A Scoping Survey to Inform Design of Digital Dementia Risk Reduction Interventions for Adults Concerned about their Cognitive Health
Abstract
Background:
Digital dementia risk reduction interventions are cost-effective and scalable. However, it is unknown how they are perceived by people already experiencing cognitive concerns or decline.
Objective:
To understand the current use, interest, and preferences for online learning courses and interest in learning about factors influencing brain health and dementia risk among adults ≥45. To explore potential differences between individuals experiencing cognitive concerns and those without.
Methods:
Adults aged 45 and older completed a survey on technology use and healthy ageing (n = 249, Mean age = 65.6, 76.3% female). The Memory Assessment Clinic-Questionnaire was used to assess subjective memory decline, and 153 participants met the study criteria for cognitive concerns (≥25).
Results:
Almost all participants (98.4%) reported using two or more digital devices, and 51.8% reported increasing device usage following COVID-19. Most (92.1%) were interested in learning about healthy living and memory within an online course, and over 80% indicated a high interest in learning about dementia risk factors. People with cognitive concerns were more likely to report using a ‘routine or system’ to aid memory than people without (82.4% versus 62.9%, p = 0.001). However, no significant difference was found in technology use, course preferences, or interest in learning about different risk factors.
Conclusions:
We conclude that adults 45 years and over are interested in online methods for learning about brain health and offer unique insights into adapting dementia prevention programs for cognitive concerns.
INTRODUCTION
The future is becoming increasingly digital, a trend likely accelerated by the global pandemic related to the coronavirus disease 2019 and government restrictions imposed in 2020 and 2021 [1]. People are more reliant on information and communication technologies (ICTs) than ever before, demonstrated by a steep rise in communication platforms during the pandemic [2, 3]. Developments in ICTs encompass traditional technologies such as improving the quality of scan images or advancing surgical robotics as well as digital ways to manage, monitor, and learn about health, for example, wearables to track blood pressure or blood sugar, improved patient access to health information, telehealth consultations, and knowledge dissemination through e-learning programs [4]. Within the last five years, ICTs have increasingly featured in dementia risk reduction interventions to address the global challenge of rising dementia prevalence, as evidenced in randomized controlled trials (e.g., [5–7]) and summarized in systematic reviews [8, 9].
Over 55 million people are affected by dementia worldwide [10]. Hence, there is a need for scalable and easy-to-implement interventions to delay or prevent cognitive decline [11]. A non-pharmacological dementia risk reduction intervention typically targets single or multiple dementia risk factors (e.g., cardiovascular health, diet, physical activity, cognitive and social activity) through psychoeducation, professional advice, and various behavior change techniques. In addition, they target mid to late-life adults often at an increased risk of developing dementia (e.g., with existing cognitive decline, a family history of dementia, or cardiovascular comorbidities) [8]. Our research team developed and evaluated the first clinical trial to utilize online educational modules as part of the dementia risk reduction intervention [12]. This study found that including a face-to-face component to accompany online modules did not significantly increase intervention efficacy or adherence. These results helped to pave the way for remote delivery to be considered an equally viable option within this area of health promotion. Currently, we see digital components employed in a variety of ways, including distributing educational materials through online modules (e.g., [12–14]), offering computer-based cognitive training (e.g., [12, 13, 15, 16]), incorporating coach-led advice via videoconferencing [17], as well as tablet-based physical activities [18]. However, optimal intervention features such as intensity, duration, and personalization remain unclear across all types of interventions [19], and currently, no research has explored user preferences in the context of digital dementia risk reduction interventions for people with cognitive concerns.
The utilization of ICTs for health interventions must be cautiously approached due to the considerable variation of internet access and use within general populations. This variation can be influenced by biological, social, economic, or organizational factors and is typically known as the ‘digital divide’ [20]. The digital divide was first coined in 1995 and has been studied in many countries [20, 21]. It posits that internet access and use are negatively related to age [21] and positively associated with higher education [22], higher income [23], and employment [24]. Further, differences also exist between racial and ethnic backgrounds [25], disability groups [26], as well as males and females, although for the latter, the divide has become intangible in some countries [22, 23, 27]. Given this variation across population groups, researchers designing digital health interventions should seek to understand population-specific preferences and barriers.
Overall, the age-related digital divide has decreased, evidenced by growing trends across the last 5–10 years that see approximately 67–75% of seniors using the internet daily [3, 28]. However, the divide can still be exacerbated by many things, for example, poor health literacy of users [29], limited visual acuity or manual dexterity [22] as well as age-related cognitive difficulties (e.g., general slowing or attention deficits) [30], subjective memory concerns [31], and clinically significant cognitive decline [32]. Individuals with cognitive impairments often encounter difficulties with ICTs due to deficits in attention, memory, language, executive functions, problem-solving and reasoning [33], making this a complex issue to address. Despite these complexities, a pre-COVID Australian-based survey recorded that up to 91.4% of people with cognitive impairment have access to the internet, and most are interested in using online tools for healthy ageing [34]. An American study conducted during COVID also reported high rates of technology use for people with subjective cognitive concerns (94.1% using smartphones, 96.8 using desktops or laptops) [35]. With these high access rates and technology increasingly featured in dementia risk reduction interventions (e.g., [8, 14, 36, 37]), ensuring interventions are tailored and suitable for people with cognitive impairments isvital.
Thus far, research has suggested several design recommendations for audiences with cognitive disabilities, such as standardized and unambiguous navigation, limiting the quantity of information, and avoiding jargon and undefined abbreviations [33, 38]. However, recommendations are often made by considering cognitive disabilities as a homogeneous group when, in reality, they encompass many different disorders with varied needs and preferences [26]. Furthermore, despite the idiosyncratic nature of technology preferences [39], no research has been conducted to understand opinions from this population for dementia risk reduction interventions specifically.
This survey will first describe the past experiences and current preferences towards technology and online learning courses for Australians over 45 years old and then address two research gaps relevant to dementia risk reduction interventions: 1) To explore the use and preferences for technology for people with cognitive concerns compared to those without cognitive concerns and 2) To explore preferences for intervention features.
MATERIALS AND METHODS
Study design
This project used a cross-sectional online survey design. A 30- to 40-min survey was presented using the REDCap (Research Electronic Data Capture) tool hosted by the University of New South Wales (UNSW) [40]. Data was collected between July 2020 and January 2021, during a period of global lockdowns due to the COVID-19 pandemic. After providing informed consent online, participants accessed the survey via a secure link on their personal devices. After individual submission, survey access was closed to avoid duplicates, and a CAPTCHA service was implemented to prevent “bot” entries. The project received approval from the UNSW Human Research Ethics Committee before commencement [HC200406], and all procedures were planned and conducted in accordance with the revised Declaration of Helsinki [41].
Recruitment
Participants across Australia were recruited via digital newsletters (i.e., University of Third Age, U3A), social media (e.g., Facebook, Twitter), and volunteer registries (i.e., StepUp for Dementia Research and Neuroscience Research Australia Healthy Volunteer Registry). Participants met the criteria for inclusion if they were 45 years or older, could access the survey online, and had a sufficient understanding of the English language (self-assessed). The recruitment materials and sampling strategy targeted people already thinking about their memory and possibly experiencing cognitive concerns; however, no data was collected about mild cognitive impairment (MCI) or dementia diagnoses.
Measures
The questionnaire consisted of multiple-choice and open-ended questions aiming to inform the development of a novel dementia risk reduction intervention. Questions related to technology and online learning were informed by our team’s extensive experience with digital components of dementia risk reduction interventions (e.g., [12, 42, 43]). This experience helped to streamline question response options to keep them concise, while the inclusion of ‘other’ as an open-ended response ensured comprehensive data collection and minimized the risk of bias or incomplete answers. The following questions were included:
Demographic measures
Socio-demographic data were collected relating to age, gender, education (in levels, from School certificate/ Record of School Achievement (RoSA)/Year 10 up until Higher Degree), occupation (or prior occupation), first language, country of birth, years in Australia, and living situation (alone or with ≥1 other(s)).
Memory measures
Subjective cognitive concerns were assessed using the Memory Assessment Clinic-Questionnaire (MAC-Q), a self-report scale whereby participants compare current memory ability to memory ability when they were 18–20 years old for given situations [44]. Overall scores range from 7 to 35, with higher scores indicative of perceived cognitive decline and ≥25 being the cut-off for subjective cognitive decline (SCD). The MAC-Q is viewed as a unidimensional questionnaire with Cronbach’s alpha scores from validation research ranging from 0.57 to 0.88, indicating acceptable internal validity [44–46]. Given that it was beyond the scope of this study to rule out MCI or dementia, participants were categorized as having ‘cognitive concerns (CC)’ (scores of ≥25) or ‘no cognitive concerns (NCC)’ (scores of <25) based on the MAC-Q SCD cut-off [44]. Participants were also asked to indicate (yes/no) whether they had noticed a decline in their memory over the last ten years and, if so, how concerned they were on a 4-point scale (choices included: not at all, slightly, moderately, or very). Finally, participants who had noticed a decline were asked to indicate (yes/no) whether they had consulted with a doctor or professional about memory or cognition.
Technology measures
Six questions in the survey were designed to address past and current usage of device(s), online resources, or apps, as well as issues with or influences on device usage. Participants were asked the following multiple-choice questions: 1) which of the following device(s) do you use? (choices included: desktop computer, laptop, mobile, tablet, smartwatch, and other); 2) In general, what do you use your device(s) for? (choices included: text/messaging, video calls, reading, games, health-related, social media, accessing general information, and other); 3) Do you think that your use of devices has increased because of COVID-19? (choices included: yes, no, and same as before); 4a) Do you currently use any apps or online resources to help with day-to-day life? (choices included: yes – with guidance from an instructor, yes – with goal setting or reminders, yes – related to stress management, yes – related to diet or food, yes – related to physical exercise, yes – related to memory, yes – other, yes – I have in the past but now stopped, no – none). For participants who answered ‘yes – I have in the past but now stopped’, they were asked 4b) Why did you stop? (choices included: no time, no motivation, was not right for me, too complex, forgot to use it, lost interest and other); 5) Do any of the following issues apply to you when using your device(s)? (choices included: slow internet, typing difficulties, viewing screen difficulties, headaches, requiring assistance, difficulty navigating, difficulty using the mouse, and other).
Online learning course measures
For this survey, an online learning course (OLC) was defined as “self-directed learning on an electronic device where the user would work through modules/chapters with written information and learning would be facilitated by activities, videos and interactive elements”. Six questions in the survey were designed to evaluate experience and preferences towards OLCs. Participants were asked the following questions: 1) If you were enrolled in an OLC, which device(s) would you prefer to use? (choices included: desktop computer, laptop, mobile, tablet, or other); 2) If you were enrolled in an OLC consisting of 6 modules/chapters, how long would you be happy to sit and complete one for? (choices included: less than 10 min, 10–20 min, 20–30 min, 30–60 min, or more than 60 min); 3) If you were enrolled in an OLC, which of the following describes how you would learn best? (choices included: I learn best when looking at pictures, diagrams and symbols, I learn best when things are explained verbally, I learn best when reading and writing down information, I learn best with activities that make me rehearse information, I learn best through homework, tasks outside of the course, other and I don’t know how I learn best); 4) If you were enrolled in an OLC, would you engage in tasks that require you to set goals and make plans to achieve them? (choices included: yes – I would be glad to, no – I prefer just reading and absorbing information, no – I don’t have time, no – I’m not interested, or other); 5) How often do you use the following memory strategies (writing things down, voice reminders, alarms or phone reminders, labels, taking photos using GPS journaling, having a routine or system, mental strategies, or other) to assist with day-to-day life (choices included: never, sometimes, often, and all the time); 6) Are you interested in learning about healthy living and memory if it was an online course? (choices included: yes or no); 7) How interested would you be in learning how the following factors (physical exercise, healthy eating, social activities, cognitive activities, stress, anxiety, and low mood) relate to brain health and preventing memory and thinking impairment? (choices included: not at all interested, not very interested, neutral, somewhat interested, very interested).
Sample size
A prior power analysis was conducted using G*Power version 3.1.9.7 [47]. Previous research demonstrated that daily use of digital devices differed between people with ‘normal cognition’ and people with MCI by 17.9% (53.6% for NC and 35.7% for MCI) [48]. Based on the difference in proportions, 80% power, and an alpha of 0.05, we estimated a minimum sample size of 240 participants for chi-square analysis. Given that the consent form and survey link were distributed with no formal screening process, it was expected that a high number of people would click on the link and only partially complete the survey. As such, a higher initial response rate was planned to allow for missing data (n≈350).
Data processing and analysis
The deidentified dataset was examined for missing data at a case level. The demographic and survey questions were presented using descriptive statistics (e.g., frequencies, percentages, means, and standard deviations where appropriate). Comparisons between cognitive groups (CC versus NCC) were conducted using Pearson’s Chi-Square test for categorical variables where feasible. The sampling and data collection methods ensured that participants were tested independently. Before analysis, we verified expected frequencies and minimum cell counts; where required, Fisher’s Exact Test was used for 2×2 tables with ≥20% of cells having expected counts less than 5, and the Likelihood Ratio test for 2×3 tables under the same condition, enhancing the accuracy of results [49]. Alpha was set at 0.05 for all analyses, and all data were collected, managed, and stored according to our ethics application and analyzed using IBM SPSS Statistics for Windows Version 25.0 [50].
RESULTS
Initially, 340 responses were collected, but 91 were excluded due to the absence of any data beyond the consent form, resulting in a final dataset of 249 entries for analysis. Throughout the analyses, the sample size was affected by branching questions, which depended on previous responses, and by surveys that were only partially completed. As a result, some analysis was conducted on a sub-sample; in all cases, the revised sample size will be indicated.
Participant demographics
Participants included 190 (76.6%) women, 58 men (23.4%), and one individual who preferred not to answer. Ages ranged from 45 to 90 (M = 65.64, SD = 10.09). Participants were highly educated, with the majority completing education at the bachelor level or higher (64.7%), and most were not in current employment (68%). Most were born in Australia (68.7%), with English as the only language spoken at home (92.3%). A full description of demographics is available in Table 1.
Table 1
Sample socio-demographic characteristics and cognitive status
| Characteristic | N | % |
| Agea | ||
| 45–64 | 113 | 45.7 |
| 65+ | 134 | 54.3 |
| Cognitive Statusb | ||
| Cognitive concerns (CC) | 153 | 63.2 |
| No cognitive concerns (NCC) | 89 | 36.8 |
| Gender | ||
| Female | 190 | 76.3 |
| Male | 58 | 23.3 |
| Prefer not to answer | 1 | 0.4 |
| Residence | ||
| Live alone | 73 | 29.3 |
| Live with 1 or more other | 175 | 70.3 |
| Prefer not to answer | 1 | 0.4 |
| Country of birth | ||
| Australia | 171 | 68.7 |
| Other | 78 | 31.3 |
| Language | ||
| English only | 230 | 92.3 |
| Other | 19 | 7.7 |
| Identify as Aboriginal or Torres Strait Islander | ||
| Yes | 2 | 0.8 |
| No | 243 | 97.6 |
| Prefer not to answer | 4 | 1.6 |
| Education | ||
| Lower than a bachelor’s degree | 85 | 35.3 |
| Bachelor’s degree or higher | 161 | 64.7 |
| Prefer not to answer | 3 | |
| Current Employment | ||
| Currently employed | 79 | 31.7 |
| Not currently employed | 170 | 68.3 |
aAge includes missing data (n = 2) due to programming error. bCognitive status includes missing data (n = 7) as the MAC-Q was not mandatory.
For cognitive status, 153 participants (63.2%) were classified in the CC group with scores of ≥25 on the MAC-Q (M = 28.59, SD = 2.97) and 89 in the NCC group with scores of <25 on the MAC-Q (M = 21.36, SD = 2.75). From the subset of participants who reported some level of decline in cognition over the last ten years, most participants indicated some level of concern about this decline (95.6%). However, few had sought help from a doctor or professional (22.5%).
Technology
Overall, participants were familiar with technology, with almost all (98.4%) using two or more technological devices and about half (51.8%) reporting that their usage had increased due to COVID-19. Mobile phones were the most common device (98.0%), and texting/messaging was the most common function (96.8%). However, around half of the participants reported some difficulties when using devices (50.6%); the most common issues were slow internet (28.9%) and difficulty viewing the screen (22.5%). Almost two-thirds of participants (61.0%) had used an app or online resource to help with day-to-day life, of which physical exercise was the most common topic (25.7%). Of those who had used an app or online resource in the past but since stopped (n = 35, 14.1%), reasons commonly included loss of interest (45.7%) or lack of motivation (22.9%). All other responses about devices, apps, and functions are summarized in Supplementary Material 1.
Online learning courses
Most (92.1%) participants indicated they were interested in learning about healthy living and memory if it was provided as an online course. Laptops (58.2%) or desktop computers (49.0%) were the preferred devices to complete an online course, and 30–60 min was the preferred time for one chapter (43.1%). The most common learning method was reading and writing things down (62.2%), and over half (63.5%) of participants indicated they were happy to engage in tasks requiring setting goals.
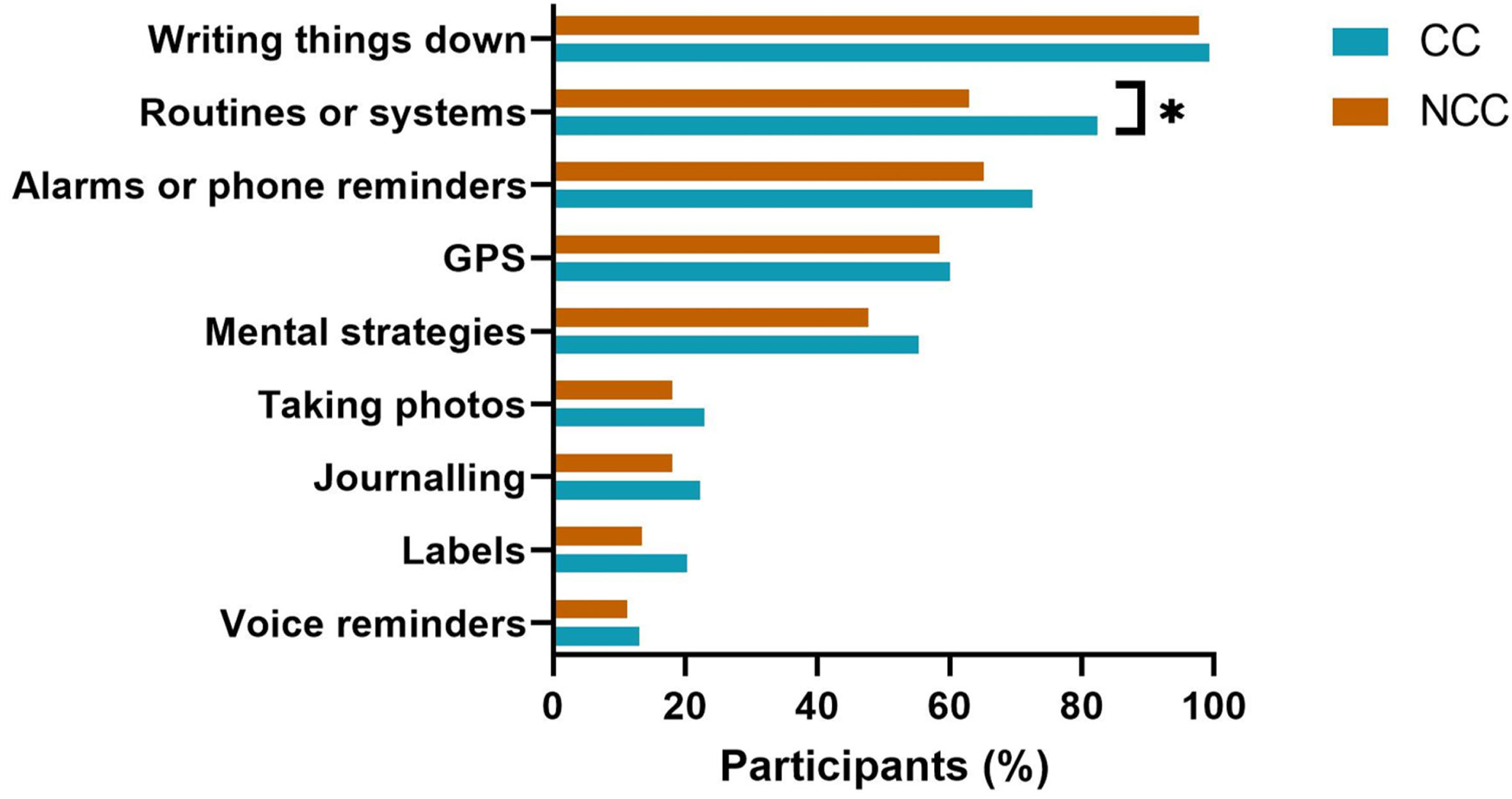
In day-to-day life, nearly all participants utilized the memory strategy of ‘writing things down’ (98.8%), followed by ‘having a routine or system’ (75.2%). Forty-nine participants included the response option of “other” and specified alternative memory strategies such as ‘asking other people for help’, ‘using technology to help (i.e., computer or email reminders)’, ‘keeping a diary’, ‘rehearsing information’, ‘using visualization’, and ‘avoidance of multitasking’. Participants showed an overwhelming interest in learning about how dementia risk factors related to brain health and preventing memory and thinking impairment. Risk factor topics with the highest level of interest were ‘cognitive activities’, ‘diet’ and ‘exercise’ (with 93.0%, 88.9%, and 88.8%, respectively, indicating ‘very’ or ‘somewhat’ interested). All other responses about online learning courses are summarized in Supplementary Material 1.
Comparisons between people with and without cognitive concerns
Demographics
No differences were found between age, sex, education, living status, country of birth or primary language spoken between people with CC and NCC. However, for employment, the CC group were employed significantly less than the NCC group (χ2 (1, n = 242) = 4.353, p = 0.046).
Technology
No differences were found between CC and NCC groups for the type of device(s) used, device function(s), the impact of COVID-19 on device use, or apps/online resources used to help with daily life. However, for a small sub-sample (n = 35) who responded that they had used an app/online resource in the past but had since stopped, participants with CC reported the reason for stopping being due to “lack of motivation” significantly more than the NCC group, as determined by Fisher’s Exact Test (n = 35, p = 0.032). Moreover, for issues using device(s), the CC group reported “headaches” significantly more than the NCC group (χ2 (1, n = 242) = 5.612, p = 0.018), and the NCC group reported ‘none’ significantly more than the CC group (χ2 (1, n = 242) = 4.823, p = 0.033).
Online learning courses
No differences were found between CC and NCC for OLC device preference, chapter duration, learning styles, or preference for the inclusion of goal setting. Although to assist with day-to-day life, the CC group indicated using the memory strategy of ‘a routine or system’ significantly more than the NCC group (χ2 (1, n = 242) = 11.394, p = 0.001) (see Fig. 1). Interest in learning about healthy living and memory, if it was presented as an OLC, did not differ between those with CC or NCC, nor did the level of interest for specific dementia risk factors (i.e., exercise, diet, social activities, cognitive activities, stress, anxiety, or mood).
Fig. 1
Day-To-Day Use of Memory Strategies Compared by Cognitive Status. *Cognitive group comparisons significant at p < 0.001.
No other significant differences were found for technology or online learning courses; all comparisons are summarized in Supplementary Material 2.
DISCUSSION
Information and communication technologies are likely to form a crucial part of future dementia risk reduction interventions [9]; this scoping survey explored experiences and preferences towards technology and online learning courses in this context. We offer practical insights for researchers developing online interventions for people experiencing cognitive concerns, an emerging and essential area of health promotion and chronic disease prevention research.
Overall insights and recommendations
Our research found that 92.1% of adults aged 45 and over are interested in learning about healthy living and memory when presented as an OLC. This interest is supported by the fact that most of our participants already used two or more devices, and almost two-thirds had tried an app or online resources to assist with day-to-day life. The COVID-19 pandemic has led to a significant increase in the use of technology for health and connectivity, leading some to call it a ‘turning point for e-health’ [51]. Half of our participants reported increased ICT use since the pandemic, and recent studies have shown that the proportion of people aged 70+ completing surveys on mobile phones has doubled between 2018–2021, and a further 10% of people (82%, 2021) now rate their ability to find information online as good or excellent since 2018 [3]. Our findings align with the broader trend towards e-health, with participants indicating interest in online learning and reporting access to technological devices.
This survey provided valuable insights into the design of OLCs for adults aged 45 and over. Firstly, participants preferred accessing OLCs on a desktop or a laptop rather than mobile phones or tablets, indicating a preference for more traditional methods. While most participants preferred chapter lengths of 30–60 min, a high percentage (56.9%) were divided between preferring less or more time, suggesting that a 30-min mandatory chapter with additional optional reading may be an optimal and accommodating approach. Finally, for goal-setting activities, one-third of participants chose that they would prefer not to engage in this activity. This finding highlights the importance of keeping a goal-setting component optional or exploring alternative behavior change techniques to cater to different preferences, even though goal-setting is recognized as an effective behavior change technique in health intervention trials [52, 53].
Insights and recommendations for people with cognitive concerns
Our results suggested no notable differences for people with and without cognitive concerns regarding the types of devices owned, their functions, or the online resources and apps used. These findings align with a pre-COVID study that investigated technology usage across three distinct stages of cognitive decline: SCD, MCI, and dementia. Researchers found no differences in the use of computers, mobiles, and social media between people with SCD and MCI however, a significant difference was observed when comparing these stages with early-stage dementia [34]. Together with our results, this may suggest that the point of divide may become discernible at later stages of objective cognitive decline.
Both LaMonica and colleagues [34] and the current study recorded the use of technology in a dichotomous yes/no fashion, however, a recent study employed a frequency scale from 0 (Never) to 6 (Many Times a Day) [35], offering an additional perspective. This approach also found no significant associations between utilized device functions (i.e., texting/video calls and social media) based on the degree of subjective cognitive concerns. However, when pooling together types of technology (i.e., smartphones, computers, and tablets), a significant correlation was found between device usage and the degree of subjective cognitive concerns, whereby the increased frequency of device use was associated with fewer cognitive concerns [35]. This underscores the importance of considering diverse usage measures to fully understand how patterns in technology use evolve with cognitive changes.
For OLC preferences, the study found minimal differences associated with the presence of cognitive concerns. However, we observed that individuals with cognitive concerns relied more on day-to-day memory strategies, mainly through the use of routines or systems. This knowledge can inform intervention design to facilitate memory and subsequent learning. For instance, interventions commonly make accommodations for older adults, such as step-by-step evaluations instead of testing comprehension all in one go [27] or mentor-assisted goal setting with a SMART goal structure [54]. Therefore, additional features could be integrated to support adults with memory concerns and leverage the benefits of routines and systems, such as the consistent and scheduled release of educational materials, session reminders, or calendars to track studycommitments.
When asked about issues with devices, “headaches” was identified significantly more by participants with cognitive concerns. Headaches are commonly associated with digital eye strain through the use of digital devices and can be exacerbated by increased cognitive demand (e.g., more challenging material) [55]. This might be pertinent for individuals with cognitive concerns, as they may find interacting with technology more challenging due to deficits with cognitive domains such as attention, memory, language, executive functions, or problem-solving [33]. Further research is needed to explore this relationship and determine the distinct impact for people with cognitive concerns. However, arguably, designers of OLCs should already be implementing strategies to assist all users and mitigate side effects. This could include minimizing cognitive demand by avoiding jargon, complicated language, or too much text or enhancing accessibility features such as adjustable font sizes, text-to-speech, or screen break reminders.
Motivation has been identified as a crucial barrier to health-related behavior change for interventions encouraging weight loss [56] and physical activity [57]. Our preliminary findings suggested that among our participants, individuals with cognitive concerns were more likely to discontinue using an app or online resource due to a “lack of motivation” than those without cognitive concerns. This observation seems to align with literature that associates cognitive decline and increased apathy [58, 59]. However, these insights are derived from a small sub-sample (n = 35) that did not meet the minimum sample requirements, thus limiting the strength and generalizability of conclusions. Therefore, whilst it might be advantageous for intervention designers to explore strategies to sustain engagement, particularly among individuals with cognitive concerns, our findings should be interpreted with caution and additional research is required to substantiate thisrecommendation.
Lastly, our study found that only a small proportion of participants (22%) concerned about their memory loss actively sought help from healthcare professionals. This finding is consistent with studies indicating that older adults can be reluctant to seek medical assistance or attend GP appointments [60] due to reasons such as a lack of understanding of symptoms, concerns about stigma, or fear regarding a possible diagnosis [60, 61]. While publicly available online interventions could represent a feasible option to bridge this gap by providing access to guidance without requiring a professional consultation, additional research is needed to evaluate the effectiveness of this solution comprehensively.
Limitations
While this research provides new insights and recommendations for designing online interventions, it is important to consider several limitations. Firstly, measuring technology engagement through an online survey necessitated a baseline level of ICT literacy and access from participants. Therefore, the generalizability of our findings is limited to individuals who already have technology access and cannot comment on the feasibility of online interventions for all people with cognitive concerns. Furthermore, the survey was conducted between mid-2020 and early 2021, and while this provides a unique snapshot of COVID-19-influenced technology usage, the result may have produced an inflated picture of ICT usage and atypical attitudes.
Next, it was beyond the scope of this self-administered survey to differentiate between stages of cognitive decline. Since literature suggests that ICT usage for people with cognitive impairments decreases over time [62], and this was a digitally administered survey, we may have failed to capture individuals with more pronounced cognitive concerns. This skew may explain the absence of an anticipated age difference between the CC and NCC groups despite age being the most prominent factor for declining cognition, and it may have diluted any potential differences between the CC and NCC groups. Moreover, as with all online surveys, the self-administered and anonymous design gives rise to additional biases, hindering the verification of participant characteristics and complicating efforts to address validity with self-report data. We hope that the use of an online consent process explaining this research’s purpose helped to mitigate this somewhat, but future research should consider a more rigorous screening process. With respect to participant characteristics, it must also be noted that the sample may not be representative of the broader population as participants were highly educated, predominantly female (76.6%), and residency (rural vs urban) was not captured. The education and sex bias was likely due to the University of Third Age (U3A) being the primary recruitment avenue [63] and females being overrepresented as volunteers in general [64].
Finally, we acknowledge limitations regarding the validity and the interpretation of our data. Although experienced researchers were involved in the design of our survey, the instrument was not externally reviewed by experts for content validity, and the self-report design did not allow for criterion-validation of reported technological devices and functions.
Conclusions and future directions
Our findings suggest that individuals with access to technology may be receptive to digital interventions for dementia risk reduction, including individuals with cognitive concerns, although the efficacy of such interventions for this population is beyond the scope of this survey. Nevertheless, researchers may consider the preferences identified in this study when developing digital dementia risk reduction interventions, such as ensuring OLCs are compatible with computers or laptops, dividing chapters into 30-min segments with additional reading materials, incorporating multiple learning styles, and keeping goal setting optional. Moreover, for interventions specifically targeting people with cognitive concerns, researchers should consider utilizing memory strategies to aid adherence and subsequent learning and further research should explore the impact of user motivation or devices issues, such as headaches, on the use of devices or online apps.
Future research is needed to validate self-reports of technology use, adopt more inclusive recruitment strategies, and could consider a variety of survey distribution approaches beyond just online formats. Additionally, assessing participants’ level of cognitive impairment would aid in determining the feasibility of digitally delivered interventions for individuals with cognitive impairments in a post-COVID-19 era.
AUTHOR CONTRIBUTIONS
Jessica Grace Amos (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Visualization; Writing – original draft; Writing – review & editing); Lidan Zheng (Supervision; Writing – review & editing); Ranmalee Eramudugolla (Conceptualization; Methodology; Writing – review & editing); Sophie C Andrews (Supervision; Writing – review & editing); Kaarin J. Anstey (Conceptualization; Funding acquisition; Methodology; Resources; Supervision; Writing – review & editing)
ACKNOWLEDGMENTS
First and foremost, the authors would like to acknowledge the dedication of time and input from all the survey participants. We would also like to thank the NeuRA research staff who assisted with the survey design.
FUNDING
This work was supported by funding from a NeuRA Discovery Grant to KJA, and ARC Laureate Fellowship FL190100011 to KJA. LZ and JA are funded on FL190100011. SCA is funded by an ARC DECRA Fellowship DE210101138. The funding bodies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or the review or approval of the manuscript.
CONFLICT OF INTEREST
KJA declares speaker honorarium from Roche. No other conflicts of interest to report.
DATA AVAILABILITY
The participants of this study did not give written consent for their data to be shared publicly, therefore due to the nature of the research supporting data is not available.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/ADR-230160.
REFERENCES
[1] | Budd J , Miller BS , Manning EM , Lampos V , Zhuang M , Edelstein M , Rees G , Emery VC , Stevens MM , Keegan N ((2020) ) Digital technologies in the public-health response to COVID-19. Nat Med 26: , 1183–1192. |
[2] | Vargo D , Zhu L , Benwell B , Yan Z ((2021) ) Digital technology use during COVID-19 pandemic: A rapid review. Hum Behav Emerg Technol 3: , 13–24. |
[3] | Orthia L, Maccora J, McCallum J, “I am trying to keep up to date…but it is moving so fast”: Older Australians’ Digital Engagement in Turbulent Times. https://nationalseniors.com.au/research/social-connectedness-communities/older-australians-digital-engagement, Accessed May 8, 2023. |
[4] | Australia Department of Industry, Australia’s tech future: Delivering a strong, safe and inclusive digital economy, http://hdl.voced.edu.au/10707/514068, Accessed May 5, 2023. |
[5] | Anstey KJ , Cherbuin N , Kim S , McMaster M , D’Este C , Lautenschlager N , Rebok G , McRae I , Torres SJ , Cox KL ((2020) ) An internet-based intervention augmented with a diet and physical activity consultation to decrease the risk of dementia in at-risk adults in a primary care setting: Pragmatic randomized controlled trial. J Med Internet Res 22: , e19431. |
[6] | Eggink E , Hafdi M , Hoevenaar-Blom MP , Song M , Andrieu S , Barnes LE , Birck C , Brooks RL , Coley N , Ford E ((2021) ) Prevention of dementia using mobile phone applications (PRODEMOS): Protocol for an international randomised controlled trial. BMJ Open 11: , e049762. |
[7] | Heffernan M , Andrews G , Fiatarone Singh MA , Valenzuela M , Anstey KJ , Maeder AJ , McNeil J , Jorm L , Lautenschlager NT , Sachdev PS ((2019) ) Maintain your brain: Protocol of a 3-year randomized controlled trial of a personalized multi-modal digital health intervention to prevent cognitive decline among community dwelling 55 to 77 year olds. J Alzheimers Dis 70: , S221–S237. |
[8] | Coley N , Giulioli C , Aisen PS , Vellas B , Andrieu S ((2022) ) Randomised controlled trials for the prevention of cognitive decline or dementia: A systematic review. Ageing Res Rev 82: , 101777. |
[9] | Bott NT , Hall A , Madero EN , Glenn JM , Fuseya N , Gills JL , Gray M ((2019) ) Face-to-face and digital multidomain lifestyle interventions to enhance cognitive reserve and reduce risk of Alzheimer’s disease and related dementias: A review of completed and prospective studies. Nutrients 11: , 2258. |
[10] | World Health Organisation, Dementia – Factsheet, https://www.who.int/en/news-room/fact-sheets/detail/dementia, Accessed March 23, 2023. |
[11] | Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , Brayne C , Burns A , Cohen-Mansfield J , Cooper C ((2020) ) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396: , 413–446. |
[12] | Anstey KJ , Bahar-Fuchs A , Herath P , Kim S , Burns R , Rebok GW , Cherbuin N ((2015) ) Body brain life: A randomized controlled trial of an online dementia risk reduction intervention in middle-aged adults at risk of Alzheimer’s disease. Alzheimers Dement (N Y) 1: , 72–80. |
[13] | Brodaty H , Heffernan M , Fiatarone Singh MA , Valenzuela M , Andrews G , Lautenschlager NT , Anstey KJ , Maeder A , Jorm LR , McNeil J ((2017) ) Maintain Your Brain: A randomised controlled trial of an internet-based multi-component lifestyle intervention to prevent cognitive decline and dementia. Alzheimers Dement 13 (Suppl 7): , P1216. |
[14] | McMaster M , Kim S , Clare L , Torres SJ , Cherbuin N , D’Este C , Anstey KJ ((2020) ) Lifestyle risk factors and cognitive outcomes from the multidomain dementia risk reduction randomized controlled trial, Body Brain Life for Cognitive Decline (BBL-CD). J Am Geriatr Soc 68: , 2629–2637. |
[15] | Ngandu T , Lehtisalo J , Solomon A , Levälahti E , Ahtiluoto S , Antikainen R , Bäckman L , Hänninen T , Jula A , Laatikainen T ((2015) ) A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): A randomised controlled trial. Lancet 385: , 2255–2263. |
[16] | Kueider AM , Parisi JM , Gross AL , Rebok GW ((2012) ) Computerized cognitive training with older adults: A systematic review. PloS One 7: , e40588. |
[17] | Richard E , van Charante EPM , Hoevenaar-Blom MP , Coley N , Barbera M , van der Groep A , Meiller Y , Mangialasche F , Beishuizen CB , Jongstra S ((2019) ) Healthy ageing through internet counselling in the elderly (HATICE): A multinational, randomised controlled trial. Lancet Digital Health 1: , e424–e434. |
[18] | Realdon O , Rossetto F , Nalin M , Baroni I , Cabinio M , Fioravanti R , Saibene FL , Alberoni M , Mantovani F , Romano M ((2016) ) Technology-enhanced multi-domain at home continuum of care program with respect to usual care for people with cognitive impairment: The Ability-TelerehABILITation study protocol for a randomized controlled trial. BMC Psychiatry 16: , 425. |
[19] | Röhr S , Kivipelto M , Mangialasche F , Ngandu T , Riedel-Heller SG ((2022) ) Multidomain interventions for risk reduction and prevention of cognitive decline and dementia: Current developments. Curr Opin Psychiatry 35: , 285–292. |
[20] | Van Dijk J ((2020) ) The digital divide. John Wiley & Sons. |
[21] | Hilbert M ((2011) ) The end justifies the definition: The manifold outlooks on the digital divide and their practical usefulness for policy-making. Telecommun Policy 35: , 715–736. |
[22] | Gallagher R , Roach K , Sadler L , Glinatsis H , Belshaw J , Kirkness A , Zhang L , Gallagher P , Paull G , Gao Y ((2017) ) Mobile technology use across age groups in patients eligible for cardiac rehabilitation: Survey study. JMIR mHealth and uHealth 5: , e8352. |
[23] | Perrin A, Duggan M, Americans’ internet access: 2000–2015: As internet use nears saturation for some groups, a look at patterns of adoption., https://www.pewresearch.org/internet/2015/06/26/americans-internet-access-2000-2015/, Accessed May 8, 2023. |
[24] | Van Dijk JAGM ((2017) ) Digital divide: Impact of access. In The International Encyclopedia of Media Effects, Rössler P, Hoffner CA, Zoonen L, eds. https://doi.org/10.1002/9781118783764.wbieme0043 |
[25] | Mitchell UA , Chebli PG , Ruggiero L , Muramatsu N ((2019) ) The digital divide in health-related technology use: The significance of race/ethnicity. Gerontologist 59: , 6–14. |
[26] | Johansson S , Gulliksen J , Gustavsson C ((2021) ) Disability digital divide: The use of the internet, smartphones, computers and tablets among people with disabilities in Sweden. Univers Access Inf Soc 20: , 105–120. |
[27] | Pappas MA , Demertzi E , Papagerasimou Y , Koukianakis L , Voukelatos N , Drigas A ((2019) ) Cognitive-based E-learning design for older adults. Soc Sci 8: , 6. |
[28] | Anderson M, Perrin A, Tech Adoption Climbs Among Older Adults, https://www.pewresearch.org/internet/2017/05/17/tech-adoption-climbs-among-older-adults/, Accessed March 11, 2023. |
[29] | Levy H , Janke AT , Langa KM ((2015) ) Health literacy and the digital divide among older Americans. J Gen Intern Med 30: , 284–289. |
[30] | Wu Y-H , Damnée S , Kerhervé H , Ware C , Rigaud A-S ((2015) ) Bridging the digital divide in older adults: A study from an initiative to inform older adults about new technologies. Clin Interven Aging 10: , 193. |
[31] | Ikeda Y , Maruta M , Shimokihara S , Nakamura A , Han G , Tabira T ((2022) ) Difficulties in the use of everyday technology among older adults with subjective memory complaint and cognitive decline. Gerontology 68: , 655–663. |
[32] | Nygård L , Pantzar M , Uppgard B , Kottorp A ((2012) ) Detection of activity limitations in older adults with MCI or Alzheimer’s disease through evaluation of perceived difficulty in use of everyday technology: A replication study. Aging Mental Health 16: , 361–371. |
[33] | Grabinger RS , Aplin C , Ponnappa-Brenner G ((2008) ) Supporting learners with cognitive impairments in online environments. TechTrends 52: , 63–69. |
[34] | LaMonica HM , English A , Hickie IB , Ip J , Ireland C , West S , Shaw T , Mowszowski L , Glozier N , Duffy S ((2017) ) Examining internet and eHealth practices and preferences: Survey study of Australian older adults with subjective memory complaints, mild cognitive impairment, or dementia. J Med Internet Res 19: , e358. |
[35] | Benge JF , Kiselica AM , Aguirre A , Hilsabeck RC , Douglas M , Paydarfar D , Scullin MK ((2023) ) Technology use and subjective cognitive concerns in older adults. Arch Gerontol Geriatr 106: , 104877. |
[36] | Yang Q-H , Lyu X , Lin Q-R , Wang Z-W , Tang L , Zhao Y , Lyu Q-Y ((2022) ) Effects of a multicomponent intervention to slow mild cognitive impairment progression: A randomized controlled trial. Int J Nurs Studies 125: , 104110. |
[37] | Cooper C , Aguirre E , Barber JA , Bass N , Brodaty H , Burton A , Higgs P , Hunter R , Huntley J , Lang I ((2020) ) APPLE-Tree (Active Prevention in People at risk of dementia: Lifestyle, bEhaviour change and Technology to REducE cognitive and functional decline) programme: Protocol. Int J Geriatr Psychiatry 35: , 811–819. |
[38] | Blazheska-Tabakovska N, Savoska S, Ristevski B, Jolevski I, Gruevski D, Web content accessibility for people with cognitive disabilities, https://eprints.uklo.edu.mk/id/eprint/2337/1/AIIT2019_ProceedingsFinal_Web%20Content%20Accessibility%20for%20People%20with.pdf, Accessed May, 17. |
[39] | LeRouge C , Van Slyke C , Seale D , Wright K ((2014) ) Baby boomers’ adoption of consumer health technologies: Survey on readiness and barriers. J Med Internet Res 16: , e3049. |
[40] | Harris PA , Taylor R , Minor BL , Elliott V , Fernandez M , O’Neal L , McLeod L , Delacqua G , Delacqua F , Kirby J ((2019) ) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95: , 103208. |
[41] | World Medical Association ((2013) ) World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 310: , 2191–2194. |
[42] | McMaster M , Kim S , Clare L , Torres SJ , D’Este C , Anstey KJ ((2018) ) Body, Brain, Life for Cognitive Decline (BBL-CD): Protocol for a multidomain dementia risk reduction randomized controlled trial for subjective cognitive decline and mild cognitive impairment. Clin Interven Aging 13: , 2397–2406. |
[43] | Anstey KJ , Bahar-Fuchs A , Herath P , Rebok GW , Cherbuin N ((2013) ) A 12-week multidomain intervention versus active control to reduce risk of Alzheimer’s disease: Study protocol for a randomized controlled trial. Trials 14: , 60. |
[44] | Crook TH , Feher EP , Larrabee GJ ((1992) ) Assessment of memory complaint in age-associated memory impairment: The MAC-Q. Int Psychogeriatr 4: , 165–176. |
[45] | Reid M , Parkinson L , Gibson R , Schofield P , D’Este C , Attia J , Tavener M , Byles J ((2012) ) Memory complaint questionnaire performed poorly as screening tool: Validation against psychometric tests and affective measures. J Clin Epidemiol 65: , 199–205. |
[46] | Buckley R , Saling MM , Ames D , Rowe CC , Lautenschlager NT , Macaulay SL , Martins RN , Masters CL , O’Meara T , Savage G ((2013) ) Factors affecting subjective memory complaints in the AIBL aging study: Biomarkers, memory, affect, and age. Int Psychogeriatr 25: , 1307–1315. |
[47] | Faul F , Erdfelder E , Lang A-G , Buchner A ((2007) ) G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39: , 175–191. |
[48] | Wu Y-H , Lewis M , Rigaud A-S ((2019) ) Cognitive function and digital device use in older adults attending a memory clinic. Gerontol Geriatr Med 5: , 2333721419844886. |
[49] | McHugh ML ((2013) ) The chi-square test of independence. Biochem Med 23: , 143–149. |
[50] | IBM Corp ((2017) ) IBM SPSS Statistics for Windows. Version 25.0. IBM Corp, Armonk, NY. |
[51] | Wind TR , Rijkeboer M , Andersson G , Riper H ((2020) ) The COVID-19 pandemic: The ‘black swan’ for mental health care and a turning point for e-health. Internet Interven 20: , 100317. |
[52] | Whitehead L , Glass C , Coppell K ((2022) ) The effectiveness of goal setting on glycaemic control for people with type 2 diabetes and prediabetes: A systematic review and meta-analysis. J Adv Nurs 78: , 1212–1227. |
[53] | Epton T , Currie S , Armitage CJ ((2017) ) Unique effects of setting goals on behavior change: Systematic review and meta-analysis. J Consult Clin Psychol 85: , 1182. |
[54] | Clare L , Nelis SM , Jones IR , Hindle JV , Thom JM , Nixon JA , Cooney J , Jones CL , Tudor Edwards R , Whitaker CJ ((2015) ) The Agewell trial: A pilot randomised controlled trial of a behaviour change intervention to promote healthy ageing and reduce risk of dementia in later life. BMC Psychiatry 15: , 25. |
[55] | Sheppard AL , Wolffsohn JS ((2018) ) Digital eye strain: Prevalence, measurement and amelioration. BMJ Open Ophthalmol 3: , e000146. |
[56] | Burgess E , Hassmen P , Pumpa KL ((2017) ) Determinants of adherence to lifestyle intervention in adults with obesity: A systematic review. Clin Obes 7: , 123–135. |
[57] | Franco MR , Tong A , Howard K , Sherrington C , Ferreira PH , Pinto RZ , Ferreira ML ((2015) ) Older people’s perspectives on participation in physical activity: A systematic review and thematic synthesis of qualitative literature. Br J Sports Med 49: , 1268–1276. |
[58] | Robert PH , Berr C , Volteau M , Bertogliati-Fileau C , Benoit M , Guerin O , Sarazin M , Legrain S , Dubois B , PréAL Study Group ((2008) ) Importance of lack of interest in patients with mild cognitive impairment. Am J Geriatr Psychiatry 16: , 770–776. |
[59] | Martin E , Velayudhan L ((2020) ) Neuropsychiatric symptoms in mild cognitive impairment: A literature review. Dement Geriatr Cogn Disord 49: , 146–155. |
[60] | Begum A , Morgan C , Chiu CC , Tylee A , Stewart R ((2012) ) Subjective memory impairment in older adults: Aetiology, salience and help seeking. Int J Geriatr Psychiatry 27: , 612–620. |
[61] | Shaw C , Brittain K , Tansey R , Williams K ((2008) ) How people decide to seek health care: A qualitative study. Int J Nurs Stud 45: , 1516–1524. |
[62] | Hedman A , Nygard L , Almkvist O , Kottorp A ((2015) ) Amount and type of everyday technology use over time in older adults with cognitive impairment. Scand J Occup Ther 22: , 196–206. |
[63] | Williamson A ((2000) ) Gender issues in older adults’ participation in learning: Viewpoints and experiences of learners in the University of Third Age (U3A). Educ Gerontol 26: , 49–66. |
[64] | Einolf CJ ((2011) ) Gender differences in the correlates of volunteering and charitable giving. Nonprofit Volunt Sect Q 40: , 1092–1112. |




