Effects of Acupuncture on Vascular Cognitive Impairment with No Dementia: A Randomized Controlled Trial
Abstract
Background:
Acupuncture has been used for treating vascular cognitive impairment, but evidence for its effectiveness remains limited.
Objective:
This single-center, patient-accessor blinded, randomized controlled trial was designed to assess whether acupuncture could improve the cognitive function of patients with vascular cognitive impairment with no dementia (VCIND).
Methods:
120 VCIND patients were randomly assigned to the electro-acupuncture (EA) or sham acupuncture (SA) group at a 1 : 1 ratio, with treatment conducted thrice weekly for 8 weeks. The primary outcome was the changes of cognitive function measured by the Montreal Cognitive Assessment (MoCA) from baseline to week 8. The secondary outcomes included the scores of the Mini-Mental State Examination (MMSE), the Modified Barthel Index (MBI) and the Self-rating Depression Scale (SDS). Follow-up assessments were performed with MoCA and MMSE at week 16 and 32. Linear mixed-effects models were used for analysis and all statistical tests were two-sided.
Results:
The results showed that patients in the EA group had a significantly greater improvement in MoCA score (23.85±4.18) than those in the SA group (21.48±4.44) at week 8 (95% CI = 0.80, 3.92, p = 0.04), as well as higher MoCA scores over time (p < 0.001 for interaction). Patients who received EA showed a greater increase in MMSE scores (26.41±3.47) than those who received SA (24.40±3.85) along 8 weeks (95% CI = 0.69, 3.34, p = 0.004). However, results diminished over time. No serious adverse events occurred during the trial.
Conclusion:
EA is a safe and effective technique to improve cognition over the short term of 8 weeks in VCIND patients.
INTRODUCTION
Vascular cognitive impairment with no dementia (VCIND) refers to cognitive disorders that arise from underlying vascular diseases in patients who do not meet the criteria for vascular dementia [1, 2]. The most common manifestations in patients with vascular cognitive impairment (VCI) are executive dysfunction and low information processing speed. Executive function comprises a number of processes for initiation, decision making, planning, cognitive flexibility, hypothesis generation, and judgment. Other common cognitive impairments in patients with VCI is reported as delayed recall of word lists and deficits in visual and spatial cognitive function [3]. In clinical practice, cognitive assessment includes the executive function, attention, memory, language, and visuo-spatial function [4]. A suitable instrument for cognitive screening in patients with vascular impairment is the Montreal Cognitive Assessment (MoCA) test [5]. A low MoCA score in post-stroke patients may be predictive of several adverse long-term outcomes including cognitive impairment [6]. The Aging, Demographics, and Memory Study reported that the prevalence of VCIND among 71-year-olds and above was 5.7%, accounting for 25.6% of the total cases, second only to the prodromal Alzheimer’s disease (AD) subtype [7]. VCIND is burdensome for caregivers, communities, and medical centers. Acetylcholinesterase inhibitors and excitatory amino acid receptor antagonists are the most frequently administered medicine for cognitive dysfunction [8]. However, pharmacological treatments are proven to have limited effects [9, 10]; consequently, a growing amount of attention has been directed to non-pharmacological interventions to preserve cognitive function and improve quality of life in patients with VCIND [11].
Acupuncture therapy is a minimally invasive non-pharmacological modality that originated in China. It is an important component of traditional Chinese Medicine (TCM) [12]. While two meta-analyses [13, 14] of acupuncture for VCIND showed insufficient evidence to recommend acupuncture, the reported studies were heterogeneous and inherently flawed in design, characterized by small sample size and poor methodological quality.
Therefore, we conducted this randomized controlled trial (RCT) comparing a sham control group to electroacupuncture (EA) in well-characterized VCIND populations. The objectives of this study were to determine the effects of EA for diminishing the cognitive decline in patients with VCIND after 8-week treatment and to investigate the maintenance of effects throughout the 24-week follow-up. We hypothesized that acupuncture would be more effective in improving patients’ cognitive function when compared with the controls.
METHODS
Study design
This was a RCT conducted during October 2017 to December 2019 at the Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai, China. All 120 participants provided written informed consent, before they were randomly assigned to the EA or sham acupuncture (SA) group at a ratio of 1:1. EA or SA sessions were conducted thrice weekly for 8 weeks. The researchers did the face-to-face screening to get the baseline MoCA scores on patients with VCIND before the intervention began. Afterward, other outcome measures were evaluated at week 8, and then at week 16 and week 32 respectively. The study was performed according to the common guidelines for clinical trials, including Declaration of Helsinki, International Conference on Harmonization, World Health Organization guidelines for Good Clinical Practice, and Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) guidelines [15]. The present trial was approved by the ethics committee of the Shanghai Municipal Hospital of Traditional Chinese Medicine (2017SHL-KY-03) and registered on www.chictr.org.cn (ChiCTR-IIR-17011513). The full trial protocol is available online [16].
Participants
Participants with VCIND were recruited from hospitals and communities via posters and WeChat public advertisements. The inclusion criteria were as follows: 1) aged 40–80 years old, male or female; 2) complained of or were reported by a relative or accompanying person as having a decline in cognitive function; 3) obtained the following results in a neuropsychological assessment under professional instruction: MoCA score < 26 points, with clinical dementia rating scale score = 0.5, modified Rankin scale score≤3 points, Hachinski ischemic score > 7 points; 4) had imaging evidence that supports cerebrovascular disease, with or without a medical history of transient ischemic attack or other types of stroke; 5) had signs and symptoms caused by cerebrovascular disease (e.g., hemiplegia, hemiparesis, problems with understanding or forming speech, numbness or strange sensations).
Participants were excluded if they 1) had a Mini-mental State Examination (MMSE) score < 21 points; 2) had co-morbidity of AD, Parkinson’s disease, frontotemporal dementia, Huntington’s disease, demyelinating disease, post-traumatic dementia, or central nervous system infection; 3) had epilepsy, psychosis or depression; 4) had clinically significant gastrointestinal, renal, hepatic, respiratory, or other systemic diseases; and 5) had severe visual or hearing impairment, severe aphasia or limb dysfunction which might affect the assessment.
Randomization and blinding
A total of 120 eligible participants were randomly assigned to receive either EA or sham SA via block random method at a ratio of 1:1. Acupuncturists obtained each patient’s group assignment through an opaque envelope from another researcher before preforming the intervention. All relevant parties were blinded to the group assignment except acupuncturists. For patients in SA group, a blunt-tipped placebo needle provided participant-blinding effects with a similar appearance to conventional needles, but without skin penetration. The sham EA apparatus was constructed with a broken internal connecting wire, thereby providing no actual current output. To test the success of blinding, an independent researcher asked the participants whether they believed they received EA or SA at week 8 for the blinding assessment.
Intervention
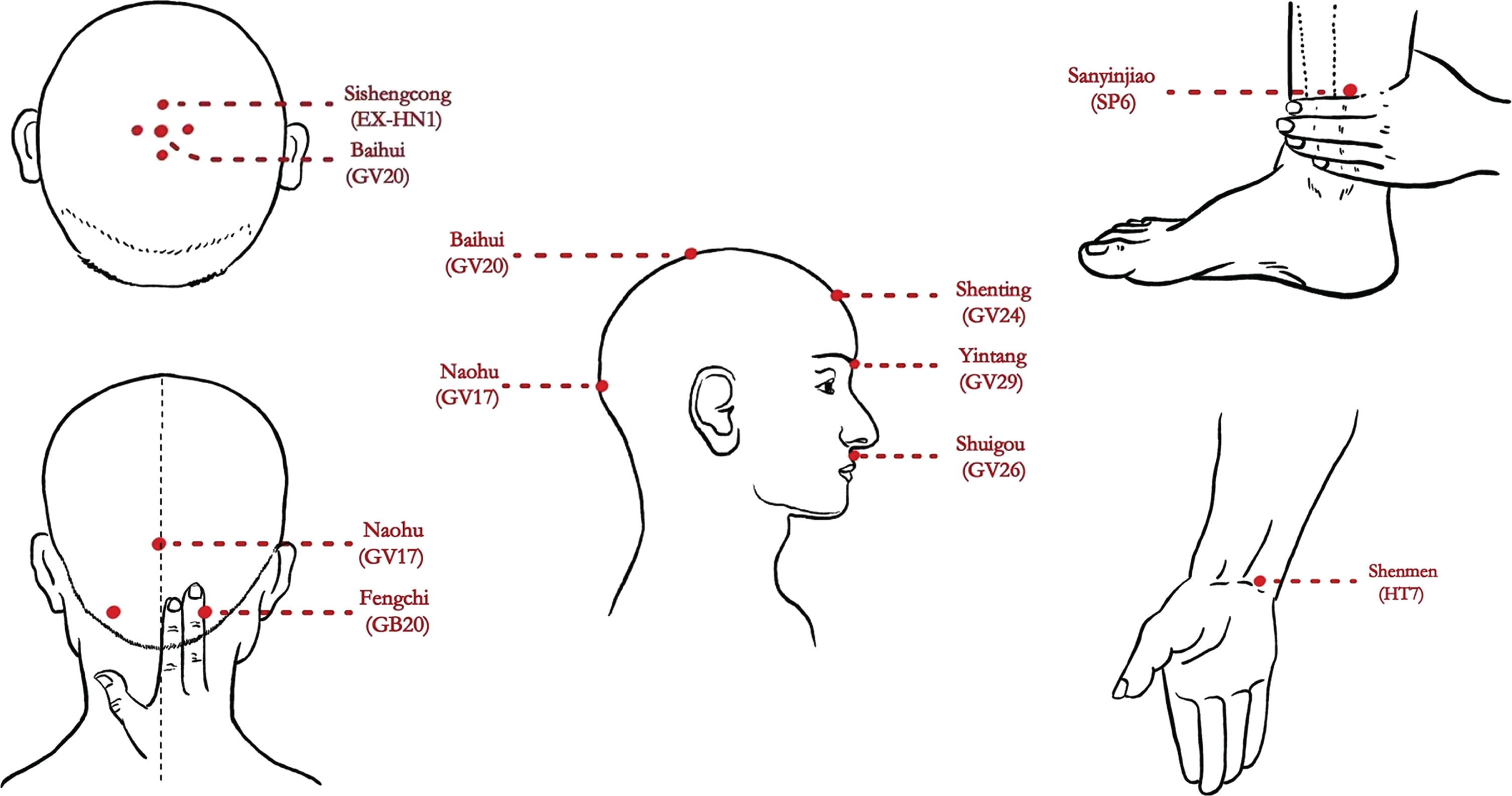
Patients in both groups were advised to maintain their regular exercise program and not take other treatment during the trial. The EA therapeutic regimen was developed by the consensus of acupuncture experts and the results of our pilot study [17]. Both treatments of EA and SA, consisted of 24, 30 min sessions that were administered over the course of 8 weeks, three times a week. Participants lay supine with eye masks while receiving treatment, conducted with disposable needles (Wuxi Jiajian Medical Material Co., Ltd., Wuxi, China). The treatment consisted of the following acupoints: Baihui (GV20), Yintang (GV29), Shenting (GV24), Shuigou (GV26), Naohu (GV17), Sishencong (EX-HN1), and bilateral Fengchi (GB20), Shenmen (HT7) and Sanyinjiao (SP6) (detailed location of acupoints can be seen in Table 1 and Fig. 1). A team of 4 acupuncturists, with at least 5-year undergraduate training and licenses to practice of TCM, did the real and sham acupuncture treatments during the trial. All research assistants, including evaluators, statisticians, and acupuncturists received a 1-week training session before the trial.
Table 1
Acupuncture method for each acupoint
| Acupoint | Needling method | Needles |
| Baihui (GV20), Shenting (GV24), Sishencong (EX-HN1) | The angle between the needle tip and the scalp is 30°. Move the needle tip backward along the anterior-posterior midline, and insert for 1 cm. | 0.25*25 mm |
| Naohu (GV17) | The angle between the needle tip and the scalp is 15°. Move the needle tip backward along the anterior-posterior midline, and then insert for 1 cm. | 0.25*25 mm |
| Shuigou (GV26) | Puncture obliquely for 1 cm, with the needle tip upward. | 0.25*25 mm |
| Yintang (GV29) | Pinch the local skin, and then puncture obliquely for about 1 cm. | 0.25*25 mm |
| Shenmen (HT7) | Puncture perpendicularly for about 1 cm. | 0.25*25 mm |
| SanYinjiao (SP6) | Puncture perpendicularly for about 2-3 cm. | 0.30*40 mm |
| Fengchi (GB20) | Puncture obliquely for about 2 cm, with the needle tip toward the nose tip. | 0.30*40 mm |
Fig. 1
Location of the acupoints.
In the EA group, all acupoints were treated with such manipulations as lifting, thrusting, and rotating, until the achievement of the Deqi sensation, characterized by a soreness, heaviness, and distention. Paired wires of the EA apparatus (Device G6805-2, Shanghai Huayi Medical Instrument Co., LTD) were attached to the needles at points GV20 and GV29. The EA stimulation was set at a frequency of 2.5 Hz and an intensity of 2-3 mA depending on the participant’s comfort level.
Participants in the SA group received sham acupuncture with the Streitberger non-insertion needles at the same acupoints as those in the EA group [18]. Each received a pricking sensation when the blunt needle tip touched to the skin, but without insertion of a real needle. Paired wires of the EA apparatus were attached to the needles at GV20 and GV29, but with no current output.
Outcome measurements
Primary outcome
The primary outcome was the cognitive function measured by the MoCA [19], recorded at week 8. MoCA is the most frequently utilized cognitive testing measurement in dementia clinical trials. It consists of 6 cognitive domains: memory, language, orientation, reason, praxis and concentration. This scale has a total score of 30, with a normal value of≥26. A test score less than 26 indicates cognitive impairment. This measurement was well validated in elderly Chinese population [20].
Secondary outcomes
Secondary outcomes included the changes in MoCA from baseline to week 32. The between-group comparisons were made of MMSE scores at week 8, 16, and 32, respectively. MMSE, another important outcome for assessing cognitive function [21], contains the functions of 7 cognitive domains: time and location orientation, immediate memory, attention and computational power, delayed memory, language and visual space. The functional outcome of daily living ability was evaluated by the Chinese version of the Modified Barthel Index (MBI) [22], covering the basic and instrumental components, with the score range of 0–100 and lower scores indicating worse functioning. Mental state was evaluated using the Depression self-rating scale (SDS) which well-validated in older individuals [23].
Safety was assessed using the Treatment Emergent Symptom Scale (TESS). Adverse events (AEs) that first appeared during the study or worsened as the study progressed were recorded per the TESS scale, including date and time of onset, duration, severity, relationship to intervention, and action taken.
Expectation was assessed at the beginning of treatment, with a question presented to each participant: “Do you believe that acupuncture can treat VCIND?” They were required to choose one from the following 4 choices: “Strongly believe,” “Believe,” “Believe a little bit,” and “Do not believe.”
Sample size calculation
The sample size calculation was based on the change of MoCA scores. Our previous research suggested that at least a 1.25-point difference in MoCA scores between acupuncture and sham acupuncture treatment was clinically significant [17]. We expected that acupuncture would outperform the sham acupuncture by 1 point in this trial. The following formula of superiority test was used to do the sample size calculation (among which Uα = 3.22, Uβ = 1.97, δ= 1.85):
Therefore, a sample size of 48 participants recruited was determined sufficient for each group. Allowing for a 20% dropout rate, the recruited sample size for this RCT was 120 participants, with 60 in each group.
Statistical analysis
All original data were entered and stored with Epidata version 3.1, before being imported into Microsoft Excel 2010. Statistical analyses were performed with SPSS version 21.0, and all data were analyzed according to the Intention-to-treat (ITT) principle. Those who completed the baseline evaluation and received at least 1 session of EA or SA treatment were included in the outcome assessment. The missing data were replaced with the last observation carried forward (LOCF) imputation method to maintain the sample size and to reduce the bias caused by the attrition of participants.
As the data were normally distributed, continuous variables were compared using Student’s t test, and the categorical variables, using Fisher’s exact test. The baseline characteristics were compared between the two groups and demonstrated using the mean (±SD) or the median (with IQR) for continuous data. For the categorical data (binary classification and multiple classification), the composition ratio was used to create a statistical description. Based on the observation of a theoretical frequency distribution, the χ2 or Fisher’s exact test was used, depending on the specific situation.
An unpaired Student’s t-test analysis of variance was applied to the primary outcome of MoCA. A linear effect mixture model was used to compare the changing trend of MoCA scores between the 2 groups from week 8 to week 32. The secondary outcomes of MMSE, SDS, and MBI were also analyzed using a Student’s t-test or Rank sum test. A safety evaluation was determined using the Safe Set (SS) dataset. All reported p values were 2-sided with confidence intervals at the 95% level. A p value of less than 0.05 was considered statistically significant.
RESULTS
Study participants
A total of 235 patients were screened between November 2017 and December 2018, and 115 patients were excluded due to various reasons: 51 did not meet the inclusion criteria, 25 could not commit the necessary time, 3 were now in other clinical trials, 11 patients’ cognitive impairment were caused by other diseases, 17 took medicine for treating VCIND in the last two weeks, and the rest 8 had serious chronic diseases (please see details in Fig. 2). The remaining 120 were enrolled and assigned into either the EA or SA group. Ultimately 27 (22.5%) patients dropped out during the trial, 12 (10%) in the EA group and 15 (12.5%) in the SA group. Table 2 showed the participants’ baseline demographic and clinical characteristics. No statistically significant difference was observed between the 2 groups in the demographic and clinical characteristics (all p > 0.05).
Fig. 2
Study flow diagram.
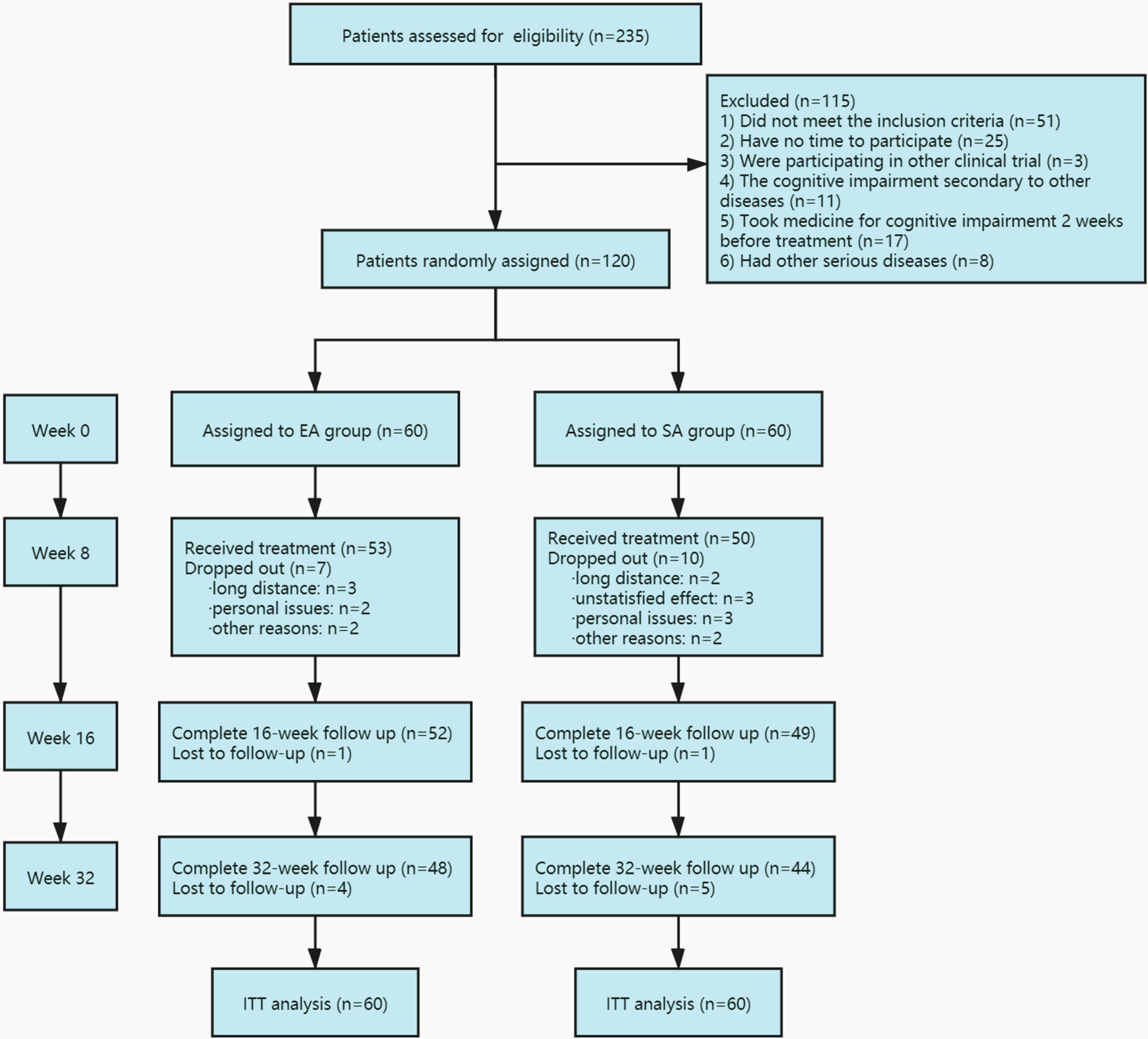
Table 2
Baseline characteristics of patients in two groups
| Variables | EA group (n = 60) | SA group (n = 60) | p |
| Mean age (SD), y | 65.1 (7.5) | 64.6(8.4) | 0.15 |
| Female, n (%) | 27(45) | 31(51.7) | 0.46 |
| Education, n | 0.03 | ||
| Middle school or lower | 40 | 50 | |
| College graduate or higher | 20 | 10 | |
| Marital status, n | 1.00 | ||
| Single | 1 | 2 | |
| Married (Divorced, separated or widowed) | 59 | 58 | |
| Drinking alcohol, n | 0.03 | ||
| Never | 54 | 45 | |
| Former or current | 6 | 15 | |
| Smoking, n | 0.41 | ||
| Never | 40 | 42 | |
| Former | 5 | 8 | |
| Current | 15 | 10 | |
| Subtypes of stroke, n | 0.97 | ||
| Cerebral infarction | 38 | 39 | |
| Cerebral hemorrhage or other | 16 | 15 | |
| Encephalatrophy | 6 | 6 | |
| Related medical condition, n | |||
| Hypertension | 33 | 35 | 0.71 |
| Coronary heart disease | 12 | 12 | 1.00 |
| Diabetes mellitus | 16 | 19 | 0.50 |
| Hyperlipidemia | 23 | 26 | 0.57 |
| Use of concomitant drugs, n | 0.27 | ||
| Any | 30 | 25 | |
| Antihypertensive | 20 | 10 | |
| Lipid-reducing | 7 | 7 | |
| Hypoglycemic | 5 | 9 | |
| Antithrombotic | 8 | 6 | |
| Mean baseline psychometric scores (Mean±SD) | |||
| MoCA | 19.80±4.08 | 20.08±4.28 | 0.71 |
| MMSE | 23.25±4.04 | 23.23±3.83 | 0.85 |
| MBI | 93.58±14.62 | 96.25±11.70 | 0.60 |
| SDS | 43.25±8.73 | 41.47±9.32 | 0.28 |
| Expectation of acupuncture, n | 0.19 | ||
| Strongly believe | 17 | 14 | |
| Believe | 23 | 22 | |
| Believe a little bit | 18 | 16 | |
| Do not believe | 2 | 8 |
EA, electroacupuncture; SA, sham electroacupuncture; MoCA, Montreal Cognitive Assessment; MMSE, Mini-Mental State Examination; MBI, Modified Barthel index; SDS, Self-rating Depression Scale.
Primary outcome
Table 3 showed the results of the between-group differences in patients’ MoCA scores from baseline to week 32. At the end of the 8-week intervention, an increase in MoCA scores was detected in EA group. Patients with EA treatment had an average 3.00 points higher (95% CI: 0.80 to 3.92, p = 0.04) in MoCA scores (23.85±4.18) than those receiving SA treatment (21.48±4.44).
Table 3
Changes of MoCA test scores of patients in two groups (Mean±SD)
| Time | EA group | SA group | EA versus SA Difference (95% CI) | p |
| (n = 60) | (n = 60) | |||
| Baseline | 19.80±4.08 | 20.08±4.28 | –0.37 (–1.80, 1.22) | 0.71 |
| Week 8 | 23.85±4.18 | 21.48±4.44 | 3.00 (0.80, 3.92) | 0.04 |
| Week 16 | 22.45±4.22 | 20.81±4.46 | 2.06 (0.06, 3.20) | 0.04 |
| Week 32 | 20.71±4.20 | 20.31±4.26 | 0.52 (–1.12, 1.92) | 0.60 |
EA, electroacupuncture; SA, sham electroacupuncture; MoCA, Montreal Cognitive Assessment.
Additionally, patients’ MoCA scores in EA group (22.45±4.22) were 2.06 points higher on average than those in SA group (20.81±4.46, 95% CI: 0.06 to 3.20, p = 0.04) at week 16. No significant difference was seen between the 2 groups at week 32 (EA: 20.71±4.20 and SA: 20.31±4.26, 95% CI: –1.12 to 1.92, p = 0.603).
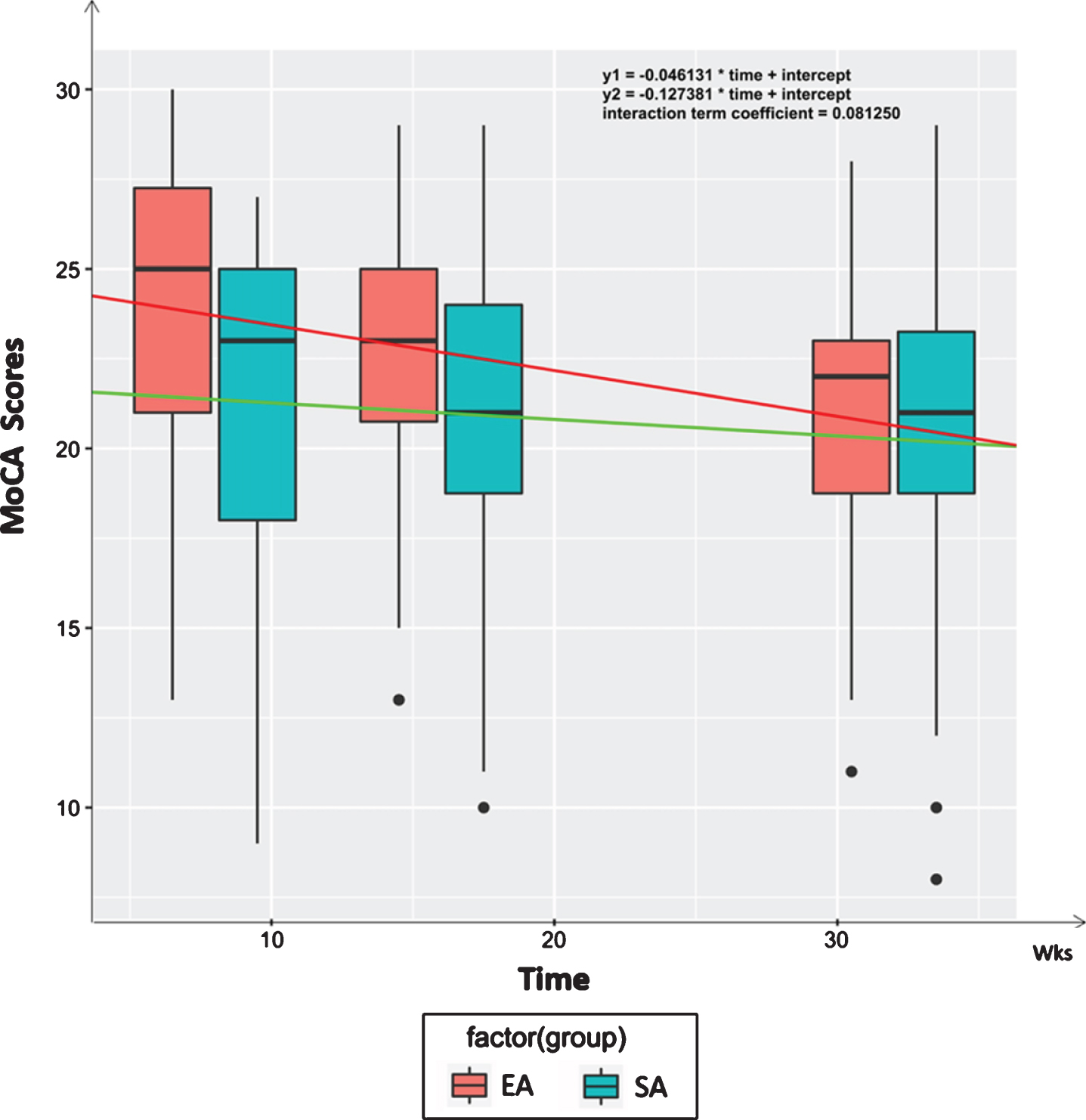
According to the changing trend of MoCA scores between the EA and SA groups, the slopes of the regression line for time-group effects were both significantly different from 0 (the coefficient of regression in time: –0.21, and the coefficient of regression in group: –2.98). As shown in Fig. 3, the slope of EA group (in red) was higher than that of SA group (in green) over time (the coefficient of regression = 0.081, p < 0.001), indicating that the changing trend of EA in MoCA scores was significantly different from that of SA, and the between-group differences persisted from week 8 to week 32.
Fig. 3
Between-group differences on MoCA scores over time.
Secondary outcomes
As indicated by Table 4 on the differences of MSE, MBI, and SDS in all randomly assigned patients during the trial. The EA group had significantly greater improvement in MMSE scores than the SA group at week 8 (EA: 26.41±3.47 & SA: 24.40±3.85, 95% CI: 0.69 to 3.34, p = 0.004) and at week 16 (EA: 25.01±3.68 & SA: 23.45±4.49, 95% CI: 0.08 to 3.05, p = 0.03). At week 32, no statistically significant difference was observed (95% CI: –1.07 to 1.70, p = 0.65) in the EA group (23.68±3.62) when compared with the SA group (23.36±4.04).
Table 4
Secondary outcome measures of patients in two groups (Mean±SD)
| Variables | EA group | SA group | EA versus SA Difference (95% CI) | p |
| (n = 60) | (n = 60) | |||
| MMSE | ||||
| Week 0 | 23.25±4.04 | 23.23±3.83 | 0.18 (–1.40, 1.43) | 0.85 |
| Week 8 | 26.41±3.47 | 24.40±3.85 | 3.01 (0.69, 3.34) | 0.004 |
| Week 16 | 25.01±3.68 | 23.45±4.49 | 2.09 (0.08, 3.05) | 0.03 |
| Week 32 | 23.68±3.62 | 23.36±4.04 | 0.45 (–1.07, 1.70) | 0.65 |
| MBI* | ||||
| Week 8 | 93.41±15.31 | 96.33±11.68 | 0.23 | |
| SDS | ||||
| Week 8 | 39.28±7.82 | 39.06±9.51 | 0.13 (–2.93, 3.36) | 0.89 |
EA, electroacupuncture; SA, sham electroacupuncture; MMSE, Mini-Mental State Examination; MBI, Modified Barthel index; SDS, Self-rating Depression Scale. *Rank sum test
Paired t-test for MBI and SDS in the EA group indicated that there were no significant differences in these scores before or after the 8-week acupuncture intervention (both p > 0.05). Compared with the SA group, the EA group showed no significant reduction in the post-treatment MBI score (p = 0.23), as well as in the post-treatment SDS (p = 0.89).
Blinding assessment
With at least one session of treatment, all participants were asked about their group assignment at the end of week 8. In the EA group, 42 patients thought that they took the real treatment, 7 of them thought that they received the sham one, and 4 of them had no idea. In the SA group, 30 patients believed that they took the real treatment, 12 of them thought that they received the sham one, and the rest, 8 of them, were unsure. No statistical difference was found between the EA and SA group in the proportion of participants (χ2 = 4.57, p = 0.10).
The successful implementation of the blinding method might be mainly owing to the sham needles. Patients in SA group had the feelings like that the blunt needle tip touched the skin and then the needle was “slightly“ inserted, but without pain or Deqi sensation, which is very important for the efficacy of EA treatment. For acupuncture-naive patients and VCIND patients with cognitive impairment, the difference between EA and SA were even harder to be detected.
Expectation and AEs
A total of 40 participants in the EA group and 36 in the SA group believed in the effect of the acupuncture treatment for VCIND; the rest of the participants doubted the efficacy before the intervention started. No significant difference was found between the groups when the patients’ expectation was evaluated (p = 0.20). During the period of intervention, acupuncture-related AEs, including local pain, headache, local subcutaneous hematoma, and dizziness, occurred in 8.3% of the EA group and 6.7% in the SA group, respectively. No significant difference was found between the groups in the proportion of participants with AEs (p = 0.61). No severe AEs were observed. No participants withdrew from the trial because of AEs.
DISCUSSION
This trial proved EA to be effective in improving cognitive function for patients with VCIND during the 8-week intervention period, but its effectiveness diminished over time. Thus, EA could be recommended as a potentially promising new therapeutic option for patients with VCIND over the short time, but its long-term efficacy needs to be further studied.
Previous studies showed that acupuncture was effective for short-term improvement of cognitive function, but few reported the long-term effectiveness of acupuncture. Our findings on the effectiveness of acupuncture on the improvement of cognitive function are consistent with those of previously published clinical trials [24–26], while to date our trial is the only one characterized by a 6-month period of follow-up. Through a long follow-up period, we found that the effects of EA may last until 16 weeks after the beginning of intervention, and there were no differences between the two groups at 32 weeks of follow up. The results suggested that acupuncture may be effective in treating patients with VCIND over the short term, and it needs further maintenance treatments with a longer intervention period to consolidate its efficacy for improving VCIND patients’ cognitive function. The proportions of participants having acupuncture related AEs in the two groups were low, and the AEs were mild or transient.
Until recently, the neuropathology of vascular dementia was poorly defined; and the exact mechanism of acupuncture for VCIND was unknown. Microinfarction, microvascular changes related to blood-brain barrier damage, focal neuronal atrophy, and low burden of co-existing neurodegenerative pathology appeared to be key substrates of vascular dementia [27]. Acupuncture may influence the process of vascular dementia through multiple aspects: protecting cerebral neurons from oxidative stress, apoptosis, and neuroinflammation, regulating glucose metabolism, and modifying neurotransmitters. Improving synaptic plasticity and blood vessel function could be another possible mechanism [28–33]. In addition, studies using functional magnetic resonance imaging (fMRI) suggested that acupuncture could increase the activity in the temporal lobe and prefrontal lobe, which are closely related to cognitive function [34].
Due to the complicated process of cognitive impairment and the difficulty of its repairment, the efficacy of EA treatment lasted for a relatively short time for patients with VCIND in this trial, compared to the long way they need to go to fight against the disease. The short intervention period of 8 weeks might be another reason of the short efficacy time. EA can temporarily prevent or delay the progress of cognitive impairment. Without other more effective measures, the time for EA treatment to take stronger effect may be slower than the time for the development of the disease.
In this study, we used two instruments to evaluate patients’ cognitive function, MoCA and MMSE. A review showed that the MoCA scale had higher sensitivity, without a ceiling effect [35]; therefore, it was more reliable at screening mild cognitive impairment patients [36]. However, the MMSE scale made up for the lack of specificity and positive predictive value of the MoCA scale during the screening process [37]. Therefore, both scales were selected to complement the deficiencies of the other. The effects were observed once the intervention was completed during week 8 and persisted through the follow-up period.
We chose many important acupoints from the Governor Vessel for the treatment of VCIND in this trial. Based on the meridian theory rooted in TCM, the Governor Vessel runs in the middle of the back of the body and is the only meridian directly running into the brain. It has the functions of controlling cognition, consciousness, and thinking activities. EX-HN1 is located on the scalp near GV20 and GB20 is located on the occiput, and both of them have close relationship to the brain functions. HT7 is the primary acupoint of the Heart meridian and can control mind. The matched HT7 and SP6 can clear mind and calm nerves, and their indications include forgetfulness, insomnia, or mental disorders such as depression and anxiety. Furthermore, mechanism studies showed that EA at GV20 can improve learning-memory ability of AD rats by downregulating the expression of IL-1β and TNF-α in the prefrontal cortex and hippocampus to reduce inflammatory reaction [38]; and stimulation at GB20 can reduce the resistance of the posterior cerebral arteries and improve the cerebral blood flow [39].
Our trial had several limitations. The therapeutic sessions and acupoints were determined based on our clinical experience for treating cognitive impairment and the results of our previous studies [17]. We also took the consensus of experienced and qualified TCM experts in China into consideration. However, 24 sessions of EA treatments may be burdensome for some patients living far away from the hospital. Next, the selection of acupoints did not take into account the symptom differentiation of Chinese medicine, even though it was simple and effective in clinical practice. Syndrome differentiation is a unique step in TCM, in which acupuncturists usually observe patients’ complexion, ask about their disease changes, and taking pulse before each session and then they may alternate acupoints each session based on the results. Moreover, the timing of stroke plays an important role in the brain functioning, affecting the cognitive function of VCI patients. Patients included in this trial were in the early stage of the cognitive decline and had mild cognitive impairment. Patients with moderate cognitive impairment were excluded in the screening process. The timing of the stroke will be taken into consideration and patients with different severity of cognitive impairment will be recruited in future trials. Additionally, all trial measures were identified prior to trial initiation and did not undergo modification thereafter, except for the removal of one objective measurement of event-related potential (ERP). ERP can reflect the changes of neuro electrophysiology in the brain during the cognitive process. However, it took a long time for testing a participant and was difficult for elderly patients to cooperate at the beginning of the trial. In our future studies, we will perform other objective measurements such as fMRI or electroencephalography to detect changes in the brain during acupuncture so that we can further explore the mechanism of electroacupuncture treatment for VCIND.
CONCLUSION
Compared with sham acupuncture, VCIND patients receiving electroacupuncture treatment had higher cognitive function after 8 weeks of treatment. Further research is needed to understand long term efficacy and the mechanism of action of this intervention.
ACKNOWLEDGMENTS
The present trial was supported by the Shanghai Science and Technology Commission (Grant number 16401930800). We are indebted to all practicing doctors who delivered the intervention and all postgraduates involved in the care for the participants. We particularly thank our instructor in our present study, Lao Lixing, for his outstanding role in coordinating the trial. We would like to thank Philippa Hazlewood, postgraduate from school of international exchange, Shanghai University of Traditional Chinese Medicine, for her editorial support.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/20-1353r2).
REFERENCES
[1] | Stephan BC , Matthews FE , Khaw KT , Dufouil C , Brayne C ((2009) ) Beyond mild cognitive impairment: Vascular cognitive impairment, no dementia (VCIND). Alzheimers Res Ther 1: , 4. |
[2] | Wentzel C , Rockwood K , MacKnight C , Hachinski V , Hogan DB , Feldman H , Østbye T , Wolfson C , Gauthier S , Verreault R , McDowell I ((2001) ) Progression of impairment in patients with vascular cognitive impairment without dementia. Neurology 57: , 714–716. |
[3] | Looi JC , Sachdev PS ((1999) ) Differentiation of vascular dementia from AD on neuropsychological tests. Neurology 53: , 670–678. |
[4] | Skrobot OA , Black SE , Chen C , DeCarli C , Erkinjuntti T , Ford GA , Kalaria RN , O’Brien J , Pantoni L , Pasquier F , Roman GC , Wallin A , Sachdev P , Skoog I , Ben-Shlomo Y , Passmore AP , Love S , Kehoe PG ((2018) ) Progress toward standardized diagnosis of vascular cognitive impairment: Guidelines from the Vascular Impairment of Cognition Classification Consensus Study. Alzheimers Dement 14: , 280–292. |
[5] | Pendlebury ST , Mariz J , Bull L , Mehta Z , Rothwell PM ((2012) ) MoCA, ACE-R, and MMSE versus the National Institute of Neurological Disorders and Stroke-Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards Neuropsychological Battery after TIA and stroke. Stroke 43: , 464–469. |
[6] | Zietemann V , Georgakis MK , Dondaine T , Müller C , Mendyk AM , Kopczak A , Hénon H , Bombois S , Wollenweber FA , Bordet R , Dichgans M ((2018) ) Early MoCA predicts long-term cognitive and functional outcome and mortality after stroke. Neurology 91: , e1838–e1850. |
[7] | Plassman BL , Langa KM , Fisher GG , Heeringa SG , Weir DR , Ofstedal MB , Burke JR , Hurd MD , Potter GG , Rodgers WL , Steffens DC , McArdle JJ , Willis RJ , Wallace RB ((2008) ) Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med 148: , 427–434. |
[8] | Anand R , Gill KD , Mahdi AA ((2014) ) Therapeutics of Alzheimer’s disease: Past, present and future. Neuropharmacology 76 Pt A: , 27–50. |
[9] | DeKosky ST , Williamson JD , Fitzpatrick AL , Kronmal RA , Ives DG , Saxton JA , Lopez OL , Burke G , Carlson MC , Fried LP , Kuller LH , Robbins JA , Tracy RP , Woolard NF , Dunn L , Snitz BE , Nahin RL , Furberg CD ((2008) ) Ginkgo biloba for prevention of dementia: A randomized controlled trial. JAMA 300: , 2253–2262. |
[10] | Dichgans M , Markus HS , Salloway S , Verkkoniemi A , Moline M , Wang Q , Posner H , Chabriat HS ((2008) ) Donepezil in patients with subcortical vascular cognitive impairment: A randomised double-blind trial in CADASIL. Lancet Neurol 7: , 310–318. |
[11] | Moll van Charante EP , Richard E , Eurelings LS , van Dalen JW , Ligthart SA , van Bussel EF , Hoevenaar-Blom MP , Vermeulen M , van Gool WA ((2016) ) Effectiveness of a 6-year multidomain vascular care intervention to prevent dementia (preDIVA): A cluster-randomised controlled trial. Lancet 388: , 797–805. |
[12] | TJ K ((2002) ) Acupuncture: Theory, efficacy, and practice. Ann Intern Med 136: , 374–383. |
[13] | Cao H , Wang Y , Chang D , Zhou L , Liu J ((2013) ) Acupuncture for vascular mild cognitive impairment: A systematic review of randomised controlled trials. Acupunct Med 31: , 368–374. |
[14] | Min D , Xu-Feng W ((2016) ) An updated meta-analysis of the efficacy and safety of acupuncture treatment for vascular cognitive impairment without dementia. Curr Neurovasc Res 13: , 230–238. |
[15] | MacPherson H , White A , Cummings M , Jobst K , Rose K , Niemtzow R ((2002) ) Standards for reporting interventions in controlled trials of acupuncture: The STRICTA recommendations. STandards for Reporting Interventions in Controlled Trails of Acupuncture. Acupunct Med 20: , 22–25. |
[16] | Li T , Wu H , Soto-Aguliar F , Huang L , Li W , Lao L , Xu S ((2018) ) Efficacy of electrical acupuncture on vascular cognitive impairment with no dementia: Study protocol for a randomized controlled trial. Trials 19: , 52. |
[17] | Chen YQ , Wu HG , Yin P , Xu J , Huang ET , Xu SF ((2019) ) [Tongdu Tiaoshen acupuncture method for mild cognitive impairment: A randomized controlled trial]. Zhongguo Zhen Jiu 39: , 1141–1145. |
[18] | Streitberger K , Kleinhenz J ((1998) ) Introducing a placebo needle into acupuncture research. Lancet 352: , 364–365. |
[19] | Kopecek M , Bezdicek O , Sulc Z , Lukavsky J , Stepankova H ((2017) ) Montreal Cognitive Assessment and Mini-Mental State Examination reliable change indices in healthy older adults. Int J Geriatr Psychiatry 32: , 868–875. |
[20] | Wang C , Zhu J , Cai Y , Cui D , Wang Q , Mao Z ((2016) ) Community-based study of the relationship between social capital and cognitive function in Wuhan, China. Asia Pac J Public Health 28: , 717–724. |
[21] | Trivedi D ((2017) ) Cochrane review summary: Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Prim Health Care Res Dev 18: , 527–528. |
[22] | Desai AK , Grossberg GT , Sheth DN ((2004) ) Activities of daily living in patients with dementia: Clinical relevance, methods of assessment and effects of treatment. CNS Drugs 18: , 853–875. |
[23] | Jokelainen J , Timonen M , Keinanen-Kiukaanniemi S , Harkonen P , Jurvelin H , Suija K ((2019) ) Validation of the Zung self-rating depression scale (SDS) in older adults. Scand J Prim Health Care 37: , 353–357. |
[24] | Yang JW , Shi GX , Zhang S , Tu JF , Wang LQ , Yan CQ , Lin LL , Liu BZ , Wang J , Sun SF , Yang BF , Wu LY , Tan C , Chen S , Zhang ZJ , Fisher M , Liu CZ ((2019) ) Effectiveness of acupuncture for vascular cognitive impairment no dementia: A randomized controlled trial. Clin Rehabil 33: , 642–652. |
[25] | Wang S , Yang H , Zhang J , Zhang B , Liu T , Gan L , Zheng J ((2016) ) Efficacy and safety assessment of acupuncture and nimodipine to treat mild cognitive impairment after cerebral infarction: A randomized controlled trial. BMC Complement Altern Med 16: , 361. |
[26] | Zeng Y , Bao Y , Zhu M , Chen S , Fang J ((2015) ) [Mild cognitive impairment of stroke at subacute stage treated with acupuncture: A randomized controlled trial]. Zhongguo Zhen Jiu 35: , 979–982. |
[27] | Kalaria RN , Akinyemi R , Ihara M ((2016) ) Stroke injury, cognitive impairment and vascular dementia. Biochim Biophys Acta 1862: , 915–925. |
[28] | Zhang ZY , Liu Z , Deng HH , Chen Q ((2018) ) Effects of acupuncture on vascular dementia (VD) animal models: A systematic review and meta-analysis. BMC Complement Altern Med 18: , 302. |
[29] | Zhang X , Wu B , Nie K , Jia Y , Yu J ((2014) ) Effects of acupuncture on declined cerebral blood flow, impaired mitochondrial respiratory function and oxidative stress in multi-infarct dementia rats. Neurochem Int 65: , 23–29. |
[30] | Yu J , Liu C , Zhang X , Han J ((2005) ) Acupuncture improved cognitive impairment caused by multi-infarct dementia in rats. Physiol Behav 86: , 434–441. |
[31] | Yang J , Litscher G , Li H , Guo W , Liang Z , Zhang T , Wang W , Li X , Zhou Y , Zhao B , Rong Q , Sheng Z , Gaischek I , Litscher D , Wang L ((2014) ) The effect of scalp point cluster-needling on learning and memory function and neurotransmitter levels in rats with vascular dementia. Evid Based Complement Alternat Med 2014: , 294103. |
[32] | Ueno M ((2017) ) Elucidation of mechanism of blood-brain barrier damage for prevention and treatment of vascular dementia. Rinsho Shinkeigaku 57: , 95–109. |
[33] | Ye Y , Zhu W , Wang XR , Yang JW , Xiao LY , Liu Y , Zhang X , Liu CZ ((2017) ) Mechanisms of acupuncture on vascular dementia-A review of animal studies. Neurochem Int 107: , 204–210. |
[34] | Zeng BY , Salvage S , Jenner P ((2013) ) Effect and mechanism of acupuncture on Alzheimer’s disease. Int Rev Neurobiol 111: , 181–195. |
[35] | Davis DH , Creavin ST , Yip JL , Noel-Storr AH , Brayne C , Cullum S ((2015) ) Montreal Cognitive Assessment for the diagnosis of Alzheimer’s disease and other dementias. Cochrane Database Syst Rev 2015: , CD010775. |
[36] | Smith T , Gildeh N , Holmes C ((2007) ) The Montreal Cognitive Assessment: Validity and utility in a memory clinic setting. Can J Psychiatry 52: , 329–332. |
[37] | Wan XY , Yang, D.Y , The application of Montreal Cognitive Assessment and mini-mental state examination in the screen of cognitive disorder in the elderly. J Chengdu Med Coll 7: , 648–650. |
[38] | Wang YY , Wu X , Tang CL , Xu Y , Wang JR , Xu J , Huang J , Qiu GP , Sheng HJ , Zhu SJ ((2020) ) [Effect of electroacupuncture of different acupoint groups on learning-memory ability and expression of IL-1β and TNF-α in hippocampus and prefrontal cortex in rats with Alzheimer’s disease]. Zhen Ci Yan Jiu 45: , 617–622. |
[39] | Kim YI , Kim SS , Sin RS , Pu YJ , Ri G , Rim KS ((2018) ) Study on the cerebral blood flow regulatory features of acupuncture at acupoints of the governor vessel. Med Acupunct 30: , 192–197. |




