Abstracts of the 27th European Workshop on Neonatology, Rotterdam, The Netherlands, September 1-3, 2019
Congenital neonatal pneumonia - A retrospective analysis of our experience
Stanislava Hitrova-Nikolova, Slancheva B, Jekova N, Radulova P, Vakrilova L, Shopova E, Pramatarova T, Popivanova A, Dimitrova V.
Department of Neonatology,University Hospital of Obstetrics and Gynecology “Maichin dom”, Faculty of Medicine, Medical University of Sofia, Bulgaria
Introduction: Neonatal pneumonia is one of the most common inflammatory processes in newborns. Microbiological examination of the lower respiratory tract identifies and guides the selection of antibacterial therapy. To analyze tracheal aspirates in newborns with congenital pneumonia, and compare them with clinic, laboratory and radiographic changes.
Methods: A retrospective study was carried out from 1.01.2018 to 31.12.2018 at Neonatology Clinic, University O&G hospital “Maichindom”, Sofia. The study included 194 newborns treated immediately after birth by invasive mechanical ventilation in the NICU. The infants were divided into groups according to their body weight. Tracheal aspirates were taken immediately after birth. We analyzed them, along with clinical-laboratory data, the treatment and the average stay.
Results: 22 positive primary tracheal aspirates (11%) were isolated with predominant Gram-negative bacteria (E.coli, S.marcescens, Achromobacter spp),and isolates of S.epidermidis, Str.viridans, C.parapsilosis. In 89% of tracheal aspirates taken immediately after birth were sterile. All patients had radiographic pulmonary changes and most of them-inflammatory activity(increased CRP-66% and leukopenia-36%).132 patients(68%)were treated with Surfactant. The following complications were identified:10 infants with pneumothorax, 2-with late Candida sepsis and acute renal failure. Two of the newborns were diagnosed with CMV and HSV2 infection with active viral replication(PCR).Standard antibiotic treatment-10day course (Ampisulbactam + Amikin) was administered to all patients. In 72% there were follow-up courses according to clinical complications and antimicrobial susceptibility.
Conclusions: Standard microbiological tests find out the specific bacterial agent, but others such as chlamydia, viruses and parasites remain undiagnosed. The antibiotic prophylaxis of mothers at the time of delivery reduces etiological evidence of congenital pneumonia.
Changing trend in bacterial etiology and antibiotic resistance in Early-Onset Neonatal Sepsis
Jekova N., Shopova E., Hitrova – Nikolova St.
Department of Neonatology, University maternity Hospital “Maichin Dom” – Sofia, Bulgaria
Introduction: Neonatal sepsis is an important cause of neonatal morbidity and mortality. The spectrum of microbial etiology of neonatal septicaemia varies from region to region and even varies in different hospitals of the same region. In addition, one organism or group of organisms may be replaced by others over a period of time. The present study examines the trends in bacterial profile and antibiotic resistance of the organisms causing early-onset sepsis in the neonates at a tertiary perinatal center in Bulgaria.
Methods: A retrospective laboratory-based analysis of blood cultures obtained from Neonatal Intensive Care Unit of a tertiary care hospital in Sofia was done for the period of 2008–2018, divided into two phases.
Results: A total of 3335 isolates were considered. Over time, methicillin-resistant (MR) organisms have replaced methicillin-sensible (MS) as frequent isolates. Initially, there was predominance of MS Staphylococcus aureus and MS Staphylococcus epidermidis, which recently has been changed with coagulase negative-Staphylococcus aureus and MR Staphylococcus epidermidis. Growing resistance against the first and second line of drugs has been noted, including MR Staphylococcus aureus and vancomycin-resistant Enterococcus and MRStaphylococcus epidermidis.
Conclusion: The etiological profile of neonatal sepsis has changed considerably in the past 10 years. High resistance against common drugs necessitates continued surveillance and review of empirical antibiotic policy for neonatal sepsis. These steps are important to effectively curtail the surge of further antibiotic resistance.
Pertussis antibody levels in infants and their mothers receiving combined Tetanus-Diphtheria toxoid and acellular pertussis vaccine during pregnancy
Mine Özdil, Cemile Sönmez, Ebru Alıcı Davutoğlu, Murat Tuğberk Bakar, Rıza Madazlı, Mehmet Vural, Yıldız Perk
Introduction: The pertussis is an important cause of morbidity and mortality in infants below two months of age and these high risk babies are dependent on maternally derived antibodies until completion of the first immunization series. The present study was performed to search for the vaccine responses of mothers administered combined tetanus-diphtheria toxoid and acellular pertussis vaccine (Tdap) during pregnancy and of their late preterm and term newborns.
Methods:A total of 70 pregnants were administered Tdap vaccine (Boostrix, GSK,) between 27-33 gestational weeks of pregnancy in this clinical study. The IgG antibodies against pertussis toxin (PT) and filamentous hemaglutinin (FHA) in maternal blood before vaccination and in both maternal and umbilical cord blood after vaccination were studied using the in-house ELISA (enzyme linked immunosorbent assay) method. The geometric mean concentrations (GMC) and placental transfer ratios of antibodies were measured.
Results: Seventy pregnants with mean ages of 29,59± 4,70 years received Tdap vaccine at 28,6± 1,31 gestational weeks. The anti-PT IgG GMCs were detected as 8,01 IU/ml (%95 CI: 4,41-11,60) and 39,48 IU/ml (%95 CI: 29,02-49,93), the anti-FHA IgG GMC were detected as 122,24 IU/ml (%95 CI: 74,02-170,46) and 183,97 IU/ml (%95 CI: 118,68-249,26) before and after vaccination at maternal blood, respectively (p=0.001 ve p<0.001). The anti-PT and anti-FHA IgG GMCs of cord blood after vaccination was 25,15 IU/ml (%95CI: 18,07-32,22) and 118,77 IU/ml (%95 CI: 84,79-152,75)24,98 IU/ml, respectively. A positive correlation was found between maternal and cord blood anti-PT IgG levels and anti-FHA IgG levels (r=0.559 and r=0.715, respectively). Plasental transfer ratios of Anti-PT ve anti-FHA IgG antibodies were detected as 0.65 ve 0.62, respectively.
Conclusion: Maternal pertussis immunization results with higher antibody levels in newborns. Immunization against pertussis during pregnancy could be effective in the protection of infants especially below two months of age.
Point Prevalence Survey on Antibiotic use in Portuguese Neonatal Intensive Care Units
MT. Neto, A. Almeida, A. Pereira, A.L Maia, C. Resende, L. Martins, E.Mendes, M. Abrantes, M. Cabral, M.Marçal, M.Tuna, O.Voutsen, S.Pissarra,T. Caldeira, T.Cezanne, T.Jacinto
Portuguese Society of Neonatology
Introduction: A point-prevalence survey (PPS) was performed in Portuguese NICUs to evaluate antibiotic prescription.
Methods: Inquiry on antibiotics prescription covering seven days (October 2017, 16th to 22nd) was sent to 18 NICUs. Participation was voluntary and anonymous.
Results: Participation rate was 77.8% (14/18 NICUs).Out of the 234 patients enrolled (median of gestational age and birth weight 33weeks and 1825g), 67 were under antibiotics (28.6%) for a total of individual antibiotic prescriptions of 128 in 53 associations; 4 patients had two cycles of antibiotics during the week; 4 patients had only one antibiotic – acyclovir, meropenem, amoxicillin + clavulanic acid, vancomycin; 43 had association of two antibiotics the most frequent being ampicillin + gentamicin (n=32); 8 had 7 different combinations of three antibiotics among ampicillin, gentamicin, metronidazol, meropenem, cefotaxime and vancomycin. In 31 out of the 67 patients with antibiotics, prescription intended to treat early-onset infection/infectious risk (47%) . Days free of antibiotics were calculated to be 1104 out of 1471 in-hospital days (75.1%). Rate of antibiotics use was 25%. Four out of the 53 prescriptions in association may be considered as inadequate. Eleven patients had positive cultures: Coagulase negative Staphylococcus, Enterobacter cloacae, E. coli, S.aureus; Kl pn ESBL.
Conclusion: Prevalence of antibiotic prescription was low and days free of antibiotics was at a good level. As it would be expected according to the main reason to prescribe antibiotics the most common association was ampicillin and gentamicin. Four out of the 53 associations could be subject of discussion.
Intrauterine growth restriction results in respiratory muscle dysfunction and exercise intolerance in childhood
G. Dimitriou, A. Vervenioti, S. Fouzas
Neonatal Intensive Care Unit & Pediatric Pulmonology Unit, Department of Pediatrics, University of Patras Medical School, Patras, Greece
Introduction: An epidemiological link exists between intrauterine growth restriction (IUGR) and exercise intolerance later in life. Our aim was to explore whether IUGR is associated with reduced exercise capacity in childhood due to a sustained skeletal and/or respiratory muscle dysfunction.
Methods: 16 children (age 8 ± 1.1 years; range 7-11 years; 9 boys) born as asymmetric IUGR (birth weight <10th percentile; gestational age [GA] 34-38 weeks) were compared with 16 matched for age, sex and GA controls. Body mass index (BMI) and body composition (bioelectrical impedance) were determined. Exercise tolerance was assessed by means of maximum oxygen consumption (VO2max, maximal cycle ergometer protocol). Respiratory muscle function was evaluated by means of tension-time index of respiratory muscles (TTImus), calculated as (Pimean/Pimax)x(Ti/Ttot) (Pimean: mean airway pressure; Pimax: maximum inspiratory pressure; Ti: inspiratory time; Ttot: total respiratory time).
Results: Children exposed to IUGR had lower BMI (16.2 ± 0.9 vs. 17.4 ± 1.0 kg/m2, p <0.001), lower percentage of muscular mass (34.2 ± 3.5 vs. 40.6 ± 3.7 %, p <0.001), lower VO2max (89.1 ± 6.0 vs. 97.1 ± 2.7 % predicted, p <0.001) and higher TTImus (0.092 ± 0.016 vs. 0.071 ± 0.012 %, p <0.001) compared to controls. Muscular mass percentage and TTImus were significantly correlated with VO2max (r 0.653 and –0.766, respectively). These relationships were independent of sex, age, GA and BMI.
Conclusion: The redistribution of fetal cardiac output in IUGR may have long-term structural and functional effects on the muscular system and respiratory muscles, thus leading to reduced exercise capacity in childhood and beyond.
The Trytophan/Kynurenine Pathway: A possible new target in Preeclamptic Human Placenta
Broekhuizen M, Klein T, Hitzerd E, Simons SH, Neuman R, De Rijke YB, Schoenmakers S, Sedlmayr P, Danser AHJ, Merkus D, Reiss IKM
Division of Neonatology, Erasmus MC, Rotterdam, The Netherlands
Introduction: Preeclampsia is characterised by impaired placental vascular development and regulation, which can be affected through the kynurenine pathway (KP). We aim to investigate how placental metabolism of tryptophan is altered in preeclampsia, focusing on the KP in particular (Figure).
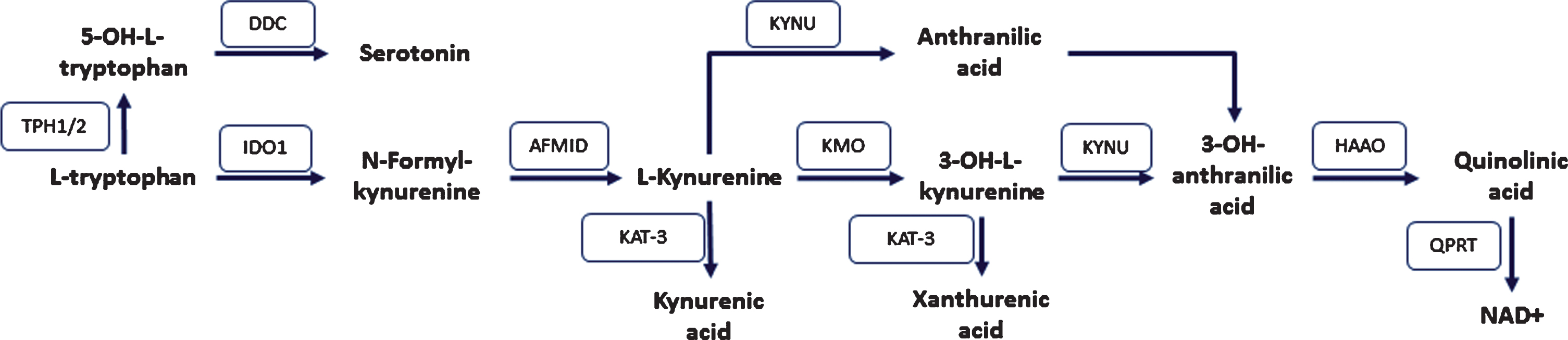
Methods:Gene expression of KP enzymes, quantified by RT-qPCR, and tissue concentrations of the KP metabolites were compared between healthy and PE placentas. Additionally, placentas were dually perfused ex vivo (4 healthy and 2 PE), and KP metabolites were measured in the maternal and fetal circulation using an QTRAP 6500 LC/MS system.
Results:During ex vivo perfusion, tryptophan and KP metabolites were released from the placenta, and the kynurenine/tryptophan ratio was ~0.15 in both the maternal and fetal circulation of healthy and preeclamptic placentas. In contrast, in healthy placental tissue the kynurenine/tryptophan ratio was ~2, and reduced to ~1 in PE. Also 3-OH-L-kynurenine and xanthurenic acid concentrations were lower, whereas kynurenic acid and 3-OH-anthranilic acid were increased on the maternal side of PE placentas. In agreement with this, gene expression data show a reduction of IDO1 and HAAO in preeclampsia, whereas AFMID and KAT-3 were upregulated. The other enzymes were unaltered.
Conclusion:Tryptophan and KP metabolites are released from the placenta into both the maternal and fetal circulation. In preeclamptic placentas the KP is more directed towards kynurenic acid formation, possibly mediating inflammation, whereas the path towards NAD+, hence energy delivery, seems to be reduced. To what degree this contributes to PE remains to be determined.
The second golden hour of Life – A Prospective observational study on post delivery room care
F.V. Hartmann, H. Küster
1 Neonatology, University Medical Centre Göttingen, Germany
Introduction: Because the quality of care in the delivery room has major effects on outcome this critical period has been termed The First Golden Hour of Life and multiple guidelines have been established. In contrast, there is little evidence on how to proceed during the Second Golden Hour of Life of transfer and admission to the NICU.
Methods: Inborn preterm infants treated in our level IV NICU between April 2017 and March 2019 were included. A single individual collected extensive data on all procedures and their timing by direct observation.
Results: Observed were 39 infants: mean gestational age 31 weeks, birth weight 1393 g, 51 % male, 67 % extremely low birth weight (ELBW), 85 % had any kind of respiratory support. Time for transfer and admission was 62 minutes. This was shorter in infants transferred by transport incubator compared to using a NICU-bed with shuttle (Giraffe). ELBW infants spend 92 % of the time in supine position, Non-ELBW 59 %. Total time of disconnection from the ventilator was 50 seconds and was longer in those with nCPAP compared to those intubated. Of those with nCPAP longer time of disconnection occurred if they were >1000 g or transferred by transport incubator.
Conclusion: Transport and admission procedure varies dependent on patient group. Prospective studies are needed to identify and optimize parameters with long-term effects.
Retinopathy of prematurity (ROP) and quality improvement in Neonatal Intensive Care in Latvia
R. Zarina, D.Sniedze, K. Rasnača
Riga Children’s Clinical University hospital, Neonatology department, Riga, Latvia
Introduction: Retinopathy of prematurity (ROP) is a multifactorial vasoproliferative disease of the developing retina, which may lead to blindness. The aim of this study was to analyze the change in ROP incidence within10 year period and associated risk factors in Latvian very low birth weight (VLBW<1500g) infants.
Methods: A retrospective analysis of VLBW infants, born between 2015 and 2018 and admitted at Children’s University hospital. Clinical and ROP treatment data during the 24-36 months follow-up assessment were reviewed. Comparison of severe ROP incidence in LBW infants in the last decade was performed.
Results: From 2015 to 2018 there were 452 eligible infants. For the entire cohort, the incidence of any ROP was 12.3% (53 of 429), and the incidence of severe ROP was 1.1% (5 of 429). We compared any ROP (mean BW 869.7g, mean GA 26.3weeks) patients with randomly chosen control group (n=106) of VLBW infants without ROP (mean BW 945.7g, mean GA 26.5weeks). Any ROP patients had longer duration of mechanical ventilation (15.1 vs 9.4 days, 95% CI 0.93-10.5, p=0.01), there was no significant difference in total oxygen exposure (53.9 vs 44.2 days, p=0.12), the rate of severe IVH, and no significant protective effect of mother’s milk feeding. The incidence of severe ROP in live born infants in Latvia has declined more then 20-fold from 0.13% (2005-2008) to 0.006% (2015-2018).
Conclusion: Advances and quality improvement in neonatal care have significantly reduced the incidence of severe ROP in Latvia.
Developmental care optimization with an innovative incubator cover device
JM Hascoët1, G Petitpas2, J Ducourneau2, I Hamon1
1 Lorraine University, DeVAH 3450, CHRU Nancy; 2 Audio prosthesis School (2) Laboratoire d’Énergétique et de Mécanique théorique et appliquée – NANCY France
Introduction: Premature infants’ neurodevelopment relies upon environment stimuli and parents-infant interaction. Infants’ centered care struggles against excessive sensorial stimulation but lack of stimulation may also lead to impair development. Complete incubator occultation may alter visual development and prevent the instauration of an adequate circadian rhythm. We aimed at evaluating light and noise control by an innovative bevel shape incubator cover device, Babycouv®, protecting baby’s head but allowing dimmed light and direct visual access.
Methods: Light intensity was compared to room’s light by a digital luminometer placed in an empty Ohmeda Giraffe® incubator at the usual site of the baby’s head. In addition, a sound level meter acquired for 1 minute the acoustic spectrum of 4 sound stimuli coming from 2 loudspeakers placed outside the incubator: a white noise, the recording of women and men voices, and the alarm of an IntelliVue MP2® monitor. Data were recorded within the incubator alone, after complete occlusion or with Babycouv®.
Results: Room light intensity varied from 70 to 370 Lux. Complete occlusion obtained an intensity from 0.2 to 0.8 vs. 4.8 to 25 Lux for Babycouv® (91-94% reduction). The noise level of the incubator was 53.2 dBA. and for each stimulus outside: 76.2, 66, 62, 77.5 dBA respectively. Noise attenuation was 12, 13, 10, 9% for the incubator alone, 16, 14, +5, 20% for complete occlusion, 14, 13, 10, 18% for Babycouv®.
Conclusion: Babycouv® allowing significant light reduction and comparable noise attenuation could be an alternative for developmental care optimization of premature infants.
Is Screening for Critical Congenital Heart Disease Useful at the first hour of Life ?
Elif Keleş, Esra Önal, Esin Koç
Neonatalogy, Department of Pediatrics, Gazi University, Ankara , Turkey
Introduction: In infants with critical congenital heart disease (CCHD), delay in diagnosis increases morbidity and mortality. Ideal recommended screening time is 24th-48th hour of life. However, there have been large number of infants who are discharged before the 24th hours of life in Turkey. We aim to determine the time of CCHD screening at the 1st and 24th hours following uneventful delivery in order to reduce the mortality and morbidity caused by early discharge.
Methods: Infants born in Gazi University hospital between August 2016 and February 2019 were included in the study. Preductal and postductal oxygen saturation and perfusion index were measured at the 1st , 24th and 72th hours post-birth by a new-generation pulse oximeter (Massimo Radical 7).The positive screening was defined as post-ductal oxygen saturation (SpO2) <= 95%, pre-postductal SpO2 gradient> 3% or PI <1.2.
Results: In our study, 18 of 1020 infants were antenatally diagnosed with CCHD. There was no significant difference between the first hour and 24th hour preductal/postductal saturation measurements; although there was a significant difference between the first hour and 24th hours in the preductal and postductal perfusion index (p<0,001). Perfusion index was increased at 24 hours due to the adaptation of postnatal physiology. Saturation parameters were more reliable for decision making in CCHD .
Conclusion: 1st hour screening results in early discharge may be useful in diagnosis of CCHD.
Changepoint analysis of gestational age and birthweight – Verifying a refinement of Diagnosis Related (DRG) Groups by monochorial and dichorial twins
O Endrich 1,2; K Triep 1; N Torbica 1; C T Nakas 3,4; M Nelle 5; M Fiedler 1,3, L Raio 6
1Medical Directorate, 2Insel Data Science Center IDSC, 3University Institute of Clinical Chemistry, 6Department of Obstetrics & Gynecology, Inselspital, Univ. Hospital of Bern, Berne, Switzerland; 4Laboratory of Biometry, School of Agriculture, Univ. of Thessaly, Nea Ionia, Magnesia, Greece; 5Neonatology Division, Univ. Hospital of Zurich, Zurich, Switzerland
Introduction: Although the complexity of treatment is connected to the newborn’s maturity and birthweight, most grouping schemes classify by birthweight alone. Monochorial/MCDA twins need more intense treatment than dichorial/DCDA twins. The objective of this study was to determine whether the definition of thresholds based on a changepoint analysis of variability of birthweight and gestational age contributes to a more homogenous classification. To demonstrate the clinical relevance, the results were applied to twin cases.
Methods: This retrospective observational study was conducted at a Tertiary Care Center with Level III Neonatal Intensive Care and included neonate cases from 2016 through 2018, see Table1. Routinely collected health data was used. The cases were categorized according to WHO gestational age and Swiss Diagnosis Related Groups birthweight classes. A changepoint analysis was conducted. Cases of twins were separated into two groups: monochorial and dichorial. The cut-off values were applied to the two groups.
Results: When grouping the cases according to the calculated changepoints the variability within the groups with regard to case related costs could be reduced. An adjusted Grouping Grid was developed. When applying it to the two groups of twins an improvement to grouping could be shown.
Table 1.
Twins study population
| diagnosis | count cases* | average case related costs** | min case related costs** | max case related costs** |
| DCDA (dichorial) | 253 | 24‘187 | 1‘826 | 447‘071 |
| MCDA (mono-chorial) | 88 | 50‘901 | 2‘025 | 312‘869 |
*Excluded: early death or transfer < 5d, cases with missing values for GA, BW, costs, cases with operation room procedures > 200 CHF; ** CHF
Conclusion: A novel method of classification of newborn cases by changepoint analysis was developed, providing the possibility to assign costs or outcome indicators to grouping mechanisms by gestational age and birthweight combined. The application to the different groups of twins suggests a usability also in the clinical context and other parameters.
Does a parent-report assessment at 2 years corrected age predict later cognitive development in very preterm infants?
M. Cuttini1, L. Herich1, I. Croci1, S. Vicari1, F. Rusconi2, M. Carrozzi3, D. Di Lallo4, F. Voller5.
1Pediatric Hospital Bambino Gesù, Rome, Italy; 2Meyer Children’s University Hospital, Florence, Italy; 3Institute for Maternal and Child Health, Trieste, Italy; 4Health Department of Lazio, Rome, Italy; 5 Health Agency of Tuscany, Florence, Italy.
Introduction: Cognitive development is a crucial outcome for very preterm (VP) infants. We used the data of the ACTION prospective follow-up study, participant in the European ReCAP collaborative project, to explore the value of early parent-based assessment in predicting cognitive development for an area-based sample of VP children followed-up at 2 and 9 years of age in three Italian regions (Lazio, Tuscany and Friuli Venezia-Giulia).
Methods: 476 Italian children were analysed. Parental informed consent and Ethics Committee approval were obtained. Cognition was measured using the PARCA-R questionnaire and the Kaufman Assessment Battery for Children (KABC-II) at 2 and 9 years respectively. Uni- and multivariable statistical analyses were performed.
Results: The association between the cognitive scores measured at two (PRC, Parent-Report Composite) and 9 years (MPI, Mental Processing Index) was modest (Pearson correlation coefficient r= 0.28, 95% CI 0.20-0.36) but statistically significant (p <0.001). The ROC analysis carried out using MPI <85 as cut-off produced an Area Under the Curve (AUC) of 0.71 (95% CI 0.64-0.77). A multivariable logistic model including as predictors both PRC and selected clinical and demographic variables (child sex, gestational age, small for gestational age status, multiple birth, cesarean delivery, bronchopulmonary dysplasia, motor and/or sensory problems at 2 years, parental education, maternal age and psychological distress) increased AUC to 0.81 (95% CI 0.75-0.86).
Conclusion: The satisfactory value of AUC provides additional evidence of the validity of the PARCA-R instrument; however, the inclusion of clinical and demographic variables may further increase the prognostic value of the parent-report assessment.
Acknowledgements: The ACTION follow-up project was funded by the Italian Ministry of Health (Programma di Ricerca Finalizzata) and by two unrestricted grants by Chiesi Farmaceutici S.p.A. Data analysis for this study was funded by the ReCAP European project (GA no. 733280).
Longterm outcome after Intra - Uterine laser coagulation for Twin-Twin-Transfusion Syndrome (ttts): Adaptive functioning and substance use at adult age
P Bartmann1, B Busch1, L Weinhold2, L Hoyler1
1 University Children’s Hospital, Bonn, 2 IMBIE University Hospital Bonn, Germany
Introduction: TTTS is a severe complication in monochorionic twin pregnancies. Without treatment, mortality is up to 90%. Intrauterine laser coagulation of the communicating placental vessels is a causal therapy and results in survival rates of 80 – 90%. Long-term outcome data for these patients are still limited. Here we present the first results on outcome at adult age. To analyse adaptive functioning and substance use at young adult age after intra-uterine laser coagulation for TTTS.
Methods: All 254 survivors (born between 1995 and 1999 at a median gestational age of 34 + 3 weeks) of 200 twin pregnancies treated with intrauterine laser coagulation for TTTS were included. 49 were excluded at adult age (2 late deaths, 4 late refusals for participation and 43 non-German speakers), so the target group consisted of 205 patients. 123 (60%) participated: 64 former recipients and 57 former donors. Two patients could not be classified. 25 were born as singletons and 98 as twins . The questionnaire “Adult Self-Report For Ages 18-59” (ASR 18-59) was applied to investigate adaptive functioning and substance use in all participants. The ASR 18-59 includes questions in the categories friends, spouse/partner, family, job, education and substance use (tobacco, alcohol and drugs).
Results: For all five adaptive functioning items the whole patient group obtained median results between the 39. and 65. percentile. No significant differences were observed within twin pairs nor comparing donors with recipients or being born as singleton or twin. Substance use was rare in all patients with median T-Scores of 50 (tobacco), 53 (alcohol) and 50 for drug use.
Conclusion: Median results in the normal range were observed for all former TTTS patients accompanied with a very low substance use.
Catch-up growth in preterm neonates with bronchopulmonary dysplasia in the first two years of life
D Couto1, G Gonçalves1, G Rocha2, F Flor-de-Lima1,2, H Guimarães1,2,3
1 Faculty of Medicine, University of Porto, Porto, Portugal, 2 Neonatal Intensive Care Unit, Department of Pediatrics, Centro Hospitalar Universitário São João, Porto, Portugal ,3 Cardiovascular R&D Unit, Faculty of Medicine, University of Porto, Porto, Portugal
Introduction: Bronchopulmonary dysplasia (BPD) is a serious problem in neonatal intensive care units. It is a multifactorial disease that may influence the growth and development of preterm neonates. The aim of this study is to evaluate the growth of preterm infants with BPD in the first two years of life, determine the risk factors associated and compare with healthy preterm infants.
Methods: Retrospective case-control study of preterm infants with BPD who were born at and discharged from our center between 1st January 2006 and 30th October 2016. Those with major congenital malformations, congenital TORCH infection, death before 36 weeks of postmenstrual age or first 28 days of life and those who were transferred during hospitalization and outborn were excluded.
Results: A total of 90 preterm neonates were enrolled and 30 (33.3%) of them had BPD. At 12 months corrected age, gestational age and pre-pregnancy mother’s weight were shown to be associated with short stature. Weight at birth was also associated with low weight and head circumference growth. At 18 and 24 months of life, no differences were found in the growth assessment.
Conclusion: In this study, the catch up growth of preterm infants with BPD was achieved during the first six months of the second year of life.
Long-term outcome of extremely premature infants after less invasive surfactant administration (LISA)
Katrin Klebermass-Schrehof1; Agnes Grill1, Albert Flunt1, Michael Hayde1, Herbert Kiss2, Renate Fuiko1, S.Brandstetter1, Angelika Berger1
1 Department of Pediatrics and Adolescent Medicine, Division of Neonatology, Pediatric Intensive Care and Neuropediatrics, Medical University of Vienna, Austria
2 Department of Obstetrics and Gynecology, Division of Obstetrics and Feto-Maternal Medicine, Medical University of Vienna, Austria
Introduction: Current metaanalyses identify less invasive surfactant administration (LISA) as an effective non-invasive treatment strategy for respiratory distress syndrome (RDS) with low rates of mortality and morbidity. Only limited data are available on long-term outcome of preterm infants subjected to LISA protocols. The aim of the study was to analyze outcome at two years corrected age of a cohort of extremely preterm infants treated with a primary respiratory care bundle including LISA compared to a historical control group.
Methods: All infants born during 01/2009-12/2014 (n=546) were initially stabilized after birth by a protocol including LISA. All infants of the same gestational age born during 01/2003-12/2008 (n=402) served as historical controls. Neurodevelopmental outcome at the corrected age of two years was assessed by Bayley Scales of Infant Development. Survival without severe intraventricular hemorrhage cystic periventricular leukomalacia, necrotizing enterocolitis, retinopathy of prematurity > grade 2 and chronic lung disease was classified as “survival without morbidity”.
Results: Within the LISA-cohort 81.7% of infants survived, compared to 58.8% of historical control infants (p<0.001). Survival without morbidity was 47.2% in the LISA-cohort compared to 33.9% in the historical control group (p= <0.001). At two years corrected age, survival with favorable outcome was 59.4% in the LISA cohort compared to 32.3% in historical controls (p<0.0001).
Conclusion: Infants treated with a protocol including LISA showed improved survival as well as improved short- and long-term outcome compared to a historical control group.
Very Low Birth Weight Newborns, Portuguese National Multicentre Study 2010-2017
A. Pereira
Hospital Braga, Braga, Portugal
Introduction: National Registry of very low birth weight newborns of the Portuguese Neonatal Society monitors clinical practices, in order to have a national standard for the self-assessment of neonatal units and to detect variations concerning assistance.
Methods: Forty-two Neonatal Intensive Care Units are collaborating, recording their data, for a prospective cohort study in a national database. We analysed the national data, and compare it to our data, Hospital Braga, from 2010-2017.
Results: Total national very low birth weight newborn 9435 versus Hospital Braga 358. National prenatal care 96,3%v.95,3%, completed antenatal steroids 68,9%v.63,7%, twins pregnancy 36,6%v.30,2%, premature rupture amniotic membranes 11,2%v.3,4%, maternal infection 4,9%v.1,7%, eclampsia 18,6%v.16,2%, diabetes 5,8% v.4,2%, caesarean section 70,7%v.65,5%, transition with mask positive pressure ventilation 51,2%v.54,5%, tracheal tube ventilation 33,8%v.23,7%, oxygen administration 59,9%v.75,7%, median weight 1254g v.1264g. Median gestational age 30 weeks in both groups. Invasive ventilation 41,8%v.34,1%, hyaline membrane disease with surfactant administration 64,9%v.62,6%, airleak 5,2%v.4,7%, pulmonary bronchodysplasia 11,6%v.11,3%, patent ductus arteriosus 23,3%v.26,3%, necrotizing enterocolitis 6,1%v.7,8%, cystic periventricular leukomalacia 3,5%v.4%, periintraventricular haemorrhage 7,2%v.9,6%, severe retinopathy of prematurity 4,7%v.4%, early sepsis 11,2%v.21,5% mainly E.Coli 48,1%v.42,9%, late sepsis with positive blood culture 29%v. 20,4% mainely CoNS 45,7%v.40%, major congenital malformations 3,5%v.3% mainly cardiac malformations 26%v.31,3%, mortality 11%v.9,8%.
Conclusion: Benchmarking activity is very important to improve neonatal care. With this study we realized that our results were, in some parameters, far from the national average. As a result we introduced improvements in some clinical practices at Hospital Braga neonatal unit to improve our results.
Low global birth rates – Should we be worried?
D. Bratlid
Department of health management and health economics,Institute of health and society, Faculty of medicine, University of Oslo, Norway.
Introduction: A mean birth rate above 2.0 is needed to have a stable population, i.e. women must on average give birth to more than two children. Presently, birth rates are steadily decreasing world-wide down to very low levels. This dramatic development, including also questions related to possible causes or measures needed to change the trend, has, however, gained very little attention, neither among health professionals, politicians nor the general public.
Methods: Data on global birth rates were obtained from the Norwegian Bureau of Statistics. Relevant causes of the development, impact on population growth and possible actions to change the trend, were analysed from epidemiological, social, and medical data.
Results: The Norwegian birth rate was 1.56 in 2018, down from 1.62 in 2017. Other European countries are worse off. If this rate continuous for three generations, the population will decline from 5.2 to 3.4 million people, if not compensated by 17-18.000 immigrants per year. In 2018 only 10.000 immigrants arrived. However, immigrant women also have low birth rates, in Oslo 1.49 versus 1.43 for resident women.
Conclusion: The global decline in birth rates represents a dramatic challenge to mankind. It is urgent to identify causes and take the appropriate political, social and medical actions. Professionals such as gynaecologists and paediatricians should be more active in this field. It is a demographic paradox that while the most important decision a woman can take to save the earth from climate crisis is to have only one child, this strategy will also extinguish mankind.
Randomized, Open label, Prospective, Feasibility Study of Caffeine and NSAID on Angiogenesis Biomarkers of Retinopathy of Prematurity (ROP) in Preterm Newborns
J. Aranda, S. Patel, C. Cazano , G. Valencia, T. Groysman, J. Horne, C. Cai, K. Beharry & The SPIPROP Trial Team
Departments of Pediatrics & Ophthalmology State University of New York Downstate Medical Center, Brooklyn, NY; and Department of Pediatrics, Wyckoff Heights Medical Center, Brooklyn, NY. USA
Introduction: We determined whether Caffeine alone or with non-steroidal anti-inflammatory drugs (NSAIDs) improve ROP outcome via their actions on angiogenesis biomarkers .
Methods: We enrolled 14 preterm ≤28 weeks; ≤1250 grams, randomized to 1) Group 1 (n=6): Cafcit (20 mg/kg + 5 mg/kg/d IV) + placebo saline IV + sterile saline eye drops (1 drop twice daily x 14 days; 2) Group 2 (n=3): Cafcit + Neoprofen- NPF (10 mg/kg and 2.5 mg/kg/day IV x 5 days + saline eye drops x 14 days; or 3) Group 3 (n=5): Cafcit + saline IV + Acuvail ACU (0.45% solution) 1 drop / 12 hrs x 14 days. Vascular endothelial growth factor (VEGF), VEGFR-1, VEGFR-2, and insulin-like growth factor (IGF)-I were assayed in placenta, cord bloods and urine samples on 1, 7, 14 and 21 days
Results.: Birth weight (grams) and gestational age (weeks) were (Mean ± SD) 731.7± 56.9, & 25.5± 1.2 (Group 1); 1119.3± 115.1 & 26.7± 1.2 (Group 2); and 1020.0± 206.3 & 26.6± 1.7 (Group 3). Pretreatment angiogenesis biomarkers were highly variable in urine. . At P21, ACU decreased VEGF from 60.3± 51.1 pcg/ml to 11.1± 21.1 (-82%) versus placebo (1229% increase) and NPF (27% decrease).VEGFR-2 increased (800%) in placebo but decreased 100% with NPF. IGF-I increased in placebo (173%) but 9% decreased with NPF and 64% increase with ACU. Infants in placebo had lower cord blood VEGF (111.1± 112.6 vs. 277.23± 120.1, p=0.056) and higher IGF-I (591.3± 280.9 vs. 217.6± 125.9, p<0.05) compared to ACU.
Conclusion: Caffeine and NSAIDs attenuate VEGF, VEGF receptors and angiogenesis markers of ROP.
The extent of reduction in vancomycin clearance after ibuprofen or indomethacin differs, and is another covariate for targeted dosing
Karel Allegaert 1,2
1Department of Pediatrics, Division of Neonatology, Erasmus MC Rotterdam, the Netherlands and 2Department of development and regeneration, KU Leuven, Belgium.
Introduction: Data on vancomycin PK and its covariates are abundant, but therapeutic drug monitoring (TDM, trough levels) observations suggest that vancomycin exposure and consequently dosage are substandard. PK modelling is an obvious tool to improve targeted exposure, with a shift from trough levels to area under the curve (AUC24h) targets, but necessitate exploration of covariates, including NSAIDS like ibuprofen or indomethacin.
Methods: We pooled a dataset, including concentration-time data of vancomycin administrated alone or in combination with either ibuprofen or indomethacin collected in UZ Leuven (Leuven, Belgium) or São Francisco Xavier Hospital (Lisbon, Portugal). The derived vancomycin pharmacokinetic model was subsequently used to propose dose adjustments that yield effective vancomycin exposure (i.e., AUC0-24h between 300-550 mg·h/L, with a probability below 0.1 of sub-therapeutic exposure) in preterm neonates with patent ductus arteriosus.
Results: We found indomethacin co-administration to reduce vancomycin clearance by 55% compared to -18 % for ibuprofen. Model simulations showed that the most recent vancomycin dosing regimen which was based on an externally validated model, requires a 20% and 60% decrease of the loading and maintenance dose of vancomycin, respectively, when aiming for optimized exposure in the neonatal population.
Conclusion: the impact of either ibuprofen or indomethacin on vancomycin clearance is significantly different, so that dosing regimens should be further adapted in these settings.
Parenteral nutrition arginine supplementation in very preterm infants and early immune system development
Burgess L1,2 Flanagan B1, Wright H1, Davies J1 Turner M1,2, Morgan C2.
1University of Liverpool, Liverpool, UK, 2Liverpool Women’s Hospital, Liverpool, UK
Introduction: We have previously shown there is both overprovision of essential amino acids (AA) and under provision of some conditionally essential AA, including arginine, in current neonatal parenteral nutrition (PN) formulations. We conducted a physiological study assessing a range of doses of arginine (6-15%) to correct arginine deficiency and investigate immunological pathways.
Methods: Very preterm infants (VPI) born <29 weeks’ gestation and/or <1200g were eligible for PN. Infants were assigned to receive standard PN only or standard PN alongside a range of doses of arginine supplementation until day 10 (D10) of life. Plasma AA levels were measured on D3 and D10 of life using ion exchange chromatography and RNA was extracted from blood and used for microarray and qPCR.
Results: 26 infants with mean gestational age of 26+4 weeks’ and a mean birth weight of 855g were recruited. Infants received PN containing 6% (n=8), 12% (n=12) and 15% (n=6) arginine. D10 plasma arginine levels were higher in supplemented infants (mean 72.8 v 45.5μmol/L, p=0.03). The microarray and subsequent qPCR validation experiments confirm significant up regulation from D3-D10 of B cell differentiation factors APRIL (p<0.01) and BAFF (p<0.05) and pathogen recognition receptors TLR2 (p<0.01) and TLR4 (p<0.01). Gene expression profiling indicates expression changes between infants with low versus normal plasma arginine levels to be similar to changes from D3 to D10 of life.
Conclusion: Arginine supplementation can ameliorate arginine deficiency in VPI. Infants with normal (versus low) plasma arginine levels exhibit changes in immune pathways similar to the temporal changes seen from D3 to D10.
Hyperglcemia in low birth weight infants
Brickmann C., Klotz D., Fuchs H., Hentschel R.
Dept. of General Pediatrics and Adolescent Medicine, Div. Neonatology/Intensive Care Medicine, Univ. Hospital Freiburg, Germany
Introduction: Hyperglycemia is a frequent problem in low birth weight infants, but neither the exact definition, nor the relevance, potential sequelae or the best mode of intervention are clear.
Methods: Retrospective observational study on VLBW infants with transient hyperglycemia treated with insulin either by i.v. boluses (BI) or by continuous i.v. infusion (CI). Enrollment of all 85 ELBW infants < 27+0/7 weeks g.a. born between 01/2013 and 12/2017. Analysis of fluctuations of blood glucose levels (BGL), rate of hyperglycemia >250 mg/dl and hypoglycemia <50 mg/dl per total BGLs and time to enduring normoglycemia from patient records in 42 patients with hyperglycemia. Statistics: Mann-Whitney-U test, unpaired T test.
Results: Inclusion of 42 patients with a median of 24+5/7 and 24+3/7 weeks g.a. (birth weight median 602g and 563g), respectively. Overall 34 episodes of BI and 33 episodes of CI, occurring between age 1 and 18 days (median 3 and 4 days (all differences n.s.)).
| boluses of insulin (BI) | continuous infusion of insulin (CI) | p | |
| glucose administration (g*kg–1*d) | 7.4 +/- 0.37 | 9.3 +/- 0.47 | < 0.05 |
| cumulative insulin dose (U*kg–1*d) | 0.61 +/- 0.07 | 2.10 +/- 0.20 | < 0.05 |
| hyperglycemia (frequency) | 96/488 | 200/1.545 | < 0.05 |
| hypoglycemia (frequency) | 5/488 | 22/1.545 | 0.50 |
| blood glucose fluctuations (mg/dl)# | 39 +/- 1.9 | 38 +/- 1.2 | 0.53 |
# mean amplitude of glucose excursion (MAGE)
Time to normoglycemia was 26-164 (median 50) hrs in 10 patients treated exclusively with BI and 56-532 (median 255) hrs in 11 patients with CI (p < 0.05).
Conclusion: With regard to BGL fluctuations and risk of hypoglycemia both modes of insulin administration seem equally effective to control hyperglycemia in VLBW infants. In the CI group the higher insulin dose may be attributable to adsorption effects of insulin on surfaces of syringes and tubes, and the higher glucose rate may be explained by the longer treatment period. Prospective controlled trials are urgently needed.
Oxytocin administration prior to planned Caesarean section: a new strategy to improve neonatal and maternal outcomes
Sven Wellman
Switserland
Introduction: The rise in Caesarean section (CS) in the past decades is linked to a significant improvement in perinatal outcomes, with stillbirths, birth asphyxia, and birth trauma dropping to levels never seen before. Yet a new set of problems has besieged neonatal units worldwide: a higher incidence of neonatal respiratory morbidity. Based on the excellent safety profile of our pilot randomized controlled trial (RCT) with an oxytocin challenge test (OCT) prior to planned CS inducing mild foetal stress hormone release (doi: 10.1097/AOG.0000000000001594) we prepared a new large RCT to test its clinical relevance, Lacarus trial.
Methods: The Lacarus trial compares OCT (infusion of oxytocin until 3 uterine contractions per 10-min interval are induced) against saline infusion 1 hour prior planned CS in 1450 participants, 1:1 randomisation. Women with singleton pregnancy, planned CS > 34 weeks of gestation and without preceding labour, rupture of the membranes or antenatal steroids are eligible. The primary endpoint is the occurrence of neonatal respiratory morbidity within 24 hours after birth. Secondary endpoints include umbilical cord blood copeptin levels, breastfeeding rate, microbiome composition and maternal and neonatal short and long-term outcomes.
Results: The trial is approved by the Swiss ethics committee (BASEC ID 2018-01842), registered at ClinicalTrials.gov (NCT03693885), funded by the Family Larsson-Rosenquist Foundation and is scheduled to start recruitment in June 2019.
Conclusion: This RCT is the first one testing the hypothesis whether oxytocin-induced labour before planned CS is a promising application of physiologic principles gleaned from natural birth to improve neonatal and maternal outcomes.
Stem cell-based therapies for intraventricular haemorrhage (IVH) and hypoxic-ischaemic encephalopathy: evidence from systematic reviews
M. Bruschettini
Cochrane Sweden, Skane University Hospital; Dept. Pediatrics, Lund University, Lund, Sweden
Introduction: No effective interventions are available for the prevention and treatment of intraventricular haemorrhage (IVH) issues in preterm newborns, whereas management of hypoxic-ischaemic encephalopathy (HIE) in term newborns is limited to hypothermia. Stem cell-based therapies offer a potential therapeutic approach to repair and regenerate injured brain tissue. Preclinical findings have now culminated in multiple human neonatal trials.
Methods: The Cochrane Central Register of Controlled Trials, MEDLINE via PubMed, Embase, and CINAHL were searched in January 2019. Clinical trials databases, conference proceedings, and the reference lists of retrieved articles for randomised controlled trials and quasi-randomised trials were searched. Randomised controlled trials (RCTs) and quasi-RCTs comparing either 1) stem cell-based interventions to control; 2) mesenchymal stromal cells (MSCs) of type or source versus MSCs of other type or source; 3) stem cell-based interventions other than MSCs of type or source versus stem cell-based interventions other than MSCs of other type or source; 4) MSCs versus stem cell-based interventions other than MSCs were included.
Results: No completed studies for inclusion were found. One RCT is registered on intracerebroventricular injection of MSCs via ventricular tap for preterm newborns with severe IVH. Four RCTs are registered on MSCs for HIE. Four and one phase-1 studies were identified on IVH and HIE, respectively.
Conclusion: There is no evidence from RCTs to determine the benefit and harms of stem cell-based interventions for the management of IVH and HIE in newborns. Optimising regenerative cells in small and large animals might provide the groundwork for future clinical trials.
Effect evaluation of doxapram therapy using continuous monitor data at the NICU
Jarinda A. Poppe, Willem van Weteringen, Swantje Völler, Sten P. Willemsen, Irwin K.M. Reiss, Sinno H.P. Simons
Division of Neonatology, Erasmus MC, Rotterdam, The Netherlands
Introduction: Pharmacotherapy in preterm newborns is hampered by difficult evaluation of pharmacodynamics. Drug effect evaluations are often based on subjective, intermittent interpretation of clinical and physiological parameters. Physiological monitor data provide the opportunity of continuous and objective evaluation of drug effects. We aimed to evaluate pharmacodynamics of doxapram using continuously available physiological and ventilatory parameters. Doxapram was prescribed for apnea of prematurity next to caffeine in preterm infants.
Methods: Preterm infants admitted to a level III NICU center who received doxapram therapy were eligible for inclusion. Stored physiological and ventilatory parameters were used to evaluate therapy effects. Additionally, the oxygen saturation (SpO2)/fraction of inspired oxygen (FiO2)-ratio and the area under the 89%-SpO2 curve (duration x depth of SpO2 dips) were calculated. Regression analyses were performed hourly to discriminate between therapy failure (intubation or death) and success (respiratory stable) using the SpO2/FiO2-ratio and patient characteristics.
Results: A total of 117 patients with a median postmenstrual age at doxapram initiation (PMA) of 28.8 weeks (Q1 - Q3; 27.6 - 30.5) met the inclusion criteria. The success rate of doxapram therapy was 56%. Doxapram therapy was related to increased SpO2 and SpO2/FiO2-ratio and less desaturations. The SpO2/FiO2-ratio, PMA and invasive ventilation in the days before doxapram start, discriminated best between therapy failure and success (AUC-ROC of 0.83).
Conclusions: The effects of doxapram can be objectively observed with physiological monitor data. The SpO2/FiO2-ratio seems most predictive for therapy failure or success. The use of continuous physiological data provides a new method for a more objective evaluation of pharmacotherapy.
Maternal serum, cord blood and breast milk profile of neutrophil gelatinase-associated lipocalin (NGAL) at the extremes of fetal growth
A. Papathanasiou1, D.D. Briana1, S. Gavrili2, S. Georgantzi2, D. Gourgiotis3, A. Marmarinos3, K. Voulgaris4, C. Christou4, A. Malamitsi-Puchner1
1 National and Kapodistrian University of Athens, Medical School, Athens, Greece. 2 Neonatal Intensive Care Unit, “Alexandra” University and State Maternity Hospital, Athens, Greece. 3 Laboratory of Clinical Biochemistry-Molecular Diagnostics, 2nd Department of Pediatrics, National and Kapodistrian University of Athens, Athens, Greece 4 Hellenic Statistical Authority, Athens, Greece
Introduction: Neutrophil gelatinase-associated lipocalin (NGAL), an adipose-derived cytokine, regulating immunity, inflammation and metabolic homeostasis, constitutes a biomarker of kidney injury. We investigated the impact of fetal growth on antepartum maternal serum, cord serum and breast milk NGAL concentrations and the associations of the latter with perinatal parameters.
Methods: Maternal serum, cord serum and breast milk NGAL concentrations were measured by ELISA in samples from 80 mothers who delivered 40 appropriate (AGA), 20 large-for gestational age (LGA) and 20 intrauterine growth restricted (IUGR) neonates, classified by customized weight centiles. NGAL concentrations were associated with birth-weight, customized centile, gender, maternal age, mode of delivery.
Results: Antepartum maternal serum NGAL concentrations were significantly higher in women delivering AGA infants compared to the other two groups. Cord blood NGAL concentrations were significantly higher compared to maternal ones; furthermore, they were significantly elevated in the IUGR group compared to the LGA one (p=0.019). Lowest concentrations were detected in breast milk, which did not differ between the three growth groups. A negative correlation was documented between cord blood NGAL concentrations and customized centiles (r: -0.304, p-value:0.007). No other associations were found.
Conclusion: The higher cord serum NGAL concentrations, compared to maternal ones, may point to its fetal origin and potential role in intrauterine growth. The negative correlation of cord NGAL concentrations with customized centiles, possibly implies reduced nephron endowment/subclinical kidney damage in IUGR neonates. The extremely low NGAL breast milk concentrations may contribute to its beneficial metabolic properties.
Thromboelastography: diagnostic and therapeutic approach in neonatology
R. Sokou1, A. Konstantinidi1, S. Valsami2, A. Gounaris3, Z. Iliodromiti4, T. Boutsikou4, A. Tsantes5, N. Iacovidou4
1 NICU Nikaia General Hospital “Aghios Panteleimon” Piraeus, Greece. 2 Hematology Laboratory-Blood Bank, Aretaieio Hospital, National and Kapodistrian University of Athens, Greece. 3 NICU, University Hospital of Larissa, Larissa, Greece. 4 Neonatal Department, National and Kapodistrian University of Athens, Aretaieio Hospital, Athens, Greece. 5 Laboratory of Haematology and Blood Bank Unit, “Attiko” Hospital, National and Kapodistrian University of Athens, Athens, Greece
Introduction: Coagulation system matures from birth to adulthood. Neonates are born with an intrinsic hemostatic deficit, functionally, though, counterbalanced: therefore the risk of hemorrhage or thrombosis is not increased. Neonatal sepsis(NS) may derange this hemostatic balance. Classic tests used for coagulation, do not provide information on the balance between coagulation-anticoagulation. Rotational thromboelastometry(ROTEM) evaluates whole-clot formation and dissolution. No reference values exist for ROTEM assays in healthy neonates, and available data on the role of ROTEM as an indicator of early NS are limited. To establish reference ranges for ROTEM assay(EXTEM) in arterial blood of healthy term and preterm neonates, and to evaluate its role in early detection of NS.
Methods: 272 healthy (198 term-84 preterms), and 91 sick neonates (group A:35 with confirmed sepsis and group B:56 with suspected sepsis) enrolled in the study. EXTEM was performed in healthy term and preterm neonates on 2nd-3rd, and 2nd-7th DOL respectively. In group B, EXTEM was performed, Score for Neonatal Acute Physiology Perinatal Extension (SNAPPE) and Tollner score were calculated.
Results: No significant differences in EXTEM parameters, between healthy preterm and term neonates were detected. In group A we observed an early appearance of hypocoagulability. In group B, EXTEM values indicative of hypercoagulability were observed, significantly different from healthy neonates.
Conclusions: Our TEM values may be considered as normal, since they refer to healthy newborns and may contribute to the broader use of TEM in neonatology, and to the establishment of algorithms for individualized therapeutic transfusions in NICUs. A clear hypocoagulable profile was observed at the early phase of NS. ROTEM may be a useful tool in the detection of coagulation abnormalities in NS improving diagnostic and prognostic applications.
Value of direct antiglobulin test using gel method in prognosing significant hyperbilirubinaemia in ABO incompatible newborns
M. Veinla, A. Antson, M. Merila, E. Kallas, A. Bärenson, H. Varendi
Introduction: Group 0 blood type mother’s newborn who is non-“0“ (ABO incompatible) can develop hemolytic disease of the neonate (HDN). A positive direct antiglobulin test (Coombs) (DAT) demonstrates the presence of maternal immunoglobulin bound to the neonates’ red blood cells. DAT has been shown to have poor positive predictive value (PPV) and good negative predictive value (NPV) regarding HDN. Laboratories are using a more sensitive, microcolumn gel technology to minimise the frequency of false-negative results in reducing risks at blood transfusion. As there was no data about PPV of non-cord blood DAT using the gel method, we estimated the PPV of positive DAT in ABO incompatible newborns born from group 0 Rh(D) positive mothers to predict HDN or hyperbilirubinaemia.
Methods: Retrospective search of Tartu University Hospital Laboratory database for neonatal DAT performed between 2013-2018. The routine has been to sample neonatal capillary or venous (not umbilical cord) blood and use of the microcolumn technology, ie “gel” method. Of 6253 DAT analyses performed in 0-6 postnatal days, 371 were positive. DAT-positive neonatal records were reviewed to obtain maternal and child blood groups and occurrence of neonatal HDN or hyperbilirubinaemia.
Results: Out of 175 DAT-positive ABO-incompatible newborns, born from 0/pos mothers, 16 cases of HDN or hyperbilirubinaemia had been diagnosed. The PPV of the gel method was 9,14%. There was positive relationship with the grade of agglutination.
Conclusion: Our results support the statement that gel method’s increased sensitivity may lead to the detection of weakly positive DAT, that is clinically insignificant.
Plasma biomarkers of hypoxic-ischemic encephalopathy identified by mass spectrometry
Kyng, KJ*1, Palmfeldt, J*2, Godsk, SH2, Vandecruys, L2, Edhager, A2, Nordbye-Nielsen, K3, Henriksen, TB1
*These authors contributed equally to the work. 1 Perinatal Research Unit, Department of Paediatrics†, 2Research Unit for Molecular Medicine, Department of Clinical Medicine†, 3Danish Paediatric Orthopaedic Research†. †Aarhus University Hospital, Denmark.
Introduction: Plasma biomarkers may contribute to diagnosis, guiding of therapeutic decisions and improved prognostication in hypoxic-ischemic encephalopathy (HIE). The aim of this study was to identify novel protein biomarkers of HIE using mass spectrometry.
Methods: Plasma was sampled within the first six hours of life from 15 term neonates with moderate-severe HIE and 8 healthy controls. Mass spectrometry (nanoLC-MS/MS) was done in three runs, each with five patients vs. all controls. Proteins were selected for further analysis if they met the following criteria for HIE vs. healthy control analysis 1) p-value < 0.05 in ≥ two runs (ttest, 2-sided) 2) p-value < 0.1 in the third run 3) fold change ≥ 2 times the global error of mean. Selected proteins were validated by Western blotting.
Results: From 865 proteins detected in plasma, 23 were found at higher concentrations and 7 in lower concentrations in HIE vs. controls. Functional annotation revealed differential regulation of glycolysis, glutamate and oxidant scavenging, coagulation, heat shock proteins, and inflammation. Western blots confirmed the results (ratio HIE:control, p two-sided ttest): Gal1 1.7 (p 0.0003), S100A8 10.0 (p 0.008), S100A9 4.0 (p 0.0003), Pfn1 3.3 (p 0.015).
Conclusion: Untargeted LC-MS enabled characterization of proteome changes in HIE. The most promising biomarker candidates were protein S100A8, S100A9 and the cytosolic aspartate aminotransferase, since they can be connected to the biological processes in HIE, and were elevated in all patients. We will continue validation in a larger patient sample.
Serum glutathione S-transferase Pi as predictor of acute kidney injury in premature newborns
Stojanovic V, Barišic N, Radovanović T, Doronjski A.
University of Novi Sad, School of Medicine, Institute for Child and Youth Health Care of Vojvodina, Novi Sad, Serbia
Introduction: The incidence of acute kidney injury (AKI) among the neonates treated at the Neonatal Intensive Care Units is high with high mortality rates. Glutathione S-transferase (GST) class Pi plays an important role in the protection of cells from cytotoxic and oncogenic agents. The aim of the study was to examine whether the levels of serum GST Pi determined after birth have any predictive value for the development of AKI in premature neonates.
Methods: The prospective study included 36 premature neonates. For all the neonates included in the study, the data about morbidity was gathered. The blood samples were taken in the first 6 hours of life and GST Pi levels were measured.
Results: The average value of GST Pi among the neonates who died was 1.904± 0.4535 mg/ml, while in the neonates who survived it was 1.434± 0.444 mg/ml (p=0.0128). Logistic regression revealed a statistically significant, positive correlation between GST Pi levels and death (p=0.0180,OR 7.5954;CI 1.4148-40.7748). The mean value of GST Pi levels in the neonates with AKI was 1.806± 0.350 mg/ml, while in the neonates without AKI it was 1.454± 0.472 mg/ml (p=0.011). Among the neonates who had GST Pi levels above 1.37 mg/ml, the incidence of AKI was statistically higher than in the neonates with GST Pi levels beneath median (p=0.018).
Conclusion: The conclusion of our study is that the serum GST Pi is a very sensitive biomarker of AKI, and of the poor outcome in prematurely born newborns.
Urinary metabolomic profile in young adults born preterm: a mirror from birth toward adulthood
Serafina Perrone1, Elisa Laschi2, Maurizio Giordano1, Mariangela Longini2, Maria Tassini2, Marco Calderisi2, Giuseppe Buonocore2.
1Department of Medicine and Surgery, University of Parma, Parma, Italy. 2Department of Molecular and Developmental Medicine, University of Siena, Siena, Italy.
Introduction: Prematurity is associated with a greater risk of developing chronic diseases in adulthood. Metabolomics is an holistic approach to non-invasively determine metabolic status of an organism. Previous studies revealed distinct urinary metabolic profiles in neonates of different gestational ages, and identified the discriminating metabolites such as hippurate, tryptophan, phenylalanine, malate, tyrosine, hydroxybutyrate, N-acetyl-glutamate, and proline. The aim of this study was to investigate the urinary metabolomic profile in adulthood, comparing young adults born preterm with young adults born at term.
Methods: Urine samples were collected from voluntary healthy 67 patients aged 18-23 years. They included 49 ex-preterm young adults (gestational age of 30.5± 2.4 weeks and birth weight 1398 ± 301.3 g) and 18 ex-term young adults (gestational age: 38.5± 2.1 weeks and birth weight of 3440 ± 298.2 g). A questionnaire about lifestyle, current weight, body mass index, health status, level of education, employment was administered and recorded. Perinatal data were retrospectively collected. Urine samples were analyzed using hydrogen spectroscopic magnetic resonance (1H-NMR) imaging. The spectra obtained were analyzed with Principal Component Analysis (PCA) on the centered mean and Pareto scaled data; the plus classification analysis was performed by means of different classification techniques.
Results:A different urine metabolic profile was found among young adults born preterm compared with young adults born at term (Figure 1). The Random Forest algorithm indicated the metabolic profile that was connected to the different gestational age at birth. Hippurate (7.6-7.8ppm), Fumarate (6.8ppm), Citrate and Creatinine (4.28 ppm) were higher in young adults ex-preterm than young adults born at term.
Conclusion:The metabolic profile of urine in young adults born preterm differs from young adults born at term and resembles those that have been reported at birth. Data suggest that preterm birth is associated with changes in physiology and body metabolism that persist over time and in later years. Metabolomics represents a noninvasive approach to study neonatal population, to early identify altered metabolic pathways, paving the way to a tailored management of neonatal disorders.
Apolipoprotein profiles in very preterm-Born preschool children
U. Kiechl-Kohlendorfer1, A. Posod1, R. Pechlaner2, M. Mayr3, S. Kiechl2
1Department of Pediatrics II (Neonatology) and 2Department of Neurology, Medical University of Innsbruck, Austria, 3King’s College London, UK
Introduction: Apolipoprotein composition might contribute to cardiometabolic outcome in later life. Little is known about plasma apolipoprotein profiles in very preterm-born and term-born preschool children compared to the adult population.
Methods: Children aged 5 to 7 years born at term or with <32 weeks of gestation were included. Twelve apolipoproteins were measured in plasma of 26 former term and 38 former very preterm infants collected after an overnight fast using multiple-reaction monitoring-based mass spectrometry. Findings were confirmed by assessing apolipoprotein levels using antibody-based assays.
Results: Term-born children showed plasma levels of ApoC-II and C-III quantitatively similar to the adult range. Hierarchical clustering analyses suggested that a higher proportion of ApoC-II and C-III reside on high-density lipoprotein particles in children than in adults given the marked correlations of ApoC-III and C-II with high-density lipoprotein cholesterol and ApoA-I in children but not adults. Comparing children born term and preterm, ApoA-I, A-IV, C-II, and C-III were significantly higher in the latter group.
Conclusion: Our study defines apolipoprotein profiles in preschoolers and reports potential effects of prematurity. Further large-scale studies are required to provide evidence whether this apolipoprotein signature of prematurity, including high ApoC-II and C-III levels, might translate into adverse cardiometabolic outcome in later life.




