Informal Caregivers’ Attitude Toward Dementia: The Impact of Dementia Knowledge, Confidence in Dementia Care, and the Behavioral and Psychological Symptoms of the Person with Dementia. A Cross-Sectional Study
Abstract
Background:
Dementia is rapidly increasing worldwide due to demographic aging. More than two-thirds of patients are cared by family members. The quality of care depends on the caregivers’ attitude toward dementia influencing patient care decisions.
Objective:
The aim of this study is to examine the factors that influence the caregivers’ attitude and whether there is an association between participation in a psycho-educational program and attitude.
Methods:
We performed a cross-sectional study using a structured closed-ended questionnaire to retrieve socio-demographic information from caregivers and the persons with dementia (N = 86). The study included validated scales such as the Dementia Attitude Scale, the Dementia Knowledge Assessment Tool 2, the Positive Aspects of Caregiving, the Zarit Burden Interview, the Confidence in Dementia Scale, and Spielberger’s State-Trait Anxiety Inventory, as well as a neuropsychological battery to assess the condition of people with dementia.
Results:
Our final model explains 55.6% of the total variance and shows a significant correlation of five factors with attitude toward dementia: confidence, behavioral and psychological symptoms of dementia, anxiety as a trait, positive aspects of caregiving, and dementia knowledge. The caregivers who participated in a psycho-educational program showed a significantly more positive attitude toward dementia, better dementia knowledge, higher confidence in dementia care, and lower anxiety as a state.
Conclusion:
The strong correlation of attitude and knowledge, as well as confidence in dementia care, supports the tripartite model of attitude, which hypothesizes the interrelation of affect, cognition, and behavior.
INTRODUCTION
The majority of people with dementia (PwD) depend largely on the care of a family member, and therefore dementia affects not only the PwD but also the informal primary caregiver [1]. The family caregiver often takes on the responsibility from an early stage of the disease, where only mild memory impairment is noted, to the later stages, when the person with dementia needs help with all activities of daily living, such as bathing, doing household chores, and cooking, and thus requires full-time care [2]. Although there are reports of carers who find caring satisfying and meaningful [3], it has been found that providing care over a prolonged time has a significant impact on the physical and mental health status [4], as well as on social isolation and the financial situation [5]. Whether caring for a relative is perceived as a burden [6] or enriching [7] may depend on numerous factors, including characteristics both of the carer (age, gender, health status, dementia knowledge, confidence in caring) and PwD (severity of dementia, behavioral and psychological symptoms of dementia (BPSD), functionality in daily living), as well as the provided support, by means of time spent while caring or free time. Since caregiving is a process that has to be adapted continuously depending on the stage of the disease, the relationship between carer and care recipient is changing continuously.
Although there is abundant literature on the determinants of caregiver burden in dementia, little is known about the factors that can influence the caregiver’s attitude toward dementia, either positively or negatively [8]. In psychology, attitude refers to the willingness of an individual, based on experience, to react in a certain way to a person, a situation, or an idea, which is reflected in the cognitive (assumptions and beliefs), affective (feelings and emotions), and behavioral (behavior) area [9]. Each of these components carries a valence: pleasurable to unpleasurable affect, favorable to unfavorable cognition, and supportive to hostile behavior [10]. A number of studies based on the three-component model of Rosenberg and Hovland [9] have concluded that affect, cognition, and behavior are interrelated, although still distinguishable from each other [11]. For a long time, social psychologists have been interested in understanding attitudes, as they were presumed to have a strong influence on behaviors, decisions, and judgments. However, the link between attitude and behavior remains unclarified [12, 13]. Attitudes toward people with mental disorders in general and especially toward PwD provoke emotional reactions that play a key factor regarding the social impact and the risks of stigmatization and discrimination [14, 15]. However, little is known about factors that contribute to the positive attitude of informal carers toward dementia or PwD.
The research regarding attitudes toward PwD typically focused on health professionals [16–19], especially nurses [20, 21] or general practitioners [22], and, furthermore, college students [23] and the general public [24–26]. A couple of studies examined the attitude of family caregivers toward dementia [8, 27–30], with all of them using not only different instruments but also different dimensions of attitudes [31]. However, only few studies [28] used a validated questionnaire in home care staff in the UK–the Approaches to Dementia Questionnaire (ADQ), which measures hopefulness and person-centered approaches on a 19-item Likert scale [32, 33]. Other studies used either self-developed questionnaires [30] or the Community Attitudes toward Mentally Ill Scale (CAMI) compromising four dimensions of attitudes, which was initially designed for schizophrenia [8, 34], or the version for caregivers “Level to Expressed Emotion (LEE) Scale” [27, 35] with one subscale measuring negative attitudes, but were not validated for measuring attitudes toward dementia [27]. Overall, although numerous self-report instruments have been developed to measure ageism and attitudes toward disabilities, only a few instruments measuring attitude toward dementia have been validated for family carers or at least for the general public. The Dementia Attitude Scale (DAS) [36] is based upon the tripartite model of attitude [9]. With this instrument, the attitudes of the general population and all individuals involved in the care and treatment of those affected by dementia, such as relatives, counselors, nursing staff, and doctors, can be recorded [37].
Research on family carers’ attitude toward dementia did not only use different, mostly not validated instruments to assess the attitude but also examined different variables, making it difficult to draw any conclusions on the factors influencing the caregivers’ attitude. For example, the relations among social factors, dementia knowledge, attitudes and beliefs have not been investigated intensively [38]. Also, studies considering a broader range of attitudes or social factors focused only on general practitioners, not on the general public or informal carers [39]. Regarding informal caregivers, factors that influence the attitude, amongst others, seem to be the feeling of burden [8, 29], decisions regarding medication [40] or nursing home placement [41], knowledge, approaches of caregivers regarding dementia, empathy, quality of life, caregivers’ sense of competence [28], and factors regarding the PwD such as agitation and severity of dementia [27], challenging behaviors or short-stay use, and length of time caregivers and PwD have lived together [30].
The burden of caregiving reported by family members, especially those who have been caring for many years, often includes unpleasant perceptions such as shame, embarrassment, guilt, and self-deception [42], in addition to the emotional, psychological, physical, and financial effects [43] and can be measured with the Zarit burden interview [44, 45]. At the same time, some caregivers experience satisfaction in caregiving [46]. The positive aspects of caregiving (PAC) are usually defined as the rewards and satisfaction that result from the relationship between those involved in caregiving [47] and are mainly related to age, relationship with the patient, duration of care, and living with the patient and other family members. The older the patient, the more likely the caregiver is to develop positive aspects of the patient’s daily care.
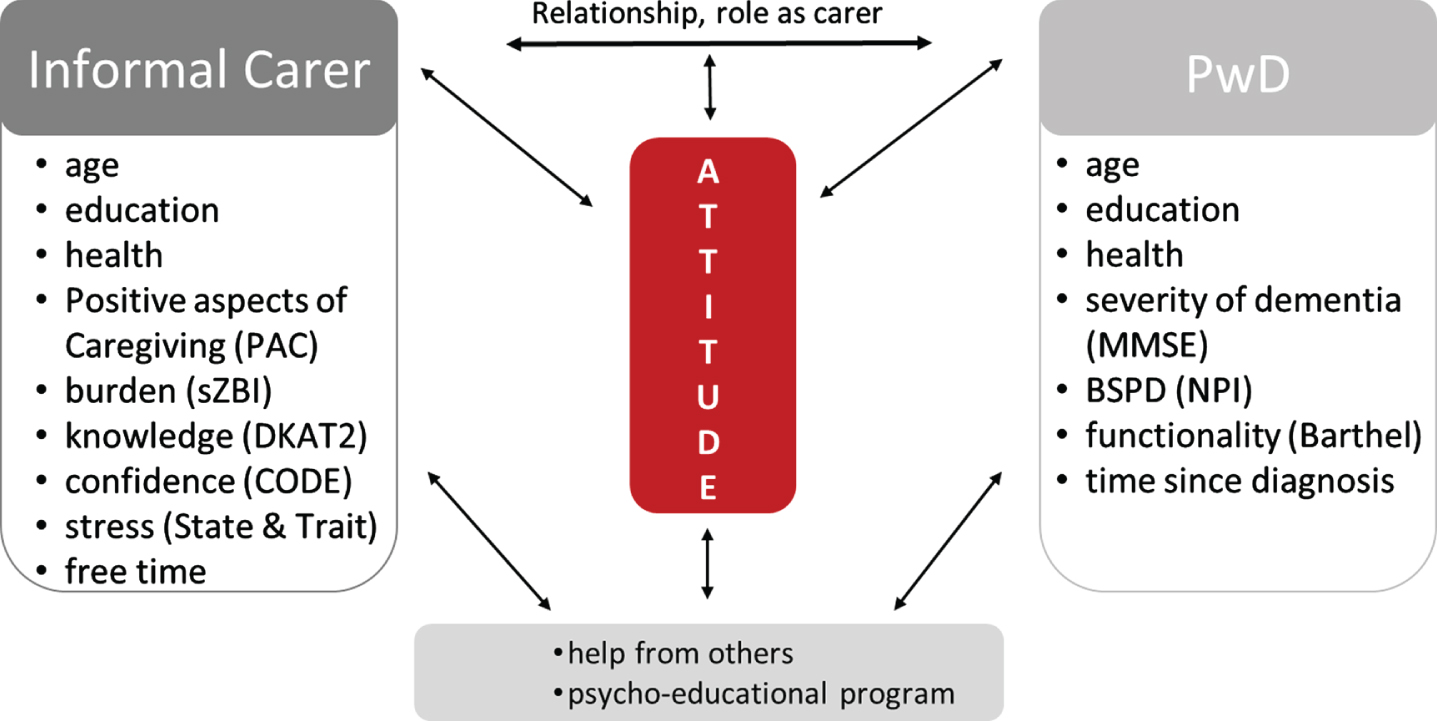
Whether caregiving is more likely to be perceived as a burden or something positive depends, besides others, on stress parameters to which the caregiver is exposed through caregiving or in general. Knowledge about dementia and how to deal with PwD can help develop confidence in dealing with people with dementia [48, 49], which in turn has a positive effect on caregiving burden and anxiety [50]. Because of the tripartite model of attitude, which is reflected in the cognitive, affective, and behavioral areas, possible factors influencing caregivers’ attitude could include, aside from demographic factors, patient-carer relationship, free time, the network of caregivers, stress, previous experience with dementia, the burden or positive aspects of caregiving, knowledge about dementia, the confidence in caring, and the attending of supportive programs for carers as well as demographic factors of PwD, the severity of dementia, the ability of independence in daily living, and the BPSD as depicted in Fig. 1. However, to our knowledge, no study has examined all these factors together, also taking into consideration dementia knowledge and confidence in caregiving. Therefore, our study aims to examine which of those factors mentioned above impact informal carers’ attitude toward the PwD and, as a secondary aim, whether there is an association between participation in a psycho-educational program and attitude.
MATERIALS AND METHODS
Study design
This was a cross-sectional, descriptive study design. The study was performed according to the carer’s ethical standards outlined in the declaration of Helsinki, which is relevant to the national and institutional committees on human experimentation. Informal carers participated voluntarily in the study. They were informed about the aim of the study and subsequently provided their written consent for participation. The General Data Protection Regulation (GDPR) in a research context [51], and the Greek Law of Data Protection were respected through the confidentiality and anonymity of the data. The study was approved by the ethics committee of the Greek Association of Alzheimer’s Disease and Related Disorders (56/04-03-2020-A).
Participants
Data for the convenience sample were collected from the Family Unit of the St. Helen Day Care Center of the Greek Association of Alzheimer’s Disease and Related Disorders (GAADRD) and at a private neurological practice in Thessaloniki from July to October 2020 through semi-structured interviews by using an additional set of questionnaires. The Family Unit provides education and support for caregivers in the form of weekly group sessions, each lasting 60 min. The informal carers learn to manage their burden and receive support in dealing with the behavioral disturbances of the PwD. The inclusion criteria for the carers’ participation were as follows: a) age ≥18 years, b) ability to communicate in Greek, c) providing written informed consent, d) an informal carer of a PwD with Mini-Mental State Examination (MMSE) ≤26. All participants were informed about the aim of the study and gave their consent to participate in the face-to-face interview. The questionnaire was completed by the researcher (BT) during the interview with the caregiver and lasted from 30 min to one hour.
Ninety-four informal caregivers fulfilled the inclusion criteria and completed the questionnaires, also answering the questions regarding the PwD, while six of them could not provide the MMSE of the PwD, and two had some missing data. Therefore, the complete data from N = 86 participants were included in the study.
Data collection
Participant demographics
A structured closed-ended questionnaire was used to retrieve the socio-demographic and household information of the caregiver and the PwD. The collected socio-demographic variables 1) from the carers were: age (chronological and subjective), gender, education, marital status, relationship with the patient, occupation, support from others, time for care, free time, attending a psycho-educational program for informal carers, previous experience with dementia and 2) from the PwD: age, sex, education, marital status, patient relationship, occupation, date of diagnosis, MMSE as depicted in Fig. 1.
Fig. 1
Factors with a possible impact on the carers’ attitude toward dementia. CODE, Confidence in Dementia Care; DKAT2, Dementia Knowledge Assessment Tool 2; MMSE, Mini-Mental Status Examination; NPI, Neuropsychiatric Inventory; PAC, Positive Aspects of Caregiving; sZBI, short Zarit Burden Interview; State and Trait, State-Trait Anxiety Inventory.
Questions about the fear of having dementia in the future, the caregiver’s support for care, and some questions regarding the caregiver’s and PwD’s health, including the number of medications taken, were also asked.
Questionnaires
The questionnaires included the Greek validated versions of the Positive Aspects of Caregiving (PAC) Scale [47], the short form of the Zarit Burden Interview (sZBI) [44, 52], the Dementia Attitude Scale (DAS) [36, 53], the Dementia Knowledge Assessment Tool 2 (DKAT2) [36, 54], the Confidence in Dementia Confidence Scale (CODE) [36, 55], and Spielberger State-Trait Anxiety Inventory (STAI) [56]. The questionnaires also included tools relating to the PwD such as the Barthel Index scale [57, 58] and the Neuropsychiatric Assessment Scale (NPI) [59, 60]. In addition, the MMSE [61] data were provided by the neurologist prior to the interview.
The Dementia Attitude Scale (DAS)
The instrument consists of 20 items on a seven-point Likert scale with responses ranging from “strongly disagree” to “strongly agree” and reflects the affective, behavioral, and cognitive components of the attitude toward dementia [53]. The total scores achievable for this scale range from 20 to 140, with a more positive attitude reflected by a higher score. Six items were reverse-scored (2, 6, 8, 9, 16, 17). Two sub-domains consist of “dementia knowledge” (items 3, 7, 10, 11, 12, 14, 15, 18, 19, and 20) and “social comfort” (items 1, 2, 4, 5, 6, 8, 9, 13, 16, and 17). The DAS was validated with college students and direct care workers but not with informal caregivers. The Greek version shows satisfactory psychometric properties [36].
Dementia Knowledge Assessment Tool 2 (DKAT2)
The DKAT2 [54] has 21 statements addressing different areas of dementia knowledge, encompassing features of Alzheimer’s disease and vascular dementia, behavioral, emotional, physiological, functional, and sensory symptoms of dementias, as well as symptoms that are not necessarily associated with dementia. There are three possible answers for each statement: “yes”, “no” and “don’t know.” Answers are scored as 1 if correct and 0 if incorrect or “don’t know”. Thirteen items are correct statements, and eight items are incorrect (5, 6, 7, 8, 12, 16, 18, 20), which were reverse-scored. The higher the final score, the higher the knowledge about dementia. The DKAT2 was translated into Greek, validated in college students, and showed good psychometric properties [36].
Confidence in Dementia (CODE)
This nine-item self-report questionnaire is used to measure confidence in hospital staff working with people with dementia [55] and is scored on a five-point Likert scale with anchored ratings of “not able”, “somewhat able”, and “very able”. The total scores achievable for this scale range from 9 to 45, with a higher score representing better confidence in caring for people with dementia. Cut-off points within the scale are as follows: 0–18 not confident, 19–35 somewhat confident, 36–45 very confident. The Greek version shows satisfactory psychometric properties [36].
Positive Aspects of Caregiving (PAC)
The Greek version of the PAC scale [47] includes 11 items that reflect several positive aspects that may emerge during caregiving. Each item begins with the words “caregiving made me feel . . . ” followed by one of the 11 items. This self-report five-point Likert scale is scored from 1 (disagree a lot) to 5 (agree a lot) (range 11–55) so that higher scores mean a more positive perception of the caregiving experience. The Greek version showed very satisfactory internal reliability.
Zarit Burden Interview (ZBI)
The ZBI measures caregivers’ perceived burden, which changes over time due to the dementia stages and progression. Most researchers use the full revised version of 22 items, scored from 0 to 4 (0 = never, 4 = nearly always), whereas the higher the total score, the higher the level of perceived burden. The Greek version, which is based on the full version, shows satisfactory psychometric properties [52]. Bedard et al. (2001) developed a short form of the Zarit Burden Interview with only 12 items, which did not affect the properties of the ZBI [44]. These 12 items (2, 3, 5, 6, 9, 10, 11, 12, 17, 19, 20, 21), which cover all the dimensions (personal strain, role strain, deprived relations, and management of care), were included in the current study.
State-Trait Anxiety Inventory (STAI): A 40-item questionnaire
The STAI measures the state and trait of anxiety in adults [56]. State anxiety (S-Anxiety) refers to the subjective and transitory feelings of tension, nervousness, worry and may be characterized by activation of the autonomous nervous system at a given moment. Trait anxiety (T-Anxiety) refers to relatively stable individual differences in anxiety as a personality trait and indicates the tendency to perceive and respond to stressful situations [56]. The S-Anxiety scale consists of 20 statements that evaluate how the respondent feels “right now, at this moment” on a four-point Likert scale, with responses ranging from 1 (not at all) to 4 (very much so). In contrast, the T-Anxiety scale consists of 20 statements that evaluate how the respondent feels “generally” on a four-point Likert scale with responses ranging from 1 (almost never) to 4 (almost always). Thus, a rating from 4 indicates the presence of high levels of anxiety for ten S-Anxiety items (3, 4, 6, 7, 9, 12, 13, 14, 17, and 18) and eleven T-Anxiety items (22, 24, 25, 28, 29, 31, 32, 35, 37, 38, 40), while the other items have a reverse score. Scores can vary from a minimum of 20 to a maximum of 80. The properties of the Greek version are similar to those reported in the international literature [56].
Barthel Index
The Barthel Index is a valid and reliable scale for measuring the degree of independence of the patients with dementia concerning daily activities and is composed of 10 subitems with varying weights. Two items with regard to grooming and bathing are evaluated on a two-score scale (0 and 5 points), six items regarding feeding, toilet use, stairs, dressing, bowel control, and bladder control are evaluated on a three-score scale (0, 5, and 10 points), and two items regarding transfers from bed to chair and mobility are evaluated on a four-score scale (0, 5, 10, and 15 points). The Barthel Index is scored in steps of 5 points to a maximum total score of 100, with higher ratings reflecting greater functional independence [57]. The Greek version has high internal consistency and reliability [58].
The Neuropsychiatric Inventory (NPI)
The NPI is administered to dementia caregivers in order to identify whether the patient has one of the following behavioral disturbances: delusions, hallucinations, agitation/aggression, dysphoria, anxiety, euphoria, apathy, disinhibition, irritability/lability, aberrant motor activity, night-time behavioral disturbances, and appetite and eating abnormalities [62]. The frequency of the symptoms is rated on a four-point scale, and the severity of the symptoms is rated on a three-point scale. Scores (frequency x severity) range between 0 and 144, with higher scores indicating abnormal behavioral symptoms [59]. The Greek version shows high internal consistency reliability as well as a positive concurrent validity [60].
Data analysis
The Statistical Package for Social Sciences (SPSS), version 26 for Windows, was used for all descriptive and inferential statistical analyses. The sample size calculation was based on the main research question (multivariable regression) for the main prognostic factors: attitude, positive aspects of care, burden, knowledge, self-confidence, stress, MMSE, ADL, and NPI and was conducted using G * Power (version 3.1.9.7) [63]. The alpha level was set to α<0.05 with a power of 0.8. A total of N = 84 participants were calculated to identify a moderate outcome size (f2= 0.2) [64].
In order to describe the characteristics of the study, mean scores and standard deviations were calculated. The bivariate correlations between the dependent variable of “attitude” and the study variables were calculated using Pearson’s r. Variables that showed a significant correlation (p < 0.01) were included in the multiple regression analysis. The stepwise regression selection method was used to obtain the final multiple regression model. Two blocks of independent variables were used: one with variables of the PwD (Barthel, NPI, MMSE) and one with caregivers’ variables (gender, years of caregiving, burden, positive aspects of caregiving, anxiety, knowledge, confidence, education, hours free time, numbers of medication, fear of dementia). Missing data were handled by conducting the analyses on complete cases. As this is an exploratory study, results were not adjusted for inflation of the type I error rate due to multiple testing. Any positive finding from this exploratory study needs to be confirmed in a pre-specified approach [65].
Independent t-tests were used to analyze the differences between the participants who participated in the psycho-educational program and those never involved in such a program. The Kolmogorov-Smirnov test was used to confirm the normal distribution. The analysis of covariance (ANCOVA) was performed to control for possible confounders. The DAS, the dependent variable, appeared to be normally distributed. Cronbach’s α was calculated to estimate the internal consistency ability of all scales used.
RESULTS
Participants characteristics
The complete data from N = 86 participants were used for data analysis in the current study. Core characteristics of the carers are reported in Table 1, those of the PwD in Table 2. Summarizing the main characteristics, the mean age of the carers was 55 years, the majority were women (n = 67, 77.9%), with 7–16 years of education (n = 66, 76.8%), married (n = 59, 68.6%), being main carers (n = 61, 71.9%), children (n = 59, 68.6%), and approximately half of them were participating in a program at the Alzheimer’s Day Care Center (n = 46, 53.5%), while 39 (45.3%) feared to suffer from dementia in the future. Almost 63% (n = 54) lived together with the PwD (although not always in the same flat but always in the same complex), cared approximately 50 hours per week, with 72% (n = 62) having somebody who helped with the care, while 26% (n = 22) had previous experience with a PwD. The carers took in average one medicine.
Table 1
Characteristics of informal carers
| Special Program (n = 46) | No special program (n = 40) | |||||
| Male n (%) | Female n (%) | Male n (%) | Female n (%) | Total N (%) | ||
| Age (mean, SD) | 55.09 (11.21) | 54.58 (12.75) | 54.85 (11.88) | |||
| Age group | 26–35 | 0 (0.0) | 1 (1.2) | 1 (1.2) | 2 (2.3) | 4 (4.7) |
| 36–45 | 2 (2.3) | 6 (7.0) | 2 (2.3) | 3 (3.5) | 13 (15.1) | |
| 46–55 | 2 (2.3) | 12 (14.0) | 5 (5.8) | 8 (9.3) | 27 (31.4) | |
| 56–65 | 1 (1.2) | 16 (18.6) | 3 (3.5) | 9 (10.5) | 29 (33.7) | |
| 66–75 | 0 (0.0) | 4 (4.7) | 1 (1.2) | 3 (3.5) | 8 (9.3) | |
| >75 | 0 (0.0) | 2 (2.3) | 2 (2.3) | 1 (1.2) | 5 (5.8) | |
| Years of education (mean, SD) | 14.13 (3.72) | 13.35 (5.27) | 13.77 (4.50) | |||
| Years of education | <6 | 0 (0.0) | 0 (0.0) | 1 (1.2) | 0 (0.0) | 1 (1.2) |
| 7–12 | 1 (1.2) | 14 (16.3) | 4 (4.7) | 14 (16.3) | 33 (38.4) | |
| 13–16 | 1 (1.2) | 22 (25.6) | 5 (5.8) | 5 (5.8) | 33 (38.4) | |
| >17 | 3 (3.5) | 5 (5.8) | 4 (4.7) | 7 (8.1) | 19 (22.1) | |
| Family status | married | 2 (2.3) | 30 (34.9) | 9 (10.5) | 18 (20.9) | 59 (68.6) |
| single | 2 (2.3) | 7 (8.1) | 4 (4.7) | 5 (5.8) | 18 (20.9) | |
| widowed | 0 (0.0) | 1 (1.2) | 0 (0.0) | 0 (0.0) | 1 (1.2) | |
| divorced | 1 (1.2) | 3 (3.5) | 1 (1.2) | 3 (3.5) | 8 (9.3) | |
| Main carer | yes | 1 (1.2) | 31 (36.0) | 9 (10.5) | 20 (23.3) | 61 (70.9) |
| no | 4 (4.7) | 10 (11.6) | 5 (5.8) | 6 (7.0) | 25 (29.1) | |
| Relationship with the PwD | partner | 0 (0.0) | 10 (11.6) | 4 (4.7) | 6 (7.0) | 20 (23.3) |
| daughter/son | 4 (4.7) | 29 (33.7) | 10 (11.6) | 16 (18.6) | 59 (68.6) | |
| brother/sister | 0 (0.0) | 1 (1.2) | 0 (0.0) | 1 (1.2) | 2 (2.3) | |
| other family member | 1 (1.2) | 1 (1.2) | 0 (0.0) | 3 (3.5) | 5 (5.8) | |
| Living together | 1 (20,0) | 29 (70,7) | 9 (64,3) | 15 (57,7) | 54 (62,8) | |
| Free time h/week (mean, SD) | 22.0 (24.7) | 17.4 (20,0) | 19,8 (22,6) | |||
| Number of medications (mean, SD) | 1.2 (1.9) | 0.9 (1.2) | 1,1 (1,6) | |||
| Occupation | employee | 4 (4.7) | 10 (11.6) | 10 (11.6) | 11 (12.8) | 35 (40.7) |
| unemployed | 1 (1.2) | 6 (7.0) | 0 (0.0) | 0 (0.0) | 7 (8.1) | |
| housewife | 0 (0.0) | 14 (16.3) | 0 (0.0) | 6 (7.0) | 20 (23.3) | |
| retiree | 0 (0.0) | 11 (12.8) | 4 (4.7) | 7 (8.1) | 22 (25.6) | |
| other | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (2.3) | 2 (2.3) | |
| Fear of dementia | yes | 2 (2.3) | 19 (22.1) | 3 (3.5) | 15 (17.4) | 39 (45.3) |
| no | 3 (3.5) | 22 (25.6) | 11 (12.8) | 11 (12.8) | 47 (54.7) | |
Table 2
Characteristics of PwD
| Mild (n = 34), n (%) | Moderate (n = 23), n (%) | Severe (n = 29), n (%) | Total N (%) | ||
| Age mean (SD) | 77.03 (7.61) | 79.30 (5.41) | 78.86 (10.94) | 78.26 (4.64) | |
| Age group | 56–65 | 2 (5.9) | 0 (0.0) | 6 (20.7) | 8 (9.30) |
| 66–75 | 11 (32.4) | 8 (34.8) | 5 (17.2) | 24 (27.91) | |
| 76–85 | 16 (47.1) | 11 (47.8) | 7 (24.1) | 34 (39.91) | |
| >86 | 5 (14.7) | 4 (17.4) | 11 (37.9) | 20 (23.26) | |
| Gender | male | 12 (35.3) | 7 (30.4) | 10 (34.5) | 29 (33.72) |
| female | 22 (64.7) | 16 (69.6) | 19 (65.5) | 57 (66.28) | |
| Education (mean y, SD) | 8.06 (4.54) | 5.52 (2.47) | 9.55 (5.36) | 7.88 (4.64) | |
| Years of education | <6 | 18 (52.9) | 20 (87.0) | 12 (41.4) | 50 (58.14) |
| 7–12 | 10 (29.4) | 3 (13.0) | 7 (24.1) | 20 (23.26) | |
| 13–16 | 5 (14.7) | 0 (0.0) | 8 (27.6) | 13 (15.12) | |
| >17 | 1 (2.9) | 0 (0.0) | 2 (6.9) | 3 (3.49) | |
| Family status | married | 18 (52.9) | 12 (52.2) | 13 (44.8) | 43 (50.00) |
| single | 0 (0.0) | 0 (0.0) | 2 (6.9) | 2 (2.33) | |
| widowed | 14 (41.2) | 11 (47.8) | 13 (44.8) | 38 (44.19) | |
| divorced | 2 (5.9) | 0 (0.0) | 1 (3.4) | 3 (3.49) | |
| MMSE (mean, SD) | 23.62 (2.31) | 15.57 (2.63) | 3.90 (3.75) | 14.81 (8.96) | |
| NPI (mean, SD) | 12.12 (13.54) | 9.74 (8.91) | 16.34 (16.98) | 12.91 (13.92) | |
| Barthel Index | 0–20 | 1 (2.9) | 1 (4.3) | 10 (34.5) | 12 (13.95) |
| 21–60 | 2 (5.9) | 5 (21.7) | 5 (17.2) | 12 (13.95) | |
| 61–90 | 14 (41.2) | 9 (39.1) | 12 (41.4) | 35 (40.70) | |
| 91–99 | 5 (14.7) | 5 (21.7) | 1 (3.4) | 11 (12.79) | |
| 100 | 12 (35.3) | 3 (13.0) | 1 (3.4) | 16 (18.60) |
The mean age of the PwD was 78.2 years. MMSE of the PwD ranged between 0 and 26, with 34 persons (39.5%) having mild dementia, 23 (26.7%) moderate, and 29 (33.7%)x severe dementia. 66.3% were female, with a mean of 8.1 years of education, half of them were still married. The PwD took in average 5 medications, and their functionality, measured with the Barthel Index, decreased with the severity of dementia.
Predictors for the dementia attitude
First, correlations were used to give an overview of the relations between the variables (Table 3). The correlation matrix shows a large positive correlation between CODE and DAS (r = 0.582, p < 0.001) and a moderate positive correlation between PAC and DAS (r = 0.457, p < 0.001), DKAT2 and CODE (r = 0.437, p < 0.001), PAC and CODE (r = 0.301, p = 0.002), DKAT2 and DAS (r = 0.349, p < 0.001), as well as the age of the caregiver and CODE (r = 0.304, p < 0.005). There was also a moderate negative correlation between NPI and DAS (r = –0.402, p < 0.001), between TRAIT anxiety and DAS (r = –0.455, p < 0.001) as well as a weak negative correlation between the education of the caregiver and PAC (r = –0.266, p < 0.005). Besides, having followed a special program showed a large negative correlation to knowledge (r = –0.579, p < 0.001) and a moderate negative correlation to DAS (r = –0.342, p = 0.001) and CODE (r = –0.383, p < 0.001).
Table 3
Pearson correlation matrix
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| 1. DAS | –– | |||||||
| 2. DKAT2 | 0.35 ** | –– | ||||||
| 3. CODE | 0.58 ** | 0.44 ** | –– | |||||
| 4. PAC | 0.46 ** | 0.01 | 0. 30 ** | –– | ||||
| 5. sZBI | 0.29 ** | 0.29 ** | 0.05 | –0.29 ** | –– | |||
| 6. STATE | –0.37 ** | –0.05 | –0.07 | –0.18 | 0.38 ** | –– | ||
| 7. TRAIT | –0.46 ** | –0.07 | –0.18 | –0.28* | 0.44 ** | 0.80 ** | –– | |
| 8. NPI | –0.40 ** | 0.01 | –0.14 | –0.23* | 0.38 ** | 0.17 | 0.27* | –– |
| Age IC | 0.14 | –0.01 | 0.31 ** | 0.23* | –0.03 | –0.01 | 0.00 | 0.04 |
| Education IC | –0.02 | 0.21 | –0.08 | –0.27* | 0.18 | –0.15 | –0.11 | 0.06 |
| PP | –0.34 ** | –0.58 ** | –0.38 ** | –0.08 | –0.15 | 0.23* | 0.19 | 0.00 |
| Free time h/week | –0.07 | –0.15 | –0.02 | 0.07 | –0.23* | –0.21 | –0.15 | 0.02 |
| Fear of dementia | 0.29 ** | –0.12 | 0.26* | 0.24* | –0.27* | –0.30 ** | –0.37 ** | –0.08 |
| Living together | –0.01 | 0.00 | –0.05 | –0.15 | –0.10 | –0.20 | –0.20 | –0.01 |
| Age PwD | 0.00 | –0.03 | 0.10 | –0.01 | 0.06 | –0.24* | –0.17 | –0.08 |
| Education PwD | –0.01 | 0.19 | 0.03 | –0.06 | 0.12 | 0.25* | 0.18 | 0.18 |
| MMSE | –0.05 | –0.31 ** | –0.19 | –0.08 | –0.29 ** | –0.03 | 0.01 | –0.16 |
| Barthel Index | –0.15 | –0.29 ** | –0.25* | –0.12 | –0.29 ** | 0.00 | 0.06 | –0.04 |
DAS, Dementia Attitude Scale; DKAT2, Dementia Knowledge Assessment Tool 2; CODE, Confidence in Dementia Care; IC, Informal Carer; NPI, Neuropsychiatric Inventory; PAC, Positive Aspects of Caregiving; PP, Psycho-educational Program; sZBI, short Zarit Burden Interview; State and Trait, State-Trait Anxiety Inventory. *p≤0.05, **p≤0.01, ***p≤0.001, all significant correlations are highlighted in bold. 0.1 < r < 0.3 weak relationship, 0.3 < r < 0.5 moderate relationship, r > 0.5 strong relationship.
Univariable linear regression was employed to estimate the possible association of each independent variable studied with DAS: the caregiver characteristics (age, gender, educational level, relationship with PwD, years of caring for a person with dementia, hours of caregiving, free time, numbers of medications, fear of dementia, special dementia training), the CODE, PAC, sZBI, DKAT2, and Spielberger’s anxiety scales, as well as the characteristics of PwD (age, gender, educational level, MMSE, Barthel Index, and NPI).
The results of the initial univariable linear regression analyses, which demonstrated a significant association with DAS, are shown in Table 4. Confidence in care was a striking predictor for the positive attitude toward dementia (F(1, 84) = 42.98, p < 0.001), explaining 33.1% of the total variance of the overall attitude (DAS).
Table 4
Univariable regression analysis (N = 86)
| Variable | β | 95% CI | Adjusted R2 | F | p |
| CAREGIVER | |||||
| Number of medications | 0.213 | 0.01 to 3.93 | 0.034 | 3.97 | 0.049* |
| PP | –0.342 | –16.10 to –4.08 | 0.106 | 11.13 | 0.001*** |
| DKAT2 | 0.349 | 0.55 to 2.07 | 0.111 | 11.63 | 0.001*** |
| CODE | 0.582 | 0.72 to 1.34 | 0.331 | 42.98 | <0.001*** |
| PAC | 0.457 | 0.42 to 1.01 | 0.2 | 22.23 | <0.001*** |
| sZBI | –0.285 | –0.76 to 0.12 | 0.07 | 7.4 | 0.008** |
| STATE | –0.369 | –0.56 to –0.16 | 0.126 | 13.2 | <0.001*** |
| TRAIT | –0.455 | –0.93 to –0.38 | 0.198 | 21.97 | <0.001*** |
| PWD | |||||
| NPI | –0.402 | –0.64 to –0.22 | 0.152 | 16.2 | <0.001*** |
The above variables correlated significantly with dementia attitude. Variables that did not correlate significantly with carers’ attitude were excluded from this table: age of caregiver, education of caregiver, fear of dementia, living together, free time, hours of caregiving, age of PwD, education of caregiver, MMSE, and Barthel Index. CODE, Confidence in Dementia Care; DKAT2, Dementia Knowledge; NPI, Neuropsychiatric Inventory; PAC, Positive Aspects of Caregiving; PP, Psycho-educational Program; sZBI, short Zarit Burden Interview. State and Trait, State-Trait Anxiety Inventory. *p≤0.05, **p≤0.01, ***p≤0.001.
Positive aspects in caregiving (PAC) (F(1, 84) = 22.23, p < 0.001, adjusted R2 = 0.200), decreased anxiety as a trait (F(1, 84) = 21.97, p < 0.001, adjusted R2 = 0.198) as well as a state (F(1, 84) = 13.2, p < 0.001, R2 = 0.126) and decreased neuropsychiatric symptoms (NPI) (F(1, 84) = 16.20, p < 0.001, adjusted R2 = 0.152) seemed to play a major role in perceptions of positive attitudes in dementia. General knowledge toward dementia (DKAT2) (F(1, 84) = 11.63, p = 0.001, adjusted R2 = 0.111) and participation in a special program for carers support (F(1, 84) = 11.13, p = 0.001, adjusted R2 = 0.106) proved to be also essential factors for the attitude. Lastly, the number of medications taken by the carers was also a predictor but with a weaker influence (F(1, 84) = 3.97, p = 0.049, adjusted R2 = 0.034).
All variables which showed a significance of p≤0.01 in the univariable regression (Table 4) were introduced stepwise into a multiple regression analysis to investigate in detail how much variance of the carers’ attitude toward dementia could be explained by those variables. The results of the multiple regression (Table 5) indicated that the final model explained 55.6% of the variance, and that it was a significant predictor of dementia attitude F(1, 80) = 22.25, p < 0.001. While the confidence in dementia care contributed most to the model (β= 0.358, p < 0.001), lower trait anxiety (β= –0.251, p = 0.002), lower NPI score (β= –0.235, p = 0.003), more positive aspects of caregiving (PAC) (β= 0.226, p = 0.006), and dementia knowledge (DKAT2) (β= 0.176, p = 0.034) were also significant predictors of the dementia attitude (DAS). On the other hand, the burden (ZBI) and the participation in a special dementia program lost their significance.
Table 5
Final multivariable model (N = 86)
| Scale | β | T | 95% CI | p |
| CODE | 0.358 | 4.176 | 0.33 to 0.93 | 0.000*** |
| TRAIT anxiety | –0.251 | –3.228 | –0.58 to –0.14 | 0.002** |
| NPI | –0.235 | –3.068 | –0.41 to –0.09 | 0.003** |
| PAC | 0.226 | 2.842 | 0.105 to 0.598 | 0.006** |
| DKAT2 | 0.176 | 2.159 | 0.05 to 1.27 | 0.034* |
CODE, Confidence in Dementia Care; DKAT2, Dementia Knowledge; NPI, Neuropsychiatric Inventory; PAC, Positive Aspects of Caregiving. Total adjusted R2 = 0.556; *p≤0.05, **p≤0.01, ***p≤0.001.
The impact of a psycho-educational dementia program for carers on the attitude, knowledge, confidence, positive aspects of caring, burden, and anxiety
As depicted in Table 6, the informal carers who attended a special program had a more positive attitude toward the PwD, both in the overall construct of attitude, t(84) = 3.34, p < 0.001, as well as in the respective factors “social comfort”, t(84) = 3,73, p < 0.001 and “knowledge”, t(84) = 2.02, p = 0.046. Moreover, carers who attended a special program had a better knowledge of the disease (DKAT2), t(84) = 6.52, p < 0.001 and their confidence in dementia (CODE) was higher, t(84) = 3.80, p < 0.001. The differences between groups were not significant in respect to the positive aspects of caring (PAC) (p = 0.445) as well as in respect to the burden measured with the short form of the ZBI (p = 0.169), which was slightly higher in those who participated in a dementia training program. Regarding the anxiety scores, carers who attended a special program had a lower score than those who did not attend a special program in the state, t(84) = –2.12, p = 0.037. The analysis of covariance (ANCOVA) could not show any association of age, relationship with the PwD, living together, occupation, fear of dementia, taking medicine, previous experience with dementia, and NPI to the participation of a special dementia program (p > 0.05). The internal consistency for all instruments was acceptable to excellent (Cronbach’s α= 0.72 to 0.95).
Table 6
Comparison of the Mean-Values (SD) between caregivers who participated in a psycho-educational dementia program and those who did not
| PE N = 46 | No PE N = 40 | Total | Range | t | 95% Confidence Interval of the difference | Cronbach’s α | ||
| M (SD) | M (SD) | N = 86 | ||||||
| lower | upper | |||||||
| DAS | 113.57 (14.72) | 103.48 (13.10) | 108.87 (14.80) | 67–137 | 3.34*** | 4.06 | 16.10 | 0.83 |
| sc | 48.48 (9.37) | 41.50 (7.73) | 45.23 (9.28) | 25–63 | 3.73*** | 3.26 | 10.70 | 0.72 |
| k | 65.09 (6.83) | 61.98 (7.44) | 63.64 (7.25) | 40–77 | 2.02* | 0.51 | 0.51 | 0.74 |
| DKAT2 | 14.83 (3.10) | 10.28 (3.37) | 12.71 (3.94) | 1–19 | 6.52*** | 3.16 | 5.94 | 0.78 |
| CODE | 32.30 (7.53) | 25.90 (8.10) | 29.33 (8.40) | 9–45 | 3.80*** | 3.05 | 9.76 | 0.91 |
| PAC | 33.28 (9.36) | 31.70 (9.75) | 32.55 (9.52) | 8–44 | 0.77 | –2.52 | –5.69 | 0.91 |
| sZBI | 16.70 (9.90) | 13.85 (9.00) | 15.37 (9.54) | 0–38 | 1.39 | –1.24 | 6.93 | 0.88 |
| STATE | 35.72 (13.85) | 42.50 (15.86) | 38.87 (15.12) | 20–79 | –2.12* | –13.15 | –0.41 | 0.95 |
| TRAIT | 35.13 (9.47) | 39.00 (11.05) | 36.93 (10.36) | 20–72 | –1.75 | –1.75 | 0.53 | 0.91 |
CODE, Confidence in Dementia Care; DAS, Dementia Attitude Scale; sc, social comfort; k, knowledge; DKAT2, Dementia Knowledge Assessment Tool 2; PAC, Positive Aspects of Caregiving; PE, Psycho-educational Program; sZBI, short Zarit Burden Interview; State and Trait, State-Trait Anxiety Inventory. *p≤0.05, **p≤0.01, ***p≤0.001.
DISCUSSION
The purpose of this study was to examine the factors that impact the informal carers’ attitude toward dementia. To our knowledge, it is the first study that takes into consideration characteristics of both informal carers and Pwd, as well as the carers’ knowledge about dementia, their participation in support and educational programs, the confidence in dementia care, the burden and positive aspects of caregiving, the caregivers’ anxiety, the severity of dementia, and the functionality of the PwD and BSPDs. Our final model, which explained 55.6% of the total variance, shows a significant correlation of five factors with attitude toward dementia: The confidence in dementia care had the strongest effect, followed by the BPSD, anxiety as a trait, positive aspects of dementia caregiving, and dementia knowledge, whereas caregivers’ or PwD’s characteristics, the severity of dementia, and the functionality did not correlate significantly with attitude. As a secondary outcome, the study compared the attitude and the aforementioned factors between carers who participated in a psycho-education program for caregivers [66] and those who never attended such a program. The participants of the psycho-education program showed a significantly more positive attitude toward dementia, significantly better knowledge about dementia, and higher confidence in dementia care. Also, they tended to see more of the positive aspects of caregiving. At the same time, study participants had significantly lower anxiety as a state and as a trait, demonstrating a slightly higher burden of care. Perhaps this feeling of higher burden was the reason why they consulted psychologists of the Greek Alzheimer’s Association.
The overall positive attitude of the total sample and the low dementia knowledge level were also observed by previous studies that showed a generally positive attitude toward PwD [8] and an unsatisfactory knowledge about dementia in family caregivers [67, 68]. Although some studies [53] support that knowing someone with dementia can significantly impact attitude and knowledge, which could be an explanation for the positive attitude seen in our sample of carers; nevertheless, the knowledge level in this sample was low, at least in those who never participated in a psycho-educational program. This finding stresses the assumption that training and psychological support can impact attitude and knowledge [69]. Unfortunately, there is still a lack of research about informal carers’ attitude toward dementia and a lack of instruments assessing all three components: affect, cognition, and behavior. Most of the existing studies used self-developed instruments or the ADQ and the DAS. ADQ seems to measure knowledge rather than attitude [19], but also the DAS reflects fewer affective and behavioral than cognitive dimensions, which can be a possible explanation of the high correlation between attitude and knowledge in those studies.
The participating carers more often perceived positive aspects of caregiving in comparison to other studies [70]. This result can be biased due to the high percentage of carers who already received support from the Family Unit of the Alzheimer’s Association. Direct comparisons with the Zarit burden interview are more complicated because most studies use the full version of the tool and not the short one used in the current study. Park et al. (2017), who investigated the effect of a dementia family support program on the carers’ attitude toward dementia, showed a statistically insignificant decrease of the burden [29].
Nearly half of the 86 caregivers included in the study participated in a psycho-educational program of the Alzheimer’s Association for carers [66]. Previous studies have already shown the positive impact on the emotional state and sense of the burden of the day centers beneficiaries after psycho-education or psychotherapeutic interventions [62, 63]. However, since the goal of our study was not the intervention in the form of a psycho-educational program, the study can only give an indirect indication using the existing data. Thus, comparing the two groups, participation in a program seems to affect both dementia knowledge and confidence in dementia care significantly and at the same time reduces the state of anxiety.
Not much evidence exists about the knowledge, attitude and confidence measurements [71, 72] among family caregivers. Nevertheless, evidence in health care staff suggests that training interventions encompass not only knowledge acquisition but also attitude and confidence [36, 73].
The highest contribution in this current model was the confidence in dementia care. To our knowledge, no study investigated family caregivers using the CODE. However, it seems to be a reliable short tool with a high correlation to the DAS and DKAT2. Generally, the level of confidence is linked to knowledge, as caregivers who know are expected to feel confident and therefore more motivated to transfer the acquired knowledge [74], so there is also an influence to a more positive attitude and reduced anxiety as indicated in other studies [75]. Moreover, caregivers’ and PwD’s characteristics showed no correlation with attitude except for the BPSDs, which is consistent with the study by Mulyani (2019), who also found no correlation of sex and the level of education with attitude [76]. Studies that focused on dementia knowledge have already shown the gap in dementia-related knowledge in informal carers [77, 78] as well as the correlation to the caregiver burden [79, 80]. In addition, informal carers with increased knowledge are more likely to seek help from care services [81] and better understand the BPSDs associated with dementia [80]. Unfortunately, most studies can hardly be compared due to their use of non-validated instruments for informal caregivers. Most instruments are designed and validated for formal caregivers who have different education and different needs for dementia knowledge. In general, data on informal caregivers are scarce, and, to our knowledge, no single study has so far investigated the correlation of all the factors examined in the present study.
Our study is in line with the findings of recent research that showed that psycho-education as an approach is among the most powerful interventions to improve carers’ attitude toward dementia [28]. However, Cowan (2019) proved that also short programs such as the Dementia Friends, which last only one hour and combine knowledge with communication techniques and five key messages, could also improve the attitude toward dementia (pre-M = 110.7, post-M 121.9) [63].
The strong correlation of attitude and knowledge, as well as confidence in dementia care, supports the tripartite model of attitude, which hypothesizes the interrelation of affect, cognition, and behavior [9]. A better knowledge also has implications on health care service utilization [38] and decisions regarding medications [40] as well as on nursing home placement [41]. Studies are needed that will take into account the already examined variables and investigate the Quality of Life (QoL) of both the carer and the PwD as well as the coping strategies. We need to design appropriate programs that also include the needs of the PwD and investigate the effect of a more positive attitude toward PwD on the QoL of PwD and the influence on BSPDs. A possible model could be to create individual training programs set up analogous to the “Trialogue Model” already approved for several psychiatric disorders, where PwD, relatives, and professionals approach each other as experts of their own side in order to learn from each other.
Our study indicates that better dementia knowledge leads to higher confidence in dementia care as well as to a more positive attitude toward dementia, which is related to the decrease of the BSPDs in PwD and therefore lowering the burden of the caregiver, contributing in that way to a better quality of life for both the carer and the PwD. However, an intervention study with a psycho-educational program is needed to confirm this hypothesis. This should include at least validated instruments to examine dementia attitude, dementia knowledge, confidence in dementia care as well as burden and positive aspects of care but takes also into account the behavioral and psychological symptoms of the person with dementia.
Limitations
There are some limitations, and, therefore, the findings have to be interpreted with caution. First, the carers recruited from the Alzheimer Hellas Association (St. Helen Day Care Center) participated in a psycho-educational program which can be a bias of the overall positive attitude, while most of those recruited at the neurological practice came there for a diagnosis for their relatives. That explains the difference between the MMSE of both groups. Second, it was a cross-sectional study. Because of the dynamic process of dementia caregiving, a longitudinal approach would allow one to observe changes in the variables over time. Because of the cross-sectional design, a definite answer regarding cause and result cannot be drawn. We can only speculate whether the informal carers who had previously participated in the psycho-educational program had even less knowledge and less positive attitudes about dementia prior to attending the program, and whether they participated in it because of a high burden. Another potential limitation is that although the instruments used were all validated in Greek, they were not always validated for the target group used.
ACKNOWLEDGMENTS
This study is independent research. The views expressed in this publication are those of the authors. We want to thank Petrina Margaritidou, Konstantina Karagiozi, the Greek Association of Alzheimer’s Disease and Related Disorders for their support during the data collection, and Anton Schoenstein for his advice regarding the statistical analysis.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/21-5731r2).
REFERENCES
[1] | Brodaty H , Donkin M ((2009) ) Family caregivers of people with dementia. Dialogues Clin Neurosci 11: , 217–228. |
[2] | Soong A , Au ST , Kyaw BM , Theng YL , Tudor Car L ((2020) ) Information needs and information seeking behaviour of people with dementia and their non-professional caregivers: A scoping review. BMC Geriatr 20: , 61. |
[3] | Yu DS , Cheng ST , Wang J ((2018) ) Unravelling positive aspects of caregiving in dementia: An integrative review of research literature. Int J Nurs Stud 79: , 1–26. |
[4] | Manzini CSS , do Vale FAC ((2020) ) Emotional disorders evidenced by family caregivers of older people with Alzheimer’s disease. Dement Neuropsychol 14: , 56–61. |
[5] | Courtin E , Jemiai N , Mossialos E ((2014) ) Mapping support policies for informal carers across the European Union. Health Policy 118: , 84–94. |
[6] | Chiao CY , Wu HS , Hsiao CY ((2015) ) Caregiver burden for informal caregivers of patients with dementia: A systematic review. Int Nurs Rev 62: , 340–350. |
[7] | Han A ((2020) ) Interventions for attitudes and empathy toward people with dementia and positive aspects of caregiving: A systematic review and meta-analysis. Res Aging 42: , 72–82. |
[8] | Zawadzki L , Mondon K , Peru N , Hommet C , Constans T , Gaillard P , Camus V ((2011) ) Attitudes towards Alzheimer’s disease as a risk factor for caregiver burden. Int Psychogeriatr 23: , 1451–1461. |
[9] | Rosenberg MJ , Hovland CI (1960) Cognitive, affective, and behavioral components of attitudes. In: Attitude organization and change: An analysis of consistency among attitude components, Rosenberg MJ, ed.,Yale University Press: New Haven, pp. 1-14. |
[10] | Breckler SJ ((1984) ) Empirical validation of affect, behavior, and cognition as distinct components of attitude. J Pers Soc Psychol 47: , 1191–1205. |
[11] | Kothandapani V ((1971) ) Validation of feeling, belief, and intention to act as three components of attitude and their contribution to prediction of contraceptive behavior. J Pers Soc Psychol 19: , 321–333. |
[12] | Cheston R , Hancock J , White P ((2016) ) A cross-sectional investigation of public attitudes toward dementia in Bristol and South Gloucestershire using the approaches to dementia questionnaire. Int Psychogeriatr 28: , 1717–1724. |
[13] | Guyer JJ , Fabrigar LR ((2015) ) Attitudes and Behavior. In International encyclopedia of the social & behavioral sciences, Wright JD, ed., 2. ed., Elsevier: Amsterdam, pp. 183–189. |
[14] | Graham N , Lindesay J , Katona C , Bertolote JM , Camus V , Copeland JRM , Mendonca Lima de CA , Gaillard M , Gély Nargeot MC , Gray J , Jacobsson L , Kingma M , Kühne N , O’Loughlin A , Rutz W , Saraceno B , Taintor Z , Wancata J ((2003) ) Reducing stigma and discrimination against older people with mental disorders: A technicalconsensus statement. }. Int J Geriatr Psychiatry 18: , 670–678. |
[15] | dem Knesebeck von O , Angermeyer MC , Lüdecke D , Kofahl C ((2014) ) Emotional reactions toward people with dementia - results of a population survey from Germany. Int Psychogeriatr 26: , 435–441. |
[16] | Zimmerman S , Williams CS , Reed PS , Boustani M , Preisser JS , Heck E , Sloane PD ((2005) ) Attitudes, stress, and satisfaction of staff who care for residents with dementia. Gerontologist 45: , 96–105. |
[17] | Kahana E , Kinney JM , Ercher K , Kahana B , Tinsley VV , King C , Stuckey JC , Ishler KJ ((1996) ) Predictors of attitudes toward three target groups of elderly persons. J Aging Health 8: , 27–53. |
[18] | Alamri BH , Xiao LD ((2017) ) Health professionals’ knowledge and attitudes toward older people in primary care in Saudi Arabia. Saudi Med J 38: , 229–236. |
[19] | de Vries K , Drury-Ruddlesden J , McGill G ((2020) ) Investigation into attitudes towards older people with dementia in acute hospital using the Approaches to Dementia Questionnaire. Dementia (London) 19: , 2761–2779. |
[20] | Norbergh KG , Helin Y , Dahl A , Hellzén O , Asplund K ((2006) ) Nurses’ attitudes towards people with dementia: Thesemantic differential technique. Nurs Ethics 13: , 264–274. |
[21] | Blaser R , Berset J ((2019) ) Setting matters: Associations of nurses’ attitudes towards people with dementia. Nurs Open 6: , 155–161. |
[22] | Mason RL , Annear MJ , Lo A , McInerney F , Tierney LT , Robinson AL ((2016) ) Development and preliminary psychometric properties of the General Practitioner Attitudes and Confidence Scale (GPACS-D) for dementia. BMC Fam Pract 17: , 105. |
[23] | Jackson EM , Cherry KE , Smitherman EA , Hawley KS ((2008) ) Knowledge of memory aging and Alzheimer’s disease in college students and mental health professionals. Aging Ment Health 12: , 258–266. |
[24] | Breining A , Lavallart B , Pin S , Léon C , Moulias S , Arwidson P , Beck F , Berr C , Verny M ((2014) ) Perception ofAlzheimer’s disease in the French population. J Nutr Health Aging 18: , 393–399. |
[25] | Tsolaki M , Paraskevi S , Degleris N , Karamavrou S ((2009) ) Attitudes and perceptions regarding Alzheimer’s disease in Greece. Am J Alzheimers Dis Other Demen 24: , 21–26. |
[26] | Cations M , Radisic G , Crotty M , Laver KE ((2018) ) What does the general public understand about prevention and treatment of dementia? A systematic review of population-based surveys. PLoS One 13: , e0196085. |
[27] | Chen CK , Clayton K , Chodosh J ((2017) ) The Relationship between “what we believe” and “how we care” among daughters caring for a parent with dementia. Am J Alzheimers Dis Other Demen 32: , 90–95. |
[28] | Hattink B , Meiland F , van der Roest H , Kevern P , Abiuso F , Bengtsson J , Giuliano A , Duca A , Sanders J , Basnett F , Nugent C , Kingston P , Dröes R-M ((2015) ) Web-based STAR e-learning course increases empathy and understanding in dementia caregivers: Results from a randomized controlled trial in the Netherlands and the United Kingdom. J Med Internet Res 17: , e241. |
[29] | Park YS , Jee YJ , Bae SH ((2017) ) Effects of a dementia family support program on families’ attitude towards dementia, desire for institutionalization, caregiving behavior and caregiving burden. AJMAHS 7: , 781–793. |
[30] | Yamamoto-Mitani N , Tamura M , Deguchi Y , Ito K , Sugishita C ((2000) ) The attitude of Japanese family caregivers toward the elderly with dementia. Int J Nurs Stud 37: , 415–422. |
[31] | TeichmannB, XiromerisiouG, TsolakiM ((2021) ) Informal caregivers𠀙 attitude toward dementia - a review. PRIME 14: , 170–189. |
[32] | Lintern TC (2001) Quality in dementia Care: Evaluating staff attitude and behavior (Thesis). Bangor University. |
[33] | Macdonald AJD , Woods RT ((2005) ) Attitudes to dementia and dementia care held by nursing staff in U.K. “non-EMI” care homes: What difference do they make? . Int Psychogeriatr 17: , 383–391. |
[34] | Taylor SM , Dear MJ ((1981) ) Scaling community attitudes toward the mentally ill. Schizophr Bull 7: , 225–240. |
[35] | Cole JD , Kazarian SS ((1988) ) The level of expressed emotion scale: A new measure of expressed emotion. J Clin Psychol 44: , 392–397. |
[36] | Gkioka M , Tsolaki M , Papagianopoulos S , Teichmann B , Moraitou D ((2020) ) Psychometric properties of dementia attitudes scale, dementia knowledge assessment tool 2 and confidence in dementia scale in a Greek sample. Nurs Open 7: , 1623–1633. |
[37] | Peng A , Moor C , Schelling HR (2011) Einstellungenzu Demenz: Übersetzung und Validierung eines Instruments zur Messung von Einstellungen gegenuüer Demenz und demenzkranken Menschen (Teilprojekt 1), Schlussbericht zuhanden des Forschungsfonds der schweizerischen Alzheimervereinigung. |
[38] | Lüdecke D , dem Knesebeck von O , Kofahl C ((2016) ) Public knowledge about dementia in Germany–results of a population survey. Int J Public Health 61: , 9–16. |
[39] | Kaduszkiewicz H , Röntgen I , Mossakowski K , van den Bussche H ((2009) ) Tabu und Stigma in der Versorgung von Patienten mit Demenz: Kann ein Fortbildungsangebot für Hausärzte und ambulante Pflegedienste zur Destigmatisierung beitragen? . Z Gerontol Geriatr 42: , 155–162. |
[40] | Lim RH , Sharmeen T ((2018) ) Medicines management issues in dementia and coping strategies used by people living with dementia and family carers: A systematic review. Int J Geriatr Psychiatry 12: , 1562–1581. |
[41] | Nguyen N , Renom-Guiteras A , Meyer G , Stephan A ((2018) ) Nursing home placement of people with dementia: A secondary analysis of qualitative data and literature review on perspectives of informal caregivers and healthcare professionals. Pflege 31: , 155–166. |
[42] | Awad A , Voruganti LNP ((2008) ) The burden of schizophrenia on caregivers: A review. Pharmacoeconomics 26: , 149–162. |
[43] | George LK , Gwyther LP ((1986) ) Caregiver well-being: A multidimensional examination of family caregivers of demented adults. Gerontologist 26: , 253–259. |
[44] | Bédard M , Molloy DW , Squire L , Dubois S , Lever JA , O’Donnell M ((2001) ) The Zarit Burden Interview: A new shortversion and screening version. Gerontologist 41: , 652–657. |
[45] | Zarit S , Reever KE , Bach-Peterson J ((1980) ) Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist 20: , 649–655. |
[46] | Lundh U ((1999) ) Family carers 3: Coping strategies among family carers in Sweden. Br J Nurs 8: , 735–740. |
[47] | Tsatali M , Egkiazarova M , Toumpalidou M , Karagiozi K , Margaritidou P , Tsolaki M ((2022) ) Greek adaptation of the Positive Aspects of Caregiving (PAC) scale in dementia caregivers. Clin Gerontol 45: , 538–547. |
[48] | Elvish R , Burrow S , Cawley R , Harney K , Graham P , Pilling M , Gregory J , Roach P , Fossey J , Keady J ((2014) ) “Getting to Know Me”: The development and evaluation of a training programme for enhancing skills in the care of people with dementia in general hospital settings. Aging Ment Health 18: , 481–488. |
[49] | Galvin JE , Kuntemeier B , Al-Hammadi N , Germino J , Murphy-White M , McGillick J ((2010) ) “Dementia-friendly hospitals: Care not crisis": An educational program designed to improve the care of the hospitalized patient with dementia. Alzheimer Dis Assoc Disord 24: , 372–379. |
[50] | Gkioka M , Teichmann B , Moraitou D , Papagiannopoulos S , Tsolaki M ((2020) ) Effects of a person centered dementia training program in Greek hospital staff-implementation and evaluation. Brain Sci 10: , 976. |
[51] | Mondschein CF , Monda C ((2019) ) The EU’s General Data Protection Regulation (GDPR) in a Research Context. In Fundamentals of Clinical Data Science, Kubben P, Dumontier M, Dekker A, eds., Springer International Publishing: Cham, pp. 55–71. |
[52] | Papastavrou E , Kalokairinou-Anagnostopoulou A , Alevizopoulos G , Papakostas S , Tsagari X , Sourtzi P ((2006) ) The reliability and validity of the scale of burden (Zarit burden interview) in Greek Cypriot caregivers of patients with dementia. Nursing 45: , 439–449. |
[53] | O’Connor ML , McFadden SH ((2010) ) Development and psychometric validation of the dementia attitudes scale. Int J Alzheimers Dis 2010: , 454218. |
[54] | Toye C , Lester L , Popescu A , McInerney F , Andrews S , Robinson AL ((2014) ) Dementia Knowledge assessment tool version two: Development of a tool to inform preparation for care planning and delivery in families and care staff. Dementia (London) 13: , 248–256. |
[55] | Elvish R , Burrow S , Cawley R , Harney K , Pilling M , Gregory J , Keady J ((2018) ) ‘Getting to know me’: The second phase roll-out of a staff training programme for supporting people with dementia in general hospitals. Dementia (London) 17: , 96–109. |
[56] | Fountoulakis KN , Papadopoulou M , Kleanthous S , Papadopoulou A , Bizeli V , Nimatoudis I , Iacovides A , Kaprinis GS ((2006) ) Reliability and psychometric properties of the Greek translation of the State-Trait Anxiety Inventory form Y: Preliminary data. Ann Gen Psychiatry 5: , 2. |
[57] | Mahoney F , Barthel D ((1965) ) Functional evaluation: The Barthel Index. Md State Med J 14: , 61–65. |
[58] | Theofanidis D ((2017) ) Validation of international stroke scales for use by nurses in Greek settings. Top Stroke Rehabil 24: , 214–221. |
[59] | Cummings JL , Mega M , Gray K , Rosenberg-Thompson S , Carusi DA , Gornbein J ((1994) ) The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology 44: , 2308–2314. |
[60] | Politis AM , Mayer LS , Passa M , Maillis A , Lyketsos CG ((2004) ) Validity and reliability of the newly translated Hellenic Neuropsychiatric Inventory (H-NPI) applied to Greek outpatients with Alzheimer’s disease: A study of disturbing behaviors among referrals to a memory clinic. Int J Geriatr Psychiatry 19: , 203–208. |
[61] | Fountoulakis KN , Tsolaki M , Chantzi H , Kazis A ((2000) ) Mini Mental State Examination (MMSE): A validation study in Greece. Am J Alzheimers Dis Other Demen 15: , 342–345. |
[62] | Cummings JL ((1997) ) The Neuropsychiatric Inventory. Neurology 48: , S10–S16. |
[63] | Faul F , Erdfelder E , Lang AG , Buchner A ((2007) ) G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39: , 175–191. |
[64] | Cohen J ((1988) ) Statistical power analysis for the behavioral sciences, 2nd ed., Erlbaum, Hillsdale, NY. |
[65] | Gaus W ((2015) ) Interpretation of statistical significance - exploratory versus confirmative testing in clinical trials, epidemiological studies, meta-analyses and toxicological screening (using ginkgo biloba as an example). Clin Exp Pharmacol 05: , doi: 10.4172/2161-1459.1000182. |
[66] | Karagiozi K , Margaritidou P , Egkiazarova M , Toumpalidou M , Makri , Marina , Tsolaki , ((2017) ) Interventions for caregivers of people with dementia in Greece. J Fam Med 4: , 1125–1134. |
[67] | Robinson A , Eccleston C , Annear M , Elliott KE , Andrews S , Stirling C , Ashby M , Donohue C , Banks S , Toye C , McInerney F ((2014) ) Who knows, who cares? Dementia knowledge among nurses, care workers, and family members of people living with dementia. J Palliat Care 30: , 158–165. |
[68] | Lüdecke D , Bien B , McKee K , Krevers B , Mestheneos E , Di Rosa M , dem Knesebeck von O , Kofahl C ((2018) ) For better or worse: Factors predicting outcomes of family care of older people over a one-year period. A six-country European study. PLoS One 13: , e0195294. |
[69] | Sahar J , Courtney M , Edwards H ((2003) ) Improvement of family carers’ knowledge, skills and attitudes in caring for older people following the implementation of a Family Carers’ Training Program in the community in Indonesia. Int J Nurs Pract 9: , 246–254. |
[70] | Abdollahpour I , Nedjat S , Salimi Y ((2018) ) Positive aspects of caregiving and caregiver burden: A study of caregivers of patients with dementia. J Geriatr Psychiatry Neurol 31: , 34–38. |
[71] | DiZazzo-Miller R , Pociask FD , Adamo DE ((2020) ) The role of confidence in family caregiving for people with dementia. Phys Occup Ther Geriatr 38: , 355–369. |
[72] | Mason R , Doherty K , Eccleston C , Winbolt M , Long M , Robinson A ((2020) ) Effect of a dementia education intervention on the confidence and attitudes of general practitioners in Australia: A pretest post-test study. BMJ Open 10: , e033218. |
[73] | Surr CA , Gates C , Irving D , Oyebode J , Smith SJ , Parveen S , Drury M , Dennison A ((2017) ) Effective dementia education and training for the health and social care workforce: A systematic review of the literature. Rev Educ Res 87: , 966–1002. |
[74] | Holton EF ((1996) ) The flawed four-level evaluation model. Hum Resour Dev Q 7: , 5–21. |
[75] | Gkioka M , Schneider J , Kruse A , Tsolaki M , Moraitou D , Teichmann B ((2020) ) Evaluation and Effectiveness of dementia staff training programs in general hospital settings: A narrative synthesis with Holton’s three-level model applied. J Alzheimers Dis 78: , 1089–1108. |
[76] | Mulyani S , Artanti E , Saifullah A ((2019) ) Knowledge and attitudes towards people with dementia among general population in Yogyakarta. In Proceedings of the Third International Conference on Sustainable Innovation 2019 - Health Science and Nursing (IcoSIHSN 2019),Mulyani S, Artani ER, Saifullah AD, eds., Atlantis Press, Paris, France. |
[77] | Banerjee S ((2010) ) Living well with dementia–development of the national dementia strategy for England. Int J Geriatr Psychiatry 25: , 917–922. |
[78] | Resciniti NV , Tang W , Tabassum M , Pearson JL , Spencer SM , Lohman MC , Ehlers DK , Al-Hasan D , Miller MC , Teixeira A , Friedman DB ((2020) ) Knowledge evaluation instruments for dementia caregiver education programs: A scoping review. Geriatr Gerontol Int 20: , 397–413. |
[79] | Schindler M , Engel S , Rupprecht R ((2012) ) The impact of perceived knowledge of dementia on caregiver burden. GeroPsych 25: , 127–134. |
[80] | Scott CB , Clay OJ , Epps F , Cothran FA , Williams IC ((2020) ) Associations of knowledge of Alzheimer’s disease and memory loss and employment status with burden in African American and Caucasian family caregivers. Dementia (London) 19: , 847–860. |
[81] | Ayalon L , Areán PA ((2004) ) Knowledge of Alzheimer’s disease in four ethnic groups of older adults. Int JGeriat Psychiatry 19: , 51–57. |




