Mindfulness and Care Experience in Family Caregivers of Persons Living with Dementia
Abstract
Background:
Greater mindfulness, the practice of awareness and living in the moment without judgement, has been linked to positive caregiving outcomes in dementia caregivers and its impact attributed to greater decentering and emotion regulation abilities. Whether the impact of these mindfulness-based processes varies across caregiver subgroups is unclear.
Objective:
Analyze cross-sectional associations between mindfulness and caregiver psychosocial outcomes, considering different caregiver and patient characteristics.
Methods:
A total of 128 family caregivers of persons living with Alzheimer’s disease and related disorders were assessed on several mindfulness measures (i.e., global; decentering, positive emotion regulation, negative emotion regulation) and provided self-reported appraisals of caregiving experience; care preparedness; confidence, burden, and depression/anxiety. Bivariate relationships between mindfulness and caregiver outcomes were assessed with Pearson’s correlations and stratified by caregiver (women versus men; spouse versus adult child) and patient (mild cognitive impairment (MCI) versus Dementia; AD versus dementia with Lewy bodies; low versus high symptom severity) characteristics.
Results:
Greater mindfulness was associated with positive outcomes and inversely associated with negative outcomes. Stratification identified specific patterns of associations across caregiver groups. Significant correlations were found between all mindfulness measures and caregiving outcomes in male and MCI caregivers while the individual mindfulness component of positive emotion regulation was significantly correlated to outcomes in most caregiver groups.
Conclusion:
Our findings support a link between caregiver mindfulness and improved caregiving outcomes and suggest directions of inquiry into whether the effectiveness of dementia caregiver-support interventions may be improved by targeting specific mindfulness processes or offering a more inclusive all-scope approach depending on individual caregiver or patient characteristics.
INTRODUCTION
Recent estimates from the Alzheimer’s Association suggest that more than 11 million Americans currently provide unpaid care for over 6 million people living with Alzheimer’s disease (AD) and related disorders (ADRD) [1]. Most of these informal caregivers are family members, including spouses and adult children, particularly adult daughters, who spend close to 21 hours per week providing care [2]. This represents 6 hours more per week than caregivers of people without dementia [2]. Caring for a family member with dementia can be overwhelming and family caregivers (FCGs) often report high levels of stress, depression, and anxiety [3, 4], physical morbidity, social isolation, financial strain [5], and increased health care utilization [6] resulting from their caregiving role and related responsibilities. While caregiving in dementia is many times described as a burden, it is important to acknowledge that FCGs also report many positive caregiving experiences including feelings of giving back and satisfaction helping others [7, 8]. These positive experiences have been linked to less perceived burden and depression [9], and greater reported caregiving preparedness [10] and care competence [11]. These can be significant coping resources that can be employed to counteract the negative impacts of caregiving for persons living with dementia (PLwD).
Addressing the emotional, physical, economic, and social impacts of caring for a relative with ADRD remains an important research and clinical goal as we continue to search for the best strategies to reduce these negative effects and improve caregiving experiences. Important for the success of these endeavors is a better understanding of the multitude of factors that contribute to these caregiver outcomes. Challenging behaviors [12], patient negative affect [13], and disease progression [14] have been identified as important patient-related contributors to caregiver burden and negative appraisals of caregiving, while healthcare system related factors including prolonged diagnostic processes, lengthy paths to supports and services, and poor interactions with care providers further exacerbate negative caregiving experiences [15]. While important, these factors are often difficult to modify. Given the success of psychosocial interventions in improving mental health in family caregivers of PLwD [16, 17], we posit that strategies to improve caregiving experience and reduce caregiver burden and emotional distress may be more successful when targeting caregiver-related factors that are more malleable to change.
One such factor is caregiver mindfulness. Mindfulness, which refers to the practice of awareness and living in the moment without judgement, has gained traction in Western medicine in recent decades and more recently in the dementia caregiving research community for its potential as a resilience factor that promotes caregiver psychological well-being and better caregiving-related outcomes. Greater mindfulness among FCGs of PLwD has been consistently linked to better caregiver emotional health including lower psychological distress [18, 19] and greater care competence, confidence, and caregiving experience [20]. In addition, greater caregiver mindfulness correlates with better patient outcomes including better cognitive performance, less subjective complaints, and higher health-related quality of life [20] further highlighting the importance of caregiver mindfulness in dementia care. Further support for the benefits of mindfulness as a regulator of caregiver psychological well-being and positive care experiences comes from clinical trials. Recent meta-analyses pooling data across multiple randomized controlled trials of mindfulness-based training interventions are consistent in reporting benefits in terms of reduced depression, burden, and perceived stress, and improved sleep quality and health-related quality of life among FCGs of PLwD [21–24]. Several potential mindfulness-related processes have been proposed including decentering and emotion regulation. Decentering refers to the ability to observe negative thoughts/feelings and regard them as temporary rather than true reflections of the self [25]. Mindful emotion regulation is a unique emotion regulation strategy that results from encountering diverse emotional states from a mindful mental state and differs from other emotion regulation strategies including cognitive reappraisal— an antecedent-focused emotion regulation strategy [26]. Decentering and mindful emotion regulation and particularly its positive emotion regulation component have been correlated with various caregiver outcomes including positive appraisals of caregiving, care preparedness, care confidence, satisfaction with life, less rumination, and reduced caregiver depression [20, 27]. Mediation analyses have supported a role for these coping strategies in explaining the benefits of mindfulness on caregiver psychological health [19, 28].
Considering the evidence that mindful decentering and emotion regulation constitute separate coping processes in dementia caregiving, one important question is whether the effect of these separate mechanisms varies across different caregiver or patient characteristics. More specifically, is decentering more likely to be evoked as a mindful coping strategy by spouse versus adult child caregivers or in female versus male caregivers? Similarly, are negativeemotion regulation processes more likely to be engaged when behavioral/symptom severity is high versus low or when caring for family members with non-AD versus AD etiologies? Empirical evidence for a gender differential in decentering in favor of men [29] and for emotion regulation (especially positive emotions) in favor of women [30] provides support for the idea that separate mindfulness-based mechanisms may be at play depending on caregiver-specific factors. We propose that their impact may also vary by patient-specific characteristics including disease stage, etiology, and symptom severity. Support for this proposition would suggest that mindfulness-based interventions to improve psychosocial outcomes in FCGs of PLwD may be more effective when tailored to caregiver group-specific mechanisms. To address the noted gap in the knowledge, our study was designed to assess baseline associations between global and specific mindfulness components/pathways and psychosocial outcomes in caregivers of PLwD and whether these associations may vary by select caregiver and patientcharacteristics.
MATERIALS AND METHODS
Study participants
Study participants consisted of caregivers of deeply phenotyped patients receiving care or participating in cognitive aging studies in our research center between October 2016 and November 2019. Having a caregiver/study partner was a requirement for enrollment in these studies or receiving care in our clinic, with caregiver/study partner defined as someone who knows the patient/research participant well and can provide a second, independent collateral source of information. Patients and research participants received identical evaluations and were diagnosed and staged based on global rating scales, neuropsychological evaluations, neurological examinations, and laboratory tests using standard dementia diagnostic criteria as described below. Caregivers completed a psychosocial self-assessment that included mindfulness and caregiving-related outcomes and provided patient-related cognitive, functional, and behavioral assessments using standard rating scales and interview-based evaluations. These caregiver and patient assessments are part of standard of care at our center and were similar across clinic and research studies. Inclusion criteria for this cross-sectional study consisted of1) caregivers of patient/research participants with cognitive impairment; 2) caregivers who were living with patients/research participants or visiting/calling them on a weekly basis; and 3) availability of data on caregiver self-assessed mindfulness. A total of 128 caregivers met inclusion criteria and were included in the study. A waiver of consent was obtained for a retrospective chart review of clinic patients and written informed consent was obtained from prospective research participants including caregivers. The study was approved by the Institutional Review Board at University of Miami.
Assessment of mindfulness
Caregiver mindfulness was assessed with the Applied Mindfulness Process Scale (AMPS), which is a quantitative self-reported measure of one’s level of mindfulness-based practices applied in daily life to address stressful situations [31]. Caregivers were asked to indicate how often they used mindfulness principles to cope with stressful events over the past week. The scale includes 15 items measured on a 5-point Likert scale (0 = never; 1 = rarely; 2 = sometimes; 3 = often, and 4 = almost always) and provides a global score (range: 0–60) and separate scores on each of three factors (5 items each; range: 0–20): decentering, positive emotion regulation, and negative emotion regulation. According to Li and colleagues, decentering (Factor 1) refers to deidentifying from and viewing negative thoughts and feelings as lacking absolute veracity, therefore allowing a more accurate assessment of one’s ability to cope with challenges. Positive emotion regulation (Factor 2) involves a refocus on positive emotions and reappraisal of adverse life events as beneficial, with the accompanying sense of reward. Lastly, negative emotion regulation (Factor 3) refers to coping with stress by allowing one to observe and accept their negative emotions without reacting to them. Higher global and factor scores (each ranging from 0–20) indicate a greater use of mindfulness practice. Strong internal consistency (Cronbach’s alpha = 0.91) and item-total reliability (range: 0.51–0.72) was reported for AMPS in healthy adults [31]. The four mindfulness parameters (global; Factors 1, 2, and 3) were used in data analyses as continuous variables.
Diagnoses
The ADRD diagnostic process was comprehensive and involved 1) patient-based subjective ratings of dementia (i.e., Quick Dementia Rating Scale (QDRS) (reliability range 0.9–0.94) [32]); reports of cognitive change (i.e., Cognitive Change Index [33]; Cognitive Function Instrument [34])); and memory complains (i.e., AD8 [35]); 2) neuropsychological testing (i.e., Montreal Cognitive Assessment [36], Hopkins Verbal Learning Task [37]; Digit Span forward/backward [38]; Number Symbol Coding Test [39]; Trail Making tests [40]; Animal Naming and Multilingual Naming Test (MINT) [38]; Noise Pareidolia Test [41]; Hospital Anxiety and Depression Scale [42]); and 3) caregiver assessments of PLwD cognitive, functional, and behavioral symptoms (i.e., informant version of the QDRS; Functional Activity Questionnaire [43]; and Neuropsychiatric Inventory-Questionnaire (NPI-Q) [44]). Cognition was not assessed in caregivers. The presence/absence of dementia and staging were assessed with the Clinical Dementia Rating Scale (CDR) and the related CDR-sum of boxes [45] and the Global Deterioration Scale [46].
Diagnoses were assigned after a consensus conference lead by a cognitive neurologist (JEG), based on these patient-based and caregiver-reported evaluations combined with results from a neurological examination and laboratory tests. Patients and research participants were categorized as either cognitively normal, MCI (prodromal stage), or dementia using standard criteria for AD [47], dementia with Lewy bodies (DLB) [48], vascular contributions to cognitive impairment and dementia (VCID) [49], and frontotemporal degeneration (FTD) [50].
Caregiver outcomes
In addition to rating the patients’ cognitive and physical functioning, mood, dementia-related symptoms, and behaviors, caregivers provided self-evaluations of their experience in a caregiver role. Five aspects of caregiving were evaluated: care preparedness, care confidence, overall caregiver experience, caregiver burden, and caregiver mood. Care preparedness, assessed with the Preparedness for Caregiving Scale (PCS) [51], requires a self-assessment of one’s preparedness with specific aspects of care including meeting patient physical and emotional needs, accessing available services, handling emergencies, navigating the health care system, and handling stress. The score ranged from 0–32 (8 items scored 0–4 from ‘not at all prepared’ to ‘very well prepared’), with higher scores indicative of greater preparedness. High test-retest reliability (0.92) was reported for the PCS [52]). Care confidence was evaluated with an investigator-derived 4-question measure rated on a 5-point Likert scale, that was based on the Dementia Care Confidence Scale [53] and was used in prior research [10]. Total confidence scores ranged from 0 to 16, with higher scores indicating better care confidence. Overall caregiver experience was measured with the Positive and Negative Appraisals of Caregiving (PANAC) Scale [10]. As part of the scale, caregivers were asked to agree/disagree with 8 statements capturing positive and 8 statements capturing negative experiences with providing care or assistance to individuals with memory disorders scored as 0 = strongly disagree to 4 = strongly agree. A total negative appraisals score (range 0–32) and a total positive appraisals score (range 0–32) were derived with higher scores indicating greater negative (worse) and greater positive (better) experiences of caregiving. Both the positive (Cronbach’s alpha of 0.84 (0.80–0.87 95% CI) and negative appraisal (Cronbach alpha of 0.82 (0.78–0.86 95% CI) domains were found to be highly reliable [10]. Caregiver burden was measured with the 12-item Zarit Burden Inventory (ZBI) [54], which evaluates the impact of providing care on various aspects of caregiver’s health and is measured on a 5-point Likert scale (0 = never to 4 = nearly always). Total burden scores ranged from 0–48, with higher scores indicating greater levels of burden. The 12-item ZBI was found to be highly reliable with a reported Cronbach’s alpha of 0.90 [55]. Finally, caregiver mood was assessed with the Personal Health Questionnaire (PHQ-4) [56], a highly reliable depression and anxiety screening tool (Cronbach’s alpha of 0.81) [57]. The PHQ-4 consists of 2 core criteria for depressive disorders and 2 criteria for generalized anxiety disorder scored on a 0 (not at all) to 3 (nearly every day) scale. The total composite score ranges from 0–12, higher scores suggesting worse mood.
Patient and caregiver characteristics
Caregiver and patient/research participant characteristics included caregiver sex (Men/Women) and relation to patient/research participant and patient-related disease stage, etiology, and symptom severity. Caregiver relation to patient was categorized as spouse/partner, adult child, sibling, friend/neighbor, paid caregiver/provider, or other. Disease stage was defined as cognitively normal (CDR = 0), MCI (CDR = 0.5), or Dementia (CDR≥1), while disease etiology was defined as AD, DLB, VCID, or FTD. Behavioral symptom severity (symptom severity hereafter) was measured with a brief clinical form of the Neuropsychiatric Inventory (NPI-Q), which includes 12 dementia-related behaviors and psychological features as endorsed by caregivers with symptom severity rated for each present symptom/feature as mild, moderate, or sever [44]. The distress sub-scale for NPI-Q was not collected and therefore was not included in this study. Total NPI-Q scores ranged from 0–36, with higher scores indicating greater symptom severity. The median NPI-Q score of 5 was used to define low versus high symptom severity.
Data analysis
Descriptive analyses were conducted to evaluate sample distribution of caregiver mindfulness (global score and individual factors) and caregiving experience (PANAC-/+), care preparedness, care confidence, burden (ZBI), and mood (PHQ-4) by caregiver characteristics (i.e., gender, relationship with patient) and differences assessed with t tests. Bivariate relationships between caregiver mindfulness level (global and individual factors) and caregiving outcomes (experience, preparedness, confidence, mood, burden) were assessed with Pearson’s R test in the overall sample and with stratification by caregiver and patient characteristics (i.e., disease stage, dementia etiology, symptom severity). Analyses were restricted to caregivers of patients with cognitive impairment (MCI and dementia). Alpha level was set at < 0.05. Given the small sample size, especially in the stratified analyses, no adjustment was made for multiple comparisons.
RESULTS
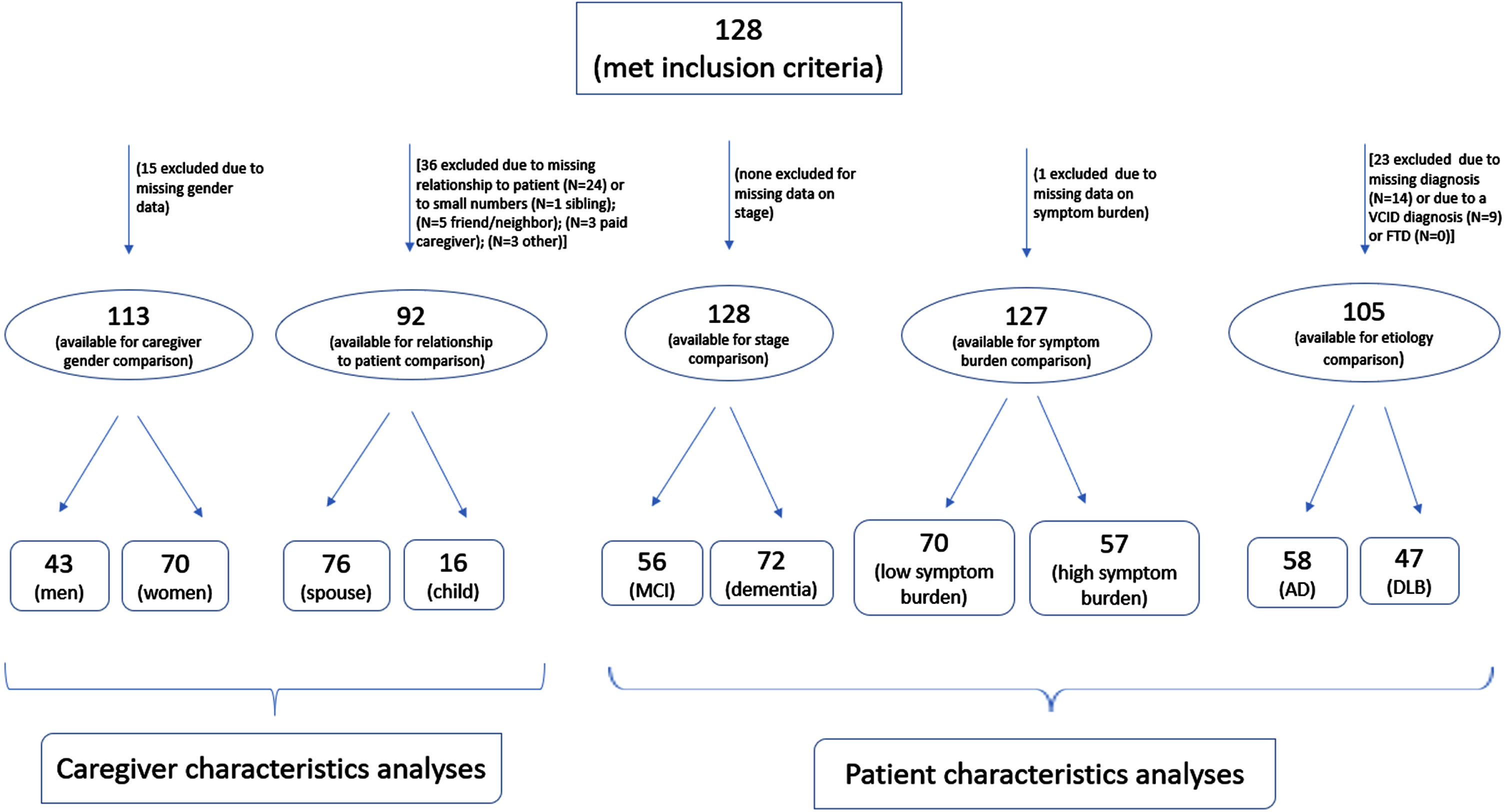
The sample selected for this analysis (N = 128) included caregivers providing care to individuals in prodromal (MCI) or dementia stage. Caregivers of cognitively normal individuals (N = 36), who were excluded from this study, were similar to those caregivers included in the study in terms of gender (47% versus 62% women, p = 0.122) and relationship to patient (74% versus 83% spouse, p = 0.323). In addition, stratified analyses were restricted to caregivers with available data on the patient- or caregiver-related characteristic being assessed. For example, due to 15 caregivers missing data on their gender, the gender comparison was based on a sample of 113 caregivers, of whom 43 were men and 70 were women. Figure 1 details the available samples for the different analyses conducted and provides information on missing data.
Fig. 1
Flow chart for analytic sample.
Sociodemographic information and average scores on mindfulness and study outcomes are presented in Table 1. The average age for caregivers was 58.4±12.2 years, with no significant differences by caregiver gender (54.6±15.8 versus 61.7±6.0, p = 0.282 for women and men, respectively). Female and male caregivers did not differ by any other caregiver characteristics assessed including mindfulness and caregiver outcomes. The only mildly significant difference was for high care recipient symptom severity, for which female caregivers reported higher levels compared to male caregivers (54.3% versus 34.9%, p = 0.045). Spouse and adult child caregivers were similar across patient-related characteristics, their socio-demographics, level of mindfulness, and caregiving experience although spouse caregivers were significantly older (61.3±7.1 versus 40.3±15.7, p = 0.003), more depressed (2.4±3.0 versus 1.0±1.3, p = 0.022), and had slightly lower positive appraisal levels (20.1±6.0 versus 23.4±4.3, p = 0.044) than adult child caregivers.
Table 1
Sample characteristics
| Mean ±SD | Total | Caregiver gender | Caregiver relationship to patient | ||||
| Women | Men | p | Spouse | Child | p | ||
| (mean±SD) | (mean±SD) | (mean±SD) | (mean±SD) | ||||
| N (%) | 128 (100) | 70 (62.9) | 43 (38.1) | – | 76 (82.6) | 16 (17.4) | – |
| Socio-demographics | |||||||
| Age, y | 58.4±12.2 | 54.6±15.8 | 61.7±6.0 | 0.282 | 61.3±7.1 | 40.3±15.7 | 0.003 |
| Woman, N (%) | 70 (61.9) | – | – | – | 40 (56.3) | 9 (64.3) | 0.582 |
| Spouse, N (%) | 76 (82.6) | 40 (81.6) | 31 (86.1) | 0.582 | – | – | – |
| Education, y | 16.2±2.5 | 16.1±2.2 | 16.3±3.0 | 0.795 | 16.2±2.6 | 16.7±2.5 | 0.569 |
| Patient characteristics | |||||||
| Dementia, % | 72 (56.3) | 41 (58.6) | 19 (44.2) | 0.137 | 43 (56.6) | 10 (41.7) | 0.202 |
| Alzheimer’s disease, % | 58 (55.2) | 28 (47.5) | 22 (62.9) | 0.148 | 32 (51.6) | 15 (75.0) | 0.066 |
| High symptom severity, % | 57 (44.9) | 38 (54.3) | 15 (34.9) | 0.045 | 40 (52.6) | 8 (33.3) | 0.099 |
| Caregiver mindfulness | |||||||
| Global score | 37.8±11.2 | 38.3±10.2 | 38.7±11.6 | 0.883 | 38.6±10.6 | 38.1±11.7 | 0.889 |
| F1 | 12.0±3.8 | 11.8±3.8 | 12.5±3.6 | 0.336 | 12.2±3.6 | 12.3±3.9 | 0.958 |
| F2 | 14.1±4.4 | 14.5±4.2 | 14.0±4.2 | 0.514 | 14.3±4.1 | 14.1±4.3 | 0.814 |
| F3 | 11.9±4.4 | 12.0±4.0 | 12.2±4.7 | 0.797 | 12.0±4.4 | 11.8±4.7 | 0.905 |
| Caregiver outcomes | |||||||
| Negative appraisals | 12.8±6.4 | 13.6±6.8 | 11.6±6.1 | 0.137 | 12.8±6.4 | 12.1±7.9 | 0.743 |
| Positive appraisals | 20.5±5.7 | 20.0±6.0 | 21.1±5.5 | 0.331 | 20.1±6.0 | 23.4±4.3 | 0.044 |
| Care preparedness | 22.3±6.4 | 22.8±5.7 | 22.6±6.6 | 0.865 | 22.7±6.4 | 20.0±5.7 | 0.145 |
| Care confidence | 10.6±2.9 | 11.0±2.9 | 10.3±2.8 | 0.227 | 10.8±2.7 | 9.7±3.3 | 0.159 |
| Depression | 2.2±2.6 | 2.4±2.7 | 1.7±2.2 | 0.163 | 2.4±3.0 | 1.3±1.3 | 0.022 |
| Burden | 11.9±9.0 | 12.4±9.4 | 10.1±7.8 | 0.199 | 11.5±9.3 | 13.1±7.6 | 0.517 |
F1, decentering; F2, positive Emotional Regulation; F3, negative Emotional Regulation. Total sample includes caregivers who met study inclusion criteria. Caregiver socio-demographics (age, gender, education, and relationship to patient) were not available for all caregivers. Specifically, 15 caregivers miss data on gender while 36 do not have data on their relationship to the patient. Total numbers for stratified analyses are provided in Fig. 1. Additionally, age was available for 17 caregivers, education for 115 caregivers, caregiver mindfulness on the full sample, PANAC on 124, care preparedness for 114, care confidence on 122, caregiver depression on 125, and caregiver burden on 118 caregivers.
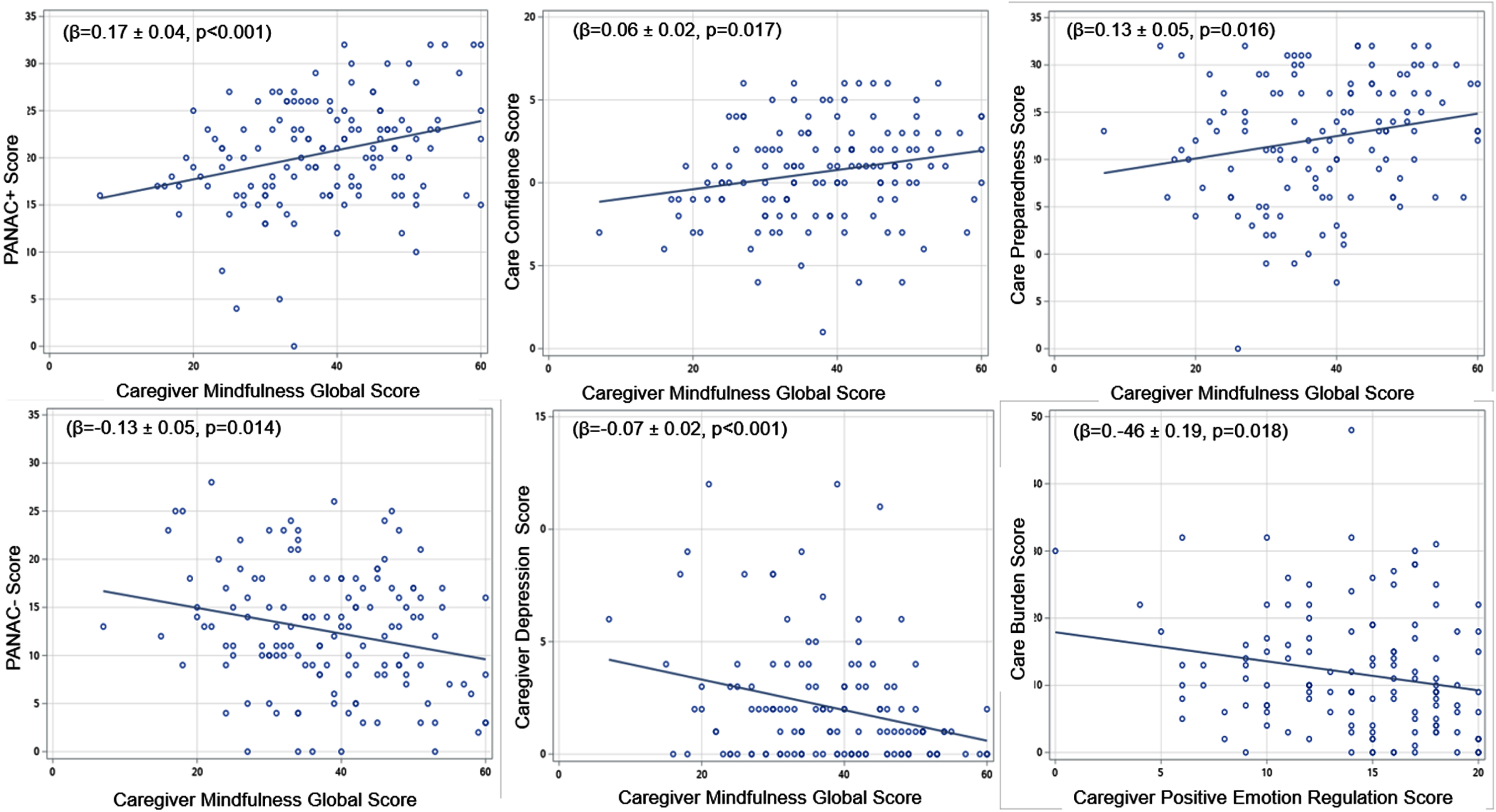
Global mindfulness was positively associated with positive appraisals (Beta = 0.17±0.04, p < 0.001), care preparedness (Beta = 0.13±0.05, p = 0.016), and care confidence (Beta = 0.06±0.02, p = 0.017) and negatively associated with negative appraisals (Beta = –0.13±0.05, p = 0.014) and depression (Beta = –0.07±0.02, p = 0.001). These relationships are captured graphically in Fig. 2. Similar patterns were found for individual mindfulness factors, particularly for Factor 2 (not shown here). Global mindfulness was not significantly associated with caregiver burden in this study (Beta = –0.11±0.08, p = 0.134) although greater positive emotion regulation was associated with lower caregiver self-reported burden (BetaF2 = –0.46±0.19, p = 0.018).
Fig. 2
Correlations between caregiver mindfulness and caregiver outcomes.
Differences by caregiver characteristics (Table 2)
Table 2
Pearson’s correlations between mindfulness and caregiver outcomes in female versus male and spouse versus child caregivers
| Negative appraisals | Positive appraisals | Care preparedness | Care confidence | Depression | Burden | ||
| R* (p) | R (p) | R (p) | R (p) | R (p) | R (p) | ||
| Global | Women | –0.10 (0.443) | 0.15 (0.215) | 0.13 (0.291) | 0.14 (0.251) | –0.23 (0.055) | –0.08 (0.539) |
| Men | –0.48 (0.001) | 0.53 (< 0.001) | 0.33 (0.054) | 0.21 (0.183) | –0.41 (0.006) | –0.12 (0.481) | |
| Spouse | –0.25 (0.035) | 0.32 (0.006) | 0.21 (0.081) | 0.15 (0.205) | –0.30 (0.009) | –0.10 (0.397) | |
| Child | –0.36 (0.168) | 0.32 (0.224) | 0.19 (0.521) | 0.24 (0.380) | –0.31 (0.237) | 0.11 (0.707) | |
| Decentering | Women | –0.05 (0.693) | 0.23 (0.056) | 0.04 (0.733) | –0.12 (0.320) | –0.13 (0.309) | –0.01 (0.956) |
| Men | –0.37 (0.017) | 0.45 (0.003) | 0.35 (0.041) | 0.25 (0.121) | –0.33 (0.031) | –0.08 (0.646) | |
| Spouse | –0.09 (0.461) | 0.32 (0.005) | 0.15 (0.212) | 0.05 (0.683) | –0.21 (0.062) | 0.001 (0.992) | |
| Child | –0.32 (0.220) | 0.37 (0.153) | 0.12 (0.686) | 0.25 (0.352) | –0.11 (0.686) | 0.05 (0.850) | |
| Positive emotional regulation | Women | –0.19 (0.143) | 0.24 (0.047) | 0.26 (0.041) | 0.22 (0.070) | –0.30 (0.014) | –0.19 (0.120) |
| Men | –0.52 (< 0.001) | 0.59 (< 0.001) | 0.19 (0.247) | 0.24 (0.126) | –0.32 (0.031) | –0.11 (0.476) | |
| Spouse | –0.33 (0.004) | 0.41 (< 0.001) | 0.29 (0.018) | 0.16 (0.168) | –0.27 (0.018) | –0.19 (0.098) | |
| Child | –0.44 (0.087) | 0.55 (0.027) | 0.31 (0.281) | 0.36 (0.167) | –0.44 (0.087) | 0.11 (0.685) | |
| Negative emotional regulation | Women | –0.08 (0.534) | –0.07 (0.560) | 0.04 (0.777) | 0.22 (0.078) | –0.17 (0.157) | 0.02 (0.846) |
| Men | –0.43 (0.005) | 0.37 (0.015) | 0.30 (0.084) | 0.12 (0.466) | –0.47 (0.001) | –0.10 (0.561) | |
| Spouse | –0.20 (0.087) | 0.13 (0.238) | 0.13 (0.286) | 0.14 (0.226) | –0.29 (0.010) | –0.05 (0.650) | |
| Child | –0.23 (0.395) | –0.01 (0.963) | 0.08 (0.778) | 0.05 (0.861) | –0.28 (0.288) | 0.11 (0.688) |
When analyses were stratified by caregiver gender, higher global mindfulness, decentering, positive emotional regulations, and negative emotional regulation scores were associated with greater positive appraisals and lower negative appraisals and depression in male caregivers. In addition, greater decentering was related to better care preparedness in this group of caregivers. Among female caregivers, the only significant associations were found for positive emotional regulation, which was positively related to positive appraisals and care preparedness and negatively related to depression.
Stratification by relationship to patient uncovered positive relationships of global mindfulness and positive emotional regulations with positive appraisals and negative relationships with negative appraisals and depression in spouse caregivers. Higher positive emotional regulation was additionally related to care preparedness, while decentering was positively associated with positive appraisals and negative emotional regulation negatively related to depression in this caregiver group. The lack of significance in adult child caregivers may be the result of the small number of child caregivers (N = 16) in our sample. Mindfulness (global and factors) was not associated with caregiver burden when analyses were stratified by caregiver characteristics (p > 0.05 across all mindfulness measures).
Differences by patient characteristics (Table 3)
Table 3
Pearson’s correlations between mindfulness and caregiver outcomes in caregivers of patients with MCI versus Dementia, AD versus DLB, and low versus high symptom severity
| Negative appraisals | Positive appraisals | Care preparedness | Care confidence | Depression | Burden | ||
| R* (p) | R (p) | R (p) | R (p) | R (p) | R (p) | ||
| Global | MCI | –0.23 (0.094) | 0.39 (0.004) | 0.48 (0.001) | 0.13 (0.336) | –0.42 (0.002) | –0.26 (0.073) |
| Dementia | –0.17 (0.162) | 0.28 (0.018) | 0.07 (0.555) | 0.27 (0.022) | –0.19 (0.106) | –0.02 (0.901) | |
| Low symptom severity | –0.19 (0.134) | 0.44 (< 0.001) | 0.21 (0.119) | 0.20 (0.103) | –0.34 (0.005) | –0.28 (0.028) | |
| High symptom severity | –0.27 (0.044) | 0.17 (0.224) | 0.19 (0.171) | 0.25 (0.065) | –0.25 (0.060) | –0.01 (0.921) | |
| AD | –0.20 (0.139) | 0.39 (0.004) | 0.25 (0.078) | 0.21 (0.131) | –0.35 (0.009) | –0.05 (0.726) | |
| DLB | –0.12 (0.429) | 0.17 (0.260) | 0.25 (0.107) | 0.27 (0.074) | –0.19 (0.200) | –0.16 (0.286) | |
| Decentering | MCI | –0.03 (0.828) | 0.40 (0.003) | 0.40 (0.007) | –0.09 (0.545) | –0.28 (0.038) | –0.06 (0.666) |
| Dementia | –0.12 (0.319) | 0.27 (0.021) | 0.02 (0.890) | 0.18 (0.139) | –0.11 (0.381) | –0.03 (0.820) | |
| Low symptom severity | –0.04 (0.771) | 0.40 (< 0.001) | 0.16 (0.220) | 0.02 (0.875) | –0.23 (0.056) | –0.18 (0.150) | |
| High symptom severity | –0.21 (0.112) | 0.24 (0.080) | 0.15 (0.302) | 0.13 (0.349) | –0.16 (0.226) | 0.02 (0.882) | |
| AD | –0.08 (0.555) | 0.41 (0.003) | 0.22 (0.138) | 0.10 (0.459) | –0.19 (0.156) | 0.06 (0.682) | |
| DLB | –0.01 (0.969) | 0.20 (0.176) | 0.07 (0.642) | –0.01 (0.966) | –0.05 (0.725) | –0.07 (0.633) | |
| Positive emotional regulation | MCI | –0.31 (0.022) | 0.47 (< 0.001) | 0.49 (< 0.001) | 0.32 (0.021) | –0.44 (< 0.001) | –0.38 (0.008) |
| Dementia | –0.21 (0.076) | 0.36 (0.002) | 0.18 (0.131) | 0.23 (0.061) | –0.18 (0.125) | –0.06 (0.624) | |
| Low symptom severity | –0.26 (0.035) | 0.49 (< 0.001) | 0.29 (0.022) | 0.34 (0.005) | –0.37 (0.002) | –0.35 (0.005) | |
| High symptom severity | –0.31 (0.022) | 0.30 (0.023) | 0.21 (0.139) | 0.21 (0.118) | –0.21 (0.112) | –0.08 (0.548) | |
| AD | –0.31 (0.020) | 0.52 (< 0.001) | 0.40 (0.004) | 0.24 (0.076) | –0.36 (0.006) | –0.17 (0.256) | |
| DLB | –0.13 (0.394) | 0.21 (0.148) | 0.24 (0.118) | 0.42 (0.004) | –0.22 (0.135) | –0.24 (0.110) | |
| Negative emotional regulation | MCI | –0.23 (0.099) | 0.18 (0.199) | 0.37 (0.014) | 0.08 (0.574) | –0.36 (0.007) | –0.21 (0.156) |
| Dementia | –0.12 (0.316) | 0.13 (0.279) | –0.01 (0.927) | 0.32 (0.007) | –0.23 (0.056) | 0.04 (0.724) | |
| Low symptom severity | –0.19 (0.133) | 0.33 (0.007) | 0.10 (0.462) | 0.15 (0.218) | –0.31 (0.009) | –0.20 (0.114) | |
| High symptom severity | –0.19 (0.155) | –0.07 (0.583) | 0.16 (0.283) | 0.30 (0.029) | –0.28 (0.035) | 0.03 (0.812) | |
| AD | –0.10 (0.463) | 0.07 (0.634) | 0.03 (0.854) | 0.17 (0.223) | –0.30 (0.025) | 0.01 (0.984) | |
| DLB | –0.14 (0.333) | 0.07 (0.688) | 0.35 (0.019) | 0.09 (0.087) | –0.24 (0.102) | –0.10 (0.518) |
Patterns of association between mindfulness and positive and negative outcomes varied by patient characteristics (i.e., stage, etiology, or symptom severity) as well. Global mindfulness and decentering were positively related to positive appraisals and care preparedness and negatively related to depression in the MCI caregiver group. In addition, negative emotional regulation was positively associated with care preparedness while positive emotional regulation was related to all caregiver outcomes in this caregiver group. When stratifying by care receiver symptom severity, we found global mindfulness and negative emotional regulation to be positively related to positive appraisals and negatively related to depression in the low symptom severity caregiver group. Additional relationships were found for global mindfulness, which was negatively associated with burden, and decentering, which was positively related to positive appraisals in the low symptom severity group, while positive emotional regulation was found to be associated with all caregiver outcomes in this caregiver group. Fewer associations were found for the high symptom severity group with global mindfulness negatively related to negative appraisals, positive emotional regulation additionally associated with both negative and positive appraisals, and negative emotional regulation positively associated with care confidence and negatively associated with depression in this caregiver group. Finally, when stratifying by disease etiology, we found evidence of a relationship between global mindfulness and positive appraisals and depression in the AD group, with decentering positively associated with positive appraisals and negative emotional regulation negatively associated with depression, while positive emotional regulation was associated with all caregiver outcomes except care confidence and burden in this caregiver group. Finally, positive associations were found for positive emotional regulation and care confidence and for negative emotional regulation and care preparedness in the DLB caregiver group.
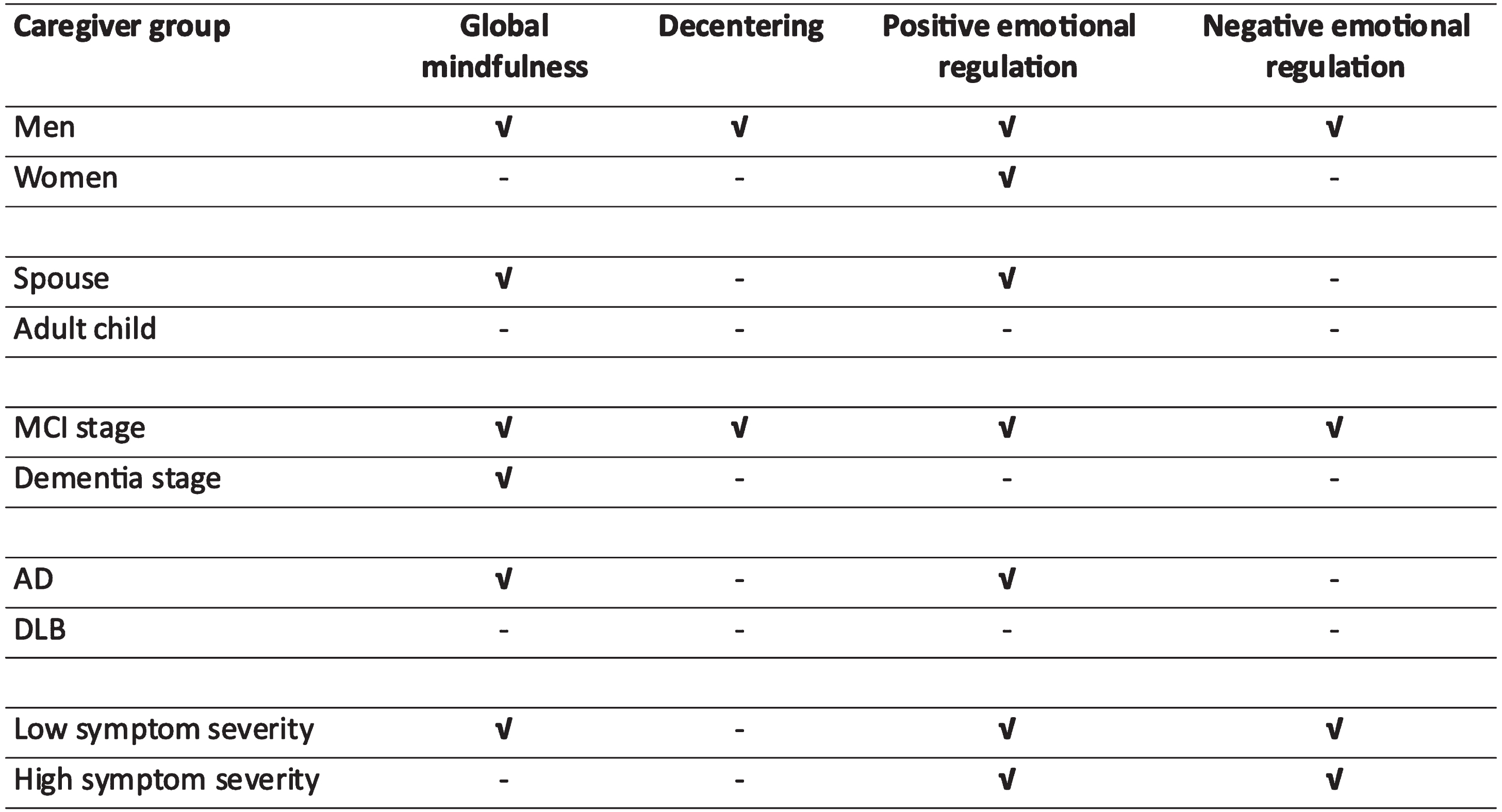
Figure 3 presents patterns of significance of individual mindfulness measures in terms of caregiving outcomes by caregiver group and patient characteristics. Significance in this context is defined as a moderate association (r > 0.2, p < 0.05) with at least two out of five caregiving outcomes and is depicted with a checkmark. No significant relationships were found for adult children and caregivers of patients with DLB. For male caregivers and those caring for patients with MCI, all mindfulness measures were significantly associated with caregiving experience, while those caring for patients with low symptom severity, significant relationships were found for global mindfulness and both emotional regulation factors. Significant relationships were found for global mindfulness and positive emotional regulation in spouse caregivers and those caring for AD patients. Finally, significance was only found for positive emotional regulation among female caregivers and for global mindfulness in those caring for patients in later stages of disease.
Fig. 3
Significant relationships between mindfulness measures and caregiver outcomes across caregiver groups. Groups are based on caregiver and patient characteristics. Significance based on at least 2 out of 5 outcomes being significantly related to each mindfulness measure at p < 0.05; MS = marginal significance (1 out of 5 outcomes significant).
DISCUSSION
This study was designed to assess the relationship between caregiver mindfulness and several caregiver psychosocial outcomes, identify significant mindfulness components, and investigate whether these select caregiver and patient characteristics appear to modulate these relationships. We found evidence to support a positive relationship between caregiver mindfulness and how caregivers perceive their caregiving experience, their preparedness and confidence in a caregiver role, and their mood. This relationship was observed for global mindfulness and individual components, with positive emotion regulation (Factor 2) having the most consistent relationship in the total sample and across subsamples defined by caregiver- and patient-related characteristics. Decentering and negative emotion regulation on the other hand appear to be significant only in specific caregiver groups.
The interest in the health benefits of mindfulness in caregivers of PLwD has peaked in the past several decades following mounting evidence of the negative impact that caring for older adults with ADRD has on various aspects of caregiver health. This in turn leads to exacerbation of patient dementia-related outcomes and psychological symptoms [58], and increased emergency department use [59] and institutionalization among PLwDs [60], further supporting the need to identify protective caregiver-specific factors such as mindfulness, that can act as coping resources. Greater caregiver mindfulness has been linked to higher patient health-related quality of life, and positive caregiver-based appraisals of caregiving, greater care preparedness and confidence, and lower self-reported depression especially when combined with higher patient mindfulness [20]. In addition, it may help pinpoint the specific coping skills that one may need to develop and/or improve on, and therefore aid in better tailoring interventions to specific needs of the individual.
We found that in male caregivers and in those providing care to patients in earlier stages of ADRD (MCI versus Dementia), greater global mindfulness, and higher scores on each of its three factors were related to better caregiver outcomes. In contrast, in female caregivers, the only significant mindfulness factor was positive emotion regulation. Our finding of a significant correlation with negative emotion regulation in male but not female caregivers is in line with reported gender differences in emotion regulation. Findings from an functional MRI study of cognitive reappraisal suggest that men may be more successful in reducing the amount of negative affect they are experiencing as evidenced by a faster down-regulation of amygdala activation and lesser control-related prefrontal activity in men than women during cognitive reappraisal of stressors/negative stimuli [30]. In women on the other hand, the ventral striatum, which is more active when processing positive stimuli, was more engaged compared to men suggesting they are more effective at increasing positive affect. The greater correlation with decentering among male caregivers in our sample is supported by recent reports of higher average decentering scores in men [29]. We found that this greater ability to step back from distressing thoughts was significant in terms of caregiver experience (i.e., more self-reported positive appraisal and less negative appraisal; better care preparedness) and better mood in male but not female caregivers or those caring for PLwD with low symptom severity or in early stages of disease. Replication in larger studies and further investigation of the potentially protective effects of decentering and negative emotion regulation on male caregivers’ emotional health and experience providing care for PLwDs are needed to better quantify the contribution of these mindfulness components to mitigation of these outcomes in male versus female caregivers.
As was the case in women, the positive association of mindfulness and caregivers’ care experience (i.e., better positive and negative appraisals) was limited to positive emotion regulation among caregivers of patients in early stages, as well as spouse caregivers and FCGs caring for patients with AD as opposed to DLB. These findings are in line with previous reports of better psychological health in caregivers with greater ability to regulate their emotions, especially positive emotions [61]. This is particularly pertinent in spouse caregivers, who along with female children represent the most common dementia caregivers [5]. Empirical evidence of effectiveness of positive emotion regulation skill building in improving emotional and physical health in caregivers and particularly spouse/significant other [62] further highlights the need for tailored interventions in these at-risk caregiver groups.
Our significant findings of positive emotion regulation in caregivers of individuals diagnosed with AD are supported by evidence of lower likelihood of negative emotions in this group of caregivers versus caregivers caring for loved ones with other types of dementia [63]. We did not find significant relationships between mindfulness and caregiving outcomes in FCGs of DLB patients, likely due to the small number of DLB patients in our study. However, the observed associations between emotion regulation and care confidence and preparedness point to the need to further evaluate the benefits of greater ability to regulate emotions in caregivers of individuals with DLB.
Our finding of significant relationships between global mindfulness but not individual components and caregiver experience among caregivers of patients in later stages of dementia in interesting. While not considered significant based on our study-specific criteria, significant associations between decentering and positive emotional regulation and positive appraisals in these caregivers, support reports of emotional detachment, a decentering-related metacognitive process [64] and separating the person from their condition as a coping strategy while providing end stage dementia care [65]. This allows them to remain engaged in their caregiver role while maintaining positive emotions and attitudes toward their affected family member, which in turn, as our findings suggest, leads to better caregiver outcomes such as more positive care appraisals and higher care confidence.
It is worthwhile to notice that while positive emotion regulation was an important coping strategy engaged by spouses and caregivers of AD patients, the significant correlations of global mindfulness and caregiving appraisal and mood in these groups suggest that best strategies to improve care outcomes in these FCGs should combine positive emotion regulation with elements of the other two coping skill building strategies. Moreover, findings of significant positive relationships between global and individual mindfulness components scores and caregiver outcomes in males and caregivers of individuals in early stages of neurodegenerative disease indicate that these caregiver groups may benefit the most from development of coping skills related to decentering, positive emotion regulation, and negative emotion regulation. While the answer to the question of why benefits of mindfulness in these last caregiver groups extend to its three components remains unclear, we posit that providing care to family members in prodromal stages of dementia, who are likely to have a lower burden of dementia-related symptoms and behaviors may be less taxing on the caregivers. This allows engagement of different meta-cognitive processes; none being overpowered by the severity and/or frequency of symptoms that characterize later stages of dementia. Finally, while caregiver mindfulness was not consistently associated with caregiver burden in our study, the evidence of a negative association between positive emotion regulation and burden in caregivers of older adults in early stages of disease or with low symptom severity is encouraging and highlights the importance of further validating these findings in larger samples of these caregiver groups.
Findings from this study should be interpreted with consideration of several potential limitations. First, this is an observational cross-sectional study, which only allows investigation of baseline correlations between mindfulness and caregiver experience, care preparedness, care confidence, care burden, and mood. Correlations help demonstrate that significant associations exist between these factors but cannot establish that mindfulness precedes the caregiver outcomes investigated here. Reverse causality is possible where mindfulness can be influenced by caregiver anxiety, stress perception, emotional exhaustion [66]. Intervention studies are better equipped to address directionality of the relationship to investigate the factors that determine mindfulness level and what aspects of mindfulness should be targeted for coping skill building in caregivers. Second, the small sample size in our study limited our ability to detect an effect of mindfulness in adult child caregivers and caregivers of individuals with DLB. Moreover, it limited our ability to assess combinations of caregiver groups or compare caregivers based on characteristics for which information was not available in the patient chart (e.g., caregiver personally identifiable information such as age was not required). Future larger studies are needed to better assess the impact of mindfulness in caregiver groups such as adult daughters of patients in later stages of AD or female spouse of patients in early stages of dementia or younger versus older caregivers, which will help better target at risk caregivers. Future studies should also explore other dementia etiologies (e.g., VCID, FTD) that may have very different caregiving experiences. Strengths of our study include the use of AMPS to assess mindfulness level and identify the specific mindfulness processes (i.e., decentering, positive emotion regulation, and negative emotion regulation) that are beneficial to caregiver mood and caregiving experience and the deeply phenotyped clinical population that allowed better characterization of patients in terms of stage and etiology of dementia.
In conclusion, our findings have clinical and public health relevance by identifying the specific processes/coping skills through which mindfulness may operate in dementia caregivers. This can aid in designing successful interventions to improve caregiving experience, care preparedness, care confidence, and caregiver mood, which are greatly impacted when providing dementia care to affected family members. Furthermore, our results suggest future venues of investigation focused on assessment of effectiveness of mindfulness-based interventions that target specific processes (i.e., improving positive emotion regulation in spouse caregivers) or are all-scope in design (i.e., improving all three mindfulness processes in male caregivers) in specific groups of caregivers. Improving the caregiving experience and decreasing caregiver distress remain important research and clinical goals in the dementia caregiver community and intervention approaches that are customized to specific caregiver groups have the potential to aid in reaching these goals.
ACKNOWLEDGMENTS
The authors have no acknowledgements to report.
FUNDING
This study was supported by grants to JEG from the National Institute on Aging (R01 AG071514, R01 AG069765, and R01 NS101483), the Research Center of Excellence Program from the Lewy Body Dementia Association, the Harry T. Mangurian Foundation, and the Leo and Anne Albert Charitable Trust. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
CONFLICT OF INTEREST
JEG is the creator of PANAC and the copyright is held by the University of Miami Miller School of Medicine. JEG has served as a consultant to Alpha Cognition, Biogen, Eisai, Genentech, and Roche. Payments were made to JEG. In conjunction with the University of Miami, JEG is patenting a Brain health platform. The patent is pending. MIT, SC, and IRC have no conflict of interest to report.
REFERENCES
[1] | Alzheimer’s Association ((2021) ) 2021 Alzheimer’s disease facts and figures, Special Report: Race, ethnicity and Alzheimer’s in America. Alzheimers Dement 17: , 1–104. |
[2] | Alzheimer’s Association ((2019) ) 2019 Alzheimer’s disease facts and figures. Alzheimers Dement 15: , 321–387. |
[3] | Wulff J , Fange AM , Lethin C , Chiatti C ((2020) ) Self-reported symptoms of depression and anxiety among informal caregivers of persons with dementia: A cross-sectional comparative study between Swand Italy. BMC Health Serv Res 20: , 1114. |
[4] | Peavy G , Mayo AM , Avalos C , Rodriguez A , Shifflett B , Edland SD ((2022) ) Perceived stress in older dementia caregivers: Mediation by loneliness and depression. Am J Alzheimers Dis Other Demen 37: , 153333175211064756. |
[5] | Brodaty H , Donkin M ((2009) ) Family caregivers of people with dementia. Dialogues Clin Neurosci 11: , 217–228. |
[6] | Rahman A , Anjum R , Sahakian Y ((2019) ) Impact of caregiving for dementia patients on healthcare utilization of caregivers. Pharmacy (Basel) 7: , 138. |
[7] | Coon DW , Rubert M , Solano N , Mausbach B , Kraemer H , Arguelles T , Haley WE , Thompson LW , Gallagher-Thompson D ((2004) ) Well-being, appraisal, and coping in Latina and Caucasian female dementia caregivers: Findings from the REACH study. Aging Ment Health 8: , 330–345. |
[8] | Haley WE , Gitlin LN , Wieniewski SR , Feeney Mahoney D , Coon DW , Winter L , Corcoran M , Schinfeld S , Ory M ((2004) ) Well-being, appraisal, and coping in African-American and Caucasian dementia caregivers: Findings from the REACH study. Aging Ment Health 8: , 316–329. |
[9] | Hilgeman MM , Allen RS , DeCoster J , Burgio LD ((2007) ) Positive aspects of caregiving as a moderator of treatment outcome over 12 months. Psychol Aging 22: , 361–371. |
[10] | Galvin JE , Tolea MI , Chrisphonte S ((2020) ) The positive and negative appraisals of caregiving (PANAC) scale: A new measure to examine the caregiving experience in Alzheimer’s disease and related dementias.. Alzheimers Dement (N Y) 6: , e12104. |
[11] | Yu DSF , Cheng ST , Wang J ((2018) ) Unravelling positive aspects of caregiving in dementia: An integrative review of research literature. Int J Nurs Stud 79: , 1–26. |
[12] | Allen AP , Buckley MM , Cryan JF , Chorcoran AN , Dinan TG , Kearney PM , O’Caoimh R , Calnan M , Clarke G , Molloy DW ((2019) ) Informal caregiving for dementia patients: The contribution of patient characteristics and behaviours to caregiver burden. Age Ageing 49: , 52–56. |
[13] | Kawano Y , Terada S , Takenoshita S , Hayashi S , Oshima Y , Miki T , Yokota O , Yamada N ((2020) ) Patient affect and caregiver burden in dementia. Psychogeriatrics 20: , 189–195. |
[14] | Lindeza P , Rodriguez M , Costa J , Guerreiro M , Rosa MM ((2020) ) Impact of dementia on informal care: A systematic review of family caregivers’ perceptions. BMJ Support Palliat Care, doi: 10.1136/bmjspcare-2020-002242. |
[15] | Prorok JC , Horgan S , Seitz DP ((2013) ) Health care experiences of people with dementia and their caregivers: A meta-ethnographic analysis of qualitative studies. CMAJ 185: , E669–680. |
[16] | Lavretsky H ((2005) ) Stress and depression in informal dementia caregivers. Health Aging 1: , 117–133. |
[17] | Lavretsky H , Siddarth P , Nazarian N , St. Cyr N , Khalsa DS , Lin J , Blackburn E , Epel ES , Irwin MR ((2013) ) A pilot study of yogic meditation for family dementia caregivers with depressive symptoms: Effects on mental health, cognition, and telomerase activity. Int J Geriatr Psychiatry 28: , 57–65. |
[18] | Weisman de Mamani A , Weintraub MJ , Maura J , Martinez de Andino A , Caitli B ((2018) ) The interplay among mindfulness, caregiver burden, and mental health in family members of individuals with dementia. Prof Psychol Res Pract 49: , 116–123. |
[19] | Murfield J , Moyle W , O’Donovan A , Ware RS ((2020) ) The role of self-compassion, dispositional mindfulness, and emotion regulation in the psychological health of family carers of older adults. Clin Gerontol, doi: 10.1080/07317115.2020.1846650. |
[20] | Innis AD , Tolea MI , Galvin JE ((2021) ) The effect of ine patient and caregiver mindfulness on dementia outcomes. J Alzheimers Dis 79: , 1345–1367. |
[21] | Liu Z , Chen QL , Sun YY ((2017) ) Mindfulness training for psychological stress in family caregivers of persons with dementia: A systematic review and meta-analysis of randomized controlled trials. Clin Interv Aging 12: , 1521–1529. |
[22] | Collins RN , Kishita N ((2019) ) The effectiveness of mindfulness- and acceptance-based interventions for informal caregivers of people with dementia: A meta-analysis. Gerontologist 59: , e363–e379. |
[23] | Molero Jurado MDM , Perez-Fuentes MDC , Barragan Martin AB , Soriano Sanchez JG , Oropesa Ruiz NF , Sisto M , Gazquez Linares JJ ((2020) ) Mindfulness in family caregivers of persons with dementia: Systematic review and meta-analysis. Healthcare (Basel) 8: , 193. |
[24] | Han A ((2021) ) Effects of mindfulness-based interventions on depressive symptoms, anxiety, stress, and quality of life in family caregivers of persons living with dementia: A systematic review and meta-analysis. Res Aging 44: , 494–509. |
[25] | Safran J , Segal ZV ((1996) ) Lanham. Interpersonal Process in Cognitive Therapy. |
[26] | Guendelman S , Medeiros S , Rampes H ((2017) ) Mindfulness and emotion regulation: Insights from neurobiological, psychological, and clinical studies. Front Psychol 8: , 220. |
[27] | Kessel R , Gecht J , Forkmann T , Drueke B , Gauggel S , Mainz V ((2016) ) Exploring the relationship of decentering to health related concepts and cognitive and metacognitive processes in a student sample. BMC Psychol 4: , 11. |
[28] | Hayes-Skelton SA , Graham JR ((2013) ) Decentering as a common link among mindfulness, cognitive reappraisal, and social anxiety. Behav Cogn Psychother 41: , 317–328. |
[29] | Naragon-Gainey K , McMahon TP , Strowger M , Lackner RJ , Stanley Seah TH , Moore MT , Fresco DM ((2020) ) A comparison of decentering across demographic groups and meditation experience: Support for the measurement invariance of the Experiences Questionnaire. Psychol Assess 32: , 197–204. |
[30] | McRae K , Ochsner KN , Mauss IB , Gabrieli JJD , Gross JJ ((2008) ) Gender differences in emotion regulation: An fMRI study of cognitive reappraisal. Group Process Intergroup Relat 11: , 143–162. |
[31] | Li MJ , Black DS , Garland EL ((2016) ) The Applied Mindfulness Process Scale (AMPS): A process measure for evaluating mindfulness-based interventions. Pers Individ Dif 93: , 6–15. |
[32] | Galvin JE ((2015) ) The Quick Dementia Rating System (QDRS): A rapid dementia staging tool. Alzheimers Dement (Amst) 1: , 249–259. |
[33] | Rattanabannakit C , Risacher SL , Gao S , Lane KA , Brown SA , McDonald BC , Unverzagt FW , Apostolova LG , Saykin AJ , Farlow MR ((2016) ) The Cognitive Change Index as a measure of self and informant perception of cognitive decline: Relation to neuropsychological tests. J Alzheimers Dis 51: , 1145–1155. |
[34] | Li C , Neugroschl J , Luo X , Zhu C , Aisen P , Ferris S , Sano M ((2017) ) The utility of the Cognitive Function Instrument (CFI) to detect cognitive decline in non-demented older adults. J Alzheimers Dis 60: , 427–437. |
[35] | Galvin JE , Roe CM , Powlishta KK , Coats MA , Muich SJ , Grant E , Miller JP , Storandt M , Morris JC ((2005) ) The AD8: A brief informant interview to detect dementia. Neurology 65: , 559–564. |
[36] | Nasreddine ZS , Phillips NA , Bedirian V , Charbonneau S , Whitehead V , Collin I , Cummings JL , Chertkow H ((2005) ) The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53: , 695–699. |
[37] | Shapiro AM , Benedict RH , Schretlen D , Brandt J ((1999) ) Construct and concurrent validity of the Hopkins Verbal Learning Test-revised. Clin Neuropsychol 13: , 348–358. |
[38] | Weintraub S , Besser L , Dodge HH , Teylan M , Ferris S , Goldstein FC , Giordani B , Kramer J , Loewenstein D , Marson D , Mungas D , Salmon D , Welsh-Bohmer K , Zhou XH , Shirk SD , Atri A , Kukull WA , Phelps C , Morris JC ((2018) ) Version 3 of the Alzheimer Disease Centers’ Neuropsychological Test Battery in the Uniform Data Set (UDS). Alzheimer Dis Assoc Disord 32: , 10–17. |
[39] | Galvin JE , Tolea MI , Moore C , Chrisphonte S ((2020) ) The Number Symbol Coding Task: A brief measure of executive function to detect dementia and cognitive impairment. PLoS One 15: , e0242233. |
[40] | Reitan RM ((1958) ) Validity of the trail making test as an indication of organic brain damange. Perceptual Motor Skills 8: , 271–276. |
[41] | Yokoi K , Nishio Y , Uchiyama M , Shimomura T , Iizuka O , Mori E ((2014) ) Hallucinators find meaning in noises: Pareidolic illusions in dementia with Lewy bodies. Neuropsychologia 56: , 245–254. |
[42] | Snaith RP ((2003) ) The Hospital Anxiety And Depression Scale. Health Qual Life Outcomes 1: , 29. |
[43] | Tappen RM , Rosselli M , Engstrom G ((2010) ) Evaluation of the Functional Activities Questionnaire (FAQ) in cognitive screening across four American ethnic groups. Clin Neuropsychol 24: , 646–661. |
[44] | Kaufer DI , Cummings JL , Ketchel P , Smith V , MacMillan S , Shelley T , Lopez OL , DeKosky ST ((2000) ) Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci 12: , 233–239. |
[45] | Morris JC ((1993) ) The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology 43: , 2412–2414. |
[46] | Reisberg B ((2007) ) Global measures: Utility in defining and measuring treatment response in dementia. Int Psychogeriatr 19: , 421–456. |
[47] | McKhann GM , Knopman DS , Chertkow H , Hyman BT , Jack CR Jr , Kawas CH , Klunk WE , Koroshetz WJ , Manly JJ , Mayeux R , Mohs RC , Morris JC , Rossor MN , Scheltens P , Carrillo MC , Thies B , Weintraub S , Phelps CH ((2011) ) The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7: , 263–269. |
[48] | McKeith IG , Boeve BF , Dickson DW , Halliday G , Taylor JP , Weintraub D , Aarsland D , Galvin J , Attems J , Ballard CG , Bayston A , Beach TG , Blanc F , Bohren N , Bonanni L , Bras J , Brundin P , Burn D , Chen-Plotkin A , Duda JE , El-Agnaf O , Feldman H , Ferman TJ , Ffytche D , Fujishiro H , Galasko D , Goldman JG , Gomperts SN , Graff-Radford NR , Honig LS , Iranzo A , Kantarci K , Kaufer D , kukull W , Lee VMY , Leverenz JB , Lewis S , Lippa C , Lunde A , Masellis M , Masliah E , McLean P , Mollenhauer B , Montine Tj , Moreno E , Mori E , Murray M , O’Brien JT , Orimo S , Postuma RB , Ramswamy S , Ross OA , Salmon DP , Singleton A , Taylor A , Thomas A , Tiraboschi P , Toledo JB , Trojanowski JQ , Tsuang D , Walker Z , Yamada M , Kosaka K ((2017) ) Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology 89: , 88–100. |
[49] | Skrobot OA , O’Brien J , Black S , Chen C , DeCarli C , Erkinjuntti T , Ford GA , Kalaria RN , Pantoni L , Pasquier F , Roman GC , Wallin A , Sachdev P , Skoog I , VICCCS group, Ben-Shlomo Y , Passmore AP , Love S , Kehoe PG ((2017) ) The Vascular Impairment of Cognition Classification Consensus Study. Alzheimers Dement 13: , 624–633. |
[50] | Olney NT , Spina S , Miller BL ((2017) ) Frontotemporal dementia. Neurol Clin 35: , 339–374. |
[51] | Archbold PG , Stewart BJ , Greenlick MR , Harvath T ((1992) ) The clinical assessmenmt of mutuality and preparedness in family caregivers to frail older people. In Key Aspects of Elder Care: Managing Falls, Incontinence and Cognitive Impairment, FunkSG, TornquistEm, ChampagneMT, CoppLA, eds. Springer, New York, pp. 328–339. |
[52] | Pucciarelli G , Savini S , Byun E , Simeone S , Barabranelli C , Vela RJ , Alvaro R , Vellone E ((2014) ) Psychometric properties of the Caregiver Preparedness Scale in caregivers of stroke survivors. Heart Lung 43: , 555–560. |
[53] | Connell C , Boise L , Stuckey JC , Holmes SB , Hudson ML ((2004) ) Attitudes toward the diagnosis and disclosure of dementia among family caregivers and primary care physicians. Gerontologist 44: , 500–507. |
[54] | Bedard M , Molloy DW , Dubois S , Lever JA , O’Donnell M ((2001) ) The Zarit Burden Interview: A new short version and screening version. Gerontologist 41: , 652–657. |
[55] | Ojifinni OO , Uchendu OC ((2018) ) Validation and reliability of the 12-item Zarit Burden Interview among Informal Caregivers of Elderly Persons in Nigeria. Arch Basic Appl Med 6: , 45–49. |
[56] | Kroenke K , Spitzer RL , Williams JBW , Lowe B ((2009) ) An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 50: , 613–621. |
[57] | Khubchandani J , Brey R , Kotecki J , Kleinfelder J , Anderson J ((2016) ) The psychometric properties of PHQ-4 Depression and Anxiety Screening Scale among college students. Arch Psychiatr Nurs 30: , 457–462. |
[58] | Stall NM , Kim SJ , Hardacre KA , Shah PS , Straus SE , Bronskill SE , Lix LM , Bell CM , Rochon PA ((2019) ) Association of informal caregiver distress with health outcomes of community-dwelling dementia care recipients: A systematic review. J Am Geriatr Soc 67: , 609–617. |
[59] | Guterman EL , Allen IE , Josephson SA , Merrilees JJ , Dulaney S , Chiong W , Lee K , Bonasera SJ , Miller BL , Possin KL ((2019) ) Association between caregiver depression and emergency department use among patients with dementia. JAMA Neurol 76: , 1166–1173. |
[60] | Eska K , Graessel E , Donath C , Schwarzkopf L , Lauterberg J , Holle R ((2013) ) Predictors of institutionalization of dementia patients in mild and moderate stages: A 4-year prospective analysis. Dement Geriatr Cogn Dis Extra 3: , 426–445. |
[61] | Jutten LH , Mark RE , Sitskoorn MM ((2019) ) Empathy in informal dementia caregivers and its relationship with depression, anxiety, and burden. Int J Clin Health Psychol 19: , 12–21. |
[62] | Moskowitz JT , Cheung EO , Snowberg KE , Verstaen A , Merrilees J , Salsman JM , Dowling GA ((2019) ) Randomized controlled trial of a facilitated online positive emotion regulation intervention for dementia caregivers. Health Psychol 38: , 391–402. |
[63] | Chen KH ((2021) ) Anger in family caregivers of people with behavioral variant frontotemporal dementia versus Alzheimer’s disease. Alzheimers Dement 17: (Suppl 7), e056230. |
[64] | Bernstein A , Hadash Y , Lichtash Y , Tanay G , Sheperd K , Fresco DM ((2015) ) Decentering and related constructs: A critical review and metacognitive processes model. Perspect Psychol Sci 10: , 599–617. |
[65] | Hochwald IH , Arieli D , Radomyslsky Z , Danon Y , Nissanholtz-Gannot R ((2022) ) Emotion work and feeling rules: Coping strategies of family caregivers of people with end stage dementia in Israel - A qualitative study. Dementia (London) 21: , 1154–1172. |
[66] | Yu J , Song Y , Hua D , Shi Y , Zhao J ((2022) ) Factors influencing mindfulness among clinical nurses in China: An observational cross-sectional study. J Nurs Manag 30: , 758–766. |




