The Dementia Assessment of Service Needs (DEMAND): Development and Validation of a Standardized Needs Assessment Instrument
Abstract
Background:
Dementia is one of the main triggers for care dependency among older adults who are predominantly cared for at home by relatives. To provide support in the care situation, health systems need valid information about the central needs of the affected people.
Objective:
The present study aimed to develop a research instrument to assess the most important needs of people with dementia and their family caregivers.
Methods:
The development of the ‘Dementia Assessment of Service Needs (DEMAND)’ took place within the project ‘Digital Dementia Registry Bavaria (digiDEM Bayern)’. A focus group and an online survey with dementia experts were conducted to identify the most relevant support services and to develop the design of the instrument. The questionnaire was deployed in the digiDEM baseline data collection. Participants were asked to evaluate the comprehensibility of the questionnaire. Readability was assessed using the Flesch reading ease score.
Results:
Seventeen experts participated in the focus group and 59 people in the online survey. The final questionnaire included 13 support services. One hundred eighty-three participants (50 people with dementia and 133 family caregivers) completed the questionnaire at baseline. The mean comprehensibility score was 3.6 (SD = 2.3). The Flesch reading ease score result was 76.
Conclusion:
A research instrument could be developed, enabling people with dementia and family caregivers to directly express their individual needs for specific support services. Results show that the DEMAND is easy to understand and short in execution. Therefore, supply gaps can be identified and transformed into a specific health care plan.
INTRODUCTION
Dementia is one of the main triggers for care dependency among older adults [1]. Most of the people with dementia are cared for at home by relatives [2, 3], which are at increased risk for burden, stress, and health-related problems [4–6]. In order to provide a health care policy that is beneficial for people with dementia and their family caregivers, health care decision-makers need valid information about the central needs of those people and how to meet them.
Hitherto, there is no theoretical conceptualization of the needs of dementia family caregivers [7]. However, Stirling et al. developed a typology of need in a mixed-methods study, referring to Bradshaw’s sociological typology of need [8]. The typology distinguishes between normative need (professionally identified caregiver burden), felt need (need for a service articulated by service users), expressed need (service usage), and comparative need (comparison between groups of service users with groups of non-service users). Within the specific care situation, the needs and burden of dementia family caregivers are highly linked to the needs and service use of the people with dementia [9]. Hence, the identification of felt and expressed needs of people with dementia affects the entire care situation and consequently the situation of the family caregiver as well. In this respect, the utilization of care services of people with dementia can provide relief for family caregivers [9].
Studies and research instruments that examine felt needs, often assess those needs on a problem-centered level, irrespective of specific support services to meet such needs [10]. In this respect, the existence of a need is derived from participants’ expression of having problems in certain (care-related) areas or from specific disease-related symptoms of the people with dementia. This can be problematic, as needs derived from a problem- or symptom-centered perspective may not be met sufficiently by the offered services [10].
Thus, the aim of the present study was to develop a short and practical assessment instrument in order to assess the most important needs of people with dementia and their family caregivers by directly asking about the need for specific support services. As felt needs and expressed needs have a strong interdependence, the instrument aims to identify both expressed needs by asking about the former utilization of services and felt needs by asking about the demand of using support services in the future.
METHODS
Development of the assessment instrument
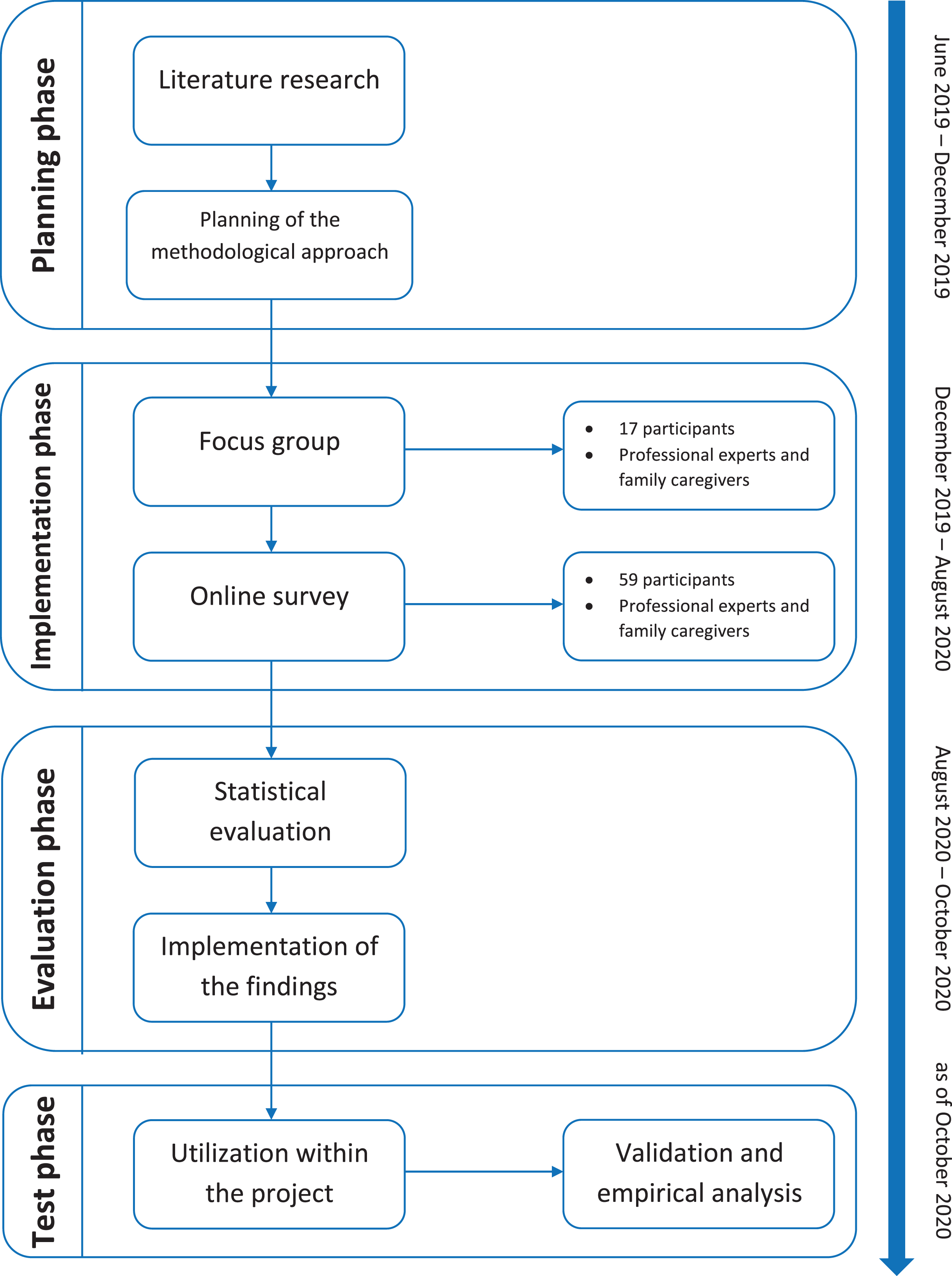
The development of the Dementia Assessment of Service Needs (DEMAND) (Fig. 1) took place in the frame of the project ‘Digital Dementia Registry Bavaria –digiDEM Bayern’. digiDEM is a multicenter, prospective, longitudinal register study including people with mild cognitive impairment (MCI) and mild to moderate dementia in Bavaria. All participants will undergo dementia screening prior to study inclusion, using Mini-Mental State Examination (MMSE) [11] and Montreal Cognitive Assessment (MoCA) [12]. The methodology of the project is described elsewhere [13]. Following the concept of Multi-criteria Decision Analysis (MCDA) [14], the development of the DEMAND was realized in close cooperation with experts from the field of dementia. In this respect, one focus group and one online survey were conducted.
Fig. 1
Development process of the DEMAND
Recruitment of experts
The definition of experts and the process of experts’ recruitment is based upon various methodological sources [15–18]. In the project, experts with different backgrounds in dementia care that dealt with dementia informally for at least two years or professionally for at least ten years were recruited. In this respect, for participating in the focus group, informal caregivers and patient representatives were recruited in order to include the perspective of the affected people as well as professional caregivers, medical staff, consultants for dementia care, and scientists. Experts were identified and chosen on dementia-specific events, past cooperation in former projects, and existing dementia networks.
Focus group
A focus group was conducted as a basis for the design of the data collection instrument, as focus groups are suitable for addressing multiple facets of and including multiple perspectives on an issue [19, 20]. Experts were asked to discuss two aspects. First, experts should identify all existing and imaginable support services for people with dementia and their family caregivers. Therefore, participants decided to distinguish support services according to the target group (people with dementia and family caregivers) and severity of dementia. The identified services were recorded on index cards and subsequently discussed with the experts in a moderated discussion. In a second step, experts should discuss the design of the different question items. Therefore, a predesigned pattern was presented and discussed in the focus group. The conversations were recorded with a digital recording device and subsequently transcribed. The content was evaluated according to the qualitative content analysis of Mayring [21], using MAXQDA 2018 (VERBI Software, 2017) [22]. The analysis of the interviews was performed according to the summarizing content analysis technique, following an iterative, inductive approach in order to identify the central categories of the transcribed conversations. The identification of the categories and the assignment of the content to the categories were performed independently by two authors. In cases of discrepancy, a consensus was reached discursively within the research group.
Online survey
In order to identify the most relevant support services, an online survey for anonymous data collection was conducted. Participants were asked to provide information about their biological sex, background, and years of experience in dementia care. Subsequently, experts should assess the identified services according to their relevance for dementia care. Based upon the analysis of the focus group, similar services were summarized in order to prevent redundant assessments. Experts should rate the services on a scale from one (not important) to ten (important). Those services rated higher than eight were included in the instrument. Following the MCDA approach, the threshold of eight for including a support service in the instrument was determined in cooperation with the experts of the focus group. A precondition for including the service in the instrument was a high rating of the service by both subgroups family caregivers and professional experts separately. Services with a rating lower than eight were not included in the instrument.
Validation
Validation measures were deployed during the development stages, including focus group and online survey, as well as during the baseline data collection stage in the frame of the research project digiDEM.
Content validity
In order to ensure content validity, the structure and phrasing of the instrument were developed in cooperation with the experts during the focus group [23]. Afterward, the online survey was used in order to make sure that the most important services in dementia care were measured [23].
Face validity
Comprehensibility
For further validation, the questionnaire was included in the data collection process of digiDEM. The study sample was completely disjunct from the sample of participants in the developmental process with no overlapping between both samples. Two disjunct samples were chosen, as participants contributing to the development of the research instrument should not be the same participating in further validation measures. Thus, a possible bias that affects the interpretation of the results should be avoided. Data collection was performed by means of standardized interviews. The questionnaire could be completed by both people with dementia and family caregivers. People with dementia were asked to complete the questionnaire only in case they participated as a single person. During the baseline interviews, participants were asked, if the instrument was clear and comprehensible by using the question: ‘On a scale of 1–10 (where 1 corresponds to very good and 10 to very poor), how understandable did you find the questions?’ Therefore, participants could assess comprehensibility on a scale from one (very good comprehensible) to ten (very bad comprehensible). Additionally, sensitivity analyses for people with MCI were performed, as most people with (amnestic) MCI do progress to dementia within five years [24].
Readability
For evaluation of the readability, the Flesch reading ease score was used [25]. The Flesch reading ease score has a range of 0 (practically unreadable) to 100 (easy for any literate person) [25].
Objectivity
For ensuring objectivity, a manual including an explanation of the content as well as the instruction for performing the instrument in an interview situation and for analyzing the results was developed. All interviewers in digiDEM received training in using the DEMAND questionnaire and got access to a manual. Training and manual comprised both paper-based and digital performance of the DEMAND.
Statistical analysis
Data of the online survey and the validation sample were analyzed using descriptive statistics (means, standard deviations (SD), and percentages) and presented in tables. In the study sample, baseline data (t0) were evaluated. Sociodemographic characteristics, caregiving time, diagnosis, and cognitive status (MMSE) were described. Data were analyzed using SPSS 28 (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp).
RESULTS
Development of the assessment instrument
Focus group
Seventeen experts participated in the focus group. Four informal caregivers, two professional caregivers, two medical practitioners, two patient representatives, three consultants for dementia care, and four scientists were included. The experts could identify 74 different support services in total. In the following qualitative evaluation process, the 74 support services could be summarized to 44 support services, which built the fundament for the subsequent online survey. Lists with all identified and summarized support services from the focus group are provided as Supplementary Material.
Online survey
Fifty-nine people finished the online survey. Participants were 30 informal caregivers, four professional caregivers, nine medical practitioners, one patient representative, eight consultants for dementia care, six scientists, and one citizen volunteer. Participants had on average 13 years of experience in dementia care (informal caregivers: 5.9 years; professional experts: 20.3 years). 66.0% of the participants were female. The five highest-rated services were primary care by a general practitioner, respite care, short-term care, adult daycare, and palliative care.
Structure and content of the instrument
The instrument consists of 13 care services. Additionally, the category “other service” is included in order to provide the option to mention the use of and need for services that are not part of the 13 care services. Each care service is provided with a formal definition in order to avoid different understandings of the care service and assessed according to the same structure. The first question assesses if a specific care service was used in the past 30 days. The time frame of 30 days was chosen in order to get valid information about frequently used services by simultaneously diminishing a possible recall bias of participants. Participants can reply that they did or did not use the service. Dependent on the answer, the interview follows two different paths.
If there was a utilization, participants should express how often the service was used and if there is a met or unmet need. Therefore, participants were asked if the utilization of the service was sufficient and satisfying (met need), if the utilization of the service was not satisfying (unmet need), or if there was a desire to use the service more often (unmet need).
In case there was no utilization of the service, participants were asked about the reasons for not using the care service. At this point, participants have the options to express that they did not know the service before the interview (no knowledge), that they do not need the service currently (no need), or if they wish to use the service but cannot do so due to certain reasons (unmet need). The prescribed answer options, in this case, are ‘The service is not available (e.g., no places available or the service doesn’t exist)’; ‘I cannot finance the service’; ‘Due to the distance I cannot reach the service or the service cannot come to me.’; ‘I am afraid that if I use the service the disease will become public; ‘The utilization is not possible due to personal (e.g., cultural) aspects’ or other reasons (free text field). Thus, changes in the availability and eligibility of services over time that result in a non-utilization of the services can be investigated. The answer ‘no knowledge’ could also be a hint at an unknown unmet need, as a specific yet unknown service might be useful in a specific situation for the respective people with dementia and their family caregivers.
For the investigation of timely changes in service use, the questionnaire should be repeated frequently every six months or annually as indicated by the International Consortium for Health Outcomes Measurement (ICHOM) for follow-up periods in research [26]. The duration of the instrument does not exceed 15 minutes on average.
Validation
One hundred eighty-three participants (50 people with dementia and 133 family caregivers) completed the DEMAND questionnaire at baseline. Additionally, 40 people with MCI completed the DEMAND questionnaire at baseline for sensitivity analysis. Baseline characteristics are summarized in Table 1. On average, participating people with dementia were 83.6 years old and predominantly female (68.0%). The mean MMSE score was 20.5 (SD = 2.3). Participating family caregivers were on average 65.1 years old and predominantly female (69.2%).
Table 1
Baseline characteristics
| Variable | People with dementia (n = 50) | Family caregivers (n = 133) | ||
| mean / number | SD / % | mean / number | SD / % | |
| Age | 83.6 | 6.4 | 65.1 | 12.8 |
| Female | 34 | 68.0% | 92 | 69.2% |
| Education | ||||
| No school-leaving qualification | 3 | 6.0% | 2 | 1.5% |
| Lower secondary school leaving certificate (Volksschulabschluss) | 30 | 60.0% | 29 | 21.8% |
| Lower secondary school leaving certificate (Hauptschulabschluss) | 4 | 8.0% | 28 | 21.1% |
| Secondary school certificate (Mittlere Reife) | 12 | 24.0% | 46 | 34.6% |
| Advanced technical college certificate (Fachhochschulreife) | 0 | 0% | 13 | 9.8% |
| Higher education entrance qualification (A-levels) (Abitur) | 1 | 2.0% | 15 | 11.3% |
| Caregiving time in hours per day | ||||
| Assistance with ADL (n = 108) | 2.8 | 3.3 | ||
| Assistance with IADL (n = 105) | 3.2 | 2.8 | ||
| Supervision (n = 99) | 1.8 | 3.2 | ||
| MMSE | 20.5 | 2.3 | ||
| Diagnosis confirmed by further diagnostic measures | 23 | 46.0% | 83* | 62.4% * |
| Type of dementia | ||||
| Dementia in Alzheimer disease (F00.*) | 10 | 43.5% | 46 | 55.4% |
| Vascular dementia (F01.*) | 0 | 0% | 14 | 16.9% |
| Dementia in other diseases classified elsewhere (F02.*) | 0 | 0% | 3 | 3.6% |
| Unspecified dementia (F03) | 13 | 56.5% | 20 | 24.1% |
ADL, Activities of daily living; IADL, Instrumental activities of daily living; MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment; SD, standard deviations. *Diagnosis of the person with dementia that is cared for by the family caregiver.
The most frequently used services were primary care by a general practitioner (GP) (55.7%), outpatient care (53.6%), and housekeeping assistance (44.3%) (Table 2). The services Caregiver Training Programs for family caregivers, short-term care, and palliative care were used by less than 5.0%. The service nursing home was not used at all as caused by exclusion criteria of the project digiDEM.
Table 2
Utilization of support services
| Support Service | Cases | Used (%) | Not used (%) |
| Outpatient care | 183 | 98 (53.6%) | 85 (46.4%) |
| Acquisition of aids | 183 | 47 (25.7%) | 136 (74.3%) |
| Primary care by a GP | 183 | 102 (55.7%) | 81 (44.3%) |
| Housekeeping assistance | 183 | 81 (44.3%) | 102 (55.7%) |
| Short-term care | 183 | 4 (2.2%) | 179 (97.8%) |
| Palliative care | 183 | 1 (0.5%) | 182 (99.5%) |
| Provision of psychosocial interventions | 183 | 58 (31.7%) | 125 (68.3%) |
| Nursing home | 183 | 0 (0%) | 183 (100%) |
| Adult daycare | 183 | 32 (17.5%) | 151 (82.5%) |
| Respite care | 132 | 10 (7.6%) | 122 (92.4%) |
| Counseling services | 183 | 38 (20.8%) | 145 (79.2%) |
| Caregiver Training Programs for family caregivers | 132 | 4 (3.0%) | 128 (97.0%) |
| Supported living and alternative housing services | 183 | 15 (8.2%) | 168 (91.8%) |
Information concerning the need for services and reasons for non-utilization are presented in Tables 3 and 4.
Table 3
Need for support services (if service was not used)
| Support Service | Cases | Service was unknown (%) | Need of service (%) | No need of service (%) |
| Outpatient care | 85 | 5 (5.9%) | 3 (3.5%) | 77 (90.6%) |
| Acquisition of aids | 136 | 11 (8.1%) | 4 (2.9%) | 121 (89.0%) |
| Primary care by a GP | 81 | 3 (3.7%) | 1 (1.2%) | 77 (95.1%) |
| Housekeeping assistance | 102 | 8 (7.8%) | 8 (7.8%) | 86 (84.3%) |
| Short-term care | 179 | 30 (16.8%) | 3 (1.7%) | 146 (81.6%) |
| Palliative care | 181 | 50 (27.6%) | 0 (0%) | 131 (72.4%) |
| Provision of psychosocial interventions | 125 | 22 (17.6%) | 10 (8.0%) | 93 (74.4%) |
| Nursing home | 183 | 10 (5.5%) | 0 (0%) | 173 (94.5%) |
| Adult daycare | 151 | 32 (21.2%) | 11 (7.3%) | 108 (71.5%) |
| Respite care | 122 | 28 (23.0%) | 2 (1.6%) | 92 (75.4%) |
| Counseling services | 145 | 41 (28.3%) | 5 (3.4%) | 99 (68.3%) |
| Caregiver Training Programs for family caregivers | 128 | 34 (26.6%) | 5 (3.9%) | 89 (69.5%) |
| Supported living and alternative housing services | 168 | 51 (30.4%) | 2 (1.2%) | 115 (68.5%) |
Table 4
Reasons for non-utilization of support services (multiple answers were possible)
| Support Service | Service is not available | Service is not financeable | Too far distance | Fear of public disclosure of dementia | No use because of personal aspects |
| Outpatient care | 2 | 0 | 0 | 0 | 1 |
| Acquisition of aids | 0 | 1 | 1 | 1 | 1 |
| Primary care by a GP | 0 | 0 | 1 | 0 | 0 |
| Housekeeping assistance | 7 | 1 | 0 | 0 | 0 |
| Short-term care | 3 | 0 | 0 | 0 | 0 |
| Palliative care | 0 | 0 | 0 | 0 | 0 |
| Provision of psychosocial interventions | 9 | 1 | 1 | 0 | 0 |
| Nursing home | 0 | 0 | 0 | 0 | 0 |
| Adult daycare | 5 | 0 | 1 | 1 | 6 |
| Respite care | 0 | 0 | 0 | 0 | 2 |
| Counseling services | 5 | 0 | 0 | 0 | 0 |
| Caregiver Training Programs for family caregivers | 4 | 0 | 0 | 0 | 2 |
| Supported living and alternative housing services | 1 | 1 | 0 | 0 | 0 |
Content validity
In order to ensure that the construct ‘need for support service’ is matched by the items investigating the construct, experts were asked to identify all existing and imaginable support services. As aforementioned, 74 different support services could be identified, encompassing the content of the construct ‘need for support service’. The identified services were then compared to scientific literature in order to ensure no important service was missed. The results of the subsequent online survey determined the items necessary to assess the construct ‘need for support service’.
Face validity
Comprehensibility
The mean comprehensibility score in the study sample was 3.6 (SD = 2.3; people with dementia: 3.8, SD = 2.3; family caregivers: 3.5, SD = 2.2) and thereby above the middle value of the scale (5.5), indicating that the questionnaire was fairly comprehensible for both people with dementia and family caregivers. Sensitivity analysis for people with MCI showed a mean comprehensibility score of 2.3 (SD = 1.5, n = 40) proving that the DEMAND is well comprehensible for people with MCI as well.
Readability
The Flesch reading ease score result was 76, which indicates that the written content is fairly easy to read according to the classification of the score [25].
Objectivity
Objectivity was ensured by providing training for the performance of the DEMAND and access to the manual (including the instruction for performing the instrument in an interview situation and for analyzing the results) on the project homepage (http://www.digidem-bayern.de). The manual includes the paper-based and digital performance of the DEMAND using REDCap [27, 28].
DISCUSSION
The specific feature of the DEMAND is that it is directly assessing the utilization of and need for care services instead of being based upon a problem-centered level. Thereby, two important and highly interdependent areas of health outcomes research are combined in one data collection instrument. Moreover, unlike other instruments, the assessment instrument is investigating the reasons for not using a service. By doing this, the DEMAND can provide essential information for improving the care situation of people with dementia and their family caregivers. Another important element is that the DEMAND is considering the needs of both people with dementia and their family caregivers. Therefore, the questionnaire implies elements concerning the care situation, which is relevant for both people with dementia and family caregivers, but also elements specifically targeting the family caregivers. In this respect, the DEMAND was specifically developed for and validated in a population of people with dementia and their family caregivers, ensuring its validity in the respective target population. A further important aspect is that the DEMAND is easy to understand and short in execution so that the application will not be overwhelming. Results of the comprehensibility assessment indicate that the questionnaire was fairly comprehensible for both people with dementia and family caregivers. The Flesch reading ease score of 76 indicates that the questionnaire is fairly easy to read. For comparison, the Camberwell Assessment of Need for the Elderly (CANE) reports a Flesch reading ease score of 71.8 [29]. Processing time does not exceed 15 minutes on average. Finally, due to his practical usability, the DEMAND aims to be applied in both scientific and clinical/consultation contexts.
Relevance of needs assessment
Support services have the potential to develop positive effects on both people with dementia and family caregivers [9]. However, international literature shows that utilization rates are low despite there is often a range of offered care services [30–32]. In this respect, low utilization rates can be a hint of a mismatch between the offered services and the demanded services of the people with dementia and their family caregivers [31]. Moreover, studies discussed a lack of knowledge about services themselves, their availability, and a lack of orientation in the complex systems as main reasons for non-utilization [31, 33, 34]. The DEMAND questionnaire is designed to display changes in the utilization of and need for support services and can provide important information when applied in longitudinal settings.
In a systematic review, Schmid et al. identified 17 needs assessment instruments. The instruments varied highly in several domains such as level of assessment, target group, validation measures and sample, duration, and application [10]. Novais et al. [35] included 70 studies in their review concerning the identification of needs of informal caregivers. However, not in all the studies, standardized research instruments were used. Mansfield et al. [36] could identify 4 studies in their review about the quality of needs assessment measures. In a recent review, Kipfer et al. [37] included 18 articles that reported psychometric measures and results for needs assessment instruments for informal caregivers.
Level of assessment
Unlike many existing assessment instruments [10], the DEMAND is directly assessing the utilization of and need for care services, avoiding the problems of concluding needs indirectly from a problem- or symptom-centered level.
By assessing needs on the problem- or symptom-centered level, services may not meet the needs sufficiently compared to an assessment of needs based upon the direct addressing of services [38, 39]. This may result from the fact, that it often remains unclear, which particular aspect of a problem is meant, and which specific intervention should be applied in order to solve this (aspect of the) problem [10].
In order to get a deeper understanding of the needs of family caregivers and a possible gap between offered and used services, the DEMAND is moreover investigating the reasons for not using a service. In this respect, the DEMAND is not only asking, if there is a need for a service but, inter alia, also if the service is existent and if there is knowledge about the service. Thus, besides the need for specific services, even barriers to resource use can be identified.
Target group
The DEMAND questionnaire is conceptualized for interviewing people with dementia and/or their family caregivers, as felt and expressed needs affect the entire care situation. However, the instrument also includes services uniquely relevant for informal caregivers.
In this respect, some of the existing instruments predominantly or only deal with the needs of people with dementia without referring to family caregivers as well [10, 35]. Yet, the needs and care situation of the people with dementia is strongly interdependent with the situation of the family caregivers [9]. Despite focusing on the needs of people with dementia, the CANE [29], the Johns Hopkins Dementia Care Needs Assessment (JHDCNA) [40], and the Care Needs Assessment Pack for Dementia (CarenapD) [41] assess the specific needs of family caregivers by several questions as well. The Carers’ Needs Assessment for Dementia (CNA-D) [42] only refers to the needs of family caregivers, and the Partnering for Better Health - Living with Chronic Illness: Dementia (PBH-LCI:D) [43] assesses the needs of family caregivers of people with dementia only indirectly.
Sample for validation
Both instruments dealing with the needs of people with dementia and instruments specifically addressing the needs of informal caregivers, often lack sufficient validation, either in general or for the specific population of people with dementia and their family caregivers [10, 35–37]. Therefore, the DEMAND was specifically developed with experts from the field of dementia and validated in a population of people with dementia and their family caregivers.
There are a couple of assessment instruments already addressing the needs of people with dementia and their family caregivers [10, 35–37]. However, some of the instruments used in the context of dementia are not specifically developed for people with dementia or their family caregivers [10]. Despite being widely used in the context of dementia the CANE was not developed specifically for people with dementia but older adults in general. Nonetheless, people with dementia were included in the validation sample [29]. The CarenapD [41] and the CNA-D [42] are instruments, developed specifically for people with dementia respectively their family caregivers.
Duration
Dementia family caregivers are at an increased risk for experiencing a high caregiver burden [4, 44]. Needs assessment measures should take the burden and time consumption of care into account. Therefore, the DEMAND needed to be easy to understand and short in execution so that the application is not overwhelming and that the instrument can be applied in different contexts. In this respect, the processing time of the DEMAND does not exceed 15 minutes on average and is therefore feasible in several settings without overwhelming participants.
Some of the existing instruments are time-consuming and might affect the attention of the interviewed people. According to Reynolds, the CANE should be feasible within 30 minutes [29]. Therefore, Stein et al. recommend the development of a shorter version of the CANE [45]. The application time of the CarenapD is about 90 minutes [10]. In practical application, the duration for completing the CNA-D is about 50 minutes due to its complex structure [42]. For most of the other existing instruments, duration time ranges between 10 and 30 minutes [10].
Application
Due to his practical usability, the DEMAND aims to be included in both scientific and clinical/consultation contexts.
Many other existing instruments are either used for clinical or research use [10, 35, 36]. The CANE can be applied in both clinical and research contexts [29]. The CarenapD was solely developed for clinical use [41]. The CNA-D is an instrument specifically and solely designed for research purposes [42].
Limitations
The data basis for the development of the DEMAND is predominantly based upon people living in Bavaria. Therefore, the external validity is limited, as Bavarian-specific care situations cannot be ruled out. Moreover, the data for validation were collected within the project digiDEM. digiDEM reflects the population of the southern part of Germany so that the results may be difficult to transfer to other health care settings and jurisdictions. There were no people with dementia participating in neither the focus group nor the online survey. Thus, in the development process, the perspective of people with dementia themselves was only represented by patient representatives and family caregivers as their proxy. In order to develop a brief instrument, the 13 highest-rated support services of both informal caregivers and professional experts were included. However, through the exclusion of further support services, comprehensive information about the entire service landscape cannot be obtained, which might lead to some imbalances.
Conclusion
The care of people with dementia is a time and resource-consuming process that can result in a high caregiver burden of family caregivers. External support services are important measures for effectively reducing caregiver burden and enabling people with dementia to remain in their home environment as long as possible. In order to do so, the identification of the utilization of and need for services of the people with dementia and their family caregivers is crucial. The DEMAND can make an important contribution by providing data that are underlying for effective health care planning by health decision-makers. By using the DEMAND, supply gaps can be identified and transformed into a specific regional health care policy. In addition, the DEMAND can foster health outcomes research by being implemented in research projects.
ACKNOWLEDGMENTS
The project ‘Digital Dementia Registry Bavaria –digiDEM Bayern’ is funded by the Bavarian State Ministry of Health and Care as part of the funding initiative ‘BAYERN DIGITAL II’ (grant number: G42d-G8300-2017/1606-83). The funder was not involved in the study design, in the collection, analysis, and interpretation of data, in the writing of the report, or in the decision to submit the article for publication. The authors are grateful to the participating experts and study participants of digiDEM Bayern. The present work was performed by Nikolas Dietzel in (partial) fulfillment of the requirements for obtaining the degree “Dr. rer. biol. hum.” at the Medical Faculty of the Friedrich-Alexander-Universität Erlangen-Nürnberg.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/22-0363r2).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-220363.
REFERENCES
[1] | Wimo A , Jönsson L , Bond J , Prince M , Winblad B ((2013) ) The worldwide economic impact of dementia 2010. Alzheimers Dement 9: , 1–11.e13. |
[2] | World Health Organization (2012) Dementia. A public health priority. |
[3] | Wimo A , Gauthier S , Prince M (2018) Global estimates of informal care. Alzheimer’s Disease International (ADI), London. |
[4] | Brodaty H , Donkin M ((2009) ) Family caregivers of people with dementia. Dialogues Clin Neurosci 11: , 217–228. |
[5] | McCabe M , You E , Tatangelo G ((2016) ) Hearing their voice: A systematic review of dementia family caregivers’ needs. Gerontologist 56: , 70–88. |
[6] | Karg N , Graessel E , Randzio O , Pendergrass A ((2018) ) Dementia as a predictor of care-related quality of life in informal caregivers: A cross-sectional study to investigate differences in health-related outcomes between dementia and non-dementia caregivers. BMC Geriatr 18: , 189. |
[7] | Bangerter LR , Griffin JM , Zarit SH , Havyer R ((2019) ) Measuring the needs of family caregivers of people with dementia: An assessment of current methodological strategies and key recommendations. J Appl Gerontol 38: , 1304–1318. |
[8] | Stirling C , Andrews S , Croft T , Vickers J , Turner P , Robinson A ((2010) ) Measuring dementia carers’ unmet need for services–an exploratory mixed method study. BMC Health Serv Res 10: , 122. |
[9] | Karrer L , Dietzel N , Wolff F , Kratzer A , Hess M , Gräßel E , Kolominsky-Rabas P ((2020) ) Use of outpatient care services by people with dementia: Results of the Bavarian Dementia Survey (BayDem). Gesundheitswesen 82: , 40–49. |
[10] | Schmid R , Eschen A , Rüegger-Frey B , Martin M ((2012) ) Instruments for comprehensive needs assessment in individuals with cognitive complaints, mild cognitive impairment or dementia: A systematic review. Int J Geriatr Psychiatry 27: , 329–341. |
[11] | Folstein MF , Folstein SE , McHugh PR ((1975) ) “Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: , 189–198. |
[12] | Nasreddine ZS , Phillips NA , Bedirian V , Charbonneau S , Whitehead V , Collin I , Cummings JL , Chertkow H ((2005) ) The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53: , 695–699. |
[13] | Dietzel N , Kürten L , Karrer L , Reichold M , Köhler L , Nagel A , Chmelirsch C , Seebahn K , Hladik M , Meuer S , Kirchner A , Holm K , Selau M , Wendel M , Trinkwalter J , Prokosch HU , Graessel E , Kolominsky-Rabas PL ((2021) ) Digital Dementia Registry Bavaria-digiDEM Bayern: Study protocol for a multicentre, prospective, longitudinal register study. BMJ Open 11: , e043473. |
[14] | Karrer L , Zhang S , Kühlein T , Kolominsky-Rabas PL ((2021) ) Exploring physicians and patients’ perspectives for current interventions on thyroid nodules using a MCDA method. Cost Eff Resour Alloc 19: , 26. |
[15] | Meuser M , Nagel U (2009) Das Experteninterview — konzeptionelle Grundlagen und methodische Anlage. In Methoden der vergleichenden Politik- und Sozialwissenschaft: Neue Entwicklungen und Anwendungen, Pickel S, Pickel G, Lauth H-J, Jahn D, eds. VS Verlag für Sozial- wissenschaften, Wiesbaden, pp. 465-479. |
[16] | Wassermann S (2015) Das qualitative Experteninterview. In Methoden der Experten- und Stakeholdereinbindung in der sozialwissenschaftlichen Forschung, Niederberger M, Wassermann S, eds. Springer VS, Wiesbaden, pp. 51-69. |
[17] | Döringer S ((2021) ) ‘The problem-centred expert interview’. Combining qualitative interviewing approaches for investigating implicit expert knowledge. Int J Soc Res Methodol 24: , 265–278. |
[18] | Ericsson K , Krampe R , Tesch-Roemer C ((1993) ) The role of deliberate practice in the acquisition of expert performance. Psychol Rev 100: , 363–406. |
[19] | Niederberger M , Mack B , Renn O (2012) Fokusgruppen in der empirischen Sozialwissenschaft: Von derKonzeption bis zur Auswertung. Springer VS, Wiesbaden. |
[20] | Krueger RA , Casey MA ((2015) ) Focus groups: A practical guide for applied research, SAGE Publications, Inc. |
[21] | Mayring P , Fenzl T (2019) Qualitative Inhaltsanalyse. In Handbuch Methoden der empirischen Sozialforschung, Baur N, Blasius J, eds. Springer Fachmedien Wiesbaden, Wiesbaden, pp. 633-648. |
[22] | VERBI Software (2017) Berlin, Germany.. |
[23] | Lienert GA , Raatz U (1998) Testaufbau und Testanalyse, Beltz, PsychologieVerlagsUnion, Weinheim. |
[24] | Inui Y , Ito K , Kato T ((2017) ) Longer-term investigation of the value of 18F-FDG-PET and magnetic resonance imaging for predicting the conversion of mild cognitive impairment to Alzheimer’s disease: A multicenter study. J Alzheimers Dis 60: , 877–887. |
[25] | Flesch R ((1948) ) A new readability yardstick. J Appl Psychol 32: , 221–233. |
[26] | ICHOM (International Consortium for Health Outcomes Measurement) (2017) Dementia. Data Collection Reference Guide (03.04.2017). |
[27] | Harris PA , Taylor R , Minor BL , Elliott V , Fernandez M , O’Neal L , McLeod L , Delacqua G , Delacqua F , Kirby J , Duda SN ((2019) ) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95: , 103208. |
[28] | Harris PA , Taylor R , Thielke R , Payne J , Gonzalez N , Conde JG ((2009) ) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: , 377–381. |
[29] | Reynolds T , Thornicroft G , Abas M , Woods B , Hoe J , Leese M , Orrell M ((2000) ) Camberwell Assessment of Need for the Elderly (CANE). Development, validity and reliability. Br J Psychiatry 176: , 444–452. |
[30] | Lethin C , Leino-Kilpi H , Roe B , Soto MM , Saks K , Stephan A , Zwakhalen S , Zabalegui A , Karlsson S ((2016) ) Formal support for informal caregivers to older persons with dementia through the course of the disease: An exploratory, cross-sectional study. BMC Geriatr 16: , 32. |
[31] | Phillipson L , Jones SC , Magee C ((2014) ) A review of the factors associated with the non-use of respite services by carers of people with dementia: Implications for policy and practice. Health Soc Care Community 22: , 1–12. |
[32] | Feldman SJ , Solway E , Kirch M , Malani P , Singer D , Roberts JS ((2021) ) Correlates of formal support service use among dementia caregivers. J Gerontol Soc Work 64: , 135–150. |
[33] | Brodaty H , Thomson C , Thompson C , Fine M ((2005) ) Why caregivers of people with dementia and memory loss don’t use services. Int J Geriatr Psychiatry 20: , 537–546. |
[34] | Stephan A , Bieber A , Hopper L , Joyce R , Irving K , Zanetti O , Portolani E , Kerpershoek L , Verhey F , de Vugt M , Wolfs C , Eriksen S , Røsvik J , Marques MJ , Goncalves-Pereira M , Sjölund BM , Jelley H , Woods B , Meyer G ((2018) ) Barriers and facilitators to the access to and use of formal dementia care: Findings of a focus group study with people with dementia, informal carers and health and social care professionals in eight European countries. BMC Geriatr 18: , 131. |
[35] | Novais T , Dauphinot V , Krolak-Salmon P , Mouchoux C ((2017) ) How to explore the needs ofinformal caregivers of individuals with cognitive impairment in Alzheimer’s disease or related diseases? A systematic review of quantitative and qualitative studies. BMC Geriatr 17: , 86. |
[36] | Mansfield E , Boyes AW , Bryant J , Sanson-Fisher R ((2017) ) Quantifying the unmet needs of caregivers of people with dementia: A critical review of the quality of measures. Int J Geriatr Psychiatry 32: , 274–287. |
[37] | Kipfer S , Pihet S ((2019) ) Reliability, validity and relevance of needs assessment instruments for informal dementia caregivers: A psychometric systematic review. JBI Database System Rev Implement Rep 18: , 704–742. |
[38] | Cummings SM , Kropf NP ((2009) ) Formal and informal support for older adults with severe mental illness. Aging Ment Health 13: , 619–627. |
[39] | Orrell M , Hancock G , Hoe J , Woods B , Livingston G , Challis D ((2007) ) A cluster randomised controlled trial to reduce the unmet needs of people with dementia living in residential care. Int J Geriatr Psychiatry 22: , 1127–1134. |
[40] | Hughes TB , Black BS , Albert M , Gitlin LN , Johnson DM , Lyketsos CG , Samus QM ((2014) ) Correlates of objective and subjective measures of caregiver burden among dementia caregivers: Influence of unmet patient and caregiver dementia-related care needs. Int Psychogeriatr 26: , 1875–1883. |
[41] | McWalter G , Toner H , McWalter A , Eastwood J , Marshall M , Turvey T ((1998) ) A community needs assessment: The care needs assessment pack for dementia (CarenapD)–its development, reliability and validity. Int J Geriatr Psychiatry 13: , 16–22. |
[42] | Wancata J , Krautgartner M , Berner J , Alexandrowicz R , Unger A , Kaiser G , Marquart B , Weiss M ((2005) ) The Carers’ Needs Assessment for Dementia (CNA-D): Development, validity and reliability. Int Psychogeriatr 17: , 393–406. |
[43] | Sadak T , Korpak A , Borson S ((2015) ) Measuring caregiver activation for health care: Validation of PBH-LCI:D. Geriatr Nurs 36: , 284–292. |
[44] | Graessel E , Behrndt EM (2016) Belastungen und Entlastungsangebote für pflegende Angehorige. In Pflege-Report 2016. Schwerpunkt: Die Pflegenden im Fokus, Jacobs K, Kuhlmey A, Greß S, Klauber J, Schwinger A, eds. Schattauer, Stuttgart, pp. 169-189. |
[45] | Stein J , Luppa M , König HH , Riedel-Heller SG ((2015) ) The German version of the Camberwell Assessment of Need for the Elderly (CANE): Evaluation of content validity and adaptation to the German-speaking context. Int Psychogeriatr 27: , 1919–1926. |




