Depression Mediates the Association Between Occupational Complexity and Late-Life Cognition in Hispanics
Abstract
There is a dearth of research in Latin America regarding risk and protective factors affecting older adults’ cognition. This study aimed to investigate the factors mediating the association between occupational complexity and late-life cognition and daily function in a sample of Hispanic older adults. Participants (n = 588) aged 65 years and older underwent clinical, functional, and cognitive assessments. Mediation analyses revealed that depressive symptoms mediated the relationship between occupational complexity and cognitive as well as functional outcomes. Results provide evidence that depression may act as a risk factor for worse outcomes, even if older adults had a cognitively demanding occupation.
INTRODUCTION
The increase in life expectancy in all regions of the world has focused attention on environmental, behavioral, and genetic variables that may influence late-life cognition [1]. For example, education has been associated with better cognitive functioning in older adults, later onset of cognitive decline, and greater cognitive reserve [1–5]. Higher education in early adulthood is correlated with not only better cognitive performance in late-life, but also greater access to jobs with greater occupational complexity [3]. Likewise, occupational complexity, a measure that captures particular skills that may reflect specific cognitive processes needed to perform job occupations, is associated with years of education and has been found to be a predictor of late-life cognition in studies conducted in developed countries [5–8]. A recent meta-analysis explored the relationship between occupational complexity and cognitive decline in late life across 43 studies, including 31 cohort studies, in several global regions [8]. However, to our knowledge, few studies conducted with Hispanic populations, or in Latin American countries, have examined the influence of occupational complexity on late-life cognitive function [3, 8].
In the Latin America and Caribbean region, the number of individuals older than 60 years of age is expected to triple and reach 144.6 million by 2050 [9]. In Panama, adults aged 60 and over accounted for 12.4% of the national population in 2020, a proportion expected to increase to 24% by 2050 [10, 11]. In our ongoing cohort study of older adults, the Panama Aging Research Initiative [12], we have begun to explore various factors associated with cognitive health in later life, including educational level, depressive symptoms [13], inflammatory markers [14], and genetic factors [15]. Notably, we have found that depression is closely associated with late-life cognition and function [13] and also with increased levels of inflammatory markers [14]. Depressive symptoms have been shown to be determinants in late-life cognition in numerous studies with older adults [16, 17]. Thus, in the present study we examined the potential mediating effect of depressive symptoms in the relationship between job complexity and cognitive function in Panamanian older adults.
MATERIALS AND METHODS
Participants
Data for this study came from the Panama Aging Research Initiative (PARI), an ongoing longitudinal study of Panamanian aging [12]. To date, PARI has collected data from two cohorts, with a total of 892 participants who completed a baseline assessment. The PARI protocol for the first cohort has been described in detail elsewhere [12]. In the second cohort, inclusion criteria were the same with the exception that the minimum enrollment age was 60 years. Exclusion criteria for both cohorts included any physical or medical condition that required hospitalization or institutionalization, or participation in an ongoing clinical study at the time of enrollment. Study protocols were approved by the National Bioethics Committee of the Instituto Conmemorativo Gorgas de Estudios de la Salud and the Institutional Bioethics Committee of the Caja del Seguro Social. Participants provided written informed consent in accordance with the principles of the Declaration of Helsinki of 1975.
The present report consists of data from 588 participants who completed a baseline and cognitive assessment, responded to the question regarding lifetime occupation, were literate and dementia-free at baseline, and were at least 65 years of age. Data regarding occupation were recoded into one of four categories of increasing skill complexity, according to the International Standard Classification of Occupations-08 (ISCO-08) [18], ranging from 1 (lowest) to 4 (highest). ISCO-08 is a four-level hierarchically structured classification that provides a way to classify and aggregate occupational information. These classifications are based on job similarity in terms of the skill level and skill specialization required for the job. Two observers independently coded the occupational data according to the ISCO-08 guidelines [18], and an inter-reliability test was performed (88.6%).
Measures
At baseline, subjects underwent a physical exam and clinical interview, and responded to items regarding demographic and lifestyle factors, chronic conditions, and difficulties performing activities in daily living. Participants who were institutionalized and/or met the National Institute on Aging and the Alzheimer’s Association (NIA-AA) clinical criteria for all-cause dementia [19] were excluded from the analysis. Three measures were used to assess cognition. The 30-item Spanish version of the Mini-Mental State Examination (MMSE) was used to measure global cognition [20]. The Clock Drawing Test is a nonverbal screening tool that engages long-term attention, auditory processing, and motor programming; scores range from 0 to 10, with greater scores indicating better performance [21]. Executive function was measured by the Trail Making Test B (TMT B) [22], and due to the large number of participants unable to complete the test within the time limit (5 min), the test was scored as having completed the assessment or not within the time limit, irrespective of the number of errors.
Performance in instrumental (IADL) and basic (BADL) activities of daily living was evaluated through self-report [23, 24]. A ratio (range 0–1) of independence in BADL and IADL was calculated as the total number of items the participant was able to perform divided by the total number of items in each test, where higher values indicated greater independence. Depressive symptoms were assessed with the Spanish version of the Geriatric Depression Scale [25]. The instrument consists of yes/no items that are used to identify depressive symptoms in elderly individuals, and was applied by the investigator reading the items out loud and registering the participant’s responses. An index was created for the number of affirmative responses over the total number of items. With regard to occupation, participants were asked “What is your current or past profession/job?”, and responses were recorded by the interviewer who instructed participants to be as specific as possible. A composite occupational score (OCC score) was calculated for each participant by first computing the proportion of variance in global cognition (as measured by the MMSE) explained by years of education (R2 = 0.127) and ISCO-08 occupational rating (R2 = 0.051), and then summing the weighted products as follows: OCC score = (years of education * 0.127) + (occupational rating * 0.051).
Statistical analyses
Statistical analyses were conducted using IBM SPSS version 23. Descriptive statistics were used to summarize baseline characteristics for the sample and across the four levels of ISCO-08 occupational rating using Chi square or one-way ANOVA for categorical or continuous variables, respectively. Kruskal Wallis H test was performed to analyze outcome variables that were non-normally distributed.
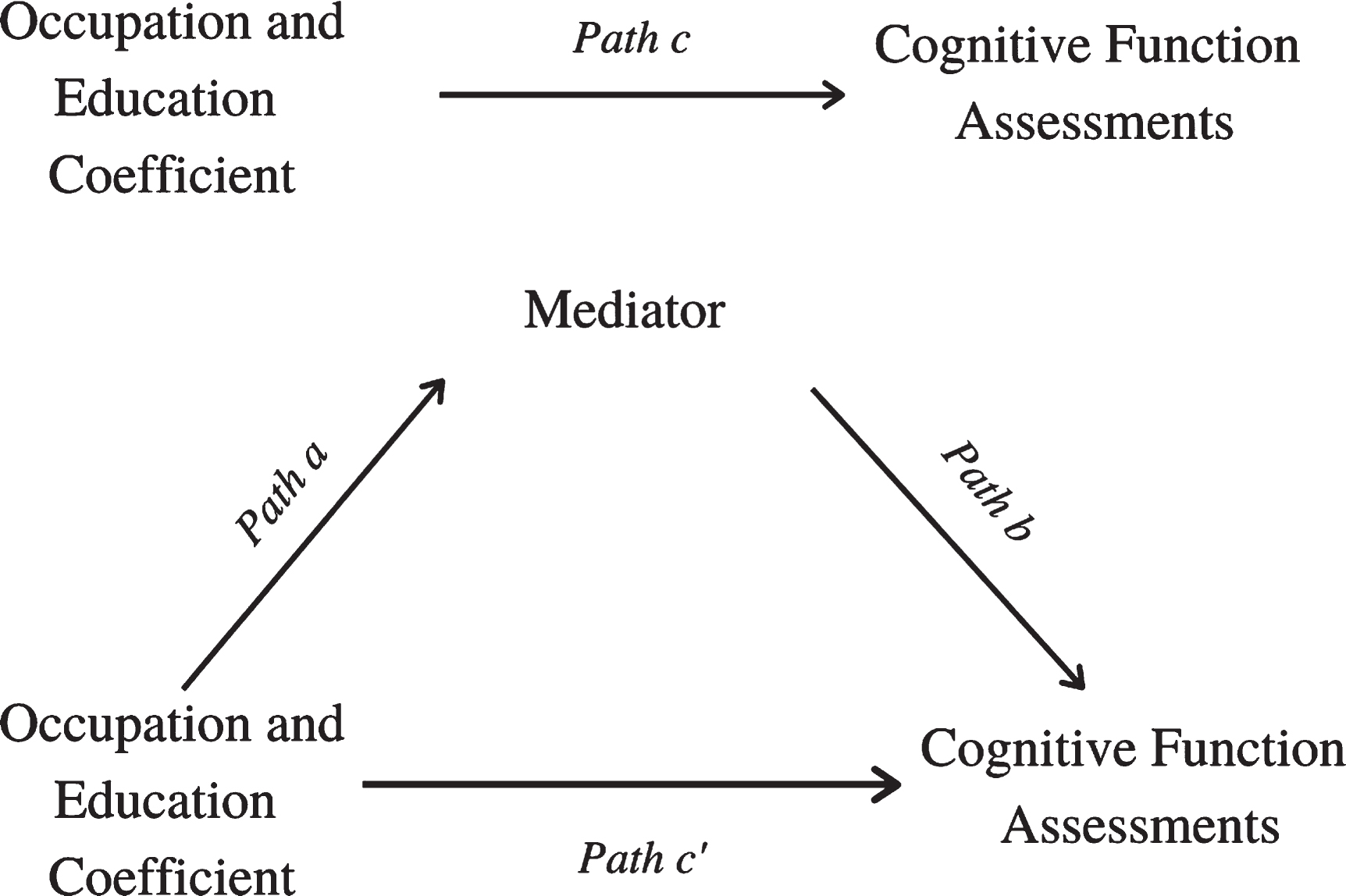
The mediation analyses examining the association between OCC score and cognitive and daily functioning was examined via nonparametric bootstrapping procedures using the SPSS macro PROCESS, suggested by Hayes [26], which does not make any assumption for normal distributions of the variables (model 4). PROCESS calculates the estimates of the direct, indirect, and total effects for the mediation model, with 95% confidence intervals based on 5000 bootstrapped sample, using a regression-based path analysis. Path coefficients (a, b, c, and c’) in the mediation model were obtained (see Fig. 1). Path a was estimated by regressing our predictor, the OCC score, and the covariates [age, sex, and the three most salient chronic diseases (i.e., hypertension, diabetes, and heart disease)], with the mediator. Path b shows the relationship between the mediator and outcome variables (cognitive/functional variables) while the predictor variable (OCC score) is controlled. Path c’, also called direct effect, indicates the association between the predictor and outcome variables excluding the mediator variable, while c-path, or total effect, shows the same association including the mediator variable. The mediation or indirect effect is indicated by a statistically significant difference between c and c’ (c-c’ = ab) and is significant with confidence intervals that do not include zero [27].
Fig. 1
Diagram of paths in the mediation models.
RESULTS
Table 1 summarizes participant characteristics for the sample and across levels of ISCO-08 occupational rating. Groups were as follows: least complex (level 1; n = 108 [18.4% ]), level 2 (n = 198 [33.7% ]), level 3 (n = 98 [16.7% ]), and most complex (level 4; n = 184 [31.3% ]). Participants were on average 74.9 years of age (SD = 7.1) with 12.2 years of education (SD = 5.7), and 69.4% were women. Kruskal-Wallis tests revealed significant differences across groups for all variables except marital status.
Table 1
Sample Characteristics (N = 588)
| Overall (N = 588) | Level 1 (n = 108) | Level 2 (n = 198) | Level 3 (n = 98) | Level 4 (n = 184) | ||
| n (%) / M(SD) | n (%) / M(SD) | n (%) / M(SD) | n (%) / M(SD) | n (%) / M(SD) | p | |
| Female Sex | 408 (69.4%) | 98 (24.0%) | 117 (28.7%) | 63 (15.4%) | 130 (31.9%) | 0.000** |
| Age | 74.9 (7.1) | 76.4 (6.8) | 76.3 (7.8) | 73.1 (6.1) | 73.4 (6.4) | 0.000** |
| Years of Education | 12.2 (5.7) | 6.6 (3.1) | 9.5 (4.4) | 14 (4.2) | 17.5 (3.5) | 0.000** |
| Marital Status | 0.408 | |||||
| Married/Partnered | 311 (52.9%) | 51 (47.2%) | 105 (53.0%) | 56 (57.1) | 99 (53.8%) | |
| Single/Widowed/Divorced | 279 (46.9%) | 57 (52.8%) | 92 (46.5) | 42 (42.9%) | 85 (46.2) | |
| Multimorbidity | 368 (62.2%) | 81 (22.0%) | 135 (36.7%) | 60 (16.3%) | 92 (25.0%) | 0.000** |
| MMSE | 26.7 (3.3) | 26 (4.3) | 26.8 (3.3) | 27.6 (2.3) | 27.5 (1.9) | 0.014* |
| TMTB Completed | 366 (62.2%) | 29 (7.9%) | 99 (27.1%) | 74 (20.2%) | 164 (44.8%) | 0.000** |
| Clock Test | 8.3 (2.3) | 7.2 (2.9) | 7.8 (2.7) | 8.9 (1.5) | 9.2 (1.3) | 0.000** |
| GDS Index | 0.1 (0.1) | 0.2 (0.2) | 0.2 (0.2) | 0.1 (0.2) | 0.1 (0.2) | 0.000** |
| BADL index | 0.8 (0.1) | 0.7 (0.3) | 0.7 (0.3) | 0.9 (0.2) | 0.9 (0.1) | 0.000** |
| IADL index | 0.8 (0.3) | 0.8 (0.2) | 0.8 (0.2) | 0.9 (0.1) | 0.9 (0.1) | 0.000** |
Significant at *p < 0.05 or **p < 0.001.
Table 2
Results of analyses identifying depression as a significant mediating factor in the relationship between occupational complexity and cognitive and functional measures
| Path a | Path b | Path c | Path c’ | Indirect Effect | Standardized Indirect Effect | |
| Mediation Analysis 1: Clock Test | ||||||
| β | –0.0656 | –1.2144 | 0.8982 | 0.9778 | 0.0796 | 0.0265 |
| LLCI | –0.085 | –2.1550 | 1.1368 | 1.2095 | 0.0061 | 0.0021 |
| ULCI | –0.0455 | –0.2737 | 0.3904 | 0.4250 | 0.1645 | 0.0545 |
| Mediation Analysis 2: TMT B* | ||||||
| β | –0.0669 | –1.7444 | 2.4272 | – | 0.1166 | – |
| LLCI | –0.0869 | –3.0695 | 1.9814 | – | 0.0297 | – |
| ULCI | –0.0468 | –0.4192 | 2.8730 | – | 0.2243 | – |
| Mediation Analysis 3: Lawton &Brody Index | ||||||
| β | –0.0669 | –0.1586 | 0.1034 | 0.1140 | 0.0106 | 0.0289 |
| LLCI | –0.0869 | –0.2674 | 0.0757 | 0.0871 | 0.0026 | 0.0070 |
| ULCI | –0.0468 | –0.0497 | 0.1311 | 0.1409 | 0.0203 | 0.0553 |
| Mediation Analysis 4: Katz Index | ||||||
| β | –0.0669 | –0.1821 | 0.0600 | 0.0722 | 0.0122 | 0.0585 |
| LLCI | –0.0869 | –0.2456 | 0.0438 | 0.0562 | 0.0064 | 0.0155 |
| ULCI | –0.0468 | –0.1185 | 0.0762 | 0.0882 | 0.0194 | 0.0304 |
The table summarizes the results of four mediation analyses. CI, confidence interval; LL, lower limit; UL, upper limit. *This model included a binary variable (i.e., completed/not completed) as its outcome variable.
Mediation analyses identified depression as a significant factor to consider when examining the relationship between OCC score and late-life cognition. Depressive symptoms significantly mediated the effect of the OCC score on the Clock Test (ab = 0.0796, 95% CI: [0.0061, 0.1645]), where more depressive symptoms were associated with worse executive function and accounted for 25% of the variance in the model (R2 = 0.25, p < 0.001). Likewise, depressive symptoms significantly mediated the effect of the OCC score on TMT B (ab = 0.1166, 95% CI: [0.0297, 0.2243]), indicating that participants with more depressive symptoms were less likely to complete the test. Depressive symptoms accounted for more than half (62%) of the variance in the total effect of the model (R2 = 0.62, p < 0.0001). Depressive symptoms also significantly mediated the effect of the OCC score on the IADL (ab = 0.0106, 95% CI: [0.0026, 0.0203]) and BADL index (ab = 0.0122, 95% CI: [0.0064, 0.0194]), where more depressive symptoms indicated greater limitations in BADL and IADL. Lastly, depressive symptoms accounted for 32% and 28% of the variance in the total effect of the IADL (R2 = 0.32, p < 0.0001) and BADL model (R2 = 0.28, p < 0.0001), respectively.
4DISCUSSION
The present study contributes to filling a gap in the studies that examine the association between occupational complexity and late-life functioning by adding evidence from Hispanic older adults in a developing country. Overall, findings were consistent with research in more developed countries, including the US [10], Sweden [7], Scotland [28], and Australia [29], and in line with the lifetime intellectual enrichment hypothesis [2] and the cognitive reserve theory [5, 6, 30]. Moreover, the present study shows that the association between OCC score and late life cognition is mediated by depression. Depression is one of the most common psychiatric disorders in older adults, with an estimated prevalence rate of major depression between 1% and 5% worldwide, and clinically significant depressive symptoms present in roughly 15% of community-dwelling older adults [16, 17]. Importantly, depression carries its own risks for chronic illness and disability, including cognitive deficits and progression from mild cognitive impairment to Alzheimer’s disease [13, 31, 32]. Our results, and others [33], suggest that depression may act as a risk factor for worse outcomes, even if older adults had an intellectually fulfilling life and a cognitively demanding occupation.
An important implication of the findings is the need for the timely identification of depression in older adults. A study conducted in six Latin American countries showed that 26.9% of older adults reported having depression [34]. Another study conducted in Bolivia reported a depression rate between 34.6% and 67.9% in older adults [35]. These results underscore the high burden of depression in the Latin American region and point to the need to assess its impact in developing countries [36].
This study had a number of limitations. First, the study may not be generalizable to adults living in rural settings because the sample was from the capital city of Panama. However, because urban settings in Latin America share many characteristics, our findings may provide insights into depression and cognitive health in older adults in the region. Second, the cross-sectional design limits the conclusions we can reach regarding changes in cognitive and functional outcomes over time. Among the study strengths was the large sample and use of various cognitive and functional assessments, which are among the most widely used in aging studies. To our knowledge, this study is the first to examine occupational complexity as a predictor of overall cognitive and daily function in older adults in Central America. Notably, the present study serves as a first step for national policies regarding older adults’ wellness as a matter of public health. Such policies should consider the importance of ensuring accessible psychological evaluations in primary care for the growing older adult population of Panama. Doing so will improve the mental health of older adults and reduce the burdens of aging populations common to less developed regions.
ACKNOWLEDGMENTS
We thank the administration and support staff of the Complejo Hospitalario Arnulfo Arias Madrid of Caja de Seguro Social for their assistance in carrying out the clinical cohort study.
FUNDING
This research was supported by the Melo Brain Project, Secretaría Nacional de Ciencia, Tecnología e Innvovación (SENACYT) of Panama, Universidad Católica Santa María la Antigua (SRUI-CPEI-ID-PSI-2013-2014-004 awarded to DCO and SRUI-CPEI-ID-PSI-2013-2014-02 awarded to GBB and), and Sistema Nacional de Investigación (SNI) of Panama (DO, MBC, AEV and GBB).
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
[1] | Deary IJ , Corley J , Gow AJ , Harris SE , Houlihan LM , Marioni RE , Penke L , Rafnsson SB , Starr JM ((2009) ) Age-associated cognitive decline. Br Med Bull 92: , 135–152. |
[2] | Vemuri P , Lesnick TG , Przybelski SA , Machulda M , Knopman DS , Mielke MM , Roberts RO , Geda YE , Rocca WA , Petersen RC , Jack CR ((2014) ) Association of lifetime intellectual enrichment with cognitive decline in the older population. JAMA Neurol 71: , 1017–1024. |
[3] | Zeki Al Hazzouri A , Haan MN , Osypuk T , Abdou C , Hinton L , Aiello AE ((2011) ) Neighborhood socioeconomic context and cognitive decline among older Mexican Americans: results from the Sacramento Area Latino Study on Aging. Am J Epidemiol 174: , 423–431. |
[4] | Feldberg C , Stefani D , Tartaglini MF , Hermida PD , García LM , Somale MV , Allegri R ((2020) ) The influence of education and occupational complexity in the cognitive performance of older adults with mild cognitive impairment. Ciencias Psicológicasgicas 14: , e–2194. |
[5] | Stern Y ((2002) ) What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc 8: , 448–460. |
[6] | Stern Y ((2009) ) Cognitive reserve. Neuropsychologia 47: , 2015–2028. |
[7] | Andel R , Silverstein M , Kareholt I ((2015) ) The role of midlife occupational complexity and leisure activity in late-life cognition. J Gerontol B Psychol Sci Soc Sci 70: , 314–321. |
[8] | Pool LR , Weuve J , Wilson RS , Bültmann U , Evans DA , Mendes De Leon CF ((2016) ) Occupational cognitive requirements and late-life cognitive aging. Neurology 86: , 1386–1392. |
[9] | United Nations, Department of Economic and Social Affairs ((2020) ) World Population Ageing 2019, UN. |
[10] | INEC (Instituto Nacional de Estadística y Censo) (2013) Boletín N°15: Estimación de lapoblación total del país, por provincia, comarca indígena y distrito, segun sexo y edad: años 2010–2020. |
[11] | Humbert F, De Villarreal N, García C, De Adames R, Palacio E, Adames Y, Cubilla Á (2015) Envejecimiento Demográfico de la Población: Período 1960–2050, Panama City, Panamá. |
[12] | Villarreal AE , Pérez-Lao AR , Oviedo DC , Grajales S , Carreira MB , Britton GB , Vernaza A , Aguilar A , Benzadon A , Montalván A , Isaza B , Dondis D , Blake E , Ferro F , Carrillo-Pujol G , Torres-Atencio I , Cedeño JA , Fletcher J , Morales J , Moscoso J , Wesley L , Gómez LA , López L , Lee L , Ortiz L , Sotillo L , Mendieta M , Novarro N , González P , Rodríguez R , Zarak R , Molino R , O’Bryant SE , González V , Castillo V , Osorio V , Vásquez V , Gutierrez Y ((2019) ) The Panama Aging Research Initiative Longitudinal Study. MEDICC Rev 21: , 54–58. |
[13] | Villarreal AE , Grajales S , Lopez L , Britton GB , Panama Aging Research Initiative ((2015) ) Cognitive impairment, depression, and cooccurrence of both among the elderly in Panama: differential associations with multimorbidity and functional limitations. Biomed Res Int 2015: , 718701. |
[14] | Britton GB , O’Bryant SE , Johnson LA , Hall JR , Villarreal AE , Oviedo DC , Pérez-Lao AR , Carreira MB ((2019) ) Inflammatory biomarkers,depressive symptoms and falls among the elderly in Panama. CurrAging Sci 11: , 236–241. |
[15] | Villarreal AE , Grajales S , O’Bryant SE , Edwards M , López L , Montalván A , Britton GB ((2016) ) Characterization of Alzheimer’sdisease and mild cognitive impairment in older adults in Panama. J Alzheimers Dis 54: , 897–901. |
[16] | Fiske A , Wetherell JL , Gatz M ((2009) ) Depression in older adults. Annu Rev Clin Psychol 5: , 363–389. |
[17] | World Health Organization. (2017) Depression and other common mental disorders: global health estimates. World Health Organization. https://apps.who.int/iris/handle/10665/254610 |
[18] | International Labour Office ((2012) ) International Standard Classification of Occupations: ISCO-08. Geneva, Switzerland. |
[19] | McKhann G , Drachman D , Folstein M , Katzman R , Price D , Stadlan EM ((1984) ) Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34: , 939–939. |
[20] | Blesa R , Pujol M , Aguilar M , Santacruz P , Bertran-Serra I , Hernández G , Sol JM , Peña-Casanova J , Soler T , Zabay C , Riera M , Castellví M , Torner L , Charques I , Toirán H , Manero RM , Peter Böhm GE , Martí AM , Meza M , Crespo MC ((2001) ) Clinical validity of the “mini-mental state” for Spanish speakingcommunities. Neuropsychologia 39: , 1150–1157. |
[21] | Brodaty H , Moore CM ((1997) ) The Clock Drawing Test for dementia of the Alzheimer’s type: a comparison of three scoring methods in a memory disorders clinic. Int J Geriatr Psychiatry 12: , 619–627. |
[22] | Reitan RM ((1971) ) Trail making test results for normal and brain-damaged children. Percept Mot Skills 33: , 575–581. |
[23] | Lawton M , Brody E ((1969) ) Assessment of older people: selfmaintaining and instrumental activities of daily living. Gerontologist 9: , 179–186. |
[24] | ValderramaE, Pérez del MolinoJ ((1997) ) Una visión crítica de las escalas de valoraciónfuncional traducidas al castellano. Rev Española Geriatr y Gerontol 32: , 297–306. |
[25] | Reisberg B , Ferris S , De Leon M , Crook T ((1982) ) The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry 139: , 1136–1139. |
[26] | Preacher KJ , Hayes AF ((2004) ) SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput 36: , 717–731. |
[27] | Bolin JH ((2014) ) Hayes, Andrew F. (2013). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press.. J Educ Meas 51: , 335–337. |
[28] | Smart EL , Gow AJ , Deary IJ ((2014) ) Occupational complexity and lifetime cognitive abilities. Neurology 83: , 2285–2291. |
[29] | Lane AP , Windsor TD , Andel R , Luszcz MA ((2017) ) Is occupational complexity associated with cognitive performance or decline? Results from the Australian Longitudinal Study of Ageing. Gerontology 63: , 550–559. |
[30] | Valenzuela MJ , Sachdev P ((2006) ) Brain reserve and dementia: A systematic review. Psychol Med 36: , 441–454. |
[31] | Bunce D , Batterham PJ , Mackinnon AJ , Christensen H ((2012) ) Depression, anxiety and cognition in community-dwelling adults aged 70 years and over. J Psychiatr Res 46: , 1662–1666. |
[32] | Snowden MB , Atkins DC , Steinman LE , Bell JF , Bryant LL , Copeland C , Fitzpatrick AL ((2015) ) Longitudinal association of dementia and depression. Am J Geriatr Psychiatry 23: , 897–905. |
[33] | Wang J , Xue J , Jiang Y , Zhu T , Chen S ((2020) ) Mediating effects of depressive symptoms on social support and quality of life among rural older Chinese. Health Qual Life Outcomes 18: , 242. |
[34] | Prina AM , Stubbs B , Veronese N , Guerra M , Kralj C , Llibre Rodriguez JJ , Prince M , Wu Y-T ((2019) ) Depression and incidence of frailty in older people from six Latin American countries. Am J Geriatr Psychiatry 27: , 1072–1079. |
[35] | Schantz K , Reighard C , Aikens JE , Aruquipa A , Pinto B , Valverde H , Piette JD ((2017) ) Screening for depression in Andean Latin America: Factor structure and reliability of the CES-D short form and the PHQ-8 among Bolivian public hospital patients. Int J Psychiatry Med 52: , 315–327. |
[36] | Guerra M , Prina AM , Ferri CP , Acosta D , Gallardo S , Huang Y , Jacob KS , Jimenez-Velazquez IZ , Llibre Rodriguez JJ , Liu Z , Salas A , Sosa AL , Williams JD , Uwakwe R , Prince M ((2016) ) A comparative cross-cultural study of the prevalence of late life depression in low and middle income countries. J Affect Disord 190: , 362–368. |




