Evaluation and Effectiveness of a Two-Day Dementia Training Program for Hospital Staff Working in an Emergency Department
Abstract
Background:
Entering the hospital via an Emergency Department (ED) is a pivotal moment in the life of People with Dementia (PwD) and often starts an avoidable downward spiral. Therefore, it is required to further educate ED staff to raise awareness of the needs of PwD. Although there are many studies about existing dementia training programs for the hospital setting, empirical evidence for the ED setting and cross-level training evaluations are lacking.
Objective:
The study aims to evaluate a two-day dementia training course for ED staff on the outcome levels of learning, individual performance, and organizational performance. Furthermore, the study examines whether the training fulfilled participants’ expectations.
Methods:
Mixed methods were used to assess data from head nurses, nursing, and administrative staff working in EDs. We conducted semi-structured interviews three weeks before (N = 18) and eight months after (N = 9) the training. Questionnaire data were assessed before the training, three months, and six months after the training (N = 44). A qualitative content analysis was conducted to analyze qualitative data; quantitative data was described descriptively.
Results:
The intervention seems to be effective on both learning and individual performance levels. However, we did not observe any changes in the organizational performance. The training program met attendees’ expectations only partly. The working environment of EDs needs to be taken more into account.
Conclusion:
Hospital staffs’ expectations of a dementia training program depend on the work area in which they operate. Results support the implementation of intervention bundles to enable sustainable cross-level changes.
INTRODUCTION
The results of a German online survey indicate a proportion of about 30% of patients over 70 years of age in the Emergency Department (ED) [1]. The literature review of Clevenger et al. [2] assumes that between 21% and 40% of older adults treated in EDs have a cognitive impairment. Furthermore, People with Dementia (PwD) have a higher rate of ED visits than people without dementia [3]. Entering the hospital via an ED is a pivotal moment in the life of PwD and often starts an avoidable downward spiral [4]. The enormous stress situation in EDs can lead to a temporary amplification of cognitive impairment, which cannot always be equally regressed in case of longer duration [5, 6].
As described in Dormann et al. [7], the ED is a functional area characterized by rapid and unpredictable changes in workflow and workload and in the individuality of each emergency situation. Working in the ED means following a symptom-oriented treatment approach, working under time-limited resources, and offering a broad treatment spectrum. Patients often tend to associate an emergency with fear and uncertainty of action. From the staff’s perspective, an emergency is no less challenging [7]. PwD have reduced capacity for resistance, and they are no longer able to protect themselves sufficiently from environmental impressions and influences [8]. Complications such as restlessness, aggression, falls, and dehydration often arise in the ED [9]. Additionally, identifying cognitive impairments in older ED patients is still insufficient [10], and dementia is often overlooked [6]. The present ED model is not designed for geriatric patients [11] and therefore does not consider the needs of PwD.
The clinical outcome of PwD, in general, is predominantly negative [12]. Surr et al. [13] collected four main reasons for adverse outcomes of hospitalized PwD: negative culture in wards and institutions, unsupportive physical environments, negative staff attitudes toward PwD, and limited staff knowledge regarding dementia [13]. In the survey by Groening et al. [1], 85% of the attending EDs endorsed specific training for staff in managing geriatric emergency patients. Despite existing dementia-specific education programs, recurring insecurities among nursing staff working in EDs in dealing with PwD were detected [14]. Researchers also noted that ED staff members should be encouraged to become aware of dementia and further educated about the needs of PwD [15]. Training staff can increase their competency in dementia care [16] and prevent complications in PwD.
The number of reviews published about dementia training programs for hospital staff in the past years reflects the importance of the issue and the growing global interest in this topic [17–20]. Most dementia training programs targeted an interprofessional/interdisciplinary group of attendees from a wide range of health setting roles [17, 18, 20]. Although some literature stresses the importance of interprofessional/interdisciplinary education and training [21], existing studies do not break down whether individual staff groups’ needs have been met in the context of their training program [18]. The same applies to the individual work areas in a hospital. We assume that employees of the same profession working in different hospital faculties might have different expectations and needs regarding a dementia training program.
Within studies evaluating dementia training programs in hospitals, specialties and disciplines of participating wards are primarily mixed. Hospital staff members who work in different types of EDs are part of several study samples. However, study samples, and thus different settings inside the hospitals, are analyzed as one population [13, 22–28]. In general, studies that included participants from EDs, differ significantly. Sample sizes ranged from N = 40 [13] to N = 517 [26], and attendees came from various health setting roles. Only one study addressed nurses solely [24]. The following brief list illustrates the wide variety of hospital work settings, besides EDs, included in the aforementioned analysis: acute wards and surgery clinics [13, 22, 24, 26–28], administrative sector, laboratories [22], day service/clinic [26, 28], geriatric ward [23, 26, 28], and intensive care unit [25], etc. To date, there has been a limited number of studies addressing dementia training, in particular for staff working in EDs [29], and a few German projects focusing on both older patients and PwD in the ED and training hospital staff [5, 30–32]. However, published results on evaluations and the effectiveness of implemented dementia training programs in the ED are scarce.
Holton’s Human Resource Development Evaluation and Research Model [33] is a comprehensive framework that integrates training evaluation and effectiveness [34]. It comprises three outcome levels: learning, i.e., desired learning outcomes achieved through the educational intervention; individual performance, i.e., changes as learning is applied in the workplace; and organizational performance as a result of changes in the individual performance. The model assumes that the outcome levels are influenced by and are a function of various factors assigned to the construct domains: ability, motivation, and environment [33]. However, as the narrative synthesis of Gkioka, Schneider et al. [20] shows, there is still a lack of adequate cross-level evaluations of dementia training programs in general.
The current project was part of a study that applied mixed methods to collect data. The questionnaire data that primarily examined outcomes on the learning level and focused on changes in attitudes toward PwD and dementia knowledge increase after attending a two-day dementia training program were published in Schneider et al. [28]. Interview data presented in this study were collected in one ED to deeper understand the results gathered with questionnaires, perform a cross-level evaluation, and eventually examine the effectiveness of the intervention. Qualitative methods enable determining reasons for the success or the failure of an intervention [35].
Aim
The study aims to examine and evaluate a two-day dementia training course for nursing and administrative staff working in German EDs, particularly on Holton’s model’s outcome levels. Primary study questions are:
1. What effect has the dementia training program “People with dementia in the general hospital” had for nursing and administrative staff working in EDs on the outcome-levels learning, individual performance, and organizational performance?
2. Did the dementia training program “People with dementia in the general hospital” meet the expectations and needs of nursing and administrative staff working in EDs? What was the role of the ED setting in particular?
MATERIALS AND METHODS
The study protocol was approved by the Ethics Committee of the Faculty of Behavioral and Cultural Studies of Heidelberg University, Germany (AZ Schn 2018 1/3).
Setting and participants
A two-day dementia training program was part of the regional action framework developed by a German hospital association to become dementia-friendly. The first action was to train nurses and administrative staff working in EDs. The hospital association includes a total of six EDs. The hospital management’s primary objectives were to raise awareness, professional handling of challenging behavior, learning alternate tools for dealing with PwD, and developing/creating and applying a medical history form to suit the needs of PwD. Dementia training sessions were obligatory for nursing and administrative staff of EDs. Not obliged to participate in the dementia training sessions were nurses who had attended the advanced training course “Emergency care”.
The training program was set up to enable up to 140 employees to attend, and approximately this number of persons was expected to participate in the questionnaire-based data collection. The details of the study participants’ recruitment of the questionnaire data collection are described in Schneider et al. [28].
Interview participants were recruited in one central ED of the hospital association, which consists of three working areas, and were randomly selected among those who were both on duty at that time and expressed their willingness to participate. We aimed to recruit 15 to 20 participants evenly from all three wards for the interview phases. Participants had to work in the central ED as a division manager, head nurse, or nursing or administrative staff. Pre-interview participants were considered potential dementia training participants. Except for division managers and head nurses, participants had to complete at least one day of the dementia training program “People with dementia in the general hospital”, to participate in the post-interviews. To be finally included in the interview phases, participants had to give their written consent and were handed a letter informing them about the study procedure.
The dementia training program
From October 2018 to December 2018, six two-day training blocks on dementia were offered and lectured by W.T. Day one provided general knowledge about dementia and promoted the understanding of the clinical picture. Day two conveyed and strengthened clinical skills. An English description of the dementia training program “People with dementia in the general hospital” [36] and the content of the training can be found in Supplementary Table 1 and Schneider et al. [28]. In order to address the ED setting, the lecturer added case studies from the ED and a group discussion with the implementation of working tasks concerning participants’ work areas were added.
Study design
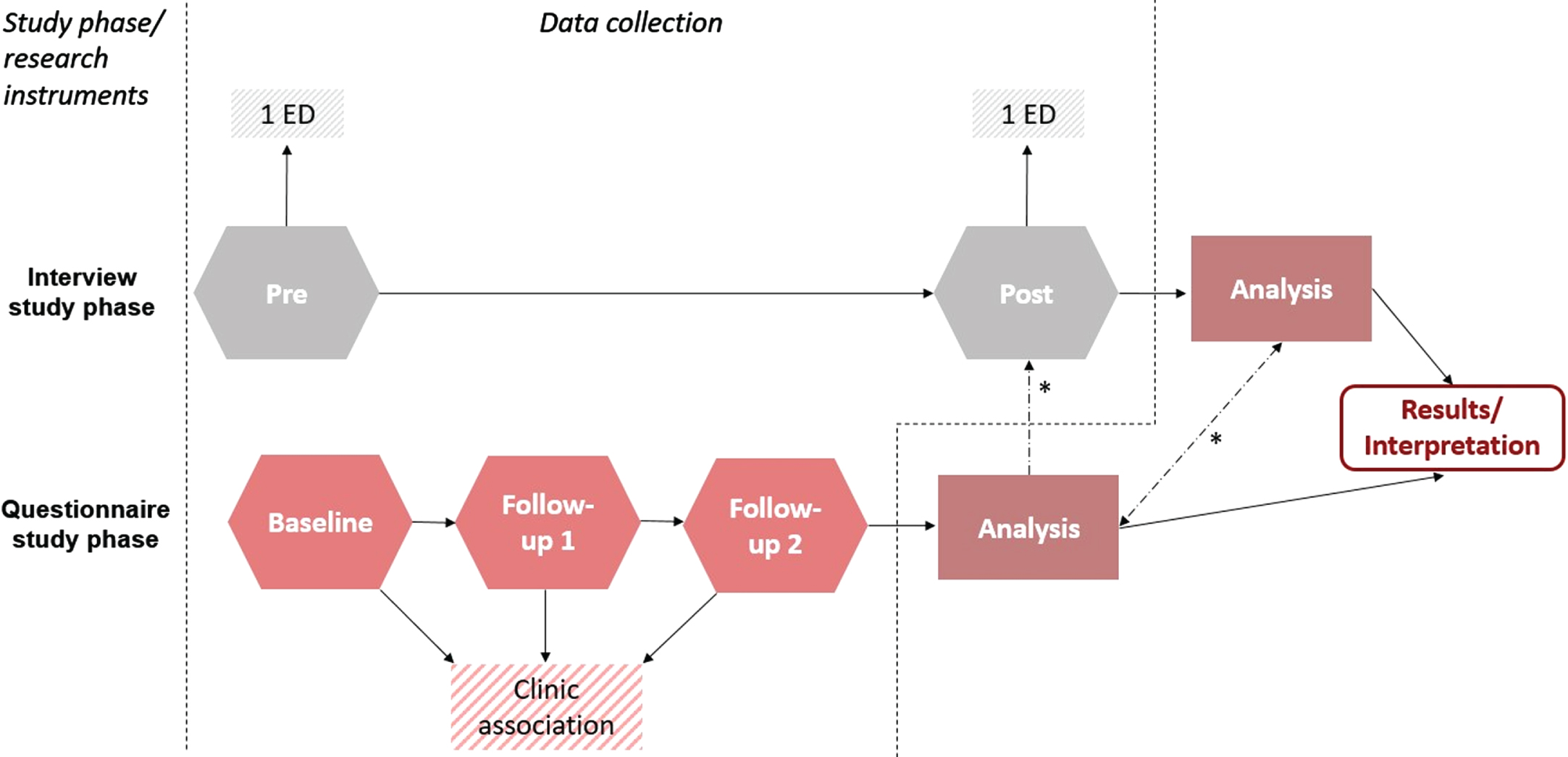
Analyzed data were part of a comprehensive mixed-methods study, including interviews and questionnaires. We used a single group repeated measures design to evaluate the two-day dementia training program on nursing and administrative ED staff. As a first step, we conducted semi-structured interviews (pre) three weeks before the first training block started. Secondly, questionnaire data were collected before the training (baseline), and follow-ups were completed three months (Follow-Up 1 (FU1)) and six months (Follow-Up 2 (FU2)) after the training. As a third step, problem-centered semi-structured interviews (post) were conducted eight months after the last training block. Figure 1 shows the study design.
Fig. 1
Study design and data collection (*shows the integration points)
Instruments
The research instruments used in the study are described according to their study phases, starting with the questionnaire study phase. Questions related to expectations, the outcome levels of Holton’s model, and the questionnaire phase’s context factors were analyzed. We asked participants baseline about their expectations in an open-ended question. The following questions were asked at FU1 and FU2, respectively. A six-point Likert scale (1 = not met; 6 = fully met) measured participants’ expectations fulfillment. Participants had the possibility to answer “no expectations”. Afterward, they could describe in an open-ended question which expectations were not met. A closed-ended question asked how often participants can apply training content in their everyday work (“frequently”, “occasionally”, “never”, and “I don’t know”). After that, they could specify what they applied in their everyday work and name reasons if they could not apply what they have learned in their everyday work (two open-ended questions). Furthermore, we asked participants if their work environment has changed for the better since the dementia training program (“yes” or “no”), and if so, in what way (comment section). A six-point Likert scale (1 = low; 6 = high) measured the overall satisfaction with their daily work. Data collected with standardized questionnaires were analyzed and published in Schneider et al. [28].
For employees and head nurses, slightly different pre- and post-interview guides, developed by J.S., were used in the interview study phase. The interview guides translated into English are listed in the Supplementary Material. The basis for the pre-interview guides’ questionnaire development was a literature search and the Holton model [33]—planned duration was 15 to 20 min. Post-interviews were problem-centered semi-structured interviews (planned duration was 20 min). Interview guides and data collection followed the description of Schmidt-Grunert [37]. Relevant examined results of the questionnaire phase were incorporated in the interview guide to better understand these results. The interview guides were discussed with co-authors (A.K. and B.T.), qualitative research experts, a researcher with experience of working in an ED, and modified step by step.
Data collection
Participants of the questionnaire study phase had to sign a declaration of consent and were then asked to complete the baseline questionnaires they received from the lecturer before the training. In addition, FU1 and FU2 questionnaires with further documents were sent by mail. Schneider et al. [28] provide a more detailed description of the data collection.
Before the pre-interview started, participants received an information letter and had to sign a declaration of consent, were asked about some demographic data, and informed about the materials used in the interview procedure (interview guide, recording device). The interviews were carried out during the regular operation of the ward in an available office room. However, we expected disturbances to occur in the course of the study. Therefore, the procedure of the post-interviews differed in the following aspects. One week before the post-interviews started, an information letter was sent to the hospital to inform the staff about the upcoming interviews. The interview participants received a questionnaire about demographic data.
Data analysis
Statistical analyses of the quantitative data were carried out with SPSS V25.0 (IBM Corp, Armonk, New York). Only data from participants stating to work in areas of EDs were analyzed. For descriptive statistics, means and standard deviations were calculated for continuous and approximately normally distributed variables. Also, we calculated absolute and relative frequencies for the descriptive analysis of the categorical variables.
Interviews were transcribed in MAXQDA Analytics Pro 2018 (Release 18.2.3) (J.M.) following transcription rules by Rädiker and Kuckartz [38]. Transcripts were rechecked and anonymized (J.S.). To explore the interview material, text sections relevant to the questions asked were paraphrased (J.M.). A qualitative content analysis, according to Mayring [39], was conducted to analyze and interpret interviews and open-ended questions in MAXQDA Analytics Pro 2020 (Release 20.2.2) (J.S.). The inductive category building and the formation of deductive categories followed the process models (p. 86, p. 98) of Mayring [39].
In the first coding pass, one researcher coded all answers to relevant questions (J.S.). After that, several data material passes were necessary to develop the coding scheme (category definition, abstraction level, category system). Another researcher (S.R.) coded 50% to 60% of the data material using the coding scheme to estimate the reliability. Coder one was available for queries. Cohen’s Kappa calculated with MAXQDA Analytics Pro 2020 (Release 20.2.2) showed a moderate to a substantial agreement [40] and ranged between κ=0.55 and κ=0.74. Non-compliant segments and disagreements with categories were discussed and adjusted if necessary (J.S. & S.R.). If changes were made, the data material was revised. In a final pass, the entire post-interviews were examined for specific thematic aspects which have not yet appeared.
RESULTS
Sample characteristics
Although attendance was mandatory, only 65 of the expected 140 persons registered for the dementia training program and were invited to participate in the questionnaire study phase. Overall, 60 employees gave their consent, participated in the study, and completed the baseline measures (return rates are listed in Schneider et al. [28]). Of those, N = 44 reported working in areas of EDs in five clinics. Core characteristics of the sample at each point in time are reported in Supplementary Table 2. Summarizing the main points, almost all participants of the baseline sample were female (n = 43, 97.7%), and the majority was under 35 years of age (n = 26, 59.1%). Half of the participants had at least ten years (n = 24, 54.5%) of school education. The participants were mainly registered nurses (n = 28, 63.6%) and medical assistants (n = 13, 29.5%). Only three participants (6.8%) had received prior training focusing on dementia, ranging from two to five hours’ duration.
For the pre-interview phase, we were able to recruit 18 study participants. The average duration of the interviews was 18 : 31 minutes. The majority of the participants were female (n = 16, 88.9%) and mainly registered nurses (n = 12, 66.8%). Two leading head nurses (11.2%) agreed to interviews. Participants came from all three work areas (area one n = 8 (44.6%), area two n = 4 (22.2%), area three n = 4 (22.2%)). In the post-interview phase, nine staff members gave their consent to participate in this study phase, and the average duration of the interviews was 24 : 09 min. The majority of participants were again female (n = 8, 88.9%) and mainly registered nurses (n = 6, 66.6%). Once again, two leading head nurses (22.2%) agreed to be interviewed. Participants came from all three work areas (area one n = 3 (33.3%), area two n = 2 (22.2%), area three n = 2 (22.2%)). While all staff members attended at least one day of the dementia training program, both leading head nurses participating in this study phase did not attend the training program.
Themes of interest
Results are presented in narrative form in the weaving approach theme-by-theme in the order in which the study phases took place [41]. Therefore, we analyzed the results concerning six themes of interest.
Theme 1: Expectations and potential for development of the training
Expectations before the dementia training
At least one-third of the pre-interview participants were unlikely to attend the dementia training sessions. When asked about expectations of the training and participation was not guaranteed, the question was asked hypothetically. The majority expected input for practice, particularly to improve handling PwD concerning different aspects (e.g., agitated, aggressive patients), communication with PwD, and the practical implication of suggestions and tips. Furthermore, participants hoped to gain theoretical knowledge, and specific topics regarding dementia were demanded. Also, the hospital staff members indicated that, besides raising awareness for this patient group, they expected changes in the organizational culture (living the changes, involvement of physicians), processes (discharge management), and resources (better staff-patient ratio, changed physical environment) accompanied with the dementia training.
The baseline questionnaire (n = 35 answered) results were less detailed and varied to a lesser extent than in the pre-interviews, but the characteristics were similar. Most participants expected input for practice (to improve and facilitate handling PwD, practical implication of knowledge and tips). This expectation was, in some cases, mentioned in connection with the working environment ED. Theoretical input (increased knowledge, better understanding of the disease, desired topics) was also expected by many. Another theme that emerged was becoming aware of PwD, including a better understanding or being more patient. A few participants had no expectations.
Expectation fulfillment
Participants ranged their expectation fulfilments regarding the dementia training program at FU1 and FU2 (n = 24 respectively) as “somewhat fulfilled” (FU1: MD = 4.44, SD = 1.34 (minimum = 1, maximum = 6); FU2: MD = 4.27, SD = 1.35 (minimum = 2, maximum = 6)). At FU1 n = 6 (25.0%) and at FU2 n = 2 (8.3%) answered not to have had expectations.
Participants explained their unfulfilled expectations in an open-ended question at FU1 n = 9 and at FU2 n = 7. Four main aspects emerged. Participants felt that theoretical training content was not sufficiently linked with practical implementation possibilities for the ED. Overall, they wished for more practical implementation possibilities for the ED and reported that recommendations and tips could not be implemented in their working practice. Also, hospital staff members felt a need for a more lively teaching of the learning contents by the lecturer. Not as a primary aspect identified but undoubtedly significant, the lack of resources (unfavorable spatiality, lack of staff and time) was mentioned as a barrier to implement training content.
The training did not meet the expectations of one head nurse asked during the post-interviews, whereas the other had no expectations due to missing knowledge about the training.
Dementia training program: potential for improvement
We assumed that the aspects mentioned above impact what has been learned in the working practice and changes in individual performance and can be seen as potential future improvements of the training program. Therefore, in a second step, the answers were phrased as statements and added to the post-interview guide. Attendees were asked to agree or disagree with each of the four statements and could explain their answers. Answers were categorized in deductive categories “fully agree”, “partly agree”, and “disagree”. Table 1 summarizes the results.
Table 1
Four main aspects of unfulfilled dementia training expectations and agreement or disagreement with post-interview participants statements
| Unfulfilled expectations (open-ended questions FU1 and FU2) | Agreement or disagreement (post-interviews) |
| 1. Theoretical training content was not sufficiently linked with practical implementation possibilities for the ED. | Almost all fully agreed |
| 2. Not enough practical implementation possibilities for the ED were discussed. | Almost all fully agreed |
| 3. Recommendations and tips could not be implemented in their working practice. | More than half fully agreed |
| 4. Learning content was not taught lively enough by the lecturer. | Roughly two-third fully agreed |
Interviewed persons commented on aspects one and two that “. . . they could have left out the theory entirely and just worked practically. Effectively using case studies, for example.” (Post-Interview Participant (PostIP)-06) or “. . . that one collects more empirical values (I: Yes.) from the same areas, . . . . Then perhaps some emergency department would have to be consulted where this works better or perhaps even optimally, and these examples are presented. . . ” (PostIP-01).
Persons who only agreed partly on aspect three said that some things could not be implemented due to hygienic reasons or staff or time shortage. One person believes that “. . . certain things are an inner attitude to how I deal with a person.” (PostIP-08).
Perception and answers regarding the fourth aspect varied; participants also disagreed. Comments ranged from the dementia training program was entertaining, not boring or unrealistic, to the training content was intangible and not practice-oriented, and critical questions were not answered.
Overall, highlighted were the interactive activities and the associated exchange with colleagues. Participants desired more interactive activities, as well as experience reports from colleagues and examples from the ED.
Theme 2: The role of the setting ED
After screening the results of the questionnaire study phase, the authors noticed that the setting ED played a significant role in fulfilling expectations and changes in the individual performance. Therefore, differences between EDs and regular wards from the perspective of the post-interview participants and their relevance for dementia training programs were explored.
Participants believe the most significant difference between EDs and regular wards is the working environment. Furthermore, the characteristic services and tasks in the ED field were mentioned as one of the main differences.
An occurred theme addressing both the working environment and the tasks was the working activity itself—containing fast work processes combined with initial assessment and prioritization of patients, interpretation of diagnostic measures, and holistic view of the patient. In addition to the symptom-oriented approach and diagnostics, less direct patient care and more treatment care for nursing staff, and administrative tasks for administrative staff are also typical for this work field. The restless environment and procedures—patient moving from room to room for diagnostics, general hectic—were identified as another theme. A post-interview participant said:
. . . somehow, you have to do ten things simultaneously, and you have to coordinate it, and you have to be able to figure out what or who has priority, what has priority now, what I have to do first and what not. And I have to lower my sights and say, ‘He has to wait now, and it’s his turn now because he’s important now.’. . . I also find, in regular wards,/ First, it’s somehow all generally calmer. (PostIP-02)
Another critical issue, which can be classified under the working environment of an ED, is the shorter length of stay of patients. The contact between patients and staff is less profound, they do not get to know them properly, and various staff members have frequent contact with a patient. Other differences were the equipment and the spatial design of an ED (e.g., they cannot provide food, narrow hospital beds, room design/construction), the predictability (no regulated ward routine, change of workload/patient occurrence, every day is different), and the patient-staff ratio (better ratio in the ED, but the answers varied). One person addressed the competencies of the ED staff members, which are higher qualified.
Participants stated that dementia training programs addressing the ED staff must be more specialized for the setting ED in general. Procedures, impulses, and approaches taught in the dementia training program must be applicable in the hectic and stressful environment and situations of the ED. Furthermore, participants pointed out that dementia is one of many themes, the ED staff has to meet many requirements and that it is an important issue also for other professions, e.g., physicians. A represented opinion was that ED staff needs less intensive dementia training because they only have short contact with patients and cannot change anything.
To enable changes, other modifications are needed, for example, adjusting the spatial design to make PwD feel more comfortable and prolonging the duration of treatment, but that would not be longer correspond with the current ED model. However, sometimes participants had difficulties describing the relevance of the differences for dementia training programs.
Theme 3: Learning outcomes
Outcomes on the learning level collected with (standardized) questionnaires are published in Schneider et al. [28]. Post-interview participants stressed that they gained better theoretical knowledge (causes, prevention, treatment, and forms of dementia), while some participants’ interest arose, presumably because they recognized the relevance of the topic. However, two persons considered the training to be a repetition, while two had no learning gain. Indeed, interviews revealed still sporadic knowledge gaps and attitudes toward PwD with a rather negative tendency.
Theme 4: Individual performance
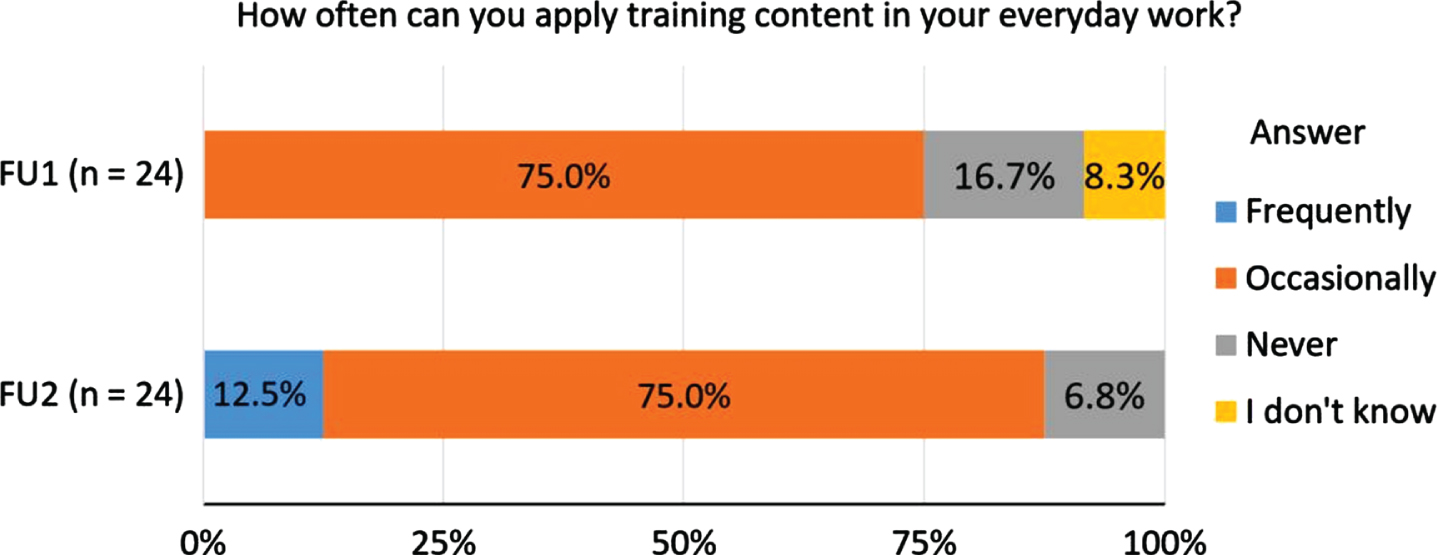
We summarized answers to how often participants can apply training content in their everyday work at FU1 and FU2 in Fig. 2. Again, a slight increase in the frequency of use is noted over time.
Fig. 2
Distribution of responses to FU1 and FU2. Possible responses were “frequently”, “occasionally”, “never”, and “I don’t know”.
Participants (n = 18) specified at FU1 to apply in their everyday work especially communication/techniques, including validation, general communication techniques—involvement of relatives; relatives can stay with the patient during the procedures/hospital stay, stronger cooperation with, and involvement of relatives; and occupation/occupational offers—participants try to occupy PwD especially their hands or to try to distract them with occupational material. They also stated to have a greater understanding of PwD and try to create a quiet environment. Each theme, as mentioned earlier, also occurred at FU2 (n = 15), although less frequent in each case, except for having a greater understanding of PwD.
At FU1 main reasons for participants (n = 17) to not apply what they have learned in their everyday work were resources, predominantly lack of time, staff shortage, unsuitable spatiality, and lack of material. Furthermore, specific characteristics of the ED such as short patient length of stay, patient contact, and high patient occurrence with urgent cases prevented implementation. Some also determined a limited implementability in the ED or found the dementia training unsuitable for their work field. The results for FU2 (n = 11) give a similar picture. However, staff shortage and short patient length of stay were not mentioned as a reason anymore.
Results of the questionnaires regarding the individual performance are not or no longer reflected in the post-interviews. Asking participants directly to what extent the learned material has influenced their work and if they changed something in how they deal with and behave around PwD, they answered that nothing has changed after attending the dementia training program. Nevertheless, interviews revealed that some have changed their communication and are using occupation activities after all. One person also tried to implement a tool but failed because colleagues did not support the idea, and the tool was found as not usable in the ED. Besides, in the interviews, the potential for improvement was still discovered, e.g., in the communication, restricting measures, and the will to change something.
Team-level
When we asked post-interview participants if the team deals with PwD in a more sensitive and understanding way since the training, most answered that they could not or did not wish to judge their team members. The response characteristics of recognized positive changes or no changes were similar. Some answered that they recognized positive changes in individual persons. While staff members were satisfied with how the topic of dementia is handled on their ward, one leading head nurse still sees potential for improvement, with the current high workload as a barrier.
Theme 5: Organizational performance and environmental changes
At FU1, more than three-quarters of 23 participants (n = 20, 87.0%) and at FU2, almost all 24 participants (n = 23, 95.8%) answered their work environment has not improved after staff members attended the dementia training program. However, three persons (13.0%) at FU1 and one (4.2%) at FU2 stated positive changes. Answers in the comment section showed predominantly changes on the team level or showed the dependence of changes concerning this topic on colleagues.
The questionnaires of the ED staff did not reveal any changes that could be assigned to theme five. During the post-interviews, we again asked participants about ward changes. Also, we provided examples of possible design, structural, and process changes known from other dementia training program evaluations or recommended in the literature: adaption of the medical history sheet or triage system, installation of orientation signage, development of a treatment pathway for PwD in the ED, or introduction of regular case conferences. Participants recognized no changes in the given examples and the organizational performance in general. One participant tried to encourage change:
(.) To be honest, I brought this up in the staff meeting and asked whether it would be possible to hang signs on the toilet doors because it is only a white door. And to be honest, I have already written an order to the janitors. . . So I really already had the incentive to do that, but it has not been implemented yet, and that was certainly half a year ago. (.) (I: Too bad.) Yes. (.) This would also be a great orientation for patients who do not have dementia (laughs). (PostIP-02)
Answers to the question of why no change occurred ranged from “there is no great need for action”, over “training content could not be applied” and “the fact that it was a mandatory training during an already burdening period”, to “I do not know what was discussed in the training courses, maybe slow processes in the hospital” and simply “I don’t know”.
Although no changes on the organizational level occurred, some participants still saw some need for action. They wished for more resources—better staffing ratio, a person responsible for PwD, and environmental changes – a room for PwD, color design, and orientation signages. In the latter aspect, participants feel little decision power and believe environmental changes need time, except for signage changes. Besides, dementia training for physicians and staff members who could not attend is necessary. Participants wished for adaptation of the patient admission process in order to have more time for patients. However, because of the short stay of the patients and the presence of relatives and emergency service, staff members did not see a need for action in the admission area of the ED. Participants also expressed general doubts about whether changes in the ED would make a difference and on focusing on the patient group PwD.
Theme 6: Context information
Communication and cooperation between professional groups and with leading head nurses and management staff (pre-interviews)
The answers of this sub-item were categorized in the deductive categories “good”, “rather good”, “rather poor”, and “poor”. Although all categories were assigned, communication and cooperation between professionals were predominantly stated as good. Some praised the team spirit and cooperation with the (specialist) physicians, the used data software, and general communication. Some others complained about the aspects mentioned above or indicated that hectic, high workload, and part-time employment lead to loss of information.
Even though all categories were assigned, almost two-thirds of the participants rated communication and cooperation with leading head nurses as good and were mostly satisfied. The most critical point was the transfer of information. Participants criticized that the higher levels of management remain distant to the staff’s daily practical work.
Satisfaction with their daily work (FU1 and FU2 questionnaires)
At FU1 n = 22 (MD = 4.50, SD = 1.06, minimum = 2, maximum = 6) and at FU2 n = 24 (MD = 4.37, SD = 1.14, minimum = 2, maximum = 6) participants ranged the overall satisfaction with their daily work as “rather high”.
Support by colleagues and leading head nurses (post-interviews)
The question regarding collegial support and support of leading head nurses in implementing training content had to be asked more general. Deductive categories in support of leading head nurses and colleagues were “full”, “sufficient”, “expandable”, and “no support at all”. Overall, participants felt fully or sufficiently supported by leading head nurses and colleagues. The majority answered to be motivated at work. Interestingly, at the same time, answers could be classified as resignation. Some are not frustrated anymore about general conditions and savings. They accepted the fact that not everything optimal for patients and staff can be implemented. Participants also noted that suggestions are fine as long as they do not cost money and staff resources. When leading head nurses were asked to what extent they support staff in implementing dementia training content, they answered to be open for and wishing for suggestions, but it depends on what it is. It became clear that dementia is not the highest priority and is also considered particularly tricky. Again, the lack of information regarding the dementia training program was a barrier.
DISCUSSION
The intervention seems to be effective on both learning and individual performance levels whereby the results’ strength depends on the measuring instrument. We did not observe any changes at the organizational performance level. The evaluated training program met attendees’ expectations partly. Dementia training programs addressing the ED staff need to take their working environment more into account.
The dementia training program conveyed at first sight mainly theoretical knowledge about dementia. Results of standardized tests support these findings, although not all results were statistically significant [28]. Interview data still detected sporadic knowledge gaps. Furthermore, the training had a positive effect on the attitudes of hospital staff toward PwD measured with the German version of the Dementia Attitudes Scale [28]. However, post-interview data revealed the use of language that can be labeled as negative toward PwD. These findings support the assumption that regular in-service training is essential to maintain awareness and permanently close knowledge gaps or prejudices about PwD [5, 42]. In-service dementia experts could be used as a resource by other staff [18] by conducting regular short training sessions or case discussions. Continuous action is necessary [5] to support a sustainable and establish a positive attitude toward PwD. Persuasion and incentives must be used complementary [43].
Results regarding the individual performance show that the input for practice was also taught, and some participants seem to have changed their individual performance. Nevertheless, the results depended on the measurement instrument. Answers in the post-interviews were more reserved, and changes were detected only occasionally. Sampson et al. [16] had similar experiences. Whether participants actually changed their individual performance is not known. Observations could be helpful to examine changes [16]. These findings support the use of mixed methods in evaluating dementia training programs and the added value of qualitative data [35]. Lack of resources, e.g., time and staff shortage, were seen as barriers that prevented individual performance change. Those barriers are already known in the literature [25, 42] but cannot be solved by dementia training programs alone [20]. Other barriers specific to the ED could be solved by rethinking the current ED model. Adams and Gerson [11] make a few suggestions, e.g., making the patient known or creating a supportive environment.
The training does not seem to have impacted the organizational performance concerning environmental, structural, and process changes. The influence of participants might not be strong enough to initiate changes at this level. A top-down strategy needs to be followed to reach positive cross-level results [5]. Medical and nursing managers, the nursing directorate, and hospital management must be involved in the innovation process [44]. These findings show that besides positive care and ward culture, it requires a positive organizational culture to enable change [12]. Therefore, structural and process changes at the organizational level are needed to facilitate sustainable changes [21]. Consequently, results demonstrate that dementia training programs should be part of an evidence-based intervention bundle [28].
Even if not all influencing factors of Holton’s model [33] were assessed and could be discussed, consideration of some may explain the effectiveness of the intervention, reveal further barriers, and guide future dementia training programs. Reviewing factors outside the training, lacking the motivation to improve work through learning, influencing learning, and individual performance was detected. Study participants also criticized the intervention as mandatory training. Giving staff the choice to attend or not increases their motivation to learn and improves learning [45]. After attending the training, some participants still saw no need for action and were satisfied with how dementia was handled in their working place or thought nothing could be changed in the ED for PwD. Therefore, the transfer of lessons learned becomes unlikely. The current understanding of an ED [11] can contribute to the transfer difficulty. However, to enable changes, processes in the ED must be adapted to the PwD’s care needs [31]. To underline the relevance, we must anchor aims and principles of action in dealing with PwD in the corporate mission statement [5] and live out in everyday work. Results demonstrated overall a supportive environment concerning colleagues and head nurses. However, these supporting conditions do not seem to have been used. Leading head nurses and physicians did not undergo the training “People with dementia in the general hospital”; dementia is one topic of many and is considered problematic. Besides the supportive conditions, hospital employees reported higher levels of workload, and some attendees perceived the training as an additional burden to their busy work. The goals pursued by head nurses and hospital management seemed not to be equal. An action plan and a precise aim are inevitable for a meaningful and sustainable educational intervention [5].
The training program partially met attendees’ expectations, which may have negatively impacted several factors such as learning, individual performance, and training motivation [45]. Dementia training programs that aim to fulfill the needs of participants’ expectations usually face multiple challenges. As it is known, German hospital staff expects concrete, practical pieces of advice [46]. However, every person with dementia and situation is different [47], so a structured algorithm based on the if-then logic for dealing with PwD can hardly be taught in these training courses. Thinking about the stressful and hectic environment of an ED and the individuality of each emergency situation [7], a severe theory-practice conflict is almost to be expected [48]. This conflict may also be reflected in the individual ability to engage with the content covered in the training and adapt it to the situation in the ED. One fundamental issue of the training, following Kitwood, was to develop an understanding for the PwD and to adopt the attitude of the staff toward them, although not all participants may have felt the need to do so. In contrast, the treatment of patients in the ED seems to be viewed primarily in somatic terms, which is understandable and partly due to the general conditions. Supportive conditions are needed to sustainably change the individual performance (e.g., dementia experts) [18, 20]. Furthermore, we must consider other practice-oriented forms of training such as bedside training for the ED.
Further desired changes regarding the organizational culture, processes, and resources accompanied by dementia training do not seem to be fulfilled. In general, increasing numbers of patients and staff shortages pose a significant challenge in EDs [5]. These unmet expectations can be transferred to the training but cannot be resolved by the training program. Also, the relevance of the topic of dementia in the ED was questioned by some participants, and a notable portion of training content was found as not usable in the ED. Participants experienced the training not enough tailored to the working activities and environment, and not all of them were able to identify themselves with content and lecturer. In general, specific dementia training material for the ED is lacking and needs to be developed. Also, as we know from the literature, the lecturer should have practical experience in the target group’s work area [5] and function as a role model for good practice [18, 44].
The hypothesis that employees of the same profession working in different hospital faculties might have different expectations and needs regarding a dementia training program can be proven. Furthermore, the administration participants mentioned that the training was too extensive and not applicable in their job. Therefore, whether interprofessional training is beneficial depends on the aim of the dementia training program. However, further research and subgroup analyses are needed to make a good statement.
Limitations
The current study has some limitations. For the questionnaire phase, a larger sample size was expected; therefore, the actual number of attendees in this phase is small. Also, the desired number of interview participants in both phases could not be reached. Participants of the interview study phase came from one central ED and might represent only one perspective. In general, the study sample is not representative of the range of professions working in a hospital. Selective dropouts for the questionnaire phase must also be considered because a remarkable proportion of attendees did not return their questionnaires. This fact may impact the generalizability of the study results. Moreover, we should also take into account social desirability. Although interview participants were encouraged to talk freely, it is unknown if they dared to express their actual thoughts and opinions. In addition, the training was delivered by one person without a nursing background. We do not know whether the impact of the training program changes when other persons deliver the training and the environment changes. Lastly, we did not observe the direct impact of the dementia training program on the patient outcome. In future studies, observational studies should examine changes in individual performance and organizational outcomes, as well as the impact on patient outcomes.
Conclusion
While delivery and learning methods of the implemented training program have the potential for improvement in the ED setting, this is a general issue. Suitable materials for hospital staff working in EDs and empirical value are necessary. Furthermore, a needs analysis or focus group interviews before the training delivery could ensure that training is more tailored to the target audience. Using Holton’s model helped to understand factors influencing the outcomes and, therefore, to understand the actual effectiveness of the intervention. Future studies examining dementia training programs must expand their evaluation focus to better understand the mode of action of their intervention. This includes the impact on PwD. Additionally, the findings strongly support the usage of mixed methods and the implementation of evidence-based intervention bundles.
ACKNOWLEDGMENTS
The authors thank all participating hospital staff, the nursing directorate, and their team involved in this study for their cooperation. The first author was reimbursed for travel costs by the clinic association for data collection, and there are no further financial conflicts to report. Furthermore, the authors thank the members of the Graduate Program “People with Dementia in General Hospitals” for their valuable recommendations, and, in particular, Sebastian Ritzi (S.R.), who supported the analysis of the qualitative data and enriched this work with his expertise.
J.S. is a member of the interdisciplinary Graduate Program “People with Dementia in General Hospitals”, located at the Network Aging Research (NAR), Heidelberg University, Germany, and received a Doctoral Fellowship funded by the Robert Bosch Foundation, Stuttgart, Germany.
The entire project “People with dementia in the general hospital” of the German Alzheimer Association, Bavaria, which includes the dementia training program of the same name, is funded by the “Bavarian State Ministry of Health and Care”. The lecturer of the dementia training program and a member of the “Alzheimer’s Society of Bavaria” W.T. had no influence in the data collection and/or analysis to avoid conflict of interest and report independent research.
Furthermore, we explicitly point out that this study is not commissioned work.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/21-0505r1).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-210505.
REFERENCES
[1] | Groening M , Grossmann F , Hilmer T , Singler K , Somasundaram R , Wilke P ((2017) ) Ältere Notfallpatienten: Blickschärfung notwendig. Dtsch Arztebl 114: , A512–A515. |
[2] | Clevenger CK , Chu TA , Yang Z , Hepburn KW ((2012) ) Clinical care ofpersons with dementia in the emergency department: A review of theliterature and agenda for research. J Am Geriatr Soc 60: , 1742–1748. |
[3] | Hunt LJ , Coombs LA , Stephens CE ((2018) ) Emergency department use bycommunity-dwelling individuals with dementia in the United States:An integrative review. J Gerontol Nurs 44: , 23–30. |
[4] | Temple BA , Krishnan P , O’Connell B , Grant LG , Demczuk L ((2017) ) Emergency department interventions for persons with dementiapresenting with ambulatory care-sensitive conditions: A scopingreview protocol. JBI Database System Rev Implement Rep 15: , 196–201. |
[5] | Kirchen-Peters S , Krupp E (2019) Praxisleitfaden zum Aufbau demenzsensibler Krankenhäuser, Stuttgart. |
[6] | Holthoff-Detto V ((2019) ) Ältere Menschen und Menschen mit Demenz in der Notaufnahme: Die Rolle des Alters. In: Erfahrungsbericht INA-Dem: Konzept- und Prozessentwicklung in einer interdisziplinären Notaufnahme zur schonenden Behandlung von Menschen mit Demenz: Ein Projekt aus dem Förderprogramm “Menschen mit Demenz im Akutkrankenhaus” der Robert Bosch Stiftung, Holthoff Detto V, ed. Berlin, pp. 10–15. |
[7] | Dormann P , Wedler K , Machner M , Fuchs A ((2017) ) Notfallpflege –was ist das eigentlich? intensiv 25: , 293–298. |
[8] | Kruse A ((2017) ) Lebensphase hohes Alter: Verletzlichkeit und Reife, Springer, Berlin. |
[9] | Amadori K ((2019) ) Aller Anfang ist schwer: Demenzsensible (Not-)Aufnahme und Anamnese. In: Das demenzsensible Krankenhaus: Grundlagen und Praxis einer patientenorientierten Betreuung und Versorgung, Horneber M, üllen R, Hübner J, eds., 1. 1053 edition, Kohlhammer, Stuttgart, pp. 111–132. |
[10] | Parke B , Beaith A , Slater L , Clarke AM ((2011) ) Contextual factorsinfluencing success or failure of emergency department interventionsfor cognitively impaired older people: A scoping and integrativereview. J Adv Nurs 67: , 1426–1448. |
[11] | Adams JG , Gerson LW ((2003) ) A new model for emergency care of geriatric patients. Acad Emerg Med 10: , 271–274. |
[12] | Dewing J , Dijk S ((2016) ) What is the current state of care for older people with dementia in general hospitals? A literature review. Dementia (London) 15: , 106–124. |
[13] | Surr CA , Smith SJ , Crossland J , Robins J ((2016) ) Impact of a person-centred dementia care training programme on hospital staff attitudes, role efficacy and perceptions of caring for people with dementia: A repeated measures study. Int J Nurs Stud 53: , 144–151. |
[14] | Reimer A-C ((2019) ) Haltung und Handlungsfähigkeiten von Pflegenden fördern. In: Erfahrungsbericht INA-Dem: Konzept- und Prozessentwicklung in einer interdisziplinären Notaufnahme zur schonenden Behandlung von Menschen mit Demenz: Ein Projekt aus dem Förderprogramm “Menschen mit Demenz im Akutkrankenhaus” der Robert Bosch Stiftung, Holthoff-Detto V, ed. Berlin, pp. 44–51. |
[15] | Watkins S , Murphy F , Kennedy C , Dewar B , Graham M ((2019) ) Caring for an older person with dementia in the emergency department (ED): An appreciative inquiry exploring family member and ED nurse experiences. J Clin Nurs 28: , 2801–2812. |
[16] | Sampson EL , Vickerstaff V , Lietz S , Orrell M ((2017) ) Improving thecare of people with dementia in general hospitals: Evaluation of awhole-system train-the-trainer model. Int Psychogeriatr 29: , 605–614. |
[17] | Scerri A , Innes A , Scerri C ((2017) ) Dementia training programmes for staff working in general hospital settings - a systematic review of the literature. Aging Ment Health 21: , 783–796. |
[18] | Surr CA , Gates C ((2017) ) What works in delivering dementia education or training to hospital staff? A critical synthesis of the evidence. Int J Nurs Stud 75: , 172–188. |
[19] | Abley C , Dickinson C , Andrews Z , Prato L , Lindley L , Robinson L ((2019) ) Training interventions to improve general hospital care forolder people with cognitive impairment: Systematic review. Br JPsychiatry 214: , 201–212. |
[20] | Gkioka M , Schneider J , Kruse A , Tsolaki M , Moraitou D , Teichmann B ((2020) ) Evaluation and effectiveness of dementia staff trainingprograms in general hospital settings: A narrative synthesis withHolton’s Three-Level Model applied. J Alzheimers Dis 78: , 1089–1108. |
[21] | Brody AA , Galvin JE ((2013) ) A review of interprofessional dissemination and education interventions for recognizing and managing dementia. Gerontol Geriatr Educ 34: , 225–256. |
[22] | Gkioka M , Teichmann B , Moraitou D , Papagiannopoulos S , Tsolaki M ((2020) ) Effects of a person centered dementia training program in Greek hospital staff-implementation and evaluation. Brain Sci 10: , 976. |
[23] | Robinson J , Longden J , Murphy J ((2015) ) Transforming dementia care in an NHS Trust. Nurs Older People 27: , 18–23. |
[24] | Ellis J ((2008) ) Carer-driven dementia education for professionals. Nurs Older People 20: , 35–39. |
[25] | Schindel Martin L , Gillies L , Coker E , Pizzacalla A , Montemuro M , Suva G , McLelland V ((2016) ) An education intervention to enhancestaff self-efficacy to provide dementia care in an acute carehospital in Canada: A nonrandomized controlled study. Am JAlzheimers Dis Other Demen 31: , 664–677. |
[26] | Elvish R , Burrow S , Cawley R , Harney K , Pilling M , Gregory J , Keady J ((2018) ) ‘Getting to Know Me’: The second phase roll-out of a staff training programme for supporting people with dementia in general hospitals. Dementia (London) 17: , 96–109. |
[27] | Elvish R , Burrow S , Cawley R , Harney K , Graham P , Pilling M , Gregory J , Roach P , Fossey J , Keady J ((2014) ) ‘Getting to Know Me’: Thedevelopment and evaluation of a training programme for enhancingskills in the care of people with dementia in general hospitalsettings. Aging Ment Health 18: , 481–488. |
[28] | Schneider J , Schönstein A , Teschauer W , Kruse A , Teichmann B ((2020) ) Hospital staff’s attitudes toward and knowledge about dementia before and after a two-day dementia training program. J Alzheimers Dis 77: , 355–365. |
[29] | Ouchi K , Wu M , Medairos R , Grudzen CR , Balsells H , Marcus D , Whitson M , Ahmad D , Duprey K , Mancherje N , Bloch H , Jaffrey F , Liberman T ((2014) ) Initiating palliative care consults for advanced dementia patients in the emergency department. J Palliat Med 17: , 346–350. |
[30] | Sniatecki S , Dudek D ((2019) ) Segregative Versorgung von kognitiv eingeschränkten Menschen in der Orthopädie/Unfallchirurgie des Florence-Nightingale-Krankenhauses in Düsseldorf. In Menschen mit Demenz im Allgemeinkrankenhaus: Innovative Konzepte für eine multiprofessionelle Betreuung und Versorgung, Löhr M, Meißnest B, Volmar B, eds., 1. edition. pp. 47–58. |
[31] | Holthoff-Detto V , ed. ((2019) ) Erfahrungsbericht INA-Dem: Konzept- und Prozessentwicklung in einer interdisziplinären Notaufnahme zur schonenden Behandlung von Menschen mit Demenz: Ein Projekt aus dem Förderprogramm “Menschen mit Demenz im Akutkrankenhaus” der Robert Bosch Stiftung, Berlin. |
[32] | (2015) Die Alters Unit - Derältere Patient in der Notaufnahme, Klinikum Frankfurt Oder, https://www.klinikumffo.de/presse/pressemeldungen/news/article/die-alters-unit-der-aeltere-patient-in-der-notaufnahme.html, Last updated July 2, 2015, Accessed December 28, 2020. |
[33] | Holton EF ((2005) ) Holton’s Evaluation Model: new evidence and construct elaborations. Adv Dev Hum Resour 7: , 37–54. |
[34] | Alvarez K , Salas E , Garofano CM ((2004) ) An integrated model of training evaluation and effectiveness. Hum Resour Dev Rev 3: , 385–416. |
[35] | Kelle U ((2018) ) “Mixed Methods“ in der Evaluationsforschung –mit den Möglichkeiten und Beschränkungen quantitativer und qualitativer Methoden arbeiten. Z Eval 17: , 25–52. |
[36] | Fortbildungsprogramm. Kliniken und Rehabilitationseinrichtungen, Deutsche Alzheimer Gesellschaft Landesver- band Bayern e. V. Selbsthilfe Demenz, https://www.alzheimer-bayern.de/images/downloads/wirfuersie/ehrenamtliche/broschuereklinikeninternet.pdf, Accessed April 22, 2021. |
[37] | Schmidt-Grunert M , ed. (1999) Sozialarbeitsforschung konkret: Problemzentrierte Interviews als qualitative Erhebungsmethode, Lambertus, Freiburg im Breisgau. |
[38] | Rädiker S , Kuckartz U ((2019) ) Analyse qualitativer Datenmit MAXQDA: Text, Audio und Video, Springer VS, Wiesbaden. |
[39] | Mayring P ((2015) ) Qualitative Inhaltsanalyse: Grundlagen und Techniken, 12., revised edition, Beltz Pädagogik, Beltz,Weinheim, Basel. |
[40] | Landis JR , Koch GG ((1977) ) The measurement of observer agreement for categorical data. Biometrics 33: , 159–174. |
[41] | Fetters MD , Freshwater D ((2015) ) Publishing a methodological mixed methods research article. J Mix Method Res 9: , 203–213. |
[42] | Galvin JE , Kuntemeier B , Al-Hammadi N , Germino J , Murphy-White M , McGillick J ((2010) ) “Dementia-friendly Hospitals: Care not Crisis”:An educational program designed to improve the care of thehospitalized patient with dementia. Alzheimer Dis AssocDisord 24: , 372–379. |
[43] | Jonas K , Stroebe W , Hewstone M , Lebherz CI , Reiss M ((2007) ) Sozialpsychologie, 5., completely revised edition, Springer-Lehrbuch, Springer, Heidelberg. |
[44] | Surr CA , Sass C , Burnley N , Drury M , Smith SJ , Parveen S , Burden S , Oyebode J ((2020) ) Components of impactful dementia training forgeneral hospital staff: A collective case study. Aging MentHealth 24: , 511–521. |
[45] | Holton EF ((1996) ) The flawed four-level evaluation model. Hum Resour Dev Q 7: , 5–21. |
[46] | Schneider J , Gkioka M , Papagiannopoulos S , Moraitou D , Metz B , Tsolaki M , Kruse A , Teichmann B ((2019) ) Expectations of nursing personnel and physicians on dementia training: A descriptive survey in general hospitals in Germany and Greece. Z Gerontol Geriatr 52: , 249–257. |
[47] | Kitwood TM ((2016) ) Demenz: Der person-zentrierte Ansatz im Umgang mit verwirrten Menschen, 7., revised and enlarged edition, Hogrefe, Bern. |
[48] | Reisch E , König A ((2019) ) Management von Fort- und Weiterbildung. In Pflegemanagement: Strategien,Konzepte, Methoden, Prölß J, Lux V, Bechtel P, eds., MWV Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, pp. 275–279. |




