COVID-19 via intrauterine transmission in a critically ill preterm infant: A case report
Abstract
A preterm infant was born emergently at 29 weeks gestation to a mother with active coronavirus disease 2019 (COVID-19). Clinical presentation and evaluation were consistent with in utero transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The neonate experienced progressive, refractory respiratory failure and catastrophic intracranial hemorrhage which ultimately led to limitation of care.
1Introduction
The coronavirus disease 2019 (COVID-19) pandemic, resulting from infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to cause widespread disease globally. Despite the total number of global COVID-19 cases now exceeding 601 million, data regarding maternal transmission to neonates remains limited. Historically, respiratory viruses similar to SARS-CoV-2 such as SARS-CoV or Middle East respiratory syndrome coronavirus are not easily transmitted in utero. Initially thought to rarely infect neonates [1], a growing number of case reports have described suspected congenital or intrapartum-acquired neonatal SARS-CoV-2 [2–19]. To date, documented infection in the very preterm infant (<32 weeks gestational age) represents an extremely small subset of reported cases; and each of those infants survived the neonatal period. Here we present the case of a premature infant born at 29 weeks with proposed in utero acquisition of SARS-CoV-2, outlining his clinical course and drawing attention to the potentially catastrophic effects of COVID-19 disease in the premature neonate.
2Case report
A 29-year-old G1P0 mother presented at 29 1/7 weeks with cough in the setting of active COVID-19 infection and new onset vaginal bleeding with decreased fetal movement. Maternal history was significant for mild COVID-19 disease diagnosed five days prior. Maternal admission labs were significant for a positive SARS-CoV-2 nucleic acid amplification test (NAAT), negative SARS-CoV-2 IgG and coagulation studies consistent with disseminated intravascular coagulopathy (DIC). Her prenatal labs were unremarkable; her Group B streptococcal status was unknown. Maternal vital signs were normal but fetal monitoring was non-reassuring. An emergent Caesarean section delivery was performed due to suspected placental abruption after one dose of betamethasone one hour prior to delivery. Fetal heart tones were in the range of 50–60 beats per minute (bpm) in the operating room. The amniotic fluid was clear; intraoperative findings were consistent with placental abruption. The placental pathology report revealed acute intervillositis with microabscess formation as well as diffuse subchorionic fibrin deposition. The maternal surface was intact and there was no evidence of villitis, chorioamnionitis or funisitis. Neither placental tissue nor amniotic fluid were evaluated for SARS-CoV-2. Postoperatively the mother required multiple rounds of blood products for treatment of DIC. She required oxygen after delivery for less than 24 hours and was discharged home on post-operative day four.
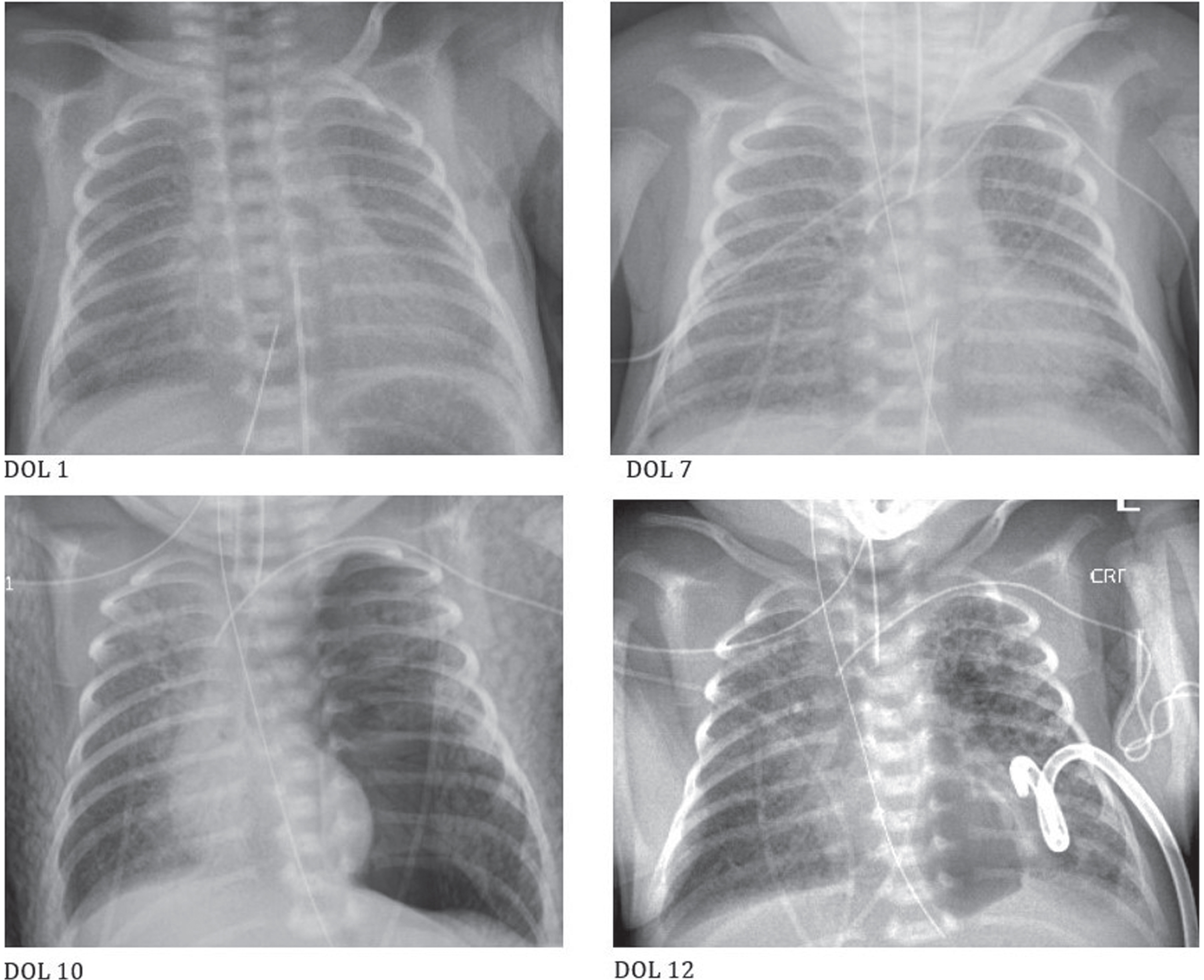
The 1460-gram appropriate for gestational age male infant was initially apneic with a heart rate of 40 bpm. Heart rate responded to positive pressure ventilation via Neopuff and with the return of spontaneous respirations, the infant was placed on nasal continuous positive airway pressure (CPAP)+5 and transported to the neonatal intensive care unit on a fraction of inspired oxygen (FiO2) of 0.35. APGAR scores were 1 at 1 minute of life and 8 at 5 minutes of life. Cord gases were 7.13/55/20/18/-11 (arterial) and 7.13/54/26/18/-11 (venous). Infant physical examination was notable for pallor and decreased capillary refill. He was escalated to nasal CPAP+6. Umbilical arterial and venous catheters were placed. The initial arterial blood gas was 7.17/43/56/16/-12 with a lactate of 8.9 and a glucose of 20, which resolved with the initiation of dextrose-containing fluids. His initial complete blood count (CBC) showed a white blood count (WBC) of 17,900/mm3 with 27% segmented neutrophils, 61% lymphocytes, and 10% monocytes, a hematocrit of 42% and a platelet count of 278,000/mm3. A blood culture was obtained, and empiric antibiotics were initiated. The admission chest X-ray showed extensive, diffuse ground glass opacities throughout both lungs (Fig. 1). Oxygen requirement gradually increased to 0.4; the infant was intubated and given surfactant at three hours of life. Over the next 24 hours, he received a second dose of surfactant and ventilatory support was weaned. He was extubated to CPAP+6 on day of life (DOL) 1 with a blood gas of 7.33/39/42/21/-5 and a FiO2 requirement of 0.23–0.30. However, his work of breathing quickly worsened and when his oxygen requirement reached the 0.60 s he was re-intubated and given a third dose of surfactant. He continued to ventilate well but his oxygen requirement remained labile and by DOL 3 he required a FiO2 of up to 0.55.
Fig. 1
Progression of chest radiographs over first twelve days of life (DOL).
The metabolic acidosis noted on admission slowly resolved over the first three days. An initial brain ultrasound on DOL 1 showed possible bilateral grade I intraventricular hemorrhage (IVH). Echocardiogram (echo) obtained on DOL 2 showed normal cardiac anatomy and function as well as a patent foramen ovale and patent ductus arteriosus (PDA), both with left to right shunting. On DOL 2, the infant received his first of multiple packed red blood cell transfusions. According to the Centers for Disease Control and Prevention (CDC) recommendations and hospital protocol, the infant was tested for SARS-CoV-2 at 24 hours of life with a nasopharyngeal swab sent for NAAT, which was positive. On DOL 3, his metabolic acidosis acutely worsened. A CBC revealed a WBC of 5,700/mm3 with 59% segmented neutrophils, 31% lymphocytes, and 10% monocytes, a hematocrit of 35% and a platelet count of 179,000/mm3. A blood culture was resent, and infant was restarted on empiric antibiotics. Repeat SARS-CoV-2 testing was sent on DOL 3; both nasopharyngeal swab and tracheal aspirates resulted as positive.
By DOL 4 the infant was stable on minimal conventional ventilatory support, ventilating well with FiO2 in 0.30 s. That day, his temperature began to increase and remained elevated thereafter. Over the next few days, his respiratory status began to deteriorate. A repeat echo was performed on DOL 5, which demonstrated no PDA and no evidence of significant pulmonary hypertension. On DOL 7, chest radiograph showed worsening granular parenchymal opacities (Fig. 1). The FiO2 requirement was up to 0.65-0.75 on mean airway pressures of 12-14 and ventilation was worsening; thus, the infant was converted to high-frequency oscillatory ventilation (HFOV). By DOL 8 he was requiring up to 1.00 FiO2. Dexamethasone was started using the Dexamethasone: A Randomized Trial (DART) protocol (0.15 mg/kg/day, tapered over ten days). A third blood culture was collected, and empiric antibiotics were restarted. CBC revealed a WBC of 7,900/mm3 with 52% segmented neutrophils, 1% bands, 36% lymphocytes, and 11% monocytes, a hematocrit of 27% and a platelet count of 143,000/mm3. C-reactive protein (CRP) was < 2.9 on DOL 9 and again on DOL 11. There appeared to be some mild improvement in respiratory status after the initiation of dexamethasone. However, on DOL 10 the infant developed a large pneumothorax requiring pigtail drain placement (Fig. 1). That same day, a brain ultrasound was performed showing right sided grade 4 IVH with large frontal-parietal hemorrhage, compression of right lateral ventricle with a left midline shift, and right temporal horn enlargement. The left side demonstrated grade 3 IVH with moderately enlarged lateral and third ventricles. Coagulation studies demonstrated a prothrombin time (PT) of 13.4 sec, an international normalized ratio (INR) of 1.03, fibrinogen level of 229 mg/dL, and a partial thromboplastin time (PTT) of 29.4 sec. The infant again tested positive for SARS-CoV-2 on DOL 10 via nasopharyngeal swab.
On DOL 11, the infant remained on stable HFOV settings and FiO2 requirement of 0.70-0.80 s after drainage of the pneumothorax. He was on day four of steroid treatment. SARS-CoV-2 IgG and IgM were sent, both of which later resulted as positive. The parents were updated about the brain imaging results and status; they requested a family meeting with the care team. On DOL 12, the infant had an increase in FiO2 requirement to 1.00 with saturations in the 70-90% range. The parents opted for redirection of care with withdrawal of support. Parents declined an autopsy.
3Discussion
The potential for transmission of SARS-CoV-2 infection from mother to infant has been of great concern since the emergence of the pandemic. Early data from small populations suggested that the risk of infection in the neonate was negligible [1, 20]. Subsequent systematic reviews involving large numbers of mother-infant dyads found positivity rates in infants ranging from 1.6–5.7% [21–23]. More recently, a living systematic review and meta-analysis found that less than 2 % of babies born to mothers with a diagnosis of SARS-CoV-2 also test positive for SARS-CoV-2 [24]. When cases were limited to antenatal or intrapartum exposure to the virus, rates were found to be lower (1%). Data has shown that clinically, the vast majority of infants testing positive for SARS-CoV-2 do very well [13, 23, 25–28]. However, reports have emerged suggesting that some infants do indeed present with varying degrees of clinical disease, ranging from mild to severe.
Infection resulting in maternal viremia within 14 days of delivery presents a theoretical risk of intrauterine transmission via placental disruption or viral material reaching the amniotic fluid [29]. It became imperative to develop a system to describe such cases but identifying an international, standardized method of defining and categorizing of the timing of mother-to-infant transmission was a challenge. In February of 2021, the World Health Organization (WHO) published a scientific brief proposing such as system [30]. The WHO categories for transmission are based on suspected timing; in utero, intrapartum, and postnatal. Based on our patient’s fetal exposure and viral persistence/immune response, we classified the case as confirmed transmission (Fig. 2). With small deviations in timing, he had a positive reverse transcription-polymerase chain reaction (RT-PCR) from a non-sterile sample (nasopharyngeal) at 27 hours of life (HOL) (not < 24 HOL) and he also had a positive RT-PCR from a sterile sample (tracheal aspirate) at 70 HOL (just outside of the 24–48 HOL range). Of note, the infant had remained NPO since birth due to acidosis thus he had not been exposed to maternal breast milk. Mother also never had physical contact with the baby after birth.
Fig. 2
WHO Categorization of the timing of in utero transmission of SARS-CoV-2 [https://www.who.int/publications/i/item/WHO-2019-nCoV-mother-to-child-transmission-2021.1].
![WHO Categorization of the timing of in utero transmission of SARS-CoV-2 [https://www.who.int/publications/i/item/WHO-2019-nCoV-mother-to-child-transmission-2021.1].](https://content.iospress.com:443/media/npm/2022/15-4/npm-15-4-npm221094/npm-15-npm221094-g002.jpg)
Our patient did have positive serology for IgM sent at 12 days of life. Unfortunately, no testing was sent prior to seven days of life, a range put forth by the WHO as a criterion for possible in utero transmission.
The placental pathology report revealed acute intervillositis with microabscess formation as well as diffuse subchorionic fibrin deposition. Case reports have demonstrated both acute [31, 32] and chronic [31, 33] intervillositis in placentas of mothers with COVID-19. Similarly, the two reports demonstrating acute intervillositis also involved emergent Cesarean deliveries due to non-reassuring fetal heart rate and the mothers also had DIC [31, 32]. However, a recent systematic review and meta-analysis of 699 placentas derived from women with SARS-CoV-2 infection suggested that the only associated pathologic placental finding was an increased prevalence of increased perivillous fibrin deposition [34].
To date, there is limited data on COVID-19 infection in the very preterm infant (<32 weeks gestational age). Cases reports have described infants 26–31 weeks at birth who tested positive for SARS-CoV-2 (Table 1). Maternal disease in these cases ranged from asymptomatic to severe. Table 1 also includes data on two infants who did not test positive themselves, but maternal and placental sources were positive for SARS-CoV-2 and infant pathology was thought to be subsequent to maternal COVID-19 disease [11, 16]. Several of the infants testing positive for SARS-CoV-2 had clinical courses typical of prematurity. While some experienced complications unexpected for preterm infants, all of those who tested positive for SARS-CoV-2 survived to discharge.
Table 1
COVID-19 infection in the very preterm infant (<32 weeks GA)
| Maternal disease | GA | ANS | Neonate SARS-CoV-2 positive? | Unexpected neonatal complications | |
| Piersigilli 2020 | HELLP syndrome | 26 weeks | Yes | Yes | None |
| Schoenmakers 2020 | Fetal distress | 31 weeks | No | No | Severe multi-organ failure, inflammatory multisystem-like syndrome including coronary artery ectasia. Positive SARS-CoV-19 from maternal and placental sources; neonatal tests were negative. Neonatal pathology thought to be due to a placental inflammatory reaction from maternal COVID-19 infection. |
| Zeng 2020 | PROM, fetal distress | 31 weeks | NR | Yes | In addition to RDS and pneumonia, infant also had Enterobacter sepsis with coagulopathy. |
| Al-Lawama 2021 | NR | 30 weeks | NR | Yes | Typical course until DOL 9; developed severe hypoxic respiratory failure requiring 100% FiO2. |
| Disse 2021 | PROM | 29 week triplets | Yes | Yes | None |
| Favre 2021 | Decreased fetal movement and NRFHT | 29 and 32 weeks | NR | Yes | PVL on head ultrasound on day of life 1 and 3 respectively |
| Kumar 2021 | Placental abruption | 27 weeks | Yes | Yes | Typical course until DOL 5; developed severe hypoxic respiratory failure requiring 100% FiO2. |
| Ng 2021 | Preterm labor | 29 weeks | Yes | Yes | None |
| Rabiei 2021 | Placental insufficiency | 29 week triplets | Yes | No, No, Yes | One died on day 3 and another on day 13; deaths attributed to complications of prematurity; both tested negative. The surviving infant tested positive but no complications from COVID-19 disease. |
ANS, antenatal steroids; GA, gestational age; HELLP, hemolysis, elevated liver enzymes, low platelet count; PROM, preterm rupture of membranes; NR, not reported; RDS, respiratory distress syndrome; NRFHT, non-reassuring fetal heart tones.
Complicating the assessment of the role that COVID-19 pneumonia played in our infant’s clinical course is the lack of antenatal steroid administration, which we know decreases the incidence/severity of respiratory distress syndrome (RDS) and mortality in preterm infants. Thus, we must consider the role that RDS alone, without the benefit of antenatal steroid administration in this case, certainly played in the severity of his respiratory course. While the infant did receive multiple doses of surfactant, we know that infants who received antenatal steroids respond better to surfactant treatment than infants who have not. Furthermore, lung injury resulting from mechanical ventilation at higher tidal volumes is decreased in lungs exposed to antenatal steroids. Therefore, we should also consider how significantly the lack of antenatal steroid administration affected his lungs’ ability to withstand the additional insult of COVID-19 pneumonia, given the assumption of ongoing surfactant inactivation in this scenario and the infant’s need for steadily increasing ventilatory support throughout his course. Maternal placental abruption along with fetal bradycardia also could have contributed to the severity of lung disease as there is an association between such complications and RDS. However, in our case the respiratory status was consistent with typical RDS up until deterioration on DOL 4, which also coincided with the onset of elevated temperatures in the setting of positive SARS-CoV-19 testing.
In consultation with our pediatric infectious disease colleagues, it was decided that at that time there was not sufficient evidence for use of remdesivir (RDV), an RNA dependent inhibitor of RNA polymerase in coronaviruses, in our very preterm neonate. Upon review of the subsequent literature, cases of use in infants in whom RDV treatment was well tolerated have been reported. Initially used in an infant with Ebola infection [35], more recently it has been given in cases of infants with COVID-19. In April 2022, the U.S. Food and Drug Administration expanded the approval of RDV to include pediatric patients 28 days of age and older weighing at least three kilograms. However, use in the premature neonatal population is still considered experimental. RDV has been used without adverse events in three former preterm neonates presenting with acute decompensation in the setting of COVID-19 infection [19, 36]. Only one of those infants was less than 28 days old and the youngest corrected gestational age was 35 2/7 weeks. All three went on to recover completely and were discharged home. None of the patients experienced any of the known RDV-related adverse drug reactions. However, it should be noted that all three infants were also treated with corticosteroids.
Early in the pandemic, corticosteroid use in the adult COVID-19 population was discouraged due to concern for decreasing the inflammatory response to viral infection noted previously with similar infections. Subsequently, steroids became a mainstay in the treatment of moderate to severe COVID-19 and are strongly recommended by the WHO [37]. However, the use of medications such as RDV and dexamethasone for treatment of COVID-19 in the pediatric and neonatal populations has been extrapolated from data in the adult population [38]. In adults, dexamethasone is only recommended for those with respiratory distress requiring oxygen or ventilatory support. Since our patient met those criteria and was quickly worsening from a respiratory standpoint, we made the choice to start dexamethasone therapy. We used the findings from the PREMILOC study to justify the use of early steroids in a premature infant [39], but chose dexamethasone instead of hydrocortisone due to the recommendations for adults.
4Conclusion
Although rare, in utero transmission of SARS-Cov-2 has been shown to occur. Our case heightens the concern that this form of vertical transmission could worsen the morbidity and mortality in neonates, especially in the steroid-naive, preterm infant. Efforts at preventing COVID-19 infection in the pregnant population could play an unquestionably key role in preventing such outcomes. Future research into therapeutic interventions for the preterm infant with COVID-19 would also be of value.
Acknowledgments
Many thanks to Steven Seidner, MD and Katherine Perez, PharmD for writing assistance and to Jorge Pablo Orezzoli, MD for technical assistance.
Funding source
No external funding for this manuscript.
Financial disclosure
The authors have indicated they have no financial relationships relevant to this article to disclose.
Conflict of interest
The authors have indicated they have no potential conflicts of interest to disclose.
References
[1] | Chen H , Guo J , Wang C , Luo F , Yu X , Zhang W , et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. (2020) ;395: :809–15. |
[2] | Sisman J , Jaleel MA , Moreno W , Rajaram V , Collins RRJ , Savani RC , et al. Intrauterine transmission of SARS-COV-2 infection in a preterm infant. Pediatr Infect Dis J. (2020) ;39: :e265–7. |
[3] | NG DC , Chin L , Choo PPL , Paramasivam U . COVID-19 in a premature infant. BMJ Case Ree. (2021) ;14: :243783. |
[4] | Alzamora MC , Paredes T , Caceres D , Webb CM , Valdez LM , La Rosa M . Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. (2020) ;37: :861–5. |
[5] | Zamaniyan M , Ebadi A , Aghajanpoor S , Rahmani Z , Haghshenas M , Azizi S . Preterm delivery, maternal death, and vertical transmission in a pregnant woman with COVID-19 infection. Prenat Diagn. (2020) ;40: :1759–61. |
[6] | Rabiei M , Soori T , Abiri A , Farsi Z , Shizarpour A , Pirjani R . Maternal and fetal effects of COVID-19 virus on a complicated triplet pregnancy: a case report. J Med Case Rep. (2021) ;15: :87. |
[7] | Farhadi R , Mehrpisheh S , Ghaffari V , Haghshenas M , Ebadi A . Clinical course, radiological findings and late outcome in preterm infant with suspected vertical transmission born to a mother with severe COVID-19 pneumonia: A case report. J Med Case Rep. (2021) ;15: :213. |
[8] | Engert V , Siauw C , Stock A , Rehn M , Wöckel A , Härtel C , et al. Severe brain damage in a moderate preterm infant as complication of post-COVID-19 response during pregnancy. Neonatology. (2021) ;118: :505–8. |
[9] | Kirtsman M , Diambomba Y , Poutanen SM , Malinowski AK , Vlachodimitropoulou E , Parks WT , et al. Probable congenital SARS-CoV-2 infection in a neonate born to a woman with active SARS-CoV-2 infection. CMAJ. (2020) ;192: :E647–50. |
[10] | Zeng L , Xia S , Yuan W , Yan K , Xiao F , Shao J , et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. Arch Pediatr Adolesc Med. (2020) ;174: :722–5. |
[11] | Schoenmakers S , Snijder P , Verdijk RM , Kuiken T , Kamphuis SSM , Koopman LP , et al. Severe acute respiratory syndrome coronavirus 2 placental infection and inflammation leading to fetal distress and neonatal multi-organ failure in an asymptomatic woman. J Pediatric Infect Dis Soc. (2021) ;10: :556–61. |
[12] | De Bernardo G , Giordano M , Zollo G , Chiatto F , Sordino D , De Santis R , et al. The clinical course of SARS-CoV-2 positive neonates. J Perinatol. (2020) ;40: :1462–9. |
[13] | Al-Lawama M , Badran E , Ghanim N , Irsheid A , Qtaishat H , Al-Ammouri I , et al. Perinatal transmission and clinical outcomes of neonates born to SARS-CoV-2-positive mothers. J Clin Med Res. (2021) ;13: :420–4. |
[14] | Farmer ML . A neonate with vertical transmission of COVID-19 and acute respiratory failure: a case report. Adv Neonatal Care. (2021) ;21: :482–92. |
[15] | Kumar V , Prasath A , Blanco C , Kenney P , Ostwald C , Meyer T , et al. Respiratory failure in an extremely premature neonate with COVID-19. Children (Basel). (2021) ;8: :477. |
[16] | Favre G , Mazzetti S , Gengler C , Bertelli C , Schneider J , Laubscher B , et al. Decreased fetal movements: a sign of placental SARS-CoV-2 infection with perinatal brain injury. Viruses. (2021) ;13: :2517. |
[17] | Mannix MK , Blood D , Gomez-Duarte OG , Davidson L . Necrotizing enterocolitis in a 34-week premature infant with COVID-19. Case Rep Infect Dis. (2021) ;2021: :1–4. |
[18] | Disse SC , Manuylova T , Adam K , Lechler A , Zant R , Klingel K , et al. COVID-19 in 28-week triplets caused by intrauterine transmission of SARS-CoV-2-case report. Front Pediatr. (2021) ;9: :812057. |
[19] | Frauenfelder C , Brierley J , Whittaker E , Perucca G , Bamford A . Infant With SARS-CoV-2 infection causing severe lung disease treated with remdesivir. Pediatrics. (2020) ;146: :1. |
[20] | Zhu H , Wang L , Fang C , Peng S , Zhang L , Chang G , et al. Clinicalanalysis of 10 neonates born to mothers with -nCoV pneumonia. Transl Pediatr. (2020) ;9: :51–60. |
[21] | Kotlyar AM , Grechukhina O , Chen A , Popkhadze S , Grimshaw A , Tal O , et al. Vertical transmission of coronavirus disease A systematic review and meta-analysis. Obstet Gynecol. (2021) ;224: :35,53.e3. |
[22] | Goh XL , Low YF , Ng CH , Amin Z , Ng YPM . Incidence of SARS-CoV-2 vertical transmission: A meta-analysis. Arch Dis Child Fetal Neonatal Ed. (2021) ;106: :112–3. |
[23] | Raschetti R , Vivanti AJ , Vauloup-Fellous C , Loi B , Benachi A , De Luca D . Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat Commun. (2020) ;11: :5164–9. |
[24] | Allotey J , Chatterjee S , Kew T , Gaetano A , Stallings E , Fernandez-García S , et al. SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: Living systematic review and meta-analysis. BMJ. (2022) ;376: :e067696. |
[25] | Woodworth KR , Olsen EO , Neelam V , Lewis EL , Galang RR , Oduyebo T , et al. Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy –SET-NET, 16 Jurisdictions, March 29-October 14 . MMWR Morb Mortal Wkly Rep;(2020) ;69: :1635–40. |
[26] | Angelidou A , Sullivan K , Melvin PR , Shui JE , Goldfarb IT , Bartolome R , et al. Association of maternal perinatal SARS-CoV-2 infection with neonatal outcomes during the COVID-19 pandemic in Massachusetts. JAMA Netw Open. (2021) ;4: :e217523. |
[27] | Congdon JL , Kair LR , Flaherman VJ , Wood KE , LoFrumento MA , Nwaobasi-Iwuh E , et al. Management and early outcomes of neonates born to women with SARS-CoV-2 in 16 U. S. hospitals. Am J Perinatol. (2021) ;38: :622–31. |
[28] | Flaherman VJ , Afshar Y , Boscardin WJ , Keller RL , H Mardy A , Prahl MK , et al. Infant outcomes following maternal infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): First report from the Pregnancy Coronavirus Outcomes Registry (PRIORITY) study. Clin Infect Dis. (2021) ;73: :e2810–3. |
[29] | Blumberg DA , Underwood MA , Hedriana HL , Lakshminrusimha S . Vertical transmission of SARS-CoV- What is the optimal definition? Am J Perinatol. (2020) ;37: :769–72. |
[30] | WHO. Definition and categorization of the timing of mother-to-child transmission of SARS CoV-2. Scientific Brief. [Internet] [updated 8 Feb 2021; cited 2 May 2022]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-mother-to-child-transmission-2021.1. |
[31] | Mongula JE , Frenken MWE , van Lijnschoten G , Arents NLA , de Wit-Zuurendonk LD , Schimmel-de Kok A.P.A , et al. COVID-19 during pregnancy: non-reassuring fetal heart rate, placental pathology and coagulopathy. Ultrasound Obstet Gynecol. (2020) ;56: :773–6. |
[32] | Vivanti AJ , Vauloup-Fellous C , Prevot S , Zupan V , Suffee C , Do Cao J , et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. (2020) ;11: :3572–6. |
[33] | Schwartz DA , Levitan D . Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infecting pregnant women and the fetus, intrauterine transmission and placental pathology during the coronavirus disease (COVID-19) pandemic: It’s complicated. Arch Path Lab Med. (2021) ;145: :925–8. |
[34] | Hessami K , Aagaard KM , Castro EC , Arian SE , Nassr AA , Barrozo ER , et al. Placental vascular and inflammatory findings from pregnancies diagnosed with coronavirus disease 2019: A systematic review and meta-analysis. Am J Perinatol. 2022. |
[35] | Dornemann J , Burzio C , Ronsse A , Sprecher A , De Clerck H , Van Herp M , et al. First newborn baby to receive experimental therapies survives Ebola virus disease. J Infect Dis. (2017) ;215: :171–4. |
[36] | Saikia B , Tang J , Robinson S , Nichani S , Lawman KB , Katre M , et al. Neonates With SARS-CoV-2 infection and pulmonary disease safely treated with remdesivir. Pediatr Infect Dis J. (2021) ;40: :e194–6. |
[37] | WHO. Therapeutics and COVID-19: Living guideline. [Internet] [updated 22 April 2022; cited 2May 2022]. Available from: https://www.who.int/publications/i/item/WHO2019-nCoV-therapeutics-2022.3. |
[38] | Younis NK , Zareef RO , Fakhri G , Bitar F , Eid AH , Arabi M . COVID- Potential therapeutics for pediatric patients. Pharmacol Rep. (2021) ;73: :1520–38. |
[39] | Baud O , Maury L , Lebail F , Ramful D , El Moussawi F , Nicaise C , et al. Effect of early low-dose hydrocortisone on survival without bronchopulmonary dysplasia in extremely preterm infants (PREMILOC): A double-blind, placebo-controlled, multicentre, randomised trial. Lancet. (2016) ;387: :1827–36. |




