The health information national trends survey (HINTS): A resource for consumer engagement and health communication research
Abstract
The contemporary healthcare system can help improve health literacy outcomes in two ways: first, by nurturing the skills and motivations needed for patients to be actively engaged in their own health and healthcare decisions; and, second, by creating a prepared and proactive healthcare system that adapts to patients’ capacities and needs in efficacious ways. In 2001, the National Cancer Institute launched the Health Information National Trends Survey (HINTS) as a way for researchers and planners to understand how the public is interacting with a rapidly changing health information environment. Original iterations of the HINTS national probability sampling strategies took place on a biennial basis, but in subsequent years the protocol moved to a yearly administration. This yields a rich resource of cross-sectional, national surveillance data to evaluate for trends across and within vulnerable populations. Sixteen studies are presented from the published literature to illustrate how HINTS data were used to explore constructs of direct interest to health literacy researchers. Suggestions are given for how this ongoing public surveillance mechanism can be used: (a) to provide a sentinel view of how the public is interacting with information in the environment to address their health needs; (b) to generate research questions and hypotheses for further exploration using complementary methodologies; and (c) to explore the diffusion of new health communication channels within and between segments of the national population.
1.Introduction
“The millions of dollars of biomedical research …aimed at a disease that was costing tens of thousands of dollars to treat and it ultimately relied on the actions of a skinny, weak, scared 20-year old to have its impact.” Jessie Gruman, Behavioral Scientist and Patient Advocate, (12/7/1953 to 7/14/2014).
As a behavioral scientist and a long-time Hodgkin’s lymphoma patient, Jessie Gruman dedicated her life to improving health outcomes for patients. Much of her energy was focused on elevating the degree to which patients could become more actively engaged in their own health and healthcare decisions. She equally emphasized the responsibility of patients to engage directly with their health and healthcare [20] and the responsibilities of healthcare systems and researchers to create real, trustworthy support for patients struggling with disease [19]. In this article, we will begin by describing a behavioral science perspective on health literacy, which connects to the inception and objectives of the NCI-sponsored Health Information National Trends Survey (HINTS). We will then introduce the history, vision, and status of HINTS and summarize research contributions to the health literacy knowledge base that are based on various iterations of the HINTS instruments. We conclude with future directions that HINTS offers to health communication researchers and practitioners, particularly those charged with moving the science of health literacy forward.
1.1.Patient activation and prepared systems
Per the goals for a healthier nation set by the Department of Health and Human Services’ Healthy People initiative, health literacy refers to the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions [47]. Supporting health literacy, therefore, means attending to the malleable, individual characteristics of the individual as well as attending to the information environment in which the public lives and thrives. Wagner and colleagues [8] take this two-fold point of interaction further by setting goals for the healthcare system in which patients are encouraged to be fully engaged, or activated, stewards of their own care while transacting with a system that is fully prepared to offer evidence-based support for patients’ personal and medical needs. On the individual side of the equation, Gruman referred to this notion of patient engagement as a critical quality encompassing the “actions people take to support their health and benefit from their health care” [4]. In a similar vein, Hibbard and Gilburt described patient activation as relating to the “knowledge, skills and confidence a person has in managing their own health and health care” [28]. Studies have demonstrated that patients who score high on measures of patient activation tend to have better care experiences [17], are less costly to the healthcare system [29], and generally experience better health outcomes than their “disengaged” counterparts [18]. Creating a public health environment that nurtures individual engagement has become a hallmark of public policy overtures in both the United Kingdom [3] and the United States [30].
Although crucial, patient motivation is only part of the formula for optimizing individual and population-level health outcomes in health service research. The other side of the equation must be considered in terms of the healthcare environment itself; that is, whether the system is built around principles of evidence-based practice in health communication and can serve as a responsive receptor site to the patient’s own engaged overtures. Systems that are unprepared, or that seek to exploit transactional value from patient encounters at the expense of long-term support (as often happens within a fee-for-service vs. a value-based incentive structure), will often fail to engender the sense of response efficacy needed to sustain action over time [50]. Patients’ intentional actions must work together with a supportive healthcare environment to produce sustainably productive outcomes [7,19]. This line of thinking is delicately intertwined throughout the Institute of Medicine’s (now the National Academies of Sciences, Engineering, Medicine) workshop series on quality improvement in healthcare [2,31,36,43]. The series adopts a human factors approach [48] by deconstructing sources of error within contemporary healthcare, and then offering a blueprint for how to build a more robust, higher quality healthcare system for the twenty-first century. Such a system would be patient-centric, and would focus on creating an environment that offered deep, comprehensive support for patients’ medical, emotional, and information needs [10,50]. Ideally, such a system would adopt a “universal design” [22] approach, in that it would become equitably accessible to all patients regardless of cultural backgrounds or level of personal health literacy [26]. These concepts are informing many healthcare reform efforts currently underway worldwide.
1.2.A health systems perspective on health literacy
When considering how to support the actions individuals take to improve their health and to benefit from healthcare – that is, in considering how to support patient engagement – behavioral scientists must take into account the relationship between the individual and the environment in which they live and thrive [46]. Donald Norman, a cognitive scientist with a legacy of influence in engineering and design [41], best described this balance of interactions. When considering human behavior, he noted that it is worthwhile to recognize that there are two sources of knowledge that drive human action: one source is internal to the individual, or “knowledge in the head;” the other is external to the individual, or “knowledge in the world.” The history of writing, literature, and, more recently, information technology has largely been a story of creating knowledge in the world so that it can supplement knowledge in the head reliably across many stakeholders within the society. Literacy, in this context, is the ability of individuals to process and act upon information using the skills and knowledge they have acquired through experience. In a very similar sense, health literacy has been defined as “the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [40]. Research on health literacy focuses generally on understanding how individuals with various levels of experience, language, and knowledge interact with the people, instructions, and tools made available to them in healthcare.
There are at least two complementary ways for intervening on behalf of patients to improve health outcomes. The first is to assess the knowledge and skills a patient might bring into the health care setting and then to supplement any deficits with education and counseling [34]. The second is to improve the availability and compatibility of information in the environment to ensure that all patients, regardless of knowledge they bring into the encounter, will fare well throughout their healthcare journeys [1]. Consider the example of a patient who presents with an early stage diagnosis of non-Hodgkin’s lymphoma. The patient is likely to know very little about this disease prior to receiving this disquieting and disorienting diagnosis. After thoughtfully explaining some of the most important aspects of the disease to the patient, the treating oncologist may then elect to give the patient an “information prescription” [34] to round out their understanding of the disease and to inform future decision-making. This “prescription” might be in the form of pamphlets or other media, an informational website, or a visit with a specialized counselor. The oncologist may further explain that the patient’s electronic portal will contain a secure messaging feature that can be used any time to ask a question, as well as a telephone number for use in emergencies. As treatment progresses, the oncologist may introduce the patient to a nurse navigator to help schedule appointments, arrange for tests, and report symptoms. These services provide informational support from the environment to complement the patient’s evolving knowledge about their condition(s) [27].
The skilled health system designer recognizes that these two leverage points must be considered together when creating resources to support patients. A well-designed decision aid using iconographs, for example, has been shown to improve decision-making for professionals with all levels of health numeracy [13,15,16]. Research from medical informatics and patient education literature strongly suggests that a patient’s ability to obtain, understand, and apply health information relies on much more than personal literacy skills alone [1]. Health systems can make universal improvements to improve outcomes across all types of patients equitably by creating an intelligent healthcare environment [23] that lowers the demand from patients through better informational design [41]. Such a system would reserve high-valued educational and counseling resources for those who need them the most [24]. In Fig. 1, we present an enhanced version of the Chronic Care Model as developed by Gee and colleagues [14] to illustrate how the post-HITECH (i.e., the Health Information Technology for Economic and Clinical Care Act of 2009) healthcare system can be engineered to support patient engagement and to compensate for deficits in health literacy. The updated model adds in components of technology-mediated communication and support typical of today’s healthcare settings [8,14].
Fig. 1.
The eHealth Enhanced Chronic Care Model (eCCM). Created by Gee, P.M., Greenwood, D.A., Paterniti, D.A., Ward, D., and Miller, L.M. [14].
![The eHealth Enhanced Chronic Care Model (eCCM). Created by Gee, P.M., Greenwood, D.A., Paterniti, D.A., Ward, D., and Miller, L.M. [14].](https://content.iospress.com:443/media/isu/2017/37-2/isu-37-2-isu830/isu-37-isu830-g001.jpg)
As depicted in the model, the “Informed, Activated Patient” brings with her a preexisting set of knowledge (“knowledge in the head”). In addition, she also comes in with prior experiences gathered from within and from outside of healthcare (“knowledge in the world”), which informs her decision making during the encounter. The “Prepared, Proactive Practice Team” interfaces with the knowledge of the patient by offering support in a variety of forms, ranging from traditional media (e.g., information pamphlets), clinical information systems like electronic patient portals, and eHealth education tools, to professionally trained navigators and other allied health professionals.
In sum, conceptualizing health literacy within the health care system can help inform the construction of a national communication surveillance program. In this way, construction of the Health Information National Trends Survey (HINTS) can serve to complement existing datasets and surveillance programs of relevance to health literacy researchers. For example, one of the main surveillance tools for literacy assessment is the Department of Education’s National Assessment of Adult Literacy (NAAL), a performance-based national- and state-based assessments of adult literacy performance. NAAL evaluates individual competencies and deficits as a diagnostic for dedicating monetary resources or modifying curricula within educational systems. In contrast, public health surveillance programs often do not include in-depth assessments but rather gather self-reported data on knowledge, attitudes, and behaviors. As a case in point, the Behavioral Risk Factors Surveillance System (BRFSS) gathers self-reported data across states and territories on behaviors known to influence public health outcomes. These data are used to track the diffusion of beliefs, knowledge, and healthy behaviors as distributed across varying populations. Public health departments may utilize the surveillance data to inform patient outreach and education efforts, while epidemiologists may analyze the data for evidence of knowledge or belief gaps among differing populations. In what follows, we will describe how HINTS is uniquely positioned to serve as a health communication surveillance tool for health literacy researchers working within healthcare systems.
2.The health information national trends survey (HINTS)
In the late 1990s, a group of health communication experts, behavioral scientists, clinicians, and public health professionals gathered at the behest of the National Cancer Institute (NCI) to identify priorities for behavioral research related to cancer control and prevention. One priority identified by the group was to seize on the opportunities afforded by a rapidly changing health communication environment to improve support for individuals’ capacities to prevent and control the disease. When recommendations from the group were published in 1999, the World Wide Web had only existed for approximately six years. Anecdotal evidence suggested that patients were already showing up at their doctors’ offices with reams of paper printed from their latest foray onto Internet search engines. Some early evaluations of Internet search data suggested that the Web was becoming the first resource for many health information seekers. Recommendations from the external group of health communication experts were to monitor these changes through public surveillance of the health information environment. The recommendations were especially sensitive to the unanticipated consequences of creating a “Digital Divide” between those facile with these new communication technologies and those struggling with access, language, or technological prowess.
2.1.Establishing a health communication data program
With those recommendations in hand, the Division of Cancer Control and Population Sciences at the NCI launched the Health Information National Trends Survey (HINTS) in 2001. The program serves as the surveillance arm of a larger investment to fund research around the opportunity afforded by this larger transition to a consumer-facing, information-age economy. The purpose of the program was to monitor knowledge, attitudes, and behaviors to provide information on the ways in which people were utilizing resources and channels in the changing information environment. In this way, program administrators could gather information for communication researchers on how populations were adapting to these changes. Were people becoming more engaged as the environment shifted from a passive broadcast medium to a mixed medium facilitating both the push and pull of health information? Were some benefiting from the diffusion of technology more than others? What were the functional literacy skills that might be helping some people fare better in this new media environment than others? By trending over time, researchers could track answers to these questions across the entire diffusion of innovations curve; that is, by gathering self-reported data from early adopters, early majority adopters, late majority adopters, and laggards [44].
The survey was originally developed to provide probability-based population estimates biennially on data from non-institutionalized adults 18 years and older in the United States [50]. The first three administrations of the survey used a randomized digit dial (RDD) methodology to collect oral responses from participants through a Computer-Assisted Telephone Interview (CATI). Response rates began to plummet during the 2000s, however, as some households with caller identification avoided telephone calls with unrecognizable caller IDs and others abandoned their land-line telephones for mobile phone options. In 2007–2008, the HINTS program fielded a separate paper-and-pencil survey using a sampling technique drawn from a newly available, comprehensive list of postal addresses in parallel with the RDD administration. The dual-frame administration of both the RDD and Postal surveys allowed methodologists to evaluate the feasibility and psychometric equivalencies of the two surveillance approaches [12]. In 2011, the program switched from its biennial administration paradigm to an annual approach, with independent cycles of the survey being launched on a yearly basis using the postal frame and paper-and-pencil methodology [11]. The HINTS IV survey also included an independent cycle funded by the Food and Drug Administration containing items specially targeted towards direct-to-consumer advertising, smoking, and the use of alternative tobacco products.
2.2.Published HINTS studies relevant to health literacy research
Shortly after publication of the first data set, communication scholars began analyzing the data to gain a better understanding of how the new communication environment might be facilitating or hindering individuals’ capacities to obtain, process, and understand health information. In Table 1, we offer a synoptic list of many of the studies using HINTS to answer questions of interest to health literacy researchers.
Table 1
Articles published from HINTS data with relevance to Health Literacy researchers
| First Author, Year | Title | Journal | Health Literacy defined | HINTS Cycle: Type of Assessment |
| Champlin (2015) | Creating a Screening Measure of Health Literacy for the Health Information National Trends Survey | American Journal of Health Promotion | The Zarcadoolas’ Model of health literacy | HINTS 4, Cycle 2: Items: E1, E2, J11, N6; performance-based |
| Chen (2014) | Numeracy, information seeking, and self-efficacy in managing health: an analysis using the 2007 Health Information National Trends Survey (HINTS). | Health Communication | Health Numeracy Confidence | HINTS 3 (2007): Items: K1/CS-02; subjective |
| Ciampa (2010) | Patient numeracy, perceptions of provider communication, and colorectal cancer screening utilization | Journal of Health Communication | Numeracy | HINTS 3 (2007): Items: K1/ CS-02, K3 [mail only]; subjective & performance-based |
| Dominick (2015) | Classification tree analysis to examine influences on colorectal cancer screening | Cancer Causes and Control | Numeracy | HINTS 3 (2007): Items: K1, CS-02; K2/CS-04; K4/CS-05; subjective |
| Ha (2011) | Determinants of consumer-driven healthcare: Self-confidence in information search, health literacy, and trust in information sources. | International Journal of Pharmaceutical and Healthcare Marketing | Perceived Literacy | HINTS 3 (2007): Items: HC-05/A5a; HC-05b/A5b; HC-05c/A5c; HC-05d/A5d; HC-06a; HC-7a; HC-20; subjective |
| Hoffman-Goetz (2009) | Literacy and cancer anxiety as predictors of health status: An exploratory study | Journal of Cancer Education | Literacy Levels | HINTS 1 (2003): Items: HC-6a; HC-7a; HC-20; subjective |
| Huang (2012) | Health Numeracy Confidence among Racial/ Ethnic Minorities in HINTS 2007: Sociodemographic, Attitudinal, and Knowledge Correlates | Literacy and Numeracy Studies | Health numeracy confidence | HINTS 3 (2007): Items: K1, CS-02; subjective |
| Jiang (2016) | Health literacy and the internet: An exploratory study on the 2013 HINTS survey | Computers in Human Behavior | Zarcadoolas’ Model | HINTS 4, Cycle 3: Items: G2a; F1; K1/4; I9; N1; performance-based |
| Kobayashi (2016) | Cancer Fatalism, Literacy, and Cancer Information Seeking in the American Public | Health Education & Behavior | Health literacy as “Newest Vital Sign” | HINTS 4, Cycle 3: Items: N1-N4; performance-based |
| Koch-Weser (2010) | The Internet as a health information source: Findings from the 2007 health information national trends survey and implications for health communication | Journal of Health Communication | Information Efficacy | HINTS 3 (2007): Items: HC-06; subjective |
| Langford (2012) | Racial and ethnic differences in direct-to-consumer genetic tests awareness in HINTS 2007: Sociodemographic and numeracy correlates | Journal of Genetic Counseling | Numeracy | HINTS 3 (2007): Items: CS-02/K1; CS-04/K2; CS-05/K4; subjective |
| Lustria (2011) | Exploring digital divides: An examination of eHealth technology use in health information seeking, communication and personal health information management in the USA | Health Informatics Journal | Numeracy | HINTS 3 (2007): Items: CS-02; CS-03; subjective |
| Manganello (2011) | The association of understanding of medical statistics with health information seeking and health provider interaction in a national sample of young adults | Journal of Health Communication | Numeracy | HINTS 3 (2007): Items: CS-02; K-1; subjective |
| Nelson (2013) | Exploring objective and subjective numeracy at a population level: Findings from the 2007 health information national trends survey (HINTS) | Journal of Health Communication | Numeracy | HINTS 3 (2007): Items: K3; CS-05/K4; subjective and performance-based |
| Patel (2015) | The Role of Health Care Experience and Consumer Information Efficacy in Shaping Privacy and Security Perceptions of Medical Records: National Consumer Survey Results | JMIR Medical Informatics | Information efficacy | HINTS 4, Cycle 1: Items: A6, N6; subjective |
| Smith (2010) | Socioeconomic status, statistical confidence, and patient-provider communication: an analysis of the Health Information National Trends Survey (HINTS 2007) | Journal of Health Communication | Statistical confidence | HINTS 4, Cycle 2: Items: E1, E2, J11, N6; performance-based |
As the table shows, several different concepts and models related to health literacy have been analyzed using HINTS items. Some of the health literacy elements studied include the components of the Zaracadoolas’ Model [49] along with numeracy, health numeracy confidence, basic literacy levels, the Newest Vital Sign, and information efficacy. These health literacy items have been studied to analyze potential associations with other psychological constructs (e.g., self-efficacy), information seeking behaviors, clinical communication, and detection/preventive behaviors (e.g., colorectal cancer screening, healthy eating). While analyzing these associations, health literacy was conceptualized as the predictive variable almost twice as often as it was conceptualized as the outcome variable.
As discussed earlier, the way health literacy has been conceptualized by researchers and policymakers has varied considerably. Similarly, the ways that health literacy has been operationalized and applied using HINTS items reflect this wide range of perspectives. One major area of difference is how researchers have chosen to define health literacy or specific elements of health literacy (e.g., numeracy). This has at times resulted in a HINTS item being used to define health literacy in one study and at the same item being conceptualized as an outcome of health literacy in another study. For example, Smith and colleagues used an item assessing the participant’s preference for obtaining health information by words or numbers as an outcome of literacy [45], while Koch-Weser and colleagues used the same item to assess the participant’s health literacy level itself [35]. Similarly, Jiang and colleagues used genetic test awareness to assess the scientific literacy component of the Zarcadoolas’ Model of health literacy [33], while Langford et al. conceptualized the same genetic test awareness item as an outcome of health literacy [37].
A second way that researchers have differed in their HINTS analyses is whether they measured literacy utilizing objective or subjective items. Objective items often ask participants questions designed to test numeric ability, reading comprehension skills, and knowledge of the scientific community to yield an overall literacy “score”. In comparison, subjective items typically assess the participant’s perceptions and confidence in his own literacy abilities during daily activities such as searching for information and interpreting statistics [39]. In this sense, objective measures may be stronger indicators of “knowledge in the head,” whereas subjective measures would be more likely to assess the interaction or interface between the “knowledge in the head” to the “knowledge in the world.” Consistent with the role of HINTS as a surveillance tool to assess the communication environment, most of the articles in Table 1 applied subjective items to measure health literacy at the interface between personal experience and the information environment.
2.3.Tracking trends over time
One of the policy-related advantages associated with conducting routine surveillance of the general population is the ability to compare snapshots of the public’s responses to literacy-related questions over time. For example, the Healthy People 2010 and 2020 initiatives represent a collective policy effort sponsored by the U.S. Department of Health and Human Services (DHHS) to identify leverage points for improving the health of the general U.S. population by targeted deadlines. The initiatives give policy makers, public health departments, intervention researchers, and local communities a set of science-based, aspirational benchmarks against which they can compare their own progress in improving the health of the nation. Targets for “Leading Health Indicators” are central to the initiatives and include objectives related to decreasing the use of tobacco products, improving access to healthcare, improving environmental quality, improving nutrition and exercise, ameliorating the negative influence of certain social determinants of health, and more. A focus on health communication and health information technology is also included in the initiative to reflect the DHHS’s concern over the role that the health information environment plays in building capacity for obtaining, processing, and utilizing health information.
HINTS is one of the national surveillance sources utilized by the DHHS to monitor progress on the Healthy People goals. The survey has been used as a check-up on policy incentives related to encouraging widespread access to the Internet, created in light of the presidential admonition stating that: “Access to high-speed broadband is no longer a luxury; it is a necessity for American families, businesses, and consumers” [42]. Data generated from the HINTS program have paralleled those of the Pew Foundation in showing that general access to the Internet has risen steadily from 63% in 2003 to over 80% in 2015. Measures related to online usage of medication ordering, emails to physicians, and access to personal medical information through online patient portals have also been incorporated into HINTS surveys since the passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009. These measures have revealed a more gradual rise in the use of online tools as the culture evolves to favor patient engagement. Analyses of sociodemographic characteristics included in the HINTS surveys can help pinpoint areas of lagging adoption within certain portions of the general population. Data from those subpopulation analyses have shown a moderation in disparity over most racial/ethnic groups as general Internet adoption rises; however, they have also shown a persistent disparity related directly to respondents’ education level. It is the critical thinking, English literacy, and functional problem-solving skills needed to find and interpret information from the Web that will likely be in short supply among low literacy populations [25]. Policy makers and health system administrators would do well to continue strengthening their support for low-literate populations through personal assistance from patient navigators, allied health professionals, and interpreters.
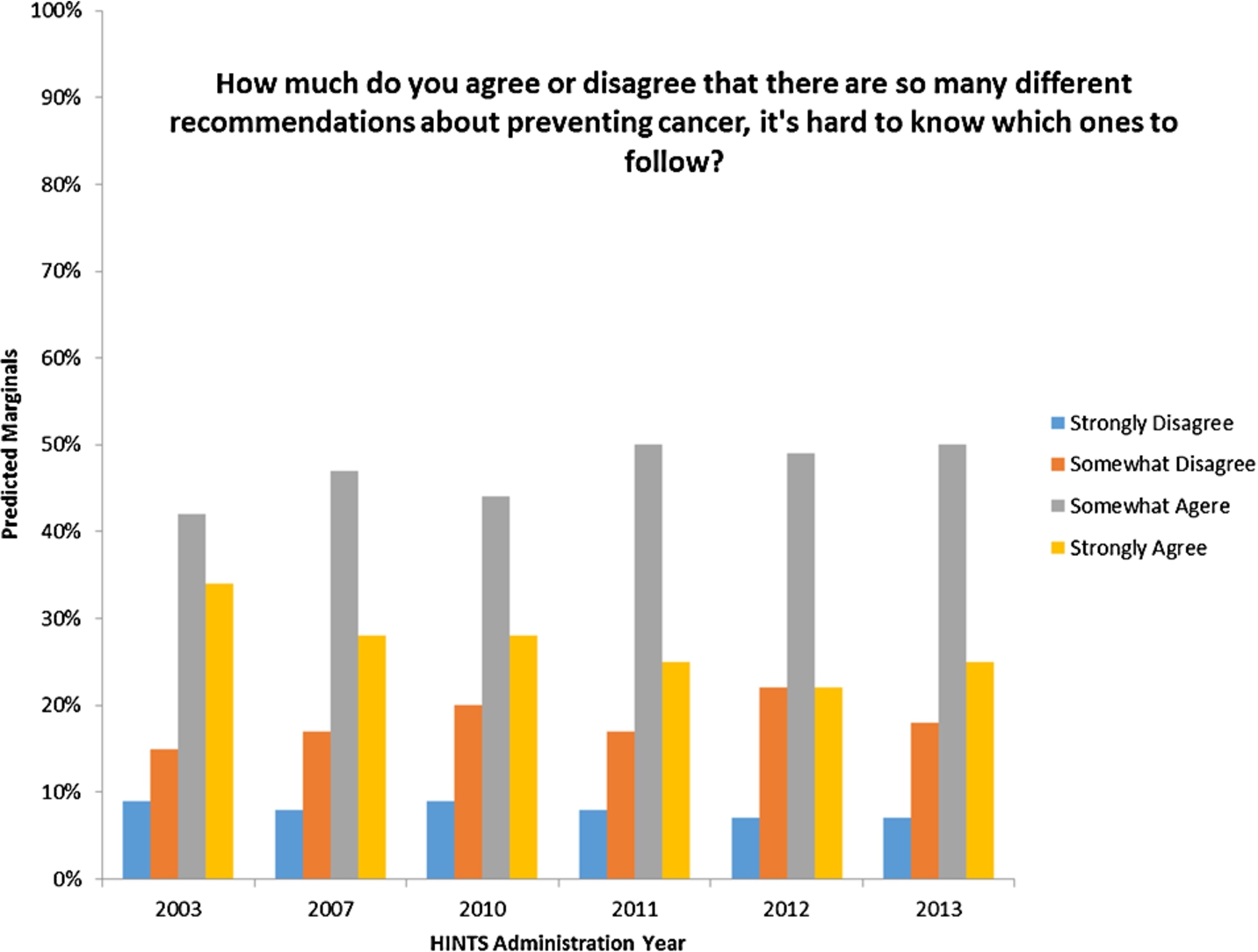
The trending capacity of repeated cross-sectional surveys of the U.S. population can also be used to assess the waxing or waning of public comprehension within the context of an increasingly multi-channel, complex, and potentially confusing media environment. In Fig. 2, we track the performance of one such indicator related to the public’s endorsement of a statement suggesting that there are “too many recommendations for preventing cancer to know which ones to follow.” Although fewer people endorsed the “Strongly Agree” option over the last decade, their endorsement of “Somewhat Agree” has risen. From these data, confusion over health recommendations from a multi-channel media environment is a pervasive problem that is only gaining small ground over the last decade.
Fig. 2.
Tracking the public’s agreement with an indicator of confusion, or cognitive overload, over a decade from 2003 to 2013.
3.Moving into the future
Prevalent reports of emerging communication technologies and media, together with new and promising cancer prevention and treatment options underscore the need to monitor the population’s capacity to obtain, process, and utilize health information for engaged decision-making. In this final section, we review the status of NCI’s HINTS surveillance program and offer further suggestions for how to utilize this resource to support research on health literacy. We also look to the HINTS data and publications as a harbinger of health literacy problems that may continue, and use our understanding of technological and medical trends to forecast emerging areas of concern.
Fig. 3.
Health Information National Trends Survey Timeline. Dotted lines indicate supplemental studies conducted in local areas.
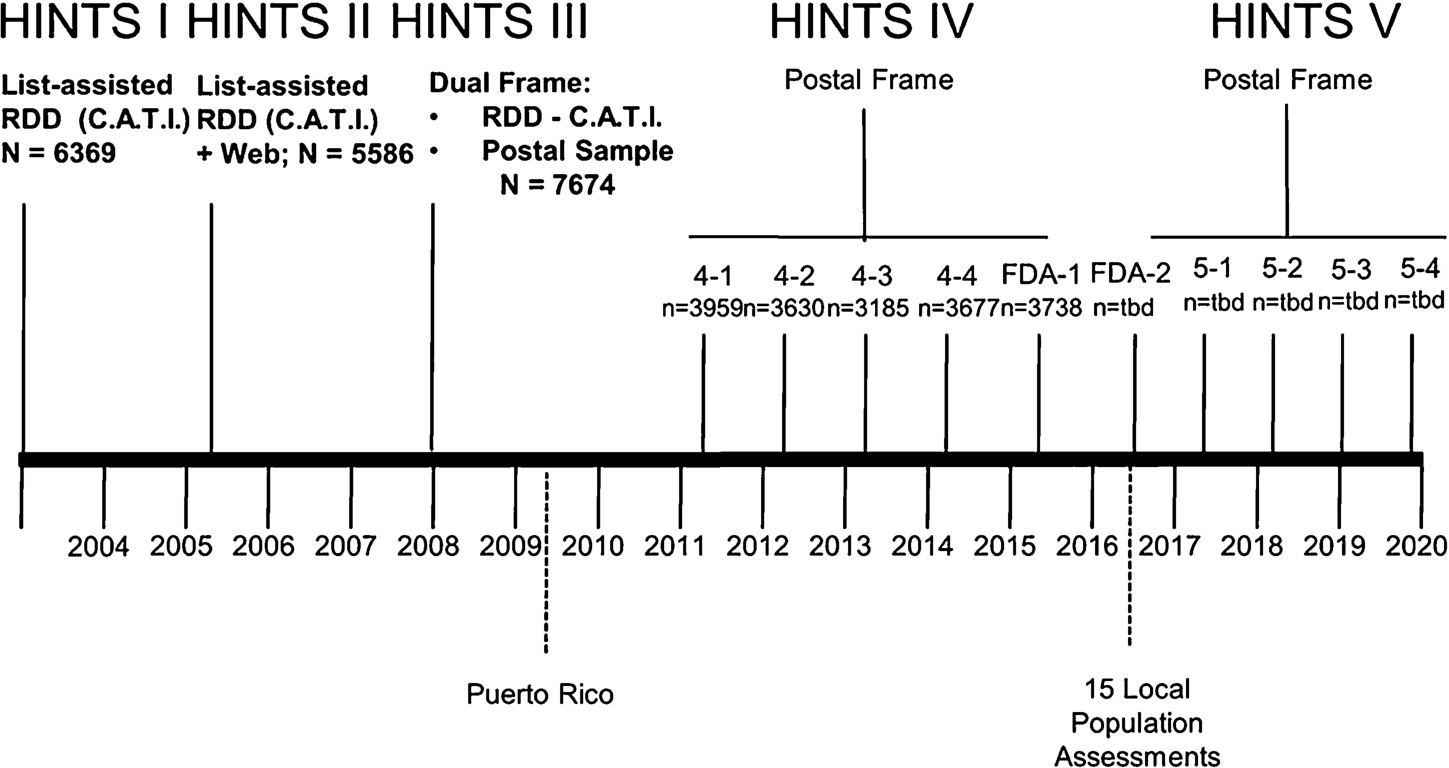
3.1.The future of HINTS
The HINTS V survey was approved in 2015. The new phase will include the same four-cycle structure as HINTS IV and will again be collected annually using a postal-frame, paper-and-pencil modality. A timeline of the HINTS program’s survey administrations is depicted in Fig. 3. De-identified data from each administration of the survey have been made available at the HINTS website (hints.cancer.gov). Taken across all its iterations, the HINTS program will continue to offer a wealth of data for health communication scholars and program planners. This survey has helped cultivate a vibrant community of researchers across disciplines who access and analyze the data, publish the results, and contribute information about their published articles back to the HINTS community. A full listing of publications using HINTS can be found on the website. Several times a year, the HINTS management team selects an intriguing article to highlight in a “HINTS Brief.” These briefs offer a high-level synthesis of significant trends emerging from the community presented in an engaging format designed for quick consumption by public health practitioners (see http://hints.cancer.gov/briefs.aspx).
In addition to depicting the national administrations of HINTS I, II, III, & IV above the bolded timeline, the figure also depicts two separately funded supplements aimed at gathering data at the local level. The first of these was a supplement awarded to researchers at the University of Puerto Rico to gather an assessment of the changing health information landscape in the largest of the U.S. territories in the Caribbean. The supplement funding allowed in-depth analyses of a health communication context that was different from the mainland. For instance, mobile phones gained traction earlier in the island territory as compared to mainland US, and the mix of monolingual and bilingual Spanish speakers provided insight from a distinct cultural context. The second funding opportunity was a supplement program designed to support 15 of the NCI-funded National Cancer Centers in gathering data from a variety of sources within their local catchment areas. Hospitals are increasingly being held accountable for population health outcomes among members within their service areas. They are encouraged to conduct community health needs assessments to take stock of community needs, and then to support community action in meeting public health goals. The supplement funding was awarded to participating cancer centers in 2016 as way to explore the utilization of communication variables in conjunction with other clinically relevant surveillance data to assist in local community planning. The intent of these supplements is to move beyond national surveillance to enable local action for the specific needs of each catchment area.
3.2.Future challenges in health literacy
With an increasing focus on multidisciplinary health research, the field of health literacy continues to grow and connect with other disciplines in health and communication. While HINTS serves as a valuable resource and stimulates new analytic opportunities, it is a cross-sectional survey with some inherent limitations; therefore, we believe the survey is best used when it complements other methods of inquiry. In the following, we highlight three key challenges and opportunities in health literacy research, and within each we discuss how HINTS can serve as a resource in addressing the challenges.
First, the field is gradually moving beyond assessing and “diagnosing” individuals’ health literacy and numeracy levels. Scholars have developed and tested a multitude of literacy assessment tools, both objective and subjective. While no tool is perfect, many well-validated instruments and survey items have been developed for researchers and care providers. Rather than continue to develop additional assessment tools to measure individuals, more work is needed to assess the environment and broader context of public health and clinical care, including family interactions, communication with providers within and across care delivery teams, and experience with the communication environment more generally. HINTS is a useful tool to consider how individuals interact with the environment by not just including items related to static “knowledge in the head,” but additionally by gauging how well the environment meets the needs of the individual. Previous HINTS work has suggested that this interaction is an important area for future research in a variety of contexts. For example, one study focused on information seeking [21] found that participants who reported difficulties finding and understanding information while searching for health information were less likely to be knowledgeable about cancer prevention and engage in healthy behaviors related to fruit/vegetable intake, smoking status and exercise. Another study that was focused on clinical communication found that young adults with lower numeracy reported more negative interactions with their health care providers [38]. Both examples illustrate the connection between one’s “knowledge in the head” and the individual’s environment. Beyond measurement, the development and testing of multi-level health literacy interventions are needed, whereby health literacy is addressed at the broader system’s level (e.g., can aspects of the information environment be modified or improved upon to facilitate sustained patient engagement or behavior change?). Health literacy is then linked to other levels of “outcomes” including behaviors. In our review of HINTS studies that have analyzed health literacy variables, much of the work has remained on a descriptive level. While a few studies have analyzed the association between health literacy elements and health behaviors (e.g., colorectal cancer screening [6,9]), more work should be done to connect health literacy with behavioral outcomes and health care utilization measurements. To this effect, it was interesting to observe that extant HINTS-based publications related to health literacy have conceptualized health literacy as a predictor, rather than an outcome, variable.
Second, to gain a more holistic understanding of the role of health literacy in communication and health care, there are opportunities to complement HINTS analyses with other methods of inquiry. HINTS can be used to generate and test hypotheses, and findings from the analyses can then inform the design and delivery of subsequent interventions. For example, HINTS cycles have been used to track the American public’s general acceptance and reported use of emerging media, such as social media and health information technologies [5,32] to solve health-related problems. These descriptive analyses can provide the baseline data to inform the development and testing of health literacy interventions using related platforms and technologies.
Finally, despite the proliferation of technology and new media in health, there has been limited health literacy research aimed at understanding the impact of new/novel communication strategies and channels (e.g. mobile and social media and other peer-to-peer communication platforms). Health information and messages are quickly becoming ubiquitous through online channels, which may increase the demand on individuals and communities to process and discern the quality of the available technology-mediated information. Moreover, the intersection of health literacy and technology literacy deserves further investigation. This includes understanding how diverse populations with varying degrees of health literacy access and make use of health information technology, and how technology-mediated interactions serving specific communities can be optimized to facilitate healthy behaviors. HINTS, with its many items related to technology and new media across the iterations, offers unique opportunities to examine the impact of the emerging health communication landscape.
4.Conclusion
For the past 13 years, researchers have used HINTS as a tool to study interrelationships and interactions between health communication items, test communication theories, and address issues related to information access and usage. Literacy-related items found in HINTS iterations are uniquely situated to increase our understanding of the health systems perspective of health literacy, both by analyzing a single cycle “snapshot” and by identifying changing trends and practices over time. In this article, we outlined different approaches for conceptualizing health literacy, described the rationale and history behind HINTS, and detailed both how HINTS has already been used to address health literacy-related questions, as well as identified gaps and opportunities for future work in this area. New trends and constantly-emerging technologies underscore the need for researchers to utilize HINTS to monitor and assess how the population’s “knowledge in the head” responds to and interacts with the constantly-evolving “knowledge in the world.”
References
[1] | J.S. Ancker, Addressing health literacy and numeracy through systems approaches, Cognitive Informatics in Health and Biomedicine: Understanding and Modeling Health Behaviors, V.L. Patel, J.F. Arocha and J.S. Ancker, eds, Springer, London, UK, in press. |
[2] | D.M. Berwick, A user’s manual for the IOM’s ‘quality chasm’ report, Health Aff (Millwood) 21: (3) ((2002) ), 80–90. doi:10.1377/hlthaff.21.3.80. |
[3] | H. Cayton, The flat-pack patient? Creating health together, Patient Educ Couns 62: (3) ((2006) ), 288–290. doi:10.1016/j.pec.2006.06.016. |
[4] | Center for Advancing Health, Here to stay: What health care leaders say about patient engagement, Center for Advancing Health, Washington, DC, 2014, p. 169. |
[5] | W.-y.S. Chou, Y.M. Hunt, E.B. Beckjord, R.P. Moser and B.W. Hesse, Social media use in the United States: Implications for health communication, J Med Internet Res 11: (4) ((2009) ), e48. doi:10.2196/jmir.1249. |
[6] | P.J. Ciampa, C.Y. Osborn, N.B. Peterson and R.R.L. Patient, Numeracy, perceptions of provider communication, and colorectal cancer screening utilization, J Health Commun 15: (Supp 3) ((2010) ), 157–168. doi:10.1080/10810730.2010.522699. |
[7] | S.B. Clauser, E.H. Wagner, E.J. Aiello Bowles, L. Tuzzio and S.M. Greene, Improving modern cancer care through information technology, Am J Prev Med 40: (5 SUPP) ((2011) ), S198–S207. doi:10.1016/j.amepre.2011.01.014. |
[8] | K. Coleman, B.T. Austin, C. Brach and E.H. Wagner, Evidence on the chronic care model in the new millennium, Health Aff (Millwood) 28: (1) ((2009) ), 75–85. doi:10.1377/hlthaff.28.1.75. |
[9] | G.M. Dominick, M.A. Papas, M.L. Rogers and W. Rakowski, Classification tree analysis to examine influences on colorectal cancer screening, Cancer Cause Control 26: (3) ((2015) ), 443–454. doi:10.1007/s10552-015-0523-6. |
[10] | R. Epstein and R.J. Street, Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering, National Cancer Institute, Bethesda, MD, (2007) . |
[11] | L.J. Finney Rutten, T. Davis, E.B. Beckjord, K. Blake, R.P. Moser and B.W. Picking, Picking up the pace: Changes in method and frame for the health information national trends survey (2011–2014), J Health Commun 17: (8) ((2012) ), 979–989. doi:10.1080/10810730.2012.700998. |
[12] | L.J. Finney Rutten, B.W. Hesse, R.P. Moser and G.L. Kreps, Building the Evidence Base in Cancer Communication, Hampton Press, Cresskill, NJ, (2010) . |
[13] | M. Galesic, R. Garcia-Retamero and G. Gigerenzer, Using icon arrays to communicate medical risks: Overcoming low numeracy, Health Psychol 28: (2) ((2009) ), 210–216. doi:10.1037/a0014474. |
[14] | P.M. Gee, D.A. Greenwood, D.A. Paterniti, D. Ward and L.M.S. Miller, The eHealth enhanced chronic care model: A theory derivation approach, J Med Internet Res 17: (4) ((2015) ), e86. doi:10.2196/jmir.4067. |
[15] | G. Gigerenzer, What are natural frequencies? Bmj 343: ((2011) ), d6386. doi:10.1136/bmj.d6386. |
[16] | G. Gigerenzer and A. Edwards, Simple tools for understanding risks: From innumeracy to insight, Bmj 327: (7417) ((2003) ), 741–744. doi:10.1136/bmj.327.7417.741. |
[17] | J. Greene, J.H. Hibbard, R. Sacks and V. Overton, When seeing the same physician, highly activated patients have better care experiences than less activated patients, Health Aff (Millwood) 32: (7) ((2013) ), 1299–1305. doi:10.1377/hlthaff.2012.1409. |
[18] | J. Greene, J.H. Hibbard, R. Sacks, V. Overton and C.D. Parrotta, When patient activation levels change, health outcomes and costs change, too, Health Aff (Millwood) 34: (3) ((2015) ), 431–437. doi:10.1377/hlthaff.2014.0452. |
[19] | J.C. Gruman, Making health information technology sing for people with chronic conditions, Am J Prev Med 40: (Supp 2) ((2011) ), S238–S240. doi:10.1016/j.amepre.2011.02.003. |
[20] | J.C. Gruman, Preparing patients to care for themselves, Am J Nurs 114: (7) ((2014) ), 11. doi:10.1097/01.NAJ.0000451657.77642.36. |
[21] | S. Ha and Y.J. Lee, Determinants of consumer-driven healthcare: Self-confidence in information search, health literacy, and trust in information sources, Int J Pharmaceutical & Healthcare Marketing 5: (1) ((2011) ), 8–24. doi:10.1108/17506121111121550. |
[22] | B.W. Hesse, Curb cuts in the virtual community: Telework and persons with disabilities, in: 28th Annual Hawaii International Conference on System Sciences, Maui, HI, (1995) , pp. 418–425. |
[23] | B.W. Hesse, Harnessing the power of an intelligent health environment in cancer control, Stud Health Technol Inform 118: ((2005) ), 159–176. |
[24] | B.W. Hesse, G.E. Cole and B.D. Powe, Partnering against cancer today: A blueprint for coordinating efforts through communication science, J Natl Cancer I Mono 2013: (47) ((2013) ), 233–239. doi:10.1093/jncimonographs/lgt024. |
[25] | B.W. Hesse, A. Gaysynsky, S. Vieux, A.J. Ottenbacher, R.P. Moser, K.D. Blake et al., Meeting the healthy people 2020 goals: Using the health information national trends survey to monitor progress on health communication objectives, J Health Commun 19: (12) ((2014) ), 1497–1509. doi:10.1080/10810730.2014.954084. |
[26] | B.W. Hesse and B. Shneiderman, eHealth research from the user’s perspective, Am J Prev Med 32: (5 SUPP) ((2007) ), S97–S103. doi:10.1016/j.amepre.2007.01.019. |
[27] | B.W. Hesse and J.M. Suls, Informatics-enabled behavioral medicine in oncology, Cancer J 17: ((2011) ), 222–230. doi:10.1097/PPO.0b013e318227c811. |
[28] | J.H. Hibbard and H. Gilburt, Supporting People to Manage Their Health: An Introduction to Patient Activation, The King’s Fund, London, UK, (2014) . |
[29] | J.H. Hibbard, J. Greene and V. Overton, Patients with lower activation associated with higher costs; delivery systems should know their patients’ ‘scores’, Health Aff (Millwood) 32: (2) ((2013) ), 216–222. doi:10.1377/hlthaff.2012.1064. |
[30] | Institute of Medicine (U.S.), Roundtable on value & science-driven health care, in: Patients Charting the Course: Citizen Engagement and the Learning Health System: Workshop Summary, L. Olsen, R.S. Saunders and J.M. McGinnis, eds, National Academies Press, Washington, D.C., (2011) . |
[31] | Institute of Medicine (U.S.), Committee on Quality of Health Care in America, Crossing the Quality Chasm: A New Health System for the 21st Century, National Academy Press, Washington, D.C., (2001) . |
[32] | D.N. Jackson, W.-Y.S. Chou, K.I. Coa, A. Oh and B. Hesse, Implications of social media use on health information technology engagement: Data from HINTS 4 cycle 3, Transl Behav Med 6: (4) ((2016) ), 566–576. doi:10.1007/s13142-016-0437-1. |
[33] | S. Jiang and C.E. Beaudoin, Health literacy and the Internet: An exploratory study on the 2013 HINTS survey, Comp Human Behav. 58: ((2016) ), 240–248. doi:10.1016/j.chb.2016.01.007. |
[34] | D.W. Kemper and M. Mettler, Information Therapy: Prescribed Information as a Reimbursable Medical Service, 1st edn, Healthwise, Inc, Boise, Idaho, (2002) . |
[35] | S. Koch-Weser, Y.S. Bradshaw, L. Gualtieri and S.S. Gallagher, The Internet as a health information source: Findings from the 2007 health information national trends survey and implications for health communication, J Health Commun 15: (Supp 3) ((2010) ), 279–293. doi:10.1080/10810730.2010.522700. |
[36] | L.T. Kohn, J. Corrigan and M.S. Donaldson, To Err Is Human: Building a Safer Health System, National Academy Press, Washington, D.C., (2000) . |
[37] | A.T. Langford, K. Resnicow, J.S. Roberts and B.J. Zikmund-Fisher, Racial and ethnic differences in direct-to-consumer genetic tests awareness in HINTS 2007: Sociodemographic and numeracy correlates, Journal of Genetic Counseling 21: (3) ((2012) ), 440–447. doi:10.1007/s10897-011-9478-2. |
[38] | J.A. Manganello and M.L. Clayman, The association of understanding of medical statistics with health information seeking and health provider interaction in a national sample of young adults, J Health Commun 16: (Supp 3) ((2011) ), 163–176. doi:10.1080/10810730.2011.604704. |
[39] | W.L. Nelson, R.P. Moser and P.K.J. Han, Exploring objective and subjective numeracy at a population level: Findings from the 2007 health information national trends survey (HINTS), J Health Commun 18: (2) ((2013) ), 192–205. doi:10.1080/10810730.2012.688450. |
[40] | L. Nielsen-Bohlman and Institute of Medicine (U.S.), Committee on Health Literacy, Health Literacy: A Prescription to End Confusion, National Academies Press, Washington, D.C., (2004) . |
[41] | D.A. Norman, The Design of Everyday Things, Revised and expanded edn, Basic Books, New York, New York, (2013) . |
[42] | B. Obama, Presidential memorandum – Expanding broadband deployment and adoption by addressing regulatory barriers and encouraging investment and training, 2015. |
[43] | P.P. Reid, W.D. Compton, J.H. Grossman, G. Fanjiang, National Academy of Engineering, Institute of Medicine (U.S.), et al.. Building a Better Delivery System: A New Engineering/Health Care Partnership, National Academies Press, Washington, D.C., (2005) . |
[44] | E.M. Rogers, Diffusion of Innovation, 4th edn, The Free Press, New York, NY, (1995) . |
[45] | S.G. Smith, M.S. Wolf and C.v. Wagner, Socioeconomic status, statistical confidence, and patient–provider communication: An analysis of the health information national trends survey (HINTS 2007), J Health Commun 15: (Supp 3) ((2010) ), 169–185. doi:10.1080/10810730.2010.522690. |
[46] | D. Stokols, J.G. Grzywacz, S. McMahan and K. Phillips, Increasing the health promotive capacity of human environments, Am J Health Promot 18: (1) ((2003) ), 4–13. doi:10.4278/0890-1171-18.1.4. |
[47] | U.S. Department of Health and Human Services, Healthy people 2010, U.S. Department of Health and Human Services, Washington, DC, 2000. |
[48] | K.J. Vicente, The Human Factor: Revolutionizing the Way People Live with Technology, 1st edn, Taylor and Francis Books, New York, (2003) . |
[49] | C. Zarcadoolas, A. Pleasant and D.S. Greer, Understanding health literacy: An expanded model, Health Promotion International 20: (2) ((2005) ), 195–203. doi:10.1093/heapro/dah609. |
[50] | S. Zuboff and J. Maxmin, The Support Economy: Why Corporations Are Failing Individuals and the Next Episode of Capitalism, Viking, New York, (2002) . |




