Vascular Mild Cognitive Impairment: Identifying Disease in Community-Dwelling Older Adults, Reducing Risk Factors, and Providing Support. The Osaki-Tajiri and Kurihara Projects
Abstract
Vascular mild cognitive impairment (MCI) is a critical disease. Its prognosis includes not only onset of vascular dementia, but also death by cardiovascular disease. The vascular risk factors for vascular MCI are treatable, and appropriate treatment can prevent or delay the progression to dementia. Therefore, this group is an excellent candidate for secondary prevention. However, community-dwelling older adults with vascular MCI are often undetected and are not clinically identified until they develop frank dementia. Furthermore, older adults with undetected vascular MCI often have decreased ability to follow their medication regimens and this poor medication adherence worsens their vascular comorbidities. This vicious cycle needs to be prevented through community-based interventions. There is evidence that treatment of hypertension or diabetes mellitus could lead to a reduced incidence of vascular MCI and dementia. In this review article, we first explain the background and etiology of vascular MCI. We then summarize phenotype of subcortical vascular dementia which is often unrecognized or “hidden” in the community. Then we introduce the Osaki-Tajiri and Kurihara Projects which have been conducted in Northern Japan, as an example of prevention projects aimed to identify early-stage vascular MCI in the community, reduce the risk factors and facilitate their treatment. Early identification of vascular MCI in the community could lead to a large reduction in the dementia burden worldwide. The outreach efforts presented here could be useful in developing secondary prevention strategies targeted to vascular MCI.
INTRODUCTION: VASCULAR MILD COGNITIVE IMPAIRMENT
Historical perspective: mild cognitive impairment
Mild cognitive impairment (MCI), the intermediate condition between normal aging and dementia, should be confirmed as early as possible for therapeutic intervention in order to prevent further deterioration. Two observational scales have been proposed: the Clinical Dementia Rating (CDR) [1, 2] and the Global Deterioration Scale (GDS) [3]. According to Morris et al. [4], CDR 0.5 (questionable dementia) already manifests with specific Alzheimer’s disease (AD) pathology, clearly different from that of normal aging (CDR 0). Also, CDR 0.5 older adults manifest neuropsychological impairments not only in memory but also in psychomotor speed and language. Thus, those with CDR 0.5 are considered to have very mild AD. Morris et al. [5] classified CDR 0.5 into three subgroups, i.e., CDR 0.5/uncertain dementia, CDR 0.5/incipient DAT (Dementia of the Alzheimer’s Type), and CDR 0.5/DAT. Previously we found [6] that those with CDR 0.5/DAT had severely deteriorated cognitive function without subjective memory complaints, suggesting that CDR 0.5 is better conceptualized as very mild clinical AD.
On the contrary, the GDS is based on the assumption that functional degenerative stages in AD appear to reverse the normal human development (the retrogenesis model [7]). The GDS stages of 1 and 2 fall within normal cognition, whereas the term MCI was first used by Reisberg et al. [8] in the description of GDS stage 3.
Petersen et al. re-proposed the concept of MCI [9]. This included normal daily activities and general intelligence, with memory complaints and memory dysfunction. MCI is differentiated from controls and even from very mild AD.
Clinical picture: issues to consider for vascular MCI
Vascular dementia (VaD) has a heterogeneous etiology and clinical course. Hachinski et al. [10] proposed the concept of vascular cognitive impairment (VCI) including a pre-stage of vascular dementia. The term VCI characterizes all forms of cognitive deficits from mild MCI of vascular origin to VaD [11, 12] The mild form of VCI is vascular MCI, and the most severe form of VCI is VaD [11, 12].
VCI could be a consequence of large vessel disease or small vessel disease or both. Large vessel disease (stroke) is more likely to cause dementia while cerebral small vessel disease is the most common cause of vascular MCI [13]. Neuroimaging is important for detecting CVD which is a cause of vascular MCI. Magnetic resonance imaging (MRI) represents the most commonly used neuroimaging technique. MRI markers of small vessels disease (white matter hyperintensities, small subcortical infarcts, enlarged perivascular spaces, and cerebral microbleeds) have been shown to correlate with cognitive impairment [14–18]. Standards for reporting vascular changes in neuroimaging (STRIVE) were proposed by an international working group of experts [19]. STRIVE has provided terms and definitions for lesions visible on MRI in small vessel disease including recent small subcortical infarcts (or lacunar infarcts), lacunes of presumed vascular origin, visible perivascular spaces, white matter hyperintensities of presumed vascular origin and cerebral microbleeds [19].
For further detail, (see Table 1) which summarizes some of the recent systematic reviews with a focus on vascular MCI since 2013 [20–25].
Table 1
Recent systematic reviews on vascular MCI before 2019
| Keywords | Authors | ||
| “mild cognitive impairment” | vascular | prevalence | van Rooij, 2016 [20] |
| Makin, 2013 [21] | |||
| “mild cognitive impairment” | vascular | neuropsychological | Sudo, 2015 [22]; Arevalo-Rodriguez, 2015 [23] |
| “mild cognitive impairment” | vascular | gait | Montero-Odasso, 2012 [24] |
| “mild cognitive impairment” | vascular | fall | Not applicable |
| “mild cognitive impairment” | vascular | intervention | Cheston, 2017 [25]; Arevalo-Rodriguez, 2015 [23] |
PubMed Date: 29 January 2019.
Erkinjuntti et al. [26] proposed the criteria for subcortical vascular dementia. Among its different subtypes, VCI associated with small vessel disease has an insidious onset due to gradually progressive vascular changes with a slowly progressive cognitive deterioration [26]. The differences in cognitive profiles between VCI and AD in the MCI phase are not immediately obvious. These groups of patients cannot be differentiated on the basis of simple cognitive assessments, such as the Mini-Mental State Examination (MMSE) [27, 28].
There are no significant clinical differences in the course of progression in the pre-dementia phase between patients with vascular MCI and amnestic MCI, even though their clinical courses differ after progressing to dementia [27]. Caution must be exercised before making a conclusion about vascular etiology of cognitive impairment in a particular patient, as cognitive function is highly variable in patients with small vessel disease, and the etiological significance of white matter lesions cannot be determined easily. There is a lack of direct correlation between white matter lesion load and cognitive function [29], and individuals with widespread white matter alterations might exhibit an age-appropriate cognitive profile [30]. Further, white matter changes might be present in patients with a coexisting cognitive disorder, such as Alzheimer’s disease [31]. We herein define vascular MCI as the MCI state of VCI or the CDR 0.5 status with cerebrovascular diseases (CVD).
Prevalence of vascular MCI
No systematic reviews on the prevalence of pure vascular MCI have been reported. However, two reviews of vascular MCI with dementia have reported prevalence rate of 21% by Makin et al. [32] and 30% by van Rooij et al. [20]. According to Harrison et al.’s systematic review [33], the prevalence of vascular MCI (vascular cognitive impairment, no dementia) varied from 24% [34] to 75% [35] in stroke-only populations, and from 4% [36] to 19% [37] in populations where stroke prevalence was low or not reported. There were several studies [38–41] showing the rates for different types which ranged from 3 to 41% depending on the classification, and one study used more than one definition to compare prevalence rates (range 10–50% depending on definition) [42].
Neurobehavioral and neuropsychological characteristics of vascular MCI
Vascular MCI is characterized by executive dysfunction, slowed information processing, memory deficit and mood and personality disorders [43]. The main neuropathological substrate for vascular MCI is a disruption of the fronto-subcortical networks due to white matter lesions. Other vascular lesions could also contribute to the cognitive impairment, damaging white matter and/or subcortical structures (thalamus and basal ganglia) [13].
There are various systematic reviews of the neuropsychological tests for vascular MCI [13, 44]. There were significant differences in all cognitive domains between VCI not demented (VCI-ND) and healthy controls, especially in processing speed, working memory, and visuospatial construction [13]. When compared with non-vascular MCI, subjects with VCI-ND had significantly greater deficits in processing speed and executive function, while those with non-vascular MCI had a greater relative deficit in delayed memory [13].
The most commonly used global cognitive screening instrument, MMSE, has low sensitivity in detecting MCI [45]. Using the MMSE, one study provided information about conversion from MCI to VaD, presenting a sensitivity of 36%, specificity of 80% with incidence of VaD of 6.2% [28]. Other widely used cognitive tests are the Montreal Cognitive Assessment (MoCA) and the Addenbrooke’s Cognitive Examination. Both showed high sensitivity and specificity for MCI [45–47]. The MoCA compares favorably to the MMSE as a screening test that is sensitive to the milder forms of cognitive impairment with cerebrovascular disease, however further longitudinal research is needed in the validity of the MoCA [44].
Other screening instruments have recently been developed specifically for vascular MCI. The Brief Memory and Executive Test includes tasks for executive functioning, processing speed, orientation and memory [48]. The Oxford Cognitive Screen incorporates tests for five cognitive domains: executive function, language, memory, number processing, and praxis [49].
One attempt to standardize the neuropsychological protocol for vascular MCI was the introduction of harmonization standards published by the National Institute of Neurological Disorders and Stroke (NINDS) and Canadian Stroke Network (CSN). These harmonization standards proposed a 60 min neuropsychological test protocol which assesses the following cognitive domains: executive functions (using categorical and letter fluency and WAIS-III Digit Symbol-Coding task), visuospatial functions (Rey-Osterrieth Complex Figure), language (Boston naming test), memory (Hopkins Verbal Learning Test-Revised or California Verbal Learning Test-2) and neuropsychiatric and depressive symptoms (Neuropsychiatric Inventory) [50].
Operational definitions of cognitive impairment (e.g., performance 1 or 1.5 standard deviations below that of an appropriate comparison group) are preferred over qualitative descriptions of cognitive symptoms [11].
Motoric cognitive risk syndrome provides a clinical approach to identify individuals at high risk for dementia, especially vascular dementia [51]. Since slower gait velocity and greater stride time variability are robust markers of mobility decline and falls, changes in these variables may lead to an early identification of vascular MCI and those at risk of falls [24, 52, 53].
VASCULAR RISK FACTORS
Development of vascular MCI
Cardiovascular risk factors play a fundamental role in the development of cognitive impairment [11]. However, the specific mechanism in which cardiovascular risk factors affect cognitive functioning is still unclear. The direction (positive or negative) of the effect may be dependent on the precise time of the personal lifespan. Two of the most important cardiovascular risk factors that play significant roles in the development of vascular MCI is arterial hypertension and blood pressure [54, 55]. Ambulatory blood pressure monitoring and home measured blood pressure (HMBP) are emerging as more reliable measurements than in-clinic blood pressure measurement. They are associated with a better correlation with target organ damage [55] including cognitive impairment.
Blood pressure
Hypertensive patients are at an elevated risk for MCI. A prospective study by Yaneva-Sirakova et al. [56] in hypertensive patients showed a correlation between higher blood pressure and MCI status. A significant, correlation between higher blood pressure variability and lower MoCA and MMSE test scores was also found.
These results are in accord with the conclusions derived from neuroimaging studies [57, 58]. They found that patients with elevated blood pressure variability have higher volume of white matter lesions than those with lower variability. One potential explanation for this association is that microvascular (including cerebrovascular) autoregulation is likely already impaired in hypertensive older adults with concomitant cardiovascular risk factors. Thus, increased blood pressure variability strains microcirculatory compensatory mechanisms beyond their limit. Periods of hypoperfusion are followed by normal or elevated blood flow. This may lead to disruption of the blood-brain barrier, small-vessel dysfunction, and impairment in the neural circuits.
Apart from blood pressure variability, the blood pressure measurements may also be associated with cognitive functioning [56, 59]. Older adults with hypertension, with HMBP <120/70 mmHg or ≥135/85 mmHg, were at an elevated risk for cognitive impairment and scored lower on neuropsychological tests than those with controlled blood pressure. The potential pathophysiological mechanism behind these results is the relative hypoperfusion of the brain after years-long adaptation to high blood pressure values. It is not clear though which is the leading cause and which is the consequence: the low blood pressure or cognitive impairment. Elevated blood pressure may be the reason for impairment in important brain centers, which may lead to deterioration of autonomic functioning and a persistent drop in blood pressure. On the other hand, low blood pressure due to treatment, may have a detrimental effect on target organs’ microvasculature, because of their previous adaptation to high blood pressure values.
Pulse pressure (PP) may be an independent risk factor for target organ damage. Yaneva-Sirakova et al. [60] showed that patients with elevated home PP (measured PP > 55 mmHg) had lower MoCA and MMSE test scores independent of other blood pressure variables. The patients with MCI had significantly higher 24 h, day and night PP values. Elevated PP in sub-optimally controlled hypertensive patients is an important independent factor for persisting target organ damage of the brain- clinically manifested with MCI. It should be evaluated routinely and treated properly in order to reduce their risk for cognitive impairment.
Central aortic pressure is a relatively new method for blood pressure measurement. It is considered a more accurate predictor of cardiovascular risk and mortality than the conventional brachial measurement. Yaneva-Sirakova et al. [61, 62] reported that the mean central pulse pressure values of patients with cognitive impairment were significantly higher than those without cognitive impairment. There was a weak negative correlation between central pulse pressure and the MoCA and MMSE test scores. Central arterial hemodynamics plays an important role in microcirculatory dysfunction and target organ damage in arterial hypertension. Central pulse pressure is a marker of arterial stiffness and a risk factor for target organ damage as well as cognitive impairment.
There are few studies on the correlation between central aortic blood pressure and cognitive impairment. Dias et al. [62] found a significant correlation between central aortic systolic pressure and intima-media thickness, and between cognitive impairment and central aortic systolic pressure. There are some large studies that confirmed the significance of central blood pressure for target organ damage [63], vascular hypertrophy, and extent of atherosclerosis, clinical outcomes and cardiovascular events [64–66]. But their role in cognitive impairment, and which parameter has the leading impact on early brain damage, are not clear so far. With age and cardiovascular risk factors, the arterial wall stiffens and the reflected wave travels at an accelerated speed, thus augmenting central systolic and pulse pressure, rather than diastolic [67]. Left ventricular afterload increases and coronary filling is compromised [68, 69]. Therefore, central hemodynamic parameters are suggested to correspond better with cardiovascular risk than peripheral blood pressure.
Atrial fibrillation
In patients with arterial hypertension non-valvular atrial fibrillation may raise the risk of MCI despite the use of anticoagulation therapy [70]. Patients with arterial hypertension, concomitant cardiovascular risk factors and atrial fibrillation had significantly lower neuropsychological test scores than patients with arterial hypertension, concomitant cardiovascular risk factors, but without atrial fibrillation.
IMPORTANCE OF OBSERVING OLDER RESIDENTS’ DAILY LIVES
The Tajiri & Kurihara Projects
Regarding the prevalence of MCI, unlike a rather clear difference between healthy controls and frank dementia, the more subtle difference between healthy controls and MCI can be affected by the method of sampling or by the neuropsychological tests used. It is important to examine community representative large samples and to perform neuropsychological tests sensitive enough to identify MCI. In the following section, we present the incidence and prevalence of vascular MCI based on the Tajiri & Kurihara Projects. Therefore, we followed our Prevalence Study conducted in 1998 (Prevalence Study 1998) [71, 72] with an Incidence Study in 2003 in Tajiri, Japan (Incidence Study 2003) [73, 74]. The data of the Kurihara Project (Prevalence Study 2008) was also analyzed [75, 76].
Briefly, our Prevalence Study in Tajiri conducted in 1998 included 497 randomly selected participants, including 346 CDR 0, 119 CDR 0.5, and 32 CDR ≥1. The first two groups were targeted for the follow-up Incidence Study in 2003. Based on the database, we reanalyzed the prevalence of subcortical VaD in the subjects with CDR 0.5 (vascular MCI) and VaD, prognosis with CVD, and two types of VaD onset (i.e., subcortical VaD and vascular MCI). The criteria for subcortical VaD were met by 67% of those with vascular dementia and by 7% of those with vascular MCI. In the cognitively normal group, CVD had no effect on prognosis; however, in the CDR 0.5 group, CVD had an effect on death by cardiovascular disease [73, 74].
In our incidence study, we found an incident VaD rate of 18% among adults aged 65 and older. Some cases developed VaD after a stroke (type I), whereas others first met the criteria for subcortical VaD with very mild stage MCI (CDR 0.5) and progressed to VaD (type II). We hypothesized that prognosis of vascular MCI included type II VaD or death due to causes associated with vascular risk factors.
The “hidden in the community” problem
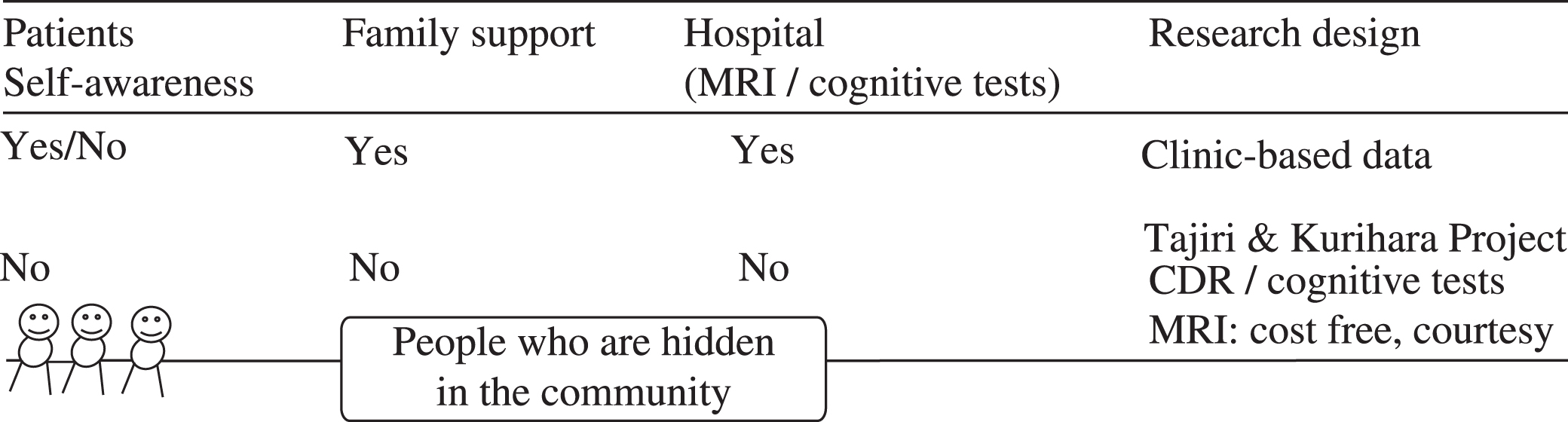
The patient clinic population might be the “tip of the iceberg.” These are the “fortunate” patients with awareness who are supported by families and who visit the outpatient clinic for care. On the contrary, suspected patients with unawareness or apathy not supported by families are easily hidden in the community. The concept is shown in (Fig. 1 and Table 2). Previously, we estimated the prevalence and severity of apathy in vascular MCI, amnestic MCI, and MCI of unknown type, and found that vascular MCI subjects have more severe apathy compared with amnestic MCI subjects on caregiver assessment (discussed detail in [77]). Gaining a full picture of those with vascular MCI requires work in the community. In the following sections, we report details of the techniques we have employed to identify those with vascular MCI “hidden in the communities” in ongoing studies in Japan, the Osaki-Tajiri and Kurihara Projects.
Fig.1
Database of outpatient clinics - The tip of an iceberg?
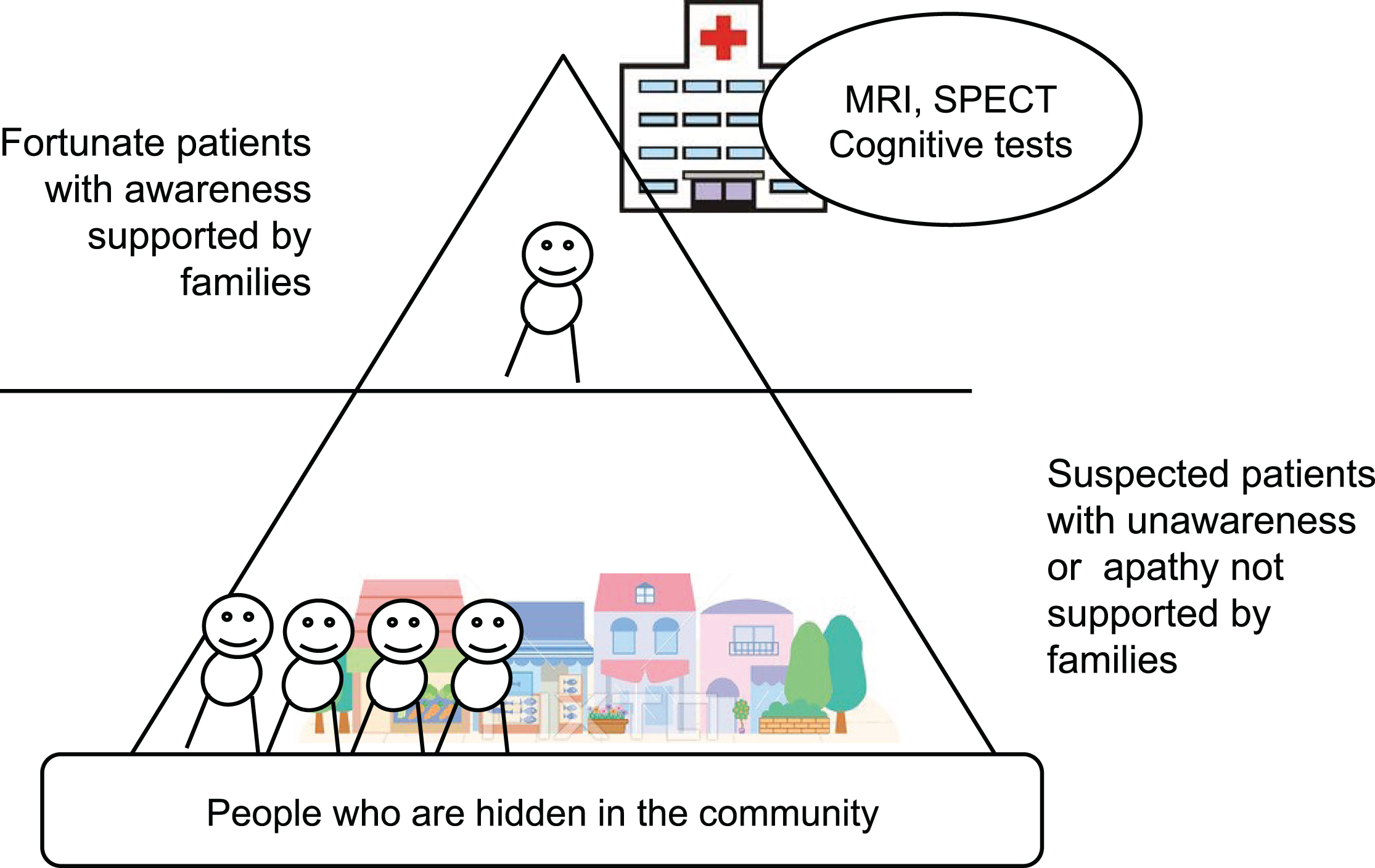
Table 2
Clinic-based data involves external validity problem?
 |
CDR assessment focusing on identifying vascular MCI
The CDR is based on memory impairment as the primary symptom since the scale is designed to detect early AD. However, non-memory conditions like frontal executive dysfunction are considered to be important for dementia, especially for the vascular contribution.
To evaluate daily lives of older residents with vascular MCI using the CDR, information from care managers or public health nurses are critical, especially for the CDR domains of Community Affairs, Home & Hobbies, and Personal Care.
The life concern form
The CDR is the international standard for this purpose, but requires long-term training to develop appropriate judgment skills. Based on our experience, we developed a “Life Concern Form” to detect people with vascular MCI in the community [78]. It was developed to assess daily lives of older adults living in the community by specifically observing the following items:
1) Activities they cannot perform in the manner as they used to do in the past;
2) Decreased activity levels at home;
3) Loss of interaction with people other than their family;
4) Need for assistance in taking medications; special attention needs to be paid to older adults taking medications for hypertension or diabetes mellitus with poor medication adherence.
Training of staff members specifically targeted to identify potential subjects with vascular MCI using the above questionnaire and focusing on specific items of CDR are encouraged.
INTERVENTION
Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) [79] examined a multidomain approach to prevent cognitive decline in at-risk elderly people in the community. Findings from their large (intervention 631 versus control 629), long-term, RCT suggest that a multidomain intervention could improve or maintain cognitive functioning in at-risk elderly people from the general population. Recently there is a report that lowering blood pressure will decrease the dementia risk [80]. We have been conducting an intervention study including exercise targeting older adults with vascular MCI in the town of Kurihara, Japan (the Kurihara project) [81]. As discussed earlier, the outpatient clinic population is only a small percentage of those affected by vascular MCI for whom fortunately there is a support network. On the contrary, patients without a support network are likely to be unaware of their disease, apathetic and remain hidden in the community. In the Kurihara Project, free transportation and MRI scans were provided to local residents. By providing free neuropsychological evaluations and MRIs, we aim to identify “hidden” MCI subjects in the community and recruit them into the intervention study. In our prevention study specifically targeted to vascular MCI [81], we examined the efficacy of three intervention approaches (cognitive stimulation or intervention (CI), physical exercise (PA), and group reminiscence approach (GRA)) on cognitive and physical functions and psychological well-being, based on a cluster randomized controlled trial (cluster RCT) design. We recruited 60 participants aged over 75 years with vascular MCI. Vascular MCI was defined as CDR 0.5 with cerebrovascular disease. Participants were randomized into four groups (CI, PA, GRA, and control). The interventions lasted 12 weeks and consisted of weekly sessions (twice per week) and homework. The cognitive and clinical outcomes included MMSE, Trail Making Test part A (TMT-A), Word Fluency, 6-meter-walk time, Geriatric Depression Scale, and quality of life. The CI intervention was found to increase MMSE scores and the PA intervention was found to improve walking speed. TMT-A, Word Fluency, and quality of life improved across all three interventions compared with the control group [81].
CONCLUSION: COMMUNITY-BASED MEASURES FOR MCI AND DEMENTIA
Vascular MCI is a critical disease. Its prognosis includes not only onset of vascular dementia, but also death by cardiovascular disease [82]. The vascular risk factors for vascular MCI are treatable, and appropriate treatment can reduce the incidence of cognitive impairment and dementia due to vascular causes. Prevention and delay of dementia through risk reduction has become increasingly important to reduce the prevalence of dementia worldwide [83]. As highlighted in this review article on vascular MCI, MCI with hypertension and diabetes is often unrecognized in the community and left untreated which further facilitates worsening of the prognosis due to poor management of risk factors and comorbidities. Special outreach efforts specifically targeted to this group include questionnaires focusing on symptoms of vascular MCI, training of staff to accurately assess CDR questions in relation to vascular MCI, and free transportation/access to MRI assessments. These community outreach efforts (as opposed to solely treating those who visit specialty clinics) are critically important for early identification of risk factors and their modifications to delay onset of frank dementia. Some of the efforts might require global initiatives through World Health Organization (WHO) and other entities, especially in low- and middle-income countries which have high prevalence of vascular risk factors and the incidence and prevalence of vascular MCI is likely to rise further. The recent establishment of The International Research Network on Dementia Prevention (IRNDP) initiatives could play a role in facilitating this effort [83].
ACKNOWLEDGMENTS
We are grateful to the discussion at ICVD 2016 conference with Drs. Milica G. Kramberger, Vuk Milosevic, Teodora Yaneva-Sirakova, Berlot Rok, Abantas-Diamla Sharimah, Junko Takada, Latchezar Traykov, Rumiana Tarnovska-Kadreva, and Amos D Korczyn. We are thankful for Ms. Nora Mattek for her superb editing.
Authors’ disclosures available online (https://www.j-alz.com/manuscript-disclosures/18-0899r1).
REFERENCES
[1] | Hughes CP , Berg L , Danziger WL , Coben LA , Martin RL ((1982) ) A new clinical scale for the staging of dementia. Br J Psychiatr 140: , 566–572. |
[2] | Morris JC ((1993) ) The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology 43: , 2412–2414. |
[3] | Reisberg B , Ferris SH , de Leon MJ , Crook T ((1982) ) The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatry 139: , 1136–1139. |
[4] | Morris JC , McKeel DW Jr , Storandt M , Rubin EH , Price JL , Grant EA , Ball MJ , Berg L ((1991) ) Very mild Alzheimer’s disease: Informant-based clinical, psychometric, and pathologic distinction from normal aging. Neurology 41: , 469–478. |
[5] | Morris J , Storandt M , Miller JP , McKeel DW , Price JL , Rubin EH , Berg L ((2001) ) Mild cognitive impairment represents early-stage Alzheimer’s disease. Arch Neurol 58: , 397–405. |
[6] | Meguro K , Ishii H , Yamaguchi S , Ishizaki J , Sato M , Hashimoto R , Meguro M , Lee E , Tanaka Y , Kasuya M , Sekita Y ((2004) ) Prevalence and cognitive performances of Clinical Dementia Rating 0.5 and mild cognitive impairment in Japan: The Tajiri Project. Alzheimer Dis Assoc Disord 18: , 3–10. |
[7] | Reisberg B , Kenowsky S , Fransses E , Auer SR , Souren LE ((1999) ) Towards a science of Alzheimer’s disease management: A model based upon current knowledge of retrogenesis. Int Psychogeriatr 11: , 7–23. |
[8] | Flicker C , Ferris SH , Reisberg B ((1991) ) Mild cognitive impairment in the elderly: Predictors of dementia. Neurology 41: , 1006–1009. |
[9] | Petersen RC , Smith GE , Waring SC , Ivnik RJ , Tangalos EG , Kokmen E ((1999) ) Mild cognitive impairment: Clinical characterization and outcome. Arch Neurol 56: , 303–308. |
[10] | Hachinski V ((1997) ) Vascular dementia: The need for a new approach. J Int Med 242: , 277–279. |
[11] | Gorelick PB , Scuteri A , Black SE , Decarli C , Greenberg SM , Iadecola C , Launer LJ , Laurent S , Lopez OL , Nyenhuis D , Petersen RC , Schneider JA , Tzourio C , Arnett DK , Bennett DA , Chui HC , Higashida RT , Lindquist R , Nilsson PM , Roman GC , Sellke FW , Seshadri S ; American Heart Association Stroke Council, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on Cardiovascular Radiology and Intervention and Council on Cardiovascular Surgery and Anesthesia ((2011) ) Vascular contributions to cognitive impairment and dementia: A statement for healthcare professionals from the American heart association/American stroke association. Stroke 42: , 2672–2713. |
[12] | Van der Flier WM , Skoog I , Schneider JA , Pantoni L , Mok V , Chen CLH , Scheltens P ((2018) ) Vascular cognitive impairment. Nat Rev Dis Primers 4: , 18003. |
[13] | Vasquez BP , Zakzanis KK ((2015) ) The neuropsychological profile of vascular cognitive impairment not demented: A meta-analysis. J Neuropsychol 9: , 109–136. |
[14] | Debette S , Markus H ((2010) ) The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: Systematic review and meta-analysis. BMJ 341: , c3666. |
[15] | Patel B , Lawrence AJ , Chung AW , Rich P , Mackinnon AD , Morris RG , Barrick TR , Markus HS ((2013) ) Cerebral microbleeds and cognition in patients with symptomatic small vessel disease. Stroke 44: , 356–361. |
[16] | Vermeer SE , Longstreth WT , Koudstaal PJ ((2007) ) Silent brain infarcts: A systematic review. Lancet Neurol 6: , 611–619. |
[17] | MacLullich A , Wardlaw J , Ferguson K , Starr JM , Seckl JR , Deary IJ ((2004) ) . Enlarged perivascular spaces are associated with cognitive function in healthy elderly men. J Neurol Neurosurg Psychiatry 75: , 1519–1523. |
[18] | Silbert LC , Howieson DB , Dodge H , Kaye JA ((2009) ) Cognitive impairment risk: White matter hyperintensity progression matters. Neurology 73: , 120–125. |
[19] | Wardlaw JM , Smith EE , Biessels GJ , Cordonnier C , Fazekas F , Frayne R , Lindley RI , O’Brien JT , Barkhof F , Benavente OR , Black SE , Brayne C , Breteler M , Chabriat H , Decarli C , de Leeuw FE , Doubal F , Duering M , Fox NC , Greenberg S , Hachinski V , Kilimann I , Mok V , Oostenbrugge Rv , Pantoni L , Speck O , Stephan BC , Teipel S , Viswanathan A , Werring D , Chen C , Smith C , van Buchem M , Norrving B , Gorelick PB , Dichgans M ; Standards for ReportIng Vascular changes on neuroimaging (STRIVE v1) ((2013) ) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12: , 822–838. |
[20] | van Rooij FG , Kessels RP , Richard E , De Leeuw FE , van Dijk EJ ((2016) ) Cognitive impairment in transient ischemic attack patients: A systematic review. Cerebrovasc Dis 42: , 1–9. |
[21] | Makin SD , Turpin S , Dennis MS , Wardlaw JM ((2013) ) Cognitive impairment after lacunar stroke: Systematic review and meta-analysis of incidence, prevalence and comparison with other stroke subtypes. J Neurol Neurosurg Psychiatry 84: , 893–900. |
[22] | Sudo FK , Alves GS , Tiel C , Ericeira-Valente L , Moreira DM , Laks J , Engelhardt E ((2015) ) Neuroimaging criteria and cognitive performance in vascular mild cognitive impairment: A systematic review. Dement Neuropsychol 9: , 394–404. |
[23] | Arevalo-Rodriguez I , Smailagic N , Roqué I Figuls M , Ciapponi A , Sanchez-Perez E , Giannakou A , Pedraza OL , Bonfill Cosp X , Cullum S ((2015) ) Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev 5: , CD010783. |
[24] | Montero-Odasso M , Annweiler C , Hachinski V , Islam A , Yang N , Vasudev A ((2015) ) Vascular burden predicts gait, mood, and executive function disturbances in older adults with mild cognitive impairment: Results from the gait and brain study. J Am Geriatr Soc 60: , 1988–1990. |
[25] | Cheston R , Ivanecka A ((2017) ) Individual and group psychotherapy with people diagnosed with dementia: A systematic review of the literature. Int J Geriatr Psychiatry 32: , 3–31. |
[26] | Erkinjuntti T , Inzitari D , Pantoni L , Wallin A , Scheltens P , Rockwood K , Roman GC , Chui H , Desmond DW ((2000) ) Research criteria for subcortical vascular dementia in clinical trials. J Neural Transm 59: (Suppl), 23–30. |
[27] | Meyer JS , Xu G , Thornby J , Chowdhury MH , Quach M ((2002) ) Is mild cognitive impairment prodromal for vascular dementia like Alzheimer’s disease? Stroke 33: , 1981–1985. |
[28] | Arevalo-Rodriguez I , Smailagic N , Roqué i Figuls M , Ciapponi A , Sanchez-Perez E , Giannakou A , Pedraza OL , Bonfill Cosp X , Cullum S ((2015) ) Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev, CD010783. |
[29] | Sabri O , Ringelstein EB , Hellwig D , Schneider R , Schreckenberger M , Kaiser HJ , Mull M , Buell U ((1999) ) Neuropsychological impairment correlates with hypoperfusion and hypometabolism but not with severity of white matter lesions on MRI in patients with cerebral microangiopathy. Stroke 30: , 556–566. |
[30] | Duning T , Kugel H , Knecht S ((2005) ) Excellent cognitive performance despite massive cerebral white matter changes. Neuroradiology 47: , 749–52. |
[31] | Leeuw FW , Barkhof F , Scheltens P ((2004) ) Alzheimer’s disease – one clinical syndrome, two radiological expressions: A study on blood pressure. J Neurol Neurosurg Psychiatry 5: , 1270–1274. |
[32] | Makin SD , Turpin S , Dennis MS , Wardlaw JM ((2013) ) Cognitive impairment after lacunar stroke: Systematic review and meta-analysis of incidence, prevalence and comparison with other stroke subtypes. J Neurol Neurosurg Psychiatry 84: , 893–900. |
[33] | Harrison SL , Tang EY , Keage HA , Taylor JP , Allan L , Robinson L , Jagger C , Rockwood K , Stephan BC ((2016) ) A systematic review of the definitions of vascular cognitive impairment, no dementia in Cohort studies. Dement Geriatr Cogn Dis 42: , 69–79. |
[34] | Stephens S , Kenny RA , Rowan E , Allan L , Kalaria RN , Bradbury M , Ballard CG ((2004) ) Neuropsychological characteristics of mild vascular cognitive impairment and dementia after stroke. Int J Geriatr Psychiatry 19: , 1053–1057. |
[35] | Rasquin SM , Van Oostenbrugge RJ , Verhey FR , Lodder J ((2007) ) Vascular mild cognitive impairment is highly prevalent after lacunar stroke but does not increase over time: A 2-year follow-up study. Dement Geriatr Cogn Disord 24: , 396–401. |
[36] | Middleton L , Kirkland S , Rockwood K ((2008) ) Prevention of CIND by physical activity: Different impact on VCI-ND compared with MCI. J Neurol Sci 269: , 80–84. |
[37] | Hsiung GYR , Donald A , Grand J , Black SE , Bouchard RW , Gauthier SG , Loy-English I , Hogan DB , Kertesz A , Rockwood K , Feldman HH ((2006) ) Outcomes of cognitively impaired not demented at 2 years in the Canadian cohort study of cognitive impairment and related dementias. Dement Geriatr Cogn Disord 22: , 413–420. |
[38] | Dong Y , Sharma VK , Chan BP , Venketasubramanian N , Teoh HL , Seet RC , Tanicala S , Chan YH , Chen C ((2010) ) The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J Neurol Sci 299: , 15–18. |
[39] | Dong Y , Venketasubramanian N , Chan BP , Sharma VK , Slavin MJ , Collinson SL , Sachdev P , Chan YH , Chen CL ((2012) ) Brief screening tests during acute admission in patients with mild stroke are predictive of vascular cognitive impairment 3-6 months after stroke. J Neurol Neurosurg Psychiatry 83: , 580–585. |
[40] | Dong Y , Slavin MJ , Chan BP , Venketasubramanian N , Sharma VK , Collinson SL , Sachdev PS , Chen CL ((2014) ) Improving screening for vascular cognitive impairment at three to six months after mild ischemic stroke and transient ischemic attack. Int Psychogeriatr 26: , 787–793. |
[41] | Akinyemi RO , Allan L , Owolabi MO , Akinyemi JO , Ogbole G , Ajani A , Firbank M , Ogunniyi A , Kalaria RN ((2014) ) Profile and determinants of vascular cognitive impairment in African stroke survivors: The CogFAST Nigeria Study. J Neurol Sci 346: , 241–249. |
[42] | Yu KH , Cho SJ , Oh MS , Jung S , Lee JH , Shin JH , Koh IS , Cha JK , Park JM , Bae HJ , Kang Y , Lee BC ; Korean-Vascular Cognitive Impairment Harmonization Standards Study Group ((2013) ) Cognitive impairment evaluated with Vascular Cognitive Impairment Harmonization Standards in a multicenter prospective stroke cohort in Korea. Stroke 44: , 786–788. |
[43] | Leys D , Englund E , Erkinjuntti T ((2003) ) Vascular dementia. In Evidence-based dementia practice, Qizilbash N, ed. Blackwell Publishing Company, Oxford, UK. |
[44] | Koski L ((2013) ) Validity and applications of the Montreal cognitive assessment for the assessment of vascular cognitive impairment. Cerebrovasc Dis 36: , 6–18. |
[45] | Pendlebury ST , Mariz J , Bull L , Mehta Z , Rothwell PM ((2012) ) MoCA, ACE-R, and MMSE Versus the National Institute of Neurological Disorders and Stroke–Canadian Stroke Network Vascular Cognitive Impairment Harmonization Standards Neuropsychological Battery After TIA and Stroke. Stroke 43: , 464–469. |
[46] | Nasreddine ZS , Phillips NA , Bédirian V , Charbonneau S , Whitehead V , Collin I , Cummings JL , Chertkow H ((2005) ) The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53: , 695–699. |
[47] | Mioshi E , Dawson K , Mitchell J , Arnold R , Hodges JR ((2006) ) The Addenbrooke’s Cognitive Examination Revised (ACE-R): A brief cognitive test battery for dementia screening. Int J Geriatr Psychiatry 21: , 1078–1085. |
[48] | Brookes RL , Hannesdottir K , Lawrence R , Morris RG , Markus HS ((2012) ) Brief Memory and Executive Test: Evaluation of a new screening test for cognitive impairment due to small vessel disease. Age Ageing 41: , 212–218. |
[49] | Demeyere N , Riddoch MJ , Slavkova ED , Bickerton WL , Humphreys GW ((2015) ) The Oxford Cognitive Screen (OCS): Validation of a stroke-specific short cognitive screening tool. Psychol Assess 27: , 883–894. |
[50] | Hachinski V , Iadecola C , Petersen RC , Breteler MM , Nyenhuis DL , Black SE , Powers WJ , DeCarli C , Merino JG , Kalaria RN , Vinters HV , Holtzman DM , Rosenberg GA , Wallin A , Dichgans M , Marler JR , Leblanc GG ((2006) ) National Institute of Neurological Disorders and Stroke-Canadian stroke network vascular cognitive impairment harmonization standards. Stroke 37: , 2220–2241. |
[51] | Verghese J , Wang C , Lipton RB , Holtzer R ((2013) ) Motoric cognitive risk syndrome and the risk of dementia. J Gerontol A Biol Sci Med Sci 68: , 412–418. |
[52] | Annweiler C , Beauchet O , Bartha R , Wells JL , Borrie MJ , Hachinski V , Montero-Odasso M ((2013) ) Motor cortex and gait in mild cognitive impairment: A magnetic resonance spectroscopy and volumetric imaging study. Brain 136: , 859–871. |
[53] | Dodge HH , Mattek NC , Austin D , Hayes TL , Kaye JA ((2012) ) In-home walking speeds and variability trajectories associated with mild cognitive impairment. Neurology 78: , 1946–1952. |
[54] | Yaneva-Sirakova T , Tarnovska-Kadreva R , Traykov L ((2012) ) The role of suboptimal home-measured blood pressure control for cognitive decline. Dement Geriatr Cogn Dis Extra 2: , 112–119. |
[55] | Mancia G , Fagard R , Narkiewiecz K , Redón J , Zanchetti A , Böhm M , Christiaens T , Cifkova R , De Backer G , Dominiczak A , Galderisi M , Grobbee DE , Jaarsma T , Kirchhof P , Kjeldsen SE , Laurent S , Manolis AJ , Nilsson PM , Ruilope LM , Schmieder RE , Sirnes PA , Sleight P , Viigimaa M , Waeber B , Zannad F ; Task Force Members ((2013) ) ESH/ESC Guidelines for the management of arterial hypertension. J Hypertens 31: , 1281–357. |
[56] | Yaneva-Sirakova T , Tarnovska-Kadreva R , Traykov L ((2013) ) Blood pressure variability and mild cognitive impairment. Bulg J Cardiol 1: , 5–14. |
[57] | Gómez-Angelats N , de la Sierra A , Sierra C , Parati G , Mancia G , Coca ((2004) ) Blood pressure variability and silent cerebral damage in essential hypertension. Am J Hypertens 17: , 696–700. |
[58] | Kario K , Matsuo T , Kobayashi H , Imiya M , Matsuo M , Shimada K ((1996) ) Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Hypertension 27: , 130–135. |
[59] | Yaneva-Sirakova T , Tarnovska-Kadreva R , Traykov L ((2013) ) Blood pressure target values and the risk for cognitive impairment. J Hypertens 31: , e-Suppl.A, e253. |
[60] | Yaneva-Sirakova T , Tarnovska-Kadreva R , Traykov L ((2012) ) Pulse pressure and mild cognitive impairment. J Cardiovasc Med (Hagerstown) 13: , 735–740. |
[61] | Yaneva-Sirakova T , Tarnovska-Kadreva R , Traykov L ((2013) ) Central aortic pulse pressure as a risk factor for cognitive impairment. Bulg J Cardiol 2: , 45–58. |
[62] | Dias E , Giollo L , Martinelli D , Mazeti C , Júnior HM , Vilela-Martin JF , Yugar-Toledo JC ((2012) ) Carotid intima-media thickness is associated with cognitive deficiency in hypertensive patients with elevated central systolic blood pressure. Cardiovasc Ultrasound 10: , 41. |
[63] | Roman M , Devereux R , Kizer J , Okin PM , Lee ET , Wang W , Umans JG , Calhoun D , Howard ((2009) ) High central pulse pressure is independently associated with adverse cardiovascular outcome. J Am Coll Cardiol 54: , 1730–1734. |
[64] | Roman M , Devereux R , Kizer J , Lee ET , Galloway JM , Ali T , Umans JG , Howard BV ((2007) ) Central pressure more strongly relates to vascular disease and outcome than does brachial pressure: The Strong Heart Study. Hypertension 50: , 197–203. |
[65] | Williams B , Lacy P , Thom S , Cruickshank K , Stanton A , Collier D , Hughes AD , Thurston H , O’Rourke M ; CAFE Investigators; Anglo-Scandinavian Cardiac Outcomes Trial Investigators; CAFE Steering Committee and Writing Committee ((2006) ) Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes. Circulation 113: , 1213–1225. |
[66] | Williams B , Lacy P ((2009) ) Central aortic pressure and clinical outcomes. J Hypertens 27: , 1123–1125. |
[67] | Safar M , Jankowski P ((2009) ) Central blood pressure and hypertension: Role in cardiovascular risk assessment. Clin Sci 116: , 273–282. |
[68] | Laurent S , Cockcroft J , Van Bortel L , Boutouyrie P , Giannattasio C , Hayoz D , Pannier B , Vlachopoulos C , Wilkinson I , Struijker-Boudier H ; European Network for Non-invasive Investigation of Large Arteries ((2006) ) Expert consensus document on arterial stiffness: Methodological issues and clinical applications. Eur Heart J 27: , 2588–2605. |
[69] | London G , Asmar R , O’Rourke M , Safar M ((2004) ) Mechanism(s) of selective systolic blood pressure reduction after a low-dose combination of perindopril/indapamide in hypertensive subjects: Comparison with atenolol. J Am Coll Cardiol 43: , 92–99. |
[70] | Yaneva-Sirakova T , Tarnovska-Kadreva R , Traykov L ((2013) ) Atrial fibrillation and mild cognitive impairment. Alzheimer Dement 9: , 770–771. |
[71] | Meguro K , Ishii H , Yamaguchi S , Ishizaki J , Shimada M , Sato M , Hashimoto R , Shimada Y , Meguro M , Yamadori A , Sekita Y ((2002) ) Prevalence of dementia and dementing diseases in Japan: The Tajiri Project. Arch Neurol 59: , 1109–1114. |
[72] | Nakata E , Kasai M , Kasuya M , Akanuma K , Meguro M , Ishii H , Yamaguchi S , Meguro K ((2009) ) Combined memory and executive function tests can screen mild cognitive impairment and converters to dementia in a community: The Osaki-Tajiri project. Neuroepidemiology 33: , 103–110. |
[73] | Meguro K , Ishii H , Kasuya M , Akanuma K , Meguro M , Kasai M , Lee E , Hashimoto R , Yamaguchi S , Asada T ((2007) ) Incidence of dementia and associated risk factors in Japan: The Osaki-Tajiri Project. J Neurol Sci 260: , 175–182. |
[74] | Meguro K ((2007) ) Community based measures for managing mild cognitive impairment: The Osaki-Tajiri Project. Psychogeriatrics 7: , 132–136. |
[75] | Meguro K , Tanaka N , Kasai M , Nakamura K , Ishikawa H , Nakatsuka M , Satoh M , Ouchi Y ((2012) ) Prevalence of dementia and dementing diseases in the old-old population in Japan: The Kurihara Project: Implications for Long-Term Care Insurance data. Psychogeriatrics 12: , 226–234. |
[76] | Meguro K , Tanaka N , Nakatsuka M , Nakamura K , Satoh M ((2012) ) Vascular lesions in mixed dementia, vascular dementia, and Alzheimer disease with cerebrovascular disease: The Kurihara Project. J Neurol Sci 322: , 157–160. |
[77] | Nakamura K , Kasai M , Ouchi Y , Nakatsuka M , Tanaka N , Kato Y , Nakai M , Meguro K ((2013) ) Apathy is more severe in vascular than amnestic mild cognitive impairment in a community: The Kurihara Project. Psychiatry Clin Neurosci 67: , 517–525. |
[78] | Takada J , Meguro K , Sato Y , Chiba Y ; Kurihara Project members ((2014) ) Life concerns of elderly people living at home determined as by Community General Support Center staff: Implications for organizing a more effective integrated community care system. The Kurihara Project. Psychogeriatrics 14: , 188–95. |
[79] | Ngandu T , Lehtisalo J , Solomon A , Levälahti E , Ahtiluoto S , Antikainen R , Bäckman L , Hänninen T , Jula A , Laatikainen T , Lindström J , Mangialasche F , Paajanen T , Pajala S , Peltonen M , Rauramaa R , Stigsdotter-Neely A , Strandberg T , Tuomilehto J , Soininen H , Kivipelto M ((2015) ) A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomized controlled trial. Lancet 385: , 2255–2263. |
[80] | Lower systolic blood pressure, sexual minority seniors, women’s reproductive history: Lessons from AAIC 2018 ((2018) ), Alzheimer Dement 14: , 1383–1385. |
[81] | Nakatsuka M , Nakamura K , Hamanosono R , Takahashi Y , Kasai M , Sato Y , Suto T , Nagatomi R , Meguro K ((2015) ) A cluster randomized controlled trial of nonpharmacological interventions for old-old subjects with a Clinical Dementia Rating of 0.5: The Kurihara Project. Dement Geriatr Cogn Disord Extra 5: , 221–232. |
[82] | Meguro K , Akanuma K , Meguro M , Kasai M , Ishii H , Yamaguchi S ((2012) ) Prognosis of vascular mild cognitive impairment Includes vascular dementia onset and death by cardiovascular disease: Reanalysis from the Osaki-Tajiri Project. J Stroke Cerebrovasc Dis 21: , 607–611. |
[83] | Anstey KJ , Peters R , Clare L , Lautenschlager NT , Dodge HH , Barnes DE , Shahar S , Brodaty H , Rees G ((2018) ) Joining forces to prevent dementia: The International Research Network on Dementia Prevention (IRNDP). Int Psychogeriatrics 29: , 1757–1760. |




