Geographical Variation in Antipsychotic Drug Use in Elderly Patients with Dementia: A Nationwide Study
Abstract
Background: Use of antipsychotics in elderly patients with dementia has decreased in the past decade due to safety regulations; however use is still high. Geographical variation may indicate discrepancies in clinical practice and lack of adherence to evidence-based guidelines for the management of behavioral symptoms.
Objective: To investigate potential geographical variances in use of antipsychotic drugs in dementia care.
Methods: A registry-based cross-sectional study in the entire elderly population of Denmark (≥65 years) conducted in 2012. Data included place of residence, prescriptions filled, and hospital discharge diagnoses. Antipsychotic drug use among elderly with (n = 34,536) and without (n = 931,203) a dementia diagnosis was compared across the five regions and 98 municipalities in Denmark, adjusted for age and sex.
Results: In 2012, the national prevalence of antipsychotic drug use was 20.7% for elderly patients with dementia, with a national incidence of 3.9%. The prevalence ranged from 17.0% to 23.3% in the five regions and from 7.5% to 33.1% in the 98 municipalities, demonstrating an over four-fold difference.
Conclusion: The observed geographical variation was more pronounced at municipal level as compared to regional level, suggesting that the variation may be related to variances in clinical practice in primary care. This study highlights an urgent need for further educating professional carers and physicians to guide non-pharmacological as well as pharmacological management of neuropsychiatric symptoms in elderly patients with dementia.
INTRODUCTION
Antipsychotics are used for treatment of certain neuropsychiatric symptoms in elderly patients with dementia, e.g., agitation, aggression, and psychotic symptoms [1]. However, the clinical effectiveness of typical and atypical antipsychotic drugs on these symptoms in patients with dementia is questionable [2–4]. The potential modest clinical effect of antipsychotic treatment needs to be balanced against numerous adverse events, including parkinsonian side effects, sedation, gait disturbance, accelerated cognitive decline, pneumonia and other infections, and thromboembolic events [1, 5]. Antipsychotics have also been associated with increased mortality risk [6], which has led the U.S. Food and Drug Administration and the European Medicines Agency to issue warnings in 2005 and 2008 regarding the mortality risk associated with use of typical and atypical antipsychotics in elderly patients with dementia [7, 8]. Best practice guidelines emphasize the need for initial assessment and treatment of contributing medical conditions, such as infections, dehydration and pain, and non-pharmacological interventions as first-line approach for management of behavioral symptoms in patients with dementia, although short-term treatment with antipsychotics may be warranted in selected patients [9].
Following the warnings, some countries launched initiatives to decrease the consumption of antipsychotics. As a result, the use of antipsychotics in elderly patients with dementia decreased in the past decade. The NHS England national prescribing audit showed a reduction in antipsychotic users from 17.0% in 2006 to 6.8% in 2011 in patients with dementia of all ages [10]. Likewise, Scotland and France demonstrated a similar decrease in use [11, 12]. In many other countries, use is still high [13–15]. In Denmark, use remains high despite a reduction from 31.3% in 2000 to 20.4% in 2012 of antipsychotic users with dementia ≥65 years of age [16]. The reasons for the high consumption of antipsychotics in patients with dementia are unknown, but the appropriateness of use has been questioned.
Geographical variation in the use of antipsychotics may indicate discrepancies in clinical practice and lack of adherence to evidence-based guidelines for the management of behavioral symptoms. Thus, geographical variation unexplained by other demographic or medical factors may indicate a mismatch between clinical practice and clinical guidelines in certain geographical areas. Danish registries are unique with respect to capturing an entire population and featuring detailed information on drug utilization [17]. Knowledge about geographical differences in the Danish population may provide further insight into the extent and nature of variation in clinical practice in the care of neuropsychiatric symptoms in an international context.
Thus, in order to determine possible factors contributing to the relatively high consumption of antipsychotics in Denmark, we aimed to investigate potential geographical variation. Consequently, we conducted a nationwide registry-based study in the entire elderly population of Denmark, comparing prevalence, incidence, and, duration of antipsychotic treatment in elderly with and without a diagnosis of dementia in 2012 between the Danish regions and municipalities.
MATERIALS AND METHODS
Study design and ethics
The study was designed as an observational cross-sectional study using data from nationwide Danish registries.
The study was approved by the Danish Data Protection Agency (ID no: 2007-58-0015/30-0667), Statistics Denmark, and the Danish Health and Medicine Authority (ID no: 6-8011-907/1). All data were anonymized and Danish law did not require ethic committee approval or informed patient consent.
Registry data sources
All permanent residents are assigned a personal civil registration number at the time of birth or immigration [18], which allows for retrieval of data at an individual level in nationwide registries [17]. The National Patient Registry contains all hospitalizations and invasive procedures registered since 1977 and all contacts to outpatient clinics and emergency departments since 1995 [19]. The Psychiatric Central Research Registry includes data on all psychiatric inpatient admissions since April 1, 1969, and outpatient contacts since 1995 [20]. Information comprises dates and discharge diagnosis, registered according to World Health Organization’s (WHO) International Classification of Diseases (ICD) codes. ICD-8 was used from 1970 to 1993 and ICD-10 from 1994 and onwards. The Danish National Prescription Registry has registered dispensed prescriptions consecutively since 1995, including prescriptions to elderly residing in nursing homes. The drugs are registered according to the Anatomical Therapeutic Chemical (ATC) classification system, with information on amount and strength of dispensed drugs as well as dispensing dates [21].
Demographic information
Denmark is divided into five regions and 98 municipalities. The regions are responsible for hospitals and for private practice specialists and general practitioners (GPs). The municipalities are local administrative bodies responsible for public healthcare, and for primary care including home care and nursing homes for the elderly. Information about place of residence, age, gender, and marital status was retrieved from the Danish Civil Registration System, while information on living status (nursing homes) was retrieved from Statistics Denmark. Since the municipalities are subunits of the regions, each individual in the study population is both accounted for in the regional and municipality analyses.
Study population
All Danish residents aged ≥65 years and alive on January 1, 2012, were identified using the Central Population Registry. The place of residence (region and municipality) on January 1, 2012, was identified using the Danish Civil Registration System. Patients with a dementia diagnosis were identified as those who had been registered with a dementia diagnosis in the National Patient Registry or Psychiatric Central Research Registry before January 1, 2012, during admission or at an outpatient visit and/or those who had filled an anti-dementia drug prescription (ATC: N06D). The individuals had to be ≥60 years at the time of the dementia diagnosis and/or first prescription because the validity of the diagnosis in those <60 years has been shown to be low [22]. The validity of registered dementia diagnoses in those ≥65 years, in contrast, has previously been shown to be high [23]. The remaining individuals formed the reference group.
Antipsychotic treatment
Prevalent users of antipsychotic drugs were defined as individuals who had at least one antipsychotic prescription filled in 2012. Incident users were defined as elderly who had their first ever antipsychotic prescription filled in 2012 since 1995. Antipsychotic drugs were classified according to ATC codes (N05A), excluding lithium. Antipsychotic drugs were assigned a defined daily dose (DDD), defined by WHO as the average maintenance dose per day for a drug used for its main indication in adults. As one DDD represents one day of treatment, the number of DDDs prescribed in 2012 was used as a marker for treatment duration.
Comorbidity
Comorbidity was assessed at baseline (January 1, 2012). Data from somatic and psychiatric hospital contacts was used to identify comorbid conditions that could potentially influence antipsychotic drug use. The Charlson comorbidity index comprises 19 chronic somatic diseases and was used to assess comorbidity [24]. Psychiatric comorbidity was defined as a registered diagnosis of prior psychotic disorders [one of the following diagnoses: schizophrenia, schizotypal, delusional disorders (ICD-8:295.x9, 296.89, 297.x9, 298.29-298.29-298.99, 299.04, 299.05, 299.09, 301.8; ICD-10: F20-29); and, manic episode and bipolar affective disorder (ICD-8:296.19, 296.39, 298.19; ICD-10: F30-F31)] registered any time since 1969 before the dementia diagnosis. The total number of different drugs used in 2011 was employed as a surrogate marker of somatic disease not captured by hospital admissions (ATC level 3, e.g., A10A: insulins and analogues).
Statistical analysis
Normality of continuous variables was graphically determined using histograms. The percentage of antipsychotic users in the various regions was compared using Pearson’s χ2-test and a Kruskal-Wallis test for analysis of variance. Logistic regression analyses were performed to evaluate the effect of individual covariates (crude analysis) on the likelihood of receiving an antipsychotic drug. A multivariate logistic regression analysis was performed to control for age, sex, and comorbidity, including Charlson comorbidity index, psychotic disorder prior to dementia diagnosis, and total number of drugs used (adjusted analysis). The percentage of antipsychotic users in the various municipalities was adjusted using direct standardization to account for differences in age and sex between geographical areas. Furthermore, in order to evaluate duration of use, the median number of DDD was calculated for each region and compared using Pearson’s χ2-test and a Kruskal-Wallis test for analysis of variance. A p-value of <0.05 was considered statistically significant. The data analysis was performed using SAS statistical software, version 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
Study population
On January 1, 2012, Denmark had 974,431 residents aged ≥65 years. We excluded 2,341 individuals because they had received a diagnosis of dementia or anti-dementia drugs before the age of 60 years and 6,351 individuals due to missing information on place of residence. This resulted in a study population of n = 965,739 individuals, n = 34,536 (3.6%) of whom were classified with dementia and n = 931,203 (96.4%) who had not been registered with a dementia diagnosis and formed the reference population (Fig. 1). Table 1 presents the characteristics of the study population stratified by dementia. The patients classified with dementia were older, more likely to be female, less likely to be married, more likely to be a nursing home resident, and suffered from comorbidity more frequently. Table 2 presents the characteristics of the study population with dementia stratified by region. Patients with dementia from the Capital Region of Denmark differed from those living in other regions in that they were older, less likely to be married and had a higher incidence of psychotic disorders prior to being registered withdementia.
National prevalent and incident antipsychotic use
At the national level, prevalence of antipsychotic users was 20.7% in elderly with dementia and 3.0% in elderly without dementia. The annual incidence rate of antipsychotic users was 3.9% among elderly with dementia and 0.7% among elderly without dementia. Among patients with dementia using antipsychotic drugs, 84.8% filled multiple prescriptions. The median (25–75% interquartile range) treatment duration was 42.0 DDD (20.0–90.0 DDD) per antipsychotic user in elderly with dementia, and 33.0 DDD (13.8–100.0 DDD) in elderly without dementia, indicating longer treatment duration in patients with dementia (p < 0.05).
Prevalent and incident antipsychotic use by region
Table 3 shows the use of antipsychotics in elderly with dementia in the regions in 2012. The amount of prevalent users varied from 17.0% in the Central Denmark Region to 23.3% in the Capital Region of Denmark. Incident antipsychotic users ranged from 3.5% in the Central Denmark Region to 4.4% in the Capital Region of Denmark. Table 4 presents the results of a multivariate logistic regression analysis for the prevalence of antipsychotic users in elderly patients with dementia stratified by region (with the Central Denmark Region as the reference). All other regions had a significantly higher prevalence of antipsychotic users, also after adjustment for age, sex, Charlson comorbidity index, psychotic disorder prior to dementia diagnosis, and total number of drugs used.
Prevalent and incident use by municipality
The age and sex standardized antipsychotic use in the 98 municipalities is listed in supplementary Table 1 and shown in Fig. 2. The percentage of antipsychotic users varied from 7.5% in Skanderborg municipality to 33.1% in Vejen municipality, demonstrating an over four-fold difference. Large differences between municipalities were present within the same region as is evident, for example, in the Central Denmark Region where the lowest use was 7.5% (Skanderborg municipality) and the highest use was 30.7% (Lemvig municipality), thus demonstrating a four-fold difference.
DISCUSSION
In this study of the entire elderly population of Denmark, the main finding was a pronounced geographical variation in the use of antipsychotics among elderly patients with dementia that could not be explained by variations in age and sex. The variation at the municipality level was prominent with an over four-fold difference (from 7.5% to 33.1%) in the prevalence of antipsychotic users, even between municipalities within the same region (from 7.5% to 30.7%).
To our knowledge, this study is the first nationwide study analyzing geographical variation in use of antipsychotics among patients with dementia. Previous studies have reported geographical differences in use of antipsychotics, but aimed at investigating the use in the general population or in patients with schizophrenia [25–27]. In accordance with our study, a study from the U.S. found local geographical variation in the use of antipsychotics that by far exceeded the observed variability between states in the general population of all ages [25]. These results may indicate that the geographical variations are not limited to patients with dementia. However, the study only captured 60% of all retail prescriptions in the population and did not have individual-level data, which limits the adjustment for characteristics/confounders and generalizability of the results. Another U.S. study, investigating antipsychotic users of all ages, found that urban residents were 1.87 times more likely than rural residents to use antipsychotic drugs [28]. The present study did not investigate the impact of urbanization; however, the high prevalence of antipsychotic users living in the urban Capital Region compared to the low prevalence in the second largest urban area (Aarhus) indicates that urbanization is not related to treatment of antipsychotics in this study.
In our study, there was an over four-fold difference at the municipal level, exceeding by far the more modest differences between the larger regions. Hospitals in Denmark are managed at a regional level. Thus, differences at the regional level would indicate differences in hospital care. Since the use of antipsychotics did not vary greatly at the regional level, it may indicate that the observed geographical variation was not primarily related to access to hospital care or to dementia specialist departments. The variation was pronounced between the 98 municipalities who are responsible for public healthcare, and for primary care including home care and nursing homes for the elderly, indicating that variation may be related to clinical practice in primary health care.
We may only speculate about the reasons for the pronounced geographical variation. However, several factors may play a role including local differences in management strategies and care of patients with neuropsychiatric symptoms, differences in knowledge or attitude about antipsychotic treatment, and various cultures in clinical practice.
In most cases, GPs are responsible for prescription of medicine, although they may not have initiated treatment. Antipsychotic drugs may be initiated in somatic hospital departments for confusion, hallucinations, or agitation related to acute physical conditions and not discontinued prior to discharge. Furthermore, it is possible that antipsychotic treatment may be initiated based on initiative of family or professional caregivers. In nursing homes, proposals for initiating antipsychotic treatment may arise from clinical observations from the staff. A previous study in Danish nursing homes demonstrated that clinical information of psychiatric morbidity provided by staff, and the recognition of neuropsychiatric symptoms, is of great importance as their assessment independently determined the use of psychotropic treatment, including antipsychotics [29]. The study indicated that antipsychotic drugs were used to treat neuropsychiatric problems because they put an overwhelming strain and workload on the staff [29]. A qualitative study from the UK showed that psychiatrists frequently felt pressured from nursing staff to prescribe medications for neuropsychiatric symptoms despite having knowledge of the limited clinical effect and serious adverse effects [30]. The study also found that the choice of medication was based on familiarity, causing medications to vary greatly between psychiatrists [30], thus suggesting that prescriptions may be related to cultures in clinical practice. Furthermore, psychiatrists also varied in monitoring the effects of their prescribed medication [30], creating the risk of long-term antipsychotic treatment occurring. In an exploratory study from Belgium, GPs and nurses, especially nurses with less education, showed very low willingness to discontinue antipsychotics in chronic antipsychotic users in nursing homes, indicating that current short-term antipsychotic users are likely to become chronic users [31]. This mechanism is supported by this study’s finding of a low proportion of incident users (3.9%) and the relatively long, national average treatment duration of 42 DDD. This is not in accordance with national guidelines, which state that the treatment duration should not exceed a week and if it does, treatment should be managed by a psychiatrist [32]. International guidelines also advise that treatment duration should be as short as possible [33, 34]. Moreover, the actual treatment duration in our population may be even longer than 42 days, as our data for treatment duration were based on DDD of each type of antipsychotic drug defined by WHO across all ages and indications. However, when prescribed for patients with dementia, the usual daily dose is often much lower, leading to an underestimation of treatment duration in this study.
Differences in the composition of the study population and their disease patterns could potentially play a role in the observed geographical differences in antipsychotic consumption. In our study, all regions had a significantly higher use of antipsychotics when compared to the Central Denmark Region, even after adjustment for age, sex, and comorbidity, including Charlson comorbidity index, psychotic disorder to dementia diagnosis and total number of drugs used. Thus, it is our interpretation that the observed major differences in the use of antipsychotics may be related to cultures, attitudes, and lack of knowledge among professional carers.
In support of this notion, the antipsychotic use was shown to be low in the Central Denmark Region, particularly in selected municipalities such as Skanderborg municipality (7.5%) and Aarhus municipality (14.1%). The Central Denmark Region may still be influenced by a leading old age psychiatrist who established an old age psychiatry department in 1987, aimed at lowering antipsychotic use among elderly patients with dementia [35]. In accordance with current guidelines, this restrictive approach to treatment with antipsychotic drugs in elderly patients with dementia may have had a long-term impact on the cultures and attitudes in clinical practice in primary and secondary health care, thus resulting in the observed low consumption in the area in 2012.
Our study indicates an overconsumption of antipsychotics among patients with dementia due to the large observed differences among the municipalities. However, it should be emphasized that there is no general agreement on a certain limit for acceptable use, although our study suggests that the national use could be reduced to a level below 10% as demonstrated by the municipality with the lowest use (Skanderborg municipality) and national data for the UK [10]. Although this study was conducted in theelderly population of Denmark, we believe thatthe extent and nature of the observed differences in the use of antipsychotics is also relevant in an international context. Other countries should be aware of how cultures, attitudes, and knowledge about medical treatment influence the management of neuropsychiatric symptoms in elderly patients with dementia and could apply geographical differences in antipsychotic prescriptions as quality indicators.
The main strength of this study is its nationwide population-based design and high reliability of data linked by a unique personal identification number, allowing investigation of the full spectrum of antipsychotic use in elderly patients with dementia and adjustment for several important confounders such as age, sex, and comorbidity. Our study investigated “real-life prescription patterns” in an entire elderly population, thus avoiding problems of selection bias. Previous research has shown that the validity of a dementia diagnosis in Danish hospital registries is high in the elderly population [23]. However, dementia is generally underdiagnosed and potentially undiagnosed cases of dementia could be included in the reference population. However, baseline characteristics of the dementia population were similar in the regions, so the underdiagnosing of dementia could not explain the observedgeographical variation in antipsychotic treatment. Data on prescriptions for antipsychotic drugs were complete, but we did not have information about indications and whether patients actually consumed their prescriptions. However, 84.8% of patients redeemed multiple prescriptions, suggesting that the majority did consume the antipsychotics. Moreover, although we had prescription data on the municipality and regional levels, we did not have data on who prescribed the antipsychotic treatment and we can therefore only hypothesize on clinical practice among professional carers and physicians in primary care as the driving force for the geographicalvariation.
In conclusion, we found a pronounced geographical variation in the use of antipsychotics among elderly patients with dementia in Denmark that could not be explained by variations in age, sex, or comorbidity. The differences were more pronounced at the municipality level, by far exceeding that of the regional level, suggesting that the differences were primarily related to variances in clinical practice and care in primary care. Implementation of guidelines for appropriate management of neuropsychiatric symptoms is a challenging task that must be addressed jointly by targeting multiple audiences and not only the prescribing doctors. Future studies should explore potential consequences for patient safety. Our study highlights an urgent need for more education to guide non-pharmacological as well as pharmacological management of neuropsychiatric symptoms in elderly patients with dementia.
ACKNOWLEDGMENTS
This Danish Dementia Research Centre is supported by grants from the Danish Health Foundation (file no. 2007B0004) and the Danish Ministry of Health (file no. 2007-12143-112/59506 and file no. 0901110 /34501). All researchers were independent of the funders.
Authors’ disclosures available online (http://j-alz.com/manuscript-disclosures/16-0485r1).
Appendices
The supplementary material is available in the electronic version of this article: http://dx.doi.org/10.3233/jad-160485.
REFERENCES
[1] | Ballard C , Howard R ((2006) ) Neuroleptic drugs in dementia: Benefits and harm. Nat Rev Neurosci 7: , 492–500. |
[2] | Schneider LS , Pollock VE , Lyness SA ((1990) ) A metaanalysis of controlled trials of neuroleptic treatment in dementia. J Am Geriatr Soc 38: , 553–563. |
[3] | Schneider LS , Dagerman K , Insel PS ((2006) ) Efficacy and adverse effects of atypical antipsychotics for dementia: Meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry 14: , 191–210. |
[4] | Ballard C , Waite J ((2006) ) The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer’s disease. Cochrane Database Syst Rev CD003476. |
[5] | Ballard CG , Gauthier S , Cummings JL , Brodaty H , Grossberg GT , Robert P , Lyketsos CG ((2009) ) Management of agitation and aggression associated with Alzheimer disease. Nat Rev Neurol 5: , 245–255. |
[6] | Schneider LS , Dagerman KS , Insel P ((2005) ) Risk of death with atypical antipsychotic drug treatment for dementia: Meta-analysis of randomized placebo-controlled trials. JAMA 294: , 1934–1943. |
[7] | Food and Drug Administration ((2005) ) Public Health Advisory: Deaths with antipsychotics in elderly patients with behavioral disturbances. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm053171.htm |
[8] | US Food and Drug Administration ((2008) ) Information for healthcare professionals: conventional antipsychotics. Available at: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124830.htm |
[9] | National Institute for Health and Clinical Excellence, Social Care Institute for Excellence ((2006) ) Supporting people with dementia and their carers in health and social care. Available at: https://www.nice.org.uk/Guidance/cg42. Last modified May 2016 |
[10] | National Health Service Information Centre for Health, Social Care ((2012) ) National Dementia and Antipsychotic Prescribing Audit. Available at: http://www.ic.nhs.uk/dementiaaudit. Last modified July 2012. Assessed at February 8th, 2016. |
[11] | Guthrie B , Clark SA , Reynish EL , McCowan C , Morales DR ((2013) ) Differential impact of two risk communications on antipsychotic prescribing to people with dementia in Scotland: Segmented regression time series analysis 2001-2011. PLoS One 8: , e68976. |
[12] | Gallini A , Andrieu S , Donohue JM , Oumouhou N , Lapeyre-Mestre M , Gardette V ((2014) ) Trends in use of antipsychotics in elderly patients with dementia: Impact of national safety warnings. Eur Neuropsychopharmacol 24: , 95–104. |
[13] | Schulze J , van den Bussche H , Glaeske G , Kaduszkiewicz H , Wiese B , Hoffmann F ((2013) ) Impact of safety warnings on antipsychotic prescriptions in dementia: Nothing has changed but the years and the substances. Eur Neuropsychopharmacol 23: , 1034–1042. |
[14] | Valiyeva E , Herrmann N , Rochon PA , Gill SS , Anderson GM ((2008) ) Effect of regulatory warnings on antipsychotic prescription rates among elderly patients with dementia: A population-based time-series analysis. CMAJ 179: , 438–446. |
[15] | Franchi C , Tettamanti M , Marengoni A , Bonometti F , Pasina L , Cortesi L , Fortino I , Bortolotti A , Merlino L , Lucca U , Riva E , Nobili A ((2012) ) Changes in trend of antipsychotics prescription in patients treated with cholinesterase inhibitors after warnings from Italian Medicines Agency. Results from the EPIFARM-Elderly Project. Eur Neuropsychopharmacol 22: , 569–577. |
[16] | Norgaard A , Jensen-Dahm C , Gasse C , Hansen HV , Waldemar G ((2015) ) Time trends in antipsychotic drug use in patients with dementia: A nationwide study. J Alzheimers Dis 49: , 211–220. |
[17] | Thygesen LC , Daasnes C , Thaulow I , Bronnum-Hansen H ((2011) ) Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scand J Public Health 39: , 12–16. |
[18] | Pedersen CB ((2011) ) The danish civil registration system. Scand J Public Health 39: , 22–25. |
[19] | Lynge E , Sandegaard JL , Rebolj M ((2011) ) The danish national patient register. Scand J Public Health 39: , 30–33. |
[20] | Mors O , Perto GP , Mortensen PB ((2011) ) The danish psychiatric central research register. Scand J Public Health 39: , 54–57. |
[21] | Kildemoes HW , Sorensen HT , Hallas J ((2011) ) The danish national prescription registry. Scand J Public Health 39: , 38–41. |
[22] | Salem LC , Andersen BB , Nielsen TR , Stokholm J , Jorgensen MB , Rasmussen MH , Waldemar G ((2012) ) Overdiagnosis of dementia in young patients - a nationwide register-based study. Dement Geriatr Cogn Disord 34: , 292–299. |
[23] | Phung TK , Andersen BB , Hogh P , Kessing LV , Mortensen PB , Waldemar G ((2007) ) Validity of dementia diagnoses in the Danish hospital registers. Dement Geriatr Cogn Disord 24: , 220–228. |
[24] | Sundararajan V , Henderson T , Perry C , Muggivan A , Quan H , Ghali WA ((2004) ) New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol 57: , 1288–1294. |
[25] | King M , Essick C ((2013) ) The geography of antidepressant, antipsychotic, and stimulant utilization in the United States. Health Place 20: , 32–38. |
[26] | Stroup TS , Gerhard T , Crystal S , Huang C , Olfson M ((2014) ) Geographic and clinical variation in clozapine use in the United States. Psychiatr Serv 65: , 186–192. |
[27] | Nielsen J , Roge R , Schjerning O , Sorensen HJ , Taylor D ((2012) ) Geographical and temporal variations in clozapine prescription for schizophrenia. Eur Neuropsychopharmacol 22: , 818–824. |
[28] | Wang CC , Farley JF ((2013) ) Patterns and predictors of antipsychotic medication use among the U.S. population: Findings from the Medical Expenditure Panel Survey. Res Social Adm Pharm 9: , 263–275. |
[29] | Sorensen L , Foldspang A , Gulmann NC , Munk-Jorgensen P ((2001) ) Determinants for the use of psychotropics among nursing home residents. Int J Geriatr Psychiatry 16: , 147–154. |
[30] | Wood-Mitchell A , James IA , Waterworth A , Swann A , Ballard C ((2008) ) Factors influencing the prescribing of medications by old age psychiatrists for behavioural and psychological symptoms of dementia: A qualitative study. Age Ageing 37: , 547–552. |
[31] | Azermai M , Vander Stichele RR , Van Bortel LM , Elseviers MM ((2014) ) Barriers to antipsychotic discontinuation in nursing homes: An exploratory study. Aging Ment Health 18: , 346–353. |
[32] | Danish Health and Medicines Authority ((2014) ) Danish Health and Medicines Authority: Vejledning om behandling med antipsykotiske lægemidler til patienter over 18 år. [Danish]. |
[33] | Hort J , O’Brien JT , Gainotti G , Pirttila T , Popescu BO , Rektorova I , Sorbi S , Scheltens P ((2010) ) EFNS guidelines for the diagnosis and management of Alzheimer’s disease. Eur J Neurol 17: , 1236–1248. |
[34] | Ihl R , Frolich L , Winblad B , Schneider L , Burns A , Moller HJ ((2011) ) World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of Alzheimer’s disease and other dementias. World J Biol Psychiatry 12: , 2–32. |
[35] | Gulmann NC ((1992) ) Dementia in Denmark from a medical view. Dan Med Bull 39: 251–253. [Danish]. |
Figures and Tables
Fig.1
Population selection.
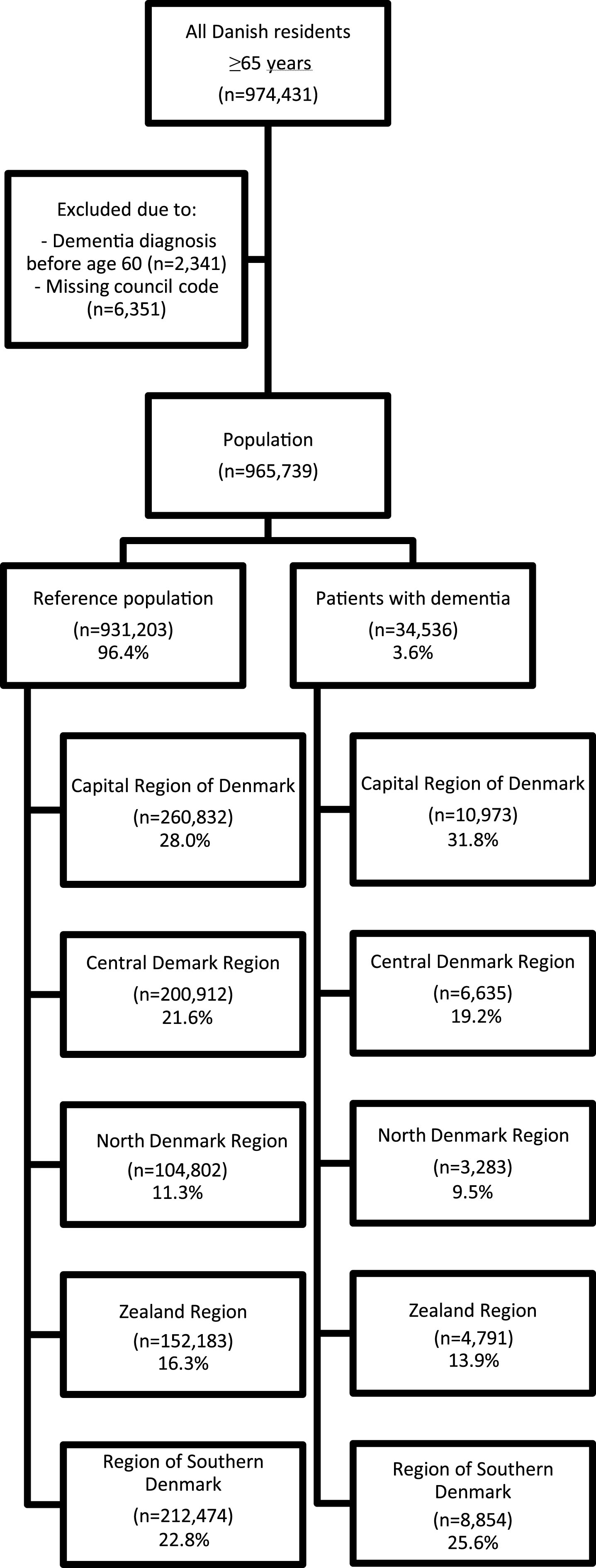
Fig.2
Age and sex standardized prevalent use of antipsychotics in elderly patients with dementia by municipality. Samsø and Læsø municipality were excluded due to insufficient amount of data (<10 antipsychotic users).
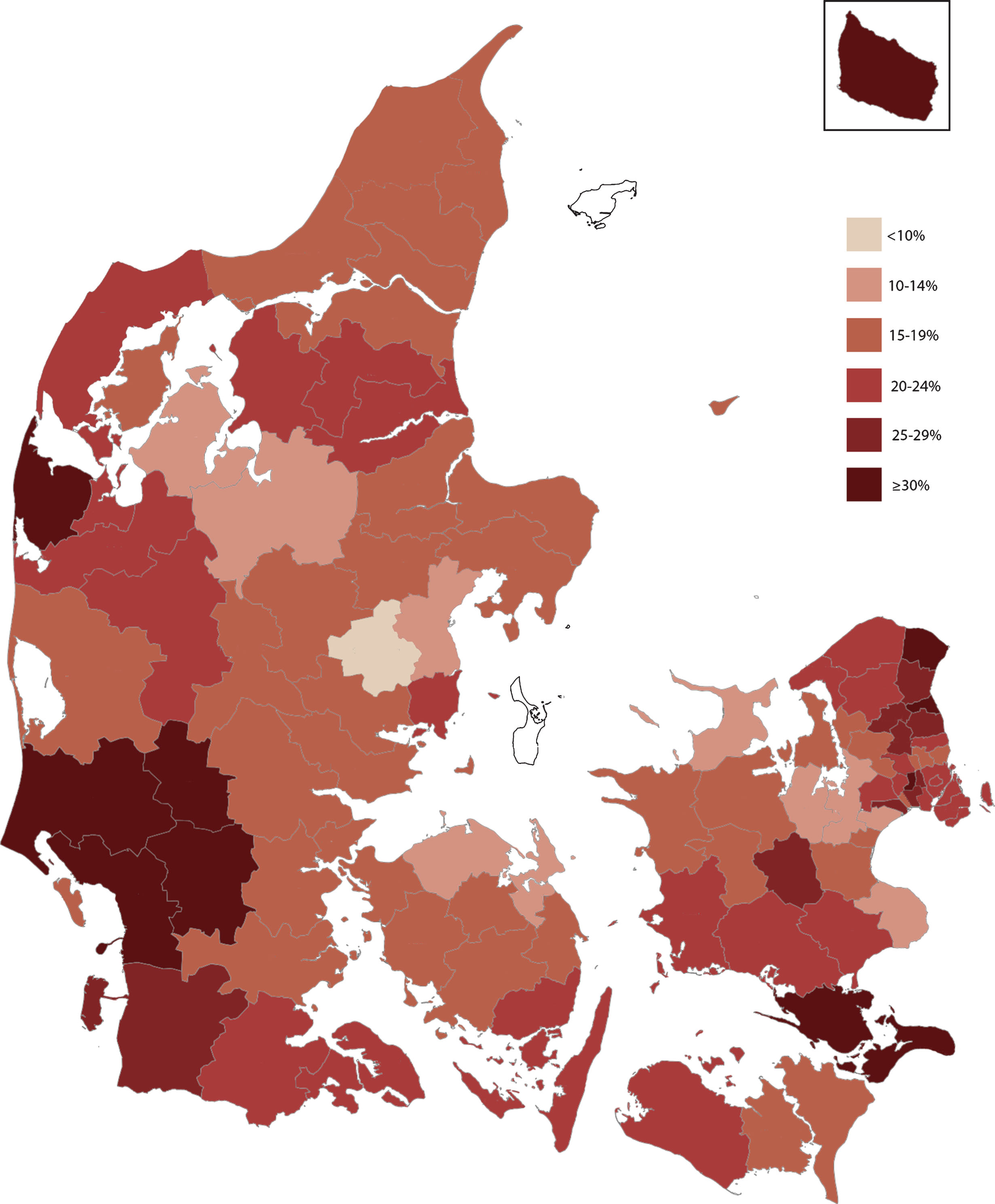
Table 1
Baseline characteristics in elderly with and without dementia
| Characteristics | Dementia (n = 34,536) | Reference (n = 931,203) |
| Age, years | 83.3 (77.6–88.1) | 72.7 (68.3–79.1) |
| Female | 64.9% | 54.7% |
| Married | 33.3% | 56.6% |
| Nursing home resident | 49.5% | 3.1% |
| Charlson comorbidity index | 2.0 (1.0–3.0) | 0.0 (0.0–2.0) |
| Total number of drugs used | 9.0 (6.0–12.0) | 5.0 (3.0–9.0) |
| Time since dementia diagnosis, years | 2.8 (1.3–5.2) | NA |
| Psychotic disorder prior to dementia diagnosis | 4.0% | NA |
Numbers are given as median (25–75% interquartile range) for data with a non-normal distribution. Frequency numbers are given as percentage. NA, not applicable.
Table 2
Baseline characteristics of elderly patients with dementia in Denmark
| Characteristics | Regions | ||||
| North Denmark | Central Denmark | Region of Southern | Capital Region of | Zealand Region | |
| Region (n = 3,283) | Region (n = 6,635) | Denmark (n = 8,854) | Denmark (n = 10,973) | (n = 4,791) | |
| Age, years | 83.5 (77.7–87.8) | 83.1 (77.8–87.7) | 83.3 (77.7–87.9) | 83.7 (77.8–88.6) | 82.8 (77.0–87.8) |
| Female | 64.9% | 64.2% | 64.1% | 66.7% | 63.5% |
| Married | 35.1% | 34.5% | 35.2% | 29.7% | 34.8% |
| Nursing home resident | 55.0% | 51.0% | 47.0% | 50.4% | 46.0% |
| Charlson comorbidity index | 1.0 (1.0–3.0) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) | 2.0 (1.0–3.0) |
| Total number of drugs used | 9.0 (6.0–12.0) | 9.0 (6.0–12.0) | 9.0 (6.0–12.0) | 9.0 (6.0–12.0) | 8.0 (5.0–11.0) |
| Time since dementia diagnosis, | 2.8 (1.2–5.1) | 2.7 (1.2–4.9) | 2.8 (1.3–5.2) | 2.9 (1.3–5.3) | 3.0 (1.4–5.4) |
| years | |||||
| Psychotic disorder prior to | 3.5% | 3.4% | 3.3% | 5.1% | 4.2% |
| dementia diagnosis | |||||
Numbers are given as median (25–75% interquartile range). Frequency numbers are given as percentage.
Table 3
Prevalent and incident use of antipsychotic drugs by regions in 2012
| Dementia | ||||||
| Regions | ||||||
| Total | North Denmark | Central Denmark | Region of Southern | Capital Region of | Zealand Region | |
| (n = 34,536) | Region | Region | Denmark | Denmark | (n = 4,791) | |
| (n = 3,283) | (n = 6,635) | (n = 8,854) | (n = 10,973) | |||
| Prevalent antipsychotic | 20.7% | 18.9% | 17.0% | 21.6% | 23.3% | 19.7% |
| user | ||||||
| Incident antipsychotic | 3.9% | 3.8% | 3.5% | 3.7% | 4.4% | 3.8% |
| user | ||||||
| Treatment duration of | 42.0 (20.0–90.0) | 36.4 (15.0–91.0) | 37.3 (18.2–86.1) | 38.0 (18.8–75.6) | 50.0 (24.0–101.5) | 41.0 (15.4–91.0) |
| antipsychotics | ||||||
| (DDD*) | ||||||
Frequency numbers are given as percentage. *Treatment duration is given as median defined daily doses (DDD) (25–75% interquartile range).
Table 4
Probability of antipsychotic use in elderly with dementia across the five regions
| Antipsychotic use | ||
| Crude OR | Adjusted OR | |
| Region | ||
| Capital Region of Denmark | 1.42 (1.37–1.60) | 1.70 (1.57–1.85) |
| Central Denmark Region | 1 | 1 |
| North Denmark Region | 1.13 (1.02–1.26) | 1.12 (1.01–1.25) |
| Zealand Region | 1.20 (1.09–1.32) | 1.36 (1.23–1.50) |
| Region of Southern Denmark | 1.35 (1.24–1.46) | 1.39 (1.28–1.51) |
Odds ratio, OR; 95% confidence interval, 95% CI. Adjustment for age, gender, Charlson comorbidity index, psychotic disorder prior to dementia diagnosis, and total number of drugs used.




