Integrating participatory design and health literacy to improve research and interventions
Abstract
Health communication is an essential health promotion strategy to convert scientific findings into actionable, empowering information for the public. Health communication interventions have shown positive outcomes, but many efforts have been disappointing. A key weakness is that expert-designed health communication is often overly generic and not adequately aligned with the abilities, preferences and life situations of specific audiences. The emergence of the field of health literacy is providing powerful theoretical guidance and practice strategies. Health literacy, in concert with other determinants of health, has greatly advanced understanding of factors that facilitate or hinder health promotion at individual, organizational and community settings. However, health literacy models are incomplete and interventions have shown only modest success to date. A challenge is to move beyond the current focus on individual comprehension and address deeper factors of motivation, self-efficacy and empowerment, as well as socio-environmental influences, and their impact to improve health outcomes and reduce health disparities.
Integrating participatory design theory and methods drawn from social sciences and design sciences can significantly improve health literacy models and interventions. Likewise, researchers and practitioners using participatory design can greatly benefit from incorporating health literacy principles into their efforts. Such interventions at multiple levels are showing positive health outcomes and reduction of health disparities, but this approach is complex and not yet widespread. This article focuses on research findings about health literacy and participatory design to improve health promotion, and practical guidance and case examples for researchers, practitioners and policymakers.
1.Introduction: Determinants of health, health disparities and health equity
People’s health is thought to promoted – or hindered – by a wide range of determinants. Under the traditional “medical model,” “health” was equated primarily with physical determinants and has had a strong focus on providing healthcare to identify and treat diseases. Since the last century, substantial research indicates that social, behavioral, economic, structural and environmental factors are even more predictive of people’s health over the course of their lives [26,64,103,122]. Research on social determinants of health typically examines socio-economic status, age, gender, sexual orientation, disabilities, race and ethnicity (including discrimination and cultural beliefs and behaviors), educational levels, neighborhood conditions and many other factors. Structural determinants have been identified that impact people’s health, such as access to health insurance and healthcare, provision of understandable information, quality of health care and patient-provider interactions, patient engagement in health care, medication adherence, health care costs, etc.
Determinants are hypothesized to operate within the public health “social-ecological” model at multiple individual, family, interpersonal, neighborhood, institutional, cultural and societal levels over the life course [12,108,109]. Individual determinants can operate within and across multiple levels, and interact with other determinants [59]. For example, the social determinant of race can interact with the structural determinant of healthcare access across individual, organizational and other levels. These interactions can be associated with multiple health outcomes such as early detection of disease and treatment. Although overall population health is improving over time, not all groups benefit equally, and among some groups, health outcomes can decline [22]. These health differences are referred to as “health disparities” (or “health inequalities”) defined by the US Department of Health and Human Services [114] as:
A type of difference in health that is closely linked with social or economic disadvantage. Health disparities negatively affect groups of people who have systematically experienced greater social or economic obstacles to health. These obstacles stem from characteristics historically linked to discrimination or exclusion such as race or ethnicity, religion, socioeconomic status, gender, mental health, sexual orientation, or geographic location. Other characteristics include cognitive, sensory, or physical disability.
There are wide health disparities/inequalities among groups, such as birth outcomes for White vs. African American women [30]. Even though exact causal pathways are difficult to identify, research indicates that few such disparities are naturally occurring because of innate genetic, or other individual differences, or non-equal group comparisons (health of older vs younger adults), but rather by interlocking external factors related to the physical and social environments [65,86]. A disparity in health outcomes that is systematic, avoidable, and unjust is frequently referred to as a “health inequity” [11,31]. A major public health and social justice goal is to improve health, [52,63,64,81,92,122] which can be defined as a state in which people have “the opportunity to attain their full health potential and no one is disadvantaged from achieving this potential because of their social position or other socially-determined circumstances” [11].
Researchers are studying how the determinants of health interrelate and impact health positively or negatively. This is a daunting challenge, given the complex web of determinants that co-interact across many dimensions. However, studies are increasingly identifying powerful health predictors. Marmot’s landmark Whitehall study of British civil servants showed that “sense of control” over work and life issues was the strongest predictor of the major differences in the health status gradient from high- to low-level workers [64] – a finding that has now been corroborated across studies worldwide. Sense of control can also be referred to as “empowerment” and is linked with “self-efficacy” [7,103]. Although socio-economic status is closely associated with empowerment – and is difficult to change – there are important public health opportunities to increase empowerment and health through health promotion interventions.
2.Health promotion and health communication
Health communication is a key health promotion strategy to convert scientific findings into actionable, empowering information for the public. Health communication can be defined as “the central social process in the provision of health care delivery and the promotion of public health” [48]. Health communication is highly interdisciplinary and interacts with many disciplines, such as public health, education, medicine, mass communication, information science, sociology, engineering, etc. Health communication comprises or interacts with many areas: mass-media and tailored health information (in multiple media formats), electronic health information, bio-informatics, m-health, health campaigns, patient-provider communication, etc. [72,73]. In this article, “health communication” refers to health research and interventions that have a core communication component, such as most health literacy initiatives.
Health communication is critical not only to improve health for the overall population, but also for socially disadvantaged groups who face barriers due to information access, including literacy/digital literacy, language, culture, discrimination, geographic location, disability, social isolation, low healthcare access or other factors. Health communication research over the past half-century provides strong evidence that well-crafted health communication efforts can help reduce health risks, disease incidence, morbidity, and mortality, as well as improve quality of life by enabling people to make informed health decisions [31,57,72,73]. However, it also shows that many health communication efforts have had disappointing outcomes and that some have even shown unintended negative consequences and have been linked with widening health inequities [17,31,57,72,73,106,118].
A key weakness of traditional health communication is that it is often overly generic and not adequately aligned with the abilities, preferences and life situations of specific audiences [32,50,51,57,73]. These weaknesses are greatly magnified for marginalized and at-risk populations who may require significant adaptation for communication content, format, and delivery [49,71]. Unfortunately, health messages for such groups are often presented in ways that are overly technical, complex, and abstract from the experience of the intended beneficiaries. Also, much health communication focuses on rational, didactic messages that overlook emotional factors, like empathy and motivation [24,25,57,72,120]. Further, expert-designed. science-based messages may not be actionable, especially for people who face many barriers in their social contexts. For example, messages that encourage people to go out and exercise, may not work if they live in unsafe neighborhoods. Likewise, communication that is available only through electronic media can disadvantage groups without such access – and may increase health disparities. Taken together, these many problems can limit the overall effectiveness of health communication efforts, especially for those groups most in need. An underlying problem is the lack of intensive participation with the intended beneficiaries [40,50,57,72].
Over the past three decades, researchers and practitioners have been drawing on research findings to strengthen traditional health communication strategies, including 1) audience analyses; 2) message design and testing with the intended audiences; 3) selection of appropriate mass communication channels (especially new media) and credible mediators for messages; and 4) more rigorous evaluation of health communication interventions [49]. Logan [57] describes conceptual and methodological shifts in health campaigns moving “from a one-way expert-to-recipient model to a range of broader interactive activities for health promotion, education, engagement, and collaboration that use diverse mass media tools and services.”
This article focuses on two other major developments during the past 20–30 years: the creation of the field of health literacy, and the increased use of participatory design, to improve health research, interventions, policy and health equity. The specific objectives of this article are to explore 1) associations between determinants of health, health disparities and health communication interventions; 2) definitions and dimensions of health literacy and its importance to improve health communication; 3) gaps in health literacy research and practice; 4) participatory design theory and methods and their value to improve health communication and health literacy interventions; 5) case examples about integrating participatory design and health literacy to improve health interventions and health equity; and 6) recommendations and new directions for researchers, practitioners and policymakers.
3.The evolution of health literacy
During the past three decades, health literacy has emerged as a critical area to advance health research, communication interventions, population health and health equity. This new field has grown in response to accumulating research showing that people’s knowledge and competencies related to accessing, understanding and using health information within their social contexts is significantly correlated with their health decisions and health outcomes. Major catalysts to the field’s development began with early observations that adults’ skills related to understanding and using health information seemed closely related, but distinct, from their general literacy skills [29].
In 2003, the National Assessment of Adult Literacy (NAAL), a national population-based survey, examined both adult literacy and health literacy skills and confirming that adult literacy and health-related literacy skills, although associated, were separate research constructs [55,121]. Findings showed that health literacy is significantly associated with many socio-demographic determinants of health including race, ethnicity, income, educational attainment and age. The survey also found that only 12% of US adults were estimated to have the “proficient” skills necessary to understand and use health information within the demands of health systems. Importantly, research indicated that health literacy can be an independent risk factor or determinant of health [5].
Health literacy has become an issue of national concern, prompting major research efforts to define and model this concept. Research findings have also motivated national and international “calls to action” about health literacy and interventions to address health literacy problems. Health literacy scholars have traced key events in the development of health literacy research, policy and interventions [47,58,83,85]. Research in other countries also indicates low levels of health literacy and increasing efforts to improve it [107]. Definitions, conceptual models and dimensions of health literacy have been constantly evolving and now cover a broad array of factors at individual, interpersonal, organizational, community and societal levels. Health literacy is highly interdisciplinary; it draws guidance from public health, medicine, psychology, education, communication, sociology, anthropology, architecture, and many other disciplines and their sub-fields. It operates in all societal sectors as illustrated in socio-ecological models.
3.1.Definitions
An early definition of health literacy from the World Health Organization [127] is “The cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand, and use information in ways which promote and maintain good health.” The American Medical Association [1] defined it as “The constellation of skills, including the ability to perform basic reading and numerical tasks required to function in the healthcare environment.” In 2004, the US Institute of Medicine (IOM) – now the National Academies of Science, Engineering and Medicine – advocated for a definition that has become the most standard one in the US: “the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions” [44]. Nutbeam [82] proposed three levels of competencies related to health literacy. In the lowest basic or “functional” level, an individual has a fundamental understanding of a health problem and the ability to comply with prescribed actions to remedy the problem. At an “interactive” level, a person has more advanced knowledge and skills to function in everyday society and the ability to seek out information in order to respond to changing needs. At the highest or “critical” level, a person has a significant level of knowledge, personal skills and confidence to manage their health, and the ability to take action to change the determinants of health in the environment.
Although early definitions focused on individual skills, the importance of contextual factors has been increasingly emphasized. For example, in its 2003 action plan objectives for Healthy People 2010, the U.S. Department of Health and Human Services emphasized that the concept of health literacy not only involves patients, but also providers, and organizations [113]. Although the IOM/NAM report proposed the above definition focused on individual skills, the report also acknowledged that health literacy is an interaction between the skills of individuals and the demands of health systems, and that there is a notable mismatch between them. The trend toward more contextual definitions highlights the multiple dimensions of health literacy, including the skills of healthcare providers to present information to individuals in a way that is understandable and actionable. The Calgary Charter [15] defined health literacy as:
Health literacy allows the public and personnel working in all health-related contexts to find, understand, evaluate, communicate, and use information.
Health literacy is the use of a wide range of skills that improve the ability of people to act on information in order to live healthier lives.
These skills include reading, writing, listening, speaking, numeracy, and critical analysis, as well as communication and interaction skills.
In addition to increasing emphasis on interpersonal interactions between individuals and health educators and other providers, health literacy definitions are also highlighting the importance of healthcare and other community contexts. Kickbush and colleagues [46] proposed this definition: “The ability to make sound health decision(s) in the context of everyday life – at home, in the community, at the workplace, the healthcare system, the market place and the political arena. It is a critical empowerment strategy to increase people’s control over their health, their ability to seek out information and their ability to take responsibility.” This definition situates the phenomenon of health literacy within the public health social-ecological model, specifying the important associations of social and structural determinants of health. A new focus is to identify attributes of “health literate” healthcare institutions based on the degree to which they provide equal, easy, and shame-free access to and delivery of health care and health information [10,98]. Further, Freedman and colleagues [34] developed a definition for “public health literacy”: “the degree to which individuals and groups can obtain process, understand, evaluate, and act upon information needed to make public health decisions that benefit the community.”
In a systematic literature review, Sorensen and colleagues [107] identified 17 health literacy definitions. In their content analysis, they condensed definitions to six cluster areas: (1) competence, skills, abilities (cognitive, social, personal and communication skills, motivation, etc.); (2) actions (accessing, understanding, processing and making decisions about health information, etc.); (3) information and resources (including kinds of health information in multiple formats, and health-related services, etc.); (4) objective (promoting/maintaining health, becoming empowered, making health decisions, interacting with healthcare environments, etc.); (5) context (healthcare, home, community, workplace and political settings, etc.); and (6) time (across the life course). In a 2016 National Academy of Medicine report, Pleasant and colleagues [90] commented on the multidisciplinary and multidimensional nature of health literacy. They advocated for the development of a new definition of health literacy that provides “a description of this multidimensionality; an explanation of a variety of settings and modes and media; and the unique psychological impact of health literacy on empowerment and health decisions.”
3.2.Health literacy models, dimensions and new directions
The evolution of health literacy definitions is linked to expanding conceptual health literacy models. In their 2012 systematic review, Sorensen and colleagues [107] identified 12 models and their dimensions and analyzed their similarities and differences. Models included many core health literacy factors: individual capacities related to knowledge, information access, reading, listening, speaking, numeracy, memory, healthcare navigation, and critical health decision-making. Some models incorporated behavioral factors such as health risk behaviors, use of healthcare, and medication adherence. These factors are considered important within the “medical health literacy” models that focus on individuals’ abilities for self-care and interacting effectively within healthcare systems. Other “public health literacy” models take a broader view and incorporate factors that go beyond personal health literacy factors to encompass determinants of health in a variety of societal situations [88]. These models have stronger emphasis on empowerment, advocacy, and group and community factors.
The models posit a wide range of antecedents and consequences of health literacy [107]. In addition to the above-mentioned capacities, antecedents include wide range of demographic, psychosocial, cultural, media use, past health experience/knowledge, social support, and social capital factors that influence a person or groups’ health literacy status. The models conceptualize that higher health literacy can result in more positive attitudes, higher motivation and self-efficacy, improved health status, improved health behaviors, lower healthcare costs, less frequent use of healthcare services, improved healthcare systems, etc. Consequences range from those at the individual level to community and societal levels, such as positive effects on social capital, intergenerational community empowerment, on (other) determinants of health, and on health equity.
The evolving definitions, conceptual models and dimensions are an impressive achievement for the relatively new field of health literacy, but important gaps remain. Sorensen and colleagues [107] suggest that these models can be improved to: 1) include more comprehensive factors related to existing knowledge about health literacy; 2) better integrate factors in “medical” and “public health” perspectives; 3) acknowledge that health literacy is not static, but rather changes over the life course; and 4) develop stronger causal pathways between antecedents and consequences [84]. They propose a new model (see their Fig. 1) that conceptualizes social, environmental, situational and personal determinants of health as antecedents, and health literacy as competencies to access, understand, appraise and apply health information as a patient in healthcare, disease prevention and health promotion domains. Their model includes individual, health system and societal consequences, with additional emphasis on empowerment, and notes that consequences reflect a process over the life course, and affect health sustainability and equity.
Just as Pleasant and colleagues [90] called for a new definition of health literacy that includes its unique psychological impact on empowerment and health decisions, conceptual frameworks should also illustrate how health literacy and other determinants of health promote or hinder motivation, empowerment, self-efficacy and behavior change. Although some health literacy conceptual frameworks include these factors either as an antecedent, a health literacy “capacity,” or a consequence of health literacy, the pathways are still vague, and many are still focused on cognitive, skills-based factors. Because some research shows that “patient activation” can compensate for low health literacy as an independent predictor of improved health behaviors, Hibbard [42] proposes that this factor be included in models. McCormack and colleagues [65] likewise call for expanding models to include various patient engagement factors.
As noted earlier, substantial research from the public health field of epidemiology shows that sense of control/empowerment is one of the strongest predictors of people’s health [64,103,122]. Therefore, epidemiological research and models can greatly contribute to building out health literacy models, as can research from other disciplines, like psychology [119] and behavioral sciences. Taking an even broader view, Logan [59] cites the need for an expanded, multidimensional conceptual framework that integrates health literacy and multiple other determinants of health to posit how they overlap and how they affect health disparities and health inequities. Because health literacy is a powerful determinant of health and mediates of determinants of health, a new model could identify unique health literacy pathways for interventions that could reduce health disparities.
4.Health literacy interventions
The new field of health literacy field has had impressive achievements over the past two decades: a growing evidence base of theoretical and empirical research; application of research into practical interventions; and advancement of policy mandates at local, national and global levels. As discussed earlier, health literacy research has created multiple conceptual frameworks with an increasing number of dimensions, causal pathways and measurable constructs. Research has also identified a large number of existing or refined instruments that can be used to examine health literacy variables. The most comprehensive listing of these instruments is Boston University’s Health Literacy Tool Shed accessible at: http://healthliteracy.bu.edu. As of 2016, the site included information on 125 tools that measure health literacy. Although the concept of health literacy emerged in the US, it has now spread globally. The ever-expanding number of scientific publications, health literacy conferences and associations, and research grants reflect the vitality of the field. Interest in the field has attracted investigators from many other disciplines who are enriching health literacy research from their perspectives.
Health literacy research has identified important relationships between health literacy levels and health knowledge, attitudes, behaviors, outcomes and disparities. According to a systematic review of the literature conducted the US Agency for Healthcare Research and Quality (AHRQ) [9], lower health literacy levels were “consistently associated with increased hospitalizations, greater emergency care use, lower use of mammography, lower receipt of influenza vaccine, poorer ability to demonstrate taking medications appropriately, poorer ability to interpret labels, health messages, and, among seniors, poorer overall health status and higher mortality.” The study concluded that “health literacy level potentially mediates disparities between blacks and whites.” Research is increasing indicating that health literacy can be considered as an independent predictor of health (a socially derived determinant of health) or as an intermediate variable that interacts with other social or structural determinants of health [5,9,59,60,111,125]. Most health literacy interventions to date are health communication initiatives focused in healthcare systems to provide easier-to-use health information, and to improve patient-provider communication and delivery of healthcare services.
The focus on redesigning health information was prompted by over 1,000 studies of health print materials (including medication labels) and websites showing that text readability significantly exceeded the estimated reading skills of the audiences for whom they were developed [23,67,78,99]. Strategies to design and assess “plain language” communications have been codified into health literacy principles that include reducing reading levels and improving syntax, cultural appropriateness, and format for easier comprehension. Descriptions of these recommended practices include those provided by the US Centers for Disease Control and Prevention CDC and AHRQ [14,27].
4.1.Results of health literacy interventions research
Although results are uneven, many studies of health information using health literacy principles show improvements in patients’ comprehension and/or behavioral outcomes [3,9,39,45,70,78,100,101,110,124,129]. Taggert and colleagues [112] found overall positive outcomes in health literacy and behavioral risk factor reduction among a wide variety of healthcare and community interventions. Another promising intervention area is applying health literacy strategies to improve medication adherence and medical device use. Some studies are showing that interventions that simplify medication labeling and instructions, combined with improved patient engagement are associated with better medication adherence and proper device use [4,9,91,100,104,105,124,128]. The US Food and Drug Administration and pharmaceutical companies are becoming increasingly active in health literacy research and interventions [33,77,104,126].
Although research about healthcare provider interactions with patients (“oral health literacy”) is at an early stage, a recommended technique is “teach back” (or, “teach to goal”) in which providers assess patient’s comprehension of important information and clarify it as needed, is showing some positive results [6,100]. Research about “health literate” systems and is nascent, but growing [97,98]. Likewise, community-level (“public health”) health literacy efforts are at an early stage, but are showing positive results [39,70,87–89]. Community-level interventions show promise to move health literacy efforts “upstream” to prevent disease and promote health.
The AHRQ [9] review assessed health literacy interventions among 42 interventions that met study design criteria. Among this relatively small pool of intervention studies, the review found uneven, and as yet “low” or “insufficient” evidence for efforts intended to redesign information for better comprehension. There was moderate evidence for positive effects of mixed interventions on healthcare use, intensive self-management interventions on behavior, and disease management interventions on disease prevalence/severity. Evidence was mixed and “insufficient” about the effects of health literacy interventions on knowledge, self-efficacy, and quality of life, and costs. The report suggested these priorities to advance the design features of interventions: testing novel approaches to increase motivation, techniques for delivering information orally or numerically, “work around” interventions such as patient advocates; determining the effective components of already-tested interventions; determining the cost-effectiveness of programs; and determining the effect of policy and practice interventions.
4.2.Gaps and new directions for health literacy interventions research
Overall, health literacy intervention research shows positive, but uneven results and an updated systematic review is needed to encompass more recent efforts. Examination of basic research and interventions research in health literacy indicates important gaps. Conceptual models need to be built out to incorporate more determinants of health and their relationship to health literacy factors, including identification of mediating and moderating variables that affect health outcomes and disparities. More examination is needed of non-cognitive variables, such as motivation and self-efficacy and their relationship to health behaviors and health/quality of life outcomes. For example, it has been frustrating to learn that even with all the important health literacy principles applied to health communications, not all “health literate” information has been shown to improve people’s comprehension, and evidence is still sparse about whether it significantly increases positive health behaviors. Health literacy design principles do not include all the factors that affect people’s interest in, comprehension of, motivation, and ability to use health information to make changes [77,78]. Similarly, “oral health literacy” interventions to improve patient-provider communication, do not always show significant outcomes in desired behaviors. This may be related to many factors, such as the patient’s anxiety in an examining room, non-verbal behavior of healthcare providers, lack of visual tools to accompany the oral communication, or lack of social support from a family member. Likewise, in these situations, a person’s health concerns may be secondary to other important issues they are dealing with in their lives.
Currently, important work is underway to define attributes of “health literate” healthcare settings engage and support patients [10]. These factors include recommendations from health literacy research such as improving the design of information resources, patient-provider communication, signage, etc. However, it will be challenging to identify many other factors that are not yet clear in the literature: What exactly is a “shame-free environment?” What colors, sounds, spaces and designs in the setting calm and engage people? How can information be presented in the setting that intrigues people to interact with it, search out their own questions, and become more “activated” to make and carry out health decisions? A deeper question is: How do researchers and practitioners even know what questions to ask? In my view, the lack of intensive participation of the users has been a major impediment to designing, implementing and evaluating more powerful health literacy interventions. The AHRQ report [9] recommends that investigators pilot test new interventions, but this is quite different from engaging users from the start as co-designers. Although health literacy models and principles offer helpful guidance and tools, researchers themselves cannot specifically define what helps or hinders people from making healthy changes within their multiple contexts and what actions would further health equity [60]. Fortunately, there is a growing body of research about the value of participatory design to improve health communication interventions, and some early guidance about applying these strategies to health literacy initiatives.
5.Participatory design
In 1978, at the Alma Ata Conference on Primary Health Care [123], WHO member states signed the first international declaration about the right to health and commitment to primary healthcare. This was also the first international declaration to emphasize the importance of participation. Point 10 specifies that primary healthcare “requires and promotes maximum community and individual self-reliance and participation in the planning, organization, operation and control of primary healthcare, making fullest use of local, national and other available resources; and to this end develops through appropriate education the ability of communities to participate.”
Since then, participation has been a core element of local, national and global health mandates. In the area of health communication/health literacy interventions, two decades of studies show that when users participate in designing and testing communication, outcomes are more successful, including those for vulnerable groups. Examples include: Hoy et al., Neuhauser & Kreps, Barton et al., Vaiana & McGlynn, Neuhauser, Wang, Vallance et al., Cooper et al., Gustafson et al., Minkler & Wallerstein, Logan, Hesse & Schneiderman, Neuhauser & Rothschild et al., Neuhauser & Kreps, Neuhauser & Kreps et al., Davis et al., Neuhauser, Kreps & Syme, Kreps & Sparks, Kreps & Neuhauser, Noar & Harrington, Schillinger et al., Wolf et al., Smith & Wallace, Yin et al., Arcia et al., Neuhauser & Constantine et al. [3,8,20,23,37,40,43,49,50,58,66,68,70,72,74–76,78,80,100,104,115,116,120,124,128]. An important outcome of many of these interventions is that they have been successful among groups that experience many health disparities, and thus can improve health equity. Despite the increasing evidence of the value of participatory design, intensive participatory processes are still not the norm in health communication/health literacy efforts. For example, in a systematic review of patient decision aids, Coulter and colleagues [21] found that only half the aids were tested with patients. Frequently, “participation” is limited to the important, but not sufficient, step of pilot testing interventions strategies initiated by researchers and/or practitioners – rather than by the users. Because many researchers and practitioners are not trained on the scientific value and specific strategies of intensive participatory design, it is useful to examine the theoretical foundation and empirical methods of participatory design.
5.1.Origin and scientific foundation of participatory design in social sciences
Theories and methods of participatory design have emerged over the past 60 years from multiple disciplinary roots. In the field of health promotion, participatory design is typically traced to its social science origins. Beginning in the middle of the last century, social scientists began to critique definitions and models of health as overly focused on clinical risk factors and medical treatment, rather than on broader health promotion within socio-ecological models, such as sociologist Aaron Antonovsky’s model of “salutogenesis” [2]. Scholars were also concerned about the tension between investigators’ agendas vs. people’s needs, such as researchers’ motivation to create constructs and publish papers rather than collaboratively engage in transformational actions to benefit groups. They thought the investigator-directed approach limited the theoretical understanding of conceptual models of health as well as empirical methods develop effective interventions. For example, Antonovsky criticized researcher-created health models as too focused on individual comprehension of health knowledge, rather motivational factors with social contexts.
Sociologist Kurt Lewin created the concept of “action research” in 1946 [56]. He described it as “a comparative research on the conditions and effects of various forms of social action and research leading to social action” that uses “a spiral of steps, each of which is composed of a circle of planning, action and fact-finding about the result of the action.” Reason and Bradbury [93] described action research as “an interactive inquiry process that balances problem solving actions implemented in a collaborative context with data-driven collaborative analysis or research to understand underlying causes enabling future predictions about personal and organizational change.” Related models that integrate highly collaborative research and action models include participatory action research and community-based participatory research [16,66,94]. These models emphasize “research for action” and “action for research, and engage researchers and community members as co-collaborators. They highlight the importance of using multiple qualitative methods in specific contexts, rather than quantitative methods to generalize research across contexts, as does traditional research. Action research, especially community-based participatory action research, generally involves long-term processes of community-researcher engagement, problem identification, reflection and intervention development, implementation and revision [66].
5.2.Origin and scientific foundation of participatory design in design sciences
Although researchers and practitioners in health communication/health literacy fields are more familiar with models and methods of participatory design derived from social sciences, participatory design also emerged in parallel through socio-technical sciences and offers important theoretical and methodological guidance. Architect and designer Buckminster Fuller introduced the term “design science” (the study of design) in 1963 [35]. Design science is considered one of three major categories of the systematic study of knowledge (epistemology); the others are the natural sciences and the human sciences [36]. In the natural sciences (e.g., physics, chemistry), researchers seek law-based explanations about phenomena in the natural world and assume that this knowledge can be generalized to multiple settings. This was the dominant scientific paradigm until the mid-20th century. At that time, the human, or interpretive, sciences emerged and are considered the second epistemological paradigm [28]. This research perspective includes social sciences and humanities, and acknowledges that because human phenomena are not as predictable or generalizable as are natural science laws, they should be studied using multiple methods in many settings [19].
Design sciences, or “sciences of the artificial” are concerned “not with how things are, but with how they might be” [102]. In design sciences, researchers study human-created (artificial) objects and phenomena intended to solve problems and meet goals. These artifacts can be symbols, material objects, activities, services, and learning or living environments [13] – such as health care and health literacy interventions. Design science fields include engineering, information systems, architecture, computer science and other primarily “socio-technical” fields. Because design sciences focus on things that do “not yet exist,” they specifically address the so-called “wicked” nature of problems [13]. In this situation, problem understanding and problem solving should happen concurrently, and there is no end to identifying problems and refining designs. Therefore, researchers should not predict solutions or hypothesize outcomes too early, but rather conduct iterative, problem identification-problem solution processes. Because of their complexity across social-ecological contexts, most health problems, such as those related to health literacy, can be considered “wicked.”
The epistemological differences between design sciences, and natural and human sciences are reflected in differences in research goals, overall research design and methods [61]. Because the goal of design science inquiry is on inductive problem solving, research is focused on studying processes to arrive at a solution. In contrast, research in both the natural and human sciences is traditionally focused on predicting and testing theories. This is an important distinction because design science research is not aligned with the traditional requirements that researchers define theories, hypotheses, interventions and analysis plans before a project is funded. Human and design sciences overlap in the area of participatory action research in which health and social interventions are collaboratively developed and studied iteratively [66,75]. From the design science perspective, participatory (or user-centered) design has been defined as “an approach to the assessment, design and development of technological and organizational systems that places a premium on the active involvement of… potential or current users of the system in design and decision-making processes” [18].
5.3.Design science methods
There are also methodological differences among the three research paradigms. Methods in natural sciences are primarily observational and quantitative, whereas those in human science are more mixed, qualitative and researcher-participative. Design science methods are mostly qualitative, user-intensive, and emphasize “problem and solution” and “build and evaluate” loops [62], as shown in Fig. 1 [95].
Fig. 1.
The general design process (Roschuni, 2012). Celeste Nicole Roschuni. Reproduced by permission of Celeste Nicole Roschuni. Permission to reuse must be obtained from the rights holder.
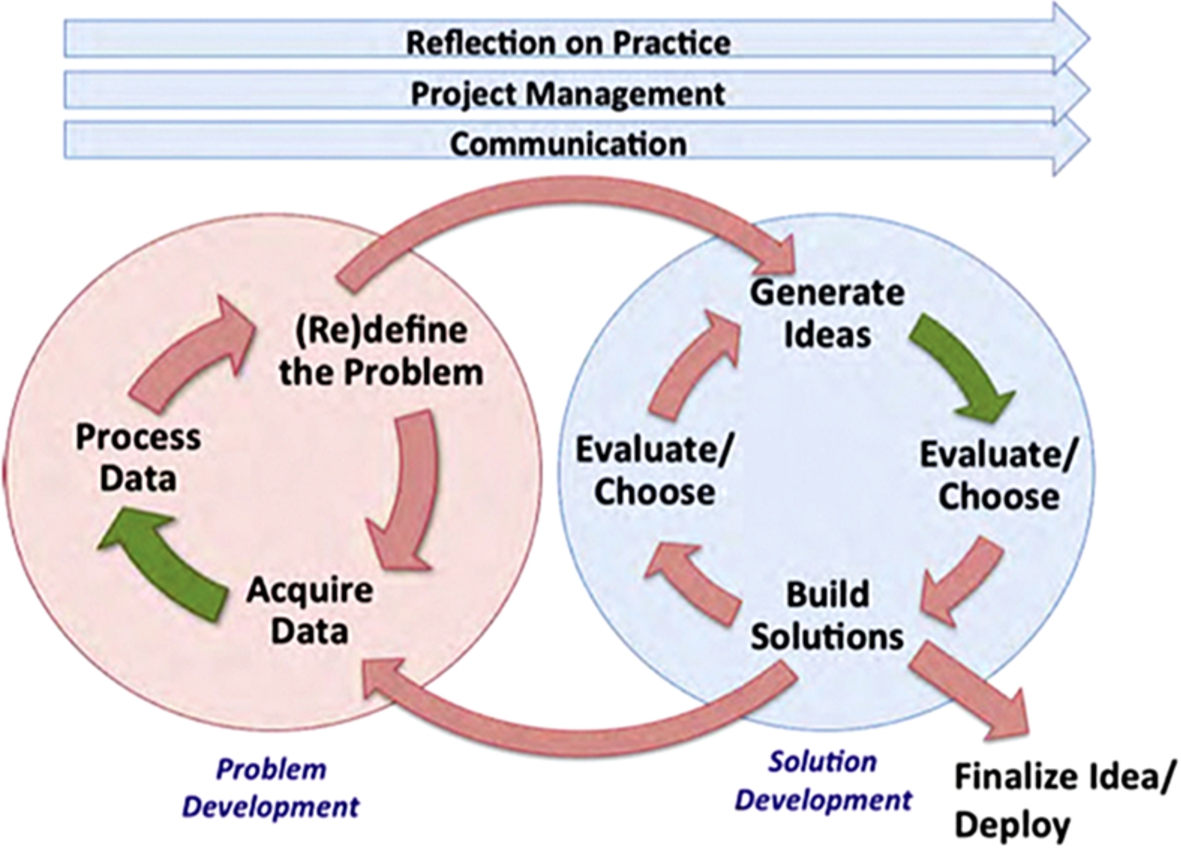
In the problem development cycle in Fig. 1, data are gathered from users and other sources, analyzed, and used to define problems and needs. In the solution development cycle, ideas are generated to build and test prototypes with users. Iterative feedback loops are used within and between the cycles. Although there is no theoretical end to problem identification and solution, there is a point where researchers and developers finalize and deploy a solution when it reaches the users’ key specifications. For example, for a health literacy materials-based intervention, user criteria might include content and format that are attractive, navigable, comprehensible, motivating, culturally appropriate, and actionable. In addition to involving users intensively, communication with other stakeholders is also important. A health literacy intervention might require that researchers, healthcare providers, members of community organizations, policymakers or others collaborate with users on the identification of specifications, barriers to implementation, and evaluation design. Evaluation and later revisions of the “solution” (prototype) continue over time using this process. Because design methods focus equally on building and evaluating solutions, evaluation is a continuous detailed process that starts at project initiation – in contrast with traditional “before” and “after” research designs. Although this conceptual model is intricate, it can guide rapid development of viable, user-designed solutions in a more pragmatic way than traditional approaches.
Design science as a form of scientific inquiry also subsumes the area known as “human factors research” which takes into consideration the interaction between the intended users and the products, systems or processes that are being designed – such as in engineering or medical informatics. Design science approaches are frequently referred to as “user-centered,” “human-centered,” or “human factors” design and include many techniques from multiple fields. “Usability testing” and “design thinking” are two commonly used methods. As mentioned earlier, even though participatory action research and community-based participatory research are traditionally considered under the human sciences branch of scientific inquiry, their methods often overlap, or are synergistic with, those in the design sciences. A positive trend is that researchers and practitioners from both human and design sciences are increasingly drawing on methods – outside their traditional disciplines – that share the commonality of engaging intended users in design and implementation. The Institute of Design at the University of California, Berkeley, is developing a repository of design methods called The Design Exchange (http://www.thedesignexchange.org) that will include many design methods and cases.
Design thinking methods originated at the Stanford University Institute of Design (http://dschool.stanford.edu) and include five stages: empathize with users, define issues, generate ideas, and prototype and test solutions. Note that the requirement to reach a deep level of empathy with users before moving on to other steps differs from traditional research strategies that begin with identifying problems. In early design thinking exercises, users and stakeholders engage in rapid problem and solution identification. These exercises are especially effective because both experts and end users participate as equals and processes are highly visual and interactive (i.e. teams draw solutions), rather than primarily cognitive and data-oriented, as in traditional health “program planning.” User-centered design is effective at individual, organizational, community and societal levels. Vechakul and colleagues [117] used these methods in a community-based project with new mothers.
Usability testing refers to a broad range of structured methods to engage users in designing communication materials [79,96]. Usability tests are often one-on-one situations that involve a tester asking a user to interact with a prototype, accomplish specific tasks related to it, and to recommend changes to it (such as to text, format, and graphics for a health communication resource). The prototype is then revised with participant input. Usability testing should continue until additional tests no longer elicit major new issues or recommendations. As participatory design becomes more widespread in health and social sciences, methods are being drawn from both the human and design sciences. One difference is that user-centered design processes are typically rapid cycles of problem identification and solution creation, whereas participatory action research emphasizes longer-term community engagement. Decisions about which approach to use and/or how to combine these approaches should be made collaboratively with participants in the specific context of a project.
6.Integrating participatory design and health literacy
As discussed earlier, two decades of research shows that participatory design strategies have improved health communication interventions, including health literacy efforts. Despite the promise of participatory design approaches in health literacy research and interventions, intensive participation is still not the norm. A problem is that health literacy researchers are typically trained in traditional research theory and methods in the human sciences. In this orientation, researchers typically build conceptual models, initiate theory-driven research, including a priori hypotheses, intervention design and analyses plans – as expected in the scientific community and as required by most funders. “Participation” may consist of pre-testing “health literate” information resources or patient engagement approaches, but is greatly limited by not having full user/stakeholder collaboration from the start. As a result, researchers often have less access to deep user/stakeholder input needed to build out better conceptual models and interventions.
The challenge to build out conceptual models of health literacy with better pathways related to the beliefs, habits, emotions, and motivations of intended users, and to apply these effectively to interventions is reflected in the modest and uneven results of health literacy efforts to date. Fortunately, health literacy researchers and practitioners are increasingly adopting participatory strategies and strengthening interventions, as demonstrated by the success of collaboratively designed health literacy initiatives to improve patient engagement and chronic disease management as mentioned earlier. Participatory design models and methods from both the social sciences and the design sciences provide important theoretical guidance and practical strategies for researchers and practitioners. Participatory action research, from the social sciences has begun to change how communities are engaged in research and action [66,93]. Because participatory action research is often a long-term process, it does not always align well with time constraints of many health literacy efforts. However, it is well suited to multi-year community health literacy initiatives. Design science theory and approaches are less familiar to health communication and health literacy researchers and practitioners, but offer powerful new opportunities to advance health literacy efforts relatively quickly.
In addition, health literacy models and principles can greatly improve the work of those using participatory design. Developers of electronic health communication apps generally intensely involve users during iterative design phases, but may not be familiar with guidance from health literacy research and practice that can assess and improve user comprehension and navigation. This was demonstrated at the 2011 Stanford University Artificial Intelligence and Health Communication conference. Computer science developers had created amazing health avatars and other interactive programs, but some showed disappointing results when used in interventions. Health literacy scholars at the conference pointed out problems with the high reading level (college), and lack of adherence to other important health literacy principles [75]. Nor are developers in the information sciences necessarily familiar with the many psycho-social factors that affect health. Hevner and colleagues [41] called for “synergistic efforts between behavioral science and design science researchers.” Similarly, researchers and practitioners involved in community interventions can significantly benefit from incorporating health literacy guidance, as described in cases below. Although evidence is increasing about the value of integrating health literacy and participatory design strategies in health interventions, there is a lack of detailed guidance for researchers, developers and practitioners about how to do so in a way that gets to the deep personal and contextual levels needed for scientific inquiry and successful interventions.
7.Strategies to integrate participatory design and health literacy
This section offers suggestions and case examples drawn from my 25 years of experience – and those of my colleagues – to integrate participatory design and health communication/health literacy. Most of my work has been done through the Health Research for Action center (HRA) at the University of California, Berkeley School of Public Health (http://www.healthresearchforaction.org). Center staff include multi-disciplinary researchers, communication/health literacy experts, public health practitioners, and policy scholars who have collaborated with thousands of local, national and global partners on health promotion over two decades. Staff work in interdisciplinary teams and use highly participatory methods with healthcare organizations, communities, government, and private industry. Our staff has been intensively involved in co-designing, co-implementing and co-evaluating health communication/health literacy interventions. Although participatory design processes must be selected and tailored to the specific project, we recommend the following six summary steps related to designing and testing health communication resources [76]. Each of the following steps should be documented as part of the formal evaluation.
1. Identify participants and set up an advisory committee. Participants include end-users, and subgroups of users, researchers and all relevant stakeholder groups, such as health and social service providers, community groups, government officials, policymakers, funders, media, etc. Consider establishing an advisory committee with representatives of participant groups to guide the project.
2. Conduct formative work with participants using varied participatory methods. Gather information from participant groups and research studies to co-identify problems and potential solutions. Use multiple formative methods, such as design thinking exercises, focus groups, surveys, health literacy assessments of existing resources, etc. Examine results with the advisory committee to iteratively define and refine project goals and strategies.
3. Draft health communication resources adhering to health literacy principles; develop initial dissemination plans. Co-develop new communication resources drawing on formative research, specific health literacy principles, and participant input. Begin developing plans to disseminate the resources; include advisory committee members and other relevant end-users, providers, funders, etc. in the planning. Design thinking exercises are especially useful to foster creativity.
4. Iteratively test and revise communication prototypes and implementation plans with intended users and stakeholders. Usability test and revise prototypes with subgroups of end-users over multiple rounds until participants approve them; incorporate expert review for content accuracy. Use design thinking or other strategies with users and stakeholders to refine the implementation plan.
5. Continuously evaluate and revise the health communication resource. During implementation, gather feedback from relevant users and stakeholders about the acceptance, use and effectiveness of the health communication resource and its implementation. Revise approaches as needed. Gather data using mixed qualitative and quantitative methods, such as interviews, design thinking exercises, focus groups, on-site observations, surveys, randomized trials, etc. Tailor reports to the communication abilities and preferences of audiences (scientific publications, user-tested brief reports, etc.).
6. Sustain and extend successful programs to other populations or regions. Use participatory methods to continuously identify problems and refine the intervention. Go through the above steps to adapt the health communication intervention to new population groups, and new social and geographical contexts. If the initial intervention is well crafted with intense participatory design and detailed documentation, adaptation elsewhere is typically easier and less expensive [69,70].
8.Case studies
8.1.Participatory development of mass communication for Medicaid beneficiaries
The problem: in the US, highly vulnerable populations like seniors and people with disabilities participating in Medicaid (a US program for low-income beneficiaries) are required to make complex choices to select a health plan. In California in 2008, only 25% of these beneficiaries made active choices, given the major communication barriers they faced related to literacy, language, culture and disabilities and the overly complex document about health plans that they were expected to comprehend [38]. The State of California engaged our HRA staff to work closely with Medicaid beneficiaries and stakeholders to create a guidebook that would meet their needs.
We followed all the above steps to: identify and engage user subgroups and stakeholders; establish an Advisory Group; set health literacy and cultural competency standards and iteratively test and refine prototypes of the What Are My Medi-Cal Choices guide; adapt the final version into 13 languages; disseminate it to hundreds of thousands of beneficiaries; and evaluate the processes and outcomes. See Neuhauser & Rothschild et al. [78] for details including the use multiple participatory methods (in-depth interviews, Advisory Group feedback, usability testing, health literacy assessments, and quantitative evaluation). The integration of health literacy principles and continuous participatory design transformed the initial ineffective state resource into a successful guide that met highly nuanced needs and preferences of intended users. In addition, the project integrated qualitative methods with a randomized-controlled trial to examine efficacy [54]. The model has now been adapted to multiple health communication interventions for people on Medicaid. Among many lessons learned, we noted that even when a prototype guide adhered to all currently accepted health literacy principles, users proposed making further changes to about one-third to one-half of the document to suit their needs and preferences.
8.2.Participatory design of a community wellness project with Chinese factory workers
The problem: China has an estimated over 250 million “migrant workers” who are moving from rural areas into industrial zones. Most of the migrants are young, have low education levels (average 7th grade) and struggle to adjust to factory jobs in urban areas. These workers one of the most vulnerable groups in China, and have little knowledge about health issues or how to access health and social services. They suffer from high rates of depression, infectious diseases and unplanned pregnancies and abortions. Taking a broader view of “health,” the workers also have little knowledge about their rights at work and as non-residents of their new city, and they struggle to handle life issues (education, housing, social life, etc.). They feel they have few opportunities to change work or city policies.
Although supporting these workers is a key objective of the Chinese government, their “top down” efforts to engage workers have shown disappointing results. One reason is that the concept of health has been mostly focused on physical health and service access, rather than the broader social, structural and environmental determinants of health – especially worker empowerment. In 2011, HRA staff were invited by national and local government officials to apply our participatory design process to co-develop a project to support factory workers in Changzhou, a large industrial city with 1.5 million migrant workers. We were invited based on the success of our participatory efforts to work with Chinese Americans in California. That project created the Chinese Wellness Guide using the above steps.
We adapted the above six steps to the Changzhou context. Our first step was get “buy-in” about the participatory approach from key national and local government officials, health and social service providers, researchers from a local university, factory managers and others. To do that, our team conducted three participatory workshops over a one-year period to introduce the concepts of multiple determinants of health and the power of participatory design. Participants examined baseline research about workers’ health and social issues and then mapped out >50 determinants of health. Surprisingly, these determinants included low health literacy – not a common concept as yet in China. After securing buy-in and enthusiasm from these decision-makers, teams of workers from two factories joined the project. Several advisory committees were established including all worker and stakeholder groups who then identified problems and solutions. Though these processes, participants defined three novel interventions: creation of an easy-to-use Changzhou Wellness Guide covering a broad range of health and social issues, service access, tips for managing life issues; a “Wellness House” in each factory where workers could socialize, solve problems, and attend trainings; and a buddy system in which established workers help new workers.
The Changzhou Wellness Guide was created using the above steps. HRA health literacy experts trained participants on health literacy principles and iterative testing and revisions of prototypes. Workers and stakeholders created guide content and formatting and conducted multiple rounds of user testing and expert feedback. Professional stakeholders were amazed at the creativity, depth and practicality of workers’ ideas. After initial publication and use over one year, workers and stakeholders have revised the guide, using the same participatory methods and adhering to health literacy principles. In 2016, the project won the Institute for Healthcare Advancement’s International Award for Outstanding Achievement in Health Literacy. The project has expanded to 27 factories, each of which is using participatory design to contribute to the next edition of the guide and to create other interventions and catalyze city-wide policy changes. Researchers from the local university and HRA are collaborating with all participant groups (including workers) to design and conduct research about the process and effectiveness of the project. Early research findings suggest significant increases in worker knowledge, confidence, service connections and positive health behaviors.
We learned key lessons from this project. It was important to ground the project in a social-ecological model with comprehensive determinants of health, including health literacy. This project is also a good example of why health literacy factors are essential to consider in participatory projects and why participatory methods are essential to consider in health literacy projects – where health literacy issues must be explored by users in their contexts. Empowerment of workers, a core goal of this project, emerged through intensive participatory methods, and the gradual development of interventions they created. The key lesson is that if end users are engaged to create and implement interventions themselves, they will do so in a way that incorporates many highly nuanced factors that are not codified into health literacy design principles. They will also design interventions that take into consideration many social, structural and environmental determinants of health that affect them, but may not be obvious to researchers or practitioners, or included in a health literacy model.
For example, factory workers cited the lack of summer school opportunities for their children as an overarching problem that determined whether they would have to leave the factory before the summer. For many workers, this problem greatly superseded health problems. They solved the problem by advocating for and developing summer schools in the factories. Government stakeholders, disappointed by outcomes of prior projects, are eagerly embracing the participatory approach and the value of health literacy principles. Workers in the original project factories are now engaging with those in new factories to share methods and ideas. Our HRA team was able to offer guidance about health determinants, health literacy, participatory design and research through periodic visits, without “running” the project, as happens in many researcher-controlled projects. Because this is a long-term project, it is an example of integrating participatory action research and design science methods, and it spans both “medical” and “public health” health literacy models.
8.3.ChronologyMD mobile app
Crohn’s disease is a serious, incurable inflammatory bowel disease that affects over 600,000 people in the US. Good patient-provider communication about disease symptoms and severity is critical, but it is difficult for patients to keep track of multiple symptoms accurately each day and for their physicians to make life-saving treatment decisions based on that information. The ChronologyMD project used design science methods, health literacy principles and artificial intelligence components to engage patients with Crohn’s disease and their healthcare providers [75]. The project used a wide variety of participatory methods to enable patients with Crohn’s disease create a mobile application that would track their detailed “observations of daily living,” including symptoms and severity, mood, medication adherence, and behaviors (exercise, diet, etc.) to take more control over their health. Through artificial intelligence components, the app also passively collected biometric data, such as weight and sleep patterns, via connected wireless devices. With the participation of the patients’ healthcare providers, a second app was created to display these data over time to improve shared decision-making with patients.
Intensive participatory design methods were necessary to create the highly refined features that patients and providers needed for the information to be effective in managing Crohn’s disease. In addition, patients wanted and received an app that allowed them to design their own “observations of daily living” over time and assess interactions among variables such as symptoms, medication taking and behaviors. From a health literacy perspective, this highly iterative approach helped identify and address many communication barriers, such as easily inputting and understanding quantitative data (medication amounts, pain levels), and having simple displays of key information that could be understood quickly by patients and providers. Because of the iterative nature of the design, evaluation methods were also continuously revised so that interim findings could be used to constantly improve the intervention (as is done in the “build and evaluate” loops mentioned earlier). Findings from the pilot evaluation showed that the app enabled patients to greatly increase their input of symptoms and other data, better understand factors that helped or hindered their condition, and make positive changes. It also helped both patients and providers improve the quality of clinical encounters and shared decision-making. An important project lesson was that understanding of health literacy factors is at an early stage in the emerging and powerful field of artificial intelligence and health communication, and that participatory design is essential to every step of development.
8.4.Other participatory health literacy projects
Statewide Parenting Education Kits. Participatory design and health literacy principles were used to create parenting education kits in five languages delivered to over 300,000 parents each year in California [70]. The project engaged many subgroups of parents with special attention to those with lower-income and/or lower-literacy. Statewide evaluation showed positive changes in knowledge and behaviors. The model has been adapted, using participatory processes, to other US states and in Australia. Participatory design activities are now underway to adapt printed information into Internet and mobile platforms.
Maternity Leave Resources for Pregnant Women. English and Spanish-speaking pregnant women on Medicaid co-designed easy-to-understand resources [53]. In-person user testing uncovered and addressed many health literacy and motivational issues, even though first drafts were developed with detailed attention to health literacy principles and tested as “superior” on standardized health literacy assessments. Similar to what we found in the development of the Medicaid choices guide mentioned earlier, health literacy principles accounted for about half of what users wanted; the other half of changes covered a wide range of factors related to attractiveness, cultural appropriateness, subtleties of document “tone,” types of graphics and their placement, resources for more help, etc.
Emergency Preparedness Communication for Deaf and Hard-of-Hearing Populations. Because people who are Deaf tend to have especially low literacy levels, and Deaf and hard-of-hearing groups have many barriers to spoken communication, major changes are needed to adapt preparedness communication to their needs. The project used intensive participatory design and health literacy principles to recommend changes to communications, including those in American Sign Language, use of captioning, etc. [71]. There is little guidance to date about health literacy factors related to communications for people who are Deaf. For example: what determines users’ comprehension of information communicated by mobile video? This area needs development through participatory design.
9.Conclusions
The emergence of the field of health literacy and the increased use of intensive participatory design are transforming theoretical guidance and empirical methods to improve health communication research and interventions. Health literacy, in association with other determinants of health, has greatly advanced our understanding of what affects people’s health and intervention opportunities to address those factors. Because health literacy has been shown to mediate other determinants of health, it offers new practical pathways to positively impact people’s health even without changes to intractable determinants of health, such as socio-economic status. Research on health literacy interventions has greatly advanced and shown positive, but uneven results to date. Participatory design theory and methods drawn from human/social sciences and design sciences can significantly improve health literacy models and interventions and vice versa. Participatory design is essential to understand deeper and elusive factors that impact health and specific ways to address them. If those most affected by these problems are not involved in identifying and addressing them, research models, interventions and broader policy changes will not likely improve.
Currently, most health literacy researchers and practitioners, such as those in public health, medicine, psychology, and communication, come from a social sciences perspective. However, the design sciences offer an existing, robust theoretical foundation that is currently underused. In my view, creating and studying health literacy interventions is especially well-aligned with the design sciences paradigm, given that intervention design relates to “what might be” rather than “what is.” The design sciences offer powerful techniques with demonstrated success in the socio-technical fields. Combining them with our current health literacy approaches is an important direction and requires that we cultivate an active, multi-disciplinary dialogue to share new ways of thinking about health literacy, designing interventions and researching their impact. Integrating health literacy and participatory design drawn from multiple scientific paradigms and methods is complex and as much an art as a science. Multi-step models and case studies can help guide the work of researchers, practitioners, and policymakers in health communication/health literacy and those in many other fields committed to health promotion and health equity.
References
[1] | AMA Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, Health literacy: Report of the council on scientific affairs, JAMA. 281: (6) ((1999) ), 552–557. doi:10.1001/jama.281.6.552. |
[2] | A. Antonovsky, Health, Stress and Coping, Jossey-Bass, San Francisco, (1979) . |
[3] | A. Arcia, N. Suero-Tejeda, M.E. Bales, J.A. Merrill, S. Yoon, J. Woollen and S. Bakken, Sometimes more is more: Iterative participatory design of infographics for engagement of community members with varying levels of health literacy, J Am Med Inform Assoc. 23: (1) ((2016) ), 174–183. doi:10.1093/jamia/ocv079. |
[4] | S.C. Bailey, C.U. Oramasion and M.S. Wolf, Rethinking adherence: A health literacy-informed model of medication self-management, J Health Commun. 18: (Suppl 1) ((2013) ), 20–30. doi:10.1080/10810730.2013.825672. |
[5] | D.W. Baker, The associations between health literacy and health outcomes: Self-reported health, hospitalization, and mortality, in: Proceedings of the Surgeon General’s Workshop on Improving Health Literacy, Office of the Surgeon General (US), Rockville, MD, (2006) . |
[6] | D.W. Baker, D.A. DeWalt, D. Schillinger, B. Hawk, B. Ruo, K. Bibbins-Domingo, M. Weinberger, A. Macabasco-O’Connell and M. Pignone, “Teach to goal”: Theory and design principles of an intervention to improve heart failure self-management skills of patients with low health literacy, J Health Commun. 16: (Suppl 3) ((2011) ), 73–88. doi:10.1080/10810730.2011.604379. |
[7] | A. Bandura, Exercise of personal and collective efficacy, in: Self-Efficacy in Changing Societies, A. Bandura, ed., Cambridge University Press, New York, (1995) , pp. 1–45. doi:10.1017/CBO9780511527692.003. |
[8] | J.L. Barton, C.J. Kooenig, L. Trupin, J. Anderson, D. Ragouzeous, M. Breslin, T. Morse, D. Schillinger, V.M. Montori and E.H. Yelin, The design of a low literacy decision aid about rheumatoid arthritis medications in three languages for use during the clinical encounter, BMC Med Inform Decis Mak. 14: ((2014) ), 104. doi:10.1186/s12911-014-0104-8. |
[9] | N.D. Berkman, S.L. Sheridan, K.E. Donahue, D.J. Halpern, A. Viera, K. Crotty, A. Holland, M. Brasure, K.N. Lohr, E. Harden, E. Tant, I. Wallace and M. Viswanathan, Health literacy interventions and outcomes: An updated systematic review, Evidence Report/Technology Assessment No. 199, prepared by RTI International – University of North Carolina Evidence-based Practice Center under contract No. 290-2007-10056-I, AHRQ publication number 11-E006, Agency for Healthcare Research and Quality, Rockville, MD, 2011. |
[10] | C. Brach, D. Keller, L.M. Hernandez, C. Baur, R. Parker, B. Dreyer, P. Schyve, A.J. Lemerise and D. Schillinger, Ten Attributes of Health Literate Organizations, Institute of Medicine, National Academy of Sciences, National Academies Press, (2012) . |
[11] | P. Braveman and S. Gruskin, Defining equity in health, J Epidemiol Community Health. 57: (4) ((2003) ), 254–258. doi:10.1136/jech.57.4.254. |
[12] | U. Bronfenbrenner, Toward an experimental ecology of human development, Am Psychol. 32: ((1977) ), 513–531. doi:10.1037/0003-066X.32.7.513. |
[13] | R. Buchanan, Wicked problems in design thinking, Design Issues. 8: ((1992) ), 5–21. doi:10.2307/1511637. |
[14] | CDC (Centers for Disease Control and Prevention), Health literacy for public health professionals, 2011. Available at http://www.cdc.gov/healthliteracy/GetTrainingCE.html (accessed November 2016). |
[15] | Centre for Health Literacy, Calgary Charter, 2008. Available at http://www.centreforliteracy.qc.ca/health_literacy/calgary_charter. |
[16] | J.M. Chevalier and D.J. Buckles, Participatory Action Research: Theory and Methods for Engaged Inquiry, Routledge, London, (2013) . |
[17] | H. Cho and C.T. Salmon, Unintended effects of health communication campaigns, J Commun. 57: ((2007) ), 293–317. doi:10.1111/j.1460-2466.2007.00344.x. |
[18] | Computer Professionals for Social Responsibility, Participatory design, 2000. Available at http://cpsr.org/issues/pd/. |
[19] | T. Cook, Post positivist critical multiplism, in: Social Science and Social Policy, R. Shotland and M. Mark, eds, Sage, Beverly Hills, CA, (1985) , pp. 25–62. |
[20] | L.A. Cooper, M.C. Beach and S.L. Clever, Participatory decision-making in the medical encounter and its relationship to patient literacy, in: Understanding Health Literacy: Implications for Medicine and Public Health, J. Schwartzberg, J. VanGeest and C. Wang, eds, American Medical Association, Chicago, IL, (2005) , pp. 101–117. |
[21] | A. Coulter, D. Stilwell, J. Kryworuchko, P.D. Mullen, C.J. Ng and T. van der Weijden, A systematic development process for patient decision aids, BMC Med Inform Decis Mak. 13: (Suppl 2) ((2013) ), S2. doi:10.1186/1472-6947-13-S2-S2. |
[22] | J. Currie and H. Schwandt, Inequality in mortality decreased among the young while increasing for older adults, 1990–2010, Science. 352: (6286) ((2016) ), 708–712. doi:10.1126/science.aaf1437. |
[23] | T.C. Davis, R.F. Holcombe, H.J. Berkel, S. Pramanik and S.G. Divers, Informed consent for clinical trials: A comparative study of standard versus simplified forms, J Natl Cancer Inst. 90: (9) ((1998) ), 668–674. doi:10.1093/jnci/90.9.668. |
[24] | E. Deci and R. Ryan (eds), Handbook of Self-Determination Research, University of Rochester Press, Rochester, NY, (2002) . |
[25] | C. Dede and L. Fontana, Transforming health education via new media, in: Health and the New Media: Technologies Transforming Personal and Public Health, L.M. Harris, ed., Erlbaum, Hillsdale, NJ, (1995) , pp. 163–183. |
[26] | M. Denton, S. Prus and V. Walters, Gender differences in health: A Canadian study of the psychosocial, structural and behavioural determinants of health, Soc Sci Med. 58: ((2004) ), 2585–2600. doi:10.1016/j.socscimed.2003.09.008. |
[27] | D.A. DeWalt, L.F. Callahan, V.H. Hawk, K.A. Broucksou, A. Hink, R. Rudd and C. Brach, Health literacy universal precautions toolkit, 2010. Available at http://www.ahrq.gov/qual/literacy/healthliteracytoolkit.pdf (accessed November 2016). |
[28] | W. Dilthey, Introduction to the Human Sciences, Wayne State University Press, Detroit, MI, (1988) . |
[29] | L.G. Doak and C.C. Doak, Lowering the silent barriers for patients with low literacy skills, Promot Health. 8: (4) ((1987) ), 6–8. |
[30] | T.P. Dominguez, C. Dunkel-Schetter, L.M. Glynn, C. Hobel and C.A. Sandman, Racial differences in birth outcomes: The role of general, pregnancy, and racism stress, Health Psychol. 27: (2) ((2008) ), 194–203. doi:10.1037/0278-6133.27.2.194. |
[31] | M.J. Dutta and G.L. Kreps (eds), Reducing Health Disparities: Communication Interventions, Peter Lang Publishers, New York, (2013) . |
[32] | K.M. Emmons, Behavioral and social science contributions to the health of adults in the United States, in: Promoting Health: Intervention Strategies from Social and Behavioral Research, B. Smedley and S.L. Syme, eds, Institute of Medicine, National Academy Press, Washington, DC, (2000) , pp. 254–321. |
[33] | B. Fischoff, N.T. Brewer and J. Downs (eds), Communicating Risks and Benefits: An Evidence-Based User’s Guide, U.S. Department of Health and Human Services, Silver Spring, MD, Food and Drug Administration, Bethesda, MD, (2011) . |
[34] | D.A. Freedman, K.D. Bess, H.A. Tucker, D.L. Boyd, A.M. Tuchman and K.A. Wallston, Public health literacy defined, Am J Prev Med. 36: (5) ((2009) ), 446–451. doi:10.1016/j.amepre.2009.02.001. |
[35] | R.B. Fuller and J. McHale, World Design Science Decade, 1965–1975, Southern Illinois University, Carbondale, IL, (1963) . |
[36] | S. Gregor, Building theory in the science of the artificial, in: Proceedings of the 4th International Conference on Design Science Research in Information Systems and Technology, Association for Computing Machinery, New York, (2009) . |
[37] | D.H. Gustafson, R. Hawkins, E. Boberg et al., Impact of a patient-centered, computer-based health information/support system, Am J Prev Med. 16: (1) ((1999) ), 1–9. doi:10.1016/S0749-3797(98)00108-1. |
[38] | Health Research for Action, Year Two Report of the Medi-Cal Access Project, University of California, Berkeley, Berkeley, (2008) . |
[39] | A. Herman and P. Jackson, Empowering low-income parents with skills to reduce excess pediatric emergency room and clinic visits through a tailored low literacy training intervention, J Health Commun. 15: (8) ((2010) ), 895–910. doi:10.1080/10810730.2010.522228. |
[40] | B.W. Hesse and B. Schneiderman, eHealth research from the user’s perspective, Am J Prev Med. 32: ((2007) ), S97–S103. doi:10.1016/j.amepre.2007.01.019. |
[41] | A. Hevner, S. March, J. Park and S. Ram, Design science in information systems research, Management Information Systems Quarterly. 28: ((2004) ), 75–105. |
[42] | J. Hibbard, Patient activation and health literacy: What’s the difference? How do each contribute to health outcomes?, in: Health Literacy: New Directions in Research, Theory and Practice, R. Logan and E. Siegel, eds, IOS Press, Amsterdam, (2018) . To appear. |
[43] | E.W. Hoy, E. Kenney and A.C. Talavera, Engaging Consumers in Designing a Guide to Medi-Cal Managed Care Quality, California HealthCare Foundation, Oakland, (2004) . |
[44] | Institute of Medicine of the National Academies, Health Literacy: A Prescription to End Confusion, The National Academies, Washington, DC, (2004) . |
[45] | T.A. Jacobson, D.M. Thomas, F.J. Morton, G. Offutt, J. Shevlin and S. Ray, Use of a low-literacy patient education tool to enhance pneumococcal vaccination rates. A randomized controlled trial, JAMA. 282: (7) ((1999) ), 646–650. doi:10.1001/jama.282.7.646. |
[46] | I. Kickbusch and D. Maag, Health literacy, in: International Encyclopedia of Public Health, Vol. 3: , H. Kris and Q. Stella, eds, Academic Press, (2008) , pp. 204–211. doi:10.1016/B978-012373960-5.00584-0. |
[47] | H.K. Koh, D.M. Berwick, C.M. Clancy, C. Baur, C. Brach, L.M. Harris and E.G. Zerhusen, New federal policy initiatives to boost health literacy can help the nation move beyond the cycle of costly ‘crisis care’, Health Affairs. 31: ((2012) ), 434–443. doi:10.1377/hlthaff.2011.1169. |
[48] | G.L. Kreps, The pervasive role of information in health and health care: Implications for health communication policy, in: Communication Yearbook, Vol. 11: , J.A. Anderson, ed., Sage, Newbury Park, CA, (1988) , pp. 238–276. |
[49] | G.L. Kreps and L. Neuhauser, Designing health information programs to promote the health and well-being of vulnerable populations: The benefits of evidence-based strategic communication, in: Meeting Health Information Needs Outside of Healthcare: Opportunities and Challenges, C. Arnott Smith and A. Kesselman, eds, Chandos Publishing, (2015) , pp. 1–16. |
[50] | G.L. Kreps and L. Sparks, Meeting the health literacy needs of immigrant populations, Patient Educ Couns. 71: ((2008) ), 328–332. doi:10.1016/j.pec.2008.03.001. |
[51] | M.W. Kreuter and S.M. McClure, The role of culture in health communication, Annual Reviews of Public Health. 25: ((2004) ), 439–455. doi:10.1146/annurev.publhealth.25.101802.123000. |
[52] | N. Krieger et al., Racism, sexism and social class: Implications for studies of health, disease and well-being, Am J Prev Med. 9: (6 Suppl) ((1993) ), 82–122. |
[53] | E. Kurtovich, S. Guendelman, L. Neuhauser, D. Edelman, M. Georges and P. Mason-Marti, Development and first phase evaluation of a maternity leave educational tool for pregnant, working women in California, PLoS ONE. 10: , e0129472. doi:10.1371/journal.pone.0129472. |
[54] | E. Kurtovich, S. Ivey, L. Neuhauser and C. Graham, Evaluation of a multilingual mass communication intervention for seniors and people with disabilities on Medicaid: A randomized controlled trial, Health Serv Res. 45: (2) ((2010) ), 397–417. doi:10.1111/j.1475-6773.2009.01073.x. |
[55] | M. Kutner, E. Greenberg, Y. Jin and C. Paulsen, The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy, NCES2006-483, U.S. Department of Education, National Center for Education Statistics, Washington, DC, 2006. |
[56] | K. Lewin, Action research and minority problems, J Soc Issues. 2: (4) ((1946) ), 34–46. doi:10.1111/j.1540-4560.1946.tb02295.x. |
[57] | R. Logan, Health campaign research: Enduring challenges and new developments, in: Routledge Handbook of Public Communication of Science and Technology, 2nd edn, M. Bucchi and B. Trench, eds, Routledge, New York, (2014) , pp. 198–213. |
[58] | R.A. Logan, Health literacy research, in: Meeting Health Information Needs Outside of Healthcare: Opportunities and Challenges, C. Arnott-Smith and A. Keselman, eds, Chandos, Waltham, MA, (2015) , pp. 19–38. doi:10.1016/B978-0-08-100248-3.00002-0. |
[59] | R.A. Logan, Seeking an expanded, multidimensional conceptual approach to health literacy and health disparities research, in: Health Literacy: New Directions in Research, Theory and Practice, R. Logan and E. Siegel, eds, IOS Press, Amsterdam, (2018) . To appear. |
[60] | R.A. Logan, W.F. Wong, M. Villaire, G. Daus, T.A. Parnell, E. Willis and M.K. Paasche-Orlow, Health literacy: A necessary element for achieving health equity, Discussion paper, National Academy of Medicine, Washington, DC, 2015. Available at http://www.nam.edu/perspectives/2015/Health-literacy-a-necessary-element-for-achieving-health-equity. |
[61] | S.T. March and G. Smith, Design and natural science research on information technology, Decision Support Systems. 15: ((1995) ), 251–266. doi:10.1016/0167-9236(94)00041-2. |
[62] | M.L. Markus, A. Majchrzak and L. Gasser, A design theory for systems that support emergent knowledge processes, Management Information Systems Quarterly. 26: ((2002) ), 179–212. |
[63] | M. Marmot, Social determinants of health inequalities, Lancet. 354: (9464) ((2005) ), 1099–1104. doi:10.1016/S0140-6736(05)74234-3. |
[64] | M.G. Marmot, G. Davey Smith, S. Stansfield et al., Health inequalities among British civil servants: The Whitehall II study, Lancet. 337: (8754) ((1991) ), 1387–1393. doi:10.1016/0140-6736(91)93068-K. |
[65] | L. McCormack, V. Thomas, M.A. Lewis and R. Rudd, Improving low health literacy and patient engagement: A social ecological approach, Patient Educ Counsel. ((2016) ). doi:10.1016/j.pec.2016.07.007. |
[66] | M. Minkler and N. Wallerstein (eds), Community Based Participatory Research for Health: Process to Outcomes, 2nd edn, Jossey-Bass, San Francisco, (2008) . |
[67] | P.W. Murphy, Reading ability of parents compared with reading level of pediatric patient education materials, Pediatrics. 93: ((1994) ), 460–468. |
[68] | L. Neuhauser, Participatory design for better interactive health communication: A statewide model in the USA, Electron J Commun. 11: (3–4) ((2001) ), 43. |
[69] | L. Neuhauser, Creating and implementing large-scale parenting education programs: Bridging research, decision-making and practice, in: Bridging the “Know-do” Gap: Knowledge Brokering to Improve Child Well-Being, G. Bammer, A. Michaux and A. Sanson, eds, Australian National University Press, (2010) . Available at http://epress.anu.edu.au/knowledge_citation.html. |
[70] | L. Neuhauser, W.L. Constantine, N.A. Constantine, K. Sokal-Gutierrez, S.K. Obarski, L. Clayton, M. Desai, G. Sumner and S.L. Syme, Promoting prenatal and early childhood health: Evaluation of a statewide materials-based intervention for parents, Am J Public Health. 97: (10) ((2007) ), 813–819. |
[71] | L. Neuhauser, S.L. Ivey, D. Huang, A. Engelman, W. Tseng, D. Dahrouge, S. Gurung and M. Kealey, Availability and readability of emergency preparedness materials for Deaf and Hard of Hearing and older adult populations: Issues and assessments, PLoS ONE. 8: (2) ((2013) ), e55614. doi:10.1371/journal.pone.0055614. |
[72] | L. Neuhauser and G. Kreps, Rethinking communication in the e-health era, J Health Psychol. 8: ((2003) ), 7–22. doi:10.1177/1359105303008001426. |
[73] | L. Neuhauser and G. Kreps, Ehealth communication and behavior change: Promise and performance, Journal of Social Semiotics. 20: (1) ((2010) ), 9–27. doi:10.1080/10350330903438386. |
[74] | L. Neuhauser and G.L. Kreps, Integrating design science theory and methods to improve the development and evaluation of health communication programs, J Health Commun. 19: (12) ((2014) ), 1460–1471. doi:10.1080/10810730.2014.954081. |
[75] | L. Neuhauser, G.L. Kreps, K. Morrison, M. Athanasoulis, N. Kirienko and D. Van Brunt, Using design science and artificial intelligence to improve health communication: ChronologyMD case example, Patient Educ Counsel. 92: (2) ((2013) ), 211–217. doi:10.1016/j.pec.2013.04.006. |
[76] | L. Neuhauser, G.L. Kreps and S.L. Syme, Community participatory design of health communication programs: Methods and case examples from Australia, China, Switzerland and the United States, in: Global Health Communication Strategies in the 21st Century: Design, Implementation and Evaluation, D.K. Kim, A. Singhal and G.L. Kreps, eds, Peter Lang Publishing, New York, (2013) . |
[77] | L. Neuhauser and K. Paul, usability, Readability, Communicating Risks and Benefits: An Evidence-Based User’s Guide, U.S. Department of Health and Human Services, Silver Spring, MD, Food and Drug Administration, Bethesda, MD, (2011) . |
[78] | L. Neuhauser, B. Rothschild, C. Graham, S.L. Ivey and S. Konishi, Participatory design of mass health communication in three languages for seniors and people with disabilities on Medicaid, Am J Public Health. 99: (12) ((2009) ), 2188–2195. doi:10.2105/AJPH.2008.155648. |
[79] | J. Nielsen, Designing Web Usability, New Riders, Indianapolis, IN, (2000) . |
[80] | S.M. Noar and N.G. Harrington (eds), eHealth Applications: Promising Strategies for Behavior Change, Routledge, New York, (2012) . |
[81] | A.M. Nuru-Jeter, T. Williams and T.A. LaVeist, Distinguishing the race-specific effects of income inequality in US metropolitan areas, Int J Health Serv 44: (3) ((2014) ), 435–456. doi:10.2190/HS.44.3.b. |
[82] | D. Nutbeam, The evolving concept of health literacy, Soc Sci Med. 67: (12) ((2008) ), 2072–2078. doi:10.1016/j.socscimed.2008.09.050. |
[83] | M.K. Paasche-Orlow, E.A.H. Wilson and L. McCormack, The evolving field of health literacy research, J Health Commun. 15: ((2010) ), 5–8. doi:10.1080/10810730.2010.499995. |
[84] | M.K. Paasche-Orlow and M.S. Wolf, The causal pathways linking health literacy to health outcomes, Am J Health Behav. 31: (Suppl 1) ((2007) ), 19–26. doi:10.5993/AJHB.31.s1.4. |
[85] | R. Parker and S.C. Ratzan, Health literacy: A second decade of distinction for Americans, J Health Commun. 15: (Suppl 2) ((2010) ), 20–33. doi:10.1080/10810730.2010.501094. |
[86] | J.C. Phelan, B.G. Link and P. Tehranifar, Social conditions as fundamental causes of health inequalities, J Health Soc Behav. 51: (1 suppl) ((2010) ), S28–S40. doi:10.1177/0022146510383498. |
[87] | A. Pleasant, Assisting vulnerable communities: Canyon Ranch Institute’s health literacy and community-based interventions, in: Health Literacy: New Directions in Research, Theory and Practice, R. Logan and E. Siegel, eds, IOS Press, Amsterdam, (2018) . To appear. |
[88] | A. Pleasant, J. Cabe, L. Martin and R.V. Rikard, A prescription is not enough: Improving public health with health literacy, in: Implications of Health Literacy for Public Health: Workshop Summary. Roundtable on Health Literacy, Board on Population Health and Public Health Practice, Institute of Medicine, National Academies Press, (2013) . |
[89] | A. Pleasant and S. Kuruvilla, A tale of two health literacies: Public health and clinical approaches to health literacy, Health Promot Int. 23: ((2006) ), 152–159. doi:10.1093/heapro/dan001. |
[90] | A. Pleasant, R.E. Rudd, C. O’Leary, M.K. Paasche-Orlow, M.P. Allen, W. Alvarado-Little, L. Myers, K. Parson and S. Rosen, Considerations for a New Definition of Health Literacy, National Academy of Medicine, Washington, DC, (2016) . Available at https://nam.edu/considerations-for-a-new-definition-of-health-literacy/. |
[91] | N. Ratanawongsa, A.J. Karter, M.M. Parker, R.L. Courtney, M. Heisler, H.H. Moffett, N. Adler, E.M. Wharton and D. Schillinger, Communication and medication adherence: The diabetes study of Northern California, JAMA Intern Med. 173: (3) ((2013) ), 210–218. doi:10.1001/jamainternmed.2013.1216. |
[92] | J.A. Rawls, Theory of Justice, Belknap/Harvard University Press, Cambridge, (1971) . |
[93] | P. Reason and H. Bradbury, Handbook of Action Research, 2nd edn, Sage, London, (2007) . |
[94] | P. Reason and H. Bradbury (eds), The Sage Handbook of Action Research: Participative Inquiry and Practice, Sage, London and Thousand Oaks, CA, (2008) . |
[95] | C.N. Roschuni, Communicating design research effectively, PhD dissertation, 2012. Available at http://escholarship.org/uc/item/75f0z49v?query=roschuni. |
[96] | J. Rubin and D. Chisnell, Handbook of Usability Testing, Wiley Publishing, Indianapolis, IN, (2008) . |
[97] | R. Rudd and J. Anderson, The health literacy environment of hospitals and health centers, 2006. Available at http://www.hsph.harvard.edu/healthliteracy/files/healthliteracyenvironment.pdf (accessed November, 2016). |
[98] | R. Rudd, D. Renzulli, A. Pereira and L. Daltory, Literacy demands in health care settings: The patient perspective, in: Understanding Health Literacy: Implications for Medicine and Public Health, J.G. Schwartzberg, J.B. VanGeest and C.C. Wang, eds, AMA Press, Chicago, (2005) . |
[99] | R.E. Rudd, J.E. Anderson, S. Oppenheimer and C. Nath, Health literacy: An update of public health and medical literature, in: Review of Adult Learning and Literacy, Vol. 7: , J.P. Comings, B. Garner and C. Smith, eds, Lawrence Erlbaum Associates, Mahwah, NJ, (2007) . |
[100] | D. Schillinger, J. Piette, C. Wilson, C. Daher, K. Leong-Grotz, C. Castro and A.B. Bindman, Closing the loop: Physician communication with diabetic patients who have low health literacy, Archives of Internal Medicine. 163: (1) ((2003) ), 83–90. doi:10.1001/archinte.163.1.83. |
[101] | S.L. Sheridan, D.J. Halpern, A.J. Viera, N.D. Berkman, K.E. Donahue and K. Crotty, Interventions for individuals with low health literacy: A systematic review, J Health Commun. 16: (Suppl 3) ((2011) ), 30–54. doi:10.1080/10810730.2011.604391. |
[102] | H. Simon, The Sciences of the Artificial, 3rd edn, MIT Press, Cambridge, MA, (1996) . |
[103] | B.D. Smedley and S.L. Syme (eds), Promoting Health: Intervention Strategies from Social and Behavioral Research, Institute of Medicine, National Academies Press, Washington, DC, (2000) . |
[104] | M.Y. Smith and L.S. Wallace, Reducing drug self-injection errors: A randomized trial comparing a “standard” versus “plain language” version of patient instructions for use, Res Soc Adm Pharm. 9: (5) ((2013) ), 621–625. doi:10.1016/j.sapharm.2012.10.007. |
[105] | P.C. Smith, J.H. Brice and J. Lee, The relationship between functional health literacy and adherence to emergency department discharge instructions among Spanish-speaking patients, J Natl Med Assoc. 104: (11–12) ((2012) ), 521–527. doi:10.1016/S0027-9684(15)30218-2. |
[106] | L.B. Snyder, M.A. Hamilton, E.W. Mitchell, J. Kiwanuka-Tondo, F. Fleming-Milici and D. Proctor, A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States, J Health Commun. 9: (Suppl. 1) ((2004) ), 71–96. doi:10.1080/10810730490271548. |
[107] | K. Sorensen, S. Van den Broucke, J. Fullam, G. Doyle, J. Pelikan, Z. Slonska, H. Brand and (HLS-EU) Consortium Health Literacy Project European, Health literacy and public health: A systematic review and integration of definitions and models, BMC Public Health. 12: ((2012) ), 80. doi:10.1186/1471-2458-12-80. |
[108] | D. Stokols, The social ecological paradigm of wellness promotion, in: Promoting Human Wellness: New Frontiers for Research, Practice, and Policy, M.S. Jamner and D. Stokols, eds, University of California Press, Berkeley, (2000) , pp. 127–146. |
[109] | D. Stokols, J. Allen and R.L. Bellingham, The social ecology of health promotion: Implications for research and practice, Am J Health Promot. 10: ((1996) ), 247–251. doi:10.4278/0890-1171-10.4.247. |
[110] | R.L. Sudore, C.S. Landefeld, B.A. Williams, D.E. Barnes, K. Lindquist et al., Use of a modified informed consent process among vulnerable patients: A descriptive study, J Gen Intern Med. 21: ((2006) ), 867–873. doi:10.1111/j.1525-1497.2006.00535.x. |
[111] | R.L. Sudore, K. Yaffe, S. Satterfield, T.B. Harris, K.M. Mehta, E.M. Simonsick, A.B. Newman, C. Rosano, R. Rooks, S.M. Rubin et al., Limited literacy and mortality in the elderly: The health, aging, and body composition study, J Gen Intern Med. 21: (8) ((2006) ), 806–812. doi:10.1111/j.1525-1497.2006.00539.x. |
[112] | J. Taggart, A. Williams, S. Dennis, A. Newall, T. Shortus, N. Zwar, E. Denney-Wilson and M.F. Harris, A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors, Database of Abstracts of Reviews for Effects (DARE): Quality-assessed reviews, 2012. Available at http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0052469/ (accessed July 22, 2015). |
[113] | U.S. Department of Health and Human Services, Communicating Health: Priorities and Strategies for Progress, U.S. Department of Health and Human Services, Washington, DC, (2003) . |
[114] | U.S. Department of Health and Human Services, Healthy people 2020, Draft, U.S. Government Printing Office, 2009. |
[115] | M.E. Vaiana and E.A. McGlynn, What cognitive science tells us about the design of reports for consumers, Med Care Res Rev. 59: (1) ((2002) ), 3–35. doi:10.1177/1077558702059001001. |
[116] | J.K. Vallance, K.S. Courneya, R.C. Plotnikoff, Y. Yasui and J.R. Mackey, Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors, J Clin Oncol. 25: (17) ((2007) ), 2352–2359. doi:10.1200/JCO.2006.07.9988. |
[117] | J. Vechakul, B.P. Shrimali and J.S. Sandhu, Human centered design as an approach for place-based innovation in public health: A CDC case study from Oakland, California. Matern Child Health J. 19: (12) ((2015) ), 2552–2559. doi:10.1007/s10995-015-1787-x. |
[118] | K. Viswanath and J.R. Finnegan, The knowledge gap hypothesis: Twenty-five years later, in: Communication Yearbook, Vol. 19: , B. Burlson, ed., Sage, Thousand Oaks, CA, (1995) , pp. 187–228. |
[119] | C. Von Wagner, A. Steptoe, M.S. Wolf and J. Wardle, Health literacy and health actions: A review and a framework from health psychology, Health Education & Behaviour. 36: (5) ((2009) ), 860–877. doi:10.1177/1090198108322819. |
[120] | R. Wang, Critical health literacy: A case study from China in schistosomiasis control, Health Promotion International. 15: (3) ((2000) ), 269–274. doi:10.1093/heapro/15.3.269. |
[121] | S. White, Assessing the Nation’s Health Literacy: Key Concepts and Findings of the National Assessment of Adult Literacy (NAAL), American Medical Association Foundation, Chicago, IL, (2008) . |
[122] | M. Whitehead, The concepts and principles of equity and health, Health Promot Int. 6: (3) ((1991) ), 217–228. doi:10.1093/heapro/6.3.217. |
[123] | WHO, International conference on primary health care, Alma-Ata, USSR, 6–12 September 1978, Report, WHO, Geneva 1978. |
[124] | M.S. Wolf, T.C. Davis, L.M. Curtis, J.A. Webb, S.C. Bailey, W.H. Shrank, L. Lindquist, B. Ruo, M.V. Bocchini, R.M. Parker and A.J.J. Wood, Effect of standardized, patient-centered label instructions to improve comprehension of prescription drug use, Medical Care. 49: (1) ((2011) ), 96–100. doi:10.1097/MLR.0b013e3181f38174. |
[125] | M.S. Wolf, S.J. Knight, E.A. Lyons, R. Durazo-Arvizu, S.A. Pickard, A. Arseven, A. Arozullah, K. Colella, P. Ray and C.L. Bennett, Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer, Urology. 68: (1) ((2006) ), 89–93. doi:10.1016/j.urology.2006.01.064. |
[126] | A. Wolka, K. Simpson, K. Lockwood and L. Neuhauser, Focus on health literacy, Ther Innov Regul Sci. 49: (3) ((2014) ), 369–376. doi:10.1177/2168479014561339. |
[127] | World Health Organization, Health Promotion Glossary, WHO, Geneva, (1998) . |
[128] | H.S. Yin, A.L. Mendelsohn, M.S. Wolf, R.M. Parker, A. Fierman, L. van Schaick, I.S. Bazan, M.D. Kline and B.P. Dreyer, Parents’ medication administration errors: Role of dosing instruments and health literacy, Arch Pediatr Adolesc Med. 164: (2) ((2010) ), 181–186. doi:10.1001/archpediatrics.2009.269. |
[129] | N.B. Zite and L.S. Wallace, Use of a low-literacy informed consent form to improve women’s understanding of tubal sterilization: A randomized controlled trial, Obstet Gynecol. 117: ((2011) ), 1160–1166. doi:10.1097/AOG.0b013e318213cbb1. |




