Progression of Blood-Brain Barrier Leakage in Patients with Alzheimer’s Disease as Measured with the Cerebrospinal Fluid/Plasma Albumin Ratio Over Time
Abstract
Background:
Studies have found a disruption of the blood-brain barrier (BBB) in patients with Alzheimer’s disease (AD), but there is little evidence of the changes in the BBB over time. The cerebrospinal fluid’s (CSF) protein concentration can be used as an indirect measurement for the permeability of the BBB using the CSF/plasma albumin quotient (Q-Alb) or total CSF protein.
Objective:
In the current study, we wanted to investigate the changes in Q-Alb in patients with AD over time.
Methods:
A total of 16 patients diagnosed with AD, who had at least two lumbar punctures performed, were included in the current study.
Results:
The difference in Q-Alb over time did not show a significant change. However, Q-Alb increased over time if the time interval was > 1 year between the measurements. No significant associations between Q-Alb and age, Mini-Mental State Examination, or AD biomarkers were found.
Conclusion:
The increase in Q-Alb suggests that there is an increased leakage through the BBB, which may become more prominent as the disease progresses. This may be a sign of progressive underlying vascular pathology, even in patients with AD without major vascular lesions. More studies are needed to further understand the role of BBB integrity in patients with AD over time and the association with the progression of the disease.
INTRODUCTION
The blood-brain barrier (BBB) is essential for normal brain function [1] and has shown to be disrupted in patients with dementia due to different etiologies [2,3]. To measure the permeability of the BBB, studies have previously used the concentration of cerebrospinal fluid (CSF) protein [4]. Specifically, the CSF cerebrospinal fluid/plasma albumin quotient (Q-Alb) serves as a standard measurement and is an ideal parameter for the permeability of the BBB. Previous studies have found that Q-Alb may be a possible marker of disease for both Lewy body dementia and vascular dementia [3,5–7].
In patients with Alzheimer’s disease (AD), the results have varied [7–11]. One meta-analysis showed that Q-Alb is not suitable as a biomarker for AD [8]. However, other studies, using dynamic contrast-enhanced magnetic resonance imaging (MRI), which uses gadolinium as a contrast agent, have shown breakdown of the BBB in the hippocampus [2] or a global BBB leakage [12] in the early stages of AD. In addition, postmortem studies of patients with AD have also shown a breakdown of the BBB [13,14], which may suggest that the BBB is part of the pathophysiological processes in AD. Since albumin is a large protein with a molecular weight of 66 kDa, it cannot be used to determine if patients have smaller leaks in the BBB. However, an increased permeability of the BBB would be expected as the disease progresses, and Q-Alb may therefore increase in patients with AD.
In the current exploratory study, we investigated the changes in the BBB over time measured with Q-Alb in patients with AD from a retrospective clinical cohort. The cross-sectional analysis of Q-Alb has previously been investigated [11]. In addition, we investigated the association between Q-Alb and age in patients with AD, as well as cognitive performance as measured with the Mini-Mental State Examination (MMSE).
METHODS
The data was obtained from the Danish Dementia Biobank (approved by the Danish Data protection agency case no RH-30-0284/00622). The included patients underwent diagnostic evaluation at the Memory Clinic, Rigshospitalet and gave informed consent for their data and biological samples to be used for research purposes. This project was approved by the Danish Data Protection agency VD-2018-62/6279.
Participants
The included patients with AD fulfilled the NIA-AA criteria or the NINCDS-ADRDA criteria for AD [15,16] and had at least two lumbar punctures performed. Standard diagnostic evaluation at the Danish Dementia Research Centre included medical history, informant-based history, standard blood tests, neurological examinations, cognitive testing, including the MMSE [17] and Addenbrooke’s Cognitive Examination (ACE) [18], as well as a structural scan (MRI or computed tomography). Based on clinical evaluation, supplementary investigations were administered; [18F]Fluro-deoxy-glucose-PET (FDG-PET), full neuropsychological examination, and in the current study, lumbar puncture. The reason for multiple lumbar punctures were either 1) participating in a clinical trial in the placebo group, 2) the finding of a slightly increased number of cells in the CSF, which at the following lumbar puncture performed within a month was normal, 3) a new referral to the clinic due to new symptoms that were interpreted as symptoms of a neurodegenerative disorder, or 4) as part of the diagnostic evaluation for idiopathic normal pressure hydrocephalus (iNPH) in patients who were later diagnosed with AD. The latter group consisted of one patient, who at the first visit fulfilled criteria for possible iNPH [19], but after evaluation the diagnosis was ruled out. After re-referral (because of progressive cognitive dysfunction), a new evaluation led to a diagnosis of AD. If the patients had any shunt operations performed, they were not included in the study. If the CSF sample was contaminated with blood (500 red blood cells/μL [20]), it was excluded. For a full overview of the patients, see Table 1.
Table 1
Characteristics of the study cohort. Table showing the sex, age, and MMSE including all Q-Alb values and time between first and last lumbar puncture for all patients
| ID | Sex (M/F) | Age at first LP | MMSE at first LP | Q-Alb at first LP | Q-Alb at second LP | Q-Alb at third LP | Q-Alb at fourth LP | Time between first at last LP (days) | Reasons for more than one LP |
| 1 | M | 80 | 28 | 12.00 | 21.42 | – | – | 1,092 | Re-referral |
| 2 | M | 52 | 26 | 3.18 | 11.75 | – | – | 1737 | Trial (placebo) |
| 3 | F | 79 | 23 | 6.50 | 8.75 | – | – | 73 | N.A. |
| 4 | M | 69 | 19 | 15.20 | 15.80 | 12.90 | 14.40 | 370 | Trial (placebo) |
| 5 | F | 57 | 23 | 6.40 | 6.80 | – | – | 58 | N.A. |
| 6 | M | 68 | N.A. | 5.40 | 5.70 | 6.40 | 8.60 | 1,688 | Trial (placebo) |
| 7 | F | 79 | 19 | 8.70 | 8.90 | – | – | 16 | Increased number of cells (14) in CSF |
| 8 | M | 63 | 24 | 8.00 | 8.60 | 6.80 | 8.00 | 396 | Trial (placebo) |
| 9 | M | 62 | 21 | 7.70 | 6.40 | 8.30 | – | 639 | Trial (placebo) |
| 10 | F | 77 | 29 | 4.20 | 4.00 | – | – | 139 | Trial (placebo) |
| 11 | F | 55 | 17 | 2.20 | 3.60 | – | – | 1,964 | Re-referral |
| 12 | F | 76 | 26 | 4.00 | 3.60 | – | – | 27 | Increased number of cells (8) in CSF |
| 13 | M | 67 | 29 | 4.90 | 3.40 | – | – | 237 | Trial (placebo) |
| 14 | M | 56 | 28 | 5.50 | 5.30 | 6.00 | – | 566 | Trial (placebo) |
| 15 | F | 77 | 23 | 4.10 | 2.80 | – | – | 224 | Trial (placebo) |
| 16 | F | 54 | 26 | 4.90 | 5.20 | – | – | 184 | Trial (placebo) |
ID, identification number; M, male; F, female; MMSE, mini mental state examination; LP, lumbar puncture; Q-Alb, CSF/plasma albumin quotient; N.A., not available; CSF, cerebrospinal fluid.
A total of 63% (10/16) of the patients underwent MRI scan at the same time as the first lumbar puncture (<6 months apart). Of the MRI scans, Fazekas score was possible to obtain in nine of the MRI scans. While some of the patients had multiple MRI scans, we did not conduct any further analysis of the association between Q-Alb and Fazekas score due to the low sample size, lack of MRI scans for some of the participants and a difference in time between MRI acquisition and lumbar puncture.
Due to the retrospective nature of the study, we were only able to obtain AD biomarker values for a limited number of participants for amyloid (n = 11), phosphorylated tau (p-tau) (n = 11) and total tau (n = 10). For phosphorylated tau and total tau, the threshold were 80 pg/ml and 400 pg/ml, respectively. For amyloid-β 1-42 (Aβ42), an upwards drift in the CSF levels has been reported [21], and we have therefore only reported whether the Aβ42 values were above or below the year-specific threshold.
Measurements
All analyses were performed as part of the routine diagnostic assessment of the patients. All analyses were performed on Cobas 8000 (Roche diagnostics) instruments at the Department of Clinical Biochemistry at Rigshospitalet, using commercial and validated kits. Plasma albumin levels were analyzed by absorption, and CSF albumin levels were analyzed by an immunoturbidimetric assay.
Statistics
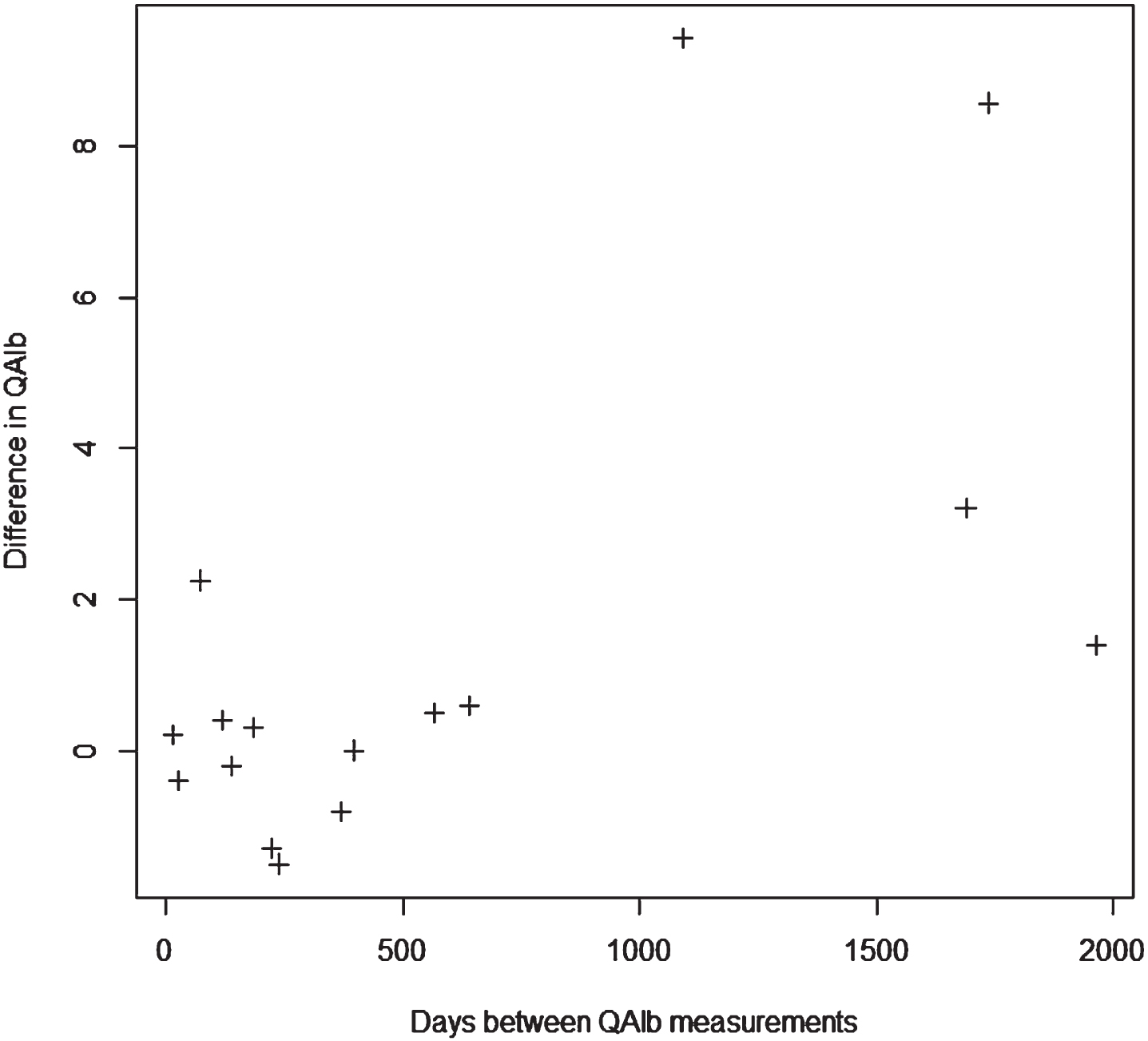
All statistics were performed in RStudio (v1.2.1335). When more than two lumbar punctures had been performed (n = 5), the first and last lumbar punctures were used for the primary analysis. Here, we performed a one-sample t-test using the percentage change between baseline and follow-up Q-Alb score (follow-up Q-Alb/baseline Q-Alb *100– 100). Furthermore, paired t-test was computed. Since we found a possible association with time between lumbar punctures and Q-Alb (see Fig. 1), we used a Mann-Whitney U test (unpaired, two-sample), to examine if the difference in Q-Alb between the first and last lumbar puncture was different between the patients, who had the first and the last lumbar punctures performed within one year (group 1), as compared to those who had the lumbar punctures performed with a time gap of more than a year (group 2).
Fig. 1
Scatterplot showing the change in QAlb and time between the two measurements. A larger difference was seen when longer time passed between lumbar punctures.
Since both gender and age have an impact on Q-Alb [22], we performed a linear regression between baseline Q-Alb and age. The number of males and females was equal, and therefore we did not consider this as a confounding factor. Furthermore, we investigated if there was an association between baseline Q-Alb and MMSE, p-tau, and total tau.
The R code and all output from the subsequent analyses can be found in the Supplementary Material.
RESULTS
Demographics
A total of 16 patients with AD were included in this study with even male (n = 8) and female (n = 8) distribution. The mean age for all patients was 66.9 (SD: 9.8), and MMSE was available for 15 patients with a mean score of 24.1 (SD: 3.7). In patients who had AD CSF markers, we found that all were amyloid positive (n = 11), but the mean total tau (mean (SD): 524.3 (271.3)) and p-tau (mean (SD): 85.3 (36.5)) values were above the cut-off values. In those who had an MRI with Fazekas score (9/16), six patients had a Fazekas score of one, whereas three had a score of two. For a full overview of the age, MMSE score and all Q-Alb values including time interval between first and last Q-Alb measurement can be seen in Table 1.
Changes in cerebrospinal fluid/plasma albumin ratio
The one-sample t-test for the difference in Q-Alb over time did not show a significant change (t = 1.7717, p = 0.0968, 95% CI: – 0.29– 3.12). Furthermore, no significant differences were found for the paired t-tests with or without log-transformation. When examining the association between Q-Alb and the time between the lumbar punctures (see Fig. 1), a larger difference was seen when longer time passed between the lumbar punctures. When performing a Mann– Whitney U test between the Q-Alb values for the participants, who had an additional lumbar puncture within one year (n = 8) and after more than one year (n = 8), a significant difference (p = 0.0281) was found.
Correlations between Q-Alb and biomarkers, age, and MMSE
No significant correlations were found between baseline Q-Alb and age at baseline (p = 0.216), MMSE (p: 0.42), p-tau (p: 0.62), or total tau (p: 0.65).
DISCUSSION
In the current retrospective study, we found that Q-Alb increased in patients with AD over time when the time interval was > 1 year between the measurements. In addition, we found that there seemed to be little variability between the measured Q-Alb if it was repeated within the first year (see Fig. 1). However, more studies are needed to further understand the variability in BBB leakage in patients with AD. No significant associations were found between baseline Q-Alb and MMSE, age, p-tau, or total tau.
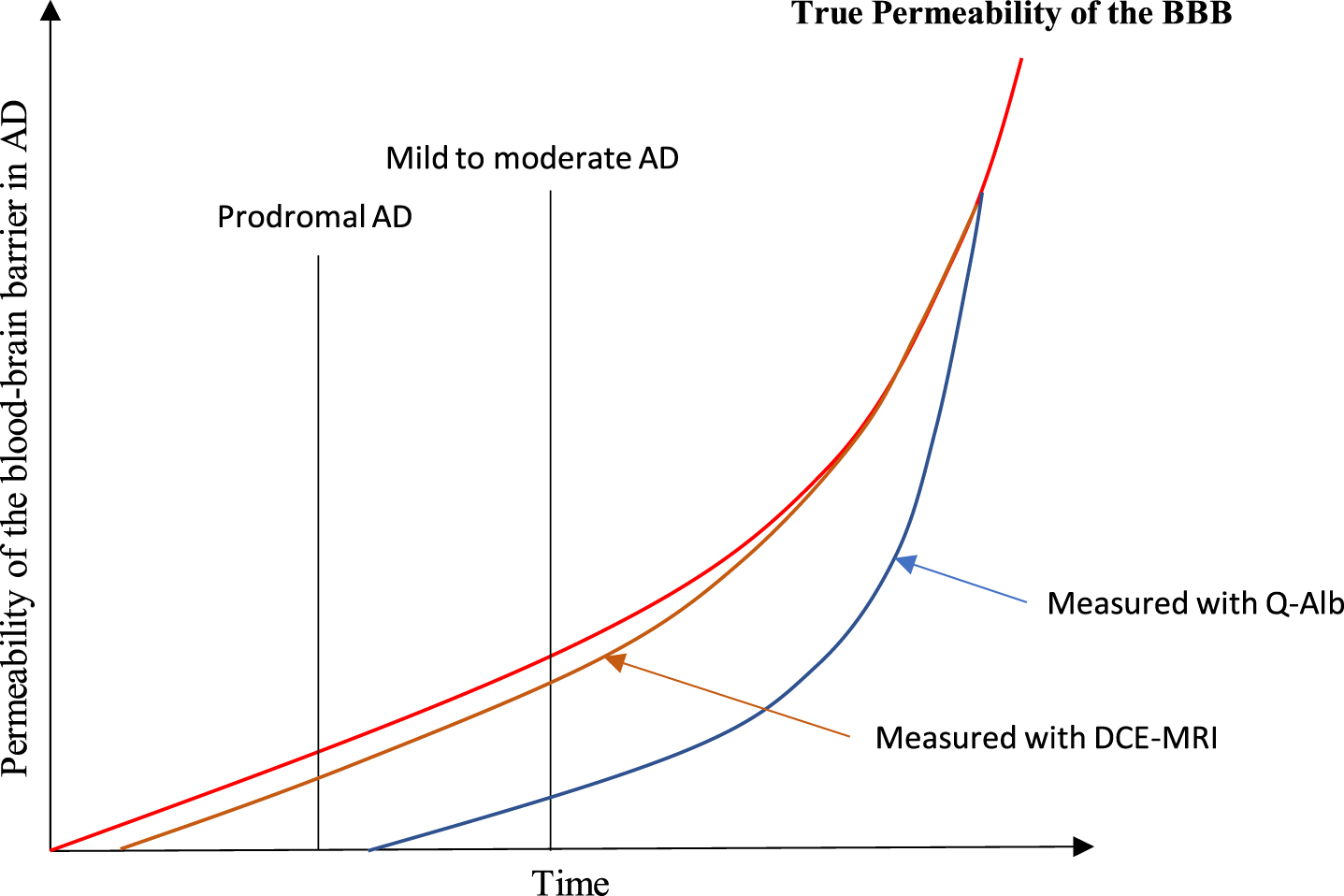
One explanation for the increasing Q-Alb in patients with AD may be an increasing load of vascular pathology, which has been shown to be an important factor for worsening of cognitive functions [23]. In patients with vascular dementia, studies have found significant higher Q-Alb as compared to healthy control [24]. This may suggest that AD leads to an increased number of vascular lesions and subsequently an increased Q-Alb. Furthermore, an autopsy study has shown that in patients with AD, 80% had vascular pathology and this was associated with worse cognitive test score [25], which suggests that vascular pathology plays a substantial role in AD. Overall, a theory, which has been named “the two-hit vascular hypothesis of AD” [26], suggests that damage to blood vessels causes BBB dysfunction and diminished brain perfusion, which leads to neuronal injury [27–29]. However, more studies are needed to confirm this theory. In addition, since albumin is a large protein, no changes in Q-Alb can be observed in early disease stages but become evident as the breakdown of the BBB worsens. This could be due to a much more rapid increase in BBB permeability at the later stages of AD. A proposed model for the BBB leakage in patients with AD and the possibility to observe these changes with dynamic contrast-enhanced MRI and Q-Alb is presented in Fig. 2. As can be seen from the figure, we hypothesize that the increased BBB permeability is only observed for Q-Alb in the later stages of AD. Therefore, dynamic contrast-enhanced MRI may be better suited to investigate the changes in the BBB in the early stages of AD. Furthermore, it would be of interest to understand other molecular biomarkers of BBB damage in CSF. Here, soluble platelet-derived growth factor β (sPDGFRβ), a biomarker of pericyte injury and subsequent BBB breakdown, could be a candidate [30]. Studies have found that increased levels of sPDGFRβ in the CSF of APOE ɛ4 carriers, which was positively correlated with Q-Alb, could predict future cognitive decline [31]. Furthermore sPDGFRβ has been shown to be present early in the disease [32]. Therefore, future studies on CSF markers of BBB injury in patients with early AD should investigate sPDGFRβ.
Fig. 2
A proposed model for the BBB leakage in patients with AD and the possibility to observe these changes with dynamic contrast-enhanced MRI and Q-Alb. As can be seen from the figure, we hypothesize that the increased BBB permeability is only observed in the later stages of AD.
In a previous study, examining the BBB using Q-Alb, Q-Alb was stable over one year of examination [33], which is similar to our findings (see Fig. 1). In the current study, we found an increasing Q-Alb over time, which could suggest that Q-Alb is associated with progression of the disease or possibly underlying vascular pathology. Further studies are needed to understand the variability of BBB leakage and the possible association with the progression of the disease.
Studies have found a positive association between Q-Alb and age in healthy controls [34, 35], and therefore we investigated the possible association with baseline Q-Alb in patients with AD. Here, we did not find any association, which may be due to the low sample size. Furthermore, we did not find any association with MMSE, which may be due to low sample size, Since leakage through the BBB in the hippocampus has been found to be present in the early disease stages [2], it would be interesting to investigate the association between Q-Alb and more specific neuropsychological tests, measuring memory.
The current study has some limitations. The data were collected retrospectively from a clinical cohort, which means that the time intervals were not set at specific time points and that multiple lumbar punctures may have been performed due to diagnostic challenges or unexpected findings (Table 1). Furthermore, information on some patient characteristics, like disease duration, could not reliably be interpreted, which meant that we could not understand the role of Q-Alb as a prognostic marker. In addition, we did not have any information of APOE carrier status, as this is not investigated during routine clinical examination. Since one APOE ɛ4 allele has been shown to be associated with elevated Q-Alb in older cognitively normal subjects [36], APOE carrier status should be included in future studies. However, the largest difference in Q-Alb was seen in the patients for whom the lumbar punctures were justified from participation in a clinical trial (placebo group), which suggests that our findings cannot be ascribed to alternative etiologies of cognitive impairment or cells in the spinal fluid. Furthermore, the low number of patients/participants may influence the findings. Therefore, more studies are needed to investigate the role of Q-Alb or dynamic contrast enhanced MRI imaging over time in order to understand the neuropathological role of the BBB and the variability in BBB leakage in patients with AD.
Conclusions
In the present study, we found that Q-Alb increases in patients with AD over time, and we speculate that this may be a sign of underlying vascular pathology. Furthermore, within the first follow-up year Q-Alb was stable for most of the patients, which suggests that longer periods of time are needed to observe changes in the BBB with Q-Alb. More studies are needed to further understand the neuropathological role and variability in BBB leakage in patients with AD over time.
ACKNOWLEDGMENTS
The authors have no acknowledgments to report.
FUNDING
The Danish Dementia Biobank was supported by the Absalon Foundation of May 1, 1978.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
DATA AVAILABILITY
Due to the legislation provided in the Danish Data Protection Act, the data that support the findings of this study are only available from the corresponding author upon reasonable request.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/ADR-230016.
REFERENCES
[1] | Daneman R , Prat A ((2015) ) The blood– brain barrier. Cold Spring Harb Perspect Biol 7: , a020412. |
[2] | Montagne A , Barnes SR , Sweeney MD , Halliday MR , Sagare AP , Zhao Z , Toga AW , Jacobs RE , Liu CY , Amezcua L , Harrington MG , Chui HC , Law M , Zlokovic BV ((2015) ) Blood-brain barrier breakdown in the aging human hippocampus. Neuron 85: , 296–302. |
[3] | Skillbäck T , Delsing L , Synnergren J , Mattsson N , Janelidze S , Nägga K , Kilander L , Hicks R , Wimo A , Winblad B , Hansson O , Blennow K , Eriksdotter M , Zetterberg H ((2017) ) CSF/serum albumin ratio in dementias: A cross-sectional study on 1861 patients. Neurobiol Aging 59: , 1–9. |
[4] | Felgenhauer K , Renner E ((1977) ) Hydrodynamic radii versus molecular weights in clearance studies of urine and cerebrospinal fluid. Ann Clin Biochem 14: , 100–104. |
[5] | Llorens F , Schmitz M , Gloeckner SF , Kaerst L , Hermann P , Schmidt C , Varges D , Zerr I ((2015) ) Increased albumin CSF/serum ratio in dementia with Lewy bodies. J Neurol Sci 358: , 398–403. |
[6] | Skoog I , Wallin A , Fredman P , Hesse C , Aevarsson O , Karlsson I , Gottfries CG , Blennow K ((1998) ) A population study on blood-brain barrier function in 85-year-olds: Relation to Alzheimer’s disease and vascular dementia. Neurology 50: , 966–971. |
[7] | Janelidze S , Hertze J , Nägga K , Nilsson K , Nilsson C , Wennström M , van Westen D , Blennow K , Zetterberg H , Hansson O ((2017) ) Increased blood-brain barrier permeability is associated with dementia and diabetes but not amyloid pathology or APOE genotype. Neurobiol Aging 51: , 104–112. |
[8] | Olsson B , Lautner R , Andreasson U , Öhrfelt A , Portelius E , Bjerke M , Hölttä M , Rosén C , Olsson C , Strobel G , Wu E , Dakin K , Petzold M , Blennow K , Zetterberg H ((2016) ) CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: A systematic review and meta-analysis. Lancet Neurol 15: , 673–684. |
[9] | Chalbot S , Zetterberg H , Blennow K , Fladby T , Andreasen N , Grundke-Iqbal I , Iqbal K ((2011) ) Blood-cerebrospinal fluid barrier permeability in Alzheimer’s disease. J Alzheimers Dis 25: , 505–515. |
[10] | Sundelöf J , Sundström J , Hansson O , Eriksdotter-Jönhagen M , Giedraitis V , Larsson A , Degerman-Gunnarsson M , Ingelsson M , Minthon L , Blennow K , Kilander L , Basun H , Lannfelt L ((2011) ) Higher cathepsin B levels in plasma in Alzheimer’s disease compared to healthy controls. J Alzheimers Dis 22: , 1223–1230. |
[11] | Musaeus CS , Gleerup HS , Høgh P , Waldemar G , Hasselbalch SG , Simonsen AH ((2020) ) Cerebrospinal fluid/plasma albumin ratio as a biomarker for blood-brain barrier impairment across neurodegenerative dementias. J Alzheimers Dis 75: , 429–436. |
[12] | van de Haar HJ , Burgmans S , Jansen JFA , van Osch MJP , van Buchem MA , Muller M , Hofman PAM , Verhey FRJ , Backes WH ((2016) ) Blood-brain barrier leakage in patients with early Alzheimer disease. Radiology 281: , 527–535. |
[13] | Sengillo JD , Winkler EA , Walker CT , Sullivan JS , Johnson M , Zlokovic BV ((2013) ) Deficiency in mural vascular cells coincides with blood-brain barrier disruption in Alzheimer’s disease. Brain Pathol 23: , 303–310. |
[14] | Ryu JK , McLarnon JG ((2009) ) A leaky blood-brain barrier, fibrinogen infiltration and microglial reactivity in inflamed Alzheimer’s disease brain. J Cell Mol Med 13: , 2911–2925. |
[15] | McKhann GM , Knopman DS , Chertkow H , Hyman BT , Jack CR , Kawas CH , Klunk WE , Koroshetz WJ , Manly JJ , Mayeux R , Mohs RC , Morris JC , Rossor MN , Scheltens P , Carrillo MC , Thies B , Weintraub S , Phelps CH ((2011) ) The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7: , 263–269. |
[16] | McKhann G , Drachman D , Folstein M , Katzman R , Price D , Stadlan EM ((1984) ) Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34: , 939. |
[17] | Folstein MF , Folstein SE , McHugh PR ((1975) ) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: , 189–198. |
[18] | Larner AJ ((2007) ) Addenbrooke’s Cognitive Examination (ACE) for the diagnosis and differential diagnosis of dementia. Clin Neurol Neurosurg 109: , 491–494. |
[19] | Relkin N , Marmarou A , Klinge P , Bergsneider M , Black PM ((2005) ) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57: , S4–16; discussion ii-v. |
[20] | Teunissen CE , Tumani H , Engelborghs S , Mollenhauer B ((2014) ) Biobanking of CSF: International standardization to optimize biomarker development. Clin Biochem 47: , 288–292. |
[21] | Simonsen AH , Musaeus CS , Christensen GL , Hasselbalch SG , Waldemar G ((2021) ) Upwards drift of cerebrospinal fluid amyloid-β 42 over twelve years in a consecutive clinical cohort. J Alzheimers Dis 81: , 1369–1373. |
[22] | Parrado-Fernández C , Blennow K , Hansson M , Leoni V , Cedazo-Minguez A , Björkhem I ((2018) ) Evidence for sex difference in the CSF/plasma albumin ratio in ∼20 000 patients and 335 healthy volunteers. J Cell Mol Med 22: , 5151–5154. |
[23] | Lorius N , Locascio JJ , Rentz DM , Johnson KA , Sperling RA , Viswanathan A , Marshall GA ((2015) ) Vascular disease and risk factors are associated with cognitive decline in the alzheimer disease . Alzheimer Dis Assoc Disord spectrum 29: , 18–25. |
[24] | Farrall AJ , Wardlaw JM ((2009) ) Blood– brain barrier: Ageing and microvascular disease – systematic review and meta-analysis. Neurobiol Aging 30: , 337–352. |
[25] | Toledo JB , Arnold SE , Raible K , Brettschneider J , Xie SX , Grossman M , Monsell SE , Kukull WA , Trojanowski JQ ((2013) ) Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer’s Coordinating Centre. Brain 136: , 2697–2706. |
[26] | Sweeney MD , Sagare AP , Zlokovic BV ((2018) ) Blood– brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol 14: , 133–150. |
[27] | Zlokovic BV ((2011) ) Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nat Rev Neurosci 12: , 723–738. |
[28] | Zhao Z , Nelson AR , Betsholtz C , Zlokovic BV ((2015) ) Establishment and dysfunction of the blood-brain barrier. Cell 163: , 1064–1078. |
[29] | Nelson AR , Sweeney MD , Sagare AP , Zlokovic BV ((2016) ) Neurovascular dysfunction and neurodegeneration in dementia and Alzheimer’s disease. Biochim Biophys Acta 1862: , 887–900. |
[30] | Sweeney MD , Sagare AP , Pachicano M , Harrington MG , Joe E , Chui HC , Schneider LS , Montagne A , Ringman JM , Fagan AM , Morris JC , Pa J , Nation DA , Toga AW , Zlokovic BV ((2020) ) A novel sensitive assay for detection of a biomarker of pericyte injury in cerebrospinal fluid. Alzheimers Dement 16: , 821–830. |
[31] | Montagne A , Nation DA , Sagare AP , Barisano G , Sweeney MD , Chakhoyan A , Pachicano M , Joe E , Nelson AR , D’Orazio LM , Buennagel DP , Harrington MG , Benzinger TLS , Fagan AM , Ringman JM , Schneider LS , Morris JC , Reiman EM , Caselli RJ , Chui HC , Tcw J , Chen Y , Pa J , Conti PS , Law M , Toga AW , Zlokovic BV ((2020) ) APOE4 leads to blood-brain barrier dysfunction predicting cognitive decline. Nature 581: , 71–76. |
[32] | Lv X , Zhang M , Cheng Z , Wang Q , Wang P , Xie Q , Ni M , Shen Y , Tang Q , Gao F ((2023) ) Changes in CSF sPDGFRβ level and their association with blood-brain barrier breakdown in Alzheimer’s disease with or without small cerebrovascular lesions. Alzheimers Res Ther 15: , 51. |
[33] | Bowman GL , Kaye JA , Moore M , Waichunas D , Carlson NE , Quinn JF ((2007) ) Blood-brain barrier impairment in Alzheimer disease: Stability and functional significance. Neurology 68: , 1809–1814. |
[34] | Eeg-Olofsson O , Link H , Wigertz A ((1981) ) Concentrations of CSF proteins as a measure of blood brain barrier function and synthesis of IgG within the CNS in ‘normal’ subjects from the age of 6 months to 30 years. Acta Paediatr 70: , 167–170. |
[35] | Hegen H , Auer M , Zeileis A , Deisenhammer F ((2016) ) Upper reference limits for cerebrospinal fluid total protein and albumin quotient based on a large cohort of control patients: Implications for increased clinical specificity. Clin Chem Lab Med 54: , 285–292. |
[36] | Halliday MR , Pomara N , Sagare AP , Mack WJ , Frangione B , Zlokovic BV ((2013) ) Relationship between cyclophilin A levels and matrix metalloproteinase 9 activity in cerebrospinal fluid of cognitively normal Apolipoprotein E4 carriers and blood-brain barrier breakdown. JAMA Neurol 70: , 1198–1200. |




