Occupational Therapist-Led Mindfulness Training Program for Older Adults Living with Early Cognitive Decline in Primary Care: A Pilot Randomized Controlled Trial
Abstract
Background:
Community-dwelling older adults with early cognitive deficits experience less efficiency in performing everyday life tasks, resulting in decreased satisfaction and other adverse psychological outcomes. Mindfulness training has been linked to cognitive and psychological improvements and, most recently, has been identified as a potential intervention supporting performance of everyday life activities.
Objective:
This study aimed to evaluate whether mindfulness practice can improve perceived performance and satisfaction with everyday life activity and secondary psychological outcomes.
Methods:
This study is a pilot randomized controlled trial (RCT) in an interprofessional primary care team practice in Toronto, Ontario, Canada. The participants were 27 older adults aged 60 years of age or older living with early cognitive deficits. Participants were randomized into an 8-Week mindfulness training program (n = 14) group or a Wait-List Control (WLC; n = 13) group compared at baseline, post-intervention and 4-weeks follow-up. MANOVAs with post-hoc independent t-tests were used to compare between groups at different time points.
Results:
There was a significant improvement in anxiety for the intervention group compared to the WLC group at post-intervention; Time-2 (mean difference = 3.90; CI = 0.04-7.75; p = 0.04) with large effect size (d = 0.80).
Conclusion:
Mindfulness training significantly improved anxiety scores for patients with early cognitive deficits post-intervention. Further work is required to test the sustainability of reduced anxiety over time, but this study demonstrated that MBSR is a promising primary care intervention for those living with early cognitive deficits. This study warrants the pursuit of a future study in exploring how long the reduced anxiety effects would be sustained.
INTRODUCTION
The prevalence of memory complaints increases with age [1, 2] as approximately a third of community-dwelling older adults will report some degree of memory complaints [3, 4]. The earliest form of memory complaint is subjective cognitive decline (SCD), a report of self- experienced persistent decline in cognitive capacity, compared with a previously cognitive status and normal performance on standardized cognitive tests used to classify MCI, adjusted for age, sex, and education [5, 6]. Next on the spectrum is mild cognitive impairment (MCI), which is described as clinically significant impairment with 1) increasing forgetfulness raised by the individual or informant, or observed by a clinician; 2) preservation of basic ADL (e.g., bathing, dressing, toileting); 3) impairment in one of the cognitive domains encompassing learning memory, language, visuospatial ability, executive function, and psychomotor skills; whereas dementia affects two or more of the cognitive domains [7, 8]. It is estimated that within five to six years of follow-up, approximately 50-80% of patients with MCI will convert to Alzheimer’s disease or a related form of dementia (ADRD) [9, 10].
Currently, 419,000 Canadians aged 65 and older are living with dementia, and 78,600 new cases are diagnosed every year. With a rapidly aging population in Canada, the total health care costs and out-of-pocket costs for Canadians with dementia care are projected to be $16.6 billion by 2031 [11]. Early cognitive decline such as SCD or MCI has been suggested to be a first possible symptomatic sign of prodromal ADRD [12]. Exploring interventions to potentially delay, prevent or mitigate the risk of dementia is critical.
Older adults living with cognitive deficits such as SCD or MCI can perform functional activities, such as basic activities of daily living (ADL) [13]. However, some individuals may perform complex everyday instrumental activities of daily living (iADL) with less efficiency [14–17]. Some examples of inefficiency of iADLs include, managing finances, handling medications, and using everyday technology such as internet/phone banking, may contribute to increased anxiety and depression [3, 18, 19]. The decreased efficiency with everyday tasks has been shown to induce stress, adversely affecting a person’s emotional health, well-being, and quality of life (QoL) compared to same age-matched control participants without cognitive deficits [18]. Studies have reported that the use of adaptive coping strategies to prevent or alleviate psychological symptoms such as anxiety may also prevent or delay further cognitive decline in this population [20, 21].
To date, there is little evidence about the benefit of pharmacological interventions in slowing down the progression of cognitive decline, preserving functional performance, or alleviating the psychological consequences for those individuals living with SCD or MCI and Alzheimer’s disease. Pharmacological interventions may also have side-effects [22], drug-drug interaction [23], and increased risk of falls related to polypharmacy [24]. Consequently, identifying alternative non-pharmacological interventions such as behavioral strategies on its own or in parallel with pharmacological interventions to support cognition, functional performance, or improve QoL for those living with SCD or MCI is critical. Psychological support, such as Mindfulness-Based Stress Reduction (MBSR), is one nonpharmacological intervention gaining increased attention for its potential to improve psychological functioning and potentially self-perceived performance of everyday life activities [25, 26].
Emerging research on older adults with SCD or MCI posits that mindfulness training, such as MBSR, may remediate cognitive difficulties [27] and improve executive function [28]. Mindfulness training has been noted to have a dual mechanism of action that improves cognitive functioning. First, mindfulness has been shown to enhance physiological changes in the brain that include amygdala morphology with reduction in perceived stress; improvements in the domain of executive function; increased cortical thickness in regions associated with sensory, cognitive, and emotional processing that may provide a reserve against age-related cognitive decline [29–32]. Second, mindfulness improves psychological symptoms of anxiety, depressive mood, and promotes an overall sense of well-being and QoL, which has favorable effects of mitigating the exacerbating impact of cognitive decline [33–36]. There is evidence that mindfulness training positively impacts performance of activities-of-daily living (ADL) among older adults with neurodegenerative conditions, including MCI and Parkinson’s disease, who were recruited from memory clinics, primary care clinics, and community settings [37, 38].
Primary care is often the first point of contact when issues related to memory arise. It is increasingly recognized that an interprofessional team approach can better meet the evolving needs of persons with cognitive deficits in primary care than physician-only care [39, 40]. As members of a primary care team, occupational therapists are well-positioned to address both the functional and psychological needs of older adults with reports of memory impairment [14, 41].
Existing literature has already demonstrated the feasibility and usefulness of mindfulness-based interventions (MBIs) for many conditions in primary care, including psychological distress [42], depression [43], overweight and obesity [44], chronic disease [45], mental health conditions [46], chronic pain [47], chronic disease self-management behaviors [48], and most recently for community-dwelling older adults with SCD or MCI [49]. A meta-analysis by Demarzo et al. (2015) concluded that mindfulness-based interventions, such as MBSR, are promising interventions to enhance mental health, well-being, and quality of life among general primary care patients [50].
Within the past ten years, there is emerging research exploring the effectiveness of MBSR among older adults with SCD or MCI on reducing brain age, and improving cognitive functions [51, 52]. Furthermore, small proof-of-concept and pilot studies with MBSR have demonstrated the intervention to be feasible, well accepted, and to improve memory self-efficacy and increase brain volume among older adults with SCD and MCI [53, 54].
To the authors’ knowledge, there is limited research on SCD and MCI in primary care, specifically focusing on interprofessional team-based environments involving occupational therapy. Furthermore, many of the MBSR studies do not examine functional performance of everyday activities as a primary outcome. Therefore, this study will further build on these small proof-of-concept and pilot studies by adding an interprofessional perspective. As such, the aim of this study was to explore the impact of an occupational therapy-led MBSR on the perceived performance and satisfaction of everyday life activities and psychological outcomes among older adults with SCD or MCI in an interprofessional primary care setting.
METHODS
Study design
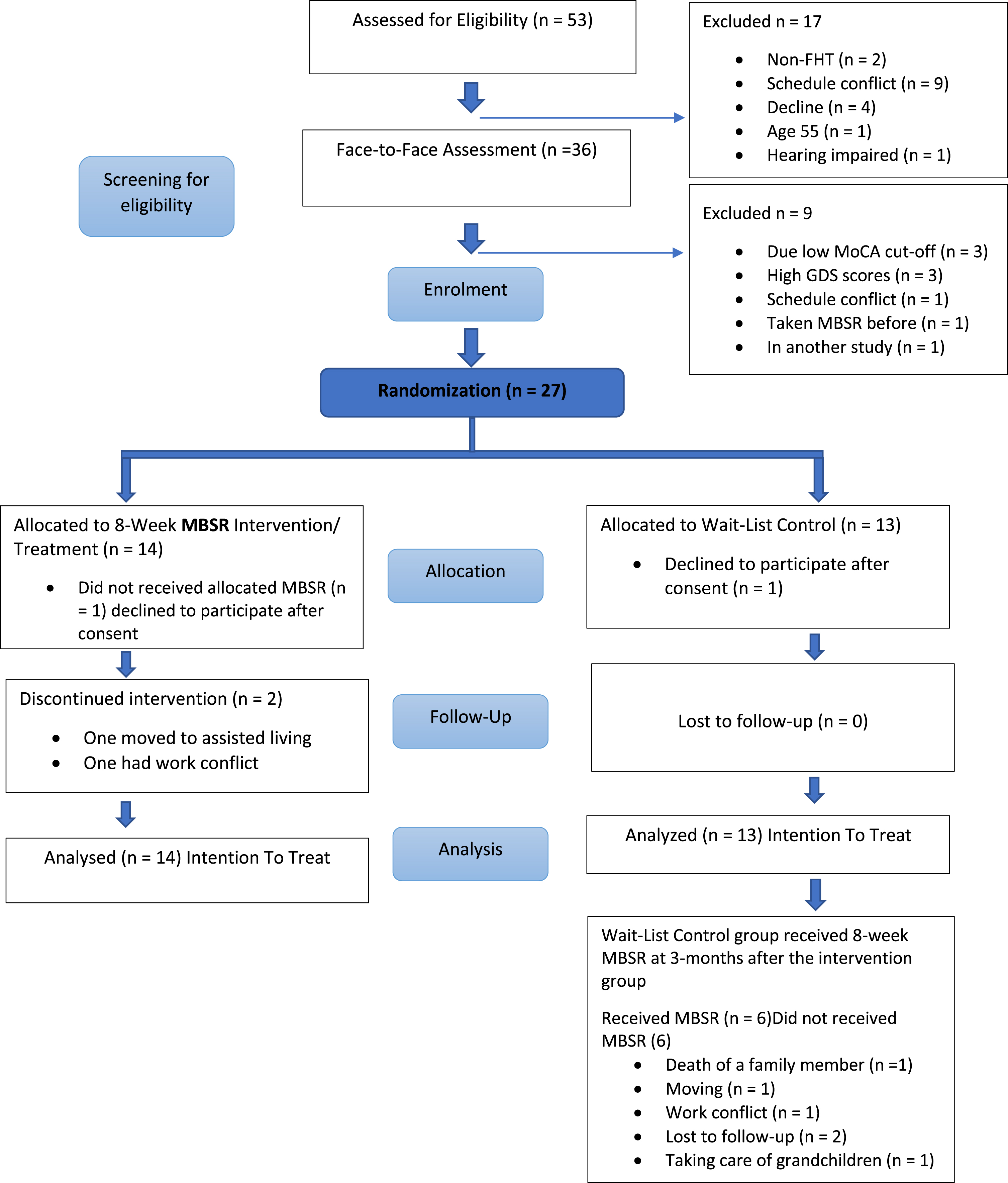
A single-blinded, pilot randomized controlled trial (RCT) with two parallel groups was used to evaluate primary and secondary clinical outcomes. Following the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) reporting [55] (See Fig. 1) was followed, and a detailed description of the study protocol has been published elsewhere [56].
Fig. 1
SPIRIT flow chart.
Study setting
The study took place between April and November 2019 at an interprofessional primary care clinic in Ontario, Canada. Approximately 25% of Ontarians receive their primary care from an interprofessional primary care team. These teams tend to focus on chronic disease management, disease prevention and health promotion [57]. The interprofessional team practice, in which the study was implemented, had 18,000 rostered patients living in an urban area, 36 physicians, two dieticians, one occupational therapist, one physiotherapist, two social workers, and one pharmacist. The primary care team provides diagnosis and treatment, internal referrals to other team members or external health care specialists, and after-hours urgent care services.
Participants
Participants were recruited through posters in the clinic waiting and examination rooms and flyers to potential participants from the primary care team, with the following inclusion criteria: 1) Age ≥ 60 years; 2) English fluency; 3) Living independently in the community; 4) Chart documented self-reported SCD or an MCI diagnosis; and 5) Rostered with the primary care team. Exclusion criteria included: 1) History of any prior participation in an MBSR or another mindfulness-based intervention in the past or current mindfulness or yoga practice ≥1.5 h per week; 2) History of significant medical (e.g., cancer), neurological (e.g., brain injury), or psychiatric condition (e.g., depression with ≥ 6 on the GDS, active psychosis), or bereavement that significantly impacts mood; 3) Substance use disorder; 4) MoCA score≤21; 5) Current participation in a community-based cognitive or memory training program or involved in another research study; or 6) Communication barriers (i.e., hearing impairment).
Recruitment
All interested participants were instructed to contact the Principal Investigator (PI), who in turn explained the purpose of the study, the study activities, and the randomization procedures into either an 8-Week MBSR program or a wait-list control (WLC) group. All interested participants were screened for eligibility by telephone, and if deemed appropriate, were scheduled for a face-to-face appointment. The Montreal Cognitive Assessment (MoCA) and Geriatric Depression Scale (GDS) were administered to screen for inclusion eligibility. Any participant with scores ≤ 19 on the MoCA or > 10 on the GDS were referred to their family physician for further assessment and were excluded from the study. Written consent was obtained from all interested participants who met the eligibility criteria.
Randomization
Study participants were randomized to either the 8-Week, MBSR program (not including orientation and one all-day silent retreat) or the 8-Week WLC group. Participants were randomized by a block size of four. Two participants were allocated into the MBSR group and two others in the WLC group, resulting in six different possible block combinations. The randomization design and sequence were carried out by an independent staff member not involved in the trial. Opaque envelopes were sealed to ensure allocation concealment. The study included 27 participants (MBSR n = 14; WLC; n = 13) based on our recruitment period between April and August, with an expected start date to run the MBSR group after three and a half months of recruitment. The WLC group received the MBSR program three months after the intervention group trial was completed.
Blinding
All research staff, including the PI, were blinded to the randomization list until the intervention and all data collection were completed. To reduce the risk of unblinding, a research assistant (RA) provided all reminder phone calls for the participants’ assessment dates and instructed them not to disclose which group they were in before their assessment. The qualified-MBSR teachers delivering the intervention were not blinded.
Sample size
As this was a feasibility study, the sample size was not formally calculated. Our goal was to recruit approximately 30-40 participants accounting for a 20% attrition rate based on other feasibility studies [58, 59]. In the three-and-a-half-month recruitment period, we were able to recruit 27participants.
Intervention procedures
The intervention was an 8-Week MBSR program established in 1979 by Kabat-Zinn [60] and followed the Mindfulness-Based interventions (MBIs) Teaching Assessment Criteria to ensure teaching integrity. Each of the nine sessions, including orientation, were three-hours in duration; a tenth session consisted of an all-day retreat of mindfulness practice (e.g., lying down body scan; sitting meditation; mindful eating; mindful movements, such as walking and light hatha yoga) and an inquiry about the practice. The all-day silent meditation retreat took place during week seven as a regular weekly session consisting of six and a half hours, rather than on a customary weekend based on the MBSR protocol. Thus, this extended the MBSR program an extra week from a standard 8-weeks to 9-week, as to make it consistent for ease of participants’ routine such as timing, location, and travel plans. However, there was no change made to the 30.5 h of classroom time based on the MBSR curriculum and participants were expected to complete a guided mindfulness practice at home for 30-45 min per day; six times a week throughout the intervention. Participants were encouraged to continue with the home practice for another four weeks after completing the MBSR group and to come back for follow-up at week 13.
Computer tablets (i.e., mini-iPads) were used to deliver the home training program and collect data on home training. Two primary qualified-MBSR teachers delivered the MBSR program, and two other secondary qualified-MBSR teachers, one of which was the PI, also supported the delivery but focused more on answering questions around technology, helping participants with positioning in mindful movement poses and assisted other administrative duties such as setting up the room. The two additional MBSR teachers supported participants with tablet use guidance before or after each session. Only participants who had access to Wi-Fi were given a computer tablet (i.e., mini-iPads) to use the Application (App) Insight Timer [61]. The App was used for home practice, and it also logged participants’ frequency and duration of mindfulness practice. Participants who did not have access to Wi-Fi were given compact discs, and they logged their home practice using pen and paper.
To track delivery and receipt fidelity, the PI: 1) monitored the MBSR curriculum to ensure the intervention was carried out per protocol by Qualified MBSR teachers; 2) collected participant attendance records and home practice diaries; 3) noted observational data of participants performing the mindfulness practices and level of engagement with inquiry and reflection during each session, 4) ensured participants who missed a session were followed-up by an research assistant with a phone call to provide the assigned home practice for the week; and last, 5) addressed any technological issues that arose.
Ethical considerations
This study was reviewed and approved by Research Ethics Board at Women’s College Hospital (REB# 2017-0056-E); and Queen’s University (REB# 6026418) Kingston, Ontario, Canada.
Measurement and timeline
The primary clinical outcome was the Canadian Occupational Performance Measure (COPM). This individualized, client-centered outcome measure aims to identify and assess an individual’s self-perceived difficulty in the performance of everyday activities and satisfaction with their performance [62]. A maximum of five everyday activities that are difficult can be identified, and each is rated on a 10-point scale. The COPM measures change in functional performance and satisfaction in these activities over time. The COPM has two main scores for each of the performance and satisfaction ratings, consisting of an average score calculated by summing individual problem scores and dividing by the number of problems. The second score is a change score calculated after a reassessment interval and then compared and evaluated for change [63].
The COPM has a strong test-retest reliability (ICC = 0.63 for performance and 0.84 for satisfaction) [64], with good responsiveness [63]. Furthermore, the COPM has been identified as a valuable tool to guide assessments as it focuses on function rather than medical symptoms and is ideal for clinicians to offer comprehensive client-centered services in an interprofessional primary care setting [65].
Secondary psychological clinical outcome measures included the Patient Health Questionnaire (PHQ-9), which has excellent internal reliability with a Cronbach’s of 0.89 in a PHQ-9 Primary Care Study, and excellent test-retest reliability [66]. The Geriatric Anxiety Inventory (GAI) has high inter-rater (r = 0.89) and test-retest (r = 0.86) reliability [67] and similarly, the Perceived Stress Scale (PSS) which has acceptable psychometric properties with satisfactory test-retest reliability criterion assessed at > 0.70 [68]. The Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) demonstrated internal consistency reliability with Cronbach’s alpha ranges from 0.61 to 0.81 [69]. In addition, the QoL-Alzheimer’s disease (QoL-AD) measure demonstrated good test-retest reliability and strong inter-rater reliability with Cohen’s kappa values > 0.70 [70]. Lastly, the Acceptance and Action Questionnaire (AAQ-II) has an alpha coefficient of 0.84 and demonstrated good test-retest reliability at 3 months at 0.81 and 12 months at 0.89 [71].
Assessments were conducted at three different time points: baseline (Time-1) at week 0, post-MBSR intervention (Time-2) at Week-9, and 1-month post-MBSR follow-up (Time-3) at Week-13. See Table 1 – Timeline. The PI conducted all assessments for both intervention and WLC participants at Time-1 (Week-0). A blinded independent assessor completed the post-intervention assessments at Time-2 (Week-9), and Time-3 (Week-12). All WLC group participants were assessed at the same intervals as the MBSR group.
Table 1
Time frame of measurements for participants
| Measures Taken | (Time 1) | (Time 2) | (Time 3) |
| Item | 0-week | 9-week (Post-MBSR) | 13-week (Follow-Up) |
| Screening | |||
| (MoCA and GDS) | X | ||
| Primary Outcome | |||
| COPM | X | X | X |
| Secondary Outcomes | |||
| GAI | X | X | X |
| AAQ-II | X | X | X |
| PHQ-9 | X | X | X |
| QoL-AD | X | X | X |
| PSS | X | X | X |
| CAMS-R | X | X | X |
Montreal Cognitive Assessment (MoCA); Geriatric Depression Scale (GDS); Canadian Occupational Performance Measure (COPM); Geriatric Anxiety Inventory (GAI); Acceptance and Action Questionnaire (AAQ-II); Patient Health Questionnaire-9 (PHQ-9); Quality-of-Life-Alzheimer’s disease (QoL-AD); Cognitive and Affective Mindfulness Scale-Revised (CAMS-R).
Data analysis
Baseline differences between the two groups, including primary and secondary outcomes, were compared using two-sample t-tests or χ2 tests or Fisher’s exact test for categorical variables. Missing data were managed using the “last observation carried forward’ (LOCF) method”, whereby the last measurement, which was taken before a participant withdrew from the study, is retained and used for data analysis [72].
To evaluate the impact of MBSR on the primary and secondary clinical outcomes, a multivariate analysis of variance (MANOVA) was conducted to compare the two groups (i.e., the MBSR and WLC groups), at Time-1 to Time-2, Time-2 to Time-3, and Time-1 to Time-3. Results for each measure were reported as between-group means, standard deviation (SD), average and change scores (for COPM only) and lastly, based on a MANOVA model, treatment effects and effect sizes in partial eta squared (np2). A 95% confidence interval (CI) and alpha of 0.05 were reported for statistical significance levels. A MANOVA was used as ANOVA would have violated this study’s assumption of the independence of the residual. Last, MANOVA uses an omnibus test (i.e., global test of time) and if significant, will be followed up by a t-test as per this study.
To investigate significant differences between the WLC and MBSR groups, post-hoc analysis using a pairwise comparison between three different time points, with a Bonferroni adjustment, was undertaken. We used an independent t-test for post-hoc analysis to investigate significant differences between the WLC and MBSR groups at three different time points, and the effect size is reported in Cohen’s d.
Participant demographics
From April to August 2019 (4.5 months), 53 participants were recruited, of which 17 were excluded at initial screening (nine were not patients of the primary care team; two had scheduling conflicts; four declined; one was below age cut-off; one had a hearing impairment). The remaining 36 participants completed a face-to-face screening where a further nine participants were deemed ineligible (three had low MoCA scores; three had high GDS scores; one was unable to attend the timing of the intervention; one had taken MBSR before; one was participating in another study). A total of 27 participants provided written consent and were randomized to the WLC (n = 13) or MBSR (n = 14) group. The overall drop-out rate in the study was 14.8%, with one WLC (one participant declined to participate after giving consent) and three MBSR groups (one moved to assisted living; one had a conflict with work; one declined to participate). Consequently, our final sample resulted in the following number of participants in our current study WLC (n = 12) and MBSR (n = 11). The SPIRIT flow chart provides the outline of the study in Fig. 1. No adverse events occurred during the duration of the study.
No differences were found between the participants in the MBSR and the WLC group, with the exception that more participants in the intervention group had a driver’s license. In addition, though not statistically significant, there was 1 male in the WLC group compared to 6 males in the MBSR group. See Table 2 for participants’ demographics.
Table 2
Demographics and characteristics of participants (n = 27)
| Characteristics | Total (No., % total) | ||
| MBSR n = 14 | Control n = 13 | Significance | |
| Age (Mean; SD), y | 71.43 (9.0) | 75.31 (9.5) | |
| Range | 60-83 | 62-92 | 0.28 |
| Sex: Female | 8 (57.1%) | 12 (92.3%) | 0.07 |
| Ethnicity | |||
| Caucasian | 8 (57.1%) | 10 (76.9%) | |
| Black | 4 (28.5%) | 2 (15.3%) | |
| Latino | 0 | 1 (7.1%) | |
| South Asian | 1 (7.1%) | 0 | |
| Asian | 0 | 1 (7.1%) | 0.93 |
| Education Level | |||
| None | 2 (14.3%) | 1 (7.7%) | |
| High School | 3 (21.4%) | 2 (15.4%) | |
| College | 0 (0%) | 3 (23.1%) | |
| University | 9 (64.3%) | 7 (53.8%) | 0.38 |
| Living Arrangement | |||
| Alone | 4 (28.6%) | 8 (61.5%) | |
| With partner | 6 (42.9%) | 2 (15.4% | |
| With family/friends | 4 w/ (28.6%) | 3 (23.1%) | 0.20 |
| Marital Status | |||
| Married | 11 (78.6%) | 11 (84.6%) | |
| Common-law | 1 (7.1%) | 2 (15.4%) | |
| Other | 2 (14.2%) | 0 | 0.38 |
| Currently Employed | |||
| Yes | 6 (42.9%) | 3 (23.1) | 0.42 |
| Household Income | |||
| < $50K | 8 (57%) | 6 (57%) | |
| $51-99K | 2 (14.2%) | 5 (38.5%) | |
| > $100K | 4 (28.6%) | 2 (15.4%) | 0.54 |
| Have Driver’s License | |||
| Yes | 11 (78.6%) | 5 (38.5%) | 0.03* |
| Currently Driving | |||
| No | 7 (50%) | 9 (69.2%) | 0.31 |
| Previous Head Injury | |||
| Yes | 5 (35.7%) | 5 (38.5%) | 1.00 |
| Physical Activity | |||
| Yes | 11 (78.6%) | 12 (92.3%) | |
| No | 3 (21.4%) | 1 (7.7%) | 0.59 |
| Duration of Physical Activity | |||
| (Mean; SD) h | 3.83 (3.21) | 6.76 (4.60) | 0.06 |
| Meditation Practice (≤1.5 h) | 3 (21.4%) | 2 (15.4%) | 1.00 |
| Montreal Cognitive Assessment | 25.00 (2.45) | 25.92 (2.29) | 0.33 |
| (MoCA) | |||
| MCI Diagnosis | |||
| Yes | 2 (14.3%) | 2 (15.4%) | 0.67 |
| Geriatric Depression Scale (GDS) | 2.14 (2.68) | 2.92 (2.49) | 0.44 |
*Significant at p (<0.05).
RESULTS
Primary clinical outcome
COPM: Performance (average and change scores)
Table 3 shows the COPM performance average and change scores, a significant main effect for time was found for both the intervention and WLC groups, with higher average and change scores post-intervention (p < 0.05; np2 =0.21). There was no significant interaction effect with group and time and no main effect comparing MBSR and WLC between the two groups on the COPM performance average and change scores. There was also no statistical significance between groups at any of the three different time points.
Table 3
Mean and Standard Deviation (All Data)
| Control (n = 13) | MBSR (n = 14) | ||||||||||||||
| Time-1 | Time-2 | Time-3 | Time-1 | Time-2 | Time-3 | Group x time | Time effect | Group effect | |||||||
| Outcome Measures | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | p (ES - h p2 **) | ||
| Canadian Occupational Performance Measure (COPM) | |||||||||||||||
| (Performance Average Scores) | 5.56 | 0.90 | 5.97 | 1.82 | 6.21 | 1.70 | 6.30 | 1.58 | 7.14 | 1.32 | 6.94 | 1.85 | 0.71 (0.02) | 0.05*(0.21) | 0.08 (0.11) |
| (Performance Change Scores) | 0.40 | 1.71 | 0.64 | 1.51 | 0.84 | 1.23 | 0.63 | 1.51 | 0.48 (0.02) | 0.96 (0.00) | 0.65 (0.00) | ||||
| Canadian Occupational Satisfaction | |||||||||||||||
| Measure (COPM) | |||||||||||||||
| (Satisfaction Average Scores) | 5.28 | 1.51 | 5.29 | 2.35 | 5.55 | 2.06 | 5.53 | 1.80 | 6.57 | 1.95 | 7.11 | 2.13 | 0.24 (0.11) | 0.11 (0.16) | 0.12 (0.09) |
| (Satisfaction Change Scores) | 0.01 | 1.76 | 0.28 | 1.93 | 1.04 | 1.48 | 1.58 | 2.40 | 0.69 (0.00) | 0.23 (0.05) | 0.69 (0.11) | ||||
| Geriatric Anxiety Inventory (GAI) | 7.38 | 7.00 | 6.62 | 4.94 | 4.77 | 4.34 | 5.93 | 7.28 | 2.71 | 4.76 | 2.64 | 4.88 | 0.07 (0.19) | 0.01*(0.33) | 0.21 (0.06) |
| Acceptance and Action Questionnaire | 17.46 | 9.70 | 17.23 | 8.44 | 16.85 | 8.15 | 20.00 | 8.44 | 15.93 | 4.56 | 15.07 | 6.15 | 0.28 (0.10) | 0.13 (0.16) | 0.95 (0.00) |
| (AAQ-II) | |||||||||||||||
| Patient Health Questionnaire | |||||||||||||||
| (PHQ-9) | 6.00 | 5.21 | 6.23 | 4.25 | 3.85 | 5.73 | 6.93 | 5.08 | 4.29 | 2.76 | 4.57 | 3.18 | 0.02*(0.26) | 0.03*(0.25) | 0.95 (0.00) |
| Quality-of-Life Alzheimer’s disease | |||||||||||||||
| (QoL-AD) | 38.69 | 7.00 | 37.62 | 8.47 | 38.77 | 6.89 | 34.36 | 5.30 | 37.29 | 3.76 | 36.79 | 4.63 | 0.03*(0.25) | 0.17 (0.14) | 0.33 (0.04) |
| Perceived Stress Scale (PSS) | 16.85 | 8.11 | 15.46 | 7.84 | 13.38 | 7.57 | 18.86 | 7.48 | 12.86 | 4.33 | 12.50 | 4.93 | 0.26 (0.11) | 0.01*(0.31) | 0.82 (0.00) |
| Cognitive Affective Mindfulness | |||||||||||||||
| Scale Revised (CAMS-R) | 29.31 | 5.87 | 29.38 | 6.79 | 28.54 | 6.35 | 27.14 | 6.20 | 29.71 | 4.97 | 31.36 | 4.31 | 0.08 (0.19) | 0.30 (0.10) | 0.87 (0.00) |
Time-1, baseline; Time-2, post-MBSR intervention; Time-3, 4-weeks follow-up; *significant at p (<0.05); (**Effect size described as partial eta squared). Table 4. Independent t-test between groups at different time points
Table 4
Independent t-test between groups at different time points
| Control (N = 13) | MBSR (N = 14) | Mean | ||||||
| M | SD | M | SD | p <0.05 | Difference | 95% CI | d | |
| COPM – Performance | ||||||||
| (Average scores) | ||||||||
| Time-1 | 5.56 | 0.90 | 6.30 | 1.58 | 0.14 | -0.73 | -1.76-0.28 | -0.56 |
| Time-2 | 5.97 | 1.82 | 7.14 | 1.32 | 0.07 | -1.17 | -2.45-0.10 | -0.74 |
| Time-3 | 6.21 | 1.70 | 6.94 | 1.85 | 0.29 | -0.72 | -2.13-0.67 | -0.41 |
| COPM – Performance | ||||||||
| (Change scores) | ||||||||
| Time-2 | 0.40 | 1.71 | 0.84 | 1.23 | 0.24. | -0.44 | -1.62-0.73 | -0.30 |
| Time-3 | 0.64 | 1.51 | 0.63 | 1.51 | 0.62 | 0.00 | -1.22-1.22 | 0.00 |
| COPM – Satisfaction | ||||||||
| (Average scores) | ||||||||
| Time-1 | 5.28 | 1.51 | 5.53 | 1.80 | 0.70 | -0.25 | -1.56-1.06 | -0.14 |
| Time-2 | 5.29 | 2.35 | 6.57 | 1.95 | 0.14 | -1.27 | -3.00-0.44 | -0.59 |
| Time-3 | 5.55 | 2.06 | 7.11 | 2.13 | 0.06 | -1.55 | -3.21-0.11 | -0.74 |
| COPM – Satisfaction | ||||||||
| (Change scores) | ||||||||
| Time-2 | 0.01 | 1.76 | 1.04 | 1.48 | 0.38 | -1.03 | -2.32-0.25 | -0.63 |
| Time-3 | 0.28 | 1.93 | 1.58 | 2.40 | 0.57 | -1.30 | -3.03-0.43 | -0.59 |
| GAI | ||||||||
| Time-1 | 7.38 | 7.00 | 5.93 | 7.28 | 0.60 | 1.45 | -4.21-7.12 | 0.20 |
| Time-2 | 6.62 | 4.94 | 2.71 | 4.76 | 0.04* | 3.90 | 0.04-7.75 | 0.80 |
| Time-3 | 4.77 | 4.34 | 2.64 | 4.88 | 0.24 | 2.12 | -1.52-5.78 | 0.44 |
| AAQ | ||||||||
| Time-1 | 17.46 | 9.70 | 20.00 | 8.44 | 0.47 | -2.53 | -9.78-4.70 | -0.28 |
| Time-2 | 17.23 | 8.44 | 15.93 | 4.56 | 0.62 | 1.30 | -4.23-6.84 | 0.19 |
| Time-3 | 16.85 | 8.15 | 15.07 | 6.15 | 0.53 | 1.77 | -4.01-7.56 | 0.24 |
| PHQ-9 | ||||||||
| Time-1 | 6.00 | 5.21 | 6.93 | 5.08 | 0.64 | -0.92 | -5.00-3.15 | -0.18 |
| Time-2 | 6.23 | 4.25 | 4.29 | 2.76 | 0.17 | 1.94 | -0.94-4.84 | 0.54 |
| Time-3 | 3.85 | 5.73 | 4.57 | 3.18 | 0.69 | -0.72 | -4.50-3.05 | -0.15 |
| QoL-AD | ||||||||
| Time-1 | 38.69 | 7.00 | 34.36 | 5.30 | 0.08 | 4.33 | -0.63-9.30 | 0.70 |
| Time-2 | 37.62 | 8.47 | 37.29 | 3.76 | 0.89 | 0.33 | -5.07-5.73 | 0.05 |
| Time-3 | 38.77 | 6.89 | 36.79 | 4.63 | 0.39 | 1.98 | -2.75-6.72 | 0.42 |
| PSS | ||||||||
| Time-1 | 16.85 | 8.11 | 18.86 | 7.48 | 0.51 | -2.01 | -8.19-4.16 | -0.25 |
| Time-2 | 15.46 | 7.84 | 12.86 | 4.33 | 0.30 | 2.60 | -2.56-7.77 | 0.41 |
| Time-3 | 13.38 | 7.57 | 12.50 | 4.93 | 0.72 | 0.88 | -4.27-6.04 | 0.89 |
| CAMS-R | ||||||||
| Time-1 | 29.31 | 5.87 | 27.14 | 6.20 | 0.36 | 2.16 | -2.61-6.94 | 0.35 |
| Time-2 | 29.38 | 6.79 | 29.71 | 4.97 | 0.88 | -0.33 | -5.10-4.45 | -0.05 |
| Time-3 | 28.54 | 6.35 | 31.36 | 4.31 | 0.19 | 0.19 | -7.19-1.55 | -0.52 |
*Significant at p (<0.05).
COPM: Satisfaction (average and change scores)
There was no significant interaction effect with group and time, no main effect for time and no main effect between the MBSR and WLC on the COPM satisfaction average or change scores. When an independent t-test between groups at different time points was undertaken, no statistical significance was found at any of the three different time points.
Secondary clinical outcomes
Table 3 shows the mean scores and standard deviations for each of the secondary clinical outcomes at Time-1 (baseline), Time-2 (9-weeks; post-intervention), and Time-3 (13-weeks; follow-up). Effect sizes were reported between groups at three different time points. At post-intervention at Time-2, there was a significant main effect for the GAI (mean difference = 3.90; CI = 0.04-7.75; p = 0.04) with a large effect size (d = 0.80). Otherwise, there were no statistically significant changes at three different time points between groups for the remainder of the secondary clinical outcomes. However, on the PHQ-9, a significant main effect for time (p < 0.03; np2 =0.25) and a significant interaction effect with group and time (p < 0.02; np2 =0.26) with large effect size was found. Additionally, a significant interaction effect with group and time was found on the QoL-AD measure with a large effect size (p < 0.03; np2 =0.25). Lastly, we found a significant main effect for time with a large effect size (p < 0.01; np2 =0.31) on thePSS.
Lastly, when we performed an independent t-test between groups at different time points,
We found a significant reduction in anxiety levels at post-intervention compared to the WLC group. See Table 4.
DISCUSSION
This study is the first known to evaluate an occupational therapist-led MBSR program for individuals with SCD or MCI in a team-based primary care setting. The study found that older adults who completed the 9-week occupational therapist-led mindfulness training program had decreased anxiety levels at post-intervention compared to those who did not. These findings are consistent with other meditation intervention studies that have found a reduction in anxiety in older adults [33, 73], veterans [74], and also among the general adult population [75]. Studies have suggested that older adults with MCI who experience anxiety have poorer cognitive performance and a greater risk of future cognitive decline [76]. A systematic review and meta-analysis conducted by Li et al. (2019) noted that meditation interventions aimed at helping those experiencing the co-occurrence of anxiety and MCI may prevent the progression to dementia [77]. Occupational therapists have been shown to play an important role in secondary prevention in primary care settings [78], and MBSR could be considered an intervention to prevent or alleviate further cognitive decline in older adults.
In this study, all qualified-MBSR teachers ensured delivery of fidelity was met by following the MBSR curriculum guide from the Brown University, School of Public Health in conjunction with the MBI Teaching Assessment Criteria. On the other hand, receipt fidelity was observed by ensuring all participants’ attendance and home practice logs were collected and analyzed. Furthermore, any missed sessions were followed-up with an RA to provide assigned home assignments. Lastly, the only change made to the MBSR curriculum was the all-day retreat was moved to the following week rather than having it on a typical weekend, thereby extending the program an extra week; from 8-weeks to 9-weeks. Otherwise, the total dosage of sessions and hours were the same as per the authorized MBSR curriculum.
The study did not find any significant differences between the intervention and control groups for the COPM, the primary outcome. Instead, participants in both the invention and control groups had gains in self-reported performance and satisfaction with their performance on self-identified activities that were difficult for them. There are a few possible explanations. First, the COPM is an interview-based assessment, requiring individuals to reflect on their daily activities. It could be that simply engaging in the interview may have prompted participants to reflect on their concerns, and this reflection, in turn, may have caused or influenced a therapeutic effect phenomenon. Studies using the COPM have theorized that improvements in a control group could be caused by interviewing participants and engaging them in that therapeutic process at baseline interviews [79]. Additionally, participants had relatively high scores at baseline, which left little room for change in the intervention group.
The COPM is individualized and therefore idiosyncratic in nature, making it difficult to compare across individuals and may be better suited as a clinical outcome than a research measure. It is also important to note that this was a pilot study and, given the small sample, was not powered to detect significant changes. Wong et al. (2017) conducted a study with older adults with MCI recruited from both specialist and primary care clinics and found a positive relationship between mindfulness home practice and an overall improvement in ADL functioning [38]. However, unlike the current study, they did not have a comparison group, and ADL functioning was measured using the Bayer Activities of Daily Living Scale, a self-reported ADL scale. Advocat et al. (2017) conducted an RCT design comparing a 6-week mindfulness training program to a WLC in adults and older adults with Parkinson’s disease. The authors found a significant improvement in the ADL item scores from the Parkinson’s Disease Questionnaire (PDQ) 6-months after the mindfulness training [37]. Interestingly, both studies used a self-report measure and focused explicitly on ADL, versus the current study that used an interview-based outcome that included a wide range of everyday occupations of varying complexity, including self-care ADL, leisure, productivity and iADL. Using a more targeted ADL measure may be worthwhile exploring in future studies as the COPM is more idiosyncratic in nature and some goals may be more challenging to address in a limited time-frame than others. Therefore, future trials investigating functional outcomes may consider using more targeted ADL measures in conjunction with an individualized outcome such as the COPM.
This study hypothesized that MBSR would have an impact on participants’ perceived satisfaction on their performance of everyday activities and psychological issues for older adults living with SCD and MCI and were surprised to have found no overall significant differences in the study’s primary clinical outcomes on the COPM. On the other hand, our findings did support our hypothesis of psychological improvement with a significant reduction in anxiety at Time-2. However, the reduction in anxiety was not maintained on follow-up.
A recent systematic review and meta-analysis by Vibe et al. (2017) found that MBSR improved QoL, and has mental health benefits, such as stress and mindfulness traits among the general and older population compared to a WLC group. The findings in this systematic review contradict our findings [80]. One possible explanation for the non-significant improvement in mood that we found in our study could be that participants with high depression scores were excluded from the study and the fact that our study was underpowered. Last, in our study, there was an uneven drop-out rate between the two groups, with more drop-outs in the MBSR group (n = 3), which may have artificially stabilized the effect sizes of our intervention as we used a conservative LOCF [81]. On the other hand, the lower attrition rate in the Control group (n = 1) may benefit from inflation due to the added effect of follow-up [82].
We found a significant improvement in anxiety in the intervention group, suggestive that MBSR could be an effective strategy to support those living with early cognitive deficits. However, long-term effects on anxiety reduction need to be further investigated as effective mindfulness-based stress reduction requires regular and sustained practice. It has been noted that once mindfulness intervention ends, there is often a decline in regular mindfulness practice and the respective gains. Thus, to maintain the benefits of mindfulness practice, the practice must be consistent and ongoing as evidence is suggestive that the extent of formal practice is associated with positive intervention outcomes [83, 84]. Given there are currently emerging pharmacological interventions that mitigate the impact of MCI psychological symptoms, including cognitive and functional outcomes among individuals with cognitive impairment however, they come with side effects [85, 86]. Mindfulness may be one non-pharmacological way to address psychological symptoms such as anxiety, and future studies may explore the potential reduction in anxiety and the associated protective benefits against cognitive decline [87] and the development of MCI and Alzheimer’s disease [88].
Primary care health team professionals are usually the first point of contact when older adults and their families have memory concerns. Thus, occupational therapists on primary care teams are well-positioned to support older adults with SCD or MCI. Offering MBSR programs in primary care will provide an additional interprofessional perspective and align well with the health promotion model supporting older adults to age-in-place. Interprofessional primary care teams can better support individuals with complex health conditions compared to physician care alone. Interdisciplinary primary care teams can provide diverse responses to older adults with memory decline, including primary care-based memory clinics [89]. MBSR program delivery is inexpensive [90], other than personal time commitment for the mindfulness practice, and it has been deemed safe with no adverse events and is feasible as indicated in earlier studies [53, 91, 92]. Thus, embedding MBSR into a primary care setting to support an ageing population has few negatives and therapeutic potential to reduce anxiety.
Study limitations
This study had a few limitations that must be considered. First, as a pilot RCT study, a small sample was not adequately powered to determine statistical significance. Our results should only be interpreted as promising and warranting a larger clinical trial or assessing minimally clinically 2-point change on the COPM. Second, our sample included predominantly highly educated participants from higher socioeconomic status, and additional research should be conducted with a more diverse sample. Third, follow-up was only 4-weeks, and a longer follow-up may be needed to determine the longer-term effects of mindfulness training [77] beyond the 4-week follow-up period examined in this study. Fourth, within four and half months of recruitment, we were able to screen 53 eligible participants, of which only 27 were randomized. Future trials may consider a longer recruitment period of greater than four and a half months in such primary care settings to obtain a larger sample size. Furthermore, future studies may consider using an active WLC to rule out if participation in a group may have an effect.
Conclusion
Primary care is usually the first point of contact when community-dwelling older adults and their families experience memory-related concerns. Occupational therapists on primary care teams are well-positioned to support those older adults with SCD or MCI by supporting and maintaining their independence, and by doing so, supporting older adults to age-in-place [93]. Team-based primary care can better support individuals with complex health conditions such as SCD or MCI than physician care alone. This study is the first occupational therapist-led MBSR program for older adults with SCD or MCI and has provided preliminary evidence that mindfulness training improves anxiety compared to a WLC group in an interprofessional primary care setting. This study has laid the groundwork for a potential larger powered clinical trial to explore further the effectiveness of mindfulness training and utilization of various performance-based functional outcomes for older adults with memory complaints.
ACKNOWLEDGMENTS
We would like to thank all participants, MBSR Teachers, research assistants and volunteers involved in this study. We would like to acknowledge the following non-author individuals for their support: Jaisa Sulit, Sarah Sheffe, Virginia Vander Hyden, Mubeenaa Rahman, and Kareena Gurbaxani. We would also like to acknowledge the vital contributions of the clinical site, Susan Hum for her research support and Christopher Meaney, for his helpful statistical advice on this manuscript.
FUNDING
This study was funded through a grant by Centre for Aging and Brain Health Innovation (CABHI) and VHA Home HealthCare Junior Research Award. Funders had no role in the design of this study and did not have any role during its execution, analyses, interpretation of data, or decision to submit results.
TRIAL REGISTRATION
This study was reviewed and approved by the Research Ethics Board in Toronto, Ontario, Canada (REB# 2017-0056-E); Queen’s University (REB# 6026418) in Kingston, Ontario, Canada, and Clinicaltrials.gov (08/03/2019; NCT03867474).
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
DATA AVAILABILITY
The data of our current study can be made available upon a written request to PI.
REFERENCES
[1] | Petersen RC ((2011) ) Mild cognitive impairment. N Engl J Med 364: , 2227–2234. |
[2] | Silva LDSVE , Silva TBLE , Falcão DVDS , Batistoni SST , Lopes A , Cachioni M , Neri AL , Yassuda MS ((2014) ) Relations between memory complaints, depressive symptoms and cognitive performance among community dwelling elderly. Rev Psiquiatr Clín 41: , 67–71. |
[3] | Reid LM , MacLullich AMJ ((2006) ) Subjective memory complaints and cognitive impairment in older people. Dement Geriatr Cogn Disord 22: , 471–485. |
[4] | Zuniga KE , Mackenzie MJ , Kramer A , McAuley E ((2016) ) Subjective memory impairment and well-being in community-dwelling older adults. Psychogeriatrics 16: , 20–26. |
[5] | Jessen F , Amariglio RE , Buckley RF , van der Flier WM , Han Y , Molinuevo JL , Rabin L , Rentz DM , Rodriguez-Gomez O , Saykin AJ , Sikkes SAM , Smart CM , Wolfsgruber S , Wagner M ((2020) ) The characterisation of subjective cognitive decline. Lancet Neurol 19: , 271–278. |
[6] | van Harten AC , Mielke MM , Swenson-Dravis DM , Hagen CE , Edwards KK , Roberts RO , Geda YE , Knopman DS , Petersen RC ((2018) ) Subjective cognitive decline and risk of MCI: The Mayo Clinic Study of Aging. Neurology 91: , e300–e312. |
[7] | American Psychiatric Association DSMTF ((2013) ) Diagnostic and statistical manual of mental disorders: DSM-5, American Psychiatric Association, Washington, D.C. |
[8] | Petersen RC , Caracciolo B , Brayne C , Gauthier S , Jelic V , Fratiglioni L ((2014) ) Mild cognitive impairment: A concept in evolution. J Intern Med 275: , 214–228. |
[9] | Schmidtke K , Hermeneit S ((2008) ) High rate of conversion to Alzheimer’s disease in a cohort of amnestic MCI patients. Int Psychogeriatr 20: , 96–108. |
[10] | Shigemizu D , Akiyama S , Higaki S , Sugimoto T , Sakurai T , Boroevich KA , Sharma A , Tsunoda T , Ochiya T , Niida S , Ozaki K ((2020) ) Prognosis prediction model for conversion from mild cognitive impairment to Alzheimer’s disease created by integrative analysis of multi-omics data. Alzheimers Res Ther 12: , 145–145. |
[11] | Public Health Agency of Canada, A dementia strategy for Canada. Public Health Agency of Canada, (Aug 2019 ed). Ottawa, Canada. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-strategy-brief.html |
[12] | Slot RER , Sikkes SAM , Berkhof J , Brodaty H , Buckley R , Cavedo E , Dardiotis E , Guillo-Benarous F , Hampel H , Kochan NA , Lista S , Luck T , Maruff P , Molinuevo JL , Kornhuber J , Reisberg B , Riedel-Heller SG , Risacher SL , Roehr S , Sachdev PS , Scarmeas N , Scheltens P , Shulman MB , Saykin AJ , Verfaillie SCJ , Visser PJ , Vos SJB , Wagner M , Wolfsgruber S , Jessen F , van der Flier WM ((2019) ) Subjective cognitive decline and rates of incident Alzheimer’s disease and non-Alzheimer’s disease dementia. Alzheimers Dement 15: , 465–476. |
[13] | Luck T , Luppa M , Wiese B , Maier W , van den Bussche H , Eisele M , Jessen F , Weeg D , Weyerer S , Pentzek M , Leicht H , Koehler M , Tebarth F , Olbrich J , Eifflaender-Gorfer S , Fuchs A , Koenig H-H , Riedel-Heller SG ((2012) ) Prediction of incident dementia: Impact of impairment in instrumental activities of daily living and mild cognitive impairment— results from the German Study on Ageing, Cognition, and Dementia in Primary Care Patients. Am J Geriatr Psychiatry 20: , 943–954. |
[14] | Belchior P , Korner-Bitensky N , Holmes M , Robert A ((2015) ) Identification and assessment of functional performance in mild cognitive impairment: A survey of occupational therapy practices. Aust Occup Ther J 62: , 187–196. |
[15] | Hughes TF , Chang C-CH , Bilt JV , Snitz BE , Ganguli M ((2012) ) Mild cognitive deficits and everyday functioning among older adults in the community: The Monongahela-Youghiogheny Healthy Aging Team Study. Am J Geriatr Psychiatry 20: , 836–844. |
[16] | Johansson MM , Marcusson J , Wressle E ((2015) ) Cognitive impairment and its consequences in everyday life: Experiences of people with mild cognitive impairment or mild dementia and their relatives. Int Psychogeriatr 27: , 949–958. |
[17] | Tomaszewski Farias S , Giovannetti T , Payne BR , Marsiske M , Rebok GW , Schaie KW , Thomas KR , Willis SL , Dzierzewski JM , Unverzagt F , Gross AL ((2018) ) Self-perceived difficulties in everyday function precede cognitive decline among older adults in the ACTIVE Study. J Int Neuropsychol Soc 24: , 104–112. |
[18] | Joosten-Weyn Banningh EWA , Vernooy-Dassen MJFJ , Olde Rikkert MGM , Teunisse JPWM ((2008) ) Mild cognitive impairment: Coping with an uncertain label. Int J Geriatr Psychiatry 23: , 148–154. |
[19] | Wettstein M , Seidl U , Wahl H-W , Shoval N , Heinik J ((2014) ) Behavioral competence and emotional well-being of older adults with mild cognitive impairment: Comparison with cognitively healthy controls and individuals with early-stage dementia. GeroPsych 27: , 55–65. |
[20] | Li XX , Li Z ((2018) ) The impact of anxiety on the progression of mild cognitive impairment to dementia in Chinese and English data bases: A systematic review and meta-analysis. Int J Geriatr Psychiatry 33: , 131–140. |
[21] | Regan B , Varanelli L ((2013) ) Adjustment, depression, and anxiety in mild cognitive impairment and early dementia: A systematic review of psychological intervention studies. Int Psychogeriatr 25: , 1963–1984. |
[22] | Andreescu C , Varon D ((2015) ) New research on anxiety disorders in the elderly and an update on evidence-based treatments. Curr Psychiatry Rep 17: , 53. |
[23] | Kok RM , Reynolds CF ((2017) ) Management of depression in older adults: A review. JAMA 317: , 2114–2122. |
[24] | Dhalwani NN , Fahami R , Sathanapally H , Seidu S , Davies MJ , Khunti K ((2017) ) Association between polypharmacy and falls in older adults: A longitudinal study from England. BMJ open 7: , e016358–e016358. |
[25] | Gu J , Strauss C , Bond R , Cavanagh K ((2015) ) How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin Psychol Rev 37: , 1–12. |
[26] | Khoury B , Sharma M , Rush SE , Fournier C ((2015) ) Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res 78: , 519–528. |
[27] | Lenze EJ , Hickman S , Hershey T , Wendleton L , Ly K , Dixon D , Dore P , Wetherell JL ((2014) ) Mindfulness-based stress reduction for older adults with worry symptoms and co-occurring cognitive dysfunction. Int J Geriatr Psychiatry 29: , 991–1000. |
[28] | Im S , Stavas J , Lee J , Mir Z , Hazlett-Stevens H , Caplovitz G ((2021) ) Does mindfulness-based intervention improve cognitive function?: A meta-analysis of controlled studies. Clin Psychol Rev 84: , 101972. |
[29] | Gard T , Hölzel BK , Lazar SW ((2014) ) The potential effects of meditation on age-related cognitive decline: A systematic review. Ann N Y Acad Sci 1307: , 89–103. |
[30] | Hölzel BK , Lazar SW , Gard T , Schuman-Olivier Z , Vago DR , Ott U ((2011) ) How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci 6: , 537–559. |
[31] | Lazar SW , Kerr CE , Wasserman RH , Gray JR , Greve DN , Treadway MT , McGarvey M , Quinn BT , Dusek JA , Benson H , Rauch SL , Moore CI , Fischl B ((2005) ) Meditation experience is associated with increased cortical thickness. Neuroreport 16: , 1893–1897. |
[32] | Whitfield T , Barnhofer T , Acabchuk R , Cohen A , Lee M , Schlosser M , Arenaza-Urquijo EM , Bottcher A , Britton W , Coll-Padros N , Collette F , Chetelat G , Dautricourt S , Demnitz-King H , Dumais T , Klimecki O , Meiberth D , Moulinet I , Muller T , Parsons E , Sager L , Sannemann L , Scharf J , Schild A-K , Touron E , Wirth M , Walker Z , Moitra E , Lutz A , Lazar SW , Vago D , Marchant NL ((2021) ) The effect of mindfulness-based programs on cognitive function in adults: A systematic review and meta-analysis. Neuropsychol Rev 32: , 677–702. |
[33] | Helmes E , Ward BG ((2017) ) Mindfulness-based cognitive therapy for anxiety symptoms in older adults in residential care. Aging Ment Health 21: , 272–278. |
[34] | Mallya S , Fiocco AJ ((2016) ) Effects of mindfulness training on cognition and well-being in healthy older adults. Mindfulness 7: , 453–465. |
[35] | Smoski MJ , McClintock A , Keeling L ((2016) ) Mindfulness training for emotional and cognitive health in late life. Curr Behav Neurosci 3: , 301–307. |
[36] | Williams JMG ((2010) ) Mindfulness and psychological process. Emotion 10: , 1–7. |
[37] | Advocat J , Enticott J , Vandenberg B , Hassed C , Hester J , Russell G ((2016) ) The effects of a mindfulness-based lifestyle program for adults with Parkinson’s disease: A mixed methods, wait list controlled randomised control study. BMC Neurol 16: , 166–166. |
[38] | Wong WP , Coles J , Chambers R , Wu DB-C , Hassed C ((2017) ) The effects of mindfulness on older adults with mild cognitive impairment. J Alzheimers Dis Rep 1: , 181–193. |
[39] | Hum S , Cohen C , Persaud M , Lee J , Drummond N , Dalziel W , Pimlott N ((2014) ) Role expectations in dementia care among family physicians and specialists. Can Geriatr J 17: , 95–102. |
[40] | Rabin LA , Smart CM , Crane PK , Amariglio RE , Berman LM , Boada M , Buckley RF , Chetelat G , Dubois B , Ellis KA , Gifford KA , Jefferson AL , Jessen F , Katz MJ , Lipton RB , Luck T , Maruff P , Mielke MM , Molinuevo JL , Naeem F , Perrotin A , Petersen RC , Rami L , Reisberg B , Rentz DM , Riedel-Heller SG , Risacher SL , Roiguez O , Sachdev PS , Saykin AJ , Slavin MJ , Snitz BE , Sperling RA , Tandetnik C , van der Flier WM , Wagner M , Wolfsgruber S , Sikkes SAM ((2015) ) Subjective cognitive decline in older adults: An overview of self-report measures used across 19 international research studies. J Alzheimers Dis 48: , S63–S86. |
[41] | Donnelly C , Leclair LL , Hand C , Wener PF , Letts LJ ((2022) ) Occupational therapy and primary care: A vision for the path forward. Canadian Association of Occupational Therapists. |
[42] | McCay E , Frankford R , Beanlands H , Sidani S , Gucciardi E , Blidner R , Danaher A , Carter C , Aiello A ((2016) ) Evaluation of mindfulness-based cognitive therapy to reduce psychological distress and to promote well-being: A pilot study in a primary health care setting. SAGE Open 6: , 215824401666954. |
[43] | Lopez-Montoyo A , Quero S , Montero-Marin J , Barcelo-Soler A , Beltran M , Campos D , Garcia-Campayo J ((2019) ) Effectiveness of a brief psychological mindfulness-based intervention for the treatment of depression in primary care: Study protocol for a randomized controlled clinical trial. BMC Psychiatry 19: , 301. |
[44] | Salvo V , Kristeller J , Montero Marin J , Sanudo A , Lourenço BH , Schveitzer MC , D’Almeida V , Morillo H , Gimeno SGA , Garcia-Campayo J , Demarzo M ((2018) ) Mindfulness as a complementary intervention in the treatment of overweight and obesity in primary health care: Study protocol for a randomised controlled trial. Trials 19: , 277. |
[45] | Snapp C , DeBusk R , Benn R ((2014) ) A whole system approach to caring for chronic disease patients in primary care: A six month mindfulness-based therapeutic lifestyle change program. J Altern Complement Med 20: , A12–A121. |
[46] | Ortiz JA , Smith BW , Shelley BM , Erickson KS ((2019) ) Adapting mindfulness to engage latinos and improve mental health in primary care: A pilot study. Mindfulness 10: , 2522–2531. |
[47] | Baker N ((2016) ) Using cognitive behavior therapy and mindfulness techniques in the management of chronic pain in primary care. Primary Care 43: , 203–216. |
[48] | Kearney DJ ((2020) ) Mindfulness training for primary care patients promotes chronic disease self-management behaviours. Evid Based Nurs 23: , 118–118. |
[49] | Tran T , Donnelly C , Nalder E , Trothen T , Finlayson M ((2023) ) Mindfulness-based stress reduction for community-dwelling older adults with subjective cognitive decline (SCD) and mild cognitive impairment (MCI) in primary care: A mixed-methods feasibility randomized control trial. BMC Primary Care 24: , 44–44. |
[50] | Demarzo M , Montero-Marin J , Cuijpers P , Zabaleta-del-Olmo E , Mahtani KR , Vellinga A , Vicens C , López-del-Hoyo Y , García-Campayo J ((2015) ) The efficacy of mindfulness-based interventions in primary care: A meta-analytic review. Ann Fam Med 13: , 573–582. |
[51] | Farhang M , Miranda-Castillo C , Rubio M , Furtado G ((2019) ) Impact of mind-body interventions in older adults with mild cognitive impairment: A systematic review. Int Psychogeriatr 31: , 643–666. |
[52] | Kurth F , Zsadanyi SE , Luders E ((2021) ) Reduced age-related gray matter loss in the subgenual cingulate cortex in long-term meditators. Brain Imaging Behav 15: , 2824–2832. |
[53] | Smart CM , Segalowitz SJ , Mulligan BP , Koudys J , Gawryluk JR ((2016) ) Mindfulness training for older adults with subjective cognitive decline: Results from a pilot randomized controlled trial. J Alzheimers Dis 52: , 757–774. |
[54] | Wells RE , Kerr CE , Wolkin J , Dossett M , Davis RB , Walsh J , Wall RB , Kong J , Kaptchuk T , Press D , Phillips RS , Yeh G ((2013) ) Meditation for adults with mild cognitive impairment: A pilot randomized trial. J Am Geriatr Soc 61: , 642–645. |
[55] | Chan A-W , Tetzlaff J , Altman D , Laupacis A , Gøtzsche P , Krleza-Jeric K , Hróbjartsson A , Mann H , Dickersin K , Berlin J , Doré C , Parulekar W , Summerskill W , Groves T , Schulz K , Sox H , Rockhold F , Rennie D , Moher D ((2013) ) SPIRIT 2013 Statement: Defining standard protocol items for clinical trials. Ann Intern Med 153: , 200–207. |
[56] | Tran T , Donnelly C , Nalder EJ , Trothen T , Finlayson M ((2020) ) Occupational therapist-led mindfulness-based stress reduction for older adults living with subjective cognitive decline or mild cognitive impairment in primary care: A feasibility randomised control trial protocol. BMJ Open 10: , e035299. |
[57] | Health Quality Ontario, Learning community: Advancing Improvement in primary care in Ontario, http://www.hqontario.ca/Portals/0/documents/qi/pc-team-building-guide-intro-en.pdf |
[58] | Aguirre E , Stott J , Charlesworth G , Noone D , Payne J , Patel M , Spector A ((2017) ) Mindfulness-Based Cognitive Therapy (MBCT) programme for depression in people with early stages of dementia: Study protocol for a randomised controlled feasibility study. Pilot Feasibility Stud 3: , 28. |
[59] | Billingham SAM , Whitehead AL , Julious SA ((2013) ) An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med Res Methodol 13: , 104–104. |
[60] | Kabat-Zinn J , University of Massachusetts Medical Center/Worcester. Stress Reduction C ((2013) ) Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness, Delta Trade Paperbacks, New York, N.Y. |
[61] | Insight Timer (2019) [Mobile Application Software] Retreived from https://insighttimer.com. |
[62] | Law M , Canadian Association of Occupational Therapists ((2005) ) Canadian Occupational Performance Measure, Canadian Association of Occupational Therapists, Ottawa, Ontario. |
[63] | Donnelly C , Carswell A ((2002) ) Individualized outcome measures: A review of the literature. Can J Occup Ther 69: , 84–94. |
[64] | Carswell A , McColl MA , Baptiste S , Law M , Polatajko H , Pollock N ((2004) ) The Canadian Occupational Performance Measure: A research and clinical literature review. Can J Occup Ther 71: , 210–222. |
[65] | Donnelly C , O’Neill C , Bauer M , Letts L ((2017) ) Canadian Occupational Performance Measure (COPM) in primary care: A profile of practice. Am J Occup Ther 71: , 7106265010p1–7106265010p8. |
[66] | Phelan E , Williams B , Meeker K , Bonn K , Frederick J , Logerfo J , Snowden M ((2010) ) A study of the diagnostic accuracy of the PHQ-9 in primary care elderly. BMC Fam Pract 11: , 63. |
[67] | Pachana NA , Byrne GJ , Siddle H , Koloski N , Harley E , Arnold E ((2007) ) Development and validation of the Geriatric Anxiety Inventory. Int Psychogeriatr 19: , 103–114. |
[68] | Lee E-H ((2012) ) Review of the Psychometric Evidence of the Perceived Stress Scale. Asian Nurs Res 6: , 121–127. |
[69] | Feldman G , Hayes A , Kumar S , Greeson J , Laurenceau J-P ((2007) ) Mindfulness and emotion regulation: The development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). J Psychopathol Behav Assess 29: , 177–190. |
[70] | Logsdon RG , Gibbons LE , McCurry SM , Teri L ((1999) ) Quality of life in Alzheimer’s disease: Patient and caregiver reports. J Ment Health Aging 5: , 21–32. |
[71] | Bond FW , Hayes SC , Baer RA , Carpenter KM , Guenole N , Orcutt HK , Waltz T , Zettle RD ((2011) ) Preliminary Psychometric Properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behav Ther 42: , 676–688. |
[72] | Wong WK , Boscardin WJ , Postlethwaite AE , Furst DE ((2011) ) Handling missing data issues in clinical trials for rheumatic diseases. Contemp Clin Trials 32: , 1–9. |
[73] | Moore RC , Depp CA , Wetherell JL , Lenze EJ ((2016) ) Ecological momentary assessment versus standard assessment instruments for measuring mindfulness, depressed mood, and anxiety among older adults. J Psychiatr Res 75: , 116–123. |
[74] | Serpa JG , Taylor SL , Tillisch K ((2014) ) Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Med Care 52: , S19–24. |
[75] | Vollestad J , Sivertsen B , Nielsen GH ((2011) ) Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behav Res Ther 49: , 281–288. |
[76] | Beaudreau SAPD , O’Hara RPD ((2008) ) Late-life anxiety and cognitive impairment: A review. Am J Geriatr Psychiatry 16: , 790–803. |
[77] | Li SYH , Bressington D ((2019) ) The effects of mindfulness-based stress reduction on depression, anxiety, and stress in older adults: A systematic review and meta-analysis. Int J Ment Health Nurs 28: , 635–656. |
[78] | Donnelly C , Leclair LL , Wener PF , Hand CL , Letts LJ ((2016) ) Occupational therapy in primary care: Results from a national survey: L’ergothérapie dans les soins primaires: Résultats d’un sondage national. Can J Occup Ther 83: , 135–142. |
[79] | Tuntland H , Aaslund MK , Espehaug B , Førland O , Kjeken I ((2015) ) Reablement in community-dwelling older adults: A randomised controlled trial. BMC Geriatrics 15: , 145–145. |
[80] | Vibe M , Bjørndal A , Fattah S , Dyrdal GM , Halland E , Tanner-Smith EE ((2017) ) Mindfulness-based stress reduction (MBSR) for improving health, quality of life and social functioning in adults: A systematic review and meta-analysis. Campbell Syst Rev 13: , 1–264. |
[81] | Molnar FJ , Hutton B , Fergusson D ((2008) ) Does analysis using “last observation carried forward” introduce bias in dementia research? Can Med Assoc J 179: , 751–753. |
[82] | McCarney R , Warner J , Iliffe S , van Haselen R , Griffin M , Fisher P ((2007) ) The Hawthorne Effect: A randomised, controlled trial. BMC Med Res Methodol 7: , 30. |
[83] | Kor PPK , Liu JYW , Chien WT ((2019) ) Effects of a modified mindfulness-based cognitive therapy for family caregivers of people with dementia: A pilot randomized controlled trial. Int J Nurs 98: , 107–117. |
[84] | Parsons CE , Crane C , Parsons LJ , Fjorback LO , Kuyken W ((2017) ) Home practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A systematic review and meta-analysis of participants’ mindfulness practice and its association with outcomes. Behav Res Ther 95: , 29–41. |
[85] | Perini G , Cotta Ramusino M , Sinforiani E , Bernini S , Petrachi R , Costa A ((2019) ) Cognitive impairment in depression: Recent advances and novel treatments. Neuropsychiatr Dis Treat 15: , 1249–1258. |
[86] | Levine AMP , Emonds EE , Smith MA , Rickles NM , Kuchel GA , Steffens DC , Ohlheiser A , Fortinsky RH ((2021) ) Pharmacist identification of medication therapy problems involving cognition among older adults followed by a home-based care team. Drugs Aging 38: , 157–168. |
[87] | Khalsa DS ((2015) ) Stress, meditation, and Alzheimer’s disease prevention: Where the evidence stands. J Alzheimers Dis 48: , 1–12. |
[88] | Larouche E , Chouinard A-M , Goulet S , Hudon C ((2016) ) O3-10-02: Mindfulness-based intervention prevents memory decline and improves mood and quality of life in older adults with mild cognitive impairment: Preliminary findings. Alzheimers Dementia 12: , P310. |
[89] | Lee L , Hillier LM , Heckman G , Gagnon M ((2014) ) Primary care-based memory clinics: Expanding capacity for dementia care. Can J Aging 33: , 307–319. |
[90] | Paller KA , Creery JD , Florczak SM , Weintraub S , Mesulam MM , Reber PJ , Kiragu J , Rooks J , Safron A , Morhardt D , O’Hara M , Gigler KL , Molony JM , Maslar M ((2015) ) Benefits of mindfulness training for patients with progressive cognitive decline and their caregivers. Am J Alzheimers Dis Other Dement 30: , 257–267. |
[91] | Cheung DSK , Kor PPK , Jones C , Davies N , Moyle W , Chien WT , Yip ALK , Chambers S , Yu CTK , Lai C ((2020) ) The use of modified Mindfulness-based Stress Reduction and Mindfulness-based Cognitive Therapy programme for family caregivers of people living with dementia: A feasibility study. Asian Nurs Res 14: , 221–230. |
[92] | Kovach CR , Evans C-R , Sattell L , Rosenau K , Gopalakrishnan S ((2018) ) Feasibility and pilot testing of a mindfulness intervention for frail older adults and individuals with dementia. Res Gerontol Nurs 11: , 137–150. |
[93] | Ciro CA ((2014) ) Maximizing ADL performance to facilitate aging in place for people with dementia. Nurs Clin North Am 49: , 157–169. |




