Idiopathic SIADH in the premature newborn, a case report
Abstract
BACKGROUND:
Hyponatremia is a common laboratory finding in premature and ill neonates. When the degree of hyponatremia is more severe, the likelihood of a pathologic entity increases. In this case report we describe a premature neonate with severe hyponatremia due to the idiopathic syndrome of inappropriate antidiuretic hormone secretion (SIADH).
CASE DESCRIPTION:
The patient is a male neonate, born prematurely. He was admitted to the neonatal intensive care unit and received non-invasive respiratory support. After 48 hours of life serum sodium (Na+) decreased to 115 mmol/l. Hyponatremia progressively worsened despite aggressive Na+ supplementation. The clinical and laboratory data were most consistent with severe SIADH. Fluid restriction was initiated which resulted in a gradual normalization of Na+. A causal factor for development of SIADH could not be identified.
CONCLUSION:
When a neonate presents with significant hyponatremia that is not responsive to conventional therapy, it is important to perform a diagnostic work-up for SIADH, even in the absence of overt triggering factors.
1Introduction
Hyponatremia is a common laboratory finding in premature and ill neonates (incidence up to 33 percent) in the first week of life. After the first week the incidence is slightly higher, occurring in 25–65 percent of all very low birth weight infants [1, 2]. In most infants hyponatremia is mild (130–135 mmol/l) and tends to be transient. Hyponatremia in premature infants is caused by a reduced sodium (Na+) retaining capacity of the proximal renal tubule, leading to excessive renal Na+ loss in the face of a relatively low serum Na+ concentration. In addition, in premature infants intestinal absorption of Na+ is reduced and insensible loss is high, leading to a lower volume in the renal peritubular space and lower tubular reabsorption of Na+ [3]. Treatment of hyponatremia consists of Na+ supplementation and can typically be weaned within the first weeks to months of life. When the degree of hyponatremia is more severe, i.e. serum Na+ < 125–130 mmol/l, the likelihood of a different pathologic entity increases. Differential diagnosis of severe neonatal hyponatremia consists among others of gastrointestinal disease with extensive Na+ losses, excessive hyperglycemia, diuretics, kidney diseases (i.e. acute tubular necrosis, acute renal failure), and endocrine disorders, most notably adrenal insufficiency and cerebral salt wasting [3]. The syndrome of inappropriate antidiuretic hormone secretion (SIADH) is another potential cause, but is relatively rare in neonates. When it does occur, there is usually an apparent underlying factor. Idiopathic neonatal SIADH without any sign of significant comorbidity has rarely been described.
In this report we describe a premature infant with severe hyponatremia due to idiopathic SIADH and an excellent clinical response to fluid restriction.
2Case description
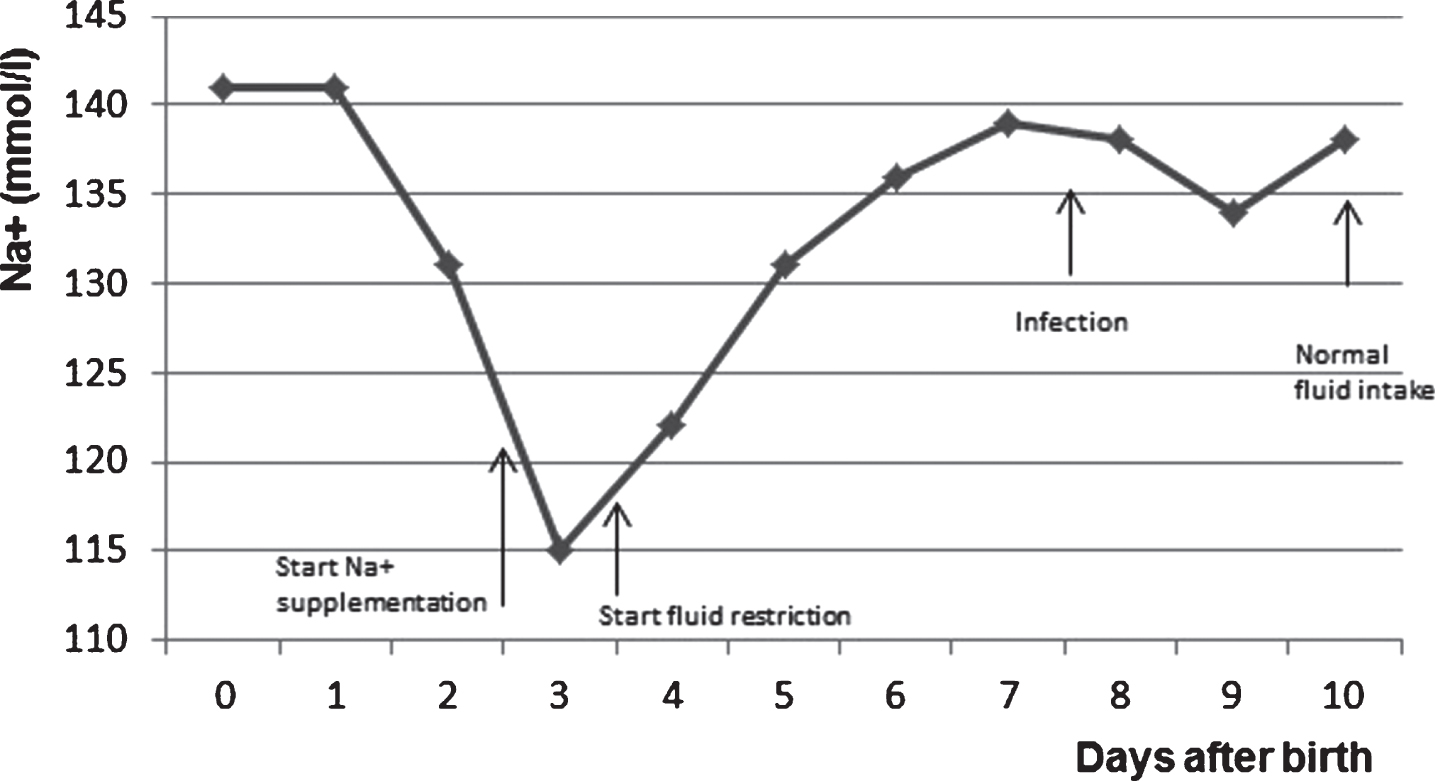
Patient A is a male neonate, born prematurely (gestational age thirty weeks and six days, birthweight 1000 grams). The mother had no medical history and was primigravida. Pregnancy was complicated by pre-eclampsia, treated with methyldopa, labetalol and magnesium sulfate. Because of the worsening pre-eclampsia with proteinuria and intra-uterine growth restriction a caesarean section was performed. The infant had a good start with Apgar scores of 8/7/9, arterial cord pH 7.26 and base excess – 4.6. He was admitted to the neonatal intensive care unit (NICU) and received non-invasive respiratory support with CPAP during three days, followed by high flow nasal cannula. At day one his total fluid was 60 ml/kg/day. According to the standard NICU protocol total fluid was raised every day with 20 ml/kg/day until 160 ml/kg/day was reached. After 48 hours of life serum Na+ decreased from 136 to 115 mmol/l by day 4 after birth. Diuresis was 2.5 ml/kg/h, the net 24 hr fluid balance was 75 ml positive, and post-partum weight loss was limited to five percent. He was clinically stable without any signs of active infection, pulmonary or neurological disease. Hyponatremia progressively worsened despite aggressive Na+ supplementation (maximum 12 mmol/kg/day). His total fluid intake was 160 ml/kg/day, according to the standard NICU protocol. Of note, diuresis was still present at 2–3 ml/kg/h and blood pressure readings were within the normal range. On physical exam, the infant appeared euvolemic and he had a normal male urogenital exam with descended testicles bilaterally. There were no midline defects visible. Additional work-up on day four showed a serum Na+ of 115 mmol/l with a low serum osmol (233 mOsmol/kg). Urea and creatinine were normal for gestational age and day of life. Other electrolytes and glucose were within the normal range. A simultaneously obtained urine sample showed elevated Na+ of 70 mmol/l and osmol of 247 mOsmol/kg. A renal ultrasound was unremarkable with a normal intra-arterial pressure gradient and normal bilateral kidney dimensions. Infection parameters were low, chest x-ray did not show any infiltrates and there was no temperature instability. Brain ultrasound revealed a grade one IVH without any signs of increased intracerebral pressure. The above clinical and laboratory data were most consistent with a diagnosis of severe SIADH, despite the absence of a potential trigger. Fluid restriction was initiated (maximal daily volume of 120 ml/kg/day) resulting in a gradual increase in serum Na+ within the next 24 hours to 127 mmol/l. In subsequent days serum Na+ gradually normalized (see Fig. 1), while additional Na+ supplementation could be discontinued. Throughout this period, his clinical condition remained stable with adequate diuresis (3–4 ml/kg/h) and euvolemia on repeated physical exams. Eight days after birth he showed multiple incidents of bradycardia and infection was suspected. C-reactive protein (CRP) was elevated to maximally 118 mg/l. Blood culture was positive for Staphylococcus epidermidis, probably related to an indwelling umbilical catheter. The umbilical catheter was removed and he was treated for 72 hours with vancomycin. During the course of the infection he remained stable and needed no respiratory support. Serum Na+ and diuresis remained within the normal range with normal fluid intake (160 ml/kg/day since eleven days after birth).
Fig.1
The serum sodium level in time.
3Discussion
SIADH is a rare cause of severe hyponatremia in the neonatal period, induced by excessive release of the anti-diuretic hormone (ADH) by the posterior pituitary. The physiologic response of the body to a low serum osmolality is suppression of ADH release, but in SIADH this feedback system is impaired, resulting in retention of water and thereby hyponatremia. Characteristics of SIADH are hyponatremia with plasma hyposmolality, high urinary osmolality relative to plasma osmolality, increased urinary Na+ excretion, euvolemia and normal renal and adrenal function [4]. Multiple subtypes of SIADH are described. In type one the ADH level fluctuates without the concomitant reaction on plasma osmolality. In type two the posterior pituitary constantly produces a small amount of ADH. A third type is called ‘reset osmostat’. This is a very rare chronic disorder, characterised by a lower plasma osmolality threshold for the excretion of ADH, with only modest hyponatremia and no indication for therapy. The last type is a nephrogenic SIADH, most commonly caused by a genetic mutation in the ADH receptor, leading to constitutional activation and persistent ADH effects, even when serum ADH levels are low [4]. In almost all cases of SIADH there is an identifiable cause for the development of the neonatal SIADH. Most important causes are: a) Pulmonary: pneumothorax or other forms of air leak, pneumonia, chronic lung disease, positive pressure ventilation; b) Central nervous system: perinatal hypoxia, brain injury; c) Infectious: pneumonia, meningitis; d) Endocrine: hyperglycemia, hypothyroidism, hypopituitarism; e) Maternal medication: tricyclic antidepressant, diuretics, oxytocin [5]. The patient in our case had a severe hyponatremia despite a normal fluid intake of 160 ml/kg/day, which is tolerated well in almost all premature infants of the same age. He was diagnosed with SIADH. There was no clear cause of SIADH at the time of diagnosis. However, four days after the gradual onset of hyponatremia and initiation of fluid restriction, he developed an infection. The patient had no symptoms of a meningitis. According to the standard NICU protocol a lumbar puncture is only performed when there are specific symptoms of a meningitis. Hence, in our case there was no indication for a lumbar puncture and therefore a lumbar puncture was not performed. Although not previously described in the literature, SIADH may have been the first clinical sign of this impending infection (pneumonia or CNS infection). Other causes of the SIADH in this specific case are highly unlikely. It is important to rapidly identify the cause of any type of hyponatremia for optimal clinical management and treatment. Most cases of hyponatremia in the neonatal period can be treated by Na+ supplementation, whereas SIADH is preferably treated by fluid restriction alone. In conclusion, hyponatremia is a common problem of prematurity. When hyponatremia is more severe and not responding to the standard therapy, it is important to reconsider the diagnosis and to consider more rare causes of hyponatremia, like SIADH. When a neonate presents with the apparent idiopathic SIADH, it is crucial to actively search for impending disease to determine an etiologic cause to guide optimal treatment. Because of the chronic nature of some subtypes of SIADH, monitoring of serum Na+ levels and diuresis pattern is indicated until complete resolution of the SIADH has occurred.
Funding source
No funding was secured for this study.
Financial disclosures
No financial relationships relevant to this article to disclose.
Conflicts of interest
No conflicts of interest to disclose.
References
[1] | Kloiber LL , Winn NJ , Shafffer SG , et al. Late hyponatraemia in very low birthweight infants: incidence and associated risk factors. J Am Diet Assoc. (1996) ;96: :880–884. |
[2] | Takahashi N , Hoshi J , Nishida H . Water balance, electrolytes and acid base balance in extremely premature infants. Acta Paediatr Jpn. (1994) ;36: :250–255. |
[3] | Modi N . Fluid and electrolyte balance. In: Robertson NRC Rennie JM, editors. Textbook of Neonatology. 5th ed. Edinburgh: Churchill Livingstone; (2012) :331–343. |
[4] | Baylis PH . The syndrome of inappropriate antidiuretic hormone secretion. Int J Biochem Cell Biol. (2003) ;35: :1495–9. |
[5] | Rose BD . Pathophysiology and etiology of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). http://www.uptodate.com/contents/pathophysiology-and-etiology-of-the-sydrome-of-inappropriate-antidiuretic-hormone-secretion-siadh |




