Neuropsychiatric Symptoms in Patients with Dementia Associated with Increased Psychological Distress in Caregivers During the COVID-19 Pandemic
Abstract
Background:
The social isolation imposed by COVID-19 pandemic can have a major impact on the mental health of dementia patients and their caregivers.
Objective:
We aim to evaluate the neurological decline of patients with dementia and the caregivers’ burden during the pandemic.
Methods:
We performed a cross-sectional study. Caregivers of dementia patients following in the outpatient clinic were included. A structured telephone interview composed of the Neuropsychiatric Inventory Questionnaire (NPI-Q), Zarit Burden Interview (ZBI), Beck Depression (BDI) and Anxiety (BAI) Inventories to address cognitive, behavioral, and functional changes associated with social distancing during the Sars-Cov-2 outbreak. Patients were divided in two groups according to caregivers’ report: with perceived Altered Cognition (AC) and Stable Cognition (SC).
Results:
A total of 58 patients (median age: 57 years [21–87], 58.6%females) and caregivers (median age: 76.5 years [55–89], 79.3%females) were included. Cognitive decline was shown by most patients (53.4%), as well as behavioral symptoms (48.3%), especially apathy/depression (24.1%), and functional decline (34.5%). The AC group (n = 31) presented increased behavioral (67.7%versus 25.9%, p = 0.002) and functional (61.3%versus 3.7%, p < 0.001) changes when compared to the SC group. In the AC group, ZBI, BDI, NPI-Q caregiver distress, and NPI-Q patient’s severity of symptoms scores were worse than the SC group (p < 0.005 for all).
Conclusion:
Patients’ neuropsychiatric worsening and caregiver burden were frequent during the pandemic. Worsening of cognition was associated with increased caregivers’ psychological distress.
INTRODUCTION
The pandemic caused by the novel coronavirus disease (COVID-19) has massively affected all countries worldwide. By the end of November 2020, almost 170 thousand deaths were caused by this disease in Brazil [1]. Older adults are the most vulnerable to the consequences of the pandemic [2], particularly for those living with dementia [3]. This vulnerability to the virus is related to their poor clinical status and their limited understanding of respiratory hygiene, such as hand sanitizing and the use of masks [4]. As a result, patients with dementia have high mortality rates [5, 6], and indeed several COVID-19 outbreaks in long-term care facilities have been reported [7–9].
Besides the direct consequences of the disease, social distancing policies have impacted the mental health of dementia patients. The burden of dementia is amplified by the decrease in environmental support such as group activities, rehabilitation therapies, and physical exercise. As dementia patients increase their demand for healthcare during the pandemic, caregiver burnout is an expected consequence. Hence, the care they provide may be hampered by their overwhelming load of work and homecare [10]. Increased physical and psychological distress brought by the pandemic increases the need for mental health assistance in both caregivers and caretakers [11]. The complexity of care for patients with dementia is probably greater in Latin America, where long-term care facilities and access to telemedicine are scarce [12].
The indirect consequences of lockdowns have been a challenge worldwide. Social distancing exacerbated psychological stressors prominently in caregivers [13]. They exhibit increased anxiety and symptoms of burden [14], probably associated with caretakers presenting clinically relevant neuropsychiatric symptoms [15]. However, it is still unclear the effects of the pandemic in neuropsychiatric symptoms of patients with dementia and the subsequent burden in caregivers. Herein, we aimed to analyze the impact of the COVID-19 pandemic on neuropsychiatric symptoms and daily habits of individuals living with dementia and the impact on their caregivers in a tertiary dementia center in southern Brazil.
METHODS
All patients in the dementia outpatient clinic of Hospital de Clínicas de Porto Alegre (southern Brazil) were screened between May 2020 to July 2020. Individuals were included if they matched the following inclusion criteria: (a) have a final diagnosis of dementia according to current criteria for specific subtypes: Alzheimer’s disease (AD) [16], vascular dementia [17], Lewy bodies dementias [18, 19], behavioral variant of frontotemporal dementia [20], primary progressive aphasia [21]; if the evaluation suggested more than one dementia etiology, it was called mixed; (b) not living in a long-term institution, (c) had a caregiver able to provide accurate clinical data. Importantly, public policies to control the spread of COVID-19 were set at the beginning of March, including mask usage and television orientations. A partial lockdown policy was imposed in Brazil on March 17, evolving to complete lockdown on July 7. The relatively short period of data collection in this study was performed to diminish the heterogeneity among respondents.
Caregivers and patients were invited to participate in this study via a telephone call. The interview was not intended to replace the medical consultation and if the caregiver required a clinical review, a teleconsultation would be scheduled. The caregiver was instructed to stay in a calm and quiet environment, and to respond to the questionnaire uninterruptedly. The standardized questionnaire included questions about the daily routine, adherence to social distancing, sleep and eating patterns, and weight changes. It also included questions about caregivers’ impression of changes in the patient’s cognition, functionality, and behavior since the beginning of the pandemic and social isolation. Cognition changes were asked directly to the caregiver and assessed in three domains, namely memory, orientation, and attention. To better understand the relationship between patients’ cognitive changes and its impact on caregivers’ mental health, we divided the whole sample into two groups: patients with Altered Cognition (AC) and patients without altered cognition (Stable Cognition, SC). Changes in functionality were measured by Pfeffer Functional Activities of daily living Questionnaire (FAQ) [22] plus additional questions about personal care, ability to feed, and urinary/fecal continence. Behavioral symptoms were assessed by the Neuropsychiatric Inventory - Questionnaire (NPI-Q) [23, 24]. We also included in the interview the Beck Anxiety Inventory (BAI) [25], the Beck Depression Inventory (BDI) [26], and the Zarit Burden Interview (ZBI) [27, 28] to measure caregivers’ psychological distress at that moment. In addition, we collected the last Mini-Mental State Examination (MMSE) [29, 30] record of each patient (all within the last year).
Data normality was assessed with the Shapiro-Wilk test. We described sociodemographic data using median, interquartile range, and total range for non-normal variables and mean and standard deviation for those with a normal distribution. We have performed multiple regression to measure the association between scales applied. Data analysis was performed using R 3.6.2 (R foundation for statistical computing, 2016). This study was approved by the Ethics Committee of the Clinics Hospital of Porto Alegre (# 2020–0423), and all caregivers gave their verbal and written consent for the study for themselves and their caretakers.
RESULTS
Of the 103 patients with dementia currently followed at the outpatient clinic, 58 caregivers (median age: 57 years [21–87], 34 (58.6%) females) and 58 patients (median age: 76.5 years [55–89], 46 (79.3%) females) met the eligibility criteria and were included in this study. The reasons for exclusion were mainly difficulties in telephone contact (n = 28), patient living in a long-term institution (n = 8), patient death (n = 6), and caregiver not willing to participate (n = 3). For those patients who were included, 29 (50%) have the final diagnosis of dementia due to AD, 7 (12.1%) of mixed dementia (AD and vascular), 7 (12.1%) of vascular dementia, and 15 (25.9%) of other diagnoses (3 Lewy bodies dementia, 3 Parkinson’s disease dementia, 2 behavioral variant frontotemporal dementia, 7 others). The median MMSE scores of the whole sample patients was 13 [1–22]. Caregivers were mostly composed of offspring (26, 44.8%) and spouses (23, 39.7%). None of the patients and four caregivers had received a confirmed Sars-CoV-2 infection (Table 1). Caregivers presented mild symptoms, and they did not mention behavioral or neurological sequelae.
Table 1
Sociodemographic and clinical characteristics of the sample
| Patients (n = 58) | Caregivers (n = 58) | |
| Age, median (range) | 76.5 (55–89) | 57 (21–87) |
| Sex, females (%) | 34 (58.6) | 46 (79.3) |
| Education, median years (range) | 4 (0–16) | 10 (0–21) |
| Sars-CoV-2 positivity (%) | 0 | 4 (6.9) |
| Caregiver’s relationship with the patient (%) | ||
| Offspring | 26 (44.8) | |
| Spouse | 23 (39.7) | |
| Other | 9 (15.5) a | |
| Full time care | – | 50 (86.2) |
| Living with the patient worsened (%) | – | 13 (22.4) |
| Medical appointments cancelled (%) | 53 (91.4) | 13 (22.4) |
| Change in exercise routine (%) | 14 (24.1) | – |
| Good/very good sleep quality (%) | – | 40 (69) |
| Medication changes b | 13 (22.4) | – |
| Sleeping medication | 9 (15.5) | |
| Change in eating habits (%) | 11 (19) | 23 (39.7) |
| Weight changes (%) | 24 (41.4) | 33 (56.9) |
| Scales and questionnaires | ||
| FAQ median score (range) | 26 (5–30) | – |
| NPI-Q | ||
| Caregiver distress, median score (range) | – | 6 (0–37) |
| Patients’ severity of symptoms, median score (range) | 6 (0–26) | – |
| ZBI, median score (range) | – | 25.5 (19–66) |
| BDI, median score (range) | – | 8 (0–42) |
| BAI, median score (range) | – | 4 (0–44) |
agrandchild, 3; ex-spouse, 2; daughter in law, 2; sister, 1; niece, 1. bstarted (antipsychotic, 4; benzodiazepine, 3; antidepressant, 2; memantine, 2); increased (antidepressant, 1); interrupted (antidepressant, 1; anticholinesterase, 3); reduced (antidepressant, 2) NPI-Q, Neuropsychiatric Inventory; ZBI, Zarit Burden Interview; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory; FAQ, Pfeffer Functional Activities of daily living Questionnaire.
In the caregivers’ viewpoint, about half patients presented worsening in cognition (31; 53.4%), namely in memory (27; 46.6%), attention (17; 29.3%), and orientation (17; 29.3%). Similarly, various neuropsychiatric manifestations worsened during the social distancing (28; 48.3%) (Fig. 1a), especially apathy/depression (14; 24.1%), anxiety (13; 22.4%), agitation (12; 20.7%), and irritability (12; 20.7%). One-third of the sample presented worsening in functional activities of daily living (20; 34.5%), most frequently in “personal care” (9; 15.5%), “pay attention/understand/discuss television program/book” (8; 13.8%), and “urinary/fecal continence” (8; 13.8%) (Fig. 1b).
Fig. 1
Frequency of (a) functional and (b) behavioral changes in patients with dementia during social isolation in caregivers’ viewpoint.
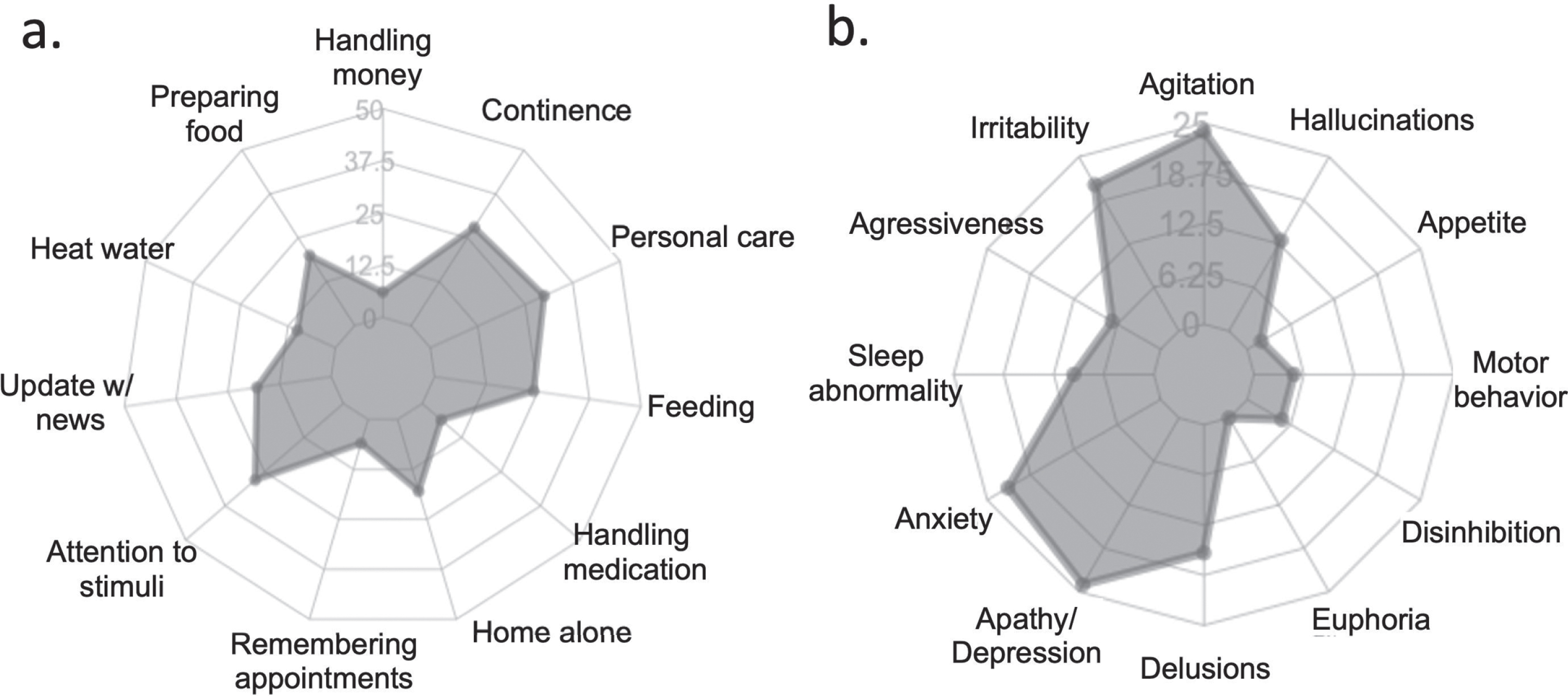
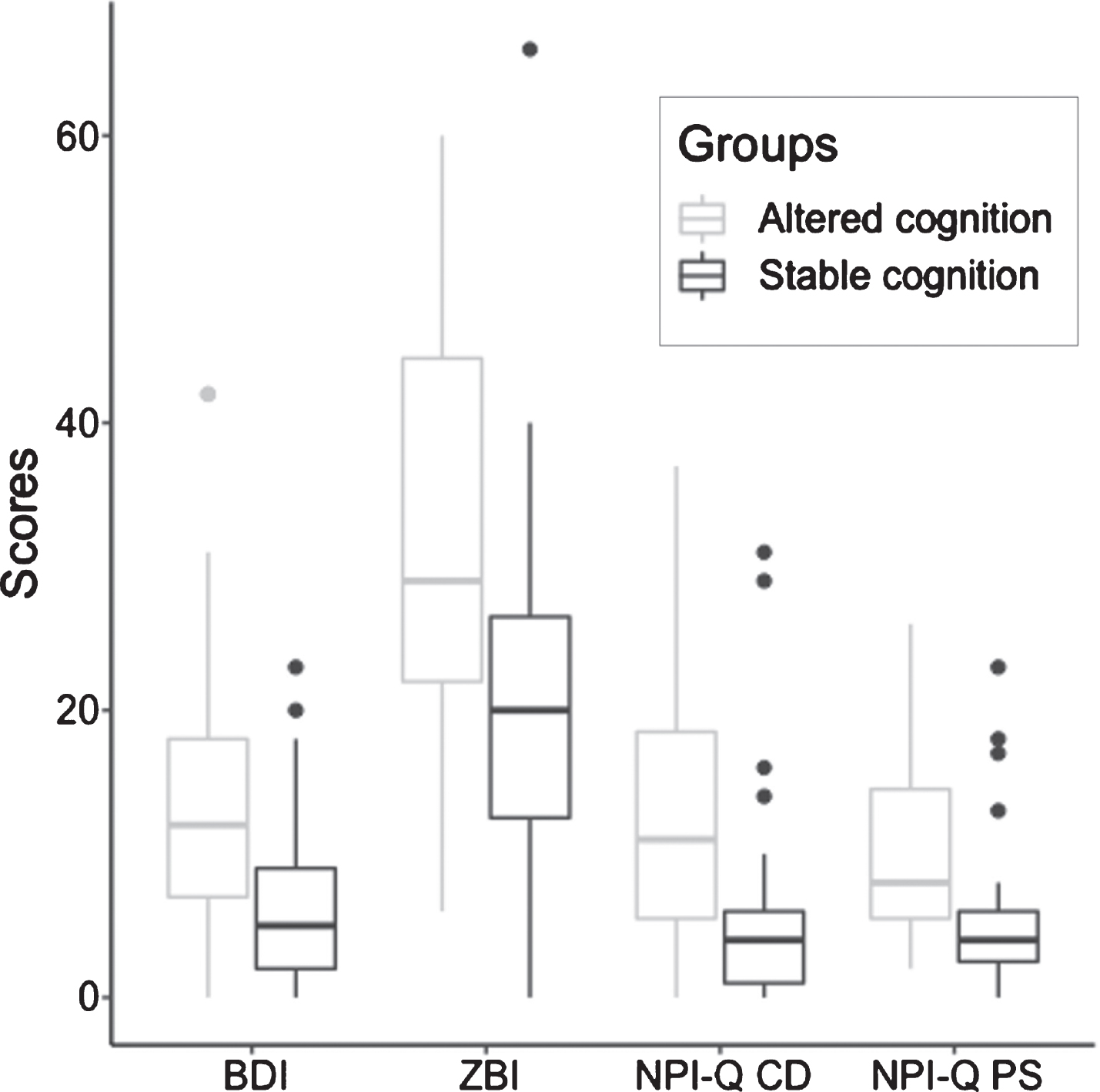
Fig. 2
Comparison of scales measuring caregivers’ mental health and burden between patients described with altered and stable cognition since the beginning of the pandemic. BDI, Beck Depression Inventory; ZBI, Zarit Burden Interview; NPI-Q CD, Neuropsychiatric Inventory Questionnaire Caregiver Distress; NPI-Q PS, Neuropsychiatric Inventory Questionnaire Patients’ Severity of Symptoms.
Daily routine and habits of patients and caregivers showed mixed results. All patients and most caregivers (49; 84.5%) were able to maintain social isolation. The majority of caregivers (52; 86.6%) used to take care of the patients full time and 15 of them asked for someone to help them in taking care of the patient. A quarter of caregivers (14, 24.1%) reported that daily living with the patient has worsened after the beginning of social isolation, while the majority described that it did not change (44, 75.9%). Medical appointments were canceled for both patients (52 consultations) and caregivers (14 consultations), though patients with dementia were more impaired by the pandemic (median one consultation/patient). As a consequence, almost a quarter of caretakers stopped taking their medications (22.4%, Table 1). The majority of caregivers (35; 60.3%) reported that they changed their total body weight (most of them, weight gain, 19/35) though most of them presented good or very good sleep quality (50; 86.2%). Patients’ exercise patterns changed during social isolation, with complete interruption or reduction in frequency in 13/58 (22.4%). Fourteen (24.1%) caregivers reported changes in daily caregiving patterns, mostly (9/14, 64.3%) an increase in the frequency of unpaid caregivers.
Caregivers’ presented a BAI median score of 4 (IQR: 8.5, 0–44), and 10 (17.2%) caregivers showed moderate to severe anxiety symptoms. Their BDI median score was 8 (IQR: 10.75, 0–42), and 10 (17.2%) showed moderate to severe depressive symptoms. The ZBI median score was 25.5 (IQR: 19, 0–66), and 9 (15.5%) caregivers showed significant symptoms of burden. Their NPI-Q score of caregiver distress had a median of 6 (IQR: 8.75, 0–26) and the NPI-Q score of the severity of patient’s symptoms had a median of 6 (IQR: 12.5, 0–37). The median FAQ score was 26 (IQR: 7, 5–30).
Caregiver’s education attainment was not associated with most patient’s functional or behavioral variables, except patients’ personal care (OR 1.23 [1.05–1.48], p = 0.046) and delusional symptoms (OR 1.16 [1.01–1.37], p = 0.01) (Supplementary Table 1). Moreover, the ZBI score was significantly associated with the BDI (p < 0.001) in a multiple regression model (Adjusted R-squared = 0.31, overall p < 0.001), but not with the BAI. There was no association between type of dementia and the ZBI (p > 0.05 for all types) (Supplementary Table 2).
Behavioral and functional changes were more frequent in the AC group (n = 31) than the SC group (n = 27) (p = 0.002 and p < 0.001, respectively, Table 2). The group AC presented increased scores in ZBI (p = 0.002), BDI (p = 0.004), NPI-Q caregiver distress (p < 0.001), and NPI-Q patient’s severity of symptoms (p = 0.001) scores. The FAQ scores were similar in both groups (Table 2).
Table 2
Clinical and sociodemographic characteristics of the sample divided by patients with altered cognition in caregivers’ viewpoint
| Altered cognition (n = 31) | Stable cognition (n = 27) | p | |
| Patients | |||
| Age, median (range) | 77 (55–89) | 76 (65–87) | 0.45 |
| Sex, F | 17 (54.8%) | 17 (63%) | 0.599 |
| MMSE scores, median (range) | 11 (1–19) | 13 (5–22) | 0.147 |
| Education, median (range) | 4 (0–12) | 4 (0–16) | 0.68 |
| Behavioral changes | 21 (67.7%) | 7 (25.9%) | 0.002 |
| Functional changes | 19 (61.3%) | 1 (3.7%) | <0.001 |
| FAQ, median (range) | 27 (23–29) | 24 (18–29) | 0.108 |
| NPI-Q patient severity of symptoms, median (range) | 8 (5–15) | 4 (2–6) | 0.001 |
| Caregivers | |||
| Age, median (range) | 57 (21–87) | 61 (22–82) | 0.27 |
| Sex, F | 27 (87.1%) | 19 (70.4%) | 0.193 |
| Education, median (range) | 11 (4–21) | 8 (0–18) | 0.21 |
| Full-time care | 24 (77.4%) | 26 (96.3%) | 0.057 |
| Changes of caregiving pattern | 8/14 | 6/14 | 1 |
| Substance use | 8 (25.8%) | 2 (7.4%) | 0.087 |
| ZBI, median (range) | 29 (21–46) | 20 (12–27) | 0.002 |
| NPI-Q caregiver distress, median (range) | 11 (5–19) | 4 (1–6) | <0.001 |
| BDI, median (range) | 12 (7–21) | 5 (2–13) | 0.004 |
| BAI, median (range) | 7 (2–13) | 4 (1–9) | 0.16 |
FAQ, Functional Activities of daily living Questionnaire; NPI-Q, Neuropsychiatric Inventory Questionnaire; BDI, Beck Depression Inventory; BAI, Beck Anxiety Inventory.
DISCUSSION
We performed a cross-sectional evaluation of social isolation’s effect due to the COVID-19 pandemic over patients with dementia and their caregivers. Our sample was representative of a majority of individuals living with dementia worldwide [31], consisting of patients attending a public health service in a low-middle income country, presenting low educational attainment. We found that, in caregivers’ viewpoint, about half of patients worsened cognition (53.4%) since March 2020, when social isolation measures started in the city of Porto Alegre, southern Brazil. Besides that, behavioral and functional alterations were also reported by caregivers. Among the behavioral changes, apathy, agitation, anxiety, and irritability were the most prominent neuropsychiatric symptoms exhibited by patients in our sample. These findings are similar to a large Italian study in which near 60%of patients with dementia worsened their behavioral symptoms [32] during pandemic. Our results are also in line with those from a recent systematic review that reported a high frequency of apathy, anxiety, and motor symptoms in patients with dementia [33] amid the social isolation imposed because of the COVID-19 pandemic.
Home isolation has enforced an abrupt disruption of patient and caregiver routines, which was associated with the onset of behavioral and psychological changes [34]. Mandatory lockdowns have greatly limited the non-pharmacological support of patients with dementia, such as social and community activities, external liveliness, and physical exercise. The withdrawal from family members, reduced social interactions such as leisure activities and a vast cancelation of medical appointments potentially influenced behavioral changes reported [35]. In this study, a significant number of patients have reported the interruption of physical exercise and almost all patients (91.4%) had a cancelation of medical appointments after the onset of the pandemic, which in turn hampered their medical treatments. Ultimately, these individuals’ neuropsychiatric symptoms lead to worsening of caregivers’ mental health [36].
Multiple factors may have moderated patients’ neurological worsening and the consequent increase of caregivers’ burden during the pandemic and social isolation. Memory was the most important cognitive alteration reported by caregivers, followed by attention and orientation. Although this is probably associated with a high prevalence of AD in our sample and worldwide, memory decline in patients with dementia has been associated with increased caregivers’ burden [37]. Caregivers also reported increased functional changes in patients with “impaired” cognition, especially in personal care, ability to pay attention to a conversation/dialogue, and fecal or urinary continence. These specific functional alterations may be due to most patients having moderate to severe dementia before the pandemic.
A global worsening of mental health results from this complex interaction between behavioral-cognitive-functional interconnections, which mainly increases a patients’ demand for help. Herein, caregivers were usually family members closely related to the patient, already committed to other daily tasks, such as work, childcare, and home tasks. An overload of tasks may easily impair their ability to cope with an increase of a patients’ demand, and a subsequent increase in psychological distress. Symptoms of depression and burden were increased in caregivers of patients with reported altered cognition in this study. Even though these symptoms can increase caregiver distress, only a minority of caregivers in our sample exhibited symptoms of increased burden (9 scored above threshold in the ZBI). However, 15 families had to ask for help when taking care of the patient, which possibly diminished the caregiver distress before this study’s procedure.
The sample of this study represents a majority of patients living with dementia worldwide, namely low and middle-income countries [31], where two-thirds of people with dementia live [38]. The impact of the pandemic is exacerbated in low-income countries, where little or no familial support is available [39] and state-driven policies are also limited for non-pharmacological treatment of these patients [40]. It is important to mention that aiming for family education is a significant strategy to mitigate the neuropsychiatric symptoms raised by the pandemic in patients with dementia, but particularly difficult in low educational settings. Some associations are already providing evidence-based orientation for caregivers [41, 42]. Technological barriers and low educational attainment are cornerstones in the spread of knowledge to patients with dementia and their caregivers. Identifying these patients and correctly addressing the caregivers’ needs may be an essential first step in mitigating the pandemic’s uncovered adverse effects both patient and caregivers’ mental health.
Our study has some limitations. Because of the study design, a single measure may not represent the pandemic’s entire period and possibly underestimate its negative impact. We classified individuals according to their cognitive alterations without a validated tool, which is a potential limitation of this method. Furthermore, the lack of previous caregiver scores in the scales may overestimate the pandemic’s impact on our sample. As our sample consists of highly dependent patients (median of Pfeffer = 26), the impact of social isolation in the early stages of dementia could not be evaluated.
In conclusion, we found that reported altered cognition in low educated patients with dementia was associated with increased caregivers’ burden and distress during the COVID-19 pandemic. Non-pharmacologic strategies to improve patients and caregivers’ mental health, already important routinely, are probably imperative in times of exception.
DISCLOSURE STATEMENT
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/20-1513r1).
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-201513.
REFERENCES
[1] | Coronavírus Brasil (2020) https://covid.saude.gov.br/. Accessed 20 November 2020. |
[2] | Armitage R , Nellums LB ((2020) ) COVID-19 and the consequences of isolating the elderly. Lancet Public Health 5: , e256. |
[3] | Iaboni A , Cockburn A , Marcil M , Rodrigues K , Marshall C , Garcia MA , Quirt H , Reynolds KB , Keren R , Flint AJ ((2020) ) Achieving safe, effective, and compassionate quarantine or isolation of older adults with dementia in nursing homes. Am J Geriatr Psychiatry 28: , 835–838. |
[4] | Tousi B ((2020) ) Dementia care in the time of COVID-19 pandemic. J Alzheimers Dis 76: , 475–479. |
[5] | Miyashita S , Yamada T , Mikami T , Miyashita H , Chopra N , Rizk D ((2020) ) Impact of dementia on clinical outcomes in elderly patients with coronavirus 2019 (COVID-19): An experience in New York. Geriatr Gerontol Int 20: , 732–734. |
[6] | Izcovich A , Ragusa MA , Tortosa F , Lavena Marzio MA , Agnoletti C , Bengolea A , Ceirano A , Espinosa F , Saavedra E , Sanguine V , Tassara A , Cid C , Catalano HN , Agarwal A , Foroutan F , Rada G ((2020) ) Prognostic factors for severity and mortality in patients infected with COVID-19: A systematic review. PLoS One 15: , e0241955. |
[7] | Iritani O , Okuno T , Hama D , Kane A , Kodera K , Morigaki K , Terai T , Maeno N , Morimoto S ((2020) ) Clusters of COVID -19 in long-term care hospitals and facilities in Japan from 16 January to 9 May 2020. Geriatr Gerontol Int 20: , 715–719. |
[8] | State Reporting of Cases and Deaths Due to COVID-19 in Long-Term Care Facilities, https://www.kff.org/coronavirus-covid-19/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities/, Accessed on April 23, 2020. |
[9] | McMichael TM , Currie DW , Clark S , Pogosjans S , Kay M , Schwartz NG , Lewis J , Baer A , Kawakami V , Lukoff MD , Ferro J , Brostrom-Smith C , Rea TD , Sayre MR , Riedo FX , Russell D , Hiatt B , Montgomery P , Rao AK , Chow EJ , Tobolowsky F , Hughes MJ , Bardossy AC , Oakley LP , Jacobs JR , Stone ND , Reddy SC , Jernigan JA , Honein MA , Clark TA , Duchin JS , Public Health–Seattle and King County, EvergreenHealth and CDC COVID-19 Investigation Team ((2020) ) Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med 382: , 2005–2011. |
[10] | Vaitheswaran S , Lakshminarayanan M , Ramanujam V , Sargunan S , Venkatesan S ((2020) ) Experiences and needs of caregivers of persons with dementia in India during the COVID-19 pandemic-a qualitative study. Am J Geriatr Psychiatry 28: , 1185–1194. |
[11] | Ryoo N , Pyun JM , Baek MJ , Suh J , Kang MJ , Wang MJ , Youn YC , Yang DW , Kim SY , Park YH , Kim S ((2020) ) Coping with dementia in the middle of the COVID-19 pandemic. J Korean Med Sci 35: , e383. |
[12] | Ibanez A , Kosik KS , Latin America and the Caribbean Consortium on Dementia (LAC-CD) ((2020) ) COVID-19 in older people with cognitive impairment in Latin America. Lancet Neurol 19: , 719–721. |
[13] | Dourado MCN , Belfort T , Monteiro A , de Lucena AT , Lacerda IB , Gaigher J , Baptista MAT , Brandt M , Kimura NR , de Souza N , Gasparini P , Rangel R , Marinho V ((2020) ) COVID-19: Challenges for dementia care and research. Dement Neuropsychol 14: , 340–344. |
[14] | Altieri M , Santangelo G ((2021) ) The psychological impact of COVID-19 pandemic and lockdown on caregivers of people with dementia. Am J Geriatr Psychiatry 29: , 27–34. |
[15] | Penteado CT , Loureiro JC , Pais MV , Carvalho CL , Sant’Ana LFG , Valiengo LCL , Stella F , Forlenza OV ((2020) ) Mental health status of psychogeriatric patients during the 2019 new coronavirus disease (COVID-19) pandemic and effects on caregiver burden. Front Psychiatry 11: , 578672. |
[16] | McKhann GM , Knopman DS , Chertkow H , Hyman BT , Jack CR Jr , Kawas CH , Klunk WE , Koroshetz WJ , Manly JJ , Mayeux R , Mohs RC , Morris JC , Rossor MN , Scheltens P , Carrillo MC , Thies B , Weintraub S , Phelps CH ((2011) ) The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7: , 263–269. |
[17] | Román GC , Tatemichi TK , Erkinjuntti T , Cummings JL , Masdeu JC , Garcia JH , Amaducci L , Orgogozo JM , Brun A , Hofman A ((1993) ) Vascular dementia: Diagnostic criteria for research studies. Report of the NINDS-AIREN International Workshop. Neurology 43: , 250–260. |
[18] | McKeith IG , Boeve BF , Dickson DW , Halliday G , Taylor J-P , Weintraub D , Aarsland D , Galvin J , Attems J , Ballard CG , Bayston A , Beach TG , Blanc F , Bohnen N , Bonanni L , Bras J , Brundin P , Burn D , Chen-Plotkin A , Duda JE , El-Agnaf O , Feldman H , Ferman TJ , Ffytche D , Fujishiro H , Galasko D , Goldman JG , Gomperts SN , Graff-Radford NR , Honig LS , Iranzo A , Kantarci K , Kaufer D , Kukull W , Lee VMY , Leverenz JB , Lewis S , Lippa C , Lunde A , Masellis M , Masliah E , McLean P , Mollenhauer B , Montine TJ , Moreno E , Mori E , Murray M , O’Brien JT , Orimo S , Postuma RB , Ramaswamy S , Ross OA , Salmon DP , Singleton A , Taylor A , Thomas A , Tiraboschi P , Toledo JB , Trojanowski JQ , Tsuang D , Walker Z , Yamada M , Kosaka K ((2017) ) Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 89: , 88–100. |
[19] | Dubois B , Burn D , Goetz C , Aarsland D , Brown RG , Broe GA , Dickson D , Duyckaerts C , Cummings J , Gauthier S , Korczyn A , Lees A , Levy R , Litvan I , Mizuno Y , McKeith IG , Olanow CW , Poewe W , Sampaio C , Tolosa E , Emre M ((2007) ) Diagnostic procedures for Parkinson’s disease dementia: Recommendations from the movement disorder society task force. Mov Disord 22: , 2314–2324. |
[20] | Rascovsky K , Hodges JR , Knopman D , Mendez MF , Kramer JH , Neuhaus J , van Swieten JC , Seelaar H , Dopper EGP , Onyike CU , Hillis AE , Josephs KA , Boeve BF , Kertesz A , Seeley WW , Rankin KP , Johnson JK , Gorno-Tempini M-L , Rosen H , Prioleau-Latham CE , Lee A , Kipps CM , Lillo P , Piguet O , Rohrer JD , Rossor MN , Warren JD , Fox NC , Galasko D , Salmon DP , Black SE , Mesulam M , Weintraub S , Dickerson BC , Diehl-Schmid J , Pasquier F , Deramecourt V , Lebert F , Pijnenburg Y , Chow TW , Manes F , Grafman J , Cappa SF , Freedman M , Grossman M , Miller BL ((2011) ) Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 134: , 2456–2477. |
[21] | Gorno-Tempini ML , Hillis AE , Weintraub S , Kertesz A , Mendez M , Cappa SF , Ogar JM , Rohrer JD , Black S , Boeve BF , Manes F , Dronkers NF , Vandenberghe R , Rascovsky K , Patterson K , Miller BL , Knopman DS , Hodges JR , Mesulam MM , Grossman M ((2011) ) Classification of primary progressive aphasia and its variants. Neurology 76: , 1006–1014. |
[22] | Pfeffer RI , Kurosaki TT , Harrah CH , Chance JM , Filos S ((1982) ) Measurement of functional activities in older adults in the community. J Gerontol 37: , 323–329. |
[23] | Camozzato AL , Godinho C , Kochhann R , Massochini G , Chaves ML ((2015) ) Validity of the Brazilian version of the Neuropsychiatric Inventory Questionnaire (NPI-Q). Arq Neuropsiquiatr 73: , 41–45. |
[24] | Cummings JL , Mega M , Gray K , Rosenberg-Thompson S , Carusi DA , Gornbein J ((1994) ) The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology 44: , 2308–2314. |
[25] | Quintão S , Delgado AR , Prieto G ((2013) ) Validity study of the Beck Anxiety Inventory (Portuguese version) by the Rasch Rating Scale model. Psicol Reflex Crit 26: , 305–310. |
[26] | Gomes-Oliveira MH , Gorenstein C , Neto FL , Andrade LH , Wang YP ((2012) ) Validation of the Brazilian Portuguese Version of the Beck Depression Inventory-II in a community sample. Braz J Psychiatry 34: , 389–394. |
[27] | Scazufca M ((2002) ) Brazilian version of the Burden Interview scale for the assessment of burden of care in carers of people with mental illnesses. Braz J Psychiatry 24: , 12–17. |
[28] | Zarit SH , Anthony CR , Boutselis M ((1987) ) Interventions with care givers of dementia patients: Comparison of two approaches. Psychol Aging 2: , 225–232. |
[29] | Folstein MF , Robins LN , Helzer JE ((1983) ) The Mini-Mental State Examination. Arch Gen Psychiatry 40: , 812. |
[30] | Kochhann R , Varela JS , Lisboa de CS M , Chaves MLF ((2010) ) The Mini Mental State Examination: Review of cutoff points adjusted for schooling in a large Southern Brazilian sample. Dement Neuropsychol 4: , 35–41. |
[31] | Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , Brayne C , Burns A , Cohen-Mansfield J , Cooper C , Costafreda SG , Dias A , Fox N , Gitlin LN , Howard R , Kales HC , Kivimäki M , Larson EB , Ogunniyi A , Orgeta V , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selbæk G , Teri L , Mukadam N ((2020) ) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396: , 413–446. |
[32] | Cagnin A , Di Lorenzo R , Marra C , Bonanni L , Cupidi C , Laganà V , Rubino E , Vacca A , Provero P , Isella V , Vanacore N , Agosta F , Appollonio I , Caffarra P , Pettenuzzo I , Sambati R , Quaranta D , Guglielmi V , Logroscino G , Filippi M , Tedeschi G , Ferrarese C , Rainero I , Bruni AC , SINdem COVID-19 Study Group ((2020) ) Behavioral and psychological effects of coronavirus disease-19 quarantine in patients with dementia. Front Psychiatry 11: , 578015. |
[33] | Simonetti A , Pais C , Jones M , Cipriani MC , Janiri D , Monti L , Landi F , Bernabei R , Liperoti R , Sani G ((2020) ) Neuropsychiatric symptoms in elderly with dementia during COVID-19 pandemic: Definition, treatment, and future directions. Front Psychiatry 11: , 579842. |
[34] | Shea YF , Shum CK , Wan WH , Chan MMK ((2020) ) Worsening behavioural and psychological symptoms of dementia during the coronavirus disease 2019 pandemic. Psychogeriatrics 20: , 916–917. |
[35] | Canevelli M , Bruno G , Cesari M ((2020) ) Providing simultaneous COVID-19-sensitive and dementia-sensitive care as we transition from crisis care to ongoing care. J Am Med Direct Assoc 21: , 968–969. |
[36] | Alexopoulos P , Soldatos R , Kontogianni E , Frouda M , Loanna Aligianni S , Skondra M , Passa M , Konstantopoulou G , Stamouli E , Katirtzoglou E , Politis A , Economou P , Alexaki M , Siarkos K , Politis A ((2021) ) COVID-19 crisis effects on caregiver distress in neurocognitive disorder. J Alzheimers Dis 79: , 459–466. |
[37] | van Maurik IS , Bakker ED , van den Buuse S , Gillissen F , van de Beek M , Lemstra E , Mank A , van den Bosch KA , van Leeuwenstijn M , Bouwman FH , Scheltens P , van der Flier WM ((2020) ) Psychosocial effects of corona measures on patients with dementia, mild cognitive impairment and subjective cognitive decline. Front Psychiatry 11: , 585686. |
[38] | Alzheimer’s Disease International, Patterson C ((2018) ) World Alzheimer Report 2018. The state of the art of dementia research: New frontiers. Alzheimer’s Disease International, London. |
[39] | Parra MA , Baez S , Allegri R , Nitrini R , Lopera F , Slachevsky A , Custodio N , Lira D , Piguet O , Kumfor F , Huepe D , Cogram P , Bak T , Manes F , Ibanez A ((2018) ) Dementia in Latin America: Assessing the present and envisioning the future. Neurology 90: , 222–231. |
[40] | Calil V , Elliott E , Borelli WV , Barbosa BJAP , Bram J , Silva de F O , Cardoso LGM , Mariano LI , Dias N , Hornberger M , Caramelli P ((2020) ) Challenges in the diagnosis of dementia: Insights from the United Kingdom-Brazil Dementia Workshop. Dement Neuropsychol 14: , 201–208. |
[41] | Coronavirus (COVID-19): Tips for Dementia Caregivers. https://alz.org/help-support/caregiving/coronavirus-(covid-19)-tips-for-dementia-care. Accessed 29 November 2020. |
[42] | Alzheimer Europe - Policy - Our opinion on... - Wellbeing of people with dementia during COVID-19 pandemic. https://www.alzheimer-europe.org/Policy/Our-opinion-on/Wellbeing-of-people-with-dementia-during-COVID-19-pandemic. Accessed 29 November 2020. |




