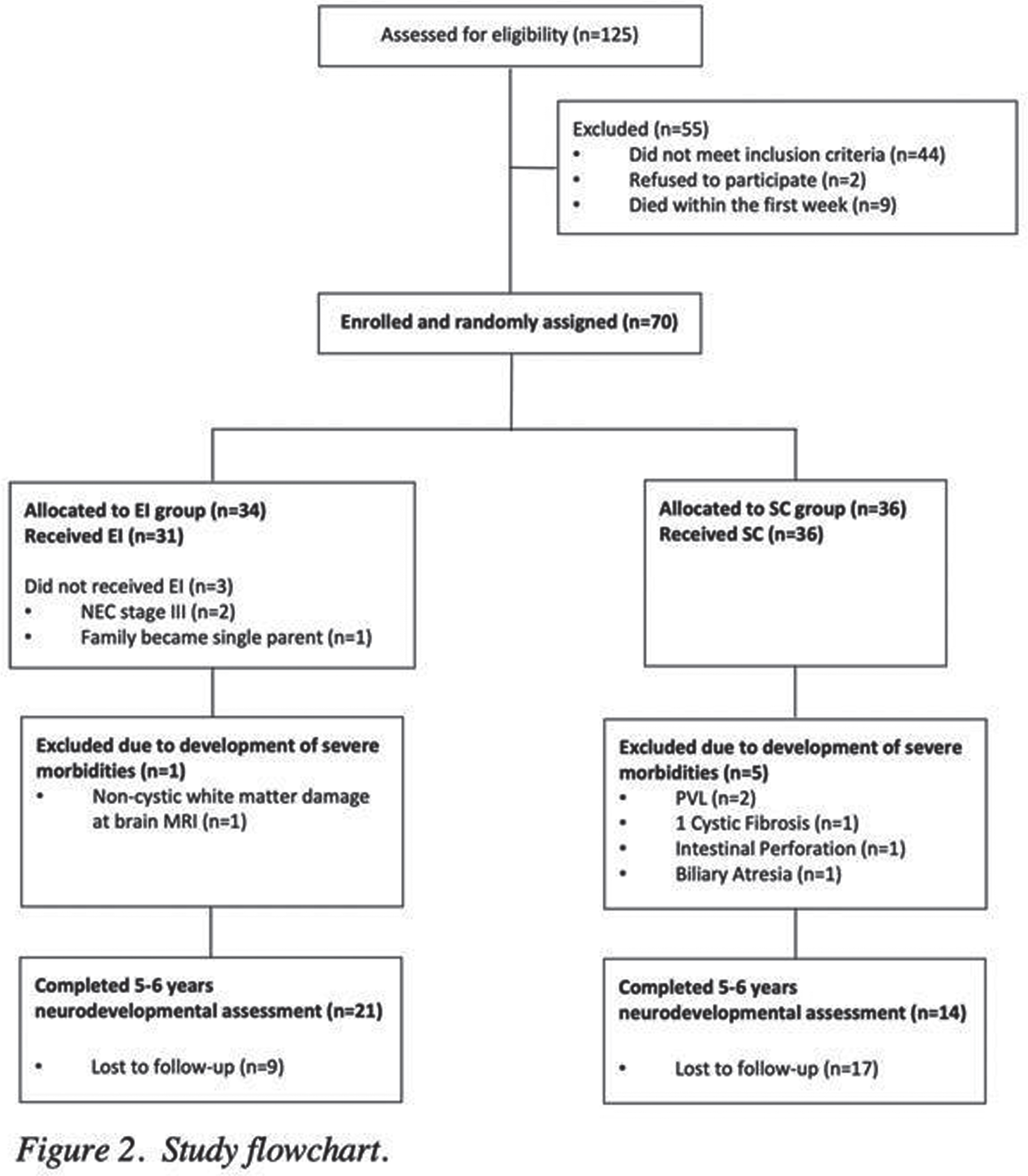
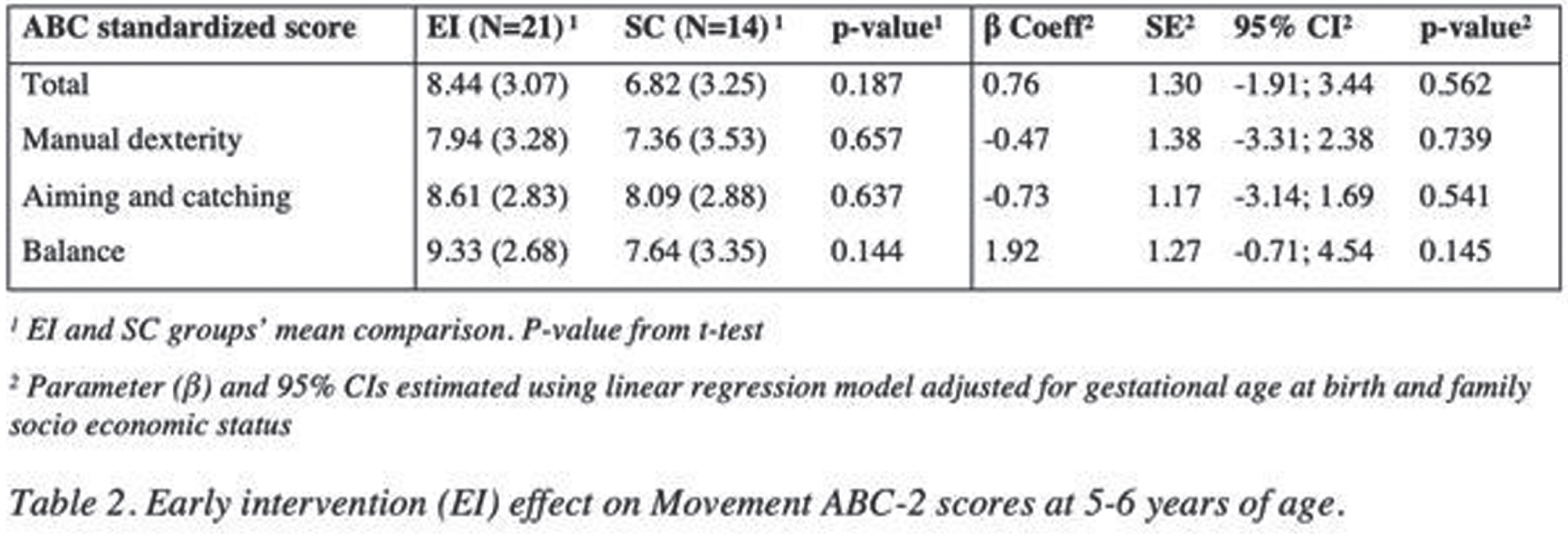
CONCLUSIONS: our study contributed to demonstrate the possible beneficial effects of early intervention strategies in ameliorating long-term neurodevelopment in infants born preterm, through the crucial involvement of parents. The main limitation of our study is the high dropout rate, mostly because of the COVID-19 pandemic, and possible selection bias that needs to be ruled out; therefore, further research is recommended.
REFERENCES
[1] Spittle A, Treyvaud K. The role of early developmental intervention to influence neurobehavioral outcomes of children born preterm. Semin Perinatol. 2016;40(8):542-548. doi:10.1053/j.semperi.2016.09.006
[2] Embarek-Hernández M, Güeita-Rodríguez J, Molina-Rueda F. Multisensory stimulation to promote feeding and psychomotor development in preterm infants: A systematic review. Pediatrics and Neonatology. 2022;63(5):452-461. doi:10.1016/j.pedneo.2022.07.001.
[3] Pierrat V, Marchand-Martin L, Marret S, et al. Neurodevelopmental outcomes at age 5 among children born preterm: EPIPAGE-2 cohort study. BMJ. Published online April 28, 2021:n741. doi:10.1136/bmj.n741
[4] Fontana C, De Carli A, Ricci D, et al. Effects of Early Intervention on Visual Function in Preterm Infants: A Randomized Controlled Trial. Front Pediatr. 2020;8:291. doi:10.3389/fped.2020.00291
[5] Newnham CA, Milgrom J, Skouteris H. Effectiveness of a Modified Mother–Infant Transaction Program on Outcomes for Preterm Infants from 3 to 24 months of age. Infant Behav Dev. 2009;32(1):17-26. doi:10.1016/j.infbeh.2008.09.004
Current practices and parental attitudes of the role of neonatal therapies during therapeutic hypothermia for hypoxic ischemic encephalopathy
Arroyo M1,2, Garcia R1
1Joe DiMaggio Children’s Hospital, Hollywood, United States, 2Stiles-Nicholson Brain Institute, Florida Atlantic University, Jupiter , United States
BACKGROUND: Neonates with moderate to severe encephalopathy qualify for therapeutic hypothermia for a presumed diagnosis of hypoxic ischemic encephalopathy (HIE). This is an incredibly stressful time for parents and a big source of hope is the potential for neurorehabilitation. Currently, there is no standard of care or curriculum for the involvement of neonatal therapists in cooling. A prior study surveying 58 neonatal therapists found variability of practice in the United States (US). The parent perspective of when to introduce therapies has not been evaluated. The objective of this study was to determine current practices across the US and parental perspective by surveying neonatal therapists, as well as parents of children with a history of cooling for HIE. Results of this study may serve to inform future propositions for national guidelines and educational curriculums to improve neurodevelopmental outcomes and optimize parent experience.
METHODS: This survey study included two separate anonymous surveys which were distributed online via REDCap’s survey link tool. The neonatal therapist survey included 34 questions pertaining to current practices while the parent/caregiver survey included 18 questions focused on the parental experience. Both surveys are ongoing with an offline date of November 22, 2022. Participants were and are being recruited by way professional organizations’ listservs, established parent support non-for-profit organizations, and social media sites. Participants include parents or caregivers of infants with HIE ages 6 to 12 months, as well as therapists working in a NICU that provides cooling and is in the US. IRB approval was received (MHS.2022.096).
RESULTS: At the time of data abstraction, there was a total of 49 parent respondents. Of all respondents, 91.8% (n=45) reported that their baby received therapy while admitted. Most parents reported that their baby started therapy after they had MRI (69%, n=29) and looking back, most of the parents would have preferred to meet with therapists earlier (34.9 % n=15 during cooling, 27.9% N=12 during rewarming). In general, the parents did not discuss MRI with therapists in context of therapy plan (68.9%, n=31). Most parents reported interest in educational materials in both written and video format (81%, n=25). Of a total of 16 neonatal therapy respondents, the majority report that their institution does not have a standardized protocol for assessing and treating babies with HIE (11, 68.8%).
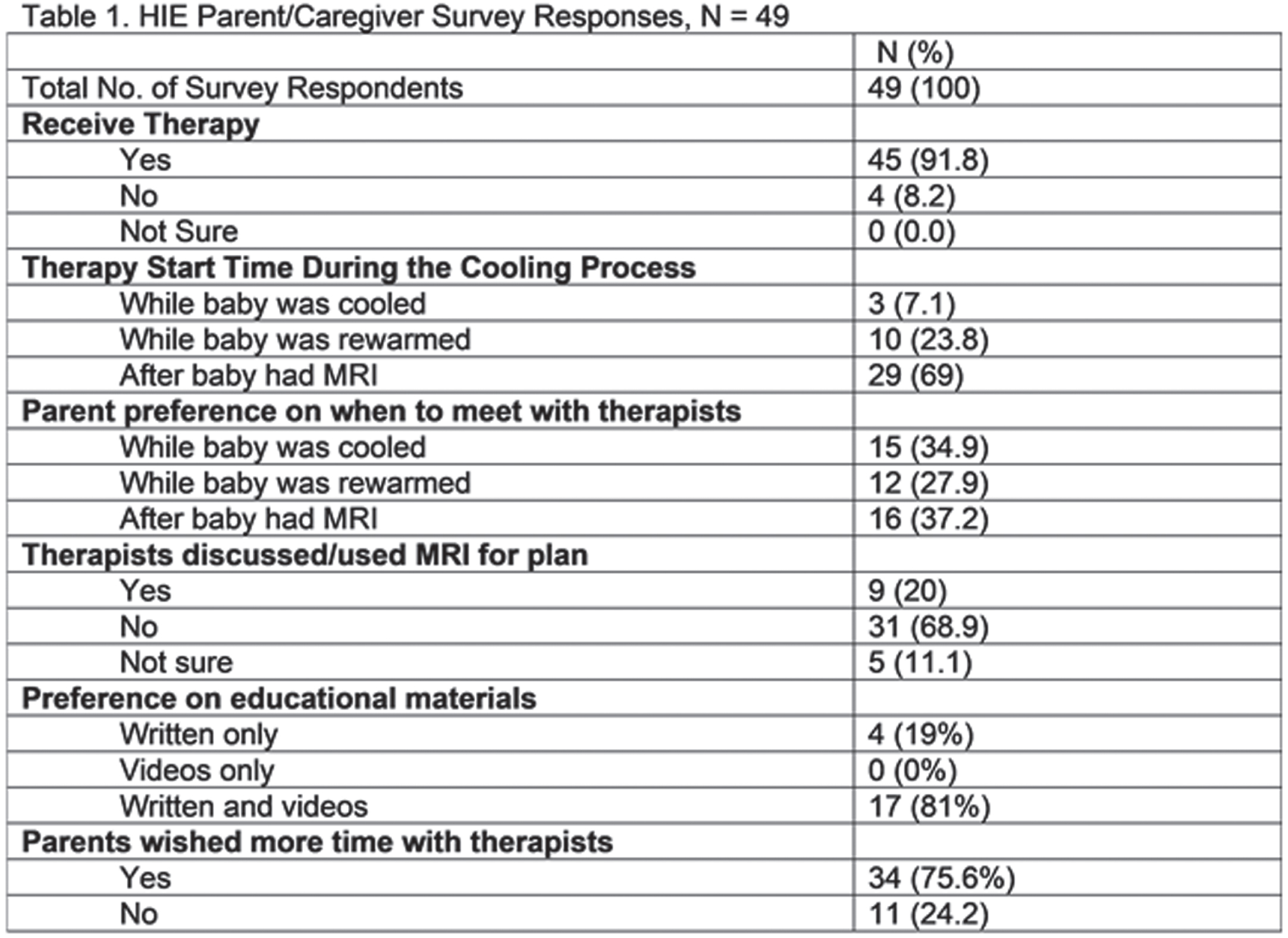
CONCLUSION/IMPACT: Most babies with HIE receive therapy in the NICU. While most therapists meet with parents after the day of MRI, a significant proportion of parents would prefer to meet earlier in the process. Parents would be interested in further education from therapists. National guidelines, neonatal therapy education on HIE patterns of injury for therapy plan design, as well as earlier parental education with a standardized curriculum are identified areas of improvement.
Pilot of Bilateral Infant Stimulation Study (BLISS) in the NICU
Garavatti E1, Cimino C2, Alsup S3, Ondusko D1, DiPietro J4, Phillips J4, Mackiewicz Seghete K5
1Department of Pediatrics, Oregon Health & Science University, Portland , United States, 2Department of Pediatric Rehabilitation Services, Oregon Health & Science University, Portland, United States, 3School of Professional Psychology, Pacific University, Hillsboro, United States, 4School of Medicine, Oregon Health & Science University , Portland, United States, 5Department of Psychiatry, Oregon Health & Science University, Portland, United States
BACKGROUND: Parents of infants admitted to the NICU often have clinically significant PTSD symptoms at time of discharge. Positive touch interventions have benefits for infants and parents, but current interventions cannot be implemented with critically ill infants. Therefore, our most at risk population is in need of interventions that use positive touch for both the parent and infant.
PURPOSE: We propose using a bilateral alternating stimulation technique as a form of positive touch for parents to engage with critically ill infants. We hypothesize this intervention will reduce infant autonomic arousal and reduce parental distress and anxiety. Our study aims to identify whether this intervention is feasible to complete in a level IV pod-based NICU and acceptable to parents and NICU staff, as a first step in intervention development.
METHODOLOGY: This single arm feasibility and acceptability study was conducted in a level IV pod-based NICU. Parents were first instructed at bedside by an interventionist and then engaged their infant in the intervention. Outcomes included: parent heart rate (via wristband smartwatch); infant vital signs from bedside monitors; acceptability questionnaires; and parent self-report measures. See Figure 1.
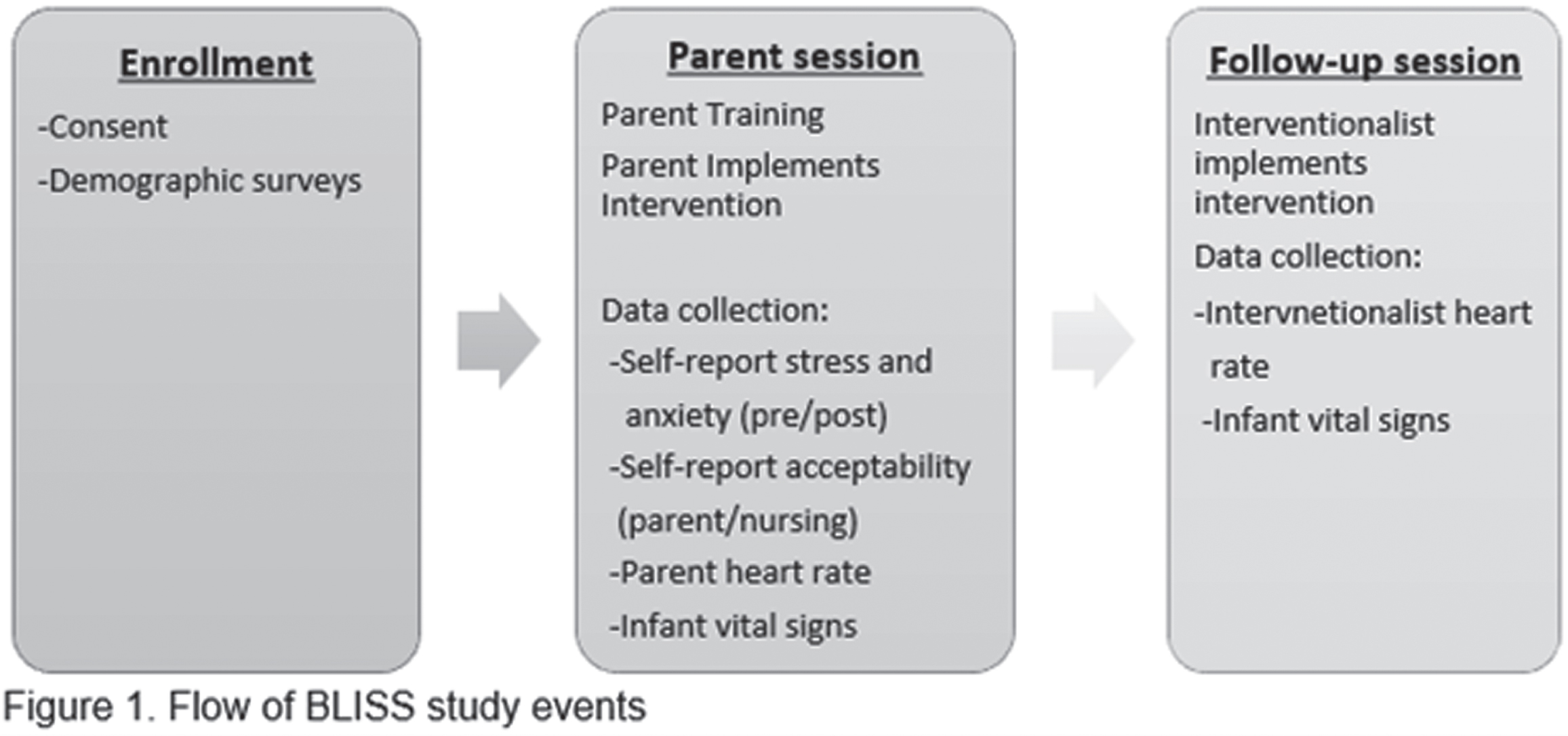
RESULTS: We enrolled 24 parent-neonate dyads between June to September 2022. Twenty-one parents completed initial sessions (88%) and 16 infants completed follow-up sessions (76%). Feasibility: Feasibility benchmarks were met (set at >80%), with 100% of sessions completed without termination. Interventionists reported 89% of teaching sessions went “smoothly” and 81% of sessions overall “went well.” No sessions were rated negatively. Parents wore wristbands for 100% of sessions. Infant vital signs were collected for 76% of sessions. Acceptability: Parents completed the Customer Satisfaction Questionnaire (CSQ), a common measure of intervention acceptability, with scores ranging from 8-32. Mean satisfaction was 30.84 (SD 1.21), reflecting high level of acceptability. Nursing staff completed surveys for 42% of sessions; 90% of responses were positive, without any negative responses. Preliminary pre-post intervention analyses were conducted to explore outcomes; analyses were not conducted to determine effects, as this is a feasibility and acceptability study. State anxiety was measured using the Visual Analog Scale- Anxiety (VAS-A) and the State Trait Anxiety Inventory (STAI). Parents reported significantly lower anxiety post-intervention (VAS-A: M= 14.76, SD=17.04; STAI: M= 30.33, SD = 12.75) compared to pre-intervention (VAS-A: M= 23.33, SD= 27.61; STAI: M= 37.33, SD= 12.85), p = .023 and p < .001. Parental distress (Distress Thermometer) was also significantly lower post-treatment compared to pre-treatment (pre: M= 5.52, SD= 2.48; post: M= 4.29, 2.72), p = .005.
CONCLUSIONS: The BLISS study is feasible to conduct in a pod-based NICU and is acceptable to both parents and nursing staff. Preliminary data suggests the intervention is promising for further pursuit on the impact on parental anxiety and distress.
Electroencephalogram patterns on follow-up visits in extremely premature infants with periventricular leukomalacia: An observational study
Obeid R1
1Beaumont Children’s Hospital, Beaumont Children’s Hospital/ Oakland University William Beaumont School of Medicine, Royal Oak, Michigan, United States
BACKGROUND AND PURPOSE: Periventricular Leukomalacia (PVL) is a common brain injury in premature newborns. Current literature provides limited guidance on the benefit of electroencephalogram (EEG) as a potential screening tool for seizure risk in this population. The purpose of this study is to describe the EEG patterns on follow-up visits in infants born premature and diagnosed with PVL.
METHODS: This is a retrospective study of premature newborns (<37 weeks gestation), who were followed in the neurodevelopmental clinic at Beaumont Children’s Hospital in Detroit MI between 2020 and 2022. Patient’s demographics, prematurity complications, head ultrasound (HUS), and EEG studies were reviewed. PVL on HUS was graded based on Agut et al 2020.
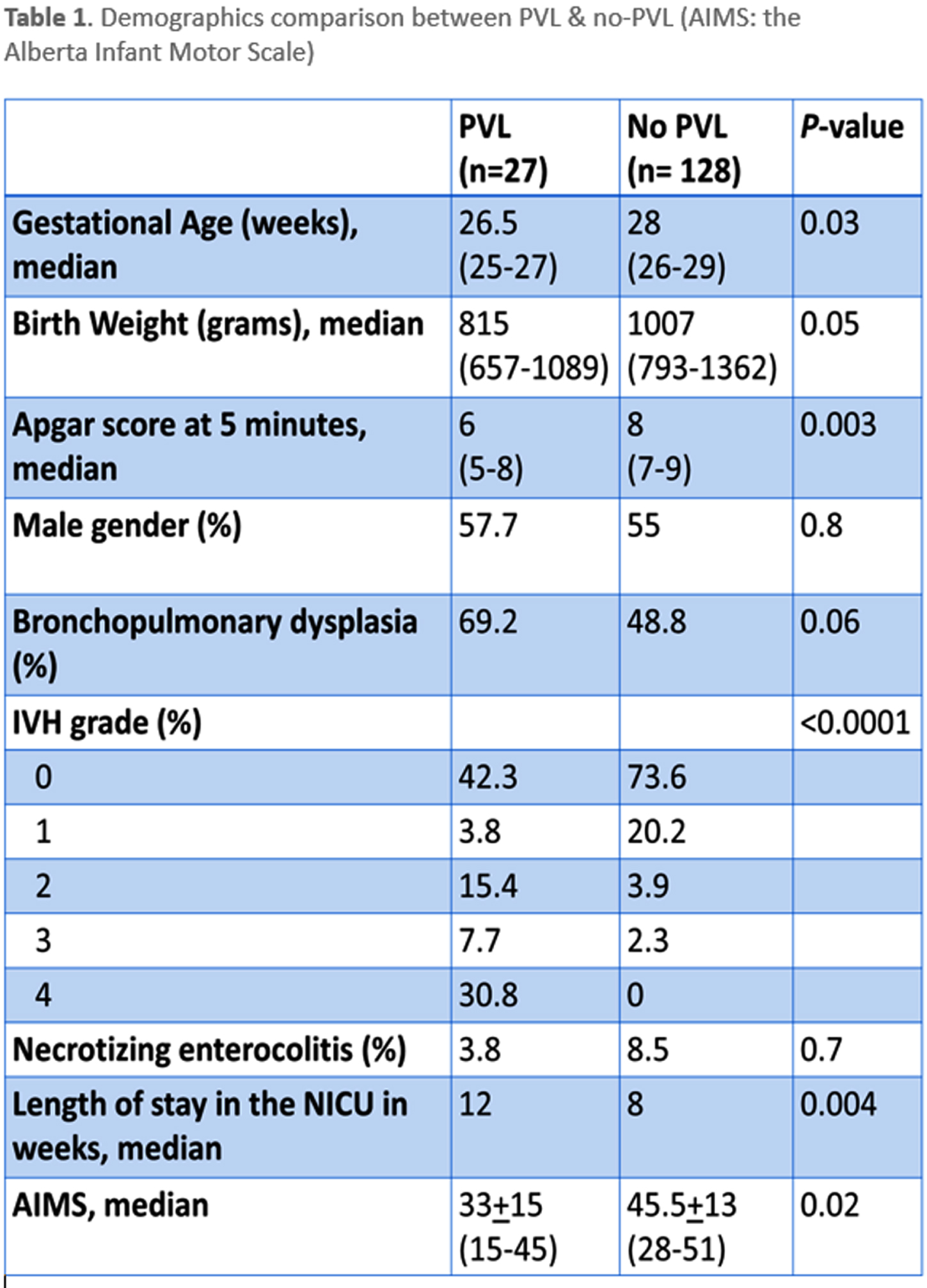
RESULTS: 155 newborns met the inclusion criteria. Within them, 27 (17%) had PVL based on HUS prior to discharge from the neonatal intensive care unit (NICU). 24 patients had grades 1-2 PVL while 3 had grade 3 based on serial HUS reviews. The mean gestational age was 26.5 ±2.3 weeks for PVL patients and 28 ±2.9 weeks for non-PVL (p=0.03). The mean birth weight for those without PVL was 1118 ±500 grams compared to 916 ±312 grams for PVL (p=0.01) (Table-1). EEG was performed on 15/27 patients with PVL at a mean age of 20 months corrected age vs. 17/128 patients without PVL at a mean age of 11.5 months corrected age. In the PVL group, EEG was normal in six patients (5/6 were grade 1), mildly slow background in two (one with grade 1 and one with grade 2). Three patients had excessive background slowing with multiple foci of excessive sharp wave discharges (three with grade 3 and two with grade 2 PVL). Patients with PVL had a trend towards worse EEG pattern (p= 0.2) when compared to no PVL. Worse PVL grade was associated with worse EEG pattern (p= 0.002).
CONCLUSION: PVL is a common brain injury in premature newborns. The relatively frequent association with an abnormal EEG, especially for high grade cystic PVL, should prompt providers to consider this test for seizure screening and early diagnosis and management.
Neonatal neuro-imaging findings and neurodevelopmental outcome at 24 months in moderate-late preterm infants: Follow-up analysis of the BIMP study
Boswinkel V1, Van Erkel F1, Nijholt I2, Boomsma M2, de Vries L3, Meijler G1
1Department of Neonatology, Isala, Zwolle, The Netherlands, 2Department of Radiology, Zwolle, The Netherlands, 3Department of Neonatology, University Medical Center Utrecht, Utrecht, The Netherlands
BACKGROUND: Moderate-late preterm (MLPT) children, born between 32 and 37 weeks of gestation, account for 80% of the 15 million children born prematurely per year worldwide (1). MLPT infants have a higher risk of neurodevelopmental and behavioral problems compared to full-term infants (2-4). During the last trimester of pregnancy, the fetal brain undergoes rapid growth and development and is therefore susceptible to injury and suboptimal development (5,6). So far, few studies assessed the relationship between neuro-imaging findings and neurodevelopment in MLPT children. These studies present conflicting results (7,8). Knowledge of this relationship may help to predict neurodevelopmental or behavioral problems and may thus enable early interventions to improve functional outcome. Our aim was to determine whether there is an association between neuro-imaging findings and neurodevelopment in MLPT infants.
METHODS: The Brain Imaging in Moderate-Late Preterm infants (BIMP) study is a prospective cohort study (9). Infants between 32+0 and 35+6 weeks’ gestation were included and underwent serial cranial ultrasonography (cUS) and a single MRI examination at term equivalent age (TEA). cUS and MRI examinations were divided into normal (no lesions) and abnormal. At corrected age of 24 months, neurodevelopment was assessed using three validated parent reported questionnaires: the Ages and Stages Questionnaire (ASQ) (10), Child Behavior Checklist (CBCL) (11) and Modified Checklist for Autism in Toddlers (M-Chat)(12). Outcome was suboptimal if a score was £ 2SD for the ASQ, 3 60 for the CBCL and 3 3 for the M-Chat. The results of the questionnaires were combined to a composite outcome i.e. if one of the results was suboptimal, the composite outcome was considered suboptimal. Associations between neuro-imaging findings and neurodevelopmental outcome were assessed with logistic regression analysis. We corrected for multiple comparisons using the Bonferroni correction.
RESULTS: In 141 MLPT infants follow-up was completed. Of the 141 children 40% were moderate preterm (MP) and 60% late preterm (LP). Of the 141 children 94% underwent serial cUS and 81% MRI. Abnormalities were seen on serial cUS and MRI in respectively 67% and 60% of the 141 children. For the ASQ and CBCL, respectively 23% and 13% of the children had a suboptimal score on one of the subdomains. None of the children had a suboptimal score on the M-Chat. In 31% of the children the composite outcome was suboptimal. No significant association was found between imaging findings and neurodevelopmental outcome. A significant association was found between suboptimal neurodevelopment and low educational level of mother and father respectively p=0.022 and p=0.047, however significance was revoked after multiple comparison correction.
CONCLUSION: Although follow-up analysis showed that nearly one in three MLPT children had a composite suboptimal outcome, we did not find a significant association between brain lesions on cUS and/or MRI and neurodevelopmental outcome at 24 months corrected age as assessed by parental questionnaires.
REFERENCES
[1] Chawanpaiboon S, Vogel J, Moller A, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health 2019;7(1):e37-e46.
[2] Voigt B, Pietz J, Pauen S, Kliegel M, Reuner G. Cognitive development in very vs. moderately to late preterm and full-term children: can effortful control account for group differences in toddlerhood? Early Hum Dev 2012;88(5):307-313.
[3] Johnson S, Evans TA, Draper ES, Field DJ, Manktelow BN, Marlow N, et al. Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch Dis Child Fetal Neonatal Ed 2015;100(4):F301-F308.
[4] Hochstedler KA, Bell G, Park H, Ghassabian A, Bell EM, Sundaram R, et al. Gestational Age at Birth and Risk of Developmental Delay: The Upstate KIDS Study. Am J Perinatol 2020.
[5] Kostović I, Sedmak G, Judaš M. Neural histology and neurogenesis of the human fetal and infant brain. Neuroimage 2019r;188:743-773.
[6] Raybaud C, Ahmad T, Rastegar N, Shroff M, Al Nassar M. The premature brain: developmental and lesional anatomy. Neuroradiology 2013;55(2):23-40.
[7] Nakasone R, Fujioka K, Kyono Y, Yoshida A, Kido T, Suga S, et al. Neurodevelopmental Outcomes at 18 Months of Corrected Age for Late Preterm Infants Born at 34 and 35 Gestational Weeks. Int J Environ Res Public Health 2021;18(2):640.
[8] Cheong JLY, Thompson D, Spittle A, Potter C, Walsh J, Burnett A, et al. Brain Volumes at Term-Equivalent Age Are Associated with 2-Year Neurodevelopment in Moderate and Late Preterm Children. J Pediatr 2016;174:91-97.e1.
[9] Boswinkel V, Krüse-Ruijter MF, Nijboer - Oosterveld J, Nijholt IM, Edens MA, Mulder - de Tollenaer SM., et al. Incidence of brain lesions in moderate-late preterm infants assessed by cranial ultrasound and MRI: The BIMP-study. Eur J Radiol 2021;136:109500.
[10] quires J, Bricker D. Ages & Stages Questionnaires®, Third Edition (ASQ®-3): A Parent-Completed Child Monitoring System. Baltimore: Paul H. Brookes Publishing Co., Inc; 2009.
[11] Achenbach TM, Rescorla L. Manual for the Child Behavior Checklist. Preschool Forms and Profiles. : Burlington VT: University of Vermont Department of Psychiatry; 2000.
[12] Robins DL, Fein D, Barton M. The Modified Checklist for Autism in Toddlers, Revised with Follow-Up (M-CHAT-R/F). 2009.




