Anger and Dementia Caregiving: A Systematic Review of the Effects of Anger and Hostility on Caregivers’ Physical Health
Abstract
Background:
Anger is commonly experienced by family caregivers of people living with dementia yet its effect on caregivers’ physical health remains unknown.
Objective:
The primary aim of this study was to systematically review current evidence on the effects of anger and hostility on caregivers’ physical health.
Methods:
We searched Medline, EMBASE, PubMed, and PsycINFO up to January 2022. Two review authors independently extracted data on study characteristics, study quality, and effect sizes of associations of anger and hostility with caregiver health outcomes.
Results:
We found eight studies examining the effects of anger and hostility on caregivers’ physical health reporting on a total of 937 participants, of which four were cross-sectional and four were longitudinal. Overall findings indicated that higher levels of anger and hostility exerted a negative effect on caregivers’ physical health. Higher anger control was longitudinally associated with increased weight gain (β= 1.13, p < 0.001), whereas higher anger out predicted higher glucose dysregulation at long-term follow-up (r = 0.27, p < 0.05). Higher levels of caregiver hostility were associated with increased risk of chronic low-grade inflammation long-term (r = 0.18, p < 0.05), and increased risk of cognitive decline over time (r = –0.16, p < 0.05).
Conclusion:
Our review provides the first systematic synthesis of the evidence demonstrating the harmful effects of anger and hostility on dementia caregivers’ health and highlights the need for preventative interventions to support family caregivers experiencing high levels of anger.
INTRODUCTION
Anger and dementia caregiving
There are currently over 50 million people with dementia worldwide [1], with family caregivers contributing most of the “front line” care [2]. Caring for someone living with dementia is a source of chronic stress [3], placing family caregivers increasingly vulnerable to negative health outcomes [4]. Systematic reviews and meta-analyses have shown that dementia caregivers generally have poorer health outcomes compared to non-caregivers and are more vulnerable at experiencing psychological and financial strain [5]. The negative effects of caregiving are most likely to be found in psychologically distressed caregivers, who often report high levels of anxiety and depression [6].
Although not all family caregivers will experience these negative affective reactions, chronic stress associated with the demands of caregiving predisposes family caregivers to difficulties in emotion regulation, which often lead to interpersonal conflict, and experiencing feelings of resentment [7]. Recent studies have consistently shown that family caregivers are also vulnerable to experiencing high levels of anger [8]. For example, they may often express anger as a response to highly distressing situations, such as when a care recipient exhibits high levels of neuropsychiatric symptoms [9]. Feelings of anger have in fact been found to be highly prevalent in dementia caregivers [9], who often report that experiencing difficulties in suppressing anger in the context of providing care can be very distressing [10, 11].
Despite anger being a commonly experienced negative affective reaction for dementia caregivers [12], it remains the least understood compared to experiences of clinically significant symptoms of depression, anxiety, and caregiver burden [13, 14]. The lack of research in the area may partly stem from the stigma associated with these feelings, or the fear of social or legal consequences for caregivers for reporting such reactions [15]. Nevertheless, several studies have shown that similarly to the general population caregiver anger and hostility, may exert a harmful effect on caregivers’ physical well-being and increase risk of ill health [12, 16]. Understanding how anger influences disease risk in dementia caregivers is important for preventing poor physical health outcomes for this vulnerable group, and for informing future clinical behavioral interventions to lower this risk.
Anger and its effects on physical health
Prior research and theory have highlighted the multifaceted nature of anger, described as a continuum of behaviors exhibited by individuals in response to challenging interpersonal situations [17]. Although manifestations of anger are considered to be quite complex, a broad conceptualization of anger and its management is illustrated in Spielberger’s State-Trait Anger Expression Inventory [18], designed to assess the experience, expression, and control of anger. Important distinctions include those between anger-in versus anger-out referring to the suppression or internalization of anger versus the expression of physical or verbal behavior [19], whereas the concept of control refers to conscious efforts by individuals to control feelings of anger and their expression [20].
Later theoretical work pointed towards the importance of measuring state versus trait anger, with state anger referring to situational responses and subjective experiences, versus measuring anger as a stable personality trait (trait anger) [21]. An important inter-related construct of trait anger is hostility [22], conceptualized as a negative psychological trait which similar to anger consists of physiological, biobehavioral, and cognitive dimensions that increase risk of chronic disease [23, 24].
Several decades of research have established a link between anger and negative health outcomes [16, 25]. For example, studies have shown that individuals who experience more frequent and severe episodes of anger are at increased risk of cardiovascular and coronary heart disease [26]. It has been postulated that both the expression of anger (i.e., internalized versus externalized) and its chronic internalization (i.e., suppression) differentially contribute to poor health outcomes, by accelerating cumulative stress, and chronic inflammation processes, thereby increasing individuals’ risk of ill health [27]. Anger and hostility may also exert their harmful effects by increasing dysregulation of cortisol levels, and compromising immunity responses, predisposing individuals to illness and morbidity over time [28]. Expression of anger in daily life has also been linked to poor health behaviors such as smoking, physical inactivity, and higher caloric intake, indicating that anger may impact physical health via both physiological as well as behavioral pathways [26].
The present study
Although several studies have examined the effects of anger and hostility on dementia caregivers’ physical health, there are currently no systematic reviews synthesizing knowledge on which physical health outcomes are influenced by caregiver anger. Understanding the association between caregiver anger and physical health is key for informing future interventions in the area and preventing the health burden experienced by this group. The primary aim of our study therefore was to systematically review current evidence on the effects of anger and hostility on caregivers’ physical health and comment on the quality of the evidence. Our secondary objective was to provide recommendations for future research in the area.
MATERIALS AND METHODS
Search strategy
We conducted a comprehensive search using four electronic databases: Medline, EMBASE, PubMed, and PsycINFO, up to January 2022 and registered our systematic review with PROSPERO (ID CRD42020198629). We used the terms anger, hostility, dementia, carer, caregiver, and several other terms closely aligned to the construct of anger (resentment, aggression) (see Supplementary Figure 1 for details of the search strategy). We additionally hand searched reference lists of retrieved articles to ensure no studies were missed.
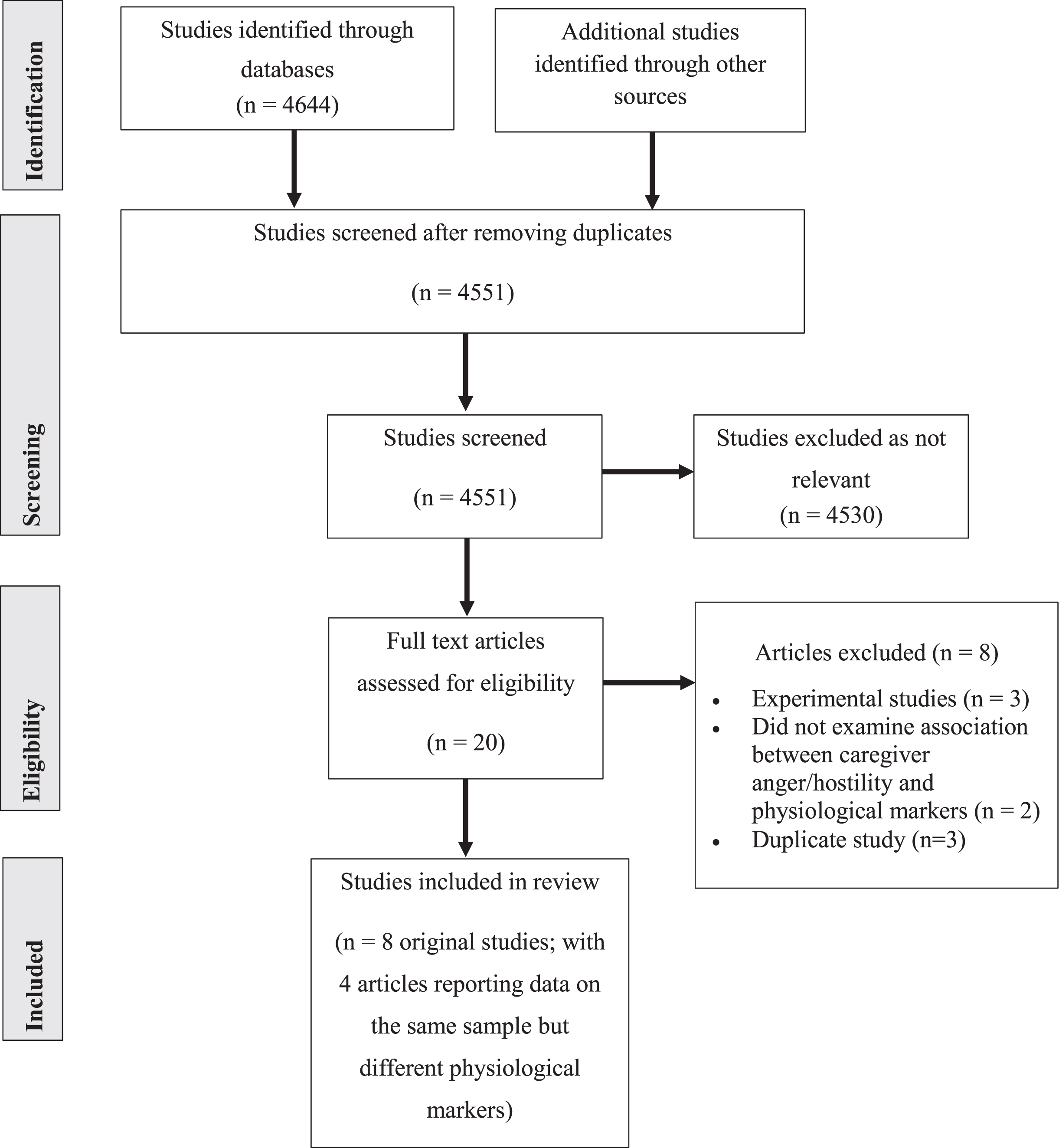
Fig. 1
PRISMA flow chart for study selection.
Inclusion and exclusion criteria
We included studies that: a) were either longitudinal or cross-sectional, b) measured anger and/or hostility as an outcome, c) included physical health status or any other physiological and/or disease marker as an outcome (i.e., blood pressure, sleep quality), and d) reported data on informal caregivers of people diagnosed with any type of dementia. We excluded experimental studies, including randomized controlled clinical trials, case reports or case series studies, and studies reporting on outcomes for formal caregivers (i.e., nursing staff or paid caregivers).
Data extraction
Two authors (YNS; PFK) independently selected eligible studies, with disagreements resolved by consulting a third author (HYK). Data extraction was also conducted independently (YNS; PFK), using a standardized data extraction form that included information on: sample characteristics and sampling method, measures of anger and/or hostility, physiological outcome measures, correlation coefficients, and/or odds ratios, and associated confidence intervals or equivalent, and number and type of confounders assessed in each study.
Study quality
Two authors assessed study quality independently (see Supplementary Table 1 for details of study quality criteria) using a modified version of the Newcastle-Ottawa quality assessment tool, which was adapted based on previous recommendations [29, 30]. The tool addressed the following domains: 1) selection of sample and measurement of outcome of interest, 2) number of confounders, and 3) outcome reporting, reporting of results, and length of follow up for longitudinal studies. Any disagreements were resolved with a third author.
Table 1
Cross-sectional and longitudinal studies of caregiver anger, hostility, and physical health outcomes
| Study | Aim | Design | Sample | Outcome measures | Results | Covariates |
| Graham et al., 2006 [35]USA | Examine the association between caregiver hostility, bodily pain, CRP, and serum IL-6 over 72 months | Longitudinal | N = 113 (F = 78; M = 35)Current/former spousal dementia caregiversMean age = 69.8 y | Hostility•Cook-Medley Hostility ScalePain•RAND 36-Item Health Survey bodily pain subscaleCRP and IL-6 levels•Plasma sample analysis using immunoassay | •Higher hostility was associated with higher CRP levels (r = 0.18, p < 0.05)•Higher hostility was associated with higher bodily pain (r = 0.25, p < 0.01)•No association with IL-6 levels | Sex, age, marital status, depression, BMI, sleep quality, smoking, exercise, caffeine use, medications |
| Leggett et al., 2015 [31]USA | Examine the association between caregiver anger and daily cortisol (AUC and CAR) | Cross-sectional | N = 164 (sex demographics not reported)Spousal and non-spousal dementia caregiversMean age = 61.8 y | Anger•Anger and hostility items from the Kessler Psychological Distress K10 and K6 scales•Cortisol•Saliva samples of AUC and CAR | •Higher anger levels were associated with lower AUC (β= –0.00, p < 0.05)•No association between anger and CAR (p > 0.05) | Sex, age, carer-related stressors, use of adult day services, duration of caregiving |
| Liu et al., 2015 [32] USA | Examine the association between caregiver anger and sleep | Cross-sectional | N = 173 (F = 150; M = 23)Spousal and non-spousal dementia caregiversMean age = 62.0 y | Anger•Anger items from the Kessler Psychological Distress K10 and K6 scalesSleep quality•1-item 5-point Likert Scale | •Higher levels of anger were associated with lower sleep quality (β= –0.21, p < 0.001) | Age, sex, spouse status, hours spent caregiving, education, ADL assistance |
| López et al., 2015 [33]Spain | Examine the association between caregiver anger and vitality | Cross-sectional | N = 108 (F = 87; M = 21)Spousal and non-spousal dementia caregiversMean age = 59.1 y | Anger•Trait Anger Reaction Scale of the STAXI-IIVitality•SF-36 Health Survey vitality subscale | •Higher levels of Trait Anger Reaction were associated with lower vitality (β= –0.32, p < 0.001) | None assessed |
| Scanlan et al., 2001 [36]USA | Examine the association between caregiver anger and lymphocyte proliferation over 15-18 months | Longitudinal | N = 82 (F = 53; M = 29)Spousal AD caregiversMean age = 69.4 y | Anger•AES•Trait Anger Scale of the STAXILymphocyte Proliferation•Assays analyses of PHA, ConA, and PW | •Higher Anger Expression (Anger Out/Anger Control) was associated with lower PHA (r = –0.26, p < 0.01)•Higher Anger Expression (Anger Out/Anger Control) was associated with lower ConA (r = –0.19, p < 0.05)•Higher Anger Expression (Anger Out/Anger Control) was associated with lower PW (r = –0.23, p < 0.01) | Depression |
| Shaw et al., 2003 [37]USA | Examine the association between caregiver hostility and blood pressure over 84 months | Cross-sectional and longitudinal | N = 111 (F = 78; M = 33)Spousal AD caregiversMean age = 71.6 y | Hostility•BSIBlood Pressure•Semi-automated sphygmomanometer | •Hostility was not associated with SBP (p > 0.05) or DBP (p > 0.05) at baseline•Hostility was not associated with SBP (p < 0.63) or DBP (p < 0.68) at follow-up | ADL assistance, care recipient behavior problems |
| Vitaliano et al., 1995 [38]*main studyUSA | Vitaliano et al., 1995Examine the association between caregiver anger and plasma lipid levels | Cross-sectional | N = 96 (F = 58; M = 38)Spousal AD caregiversMean age = 69.8 y | Anger•Trait Anger Scale of the STAXI•AESPlasma lipids•HDLC•LDLC•TG | •Higher Anger In was associated with higher HDLC (β= 0.12; p < 0.05)•Higher Anger In was associated with lower TG (β= –0.26; p < 0.001)•Higher Anger Control was associated with lower HDLC (β= –0.16; p < 0.01)•Higher Anger Out was associated with lower LDLC in females (β= –0.55; p < 0.05) | Sex, BMI, volume active drugs, vasoactive drugs, estrogen use, alcohol use |
| Vitaliano et al., 1996[39]Examine the association between caregiver anger and BMI changes over 15-18 months | Longitudinal | N = 81 (F = 52; M = 29)Spousal AD caregiversMean age = 69.8 years | Anger•AESBMI•Calculated from weight and height | •Higher Anger Control was associated with higher weight gain in females (β= 1.13; p < 0.001) | Age, average exercise per year, changes in diet, depression, perceived control, perceived burden | |
| Vitaliano et al., 1996[40]Examine the association between caregiver anger and insulin and glucose over 15-18 months | Longitudinal | N = 78 (F = 51; M = 27)Spousal AD caregiversMean age = 69.8 y | Anger•AES•Trait Anger Scale of the STAXIGlucose•Hexokinase•Glucose-6-phosphate dehydrogenaseInsulin•Radioimmunoassay antibody | •Higher Anger Out/Hostility was associated with higher insulin in females (r = 0.23; p < 0.05)•Higher Anger Out/Hostility was associated with higher glucose (r = 0.27; p < 0.05) | Sex, obesity, lipid levels, CVD | |
| Vitaliano et al., 2002[41]Examine the association between caregiver anger and CHD over 27-30 months | Longitudinal | N = 72 (F = 48; M = 24)Spousal AD caregiversMean age = 70.4 y | Anger•AES•Trait Anger Scale of the STAXICHDDate and type of diagnosis, treatment, prognosis, and medication | •Anger was not associated with incidence of CHD (p > 0.05) | Medication, chronic stress, personal and social resources | |
| Vitaliano et al., 2005[42]Examine the association between caregiver hostility and cognitive decline over 24 months | Longitudinal | N = 96 (F = 58; M = 38)Spousal AD caregiversMean age = 72.2 y | Hostility•Abbreviated Cook-Medley Hostility ScaleCognitive function•Shipley Institute of Living Scale | •Higher hostility was associated with lower cognition (r = –0.16; p < 0.05) | Sex, ethnicity, education, income, medications, CVD, depression, anxiety, sleep quality | |
| Wilcox et al., 1999 [34]USA | Examine the association between caregiver anger and sleep complaints | Cross-sectional | N = 90 (F = 90; M = 0)Spousal and non-spousal dementia caregiversMean age = 62.8 y | Anger•AESSleep•PSQI | •Lower Anger In was associated with higher overall global PSQI scores (r = –0.24; p < 0.05)•Lower Anger In was associated with lower quality of sleep (r = –0.32; p < 0.05)•Lower Anger In was associated with lower sleep efficiency (r = –0.25; p < 0.05) | Age, education, self-rated health, hours caregiving, care recipient night-time disruptions, psychological distress, perceived burden |
All studies conducted by Vitaliano and Zhang used the same sample, as confirmed by the study author. CRP, C-reactive protein; IL-6, interleukin-6; F, female; M, male; BMI, body mass index; AUC, area under the curve; CAR, cortisol awakening response; ADL, Activities of daily living; STAXI-II, State-Trait Anger Expression Inventory – revised version; AD, Alzheimer’s disease; AES, Anger Expression Scale (AX); STAXI, State-Trait Anger Expression Inventory; PHA, phytohemagglutmin; ConA, concanavlin A; PW, pokeweed mitogen; BSI, Brief Symptom Inventory; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDLC, high-density lipoprotein cholesterol; LDLC, low-density lipoprotein cholesterol; TG, triglycerides; CVD, cardiovascular disease; CHD, coronary heart disease; PSQI, Pittsburgh Sleep Quality Index.
RESULTS
Search results
We identified a total of 4,644 references (see Fig. 1 for details of the search process), of which 77 were duplicates, with an additional 5 studies identified from other sources. A total of 4,551 articles were screened by title and abstracts, of which 4,530 were excluded as not relevant, leaving 20 studies to be assessed for full text eligibility. Of these, eight studies were excluded with reasons (see Supplementary Table 2), leaving eight original studies meeting our inclusion criteria.
Table 2
Results of risk of bias ratings
| Study | Selection | Confounders | Outcome and results | Overall quality | ||||
| (1) | (2) | (3) | (1) | (1) | (2) | (3) | ||
| Graham et al., 2006 [35] | b | a | a | a | A | a | b | Good |
| Leggett et al., 2015 [31] | b | b | a | a | a | N/A | b | Fair |
| Liu et al., 2015 [32] | b | b | b | a | a | N/A | b | Poor |
| Lopez et al., 2015 [33] | b | a | a | c | a | N/A | a | Poor |
| Scanlan et al., 2001 [36] | b | a | a | a | a | a | a | Good |
| Shaw et al., 2003 [37] | b | a | a | a | a | a | b | Good |
| Vitaliano et al., 1995 [38] | b | a | a | a | a | a | a | Good |
| Wilcox et al., 1999 [34] | b | a | a | a | a | N/A | b | Fair |
Characteristics of included studies
Characteristics of included studies are presented in Table 1. There were four cross-sectional studies [31–34], and four longitudinal studies [35–38], reporting on a total of 937 participants; two studies [37, 38] reported both cross-sectional and longitudinal data. One study reported data based on the same sample across five published articles [38–42], with each examining a different physiological marker and its association with caregiver anger and/or hostility. Follow-up duration for the longitudinal studies varied from 15 to 84 months.
Participants
Across studies, family caregivers were recruited primarily from community settings via mass mailings, with sample sizes ranging from 82 to 173. Most caregivers were female, and the primary caregiver of the care recipient. Mean caregiver age was 65.8 years, with half of the studies recruiting spousal caregivers and the remaining half both spousal and non-spousal caregivers.
Outcome measures of anger and hostility
The most common measure used to assess anger was the Anger Expression Scale (AX) [43], followed by the State-Trait Anger Expression Inventory (STAXI) [18], and the State-Trait Anger Expression Inventory – revised version (STAXI-II) [44]. Two studies measured hostility using the Cook-Medley Hostility Scale [45], and a further two studies used items from the Kessler Psychological Distress K10 and K6 scales [46]. One study measured hostility using the Brief Symptoms Inventory (BSI) [47].
Main results
Caregiver anger, weight gain, and insulin and glucose levels
In one longitudinal study [39], higher anger control was associated with higher weight gain at 15–18 months in female caregivers (β= 1.13, p < 0.001), whereas follow-up data of the same sample [40], showed higher anger-out being associated with higher levels of glucose dysregulation (r = 0.27; p < 0.05) at long-term follow-up (15–18 months), and higher insulin over time but only in female caregivers (r = 0.23; p < 0.05).
Caregiver anger and plasma lipids
One cross-sectional study [38] examining the association between caregiver anger and plasma lipids found that higher anger-in was associated with higher high-density lipoprotein cholesterol (HDLC) levels (β= 0.12, p < 0.05), but lower triglycerides (TG) (β= –0.26, p < 0.001). In the same study, higher anger-control predicted lower HDLC (β= –0.16, p < 0.01), whereas higher anger-out was associated with lower low-density lipoprotein cholesterol (LDLC); an effect which was observed only in female caregivers (β= –0.55, p < 0.05).
Caregiver anger, daily cortisol levels, and lymphocyte proliferation
In the cross-sectional study by Leggett et al. (2015) [31] higher levels of daily fluctuations of anger were associated with lower area under the curve (AUC) cortisol (β= –0.00, p < 0.05), but not with overall cortisol awakening response (CAR) (p > 0.05). In the longitudinal study by Scanlan et al. (2001) [36], higher anger-out/anger control predicted lower phytohemagglutinin (PHA) (r = –0.26, p < 0.01), concanavalin A (ConA) (r = –0.19, p < 0.05), and pokeweed (PW) (r = –0.23, p < 0.01) at long-term follow-up (15–18 months).
Caregiver anger and prevalence of CHD
One study investigated the longitudinal association between caregiver anger and future risk of coronary heart disease (CHD) [41]; this study reported no significant association between caregiver anger and risk of CHD over a 27 to 30 month period (p > 0.05).
Caregiver anger, sleep quality, and overall vitality levels
Two studies examined the cross-sectional association between caregiver anger and sleep quality. Liu et al. (2015) [32] found that higher anger reported by caregivers predicted lower quality of sleep (β= –0.21, p < 0.001). Wilcox and King (1999) [34] reported that lower levels of anger-in were associated with higher sleep disturbances overall (r = –0.24; p < 0.05), and both lower sleep quality (r = –0.32; p < 0.05), and sleep efficiency (r = –0.25; p < 0.05). One study investigated the association between vitality levels and caregiver anger [33]; increased anger-reaction by caregivers was cross-sectionally associated with lower vitality levels (β= –0.32; p < 0.001).
Caregiver hostility, inflammation, and bodily pain
In the study by Graham et al. (2006) [35] higher hostility was associated with higher levels of C-reactive protein (CRP) (r = 0.18, p < 0.05), and self-reported bodily pain (r = 0.25, p < 0.01) over a period of 7 years, but no association was found between hostility and serum IL-6 levels.
Caregiver hostility, hypertension risk, and cognitive decline
In the longitudinal study by Shaw et al. (2003) [37] hostility was not associated with increased risk of hypertension, which was measured by both systolic (p < 0.63), and diastolic blood pressure levels (p < 0.68) at 84 months. Vitaliano et al. (2005) [42] examined the longitudinal association between caregiver hostility and risk of cognitive decline and found that higher hostility levels in caregivers were associated with increased risk of cognitive decline over time (r = –0.16, p < 0.05) (2-year follow-up).
Risk of bias and quality of studies
Quality ratings of the included studies are summarized in Table 2. Most studies were rated as having low risk of bias on the domains of measurement of outcome, and assessment of physiological markers. The majority of studies reported controlling for several confounders, and adequate follow-up rates and/or accounting for loss to follow up (longitudinal studies). Two studies were rated as being of poor quality [32, 33], due to not using well-validated scales to measure anger and sleep [32], or not including a control group [33].
DISCUSSION
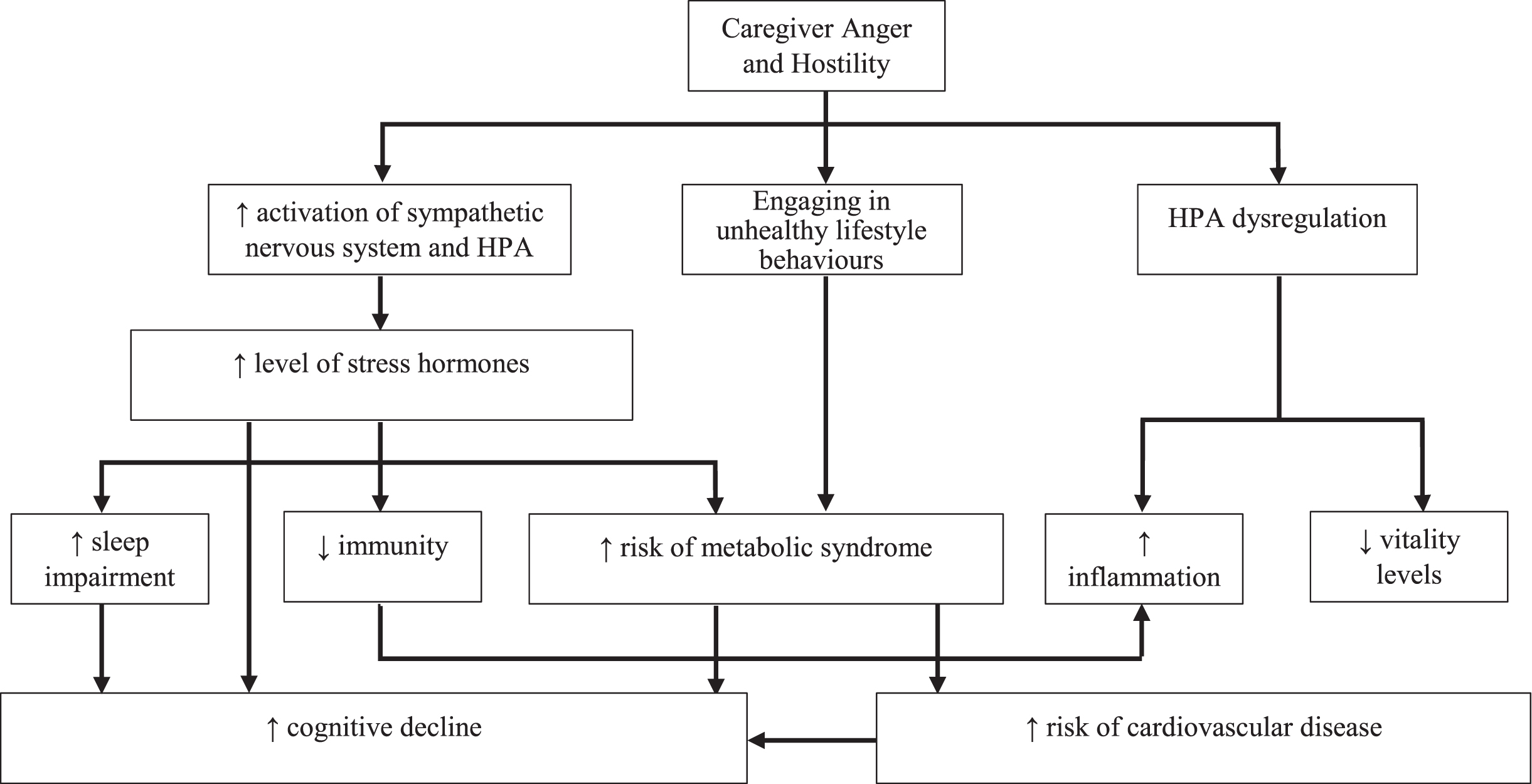
To our knowledge, this is the first systematic review examining the effects of anger and hostility on dementia caregivers’ physical health. The results of our review are important as they provide the first systematic synthesis of the evidence on how anger and hostility influence health outcomes in dementia caregivers. Overall, our results are consistent with evidence in the general population that both anger and hostility increase risk of poor health outcomes by triggering stress-induced physiological processes [16, 25]. An important contribution of our review is the finding that both caregiver anger and caregiver hostility increased risk of poor outcomes across several clinical markers of ill health [24]. Similarly to studies conducted in non-caregiving populations, we found that different anger dimensions and their biobehavioral sequelae contribute differently in increasing risk of poor health [27]. Figure 2 provides an overview of how caregiver anger and hostility may affect health outcomes in the context of dementia caregiving as informed by the current evidence.
Fig. 2
Mechanisms of caregiver anger and hostility and their link to physical illness in dementia caregivers. HPA, hypothalamic–pituitary–adrenal axis.
Summary of main findings
Caregiver anger, weight gain, and insulin and glucose levels
In one longitudinal study, higher levels of anger control in female caregivers were associated with higher weight gain over 18 months [39]. These results indicate that female caregivers engaging in anger control may be more vulnerable to increases in weight gain over time, which may in turn heighten risk of health conditions such as obesity, diabetes, and heart disease [48]. Anger may also predispose family caregivers to unhealthy lifestyle behaviors such as over-eating, and being physically inactive, which may further heighten risk of chronic health conditions. Given the limited evidence base future studies will be key in identifying which specific physiological and behavioral changes triggered by anger increase weight gain in caregivers, and whether these changes increase risk for other chronic conditions long-term [49].
In the study by Vitaliano et al. (1996) [40] higher levels of anger expression increased risk of glucose dysregulation over time. Caregivers reporting higher anger were more likely to have higher levels of glucose at long-term follow-up, and higher anger expression in female caregivers predicted higher insulin long-term. These results are important as they demonstrate that caregiver anger is longitudinally associated with several clinical indicators of glycemic control, an effect that may differ by caregiver sex. Anger expression may lead to excessive glucocorticoids, leading to dysregulation of specific neuroendocrine pathways, which may in turn place dementia caregivers at greater risk of developing chronic health conditions associated with glucose dysregulation such as diabetes [23, 50].
Caregiver anger and plasma lipid levels
In the cross-sectional study by Vitaliano et al. (1995) [38] anger was associated with higher lipid profile dysregulation, with higher anger control predicting lower HDLC which increases risk of coronary heart disease [51]. On the contrary, high anger-in and high anger-out scores were found to be protective; high anger-in scores were associated with high HDLC and low TG levels, and high anger-out with lower LDLC levels only in female caregivers. Although preliminary these data suggest that anger-in and anger-out may be more effective emotion regulation strategies by preventing chronic emotional arousal compared to anger-control, which requires to continuously monitor anger responses. Given the cross-sectional nature of these findings, future longitudinal studies are needed to estimate the positive, neutral, or negative influence of the different anger dimensions on profile lipid dysregulation and cardiovascular outcomes [52], and how these effects are influenced by caregiver gender.
Caregiver anger, daily cortisol levels, and lymphocyte proliferation
Although prior research has associated higher anger with both diminished and elevated cortisol responsiveness, data from one cross-sectional study identified in our review lend support for overall diminished cortisol levels in the context of anger expression in dementia caregivers [31]. Continued exposure to prolonged stress associated with caregiving may create a counter-regulatory response, resulting in below normal levels of cortisol long-term [53]. Although these findings do suggest that it will be important to introduce biological indicators such as cortisol levels in future health promotion programs, large-scale prospective cohort studies are necessary to examine how caregiver anger influences daily cortisol levels over long periods of time.
We found one study examining the longitudinal association between anger expression and regulation of immune responses. As predicted, higher anger expression reported by caregivers was associated with lower levels of lymphocyte proliferation over 18 months across several immune markers [36]. These findings are important as they suggest that higher anger expression directly contributes towards a decline in various cytokines, weakening caregivers’ immune responses, and increasing susceptibility to disease [54, 55].
Caregiver anger and prevalence of CVD
Despite evidence that anger expression generally increases risk of CHD, data from one study [41] found no association between caregiver anger and increased prevalence of CHD over 30 months. It is highly likely that the biological mechanisms through which anger increases risk of CHD are complex [24], and establishing whether anger and hostility do influence CHD risk in dementia caregivers, requires carefully designed etiological studies identifying which specific physiological and behavioral covariates may moderate this association.
Caregiver anger, sleep quality, and overall vitality levels
Data from two cross-sectional studies [32, 34] showed that caregiver anger was consistently associated with overall sleep quality. Higher levels of anger were associated with higher sleep disturbances, with one study reporting that lower anger suppression in particular predicted worse sleep outcomes [34]. Although these findings need to be replicated using longitudinal data, they are in line with large-scale epidemiological studies showing that sleep disturbances are consistently associated with increased anger and hostility [56]. Understanding how anger expression influences sleep quality may lead to useful preventative interventions that can limit the impact of sleep disturbances on caregivers’ physical health and the ability to cope with the demands of the caregiving role [57].
In one cross-sectional study trait anger was associated with lower levels of vitality in caregivers [33]. Despite being preliminary these findings highlight that anger regulation skills may potentially influence caregivers’ ability to manage every-day caregiving duties, and that similarly to non-caregiver populations the ability to control anger impacts on caregivers’ health-related quality of life and general well-being [58].
Caregiver hostility, inflammation, and bodily pain
Data from one longitudinal study [35], showed that higher hostility was associated with higher levels of proinflammatory biomarkers such as CRP long-term. In the same study high levels of hostility were also associated with higher levels of self-reported pain over time. These findings have important clinical implications as they suggest that higher hostility may increase disinhibition of inflammatory responses, predisposing caregivers to increased risk of cardiovascular disease [59, 60], and negatively affect caregivers’ health-related quality of life by increasing bodily pain over time [61].
Caregiver hostility, hypertension risk, and cognitive decline
Contrary to previous longitudinal studies where hostility increases risk of hypertension [62], the longitudinal study by Shaw et al. (2003) [37] found no association between caregiver hostility and both systolic and diastolic arterial blood pressure. As this is the only study in the literature to test for this association, it is important that future large-scale studies are conducted to examine whether hostility influences hypertension control and blood pressure burden. An important finding of our review is that higher caregiver hostility was associated with increased risk of cognitive decline over time [42]. Although preliminary these findings suggest that routine screening for anger and hostility is important for both physical and cognitive health in dementia caregivers. Future work will be key in terms of understanding how individual differences in expression of hostility may predict changes in cognitive impairment over time [63], and how cardiovascular, neuroendocrine, and inflammatory responses associated with hostility and anger, influence both physical and cognitive health [64, 65].
Implications
Our findings have important clinical implications. The consistent harmful effect of anger and hostility for several outcomes suggests that interventions supporting caregivers to manage high levels of anger will be protective long-term [8]. Given the consistent effects of both anger and hostility on caregivers’ physical health, routine screening, and the provision of support to manage anger may prevent or reduce risk of chronic disease [10]. Raising awareness about anger and hostility and its effects on caregivers’ physical health will be key in reducing the stigma associated with its recognition and management. Incorporating anger management in caregiver education may not only promote good physical health and prevent illness, but may additionally decrease carer psychological distress [8]. For example, anger management psychoeducation may increase positive coping skills for caregivers supporting them to cope better with the caregiving role, by preventing high levels of distress and anger when dealing with caregiving duties.
Limitations and directions for future research
Despite the originality of our review, there are several important limitations. The overall small number of studies identified, limits the conclusion of our review and our confidence in the results. Due to the heterogeneity of physiological markers tested, it was not possible to quantify the effect of anger and hostility on caregivers’ physical health. As a result, we were only able to describe and synthesize results narratively, which is an important limitation of our review. Most of the included studies were conducted in the US, which means our results may not be widely applicable to the wider population of caregivers. The majority of studies recruited family caregivers who were healthy at baseline which limits the generalization of our findings. The average length of duration of care was 4.9 years, so the results of our review may not be applicable to caregivers new to the caregiving role or those caring for longer periods of time. Although some of the studies meeting our inclusion criteria controlled for several caregiving variables such as duration and hours spent caregiving, and levels of perceived burden, none of the studies examined the role of the caregiving relationship, which may be an important mediator of the expression of anger on caregivers’ physical health.
Our review highlights that future studies are needed to examine the effect of several important mediators on the association between anger and caregivers’ physical health such as age, sex, patient-specific factors and interpersonal variables [66]. Despite the growth of research in the area large-scale prospective population-based studies will be important in understanding how anger and hostility may influence both caregiver and patient outcomes. These studies may help identify the specific physiological and behavioral mechanisms that mediate the relationship between caregiver anger and vulnerability to disease and apply this knowledge to inform future interventions. Given the limited knowledge of the psychometric performance of anger questionnaires for caregivers, additional studies are needed to examine the validity and reliability of both anger and hostility measures in the context of dementia caregiving.
Conclusions
To our knowledge this is the first systematic review synthesizing current evidence on the association between anger, hostility, and physical health outcomes in dementia caregivers. Our findings are important as they demonstrate that both anger and hostility increase caregivers’ vulnerability to poor health outcomes. Caregiver anger and caregiver hostility influence a variety of biological and clinical health indicators, such as weight gain, glucose dysregulation, immunity, higher cellular inflammatory levels as well vulnerability to cognitive decline over time. Further larger-scale longitudinal studies are needed to replicate these findings and increase our understanding of the key mechanisms through which anger and hostility increase disease vulnerability in dementia caregivers.
FUNDING
This review did not receive any specific funding. Vasiliki Orgeta is supported by the UCLH BRC (Biomedical Research Centre).
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
ACKNOWLEDGMENTS
The authors have no acknowledgments to report.
SUPPLEMENTARY MATERIAL
[1] The supplementary material is available in the electronic version of this article: http://dx.doi.org/10.3233/ADR-220040
References
[1] | Livingston G , Huntley J , Sommerlad A , Ames D , Ballard C , Banerjee S , Brayne C , Burns A , Cohen-Mansfield J , Cooper C , Costafreda SG , Dias A , Fox N , Gitlin LN , Howard R , Kales HC , Kivimaki M , Larson EB , Ogunniyi A , Orgeta V , Ritchie K , Rockwood K , Sampson EL , Samus Q , Schneider LS , Selbaek G , Teri L , Mukadam N ((2020) ) Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396: :413–446. |
[2] | Jutkowitz E , Kane RL , Gaugler JE , MacLehose RF , Dowd B , Kuntz KM ((2017) ) Societal and family lifetime cost of dementia: Implications for policy. J Am Geriatr Soc 65: :2169–2175. |
[3] | Kumar A , Rinwa P , Kaur G , Machawal L ((2013) ) Stress: Neurobiology, consequences and management. J Pharm Bioallied Sci 5: :91–97. |
[4] | Mausbach BT , Patterson TL , Rabinowitz YG , Grant I , Schulz R ((2007) ) Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychol 26: :539–544. |
[5] | Pinquart M , Sorensen S ((2003) ) Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol Aging 18: :250–267. |
[6] | Mahoney R , Regan C , Katona C , Livingston G ((2005) ) Anxiety and depression in family caregivers of people with Alzheimer disease: The LASER-AD study. Am J Geriatr Psychiatry 13: :795–801. |
[7] | Williamson GM , Shaffer DR ((2001) ) Relationship quality and potentially harmful behaviors by spousal caregivers: How we were then, how we are now. The Family Relationships in Late Life Project. Psychol Aging 16: :217–226. |
[8] | Coon DW , Thompson L , Steffen A , Sorocco K , Gallagher-Thompson D ((2003) ) Anger and depression management: Psychoeducational skill training interventions for women caregivers of a relative with dementia. Gerontologist 43: :678–689. |
[9] | Kramer B , Gibson J , Teri L. ((1993) ) Interpersonal family stress in Alzheimer’s disease. Perceptions of patients and caregivers. Clin Gerontol 12: :57–75. |
[10] | Gallagher-Thompson D , DeVries HM ((1994) ) “Coping with frustration” classes: Development and preliminary outcomes with women who care for relatives with dementia. Gerontologist 34: :548–552. |
[11] | Lilly M , Beckstrand J ((2011) ) Anger by any other name: Sampling the domain. Internet J Ment Health 7: . |
[12] | Vitaliano PP , Young HM , Russo J , Romano J , Maganaamato A ((1993) ) Does expressed emotion in spouses predict subsequent problems among care recipients with Alzheimer’s disease. J Gerontol 48: :P202𠄓P209. |
[13] | del-Pino-Casado R , Cardosa MR , Lopez-Martinez C , Orgeta V ((2019) ) The association between subjective caregiver burden and depressive symptoms in carers of older relatives: A systematic review and meta-analysis. PLoS One 14: :e0217648. |
[14] | del-Pino-Casado R , Priego-Cubero E , Lopez-Martinez C , Orgeta V ((2021) ) Subjective caregiver burden and anxiety in informal caregivers: A systematic review and meta-analysis. PLoS One 16: :e0247143. |
[15] | Gallagher-Thompson D , Wang PC , Liu W , Cheung V , Peng R , China D , Thompson LW ((2010) ) Effectiveness of a psychoeducational skill training DVD program to reduce stress in Chinese American dementia caregivers: Results of a preliminary study. Aging Ment Health 14: :263–273. |
[16] | Trudel-Fitzgerald C , Reduron LR , Kawachi I , Kubzansky LD ((2021) ) Specificity in associations of anger frequency and expression with different causes of mortality over 20 years. Psychosom Med 83: :402–409. |
[17] | Yamaguchi A , Kim MS , Oshio A , Akutsu S ((2017) ) The role of anger regulation on perceived stress status and physical health. Pers Individ Differ 116: :240–245. |
[18] | Spielberger CD , Jacobs G , Russell S , Crane RS ((1983) ) Assessment of anger: The state-trait anger scale. In Advances in Personality Assessment, Butcher JN, Spielberger CD, eds. Erlbaum, Hillsdale, NJ, pp. 159–187. |
[19] | Spielberger CD , Reheiser EC ((2010) ) The nature and measurement of anger. In International Handbook of Anger: Constituent and concomitant biological, psychological, and social processes, Potegal M, Stemmler G, Spielberger C, eds. Springer New York, New York, pp. 403–412. |
[20] | Bridewell WB , Chang EC ((1997) ) Distinguishing between anxiety, depression, and hostility: Relations to anger-in, anger-out, and anger control. Pers Individ Differ 22: :587–590. |
[21] | Deffenbacher JL , Oetting ER , Thwaites GA , Lynch RS , Baker DA , Stark RS , Thacker S , EiswerthCox L ((1996) ) State-trait anger theory and the utility of the trait anger scale. J Couns Psychol 43: :131–148. |
[22] | Fernandez E ((2013) ) Anger dysfunction and its treatment. In Treatments for Anger in SpecificPopulations: Theory, Application, and Outcome, Fernandez E, ed. Oxford University Press, New York, pp. 1–14. |
[23] | Staicu ML , Cutov M ((2010) ) Anger and health risk behaviors. J Med Life 3: :372–375. |
[24] | Chida Y , Steptoe A ((2009) ) The association of anger and hostility with future coronary heart disease: A meta-analytic review of prospective evidence. J Am Coll Cardiol 53: :936–946. |
[25] | Steptoe A , Marmot M ((2003) ) Burden of psychosocial adversity and vulnerability in middle age: Associations with biobehavioral risk factors and quality of life. Psychosom Med 65: :1029–1037. |
[26] | Golden SH , Williams JE , Ford DE , Yeh HC , Sanford CP , Nieto FJ , Brancati FL ((2006) ) Anger temperament is modestly associated with the risk of type 2 diabetes mellitus: The atheroslcerosis risk in communities study. Psychoneuroendocrinology 31: :325–332. |
[27] | Schum JL , Jorgensen RS , Verhaeghen P , Sauro M , Thibodeau R ((2003) ) Trait anger, anger expression, and ambulatory blood pressure: A meta-analytic review. J Behav Med 26: :395–415. |
[28] | Revesz D , Verhoeven JE , Milaneschi Y , de Geus EJ , Wolkowitz OM , Penninx BW ((2014) ) Dysregulated physiological stress systems and accelerated cellular aging. Neurobiol Aging 35: :1422–1430. |
[29] | Boyle MH ((1998) ) Guidelines for evaluating prevalence studies. EBMH 1: :37–39. |
[30] | Viswanathan M , Berkman ND , Dryden DM , Hartling L ((2013) ) Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item Bank, Rockville (MD). |
[31] | Leggett AN , Zarit SH , Kim K , Almeida DM , Klein LC ((2015) ) Depressive mood, anger, and daily cortisol of caregivers on high- and low-stress days. J Gerontol B Psychol Sci Soc Sci 70: :820–829. |
[32] | Liu Y , Kim K , Almeida DM , Zarit SH ((2015) ) Daily fluctuation in negative affect for family caregivers of individuals with dementia. Health Psychol 34: :729–740. |
[33] | Lopez J , Romero-Moreno R , Marquez-Gonzalez M , Losada A ((2015) ) Anger and health in dementia caregivers: Exploring the mediation effect of optimism. Stress Health 31: :158–165. |
[34] | Wilcox S , King AC ((1999) ) Sleep complaints in older women who are family caregivers. J Gerontol B Psychol Sci Soc Sci 54: :P189–198. |
[35] | Graham JE , Robles TF , Kiecolt-Glaser JK , Malarkey WB , Bissell MG , Glaser R ((2006) ) Hostility and pain are related to inflammation in older adults. Brain Behav Immun 20: :389–400. |
[36] | Scanlan JM , Vitaliano PP , Zhang JP , Savage M , Ochs HD ((2001) ) Lymphocyte proliferation is associated with gender, caregiving, and psychosocial variables in older adults. J Behav Med 24: :537–559. |
[37] | Shaw WS , Patterson TL , Semple SJ , Dimsdale JE , Ziegler MG , Grant I ((2003) ) Emotional expressiveness, hostility and blood pressure in a longitudinal cohort of Alzheimer caregivers. J Psychosom Res 54: :293–302. |
[38] | Vitaliano PP , Russo J , Niaura R ((1995) ) Plasma-lipids and their relationships with psychosocial factors in older adults. J Gerontol B Psychol Sci Soc Sci 50: :P18–P24. |
[39] | Vitaliano PP , Russo J , Scanlan JM , Greeno CG ((1996) ) Weight changes in caregivers of Alzheimer’s care recipients: Psychobehavioral predictors. Psychol Aging 11: :155–163. |
[40] | Vitaliano PP , Scanlan JM , Krenz C , Fujimoto W ((1996) ) Insulin and glucose: Relationships with hassles, anger, and hostility in nondiabetic older adults. Psychosom Med 58: :489–499. |
[41] | Vitaliano PP , Scanlan JM , Zhang JP , Savage MV , Hirsch IB , Siegler IC ((2002) ) A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom Med 64: :418–435. |
[42] | Vitaliano PP , Echeverria D , Yi J , Phillips PE , Young H , Siegler IC ((2005) ) Psychophysiological mediators of caregiver stress and differential cognitive decline. Psychol Aging 20: :402–411. |
[43] | Spielberger CD , Johnson EH , Jacobs GA , Worden TJ ((1985) ) The experience and expression of anger: Construction and validation of an anger expression scale. In Anger and Hostility in Cardiovascular and Behavioural Disorders, Chesney MA, Rosenman RH, eds. Hemisphere, New York, pp. 5–30. |
[44] | Spielberger CD ((1988) ) Manual for the State-Trait Anger Expression Scale, Psychological Assessment Resources, Inc, Odessa, FL. |
[45] | Cook WW , Medley DM ((1954) ) Proposed hostility and pharisaic - virtue scales for the MMPI. J Appl Psychol 38: :414–418. |
[46] | Kessler RC , Andrews G , Colpe LJ , Hiripi E , Mroczek DK , Normand SLT , Walters EE , Zaslavsky AM ((2002) ) Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 32: :959–976. |
[47] | Derogatis LR , Melisaratos N ((1983) ) The Brief Symptom Inventory – an introductory report. Psychol Med 13: :595–605. |
[48] | Biener A , Cawley J , Meyerhoefer C ((2017) ) The high and rising costs of obesity to the US health care system. J Gen Intern Med 32: :6–8. |
[49] | Al-Goblan AS , Al-Alfi MA , Khan MZ ((2014) ) Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes 7: :587–591. |
[50] | Tsenkova VK , Carr D , Coe CL , Ryff CD ((2014) ) Anger, adiposity, and glucose control in nondiabetic adults: Findings from MIDUS II. J Behav Med 37: :37–46. |
[51] | Barter P , Gotto AM , LaRosa JC , Maroni J , Szarek M , Grundy SM , Kastelein JJP , Bittner V , Fruchart JC , Treating to New Targets Investigators ((2007) ) HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med 357: :1301–1310. |
[52] | Emerging Risk Factors C , Di Angelantonio E , Sarwar N , Perry P , Kaptoge S , Ray KK , Thompson A , Wood AM , Lewington S , Sattar N , Packard CJ , Collins R , Thompson SG , Danesh J ((2009) ) Major lipids, apolipoproteins, and risk of vascular disease. JAMA 302: :1993–2000. |
[53] | Herriot H , Wrosch C , Hamm JM , Pruessner JC ((2020) ) Stress-related trajectories of diurnal cortisol in older adulthood over 12 years. Psychoneuroendocrinology 121: :104826. |
[54] | Segerstrom SC , Miller GE ((2004) ) Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychol Bull 130: :601–630. |
[55] | D’Acquisto F ((2017) ) Affective immunology: Where emotions and the immune response converge. Dialogues Clin Neurosci 19: :9–19. |
[56] | Van Veen MM , Lancel M , Beijer E , Remmelzwaal S , Rutters F ((2021) ) The association of sleep quality and aggression: A systematic review and meta-analysis of observational studies. Sleep Med Rev 59: :101500. |
[57] | Hirotsu C , Tufik S , Andersen ML ((2015) ) Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci 8: :143–152. |
[58] | Julkunen J , Ahlstrom R ((2006) ) Hostility, anger, and sense of coherence as predictors of health-related quality of life. Results of an ASCOT substudy. J Psychosom Res 61: :33–39. |
[59] | Fries E , Hesse J , Hellhammer J , Hellhammer DH ((2005) ) A new view on hypocortisolism. Psychoneuroendocrinology 30: :1010–1016. |
[60] | Suarez EC ((2004) ) C-reactive protein is associated with psychological risk factors of cardiovascular disease in apparently healthy adults. Psychosom Med 66: :684–691. |
[61] | Fernandez E , Turk DC ((1995) ) The scope and significance of anger in the experience of chronic pain. Pain 61: :165–175. |
[62] | Helmers KF , Baker B , O’Kelly B , Tobe S ((2000) ) Anger expression, gender, and ambulatory blood pressure in mild, unmedicated adults with hypertension. Ann Behav Med 22: :60–64. |
[63] | Toussaint LL , Shields GS , Green E , Kennedy K , Travers S , Slavich GM ((2018) ) Hostility, forgiveness, and cognitive impairment over 10 years in a national sample of American adults. Health Psychol 37: :1102–1106. |
[64] | Lucassen PJ , Pruessner J , Sousa N , Almeida OFX , Van Dam AM , Rajkowska G , Swaab DF , Czeh B ((2014) ) Neuropathology of stress. Acta Neuropathol 127: :109–135. |
[65] | Smith TW , Glazer K , Ruiz JM , Gallo LC ((2004) ) Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. J Pers 72: :1217–1270. |
[66] | Phillips LH , Henry JD , Hosie JA , Milne AB ((2006) ) Age, anger regulation and well-being. Aging Ment Health 10: :250–256. |




