Disparities in public understanding, attitudes, and intentions during the Covid-19 pandemic: The role of health literacy
Abstract
The Covid-19 pandemic has highlighted the need to address health literacy as a critical priority for public health. Health literacy is crucial during a pandemic for understanding and following health advice and for navigating vast amounts of information and misinformation. However, public health communication globally has inadequately met the needs of low literacy and culturally and linguistically diverse groups. This review examines the role of health literacy and how it is related to Covid-19 related outcomes, as well as how public health communication has routinely failed to follow basic health literacy principles. Lessons from the pandemic about health communication and recommendations for how health literacy needs can be addressed in the future are discussed. Improving public health communication requires an immediate short-term response and longer-term investment to build the health literacy responsiveness of public health units, health organisations, and government departments to meet health literacy population needs.
1.Background
The COVID-19 pandemic has led to unprecedented health, social and economic consequences. These were not only considerable, they continue to be unevenly spread, disproportionately falling on those already socially and economically disadvantaged [1]. The data from numerous high-income countries suggest there are important differences in COVID-19 mortality for people from different socioeconomic and cultural and/or linguistic backgrounds [2–5] (Table 1). Much of these differences are attributable to pre-existing social and structural inequalities including limited access to education, healthcare, housing, and employment, exposure to occupational and environmental risk factors, and higher rates of comorbid diseases known to affect COVID-19 symptom severity [1,6,7]. However, health literacy also may have played a role. There is increasing evidence that the extant health information environment poorly met the needs of people with lower health literacy and the same populations showed lower levels of understanding and engagement with COVID-19 health advice.
Table 1
Racial and ethnic differences in COVID-19 mortality in selected countries
| Country | Reference group | Ethnic/racial group | Age-adjusted Mortality rate | Data accessed |
| Australiaa | ||||
| Australian Born | Overseas born (all) | 1.9× | 31 Jul 2022 [3 ] | |
| Australian Born | Middle East born | 5.5× | 31 Jul 2022 | |
| Australian Born | North Africa born | 3.1× | 31 Jul 2022 | |
| Australian Born | South-east Europe born | 2.9× | 31 Jul 2022 | |
| Englandb | ||||
| White British | Black/Black British | 2.5× | 31 Jan 2022 [4 ] | |
| White British | Asian British | 2× | 31 Jan 2022 | |
| USc | ||||
| White American | Black American | 1.7× | 9 Sep 2022 [5 ] | |
| White American | Latino American | 1.8× | 9 Sep 2022 | |
| White American | Asian American | 0.8× | 9 Sep 2022 | |
| White American | Native American | 2.1× | 9 Sep 2022 |
[i] Note. It is important to note that racial and ethnic COVID-19 mortalities were generally larger during the earlier waves of the pandemic, reflecting the effect of COVID-19 being disproportionately experienced first among minority ethnic and racial groups.aSelected migrant groups presented with worst COVID-19 outcomes. Large heterogeneity across all migrant groups.bHighest mortality rates seen in Pakistani and Bangladeshi ethnic groups [93].cNon-Hispanic White.
Health literacy refers to the personal skills and capacities as well as the informational and organisational environment that enables people to find, understand, and use health information and services to manage their health (See Fig. 1) [8,9]. This paper describes the accumulating evidence of the role that health literacy played during the pandemic in the public’s understanding, attitudes, and engagement with COVID-19 public health advice, as well as the health literacy burden created by the informational environment during a crucial time for effective public communication.
Fig. 1.
Health literacy.
1.1.Health literacy is related to socioeconomic circumstances, language and migration
The prevalence of lower health literacy is socio-economically patterned. Low health literacy is consistently associated with markers of social and economic disadvantage, including lower education, lower income, and unemployment. It also is associated with indicators of language fluency and migration, such as lower English fluency in English speaking nations or fluency of the dominant national language of residence [10–15]. As a construct, health literacy has been advanced as a potential mid-stream and modifiable social determinant of health. This means there is potential to improve health outcomes through investment in interventions to build personal health literacy skills and capacities, and in efforts (such as policies, systems, and processes) to reduce the complexity and demand of the healthcare environment to enable better access to health information and services [16].
1.2.Health literacy and COVID-19 public communication: a complex health environment
Early in the pandemic, there was pressure to respond rapidly to the COVID-19 outbreak and communicate quickly to the public. Although there are established health literacy principles to guide public health communication - such as ensuring health information is readable and actionable, avoids medical jargon, and uses simple language - these often were not well integrated into communication by government and prominent health organisations [17–23]. This resulted in much of the COVID-19 public health advice being highly complex and requiring a high level of personal health literacy skills.
For example, early in the pandemic (mid-2020), Mishra and Dexter analysed COVID-19 information produced by 15 prominent national and international health websites [19]. They found a very high level of complexity in written government and health organisation texts regarding COVID-19. Mishra and Dexter found written health information did not meet recommended guidelines for reading level grade (e.g. Grade 8 reading age for readers of average population literacy). Instead, the reading grade level exceeded average reading ability ranging from 2–10 grades higher than the recommended grade 8 level. The authors found no resources that were written at the level advised as suitable for people with lower literacy (Grade 6) [19].
In the past three years, there have since been dozens of studies examining the complexity of written health information about COVID-19 [20,24–33]. The authors’ research in July 2021 assessed communication when COVID-19 vaccine communication dominated public communication. It suggested there was little improvement in the readability of written information on official government websites [20].
Of ten websites assessed in July 2021, the median reading grade of the health information was age 12, (four grades higher than the recommended grade 8 level) [20]. Only two sites had resources developed for low literacy readers. While these analyses do not consider infographic and audio-visual communications to the public, they address the written communication provided to the public by major health organisations and governments internationally.
1.3.Health literacy and its relationship with COVID-19 understanding, attitudes, and intentions
Health literacy has been linked to a range of knowledge and behavioural outcomes related to COVID-19 (see Box Box 1) [34–39]. Australian research from early in the pandemic (April 2020) suggested people with lower health literacy and those who spoke a language other than English at home had poorer knowledge and understanding of COVID-19 health advice and reported greater difficulty in finding reliable health information. The national survey of >4000 Australian adults suggested the same groups also perceived the risk of COVID-19 as lower and rated COVID-19 prevention behaviours as less important than people with higher health literacy. Similarly, Australians with lower health literacy were less willing to be vaccinated, either for flu or a potential COVID-19 vaccine (note: no COVID vaccine was available in Australia at the time of the study) [40]. There also were important differences in knowledge, attitudes, and reported adherence to COVID-19 prevention behaviours by age and gender, which suggested messaging was not reaching population sub-groups, such as young people and men [39,41].
Box 1.
Summary of associations between health literacy and COVID-19 related outcomes.
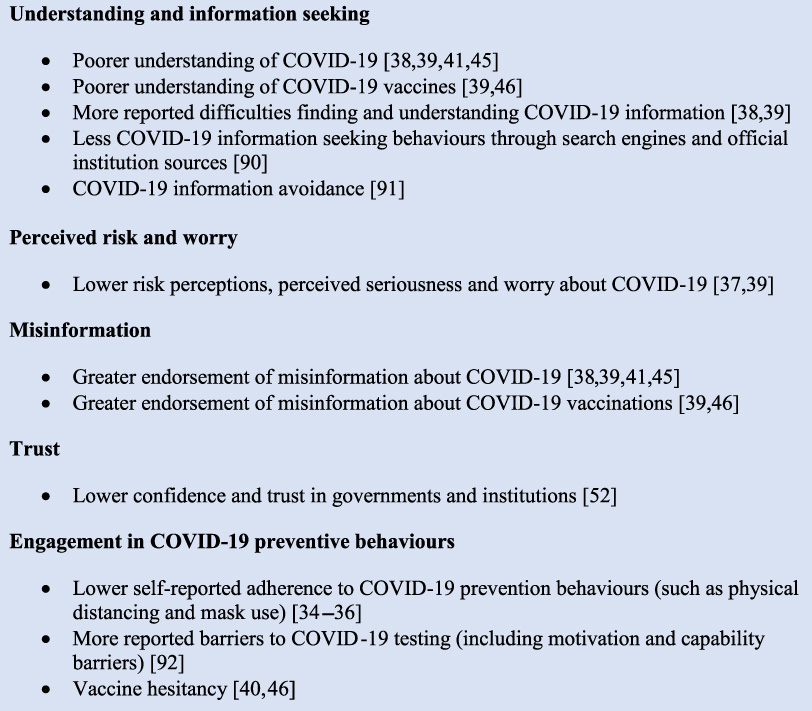
Research from France around the same period (April 2020) assessed COVID-19 knowledge using a COVID-19-specific measure of health literacy and reported similar findings. Low health literacy was associated with lower self-reported compliance with mask wearing and physical distancing [35]. Research in Germany, also using a COVID-19-specific health literacy measure (HLS-COVID-Q22), identified 15 percent of the population with ‘problematic’ COVID-19 specific health literacy and 34 percent with inadequate levels. They found low COVID-19 health literacy was associated with feeling less informed and more confused about COVID-19 [38].
In the U.S., adults with one or more chronic conditions who had low health literacy, or were African-American and low income, were less worried about COVID-19 and less likely to believe they would become infected. These groups also felt less prepared for an outbreak [37,42]. Similarly, a lower perceived risk of COVID-19 (assessed at the pandemic outset) among people with lower health literacy was associated with a greater likelihood of COVID-19 infection in a subsequent 12-month period. The latter study was conducted at potentially the most risky time to catch COVID-19, before vaccination and evidence-based treatments were widely available [43].
1.4.Health literacy and endorsement of COVID-19 misinformation
The pandemic also has been characterised by an explosion of online information (an ‘infodemic’) presenting new and formidable challenges for finding reliable COVID-19 information [44]. Skills for thinking critically about health information have become increasingly important as the digital health information environment has transformed.
For example, lower health literacy, numeracy (the ability to understand and use numeric information including probabilities) and analytical thinking, all have been associated with increased endorsement of COVID-19 misinformation beliefs [41,45–49]. In the authors’ Australian research (including three national surveys between April to July 2020), stronger endorsement of misinformation was associated with: younger age, male gender, lower education level, and speaking a language other than English at home. After controlling for these variables, misinformation beliefs were significantly associated with lower levels of health literacy and digital health literacy [39,41].
Another study of younger adults in Australia aged 18–49 years not yet vaccinated (July–August 2021) found up to two thirds of participants agreed with at least one misinformation belief about COVID-19 vaccines. Misinformation beliefs were significantly associated with lower health literacy, lower education, less knowledge about vaccines, lower perceived personal risk of COVID-19, and lower confidence and trust in government and scientific institutions [46].
In aggregate, these findings are similar to a systematic review that investigated COVID-19 conspiracy beliefs from around the world [50]. Across 85 studies, the review found consistent associations between misinformation, education, and income level; with lower education and income associated with higher endorsement of misinformation. Although health literacy is not reported in the review, its socio-demographic measures of disadvantage are commonly associated with lower health literacy [11–15,51].
1.5.Health literacy is associated with trust related to the COVID-19 response
Trust in governments, institutions, scientists, and medical researchers are an important correlate of misinformation beliefs and vaccine hesitancy, and vary by health literacy and other markers of social disadvantage and marginalisation [39,45,50,52,53]. The authors’ Australian research across a nationally representative sample showed lower confidence and trust (in scientists, researchers, and medical institutions) were associated with low health literacy [41,54]. Lower trust also was associated with use of non-official information as a leading source of information about COVID-19 [52]. In contrast, U.S. research among a chronic disease cohort found people with low health literacy expressed increased trust in the federal government’s response. However, the study participants perceived they were less prepared for a COVID-19 outbreak and there was no association with trust in vaccines (leading up to their availability) [55].
2.COVID-19 communication for culturally and linguistically diverse populations
Migrants, people from different cultural and ethnic minority groups, and First Nations populations often have lower levels of health literacy - particularly when there are language barriers, low income, fewer years of education, and experiences of racism and marginalisation within these groups [14,15,55–61]. These same populations also experienced increased COVID-19 infection, hospitalisation, and mortality, and simultaneous high levels of social, psychological, and financial burden during the pandemic [1–7,62]. Many also experienced further racism and xenophobia associated with COVID-19 [63]. As such, it seems imperative to provide culturally safe and appropriate public health communication that is tailored to specific communities’ needs, and assist disadvantage groups that are already marginalized.
2.1.The health information environment for culturally and linguistically diverse populations
COVID-19 public health communication in many countries around the world frequently did not meet the needs of cultural and linguistic minorities [22,64]. In Australia, the government released information about COVID-19 in English alone, with translations in other languages coming many weeks later, or sometimes not at all [22,65,66]. Translated COVID-19 health information on government websites was often of low quality and sometimes relied only on automated machine translations so the information was inaccurate or culturally inappropriate [65,67]. Although there were examples of community-based education initiatives, these often were not widespread and may have left people from culturally and linguistically diverse backgrounds vulnerable to low quality or inaccurate health information and misinformation [64,68]. As the pandemic progressed, initiatives to improve the availability of translated and plain language COVID-19 health information increased worldwide, however, this often ignored timely public communication strategies and occurred later than needed [69].
2.2.COVID-19 understanding, attitudes, misinformation beliefs and behavioural intentions among culturally and linguistically diverse populations
This inadequacy of the health information environment has led to further marginalisation of culturally and linguistically diverse communities. Poor outcomes including lower knowledge and understanding about COVID-19, negative attitudes and behaviours related to COVID-19, have been observed among different cultural and linguistic groups in many countries, including Australia [37,39,70–73]. In the authors’ Australian national survey, people who spoke another language at home reported: a greater perceived difficulty in finding health information; a lower perceived risk of COVID-19; a lower understanding of COVID-19 prevention behaviours; a higher endorsement of misinformation; and a lower willingness to be vaccinated compared to people who spoke English [40].
Similar patterns additionally vary widely across different communities. A subsequent study of >700 participants whose first language was not English suggested significant variations among different cultural groups regarding COVID-19 knowledge, misinformation beliefs, risk perceptions, interest in testing and vaccination, and diverse patterns of how COVID-19 information is sourced [71]. Health literacy also was associated with increased difficulty accessing easy to understand health information. Evidence from a systematic review suggests higher endorsement of COVID-19 conspiracy beliefs among some racial and ethnic minority groups when this parallels socio-economic disadvantage [50].
Some communities also exhibit a compromised trust in government advice, based on a history of racism in medical research and care, uncertainty about visa status, and a lack of government support for those in precarious or hazardous employment. For instance, whilst Light et al. reported that some Latino Americans trusted COVID-19 vaccines, others worried the vaccines had been manipulated [73]. Fear about attending a vaccine site also was reported due to immigration status as well as concerns about missing work due to short-term vaccination side effects. Together, this body of research highlights why non-tailored mass communication efforts are unlikely to be effective within some communities.
3.What can we do better in the future?
Improving public health communication requires an immediate short-term response and longer-term investment in building the health literacy responsiveness of public health units, health organisations, and government departments to meet the health literacy needs of the population. In addition, investments in supporting health literacy skill development in the community is imperative.
3.1.Short term actions to address health literacy
Efforts are needed to improve public health communication to meet the needs of lower literacy and culturally and linguistically diverse populations, and to do so in a timely, systematic fashion. Below the authors list four evidence-based activities for focused attention to health literacy:
1. Develop standards and systems to ensure public health communication complies with best practice health literacy advice and Universal Precautions principles. This includes, writing text at a Grade 8 reading level for average readers (and grade 6 for low literacy audiences). This requires reducing jargon and complex language, using images to support the key messages, and limiting information overload through use of white space and formatting.
2. Ensure high quality translated materials are available concurrently with materials presented in the dominant national language, which are easy to find. Information should be available using multimedia formats (such as audio and animated information) that support understanding for people who are non-literate. Health information that adheres to health literacy principles of readability (i.e. is written at grade 7–10 before translation) is faster to translate and more accurately translated than information written at a higher reading grade level [74]. This may be important in time critical situations. Attention to navigation and information architecture also is needed so accurate, trustworthy health information can be easily found and accessed by those who need it most (for example, see the Office of Disease Prevention and Health Promotion, Health Literacy Online) [75].
3. Use development processes that involve co-design with consumers/users of healthcare. In time-sensitive situations this may require establishing committees of citizens, consumers and patient-partners who are resourced and supported to rapidly review materials at short notice who also represent dimensions of diversity - including culture, language, age, gender, disability, and vulnerable illness cohorts. Not only is this ethically appropriate but evidence suggests this approach results in health information that is more readable and better understood [76,77].
4. Establish fact checking systems and ensure myth busting information is available in multiple languages, adhering to health literacy principles to address misinformation circulating in communities quickly and proactively. These will be most effective if initiatives follow best practices guidance on myth busting (e.g. Schmid and Betsch) [78].
There are numerous guidelines for effective pandemic communication which should be considered alongside health literacy e.g. see: Hyland-Wood et al., West et al., Leask et al. [79–81]. Information must be urgently promoted using diverse mass media channels, including established and emerging social media (e.g. Facebook, TikTok, Twitch) as well as diverse traditional media channels (e.g. radio, TV). The use of appropriate and trusted spokespeople for different communities also is critical and needs to be combined with the aforementioned measures to optimize outreach to diverse communities [82].
3.2.Longer term efforts to address health literacy
In the long term, international efforts are required to build health literacy skills and capacities among community members and the health workforce as well as systems and processes for health organisations to embed into practice. This means investing in programs for individuals and communities to build functional, communicative, and critical health literacy including digital and numeracy skills. For the healthcare workforce, enduring efforts need to provide leadership and training in good health literacy communication practices that promote enhanced understanding among diverse healthcare users. For organisations, it means developing policies, practices, and leadership in health literacy to require attention to health literacy as an integral part of business. There is a large and growing literature on interventional strategies to build health literacy in health organisations and services, which supports the development of health literacy among children, community members, patients, and health professionals [83–89].
3.3.A systems-based approach is needed
Attention to health literacy is only a start and is unlikely to succeed if it relies on individual behavioural or organisational change alone. For genuine and sustainable improvement across the health sector and beyond, a systems-based approach is needed so health literacy can be systematically and sustainably addressed in crisis situations at speed, as well as an integral part of every-day activities. Sørensen et al. outline a comprehensive framework to build health literacy system capacity [9]. Sørensen et al. identify eight targets for actions including: a health literate workforce; health literate health organisations; health literate data governance; partnerships and intersectoral collaborations; people-centred services based on user engagement; health literacy informed technology/innovation; health literacy investments/financial resource; and health literacy leadership. This recommended approach suggests changes at the micro level among people and professionals, at the meso level among organisations, institutions, markets, and technologies and at the macro level, in policy, political, social values, and priorities.
4.Conclusion
COVID-19 exposed the inadequacies of many government, health, and community organisations and services to address health literacy and the needs of culturally and linguistically diverse communities. These inadequacies had deleterious consequences on public and individual health during the COVID-19 pandemic. Since health literacy is a modifiable determinant of health, there is a responsibility to address it. The latter means investing in services that meet the needs of people with lower health literacy, especially those from different cultural and linguistic backgrounds.
The efforts to build health literacy will be more successful if they are part of a broader policy to develop strategies to address the structural inequalities that directly impact public health. COVID-19 has shown how all citizens are impacted by each other’s understanding of health and health decisions. As we move forward with an aging society, increasing digitalisation, and disruption of traditional forms of media, we are likely to see increasing climate-related emergencies including further pandemics. In turn, investing in health literacy efforts among organisations and communities may need to be seen more as a first line of defence rather than something desirable to attain.
Declaration of interest statement
JA, DMM, CB, and KJM are directors of a health literacy consultancy (Health Literacy Solutions Ltd, Pty). The company provides health literacy advice to health services/organisations to support increased access to health information for low literacy adults. Any revenue raised is used to support the development of tools to support health literacy document design. No personal income is received by JA, KJM, DMM or CB.
MSW has had paid consultancies, unrelated to this work with Abbvie, Lundbeck, Pfizer, and Sanofi as well as with Luto UK. In addition, he has received institutional grants from Eli Lilly, Merck, Sharpe & Dohme, Pfizer and Lundbeck. MW is also supported by the National Institute on Aging (P30AG059988).
Authors’ contributions
KJM conceived and drafted the manuscript, which was reviewed and edited by all other authors. All authors approved the final version of the manuscript.
References
[1] | S. Magesh, D. John, W.T. Li, Y. Li, A. Mattingly-App, S. Jain , Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: A systematic-review and meta-analysis, JAMA Netw Open 4: (11) ((2021) ), e2134147. doi:10.1001/jamanetworkopen.2021.34147. |
[2] | A. Cheshmehzangi, Vulnerability of the UK’s BAME communities during COVID-19: The review of public health and socio-economic inequalities, Journal of Human Behavior in the Social Environment 32: (2) ((2022) ), 172–188. doi:10.1080/10911359.2021.1875949. |
[3] | Australian Bureau of Statistics. COVID-19 mortality in Australia: Deaths registered until 31 July 2022 [Internet]. 2022. Available from: https://www.abs.gov.au/articles/covid-19-mortality-australia-deaths-registered-until-31-july-2022. Retrieved September 19, 2022. |
[4] | UK Health Security Agency. COVID-19 confirmed deaths in England (to 31 January 2022): report [Internet]. 2022. Available from: https://www.gov.uk/government/publications/covid-19-reported-sars-cov-2-deaths-in-england/covid-19-confirmed-deaths-in-england-to-31-january-2022-report. Retrieved August 10, 2022. |
[5] | Centers for Disease Control and Prevention. Risk for COVID-19 infection, hospitalization, and death by race/ethnicity [Internet]. 2022. Available from: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html. Retrieved September 19, 2022. |
[6] | G.D. Batty, B. Gaye, C.R. Gale, M. Hamer and C. Lassale, Explaining ethnic differentials in COVID-19 mortality: A cohort study, Am J Epidemiol 191: (2) ((2022) ), 275–281. doi:10.1093/aje/kwab237. |
[7] | K. Mackey, C.K. Ayers, K.K. Kondo, S. Saha, S.M. Advani, S. Young , Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review, Ann Intern Med 174: (3) ((2021) ), 362–373. doi:10.7326/M20-6306. |
[8] | D. Nutbeam and D.M. Muscat, Health Promotion Glossary 2021, Health Promot Int 36: (6) ((2021) ), 1811. doi:10.1093/heapro/daab067. |
[9] | K. Sørensen, D. Levin-Zamir, T.V. Duong, O. Okan, V.V. Brasil and D. Nutbeam, Building health literacy system capacity: A framework for health literate systems, Health Promot Int 36: (Supplement_1) ((2021) ), i13–i23. doi:10.1093/heapro/daab153. |
[10] | R.E. Rudd, J.E. Anderson, S. Oppenheimer and C. Nath, Health literacy: An update of medical and public health literature, Review of Adult Learning and Literacy 7: : ((2007) ), 175–203. |
[11] | K. Sorensen, J.M. Pelikan, F. Röthlin, K. Ganahl, Z. Slonska, G. Doyle , Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU), Eur J Public Health 25: (6) ((2015) ), 1053–1058. doi:10.1093/eurpub/ckv043. |
[12] | T.V. Duong, A. Aringazina, G. Baisunova, N. Nurjanah, T.V. Pham, K.M. Pham , Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries, J Epidemiol 27: (2) ((2017) ), 80–86. doi:10.1016/j.je.2016.09.005. |
[13] | U.S. Department of Education. Highlights of the 2017 U.S. PIACC Results Web Report [Internet]. 2020. Available from: https://nces.ed.gov/surveys/piaac/current_results.asp. Retrieved September 12, 2022. |
[14] | Australian Bureau of Statistics. National health survey: Health literacy [Internet]. 2018. Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-health-literacy/latest-release. Retrieved September 12, 2022. |
[15] | Australian Bureau of Statistics. Health literacy, Australia, 2006 [Internet]. 2008. Available from: https://www.abs.gov.au/ausstats/[email protected]/Latestproducts/4233.0Main%20Features22006. Retrieved September 29, 2022. |
[16] | D. Nutbeam and J.E. Lloyd, Understanding and responding to health Literacy as a social determinant of health, Ann Rev Public Health 42: (1) ((2021) ), 159–173. doi:10.1146/annurev-publhealth-090419-102529. |
[17] | Agency for Healthcare Research and Quality. AHRQ health literacy universal precaustion toolkit [Internet]. 2020. Available from: https://www.ahrq.gov/health-literacy/improve/precautions/index.html. Retrieved September 22, 2022. |
[18] | K. McCaffery, D. Muscat and J. Donovan, An urgent call for governments to improve pandemic communications, and address health literacy concerns. [Internet]. 2020. Available from: https://www.croakey.org/an-urgent-call-for-governments-to-improve-pandemic-communications-and-address-health-literacy-concerns/. Retrieved September 19, 2022. |
[19] | V. Mishra and J.P. Dexter, Comparison of readability of official public health information about COVID-19 on websites of international agencies and the governments of 15 countries, JAMA Netw Open 3: (8) ((2020) ), e2018033. doi:10.1001/jamanetworkopen.2020.18033. |
[20] | O.A. Mac, D. Muscat, J. Ayre, P. Patel and K.J. McCaffery, Coronavirus (COVID-19) vaccination information must pay attention to health literacy: Analysis of readability of official COVID-19 public health information, Med J Aust 215: (8) ((2021) ), 373–375. |
[21] | T. Sentell, S. Vamos and O. Okan, Interdisciplinary perspectives on health literacy research around the world: More important than ever in a time of COVID-19, Int J Environ Res Public Health 17: (9) ((2020) ), 3010. doi:10.3390/ijerph17093010. |
[22] | I. Abdi, B. Murphy and H. Seale, Evaluating the health literacy demand and cultural appropriateness of online immunisation information available to refugee and migrant communities in Australia, Vaccine 38: (41) ((2020) ), 6410–6417. doi:10.1016/j.vaccine.2020.07.071. |
[23] | O. Okan, M. Messer, D. Levin-Zamir, L. Paakkari and K. Sørensen, Health literacy as a social vaccine in the COVID-19 pandemic, Health Promot Int ((2022) ), daab197. doi:10.1093/heapro/daab197. |
[24] | L.S. Bothun, S.E. Feeder and G.A. Poland, Readability of COVID-19 vaccine information for the general public, Vaccine 40: (25) ((2022) ), 3466–3469. doi:10.1016/j.vaccine.2022.04.096. |
[25] | N.S. Mani, T. Ottosen, M. Fratta and F. Yu, A health literacy analysis of the consumer-oriented COVID-19 information produced by ten state health departments, J Med Libr Assoc 109: (3) ((2021) ), 422–431. doi:10.5195/jmla.2021.1165. |
[26] | M. Sakhuja, B. Yelton, M.A. Arent, S. Noblet, M.M. Macauda, D. Fedrick , Words matter: An analysis of the content and readability of COVID-19 information on clinic websites, Front Commun 6: ((2021) ), 738467. doi:10.3389/fcomm.2021.738467. |
[27] | H. Moon, G.H. Lee and Y.J. Cho, Readability of Korean-Language COVID-19 information from the South Korean national COVID-19 portal intended for the general oublic: Cross-sectional infodemiology study, JMIR Form Res 6: (3) ((2022) ), e30085. doi:10.2196/30085. |
[28] | C.H. Basch, J. Mohlman, G.C. Hillyer and P. Garcia, Public health communication in time of crisis: Readability of on-Line COVID-19 information, Disaster Med Public Health Prep 14: (5) ((2020) ), 635–637. doi:10.1017/dmp.2020.151. |
[29] | A.P. Worrall, M.J. Connolly, A. O’Neill, M. O’Doherty, K.P. Thornton, C. McNally , Readability of online COVID-19 health information: A comparison between four English speaking countries, BMC Public Health 20: (1) ((2020) ), 1635. doi:10.1186/s12889-020-09710-5. |
[30] | E. Halboub, M.S. Al-Ak’hali, H.M. Al-Mekhlafi and M.N. Alhajj, Quality and readability of web-based Arabic health information on COVID-19: An infodemiological study, BMC Public Health 21: (1) ((2021) ), 151. doi:10.1186/s12889-021-10218-9. |
[31] | H. Costantini and R. Fuse, Health Information on COVID-19 Vaccination: readability of online sources and newspapers in Singapore, Hong Kong, and the Philippines, Journalism and Media 3: (1) ((2022) ), 228–237. |
[32] | C. Ferguson, M. Merga and S. Winn, Communications in the time of a pandemic: The readability of documents for public consumption, Aust N Z J Public Health 45: (2) ((2021) ), 116–121. doi:10.1111/1753-6405.13066. |
[33] | R. Jayasinghe, S. Ranasinghe, U. Jayarajah and S. Seneviratne, Quality of online information for the general public on COVID-19, Patient Educ Couns 103: (12) ((2020) ), 2594–2597. doi:10.1016/j.pec.2020.08.001. |
[34] | J. Thacker, D. Sturman and J. Auton, Predictors of social distancing compliance in an Australian sample, Health Educ Res 36: (6) ((2022) ), 601–614. doi:10.1093/her/cyab035. |
[35] | C. Rodon, J. Chin and A. Chevalier, Assessing COVID-19 Health Literacy (CoHL) and its relationships with sociodemographic features, locus of control and compliance with social distancing rules during the first lockdown in France, Health Educ Res 37: (3) ((2022) ), 143–154. doi:10.1093/her/cyac009. |
[36] | M.A. Bekalu, D. Dhawan, R. McCloud, R. Pinnamaneni and K. Viswanath, Adherence to COVID-19 mitigation measures among American adults: The need for consistent and unified messaging, Health Educ Res 36: (2) ((2021) ), 178–191. doi:10.1093/her/cyab002. |
[37] | M.S. Wolf, M. Serper, L. Opsasnick, R.M. O’Conor, L. Curtis, J.Y. Benavente , Awareness, attitudes, and actions related to COVID-19 among adults with chronic conditions at the onset of the U.S. outbreak: A cross-sectional survey, Ann Intern Med 173: (2) ((2020) ), 100–109. doi:10.7326/M20-1239. |
[38] | O. Okan, T.M. Bollweg, E.-M. Berens, K. Hurrelmann, U. Bauer and D. Schaeffer, Coronavirus-related health literacy: A cross-sectional study in adults during the COVID-19 infodemic in Germany, Int J Environ Res Public Health 17: (15) ((2020) ), 5503. doi:10.3390/ijerph17155503. |
[39] | K.J. McCaffery, R.H. Dodd, E. Cvejic, J. Ayrek, C. Batcup, J.M. Isautier , Health literacy and disparities in COVID-19-related knowledge, attitudes, beliefs and behaviours in Australia, Public Health Res Pract 30: (4) ((2020) ), e30342012. doi:10.17061/phrp30342012. |
[40] | R.H. Dodd, E. Cvejic, C. Bonner, K. Pickles, K.J. McCaffery , S.H.L.L.C. group. Willingness to vaccinate against COVID-19 in Australia, Lancet Infect Dis 21: (3) ((2020) ), 318–319. doi:10.1016/S1473-3099(20)30559-4. |
[41] | K. Pickles, E. Cvejic, B. Nickel, T. Copp, C. Bonner, J. Leask , COVID-19 Misinformation trends in Australia: Prospective longitudinal national survey, J Med Internet Res 23: (1) ((2021) ), e23805. doi:10.2196/23805. |
[42] | S.C. Bailey, M. Serper, L. Opsasnick, S.D. Persell, R. O’Conor, L.M. Curtis , Changes in COVID-19 knowledge, beliefs, behaviors, and preparedness among high-risk adults from the onset to the acceleration phase of the US outbreak, Journal of General Internal Medicine: JGIM 35: (11) ((2020) ), 3285–3292. doi:10.1007/s11606-020-05980-2. |
[43] | S.W. Light, L. Opsasnick, S.C. Bailey, J.Y. Benavente, M. Eifler, R.M. Lovett , Early COVID-19 attitudes and behaviors and their associations with later infection: A local perspective from One U.S. City, Medical Care 61(6) (2023), 409-414. doi:10.1097/MLR.0000000000001855. Epub 2023 Apr 1. |
[44] | World Health Organistion. Infodemic [Internet]. 2023. Available from: https://www.who.int/health-topics/infodemic. Retrieved March 21, 2023. |
[45] | J. Roozenbeek, C.R. Schneider, S. Dryhurst, J. Kerr, A.L.J. Freeman, G. Recchia , Susceptibility to misinformation about COVID-19 around the world, R Soc Open Sci 7: (10) ((2020) ), 201199. doi:10.1098/rsos.201199. |
[46] | K. Pickles, T. Copp, G. Meyerowitz-Katz, R.H. Dodd, C. Bonner, B. Nickel , COVID-19 vaccine misperceptions in a community sample of adults aged 18–49 uears in Australia, Int J Environ Res Public Health 19: (11) ((2022) ), 6883. doi:10.3390/ijerph19116883. |
[47] | B. Bago, D.G. Rand and G. Pennycook, Fake news, fast and slow: Deliberation reduces belief in false (but not true) news headlines, J Exp Psychol Gen 149: (8) ((2020) ), 1608–1613. doi:10.1037/xge0000729. |
[48] | V. Swami, M. Voracek, S. Stieger, U.S. Tran and A. Furnham, Analytic thinking reduces belief in conspiracy theories, Cognition 133: (3) ((2014) ), 572–585. doi:10.1016/j.cognition.2014.08.006. |
[49] | M.S. Nurse, R.M. Ross, O. Isler and D. Van Rooy, Analytic thinking predicts accuracy ratings and willingness to share COVID-19 misinformation in Australia, Mem Cognit 50: (2) ((2021) ), 425–434. doi:10.3758/s13421-021-01219-5. |
[50] | V. van Mulukom, L.J. Pummerer, S. Alper, H. Bai, V. Čavojová, J. Farias , Antecedents and consequences of COVID-19 conspiracy beliefs: A systematic review, Soc Sci Med 301: ((2022) ), 114912. doi:10.1016/j.socscimed.2022.114912. |
[51] | R.E. Rudd, Health literacy skills of U.S. adults, Am J Health Behav 31: (1) ((2007) ), S8–S18. |
[52] | B. Nickel, K. Pickles, E. Cvejic, T. Copp, R.H. Dodd, C. Bonner , Predictors of confidence and trust in government and institutions during the COVID-19 response in Australia, Lancet Reg Health West 23: ((2022) ), 100490. doi:10.1016/j.lanwpc.2022.100490. |
[53] | E.U. Joseph, M.E. Adam, K. Casey, S. Michelle, F. John, E. Caleb , Why do people believe COVID-19 conspiracy theories? Harvard Kennedy School Misinformation Review 1: (3) ((2020) ). doi:10.37016/mr-2020-015. |
[54] | K. Pickles, T. Copp, R.H. Dodd, E. Cvejic, H. Seale, M.S. Steffens , COVID-19 vaccine intentions in Australia, Lancet Infect Dis 21: (12) ((2021) ), 1627–1628. doi:10.1016/S1473-3099(21)00686-1. |
[55] | M.S. Zanchetta and I.M. Poureslami, Health literacy within the reality of immigrants’ culture and language, Canadian J Public Health 97: (3) ((2006) ), S26–S30. doi:10.1007/BF03405370. |
[56] | S. Park and R. Ahmed, Communication dimensions of healthcare engagement and patient health literacy for immigrant populations: A systematic review, Health Commun 38: (7) ((2021) ), 1–14. doi:10.1080/10410236.2021.2010328. |
[57] | M. Kutner, E. Greenburg, Y. Jin and C. Paulsen, The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy, US Department of Education, Washington, DC, National Center for Education Statistics, 2006. |
[58] | C.C. Cutilli and I.M. Bennett, Understanding the health literacy of America: Results of the National Assessment of Adult Literacy, Orthop Nurs 28: (1) ((2009) ), 27–32. doi:10.1097/01.NOR.0000345852.22122.d6. |
[59] | C.Y. Osborn, K. Cavanaugh, K.A. Wallston, S. Kripalani, T.A. Elasy, R.L. Rothman , Health literacy explains racial disparities in diabetes medication adherence, J Health Commun 16: (sup3) ((2011) ), 268–278doi:10.1080/10810730.2011.604388. |
[60] | L. Sa’u Lilo, E.-S. Tautolo and M. Smith, Health literacy, culture and Pacific peoples in Aotearoa, New Zealand: A review, Pacific Health 3: (0) ((2020) ), 1–10. doi:10.24135/pacifichealth.v3i0.4. |
[61] | R.M. Simpson, E. Knowles and A. O’Cathain, Health literacy levels of British adults: A cross-sectional survey using two domains of the Health Literacy Questionnaire (HLQ), BMC Public Health 20: (1) ((2020) ), 1819. doi:10.1186/s12889-020-09727-w. |
[62] | D.M. Muscat, J. Ayre, O. Mac, C. Batcup, E. Cvejic, K. Pickles , Psychological, social and financial impacts of COVID-19 on culturally and linguistically diverse communities in Sydney, Australia, BMJ Open 12: (5) ((2022) ), e058323. doi:10.1136/bmjopen-2021-058323. |
[63] | A. Elias, J. Ben, F. Mansouri and Y. Paradies, Racism and nationalism during and beyond the COVID-19 pandemic, Ethnic and Racial Studies 44: (5) ((2021) ), 783–793. doi:10.1080/01419870.2020.1851382. |
[64] | I. Piller, J. Zhang and J. Li, Linguistic diversity in a time of crisis: Language challenges of the COVID-19 pandemic, Multilingua 39: (5) ((2020) ), 503–515. doi:10.1515/multi-2020-0136. |
[65] | M. Civico, Covid-19 and language barriers. Working paper 21:4. REAL Research Group Economics, policy analysis and language, 2021, https://www.ulster.ac.uk/__data/assets/pdf_file/0010/931492/REAL21-4.pdf. |
[66] | S. Dalzell and G. Coote, Australia’s official COVID-19 health information translations left to become eight weeks out of date [Internet]. 2021. Available from: https://www.abc.net.au/news/2021-08-12/covid-19-information-weeks-out-of-date/100369794. Retrieved September 13, 2021. |
[67] | S. Dalzell, Government coronavirus messages left ‘nonsensical’ after being translated into other languages [Internet]. 2020. Available from: https://www.abc.net.au/news/2020-08-13/coronavirus-messages-translated-to-nonsense-in-other-languages/12550520. Retrieved August 10, 2021. |
[68] | L. Guadagno, Migrants and the COVID-19 Pandemic: An Initial Analysis International Organization for Migration, (2020) . |
[69] | I. Feinberg, Building a culture of health literacy during COVID-19, New Horizons in Adult Education & Human Resource Development 33: (2) ((2021) ), 60–64. doi:10.1002/nha3.20316. |
[70] | M. Arvanitis, L. Opsasnick, R. O’Conor, L.M. Curtis, C. Vuyyuru, J. Yoshino Benavente , Factors associated with COVID-19 vaccine trust and hesitancy among adults with chronic conditions, Prev Med Rep 24: ((2021) ), 101484. doi:10.1016/j.pmedr.2021.101484. |
[71] | J. Ayre, D.M. Muscat, O. Mac, C. Batcup, E. Cvejic, K. Pickles , Main COVID-19 information sources in a culturally and linguistically diverse community in Sydney, Australia: A cross-sectional survey, Patient Educ Couns 105: (8) ((2022) ), 2793–2800. doi:10.1016/j.pec.2022.03.028. |
[72] | D. Freeman, F. Waite, L. Rosebrock, A. Petit, C. Causier, A. East , Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England, Psychol Med 52: (2) ((2022) ), 251–263. doi:10.1017/S0033291720001890. |
[73] | S.W. Light, A. Pack, A. Vela, S.C. Bailey, A. Zuleta, R. O’Conor , Perceptions and motivating factors regarding COVID-19 vaccination in Latinx older adults in Chicago: A local, qualitative perspective, Patient Prefer Adherence 16: : ((2022) ), 2321–2333. |
[74] | J.-L. Kruger, M. Orlando, P. Peters, C. Liao and H. Sturgess, Assessing the Impact of Readability on Translation Quality and Productivity Macquarie University, (2022) . |
[75] | Office of Disease Prevention and Health Promotion. Health literacy online: A guide for simplifying the user experience [Internet]. 2016. Available from: https://health.gov/healthliteracyonline/. Retrieved September 29, 2022. |
[76] | R.J. Mullen, J. Duhig, A. Russell, L. Scarazzini, F. Lievano and M.S. Wolf, Best-practices for the design and development of prescription medication information: A systematic review, Patient Educ Couns 101: (8) ((2018) ), 1351–1367. doi:10.1016/j.pec.2018.03.012. |
[77] | F. Mastroianni, Y.-C. Chen, L. Vellar, E. Cvejic, J.K. Smith, K.J. McCaffery , Implementation of an organisation-wide health literacy approach to improve the understandability and actionability of patient information and education materials: A pre-post effectiveness study, Patient Educ Couns 102: (9) ((2019) ), 1656–1661. doi:10.1016/j.pec.2019.03.022. |
[78] | P. Schmid and C. Betsch, Effective strategies for rebutting science denialism in public discussions, Nat Hum Behav 3: (9) ((2019) ), 931–939. doi:10.1038/s41562-019-0632-4. |
[79] | J. Leask, S.J. Carlson, K. Attwell, K.K. Clark, J. Kaufman, C. Hughes , Communicating with patients and the public about COVID-19 vaccine safety: Recommendations from the Collaboration on Social Science and Immunisation, Med J Aust 215: (1) ((2021) ), 9–12. doi:10.5694/mja2.51136. |
[80] | B. Hyland-Wood, J. Gardner, J. Leask and U.K.H. Ecker, Toward effective government communication strategies in the era of COVID-19, Humanit and Soc Sciences Commun 8: (1) ((2021) ), 30. doi:10.1057/s41599-020-00701-w. |
[81] | R. West, S. Michie, G.J. Rubin and R. Amlôt, Applying principles of behaviour change to reduce SARS-CoV-2 transmission, Nat Hum Behav 4: (5) ((2020) ), 451–459. doi:10.1038/s41562-020-0887-9. |
[82] | D. Zachariah, D. Mouwad, D.M. Muscat, J. Ayre, D. Nutbeam and K.J. McCaffery, Addressing the health literacy needs and experiences of culturally and linguistically diverse populations in Australia during COVID-19: A research embedded participatory approach, J Health Commun 27: (7) ((2022) ), 1–11. doi:10.1080/10810730.2022.2118910. |
[83] | M.S. Kaper, J. Sixsmith, S.A. Reijneveld and A.F. de Winter, Outcomes and critical factors for successful implementation of organizational health literacy interventions: A scoping review, Int J Environ Res Public Health 18: (22) ((2021) ), 11906. doi:10.3390/ijerph182211906. |
[84] | N.D. Berkman, S.L. Sheridan, K.E. Donahue, D.J. Halpern, A. Viera, K. Crotty , Health literacy interventions and outcomes: An updated systematic review, Evid Rep Technol Assess (Full Rep) 199: : ((2011) ), 1–941. |
[85] | R. Nash, K. Patterson, A. Flittner, S. Elmer and R. Osborne, School-based health literacy programs for children (2–16 Years): An international review, J Sch Health 91: (8) ((2021) ), 632–649. doi:10.1111/josh.13054. |
[86] | C. Stormacq, J. Wosinski, E. Boillat and S. Van den Broucke, Effects of health literacy interventions on health-related outcomes in socioeconomically disadvantaged adults living in the community: A systematic review, JBI Evid Synth 18: (7) ((2020) ), 1389–1469. doi:10.11124/JBISRIR-D-18-00023. |
[87] | S. Nickel and O. von dem Knesebeck, Effectiveness of community-based health promotion interventions in urban areas: A systematic review, J Commun Health 45: (2) ((2019) ), 419–434. doi:10.1007/s10900-019-00733-7. |
[88] | L. Fernández-González and P. Bravo-Valenzuela, Effective interventions to improve the health literacy of cancer patients, Ecancermedicalscience 13: ((2019) ), 966. doi:10.3332/ecancer.2019.966. |
[89] | P. Nurash, K. Kasevayuth and U. Intarakamhang, Learning programmes and teaching techniques to enhance oral health literacy or patient-centred communication for healthcare providers: A systematic review, Eur J Dent Educ 24: (1) ((2020) ), 134–144. doi:10.1111/eje.12477. |
[90] | C.K. Bak, J.Ø. Krammer, K. Dadaczynski, O. Orkan, J. von Seelen, C. Prinds , Digital health literacy and information-seeking behavior among university college students during the COVID-19 pandemic: A cross-sectional study from Denmark, Int J Environ Res Public Health 19: (6) ((2022) ), 3676. doi:10.3390/ijerph19063676. |
[91] | X. Chen, M. Li and G.L. Kreps, Double burden of COVID-19 knowledge deficit: Low health literacy and high information avoidance, BMC Res Notes 15: (1) ((2022) ), 27. doi:10.1186/s13104-022-05913-8. |
[92] | C. Bonner, C. Batcup, J. Ayre, K. Pickles, E. Cvejic, T. Copp , Behavioural barriers to COVID-19 testing in Australia: Two national surveys to identify barriers and estimate prevalence by health literacy level. medRxiv [preprint], 2021. doi:10.1101/2021.08.26.21262649. |
[93] | Office for National Statistics. Updating ethnic contrasts in deaths involving the coronavirus (COVID-19), England: 10 January 2022 to 16 February 2022 [Internet]. 2022. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/updatingethniccontrastsindeathsinvolvingthecoronaviruscovid19englandandwales/10january2022to16february2022. Retrieved September 29, 2022. |




