Cerebrospinal Fluid Diagnostics of Alzheimer’s Disease in Patients with Idiopathic Normal Pressure Hydrocephalus
Abstract
Background:
Alzheimer’s disease (AD) is the most common cause of dementia worldwide and a frequent comorbidity in idiopathic normal pressure hydrocephalus (iNPH). The presence of AD pathology is associated with worse outcomes after a shunt procedure in iNPH. Preoperative diagnosis of AD is challenging in patients with iNPH, which involves reduced concentrations of the cerebrospinal fluid (CSF) AD biomarkers.
Objective:
Our aim was to estimate the effect size of iNPH as a factor in CSF levels of AD biomarkers and to test if correction could be used to improve diagnostic value.
Methods:
Our cohort included 222 iNPH patients with data in the Kuopio NPH registry and brain biopsy and CSF samples available. We divided the patients into groups according to AD pathology per brain biopsy. For control cohorts, we had CSF samples from cognitively healthy individuals (n = 33) and patients with diagnosed AD and no iNPH (n = 39).
*-31pt
Results:
Levels of all investigated biomarkers differed significantly between groups, with the exception of t-Tau levels between healthy individuals and iNPH patients with AD pathology. Applying a correction factor for each biomarker (0.842*Aβ1 - 42, 0.779*t-Tau, and 0.610*P-Tau181) for the effect of iNPH yielded a sensitivity of 2.4% and specificity of 100%. The ratio of P-Tau181 to Aβ1 - 42 was moderately effective in aiding recognition of AD pathology in iNPH patients (sensitivity 0.79, specificity 0.76, area under the curve 0.824).
Conclusion:
Correcting for iNPH as a factor failed to improve diagnostic effectiveness, but the P-Tau181/Aβ1 - 42 ratio showed some utility in the diagnosis of AD in iNPH patients.
INTRODUCTION
Idiopathic normal pressure hydrocephalus (iNPH) is a neurological disorder characterized by the triad of gait difficulty, cognitive impairment, and urinary incontinence [1]. In aging populations, iNPH has growing importance as a cause of dementia, with a prevalence of 0.18% among those over age 60 and an estimated 3.7% prevalence in people over age 65, which increases with age [2]. Differences in prevalence likely trace to differences in clinical decision-making among countries [3]. The symptoms of iNPH can be reversed with shunt surgery, and early diagnosis is vital for patient quality of life and reduced costs [4, 5]. The cause of iNPH remains unconfirmed, but cilial dysfunction is considered to be a key element in its development [6]. Comorbid neurological disorders or former ischemic events can lead to a poor outcome of shunt surgery [7, 8], and co-occurring conditions such as Alzheimer’s disease (AD) are relevant in selecting patients who would benefit from shunt surgery. Furthermore, around 20% of shunted iNPH patients will have developed clinical AD at follow-up [9].
AD is the most common cause of dementia worldwide. No curative treatments are available, but biomarkers of early pathological changes may offer potential targets for preventive or disease-modifying therapies [10–13]. Reducing secondary risk factors for AD in the early phases also can slow its progress [14–16]. The pathological features of AD are extracellular accumulation of amyloid-β (Aβ) peptide and intracellular aggregation of tau proteins in brain tissue, causing neuronal dysfunction and neurodegeneration [17]. Traditional biomarkers for AD are cerebrospinal fluid (CSF) amyloid-β1 - 42 (Aβ1 - 42), total tau protein (t-Tau), and phosphorylated tau protein (P-Tau181). Of these, CSF Aβ1 - 42 concentration changes earliest in the disease, in response to accumulation of Aβ in the brain parenchyma [18]. Increases in t-Tau and P-Tau181 in CSF are seen in AD, signifying tau-related pathology [19]. These biomarker values thus are useful in AD diagnostics but may be misleading in iNPH. In patients with iNPH, Aβ1 - 42 CSF levels are as low as in patients with AD because of a general reduction in soluble Aβ and Aβ protein precursor [20–22]. Meanwhile, t-Tau and P-Tau181 levels in iNPH patients are lower than or comparable to those of healthy individuals. iNPH seems to reduce CSF biomarker levels overall, possibly because of dilution, abnormal CSF dynamics, decreased clearance, or reduced cortical metabolism [20–22]. Currently, differential diagnostics of AD in iNPH patients is laborious, and although cortical biopsy during shunt surgery can be indicated for earlier diagnosis of comorbid AD [9], this approach obviously does not contribute to preoperative differential diagnosis and decision making.
In this study, our aim was to investigate the ratios of CSF biomarkers between iNPH and non-iNPH groups to determine the potential benefit of using a correction factor for the effects of iNPH on biomarkers. Another goal was to see if we could use CSF biomarkers of AD to differentiate between iNPH patients with and without AD pathology on biopsies. The ability to make this distinction would aid in diagnosis of AD and in predicting shunt response in iNPH patients.
MATERIALS AND METHODS
Patient cohort
Data for the patient and control cohorts are presented in Table 1. Boxplots for CSF biomarkers between each group are presented in Fig. 1.
Fig. 1
Boxplots for AD biomarkers with cutoff values. Horizontal lines indicate cutoff value for diagnosis of AD in standard population. 715 pg/ml for Aβ1 - 42, 260 pg/ml for t-Tau, and 26 pg/ml for P-Tau181.
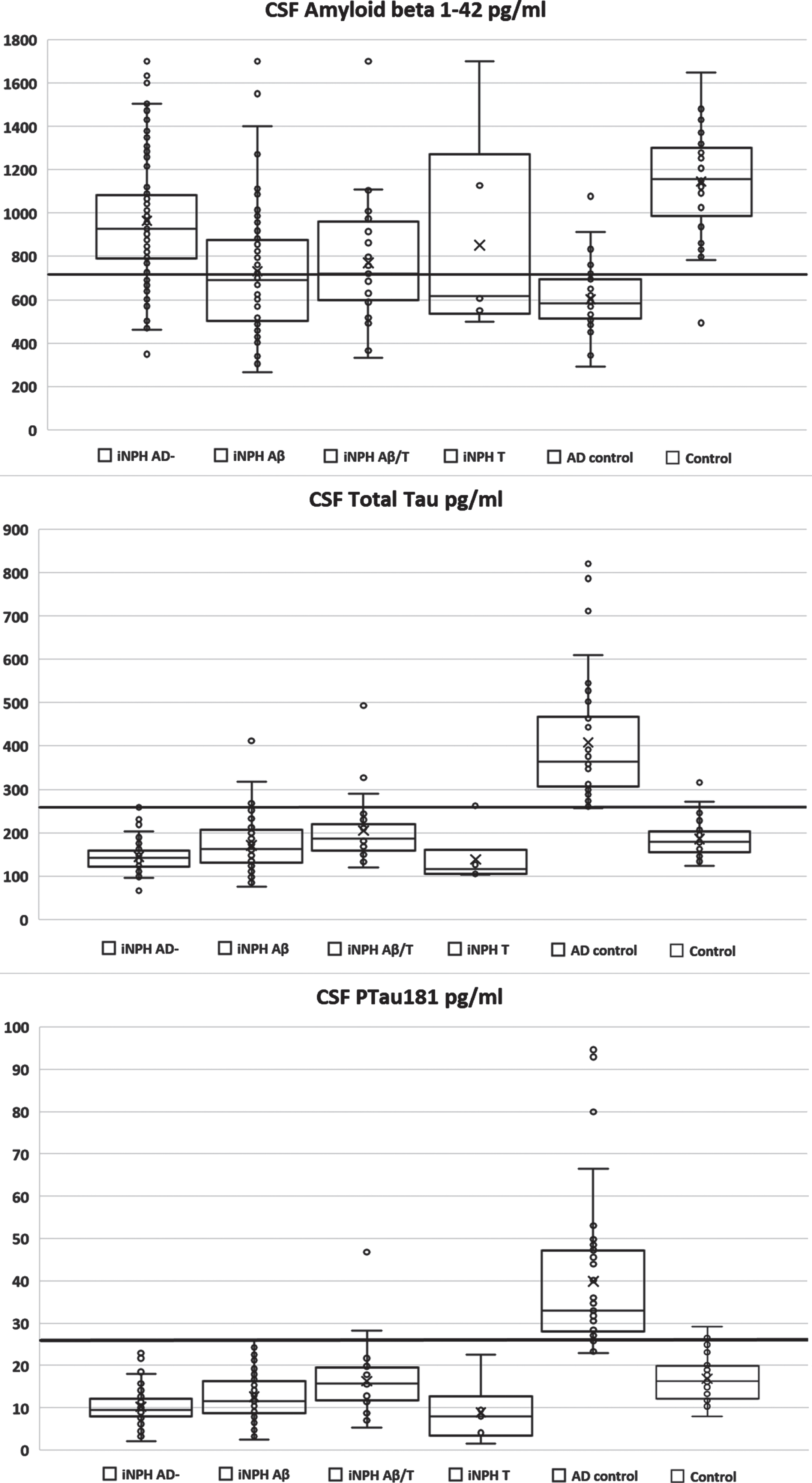
Table 1
Patient demographics
| Category | Control | AD control | iNPH AD– | iNPH Aβ | iNPH Aβ/T | iNPH T | iNPH Aβ pooled |
| N | 33 | 39 | 98 | 90 | 28 | 6 | 118 |
| Aβ1 - 42, mean (SD) | 1145.60 (237.73)*, ** | 602.70 (154.28)*, ** | 964.96 (278.95)** | 730.81 (290.41) | 771.13 (274.02) | 851.11 (474.18) | 740.38 (285.97)* |
| t-Tau, mean (SD) | 185.83 (42.35)* | 408.29 (141.87)*, ** | 144.76 (33.44)** | 170.86 (55.11) | 204.57 (73.06) | 138.57 (61.51) | 178.86 (61.23)* |
| P-Tau181, mean (SD) | 16.84 (5.24)*, ** | 39.92 (17.53)*, ** | 10.27 (3.90)** | 12.61 (5.08) | 16.34 (7.87) | 8.97 (7.30) | 13.50 (6.04)* |
| MMSE***, median (SD) | – | – | 24.00 (3.75) | 24.00 (4.82) | 20.50 (5.26) | 20.00 (6.04) | 23.00 (4.95) |
| Age, mean (SD) | – | – | 73.56 (6.68) | 76.07 (5.22) | 80.34 (3.79) | 70.78 (3.41) | 77.08 (5.23) |
| Shunt response# (%) | 83 (84.7%) | 69 (76.7%) | 23 (82.1%) | 4 (66.7%) | 92 (78.0%) |
Control, healthy participants; iNPH AD– , iNPH patients with no AD pathology on biopsy; iNPH Aβ, iNPH patients with amyloid pathology on biopsy; iNPH Aβ/T, iNPH patients with amyloid and tau pathology in biopsy; iNPH T, iNPH patients with tau pathology on biopsy; iNPH Aβ pooled, iNPH patients with only amyloid and those with amyloid and tau pathology; AD control, patients with diagnosed AD and no iNPH. Aβ1 - 42, amyloid beta in lumbar CSF; t-Tau, t-Tau in lumbar CSF; P-Tau181, phosphorylated tau in lumbar CSF; MMSE, Mini-Mental State Examination; SD, standard deviation. *p < 0.05 versus iNPH AD– ; **p < 0.05 versus iNPH AD pooled; p values from independent samples t-tests. ***Missing MMSE from one patient in the iNPH AD– and one in the iNPH T groups. #Shunt response on 3 month follow up visit evaluated by clinician.
Patients presenting with at least one of the characteristic symptoms of iNPH (gait difficulty, impaired cognition, urinary incontinence) combined with enlarged brain ventricles on MRI were evaluated in the Department of Neurosurgery, Kuopio University Hospital (KUH). KUH provides acute and elective neurosurgical care for a catchment population of approximately 800,000 in Eastern Finland. Our patient cohort included 222 consecutive patients shunted for probable iNPH [1]. Diagnosis of iNPH in these patients was done according to a protocol [23] published between 2019 and 2021. Our study relies on patient data that we also used in a previous study (N = 119) [24]. All patients from the KUH catchment population with suspected iNPH are included in the Kuopio NPH registry and tissue bank, which features follow-up data, other diagnoses, medications, and causes of death together with collected biopsy and CSF samples (http://www.uef.fi/nph). CSF samples were obtained by lumbar puncture prior to shunt surgery. Shunt response was evaluated at outpatient clinic 2 to 3 months after shunt surgery by a clinician. Shunt response was defined as improvement in gait, memory, or urinary incontinence [9].
Control cohorts
The cohort of healthy individuals for this study has been described previously [24]. Briefly, CSF samples were obtained from 33 cognitively healthy individuals undergoing knee surgery with spinal anesthesia [25]. In addition, we collected data from a cohort of AD patients attending KUH neurology (n = 39). Patients were classified as likely AD (either amnestic variant or posterior cortical atrophy). Levels of at least two of three AD biomarkers in the CSF had to be pathological for cohort inclusion.
CSF samples
CSF samples from iNPH patients and control participants were obtained by lumbar puncture, centrifuged, and stored in polypropylene tubes at – 80°C until analysis at the UEF Biomarker Laboratory according to standardized protocols. Before 2020, CSF levels of AD biomarkers (Aβ1 - 42, t-Tau, and P-Tau181) were analyzed using a commercial enzyme-linked immunosorbent assay (Innotest, Fujirebio, Ghent, Belgium). Since 2020, AD biomarkers have been analyzed using automated Elecsys immunoassays (Roche Diagnostics, Penzberg, Germany). CSF samples had to be transferred to different tubes for analyses, which carries a risk of decreasing Aβ1 - 42 levels. AD biomarker results measured using Innotest were converted to Elecsys levels using the conversion equations presented in Table 2. These equations have been established at the UEF Biomarker Laboratory using 100 CSF samples analyzed with both methods and are similar to previously presented conversions [26]. Cutoff points for CSF diagnostics of AD, as defined at the UEF Biomarker Laboratory, were <715 pg/ml for Aβ1 - 42,>260 pg/ml for t-Tau, and >26 pg/ml for P-Tau181.
Table 2
Conversion equations for CSF biomarkers
| Marker | Function |
| Aβ1 - 42 | Elecsys(Aβ1 - 42) = (1.22*Innotest[Aβ1 - 42]) + 7.15 |
| T-Tau | Elecsys(T-Tau) = (0.475*Innotest[T-Tau]) + 66.0 |
| P-Tau181 | Elecsys(P-Tau181) = (0.419*Innotest[P-Tau181]) – 3.87 |
Aβ1 - 42, amyloid beta 1–42; t-Tau, total tau protein; P-Tau181, phosphorylated tau. Elecsys(x) = Elecsys value for biomarker x; Innotest[x] = Innotest value for biomarker x.
Brain biopsies
The brain biopsy procedure has been described in detail previously [23]. Briefly, three cylindrical brain biopsies 2–5 mm in diameter and 3–7 mm in length were acquired during shunt surgery, prior to the insertion of a CSF shunt, using a TTI46 biopsy needle (Merit Medical Systems Inc, South Jordan, UT, USA). Biopsy samples were placed in buffered formalin and embedded in paraffin. Paraffin-embedded samples were cut into sections 7μm thick that were stained with hematoxylin-eosin and subjected to immunohistochemistry for Aβ (Clone; 6F/3D, Company; Dako), hyperphosphorylated tau (Clone; AT8, company; Innogenetics, Ghent, Belgium), and p62 (Clone; 3, Company; BD Biosciences Pharmingen, Franklin Lakes, NJ, USA). The stained sections were assessed under a light microscope by a neuropathologist. Aβ pathology was semiquantitatively assessed by a neuropathologist by counting plaques under a light microscope, and tau pathology was graded as either present or absent [23, 27, 28]. iNPH patients were divided into groups based on AD pathology, as follows: Aβ– τ– , Aβ+ τ– , Aβ+ τ+, and Aβ– τ+. For this study, the groups were designated accordingly as iNPH AD– , iNPH Aβ, iNPH Aβ/T, and iNPH T.
Statistical methods
SPSS Statistics (version 27.0 SPSS Inc, Chicago, IL, USA) was used for statistical analyses. Independent samples t-tests were used to compare groups. Ratios between groups were calculated, as were sensitivities and specificities for different cutoff values. The correction factor for the effect of iNPH was calculated by determining the ratio of means between the iNPH AD- and healthy control groups. Linear regression was used to determine the optimal cutoff value for the ratio of P-Tau181 and Aβ1 - 42. This cutoff was chosen by ignoring the intercept of linear regression and using the regression coefficient between P-Tau181 and Aβ1 - 42 as the suggested cutoff value. A receiver operating characteristic curve was used to determine the goodness of the model for the ratio of P-Tau181 and Aβ1 - 42 in predicting AD pathology in iNPH patients. Sensitivity and specificity for the model were calculated.
Six patients had Aβ1 - 42 values over the highest measurement limit of 1700 ng/ml, and these values were replaced with 1700 ng/ml for analyses. Fifteen patients had P-Tau181 values below the lower limit of 8 pg/ml, and these were replaced with 8 pg/ml for analyses. One patient had P-Tau181 under the lower limit of detection of the Innotest kit (13 pg/ml), and this value was replaced with 13 pg/ml and converted to the Elecsys level. Including these patients in the analyses with the chosen values created less skew in the study than eliminating them.
Ethics statement
The study was approved by the Research Ethics Committee of the Northern Savo Hospital District. All participants gave written informed consent, and this study was conducted according to the latest revision of the Declaration of Helsinki.
RESULTS
All between-group comparisons of healthy control, iNPH AD– , iNPH AD+, and AD control groups were statistically significant (p < 0.05) for all investigated biomarkers, with the exception of t-Tau between the control and iNPH AD+ groups. Shunt response did not have statistically significant difference between groups using chi-square test. Using current cutoffs for the general population yielded a sensitivity of 0.8% and specificity of 100% for AD pathology in the iNPH population. Correction factors calculated for the different biomarkers in iNPH were as follows: 0.842 for Aβ1 - 42, 0.779 for t-Tau, and 0.610 for P-Tau181. Using these factors to determine the cutoff for AD in iNPH patients yielded a sensitivity of 2.4% and specificity of 100% .
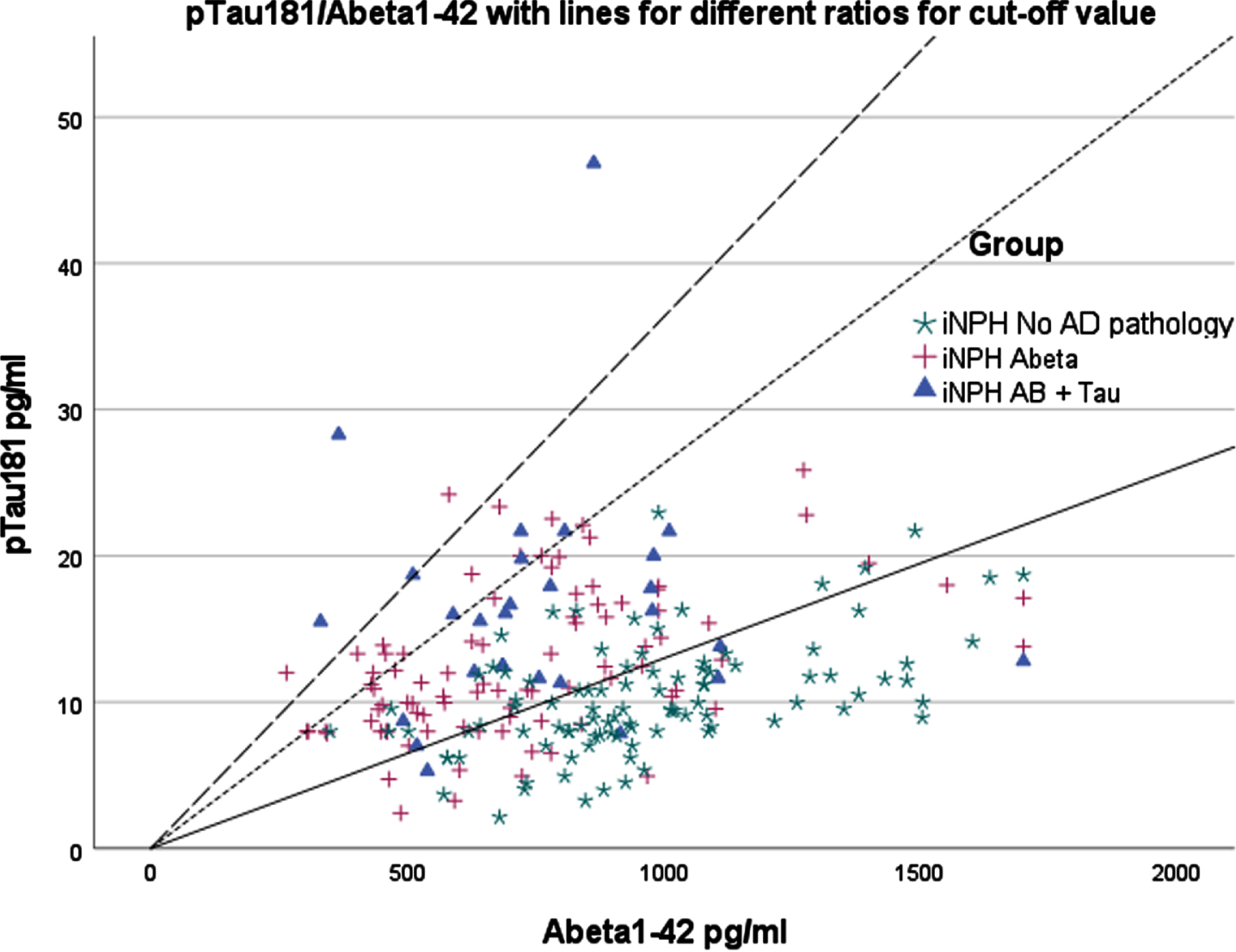
Since correction for cutoff values did not give satisfactory results, we evaluated the ratio of P-Tau181 and Aβ1 - 42 for this purpose. Figure 2 shows the P-Tau181/Aβ1 - 42 ratios and three different cutoff points. With a cutoff determined by linear regression analysis (P-tau181/Aβ1 - 42 = 0.013), the model sensitivity was 0.79, and its specificity was 0.76. The P-Tau181/Aβ1 - 42 ratio yielded a receiver operating characteristic area under the curve of 0.824 (95% confidence interval 0.769–0.880).
Fig. 2
P-Tau181/Aβ1 - 42 ratio. Different lines indicate different potential cutoffs for the ratio. pTau181, phosphorylated tau from lumbar sample; Abeta1-42, Aβ1 - 42 from lumbar sample. Continuous line indicates ratio obtained from linear regression analysis (0.013). Line with large dashes indicates ratio as defined by cutoffs used for general population (0.0364). Line with short dashes indicates ratio with cutoffs using correction factor (0.0263).
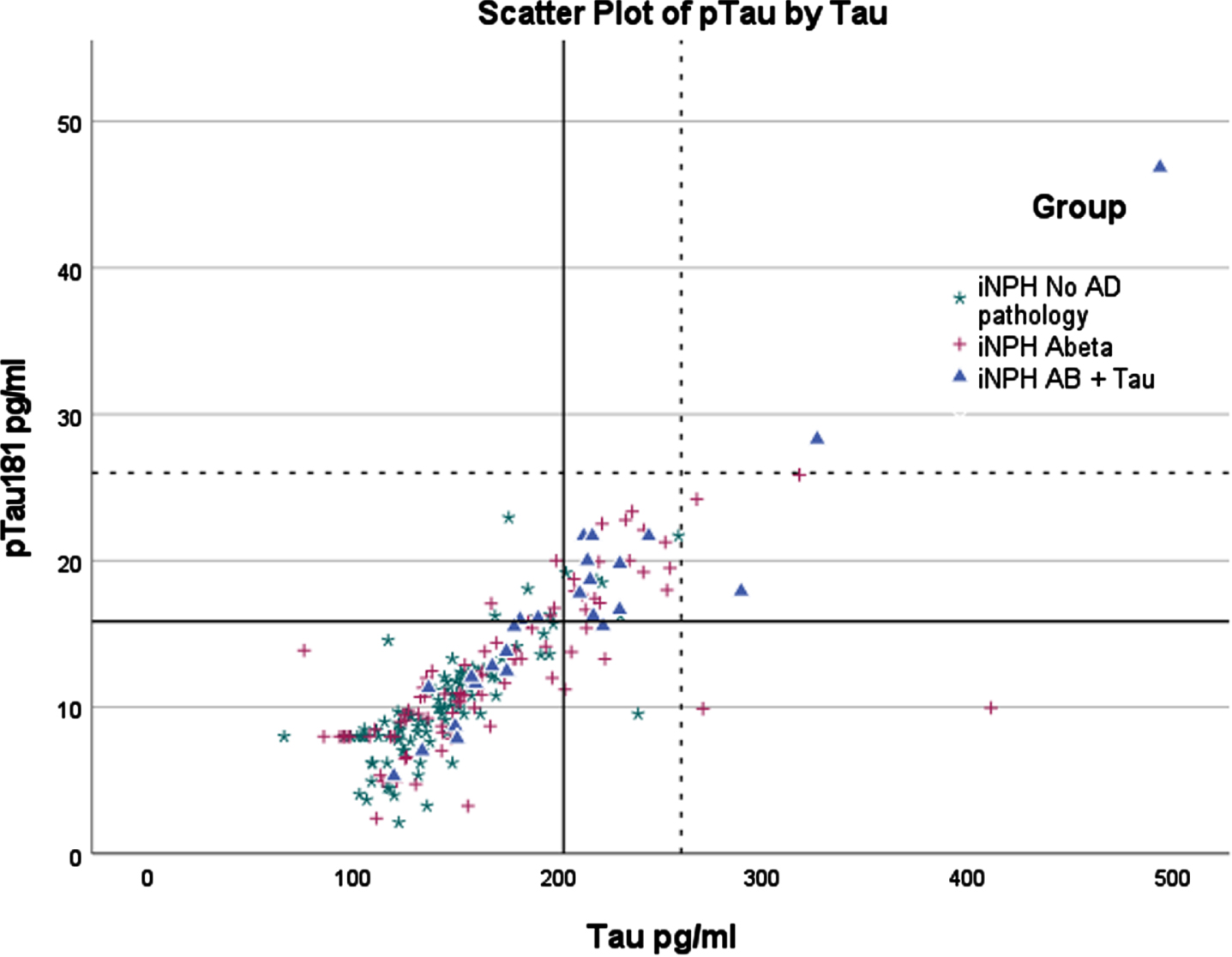
Figures 3–5 depict cutoff values for each biomarker with and without the correction factors applied. As the figures show, using uncorrected biomarker levels as the cutoff values yielded low diagnostic accuracy for AD pathology.
Fig. 3
Scatterplot of P-Tau181 and Aβ1 - 42 with upper left quadrant indicating pathological values. pTau181, phosphorylated tau from lumbar sample; Abeta1-42, Aβ1 - 42 from lumbar sample. Axis values are in pg/ml. Continuous line indicates cutoff values with correction factor. Dotted line indicates cutoff values for general population.
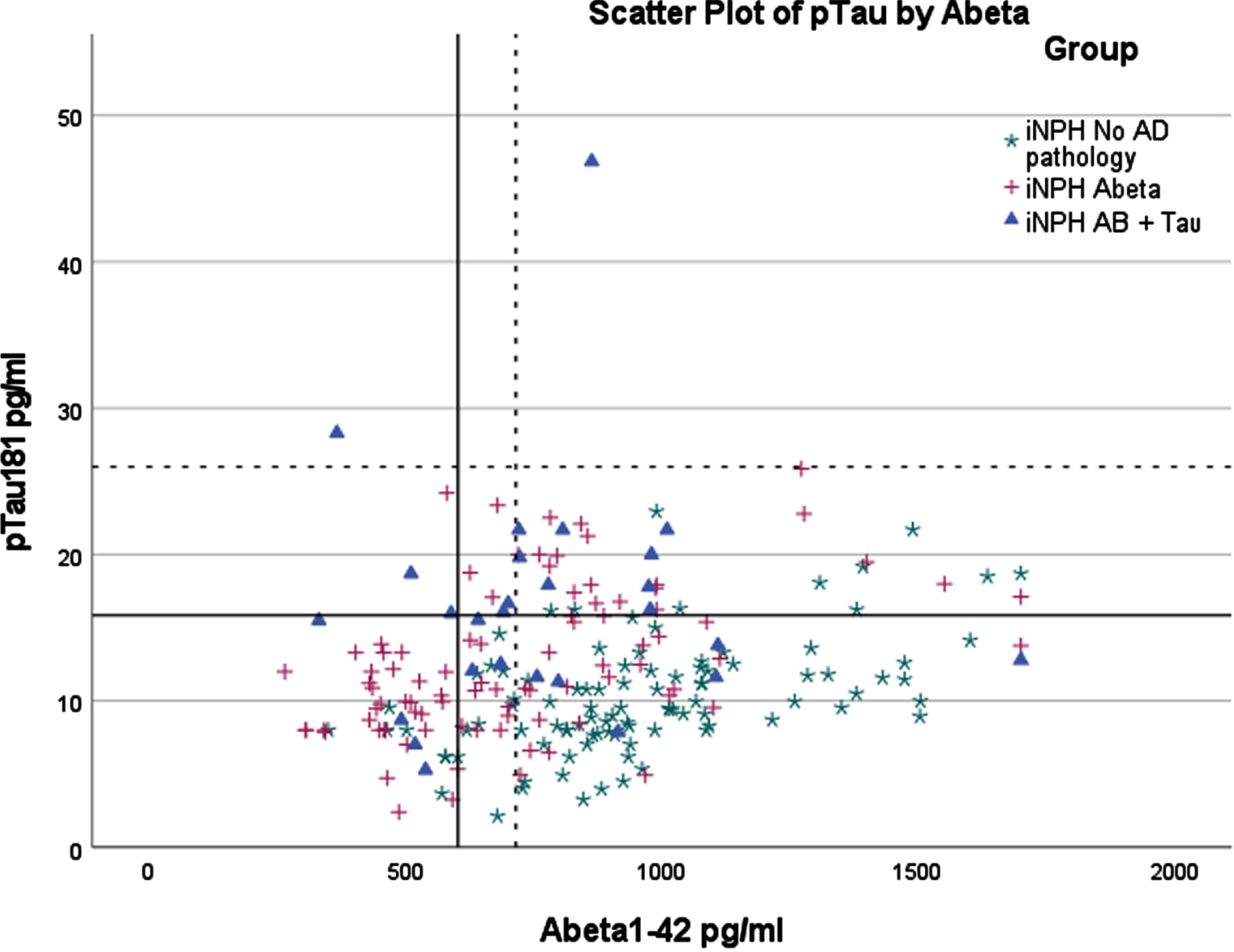
Fig. 4
Scatterplot of t-Tau and Aβ1 - 42 with upper left quadrant indicating pathological values. t-Tau, t-Tau from lumbar sample; Abeta1-42, Aβ1 - 42 from lumbar sample. Axis values are in pg/ml. Continuous line indicates cutoff values with correction factor. Dotted line indicates cutoff values for general population.
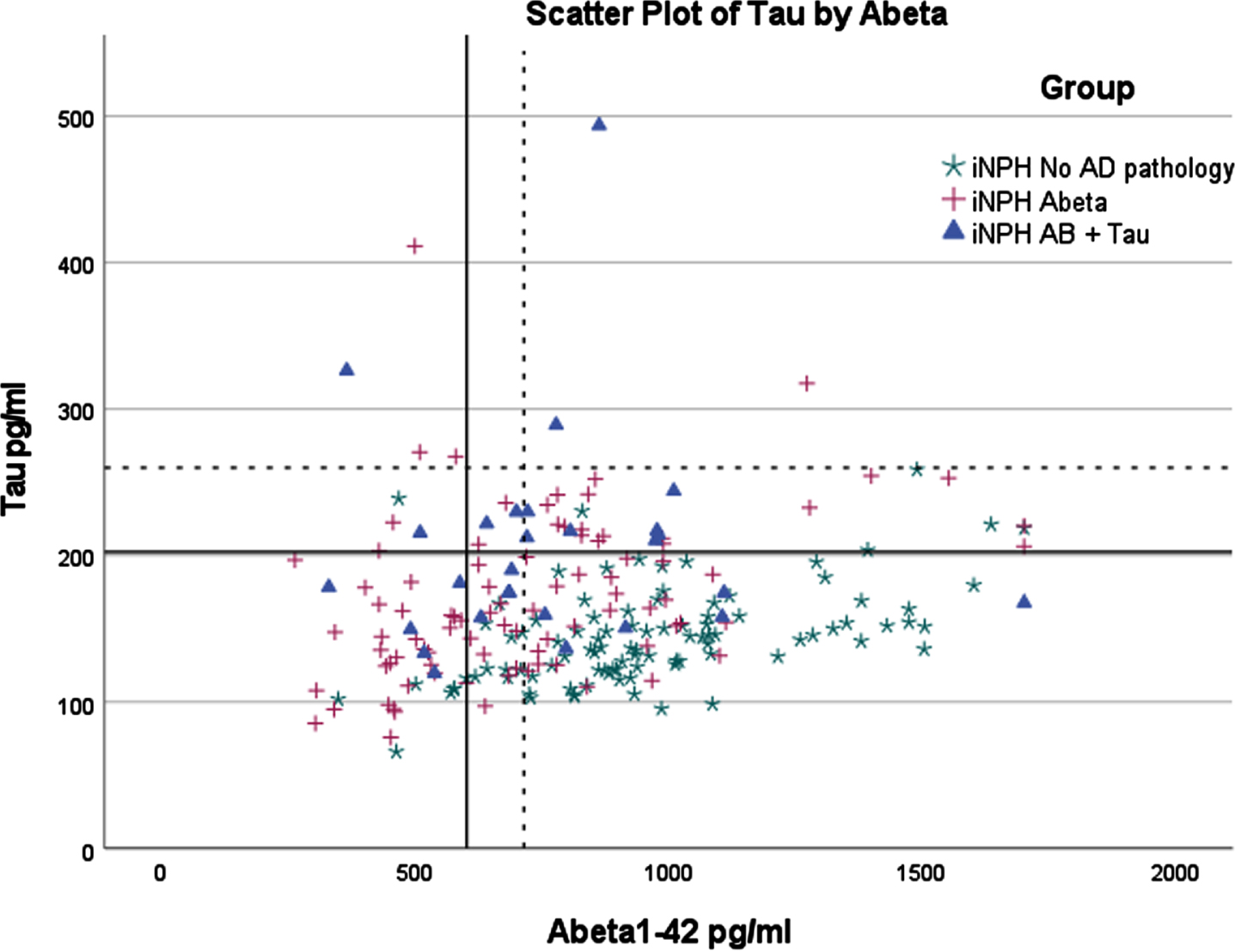
Fig. 5
Scatterplot for p-Tau181 and t-Tau. Upper right quadrant indicates pathological values. pTau181, phosphorylated tau from lumbar sample; t-Tau, t-Tau from lumbar sample. Axis values are in pg/ml. Continuous line indicates cutoff values with correction factor. Dotted line indicates cutoff values for general population.
DISCUSSION
Here, we investigated the diagnostic value of AD biomarkers in the iNPH population and found that correction factors cannot compensate for the effect of iNPH on CSF AD biomarkers. Applying the correction yielded a high specificity with almost no sensitivity but using cutoffs for the general population had even lower sensitivity. One possible explanation is that in patients shunted because of iNPH, AD is still in the early stage compared with the usual timing of an AD diagnosis reliant on clinical symptoms only. Aβ1 - 42 levels decrease as AD progresses, while t-Tau and P-Tau181 levels increase. The decline in Aβ1 - 42 is considered to be the result of aggregation of Aβ plaques, whereas increased tau can be seen as a sign of neuronal damage [19, 29]. This pattern might explain why even though biomarker levels are generally reduced in iNPH, amyloid levels in iNPH patients with AD pathology were higher than in our AD control group. For t-Tau and P-Tau181, this effect appeared to be less pronounced. Another possible explanation for this difference is that the clearance mechanism of Aβ1 - 42 differs in the context of iNPH with AD when compared with non-comorbid AD [30, 31]. A possible explanation for this is difference between white matter lesions between AD and iNPH, which may affect CSF flow in iNPH patients. Although, these changes may also be caused by impaired CSF flow [32]. Genome mapping has revealed that Aβ1 - 42 and P-Tau181 levels are mainly associated with different genetic loci, hinting at independent pathological processes and potentially explaining the different behavior of these biomarkers in iNPH. That study further identified a potential overlap in genetic etiology for tau levels and ventricular volume [33].
We also found that the ratio of P-Tau181 and Aβ1 - 42 was fairly good at predicting AD pathology in iNPH patients. A high ratio of P-Tau181 to Aβ1 - 42 has been reported previously in patients experiencing a poor response to shunting and as correlating with AD pathology [34].
The strengths of our study include the relatively large number of iNPH patients whose CSF biomarker, biopsy, and follow-up data could be gathered systematically. The presence of amyloid pathology in biopsy is a strong predictor for a future clinical diagnosis of AD [9]. Furthermore, presence of amyloid on biopsy is correlated with amyloid pathology on PET imaging [35]. Still, due to the potentially patchy nature of amyloid pathology, a false negative finding should be considered. The most significant limitation of our study is the lack of follow-up AD diagnosis data for shunted patients. This lack is largely because most patients in this cohort had been recently shunted, so the follow-up period could still be considered as in progress. Another limitation is that the Roche Elecsys method used in the CSF analyses included transferring samples, which has the potential to decrease Aβ1 - 42 levels. It might be considered a limitation that we did not investigate ventricular CSF in this study because our aim was to investigate lumbar CSF available for diagnostic purposes.
The cause of decreased CSF biomarker levels in iNPH is not yet clear, but among the plausible hypotheses is a dilution effect from the increased CSF volume. The results of one study using volumetric analysis and the association of ventricular volume with CSF AD biomarkers do not support this hypothesis, but further research in this area is needed [36]. Other reasonable hypotheses include reduced cortical metabolism, decreased clearance, or changes in CSF flow [20, 21, 22, 37].
Interestingly, in our cohort there was no significant difference in shunt response between groups. This may be due to the short follow-up period available in our cohort. With longer follow-up period the presence of AD pathology is associated with development of clinical AD [9]. Elevated levels of P-Tau181 and t-Tau seem to be associated with worse response to shunt surgery while Aβ1 - 42 levels do not seem to differentiate shunt responders from non-responders [38]. In a recent study iNPH patients with AD seem to get similar gains from shunt surgery initially but failed to keep improvements in executive functions. Although the study lost a significant number of participants during follow-up, which may affect results [39]. In our study patients with amyloid pathology in cortical biopsy have higher levels of both P-Tau181 and t-Tau, which could indicate that patients with elevated levels of tau-proteins are at higher risk of developing AD at follow-up, which logically leads to worse outcome of shunt procedure. More research is still needed to figure out whether AD-related CSF markers can be used to determine shunt response.
Overall, our findings indicate that the ratio of P-Tau181 and Aβ1 - 42 is a useful tool for predicting AD pathology in iNPH patients but should not be used to exclude patients from a shunt operation. We also determined that attempting to address the effect of iNPH on biomarkers by using a correction factor did not improve accuracy in AD diagnosis of iNPH patients at the preoperative stage.
ACKNOWLEDGMENTS
We acknowledge Marita Parviainen, RN, and Tiina Laaksonen, RN, for assistance and cognitive testing and San Francisco Edit for editing.
FUNDING
The study was funded by Kuopio University Hospital VTR fund (Grant number: 5252614), Academy of Finland (#339767, 338182), Sigrid Juselius Foundation (no specified grant number), the Strategic Neuroscience Funding of the University of Eastern Finland, the Finnish Cultural Foundation, North Savo Regional Fund (#65221674), Alzheimer’s Association AD Strategic Fund (#ADSF-21-831386-C), Maire Taponen Foundation, and The Finnish Medical Foundation. HZ is a Wallenberg Scholar supported by grants from the Swedish Research Council (#2022-01018), the European Union’s Horizon Europe research and innovation programme under grant agreement No 101053962, Swedish State Support for Clinical Research (#ALFGBG-71320), and the AD Strategic Fund and the Alzheimer’s Association (#ADSF-21-831376-C, #ADSF-21-831381-C, and #ADSF-21-831377-C).
CONFLICT OF INTEREST
HZ has served on scientific advisory boards or as a consultant for Abbvie, Acumen, Alector, Alzinova, ALZPath, Annexon, Apellis, Artery Therapeutics, AZTherapies, CogRx, Denali, Eisai, Nervgen, Novo Nordisk, Optoceutics, Passage Bio, Pinteon Therapeutics, Prothena, Red Abbey Labs, reMYND, Roche, Samumed, Siemens Healthineers, Triplet Therapeutics, and Wave; has given lectures at symposia sponsored by Cellectricon, Fujirebio, Alzecure, Biogen, and Roche; and is a co-founder of Brain Biomarker Solutions in Gothenburg AB (BBS), which is a part of the GU Ventures Incubator Program (outside submitted work).
Heikki Lukkarinen and Henrik Zetterberg are Editorial Board Members of this journal but were not involved in the peer-review process nor had access to any information regarding its peer-review.
The other authors report no conflicts of interest.
DATA AVAILABILITY
Study data cannot be made public because of patient confidentiality issues. Anonymized data can be made available upon a reasonable request.
REFERENCES
[1] | Relktin N , Marmarou A , Klinge P , Bergsneider M , Black PML ((2005) ) INPH guidelines, part II: Diagnosing idio-pathic normal-pressure hydrocephalus. Neurosurgery 57: , A2-4-S2-16. |
[2] | Andersson J , Rosell M , Kockum K , Lilja-Lund O , Söderström L , Laurell K ((2019) ) Prevalence of idiopathic normal pressure hydrocephalus: A prospective, population based study. PLoS One 14: , e0217705. |
[3] | Alvi MA , Brown D , Yolcu Y , Zreik J , Javeed S , Bydon M , Cutsforth-Gregory JK , Graff-Radford J , Jones DT , Graff-Radford NR , Cogswell PM , Elder BD ((2021) ) Prevalence and trends in management ofidiopathic normal pressure hydrocephalus in the United States:Insights from the national inpatient sample. World Neurosurg 145: , e38–e52. |
[4] | Nakajima M , Yamada S , Miyajima M , Ishii K , Kuriyama N , Kazui H , Kanemoto H , Suehiro T , Yoshiyama K , Kameda M , Kajimoto Y , Mase M , Murai H , Kita D , Kimura T , Samejima N , Tokuda T , Kaijima M , Akiba C , Kawamura K , Atsuchi M , Hirata Y , Matsumae M , Sasaki M , Yamashita F , Aoki S , Irie R , Miyake H , Kato T , Mori E , Ishikawa M , Date I , Arai H ; research committee of idiopathic normal pressure hydrocephalus ((2021) ) Guidelines for management of idiopathic normal pressure hydrocephalus (Third edition): Endorsed by the Japanese society of normal pressure hydrocephalus. Neurol Med Chir (Tokyo) 61: , 63–97. |
[5] | Junkkari A , Häyrinen A , Rauramaa T , Sintonen H , Nerg O , Koivisto AM , Roine RP , Viinamäki H , Soininen H , Luikku A , Jääskeläinen JE , Leinonen V ((2017) ) Health-related quality-of-life outcome in patients with idiopathic normal-pressure hydrocephalus – a 1-year follow-up study. Eur J Neurol 24: , 58–66. |
[6] | Yang HW , Lee S , Yang D , Dai H , Zhang Y , Han L , Zhao S , Zhang S , Ma Y , Johnson MF , Rattray AK , Johnson TA , Wang G , Zheng S , Carroll RS , Park PJ , Johnson MD ((2021) ) Deletions in CWH43 cause idiopathic normal pressure hydrocephalus. EMBO Mol Med 13: , e13249. |
[7] | Koivisto AM , Alafuzoff I , Savolainen S , Sutela A , Rummukainen J , Kurki M , Jääskeläinen JE , Soininen H , Rinne J , Leinonen V ; Kuopio NPH Registry (www.uef.finph) ((2013) ) Poor cognitive outcome in shunt-responsive idiopathic normal pressure hydrocephalus. Neurosurgery 72: , 1–8. |
[8] | Bådagård H , Braun M , Nilsson D , Stridh L , Virhammar J ((2020) ) Negative predictors of shunt surgery outcome in normal pressure hydrocephalus. Acta Neurol Scand 141: , 219–225. |
[9] | Luikku AJ , Hall A , Nerg O , Koivisto AM , Hiltunen M , Helisalmi S , Herukka SK , Junkkari A , Sutela A , Kojoukhova M , Korhonen V , Mattila J , Lötjönen J , Rummukainen J , Alafuzoff I , Jääskeläinen JE , Remes AM , Solomon A , Kivipelto M , Soininen H , Rauramaa T , Leinonen V ((2019) ) Predicting development of Alzheimer’s disease in patients with shunted idiopathic normal pressure hydrocephalus. J Alzheimers Dis 71: , 1233–1243. |
[10] | Zetterberg H , Bendlin BB ((2021) ) Biomarkers for Alzheimer’s disease— preparing for a new era of disease-modifying therapies. Mol Psychiatry 26: , 296–308. |
[11] | Shim YS , Yoon B , Na S , Lim EY , Hong YJ , Yang DW ((2021) ) A systematic review and meta-analysis of the clinical effects of Souvenaid in patients with Alzheimer’s disease. Asia Pac J Clin Nutr 30: , 30–41. |
[12] | Cummings JL , Tong G , Ballard C ((2019) ) Treatment combinations for Alzheimer’s disease: Current and future pharmacotherapy options. J Alzheimers Dis 67: , 779–794. |
[13] | van Dyck CH , Swanson CJ , Aisen P , Bateman RJ , Chen C , Gee M , Kanekiyo M , Li D , Reyderman L , Cohen S , Froelich L , Katayama S , Sabbagh M , Vellas B , Watson D , Dhadda S , Irizarry M , Kramer LD , Iwatsubo T ((2022) ) Lecanemab in early Alzheimer’s disease. N Engl J Med 388: , 9–21. |
[14] | Nelson L , Tabet N ((2015) ) Slowing the progression of Alzheimer’s disease; what works? Ageing Res Rev 23: , 193–209. |
[15] | Cacabelos R , Naidoo V , Martínez-Iglesias O , Corzo L , Cacabelos N , Pego R , Carril JC ((2022) ) Personalized management and treatment of Alzheimer’s disease. Life (Basel) 12: , 460. |
[16] | De la Rosa A , Olaso-Gonzalez G , Arc-Chagnaud C , Millan F , Salvador-Pascual A , García-Lucerga C , Blasco-Lafarga C , Garcia-Dominguez E , Carretero A , Correas AG , Viña J , Gomez-Cabrera MC ((2020) ) Physical exercise in the prevention and treatment of Alzheimer’s disease. J Sport Heal Sci 9: , 394–404. |
[17] | Scheltens P , Strooper B De , Kivipelto M , Holstege H , Chételat G , Teunissen CE , Cummings J , Flier WM Van Der ((2021) ) Alzheimer’sdisease. Lancet 397: , 1577–1590. |
[18] | Jack CR , Knopman DS , Jagust WJ , Petersen RC , Weiner MW , Aisen PS , Shaw LM , Vemuri P , Wiste HJ , Weigand SD , Lesnick TG , Pankratz VS , Donohue MC , Trojanowski JQ ((2013) ) Tracking pathophysiological processes in Alzheimer’s disease: An updated hypothetical model of dynamic biomarkers. Lancet Neurol 12: , 207–216. |
[19] | Blennow K , Zetterberg H ((2018) ) Biomarkers for Alzheimer’s disease: Current status and prospects for the future. J Intern Med 284: , 643–663. |
[20] | Graff-Radford NR ((2014) ) Alzheimer CSF biomarkers may be misleading in normal-pressure hydrocephalus. Neurology 83: , 1573–1575. |
[21] | Jeppsson A , Zetterberg H , Blennow K , Wikkelsø C ((2013) ) Idiopathic normal-pressure hydrocephalus pathophysiology and diagnosis by CSF biomarkers. Neurology 80: , 1385–1392. |
[22] | Jeppsson A , Wikkelsö C , Blennow K , Zetterberg H , Constantinescu R , Remes AM , Herukka SK , Rauramaa T , Nagga K , Leinonen V , Tullberg M ((2019) ) CSF biomarkers distinguish idiopathic normal pressure hydrocephalus from its mimics. J Neurol Neurosurg Psychiatry 90: , 1117–1123. |
[23] | Junkkari A , Luikku AJ , Danner N , Jyrkkänen HK , Rauramaa T , Korhonen VE , Koivisto AM , Nerg O , Kojoukhova M , Huttunen TJ , Jääskeläinen JE , Leinonen V ((2019) ) The Kuopio idiopathic normal pressure hydrocephalus protocol: Initial outcome of 175 patients. Fluids Barriers CNS 16: , 21. |
[24] | Vanninen A , Nakajima M , Miyajima M , Rauramaa T , Kokki M , Musialowicz T , Mäkinen PM , Herukka SK , Koivisto AM , Jääskeläinen JE , Hiltunen M , Leinonen V ((2021) ) Elevated CSF LRG and decreased Alzheimer’s disease biomarkers in idiopathic normal pressure hydrocephalus. J Clin Med 10: , 1105. |
[25] | Kokkonen N , Herukka SK , Huilaja L , Kokki M , Koivisto AM , Hartikainen P , Remes AM , Tasanen K ((2017) ) Increased levels of the bullous pemphigoid BP180 autoantibody are associated with more severe dementia in Alzheimer’s disease. J Invest Dermatol 137: , 71–76. |
[26] | Willemse EAJ , van Maurik IS , Tijms BM , Bouwman FH , Franke A , Hubeek I , Boelaarts L , Claus JJ , Korf ESC , van Marum RJ , Roks G , Schoonenboom N , Verwey N , Zwan MD , Wahl S , van der Flier WM , Teunissen CE ((2018) ) Diagnostic performance of Elecsys immunoassays for cerebrospinal fluid Alzheimer’s disease biomarkers in a nonacademic, multicenter memory clinic cohort: The ABIDE project. Alzheimers Dement 10: , 563–572. |
[27] | Seppälä TT , Nerg O , Koivisto AM , Rummukainen J , Puli L , Zetterberg H , Pyykkö OT , Helisalmi S , Alafuzoff I , Hiltunen M , Jääskeläinen JE , Rinne J , Soininen H , Leinonen V , Herukka SK ((2012) ) CSF biomarkers for Alzheimer disease correlate with cortical brain biopsy findings. Neurology 78: , 1568–1575. |
[28] | Leinonen V , Rauramaa T , Johansson J , Bottelbergs A , Tesseur I , Van Der Ark P , Pemberton D , Koivisto AM , Jääskeläinen JE , Hiltunen M , Herukka SK , Blennow K , Zetterberg H , Jokinen P , Rokka J , Helin S , Haaparanta-Solin M , Solin O , Okamura N , Kolb HC , Rinne JO ((2018) ) S-[18 F]THK-5117-PET and [11 C]PIB-PET imaging in idiopathic normal pressure hydrocephalus in relation to confirmed amyloid-β plaques and tau in brain biopsies. J Alzheimers Dis 64: , 171–179. |
[29] | Ibarra R , Radanovic M , Pais MV , Talib LL , Forlenza OV ((2021) ) AD-related CSF biomarkers across distinct levels of cognitive impairment: Correlations with global cognitive state. J Geriatr Psychiatry Neurol 34: , 659–667. |
[30] | Kim HJ , Lim TS , Lee SM , Kim TS , Kim Y , An YS , Youn YC , Park SA , Chang J , Moon SY ((2019) ) Cerebrospinal fluid levels of β-amyloid 40 and β-amyloid 42 are proportionately decreased in amyloid positron-emission tomography negative idiopathic normal-pressure hydrocephalus patients. J Clin Neurol 15: , 353–359. |
[31] | Jingami N , Asada-Utsugi M , Uemura K , Noto R , Takahashi M , Ozaki A , Kihara T , Kageyama T , Takahashi R , Shimohama S , Kinoshita A ((2015) ) Idiopathic normal pressure hydrocephalus has a different cerebrospinal fluid biomarker profile from Alzheimer’s disease. J Alzheimers Dis 45: , 109–115. |
[32] | Kuroda T , Honma M , Mori Y , Futamura A , Sugimoto A , Kasai H , Yano S , Hieda S , Kasuga K , Ikeuchi T , Ono K ((2022) ) White matter lesions may aid in differentiating idiopathic normal pressure hydrocephalus and Alzheimer’s disease. J Alzheimers Dis 85: , 851–862. |
[33] | Jansen IE , van der Lee SJ , Gomez-Fonseca D , de Rojas I , Dalmasso MC , Grenier-Boley B , Zettergren A , Mishra A , Ali M , Andrade V , Bellenguez C , Kleineidam L , Küçükali F , Sung YJ , Tesí N , Vromen EM , Wightman DP , Alcolea D , Alegret M , Alvarez I , Amouyel P , Athanasiu L , Bahrami S , Bailly H , Belbin O , Bergh S , Bertram L , Biessels GJ , Blennow K , Blesa R , Boada M , Boland A , Buerger K , Carracedo Á , Cervera-Carles L , Chene G , Claassen JAHR , Debette S , Deleuze JF , de Deyn PP , Diehl-Schmid J , Djurovic S , Dols-Icardo O , Dufouil C , Duron E , Düzel E , Fladby T , Fortea J , Frölich L , García-González P , Garcia-Martinez M , Giegling I , Goldhardt O , Gobom J , Grimmer T , Haapasalo A , Hampel H , Hanon O , Hausner L , Heilmann-Heimbach S , Helisalmi S , Heneka MT , Hernández I , Herukka SK , Holstege H , Jarholm J , Kern S , Knapskog AB , Koivisto AM , Kornhuber J , Kuulasmaa T , Lage C , Laske C , Leinonen V , Lewczuk P , Lleó A , de Munain AL , Lopez-Garcia S , Maier W , Marquié M , Mol MO , Montrreal L , Moreno F , Moreno-Grau S , Nicolas G , Nöthen MM , Orellana A , Pålhaugen L , Papma JM , Pasquier F , Perneczky R , Peters O , Pijnenburg YAL , Popp J , Posthuma D , Pozueta A , Priller J , Puerta R , Quintela I , Ramakers I , Rodriguez-Rodriguez E , Rujescu D , Saltvedt I , Sanchez-Juan P , Scheltens P , Scherbaum N , Schmid M , Schneider A , Selbæk G , Selnes P , Shadrin A , Skoog I , Soininen H , Tárraga L , Teipel S , Tijms B , Tsolaki M , VanBroeckhoven C , Van Dongen J , van Swieten JC , Vandenberghe R , Vidal JS , Visser PJ , Vogelgsang J , Waern M , Wagner M , Wiltfang J , Wittens MMJ , Zetterberg H , Zulaica M , van Duijn CM , Bjerke M , Engelborghs S , Jessen F , Teunissen CE , Pastor P , Hiltunen M , Ingelsson M , Andreassen OA , Clarimón J , Sleegers K , Ruiz A , Ramirez A , Cruchaga C , Lambert JC , van der Flier W ((2022) ) Genome-widemeta-analysis for Alzheimer’s disease cerebrospinal fluidbiomarkers. Acta Neuropathol 144: , 821–842. |
[34] | Patel S , Lee EB , Xie SX , Law A , Jackson EM , Arnold SE , Clark CM , Shaw LM , Grady MS , Trojanowski JQ , Hamilton RH ((2012) ) Phosphorylated tau/amyloid beta 1-42 ratio in ventricular cerebrospinal fluid reflects outcome in idiopathic normal pressure hydrocephalus. Fluids Barriers CNS 9: , 7. |
[35] | Rinne JO , Wong DF , Wolk DA , Leinonen V , Arnold SE , Buckley C , Smith A , McLain R , Sherwin PF , Farrar G , Kailajärvi M , Grachev ID ((2012) ) Flutemetamol PET imaging and cortical biopsy histopathology for fibrillar amyloid β detection in living subjects with normal pressure hydrocephalus: Pooled analysis of four studies. Acta Neuropathol 124: , 833–845. |
[36] | Lidén S , Farahmand D , Laurell K ((2022) ) Ventricular volume inrelation to lumbar CSF levels of amyloid-β 1–42, tauand phosphorylated tau in iNPH, is there a dilution effect? Fluids Barriers CNS 19: , 59. |
[37] | Lindstrøm EK , Ringstad G , Mardal KA , Eide PK ((2018) ) Cerebrospinal fluid volumetric net flow rate and direction in idiopathic normal pressure hydrocephalus. Neuroimage Clin 20: , 731–741. |
[38] | Thavarajasingam SG , El-Khatib M , Vemulapalli KV , Iradukunda HAS , Laleye J , Russo S , Eichhorn C , Eide PK ((2022) ) Cerebrospinal fluid and venous biomarkers of shunt-responsive idiopathic normal pressure hydrocephalus: A systematic review and meta-analysis. Acta Neurochir (Wien) 164: , 1719–1746. |
[39] | Gold D , Wisialowski C , Piryatinsky I , Malloy P , Correia S , Salloway S , Klinge P , Gaudet CE , Niermeyer M , Lee A ((2022) ) Longitudinal post-shunt outcomes in idiopathic normal pressure hydrocephalus with and without comorbid Alzheimer’s disease.. J Int Neuropsychol Soc. doi: 10.1017/S1355617722000868. |




